- 1The Centre for Healthcare Resilience and Implementation Science, Australian Institute of Health Innovation, Faculty of Medicine, Health and Human Science, Macquarie University, Macquarie, NSW, Australia
- 2Centre for the Health Economy, Macquarie University Business School, Macquarie University, Macquarie, NSW, Australia
- 3Western Sydney Local Health District, New South Wales Health, Sydney, NSW, Australia
- 4Emergency Care Institute, New South Wales Agency for Clinical Innovation, New South Wales Health, Sydney, NSW, Australia
- 5Quality and Safeguards Commission, National Disability Insurance Scheme, Sydney, NSW, Australia
Background: Care delivery for the increasing number of people presenting at hospital emergency departments (EDs) with mental illness is a challenging issue. This review aimed to synthesise the research evidence associated with strategies used to improve ED care delivery outcomes, experience, and performance for adults presenting with mental illness.
Method: We systematically reviewed the evidence regarding the effects of ED-based interventions for mental illness on patient outcomes, patient experience, and system performance, using a comprehensive search strategy designed to identify published empirical studies. Systematic searches in Scopus, Ovid Embase, CINAHL, and Medline were conducted in September 2023 (from inception; review protocol was prospectively registered in Prospero CRD42023466062). Eligibility criteria were as follows: (1) primary research study, published in English; and (2) (a) reported an implemented model of care or system change within the hospital ED context, (b) focused on adult mental illness presentations, and (c) evaluated system performance, patient outcomes, patient experience, or staff experience. Pairs of reviewers independently assessed study titles, abstracts, and full texts according to pre-established inclusion criteria with discrepancies resolved by a third reviewer. Independent reviewers extracted data from the included papers using Covidence (2023), and the quality of included studies was assessed using the Joanna Briggs Institute suite of critical appraisal tools.
Results: A narrative synthesis was performed on the included 46 studies, comprising pre-post (n = 23), quasi-experimental (n = 6), descriptive (n = 6), randomised controlled trial (RCT; n = 3), cohort (n = 2), cross-sectional (n = 2), qualitative (n = 2), realist evaluation (n = 1), and time series analysis studies (n = 1). Eleven articles focused on presentations related to substance use disorder presentation, 9 focused on suicide and deliberate self-harm presentations, and 26 reported mental illness presentations in general. Strategies reported include models of care (e.g., ED-initiated Medications for Opioid Use Disorder, ED-initiated social support, and deliberate self-harm), decision support tools, discharge and transfer refinements, case management, adjustments to liaison psychiatry services, telepsychiatry, changes to roles and rostering, environmental changes (e.g., specialised units within the ED), education, creation of multidisciplinary teams, and care standardisations. System performance measures were reported in 33 studies (72%), with fewer studies reporting measures of patient outcomes (n = 19, 41%), patient experience (n = 10, 22%), or staff experience (n = 14, 30%). Few interventions reported outcomes across all four domains. Heterogeneity in study samples, strategies, and evaluated outcomes makes adopting existing strategies challenging.
Conclusion: Care for mental illness is complex, particularly in the emergency setting. Strategies to provide care must align ED system goals with patient goals and staff experience.
1 Introduction
Emergency departments (EDs) are tasked with providing high-quality, safe, and timely acute care. To meet the changing needs of the community, care safety and quality are continually assessed to identify targeted areas for improvement. Inadequately resourced mental healthcare elsewhere in the system has contributed to rising presentations to ED (1, 2), but EDs experiencing overcrowding and access block (delay in transferring the person to an admitted hospital ward bed) may be unsuitable for the management of mental illness (3). The high-stimulus environment and lengthy wait times can result in poor patient outcomes, including leaving before completion of care, or escalating patient agitation and use of restrictive interventions, including traumatic use of restraint (4, 5). Patients seeking ED care for mental illness report poor staff attitudes and knowledge, and feeling powerless to access needed care (6). Negative experiences can discourage a person from accessing care in the future (6–8). Similarly, ED staff report being inadequately prepared or resourced to provide care for some presenting mental illness, and an inability to obtain timely patient assessment by specialist mental health staff (9–11). Patient and staff experiences are reflected in ED system performance, with measures such as wait times, total ED length of stay (LoS), and left at own risk (left the ED prior to completion of care) (12) reflecting problems in care provision for adults with mental illness in the ED. Thus, an imperative exists to improve care delivery for adults presenting to ED with mental illness.
The ED has a long history of innovating practices and processes, such as clinical pathways to expedite standardised intervention, as well as expanding the ED team composition to include advanced nursing and allied health roles to improve care delivery (13). The desire to improve care for adults presenting to ED with mental illness has prompted better understanding of the characteristics of ED presentations such as deliberate self-harm (14–16), suicidal ideation (17, 18), anxiety and depression (19, 20), substance use (21), specific vulnerabilities among the homeless (22, 23) or incarcerated adults (24, 25), and symptomatology including agitation resulting in restraint (26, 27). Similarly, systematic reviews shed light on the strategies employed to improve care for adults presenting to ED with acute mental illness, exploring the effectiveness of case management (28), various liaison psychiatry models (29), as well as strategies specifically targeting frequent users (30), deliberate self-harm (31), and opioid use disorder (32). These systematic reviews provide insights into the impact of strategies to improve care delivery in the ED for individual models of care and specific patient presentations, they do not provide a comprehensive synthesis of reported strategies and their impact on system performance, patient outcomes, patient experience, and staff experience.
A 2019 scoping review by Johnston and colleagues (33) identified a wide range of strategies implemented or delivered in the ED for adults presenting with mental illness. Strategies were patient-focused, including information, education, psychotherapy, and pharmacology; staff-focused, such as education and assessment processes; or system-focused, for example, new referral processes and the capacity to case manage, with some studies focusing on staff and patients (33). While comprehensive, the 2019 review did not identify strategies to improve patient experience. Understanding and improving patient experience is essential for patient engagement and clinical outcomes (34). Consequently, identifying strategies to improve patient experience is critical for informing changes in ED care delivery. Given the increasing volume of mental health presentations (35, 36), as well as workforce constraints and increasing service demand (35), it is necessary to revisit the question of what strategies have been used to improve care delivery outcomes and experiences for adults with mental illness in the ED, to guide service adaptation.
Understanding the strategies that have been successful in improving care delivery or experience will enable ED clinicians, managers, and hospital executives to make more informed decisions about what can be done to improve care in their local context. We sought to identify interventions implemented in the ED for people presenting with mental illness as a foundation for a comprehensive programme to codesign new or adapted models of ED care for this cohort (37). Therefore, the purpose of this systematic review was to examine the research evidence provided in the peer-reviewed literature to identify the relationship between the strategies used to improve ED care delivery for adult mental illness presentations and measures of (1) system performance, (2) patient outcomes, (3) patient experience, and (4) staff experience.
2 Methods
The study protocol was registered in September 2023 in Prospero (CRD42023466062). The study protocol guided the review in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (38).
2.1 Search strategy
A comprehensive search strategy using medical subject headings and text words for the general concepts of ED, improvement, outcomes, and mental illness was developed in consultation with a research librarian. Scopus, Ovid Embase, CINAHL, and Medline were searched on 22 September 2023 for peer-reviewed English language articles. No date limits were set. The full search strategy is shown in Supplementary File A.
2.2 Eligibility criteria
Empirical peer-reviewed research articles were included in the systematic review if they met the following criteria:
Population: (1) Mental health presentations [e.g., undifferentiated, suicidal, deliberate self-harm, scheduled, substance-related and addictive disorders (e.g., drug and alcohol), depressive disorders, anxiety disorders]; (2) adults; and (3) in the ED.
Intervention: Implemented models of care or system changes (e.g., redesigning the environment to reduce stimulation, new care pathway).
Comparison: Usual care or other form of care.
Outcome: Measures of (1) system performance (e.g., waiting time, LoS, time to treatment/assessment etc., admissions, and referrals); (2) patient outcomes (e.g., readmission, adverse events, medical errors, missing diagnosis, pain, and quality of life); (3) patient experience (e.g., patient experience, complaints, did not wait, left without being seen, and left at own risk); or (4) staff experience (e.g., staff experience, job satisfaction, and intention to stay).
