- 1Department of Psychiatry, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 2Department of Psychiatry, College Medical and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 3College of Health Sciences, Woldia University, Woldia, Ethiopia
Background: People who have encountered adverse childhood experiences (ACEs) are predisposed to developing schizophrenia, experiencing exacerbated symptoms, and facing an elevated risk of disease relapse. It is imperative to evaluate the prevalence of ACEs to comprehend the specific attributes of this condition and enable the implementation of suitable interventions.
Aims: The aim of this study was to assess the prevalence of ACEs and its determinants among people with schizophrenia and the patient attendants in Bahir Dar, Ethiopia.
Method: A comparative cross-sectional study was carried out at the Comprehensive Specialized Hospitals in Bahir Dar, Ethiopia, from April 26 to June 10, 2023. A total of 291 individuals with schizophrenia and 293 individuals from the patient attendants were selected using a systematic random sampling method. A proportional odds model ordinal logistic regression analysis was used to identify the factors associated with ACEs.
Results: The occurrence of at least one ACE among individuals diagnosed with schizophrenia was 69.4%, while patient attendants had a 46.8%, as indicated by the Chi-square test, which showed a significant difference at p <0.05. The study findings indicated that individuals with schizophrenia who have encountered four or more ACEs are more inclined to have lower educational attainment (AOR: 4.69 [1.94 - 11.61]), low resilient coping mechanisms (AOR: 2.07 [1.11 - 3.90]), and poor social support (AOR: 3.93 [2.13 - 7.32]). Conversely, factors such as rural residency, illiteracy, and heightened attachment-related anxiety were found to be notably associated with the patient attendants.
Conclusion: In this study, the substantial prevalence of ACEs emphasized the necessity for ACE screening and the implementation of evidence-based interventions to address and alleviate the overall burden of ACEs.
Introduction
ACEs are events of a potentially traumatic nature that take place prior to reaching 18 years of age, and have been connected to the primary causes of morbidity and mortality in adulthood (1, 2). These ACEs encompass occurrences involving physical, psychological, and sexual abuse, as well as physical and mental neglect, and dysfunction within the family (3). Individuals with schizophrenia as well as those with other non-psychiatric diseases with severe ACEs, displayed higher levels of comorbidity, necessitated increased medication usage, and required the involvement of a care coordinator compared to individuals with moderate or no ACEs (4–6).
The impact of ACEs extends to diminished well-being, factors influencing quality of life, and substantial impediments in psycho-social functioning that emerge early on in life (7–10). ACEs is associated with unfavorable outcomes, and one possible mechanism through which it can influence results is by causing delays in treatment and a diminished response to antipsychotic interventions (11, 12).
Globally, the prevalence of ACEs among the general population varies from 25% to 85% for individuals with at least one ACE, and from 5.93% to 34.2% for those with four or more ACEs (13–23), while in Africa, percentages range from 58.3% to 72.2% for at least one ACE, and from 14.4% to 39% for three or more ACEs (24, 25). In comparison to the general population, individuals with schizophrenia encountered two to three times more ACEs during childhood (26–30).The occurrence of ACEs among individuals with schizophrenia ranged from 47.2% to 90% for at least one ACE, and from 25% to 52% for four or more ACEs (6, 26–28, 30–32). Although each ACE has detrimental effects on an individual’s health, behavior, and psychological growth, exposure to multiple adverse experiences results in a significantly more damaging impact (33, 34). This implies a dose-response connection, where the risk of adverse effects on physical and mental health exponentially rises with additional ACEs (33, 35). Individuals with schizophrenia who had multiple ACEs histories exhibited more severe symptoms and unfavorable clinical results (4, 36–38). Those with higher levels of ACEs tended to have lower levels of social support, which exhibited a positive correlation with suicide in individuals with schizophrenia, and decreased coping abilities (39–41).
Assessing one’s history of ACEs in adulthood can be advantageous, as it may mitigate the negative repercussions of ACEs on mental health and resilience, and can aid families in breaking the cycle of adversity, subsequently reducing risks and enhancing treatment results (42–46).
Nonetheless, there exists limited evidence regarding ACEs among individuals with schizophrenia in Ethiopia. Therefore, the objective of this research was to ascertain the prevalence of ACEs and their associated factors among individuals with schizophrenia in comparison to the patient attendants. This endeavor could provide valuable insights for healthcare professionals, researchers, and stakeholders interested in working this issue.
Method
Study design and setting
A comparative cross-sectional study was conducted from April 26 to June 10, 2023, at Comprehensive Specialized Hospitals in Bahir Dar, Ethiopia.
Participants
The target participants comprised all individuals with schizophrenia who were hospitalized and receiving outpatient follow-up care, as well as patient attendants (often relatives of the patient) seeking medical treatment from various departments in Hospitals. The study participants included people with schizophrenia who were on follow up and the patient attendants present during the data collection period.
Inclusion and exclusion criteria
Individuals aged 18 and above with schizophrenia who on follow up, and the patient attendants from medical, surgical, gynecology, obstetric, and pediatric sites in both hospitals (not including psychiatry unit patient relatives)were included in the study. Those who were severely ill or mentally incapacitated were excluded from the study during the data collection period. Furthermore, those who had low cognitive scores in individuals with schizophrenia were excluded using a Mini-Mental State Examination(MMSE) assessment with a total score of less than or equal to 24 on a commonly used cutoff score to define impairment (47). Among the patient attendants, the existence of symptoms of mental illness was assessed using the 18-item Brief Psychiatry Rating Scale (BPRS). Excluded from the study were those who received a BPRS score of 30 or higher, which is considered a baseline for mild mental disorder symptoms (48).
Sample size estimation and sampling procedure
A formula that is quite general and applies to cross-sectional, case-control, and cohort studies for comparison studies between two proportions (equal sample sizes) was used to determine the sample size (49).
To test the hypothesis P1=P2 versus H1: P1≠P2, for detecting a specific effect: Sample size: n1 = n2; equal ratio: 1:1 = 1; the number of participants required in the two populations.
Effect size: the prevalence of at least one ACE, P1 (cases) (94%), and P2 (healthy participants) (87%), were taken from a previous study (50). P = average proportion exposed (P1 + P2)/2, q = 1-p. Significance Z alpha = power at 95%; statistical power Z beta = power at 80%. Adding 10% of the non-respondent rates, a total of 604 participants were sampled, which means the sample size for each group were 302 in the study.
Then, the final sample size was proportionally allocated to TGCSH and FHCSH based on their anticipated monthly case flow (Figure 1). A systematic random sampling method was employed, with the patient card list serving as the sampling frame to select the participants. After the sampling interval (K) was determined the first participant was selected through a lottery method, with subsequent participants chosen by adding the calculated K value within each group. In cases where multiple individuals were present in the patient attendants, one was randomly selected.
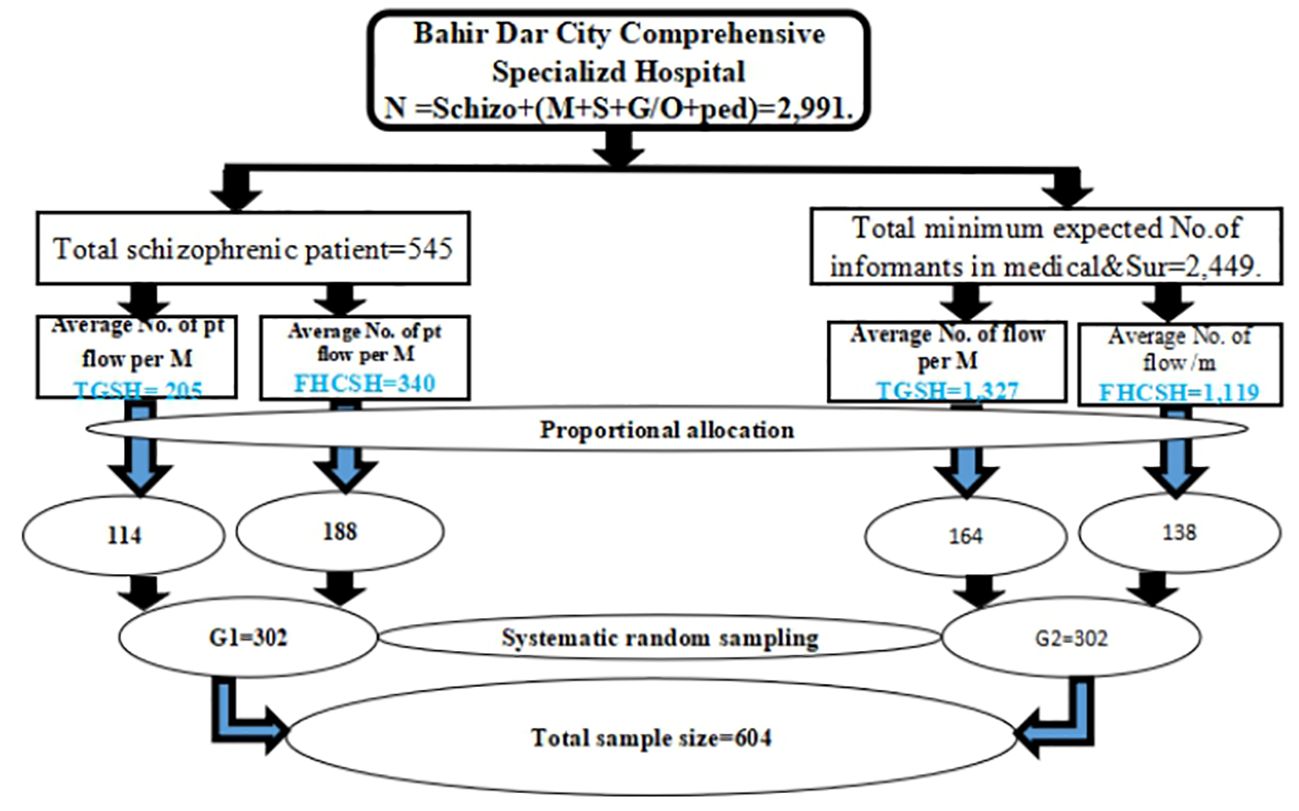
Figure 1 Sampling procedure of selecting study samples from TGSH and FHCSH Bahir Dar, Ethiopia, 2023.
