- 1Department of Midwifery, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan, Ethiopia
- 2School of Public Health, College of Medicine and Health Sciences, Mizan-Tepi University, Mizan Aman, Ethiopia
- 3Department of Laboratory, College of Medicine and Health Sciences, Mizan Tepi University, Mizan Aman, Ethiopia
- 4College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
Background: Antenatal depression in Human Immunodeficiency Virus (HIV) positive pregnant women can have significant adverse effects on both the mother and newborns, yet it is often overlooked in pregnancy care in Sub-Saharan Africa (SSA). Despite this, there is limited data on the combined prevalence of antenatal depression and its predictors among HIV-positive women in the region.
Objective: To assess the pooled prevalence of antenatal depression and its associated factors among HIV-positive women in SSA.
Methods: All primary cross-sectional studies published before 1st January/2024, were included. We conducted searches in relevant databases; PubMed, HINARI, Web of Science, PsycINFO, Psychiatry Online, ScienceDirect, and Google Scholar. The Joanna Briggs Institute checklist was used to critically appraise the selected studies. To assess heterogeneity among the studies, we utilized the I2 test. Publication bias was evaluated using a funnel plot and Egger’s test. The forest plot was used to present the combined proportion of antenatal depression and odds ratio, along with a 95% confidence interval.
Results: The pooled prevalence of antenatal depression among HIV-positive women in Sub-Saharan Africa was found to be 30.6% (95% CI, 19.8%-41.3%). Factors significantly associated with antenatal depression among HIV-positive women in SSA included being unmarried (AOR: 3.09, 95% CI: 1.57 – 6.07), having a previous history of depression (AOR: 2.97, 95% CI: 1.79 – 4.91), experiencing intimate partner violence (IPV) (AOR: 2.11, 95% CI: 1.44 – 3.09), and experiencing stigma (AOR: 1.36, 95% CI: 1.05 – 1.76).
Conclusion: High prevalence of antenatal depression among HIV-positive women in SSA underscores the need for prioritizing identification and management. Interventions addressing factors like IPV and stigma, along with training for healthcare providers in recognizing symptoms and providing support, are recommended.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42024508236.
Introduction
Antenatal depression is a common mental health disorder that affects pregnant women worldwide (1), with lower and middle-income countries bearing the highest burden (2). In Sub-Saharan Africa (SSA), where the prevalence of HIV is high (3), antenatal depression is a significant public health concern among HIV positive women (4–6). Serious forms of depression characterized by the idea of suicide or self-harming are common during pregnancy (7).
Antenatal depression in HIV-positive pregnant women can accelerate HIV disease progression (8, 9) and raise maternal morbidity and mortality rates (8, 10). Additionally, HIV-positive women with depression tend to have poor adherence to antiretroviral therapy (ART) (9, 11–13). Untreated depression during pregnancy is also a risk factor for postpartum depression (14), and reduces the likelihood of exclusive breastfeeding for newborns (15). Furthermore, antenatal depression has a lasting impact on both mothers, infants, and children across generations (16–20).
By 2030, depression and HIV/AIDS are expected to be the main global disease burdens (21). To improve mental health, national and international strategies have been implemented for vulnerable groups like postpartum women, and those living with HIV/AIDS (22, 23). However, in SSA, antenatal depression with HIV-positive women is prevalent, as the primary studies conducted in different places in the region have indicated (2, 13, 24–34). HIV has been documented to have effects on the fetus, including low birth weight, preterm births, small for gestational age, delayed cognitive and language development, behavioral problems, poor academic performance, and emotional issues (35–37).
Previous studies in SSA countries have reported varying rates of antenatal depression among HIV-positive pregnant women, ranging from 6.5% to 67% (27, 32), and being unmarried, unemployed, unplanned pregnancy, length of time on ART, experienced intimate partner violence during the current pregnancy, ART non-adherence, experienced internalized AIDS stigma, poor social support, and history of depression have been found to be associated with developing antenatal depression among HIV-positive pregnant women (2, 4, 13, 24–34, 38–40).
These primary studies were conducted in a fragmented manner across different SSA countries, and the pooled prevalence of antenatal depression among HIV-positive pregnant women has not been determined in SSA. Therefore, in this systematic review and meta-analysis, we aimed to synthesize the available evidence on the pooled prevalence of antenatal depression and its predictors among HIV positive women in SSA. The findings will provide valuable insights into the burden of antenatal depression in this population, inform the development of effective interventions, and contribute to the achievement of Sustainable Development Goal (SDG) 3, which aims to ensure healthy lives and promote well-being for all at all ages by 2030.
Methods
Study setting and period
We included studies conducted among countries listed in the Sub-Saharan Africa region. The search period was from October 1, 2023 to January 1, 2024.
Search strategies
This systematic review has adhered to the Preferred Reporting Item for Systematic Review and Meta-Analyses (PRISMA) guideline and checklist (41). PubMed, HINARI, Web of Science, PsycINFO, Psychiatry Online, ScienceDirect, and Google Scholar were searched for relevant studies on antenatal depression among HIV positive women in Sub-Saharan Africa. Moreover, reference lists of eligible studies were retrieved to account for the missed studies in the database searching. All studies reporting the proportion or prevalence of antenatal depression among HIV positive women were the target of this review. All primary cross-sectional studies published before January 1, 2024 were included. The search was done using keywords such as antenatal depression, or depression in antenatal period, depression during pregnancy and associated factors, or determinants, or predictors, and country found in Sub-Saharan Africa. Combinations of Boolean operators (AND, OR), free keywords, and MeSH terms were used in the search process (Additional File 1).
Eligibility criteria
The inclusion criteria encompassed: (1) studies conducted in Sub-Saharan Africa country, (2) all cross-sectional studies, (3) studies reporting the prevalence of antenatal depression and/or associated or determinant factors or predictors, and (4) studies published as full-length articles in English. Whereas, conference papers or abstracts, articles lacking full texts, anonymous reports, editorial reports, and qualitative studies were not included in this study.
Data extraction
The data from all the studies included in the analysis were collected and organized in a customized Microsoft Excel spreadsheet. This extraction process was carried out by three authors (GA, DG, AA, and MA) using a standardized extraction form. In case of any discrepancies between the data extractors, discussions were held and resolved by the three authors (AA, TT, and DA). We extracted important information from each study, which included the author’s name, publication year, antenatal depression event, prevalence, country, study design, and associated factors such as odds ratios.
Quality assessment/critical appraisal
The Joanna Briggs Institute (JBI) Critical Appraisal Checklist for cross-sectional studies was used to assess the quality of the study (42). Two authors (GA and AA) independently assessed the quality of each article using a critical appraisal checklist adapted from JBI. During the critical appraisal process, if any discrepancies arose, the reviewers held discussions led by the fourth author (TT) to address and resolve the issues. Finally, a total of 13 studies that fulfill the inclusion criteria were considered in this meta-analysis (Additional File 2).
Statistical analysis
Data entry was performed using the Microsoft Excel Database, and the entered data was subsequently imported into R software version 4.1.3 for further analysis utilizing the Meta-package. The heterogeneity between studies was evaluated using the I2 index (43), where values of 25%, 50%, and 75% indicated low, medium, and high heterogeneity, respectively (44). Publication bias was evaluated by visually inspecting the symmetry of the funnel plot and conducting the Egger test. A p-value of less than 0.05 on the Egger test indicated the presence of publication bias among the included studies. In order to identify potential sources of heterogeneity, a univariate Meta-regression analysis was conducted, taking into account the sample size and year of publication. Additionally, a leave-one-out sensitivity analysis was performed, systematically removing one study at a time to assess the impact of each individual study on the overall estimate (45). Furthermore, a trim-and-fill analysis was conducted to assess the extent of distortion in the pooled prevalence of male involvement caused by publication bias. The results are presented in a forest plot, displaying a point estimate along with 95% confidence intervals. All analyses were performed using R software version 4.1.3.