Articles were excluded if they (1) reported on interventions that were conducted primarily in the pre-hospital, post-hospital, or a ward/clinic setting other than the ED; (2) involved persons under 18 years of age; (3) focused on disability or neurodiversity (e.g., autism); (4) did not report an intervention (e.g., reported only trends or characterisations), screened presentations with no accompanying intervention within the ED; (5) were literature reviews, conference poster or abstract, grey literature, and case report; or (6) were published in a language other than English.
2.3 Screening and data extraction
The search results were entered into EndNote citation management software (version 20.6; Thompson Reuters, New York, NY) and duplicates were removed. References were uploaded into Covidence, a subscription web-based tool for conducting screening, data extraction, and critical appraisal for systematic reviews. During the title and abstract, and full-text screening phases of the review, each article was screened independently by pairs of reviewers for inclusion according to the predefined criteria. Disagreements were resolved by an independent third reviewer.
Data were extracted by independent reviewers in the Covidence platform (2023) (39) using a customised extraction tool specifically developed for the review. The data extraction form was piloted for usability on four articles by four independent reviewers before data extraction commenced. The data extraction form included information on the country where the study was conducted, the aim of the study, the study design, the number of EDs included, the aim of the intervention, description of the intervention, number of participants, the mental illness focus, participant inclusion and exclusion criteria, participant characteristics, evaluated outcomes (i.e., system performance, patient outcomes, patient experience, and staff experience), and study limitations. The data extraction form is shown in Supplementary File B.
2.4 Risk of bias
The methodological quality of the included articles was assessed using the Joanna Briggs Institute critical appraisal tool for the study type: Checklist for Cohort Studies, Checklist for Case–Control Studies, Checklist for Analytical Cross-Sectional Studies, Checklist for Randomised Controlled Trials, Checklist for Quasi-Experimental Studies, and the Checklist for Qualitative Research Studies (40, 41). Four articles were used to pilot the critical appraisal tool. Each article was critically appraised by pairs of independent reviewers in Covidence, with disagreements resolved via discussion. Covidence does not have a mechanism for allocating a subset of studies, nor is there a mechanism to calculate a metric of inter-rater reliability for critical appraisal. Instead, reviewers are allocated a number of papers to appraise to ensure that the work is divided in a just way.
2.5 Data processing and analysis
Because of the heterogeneity of included articles, a narrative synthesis was conducted for this review. Data were synthesised according to the mental illness focus of the presentation and included numerical statistical summaries, textual commentaries, and tabular and graphical representations.
2.6 Patient and public involvement
Patients and the public were not involved in the design and conduct of this review.
3 Results
3.1 Literature search
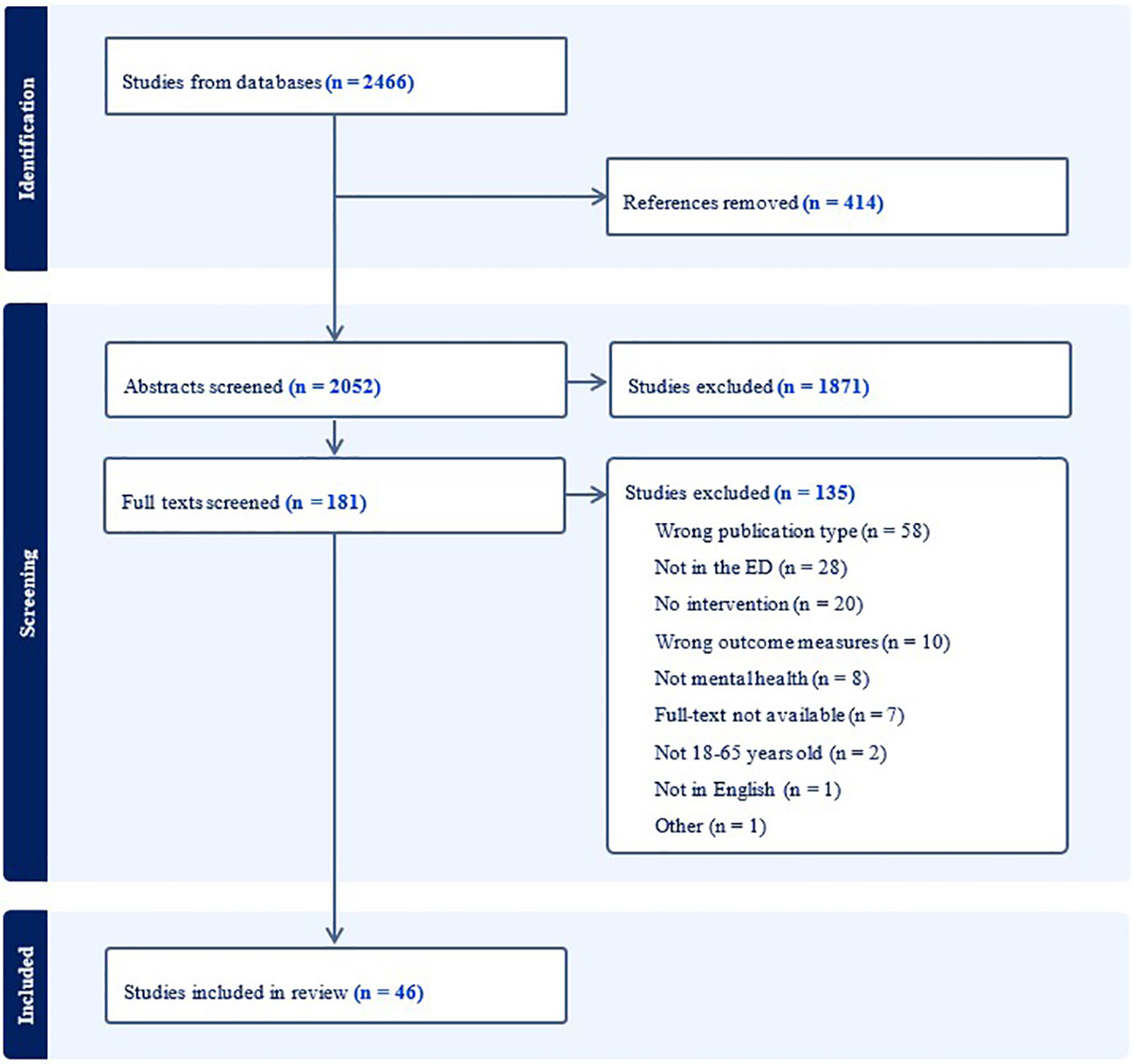
The combined searches yielded 2,466 articles, including 414 duplicate articles. Of these, 2,052 abstracts and 181 full texts were screened with 46 articles meeting the inclusion criteria. Figure 1 depicts the PRISMA diagram for the identification, screening, and inclusion processes.
3.2 Description of included studies
Characteristics of the included studies are in Supplemetary File C. Included articles were published between 2000 and 2023 and primarily conducted in high-income countries including the USA (54%, n = 25), Australia (15%, n = 7), the UK (13%, n = 6), and Canada (9%, n = 4). One study each was conducted in Ireland, Israel, Japan, and Norway.