Study variables
The study variables included the dependent variable of ACEs (0, 1, 2 and 3, greater than or equal 4). Sociodemographic variables encompassed sex, age, residency, religion, educational status, occupational status, marital status, and ethnicity. Psychosocial factors such as social support, adult attachment, coping strategy, substance-related factors (including alcohol use, khat use, tobacco use), and Clinical factors like suicide behavior and somatic symptoms were also considered.
Data collection and measurements tool
Structured questionnaire were employed in conducting face-to-face interviews for data collection purposes. The data were acquired by a team of six individuals and supervised by two professionals holding a Bachelor of Science in Psychiatry in each designated study area. The Adverse Childhood Experiences - questionnaire (ACEs-Q), a standardized tool consisting of ten items, was utilized to evaluate the history of ACEs (34). ACEs-Q represents various symptoms of ACEs such as emotional abuse, physical abuse, sexual abuse, emotional neglect, physical neglect, domestic violence, parental separation or death, household substance abuse, household mental illness, and incarcerated household members.
Initially, each ACE was assessed individually. Individuals were classified as exposed to ACEs if they responded affirmatively to one or more questions within a specific category; subsequently, an ACEs score was calculated, assigning one point for each positive response. This scoring system yielded total scores ranging from 0 (no ACEs) to 10 points (exposed to all ACEs). The number of ACEs was grouped into categories of 0, 1, 2 to 3, greater than or equal to 4 ACEs; this was created based on previous studies (34, 51, 52). The ACEs-Q scale has demonstrated strong internal consistency (α=0.86).
Experiences in close relationships
Attachment security in an adult population was evaluated using the Experiences in Close Relationships- Relationship Structures (ECR-RS) questionnaire general form (53). ECR-RS general have two scores, one for attachment-related avoidance and the other for attachment-related anxiety. Mean scores were utilized to establish statistical cut-off points for defining high and low anxious or avoidant attachment categories. Scores below the mean on both subscales indicated low anxious or avoidant attachment, while scores equal to or above the mean signified high anxious or avoidant attachment. The ECR-RS scale exhibited excellent internal consistency (α=0.947). The Brief Resilient Coping Scale (BRCS) was applied to gauge individuals’ tendencies to cope effectively with stress. Scores falling within the ranges of four to thirteen, fourteen to sixteen, and seventeen to twenty were categorized as representing low, medium, and high resilient coping, respectively (54). The BRCS, a 4-item measure, displayed good internal consistency (α=0.812). Social support levels were assessed using the Oslo Social Support Scale (OSSS-3), with scores ranging from 3 to 14. Participants were classified as having poor support, intermediate support, or strong social support based on scores of 3 to 8, 9 to 11, and 12 to 14, respectively (55). The OSSS-3 demonstrated acceptable internal consistency (α=0.787).
The assessment of alcohol use extent was carried out utilizing the Alcohol Use Disorder Identification Test (AUDIT) developed by the World Health Organization (WHO). The AUDIT serves as a screening tool to evaluate alcohol use severity levels, categorizing individuals into “no alcohol use,” “social use,” “harmful drinking,” “hazardous drinking,” and “ probable alcohol dependency” in increasing order of severity dependence (56). In the present investigation, the AUDIT exhibited acceptable internal consistency, supported by a Cronbach alpha value of 0.718.Suicide behaviors were measured through the 4-item Suicide Behaviors Questionnaire-Revised (SBQ-R), with individuals scoring seven or more being identified as displaying suicidal behaviors (57). Additionally, the Somatic Symptom Scale-8 (SSS-8) was utilized as a concise 8-item version of the Patient Health Questionnaire-15 (PHQ-15).
The severity categories of SSS-8 were determined based on percentile ranks: ranging from no to minimal (0-3 points), low (4-7 points), medium (8-11 points), high (12-15 points), to very high (16-32 points) somatic symptom burden (58). The SSS-8 is a reliable and valid self-report measure of somatic symptom burden (59). The internal consistency was deemed acceptable with a reliability coefficient of α=0.806.
Data quality assurance
Data quality assurance was ensured through a meticulous process. Initially, the questionnaire was developed in English, translated into Amharic, and back-translated into English by various language experts to enhance the tool’s reliability and comprehensibility. Subsequently, the tools underwent pretesting with a 5% (31) sample size at FHCSH. Following feedback from the pretest, the final version of the questionnaire was refined. Rigorous training was provided to both data collectors and supervisors, and daily checks on data collection were conducted by the principal investigator and supervisors.
Data processing and analysis
The data underwent thorough scrutiny for completeness before being exported to Statistical Package for Social Sciences (SPSS) software version 26 for coding and analysis. Utilizing descriptive and inferential statistics, the analysis aimed to describe the findings and explore associations between dependent and independent variables through proportional odds model ordinal logistic regression. Variables with a p-value < 0.25 were included in the final model, which underwent assessments for fitness, goodness of fit and parallel lines. Statistical significance was established at a p-value < 0.05, with the strength of associations estimated through odds ratios with a 95% confidence interval.
Ethical consideration and consent to participate
Ethical approval was granted by Bahir Dar University College of Medical and Health Science Institutional Review Board (IRB) under protocol number 781/2023, in adherence to local regulations and institutional guidelines. The study adhered to the principles of the Helsinki Declaration on Medical Research Ethics (60). Participants provided written informed consent, and permission was obtained from TGCSH and FHCSH. Participants were assured of their right to withdraw at any time, and information confidentiality and anonymity were strictly maintained.
Results
Sociodemographic profile of study participants
In this study, 302 people with schizophrenia and 302 from the patient attendants participated, yielding response rates of 96.35% and 97.02% respectively. Among people with schizophrenia, significant portions were single 103 (35.4%) and aged between 18 and 24 years 115 (39.5%). The majority of people with schizophrenia were female 147 (50.5%) and urban residents 161 (55.3%). In comparison, the patient attendants had a higher proportion of married individuals 179 (60.1%), males 148 (50.5%), and urban residents 151 (51.5%). A statistically significant chi-square test was observed for occupation and marital status, while gender, age, residency, religion, education, and ethnicity did not exhibit significant differences (Table 1).
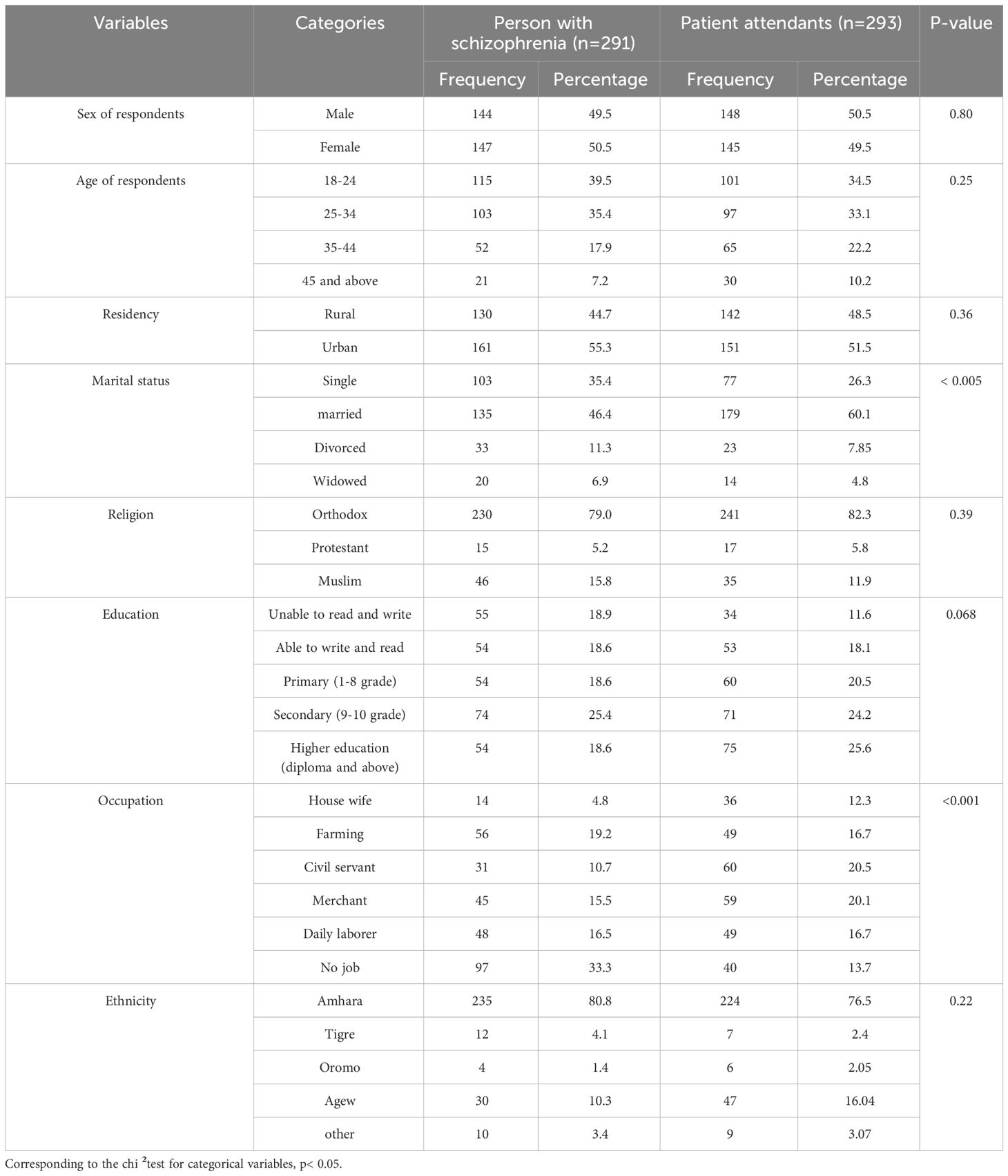
Table 1 Sociodemographic information among people with schizophrenia and patient attendant participants included in the study at TGCSH and FHCSH, Bahir Dar, Ethiopia, in 2023.
