- Charité – Universitatsmedizin-Berlin - Tinnitus Center, Berlin, Germany
Background: Gold-standard approaches for chronic tinnitus involve hearing amplification measures and psychological therapy, where applicable. Whilst schema therapy is accumulating evidence as a transdiagnostically useful treatment framework, its applicability for patients with chronic tinnitus has not yet been examined. The present study (a) explores latent dimensions of psychological distress in a sample of chronic tinnitus patients, and (b) examines whether the schema mode model might explain these dimensions – thus constituting a potentially helpful conceptualization and treatment framework.
Methods: N = 696 patients with chronic tinnitus completed the Tinnitus Questionnaire, Tinnitus Handicap Inventory, Hospital Anxiety and Depression Scale, Perceived Stress Questionnaire and ICD-10 Symptom Rating. As criterion, patients further completed the Schema Mode Inventory (SMI-r) – which assesses psychological constructs linked to negative self-beliefs (“parent modes”), primary emotions resulting from unmet psychological needs (“child modes”), and secondary emotional or behavioral attempts to reinstate or maintain psychological equilibrium (“coping modes”). A varimax-rotated principal axis factor analysis grouped the primary item pool. Factor scale scores were then correlated with the SMI-r.
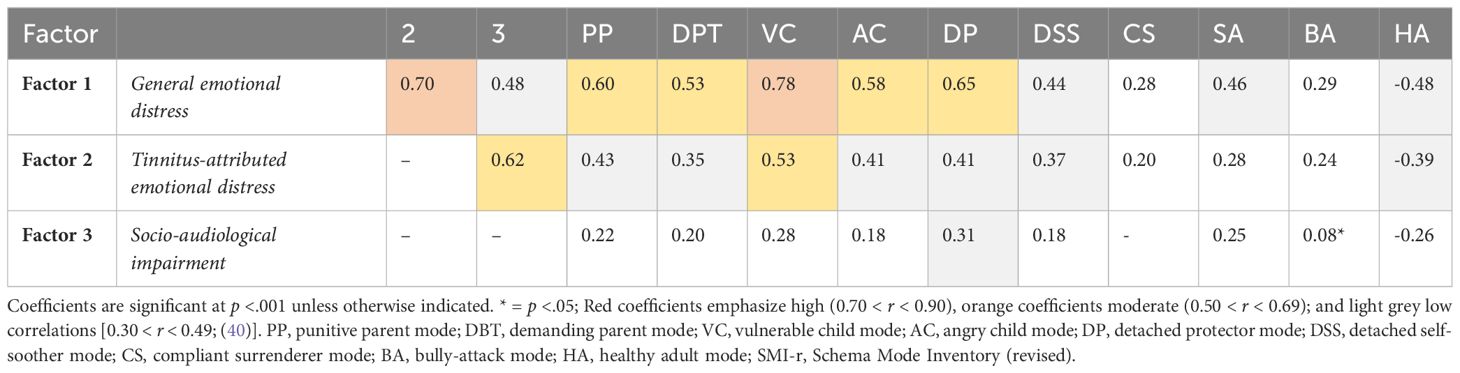
Results: A three-factor solution explained 37.4% of variance and represented 78% of the included items. Following item content examination, the factors represented (1) General emotional distress, (2) Tinnitus-attributed emotional distress, and (3) Socio-audiological impairment. Factors 1|2 correlated highly (r = 0.70), Factors 2|3 moderately (r = 0.62). Linked to the schema mode model, Factor 1 correlated highly with the “vulnerable child” (r = 0.78), and moderately with the “parent”, “angry child”, and “detached protector” modes (0.53 < r < 0.65). Factor 2 correlated moderately with the “vulnerable child” (r = 0.53). Factor 3 was largely uncorrelated with SMI-r scores – although a low correlation with the “detached protector” warrants further examination.
Conclusion: “General” and “tinnitus-attributed” emotional distress correlate highly – warranting holistic (not symptom-specific) psychological case conceptualization and treatment planning. Viewed from a schema mode perspective, the “vulnerable child” explains substantial variance across both dimensions. Consequently, autobiographically anchored, unmet emotional needs and emotional detachment constitute key treatment targets. Social-audiological impairment should be multimodally conceptualised and treated with hearing aids and psychological support measures, as applicable.
Introduction
Chronic tinnitus is a common and frequently disabling symptom which denotes “the conscious awareness of a tonal or composite noise for which there is no identifiable corresponding external acoustic source” [(1) p. 1]. Depending on a person’s internal psychological context, the symptom can be very distressing and place a significant burden on healthcare systems (2).
Often (though not always), chronic tinnitus occurs alongside high frequency hearing loss (3) – and both phenomena can contribute to psychological distress in emotionally vulnerable individuals. According to current treatment guidelines, chronic tinnitus is best treated with a combination of hearing aids and psychotherapy, where indicated (4–6). Evidence for the latter centers on cognitive-behavioral therapies (CBTs) as gold standard treatments (7). CBTs are a group of psychological treatment approaches that focus on individuals’ stimulus appraisals and behavior patterns - which interact to cause and maintain emotional distress and functional impairment (8). Therapeutic strategies aim to (1) flexibilise and expand individuals’ cognitive, emotional and behavioral range, and (2) help individuals to identify and meet their psychological needs through less maladaptive means than psychological symptom expression.
The basic tenets of this therapeutic method have been applied to a broad variety of psychological syndromes. Contrary to what is often assumed, however, “CBTs” are not uniform therapies. Rather, “CBT” is an umbrella term for numerous treatment approaches (9) – which differ in terms of their theories of etiology (how does psychopathology emerge?), process (how do respective theories of etiology imply ways of change?), and procedure (which therapeutic strategies are used to effect change?) (8). CBT approaches include, amongst others, cognitive therapy (CT; 10), problem-solving therapy (11), dialectical behavior therapy (12), metacognitive therapy (13), rational-emotive behavior therapy (14), cognitive processing therapy (15), mindfulness-based cognitive therapy (16), the cognitive-behavioural analysis system of psychotherapy (17), and schema-focused therapy [ST; (18)].
ST adopts a transdiagnostic, emotion-focused perspective, and integrates elements from cognitive, humanistic and psychodynamic treatments in its theory of distress-etiology, process, and change. Unlike “classic” CT, ST emphasizes biographical and relational influences on the development of maladaptive emotional-cognitive-behavioral patterns – so-called “schema modes” (19). These dynamic “self-states” (20) emerge or shift depending on interactions of internal or external circumstances and underlying, more stable personality traits (19). Schema modes can be broadly divided into (1) maladaptive parent, (2) maladaptive child, and (3) maladaptive coping modes as well as (4) a healthy adult mode (21). Maladaptive coping modes can further be grouped into (a) avoidant, (b) subordinating, and (c) overcompensatory strategies. In “parent mode”, individuals’ experiences and behaviours fuse with autobiographically shaped punitive or demanding beliefs; in “child mode” with primary emotions linked to unmet emotional needs; and in “coping mode” with secondary emotions or behaviours which aim to regulate or avoid emotion. Importantly, the schema mode model explicitly postulates that “psychopathology” differs from “normality” merely in terms of frequency and intensity (not “presence” or “quality”) of mode activations (18).
