- Iraqi Board for Medical Specialities, Baghdad, Iraq
Background: The current work reviews the psychosocial factors associated with different urinary methamphetamine concentration levels.
Methods: From April to November 2023, 243 participants from Baghdad’s Al-Ataa Hospital were the subjects of a cross-sectional descriptive analysis study. We included 73 patients in this study.
Result: The urinary methamphetamine concentration levels were from 3 to 92,274 ng/ml, with a mean ± SD of 10,873.6 ± 18,641. Patients diagnosed with major depression disorder exhibited higher scores on GHQ-30, UCLA, MOAS, and BDI-II with a significant P-value of 0.0001, 0.001, 0.0001, and 0.0001, consequently with an effect size of 0.015, 0.001, 1.05, and 3.24, respectively.
Conclusions: The multi-screening test can produce a false positive. It frequently interferes with other drugs, especially antidepressants. This will result in patients being stigmatized and accused. On the other hand, those who accidentally come into contact with crystal smoke will experience the same withdrawal symptoms as the addicted patients. Their urinary methamphetamine level (titer) could have negative results. Urinary methamphetamine levels should be zero in healthy patients. In this situation, screening tests, expert opinion, and urine methamphetamine testing are strongly recommended.
1 Background
Methamphetamine is prescribed for obesity, narcolepsy, and attention deficit hyperactivity disorder (1). Methamphetamine is a member of a group of synthetic compounds referred to as amphetamines (2). Amphetamines are referred to as ice and crystal meth on the street. Shabu was its Egyptian name (3). There are four commonly used amphetamines in the US, and methamphetamine is one of them (4). In Iraq, dextroamphetamine is in addition to methamphetamine (5). People who utilize methamphetamine frequently take polydrugs, which needs to be evaluated. Higher rates of dependency and hazardous use are linked to crystalline methamphetamine (6). The primary effects are neurocognitive; these include depression, psychosis, and other neuropsychiatric and cognitive consequences, in addition to a pleasurable and energetic mood (7). Chronic methamphetamine usage causes neurotoxicity in dopaminergic axon terminals, which is linked to decreased dopamine synthesis and decreased expression of the dopamine transporter despite the fact that this causes acute elevations in dopamine and norepinephrine signaling that drive the methamphetamine-associated euphoria (8). One of the key contributing factors to the development and maintenance of drug misuse is distress tolerance (9). When a substance is used repeatedly, tolerance and dependent use develop over weeks or months. A disorder of the regulation of stimulant use, stimulant dependence is caused by the repeated or continuous use of stimulants and is characterized by subjective cravings and strong internal desires to use (i.e., impaired control over use, prioritizing use over other activities, and persistent use despite harm or negative consequences). When stimulants are used consistently for at least a month—that is, nearly every day—for at least a year, signs of dependence typically become apparent (6). Stimulant use disorder is defined by a pattern of usage that results in clinically significant impairment or distress, escalation of the dose used, unsuccessful attempts to reduce, cravings, problems in social or professional settings, and physical or psychological issues (6).
1.1 Rationale of the study
Al-Hemiary et al. (2014) in Iraq verified a sharp rise in the use of illicit Amphetamine-Type Stimulants, especially methamphetamine, and captagon. Also, Al-Basrah governorate showed a particularly noticeable increase (10, 11). Ciccarone and Shoptaw (2022) examined an alarming shift in the global overdose mortality rate from opioids, from the third wave to a more severe fourth wave, characterized by methamphetamine and cocaine usage (12). The psychological strains and extreme stress that members of society have experienced as a result of terrorism and the precarious social and economic circumstances that Iraq is currently experiencing are among the reasons why drug usage has become more common in recent years. There is proof that drug outbreaks result in major issues (13).
Abuse of methamphetamine results in psychological symptoms, such as depression, and irreparable brain damage (14). Subjectively upsetting, loneliness is a feeling that develops when someone feels that they are not interacting with others enough, either in terms of quantity or quality. Several researches have linked addictive behaviors to mental health issues like anxiety, depression, and loneliness. More people feel lonely when they abuse drugs than when they do not. Drug misuse and participation in dangerous activities are more likely to occur in lonely people (15).
Whether or not it is thought to be caused by methamphetamine, a diagnosable psychotic disease must have symptoms that go beyond what would be expected from intoxication or withdrawal from methamphetamine. When psychotic symptoms that began in the context of methamphetamine use persist for more than a month after stopping methamphetamine use or when symptoms resurface in the absence of methamphetamine use, differential diagnostic problems regarding the etiology of a psychotic condition among methamphetamine users generally arise (16).
According to L. Curran et al., three categories of patient diseases could be the focus of prevention and therapy, and mental health disorders constitute one of them. Several risk markers were found to indicate that methamphetamine users were younger and more likely to be male than the total hospitalized population under investigation. Users of methamphetamine were significantly more likely to have anxiety and depression than nonusers, and they were also more likely to have a lower socioeconomic status (17).
SA Nia et al. claim that while methamphetamine use increased rapidly, so did the drug’s supply in Iran. Methamphetamine holds the leading position in Iran’s pharmaceutical industry (18).
1.2 Aim of the study
This study aims to investigate the relationship between methamphetamine urine concentration levels and psychosocial variable parameters in patients with substance addiction or abuse.
1.3 Study question
Do urinary methamphetamine concentration levels have a significant association with psychological and behavioral characteristics, such as depression, loneliness, and aggression, in patients with substance addiction or abuse?
1.4 Study hypothesis
Patients with methamphetamine urine concentrations above 300 ng/mL do not demonstrate statistically significant associations with non-inferior levels of psychosocial variable parameters, including loneliness, social isolation, and depression, in comparison to aggressive behaviors.
2 Materials and methods
2.1 Research ethics
The current study has received ethical approval from (1) the Ethical Committee, Iraqi Board for Medical Specializations. The approval was granted according to number 739 on the 27th of February 2023; (2) the Iraqi Ministry of health. The approval was granted according to protocol number 2 in 2021 (https://moh.gov.iq/?page=51); and (3) Al-Rusafa health directorate, Baghdad. The approval was granted according to number 42397 on the 20th of March 2023. Additionally, this study is a research output of the Iraqi Medical Board thesis, clinical pharmacy department.
