- 1Department of Child Psychiatry, Chang Gung Memorial University Hospital at Linkou, Taoyuan, Taiwan
- 2School of Public Health, National Defense Medical Center, Taipei, Taiwan
- 3Department of Psychiatry, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan
- 4Department of Psychiatry, Tri-Service General Hospital, School of Medicine, National Defense Medical Center, Taipei, Taiwan
- 5Student Counseling Center, National Defense Medical Center, Taipei, Taiwan
Background: Disaster-related psychiatric disorders (DRPD) present a significant challenge to mental health professionals, yet there is a notable lack of emphasis on the preparedness of psychiatrists in managing these conditions within post-graduate medical education.
Methods: This study utilized a questionnaire to collect data from psychiatrists, focusing on their prior involvement in managing DRPD, perceived competence, medication preferences, and factors influencing their experiences in handling such disorders. Analysis included distribution and ranking of variables, alongside cross-analysis examining associations between demographic factors (age, gender, hospital levels, years of practice, board certification) and treatment experiences, as well as readiness for in-hospital or outside-hospital mobilization in DRPD management.
Results: One hundred and three Taiwanese psychiatrists participated in the study, with the majority reporting involvement in managing DRPD (71.8%), particularly in post-traumatic stress disorder (PTSD) and depression. Antidepressants, specifically serotonin selective reuptake inhibitors, were commonly preferred for DRPD treatment, including PTSD and depression. Psychiatrists aged over 40, with more than 10 years of practice, and hold the board-certified status, showed greater experiences for outside- or inside- the hospital mobilization in DRPD management.
Conclusion: Findings suggest that within post-graduate medical education, Taiwanese psychiatrists demonstrate significant experience, willingness, and capacity to effectively manage DRPD. However, there is a need to integrate comprehensive training on disaster psychiatry into post-graduate psychiatric education programs to further enhance preparedness and optimize outcomes in managing these challenging conditions.
Introduction
Disasters, characterized by their unpredictability and capacity for causing death, trauma, and property destruction (1), affect millions globally each year. The frequency and impact of these events are escalating due to climate change and population density growth (2), defining disasters by three key characteristics of large-scale traumatic events: significant harm or fatalities among a large group of people, societal disruption, and ensuing mental and physical health consequences (1, 3, 4).
The aftermath of disasters encompasses cognitive, emotional, and physiological responses, leading to predictable psychiatric morbidity (5, 6). Beyond post-traumatic stress disorder, common mental health effects include distress, grief, anxiety disorders, and depression (5–7), for examples, from the exposure to natural (8) or deliberately caused (9) disasters. Individuals often resort to self-medication, primarily with alcohol, risking harm and substance use disorders while delaying the recognition of mood and anxiety disorders (10).
The demands on psychiatrists differ significantly from routine clinical practice (10). Psychiatrists in hospitals must be informed about disaster plans and engage in planning processes, ensuring patients have crisis plans covering mental health management and accessing post-disaster treatment and medication (11, 12). Rapidly mobilized mental health teams, equipped with specialized disaster mental health skills, play a pivotal role in disaster intervention (13). Psychiatrists, as responders, can lead multidisciplinary teams to organize post-disaster psychiatric care, providing crucial assessments and interventions (14). Hence, acquiring fundamental competency in disaster psychiatry is vital for every psychiatrist.
Post-graduate medical education emphasizes clinical training for healthcare professionals, which focused on the standardized training and, under senior physicians’ guidance, develop independent healthcare skills for medical graduates (15, 16). In Taiwan, psychiatric training also following the principles of post-graduate medical education as aforementioned (17, 18), yet there’s a shortage of training competencies incorporating perspectives from both high- and low-income countries (19). In addition, the training for psychiatric trainee might also influence the psychiatrists’ preparedness (20).
Given the heightened risk for natural disasters in several Asian countries, notably by earthquakes, volcanic eruptions, typhoon, and cyclones (21), scant attention has been directed toward assessing psychiatrists’ readiness in managing disaster-related mental health crises (13). This study aims to examine the readiness of Taiwanese psychiatrists in responding to disaster-related mental health crises. We hypothesize discrepancies among psychiatrists based on training in the post-graduate medical education duration and prior clinical experiences.
Materials and methods
Study design and participants
This descriptive study employed an innovative questionnaire to assess Taiwanese psychiatrists’ readiness in managing disaster-related psychiatric disorders (DRPD). We distributed 103 questionnaires among Taiwanese psychiatrists in a cross-sectional approach. Inclusion criteria comprised psychiatrists practicing in Taiwan, completing the questionnaire autonomously, comprehending the study’s objectives, and consenting to their questionnaire’s use in the analysis by providing informed consent. The participants completed the self-administered paper-based the questionnaires.
