
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 11 June 2024
Sec. Anxiety and Stress Disorders
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1373602
This article is part of the Research Topic Traumatic Brain Injury and Post-Traumatic Stress Disorder: From Neurobiology to Treatment View all 6 articles
 Desalegn Adugna1
Desalegn Adugna1 Tesfaye Assebe Yadeta2
Tesfaye Assebe Yadeta2 Jerman Dereje3*†
Jerman Dereje3*† Dawit Firdisa1*†
Dawit Firdisa1*† Samuel Demissie Darcho1
Samuel Demissie Darcho1 Obsan Kassa1
Obsan Kassa1 Monas Kitessa4
Monas Kitessa4 Asefa Tola Gemeda1
Asefa Tola Gemeda1Background: Post-traumatic stress disorder (PTSD) is characterized by heightened stress and anxiety after experiencing a traumatic event. While numerous studies have been conducted to investigate the magnitude and factors associated with PTSD, there is limited evidence available on specific study populations of military personnel.
Objective: The study aimed to determine the magnitude of post-traumatic stress disorder and associated factors among military personnel admitted to the Eastern Command Referral Hospital in Eastern Ethiopia from May 1 to 30, 2023.
Methods and materials: A cross-sectional study was carried out at an institution. Face-to-face interviews were conducted to collect data using the post-traumatic stress disorder military version checklist for the Diagnostic and Statistical Manual, Fifth Edition. Data were entered and analyzed using EpiData version 3.1 and STATA version 14. Descriptive statistics were employed to summarize the information. To investigate factors linked with outcome variables, bivariate and multivariate logistic regression analyses were conducted. The results were presented using odds ratios with 95% confidence intervals, with statistical significance given at a p-value of 0.05.
Results: This study found that approximately 23.6% (95% CI = 19.9–27.8) of admitted military members fulfilled the diagnostic criteria for PTSD. Participants’ history of mental illness [adjusted odds ratio (AOR) = 5.73, 95% CI = 2.66–12.31], family history of mental illness (AOR = 10.38, 95% CI = 5.36–20.10), current chewing of khat (AOR = 2.21, 95% CI = 1.13–4.32), physical trauma (AOR = 2.03, 95% CI = 1.00–4.13), moderate social support (AOR = 0.27, 95% CI = 0.1–4.53), strong social support (AOR = 0.09, 95% CI = 0.02–0.35), and severe depression (AOR = 2.06, 95% CI = 1.74–5.71) were factors significantly associated with post-traumatic stress disorder.
Conclusions: The magnitude of post-traumatic stress disorder is high among military personnel. Factors such as participants’ history of mental illness, family history of mental illness, depression, lack of social support, current use of khat, and physical trauma are significantly associated with PTSD. It is crucial to identify and intervene early in individuals with these risk factors to address PTSD effectively.
Post-traumatic stress disorder (PTSD) is a common mental health problem for military members (1). This illness can have a substantial influence on all parts of life and is frequently chronic. Public safety workers, such as firefighters and military personnel, are constantly subjected to stressful situations because of the nature of their work (2). They may risk their lives to preserve others or property, resulting in potentially painful events (3). Military personnel deployed in conflict zones endure extra stressors, such as exposure to explosives, which can contribute to the development of PTSD (4). PTSD can develop from experiencing or witnessing life-threatening situations, manifesting as symptoms like flashbacks, nightmares, hyperarousal, avoidance behaviors, and mood changes (5). PTSD frequently coexists with other mental health problems, such as anxiety and depression, among military members (4). The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) describes a traumatic event as having encountered a major injury, approaching death, or sexual violence (6).
PTSD is an extensively researched mental health disorder, especially after traumatic events and disasters (7). The likelihood of experiencing PTSD can vary based on factors such as occupation, level of exposure to trauma, and other variables (8). Workers, especially those in the military, are at a high risk for developing PTSD (2). Untreated PTSD can lead to long-term health problems, reduced daily functioning, and an overall decline in productivity, health, and social interactions, placing a burden on society (9–11). A significant portion of disability cases in both developed and developing countries are linked to PTSD (12). While preventing PTSD is difficult, secondary preventative strategies are successful. Treatment can also be helpful for certain individuals, especially veterans (13).
The World Health Organization (WHO) suggests that the magnitude of mental disorders is higher in war settings. PTSD is one of the most commonly reported mental health concerns among veterans and service personnel, accounting for 22.1% of all cases (14). There are 316 million adult war survivors worldwide suffering from PTSD and/or depression, mostly in low- and middle-income countries, with a combined burden of 3 million disability-adjusted life years due to PTSD (15). The occurrence of PTSD, affecting 5% to 20% of the 2.7 million Americans deployed to Iraq and Afghanistan since 2001, is influenced by the degree of battle exposure (16, 17). A study of 613 US soldiers hospitalized after combat injury found that 4.2% had probable PTSD at 1 month, increasing to 12.2% at 4 months and remaining at 12.0% at 7 months (18). Another study of 1,777 US military personnel post-deployment health assessment showed that approximately 25.15% had PTSD (19).
According to Virgil Hawkins’s stealth conflict map, the African continent accounts for approximately 88% of global morbidity and mortality related to conflicts (20). More than 75% of African countries have been engaged in wars in the last three decades, with more than 70% of victims being fighters (21). This has led to significant human losses, infrastructure destruction, and immense suffering for millions of Africans (15, 22). Studies on the magnitude of PTSD in Sub-Saharan Africa have shown estimates ranging from 0% to 74% at national and regional levels, with a combined magnitude of 30% in war-affected areas (23). In Nigeria, recent research indicates that three out of 10 military combatants are at risk of developing PTSD (24).
PTSD is not well understood, especially in relation to military personnel. Studies have shown that individuals can develop PTSD after experiencing traumatic events like landslides and traffic accidents (25). This study intends to fill this gap by assessing the post-traumatic disorder and associated factors among military personnel at the Eastern Command Referral Hospital in Dire Dawa Administration, Eastern Ethiopia, from May 1 to 30, 2023. This study is critical for better understanding and meeting the mental health requirements of military personnel in this region.
A cross-sectional study was conducted at Eastern Command Referral Hospital in Dire Dawa Administration from May 1 to 30, 2023. Dire Dawa Administration is located 515 km from Addis Ababa in the eastern part of Ethiopia. The hospital serves as the base hospital for casualties and provides family planning, psychiatric, medical, and surgical services for inpatients and medical and surgical services for outpatients. It also offers services to military personnel requiring inpatient or mental care. The hospital has a total of 1,200 beds and a staff that includes 10 medical doctors, 8 emerging surgeons, 12 midwives, 50 clinical nurses, 33 health officers, 9 laboratory technicians, 8 pharmacists, 6 psychiatrists, 1 psychologist, and 25 health extensions (Eastern Command Referral Hospital Report, 2023).