Magnitude of ACEs among people with schizophrenia and the patient attendants
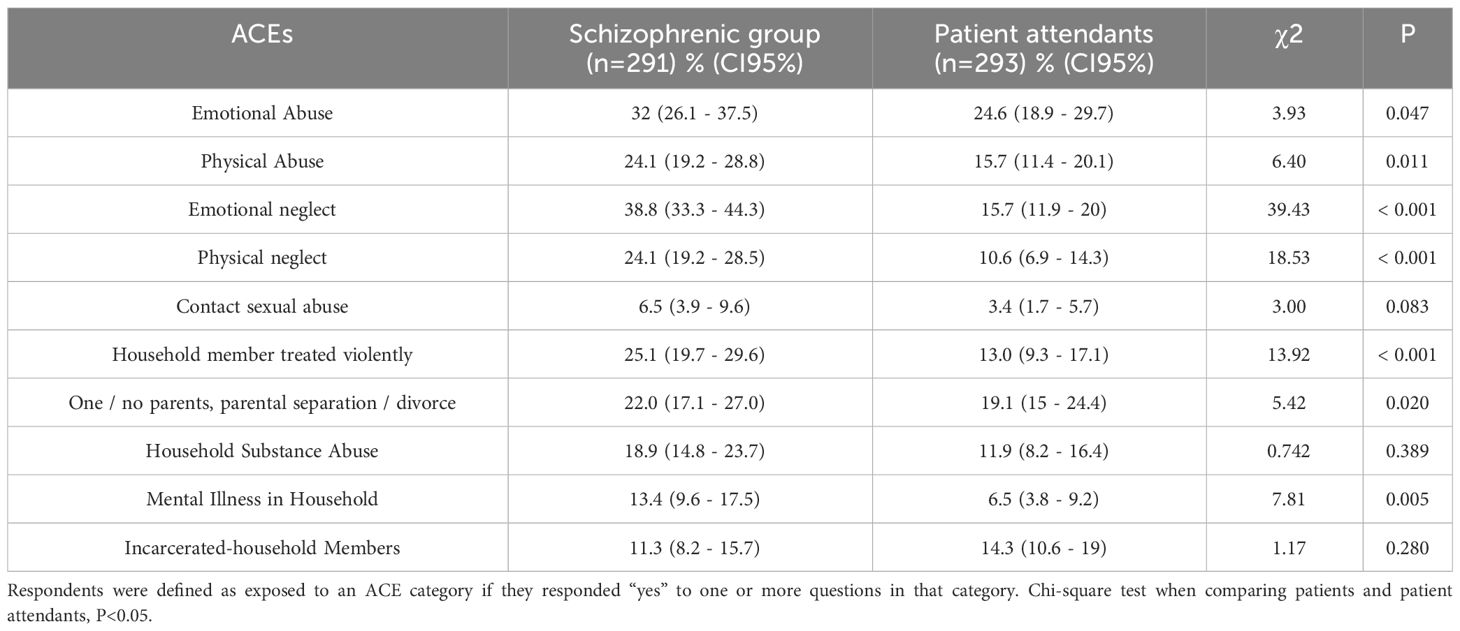
In exploring the nature of ACEs, prevalent ACEs in individuals with schizophrenia included emotional neglect at 38% and emotional abuse at 32%. Conversely, emotional abuse was reported in 24.6% of the patient attendants, while 19.1% experienced situations like having one or no parents, parental separation, or divorce. Sexual abuse emerged as the least common ACEs in both groups. Except for a history of family member incarceration, all other ACEs types were more frequent in individuals with schizophrenia. Statistical analysis through the Chi-square test revealed that household substance abuse, contact sexual abuse, and family member imprisonment did not display significant differences between the two groups (Table 2).
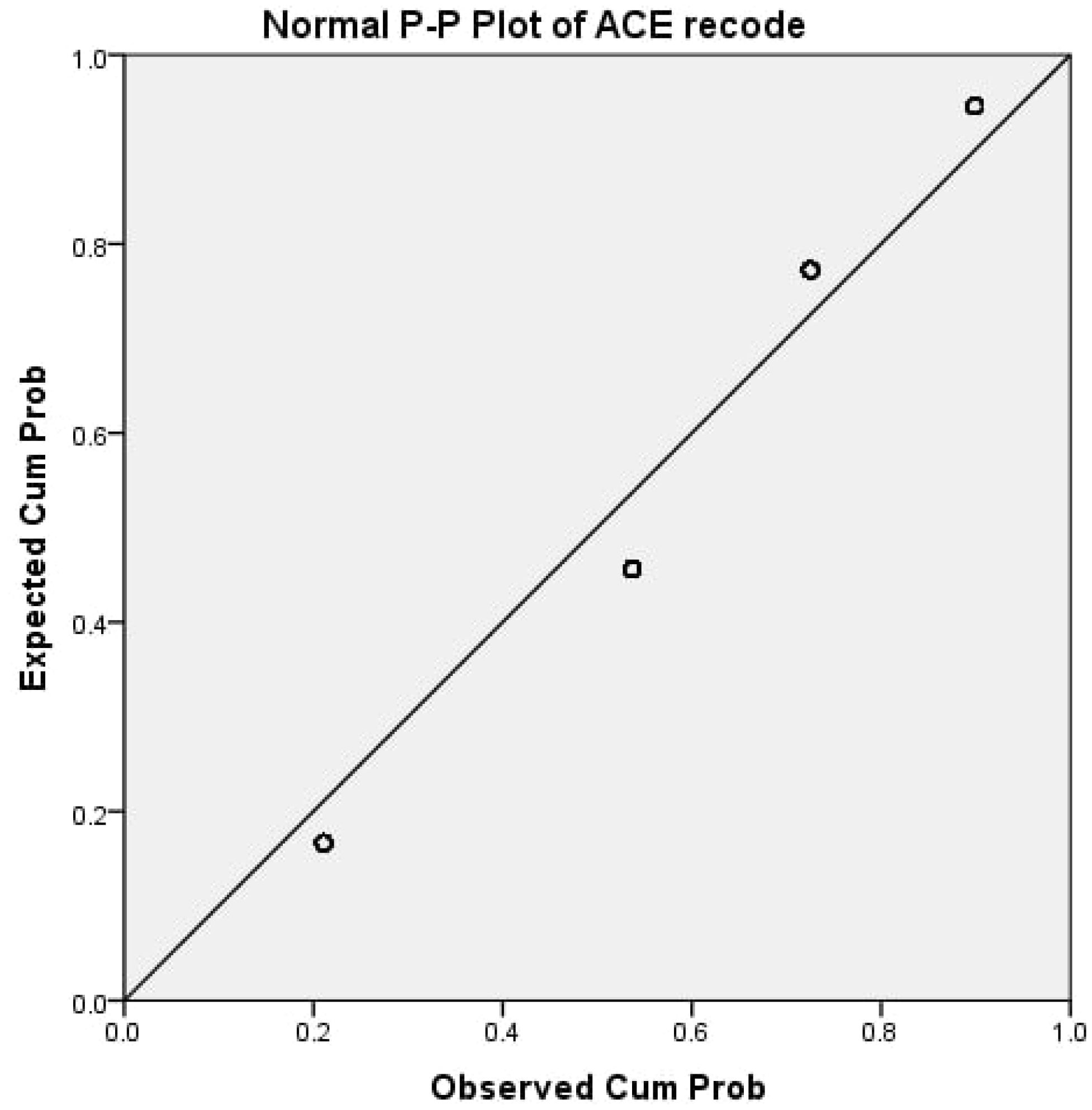
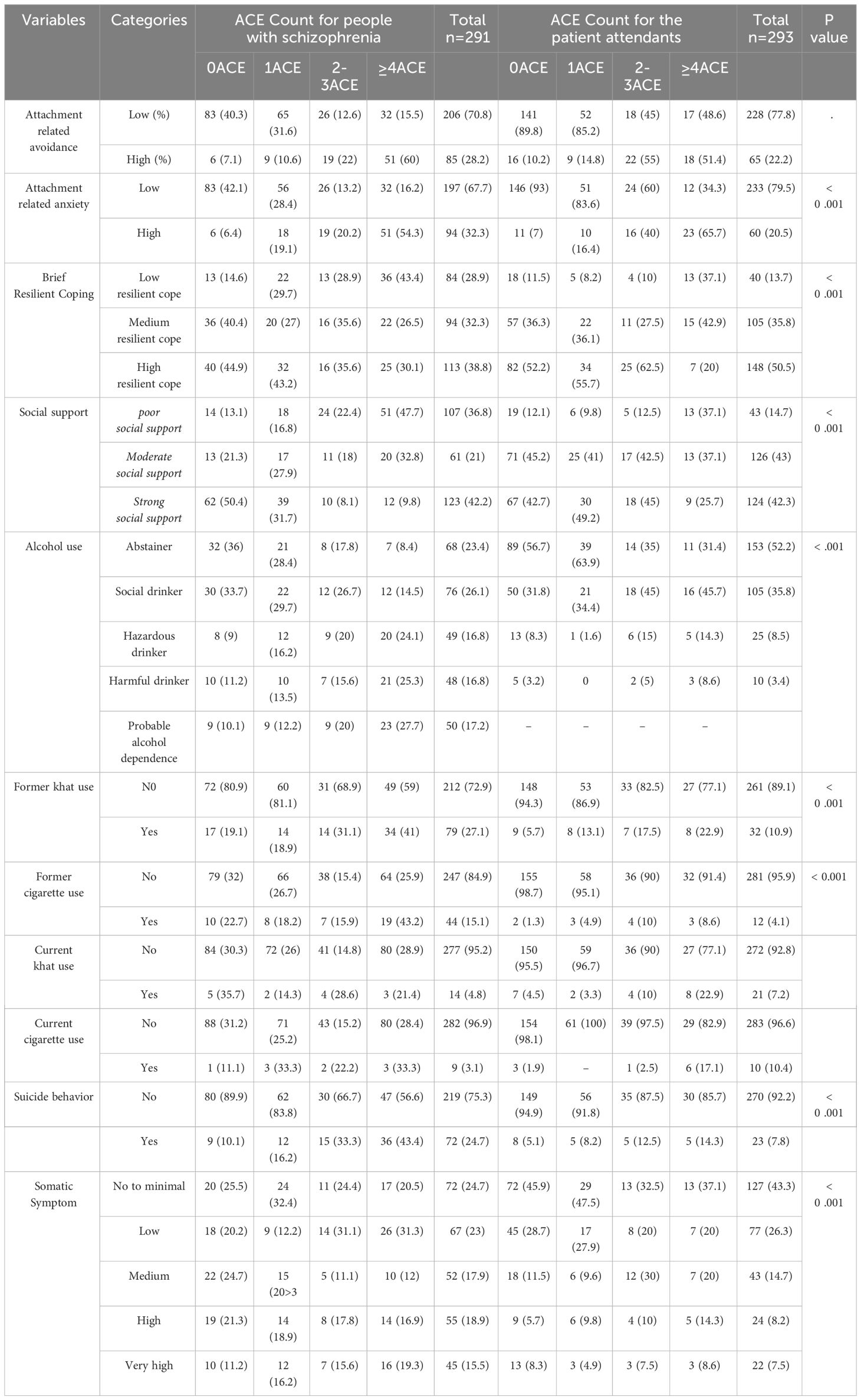
A p-p plot illustrates how the ACEs scores were distributed among all participants (Figure 2). Approximately 30.6% of individuals with schizophrenia and 53.2% of the patient attendants did not report any ACEs. On the other hand, 28.5% of those with schizophrenia and 11.9% of the patient attendants encountered four or more ACEs. Moreover, the prevalence of at least one ACE was notably higher among individuals with schizophrenia, with 69.4% reporting ACEs compared to 46.8% in the patient attendants. The statistical significance of this difference was confirmed through the Chi-square test (p < 0.05). When examining the distribution of ACEs scores between the schizophrenia and patient attendants groups, no statistically significant variance was found for individuals with only one type of ACEs or two to three ACEs (Figure 3).