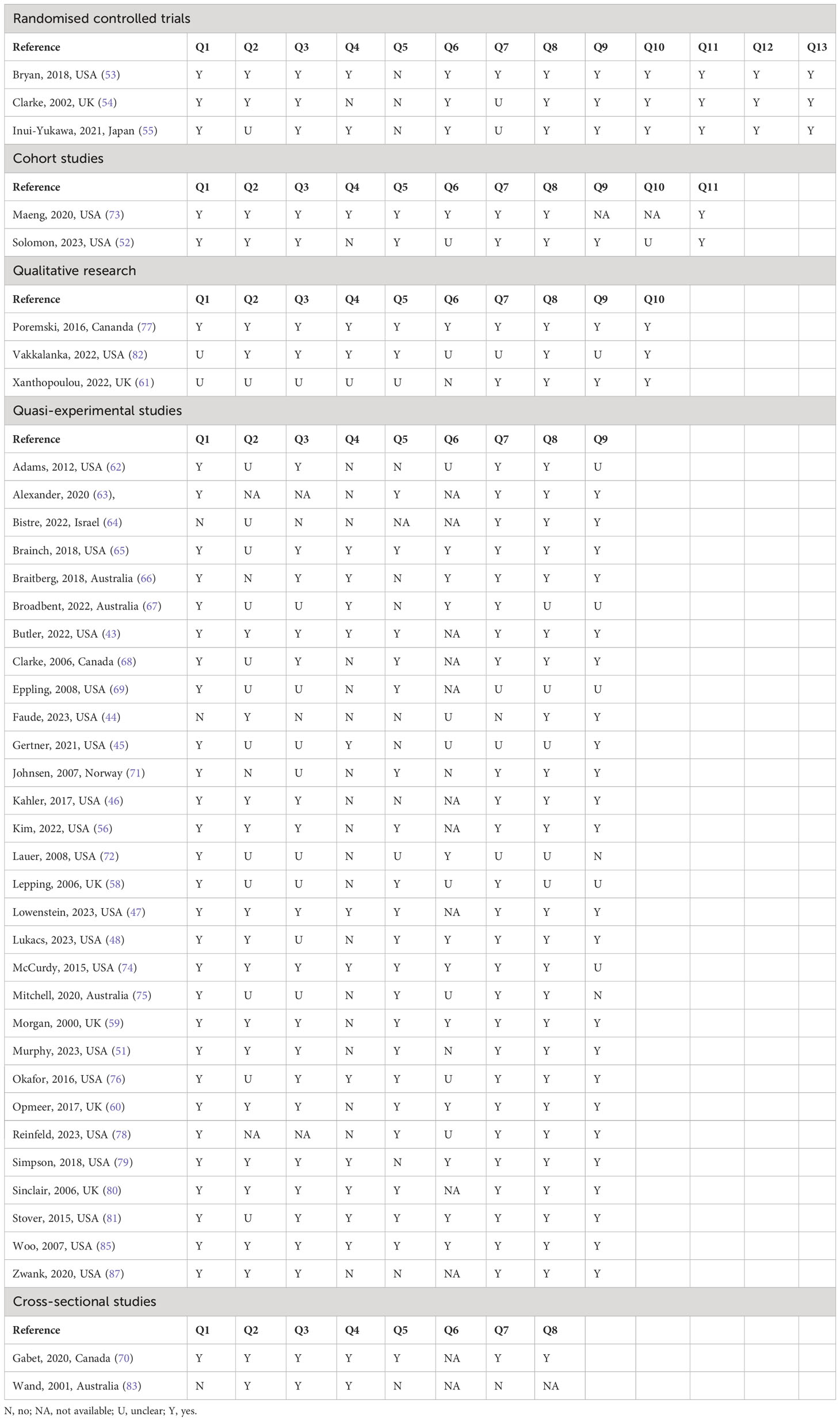
3.3 Quality assessment
Most studies were assessed as having potential flaws or limitations in their design, conduct, or analysis that could distort the results. While risk of bias is important to report, all studies were retained in this review for the potential learning that may be derived about the interventions and measures that might be tested more rigorously in subsequent studies should they have potential for the readers’ context. The outcomes from the quality assessment are shown in Table 1.
3.4 Mental health presentations
Eleven of the 46 included articles (23.9%) focused on substance-related and addictive disorders (e.g., substance use disorder) and 9 (19.6%) focused on suicidal or deliberate self-harm, whereas 26 (56.5%) sought to address care delivery for all mental illness presentations.
3.5 Innovations for substance-related and addictive disorder presentations
Eleven of the 46 articles reported on strategies focusing on substance-related and addictive disorder presentations (Table 2). Four types of strategies were evaluated, including the ED-initiated Medications for Opioid Use Disorder (MOUD) model of care (42–45, 49–52), decision support tools (42, 46, 47), ED-initiated social support model of care (48), and discharge and transfer of care (42, 46). Overall, the ED-initiated MOUD model of care reported effects across all four domains of interest; however, not one study reported on all four. System performance effects (e.g., identification of eligible patients) were reported for three of the four strategies; all four strategies evaluated patient outcomes (e.g., engagement with formal treatment); one strategy evaluated patient experience (e.g., satisfaction); and one strategy evaluated staff experience (e.g., readiness). Eight of the 11 articles included at least one academic medical centre (42–47, 49, 51), with three of the eight articles including at least one community hospital (42, 47, 49). One of the eight articles also included a private hospital (42). Three of the 11 studies did not report the type of participating hospital (48, 50, 52). Eight of the 11 articles were conducted in urban settings (43, 44, 46–51), with one reporting an additional rural site (49). Three of the 11 studies did not report the setting as either urban or rural (42, 45, 52). Three articles reported that the participating EDs were connected with psychiatric crisis centres or psychiatric EDs (44, 45, 47).
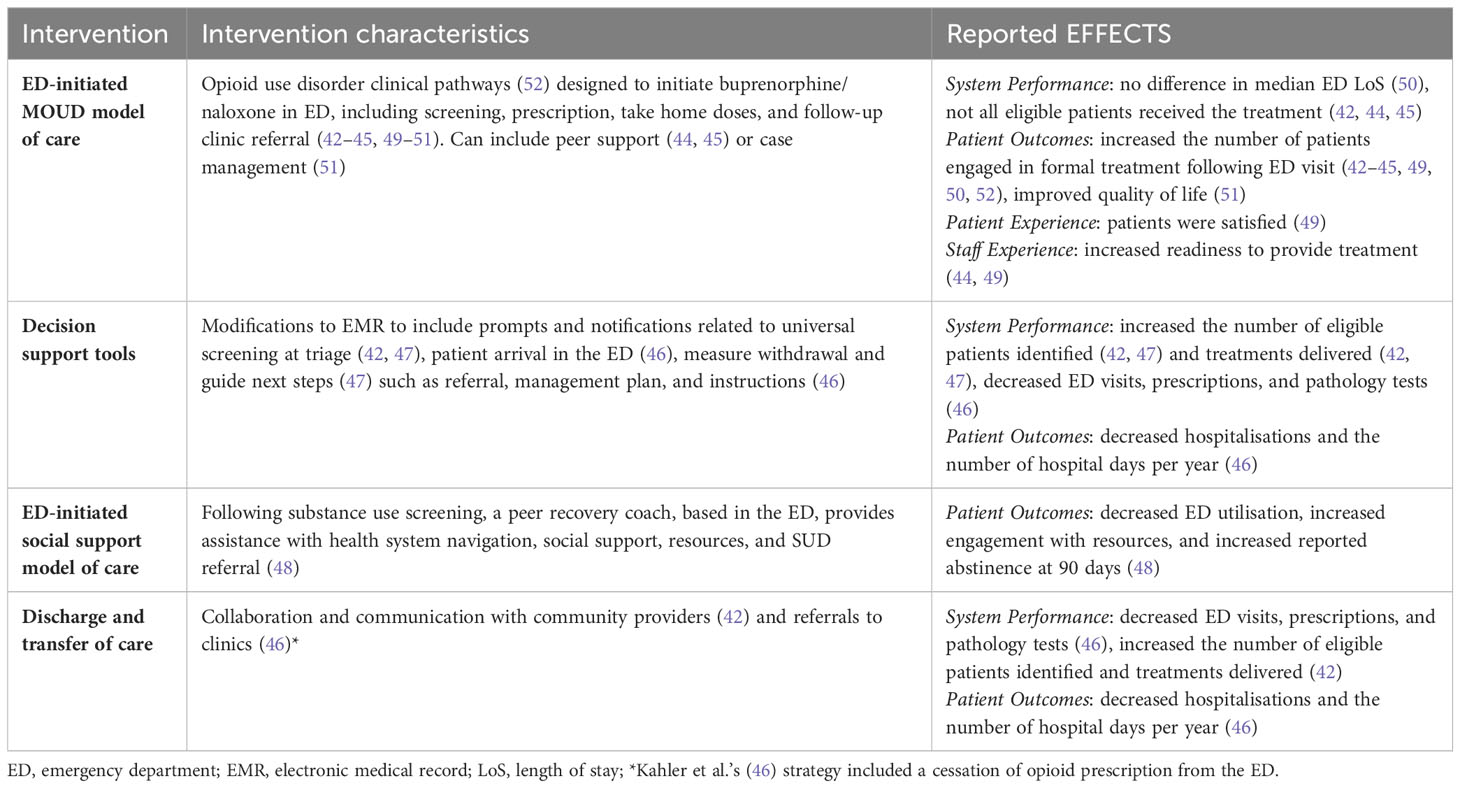
Table 2 Substance-related and addictive disorder focused interventions, intervention characteristics, and their reported effects.