2.2 Study structure
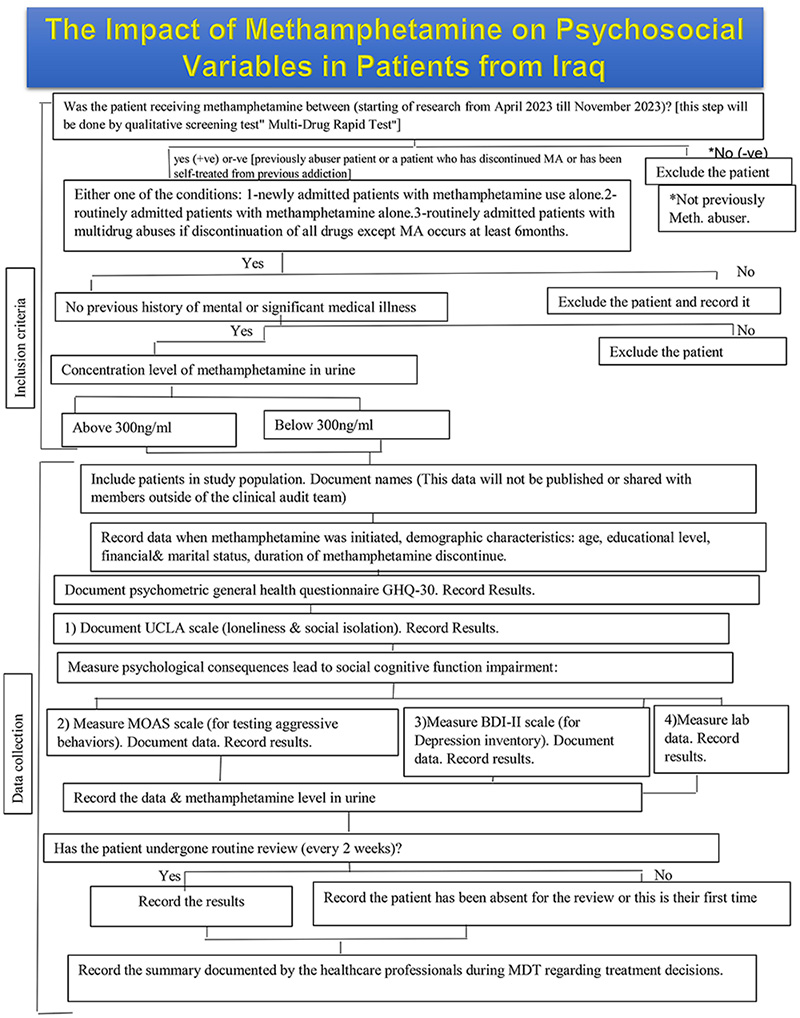
A cross-sectional descriptive analysis study would be conducted on 243 participants (all patients were male) from Al-Ataa Hospital in Baghdad, Iraq, between April 2023 and November 2023. The patients were seeking treatment for methamphetamine dependence. The flowchart describes the work plan in Appendix A.
2.3 Study participants
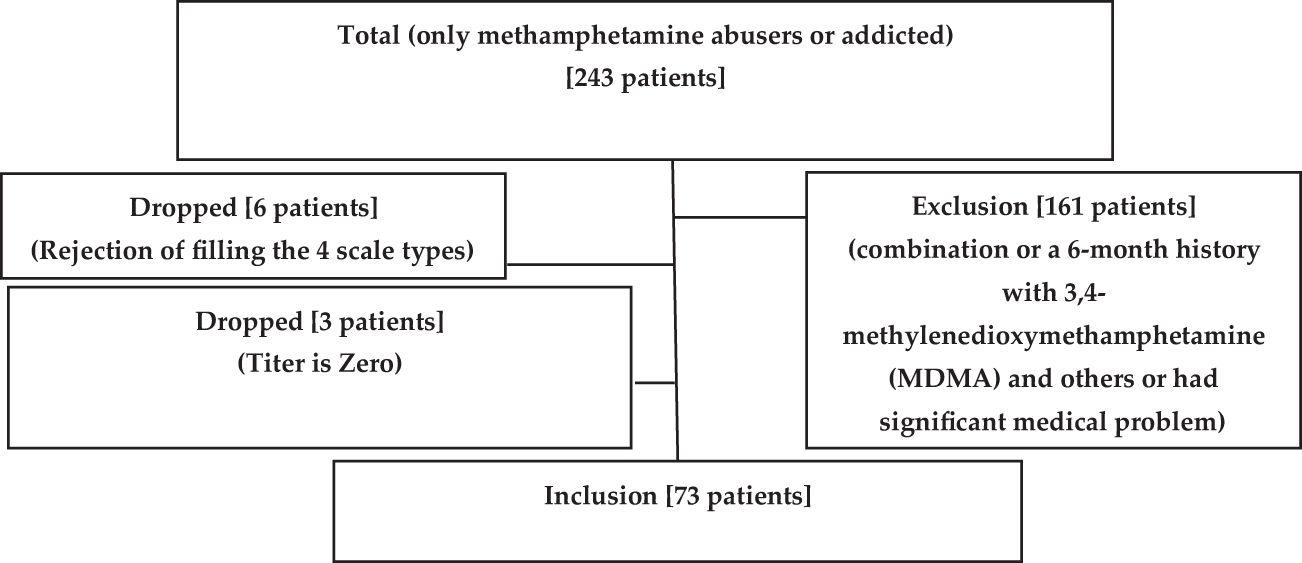
In this study, out of 161 patients, 73 patients were admitted due to methamphetamine contaminants (combination, a 6-month history with multi-drugs including 3,4-methylenedioxymethamphetamine or a significant medical problem). Nine patients were dropped from the study (six patients because of rejection filling out the four scale types and three patients due to their pure titer result being zero) as shown in Figure 1.
2.3.1 Inclusion criteria
1. Patients eligible for the study must have a history of methamphetamine addiction or abuse.
2. They must have undergone a multi-drug screening test.
3. Patients may fall into one of the following categories:
- Newly admitted patients with methamphetamine use only.
- Routinely admitted patients with methamphetamine use only.
- Routinely admitted patients with a history of multidrug abuse, provided that they have abstained from all drugs for at least 6 months except methamphetamine.
4. Methamphetamine urine concentration must be tested, with patients falling into one of two categories:
- Positive for detectable methamphetamine urine concentration.
- Negative, indicating either past methamphetamine use or cessation of use.
2.3.2 Exclusion criteria
1- Participants who had abused drugs other than methamphetamine for at least 6 months, except amphetamine.
2- Patients with a previous history of mental or significant medical illness.
3- Patients who fulfilled the Diagnostic and Statistical Manual of Mental Disorders-5 criteria for dependency on any compounds other than methamphetamine and those who show positive for many drugs during drug screening.
2.4 Study variables
Using the survey, data collection encompassed several key variables representing different aspects of the study objectives: (1) socio-demographic characteristics of the studied population: This field included information about participants’ age, gender, educational background, marital status, and employment status; (2) patterns of methamphetamine abuse associated with different methamphetamine urine concentration levels: In this part, the collected data from the condition of receiving methamphetamine, duration of discontinuation, and years of abusing and routine reviewing; (3) psychosocial variables associated with different methamphetamine urine concentration levels: This is the major part of assessing patients by using the tools: General Health Questionnaire-30, Beck Depression Inventory-II, University of California, Los Angeles Loneliness Scale, and Modified Overt Aggression Scale; (4) comparison of laboratory data with methamphetamine urine concentration levels: to mainly assess the liver and renal function; and (5) medication decision with methamphetamine urine concentration levels: this section deals with the drugs that are used to relieve the symptomatic effect of methamphetamine, which include antipsychotics, antidepressants, analgesia, sedatives, anticonvulsants, and GABA analog (antiseizure). By analyzing these variables, the study aimed (1) to determine the psychosocial variables associated with different urinary methamphetamine concentration levels and (2) to find the relationship between different psychosocial variables and other parameters with urinary methamphetamine concentration levels.
2.5 Criteria for eligibility
Diagnosis of methamphetamine use disorder was done by the initial urine screening test, the stated history of misuse, the Diagnostic and Statistical Manual of Mental Disorders (DSM) -5, and major depression disorder (MDD).
