- Department of Psychiatry, Qiqihar Medical University, Qiqihar, China
Background: Globally, early-life adversity (ELA) is linked to an increased risk of developing depression in adulthood; however, only a few studies have examined the specific effects of various types of ELA on depression in children and adolescents. This meta-analysis explores the association between the subtypes of ELA and the risk for youth-onset depression.
Methods: We searched three electronic databases for reporting types of ELA, namely, emotional abuse, physical abuse, sexual abuse, emotional neglect, physical neglect, family conflict/violence, divorce, low socioeconomic status, and left-behind experience, associated with depression before the age of 18 years. Our meta-analysis utilized the odds ratio (OR) and relied on a random effects model. Large heterogeneous effects were detected. Some factors moderated the association between ELA and depression in youths. The homogeneity of variance test and meta-regression analysis were used to detect these relationships.
Results: A total of 87 studies with 213,006 participants were ultimately identified via several strategies in this meta-analysis. Individuals who experienced ELA were more likely to develop depression before the age of 18 years old than those without a history of ELA (OR=2.14; 95% CI [1.93, 2.37]). The results of the subgroup analysis revealed a strong association between ELA and depression in youth, both in terms of specific types and dimensions. Specifically, emotional abuse (OR = 4.25, 95% CI [3.04, 5.94]) was more strongly related to depression in children and adolescents than other forms of ELA were. For both dimensions, threat (OR = 2.60, 95% CI [2.23, 3.02]) was more closely related to depression than deprivation was (OR = 1.76, 95% CI [1.55, 1.99]).
Conclusion: This meta-analysis revealed that the adverse effects of a broader consideration of ELA on the risk of youth-onset depression vary according to the subtypes of ELA.
Systematic review registation: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42023405803, identifier 42023405803.
1 Introduction
According to the World Health Organization in 2019, depression is the fourth leading cause of illness and disability in children and adolescents, seriously affecting their physical health and academic life and further placing a heavy economic burden on families and society (1). The prevalence of depression in children and adolescents has reached 15%-20% (2). In particular, in recent years, the COVID-19 pandemic has had a more serious impact on children and adolescents with mood disorders (3, 4). According to the 2022 National Depression Blue Book, the global burden of mental disorders has increased since the pandemic, with a surge of 53 million patients with depression (an increase of up to 27.6%), with 50% of patients with depression being school-age students (5). For these reasons, identifying the risk factors for depression in children and adolescents is a key issue for prevention and intervention. Some relatively common risk factors for depression in young individuals include genetic factors, such as temperament (6), and environmental factors, such as early-life adversity (7). In recent years, interest in exploring the impact of early-life adversity on depression in children and adolescents in terms of cumulative risk to the family has been growing (8).
Early life adversity (ELA) refers to the adverse environment experienced by individuals in their early years (infancy, childhood, and adolescence) and may be a significant risk factor for depression in children and adolescents (9, 10). More than half of youth have experienced at least one form of ELA (e.g., abuse, neglect, poverty, or loss of a parent), and youths who experience ELA develop an increased risk for mood disorders by age 18 (11). Recent meta-analyses suggest that ELA is linked to a twofold increase in the risk for major depressive disorder in adolescents (7). In addition, some studies have shown that ELA can be further categorized into two distinct subtypes of threat and deprivation (12), with threat referring to life-threatening, injurious, sexually assault, or other harm to an individual’s physical integrity, and deprivation primarily refers to a lack of expected environmental input in the cognitive (e.g., language) and social domains and a lack of complexity of environmental stimuli appropriate to the species and age (12). Based on threat and deprivation typology is a novel conceptual framework for examining the impact of early family adversity on an individual’s neurodevelopment, which in turn leads to different forms and degrees of physical and psychological problems (12, 13). Subtyping is thus more useful for synthesizing and quantitatively analyzing the relationship between ELA and adolescent depression.
While these studies provide valuable information, certain limitations are noteworthy. First, previous meta-analytic studies have focused primarily on adult populations (14, 15), with less focus on exploring the effects of ELA on MDD in adolescent populations. This is pertinent because the etiology, clinical presentation, and course of depression differ between adolescents and adults (16), and it is reasonable to assume that the nature of the relationship between ELA and depression may also vary depending on the stage of development (7). Second, previous meta-analytic studies on the relationship between ELA and depression have shown a more homogenous form of ELA, focusing mainly on childhood traumatic experiences (17). Based on the cumulative risk model and the family stress model, the measures of family risk, in addition to family climate risk (e.g., child abuse and neglect, domestic violence), family structural risk (e.g., divorce), and family resource insufficiency risk (e.g., poverty), are underexplored in terms of their relationship with depression (18). Third, the findings of the few studies on ELA and adolescent depression are not entirely consistent with each other; this is due not only to the choice of the specific form of ELA or its measurement (7) but also to the small number of studies that have opted to enter the meta-analysis, limiting the scope of the analysis of the moderating effects that influence the relationship.
In summary, the current study explored the relationships between the nine specific forms of ELA (including sexual abuse, physical abuse, psychological abuse, physical and emotional neglect, divorce, being left behind, low socioeconomic status, and domestic violence) and its subtypes (threat and deprivation) and risk for youth-onset depression via meta-analysis, as well as the moderating variables affecting the relationship between ELA and depression. The meta-analytic technique not only integrates the results of multiple studies and effectively reduces the measurement and sampling errors that exist in the results of a single study but also helps identify the extent to which different ELA experiences impact depression based on a quantitative review of many research results and a comprehensive analysis technique to provide a certain guiding value for the intervention of clinical mood disorders. Specifically, this study used meta-analytic techniques to answer the following two questions: first, to what extent do the nine ELA experiences and two subtypes influence depression? Second, what demographic and/or methodological factors moderate the association between ELA and depression?
2 Methods
This meta-analysis followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (19), and the protocol was registered in the PROSPERO system (registration number CRD42023405803).
2.1 Inclusion and exclusion criteria
The studies included the following criteria in this meta-analysis: (1) operational definition of ELA in the research included nine specific forms (emotional abuse, physical abuse, sexual abuse, emotional neglect, physical neglect, family conflict/violence, divorce, low socioeconomic status, and left-behind experience); (2) depression prior to a mean age of 18 years old and evaluation of relevant depression measures; (3) empirical studies must have reported numerical results, and the effect sizes of the relationships between subtypes of ELA and depression were directly obtained; and (4) selection of only one article when multiple articles were published using the same set of data. The exclusion criteria were as follows: (1) studies on adult samples; (2) the nine specific ELA types were not mentioned in the study or mixed together (e.g., childhood maltreatment) and could not be obtained in relation to depression; (3) lack of sufficient data needed to calculate effect size; and (4) conference abstracts with no empirical data (e.g., reviews, editorials).