In clinical research and practice, the schema mode model is a helpful transdiagnostic concept that allows both patients and therapists to understand (shifts in) their ways of experiencing themselves, others and the world. The therapeutic process is guided by mode-specific goals that involve reducing maladaptive coping modes, facilitating the expression of child modes, and strengthening the healthy adult by means of cognitive, emotion-focused/experiential, and behavioral interventions.
Patients with chronic tinnitus frequently present with psychiatric syndromes – most notably major depressive-, anxiety-, or somatoform disorders (22, 23). Adopting a transdiagnostic perspective these psychiatric “comorbidities” may be understood as differential expressions of underlying, continuously distributed psychological dimensions (24, 25).
In line with ST’s conceptualization as a transdiagnostic approach (26), ST has demonstrated encouraging effects across a variety of syndrome categories – including those commonly encountered in patients with chronic tinnitus (27, 28). Surprisingly, however, STs’ utility has not yet been investigated in this population. Only one paper examined schema modes in patients with chronic tinnitus (29). The study demonstrated high expressions of child, avoidant, and subordinating coping modes, and a conspicuously low expression of the “punitive parent” mode. In extension of these results, the present study investigates (1) underlying dimensions of psychological distress in patients with chronic tinnitus, and (2) the usefulness of the schema mode model to help explain psychological distress variation in this population.
Methods
Participants
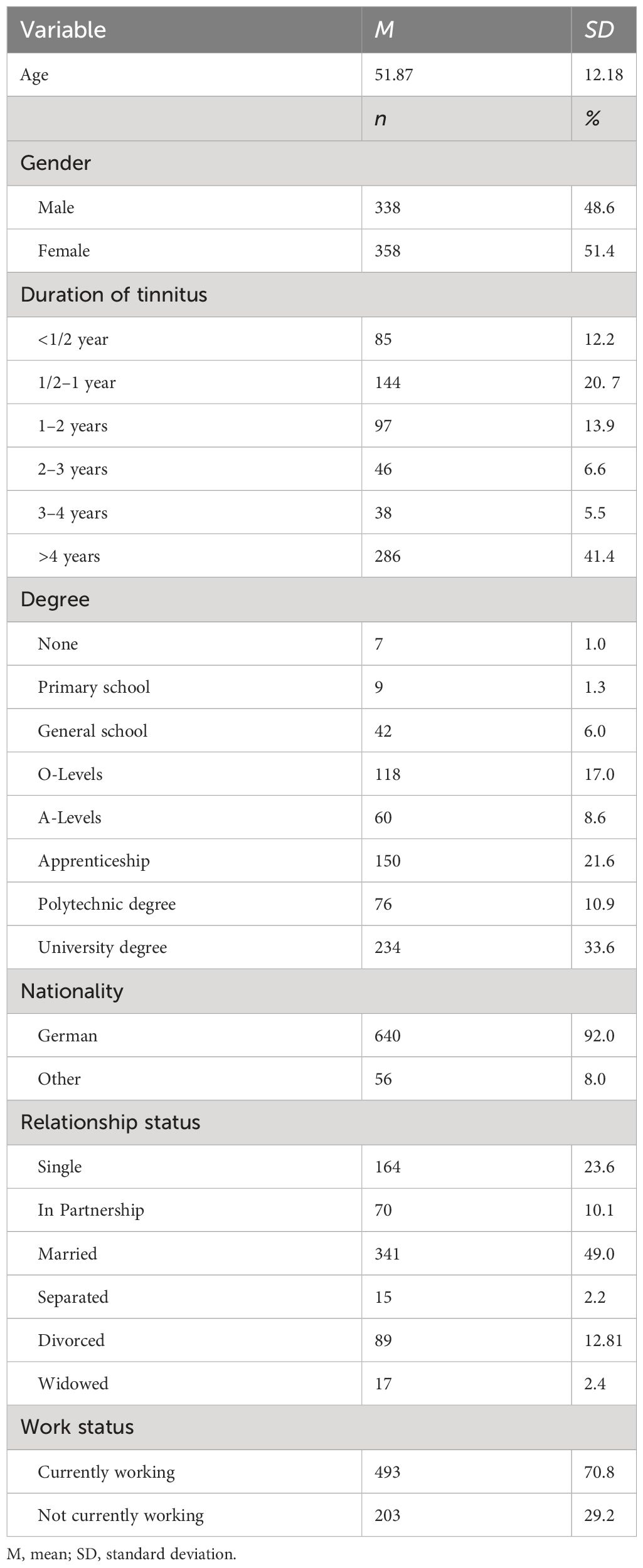
The present study reports self-report data from N = 696 patients who were sampled over a period of two years in routine clinical practice. Note that this paper uses parts of the same data set as reported in (29).
The sample comprised psychological self-report data from adult patients who (a) self-referred to the Tinnitus Centre at Charité Universitätsmedizin Berlin over a two-year period (January 2019 - December 2020), (b) suffered from chronic tinnitus (lasting for > 3 months). Upon joining the center, patients completed a psychological questionnaire battery which included, amongst other measures, German versions of the Tinnitus Questionnaire (TQ), Tinnitus Handicap Inventory (THI), Hospital Anxiety and Depression Scale (HADS), Perceived Stress Questionnaire (PSQ) and ICD-10 Symptom Rating (ISR). Serving as criterion, patients further completed 10 main scales of the revised Schema Mode Inventory (SMI-r). Patients were excluded if they suffered from acute psychotic illness or addiction, (untreated) deafness, or had insufficient knowledge of the German language. Roughly half of the sample (51%) was female. On average, patients were 52 years old (SD = 12 years; range = 19 – 82 years). Upon arrival at the Tinnitus Centre, patients completed a routine questionnaire assessment battery on electronic tablet devices. Participants provided written consent for data to be collected and used for research purposes, and the Charité Universitätsmedizin Berlin’s ethics committee approved data collection and analysis (No: EA4/216/20). Table 1 [see also (29)] provides an overview of the sample’s sociodemographic characteristics.
Measures
Primary measures
Tinnitus
The German version of the Tinnitus Questionnaire (30) is a self-report instrument measuring tinnitus-related distress. The German version consists of 52 items which are rated on a 3-point Likert scale (0 = not true, 1 = partly true, 2 = true). Forty items are used to calculate the total score. Because two items are included twice, the TQ total score ranges from 0 to 84 points. In the current sample, the scale’s internal consistency was excellent (α= 0.94).
Tinnitus handicap inventory (THI)
Subjective tinnitus handicap severity was additionally measured by the Tinnitus Handicap Inventory [(31); German version: (32)]. The THI consists of 25 items that are answered on a 3-point scale (0 = no; 2 = sometimes; 4 = yes) resulting in a total score between 0 and 100. In the current sample, the measure’s internal consistency was excellent (α = 0.93).