3.6 Innovations for suicide and deliberate self-harm presentations
Nine of the 46 articles reported on strategies focusing on suicide and deliberate self-harm presentations. The five types of strategies comprised case management, liaison psychiatry services, deliberate self-harm models of care, and specialised units, and focused on assessment (53–56, 58–61), brief interventions (56, 60, 61), monitoring (57), care plan development (53–55), and referral to community-based support (53, 54, 56). System performance effects (e.g., wait time for assessment) were reported for three of the five strategies, four strategies reported patient outcomes (e.g., rate of self-harm), one strategy reported patient experience, and one strategy reported staff experience (e.g., favourability). A description of the characteristics of each type of suicide or self-harm strategy and their reported effect is provided in Table 3. Two of the nine articles included an academic medical centre and one general hospital (30, 57, 59). Six of the nine studies did not report the type of participating hospital (53–55, 58, 60, 61). Two of the nine articles were conducted in urban settings (57, 58), with one reporting a semi-rural site (59). Six of the nine studies did not report the setting as either urban or rural (53–56, 60, 61). Four articles reported that the participating EDs were connected with psychiatric services such as liaison psychiatry (56, 58–60), one reported not having access to psychiatric services (57), and four did not report on access to psychiatric services (53–55, 61).
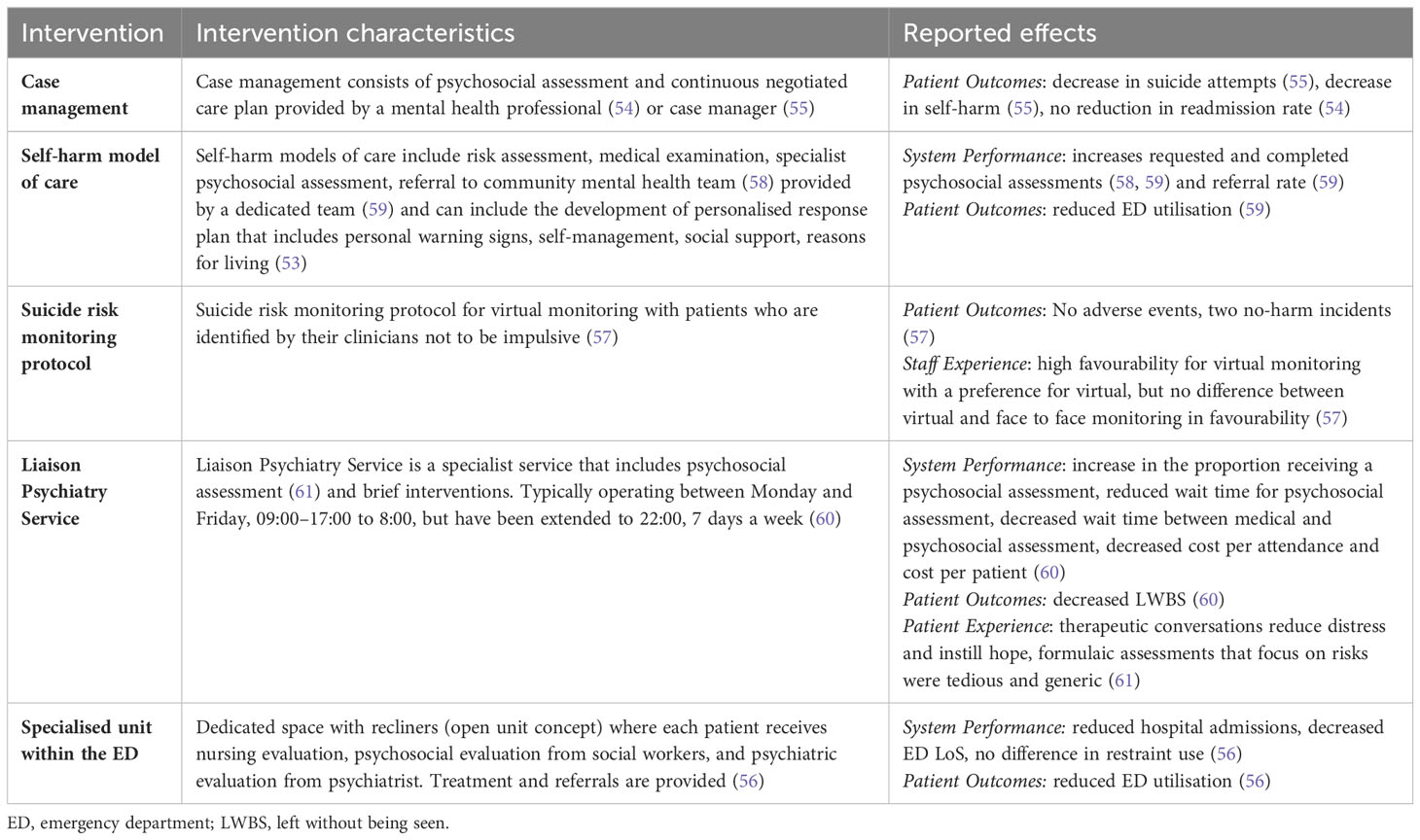
Table 3 Suicide or deliberate self-harm interventions, intervention characteristics, and reported effects.
3.7 Innovations for mental health presentations
Twenty-six of the 46 articles reported on strategies that encompassed all mental illness presentations to the ED (Table 4). The 11 types of strategies implemented in ED included decision support tools [e.g., modifications to electronic medical record (EMR)] (62, 63, 67, 79), discharge and transfer of care (e.g., collaboration and communication processes) (62, 63, 81), liaison psychiatry services (e.g., included ED staff in meetings) (63), telepsychiatry (e.g., assessment) (64, 82), changes to roles and rostering (e.g., mental health professions in ED) (63, 65, 69, 73, 78, 80, 83), specialised units within ED (e.g., behavioural assessment unit) (66, 72, 75, 76, 85, 86), education and training (e.g., related to mental illness) (68), intervention teams (e.g., multidisciplinary team) (70, 84), standardising protocols (e.g., procedures for agitated behaviour management) (71, 78, 79, 86, 87), environmental design (e.g., glass doors) (74), and case management (e.g., facilitating connections with services) (77, 86). System performance effects (e.g., ED LoS and use of restraint) were reported for all 11 strategies, 7 strategies reported patient outcomes (e.g., ED utilisation), 6 strategies reported patient experience (e.g., preferences), and 8 strategies reported staff experience (e.g., confidence). Fourteen of the 26 articles included an academic medical centre (63, 65, 66, 68, 70, 74, 76, 77, 79, 83–87), and 3 of the 26 included a community hospital (62, 69, 73). Nine of the 26 studies did not report the type of participating hospital (64, 67, 71, 72, 75, 78, 80–82). Eighteen of the 26 articles were conducted in urban settings (63, 65, 66, 68–70, 72, 75–77, 79–81, 83–87), with one reporting an additional rural site (84), and two reported only rural sites (73, 82). Five of the 26 studies did not report the setting as either urban or rural (62, 64, 67, 71, 74, 78). Thirteen articles reported that the participating EDs were connected with psychiatric crisis services (62, 69–71, 74–76, 78, 79, 82, 85–87), and 13 did not (20, 63–68, 72, 73, 77, 80, 81, 83).