Result
Characteristics of the studies included in the meta-analysis and systematic review
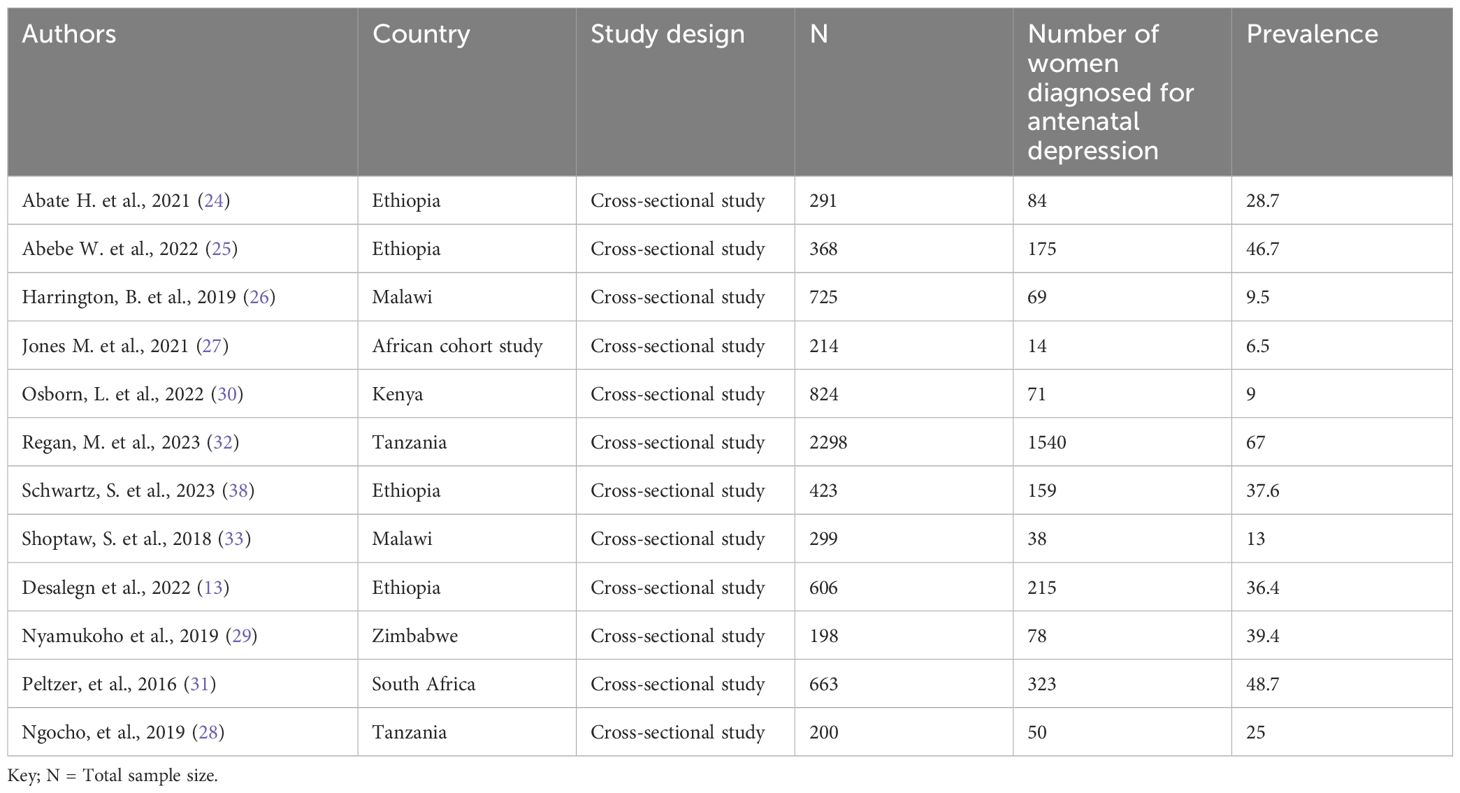
Out of the 7,395 articles identified through different search strategies, 148 records were eliminated due to duplication. An additional 7,226 articles were excluded because their titles and abstracts were deemed inappropriate. Additionally, 9 were excluded due to noncompliance with the inclusion criteria. Finally, only 12 studies met the eligibility criteria and were considered in this study (Figure 1). This study incorporated a total of 7,109 participants from 12 studies, with sample sizes ranging from 198 to 2298 (13, 24–33, 38) (Table 1).
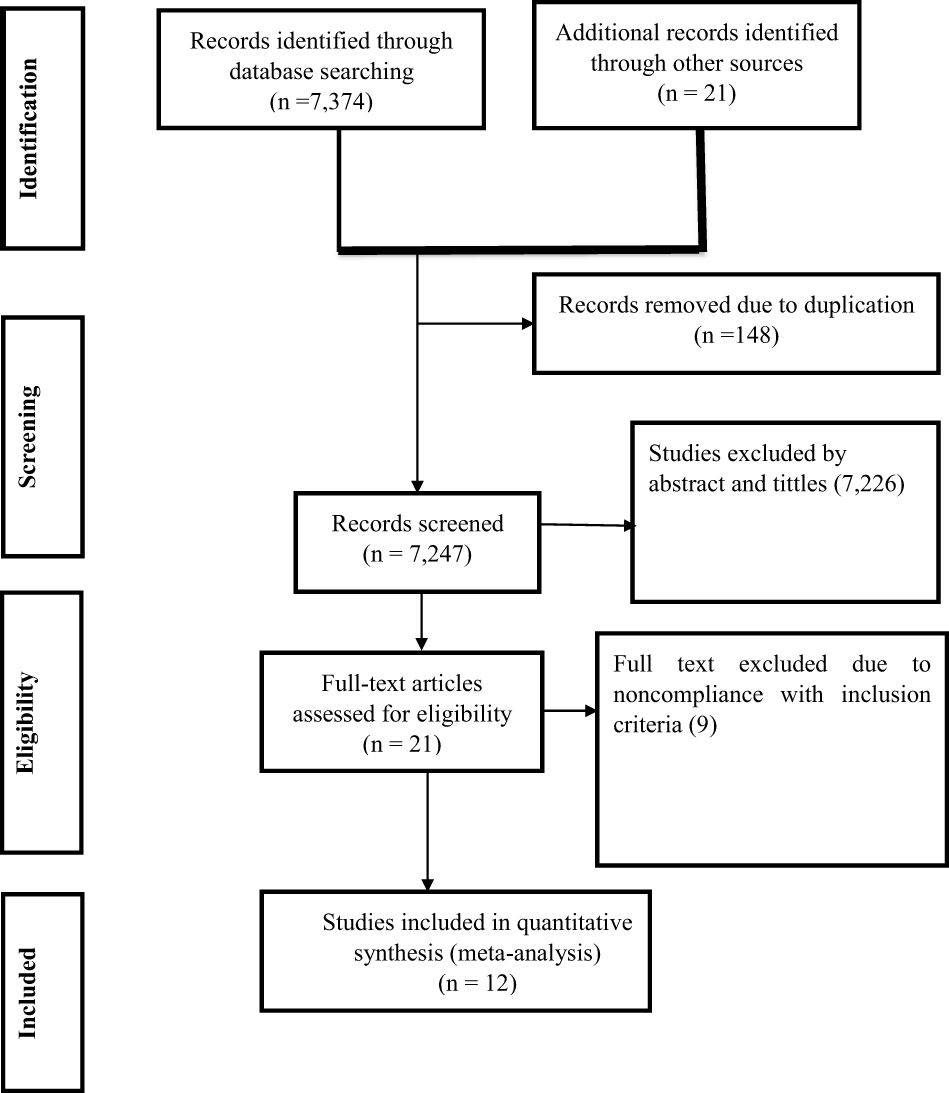
Figure 1 PRISMA flow chart showing the process of search and selection of studies included in the systematic review and meta-analysis.
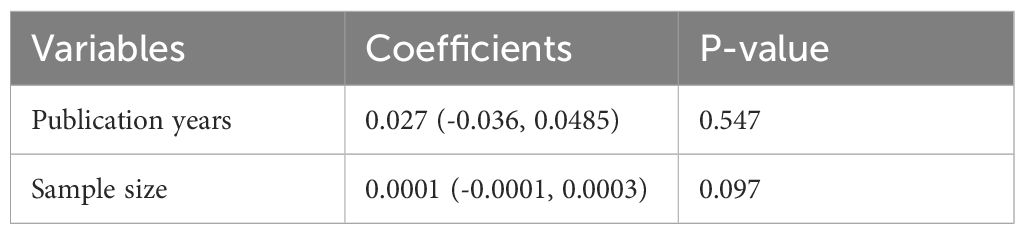
Pooled prevalence of antenatal depression among HIV positive women in SSA
The overall pooled prevalence of antenatal depression among HIV positive women in SSA was 30.6% (95% CI, 19.8%-41.3%) (Figure 2). A subgroup analysis was conducted by country in SSA, revealing that the lowest prevalence was reported from African cohort, 6.5%, while the highest prevalence was reported from South Africa, 48.7% (Figure 3).