The source population for this study included all members of the armed forces who visited the inpatient department of the Eastern Command Referral Hospital in the Dire Dawa Administration. The study population consisted of military personnel who had been exposed to battlefields or sustained injuries on the battlefield and sought treatment at the hospital during the study period. The study included military members who were admitted to the inpatient department and were able to participate in the questionnaire. Individuals who were unable to communicate or were critically ill were excluded from the study.
This study has two separate objectives: the first is to assess post-traumatic stress disorder, and the second is to identify factors associated with post-traumatic stress disorder. The sample size for the first objective was determined using a single population proportion formula by taking the magnitude of PTSD to be 22% from a study conducted in Northwest Ethiopia, Bahir Dar (26). With a 4% margin of error, the 95% confidence interval was calculated as n = Z2p (l − p)/d2, where d is the margin of error, Z is the confidence level (95%) = 1.96, and p is the population proportion = 0.22.
Accounting for a 10% non-response rate, the final sample size was adjusted to 453. For specific objective 2 focusing on the factors associated with PTSD, the sample size was determined using EPI-Info version 3.1 software. The calculations were based on assumptions of 80% power, 95% confidence interval, and a 1:1 ratio of cases to controls sourced from a previous study (26). The sample size for the first objective was larger than that of the second, resulting in a final sample size of 453.
Participants in the study were chosen using a simple random sampling technique. A sampling frame was created by naming all military personnel from each ward and assigning bed numbers. Four data collectors designated the bed numbers 2 days prior to data collection. Then, study participants were selected using a computer-generated random number.
Data were collected by three BSc nurses and one BSc psychiatry professional using a structured questionnaire derived from previous studies (27–31). The questionnaire was initially prepared in English, translated into Amharic, and then back-translated to English to ensure clarity. It included sociodemographic, psycho-social, and clinical factors. Face-to-face interviews were conducted with participants at a convenient time in the hospital, with on-site supervision by the principal investigator. Any doubts or errors in the collected data were resolved immediately. The completeness of the data was also checked.
Prior to the actual data collection study, a pretest was conducted outside the study area with 5% of the calculated sample size. Data collectors underwent a 2-day training session. Strict supervision and cross-checking of data were implemented for quality control. The supervisor and principal investigator conducted daily inspections to ensure completeness and quality of data collection, providing detailed feedback to data collectors. Feedback from data collectors was used to enhance the questionnaire. The principal investigator reviewed all questionnaires collected each day, addressing any unclear, missing, or confusing information with the respective data collector for correction.
The dependent variable was measured using 17 items from the PCL-M for DSM-5. This self-report rating scale assesses PTSD symptoms based on the DSM-5 criteria. Participants rate each item on a 5-point Likert scale (0 = not at all, 1 = a little bit, 2 = moderately, 3 = quite a bit, and 4 = extremely). The total score was calculated by summing the ratings of the 17 items, resulting in scores ranging from 0 to 85. A cutoff point of ≥50 was used to indicate the presence of PTSD symptoms (32).
The level of social support was assessed using the Oslo-3 social support scale, which assigns scores ranging from 3 to 14. Poor social support was indicated by scores of 3 to 8, moderate social support by scores of 9 to 11, and strong social support by scores of 12 to 14 (31).
The participants were assessed using the Patient Health Questionnaire-9 (PHQ-9) questionnaire, which consists of nine items. Scores were categorized as follows: minimal (1–4), mild (5–9), moderate (10–14), severe (15–19), and very severe depression (20–27) (33).
Anxiety levels were assessed using the Generalized Anxiety Disorder 7-item (GAD-7) scale. The cutoff points of 5, 10, and 15 were used to classify anxiety levels as none/normal (0–4), mild (5–9), moderate (10–14), and severe (15–21). Participants scoring<10 on the GAD-7 scale were considered to have anxiety, while those scoring 8 or higher were deemed to have significant anxiety symptoms (34).
To assess family history of mental illness, respondents were asked if they had any family members who had been clinically diagnosed with a mental illness (34).
The data collected were coded, entered, and cleaned using EpiData Software version 3.1. Subsequently, the data were exported and analyzed using STATA version 14. Descriptive statistics such as means, frequencies, percentages, and standard deviations were computed with STATA version 14 and presented in the form of numbers, texts, and tables. Initially, each variable underwent bivariate logistic regression analysis to identify associations with the dependent variable. Variables with a p-value of<0.25 were then included in multivariate logistic regression for further analysis. Variables with a p-value<0.05 in the multivariate models were considered significantly associated with the dependent variable and determined using adjusted odds ratios with 95% confidence intervals. The model’s goodness of fit was assessed using the Hosmer–Lemeshow test.
A total of 445 military personnel were included in the study out of the 453 sampled participants, resulting in a response rate of 98.2%. The average age of the participants was 24.8 years with a standard deviation of 6.31. The majority of the respondents (87.4%) were male, and most of them (76.4%) were single. More than half (55.5%) identified as orthodox, and the majority (69.2%) had a secondary educational status. A significant portion (61.1%) held a soldier/army military rank, and the majority (89.7%) belonged to the branch of the military force of the earth mechanized (Table 1).
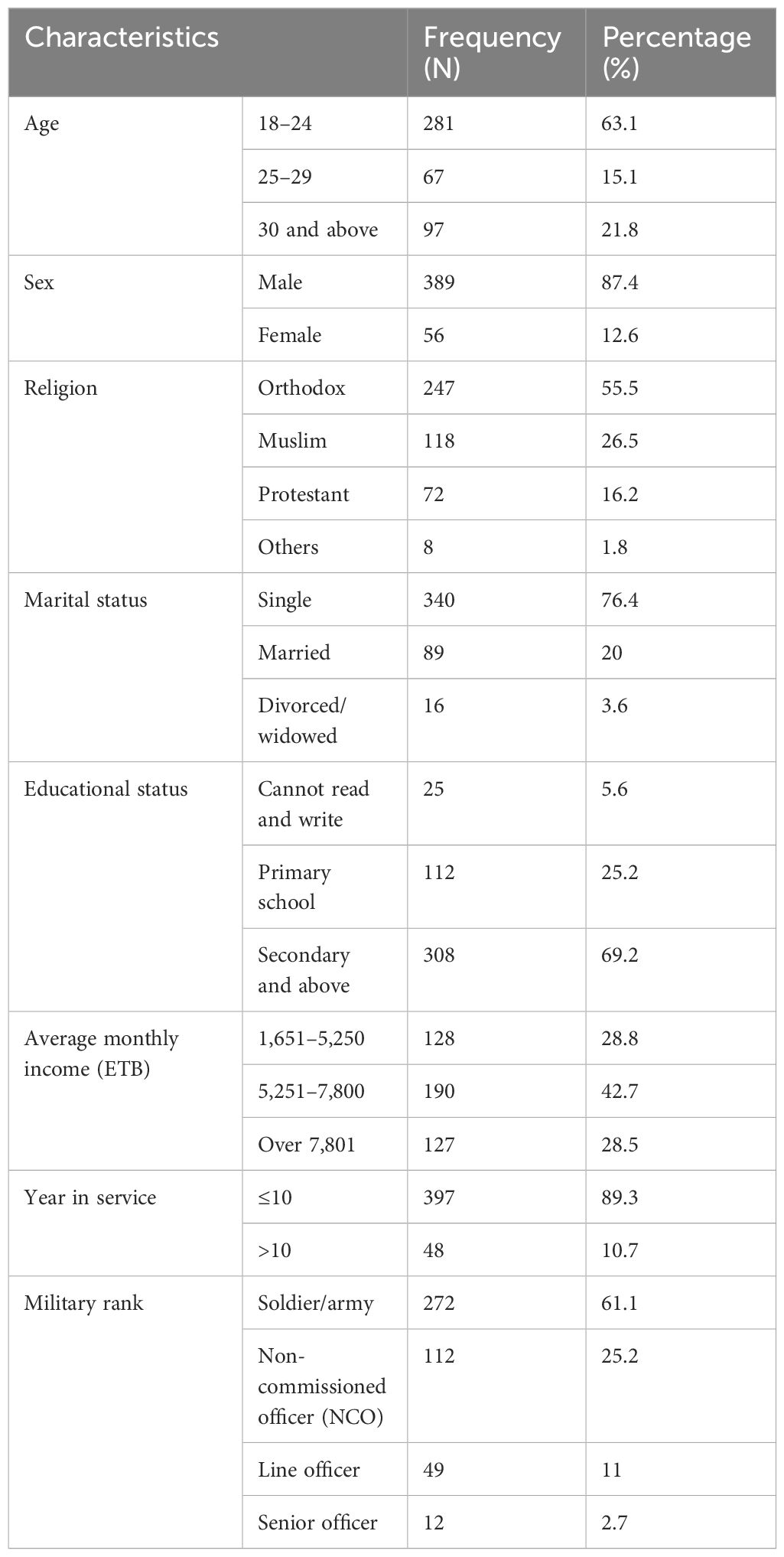
Table 1 Sociodemographic and military characteristics among military members at Eastern Command Referral Hospital, Eastern Ethiopia, 2023 (n = 445).