Hospital anxiety and depression scale (HADS)
Anxiety and depressive symptoms were measured using the Hospital Anxiety and Depression Scale (33, 34). The questionnaire combines two 7-item scales that measure anxious or depressive symptoms “during the last week” (0 = “not at all” to 3 = “mostly”). For the current sample, internal consistencies were good (αanxiety = 0.80; αdepression = 0.88).
Perceived stress questionnaire (PSQ)
The Perceived Stress Questionnaire (35, 36) assesses subjective stress experiences across four dimensions labelled “tension” [disquietude, exhaustion and lack of relaxation], “worries” [anxious concern for the future, and feelings of desperation and frustration], “joy” [positive feelings of challenge, joy, energy, and security] and “demands” [perceived environmental demands such as lack of time, pressure, and overload]). The scale consists of 30 items that are rated on a 4-point scale (1 = almost never, 2 = sometimes, 3 = often, 4 = almost always). All indices are linearly transformed to range from 0 to 100, and averaged into a total score for which joy is recoded. In the current sample, internal consistency was excellent (α = 0.94).
ICD-10 symptom rating
The ICD-10 Symptom Rating questionnaire measures diagnostic approximations for five psychiatric syndromes as operationalized in the International Classification of Diseases [ICD; (37)]. The ISR comprises 29 items that are answered on a 5-point Likert scale from 0 = strongly disagree to 4 = strongly agree. Item scores are averaged for five subscales that measure depressive, anxiety, obsessive-compulsive, somatoform and eating disorder-related phenomena. Averaging these subscale scores and including an additional scale’s score twice, a total score is computed. For the current sample, the measure’s internal consistency was excellent (αtotal = 0.92).
Criterion
Schema mode inventory – revised
The revised version of the Schema Mode Inventory (SMI-r) is a 124-item self-report questionnaire which measures the frequency of occurence of 14 schema modes (i.e. cognitive-affective-behavioural self-states) (38). As previously reasoned in (29), we selected the 10 most common modes for reasons of theoretical relevance and in order to reduce response burden. Participants thus rated 86 items on a 6-point Likert scale from 1 = “never or hardly ever” to 6 = “always”. Ratings were averaged into mode scores – with higher scores indicating higher frequency of mode manifestations.
The present study assessed (1) two maladaptive parent modes: the punitive parent (PP) and the demanding parent (DPT), (2) two maladaptive child modes: the vulnerable child (VC) and the angry child (AC), (3) five maladaptive coping modes that are subdivided into (a) two avoidant coping modes: the detached protector (DP) and the detached self-soother (DSS), (b) one subordinating coping mode: the compliant surrenderer (CS), and (c) two overcompensating modes: the self-aggrandizer (SA), and bully-and-attack (BA). Last, healthy emotion-regulation abilities and cognitive-affective resources were measured via (4) the healthy adult (HA).
On an individual’s inner stage, the PP devalues, criticizes, blackmails, and punishes the self or others. The DPT places high responsibilities and standards on the self or others and pressures the individual never to make mistakes or fail to live up to (others’) high expectations.
The VC experiences deep feelings of loneliness, fear, unhappiness, and helplessness; whilst the AC feels infuriated, angry, and indignant that the VC’s needs are not met.
The DP avoids, and withdraws or disconnects from both emotional states and meaningful human contact. The DP can involve ‘cognitive’ ways of dealing with emotional distress (e.g. being overly rational or intellectualizing, superficial, vague or in demand of concrete ‘solutions’). The DSS has a similar agenda, yet uses repetitive, seemingly pleasurable activities to distance a person from emotions or meaningful connections.
The CS appears to comply with others’ demands in order to avoid emotional vulnerability. Whilst appearing subordinate, passive, or dependent, the CS may equally be characterized by strong indirect expressions of anger and self-assertion.
The SA feels superior, special, and powerful. It stabilizes the self by dismissing or devaluing others’ opinions, feelings, or needs; and may resort to boastful or exploitative behaviors to achieve a sense of safety. The BA Mode aims to secure the vulnerable child by humiliating, intimidating, and destroy other people – both psychologically and behaviorally.
The German version of the SMI-r yields good-to-excellent internal consistency and construct validity (39). In the current sample, internal consistencies were acceptable-to-excellent (αpunitive parent = 0.84; αdemanding parent = 0.84; αvulnerable child = 0.93; αangry child = 0.84; αdetached protector = 0.86; αdetached self-soother = 0.72; αcompliant surrenderer = 0.73; αself-aggrandizer = 0.79; αbully and attack = 0.79; αhealthy adult = 0.81).
Data analysis
Analyses were conducted using IBM SPSS Statistics for Windows, Version 24. First, we report descriptive statistics and correlation coefficients r for the primary measures. Note that the reported descriptives in Tables 2 and 3 were previously reported in (29) - and are repeated here to provide background for the interpretation of the factor analysis. Next, the overall item-pool of the TQ, THI, PSQ, HADS, and ISR (128 items) underwent a principal axis factor analysis with varimax rotation. Following the identification of an appropriate factor solution, we computed factor scores as the mean of the respectively loading items per factor1. These factor scores were then correlated with the SMI-r to aid factor interpretation by means of the schema mode model. Correlation coefficients were defined as negligible (0.00–0.29), low (0.30 – 0.49), moderate (0.50–0.69), high (0.70–0.89) or very high [≥ 0.90; (40)].
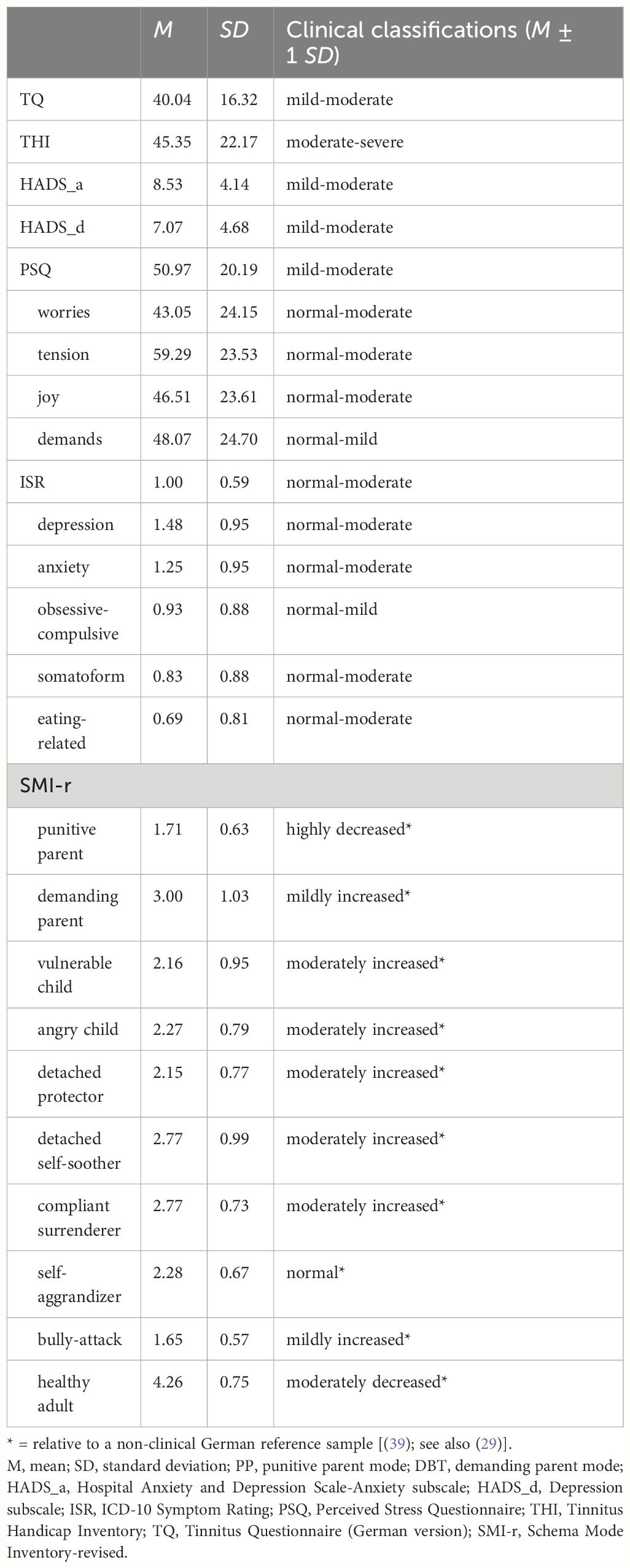
Table 2 Means and standard deviations for the examined questionnaires for N = 696 patients with chronic tinnitus.