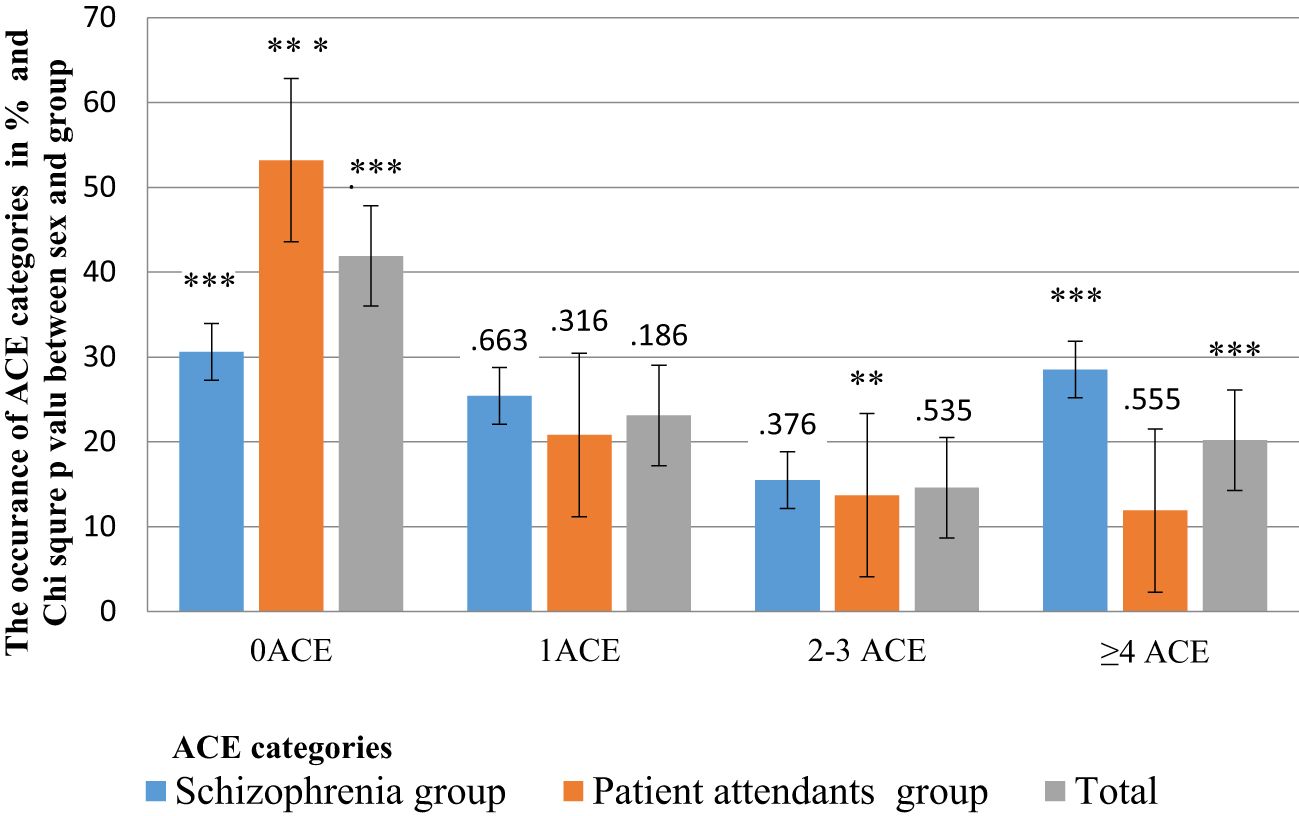
Figure 3 Magnitude of ACEs among people with schizophrenia and the patient attendants. Asterisks denote statistically significant “p” according to the scheme: *p ≤ 0.1, **p ≤ 0.05, ***p ≤ 0.01.
Health-related risk factors
A considerable proportion, 94 (32.3%) of individuals with schizophrenia and 60 (20.5%) of the patient attendants, exhibited high attachment-related anxiety. Similarly, poor social support was prevalent in 107 (36.8%) of individuals with schizophrenia compared to 43 (14.7%) in the patient attendants. In terms of resilient coping skills, 84 (28.9%) of individuals with schizophrenia and 40 (13.7%) of the patient attendants displayed low levels of resilience (Table 3).
Factors associated with ACEs
Before examining the impact of each independent variable in the model, it is needed to ascertain whether the model enhances our capability to forecast the outcome. The significant chi-square value (p<0.05) suggests a significant enhancement of the Final model compared to the baseline intercept-only model, signifying that the model provides more valuable insights than mere random predictions based on marginal probabilities for the outcome categories (Table 4).
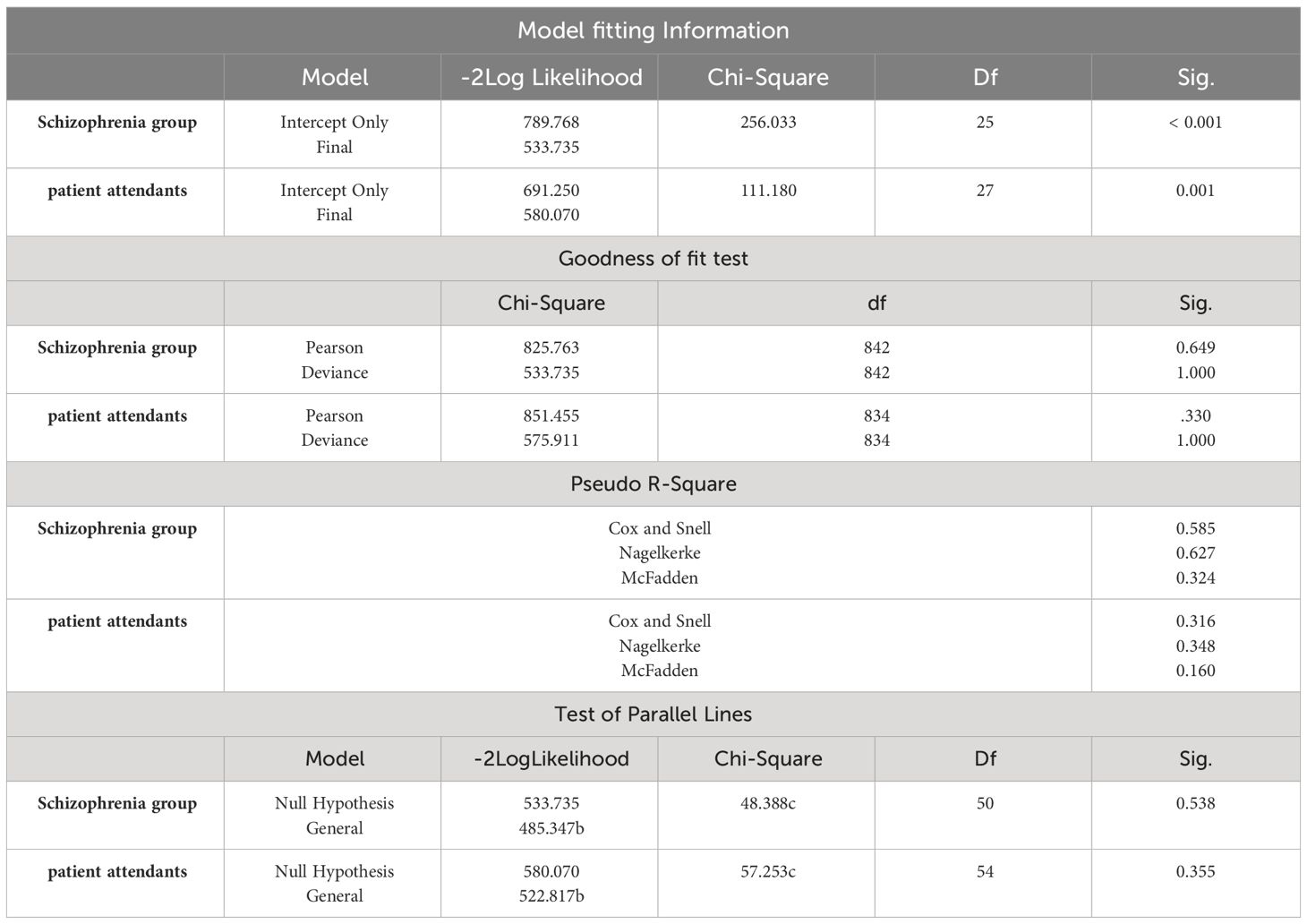
Table 4 Showing the Model fitting Information, Goodness of fit Test, Pseudo R-Square, and Test of Parallel Lines of both groups.