Approximately two-fifths (44.3%) of the participants had ever used alcohol, and approximately one-third (29.7%) had ever used khat. Also, 26.3% of participants had a family history of mental illness, while 59.8% had a history of chronic medical illness. Among those with a chronic medical condition, 30.1% had a history of mental illness. Additionally, 61.4% of participants screened positive for depression. Moreover, approximately 14.6% of the participants reported having strong social support, while approximately 41.4% of the respondents indicated that they have three to five close individuals who they can rely on for help (Table 2).
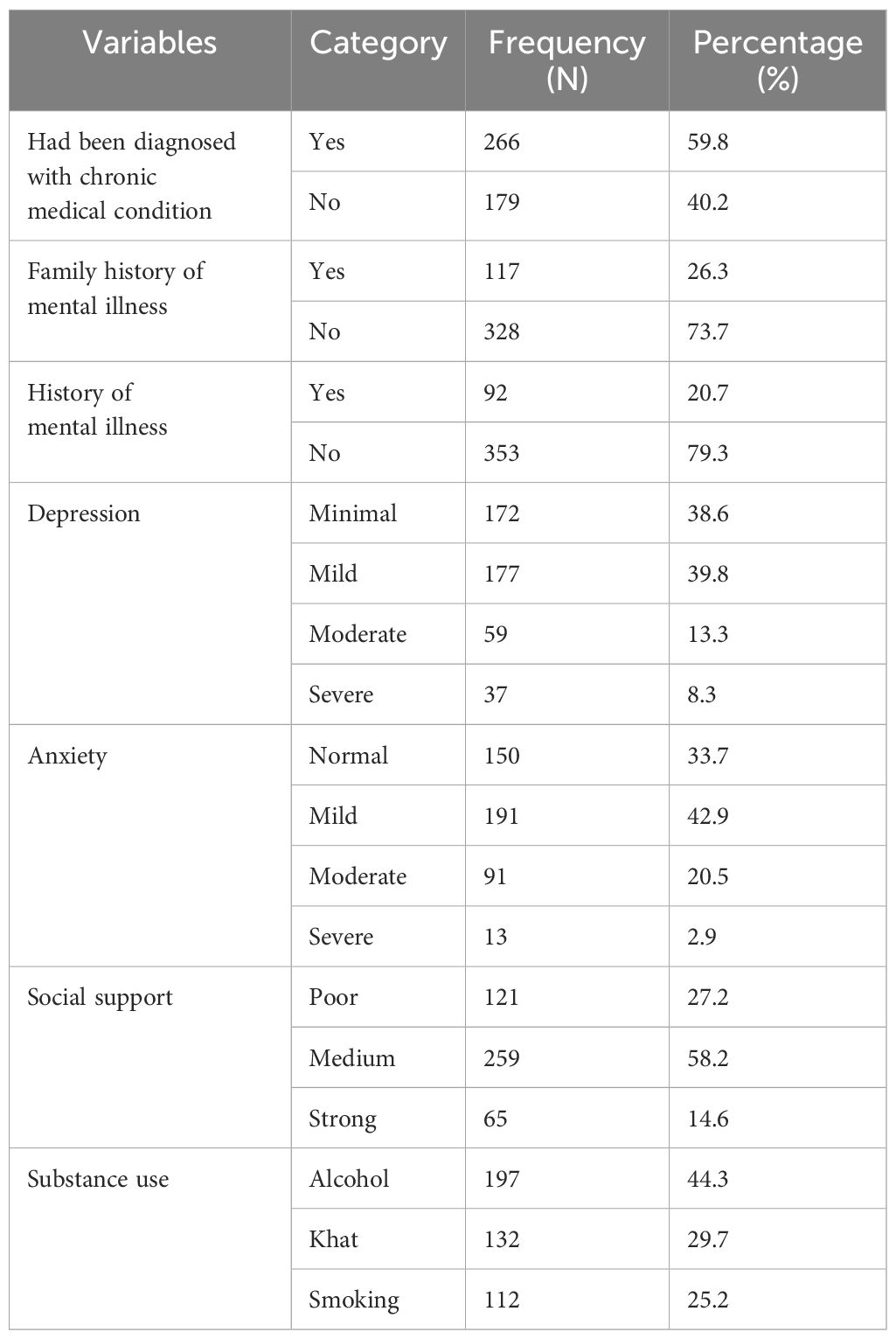
Table 2 Clinical, substance use, and psycho-social factors of the military members at Eastern Command Referral Hospital, Eastern Ethiopia, 2023 (n = 445).
The majority of respondents (96.4%) stated that they were without food or drink, and almost 94.4% claimed to have witnessed a friend or family member being killed. Approximately 67.9% of the respondents had physical trauma or serious injury, and approximately 61.4% experienced destruction of personal property (Table 3). Approximately one-quarter of the participants, 23.6% (95% CI = 19.9–27.8), had PTSD (Figure 1).

Table 3 Exposure to traumatic event factors of the military personnel, Eastern Command Referral Hospital, Ethiopia, 2023 (n = 445).