Results
Descriptive indices
Table 2 reports means and standard deviations for the completed questionnaires. Overall, the questionnaire scores yielded relatively broad distributions suggesting substantial psychological heterogeneity (41).
Table 3 reports Pearson’s correlation coefficients (r) between the primary outcome measures. All measures correlated at p <.001.
To identify latent psychological dimensions, a varimax-rotated principal axis factor analysis was conducted on the 128 items of the primary measures (TQ, THI, HADS_a, HADS_d, PSQ, and ISR). The Kaiser-Meyer-Olin measure verified the sampling adequacy for the analysis [KMO = 0.96; ‘marvelous’ (42)]. The scree plot was ambiguous and showed inflexions that would justify a 3- or 4-factor solution (see Figure 1). Because of the relatively small sample size and small relative increase in explained variance, we opted for the 3-factor solution (37.41% of the variance [vs. 40.25% for the 4-factor solution2]).
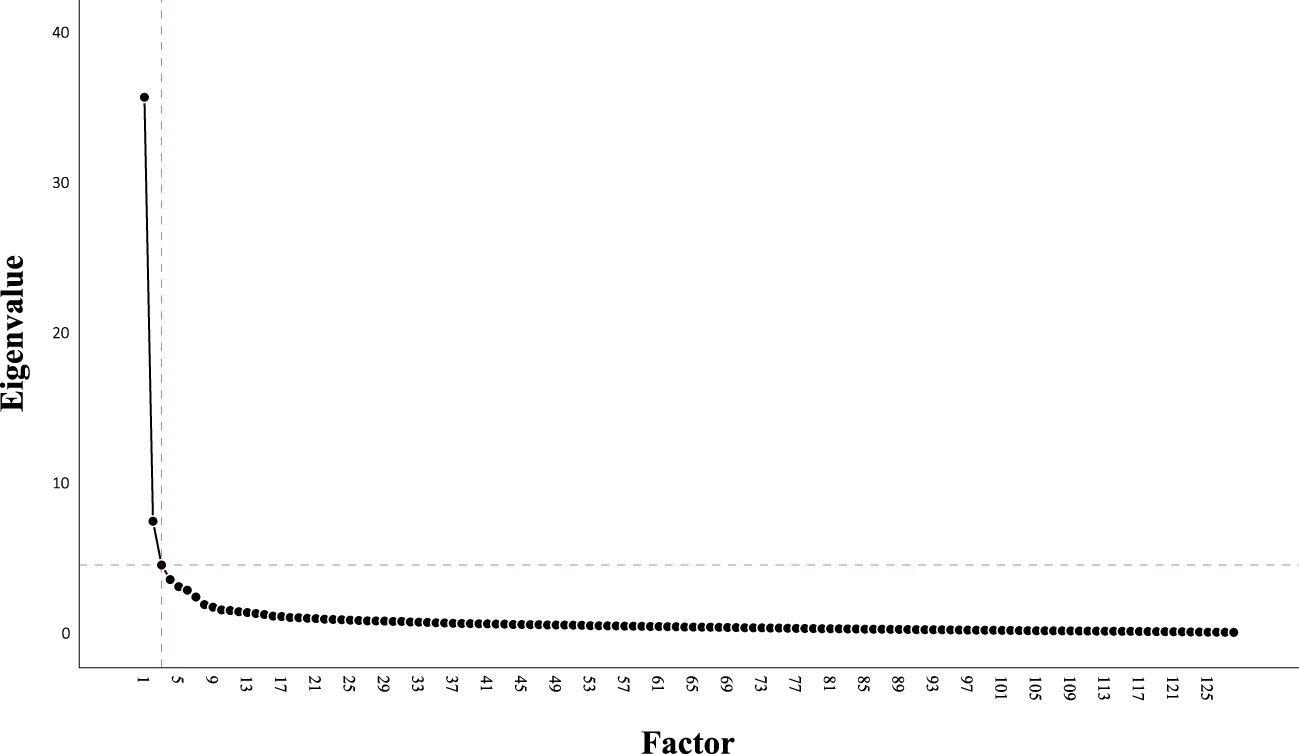
Figure 1 Scree plot of principal axis factor analysis with varimax rotation for N = 696 patients with chronic tinnitus on all items from the TQ, THI, HADS_a, HADS_d, PSQ, and ISR.
Following item-content screening, Factor 1 likely represents “General emotional distress” (27.93% of variance; highest loading items: “I feel happy”, “You have fun” [-0.78, -0.76]), Factor 2 “Tinnitus-attributed emotional distress” (5.88% of variance; highest loading items: “Are you depressed because of the tinnitus?”, “Do you feel desperate because of the tinnitus?” [0.69, 0.68]), and Factor 3 “Socio-audiological impairment” (3.60% of variance; highest loading items: “Because of the tinnitus, it is more difficult for me to follow a conversation”, “Does the volume of your tinnitus prevent you from understanding other people?” [0.81, 0.79]). For an overview of items and factor loadings, see Online Supplementary 1.
To examine, if the factor solution could be interpreted within the schema mode model, correlation coefficients r examined associations between the factor scores and the SMI-r (see Table 4 and Figure 2). High correlations emerged between Factors 1 and 2, as well as Factor 1 and the "vulnerable child". Moderate correlations emerged for Factors 2 and 3; Factor 1 and the “parent”, “angry child”, and “detached protector”; and Factor 2 and the “vulnerable child”. Factor 3 was largely uncorrelated with SMI-r scores – although a low correlation with the “detached protector” warrants further examination.