All participants were exclusively Taiwanese, with no inclusion of a control group. Data pertaining to the general population were sourced from prior studies for subsequent discussions in both civilian (22, 23) and military populations (24–26). The questionnaire collected demographic data, including gender, years of clinical experience in psychiatry, and practice facility type. A 5-level rating scale assessed psychiatrists’ preparedness when encountering disasters, gauging familiarity from high to low across several facets: participation in DRPD management, familiarity with disaster-related psychotherapy, acquaintance with medications for DRPD (e.g., PTSD, depression, anxiety, and sleep disorders), and willingness to be mobilized for DRPD relief efforts.
Statistical analysis
This study employed SPSS statistical software for documentation and analysis. Continuous variables were described using mean and standard deviation. Categorical variables were presented as frequency and percentage. Subjective perceptions of psychiatric drugs and psychotherapy for DRPD. Psychiatrists’ emergency response to DRPD, long-term follow-up willingness, and mobilization readiness were documented using mean and standard deviation. Cross-analysis explored demographic associations with psychotropic medications or psychotherapy, long-term follow-up, and willingness to participate. T-tests, chi-square tests, variance analysis, correlation, regression, and other statistical methods were employed for verification and inference, with statistical significance set at p < 0.05. Multiple linear regression was also used in the assessment of the relationship between factors in unison psychiatrists’ preferences and experiences, with statistical significance set at p < 0.05.
Results
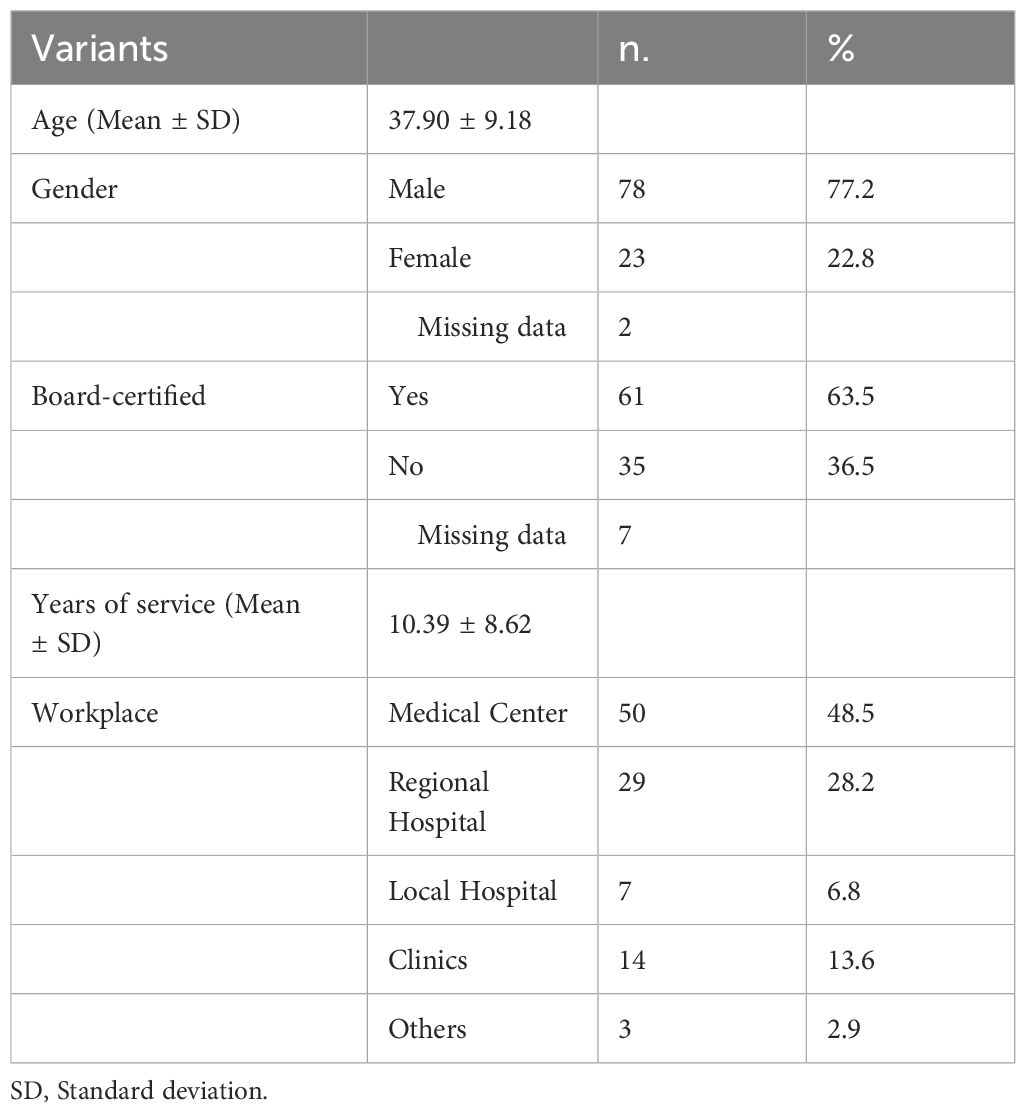
A total of 103 psychiatrists participated in this study, with male participants, board-certified professionals, and those working in regional hospitals or medical centers comprising the majority (Table 1). Notably, 82.5% of these psychiatrists expressed varying degrees of intent to treat, follow up, and even be deployed for the management of DRPD within the scope of this investigation.