(1) Urinary drug screening by multi-drug rapid test panel, (2) amphetamines II (AMPS2) urinary test from Roche/Hitachi company. A Cobas C analyzer is used. One single AMPS2 test costs US $9. In our work, some patients used three tests due to the turbidity of urine, (3) General Health questionnaire GHQ30 (19) (with permission from a publishing company Mapi Research Trust with order number 2315915), (4) Beck Depression Inventory-II (20): the Arabic version was used, (5) University of California, Los Angeles (version 3) (15): the Arabic version was used (21), and (6) Modified Overt Aggression Scale: the Arabic version was used (3, 22, 23).
2.6 Data analysis
(1) Sample size determination: 73 patients.
(2) The statistical tests used: chi-square, mean with or without SD, P-value, and t-test with Cohen’s d value.
(3) The statistical package used is IBM SPSS version 29.
3 Results
The number of patients included in the current study is 73. The studied sample was analyzed across two groups: group B (the control group) representing individuals with normal mental health (comprising normal, mild, and borderline cases) and group A (the major group) representing individuals diagnosed with major depressive disorder (MMD) encompassing moderate, severe, and extreme depression.
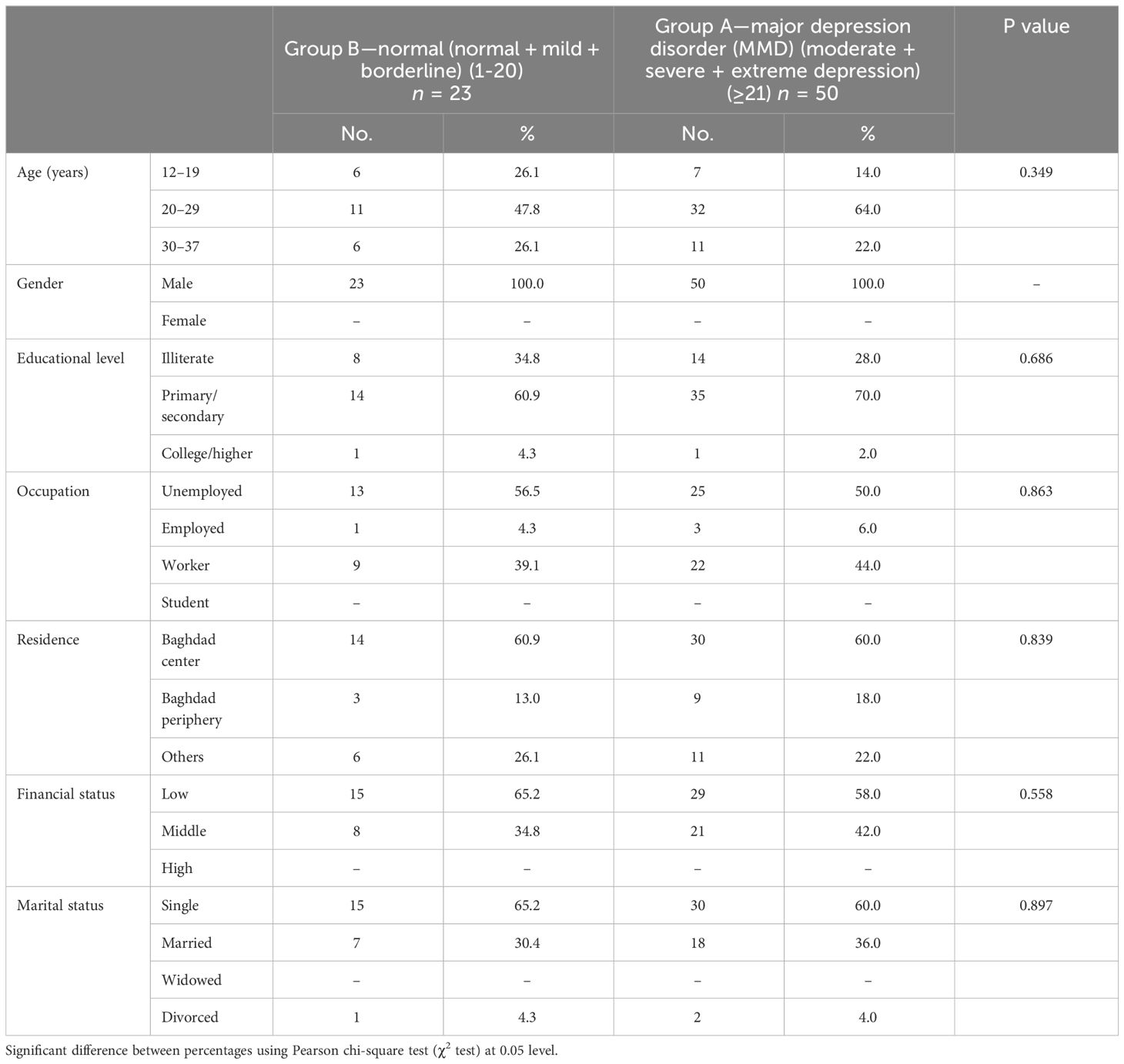
The socio-demographic features shown in Table 1 illustrate that all patients are male. No statistically significant associations were found between the two groups across all variables (p > 0.05 for all comparisons), including educational level (p = 0.686), occupation (p = 0.863), residence (p = 0.839), financial status (p = 0.558), and marital status (p = 0.897). While age exhibited variation in major depressive disorder (MDD) prevalence across different age groups, the overall difference was not statistically significant (p = 0.349).
Patterns of Methamphetamine abuse: Table 2 illustrates significant associations that emerge between various clinical factors and methamphetamine abuse patterns. Patients diagnosed with major depressive disorder (MDD) exhibited notably higher urine methamphetamine concentrations (p = 0.001). Admission status also played a crucial role, with newly admitted and routinely admitted patients displaying significantly elevated levels (p = 0.011 and p = 0.009, respectively). Moreover, longer periods of methamphetamine discontinuation were linked with lower concentrations (p = 0.021, p = 0.020, p = 0.008 for 14–20 days, 21–27 days, and 28 days or more, respectively), while longer durations of methamphetamine use correlated with higher concentrations (p = 0.015 and p = 0.029 for 1–4 years and 5–8 years). Routine reviews every 3 months were associated with lower concentrations (p = 0.009), and individuals testing positive for methamphetamine had significantly higher concentrations (p = 0.044).