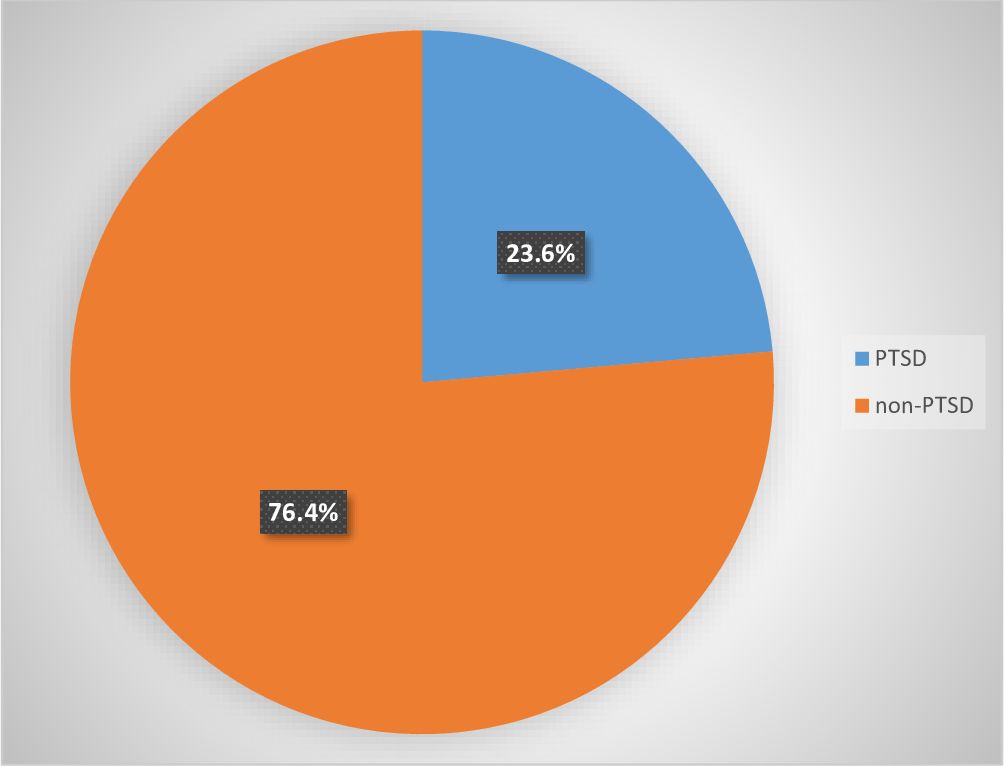
Figure 1 Magnitude of PTSD among military members at Eastern Command Referral Hospital, Eastern Ethiopia, 2023 (n = 445). PTSD, post-traumatic stress disorder.
Among respondents, patients with known chronic medical illnesses, compared to those without, have a higher proportion of PTSD (67.6% vs. 42.6%, respectively). Respondents who have been exposed to heavy noise of weapons, compared to those who have not been exposed, have a higher proportion of PTSD (32% vs. 21.9%, respectively). Also, respondents who have a history of chewing khat, compared to those without, have a higher proportion of PTSD (29.3% vs. 21.4%, respectively; Table 4).
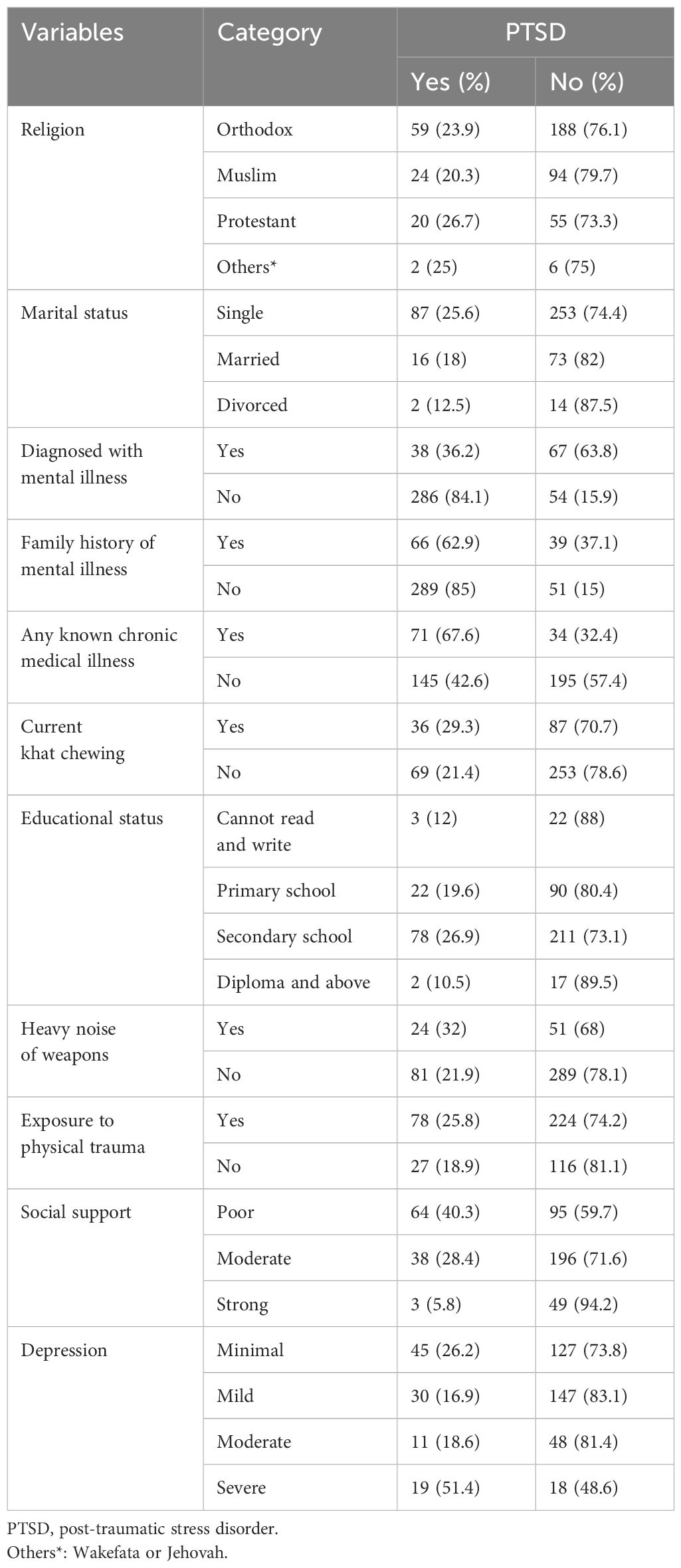
Table 4 Post-traumatic stress disorder by clinical, substance use, and psycho-social factors among the military personnel, Eastern Command Referral Hospital, Ethiopia, 2023 (n = 445).
In bivariate regression, various factors such as sex, age, military rank, service years, marital status, education level, branch of military, salary, medical and mental health history, social support, substance use, traumatic experiences, and exposure to violence were examined for their relationship with PTSD. In multivariate binary logistic regression, after adjusting for other variables, a history of mental illness, family history of mental illness, current use of khat, physical trauma, social support, and depression were found to be significant predictors of PTSD (Table 5).