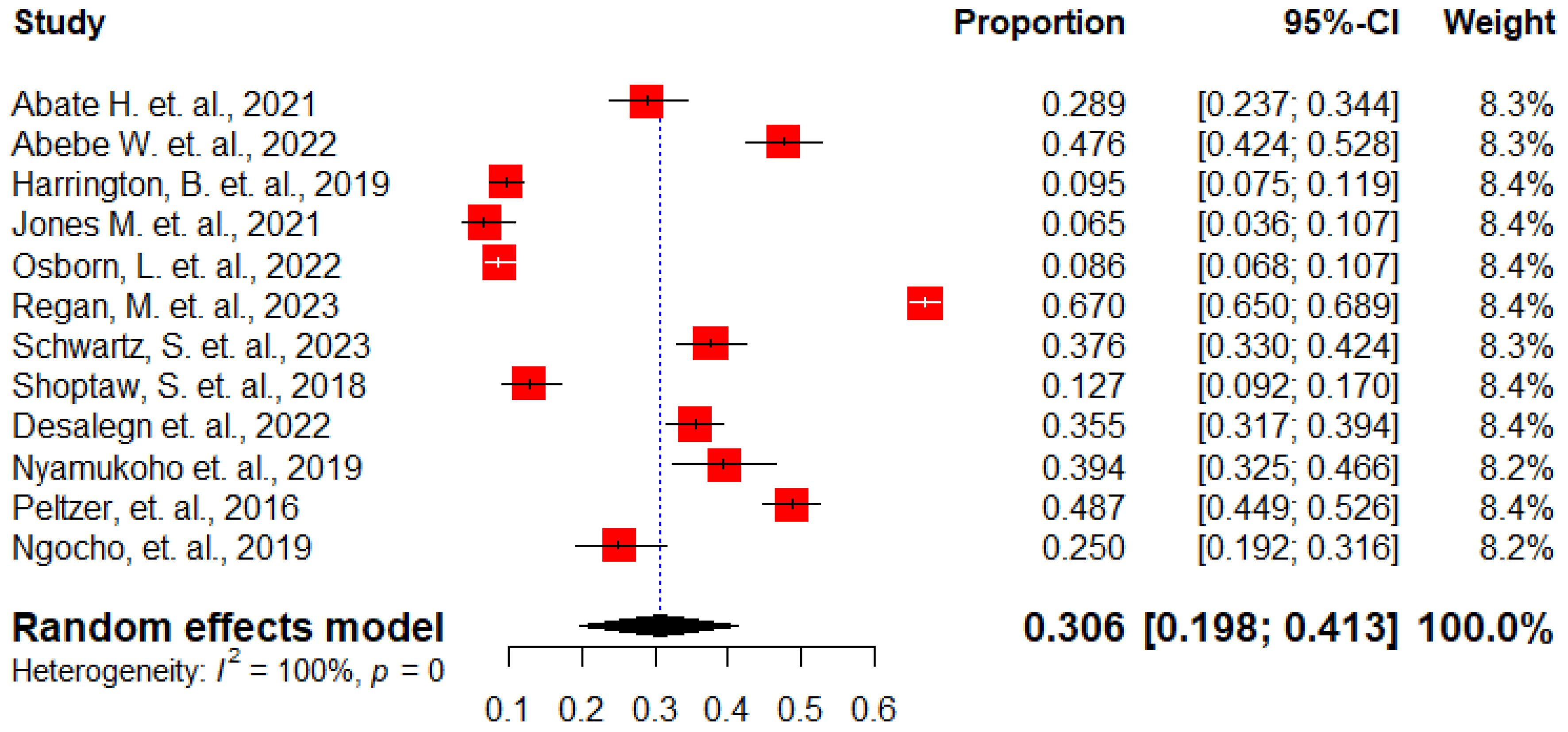
Figure 2 The forest plots show the pooled prevalence of antenatal depression among HIV positive women in Sub-Saharan Africa, 2024.
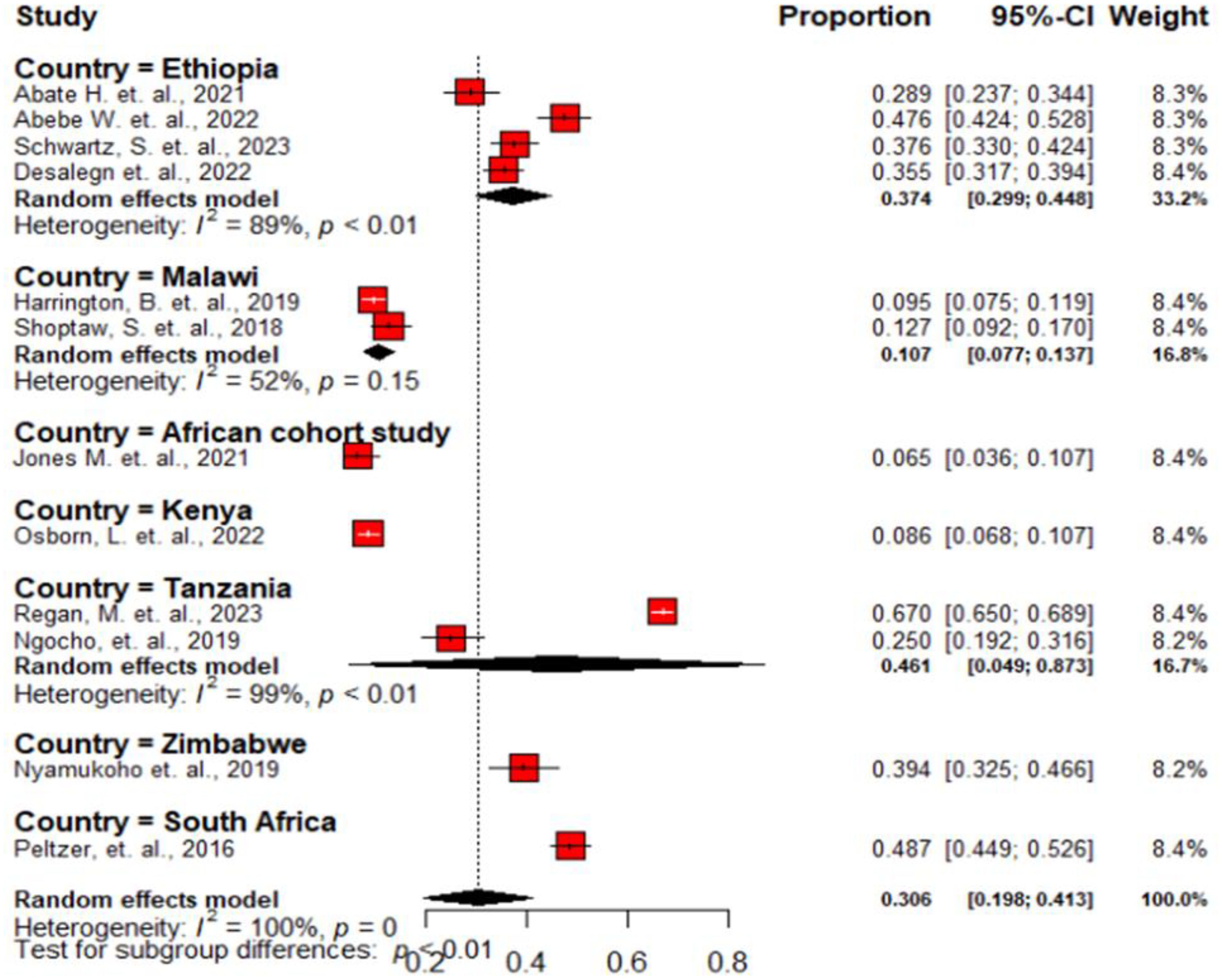
Figure 3 Forest plot showing the subgroup analysis of the pooled prevalence of antenatal depression among HIV positive women in Sub-Saharan Africa, 2024.
Assessment of publication bias
We used both subjective and objective measures to evaluate publication bias. First, funnel plot visual inspection was done. Then, we employed the Egger’s test. Our findings revealed that the funnel plot displayed symmetrical distribution of studies in the line of effect (Figure 4). The Egger’s test also noted a non-significant value for publication bias (P = 0.916).