2.2 Search strategy
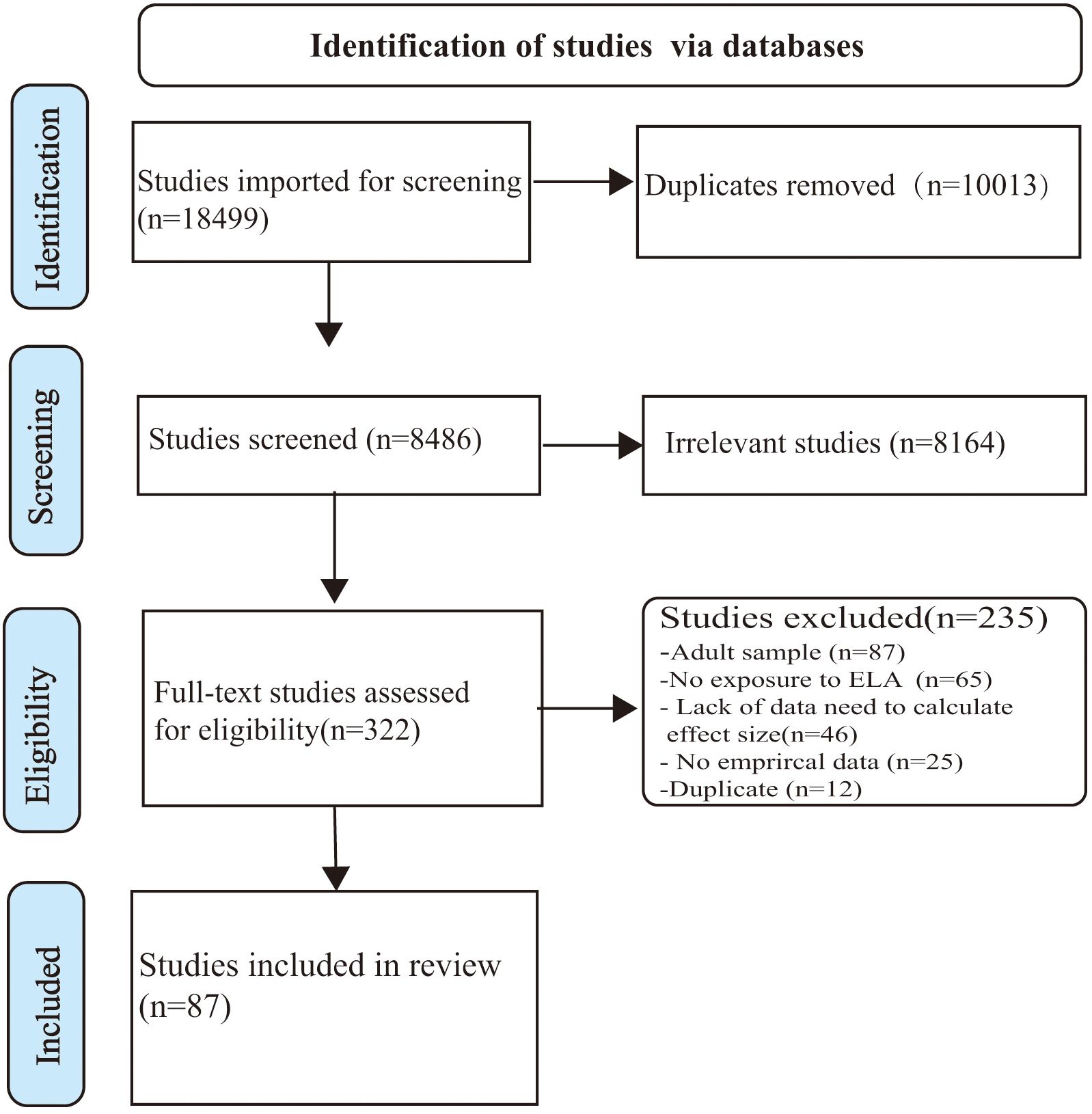
First, we conducted computer-based searches in the Web of Science and PubMed for articles published in English and the CNKI Database for articles published in Chinese from inception to December 2022. These articles were searched using the following keywords (or stems): (“Affective Disorder” OR “Mood Disorder” OR “Depressive symptoms” OR Depress OR MDD) AND (Child OR Childhood OR Children OR Adolescent OR Adolescence) AND (“Early life stress” OR “Early life adversity” OR “Adverse childhood experiences” OR Maltreatment OR “Physical abuse” OR “Sexual abuse” OR “Emotional abuse” OR “Psychological abuse” OR Trauma OR Neglect OR “Domestic violence” OR Divorce OR “Socioeconomic status” OR Left-behind). Second, we consulted the bibliography using both forward and backward searches to find additional studies, especially relevant meta-analyses and systematic reviews. The early life adversity subtypes were we have checked they are diplayed correctly clearly defined in this meta-analysis (see Supplementary 1). The results are outlined in the PRISMA flow chart (Figure 1).
2.3 Data extraction
Duplicate documents were removed using Endnote X9 and then independently screened by two authors. The effect sizes, moderator codes, and study quality assessments were extracted with essentially the same results. Disagreements were resolved in consensus meetings, and the lead authors made a final determination. Rater agreement at the screening stage was 96%.
2.4 Moderator variables of encoding
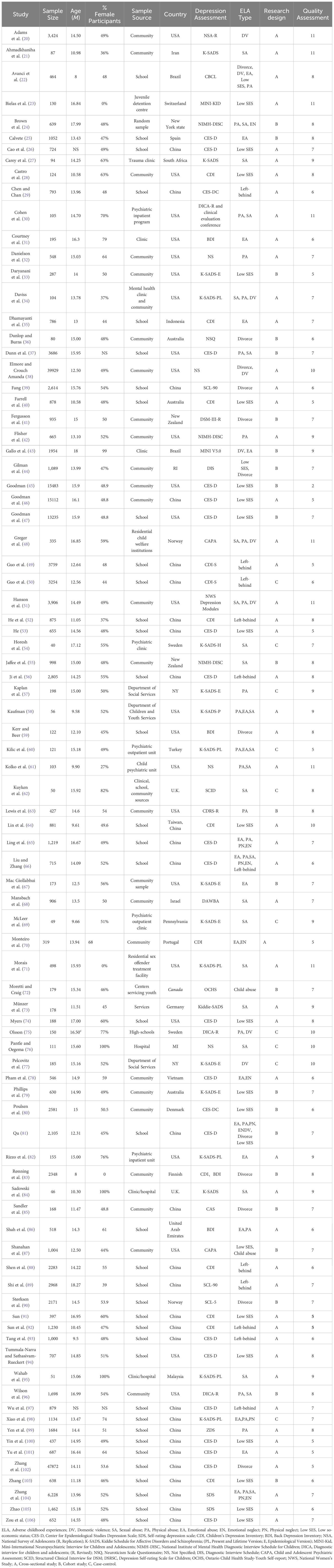
The studies included in the meta-analysis were coded as follows when available (see Table 1). Study information (first author + publication year), sample size, female rates, average age, sample source (school, community, services, clinic/hospital), country (countries were coded as developing or developed for data analysis), assessment tools of depression, research design (cross-sectional, case-control, and cohort study), and subtypes of ELA (dimensions: threat and deprivation; the former in this study included emotional abuse, physical abuse, sexual abuse, and family violence, and the latter mainly included low socioeconomic status, divorce, and being left with two parents away).
In terms of the number of individual studies by country, China (n=29) and the United States (n=27) accounted for the majority of studies, and most of the remaining countries only had one or two studies. Depression measurement tools were dominated by the CES-D (n=22), CDI (n=13), and K-SADS (n=16), while the use of the BDI, CBCL, SCL-90, and other instruments was less relevant. The research methods used were mostly cross-sectional studies (n=54), whereas cohort studies (n=23) and case−control studies (n=10) were relatively rare.
2.5 Quality evaluation
The studies included in this meta-analysis included cross-sectional studies, cohort studies, and case-control studies. We coded study quality using the Agency for Healthcare Research and Quality (AHRQ) to assess cross-sectional studies, and the AHRQ score was 11 points. Each entry is given a score of 1 point, with 8 points or more indicating high quality, 4-7 points indicating medium quality, and 0-3 points indicating low quality (107). We used the Newcastle Ottawa Scale (NOS) to assess cohort studies and case−control studies, with NOS scores of 9 points (108). A score of 7 or higher indicates high quality, 4-6 indicates medium quality, and 0 to 3 indicates low quality (see Table 1).
2.6 Statistical analysis
2.6.1 Calculation of effect sizes
The correlation coefficient (r), standardized mean difference (d), or odds ratio (OR) for the relationship between adverse childhood experiences and depression in childhood or adolescence were reported for these 101 effect sizes. The extracted data were converted to OR effect sizes, which were used to integrate the relationship between ELA and depression in children and adolescents. We used CMA 2.0 to conduct statistical analyses, which allowed the direct input of multiple effect sizes, which can be converted into ORs (109). First, the effect size r is converted to d, and then d is converted to OR. The conversion formula is as follows:
Heterogeneity test The standard Cochran Q test (calculation of I2-value) was used to test the heterogeneity of the effect size. When I 2 ≧ 50, indicating the presence of heterogeneity, a random effects model was chosen (110).
2.6.2 Publication bias test
Publication bias may severely affect the results of the meta-analysis. Generally, the publication bias of a meta-analysis is comprehensively evaluated using funnel plots, the classic fail-safe N test (no publication bias when the N value is greater than 5k+10), and Egger’s test (no publication bias when the intercept in the regression equation is zero). Among the three methods, Egger’s test was relatively more objective and accurate in assessing publication bias.
2.6.3 Meta-analysis procedure
First, the relationships between the different forms of ELA and depression in children and adolescents were explored by meta-analytic techniques, and then, demographic and methodological factors were tested to determine whether they moderated the association between ELA and depression. Specifically, the homogeneity of variance test in the Q test was used for categorical moderated variables, and the moments of random effects model regression analysis were used for continuous variables.