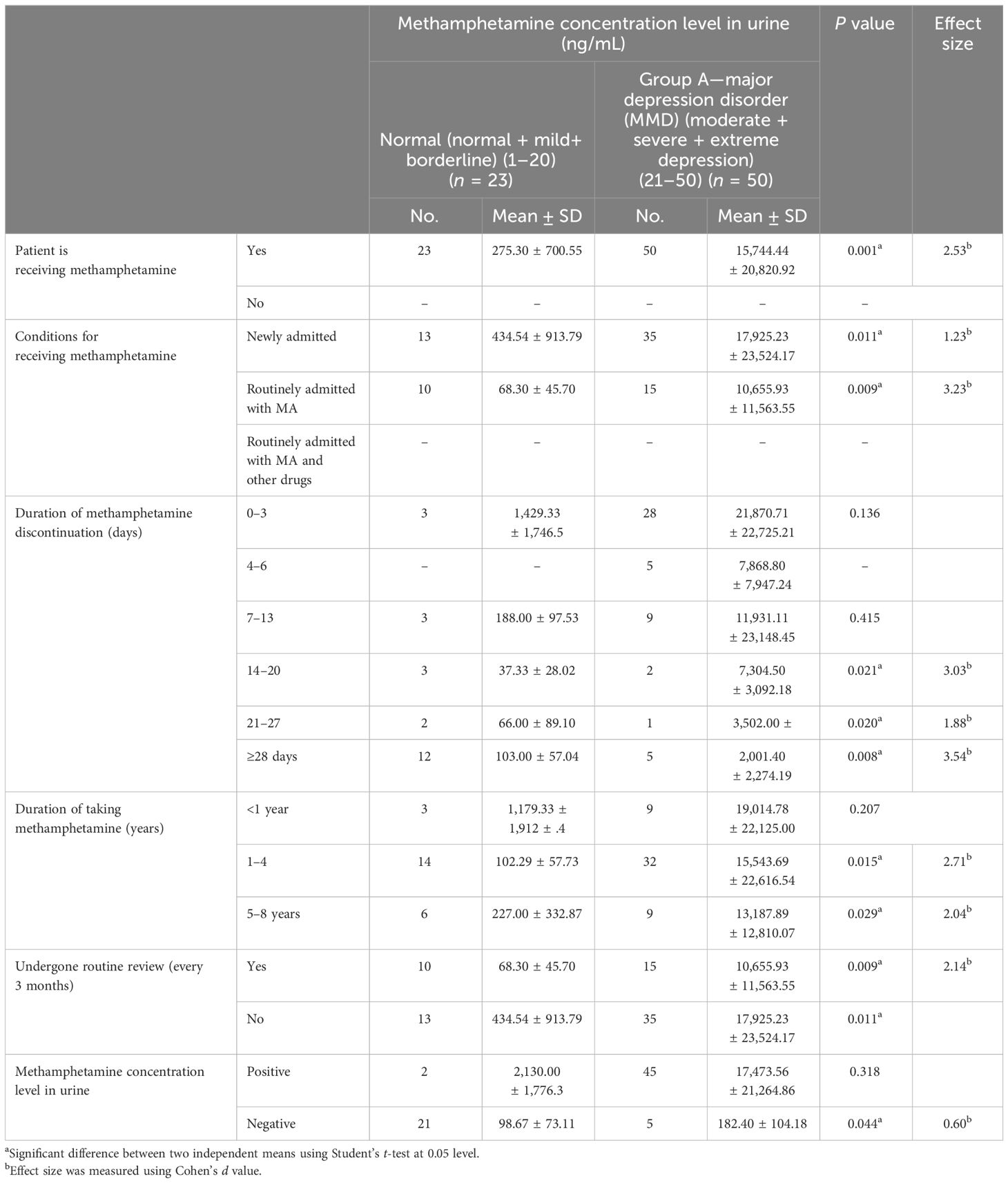
Table 2 Patterns of methamphetamine abuse associated with different methamphetamine urine concentration levels.
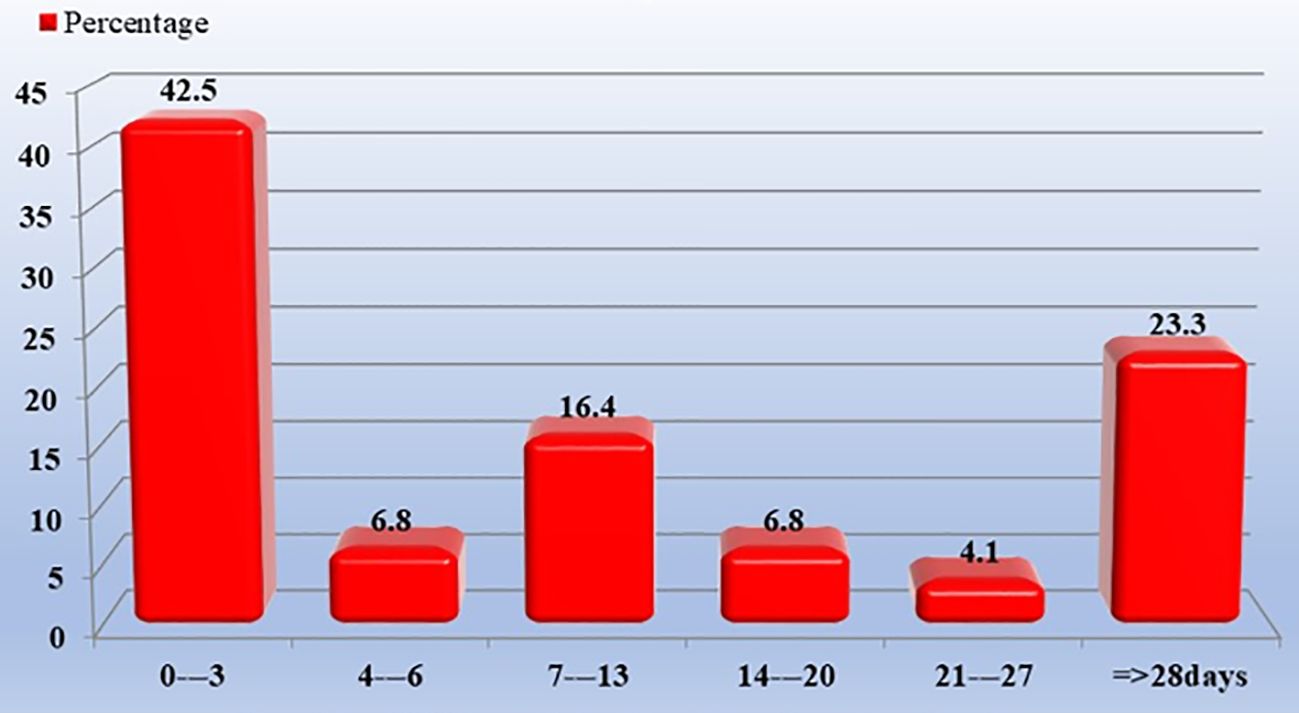
Figure 2 shows the duration of methamphetamine discontinuation (days). A duration from 0 to 3 day(s) had 42.5% and that of 28 days or more had 23.3%.
Methamphetamine concentration levels were determined using the Amphetamines II (AMPS2) test. In the sample (73 patients), the methamphetamine concentration levels in urine were from 3 to 92,274 ng/mL, with mean ± SD 10,873.6 ± 18,641.
Psychosocial Variables assessment: Table 3 depicts significant associations with notable effect sizes. Patients diagnosed with major depression disorder (MDD) exhibited higher scores on the General Health Questionnaire (GHQ-30) compared to those without MDD (p = 0.0001, Cohen’s d = 0.015). Additionally, higher urine methamphetamine concentrations were associated with increased loneliness, as measured by the University of California, Los Angeles (UCLA) Loneliness Scale (p = 0.001, Cohen’s d = 0.001). Levels of aggression, assessed using the Modified Overt Aggression Scale (MOAS), were significantly elevated in individuals with higher methamphetamine concentrations (p = 0.0001, Cohen’s d = 1.05). Beck Depression Inventory (BDI-II) scores demonstrated a significant increase with higher methamphetamine concentrations, indicating more severe depression (p = 0.0001, Cohen’s d = 3.24). Patients ranging from moderate to extreme depression levels meet the DSM-5 criteria for MDD.