Among these psychiatrists, a significant majority—ranging from 74% to 85%—reported previous experience in treating various forms of DRPD, including PTSD, depressive disorders, anxiety disorders, sleep disorders, and other conditions such as conversion disorders, dissociative disorders, and adjustment disorders. However, only 24% had prior experience in external deployment for DRPD management, while 40% had experience with internal hospital deployment (Table 2).
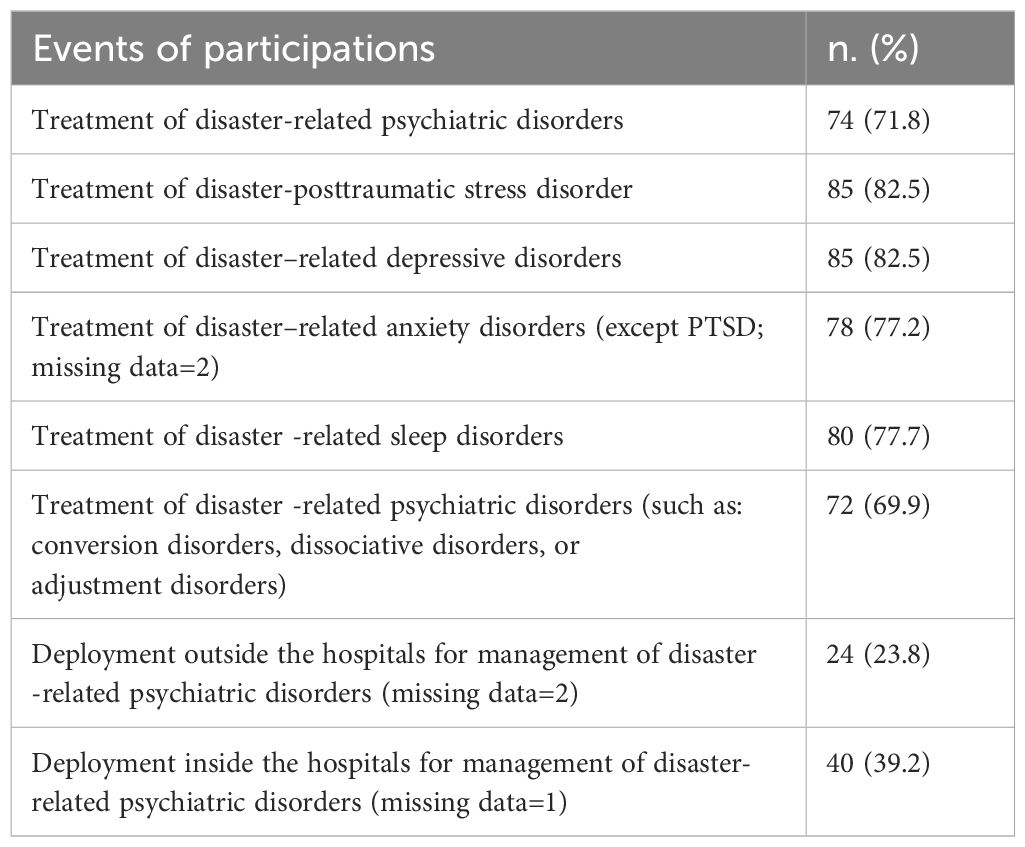
Table 2 Psychiatrists’ previous experiences in the participations in the relief of disaster-related psychiatric disorders (n=103).
Table 3 outlines the subjective confidence levels of psychiatrists regarding their competence in managing DRPD through psychotherapy. Across various conditions such as PTSD, depressive disorders, anxiety disorders, sleep disorders, and other related disorders, all participating psychiatrists involved conveyed a moderate level of confidence, in a 5-level rating scale, in their ability to conduct both individual and group therapies.

Table 3 Subjective feelings of competence in the management of disaster-related psychiatric disorders by psychotherapy (n=103).
Regarding the choice of psychotropic medications for DRPD treatment, the majority of psychiatrists in this study leaned toward Selective Serotonin Reuptake Inhibitors (SSRIs) and benzodiazepines (for anxiolysis or sleep) (Table 4). Specifically, when addressing disaster-related PTSD, most preferred sertraline, escitalopram, and fluoxetine as their antidepressant choices (Table 4).
Table 5 presents data indicating that SSRIs, Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), and Z-drugs/benzodiazepines were the most frequently selected psychotropic medications for addressing disaster-related depressive disorders, anxiety disorders, sleep disorders, and other associated conditions.
Table 6 illustrates that psychiatrists with longer years of service (10 years or more) and holding board-certified status are associated with greater experience in managing DRPD and demonstrate a preference for specific mobilization locations, whether out of hospital or within hospital settings, for interventions, by the multiple linear regression analysis. Psychiatrists aged 40 or older exhibit more experience in managing DRPD, with statistically significant associations found for DRPD in general, particularly anxiety disorders, and both out-of-hospital and in-hospital intervention mobilizations. There is no discernible association between gender and hospital levels with regard to experience in managing DRPD.