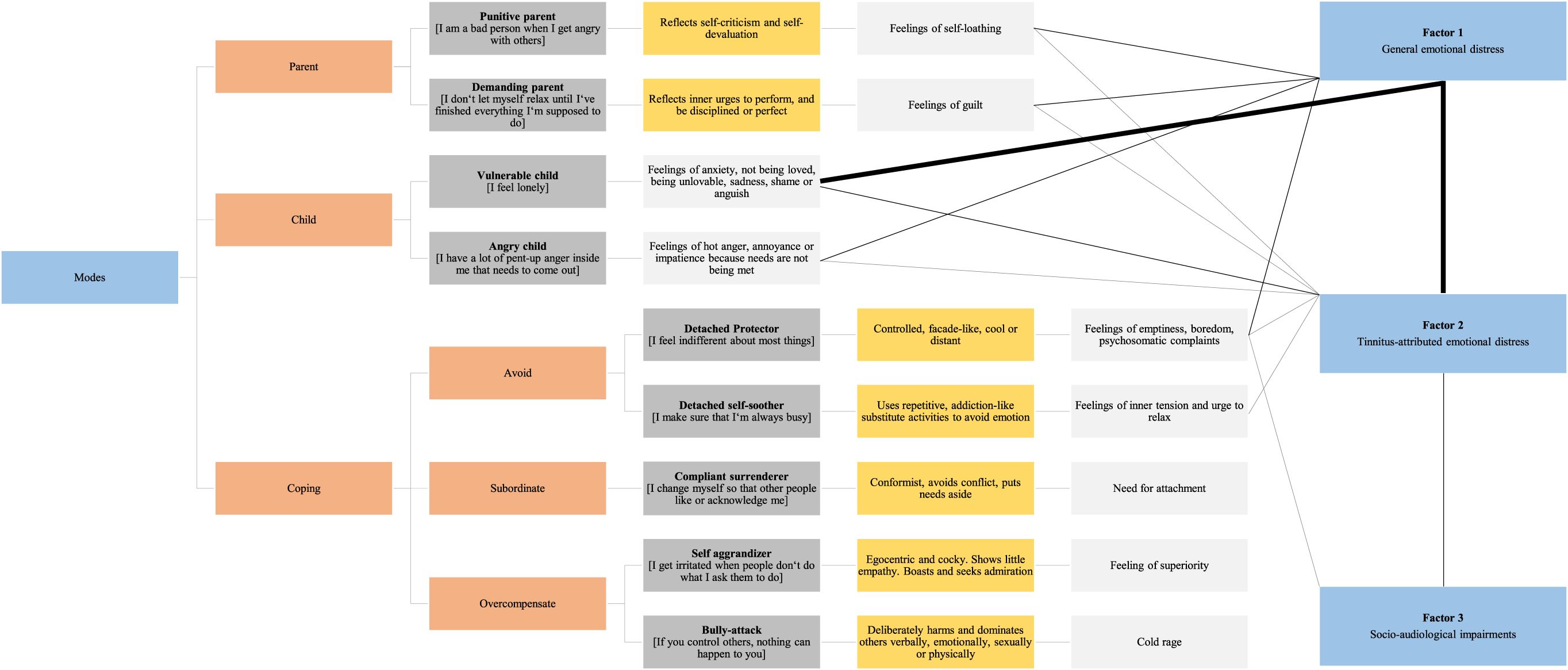
Figure 2 The schema mode model (left) and identified dimensions of psychological distress (right). Orange boxes indicate superordinate mode groups, dark grey boxes associated modes and exemplary measurement items, yellow boxes the “quality” of the mode as reflected in the actualized clinical patient presentation, and light grey boxes associated emotions or emotional needs respectively. Strong black lines represent high (0.70 < r < 0.90), thin black lines moderate (0.50 < r < 0.69), and grey lines low correlations [0.30 < r < 0.49; (40)].
Discussion
The present study examined self-report data from N = 696 patients with chronic tinnitus. Participants completed measures of tinnitus-related distress, anxiety, depression, perceived stress, and psychological symptoms across a variety of common psychiatric syndrome diagnoses. The study aimed to identify transdiagnostic dimensions of psychological distress – and whether schema modes might help formulate these dimensions.
In keeping with common observations in this patient population (41), all psychological distress measures (a) intercorrelated highly and (b) yielded broad confidence intervals suggesting high levels of heterogeneity. Factor-analytic models exploit such correlational patterns in order to empirically identify psychological, behavioral or physiological risk factors for psychopathology (43, 44). The present study used a varimax-rotated principal axis factor analysis and identified a three-factor structure which explained 37.41% of variance. The factors likely represented (1) General emotional distress, (2) Tinnitus-attributed emotional distress, and (3) Socio-audiological impairment. Factors 1|2 correlated highly at r = 0.70, Factors 2|3 moderately at r = 0.62. Conceptually, the measures’ indices of “anxiety”, “depression”, “perceived stress”, and “psychiatric syndromes” all constitute differential expressions of a common underlying factor – which may either precede or ‘incorporate’ the tinnitus symptom (45, 46). The current factor solution somewhat reflects results from a previous study that labelled “stress”, “pain experience”, “fatigue”, “autonomy”, and “educational level” as dimensions of tinnitus-related distress in a sample of N = 1958 patients with chronic tinnitus (47).
Clinically, the data support the importance of formulating the tinnitus symptom in context of individuals’ autobiographical and current distress experiences (48–50). Consequently, psychologists and psychotherapists ought to move beyond somewhat simplistic symptom-specific (“depressed because of tinnitus”) or categorical, syndrome-specific understandings of emotional distress (“treat ‘the tinnitus’ – then ‘the depression’”). Rather, it is important to adopt a person- (not symptom-) centered perspective that (1) shifts its therapeutic focus away from the tinnitus symptom towards its idiographic appraisal and assigned meaning in context of individuals’ biographies and current lives, and (2) adopts an emotion-focused stance in order to understand and ameliorate patients’ distress in context of their autobiographical, affective and relational complexity (51–53).
One such perspective is offered by so-called “schema mode” approach – which is located in the overall landscape of cognitive-behavioural therapies (18, 21, 54). In the present study, the “vulnerable child” accounted for substantial proportions of psychological distress (61% of Factor 1 and 28% of Factor 2’s variance). Thus, patients’ distress experiences appear to be characterized by feelings of inadequacy, worthlessness, despair, loneliness, fear, and helplessness. These emotional states (1) may reflect difficult biographical experiences (as indexed by moderate correlations between Factor 1 and the parent modes) and (2) are primarily managed by the “detached protector” (as similarly indexed by its moderate correlation with Factor 1). Whilst the importance of these feelings has been previously highlighted (55), the available literature tends to link (and discuss) these feelings exclusively (with regard) to the tinnitus-symptom. In doing so, correlation and causation are frequently confounded at the expense of (1) biographical experiences that shape the habitual appraisal of stimuli as well as unmet emotional needs (which inform symptom function), and (2) third variables that may influence both tinnitus-symptom onset and tinnitus-distress variability (56–58). Overall, therapeutic endeavors ought to (1) focus on reducing emotional avoidance and (2) explore the symptom’s intrapsychic and interpersonal functions en route to discovering and integrating distressing affective states into the healthy adult mode.