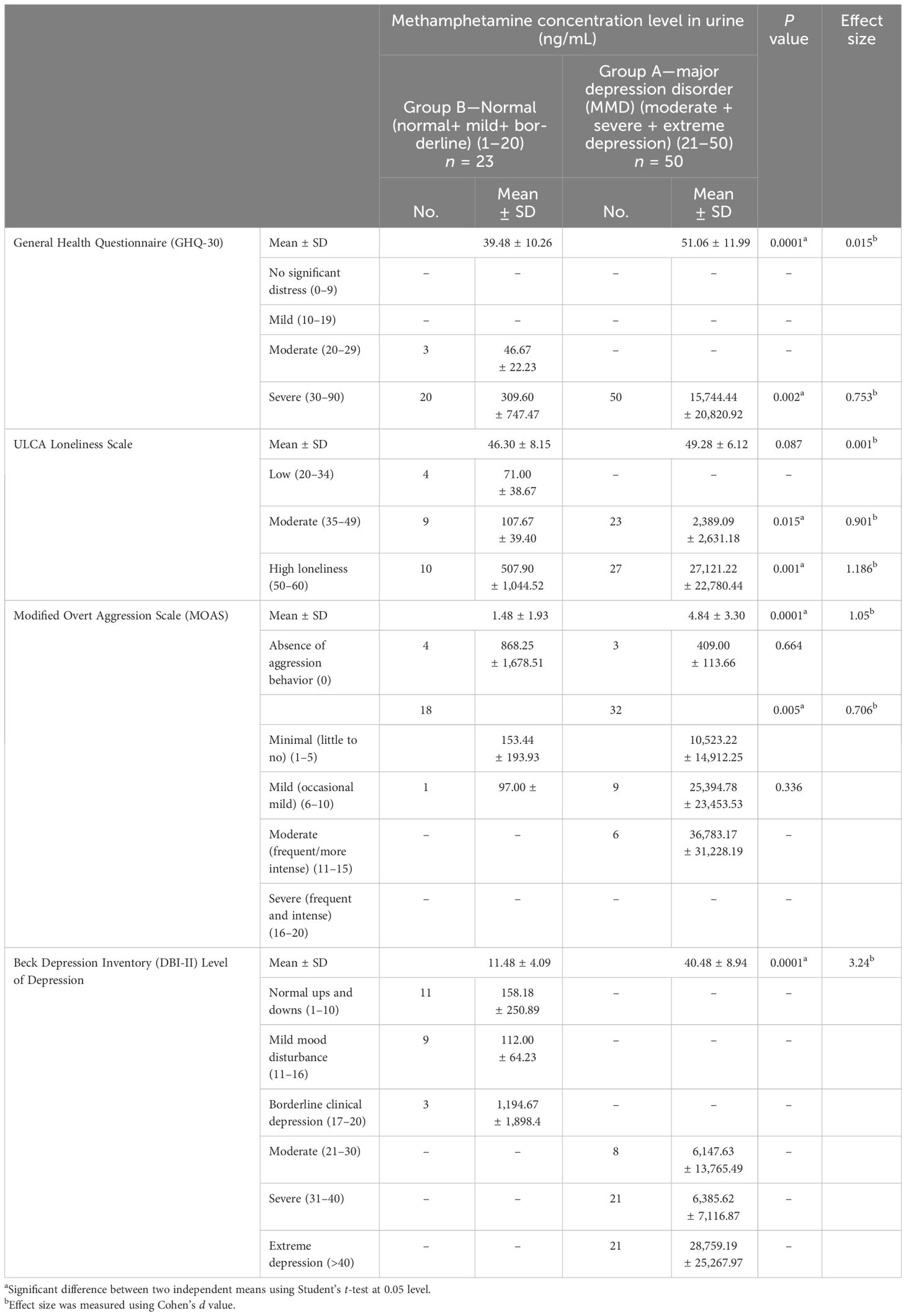
Table 3 Psychosocial variables associated with different methamphetamine urine concentration levels.
Figure 3A shows the Beck Depression Inventory-II across group A (MDD) and group B (normal) associated with different methamphetamine urine concentration levels.

Figure 3 (A) The Beck Depression Inventory-II score differs between group A (MDD) and group B (normal) in association with varying methamphetamine urine concentration levels. (B) University of California, Los Angeles (UCLA) scale differs between group A (MDD) and group B (normal) in association with varying methamphetamine urine concentration levels. (C) Modified Overt Aggression (MOAS) scale differs between group A (MDD) and group B (normal) in association with varying methamphetamine urine concentration levels.
Figure 3B shows the University of California, Los Angeles (UCLA) scale across group A (MDD) and group B (normal) associated with different methamphetamine urine concentration levels.
Figure 3C shows the Modified Overt Aggression (MOAS) scale across group A (MDD) and group B (normal) associated with different methamphetamine urine concentration levels.
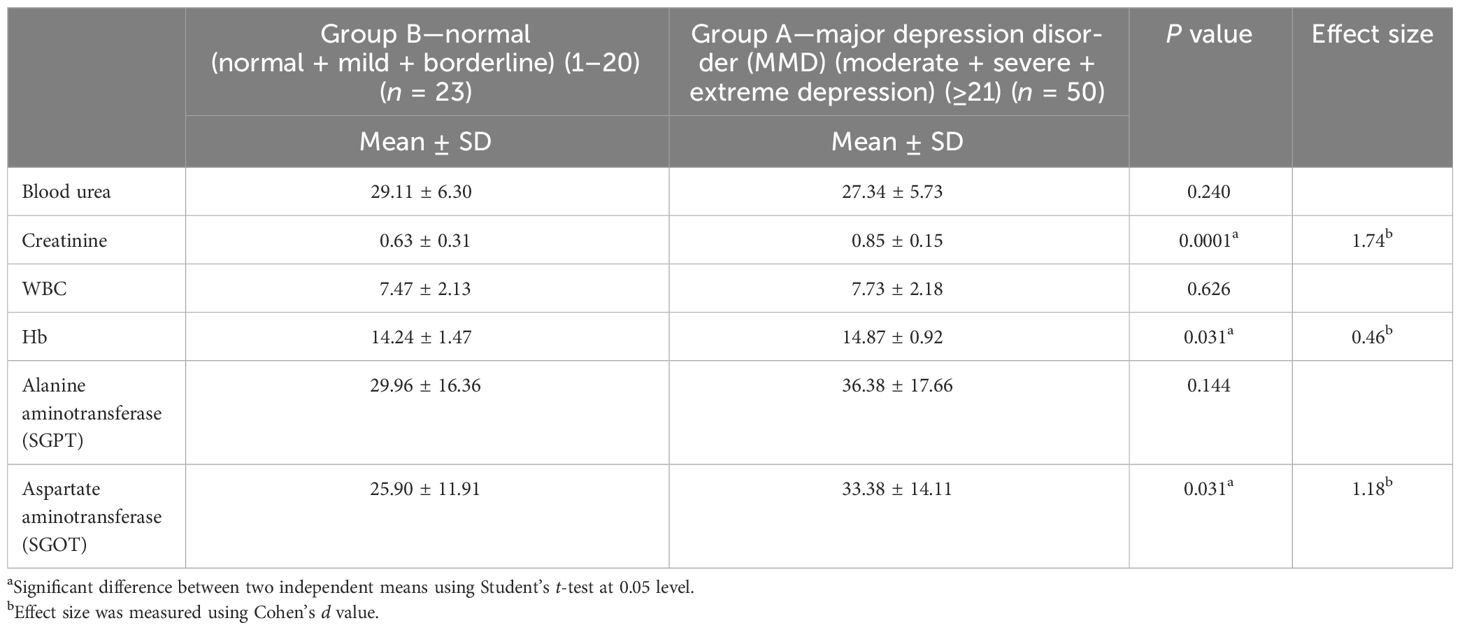
Laboratory data with methamphetamine: Table 4 shows the laboratory data with methamphetamine. Significant differences were observed in creatinine levels (p = 0.0001, Cohen’s d = 1.74), hemoglobin (Hb) levels (p = 0.031, Cohen’s d = 0.46), and aspartate aminotransferase (SGOT) levels (p = 0.031, Cohen’s d = 1.18) between patients with normal and elevated methamphetamine concentrations.