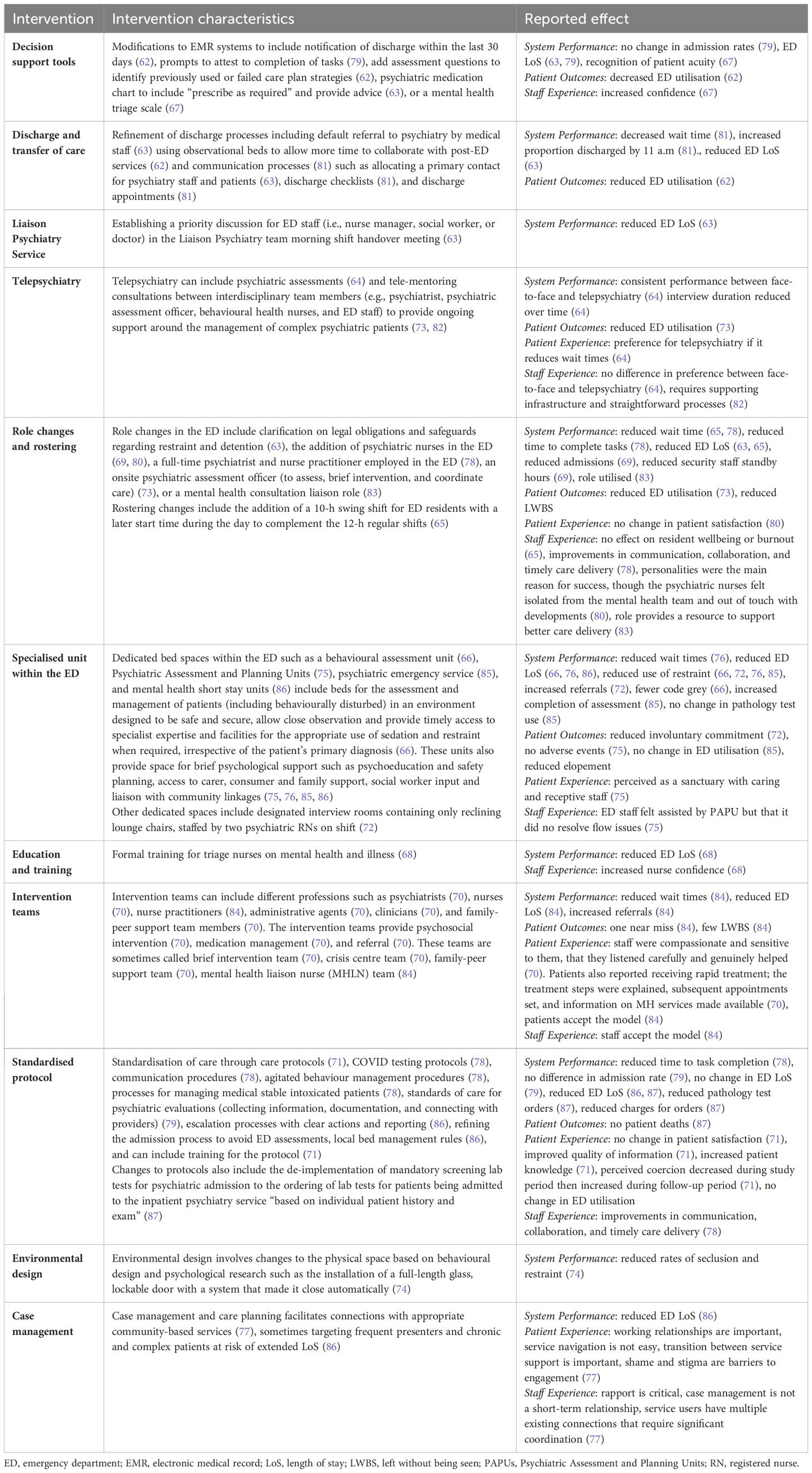
Table 4 Mental health presentation interventions, intervention characteristics, and reported effects.
4 Discussion
We examined the research evidence provided by peer-reviewed literature describing strategies to improve ED care delivery for adults presenting with mental illness and measures of system performance, patient experience, patient outcomes, and staff experience. This systematic review found illness-specific strategies oriented to longer-term care delivery beyond the ED, and general mental illness interventions oriented to process improvements. Substance-related and addictive disorder interventions focused on the initiation of initial dose (e.g., buprenorphine or naloxone) with take home doses and clinic follow-up (42–45, 49–52). Similarly, strategies for suicide and deliberate self-harm presentations focused on assessment, care plan development and connecting with community-based support (53–55, 58–61). Strategies for mental illness presentations in general included modifications to the EMR to support decision making (62, 63, 67, 79), additional mental health roles (69, 73, 78, 80, 83) and intervention teams (70, 84), designated spaces for psychosocial assessment, treatment and referral (66, 72, 75, 76, 86), and refined discharge processes (62, 63, 81). For EDs and the communities they serve, considered selection of strategies and measures is essential in ensuring responsive, safe, and timely emergency care; however, without detailed descriptions of ED settings and use of common outcome measures, identification of high-impact interventions that might be transferable is challenging.
4.1 Identifying high-impact interventions for the local context
ED interventions interact with the characteristics, circumstances, and unique factors of the ED where they are implemented (88). Where an intervention was associated with favourable outcomes, contextual factors may have influenced these outcomes, but these were not consistently described across studies. More consistent reporting of interventions using reporting guidelines, such as the Template for Intervention Description and Replication (TIDieR) checklist (89), would be helpful in future research and for the overall development of the field. It was also challenging to judge unvalidated patient satisfaction surveys, particularly as patient characteristics such as education level and age have been associated with higher patient satisfaction scores (90). More consistent reporting of patient outcome measures, such as those advanced by the International Consortium for Health Outcomes Measurement (91), may assist in better identifying replicable high-impact interventions. While presentation-specific and systems-based solutions have the potential to improve the capacity of ED staff to provide care safely and ethically for adults presenting with mental illness, interventions must be aligned with current clinical guidelines and the purpose of the ED system. The evidence currently supporting the effectiveness of these strategies is limited with more detailed development of strategies and analysis needed to make meaningful progress in improving care delivery.
4.2 Evaluating the impact of interventions
Differences between the communities each ED served were reflected in the diverse selection of strategies and the measures employed to understand their effect. The importance of a comprehensive understanding of the effect of strategies on all of system performance, patient outcomes, patient experience, and staff experience, and the outcomes valued or prioritised locally was identified in this review. Only one of the implemented strategies, the ED-initiated MOUD model of care, reported outcomes across all four domains, accrued through eight separate studies. Furthermore, the outcomes reported by Sinclair et al. (80), Mitchell et al. (75), and Woo et al. (85) suggest that improvements in one domain, such as system performance, may not always translate to improvements in others, for example, patient and staff experience. For example, Sinclair measured an increase in the number of patients assessed but no difference in patient satisfaction, potentially because there was no difference in waiting time (a system performance measure that may be valued more highly by patients). Furthermore, Sinclair reported that while ED staff appreciated the addition of a specialist mental health nurse, the mental health staff integrated in the ED felt isolated from the mental health team and out of touch with developments in their specialty. Therefore, it is crucial to understand system performance goals as well as what patients and staff value, and evaluate interventions across all four domains to support the sustainability of improvement efforts.
4.3 Implications for clinical practice, policy, and research
The characteristics of the strategies and their evaluated outcomes suggest that adults are seeking ED care for mental illness that EDs are not resourced to provide. In attempting to bridge the care gap, EDs are often having to implement practices outside their operational and structural role of rapid assessment, stabilisation, and referral to hospital inpatient or community-based care, as one component of an integrated health system. This means that some of the reviewed strategies to improve care are not aligned with the ED system purpose, potentially exhausting the EDs’ capacity to respond to all patients’ needs effectively (92) and potentially diminishing the resilience of the ED system (93). Nevertheless, the ED is an important component of the care continuum and must therefore be integrated into the health system that cares for adults with mental illness, often in conjunction with comorbid, physical health issues. In this review, Consultation Liaison Psychiatry (CLP) in ED was found to improve system performance, patient outcomes, and patient experience (i.e., Opmeer et al. and Xanthopoulou et al.) (60, 61). CLP is a subspeciality of adult psychiatry that provides specialist medical expertise of the management of conditions occurring in areas overlapping mental and physical health (94). CLP has developed ad hoc over the last 20 years to meet needs, and has been variably funded with or without nursing or allied health representation (95). A 2023 review of CLP in 129 Australian hospitals found that the CLP interventions were all under-resourced in relation to need (94). Development of CLP as an appropriately resourced subspecialty may build capacity among existing non-mental health workforce and contribute to better outcomes and experiences for patients and staff, and better system performance. We echo Evans et al.’s (2018) recommendation for more rigorous evaluation of CLP models in ED using standardised outcomes. Going further, we emphasise the importance of describing interventions consistently, and measuring outcomes across all four domains of system performance, patient outcomes, and patient and staff experience.