The moderate correlation between Factors 2|3 suggests that “socio-audiological impairment” (Factor 3) interacts with tinnitus-attributed distress - and thus represents an important psychosocial treatment goal. Although hearing-related difficulties undoubtedly underlie a major part of audiological impairments and initial tinnitus-symptom onset (3), psychological factors also influence both groups of phenomena (59–63). Whilst current treatment guidelines recommend hearing amplification measures for patients with chronic tinnitus and hearing loss (5, 6), it is crucial to conceptualize hearing loss with a view to its broader socio-psychological consequences (60, 62, 64, 65). In our data, the small-yet-significant correlation between Factor 3 and the “detached protector” raises the interesting possibility that emotional avoidance may interact with socio-audiological difficulties – which thus ought to be conceptualized holistically.
The current study has several limitations. For example, self-report data feature common limitations [(66); yet see also 67)]. In addition, factor analytic results and factor interpretations are never “true”. Rather, they depend on the selection and content of the originally included item set, as well as statistical and theoretical considerations regarding the number and nature of the extracted factors. Last, factor analyses are a regression-based method which disallows causal conclusions. Thus, future studies need to demonstrate the clinical usefulness of schema therapeutic approaches in addressing common underlying factors of emotional distress in patients with chronic tinnitus. Clinically and crucially, a mechanistic or medicalized view of psychological interventions risks underestimating or ignoring strong evidence for relational humanistic factors that actually make psychotherapy effective (68–71).
Nonetheless, the present study (1) replicates and expands previous factor analytic work regarding tinnitus-related psychopathology (47), (2) identifies three transdiagnostic psychological dimensions, (3) links these constructs to a potentially useful emotion-focused “new” cognitive-behavioural therapy framework (54, 72), and, thereby (4) encourages future empirical examination of short-term group or individual schema-therapy-based interventions in patients with chronic tinnitus (73–75). With its dynamic focus on intra- and interpersonal cognitive-emotional states, the schema-mode model offers a useful approach for researchers and clinicians alike to conceptualize and alleviate emotional distress in patients with chronic tinnitus.
Data availability statement
The datasets presented in this article are not readily available. As per Charité Universitaetsmedizin Berlin’s ethics committee, the data cannot be made public without restrictions because patients did not give consent at the time. Requests to access the data should be directed to the directorate of the Tinnitus Center Charité Universitaetsmedizin Berlin (YmlyZ2l0Lm1henVyZWtAY2hhcml0ZS5kZQ==) or Charité's Open Data and Research Data Management Officer, Dr. Evgeny Bobrov (ZXZnZW55LmJvYnJvdkBjaGFyaXRlLmRl).
Ethics statement
The studies involving humans were conducted in accordance with the Declaration of Helsinki, and approved by the ethics committee of Charité Universitatsmedizin Berlin (EA4/216/20). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BB: Writing – review & editing, Writing – original draft, Visualization, Project administration, Methodology, Formal analysis, Data curation, Conceptualization. PB: Writing – review & editing. BM: Writing – review & editing, Supervision, Resources.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1375813/full#supplementary-material
Footnotes
- ^ Items who loaded on more than one factor, were included once in the factor score of their highest loading.
- ^ Factor 4 appeared to reflect "Overstraining" (5 items [PSQ 3, 20, 2, 19, 11]; 2.84% of variance; highest loading items “You have too much to do”, “You feel under deadline pressure” [0.80, 0.77]) – and correlated moderately with Factor 1 (r = 0.51) and the “demanding parent” mode (r = 0.54).
References
1. De Ridder D, Schlee W, Vanneste S, Londero A, Weisz N, Kleinjung T, et al. Tinnitus and tinnitus disorder: Theoretical and operational definitions (an international multidisciplinary proposal). Prog Brain Res. (2021) 260:1–25. doi: 10.1016/bs.pbr.2020.12.002
2. Biswas R, Lugo A, Akeroyd MA, Schlee W, Gallus S, Hall DA. Tinnitus prevalence in Europe: A multi-country cross-sectional population study. Lancet Regional Health-Europe. (2022) 12:100250. doi: 10.1016/j.lanepe.2021.100250
3. Biswas R, Genitsaridi E, Trpchevska N, Lugo A, Schlee W, Cederroth CR, et al. Low evidence for tinnitus risk factors: A systematic review and meta-analysis. J Assoc Res Otolaryngol. (2023) 24(1):81–94. doi: 10.1007/s10162-022-00874-y
4. Fuller T, Haider HF, Kikidis D, Lapira A, Mazurek B, Norena A, et al. Different teams, same conclusions? A systematic review of existing clinical guidelines for the assessment and treatment of tinnitus in adults. Front Psychol. (2017) 8:206. doi: 10.3389/fpsyg.2017.00206
5. Cima RFF, Mazurek B, Haider H, Kikidis D, Lapira A, Noreña A, et al. A multidisciplinary European guideline for tinnitus: Diagnostics, assessment, and treatment. HNO. (2019) 67:1. doi: 10.1007/s00106-019-0633-7
6. Mazurek B, Hesse G, Sattel H, Kratzsch V, Lahmann C, Dobel C. S3 guideline: chronic tinnitus: german society for otorhinolaryngology, head and neck surgery e. V.(DGHNO-KHC). HNO. (2022) 70:11. doi: 10.1007/s00106-022-01207-4
7. Fuller T, Cima R, Langguth B, Mazurek B, Vlaeyen JW, Hoare DJ. Cognitive behavioural therapy for tinnitus. Cochrane Database Systematic Rev. (2020) 1:1. doi: 10.1002/14651858.CD012614.pub2
8. Hollon SD, Beck AT. Cognitive and cognitive-behavioral therapies. In: Bergin and Garfield’s handbook of psychotherapy and behavior change. (New York: Wiley), vol. 6. (2013). p. 393–442.
9. Gaudiano BA. Cognitive-behavioural therapies: Achievements and challenges. BMJ Ment Health. (2008) 11:5–7. doi: 10.1136/ebmh.11.1.5
10. Beck AT. Cognitive therapy and the emotional disorders. New York, NY: International Universities Press (1979).
11. D’Zurilla TJ, Nezu AM. Problem-solving therapy. In: Handbook of cognitive-behavioral therapies. 3rd edition. New York: Guilford Press (2010). p. 197–225.
12. Linehan MM. Dialectical behavior therapy for borderline personality disorder: Theory and method. Bull Menninger Clinic. (1987) 51:261.
14. Ellis A. Rational emotive behaviour therapy. In: Six key approaches to counseling & therapy. Paston PrePress, London (2000). p. 181–227.
15. Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. J consulting Clin Psychol. (1992) 60:748. doi: 10.1037//0022-006X.60.5.748
16. Segal ZV, Teasdale JD, Williams JMG. Mindfulness-Based Cognitive Therapy: Theoretical Rationale and Empirical Status. New York: Guilford Press (2004).