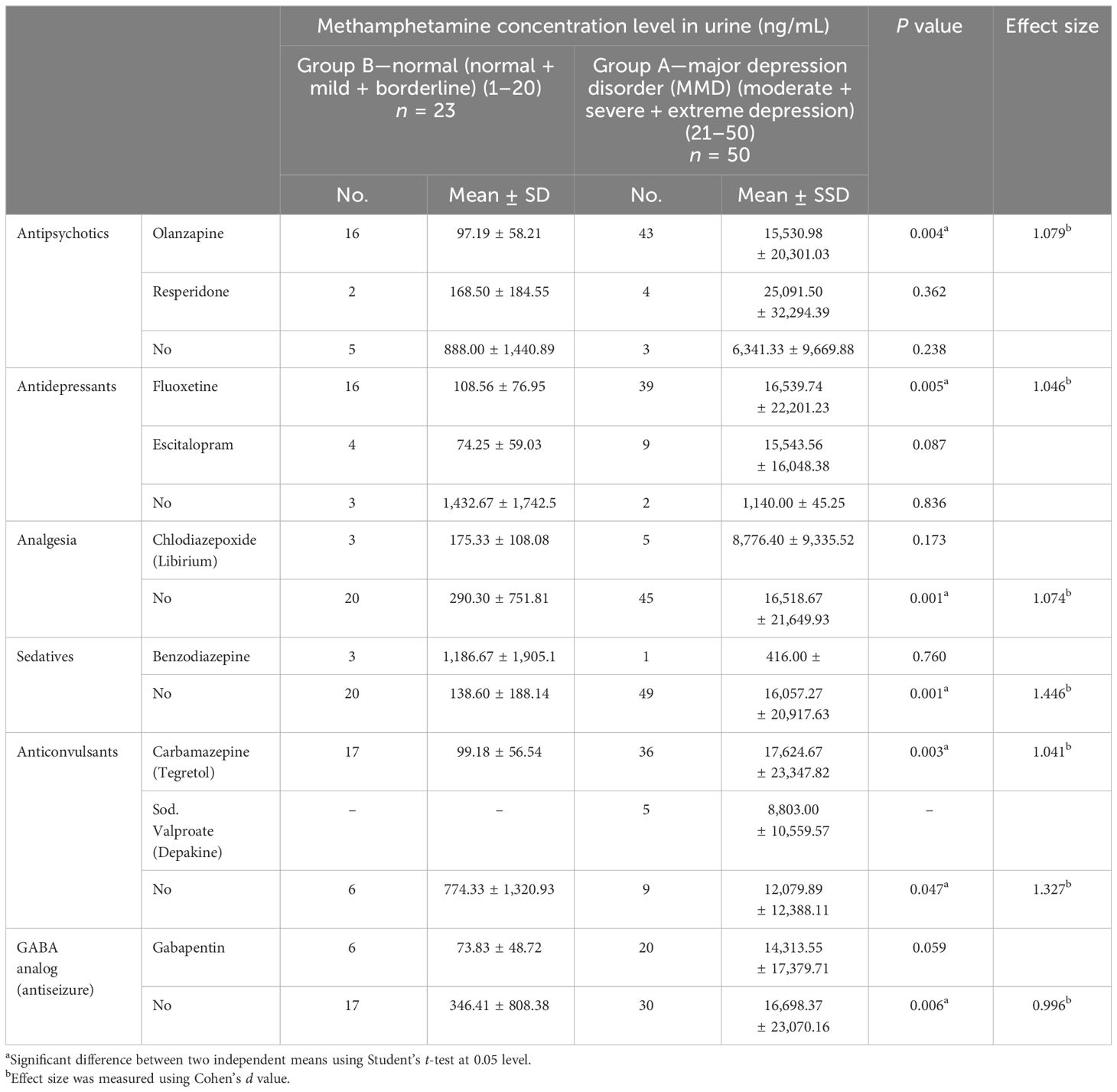
Significant differences were found in medication decisions (as detox medications), as shown in Table 5, associated with methamphetamine urine concentration levels. Olanzapine usage was significantly higher in patients with elevated methamphetamine concentrations (p = 0.004, Cohen’s d = 1.079). Fluoxetine (p = 0.005, Cohen’s d = 1.046) and analgesia use without specific medication (p = 0.001, Cohen’s d = 1.074) were also notably higher in this group. Furthermore, sedative use, specifically benzodiazepine (p = 0.001, Cohen’s d = 1.446), and anticonvulsant use, particularly carbamazepine (p = 0.003, Cohen’s d = 1.041), demonstrated significant differences between the two groups.
In Table 2–5, the p-values were computed at the 0.05 level using Student’s t-test with Cohen’s d value. According to Cohen’s guidelines, the effect size can be interpreted as small (around 0.2), medium (around 0.5), or large (around 0.8).
4 Discussion
The occurrence of major depression disorder (MMD) and its association with methamphetamine abuse was highlighted, emphasizing the severity of mental health comorbidities in methamphetamine users and echoing observations by Hashisha et al. (2022) (3). The findings underscore the profound impact of methamphetamine on psychosocial factors, particularly among individuals with varying urine concentration levels of the substance.
The observed gender disparity in rehabilitation facilities, attributed to male-exclusive wards, underscores the need for gender-sensitive treatment approaches. Moreover, the socio-demographic profile of the studied sample, with a prevalence of urban residency and primary to secondary education attainment, resonates with the findings of Al-imam et al. (2023) and Chachan et al. (2022), suggesting a correlation between drug availability and population density (4, 5). However, the discrepancy in illiteracy rates, covering one-third of the sample, deviates from earlier studies, indicating potential unique local factors or variations in educational infrastructure (4, 5). Similarly, marital status trends align with those observed by Chachan et al., suggesting societal or cultural influences on divorce rates (5).
The findings align with global perspectives linking unemployment among young individuals with increased drug consumption, as highlighted in previous research (3, 24). Another study from Erbil declares the comparable consequences published by N. Mahmood et al. (25). Moreover, the significant rise in methamphetamine screening results corroborates data from Curran et al. (2022), emphasizing the widespread prevalence of substance abuse within society (17). Notably, minor cross-reactivity in multidrug screening tests may occur, potentially resulting in false positive amphetamine screening results (20).
Exclusion criteria ensuring the focus on individuals with methamphetamine addiction or abuse without pre-existing mental or medical conditions align with the study’s objective. The prolonged duration of methamphetamine abuse observed in the study cohort raises clinical concerns regarding the chronicity of substance use disorders and the challenges associated with long-term management and intervention, consistent with previous research (13).