4.4 Strengths and limitations
A comprehensive search and review process was used to identify and appraise empirical studies reporting strategies to improve care delivery for adults presenting to ED with mental illness. Limitations of the current review include our pragmatic choice to only include strategies implemented within the ED itself. As such, interventions outside of the ED including clinics that connect individuals with psychosocial support (e.g., agile psychological medicine clinics (96)) were not included, though these may impact care delivery in the ED. To align with legal frameworks in Australia, interventions for people with disability such as neurocognitive impairment were not included in this review. Patient and public were not involved in this review who may have contributed valuable insights into the experiences and outcomes of interest. We also chose to only include articles published in English, omitting potentially useful reports in other languages.
Owing to the volume of references identified by the search strategies and our aim to capture measures of effectiveness, we made a pragmatic decision to only include empirical studies and not include a grey literature review, hand searching, or subject matter expert consultation. As such, implemented but unpublished interventions were not included, which may have also contributed important information. Most studies did not report clear information regarding patient characteristics and intervention details; nor were the evaluation measures comprehensive. The nature of pragmatic naturalistic study designs may also introduce bias: allocation concealment was not used in two out of three randomised controlled trial (RCT) studies, and blinding did not occur or was not possible in two studies; most studies were quasi-experimental or non-randomised studies—participants in comparisons were not always similar, or it was unclear if participants were similar in 16 of 29 (55%) studies. The hospital context may also introduce bias: the type of hospital was not reported for 18 of 46 (39%) studies, and access to psychiatric services was not reported in 21 of 46 (45%) studies; most studies were conducted in urban settings, with only 4 of 46 (8%) including a rural site. Consequently, it was not possible to identify the key elements of interventions and features of ED environments that influence strategy evaluation measures. As a result, it is unclear what interventions are successful for whom, or if interventions result in negative impacts on patient outcomes, experiences, and staff experience.
4.5 Conclusion
We identified strategies for improving ED care delivery for mental illness presentations. The strategies included models of care (e.g., ED-initiated MOUD, ED-initiated social support, and deliberate self-harm), decision support tools, discharge and transfer refinements, case management, adjustments to liaison psychiatry services, telepsychiatry, changes to roles and rostering, environmental changes (e.g., specialised units within the ED), education, new multidisciplinary teams, and standardisations of care (e.g., assessment and monitoring). No single study evaluated all four domains of system performance, patient outcomes, patient experience, and staff experience. Furthermore, many strategies fill a gap in service delivery for patients that does not align with the functional purpose of the ED. The expanded scope of care delivered by EDs puts the system under considerable strain. We need to think critically about whether care is delivered in the right place at the right time for adults with mental illness. This would include developing capacity in community services as well as appropriately resourced CLP to support the ED to fulfil its role in delivering safe and timely urgent care.
Author contributions
EA: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. CC: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. LR: Methodology, Project administration, Validation, Writing – review & editing, Conceptualization, Data curation, Investigation. LT: Conceptualization, Data curation, Investigation, Methodology, Validation, Writing – review & editing. AD: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. JL: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. AC: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. LE: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. AN: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. MM: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. KS: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. DG: Conceptualization, Data curation, Investigation, Methodology, Writing – review & editing. RC-W: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Resources, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was made possible through the Australian Government Medical Research Future Fund (2022:APP2018361).
Acknowledgments
We would like to acknowledge the MyED project partners: the Australian Institute of Health Innovation at Macquarie University, the Western Sydney Local Health District (WSLHD), the University of the Sunshine Coast, the University of New South Wales, the NSW Agency for Clinical Innovation (ACI), the Department of Social Services (DSS), the NDIS Quality and Safeguards Commission, and Health Consumers NSW. We acknowledge the Australian Government Medical Research Future Fund (2022:APP2018361) who provided us with support to establish the MyED collaborative project, and consumer and clinical representatives for their role in providing expert advice and input.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1368129/full#supplementary-material
References
1. Australian Government Productivity Commission. Mental Health (2020). Available online at: https://www.pc.gov.au/inquiries/completed/mental-health#report.
2. Lavergne MR, Shirmaleki M, Loyal JP, Jones W, Nicholls TL, Schütz CG, et al. Emergency department use for mental and substance use disorders: Descriptive analysis of population-based, linked administrative data in British Columbia, Canada. BMJ Open. (2022) 12:e057072. doi: 10.1136/bmjopen-2021-057072
3. Mérelle SYM, Boerema I, van der Linden MC, Gilissen R. Issues in emergency care for people who attempted suicide. Ned Tijdschr Geneeskd. (2018) 162:D2463.
4. Pearlmutter MD, Dwyer KH, Burke LG, Rathlev N, Maranda L, Volturo G. Analysis of emergency department length of stay for mental health patients at ten massachusetts emergency departments. Ann Emergency Med. (2017) 70:193–202.e16. doi: 10.1016/j.annemergmed.2016.10.005
5. Judkins S, Fatovich D, Ballenden N, Maher H. Mental health patients in emergency departments are suffering: the national failure and shame of the current system. A report on the Australasian College for Emergency Medicine’s Mental Health in the Emergency Department Summit. Australas Psychiatry. (2019) 27:615–7. doi: 10.1177/1039856219852282
6. Bergen C, Bortolotti L, Temple RK, Fadashe C, Lee C, Lim M, et al. Implying implausibility and undermining versus accepting peoples' experiences of suicidal ideation and self-harm in emergency department psychosocial assessments. Front Psychiatry. (2023) 14:1197512. doi: 10.3389/fpsyt.2023.1197512
7. Meehan T, Baker D, Blyth D, Stedman T. Repeat presentations to the emergency department for non-fatal suicidal behaviour: Perceptions of patients. Int J Ment Health Nursing. (2021) 30:200–7. doi: 10.1111/inm.12773
8. Cerel J, Currier GW, Conwell Y. Consumer and family experiences in the emergency department following a suicide attempt. J Psychiatr Pract. (2006) 12:341–7. doi: 10.1097/00131746-200611000-00002
9. Pawaskar R, Mahajan N, Wangoo E, Khan W, Bailey J, Vines R. Staff perceptions of the management of mental health presentations to the emergency department of a rural Australian hospital: Qualitative study. BMC Health Serv Res. (2022) 22:87. doi: 10.1186/s12913-022-07476-7
10. Morphet J, Griffiths D, Plummer V, Innes K, Fairhall R, Beattie J. At the crossroads of violence and aggression in the emergency department: Perspectives of Australian emergency nurses. Aust Health Review. (2014) 38:194–201. doi: 10.1071/AH13189
11. Ogundipe KO, Etonyeaku AC, Adigun I, Ojo EO, Aladesanmi T, Taiwo JO, et al. Violence in the emergency department: A multicentre survey of nurses’ perceptions in Nigeria. Emergency Med J. (2013) 30:758. doi: 10.1136/emermed-2012-201541
12. Australasian College for Emergency Medicine. Waiting times in the emergency department for people with acute mental and behavioural conditions (2018). Available online at: https://acem.org.au/getmedia/0857d22e-af03-40bb-8e9f-f01a2a2bf607/ACEM_Mental-Health-Access-Block.aspx.