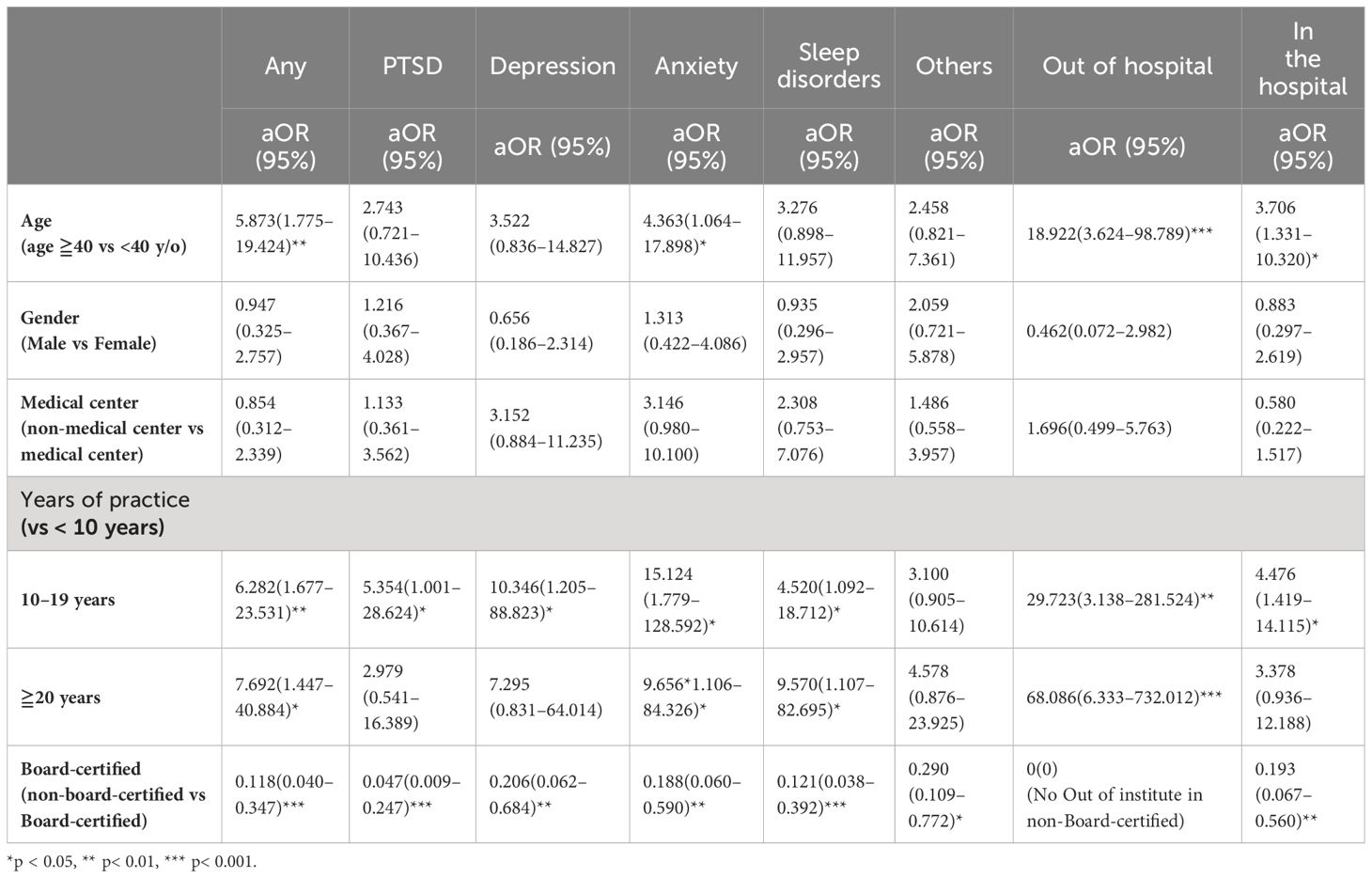
Table 6 Factors related to the experiences in dealing with disaster-related psychiatric disorders and the places of mobilization for interventions by multiple linear regression analysis (n=98).
Discussion
Disasters and public health crises pose multifaceted challenges, emphasizing the pivotal role psychiatrists play in addressing post-disaster psychiatric needs (11, 13, 27). This study represents the first exploration of disaster preparedness among Taiwanese psychiatrists and presents several notable findings. Primarily, a significant majority of these professionals exhibit substantial experience, willingness, and capability in managing DRPD. However, while many have treated DRPD, fewer have been involved in hospital deployments for DRPD management, signaling potential areas for improvement.