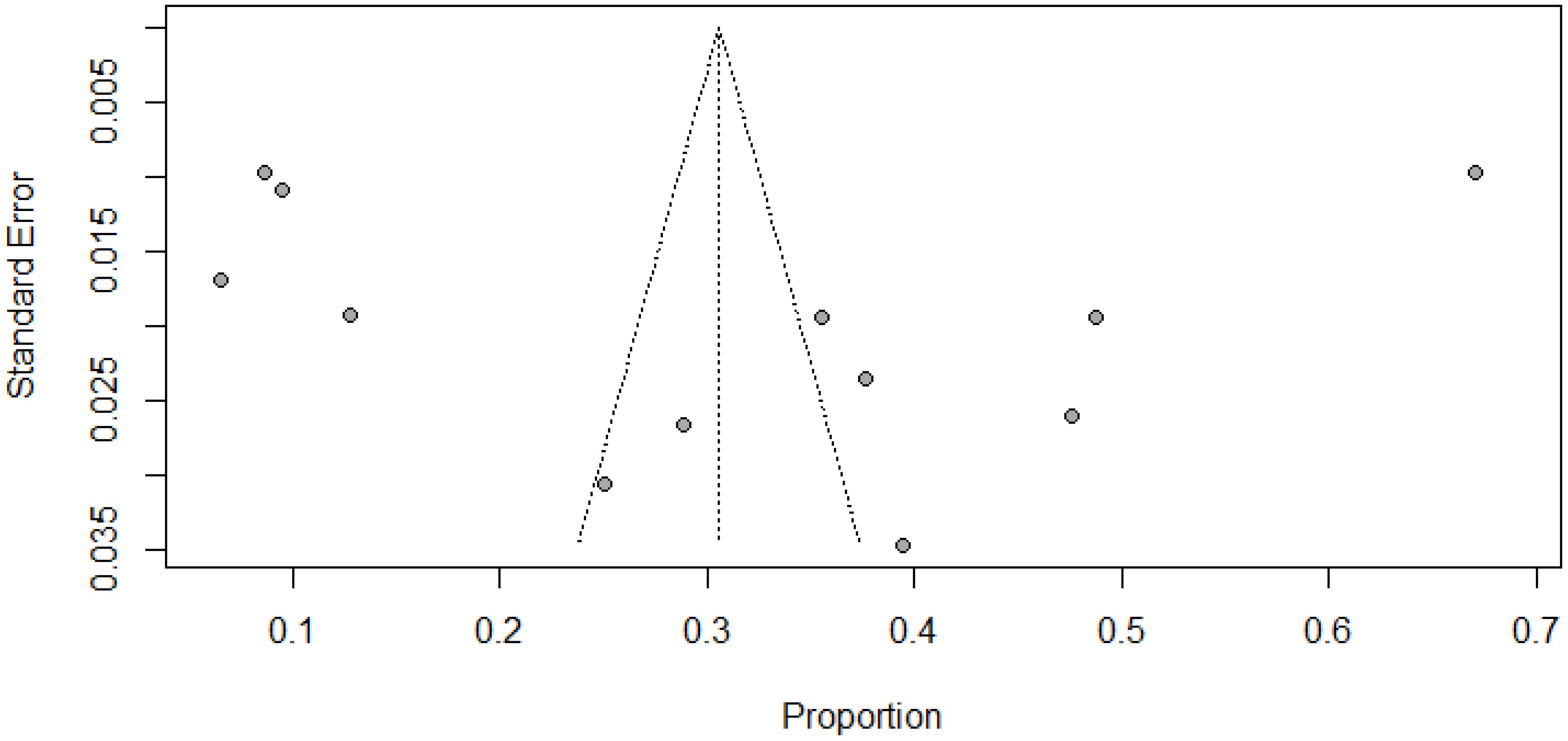
Figure 4 Funnel plot showing publication bias among studies used to compute the pooled prevalence of antenatal depression among HIV positive women in SSA, 2024.
Meta-regression and sensitivity analysis
The impact of study characteristics on the pooled estimate was assessed using meta-regression. However, none of the study characteristics, such as publication year and sample size, showed any association with the pooled estimates (P > 0.05) (Table 2).
To assess the impact of each study on the pooled estimates, a thorough sensitivity analysis was conducted by systematically excluding one study at a time. The results showed that almost all studies made comparable contributions to the overall prevalence of antenatal depression among HIV-positive women in SSA. When each study was omitted from the analysis, the pooled prevalence of antenatal depression ranged from 27.2% to 32.7% (Figure 5).
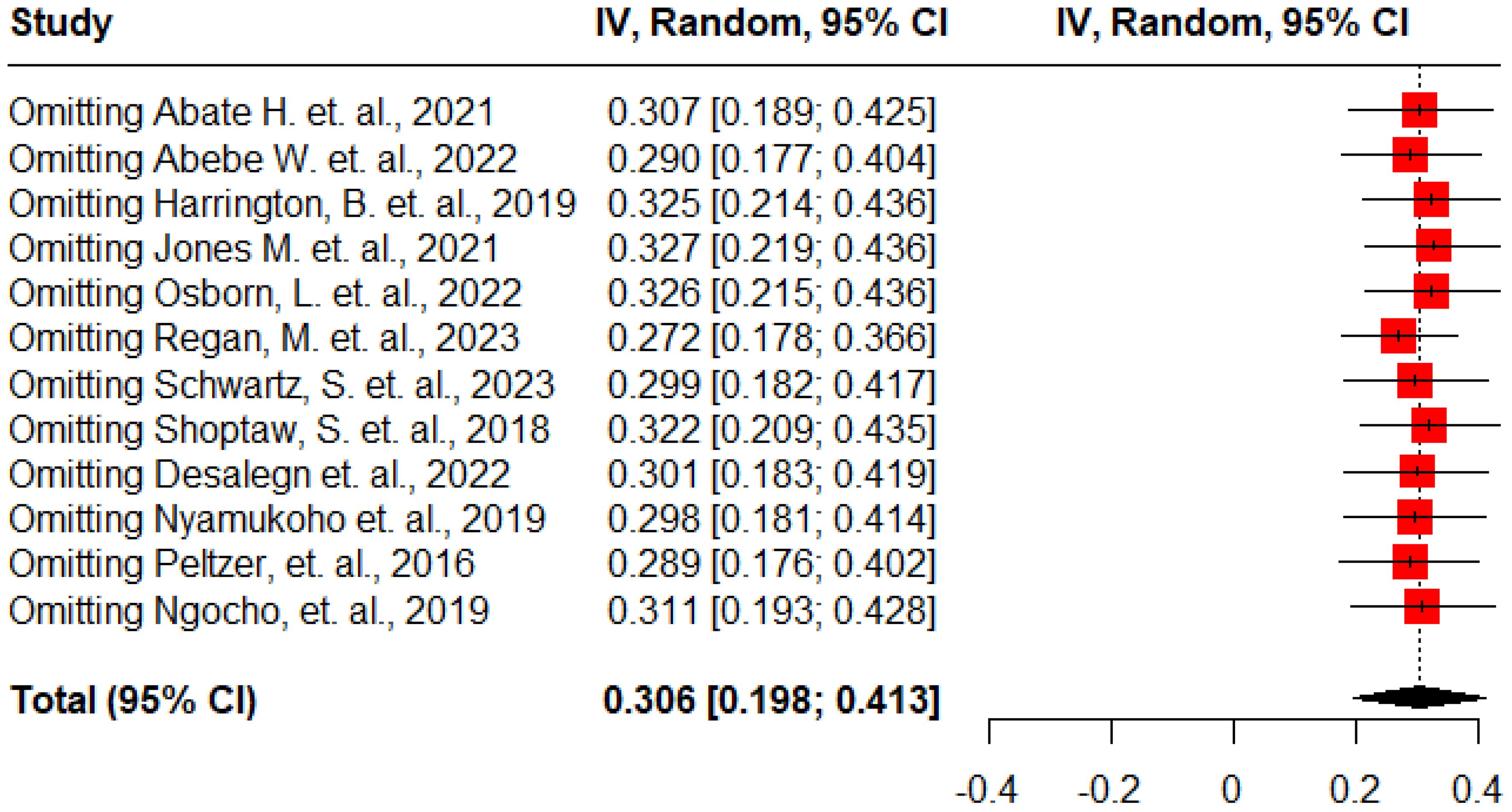
Figure 5 Sensitivity analysis for the pooled prevalence of antenatal depression among HIV positive women in Sub-Saharan Africa, 2024.
Factors associated with antenatal depression among HIV positive women in SSA
In this meta-analysis, we found significant factors associated with antenatal depression among HIV-positive women in SSA. These factors include being unmarried, employed, a previous history of depression, experiencing IPV, experiencing stigma, and ART non-adherence.
Two studies (13, 28), involving a total of 806 participants, examined the association between unmarried HIV-positive pregnant women and developing antenatal depression. The random effect model analysis revealed a significant association between being unmarried and developing of antenatal depression. Thus, the odds of developing antenatal depression were three times higher among unmarried HIV-positive pregnant women compared to those married women (AOR: 3.09, 95% CI: 1.57 – 6.07) (Figure 6).