3 Results
3.1 ELA (all forms) and depression
In this meta-analysis, a total of 87 studies with 136 effect sizes and 213,006 unique individuals were included to examine the relationship between ELA and depression in children and adolescents (see Table 1), with a broad range of ORs (see Supplementary Figures S1–S9). Random effects meta-analysis showed that those who experienced ELA are more likely to suffer from depression in childhood or adolescence than those with no history of ELA (OR = 2.14, 95% CI = 1.93, 2.37), an effect that differed significantly from zero (Z = 14.65, p < 0.001). There was significant heterogeneity across studies (Q100 = 2740.73, p < 0.001, I 2 = 95.04%), and we further conducted moderation effect analysis (see Table 2).
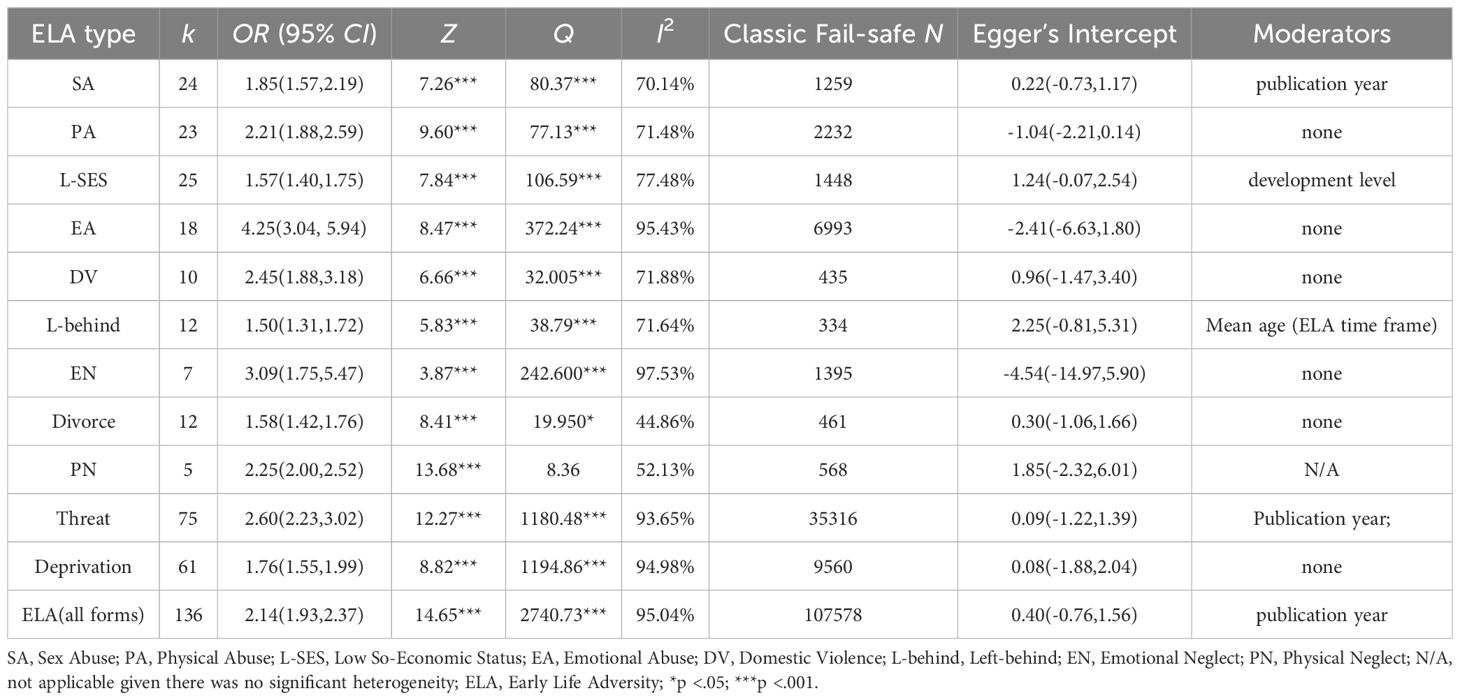
Table 2. Results From Random-Effects Meta-analyses for Each Type of ELA Examined in Relation to depression.
3.2 Specific types of ELA and depression
Table 2 presents the results of random-effects meta-analyses for each of the nine types of ELA examined in relation to the risk for depression. The forest plots are presented in Supplementary Figures S1–S9. Specifically, the risk factors for depression for each of the nine specific forms of early-life adversity, in order of magnitude, were emotional abuse (OR = 4.25, 95% CI = 3.04, 5.94), emotional neglect (OR = 3.09, 95% CI = 1.75, 5.47), domestic violence (OR = 2.45, 95% CI = 1.88, 3.18), physical neglect (OR = 2.25, 95% CI = 2.00, 2.52), physical abuse (OR = 2.21, 95% CI = 1.88, 2.59), sexual abuse (OR = 1.85, 95% CI = 1.57, 2.19), low socioeconomic status (OR = 1.57, 95% CI = 1.40, 1.75), divorce (OR = 1.58, 95% CI = 1.42, 1.76), and being left behind (OR = 1.50, 95% CI = 1.31, 1.72) (see Table 2). Moreover, in terms of threat and deprivation, which are two types of ELA, threats had a more severe impact on depression in children and adolescents (OR = 2.60, 95% CI = 2.23, 3.02) than did the deprivation of adversity experiences (OR = 1.76, 95% CI = [1.55, 1.99]). Similarly, we also conducted a moderating effect analysis for each subtype of ELA in which there was significant heterogeneity.
3.3 Moderating effect test
We examined the role of each moderating variable separately in the relationship between all forms or subtypes of ELA and depression in children and adolescents (see Table 2). First, development level was coded as a dummy variable based on whether the level of socioeconomic development was indicative of a developing or developed country. Both sets of analyses revealed a statistically significant effect of development level on the association between low social status and depression in children and adolescents. Specifically, the studies that were based in developing countries (k = 11; OR =1.79; 95% CI = [1.60, 2.01]) had a larger estimated effect size than did the studies that included developed countries (k = 14; OR = 1.36; 95% CI = [1.18, 1.57]).
Second, there was a strong positive moderating effect of year of publication on ELA and youth-onset depression. The ELA variables involved were primarily all forms of ELA (slope = 0.02; 95% CI = [0.007, 0.028]; Z = 3.18; p < 0.01; k = 137), threat (slope = 0.025; 95% CI = [0.009, 0.041]; Z = 3.081; p < 0.01; k = 76), and SA (slope = 0.023; 95% CI = [0.006, 0.041]; Z = 2.635; p < 0.01; k = 25). Third, the ELA time frame had an important negative moderating effect on the relationship between being left behind and depression in children and adolescents. (slope = -0.054; 95% CI = [-0.105, -0.003]; Z = -2.072; p < 0.05; k = 12). The results revealed that the effects of parental absence or lack of resources on depression in children and adolescents weakened or diminished with age.
3.4 Heterogeneity test
The results of the heterogeneity test for the subtypes of ELA and depression in childhood or adolescence are shown in Table 2. The results of Table 2 show that the Q test was significant, where I2 > 50%, except divorce, indicating that there was substantial heterogeneity in the effect sizes of most of the studies in the meta-analysis and that the random effects model selected for the meta-analysis was accurate.
3.5 Publication bias test
First, a funnel plot was used to check for publication bias in the meta-analysis, as shown in Supplementary Figure S10. According to the funnel plots, the literature on the relationship between ELA and depression in childhood or adolescence was more evenly distributed on both sides of the total effect size, which suggested that there may be no publication bias in the studies. Second, the classic fail-safe N and Egger’s regression methods were examined overall (see Table 2). The classic fail-safe N values were sufficiently large to indicate the absence of serious publication bias (>5k+10), and the results of Egger’s regression test showed that the intercept was not significantly different from zero, which means that there was no serious publication bias in this meta-analysis.
4 Discussion
In terms of overall ELA, individuals exposed to ELA during childhood or adolescence were twice more likely to be at risk of depression than those not exposed to ELA, which was not entirely consistent with other studies. For example, LeMoult (7) found that ELA-exposed individuals were 2.5 times more likely to be at risk of depression than those not exposed to ELA. Similarly, Nelson et al. (111) found that any type of abuse was related to depression in adults (OR = 2.66). Notably, differences in outcome indicators may be due to differences in the specific forms of early adversity explored and factors such as the study population and methods, which results in differences in the fitted indicators. Considering ELA more generally seems to be a comparable environmental risk factor for depression onset in both youth and adults. While meta-analytic studies were unable to fit the cumulative effects of ELA, there was general agreement that ELA exhibited a dose-response relationship for depression in children and adolescents (112, 113).