In Taiwan’s psychiatric resident training, the clinical training program must contain the Suicide Prevention and Disaster Psychiatry Program (17). However, in the results of this study, the average of the participants’ subjective feelings of competence in the 5-level rating scales are between 1.91–2.97 in the psychotherapeutic methods for DRPD. Among these psychotherapeutic techniques, the lowest feelings of competence are group and individual psychotherapies. In addition, the 3rd rank of medications chosen by psychiatrists for PTSD are benzodiazepine. However, benzodiazepines are better avoided the pharmacotherapy for PTSD (28–30).
In the disaster psychiatric response, the interdisciplinary team is needed (31–34). The post-graduate education about the disaster responses for nurses (35), psychologists/counselors (36, 37), and social workers (38) for disaster-related general and mental health services are also important. Therefore, the core competence in the training psychiatric residents is needed, in the post-graduate medical education.
The study notes a perceived lack of competence in utilizing psychotherapeutic approaches for DRPD. Core competence training in the postgraduate psychiatric education programs might enhance the subjective and objective competence in individual and group psychotherapies (39), even for the DRPD (40).
In this study, the deployment experiences of participants are associated with age, the length of practice, and board-ship in psychiatry. Incorporating real-world deployment experiences into postgraduate training might enhance psychiatrists’ readiness and confidence in disaster response (41, 42).
The variance in reported DRPD prevalence (ranging from 1.5% to 74%) in prior Taiwan-based studies may stem from methodological disparities, differing study populations, diagnostic criteria, and case definitions. This variance could also be attributed to Taiwan experiencing fewer wars and natural disasters compared to other regions. As a result, the populace might initially seek primary care providers over psychiatrists during disasters, highlighting potential gaps in popularizing disaster psychiatry in Taiwan (43).
Recent clinical guidelines underscore the efficacy of SSRIs and SNRIs in managing post-traumatic stress, recommending these medications for eligible patients (44). Complementary studies have also highlighted the benefits of benzodiazepines or nonbenzodiazepine agents for disaster-related anxiety and sleep disorders (45, 46). Correspondingly, the preference of Taiwanese psychiatrists for SSRIs, SNRIs, and Z-drugs/benzodiazepines aligns with international guidelines, indicating their substantial knowledge in managing DRPD through pharmacotherapy.
Psychotherapy’s significance in post-disaster mental health recovery cannot be overstated, especially in providing continuous psychological support (47–50). Despite evidence favoring psychotherapy’s efficacy over medications (51, 52), our study revealed psychiatrists’ perceived lack of competence in utilizing psychotherapeutic approaches for DRPD. This underscores the need for bolstering psychotherapy training among Taiwanese psychiatrists.
Limitations
This study’s limitations include its cross-sectional nature, hindering causal inference, and the lack of differentiation in the questionnaire regarding special needs among different age groups, such as children and the elderly. Additionally, a low response rate might introduce non-response bias, potentially attributed to various factors like workload and insufficient incentives. Therefore, we admitted that non-response bias existed in this study. One potential way to solve this problem in enhancing post-graduate medical education, since several studies have proved that post-graduate medical education could enhance the for the manpower development and capacity building in academic and research competence (53), workers’ skills in child and adolescent mental health (54), or providing culturally relevant and sensitive psychiatric training (55). Thirdly, in this study, we didn’t conduct the competence of the knowledge in the psychiatrists for the international treatment guidelines for DRPD. Further studies for this competence in the psychiatrists are needed in the future, since evidence-based guidelines for diagnosing and treating DRPD, such as PTSD, serve as valuable tools for psychiatrists and other healthcare professionals, facilitating the formulation of tailored treatment plans for their patients (56).
Conclusions
The study revealed that over 90% of participants exhibited intent to treat, follow-up, or be involved in the management of DRPD, while nearly 80% possessed prior experience in treating these disorders. Findings suggest that within post-graduate medical education, Taiwanese psychiatrists demonstrate significant experience, willingness, and capacity to effectively manage DRPD. However, there is a need to integrate comprehensive training on disaster psychiatry into post-graduate psychiatric education programs to further enhance preparedness and optimize outcomes in managing these challenging conditions.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