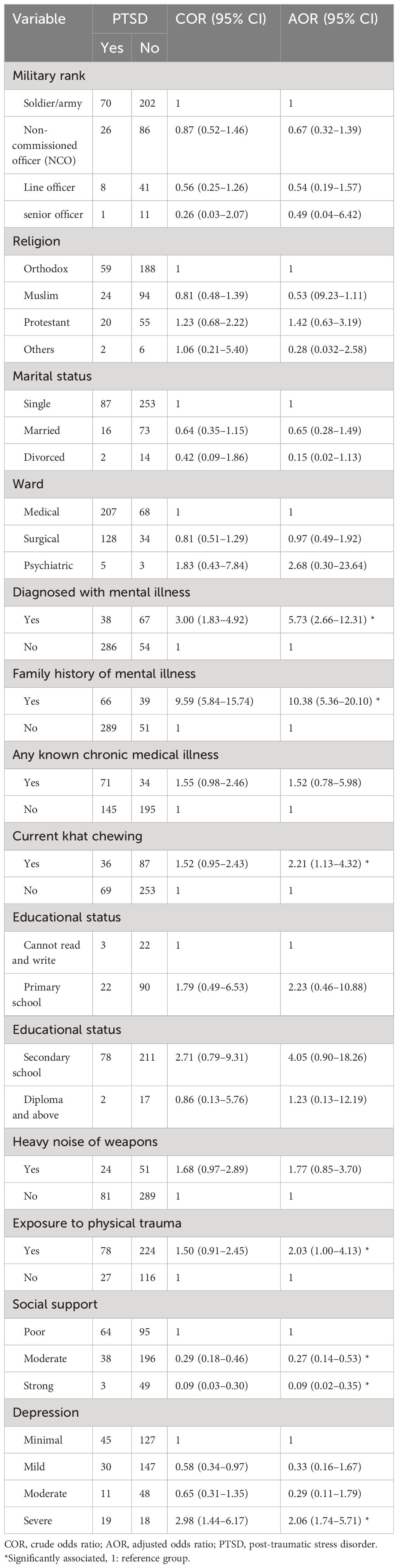
Table 5 Bivariate and multivariate analyses of factors associated with PTSD among military personnel in Eastern Command Referral Hospital, Ethiopia, 2023 (n = 445).
The likelihood of developing PTSD was significantly higher among respondents who had a previous diagnosis of mental illness [adjusted odds ratio (AOR) = 5.73, 95% CI = 2.66–12.31]. Similarly, individuals with a family history of mental illness had significantly higher odds of developing PTSD (AOR = 10.38, 95% CI = 5.36–20.10). Current khat users were also more likely to develop PTSD (AOR = 2.21, 95% CI = 1.13–4.32) compared to non-users. Additionally, individuals who had experienced physical trauma or serious injuries had higher odds of PTSD (AOR = 2.03, 95% CI = 1.00–4.13) compared to those who had not been exposed. Participants with strong social support had 91% lower odds of developing PTSD compared to those with poor social support (AOR = 0.09, 95% CI = 0.02–0.35). Similarly, participants with moderate social support had 73% lower odds of developing PTSD (AOR = 0.27, 95% CI = 0.14–0.53) compared to those with poor social support. Additionally, respondents with severe depression had 2.06 times higher odds of developing PTSD compared to those without depression (AOR = 2.06, 95% CI = 1.74–5.71) (Table 5).
The study aimed to assess the magnitude of PTSD and its related factors among military personnel hospitalized at the Eastern Command Referral Hospital in Dire Dawa Administration. The research identified several key risk factors for PTSD, including a personal or family history of mental illness, current khat use, physical trauma, level of social support, and depression.
This study found that the magnitude of PTSD among military personnel hospitalized after significant combat injury with complex polytrauma was 23.6% (95% CI = 19.9–27.8). This rate is similar to studies conducted in Nepal (21.9%) (35), Nigeria (25.1%) (36), and the USA (22%) (37). However, it is lower than the rates reported in earlier research on military veterans in South Africa (33%) (38), Uyghur and Han military veterans in China’s Xinjiang region (29%) (39), soldiers with amputation of a limb or spinal injury in Sri Lanka 41.7% (40), New Zealand military personnel (30%) (41), US military service members (47%) (42), and US War Veterans receiving post-deployment VA Health Care (37.8%) (43). Possible reasons for the high magnitude in the study conducted in Sri Lanka, Western countries, the USA (42, 43), and New Zealand personnel (41) may be military personnel who were amputated, have spinal injuries, and have higher rates of anxiety and depression (44), which was associated with PTSD. The possible reason for the lower magnitude of PTSD in the study area compared to previous studies may be that traditional societies, such as Ethiopia, have more frequent intimate family structures and a stronger extended family system than societies in Western countries. According to the study, people who have strong support networks (family and community) are more resilient, are able to cope, and can also minimize some of the psychological impacts of serious battlefield injury events, including PTSD (45, 46).
In this study, individuals with a history of mental illness were found to have 5.73 times higher odds of experiencing PTSD compared to those without a previous diagnosis (AOR = 5.73, 95% CI = 2.66–12.31). This finding aligns with previous research (47) and suggests that pre-existing mental health conditions may exacerbate the development of PTSD. Additionally, the study indicated that individuals with a family history of mental illness had 10.38 times higher odds of developing PTSD compared to those without such a history, consistent with earlier studies (27, 48). This association may be attributed to the increased vulnerability to mental health issues in individuals with a familial predisposition, potentially leading to the onset of PTSD (49).
The study found that individuals who currently chewed khat were 2.21 times more likely to develop PTSD compared to those who did not use khat. This finding is consistent with previous studies conducted in Southwestern Uganda (50), Ethiopia (51), China (52), and Somalia (53). Substance abuse, like khat use, can hinder the body’s natural ability to cope with trauma, increase physiological arousal, and worsen PTSD symptoms (54). Additionally, khat is a stimulant that can heighten anxiety levels, potentially exacerbating PTSD symptoms or increasing susceptibility to the disorder (55).
The study revealed that individuals who had experienced physical trauma or serious injuries were 2.03 times more likely to develop PTSD compared to those who had not been exposed. This finding is consistent with previous research that showed higher rates of PTSD among injured soldiers compared to uninjured soldiers (56). Additionally, individuals hospitalized after physical trauma were found to have elevated rates of both PTSD and major depression (57). Moreover, individuals with a history of prior traumatic events and PTSD were at a higher risk of developing PTSD after subsequent trauma (58). This association may be attributed to the strong connection between peritraumatic dissociation during an injury event and the development of PTSD (59). Furthermore, individuals with coexisting depression are more likely to encounter traumatic situations and are at an increased risk of developing PTSD (60).