We also examined the effects of nine different types of ELA. Emotional abuse, physical abuse, sexual abuse, emotional neglect, physical neglect, family conflict/violence, divorce, low socioeconomic status, and being left behind were associated with a significantly greater risk for depression than for youth-onset depression. The results suggested that emotional abuse was more strongly associated with depression than other forms of adversity were, which was consistent with previous research (7, 17). Emotional abuse was a more effective predictor of periodic major depression than sexual abuse, physical abuse, and neglect (114). Emotional abuse had a very prominent impact on depression in both youth and adult populations. Because emotional abuse can be a direct attack on a person’s self-worth, it is more likely to lead to negative perceptions and hopelessness depression. The non-physical forms of rejection or hostile treatment can be strongly associated with depressive disorders at different ages (115). The present study also showed that neglect (both emotional and physical neglect) can have a significant impact on depression in children and adolescents, especially emotional neglect, which is second only to emotional abuse in terms of its impact on depression (15). In terms of causes, emotional neglect and emotional abuse share the same psycho-cognitive mechanisms that may lead to feelings of powerlessness and lower self-esteem in children and adolescents, resulting in the development of emotional disorders such as depression (116).
Notably, physical abuse was more strongly associated with depression than was sexual abuse, which is consistent with the results of LeMoult (7) but different from the results of an adult population study (117). The reason for this may be that negative consequences from sexual abuse may manifest in other ways in children and adolescents, such as post-traumatic stress disorder (PTSD) (118), suicide (119), and the risk of sexual promiscuity (120). Furthermore, while the majority of offenders of physical abuse are inside the home, the majority of instances of sexual abuse occur outside of the home. Thus, physical abuse may undermine the sense of safety in the family environment more directly than sexual abuse (7), and a lack of safety can have lasting and profound effects on mood disorders in youth (121, 122).
The importance of a sense of security in the family for the development of mental health was further corroborated by domestic violence and divorce. First, the results of this study suggested that the strength of the association between domestic violence and depression was second only to that between emotional abuse and neglect. Domestic violence can directly contribute to family disharmony and is the main form of adversity that causes a high level of insecurity in children and adolescents. In addition, it is an independent and effective predictor of developmental psychopathology (123) and often coexists with other forms of adversity (124). However, the results of this study showed that divorce was less strongly associated with depression than domestic violence was, which is consistent with the divorce stress release hypothesis (125). Divorce is a stressful life event, and parental conflict is an ongoing chronic stressor for children and adolescents. If children live in an environment with frequent conflict, hostility, and even violence between parents before divorce, then parental divorce may provide children with relief from constant chronic stress, which may even have a stress-releasing effect and even alleviate depression after parental divorce (126, 127). On the other hand, this finding also reflects the importance of the sense of security brought by a harmonious family environment atmosphere for the emotional health development of children and adolescents. The results of the present study demonstrated the small effect size of divorce associated with depression in children and adolescents and the tendency for the negative effects of divorce on youth to gradually decrease over time, which further reflects the view that divorce has a limited impact (128).
This study also revealed a strong association between low socioeconomic status and youth-onset depression, but a recent meta-analytic study (7) revealed no direct association between poverty and depression in children and adolescents. There may be two reasons for this. First, the two fit different indicators, with low socioeconomic status accounting for not only income but also parental occupation and education level, especially parental education level. Research has shown that children of highly educated parents exhibit fewer mental health problems in stressful life situations (129). Additionally, the results of this study indicate that the level of development of the national economy has different effects on the relationship between low SES and youth depression. Low SES is more closely related to adolescent depression in developing countries than in developed countries. This result suggested that low SES might not be “low” in developed countries relative to developing countries and that the level of disparity between SESs is not large. Studies have shown that low SES is more strongly associated with depression in black populations than in white populations (28). In summary, the disadvantage of socioeconomic status may be an important risk factor for depression in youth, and a reduction in socioeconomic inequalities and interventions for families with low parental education might help reduce depression in youths (104, 129).
Left-behind experience refers to the prolonged separation of children from their parents the age of 16 because their parents work outside the country. Children and adolescents who suffered from being left behind have received attention from the state and scholars. The results of the meta-analysis revealed that the sample source was mainly from the central and western regions of China (mainly Chongqing, Sichuan, Anhui, and Guizhou), and the results of this study suggest that the left-behind experience is also a risk predictor of depression, which may increase emotional neglect and weaken parent-child cohesion, thus leading to depression (92). However, the effect size of being left behind during childhood and adolescence associated with depression was relatively small and tended to diminish with age. In summary, parents should try to strengthen their contact with their children and parents avoid prolonged separation from their children in the early years, which can help reduce depression and anxiety in left-behind children (130).
The above results fully illustrate that subtypes of ELA can have different degrees of impact on depression during childhood and adolescence. However, meta-analytic studies that can clarify the variability and plasticity of early adverse experiences are of greater practical value and significance. In terms of both dimensions of ELA, children and adolescents are at greater risk of depression when exposed to a poor family upbringing or domestic violence than being deprived when experiencing poverty or parental absence. The moderated analysis by year of publication revealed that the early-life adversity and threat dimensions increase in relation to depression over time, indicating that increasing attention to the impact of early-life adversity on depression in youth may also reflect that the impact of the COVID-19 pandemic could increasing the type, intensity, and duration of early-life adversity, which in turn may produce a range of mental health problems such as depression and anxiety (131, 132). However, from an intervention perspective, threat adversity is more malleable or intervening, whereas deprivation experiences such as divorce, retention, and poverty are less malleable or intervening, suggesting that positive interventions for threats may have a more important impact on improving psychopathology in youth, which has important implications for future interventions.
4.1 Strengths and limitations
There are several limitations in our meta-analysis. First, the sample of different potential moderating variables in this study was small and unevenly distributed, which may affect the results of the moderation analysis to some extent. Second, the present study only considered ELA in the context of unfavorable family environments originating from the family and ignored the influence of micro-systems outside the family on adolescents’ depressive relationships, such as peer isolation and bullying. Third, the majority of the studies included in this meta-analysis were cross-sectional studies, and causal inferences on the relationship between early adversity and depression could not be made for most cross-sectional studies. Fourth, according to the cumulative risk model, separate risk factors do not act individually; rather, they tend to manifest themselves in the form of clusters, but the current data do not allow us to address the cumulative effects of ELA.
Future research can be conducted in the following areas. First, the present meta-analytic study identified ELA as a risk factor for depression in children and adolescents, and we need to further explore the relationships between ELA and other affective disorders or behavioral problems. Second, we need to further examine the neuro-biological mechanisms by which exposure to ELA may increase an individual’s risk of depression and the protective mechanisms of psychological resilience resources by which exposure to ELA may decrease the risk of depression. In conclusion, focusing on the risk and protective factors for mood disorders in youths and their mechanisms of action can help children and adolescents develop emotional health. Moreover, the quality of the literature included can be improved in the future by expanding the number of databases searched and the way they are searched, facilitating in-depth analysis.
5 Conclusion
The present results highlight the complexity of the relationship between ELA and depression in children and adolescents. Specifically, emotional abuse was more strongly related to depression in children and adolescents than other forms of ELA. In both dimensions, threat was more closely related to depression than deprivation.