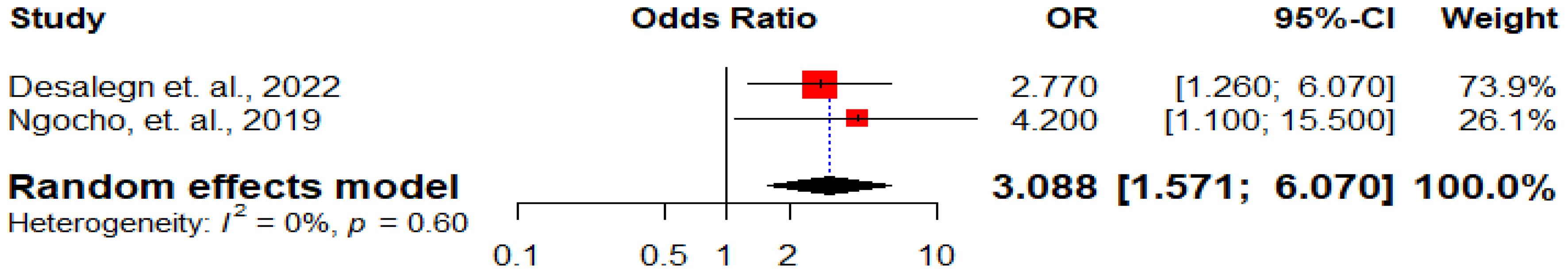
Figure 6 Forest plot displaying the association between being unmarried and antenatal depression among HIV positive women in Sub-Saharan Africa, 2024.
Two studies (26, 29) examined the correlation between a history of depression and the occurrence of antenatal depression. The overall estimate indicated that the odds of occurrence of antenatal depression were three times higher among HIV positive women with a previous history of depression compared to their counterparts (AOR: 2.97, 95% CI: 1.79 – 4.91) (Figure 7).
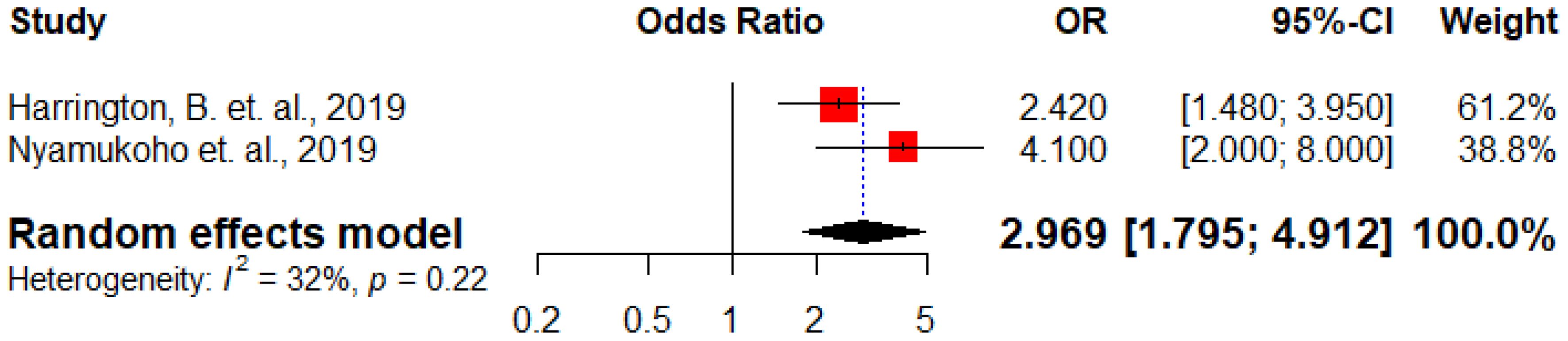
Figure 7 Forest plot displaying the association between previous history of depression and antenatal depression among HIV positive women in Sub-Saharan Africa, 202.
Five studies (13, 26, 29–31) demonstrated the correlation between HIV-positive pregnant women experiencing intimate partner violence (IPV) and the occurrence of antenatal depression. The overall analysis indicated that HIV-positive pregnant women who experienced IPV had twice the odds of developing antenatal depression compared to their counterparts (AOR: 2.11, 95% CI: 1.44 – 3.09) (Figure 8).
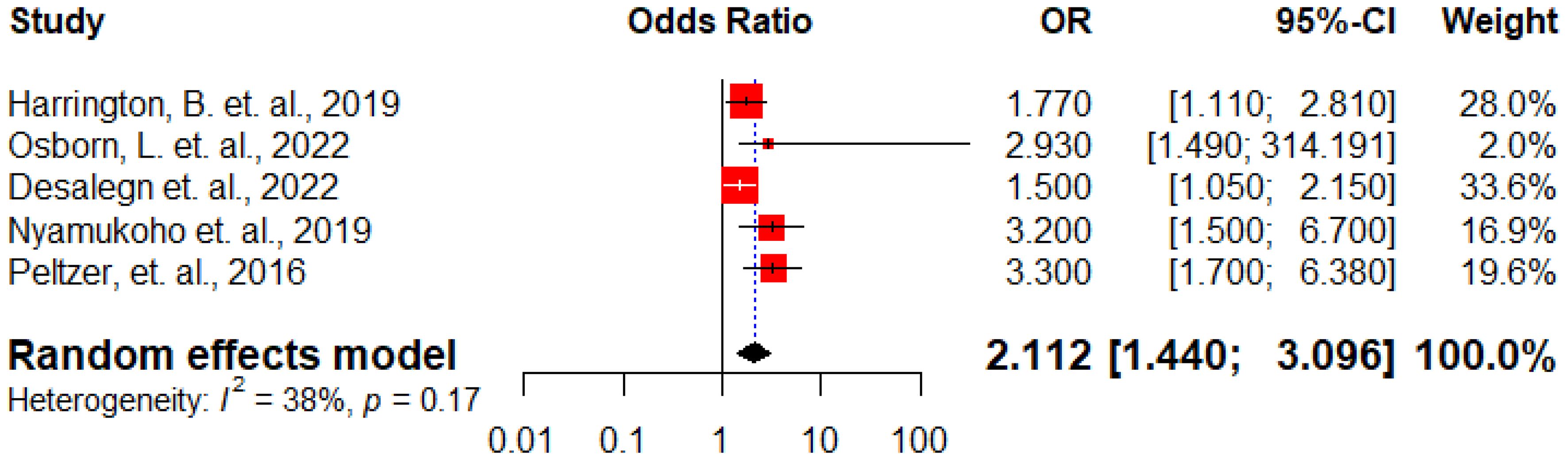
Figure 8 Forest plot displaying the association between experiencing IPV and antenatal depression among HIV positive women in Sub-Saharan Africa, 2024.
Three studies (13, 28, 30) assessed the correlation between stigma experienced by HIV-positive pregnant women and the occurrence of antenatal depression. The overall analysis showed that those who had experienced stigma had 1.4 times higher odds of developing antenatal depression compared to those who had not experienced stigma (AOR: 1.36, 95% CI: 1.05 – 1.76) (Figure 9).
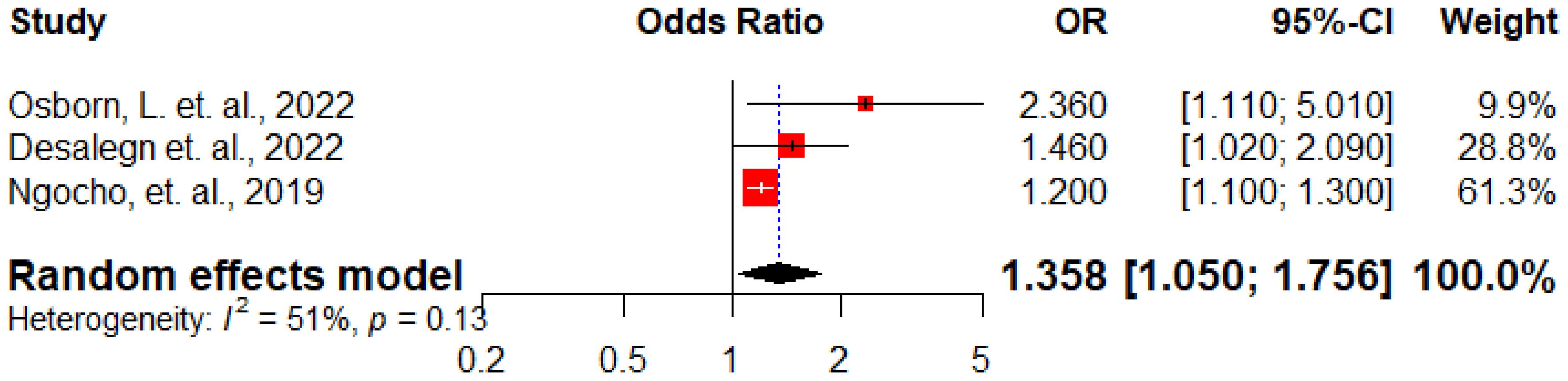
Figure 9 Forest plot displaying the association between presence of stigma and antenatal depression among HIV positive women in Sub-Saharan Africa, 2024.