Assessments of psychosocial variables reveal severe distress levels among the sample, consistent with prior findings (26) and echoing observations by Hashisha et al. (2022) (3). Moreover, correlations between methamphetamine abuse and scores on psychological scales highlight the global impact of substance abuse on mental wellbeing (15).
The psychological impact of drug addiction, particularly methamphetamine use, extends beyond mere substance dependence, encompassing a spectrum of social and psychological challenges. This study echoes prior research (27). The concerning relationship between methamphetamine concentration levels and psychological distress underscores the heightened vulnerability of individuals with methamphetamine addiction to mood disturbances, emphasizing the importance of comprehensive psychiatric assessment and tailored interventions (28). Additionally, associations between methamphetamine use and aggression align with previous research, emphasizing the need for vigilant monitoring and targeted interventions to mitigate aggression (3, 28).
The utilization of specific medications such as olanzapine, fluoxetine, and carbamazepine in managing methamphetamine addiction emphasizes the diverse treatment approaches influenced by physician preferences and patient responses, consistent with prior research (6, 29).
The prevalence of major depression disorder (MMD) within the cohort of individuals grappling with methamphetamine abuse unveils a striking correlation that echoes global observations. This connection highlights a profound vulnerability to mood disturbances among this demographic group (28). Delving deeper, the study sheds light on how varying levels of methamphetamine concentration in urine intertwine with psychological distress, magnifying the substantial toll methamphetamine abuse exacts on mental wellbeing (28). These revelations not only emphasize the urgency of acknowledging and addressing the intricate relationship between substance abuse and mental health but also underline the need for nuanced interventions tailored to this complexity.
What is particularly intriguing is how these findings resonate with prior research by Hashemzadeh et al. (2021) and Marquez-Arrico et al. (2020), where similar patterns were observed (30, 31). This confluence of evidence adds weight to the argument that major depression disorder (MMD) is not just a concurrent issue but rather an integral facet of the intricate tapestry of challenges faced by those entangled in methamphetamine abuse.
4.1 Limitation and strength of the study
The study’s sample size is small, yet it comprises individuals exclusively using pure methamphetamine, which is typically challenging to encounter. The presence of other mental disorders or significant medical illnesses is another factor. These individuals were sourced from a population known to consume raw or combination drugs. Variations in urinary multi-drug test thresholds across centers necessitate remaining within a single facility. Furthermore, the study’s focus on detoxification programs for long-term drug abusers represents another potential limitation. Moreover, the study’s cross-sectional design limits its ability to establish causality or assess long-term effects. Despite these limitations, the study provides valuable insights into the complex relationship between methamphetamine use and various psychosocial factors, highlighting the need for further research in this area.
5 Conclusions
Concentrations above 300 ng/mL, which is the detectable level, demonstrate statistically significant non-inferior levels of psychosocial variables, including loneliness, social isolation, and depression, in comparison to aggressiveness behaviors. Methamphetamine urinary concentration levels increase with a dramatically significant elevation of depression, loneliness, and social isolation and a mild significant elevation of aggressiveness behavior. The multi-screening test could give a false positive. It tends to interact with other medications, particularly antidepressants. This will lead to accused patients and stick a stigma on them—a negative result with a patient who does not have any previous diseases and/or problems but undergoes withdrawal symptoms of drug abuse. Methamphetamine smoking makes people become abusers accidentally. We highly recommended using a urinary methamphetamine test in addition to a screening test and specialist decision.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Research Ethics: The current study has received ethical approval from: The Ethical Committee, Iraqi Board for Medical Specializations. The approval was granted according to number 739 on the 27th of February 2023, The Iraqi Ministry of Health. The approval was granted according to protocol number 2 in 2021, Al-Rusafa Health Directorate, Baghdad. The approval was granted according to number 42397 on the 20th of March 2023. Additionally, this study is a research output of the Iraqi Medical Board thesis, Clinical Pharmacy Department. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
MA: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. NA-H: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing. HS: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We acknowledge the efforts of Prof. Mustafa Mohammed Al-Ameen Al-Hiti, Ph.D., in pharmaceutical sciences: a chairman of Iraqi pharmacists, for his leadership, sound counsel, and kindness during this study project. This research idea belongs to him. We thank Dr. Hassan M. Abbas, Ph.D. in clinical pharmacy, a general director of the Medical City Complex and director trainer of the Iraqi Board of Clinical Pharmacy, Baghdad, for his invaluable assistance, great support, and encouragement throughout the study; Prof. Hasan A. Farhan, a consultant of cardiology and medical educationalist, acting chairman of the clinical pharmacy committee, for his great help and support throughout the study; Dr. Haydar Muneer Makki, a psychiatrist, for his invaluable assistance throughout the study; Al-Ataa Hospital Laboratory for their help and cooperation throughout the study; Dr. Waleed Arif Tawfiq, a pediatrician and community medicine specialist; Dr. Asma A. Saleh, a gynecology and obstetric and community medicine specialist, and Engineer Mamoon Abbass Abdulrazak for administrative and technical support.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The statements, opinions, and data contained in all publications are solely those of the individual author(s), contributor(s), and editor(s). The editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions, or products referred to in the content.
References
1. Schwarzbach V, Lenk K, Laufs U. Methamphetamine-related cardiovascular diseases. Esc Heart Failure. (2020) 7:407–14. doi: 10.1002/ehf2.12572
2. Lewis D, Kenneally M, Van denHeuvel C, Byard RW. Methamphetamine deaths: Changing trends and diagnostic issues. Medicine Sci Law. (2021) 61:130–7. doi: 10.1177/0025802420986707
3. Hashisha RKH, Hassan H, Ali S. Crystal methamphetamine abuse among patients attending ismailia mental health clinic: Aggressive behavior and psychiatric comorbidity. Ain Shams J Forensic Med Clin Toxicol. (2022) 39:48–55. doi: 10.21608/ajfm.2022.249591
4. Al-Imam A, Motyka M, Hoffmann B, Al-Ka’aby H, Younus MM, Al-Hemiary NJ, et al. Risk factors of suicidal ideation in Iraqi crystal methamphetamine users. Brain Sci. (2023) 13:1279. doi: 10.3390/brainsci13091279
5. Chachan E, Al-Hemiary NJ. Socio-demographic, clinical characteristics and risk factors of crystal meth use in Baghdad/Iraq. Muthanna Med J. (2023) 10:53–66. doi: 10.52113/1/1/2023-53-66
6. Grigg J. Methamphetamine treatment guidelines: Practice Guidelines for Health Professionals. Turning Point, 110 Church St, Richmond, Victoria 3121, Australia: Turning Point, funded by the Victorian Department of Health and Human Services (2018).