The results of this study have implications for interventions. First, educators and parents should pay close attention to threat-related forms of adversity, especially emotional abuse, which has the greatest impact on emotional problems such as depression. Conscious efforts to reduce or eliminate childhood abuse and neglect, and domestic violence and a favorable emotional climate in the familial environment are important for positive adolescent development. In addition, deprivation adversities such as low socioeconomic status, being left behind, and divorce have relatively small effects on depression in adolescents relative to threats. According to the moderating effect analysis, the effect of left-behind experience on adolescents’ depression diminishes with age, which also suggests that the older age at which children and adolescents experience deprivation, the lower their risk of depression is.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
ZY: Writing – original draft, Formal analysis. YC: Writing – original draft, Data curation. TS: Writing – original draft, Data curation. PL: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was funded by Key Project of Social Science Foundation of Qiqihar Medical College (QYSKL2022-03ZD)
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1378807/full#supplementary-material
References
1. National Institute of Mental Health. Major depression (2019). Available online at: https://www.nimh.nih.gov/health/statistics/major-depression. Accessed (August 10, 2023)
2. Thapar A, Collishaw S, Pine DS, Thapar AK. Depression in adolescence. Lancet. (2012) 379:1056–67. doi: 10.1016/S0140-6736(11)60871-4
3. Guessoum SB, Lachal J, Radjack R, Carretier E, Minassian S, Benoit L, et al. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. (2020) 291:113264. doi: 10.1016/j.psychres.2020.113264
4. Jiao WY, Wang LN, Liu J, Fang SF, Jiao FY, Pettoello-Mantovani M, et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. (2020) 221:264–6. doi: 10.1016/j.jpeds.2020.03.013
5. National Blue Book on Depression (2022). Available online at: https://www.163.com/dy/article/HICKKLGH0514ADB4.html. Accessed (February 19, 2024)
6. Compas BE, Connor-Smith J, Jaser SS. Temperament, stress reactivity, and coping: Implications for depression in childhood and adolescence. J Clin Child Adolesc Psychol. (2004) 33:21–31. doi: 10.1207/S15374424JCCP3301_3
7. LeMoult J, Humphreys KL, Tracy A, Hoffmeister JA, Ip E, Gotlib IH. Meta-analysis: exposure to early life stress and risk for depression in childhood and adolescence. J Am Acad Child Adolesc Psychiatry. (2020) 59:842–55. doi: 10.1016/j.jaac.2019.10.011
8. Stein CR, Sheridan MA, Copeland WE, Machlin LS, Carpenter KL, Egger HL. Association of adversity with psychopathology in early childhood: Dimensional and cumulative approaches. Depression Anxiety. (2022) 39:524–35. doi: 10.1002/da.23269
9. Stroud CB, Chen FR, Doane LD, Granger DA. Individual differences in early adolescents’ latent trait cortisol (LTC): Relation to recent acute and chronic stress. Psychoneuroendocrinology. (2016) 70:38–46. doi: 10.1016/j.psyneuen.2016.04.015
10. Iob E, Lacey R, Giunchiglia V, Steptoe A. Adverse childhood experiences and severity levels of inflammation and depression from childhood to young adulthood: a longitudinal cohort study. Mol Psychiatry. (2022) 27:2255–63. doi: 10.1038/s41380-022-01478-x
11. LeMoult J, Humphreys KL, King LS, Colich NL, Price AN, Ordaz SJ, et al. Associations among early life stress, rumination, symptoms of psychopathology, and sex in youth in the early stages of puberty: A moderated mediation analysis. J Abnormal Child Psychol. (2019) 47:199–207. doi: 10.1007/s10802-018-0430-x
12. McLaughlin KA, Sheridan MA. Beyond cumulative risk: A dimensional approach to childhood adversity. Curr Dir Psychol Sci. (2016) 25:239–45. doi: 10.1177/0963721416655883
13. Sheridan MA, McLaughlin KA. Dimensions of early experience and neural development: deprivation and threat. Trends Cognit Sci. (2014) 18:580–5. doi: 10.1016/j.tics.2014.09.001
14. Lindert J, von Ehrenstein OS, Grashow R, Gal G, Braehler E, Weisskopf MG. Sexual and physical abuse in childhood is associated with depression and anxiety over the life course: Systematic review and meta-analysis. Int J Public Health. (2014) 59:359–72. doi: 10.1007/s00038-013-0519-5
15. Infurna MR, Reichl C, Parzer P, Schimmenti A, Bifulco A, Kaess M. Associations between depression and specific childhood experiences of abuse and neglect: A meta-analysis. J Affect Disord. (2016) 190:47–55. doi: 10.1016/j.jad.2015.09.006
16. Garnefski N, Legerstee J, Kraaij V, Van T, Teerds J. Cognitive coping strategies and symptoms of depression and anxiety: a comparison between adolescents and adults. J Adolesc. (2002) 25:603–11. doi: 10.1006/jado.2002.0507
17. Yu Z, ZHAO A, LIU A. Childhood maltreatment and depression: a meta-analysis. Acta Psychol Sin. (2017) 49:40. doi: 10.3724/SP.J.1041.2017.00040
18. Buehler C, Gerard JM. Cumulative family risk predicts increases in adjustment difficulties across early adolescence. J Youth & Adolescence. (2013) 42:905–920. doi: 10.1007/s10964-012-9806-3
19. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Ann Internal Med. (2009) 151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135
20. Adams ZW, McCart MR, Zajac K, Danielson CK, Sawyer GK, Saunders BE, et al. Psychiatric problems and trauma exposure in nondetained delinquent and nondelinquent adolescents. J Clin Child Adolesc Psychol. (2013) 42:323–31. doi: 10.1080/15374416.2012.749786
21. Ahmadkhaniha HR, Shariat SV, Torkaman-nejad S, Hoseini Moghadam MM. The frequency of sexual abuse and depression in a sample of street children of one of deprived districts of Tehran. J Child Sex Abuse. (2007) 16:23–35. doi: 10.1300/J070v16n04_02
22. Avanci J, Assis S, Oliveira R, Pires T. Childhood depression. Exploring the association between family violence and other psychosocial factors in low-income Brazilian schoolchildren. Child Adolesc Psychiatry Ment Health. (2012) 6:1–9. doi: 10.1186/1753-2000-6-26
23. Bielas H, Barra S, Skrivanek C, Aebi M, Steinhausen HC, Bessler C, et al. The associations of cumulative adverse childhood experiences and irritability with mental disorders in detained male adolescent offenders. Child Adolesc Psychiatry Ment Health. (2016) 10:34. doi: 10.1186/s13034-016-0122-7
24. Brown J, Cohen P, Johnson JG, Smailes EM. Childhood abuse and neglect: specificity of effects on adolescent and young adult depression and suicidality. J Am Acad Child Adolesc Psychiatry. (1999) 38:1490–6. doi: 10.1097/00004583-199912000-00009
25. Calvete E. Emotional abuse as a predictor of early maladaptive schemas in adolescents: contributions to the development of depressive and social anxiety symptoms. Child Abuse Negl. (2014) 38:735–46. doi: 10.1016/j.chiabu.2013.10.014
26. Cao M, Tian Y, Lian S, Yang X, Zhou Z. Family socioeconomic status and adolescent depressive symptoms: A moderated mediation model. J Child Family Stud. (2021) 30:2652–63. doi: 10.1007/s10826-021-02068-1
27. Carey PD, Walker JL, Rossouw W, Seedat S, Stein DJ. Risk indicators and psychopathology in traumatised children and adolescents with a history of sexual abuse. Eur Child Adolesc Psychiatry. (2008) 17:93–8. doi: 10.1007/s00787-007-0641-0
28. Castro IE, Hruska B, Gump BB. Race differences in the effect of subjective social status on hostility and depressive symptoms among 9- to 11-year-old children. J Racial Ethn Health Disparities. (2020) 7:844–53. doi: 10.1007/s40615-020-00707-9
29. Chen M, Chan KL. Parental absence, child victimization, and psychological well-being in rural China. Child Abuse Negl. (2016) 59:45–54. doi: 10.1016/j.chiabu.2016.07.009
30. Cohen Y, Spirito A, Sterling C, Donaldson D, Seifer R, Plummer B, et al. Physical and sexual abuse and their relation to psychiatric disorder and suicidal behavior among adolescents who are psychiatrically hospitalized. J Child Psychol Psychiatry Investig. (1996) 37:989–93. doi: 10.1111/j.1469-7610.1996.tb01495.x
31. Courtney EA, Johnson JG, Alloy LB. Associations of childhood maltreatment with hopelessness and depression among adolescent primary care patients. Int J Cogn Ther. (2008) 1:4–17. doi: 10.1521/ijct.2008.1.1.4
32. Danielson CK, de Arellano MA, Kilpatrick DG, Saunders BE, Resnick HS. Child maltreatment in depressed adolescents: Differences in symptomatology based on history of abuse. Child Maltreat. (2005) 10:37–48. doi: 10.1177/1077559504271630
33. Daryanani I, Hamilton JL, McArthur BA, Steinberg L, Abramson LY, Alloy LB. Cognitive vulnerabilities to depression for adolescents in single-mother and two-parent families. J Youth adolescence. (2017) 46:213–27. doi: 10.1007/s10964-016-0607-y
34. Daviss WB, Diler RS, Birmaher B. Associations of lifetime depression with trauma exposure, other environmental adversities, and impairment in adolescents with ADHD. J Abnorm Child Psychol. (2009) 37:857–71. doi: 10.1007/s10802-009-9318-0
35. Dhamayanti M, Noviandhari A, Masdiani N, Pandia V, Sekarwana N. The association of depression with child abuse among Indonesian adolescents. BMC Pediatr. (2020) 20:1–6. doi: 10.1186/s12887-020-02218-2
36. Dunlop R, Burns A. The sleeper effect. Myth or reality? J Marriage Family. (1995) 57:375–86. doi: 10.2307/353691
37. Dunn EC, McLaughlin KA, Slopen N, Rosand J, Smoller JW. Developmental timing of child maltreatment and symptoms of depression and suicidal ideation in young adulthood: results from the National Longitudinal Study of Adolescent Health. Depress Anxiety. (2013) 30:955–64. doi: 10.1002/da.22102
38. Elmore AL, Crouch E. The association of adverse childhood experiences with anxiety and depression for children and youth, 8 to 17 years of age. Acad Pediatr. (2020) 20:600–8. doi: 10.1016/j.acap.2020.02.012
39. Fang QF. Mental health status ans related factors of middle school students in Nanning. Nanning: Guangxi Medical University (2007).