This study received approval from the Institutional Review Board at Tri-Service General Hospital, and written informed consent was obtained from all participants (TSGH IRB: 2-104-05-136). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
P-CL: Data curation, Formal analysis, Funding acquisition, Investigation, Writing – original draft. Y-CC: Data curation, Investigation, Writing – original draft, Methodology, Validation. L-CK: Data curation, Investigation, Methodology, Writing – original draft, Conceptualization, Formal analysis, Resources. F-JW: Conceptualization, Data curation, Investigation, Methodology, Resources, Writing – original draft. N-ST: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Writing – original draft, Funding acquisition, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. We acknowledge the support provided by the Medical Affairs Bureau, Ministry of Defense of Taiwan (MND-MAB-D-111–075 and MND-MAB-D-113059), Tri-Service General Hospital Research Foundation (TSGH-B-109–010, TSGH-E-110240, TSGH-B-111–018, and TSGH-D-111–121), Taoyuan Armed Forces General Hospital (TYAFGH-A-110–020), and National Defense Medical Center-Cardinal Tien Memorial Hospital Joint Foundation (). None of the sponsors played a role in the study design, data collection and analysis, decision to publish, or manuscript preparation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Neria Y, Nandi A, Galea S. Post-traumatic stress disorder following disasters: a systematic review. Psychol Med. (2008) 38:467–80. doi: 10.1017/S0033291707001353
2. McFarlane AC, Williams R. Mental health services required after disasters: learning from the lasting effects of disasters. Depress Res Treat. (2012) 2012:970194. doi: 10.1155/2012/970194
3. Goldmann E, Galea S. Mental health consequences of disasters. Annu Rev Public Health. (2014) 35:169–83. doi: 10.1146/annurev-publhealth-032013-182435
4. Norris FH, Friedman MJ, Watson PJ, Byrne CM, Diaz E, Kaniasty K. 60,000 disaster victims speak: Part I. An empirical review of the empirical literature, 1981–2001. Psychiatry. (2002) 65:207–39. doi: 10.1521/psyc.65.3.207.20173
5. Foreman T, Dickstein LJ, Garakani A. A Resident’s Guide To Surviving Psychiatric Training American Psychiatric Association(2007). Available online at: https://www.psychiatry.org/File%20Library/Residents-MedicalStudents/Residents/Residents_Guide_Psychiatric_Training.pdf (Accessed Dec. 1, 2023)
6. North CS, Nixon SJ, Shariat S, Mallonee S, McMillen JC, Spitznagel EL, et al. Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA. (1999) 28(8):755–62. doi: 10.1001/jama.282.8.755
7. Tol WA, van Ommeren M. Evidence-based mental health and psychosocial support in humanitarian settings: gaps and opportunities. Evid Based Ment Health. (2012) 15:25–6. doi: 10.1136/ebmental-2012-100644
8. Keya TA, Leela A, Habib N, Rashid M, Bakthavatchalam P. Mental health disorders due to disaster exposure: A systematic review and meta-analysis. Cureus. (2023) 15:e37031. doi: 10.7759/cureus.37031
9. Wesemann U, Applewhite B, Himmerich H. Investigating the impact of terrorist attacks on the mental health of emergency responders: systematic review. BJPsych Open. (2022) 8:e107. doi: 10.1192/bjo.2022.69
10. Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. Am J Psychiatry. (2001) 158:1184–90. doi: 10.1176/appi.ajp.158.8.1184
11. Ng AT. Disaster Psychiatry: What Psychiatrists Need to Know. (2010) Available Online at: https://www.psychiatrictimes.com/view/disaster-psychiatry-what-psychiatrists-need-know. (Aceessed Dec. 1, 2023).
12. Disaster Psychiatry Outreach. Disaster Psychiatry Outreach: DPO Clinical Protocal(2024). Available online at: https://www.vibrant.org/what-we-do/advocacy-policy-education/crisis-emotional-care/ (Accessed Jan. 1, 2024)
13. Outreach. DP. The Essentials of Disaster Psychiatry: A Training Course for Mental Health Professionals(2024). Available online at: https://www.vibrant.org/what-we-do/advocacy-policy-education/crisis-emotional-care/ (Accessed Dec. 1, 2023)
14. Ursano RJ, Fullerton CS, Norwood AE. Psychiatric dimensions of disaster: patient care, community consultation, and preventive medicine. Harv Rev Psychiatry. (1995) 3:196–209. doi: 10.3109/10673229509017186
15. Joint Commission of Taiwan. Ministry of Health and Welfare. Post Graduate Year Training(2022). Available online at: https://www.jct.org.tw/cp-1358–8378-3986b-2.html (Accessed Feb. 19, 2024)
16. Davis DJ, Ringsted C. Accreditation of undergraduate and graduate medical education: how do the standards contribute to quality? Adv Health Sci Educ Theory Pract. (2006) 11:305–13. doi: 10.1007/s10459-005-8555-4