17. McCullough JP Jr. Treatment for chronic depression: Cognitive behavioral analysis system of psychotherapy (CBASP). J Clin Psychol. (2003) 59(8):833–84. doi: 10.1002/jclp.10176
18. Young JE, Klosko JS, Weishaar ME. Schema therapy: A practitioner’s guide. New York: Guilford Press (2003).
19. Fassbinder E, Brand-de Wilde O, Arntz A. Case formulation in schema therapy: Working with the mode model. In: Case formulation for personality disorders. Academic Press (2019). p. 77–94.
20. Siegel DJ. The developing mind: How relationships and the brain interact to shape who we are. New York: Guilford Press (2020).
21. Arntz A, Jacob G. Schema therapy in practice: An introductory guide to the schema mode approach. John Wiley & Sons (2017).
22. Zöger S, Svedlund J, Holgers K-M. Relationship between tinnitus severity and psychiatric disorders. Psychosomatics. (2006) 47:4. doi: 10.1176/appi.psy.47.4.282
23. Zirke N, Seydel C, Arsoy D, Klapp BF, Haupt H, Szczepek AJ, et al. Analysis of mental disorders in tinnitus patients performed with Composite International Diagnostic Interview. Qual Life Res. (2013) 22:8. doi: 10.1007/s11136-012-0338-9
24. Kleinstäuber M, Weise C. Psychosocial variables that predict chronic and disabling tinnitus: A systematic review. In: Searchfield G, Zhang H, editors. The Behavioral Neuroscience of Tinnitus. Current Topics in Behavioral Neurosciences, vol. 51 . Springer, Cham (2021). p. 361–80.
25. Boecking B, von Sass J, Sieveking A, Schaefer C, Brueggemann P, Rose M, et al. Tinnitus-related distress and pain perceptions in patients with chronic tinnitus–Do psychological factors constitute a link? PloS One. (2020) 15:6. doi: 10.1371/journal.pone.0234807
26. Fassbinder E, Arntz A. Schema therapy. In Wenzel A. (Ed.) Handbook of cognitive behavioral therapy: Overview and approaches. American Psychological Association. (2021) 493–537. doi: 10.1037/0000218‐017
27. Hawke LD, Provencher MD. Schema theory and schema therapy in mood and anxiety disorders: A review. J Cogn Psychother. (2011) 25:4. doi: 10.1891/0889-8391.25.4.257
28. Henker J, Keller A, Reiss N, Siepmann M, Croy I, Weidner K. Early maladaptive schemas in patients with somatoform disorders and somatization. Clin Psychol Psychother. (2019) 26:4. doi: 10.1002/cpp.2363
29. Boecking B, Stoettner E, Brueggemann P, Mazurek B. Emotional self-states and coping responses in patients with chronic tinnitus: A schema mode model approach. Front Psychiatry. (2024) 15:1257299. doi: 10.3389/fpsyt.2024.1257299
30. Goebel G, Hiller W. Tinnitus-Fragebogen (TF). Standardinstrument zur Graduierung des Tinnitusschweregrades. Erbebnisse einer Multicenterstudie mit dem Tinnitus-Fragebogen (TF). HNO. Hals- Nasen- Ohrenärzte. (1994) 42(3):166–72.
31. Newman CW, Jacobson GP, Spitzer JB. Development of the tinnitus handicap inventory. Arch Otolaryngology–Head Neck Surg. (1996) 122:2. doi: 10.1001/archotol.1996.01890140029007
32. Kleinjung T, Fischer B, Langguth B, Sand PG, Hajak G, Dvorakova J, et al. Validierung einer deutschsprachigen Version des „Tinnitus Handicap Inventory”. Psychiatrische Praxis. (2007) 34:1. doi: 10.1055/s-2006-940218
33. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta psychiatrica scandinavica. (1983) 67:6. doi: 10.1111/j.1600-0447.1983.tb09716.x
34. Herrmann C, Buss U, Snaith RP. HADS-D: Hospital anxiety and depression scale-German version. Bern: Hans Huber. (1995) 1:995.
35. Fliege H, Rose M, Arck P, Levenstein S, Klapp BF. Validierung des “perceived stress questionnaire”(PSQ) an einer deutschen Stichprobe.[Validation of the “Perceived Stress Questionnaire”(PSQ) in a German sample.]. Diagnostica. (2001) 47:3. doi: 10.1026//0012-1924.47.3.142
36. Fliege H, Rose M, Arck P, Walter OB, Kocalevent R-D, Weber C, et al. The Perceived Stress Questionnaire (PSQ) reconsidered: Validation and reference values from different clinical and healthy adult samples. Psychosomatic Med. (2005) 67:1. doi: 10.1097/01.psy.0000151491.80178.78
37. World Health Organization. The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research. World Health Organization (1993).
38. Lobbestael J, van Vreeswijk M, Spinhoven P, Schouten E, Arntz A. Reliability and validity of the short Schema Mode Inventory (SMI). Behav Cogn Psychother. (2010) 38:4. doi: 10.1017/S1352465810000226
39. Reiss N, Dominiak P, Harris D, Knörnschild C, Schouten E, Jacob GA. Reliability and validity of the German version of the Schema Mode Inventory. Eur J psychol Assessment. (2012) 28:297–304. doi: 10.1027/1015-5759/a000110