40. Farrell L, Sijbenga A, Barrett P. An examination of childhood anxiety depression and self-esteem across socioeconomic groups: a comparsion study between hight and low socio-economic status school communities. Adv School Ment Health Promotion. (2009) 2:5–19. doi: 10.1080/1754730X.2009.9715694
41. Fergusson DM, Horwood LJ, Lynskey MT. Parental separation, adolescent psychopathology, and problem behaviors. J Am Acad Child Adolesc Psychiatry. (1994) 33:1122–33. doi: 10.1097/00004583-199410000-00008
42. Flisher AJ, Kramer RA, Hoven CW, Greenwald S, Alegria M, Bird HR, et al. Psychosocial characteristics of physically abused children and adolescents. J Am Acad Child Adolesc Psychiatry. (1997) 36:123–31. doi: 10.1097/00004583-199701000-00026
43. Gallo EAG, De Mola CL, Wehrmeister F, Gonçalves H, Kieling C, Murray J. Childhood maltreatment preceding depressive disorder at age 18 years: a prospective Brazilian birth cohort study. J Affect Disord. (2017) 217:218–24. doi: 10.1016/j.jad.2017.03.065
44. Gilman SE, Kawachi I, Fitzmaurice GM, Buka L. Socio-economic status, family disruption and residential stability in childhood: relation to onset, recurrence and remission of major depression. Psychol Med. (2003) 33:1341–55. doi: 10.1017/S0033291703008377
45. Goodman E. The role of socioeconomic status gradients in explaining differences in US adolescents’ health. Am J Public Health. (1999) 89:1522–8. doi: 10.2105/AJPH.89.10.1522
46. Goodman E, Huang B, Wade TJ, Kahn RS. A multilevel analysis of the relation of socioeconomic status to adolescent depressive symptoms: does school context matter? J Pediatr. (2003) 143:451–6. doi: 10.1067/S0022-3476(03)00456-6
47. Goodman E, Slap GB, Huang B. The public health impact of socioeconomic status on adolescent depression and obesity. Am J Public Health. (2003) 93:1844–50. doi: 10.2105/AJPH.93.11.1844
48. Greger HK, Myhre AK, Lydersen S, Jozefiak T. Previous maltreatment and present mental health in a high-risk adolescent population. Child Abuse Negl. (2015) 45:122–34. doi: 10.1016/j.chiabu.2015.05.003
49. Guo J, Ren X, Wang X, Qu Z, Zhou Q, Ran C, et al. Depression among migrant and left-behind children in China in relation to the quality of parent-child and teacher-child relationships. PloS One. (2015) 10:e0145606. doi: 10.1371/journal.pone.0145606
50. Guo J, Chen L, Wang X, Liu Y, Chui CHK, He H, et al. The relationship between Internet addiction and depression among migrant children and left-behind children in China. Cyberpsychol Behavior Soc Netw. (2012) 15:585–90. doi: 10.1089/cyber.2012.0261
51. Hanson RF, Self-Brown S, Borntrager C, Kilpatrick DG, Saunders BE, Resnick HS, et al. Relations among gender, violence exposure, and mental health: The national survey of adolescents. Am J Orthopsy. (2008) 78:313–21. doi: 10.1037/a0014056
52. He B, Fan J, Liu N, Li H, Wang Y, Williams J, et al. Depression risk of ‘left-behind children’in rural China. Psychiatry Res. (2012) 200:306–12. doi: 10.1016/j.psychres.2012.04.001
53. He D. The effect of SES on adolescents’ Depression: the mediating Role of self-esteem. Psychol: Techn Appl. (2017) 5:723–7. doi: 10.16842j.cnki.issn2095-5588.2017.12.003
54. Horesh N, Sever J, Apter A. A comparison of life events between suicidal adolescents with major depression and borderline personality disorder. Compr Psychiatry. (2003) 44:277–83. doi: 10.1016/S0010-440X(03)00091-9
55. Jaffee SR, Moffitt TE, Caspi A, Fombonne E, Poulton R, Martin J. Differences in early childhood risk factors for juvenile-onset and adult-onset depression. Arch Gen Psychiatry. (2002) 59:215–22. doi: 10.1001/archpsyc.59.3.215
56. Ji Y, Zhang Y, Yin F, Yang S, Yang Y, Liu Q. The prevalence of depressive symptoms and the relationships between depressive symptoms, self-esteem and social support among rural left-behind children in Sichuan province. Mod Prev Med. (2017) 44:239–42.
57. Kaplan SJ, Pelcovitz D, Salzinger S, Weiner M, Mandel FS, Lesser ML, et al. Adolescent physical abuse: Risk for adolescent psychiatric disorders. Am J Psychiatry. (1998) 155:954–9. doi: 10.1176/ajp.155.7.954
58. Kaufman J. Depressive disorders in maltreated children. J Am Acad Child Adolesc Psychiatry. (1991) 30:257–65. doi: 10.1097/00004583-199103000-00014
59. Kerr J, Beer J. Specific and diversive curiosity and depression in junior high school students of divorced and nondivorced parents. psychol Rep. (1992) 71:227–31. doi: 10.2466/pr0.1992.71.1.227
60. Kilic F, Coskun M, Bozkurt H, Kaya I, Zoroglu S. Self-injury and suicide attempt in relation with trauma and dissociation among adolescents with dissociative and non-dissociative disorders. Psychiatry Investig. (2017) 14:172–8. doi: 10.4306/pi.2017.14.2.172
61. Kolko DJ, Moser JT, Weldy SR. Behavioral/emotional indicators of sexual abuse in child psychiatric inpatients: A controlled comparison with physical abuse. Child Abuse Negl. (1998) 12:529–41. doi: 10.1016/0145-2134(88)90070-1
62. Kuyken W, Howell R, Dalgleish T. Overgeneral autobiographical memory in depressed adolescents with, versus without, a reported history of trauma. J Abnormal Psychol. (2006) 115:387. doi: 10.1037/0021-843X.115.3.387
63. Lewis CC, Simons AD, Nguyen LJ, Murakami JL, Reid MW, Silva SG, et al. Impact of childhood trauma on treatment outcome in the Treatment for Adolescents with Depression Study (TADS). J Am Acad Child Adolesc Psychiatry. (2010) 49:132–40.