Evaluation of the fitted model
The purpose of these statistics is to determine if the fitted model and the observed data are consistent. It starts from the null hypothesis that the fit is good. If we do not reject this hypothesis (i.e., if the p value is large), we can conclude that the data and the model predictions are similar and have a good model. The results of this analysis show that the model does fit very well for both groups (p > 0.05).Additionally, Nagelkerke’s R was 0.627 for individuals with schizophrenia and 0.348 for the patient attendants, suggesting that 62.7% and 34.8% of the variations in outcome variables were elucidated by the model’s independent variables, while the residual 37.3% and 65.2% were attributed to unexplained factors and errors. On the other hand, McFadden’s pseudo-R2 was 0.324 for people with schizophrenia and 0.16 for the patient attendants, suggesting that 32.4% and 16% of the variations in outcome variables were explained by the model’s explanatory variables, while the remaining 67.6% and 84% were attributed to unexplained factors and errors (Tables 4).
Evaluation of the of proportional odds model
The evaluation involves the use of the parallel line test to determine conformity with the proportional odds model assumption. If the general model exhibits a substantially superior fit with the data compared to the ordinal (proportional odds) model (i.e., if p<0.05), the assumption of proportional odds is refuted. Conversely, the parallel line test for both group (Table 4) displayed a non-significant value (p-value>0.05), leading to the acceptance of the proportional odds assumption.
In the bivariable ordinal logistic analysis, variables such as Age, occupation, prior history of tobacco use, and marital status did not show statistical significance in either group. The multivariable ordinal logistic regression analysis among individuals with schizophrenia (Table 5) showed that the first two lower education categories (unable to read and write and able to read and write), attachment-related anxiety, low resilience coping, low and moderate social support, alcohol abstention, social drinking, and suicidal tendencies exhibited statistical significance in association with ACEs.
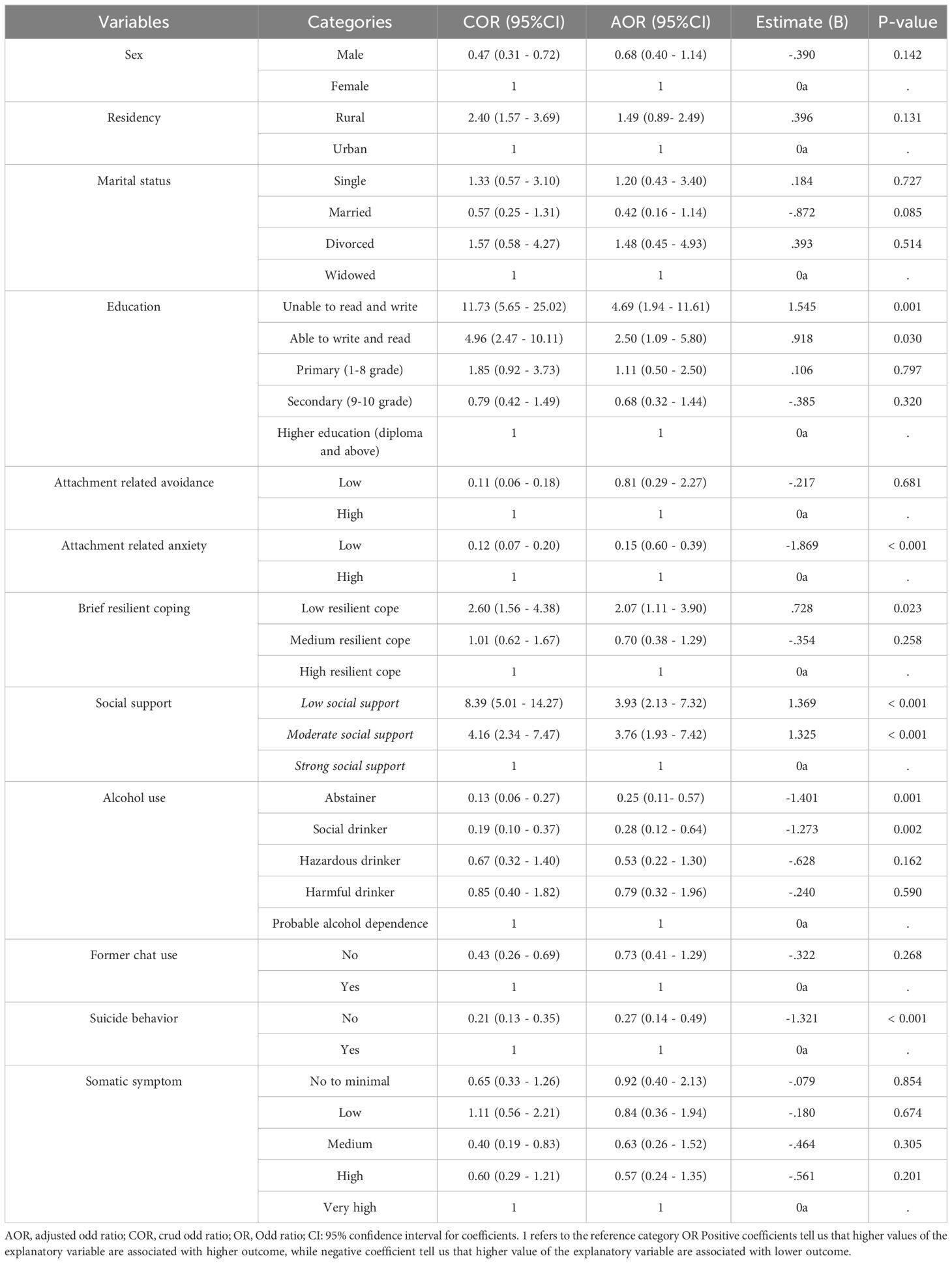
Table 5 Bivariable and multivariable ordinal logistic regression analysis of ACEs among people with schizophrenia, Bahir Dar, Amhara, Ethiopia, 2023.
The likelihood of experiencing four or more ACEs was 4.7 times (AOR, 95% CI: 1.94 -11.61) and 2.5 times (AOR, 95% CI: 1.09 - 5.79) higher among people with schizophrenia who are unable to read and write, and able to read and write, respectively, compared to those with higher education. The probability of having four or more ACEs was 84.6% lower (AOR, 95% CI: 0.59–0.39) among people with schizophrenia exhibiting low attachment-related anxiety compared to those with high attachment-related anxiety. The probability of experiencing four or more ACEs among individuals with schizophrenia with poor social support was 3.93 times higher (AOR, 95% CI: 2.13 - 7.32) than those with strong social support.
The multivariable ordinal logistic regression analysis conducted in the patient attendants (Table 6) revealed significant associations between being unable to read and write, attachment-related anxiety, rural residency, and ACEs. The analysis indicated that rural residents in the patient attendants were 1.73 times more likely to report four or more ACEs compared to urban residents (AOR, 95% CI: 1.05–2.85).