40. Mukaka MM. A guide to appropriate use of correlation coefficient in medical research. Malawi Med J. (2012) 24:69–71.
41. Cederroth CR, Gallus S, Hall DA, Kleinjung T, Langguth B, Maruotti A, et al. Towards an understanding of tinnitus heterogeneity. Front Aging Neurosci. (2019) 11:53. doi: 10.3389/fnagi.2019.00053
42. Kaiser HF, Rice J. Little jiffy, mark IV. Educ psychol measurement. (1974) 34:111–7. doi: 10.1177/001316447403400115
43. Waszczuk MA, Kotov R, Ruggero C, Gamez W, Watson D. Hierarchical structure of emotional disorders: From individual symptoms to the spectrum. J Abnormal Psychol. (2017) 126:613. doi: 10.1037/abn0000264
44. Conway CC, Forbes MK, Forbush KT, Fried EI, Hallquist MN, Kotov R, et al. A hierarchical taxonomy of psychopathology can transform mental health research. Perspect psychol Sci. (2019) 14:419–36. doi: 10.31234/osf.io/wsygp
45. Trevis KJ, McLachlan NM, Wilson SJ. Psychological mediators of chronic tinnitus: The critical role of depression. J Affect Disord. (2016) 204:234–40. doi: 10.1016/j.jad.2016.06.055
46. Wallhäusser-Franke E, D’Amelio R, Glauner A, Delb W, Servais JJ, Hörmann K, et al. Transition from acute to chronic Tinnitus: Predictors for the Development of chronic Distressing Tinnitus. Front Neurol. (2017) 8:605. doi: 10.3389/fneur.2017.00605
47. Brueggemann P, Mebus W, Boecking B, Amarjargal N, Niemann U, Spiliopoulou M, et al. Dimensions of tinnitus-related distress. Brain Sci. (2022) 12:2. doi: 10.3390/brainsci12020275
48. Boecking B, Brueggemann P, Mazurek B. Tinnitus: psychosomatische aspekte. HNO. (2019) 67:137–52. doi: 10.1007/s00106-019-0609-7
49. Biehl R, Boecking B, Brueggemann P, Grosse R, Mazurek B. Personality traits, perceived stress, and tinnitus-related distress in patients with chronic tinnitus: support for a vulnerability-stress model. Front Psychol. (2020) 10. doi: 10.3389/fpsyg.2019.03093
50. Boecking B, Brueggemann P, Rose M, Mazurek B. Chronischer Tinnitus im Wechselspiel somatischer und psychischer Faktoren. HNO. (2023) 71:719–30. doi: 10.1007/s00106–023-01370–2
51. Johnstone L, Dallos R. Formulation in psychology and psychotherapy: Making sense of people’s problems. London, New York: Routledge (2013). doi: 10.4324/9780203380574
52. Ong CW, Hayes SC, Hofmann SG. A process-based approach to cognitive behavioral therapy: A theory-based case illustration. Front Psychol. (2022) 13:6840. doi: 10.3389/fpsyg.2022.1002849
53. Moskow DM, Ong CW, Hayes SC, Hofmann SG. Process-based therapy: A personalized approach to treatment. J Exp Psychopathol. (2023) 14:1. doi: 10.1177/20438087231152848
54. Bär A, Bär HE, Rijkeboer MM, Lobbestael J. Early Maladaptive Schemas and Schema Modes in clinical disorders: A systematic review. Psychol Psychotherapy: Theory Res Practice. (2023) 96(3):716–47. doi: 10.1111/papt.12465
55. Marks E, Smith P, McKenna L. Living with tinnitus and the health care journey: An interpretative phenomenological analysis. Br J Health Psychol. (2019) 24:2. doi: 10.1111/bjhp.12351
56. Probst T, Pryss R, Langguth B, Schlee W. Emotional states as mediators between tinnitus loudness and tinnitus distress in daily life: Results from the “TrackYourTinnitus” application. Sci Rep. (2016) 6:20382. doi: 10.1038/srep20382
57. Probst T, Pryss R, Langguth B, Schlee W. Emotion dynamics and tinnitus: Daily life data from the “TrackYourTinnitus” application. Sci Rep. (2016) 6:1. doi: 10.1038/srep31166
58. Simoes J, Bulla J, Neff P, Pryss R, Marcrum SC, Langguth B, et al. Daily contributors of tinnitus loudness and distress: An ecological momentary assessment study. Front Neurosci. (2022) 16:883665. doi: 10.3389/fnins.2022.883665
59. Nilo ER, Saunders WH. Functional hearing loss. Laryngoscope. (1976) 86:501–5. doi: 10.1288/00005537-197604000-00004
60. Arlinger S. Negative consequences of uncorrected hearing loss-a review. Int J audiology. (2003) 42:2S17–20. doi: 10.3109/14992020309074639
61. Keidser G, Seeto M, Rudner M, Hygge S, Rönnberg J. On the relationship between functional hearing and depression. Int J Audiology. (2015) 54:10. doi: 10.3109/14992027.2015.1046503
62. Blazer DG, Tucci DL. Hearing loss and psychiatric disorders: A review. psychol Med. (2019) 49:6. doi: 10.1017/S0033291718003409
63. Lawrence BJ, Jayakody DM, Bennett RJ, Eikelboom RH, Gasson N, Friedland PL. Hearing loss and depression in older adults: A systematic review and meta-analysis. Gerontologist. (2020) 60:3. doi: 10.1093/geront/gnz009
64. Austen S, Lynch C. Non-organic hearing loss redefined: Understanding, categorizing and managing non-organic behaviour. Int J Audiology. (2004) 43:8. doi: 10.1080/14992020400050057
65. Hoare DJ, Edmondson-Jones M, Sereda M, Akeroyd MA, Hall D. Amplification with hearing aids for patients with tinnitus and co-existing hearing loss. Cochrane Database systematic Rev. (2014) 1:1. doi: 10.1002/14651858.CD010151.pub2
66. Razavi T. Self-report measures: An overview of concerns and limitations of questionnaire use in occupational stress research. (2001). Available online at: https://eprints.soton.ac.uk/35712.
67. Chan D. So why ask me? Are self-report data really that bad? In: Statistical and methodological myths and urban legends. New York: Routledge (2010). p. 329–56. doi: 10.4324/9780203867266–22/ask-self-report-data-really-bad-david-chan
68. Martin DJ, Garske JP, Davis MK. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. J consulting Clin Psychol. (2000) 68:438. doi: 10.1037//0022-006X.68.3.438
69. Wampold BE. Humanism as a common factor in psychotherapy. Psychotherapy. (2012) 49:4. doi: 10.1037/a0027113
70. Baier AL, Kline AC, Feeny NC. Therapeutic alliance as a mediator of change: A systematic review and evaluation of research. Clin Psychol Rev. (2020) 82:101921. doi: 10.1016/j.cpr.2020.101921
71. Wampold BE. How important are the common factors in psychotherapy? An update. World Psychiatry. (2015) 14:3. doi: 10.1002/wps.20238
72. Lazarus G, Rafaeli E. Modes: Cohesive personality states and their interrelationships as organizing concepts in psychopathology. J Psychopathol Clin Sci. (2023) 132:238. doi: 10.1037/abn0000699
73. van Vreeswijk M, Broersen J. Schema therapy in groups: a short-term schema CBT protocol. In: van Vreeswijk M, Broersen J, Nadort M (Eds.), The WileyBlackwell handbook of schema therapy. Sussex: Wiley (2012). pp. 373–82.
74. Van Vreeswijk MF, Spinhoven P, Eurelings-Bontekoe EHM, Broersen J. Changes in symptom severity, schemas and modes in heterogeneous psychiatric patient groups following short-term schema cognitive–behavioural group therapy: A naturalistic pre-treatment and post-treatment design in an outpatient clinic. Clin Psychol Psychother. (2014) 21:29–38. doi: 10.1002/cpp.1813
Keywords: tinnitus, schema therapy, schema mode model, perceived stress, anxiety, depression, psychological therapy
Citation: Boecking B, Brueggemann P and Mazurek B (2024) “I feel [so alone] nothing” – emotional vulnerability and detachment as transdiagnostic key characteristics of patients with chronic tinnitus: a schema mode model approach. Front. Psychiatry 15:1375813. doi: 10.3389/fpsyt.2024.1375813
Received: 24 January 2024; Accepted: 26 April 2024;
Published: 18 June 2024.
Edited by:
Stephan Zipfel, University of Tübingen, GermanyReviewed by:
Soly I. Erlandsson, University West, SwedenHeike Argstatter, Musikpraxis Heidelberg, Germany
Copyright © 2024 Boecking, Brueggemann and Mazurek. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Benjamin Boecking, YmVuamFtaW4uYm9lY2tpbmdAY2hhcml0ZS5kZQ==; Birgit Mazurek, YmlyZ2l0Lm1henVyZWtAY2hhcml0ZS5kZQ==
 Benjamin Boecking
Benjamin Boecking Petra Brueggemann
Petra Brueggemann Birgit Mazurek
Birgit Mazurek