64. Lin JD, Hsieh YH, Lin FG. Modification effects of family economic status and school factors on depression risk of single-father family children in Mid-Taiwan area. Res Dev Disabil. (2013) 34:1468–77. doi: 10.1016/j.ridd.2013.01.036
65. Ling Y, Yang J, Zhong B, Zhang C, Yao S. Effects of childhood traumatic experience and self-esteem on adolescents’ depression. Chin J Clin Psychol. (2009) 17:54–6. doi: 10.16128/j.cnki.1005-3611.2009.01.036
66. Liu X, Zhang YB. Relationships between depressive symptoms and adverse childhood expericences of rural middle school students. Chin J Child Health Care. (2021) 29:951–954 + 959. doi: 10.11852/zgetbjzz2021-001
67. Mac Giollabhui N, Hamilton JL, Nielsen J, Connolly SL, Stange JP, Varga S, et al. Negative cognitive style interacts with negative life events to predict first onset of a major depressive episode in adolescence via hopelessness. J Abnorm Psychol. (2018) 127:1–11. doi: 10.1037/abn0000301
68. Mansbach-Kleinfeld I, Ifrah A, Apter A, Farbstein I. Child sexual abuse as reported by Israeli adolescents: Social and health related correlates. Child Abuse Negl. (2015) 40:68–80. doi: 10.1016/j.chiabu.2014.11.014
69. McLeer SV, Callaghan M, Henry D, Wallen J. Psychiatric disorders in sexually abused children. J Am Acad Child Adolesc Psychiatry. (1994) 33:313–9. doi: 10.1097/00004583-199403000-00003
70. Monteiro S, Matos AP, Oliveira S. The moderating effect of gender: Traumatic experiences and depression in adolescence. Procedia-Social Behav Sci. (2015) 165:251–9. doi: 10.1016/j.sbspro.2014.12.629
71. Morais HB, Alexander AA, Fix RL, Burkhart BR. Childhood sexual abuse in adolescents adjudicated for sexual offenses: mental health consequences and sexual offending behaviors. Sex Abuse. (2018) 30:23–42. doi: 10.1177/1079063215625224
72. Moretti MM, Craig SG. Maternal versus paternal physical and emotional abuse, affect regulation and risk for depression from adolescence to early adulthood. Child Abuse Negl. (2013) 37:4–13. doi: 10.1016/j.chiabu.2012.09.015
73. Münzer A, Fegert JM, Goldbeck L. Psychological symptoms of sexually victimized children and adolescents compared with other maltreatment subtypes. J Child sexual Abuse. (2016) 25:326–46. doi: 10.1080/10538712.2016.1137667
74. Myers WH. A structural equation model of family factors associated with adolescent depression. Memphis: The University of Memphis (2000).
75. Olsson G. Violence in the lives of suicidal adolescents: a comparison between three matched groups of suicide attempting, depressed, and nondepressed high school students. Int J Adolesc Med Health. (1999) 11:369–80. doi: 10.1515/IJAMH.1999.11.3-4.369
76. Pantle ML, Oegema SL. Sexual abuse and depression in an adolescent female inpatient population. J Psychol Christianity. (1990) 9:55–63.
77. Pelcovitz D, Kaplan SJ, DeRosa RR, Mandel FS, Salzinger S. Psychiatric disorders in adolescents exposed to domestic violence and physical abuse. Am J Orthopsy. (2000) 70:360–9. doi: 10.1037/h0087668
78. Pham TS, Qi H, Chen D, Chen H, Fan F. Prevalences of and correlations between childhood trauma and depressive symptoms, anxiety symptoms, and suicidal behavior among institutionalized adolescents in Vietnam. Child Abuse Negl. (2021) 115:105022. doi: 10.1016/j.chiabu.2021.105022
79. Phillips NK, Hammen CL, Brennan PA, Najman JM, Bor W. Early adversity and the prospective prediction of depressive and anxiety disorders in adolescents. J Abnorm Child Psychol. (2005) 33:13–24. doi: 10.1007/s10802-005-0930-3
80. Poulsen PH, Biering K, Winding TN, Aagaard Nohr E, Andersen JH. Influences of childhood family factors on depressive symptoms in adolescence and early adulthood: A Danish longitudinal study. Scandinavian J Public Health. (2020) 48:715–25. doi: 10.1177/1403494819870056
81. Qu GB. Study on the effect of positive and negative childhood experiences on anxiety and depression of primary and middle school students and the mediating effect of inflammatory burden. Anhui Medical University, Hefei (2022).
82. Rizzo CJ, Esposito-Smythers C, Spirito A, Thompson A. Psychiatric and cognitive functioning in adolescent inpatients with histories of dating violence victimization. J Aggress Maltreat Trauma. (2010) 19:565–83. doi: 10.1080/10926771.2010.495034
83. Rønning JA, Haavisto A, Nikolakaros G, Helenius H, Tamminen T, Moilanen I, et al. Factors associated with reported childhood depressive symptoms at age 8 and later self-reported depressive symptoms among boys at age 18. Soc Psychiatry Psychiatr Epidemiol. (2011) 46:207–18. doi: 10.1007/s00127-010-0182-6
84. Sadowski H, Trowell J, Kolvin I, Weeramanthri T, Berelowitz M, Gilbert LH. Sexually abused girls: patterns of psychopathology and exploration of risk factors. Eur Child Adolesc Psychiatry. (2003) 12:221–30. doi: 10.1007/s00787-003-0334-2
85. Sandler IN, Reynolds KD, Kliewer W, Ramirez R. Specificity of the relation between life events and psychological symptomatology. J Clin Child Adolesc Psychol. (1992) 21:240–8. doi: 10.1207/s15374424jccp2103_5
86. Shah SM, Nowshad G, Dhaheri FA, Al-Shamsi MH, Al-Ketbi AM, Galadari A, et al. Child maltreatment and neglect in the United Arab Emirates and relationship with low self-esteem and symptoms of depression. Int Rev Psychiatry. (2021) 33:326–36. doi: 10.1080/09540261.2021.1895086
87. Shanahan L, Copeland WE, Costello EJ, Angold A. Child-, adolescent- and young adult-onset depressions: differential risk factors in development? Psychol Med. (2011) 41:2265–74. doi: 10.1017/S0033291711000675
88. Shen M, Gao J, Liang Z, Wang Y, Du Y, Stallones L. Parental migration patterns and risk of depression and anxiety disorder among rural children aged 10–18 years in China: a cross-sectional study. BMJ Open. (2015) 5:e007802. doi: 10.1136/bmjopen-2015-007802
89. Shi J, Chen Z, Yin F, Zhao J, Zhao X, Yao Y. Resilience as moderator of the relationship between left-behind experience and mental health of Chinese adolescents. Int J Soc Psychiatry. (2016) 62:386–93. doi: 10.1177/0020764016636910
90. Størksen I, Røysamb E, Moum T, Tambs K. Adolescents with a childhood experience of parental divorce: a longitudinal study of mental health and adjustment. J adolescence. (2005) 28:725–39. doi: 10.1016/j.adolescence.2005.01.001
91. Sun KX. Family socioeconomic status and adolescent depressive symptoms: the mediation effect of negative life events and its gender difference. Psychol Month. (2021) 16:15–17 + 113. doi: 10.19738/j.cnki.psy.2021.24.004
92. Sun XX, Ren H, Shi PX, Shen ST, Chen ZH, Dai Q. Study on parent- child alienation status quo and its mediating effect between life-event and depression rural left-behind children. Chongqing Med J. (2020) 49:3463–7. doi: 10.3969/j.issn.1671-8438.2020.20.033
93. Tang JH, Li XH, Wu EZ, Sun XQ. Rural left-behind children’s personality emotions and behavior characteristics and psychological nursing countermeasures. J International Psychiatry. (2017) 44:298–300 + 314. doi: 10.13479/j.cnki.jip.2017.02.030
94. Tummala-Narra P, Sathasivam-Rueckert N. Perceived support from adults, interactions with police, and adolescents’ depressive symptomology: an examination of sex, race, and social class. J Adolesc. (2013) 36:209–19.
95. Wahab S, Tan SM, Marimuthu S, Razali R, Muhamad NA. Young female survivors of sexual abuse in Malaysia and depression: what factors are associated with better outcome? Asia Pac Psychiatry. (2013) 5:95–102. doi: 10.1111/appy.12051101
96. Wilson S, Vaidyanathan U, Miller MB, McGue M, Iacono WG. Premorbid risk factors for major depressive disorder: are they associated with early onset and recurrent course? Dev Psychopathol. (2014) 26:1477–93. doi: 10.1017/S0954579414001151
97. Wu XY, Lan LY, Tan YN, Zhang YY. Personality, emotional and behavioral characteristics of rural left-behind children and psychological care measures. Guangxi Med J. (2011) 33:1052–4.