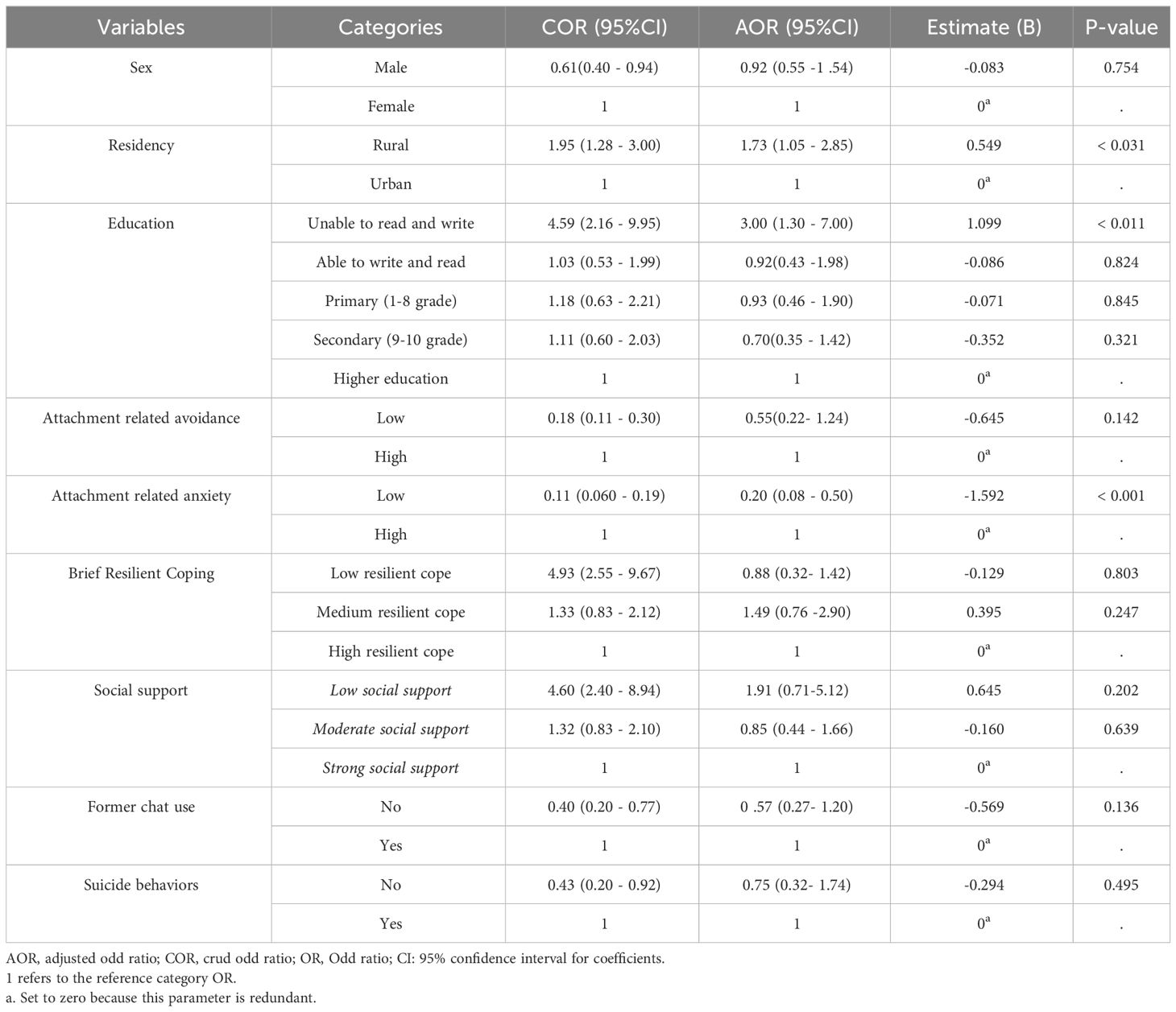
Table 6 Bivariable and multivariable ordinal logistic regression analysis of ACEs among patient attendants, Bahir Dar, Amhara, Ethiopia, 2023.
Discussions
This study compared a group of 293 healthy controls of the patient attendants with 291 individuals diagnosed with schizophrenia to assess the prevalence of ACEs. In the current study, results showed that 46.8% of the patient attendants and 69.4% of individuals with schizophrenia reported at least one ACE, lower than rates in South Africa and Argentina (94% and 87% respectively) (50, 61). This discrepancy may be due to variations in measurement tools such as the Childhood Trauma Questionnaire (CTQ) used in previous studies.
People with schizophrenia had higher rates of at least one ACE and four or more ACEs compared to the patient attendants group (69.4% and 28.5% vs. 46.8% and 11.9% respectively). Notably, the study found that schizophrenia patients were over twice as likely to report four or more ACEs compared to patient attendants participants. These results align with previous studies indicating a higher prevalence of ACEs among individuals with schizophrenia, supporting the trauma multiplicity theory. The dose-response model suggests that accumulating multiple ACEs increases the risk of developing schizophrenia (62–64).
While ACEs are doubtless associated with poorer mental health, there are also plenty of healthy individuals with several ACEs but without any mental problems. The reason why all people who had ACEs do not develop schizophrenia indicates that schizophrenia is considered to be a biological (65–67). “A Neural Diathesis-Stress Model of Schizophrenia” Reiterate the commonly held belief that stressors can exacerbate symptoms but do not constitute causative factors. Cite standard research suggesting heightened susceptibility to stressors is linked to schizophrenia vulnerability. ACEs are considered relevant only to the extent that they exacerbate premorbid behavioral dysfunction or, at most, accelerate the onset of the initial clinical episode (67). The reason why some individuals without ACEs also have schizophrenia is that there exists a model that suggests that factors such as ACEs are not the only ones that determine a person’s susceptibility to symptoms of schizophrenia. The first is the multiple etiological hypotheses of schizophrenia that are in use today (68). Our intention was related to the models that suggest examining with an open mind and conducting appropriate research to determine whether adverse childhood events could be a contributing factor, either alone or in combination with the effects of genetic risk or prenatal factors (69).
In terms of health-related risk factors, the study revealed that individuals with schizophrenia and low social support had nearly four times higher odds of reporting four or more ACEs compared to those with strong social support (AOR = 3.93, 95% CI: 2.13 - 7.32). Additionally, individuals with medium social support had 3.76 times higher odds of experiencing four or more ACEs. This underscores the association between low social support and ACEs among individuals with schizophrenia, highlighting the potential benefits of social support interventions in preventing psychosis development in individuals with a history of child maltreatment (70).
Suicidal behaviors in people with schizophrenia have been linked to a history of multiple ACEs, a connection not observed in the patient attendants. Individuals with schizophrenia who exhibited suicidal behaviors were 3.75 times more likely to report four or more ACEs compared to those without such behaviors, a correlation also noted in previous research (27, 71). These chronically ACEs may impact the hypothalamic pituitary adrenal axis, leading to brain changes that increase susceptibility to stress in adulthood (26).
In the context of schizophrenia, people with low resilient coping skills are 2.07 times more likely to have four or more ACEs compared to those with high resilient coping skills, aligning with findings that childhood emotional and sexual abuse are linked to passive and avoidance coping in those with psychotic disorders (41).
Among people with schizophrenia, the odds of reporting four or more ACEs were 75% lower for alcohol abstainers (AOR = 0.25, 95% CI: 0.11 - 57) and 72% lower for social drinkers (AOR = 0.28, 95% CI: 0.12 - 0.64) when compared to those with probable alcohol dependence. This difference could be attributed to ACEs heightening the risk of psychosis development by hindering the maturation of adaptive emotion regulation mechanisms and fostering maladaptive coping strategies (40).
People with schizophrenia experiencing low attachment-related anxiety are 85% (AOR = 0.15, 95% CI: 0.59–0.39) less likely to have four or more ACEs than those with high attachment-related anxiety, consistent with evidence suggesting that disrupted attachment plays a role in connecting childhood trauma to adult psychotic symptoms (72, 73). Regarding education, individuals with less than primary school education showed a notable increase in the likelihood of having four or more ACEs, while those with primary or high school education did not exhibit a significant rise compared to those with higher education, in line with research findings (74).
Strengths and limitations
The study has several strengths. First, the data were collected by mental health professionals proficient in clinical interviews, enhancing data reliability in a cost-effective manner. Second, we approached ACEs as an ordinal outcome variable, enabling an assessment of category frequency between population groups. The inference of ACEs prevalence in individuals with schizophrenia and the patient attendants depends on observing each category, rather than just the presence or absence of ACEs. This method also reveals the correlation between ACEs and the independent variable as ACEs increase exponentially, ranging from low to high. Compared to multinomial logistic regression or binary logistic regression, this approach reduces information loss between categories, affecting the drawn conclusions. However, limitations of the study include the retrospective data collection method, which introduces risks of recall bias, and the potential influence of defense mechanisms on recollection was not accounted for. The data collection process was interviewer administered and focused on sensitive topics, possibly prompting respondents to provide socially desirable responses. The use of patient attendants as control might not representative of the general population because it might inflate the rate of reported ACEs. The other thing, we did not adjust the significance value for multiple testing and that certain tests would therefore not survive a stricter alpha criterion. In the long run, we acknowledge that the study’s shortcoming was that we did not examine the relationship between ACEs and clinical characteristics such as the amount of medications taken, the length of treatment, and the type or severity of symptoms.
Conclusion and recommendation
ACEs, although reported by the patient attendants, are depicted as being more abundant, widespread, and significantly associated with a higher number of health-related risk factors in people with schizophrenia. Recognizing the multiplicity and interconnectedness of these factors could prove beneficial for psycho-social interventions. Further research is warranted to explore which relational and individual protective variables contribute to the resilience exhibited by some adults who have faced ACEs without developing psychopathology. The extensive correlation between ACEs and health-related risk factors underscores the critical importance of primary prevention strategies to mitigate the occurrence of ACEs.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Bahir Dar University College of Medical and Health Science Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BA: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. TBel: Conceptualization, Data curation, Investigation, Methodology, Resources, Software, Supervision, Visualization, Writing – review & editing. RD: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Supervision, Visualization, Writing – review & editing, Writing – original draft. TBet: Conceptualization, Formal analysis, Investigation, Writing – review & editing. SM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was funded by Bahir Dar University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Glossary

References
1. Forty L. How early childhood events impact upon adult health. In: A Prescription for Healthy Living. Cardiff, United Kingdom: Elsevier (2021). p. 17–29.