13. Austin EE, Blakely B, Tufanaru C, Selwood A, Braithwaite J, Clay-Williams R. Strategies to measure and improve emergency department performance: A scoping review. Scandinavian J Trauma Resuscitation Emergency Med. (2020) 28:55. doi: 10.1186/s13049-020-00749-2
14. Bennewith O, Peters TJ, Hawton K, House A, Gunnell D. Factors associated with the non-assessment of self-harm patients attending an accident and emergency department: results of a national study. J Affect Disord. (2005) 89:91–7. doi: 10.1016/j.jad.2005.08.011
15. Voshaar RCO, Cooper J, Murphy E, Steeg S, Kapur N, Purandare NB. First episode of self-harm in older age: a report from the 10-year prospective Manchester Self-Harm project. J Clin Psychiatry. (2011) 72:6557. doi: 10.4088/JCP.10m06501
16. Zanus C, Battistutta S, Aliverti R, Montico M, Cremaschi S, Ronfani L, et al. Adolescent admissions to emergency departments for self-injurious thoughts and behaviors. PLoS One. (2017) 12:e0170979. doi: 10.1371/journal.pone.0170979
17. Cripps RL, Hayes JF, Pitman AL, Osborn DPJ, Werbeloff N. Characteristics and risk of repeat suicidal ideation and self-harm in patients who present to emergency departments with suicidal ideation or self-harm: A prospective cohort study. J Affect Disord. (2020) 273:358–63. doi: 10.1016/j.jad.2020.03.130
18. Suokas J, Suominen K, Lönnqvist J. Chronic alcohol problems among suicide attempters – post-mortem findings of a 14-year follow-up. Nordic J Psychiatry. (2005) 59:45–50. doi: 10.1080/08039480510018823
19. Marchesi C, Brusamonti E, Borghi C, Giannini A, Di Ruvo R, Minneo F, et al. Anxiety and depressive disorders in an emergency department ward of a general hospital: A control study. Emergency Med J. (2004) 21:175. doi: 10.1136/emj.2003.006957
20. Wang M, Wang Y, Meng N, Li X. The factors of patient-reported readiness for hospital discharge in patients with depression: A cross-sectional study. J Psychiatr Ment Health Nursing. (2021) 28:409–21. doi: 10.1111/jpm.12693
21. Hann J, Wu H, Gauri A, Dong K, Lam N, Bakal JA, et al. Identification of emergency department patients for referral to rapid-access addiction services. Can J Emergency Med. (2020) 22:170–7. doi: 10.1017/cem.2019.453
22. Somers JM, Moniruzzaman A, Currie L, Rezansoff SN, Russolillo A, Parpouchi M. Accuracy of reported service use in a cohort of people who are chronically homeless and seriously mentally ill. BMC Psychiatry. (2016) 16:41. doi: 10.1186/s12888-016-0758-0
23. Parker RD, Dykema S. The reality of homeless mobility and implications for improving care. J Community Health. (2013) 38:685–9. doi: 10.1007/s10900-013-9664-2
24. Martin RA, Couture R, Tasker N, Carter C, Copeland DM, Kibler M, et al. Emergency medical care of incarcerated patients: opportunities for improvement and cost savings. PLoS One. (2020) 15:e0232243. doi: 10.1371/journal.pone.0232243
25. Al-Khafaji K, Loy J, Kelly A-M. Characteristics and outcome of patients brought to an emergency department by police under the provisions (Section 10) of the Mental Health Act in Victoria, Australia. Int J Law Psychiatry. (2014) 37:415–9. doi: 10.1016/j.ijlp.2014.02.013
26. Fusunyan M, Dotson S, Masaki C, Macias-Konstantopoulos W, Smith F, Beach S. Sedation and intubation of agitated patients in the emergency department. J Acad Consultation-Liaison Psychiatry. (2022) 63:S107–S8. doi: 10.1016/j.jaclp.2022.03.222
27. Isenberger KM, Westgard BC, Uzpen J. Emergency department use of a restraint chair is associated with shorter restraint periods and less medication use than the use of 4-point restraints. Western J Emergency Medicine: Integrating Emergency Care Population Health. (2023) 24.
28. Kumar GS, Klein R. Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: A systematic review. J Emergency Med. (2013) 44:717–29. doi: 10.1016/j.jemermed.2012.08.035
29. Evans R, Connell J, Ablard S, Rimmer M, O'Keeffe C, Mason S. The impact of different liaison psychiatry models on the emergency department: A systematic review of the international evidence. J Psychosomatic Res. (2019) 119:53–64. doi: 10.1016/j.jpsychores.2019.01.013
30. Gabet M, Armoon B, Meng X, Fleury M-J. Effectiveness of emergency department based interventions for frequent users with mental health issues: a systematic review. Am J Emergency Med. (2023) 74:1–8. doi: 10.1016/j.ajem.2023.09.008
31. Witt KG, Hetrick SE, Rajaram G, Hazell P, Taylor Salisbury TL, Townsend E, et al. Psychosocial interventions for self-harm in adults. Cochrane Database Systematic Rev. (2021) 4). doi: 10.1002/14651858.CD013668.pub2
32. Irwin MN, Walkerly A. Role of the pharmacist in acute care interventions for opioid use disorder: A scoping review. J Am Coll Clin Pharmacy. (2022) 5:193–202. doi: 10.1002/jac5.1547
33. Johnston ANB, Spencer M, Wallis M, Kinner SA, Broadbent M, Young JT, et al. Review article: interventions for people presenting to emergency departments with a mental health problem: A systematic scoping review. Emergency Med Australasia. (2019) 31:715–29. doi: 10.1111/1742-6723.13335
34. Boulding W, Glickman SW, Manary MP, Schulman KA, Staelin R. Relationship between patient satisfaction with inpatient care and hospital readmission within 30 days. Am J Manag Care. (2011) 17:41–8.
35. Australian Institute of Health and Welfare. Mental health services provided in emergency departments (2023). Available online at: https://www.aihw.gov.au/mental-health/topic-areas/emergency-departments.
36. Anderson KN, Radhakrishnan L, Lane RI, Sheppard M, DeVies J, Azondekon R, et al. Changes and inequities in adult mental health–related emergency department visits during the COVID-19 pandemic in the US. JAMA Psychiatry. (2022) 79:475–85. doi: 10.1001/jamapsychiatry.2022.0164
37. Cheek C, Hayba N, Richardson L, Austin EE, Francis-Auton E, Safi M, et al. Experience-based codesign approach to improve care in Australian emergency departments for complex consumer cohorts: The MyED project protocol, Stages 1.1–1.3. BMJ Open. (2023) 13:e072908. doi: 10.1136/bmjopen-2023-072908
38. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surgery. (2010) 8:336–41. doi: 10.1016/j.ijsu.2010.02.007
39. Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at: www.covidence.org.
40. Tufanaru C, Munn Z, Aromataris E, Campbell J, Hopp L. Chapter 3: systematic reviews of effectiveness. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis. JBI (2020). doi: 10.46658/JBIMES-20-04
41. Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Chapter 7: Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. JBI Manual for Evidence Synthesis, vol. 5 . JBI (2020). p. 217–69. doi: 10.46658/JBIMES-20-08
42. Bogan C, Jennings L, Haynes L, Barth K, Moreland A, Oros M, et al. Implementation of emergency department–initiated buprenorphine for opioid use disorder in a rural southern state. J Subst Abuse Treat. (2020) 112:73–8. doi: 10.1016/j.jsat.2020.02.007
43. Butler K, Chavez T, Wakeman S, Robertson T, Leifer J, Barofsky J, et al. Nudging emergency department initiated addiction treatment. J Addict Med. (2022). doi: 10.1097/ADM.0000000000000926
44. Butler K, Chavez T, Wakeman S, Robertson T, Leifer J, Barofsky J, et al. Nudging Emergency Department Initiated Addiction Treatment. J Addict Med. (2023). doi: 10.1097/ADM.0000000000000926
45. Gertner AK, Roberts KE, Bowen G, Pearson BL, Jordan R. Universal screening for substance use by peer support specialists in the emergency department is a pathway to buprenorphine treatment. Addictive Behav Rep. (2021) 14:100378. doi: 10.1016/j.abrep.2021.100378
46. Kahler ZP, Musey PI, Schaffer JT, Johnson AN, Strachan CC, Shufflebarger CM. Effect of a "No Superuser Opioid Prescription" policy on ED visits and statewide opioid prescription. Western J Emergency Med. (2017) 18:894–902. doi: 10.5811/westjem.2017.6.33414
47. Lowenstein M, Perrone J, McFadden R, Xiong RA, Meisel ZF, O’Donnell N, et al. Impact of universal screening and automated clinical decision support for the treatment of opioid use disorder in emergency departments: A difference-in-differences analysis. Ann Emergency Med. (2023) 82:131–44. doi: 10.1016/j.annemergmed.2023.03.033