Inconsistent findings were reported regarding the correlation between employment status and the occurrence of antenatal depression. Harrington et al. (26) found that employed women had higher odds of experiencing antenatal depression, while Peltzer et al. (31) showed a negative association between employment and antenatal depression. The overall analysis indicated no significant association between employment status and antenatal depression (AOR: 0.94, 95%CI: 0.35 – 2.53) (Figure 10).
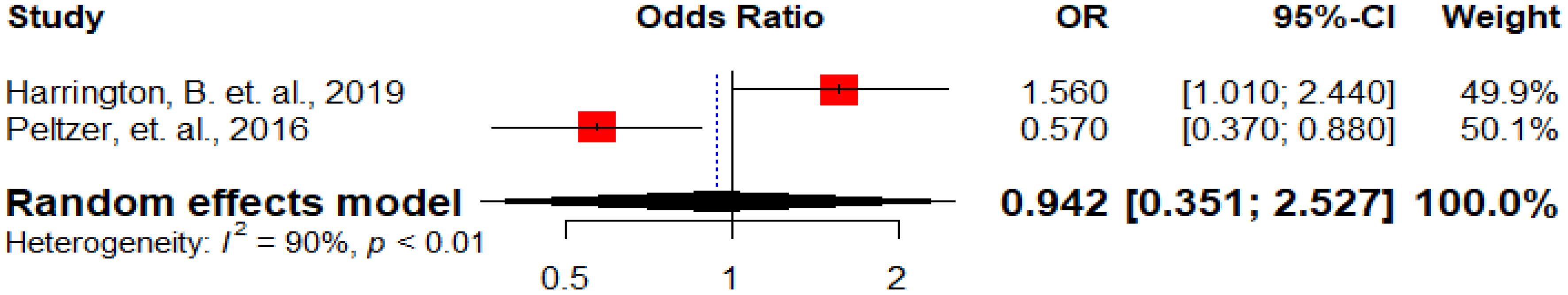
Figure 10 Forest plot displaying the association between being employed and antenatal depression among HIV positive women in Sub-Saharan Africa, 2024.
Inconsistent findings have been reported regarding the correlation between non-adherence to ART and the occurrence of antenatal depression. Desalegn et al. (13) noted that HIV-positive pregnant women who were not adherent to ART had higher odds of developing antenatal depression, while Peltzer et al. (31) indicated that those who were not adherent to ART had lower odds of developing antenatal depression. The overall analysis showed no significant association between non-adherence to ART and the occurrence of antenatal depression (AOR: 1.06, 95%CI: 0.25 – 4.39) (Figure 11).
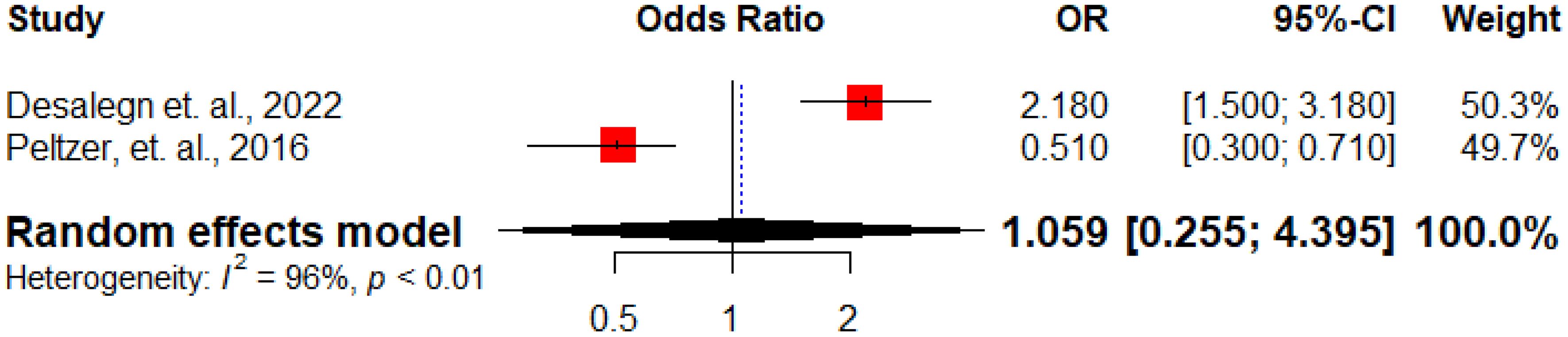
Figure 11 Forest plot displaying the association between ART non-adherence and antenatal depression among HIV positive women in Sub-Saharan Africa, 2024.
Discussion
Despite the significant negative impact of antenatal depression on the health of both women and fetuses in Sub-Saharan Africa, it has received less attention than postnatal depression (46). As a result, there is limited data on the pooled prevalence of antenatal depression and its associated factors among HIV-positive women in the region. Therefore, this systematic review and meta-analysis aim to synthesize the available evidence on the prevalence of antenatal depression and its predictors among HIV-positive women in SSA.
The pooled prevalence of antenatal depression among HIV-positive women in SSA was found to be 30.6% (95% CI, 19.8%-41.3%), consistent with studies done in Ukraine (27%) (47), China (28.5%) (48), and America (36%) (49). However, this finding is higher than a study done in Bangladesh (18%) (50). This divergence might be due to the difference in the gaps in the study period, and source populations; in which most of the participants in the later study (50) included all pregnant women, regardless of HIV status.
On the other hand, this figure is lower than the 44% reported in a study conducted in the United States (51). The difference might be attributed to the timing of the study; for instance, a study in the United States was done during the COVID-19 pandemic and due to its higher transmission rates, HIV-positive pregnant women faced higher rate of depression (52).
According to this meta-analysis, unmarried HIV-positive pregnant women were found to have three times higher odds of developing antenatal depression compared to married women. This could be attributed to the increased vulnerability of single women to economic, social, and psychological hardships, which may contribute to higher rates of depression (53). Research has also shown that partner support plays a significant role in reducing depression during pregnancy (54). Furthermore, societal norms and cultural factors may contribute to the triggering of depression, as single motherhood is often not socially accepted in most African countries.
In line with study done by Biaggi A. et. al., 2016 (55), the odds of the occurrence of antenatal depression among HIV-positive women with a previous history of depression were three times higher compared to their counterparts. This might be due to the physical and hormonal changes occurring during pregnancy and the recurrence of depressive symptoms (56). However, contrary to this finding, a study conducted in Pakistan found that a personal history of previous psychiatric illness was not significantly associated with antenatal depression (57).
Consistent with study done in United States (58), the odds of developing antenatal depression among HIV-positive pregnant women were higher among women experiencing HIV-related stigma as compared to those who had not experienced stigma. This could be attributed to the fact that acquiring HIV, a chronic lifelong disease, often leads to significant levels of stigma. Also, some patients may choose to withdraw from society to avoid this stigma, which can further contribute to feelings of exclusion or loneliness and exacerbate depression.
The study indicated that the odds of developing antenatal depression among HIV-positive women were two times higher among women who experienced IPV as compared to women who doesn’t experience IPV. This could be explained by the fact that psychological, physical, and sexual violence perpetrated by an intimate partner can exacerbate depression (59, 60).
Additionally, the findings of this systematic review indicate that there is no substantial correlation between non-compliance with antiretroviral therapy (ART) and the incidence of antenatal depression.
Strength and limitation
This systematic review has several strengths. Firstly, we utilized a robust search algorithm to include studies from multiple databases. Secondly, our study provides the first-ever prevalence estimates of antenatal depression among HIV-positive women in Sub-Saharan Africa. Additionally, we identified the factors associated with the development of depression in HIV-positive women, which is crucial for preventive public health efforts. However, there are certain limitations to this review. Firstly, we only included articles published in English. Secondly, the cross-sectional design of the included studies may limit our ability to establish a causal association between antenatal depression in HIV-positive women and the associated factors. Lastly, some factors were only reported in a single study, preventing the calculation of a pooled effect size.