98. Xiao Y, Ran H, Fang D, Che Y, Peng J, Sun H, et al. Childhood maltreatment and depressive disorders in Chinese children and adolescents: A population-based case-control study. Asian J Psychiatry. (2022) 78:103312. doi: 10.1016/j.ajp.2022.103312
99. Yen CF, Yang MS, Chen CC, Yang MJ, Su YC, Wang MH, et al. Effects of childhood physical abuse on depression, problem drinking and perceived poor health status in adolescents living in rural Taiwan. Psychiatry Clin Neurosci. (2008) 62:575–83. doi: 10.1111/j.1440-1819.2008.01836.x
100. Yin HM, Niu XQ, Dong D, Niu GF, Sun LJ. The effect of family socioeconomic status on adolescents’ depression:The mediating effect of self–esteem and moderating effect of resilience. psychol Res. (2018) 11:465–71.
101. Yu T, Hu J, Zhang W, Zhang L, Zhao J. Psychological maltreatment and depression symptoms among Chinese adolescents: A multiple mediation model. Child Abuse Negl. (2022) 134:105940. doi: 10.1016/j.chiabu.2022.105940
102. Zhang HY, Wang J, Li XY. Influence of parental marital status and family atmosphere on the adolescent depressive symptoms and the moderating function of character strengths. J Guangdong Med. (2017) 38:598–603. doi: 10.13820/j.cnki.gdyx.20170309.007
103. Zhang L. Dynamic associations between academic achievement and externalizing and internalizing symptoms from early to middle adolescence and the role of peer context Jinan. Jinan: Shandong Normal University (2018).
104. Zhang YH, Li JY, Yin XQ, Wang JL. Relative weights analysis on the impacts of childhood maltreatment forms on adolescent anxiety and depression. Chin J Sch Health. (2022) 43:407–10. doi: 10.16835/j.cnki.1000-9817.2022.03.021
105. Zhao GM. The relationship between middle school students’ Depression and family socioeconomic status and mental resilience Guiyang. Guiyang: Guizhou Normal University (2020).
106. Zou R, Xu X, Hong X, Yuan J. Higher socioeconomic status predicts less risk of depression in adolescence: serial mediating roles of social support and optimism. Front Psychol. (2020) 11:1955. doi: 10.3389/fpsyg.2020.01955
107. Rostom A, Dubé C, Cranney A, Saloojee N, Sy R, Garritty C, et al. Appendix E. Summary ROC Curves. Celiac disease. Rockville (MD): agency for healthcare research and quality (US). (2014). Available: https://www.ncbi.nlm.nih.gov/books/NBK35138/.
108. Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hosp Res Instit. (2011) 2:1–12.
109. Borenstein M, Hedges LV, Higgins JP, Rothstein HR. Introduction to meta-analysis. New York, America: Wiley Press (2009).
110. Huedo-Medina TB, Sánchez-Meca J, Marin-Martinez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I² index? psychol Methods. (2009) 11:193. doi: 10.1037/1082-989X.11.2.193
111. Nelson J, Klumparendt A, Doebler P, Ehring T. Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry. (2017) 210:96–104. doi: 10.1192/bjp.bp.115.180752
112. Hovens JG, Giltay EJ, Spinhoven P, van Hemert AM, Penninx BW. Impact of childhood life events and childhood trauma on the onset and recurrence of depressive and anxiety disorders. J Clin Psychiatry. (2015) 76:931–8. doi: 10.4088/JCP.14m09135
113. Spinhoven P, Elzinga BM, van Hemert AM, de Rooij M, Penninx BW. Childhood maltreatment, maladaptive personality types and level and course of psychological distress: A six-year longitudinal study. J Affect Disord. (2016) 191:100–8. doi: 10.1016/j.jad.2015.11.036
114. Bifulco A, Moran PM, Baines R, Bunn A, Stanford K. Exploring psychological abuse in childhood: IIAssociation with other abuse and adult clinical depression. Bull Menninger Clinic. (2002) 66:241–58. doi: 10.1521/bumc.66.3.241.23366
115. Melmed LR. Cognitive style as a mediator between parental psychological maltreatment and depression in adolescent boys (Unpublished doctorial dissertation). New York: Columbia University (2012).
116. Shapero BG, Black SK, Liu RT, Klugman J, Bender RE, Abramson LY, et al. Stressful life events and depression symptoms: The effect of childhood emotional abuse on stress reactivity. J Clin Psychol. (2014) 70:209–23. doi: 10.1002/jclp.22011
117. Mandelli L, Petrelli C, Serretti A. The role of specific early trauma in adult depression: A meta-analysis of published literature. Childhood trauma and adult depression. Eur Psychiatry. (2015) 30:665–80. doi: 10.1016/j.eurpsy.2015.04.007
118. Rinne-Albers MA, Boateng CP, van der Werff SJ, Lamers-Winkelman F, Rombouts SA, Vermeiren RR, et al. Preserved cortical thickness, surface area and volume in adolescents with PTSD after childhood sexual abuse. Sci Rep. (2020) 10:3266. doi: 10.1038/s41598-020-60256-3
119. Alix S, Cossette L, Cyr M, Frappier JY, Caron PO, Hébert M. Self-blame, shame, avoidance, and suicidal ideation in sexually abused adolescent girls: a longitudinal study. J Child sexual Abuse. (2020) 29:432–47. doi: 10.1080/10538712.2019.1678543
120. Noll JG, Guastaferro K, Beal SJ, Schreier HM, Barnes J, Reader JM, et al. Is sexual abuse a unique predictor of sexual risk behaviors, pregnancy, and motherhood in adolescence? J Res Adolescence. (2019) 29:967–83. doi: 10.1111/jora.12436
121. Gee DG, Cohodes EM. Influences of caregiving on development: A sensitive period for biological embedding of predictability and safety cues. Curr Dir psychol Sci. (2021) 30:376–83. doi: 10.1177/09637214211015673
122. Kim Y, Lee H, Park A. Patterns of adverse childhood experiences and depressive symptoms: self-esteem as a mediating mechanism. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:1–11. doi: 10.1007/s00127-021-02129-2
123. Wolfe DA, Crooks CV, Lee V, McIntyre-Smith A, Jaffe PG. The effects of children’s exposure to domestic violence: A meta-analysis and critique. Clin Child Family Psychol Rev. (2003) 6:171–87. doi: 10.1023/A:1024910416164
124. Holt S, Buckley H, Whelan S. The impact of exposure to domestic violence on children and young people: A review of the literature. Child Abuse Negl. (2008) 32:797–810. doi: 10.1016/j.chiabu.2008.02.004
125. Wheaton B. Life transitions, role histories, and mental health. Am sociol Rev. (1990) 55:209–23. doi: 10.2307/2095627
126. Jekielek SM. Parental conflict, marital disruption and children’s emotional well-being. Soc Forces. (1998) 76:905–36. doi: 10.2307/3005698
127. Deng LY, Zhao XY, Fang XY. The influence of parental divorce on children and adolescents’ Mental development: the important role of inter-parental conflict. Acta Meteorol Sin. (2016) 32:246–56. doi: 10.16187/j.cnki.issn1001-4918.2016.02.14
128. Amato PR. Research on divorce: Continuing trends and new developments. J marriage Family. (2010) 72:650–66. doi: 10.1111/j.1741-3737.2010.00723.x
129. Reiss F, Meyrose AK, Otto C, Lampert T, Klasen F, Ravens-Sieberer U. Socioeconomic status, stressful life situations and mental health problems in children and adolescents: Results of the German BELLA cohort-study. PloS One. (2019) 14:e0213700. doi: 10.1371/journal.pone.0213700
130. Gao WB, Wang T, Liu ZK, Wang XL. A study on depression characteristics and its influencing factors in children left in rural areas. Chin J Behav Med Sci. (2007) 16:238–40. doi: 10.3760/cma.j.issn.1674-6554.2007.03.019
131. Roubinov D, Bush NR, Boyce WT. How a pandemic could advance the science of early adversity. JAMA Pediatr. (2020) 174:1131–2. doi: 10.1001/jamapediatrics.2020.2354
Keywords: depression, adversity, threat, deprivation, youth
Citation: Yu Z, Cao Y, Shang T and Li P (2024) Depression in youths with early life adversity: a systematic review and meta-analysis. Front. Psychiatry 15:1378807. doi: 10.3389/fpsyt.2024.1378807
Received: 30 January 2024; Accepted: 19 August 2024;
Published: 12 September 2024.
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyCopyright © 2024 Yu, Cao, Shang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ping Li, bGlwaW5nY2h4eXlAMTYzLmNvbQ==
 Zengyan Yu
Zengyan Yu Yunhua Cao
Yunhua Cao Tinghuizi Shang
Tinghuizi Shang Ping Li
Ping Li