17. Taiwanese Society of Psychiatry. Criteria for Recognition of Board-certified Psychiatrist Training Program (2017). Taiwanese Society of Psychiatry. Available online at: https://www.sop.org.tw/hospital/index_eva.asp (Accessed Feb. 7, 2024)
18. Brook P. The post-graduate education and training of consultant psychiatrists. Br J Psychiatry. (1974) 124:109–24. doi: 10.1192/bjp.124.2.109
19. Buzza C, Fiskin A, Campbell J, Guo J, Izenberg J, Kamholz B, et al. Competencies for global mental health: developing training objectives for a post-graduate fellowship for psychiatrists. Ann Glob Health. (2018) 84(4):717–26. doi: 10.29024/aogh.2382
20. Algaali KY, Djalali A, Della Corte F, Ismail MA, Ingrassia PL. Postgraduate education in disaster health and medicine. Front Public Health. (2015) 3:185. doi: 10.3389/fpubh.2015.00185
21. Kokai M, Fujii S, Shinfuku N, Edwards G. Natural disaster and mental health in Asia. Psychiatry Clin Neurosci. (2004) 58:110–6. doi: 10.1111/j.1440-1819.2003.01203.x
22. Chang HC, Wu YS, Tzeng WC, Wu HY, Lee PC, Wang WY. Sex differences in risk factors for metabolic syndrome in middle-aged and senior hospital employees: a population-based cohort study. BMC Public Health. (2023) 23:587. doi: 10.1186/s12889-023-15491-4
23. Tzeng WC, Tzeng NS, Chang PC, Chien WC, Feng HP, Lin CH. Gender difference in emotional distress among nursing and health science college students: An online survey. Arch Psychiatr Nurs. (2024) 48:36–42. doi: 10.1016/j.apnu.2024.01.007
24. Chou HW, Tzeng WC, Chou YC, Yeh HW, Chang HA, Kao YC, et al. Psychological morbidity, quality of life, and self-rated health in the military personnel. Neuropsychiatr Dis Treat. (2014) 10:329–38. doi: 10.2147/NDT
25. Hsu YC, Chou YC, Chang HA, Kao YC, Huang SY, Tzeng NS. Dilemma of prescribing aripiprazole under the Taiwan health insurance program: a descriptive study. Neuropsychiatr Dis Treat. (2015) 11:225–32. doi: 10.2147/NDT.S75609
26. Chou HW, Tzeng WC, Chou YC, Yeh HW, Chang HA, Kao YC, et al. Stress, sleep and depressive symptoms in active duty military personnel. Am J Med Sci. (2016) 352(2):146–53. doi: 10.1016/j.amjms.2016.05.013
27. Chou FH, Wu HC, Chou P, Su CY, Tsai KY, Chao SS, et al. Epidemiologic psychiatric studies on post-disaster impact among Chi-Chi earthquake survivors in Yu-Chi, Taiwan. Psychiatry Clin Neurosci. (2007) 61:370–8. doi: 10.1111/j.1440-1819.2007.01688.x
28. Asnis GM, Kohn SR, Henderson M, Brown NL. SSRIs versus non-SSRIs in post-traumatic stress disorder: an update with recommendations. Drugs. (2004) 64:383–404. doi: 10.2165/00003495-200464040-00004
29. Friedman MJ. Toward rational pharmacotherapy for posttraumatic stress disorder: an interim report. Am J Psychiatry. (1988) 145:281–5. doi: 10.1176/ajp.145.3.281
30. Sutherland SM, Davidson JR. Pharmacotherapy for post-traumatic stress disorder. Psychiatr Clin North Am. (1994) 17:409–23. doi: 10.1016/S0193-953X(18)30122-9
31. Procter NG. Emergency mental health nursing for self-harming refugees and asylum seekers. Int J Ment Health Nurs. (2005) 14:196–201. doi: 10.1111/j.1440-0979.2005.00381.x
32. Slaby AE, Goldberg RJ, Wallace SR. Interdisciplinary team approach to emergency psychiatric care. Psychosomatics. (1983) 24:627–37. doi: 10.1016/S0033-3182(83)73172-5
33. Wallace SR, Ward JT, Goldberg RJ, Slaby AE. The social worker as primary psychiatric consultant to the general hospital emergency room. Emerg Health Serv Rev. (1985) 3:11–24. doi: 10.1300/J261v03n01_03
34. Zealberg JJ, Santos AB, Hiers TG, Ballenger JC, Puckett JA, Christie SD. From the benches to the trenches: training residents to provide emergency outreach services-a public/academic project. Acad Psychiatry. (1990) 14:211–7. doi: 10.1007/BF03341357
35. Loke AY, Li S, Guo C. Mapping a postgraduate curriculum in disaster nursing with the International Council of Nursing’s Core Competencies in Disaster Nursing V2.0: The extent of the program in addressing the core competencies. Nurse Educ Today. (2021) 106:105063. doi: 10.1016/j.nedt.2021.105063
36. Daneman EA, Smith JI. Post-graduate pastoral counseling seminars. Dis Nerv Syst. (1959) 20:575–81.
37. Hunt AD Jr., Parmet M. Collaboration between pediatrician and child psychiatrist in a rural medical center; case studies illustrating the role of this relationship in the post-graduate education of the family physician. Pediatrics. (1957) 19:462–6. doi: 10.1542/peds.19.3.462
39. Stricker G. Len Sperry: core competencies in counseling and psychotherapy: becoming a highly competent and effective therapist. J Contemp Psychotherapy. (2012) 42:121–2. doi: 10.1007/s10879-011-9186-0
40. King RV, Burkle FM Jr., Walsh LE, North CS. Competencies for disaster mental health. Curr Psychiatry Rep. (2015) 17:548. doi: 10.1007/s11920-015-0548-2
41. Lofchy J, Boyles P, Delwo J. Emergency psychiatry: clinical and training approaches. Can J Psychiatry. (2015) 60:1–7.