Conclusion
The high prevalence of antenatal depression among HIV-positive women in SSA and the significant factors associated with it underscore the need for healthcare providers to prioritize the identification and management of antenatal depression in this population. Interventions addressing the underlying factors contributing to antenatal depression should be developed and implemented. Healthcare providers should also be trained to recognize the signs and symptoms of antenatal depression and provide appropriate support and referrals for mental health services when needed. Addressing antenatal depression among HIV-positive women in Sub-Saharan Africa can improve maternal and child health outcomes and reduce the burden of mental illness in this population.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
GA: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. MA: Writing – review & editing, Writing – original draft, Visualization, Software, Methodology, Formal analysis, Data curation, Conceptualization. AAd: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. DA: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Data curation, Conceptualization. TT: Writing – review & editing, Writing – original draft, Visualization, Supervision, Software, Formal analysis, Data curation, Conceptualization. DG: Writing – review & editing, Writing – original draft, Visualization, Validation, Software, Methodology, Data curation, Conceptualization. AAs: Writing – review & editing, Writing – original draft, Validation, Software, Methodology, Investigation, Formal analysis.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1385323/full#supplementary-material
Abbreviations
CI, Confidence Interval; HIV, Human Immunodeficiency Virus; OR, Odds ratio.
References
1. Austin M, Highest N, The Expert Working Group. Mental health care in th e perinatal period: Australian clinical practice guideline Centre of perinatal excellenc e depression during pregnancy. (2017).
2. Dadi AF, Miller ER, Bisetegn TA, Mwanri L. Global burden of antenatal depression and its association with adverse birth outcomes: an umbrella review. BMC Public Health. (2020) 20:1–16. doi: 10.1186/s12889-020-8293-9
3. WHO. HIV and AIDS (2023). Available online at: https://www.who.int/news-room/fact-sheets/detail/hiv-aids.
4. Chibanda D, Benjamin L, Weiss HA, Abas M. Mental, neurological, and substance use disorders in people living with HIV/AIDS in low-and middle-income countries. JAIDS J Acquired Immune Deficiency Syndr. (2014) 67:S54–67. doi: 10.1097/QAI.0000000000000258
5. Arseniou S, Arvaniti A, Samakouri M. HIV infection and depression. Psychiatry Clin Neurosci. (2014) 68:96–109. doi: 10.1111/pcn.12097
6. Kapetanovic S, Dass-Brailsford P, Nora D, Talisman N. Mental health of HIV-seropositive women during pregnancy and postpartum period: a comprehensive literature review. AIDS Behav. (2014) 18:1152–73. doi: 10.1007/s10461-014-0728-9
7. Arachchi NSM, Ganegama R, Husna AWF, Chandima DL, Hettigama N, Premadasa J, et al. Suicidal ideation and intentional self-harm in pregnancy as a neglected agenda in maternal health; an experience from rural Sri Lanka. Reprod Health. (2019) 16:1–7. doi: 10.1186/s12978-019-0823-5
8. Antelman G, Kaaya S, Wei R, Mbwambo J, Msamanga GI, Fawzi WW, et al. Depressive symptoms increase risk of HIV disease progression and mortality among women in Tanzania. J acquired Immune deficiency syndr. (2007) 44:470. doi: 10.1097/QAI.0b013e31802f1318
9. Mills EJ, Nachega JB, Bangsberg DR, Singh S, Rachlis B, Wu P, et al. Adherence to HAART: a systematic review of developed and developing nation patient-reported barriers and facilitators. PloS Med. (2006) 3:e438. doi: 10.1371/journal.pmed.0030438
10. Mills JC, Pence BW, Todd JV, Bengtson AM, Breger TL, Edmonds A, et al. Cumulative burden of depression and all-cause mortality in women living with human immunodeficiency virus. Clin Infect Dis. (2018) 67:1575–81. doi: 10.1093/cid/ciy264
11. Sin NL, DiMatteo MR. Depression treatment enhances adherence to antiretroviral therapy: a meta-analysis. Ann Behav Med. (2014) 47:259–69. doi: 10.1007/s12160-013-9559-6
12. Sheth SS, Coleman J, Cannon T, Milio L, Keller J, Anderson J, et al. Association between depression and nonadherence to antiretroviral therapy in pregnant women with perinatally acquired HIV. AIDS Care. (2015) 27:350–4. doi: 10.1080/09540121.2014.998610
13. Desalegn SY, Asaye MM, Temesgan WZ, Badi MB. Antenatal depression and associated factors among HIV-positive pregnant women in South Gondar zone public health facilities, northwest Ethiopia, a cross-sectional study. Clin Epidemiol Global Health. (2022) 16:101072. doi: 10.1016/j.cegh.2022.101072
14. Nhiwatiwa S, Patel V, Acuda W. Predicting postnatal mental disorder with a screening questionnaire: a prospective cohort study from Zimbabwe. J Epidemiol Community Health. (1998) 52:262. doi: 10.1136/jech.52.4.262
15. Tuthill EL, Pellowski JA, Young SL, Butler LM. Perinatal depression among HIV-infected women in KwaZulu-Natal South Africa: prenatal depression predicts lower rates of exclusive breastfeeding. AIDS Behav. (2017) 21:1691–8. doi: 10.1007/s10461-016-1557-9
16. Hartley M, Tomlinson M, Greco E, Comulada WS, Stewart J, Le Roux I, et al. Depressed mood in pregnancy: prevalence and correlates in two Cape Town peri-urban settlements. Reprod Health. (2011) 8:1–7. doi: 10.1186/1742-4755-8-9
17. Bonari L, Pinto N, Ahn E, Einarson A, Steiner M, Koren G. Perinatal risks of untreated depression during pregnancy. Can J Psychiatry. (2004) 49:726–35. doi: 10.1177/070674370404901103
18. Wagner GJ, McBain RK, Akena D, Ngo V, Nakigudde J, Nakku J, et al. Maternal depression treatment in HIV (M-DEPTH): study protocol for a cluster randomized controlled trial. Medicine. (2019) 98:27. doi: 10.1097/MD.0000000000016329
19. Dadi AF, Miller ER, Mwanri L. Postnatal depression and its association with adverse infant health outcomes in low-and middle-income countries: a systematic review and meta-analysis. BMC pregnancy childbirth. (2020) 20:1–15. doi: 10.1186/s12884-020-03092-7
20. Shen H, Magnusson C, Rai D, Lundberg M, Le-Scherban F, Dalman C, et al. Associations of parental depression with child school performance at age 16 years in Sweden. JAMA Psychiatry. (2016) 73:239–46. doi: 10.1001/jamapsychiatry.2015.2917
21. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PloS Med. (2006) 3:e442. doi: 10.1371/journal.pmed.0030442
22. Saxena S, Funk M, Chisholm D. World health assembly adopts comprehensive mental health action plan 2013–2020. Lancet. (2013) 381:1970–1. doi: 10.1016/S0140-6736(13)61139-3
23. Health FDRoEMo. National Mental Health Strategy 2012/13–2015/16. Public policy document, Federal Democratic Republic of Ethiopia (2012).