The study found that individuals with strong social support had a 91% lower chance of developing PTSD compared to those with poor social support. Similarly, participants with moderate social support had a 73% lower risk of PTSD. These results are consistent with previous research (61–64), suggesting that social support plays a crucial role in mitigating the impact of trauma. Individuals with strong social networks are better equipped to cope with emergencies, while those lacking support may struggle to recover, increasing their vulnerability to PTSD (65). The study found that individuals with severe depression were 2.06 times more likely to have PTSD compared to those without depression. This result is consistent with previous research (42, 66) and may be attributed to the shared symptoms and heightened emotional distress experienced in both conditions (67).
The study’s cross-sectional design may not establish temporal relationships between PTSD and its predictors. The tool was not validated in the local language due to budget constraints. However, steps were taken to ensure data validity, including translating the questionnaire, pretesting it, and training the supervisor and data collector.
The magnitude of post-traumatic stress disorder is high among military personnel. Factors such as a history of mental illness, family history of mental illness, depression, lack of social support, current use of khat, and physical trauma are significantly associated with PTSD. It is crucial to identify and intervene early in individuals with these risk factors to address PTSD effectively.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethical clearance was obtained from the Institutional Health Research Review Committee (IHRERC) of Haramaya University. Formal letters of permission were obtained from the School of Public Health and submitted to the hospital’s responsible authorities. Voluntary, informed, written, and signed consent was obtained from the hospital head. The objectives, significance, benefits, and risks of the study and the procedural details of the study were explained to the study participants. Voluntary, informed, written, and signed consent was obtained from each study participant before conducting the interview. Participants were informed of the purpose of the study, and no identification or names were recorded to maintain confidentiality. Study participants were informed of their right to refuse or stop participating at the time during the interview.
DF: Conceptualization, Formal Analysis, Investigation, Methodology, Software, Supervision, Writing – original draft, Writing – review & editing. DA: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. TY: Supervision, Writing – original draft, Writing – review & editing. JD: Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. SD: Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. OK: Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. MK: Formal Analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. AG: Supervision, Writing – original draft, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Haramaya University.
The authors thank Haramaya University College of Health and Medical Sciences, School of Public Health, for the opportunities and support while this research was conducted.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AEA, Assignment Eligibility and Availability; APA, American Psychological Association; APD, Admitted Patient Department; CIDI, Composite International Diagnostic Interview; DMS, Diagnostic and Statistical Manual; ENDF, Ethiopian National Defense Force; GAD, General Anxiety Questionnaire; HTQ, Harvard Trauma Questionnaire; NACM, negative alteration in cognition and mood; OEF, Operation Enduring Freedom; OIF, Operation Iraqi Freedom; OSSS, Oslo Social Support Scale; PCL-M, Post-Traumatic Stress Disorder, military version; PC-PTSD, Primary Care Post Traumatic Stress Disorder; QASS, Questionnaire Assessing Social Support; SADF, South African Defence Force; STATA, Statistic Data Analysis; TE, traumatic event; UN, United Nations; WHO, World Health Organization.
1. Smith SM, Goldstein RB, Grant BF. The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: Data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). J Psychiatr Res. (2016) 82:16–22. doi: 10.1016/j.jpsychires.2016.06.022
2. Wilson S, Guliani H, Boichev G. On the economics of post-traumatic stress disorder among first responders in Canada. BMJ Global Health. (2016) 1:26–31. doi: 10.35502/jcswb.6
3. Benedek DM, Fullerton C, Ursano RJ. First responders: mental health consequences of natural and human-made disasters for public health and public safety workers. Annu Rev Public Health. (2007) 28:55–68. doi: 10.1146/annurev.publhealth.28.021406.144037
4. Marmar CR, Schlenger W, Henn-Haase C, Qian M, Purchia E, Li M, et al. Course of posttraumatic stress disorder 40 years after the Vietnam War: Findings from the National Vietnam Veterans Longitudinal Study. JAMA Psychiatry. (2015) 72(9):875–81. doi: 10.1001/jamapsychiatry.2015.0803
5. Bandelow B, Koch M, Zimmermann P, Biesold K-H, Wedekind D, Falkai P, et al. Posttraumatic stress disorder (PTSD) in the German Armed Forces: a retrospective study in inpatients of a German army hospital. Eur Arch Psychiatry Clin Neurosci. (2012) 262:459–67. doi: 10.1007/s00406-012-0289-8
6. American Psychiatric Association D, Association AP. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American psychiatric association (2013). doi: 10.1176/appi.books.9780890425596
7. Wilson JP, Smith W, Johnson SK. A Comparative analysis of PTSD among various. Trauma And Its Wake (2013) 1:142.
8. Berger W, Coutinho ESF, Figueira I, Marques-Portella C, Luz MP, Neylan TC, et al. Rescuers at risk: a systematic review and meta-regression analysis of the worldwide current magnitude and correlates of PTSD in rescue workers. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:1001–11. doi: 10.1007/s00127-011-0408-2
9. Association AP. Diagnostic and statistical manual of mental disorders. Arlington, VA, US: American Psychiatric Publishing, Inc (1995).
10. Atwoli L, Stein DJ, Williams DR, Mclaughlin KA, Petukhova M, Kessler RC, et al. Trauma and posttraumatic stress disorder in South Africa: analysis from the South African Stress and Health Study. BMC Psychiatry. (2013) 13:1–12. doi: 10.1186/1471-244X-13-182
11. Miller MW, Sadeh N. Traumatic stress, oxidative stress and post-traumatic stress disorder: neurodegeneration and the accelerated-aging hypothesis. Mol Psychiatry. (2014) 19(11):1156–62. doi: 10.1038/mp.2014.111
12. Jackson J, Pandharipande P, Girard T, Brummel N, Thompson J, Hughes C, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. (2014) 2(5):369–79. doi: 10.1016/S2213-2600(14)70051-7
13. Richards A, Kanady JC, Neylan TC. Sleep disturbance in PTSD and other anxiety-related disorders: an updated review of clinical features, physiological characteristics, and psychological and neurobiological mechanisms. Neuropsychopharmacology. (2020) 45(1):55–73. doi: 10.1038/s41386-019-0486-5
14. Inoue C, Shawler E, Jordan CH, Jackson CA. Veteran and military mental health issues. Europe PubMed Central (Europe PMC). (2021).