7. Ben-Yehuda O, Siecke N. Crystal methamphetamine. JACC: Heart Failure. (2018) 6:219–21. doi: 10.1016/j.jchf.2018.01.004
8. Kevil CG, Goeders NE, Woolard MD, Bhuiyan MDS, Dominic P, Kolluru GK, et al. Methamphetamine use and cardiovascular disease. Arteriosclerosis Thrombosis Vasc Biol. (2019) 39:1739–46. doi: 10.1161/atvbaha.119.312461
9. Manning K, Rogers AH, Bakhshaie J, Hogan J, Buckner JD, Ditre JW, et al. The association between perceived distress tolerance and cannabis use problems, cannabis withdrawal symptoms, and self-efficacy for quitting cannabis: The explanatory role of pain-related affective distress. Addictive Behav. (2018) 85:1–7. doi: 10.1016/j.addbeh.2018.05.009
10. Al-Hemiary NJ, Al-Diwan JK, Hasson A, Rawson RA. Drug and alcohol use in Iraq: Findings of the Inaugural Iraqi Community Epidemiological Workgroup. Subst Use Misuse. (2014) 49:1759–63. doi: 10.3109/10826084.2014.913633
11. Al-Imam A, Santacroce R, Román-Urrestarazu A, Chilcott RP, Bersani G, Martinotti G, et al. Captagon: use and trade in the Middle East. Hum Psychopharmacology: Clin Exp. (2016) 32:3–8. doi: 10.1002/hup.2548
12. Ciccarone D, Shoptaw S. Understanding stimulant use and use disorders in a new era. Med Clinics North America. (2022) 106:81–97. doi: 10.1016/j.mcna.2021.08.010
13. Moore T, Pacula RL. Causes and consequences of illicit drug epidemics. Springer Nature Switzerland AG: Springer eBooks (2021) p. 1–37. doi: 10.1007/978-3-319-57365-6_147-1
14. Wang X, Tong B, Hui R, Hou C, Zhang Z, Zhang L, et al. The role of Hyperthermia in Methamphetamine-Induced Depression-Like Behaviors: Protective effects of coral calcium hydride. Front Mol Neurosci. (2022) 14:808807. doi: 10.3389/fnmol.2021.808807
15. Tsai TY, Wang T, Tseng HH, Chen KC, Chiu CJ, Chen PS, et al. Correlation between loneliness, personality traits, and treatment outcomes in patients with methamphetamine use disorder. Sci Rep. (2022) 12:2-10. doi: 10.1038/s41598-022-11901-6
16. Glasner-Edwards S, Mooney L. Methamphetamine psychosis: Epidemiology and management. CNS Drugs. (2014) 28:1115–26. doi: 10.1007/s40263-014-0209-8
17. Curran L, Nah G, Marcus GM, Tseng ZH, Crawford MH, Parikh NI. Clinical correlates and outcomes of Methamphetamine-Associated cardiovascular diseases in hospitalized patients in California. J Am Heart Assoc. (2022) 11:3-9. doi: 10.1161/jaha.121.023663
18. Nia SA, Safarzadeh S, Hooman F. The effectiveness of group dialectical behavior therapy and structured matrix treatment on quit addiction self-efficacy, distress tolerance, and mindfulness in individuals with stimulant drug abuse. J Health Rep Technol. (2022) 8:1–7. doi: 10.5812/jhrt-127427
19. Cyranka K, Matejko B, Klupa T, Małecki M, Cyganek K, Kieć-Wilk B, et al. Type 1 Diabetes and COVID-19: the level of anxiety, stress and the general mental health in comparison to healthy control. Psychiatria Polska. (2021) 55:511–23. doi: 10.12740/pp/onlinefirst/133356
20. Hubley AM. Beck Depression inventory. Springer Nature Switzerland AG: Springer eBooks (2021) p. 1–11. doi: 10.1007/978-3-319-69909-7_156-2
21. AlSumait L, Alheneidi H, Smith AP. Exploring the effects of loneliness and internet addiction on adults’ Well-being during COVID-19 quarantine. In: Lecture Notes in Computer Science Springer. (2021). p. 491–501. doi: 10.1007/978-3-030-88163-4_42
22. Khan YS, Khan AW, Tahir ME, Hammoudeh S, Shamlawi MA, Alabdulla M. The impact of COVID-19 pandemic social restrictions on individuals with autism spectrum disorder and their caregivers in the Stateof Qatar: A cross-sectional study. Res Dev Disabil. (2021) 119:104090. doi: 10.1016/j.ridd.2021.104090
23. Refaat N, Fahmy M, El-Leithy W, Hassan H, Moez KAE. Correlation between aggressive behavior and sociodemographic characteristics in patients with schizophrenia at a psychiatry outpatient clinic. Middle East Curr Psychiatry. (2017) 24:30–5. doi: 10.1097/01.XME.0000508431.34826.db
24. Amin DM, Elnagdi SA, Amer SA. Drug abuse in Zagazig University Students, Egypt: Cross sectional study. Occup Dis Environ Med. (2019) 07:37–49. doi: 10.4236/odem.2019.72004
25. Mahmood NA, Othman SM, Al-Tawil NG, Al-Hadithi TS. Substance use among high school students in Erbil City, Iraq: prevalence and potential contributing factors. Eastern Mediterr Health J. (2019) 25:806–12. doi: 10.26719/emhj.19.022
26. Moradi A, Massah O. Women and methamphetamine in Iran: a report from the most populous Persian Gulf country. Iranian Rehabil J. (2019) 17(4):313–8. doi: 10.32598/irj.17.4.313
27. Jones R, Jackson D, Woods C, Usher K. Social issues, crisis, and care coordination: First responders experience responding to people affected by methamphetamines. Int J Ment Health Nurs. (2023) 32:755–66. doi: 10.1111/inm.13119
28. Foulds J, Boden JM, McKetin R, Newton-Howes G. Methamphetamine use and violence: Findings from a longitudinal birth cohort. Drug Alcohol Depend. (2020) 207:107826. doi: 10.1016/j.drugalcdep.2019.107826
29. Javdan NS, Ghoreishi FS, Sehat M, Ghaderi A, Banafshe HR. Mental health and cognitive function responses to quetiapine in patients with methamphetamine abuse under methadone maintenance treatment. J Affect Disord. (2019) 251:235–41. doi: 10.1016/j.jad.2019.03.078
30. Hashemzadeh I, Marquez-Arrico JE, Hashemzadeh K, Navarro JF, Adán A. Circadian functioning and quality of life in substance use disorder patients with and without comorbid major depressive disorder. Front Psychiatry. (2021) 12. doi: 10.3389/fpsyt.2021.750500
31. Marquez-Arrico JE, Navarro JF, Adán A. Health-Related Quality of Life in Male Patients under Treatment for Substance Use Disorders with and without Major Depressive Disorder: Influence in Clinical Course at One-Year Follow-Up. J Clin Med. (2020) 9:3110. doi: 10.3390/jcm9103110
Appendix A. Flowchart describing the processing of work.
Keywords: methamphetamine, crystal, psychosocial variables, urinary methamphetamine concentration levels (ng/ml), Baghdad
Citation: Abbass M, Al-Hemiary N and Sahib HB (2024) The impact of methamphetamine on psychosocial variables in patients from Iraq. Front. Psychiatry 15:1376636. doi: 10.3389/fpsyt.2024.1376636
Received: 25 January 2024; Accepted: 15 April 2024;
Published: 08 May 2024.
Edited by:
Andreas Guenter Franke, University of Applied Labour Studies of the Federal Employment Agency, GermanyReviewed by:
Tanay Maiti, Black Country Partnership NHS Foundation Trust, United KingdomAna Adan, University of Barcelona, Spain
Copyright © 2024 Abbass, Al-Hemiary and Sahib. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marwah Abbass, dGhlc2hpbmVfbWluZEB5YWhvby5jb20=
 Marwah Abbass
Marwah Abbass Nesif Al-Hemiary
Nesif Al-Hemiary