2. Merrick MT, Ford DC, Ports KA, Guinn AS, Chen J, Klevens J, et al. Vital signs: Estimated proportion of adult health problems attributable to adverse childhood experiences and implications for prevention—25 States, 2015–2017. Morbidity Mortality Weekly Rep. (2019) 68:999. doi: 10.15585/mmwr.mm6844e1
3. Schulz A-C, Kasinger C, Beutel M, Fegert JM, Clemens V, Brähler E. Adverse childhood experiences growing up in East or West Germany or abroad. Front Psychiatry. (2022) 13. doi: 10.3389/fpsyt.2022.908668
4. Yousef AM, Mohamed AE, Eldeeb SM, Mahdy RS. Prevalence and clinical implication of adverse childhood experiences and their association with substance use disorder among patients with schizophrenia. Egyptian J Neurol Psychiatry Neurosur. (2022) 58:4. doi: 10.1186/s41983-021-00441-x
5. Koball AM, Rasmussen C, Olson-Dorff D, Klevan J, Ramirez L, Domoff SE. The relationship between adverse childhood experiences, healthcare utilization, cost of care and medical comorbidities. Child Abuse Neglect. (2019) 90:120–6. doi: 10.1016/j.chiabu.2019.01.021
6. Yousef AM, Mohamed AE, Eldeeb SM, Mahdy RS. Prevalence and clinical implication of adverse childhood experiences and their association with substance use disorder among patients with schizophrenia. Egyptian J Neurol Psychiatry Neurosur. (2022) 58:1–11. doi: 10.1186/s41983-021-00441-x
7. Nurius PS, Green S, Logan-Greene P, Borja S. Life course pathways of adverse childhood experiences toward adult psychological well-being: A stress process analysis. Child Abuse neglect. (2015) 45:143–53. doi: 10.1016/j.chiabu.2015.03.008
8. Narayan AJ, Kalstabakken AW, Labella MH, Nerenberg LS, Monn AR, Masten AS. Intergenerational continuity of adverse childhood experiences in homeless families: Unpacking exposure to maltreatment versus family dysfunction. Am J Orthopsychiatry. (2017) 87:3. doi: 10.1037/ort0000133
9. Rokita KI, Dauvermann MR, Donohoe G. Early life experiences and social cognition in major psychiatric disorders: a systematic review. Eur Psychiatry. (2018) 53:123–33. doi: 10.1016/j.eurpsy.2018.06.006
10. Giovanelli A, Reynolds AJ, Mondi CF, Ou S-R. Adverse childhood experiences and adult well-being in a low-income, urban cohort. Pediatrics. (2016) 137. doi: 10.1542/peds.2015-4016
11. Veru F, MacDonald K, Malla A, Pruessner M, King S, Joober R, et al. The effects of childhood adversity on treatment delays and its components in first-episode psychosis. Psychiatry Res. (2022) 308:114341. doi: 10.1016/j.psychres.2021.114341
12. Kilian S, Asmal L, Phahladira L, Plessis SD, Luckhoff H, Scheffler F, et al. The association between childhood trauma and treatment outcomes in schizophrenia spectrum disorders. Psychiatry Res. (2020) 289:113004. doi: 10.1016/j.psychres.2020.113004
13. Chang X, Jiang X, Mkandarwire T, Shen M. Associations between adverse childhood experiences and health outcomes in adults aged 18–59 years. PLoS One. (2019) 14:e0211850. doi: 10.1371/journal.pone.0211850
14. Alhowaymel FM, Alenezi A eds. Adverse childhood experiences and health in rural areas of Riyadh province in Saudi Arabia: A cross-sectional study. In: Healthcare. MDPI. (2021) 2502.
15. Soares ALG, Howe LD, Matijasevich A, Wehrmeister FC, Menezes AM, Goncalves H. Adverse childhood experiences: Prevalence and related factors in adolescents of a Brazilian birth cohort. Child Abuse neglect. (2016) 51:21–30. doi: 10.1016/j.chiabu.2015.11.017
16. Ho GW, Chan AC, Chien W-T, Bressington DT, Karatzias T. Examining patterns of adversity in Chinese young adults using the Adverse Childhood Experiences—International Questionnaire (ACE-IQ). Child Abuse neglect. (2019) 88:179–88. doi: 10.1016/j.chiabu.2018.11.009
17. Kim YH. Associations of adverse childhood experiences with depression and alcohol abuse among Korean college students. Child Abuse neglect. (2017) 67:338–48. doi: 10.1016/j.chiabu.2017.03.009
18. Björkenstam E, Hjern A, Vinnerljung B. Adverse childhood experiences and disability pension in early midlife: results from a Swedish National Cohort Study. Eur J Public Health. (2017) 27:472–7. doi: 10.1093/eurpub/ckw233
19. Giano Z, Wheeler DL, Hubach RD. The frequencies and disparities of adverse childhood experiences in the US. BMC Public Health. (2020) 20:1–12. doi: 10.1186/s12889-020-09411-z
20. Hustedde C. Adverse childhood experiences. Primary Care. (2021) 48:493–504. doi: 10.1016/j.pop.2021.05.005
21. Velemínský M, Dvořáčková O, Samková J, Rost M, Sethi D, Velemínský M Jr. Prevalence of adverse childhood experiences (ACE) in the Czech Republic. Child Abuse Negl. (2020) 102:104249. doi: 10.1016/j.chiabu.2019.104249
22. Witt A, Sachser C, Plener PL, Brähler E, Fegert JM. The prevalence and consequences of adverse childhood experiences in the german population. Dtsch Arztebl Int. (2019) 116:635–42. doi: 10.3238/arztebl.2019.0635
23. Ujhelyi Nagy A, Kuritár Szabó I, Hann E, Kósa K. Measuring the prevalence of adverse childhood experiences by survey research methods. Int J Environ Res Public Health. (2019) 16:1048. doi: 10.3390/ijerph16061048
24. Zhang J, Tang BW, Liu MW, Yuan S, Yu HJ, Zhang R, et al. Association of adverse childhood experiences with health risk behaviors among college students in Zambia. Int J Behav Med. (2020) 27:400–5. doi: 10.1007/s12529-020-09863-y
25. Amone-P'Olak K. Prevalence, distribution and attributable risks of adverse childhood experiences in different family types: A survey of young adults in Botswana. Child Abuse Negl. (2022) 126:105513. doi: 10.1016/j.chiabu.2022.105513
26. Trotta A, Murray R, Fisher H. The impact of childhood adversity on the persistence of psychotic symptoms: a systematic review and meta-analysis. psychol Med. (2015) 45:2481–98. doi: 10.1017/S0033291715000574
27. Prokopez CR, Vallejos M, Farinola R, Alberio G, Caporusso GB, Cozzarin LG, et al. The history of multiple adverse childhood experiences in patients with schizophrenia is associated with more severe symptomatology and suicidal behavior with gender-specific characteristics. Psychiatry Res. (2020) 293:113411. doi: 10.1016/j.psychres.2020.113411
28. Peh OH, Rapisarda A, Lee J. Childhood adversities in people at ultra-high risk (UHR) for psychosis: a systematic review and meta-analysis. psychol Med. (2019) 49:1089–101. doi: 10.1017/S003329171800394X
29. Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective-and cross-sectional cohort studies. Schizophr bulletin. (2012) 38:661–71. doi: 10.1093/schbul/sbs050
30. Seidenfaden D, Knorr U, Soendergaard MG, Poulsen HE, Fink-Jensen A, Jorgensen MB, et al. The relationship between self-reported childhood adversities, adulthood psychopathology and psychological stress markers in patients with schizophrenia. Compr Psychiatry. (2017) 72:48–55. doi: 10.1016/j.comppsych.2016.09.009
31. Prokopez CR, Cesoni OM, Caporusso GB, Reffino-Pereyra ML, Alberio G, Vallejos M. Prevalence and clinical impact of childhood adversities in women with schizophrenia. Clin Schizophr Relat Psychoses. (2018). doi: 10.3371/CSRP.PRCE.061518
32. Wells R, Jacomb I, Swaminathan V, Sundram S, Weinberg D, Bruggemann J, et al. The impact of childhood adversity on cognitive development in schizophrenia. Schizophr Bulletin. (2019) 46:140–53. doi: 10.1093/schbul/sbz033
33. Anda R, Tietjen G, Schulman E, Felitti V, Croft J. Adverse childhood experiences and frequent headaches in adults. Headache. (2010) 50:1473–81. doi: 10.1111/j.1526-4610.2010.01756.x
34. Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. (1998) 14:245–58. doi: 10.1016/S0749-3797(98)00017-8
35. Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. Eur Arch Psychiatry Clin Neurosci. (2006) 256:174–86. doi: 10.1007/s00406-005-0624-4
36. Li X-B, Li Q-Y, Liu J-T, Zhang L, Tang Y-L, Wang C-Y. Childhood trauma associates with clinical features of schizophrenia in a sample of Chinese inpatients. Psychiatry Res. (2015) 228:702–7. doi: 10.1016/j.psychres.2015.06.001
37. Carbone EA, Pugliese V, Bruni A, Aloi M, Calabrò G, Jaén-Moreno MJ, et al. Adverse childhood experiences and clinical severity in bipolar disorder and schizophrenia: a transdiagnostic two-step cluster analysis. J Affect Disord. (2019) 259:104–11. doi: 10.1016/j.jad.2019.08.049
38. Kasznia J, Pytel A, Stańczykiewicz B, Samochowiec J, Preś J, Rachubińska K, et al. Adverse childhood experiences and neurocognition in schizophrenia spectrum disorders: age at first exposure and multiplicity matter. Front Psychiatry. (2021) 12:1092. doi: 10.3389/fpsyt.2021.684099
39. Sheffler JL, Piazza JR, Quinn JM, Sachs-Ericsson NJ, Stanley IH. Adverse childhood experiences and coping strategies: identifying pathways to resiliency in adulthood. Anxiety stress coping. (2019) 32:594–609. doi: 10.1080/10615806.2019.1638699
40. Sheffler JL, Stanley I, Sachs-Ericsson N. Chapter 4 - ACEs and mental health outcomes. In: Asmundson GJG, Afifi TO, editors. Adverse Childhood Experiences. Tallahassee, FL, United States: Academic Press (2020). p. 47–69.
41. Renkema TC, De Haan L, Schirmbeck F, Alizadeh BZ, van Amelsvoort T, Bartels-Velthuis AA, et al. Childhood trauma and coping in patients with psychotic disorders and obsessive-compulsive symptoms and in un-affected siblings. Child Abuse Neglect. (2020) 99:104243. doi: 10.1016/j.chiabu.2019.104243
42. Basile KC, DeGue S, Jones K, Freire K, Dills J, Smith SG, et al. STOP SV: A Technical Package to Prevent Sexual Violence. Atlanta, GA, USA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. (2016). Available at: https://www.cdc.gov/violenceprevention/pdf/sv-prevention-technical-package.pdf.