24. Abate HK, Mekonnen CK. Depression among HIV-positive pregnant women at northwest Amhara referral hospitals during COVID-19 pandemic. Dove Press. (2021) 14:4897–905. doi: 10.2147/RMHP.S320311
25. Abebe W, Gebremariam M, Molla M, Teferra S, Wissow L, Ruff A. Prevalence of depression among HIV-positive pregnant women and its association with adherence to antiretroviral therapy in Addis Ababa, Ethiopia. PloS One. (2022) 17:e0262638. doi: 10.1371/journal.pone.0262638
26. Harrington BJ, Pence BW, John M, Melhado CG, Phulusa J, Mthiko B, et al. Prevalence and factors associated with antenatal depressive symptoms among women enrolled in Option B+ antenatal HIV care in Malawi: a cross-sectional analysis. J Ment Health (Abingdon England). (2019) 28:198–205. doi: 10.1080/09638237.2018.1487542
27. Jones MU, Esber AL, Dear N, Bahemana E, Kibuuka H, Iroezindu M, et al. Ake JA et al: The pregnancy factor: the prevalence of depression among women living with HIV enrolled in the African Cohort Study (AFRICOS) by pregnancy status. Arch women’s Ment Health. (2021) 24:649–58. doi: 10.1007/s00737-021-01117-4
28. Ngocho JS, Watt MH, Minja L, Knettel BA, Mmbaga BT, Williams PP, et al. Depression and anxiety among pregnant women living with HIV in Kilimanjaro region, Tanzania. PloS One. (2019) 14:e0224515. doi: 10.1371/journal.pone.0224515
29. Nyamukoho E, Mangezi W, Marimbe B, Verhey R, Chibanda D. Depression among HIV positive pregnant women in Zimbabwe: a primary health care based cross-sectional study. BMC pregnancy childbirth. (2019) 19:1–7. doi: 10.1186/s12884-019-2193-y
30. Osborn L, Ronen K, Larsen AM. Antenatal depressive symptoms in Kenyan women living with HIV: contributions of recent HIV diagnosis. stigma partner viol. (2022) 34:69–77. doi: 10.1080/09540121.2021.1981216
31. Peltzer K, Rodriguez VJ, Jones D. Prevalence of prenatal depression and associated factors among HIV-positive women in primary care in Mpumalanga province, South Africa. SAHARA-J: J Soc Aspects HIV/AIDS. (2016) 13:60–7. doi: 10.1080/17290376.2016.1189847
32. Regan M, Muhihi A, Saleh A, Duggan CP, Ulenga N, Alwy Al-Beity FM, et al. Antenatal depression and adverse birth outcomes among pregnant women living with HIV in Dar es Salaam, Tanzania. J Affect Disord. (2023) 339:82–8. doi: 10.1016/j.jad.2023.07.047
33. Shoptaw S, Moucheraud C, Mvududu R, Essack Z, Gorbach PM, Myer L, et al. Maliwichi M et al: Prevalence and incidence of probable perinatal depression among women enrolled in Option B+ antenatal HIV care in Malawi. J Acquir Immune Defic Syndr. (2018) 239:115–22. doi: 10.1016/j.jad.2018.06.001
34. Yator O, Mathai M, Vander Stoep A, Rao D, Kumar M. Risk factors for postpartum depression in women living with HIV attending prevention of mother-to-child transmission clinic at Kenyatta National Hospital, Nairobi. AIDS Care. (2016) 28:884–9. doi: 10.1080/09540121.2016.1160026
35. Habib NA, Daltveit AK, Bergsjø P, Shao J, Oneko O, Lie RT. Maternal HIV status and pregnancy outcomes in northeastern Tanzania: a registry-based study. BJOG: Int J Obstet Gynaecol. (2008) 115:616–24. doi: 10.1111/j.1471-0528.2008.01672.x
36. Lopez M, Figueras F, Hernandez S, Lonca M, Garcia R, Palacio M, et al. Association of HIV infection with spontaneous and iatrogenic preterm delivery: effect of HAART. Aids. (2012) 26:37–43. doi: 10.1097/QAD.0b013e32834db300
37. Le Doare K, Bland R, Newell M-L. Neurodevelopment in children born to HIV-infected mothers by infection and treatment status. Pediatrics. (2012) 130:e1326–44. doi: 10.1542/peds.2012-0405
38. Schwartz S, Mudavanhu M, Hanrahan C, France H, Nel J, Mutunga L, et al. Tibebu NS et al: Depression, anxiety and stress among HIV-positive pregnant women in Ethiopia during the COVID-19 pandemic. AIDS Care. (2023) 117:317–25. doi: 10.1093/trstmh/trac126
39. Halim N, Beard J, Mesic A, Patel A, Henderson D, Hibberd P. Intimate partner violence during pregnancy and perinatal mental disorders in low and lower middle income countries: A systematic review of literature, 1990–2017. Clin Psychol Rev. (2018) 66:117–35. doi: 10.1016/j.cpr.2017.11.004
40. Leigh B, Milgrom J. Risk factors for antenatal depression, postnatal depression and parenting stress. BMC Psychiatry. (2008) 8:1–11. doi: 10.1186/1471-244X-8-24
41. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. (2021) 88:105906. doi: 10.1016/j.ijsu.2021.105906
42. Institute JB. JBI critical appraisal checklist for analytical cross sectional studies. Diakses pada. (2017) 22:2019–05.
43. Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to meta-analysis. John Wiley & Sons (2021). doi: 10.1002/9781119558378
44. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
45. Cooper H, Hedges LV, Valentine JC. The handbook of research synthesis and meta-analysis. Russell Sage Foundation (2019). Available at: https://www.russellsage.org/publications/handbook-research-synthesis-and-meta-analysis-second-edition.
46. Shidhaye P, Giri P. Maternal depression: a hidden burden in developing countries. Ann Med Health Sci Res. (2014) 4:463–5. doi: 10.4103/2141-9248.139268
47. Bailey H, Malyuta R, Semenenko I, Townsend CL, Cortina-Borja M, Thorne C. EuroCoord UECSi: Prevalence of depressive symptoms in pregnant and postnatal HIV-positive women in Ukraine: a cross-sectional survey. Reprod Health. (2016) 13:1–10. doi: 10.1186/s12978-016-0150-z
48. Zeng Y, Cui Y, Li J. Prevalence and predictors of antenatal depressive symptoms among Chinese women in their third trimester: a cross-sectional survey. BMC Psychiatry. (2015) 15:1–7. doi: 10.1186/s12888-015-0452-7
49. Bonacquisti A, Geller PA, Aaron E. Rates and predictors of prenatal depression in women living with and without HIV. AIDS Care. (2014) 26:100–6. doi: 10.1080/09540121.2013.802277
50. Nasreen HE, Kabir ZN, Forsell Y, Edhborg M. Prevalence and associated factors of depressive and anxiety symptoms during pregnancy: a population based study in rural Bangladesh. BMC women’s Health. (2011) 11:1–9. doi: 10.1186/1472-6874-11-22
51. Waldron EM, Burnett-Zeigler I, Wee V, Ng YW, Koenig LJ, Pederson AB, et al. Mental health in women living with HIV: the unique and unmet needs. J Int Assoc Providers AIDS Care (JIAPAC). (2021) 20:2325958220985665. doi: 10.1177/2325958220985665
52. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA netw Open. (2020) 3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686
53. Stack RJ, Meredith A. The impact of financial hardship on single parents: An exploration of the journey from social distress to seeking help. J Family econ Issues. (2018) 39:233–42. doi: 10.1007/s10834-017-9551-6
54. Baranowska-Rataj A, Matysiak A, Mynarska M. Does lone motherhood decrease women’s happiness? Evidence from qualitative and quantitative research. J Happiness Stud. (2014) 15:1457–77. doi: 10.1007/s10902-013-9486-z
55. Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J Affect Disord. (2016) 191:62–77. doi: 10.1016/j.jad.2015.11.014
56. Yanikkerem E, Ay S, Mutlu S, Goker A. Antenatal depression: prevalence and risk factors in a hospital based Turkish sample. J Pak Med Assoc. (2013) 63:472–7.
58. Rao D, Feldman BJ, Fredericksen RJ, Crane PK, Simoni JM, Kitahata MM, et al. A structural equation model of HIV-related stigma, depressive symptoms, and medication adherence. AIDS Behav. (2012) 16:711–6. doi: 10.1007/s10461-011-9915-0
59. Van Parys A-S, Verhamme A, Temmerman M, Verstraelen H. Intimate partner violence and pregnancy: a systematic review of interventions. PloS One. (2014) 9:e85084. doi: 10.1371/journal.pone.0085084
Keywords: antenatal depression, HIV-positive women, Sub-Saharan Africa, systematic review, meta-analysis
Citation: Abebe GF, Alie MS, Adugna A, Asemelash D, Tesfaye T, Girma D and Asres A (2024) Antenatal depression and its predictors among HIV positive women in Sub-Saharan Africa; a systematic review and meta-analysis. Front. Psychiatry 15:1385323. doi: 10.3389/fpsyt.2024.1385323
Received: 12 February 2024; Accepted: 28 May 2024;
Published: 11 June 2024.
Edited by:
Laura Orsolini, Marche Polytechnic University, ItalyReviewed by:
Chonnakarn Jatchavala, Prince of Songkla University, ThailandGiulio Longo, Marche Polytechnic University, Italy
Copyright © 2024 Abebe, Alie, Adugna, Asemelash, Tesfaye, Girma and Asres. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gossa Fetene Abebe, Feteneg2119@gmail.com
†ORCID: Gossa Fetene Abebe, orcid.org/0000-0002-8495-3022
 Gossa Fetene Abebe
Gossa Fetene Abebe Melsew Setegn Alie
Melsew Setegn Alie Amanuel Adugna
Amanuel Adugna Daniel Asemelash
Daniel Asemelash Tamirat Tesfaye
Tamirat Tesfaye Desalegn Girma
Desalegn Girma Abyot Asres2
Abyot Asres2