42. The Royal Australian and New Zealand College of Psychiatrists. Rural Psychiatry Roadmap 2021–31(2021). Available online at: https://www.ranzcp.org/getmedia/f2adde4a-30dc-49c1-a959-a7543e757d34/rural-psychiatry-roadmap-2021–31.pdf (Accessed Feb. 7, 2024).
43. Angela Lo HW, Su CY, Chou FH. Disaster psychiatry in Taiwan: A comprehensive review. J Exp Clin Med. (2012) 4:77–81. doi: 10.1016/j.jecm.2012.01.005
44. Alexander W. Pharmacotherapy for post-traumatic stress disorder in combat veterans: focus on antidepressants and atypical antipsychotic agents. P T. (2012) 37:32–8.
45. Bandelow B, Zohar J, Hollander E, Kasper S, Möller HJ, WFSBP Task Force on Treatment Guidelines for Anxiety, Obsessive-Compulsive and Post-Traumatic Stress Disoders, et al. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for the pharmacological treatment of anxiety, obsessive-compulsive and post-traumatic stress disorders - first revision. World J Biol Psychiatry. (2008) 9:248–312. doi: 10.1080/15622970802465807
46. Lavie P. Sleep disturbances in the wake of traumatic events. N Engl J Med. (2001) 345:1825–32. doi: 10.1056/NEJMra012893
47. Kun P, Han S, Chen X, Yao L. Prevalence and risk factors for posttraumatic stress disorder: a cross-sectional study among survivors of the Wenchuan 2008 earthquake in China. Depress Anxiety. (2009) 26:1134–40. doi: 10.1002/da.v26:12
48. Ruzek J, Walser RD, Naugle AE, Litz B, Mennin DS, Polusny MA, et al. Cognitive-behavioral psychology: implications for disaster and terrorism response. Prehosp Disaster Med. (2008) 23(5):397–410. doi: 10.1017/S1049023X00006130
49. Stoddard FJ, Katz CL, Merlino JP. What You Need to Know for the Next Disaster: A Practical Mental Health Guide for Clinicians. Sudbury, Massachusetts: Jones & Bartlett Pub Inc (2009).
50. Rosen CS, Cohen M. Subgroups of New York City children at high risk of PTSD after the September 11 attacks: A signal detection analysis. Psychiatr Services. (2010) 61:64–9. doi: 10.1176/ps.2010.61.1.64
51. McLaughlin KA, Fairbank JA, Gruber MJ, Jones RT, Lakoma MD, Pfefferbaum B, et al. Serious emotional disturbance among youths exposed to Hurricane Katrina 2 years postdisaster. J Am Acad Child Adolesc Psychiatry. (2009) 48(11):1069–78. doi: 10.1097/CHI.0b013e3181b76697
52. Sakauye KM, Streim JE, Kennedy GJ, Kirwin PD, Llorente MD, Schultz SK, et al. AAGP position statement: disaster preparedness for older Americans: critical issues for the preservation of mental health. Am J Geriatr Psychiatry. (2009) 17:916–24. doi: 10.1097/JGP.0b013e3181b4bf20
53. Thakurdesai A, Ghosh A, Menon V, Sahoo S, Tripathi A, Harshe D, et al. Electronic journal clubs for capacity building: A case study in psychiatry as a model for medical disciplines in developing countries. Asian J Psychiatr. (2018) 34:93–7. doi: 10.1016/j.ajp.2018.04.026
54. Russell PS, Tsheringla S, Nair MK, Minju KA. Priority mental health disorders of children and adolescents in primary-care pediatric settings in India 4: training and capacity building. Indian J Pediatr. (2012) 79 Suppl 1:S39–44. doi: 10.1007/s12098-011-0429-6
55. Chang OA, Allen MM, Pandit B. Capacity building for Pacific Island countries: the challenges and benefits of developing a postgraduate clinical training programme. Australas Psychiatry. (2015) 23:32–4. doi: 10.1177/1039856215608294
Keywords: disasters, psychiatrists, depression, post-traumatic stress disorder, antidepressants, post-graduate medical education
Citation: Lin P-C, Chou Y-C, Kao L-C, Wan F-J and Tzeng N-S (2024) Assessment of psychiatrists’ preparedness in managing disaster-related psychiatric disorders: a survey in Taiwan from post-graduate medical education perspective. Front. Psychiatry 15:1368242. doi: 10.3389/fpsyt.2024.1368242
Received: 10 January 2024; Accepted: 20 May 2024;
Published: 06 June 2024.
Edited by:
Ulrich Wesemann, Military Hospital Berlin, GermanyReviewed by:
Yia-Ping Liu, Cheng Hsin General Hospital, TaiwanOliver Hochfeld, Charité University Medicine Berlin, Germany
Copyright © 2024 Lin, Chou, Kao, Wan and Tzeng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nian-Sheng Tzeng, pierrens@mail.ndmctsgh.edu.tw
 Po-Chun Lin
Po-Chun Lin Yu-Ching Chou
Yu-Ching Chou Lien-Cheng Kao1,3
Lien-Cheng Kao1,3 Nian-Sheng Tzeng
Nian-Sheng Tzeng