43. David-Ferdon C, Vivolo-Kantor AM, Dahlberg LL, Marshall KJ, Rainford N, Hall JE. A Comprehensive Technical Package for the Prevention of Youth Violence and Associated Risk Behaviors. Atlanta, GA, USA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. (2016). Available at: https://stacks.cdc.gov/view/cdc/43085.
44. Fortson BL, Klevens J, Merrick MT, Gilbert LK, Alexander SP. Preventing child abuse and neglect: A technical package for policy, norm, and programmatic activities. Atlanta, GA, USA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention. (2016). Available at: https://www.cdc.gov/violenceprevention/pdf/can-prevention-technical-package.pdf.
45. Niolon PH, Centers for Disease Control Prevention. Preventing intimate partner violence across the lifespan: A technical package of programs, policies, and practices. Atlanta, Georgia: Government Printing Office (2017).
46. Stone DM, Holland KM, Bartholow BN, Crosby AE, Davis SP, Wilkins N. Preventing suicide: A technical package of policies, programs, and practice (United States: National Center for Injury Prevention and Control; division of Violence Prevention). (2017).
47. Moore DJ, Palmer BW, Jeste DV. Use of the mini-mental state exam in middle-aged and older outpatients with schizophrenia: cognitive impairment and its associations. Am J Geriatric Psychiatry. (2004) 12:412–9. doi: 10.1176/appi.ajgp.12.4.412
48. Leucht S, Engel RR, Davis JM, Kissling W, Meyer zur Capellen K, Schmauß M, et al. Equipercentile linking of the Brief Psychiatric Rating Scale and the Clinical Global Impression Scale in a catchment area. Eur Neuropsychopharmacol. (2012) 22:501–5. doi: 10.1016/j.euroneuro.2011.11.007
49. Hajian-Tilaki K. Sample size estimation in epidemiologic studies. Caspian J Internal Med. (2011) 2:289–98.
50. Mall S, Platt JM, Temmingh H, Musenge E, Campbell M, Susser E, et al. The relationship between childhood trauma and schizophrenia in the Genomics of Schizophrenia in the Xhosa people (SAX) study in South Africa. psychol Med. (2020) 50:1570–7. doi: 10.1017/S0033291719001703
51. Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the childhood trauma questionnaire in an adolescent psychiatric population. J Am Acad Child Adolesc Psychiatry. (1997) 36:340–8. doi: 10.1097/00004583-199703000-00012
52. Fink LA, Bernstein D, Handelsman L, Foote J, Lovejoy M. Initial reliability and validity of the childhood trauma interview: a new multidimensional measure of childhood interpersonal trauma. Am J Psychiatry. (1995) 152:1329–35. doi: 10.1176/ajp.152.9.1329
53. Sarling A, Jansson B, Englén M, Bjärtå A, Rondung E, Sundin Ö. Psychometric properties of the Swedish version of the experiences in close relationships – relationship structures questionnaire (ECR-RS global nine-item version). Cogent Psychol. (2021) 8:1926080. doi: 10.1080/23311908.2021.1926080
54. Sinclair VG, Wallston KA. The development and psychometric evaluation of the Brief Resilient Coping Scale. Assessment. (2004) 11:94–101. doi: 10.1177/1073191103258144
55. Bøen H, Dalgard OS, Bjertness E. The importance of social support in the associations between psychological distress and somatic health problems and socio-economic factors among older adults living at home: a cross sectional study. BMC Geriatrics. (2012) 12:27. doi: 10.1186/1471-2318-12-27
56. Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption–II. Addict (Abingdon England). (1993) 88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x
57. Osman A, Bagge CL, Gutierrez PM, Konick LC, Kopper BA, Barrios FX. The Suicidal Behaviors Questionnaire-Revised (SBQ-R): validation with clinical and nonclinical samples. Assessment. (2001) 8:443–54. doi: 10.1177/107319110100800409
58. Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosomatic Med. (2002) 64:258–66. doi: 10.1097/00006842-200203000-00008
59. Gierk B, Kohlmann S, Kroenke K, Spangenberg L, Zenger M, Brähler E, et al. The somatic symptom scale–8 (SSS-8): A brief measure of somatic symptom burden. JAMA Internal Med. (2014) 174:399–407. doi: 10.1001/jamainternmed.2013.12179
60. Shrestha B, Dunn L. The declaration of Helsinki on medical research involving human subjects: a review of seventh revision. J Nepal Health Res Council. (2019) 17:548–52. doi: 10.33314/jnhrc.v17i4
61. Vallejos M, Cesoni OM, Farinola R, Bertone MS, Prokopez CR. Adverse childhood experiences among men with schizophrenia. Psychiatr Quarterly. (2017) 88:665–73. doi: 10.1007/s11126-016-9487-2
62. Croft J, Heron J, Teufel C, Cannon M, Wolke D, Thompson A, et al. Association of trauma type, age of exposure, and frequency in childhood and adolescence with psychotic experiences in early adulthood. JAMA Psychiatry. (2019) 76:79–86. doi: 10.1001/jamapsychiatry.2018.3155
63. Trauelsen AM, Bendall S, Jansen JE, Nielsen H-GL, Pedersen MB, Trier CH, et al. Childhood adversity specificity and dose-response effect in non-affective first-episode psychosis. Schizophr Res. (2015) 165:52–9. doi: 10.1016/j.schres.2015.03.014
64. Rubino IA, Nanni RC, Pozzi DM, Siracusano A. Early adverse experiences in schizophrenia and unipolar depression. J Nervous Ment Disease. (2009) 197:65–8. doi: 10.1097/NMD.0b013e3181925342
65. Chua SE, Murray RM. The neurodevelopmental theory of schizophrenia: evidence concerning structure and neuropsychology. Ann Med. (1996) 28:547–55. doi: 10.3109/07853899608999119
66. Mcguffin P, Asherson P, Owen M, Farmer A. The strength of the genetic effect: is there room for an environmental influence in the aetiology of schizophrenia? Br J Psychiatry. (1994) 164:593–9. doi: 10.1192/bjp.164.5.593
67. Walker EF, Diforio D. Schizophrenia: a neural diathesis-stress model. psychol review. (1997) 104:667. doi: 10.1037//0033-295X.104.4.667
68. Tienari PJ, Wynne LC. Adoption studies of schizophrenia. Ann Med. (1994) 26:233–7. doi: 10.3109/07853899409147896
69. Kunugi H, Nanko S, Murray R. Obstetric complications and schizophrenia: prenatal underdevelopment and subsequent neurodevelopmental impairment. Br J Psychiatry. (2001) 178:s25–s9. doi: 10.1192/bjp.178.40.s25
70. Gayer-Anderson C, Fisher HL, Fearon P, Hutchinson G, Morgan K, Dazzan P, et al. Gender differences in the association between childhood physical and sexual abuse, social support and psychosis. Soc Psychiatry Psychiatr Epidemiol. (2015) 50:1489–500. doi: 10.1007/s00127-015-1058-6
71. Xie P, Wu K, Zheng Y, Guo Y, Yang Y, He J, et al. Prevalence of childhood trauma and correlations between childhood trauma, suicidal ideation, and social support in patients with depression, bipolar disorder, and schizophrenia in southern China. J Affect Disord. (2018) 228:41–8. doi: 10.1016/j.jad.2017.11.011
72. Bortolon C, Seillé J, Raffard S. Exploration of trauma, dissociation, maladaptive schemas and auditory hallucinations in a French sample. Cogn neuropsychiatry. (2017) 22:468–85. doi: 10.1080/13546805.2017.1387524
73. Pilton M, Bucci S, McManus J, Hayward M, Emsley R, Berry K. Does insecure attachment mediate the relationship between trauma and voice-hearing in psychosis? Psychiatry Res. (2016) 246:776–82. doi: 10.1016/j.psychres.2016.10.050
74. Houtepen LC, Heron J, Suderman MJ, Fraser A, Chittleborough CR, Howe LD. Associations of adverse childhood experiences with educational attainment and adolescent health and the role of family and socioeconomic factors: a prospective cohort study in the UK. PLoS Med. (2020) 17:e1003031. doi: 10.1371/journal.pmed.1003031
Keywords: schizophrenia, adverse childhood experiences, comparative study, amhara, Ethiopia
Citation: Assefa Fentahun B, Belete Mossie T, Damtew Hailu R, Bete T and Moges Demeke S (2024) Adverse childhood experiences among people with schizophrenia at comprehensive specialized hospitals in Bahir Dar, Ethiopia: a comparative study. Front. Psychiatry 15:1387833. doi: 10.3389/fpsyt.2024.1387833
Received: 18 February 2024; Accepted: 29 April 2024;
Published: 21 May 2024.
Edited by:
Jerome Brunelin, INSERM U1028 Centre de Recherche en Neurosciences de Lyon, FranceReviewed by:
Anushree Bose, National Institute of Mental Health and Neurosciences (NIMHANS), IndiaMarco Hirnstein, University of Bergen, Norway
Copyright © 2024 Assefa Fentahun, Belete Mossie, Damtew Hailu, Bete and Moges Demeke. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Birhanu Assefa Fentahun, YXNzZWZhYmlyaGFudTI3QGdtYWlsLmNvbQ==
 Birhanu Assefa Fentahun
Birhanu Assefa Fentahun Tilahun Belete Mossie
Tilahun Belete Mossie Rekik Damtew Hailu2
Rekik Damtew Hailu2 Tilahun Bete
Tilahun Bete Solomon Moges Demeke
Solomon Moges Demeke