15. Hoppen TH, Priebe S, Vetter I, Morina N. Global burden of post-traumatic stress disorder and major depression in countries affected by war between 1989 and 2019: a systematic review and meta-analysis. BMJ Global Health. (2021) 6:e:006303. doi: 10.1136/bmjgh-2021-006303
16. Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. (2004) 351(1):13–22. doi: 10.1056/NEJMoa040603
17. Kok BC, Herrell RK, Thomas JL, Hoge CW. Posttraumatic stress disorder associated with combat service in Iraq or Afghanistan: reconciling magnitude differences between studies. J Nerv Ment Dis. (2012) 200(5):444–50. doi: 10.1097/NMD.0b013e3182532312
18. Grieger TA, Cozza SJ, Ursano RJ, Hoge C, Martinez PE, Engel CC. Posttraumatic stress disorder and depression in battle-injured soldiers. Am J Psychiatry. (2006) 163(10):1777–83. doi: 10.1176/ajp.2006.163.10.1777
19. MacGregor AJ, Dougherty AL, Tang JJ, Galarneau MR. Postconcussive symptom reporting among US combat veterans with mild traumatic brain injury from Operation Iraqi Freedom. J Head Trauma Rehabil. (2013) 28(1):59–67. doi: 10.1097/HTR.0b013e3182596382
20. Matheson D. The ethics of war reporting. Routledge Companion to News Journalism: Routledge. (2022), 267–75.
21. Morina N, Stam K, Pollet TV, Priebe S. Magnitude of depression and posttraumatic stress disorder in adult civilian survivors of war who stay in war-afflicted regions. A systematic review and meta-analysis of epidemiological studies. J Affect Disord. (2018) 239:328–38. doi: 10.1016/j.jad.2018.07.027
22. Kassaye A, Demilew D, Fanta B, Mulat H, Ali D, Seid J, et al. Magnitude of post-traumatic stress disorder and its associated factors among war-affected residents in woldia town, north east Ethiopia. Community Based Cross-sectional Study. (2022) 2022. doi: 10.21203/rs.3.rs-2319793/v1
23. Ng LC, Stevenson A, Kalapurakkel SS, Hanlon C, Seedat S, Harerimana B, et al. National and regional magnitude of posttraumatic stress disorder in sub-Saharan Africa: a systematic review and meta-analysis. Plos Med. (2020) 17(5):. doi: 10.1371/journal.pmed.1003090
24. Abel J, Anongo F, Dami B, Ogbole A, Abel A, Dagona Z, et al. Combat exposure and peritraumatic factors predicting PTSD among military personnel fighting insurgency in Nigeria. J Anxiety & Depression. (2018) 1:108. doi: 10.46527/2582-3264.108
25. Ali D, Azale T, Wondie M, Tadesse J. About six in ten survivors of the november 2020 Maikadra massacre suffer from posttraumatic stress disorder, northwest Ethiopia. Psychol Res Behav Manag. (2022) 15:251. doi: 10.2147/PRBM.S338823
26. Tedla A, Tareke M, Beka M. Magnitude of Post-Traumatic Stress Disorder and its Associated Factors Among Military Personnel who Were Admitted at North West Command Level Three Military Hospital, Bahir Dar, Northwest, Ethiopia. (2022). unpublished.
27. Asnakew S, Shumet S, Ginbare W, Legas G, Haile K. Magnitude of post-traumatic stress disorder and associated factors among Koshe landslide survivors, Addis Ababa, Ethiopia: a community-based, cross-sectional study. BMJ open (2019) 9(6):. doi: 10.1136/bmjopen-2018-028550
28. PTSD NCf. PTSD checklist for DSM-5 (PCL-5) (2013). Available online at: https://www.ptsd.va.gov/professional/assessment/adult-sr/ptsd-checklist.asp.
29. Verhey R, Gibson L, Brakarsh J, Chibanda D, Seedat S. Magnitude and correlates of probable post-traumatic stress disorder and common mental disorders in a population with a high magnitude of HIV in Zimbabwe. Eur J Psychotraumatol. (2018) 9(1):1536286. doi: 10.1080/20008198.2018.1536286
30. Gelaye B, Williams MA, Lemma S, Deyessa N, Bahretibeb Y, Shibre T, et al. Validity of the patient health questionnaire-9 for depression screening and diagnosis in East Africa. Psychiatry Res. (2013) 210(2):653–61. doi: 10.1016/j.psychres.2013.07.015
31. Kocalevent R-D, Berg L, Beutel ME, Hinz A, Zenger M, Härter M, et al. Social support in the general population: standardization of the Oslo social support scale (OSSS-3). BMC Psychol. (2018) 6:31. doi: 10.1186/s40359-018-0249-9
32. Association AP. Diagnostic and statistical manual of mental disorders fifth edition DSM-5, 2012-2013. Washington, DC: American Psychiatric Publishing (2013).
33. Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. (2012) 184(3):E191–E6. doi: 10.1503/cmaj.110829
34. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166(10):1092–7. doi: 10.1001/archinte.166.10.1092
35. Rawal N, Karki R, Shrestha D, Manandhar P, Pathak N. Factors associated with post traumatic stress disorder and depression among Nepalese combatants during armed insurgency. Journal of Psychiatrists' Association of Nepal. (2017) 6(1):24–8. doi: 10.3126/jpan.v6i1.21768
36. Okulate G, Jones O. Post-traumatic stress disorder, survivor guilt and substance use-a study of hospitalised Nigerian army veterans. S Afr Med J. (2006) 96(2):144–6.
37. MacGregor AJ, Tang JJ, Dougherty AL, Galarneau MR. Deployment-related injury and posttraumatic stress disorder in US military personnel. Injury. (2013) 44:1458–64. doi: 10.1016/j.injury.2012.10.009
38. Connell M, Omole O, Subramaney U, Olorunju S. Post traumatic stress disorder and resilience in veterans who served in the South African border war: original. Afr J Psychiatr. (2013) 16(6):430–6. doi: 10.4314/ajpsy.v16i6.55
39. Liu B, Li R, Lu D, Zhao J, Guan S, Tang J, et al. Risk factors associated with post-traumatic stress disorder among Uyghur and Han veterans in Xinjiang region of China. Int J Clin Exp Med. (2016) 9:22232–40.
40. Abeyasinghe NL, de Zoysa P, Bandara K, Bartholameuz N, Bandara J. The magnitude of symptoms of Post-Traumatic Stress Disorder among soldiers with amputation of a limb or spinal injury: A report from a rehabilitation centre in Sri Lanka. Psychol Health Med. (2012) 17(3):376–81. doi: 10.1080/13548506.2011.608805
41. Richardson A, Gurung G, Samaranayaka A, Gardner D, deGraaf B, Wyeth EH, et al. Risk and protective factors for post-traumatic stress among New Zealand military personnel: A cross sectional study. Plos One (2020) 15(4):. doi: 10.1371/journal.pone.0231460
42. Armenta RF, Rush T, LeardMann CA, Millegan J, Cooper A, Hoge CW. Factors associated with persistent posttraumatic stress disorder among US military service members and veterans. BMC Psychiatry. (2018) 18(1):1–11. doi: 10.1186/s12888-018-1590-5
43. Jakupcak M, Luterek J, Hunt S, Conybeare D, McFall M. Posttraumatic stress and its relationship to physical health functioning in a sample of Iraq and Afghanistan War veterans seeking postdeployment VA health care. J Nerv Ment Dis. (2008) 196(5):425–8. doi: 10.1097/NMD.0b013e31817108ed
44. Horgan O, MacLachlan M. Psychosocial adjustment to lower-limb amputation: a review. Disabil Rehabil. (2004) 26(14-15):837–50. doi: 10.1080/09638280410001708869
45. Thompson NJ, Fiorillo D, Rothbaum BO, Ressler KJ, Michopoulos V. Coping strategies as mediators in relation to resilience and posttraumatic stress disorder. J Affect Disord. (2018) 225:153–9. doi: 10.1016/j.jad.2017.08.049
46. Kopinak JK. Mental health in developing countries: challenges and opportunities in introducing western mental health system in Uganda. Int J MCH AIDS. (2015) 3(1):22. doi: 10.21106/IJMA
47. Ojeahere MI, Uwakwe R, Piwuna CG, Audu M, Goar SG, Armiyau A, et al. Assessment of full and subsyndromal PTSD and quality of life of internally displaced older adults in northern Nigeria. Aging Health Res. (2021) 1(4):100040. doi: 10.1016/j.ahr.2021.100040
48. Bezabh YH, Abebe SM, Fanta T, Tadese A, Tulu M. Magnitude and associated factors of post-traumatic stress disorder among emergency responders of Addis Ababa Fire and Emergency Control and Prevention Service Authority, Ethiopia: institution-based, cross-sectional study. BMJ Open. (2018) 8(7):. doi: 10.1136/bmjopen-2017-020705
49. Lemke S. [A historical medical study of post-traumatic stress disorders in World War I soldiers]. Der Nervenarzt. (2007) 78 1:92–9.
50. Bapolisi AM, Song SJ, Kesande C, Rukundo GZ, Ashaba S. Post-traumatic stress disorder, psychiatric comorbidities and associated factors among refugees in Nakivale camp in southwestern Uganda. BMC Psychiatry. (2020) 20(1):1–10. doi: 10.1186/s12888-020-2480-1
51. Wolde A, Dessalegn N. Posttraumatic stress disorder, suicidal behavior, substance use, and sexual victimization among adolescent girls aged 10-19 years living under ethnic-based civil war in Ethiopia. Neuropsychiatr Dis Treat. (2022) 18:2239–50. doi: 10.2147/NDT.S381461
52. Zhang S, Li P, Zhang Z, Wang W. Anterior capsulotomy improves persistent developmental stuttering with a psychiatric disorder: a case report and literature review. Neuropsychiatr Dis Treat. (2014) 10:553–8. doi: 10.2147/NDT
53. Odenwald M, Hinkel H, Schauer E, Schauer M, Elbert T, Neuner F, et al. Use of khat and posttraumatic stress disorder as risk factors for psychotic symptoms: a study of Somali combatants. Soc Sci Med (1982). (2009) 69:1040–8. doi: 10.1016/j.socscimed.2009.07.020
54. Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. Am J Psychiatry. (2001) 158(8):1184–90. doi: 10.1176/appi.ajp.158.8.1184
55. Lemieux A, Nakajima M, Saif-Ali R, Al-Habori M, Dokam A, al’Absi M. Anger, anxiety, and depressive affect as predictors of stress-induced cortisol production in khat and tobacco users. Addictive Behaviors. (2018) 82:195–201. doi: 10.1016/j.addbeh.2018.02.033
56. Koren D, Norman D, Cohen A, Berman JS, Klein EM. Increased PTSD risk with combat-related injury: a matched comparison study of injured and uninjured soldiers experiencing the same combat events. Am J Psychiatry. (2005) 162 2:276–82. doi: 10.1176/appi.ajp.162.2.276
57. Shih RA, Schell TL, Hambarsoomian K, Belzberg H, Marshall GN. Magnitude of posttraumatic stress disorder and major depression after trauma center hospitalization. J Trauma Acute Care Surg. (2010) 69 6:1560–6. doi: 10.1097/TA.0b013e3181e59c05
58. Breslau N, Peterson EL, Schultz LR. A second look at prior trauma and the posttraumatic stress disorder effects of subsequent trauma: a prospective epidemiological study. Arch Gen Psychiatry. (2008) 65 4:431–7. doi: 10.1001/archpsyc.65.4.431
59. Michaels AJ, Michaels CE, Moon CH, Smith JS, Zimmerman MA, Taheri PA, et al. Posttraumatic stress disorder after injury: impact on general health outcome and early risk assessment. J Trauma Acute Care Surg. (1999) 47(3):460–6; discussion 6-7. doi: 10.1097/00005373-199909000-00005
61. Amare TA, Mohamedhagos H, Awoke T. Magnitude and factors associated with post-traumatic stress disorder among military personnel admitted to Armed Forces Referral and Teaching Hospital, Addis Ababa, Ethiopia: Cross-sectional study. East African Journal of Health Sciences (2019) 1(2):116–27. Available at: https://journal.mu.edu.et/index.php/eajhs/article/view/318.
62. Xue C, Ge Y, Tang B, Liu Y, Kang P, Wang M, et al. A meta-analysis of risk factors for combat-related PTSD among military personnel and veterans. Plos One (2015) 10(3):e0120270. doi: 10.1371/journal.pone.0120270
63. Iversen AC, Fear NT, Ehlers A, Hughes JH, Hull L, Earnshaw M, et al. Risk factors for post-traumatic stress disorder among UK Armed Forces personnel. Psychol Med. (2008) 38(4):511–22. doi: 10.1017/S0033291708002778
64. Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, Southwick SM. Psychological resilience and postdeployment social support protect against traumatic stress and depressive symptoms in soldiers returning from Operations Enduring Freedom and Iraqi Freedom. Depress Anxiety. (2009) 26(8):745–51. doi: 10.1002/da.v26:8
65. Liu C, Zhang Y, Jiang H, Wu H. Association between social support and post-traumatic stress disorder symptoms among Chinese patients with ovarian cancer: A multiple mediation model. Plos One (2017) 12(5):. doi: 10.1371/journal.pone.0177055
66. Shahini M, Shala M. Post-traumatic stress disorder in Kosovo veterans. Sage Open (2016) 6(1):2158244016633737. doi: 10.1177/2158244016633737
Keywords: post-traumatic stress disorder, traumatic events, armed forces of military members, Dire Dawa, Ethiopia
Citation: Adugna D, Yadeta TA, Dereje J, Firdisa D, Demissie Darcho S, Kassa O, Kitessa M and Gemeda AT (2024) Post-traumatic stress disorder and associated factors among inpatients at Eastern Command Referral Hospital in Dire Dawa, Eastern Ethiopia. Front. Psychiatry 15:1373602. doi: 10.3389/fpsyt.2024.1373602
Received: 20 January 2024; Accepted: 21 May 2024;
Published: 11 June 2024.
Edited by:
Kaloyan Tanev, Massachusetts General Hospital and Harvard Medical School, United StatesReviewed by:
Yonas Geda, Barrow Neurological Institute (BNI), United StatesCopyright © 2024 Adugna, Yadeta, Dereje, Firdisa, Demissie Darcho, Kassa, Kitessa and Gemeda. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dawit Firdisa, ZmlyZGlzYWRhd2l0QGdtYWlsLmNvbQ==; Jerman Dereje, amVybWFuZGVyZWplODJAZ21haWwuY29t
†ORCID: Jerman Dereje, orcid.org/0000–0002-5845–8458
Dawit Firdisa, orcid.org/0009–0000-2258–0550
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.