48. Lukacs T, Klein L, Bramante R, Logiudice J, Raio CC. Peer recovery coaches and emergency department utilization in patients with substance use disorders. Am J Emergency Med. (2023) 69:39–43. doi: 10.1016/j.ajem.2023.03.039
49. McCormack RP, Rotrosen J, Gauthier P, D’Onofrio G, Fiellin DA, Marsch LA, et al. Implementing programs to initiate buprenorphine for opioid use disorder treatment in high-need, low-resource emergency departments: A nonrandomized controlled trial. Ann Emergency Med. (2023) 82:272–87. doi: 10.1016/j.annemergmed.2023.02.013
50. McLane P, Scott K, Suleman Z, Yee K, Holroyd BR, Dong K, et al. Multi-site intervention to improve emergency department care for patients who live with opioid use disorder: A quantitative evaluation. Can J Emergency Med. (2020) 22:784–92. doi: 10.1017/cem.2020.438
51. Murphy CE, Coralic Z, Wang RC, Montoy JCC, Ramirez B, Raven MC. Extended-release naltrexone and case management for treatment of alcohol use disorder in the emergency department. Ann Emergency Med. (2023) 81:440–9. doi: 10.1016/j.annemergmed.2022.08.453
52. Solomon KT, O’Connor J, Gibbons JB, Kilaru AS, Feder KA, Xue L, et al. Association between hospital adoption of an emergency department treatment pathway for opioid use disorder and patient initiation of buprenorphine after discharge. JAMA Health Forum. (2023) 4:e230245–e. doi: 10.1001/jamahealthforum.2023.0245
53. Bryan CJ, Mintz J, Clemans TA, Burch TS, Leeson B, Williams S, et al. Effect of crisis response planning on patient mood and clinician decision making: a clinical trial with suicidal U. S. soldiers. Psychiatr Serv. (2017) 69:108–11. doi: 10.1176/appi.ps.201700157
54. Clarke T, Baker P, Watts CJ, Williams K, Feldman RA, Sherr L. Self-harm in adults: A randomised controlled trial of nurse-led case management versus routine care only. J Ment Health. (2002) 11:167–76. doi: 10.1080/09638230020023561-1
55. Inui-Yukawa M, Miyaoka H, Yamamoto K, Kamijo Y, Takai M, Yonemoto N, et al. Effectiveness of assertive case management for patients with suicidal intent. Psychiatry Res. (2021) 304:114125. doi: 10.1016/j.psychres.2021.114125
56. Kim AK, Vakkalanka JP, Van Heukelom P, Tate J, Lee S. Emergency psychiatric assessment, treatment, and healing (EmPATH) unit decreases hospital admission for patients presenting with suicidal ideation in rural America. Acad Emergency Med. (2022) 29:142–9. doi: 10.1111/acem.14374
57. Kroll DS, Stanghellini E, DesRoches SL, Lydon C, Webster A, O'Reilly M, et al. Virtual monitoring of suicide risk in the general hospital and emergency department. Gen Hosp Psychiatry. (2020) 63:33–8. doi: 10.1016/j.genhosppsych.2019.01.002
58. Lepping P, Woodworth B, Roberts L, Turner J. Increasing psychosocial assessment by introducing a self-harm pathway. Psychiatr Bulletin. (2006) 30:169–72. doi: 10.1192/pb.30.5.169
59. Morgan V, Coleman M. An evaluation of the implementation of a liaison service in an A&E department. J Psychiatr Ment Health Nursing. (2000) 7:391–7. doi: 10.1136/bmjopen-2017-016906
60. Opmeer BC, Hollingworth W, Marques EMR, Margelyte R, Gunnell D. Extending the liaison psychiatry service in a large hospital in the UK: A before and after evaluation of the economic impact and patient care following ED attendances for self-harm. BMJ Open. (2017) 7:e016906. doi: 10.1136/bmjopen-2017-016906
61. Xanthopoulou P, Ryan M, Lomas M, McCabe R. Psychosocial assessment in the emergency department: The experiences of people presenting with self-harm and suicidality. Crisis: J Crisis Intervention Suicide Prev. (2022) 43:299–306. doi: 10.1027/0227-5910/a000786
62. Adams P, Nielson H. Evidence based practice: decreasing psychiatric revisits to the emergency department. Issues Ment Health Nursing. (2012) 33:536–43. doi: 10.3109/01612840.2012.687803
63. Alexander L, Moore S, Salter N, Douglas L. Lean management in a liaison psychiatry department: implementation, benefits and pitfalls. BJPsych Bulletin. (2020) 44:18–25. doi: 10.1192/bjb.2019.64
64. Bistre M, Juven-Wetzler A, Argo D, Barash I, Katz G, Teplitz R, et al. Comparable reliability and acceptability of telepsychiatry and face-to-face psychiatric assessments in the emergency room setting. Int J Psychiatry Clin Practice. (2022) 26:228–33. doi: 10.1080/13651501.2021.1979586
65. Brainch N, Schule P, Laurel F, Bodic M, Jacob T. Psychiatric emergency services - can duty-hour changes help residents and patients? Psychiatr Q. (2018) 89:771–8. doi: 10.1007/s11126-018-9579-2
66. Braitberg G, Gerdtz M, Harding S, Pincus S, Thompson M, Knott J. Behavioural assessment unit improves outcomes for patients with complex psychosocial needs. Emergency Med Australasia. (2018) 30:353–8. doi: 10.1111/1742-6723.12905
67. Broadbent M, Jarman H, Berk M. Improving competence in emergency mental health triage. Accident Emergency Nursing. (2002) 10:155–62. doi: 10.1054/aaen.2001.0377
68. Clarke DE, Brown A-M, Hughes L, Motluk L. Education to improve the triage of mental health patients in general hospital emergency departments. Accident Emergency Nursing. (2006) 14:210–8. doi: 10.1016/j.aaen.2006.08.005
69. Eppling J. First encounters: a psychiatric emergency program. J Emergency Nursing. (2008) 34:211–7. doi: 10.1016/j.jen.2007.04.020
70. Gabet M, Grenier G, Cao Z, Fleury M-J. Implementation of three innovative interventions in a psychiatric emergency department aimed at improving service use: a mixed-method study. BMC Health Serv Res. (2020) 20:854. doi: 10.1186/s12913-020-05708-2
71. Johnsen L, Øysæd H, Børnes K, Jacob Moe T, Haavik J. A systematic intervention to improve patient information routines and satisfaction in a psychiatric emergency unit. Nordic J Psychiatry. (2007) 61:213–8. doi: 10.1080/08039480701352579
72. Lauer M, Brownstein R. Replacing the revolving door: a collaborative approach to treating individuals in crisis. J Psychosocial Nurs Ment Health Services. (2008) 46:24–32. doi: 10.3928/02793695-20080601-06
73. Maeng D, Richman JH, Lee HB, Hasselberg MJ. Impact of integrating psychiatric assessment officers via telepsychiatry on rural hospitals' emergency revisit rates. J Psychosomatic Res. (2020) 133:109997. doi: 10.1016/j.jpsychores.2020.109997
74. McCurdy JM, Haliburton JR, Yadav HC, Yoder AM, Norton LR, Froehlich JA, et al. Case study: Design may influence use of seclusion and restraint. HERD: Health Environments Res Design J. (2015) 8:116–21. doi: 10.1177/1937586715575905
75. Mitchell DA, Crawford N, Newham BJ, Newton JR. The efficacy, safety and acceptability of emergency embedded psychiatry assessment and planning units: an evaluation of Psychiatry assessment and planning units in close proximity to their associated emergency departments. Aust New Z J Psychiatry. (2020) 54:609–19. doi: 10.1177/0004867419899717
76. Okafor M, Wrenn G, Ede V, Wilson N, Custer W, Risby E, et al. Improving quality of emergency care through integration of mental health. Community Ment Health J. (2016) 52:332–42. doi: 10.1007/s10597-015-9978-x
77. Poremski D, Harris DW, Kahan D, Pauly D, Leszcz M, O'Campo P, et al. Improving continuity of care for frequent users of emergency departments: Service user and provider perspectives. Gen Hosp Psychiatry. (2016) 40:55–9. doi: 10.1016/j.genhosppsych.2016.01.004
78. Reinfeld S, Gill P, Cáceda R, Batra J. Integrating psychiatric services in the emergency room to improve patient care by using quality improvement methods. J Nervous Ment Disease. (2023) 211:438–44. doi: 10.1097/NMD.0000000000001664
79. Simpson SA, Monroe C. Implementing and evaluating a standard of care for clinical evaluations in emergency psychiatry. J Emergency Med. (2018) 55:522–9.e2. doi: 10.1016/j.jemermed.2018.07.014
80. Sinclair L, Hunter R, Hagen S, Nelson D, Hunt J. How effective are mental health nurses in A&E departments? Emergency Med J. (2006) 23:687. doi: 10.3928/02793695-20080601-06
81. Stover PR, Harpin S. Decreasing psychiatric admission wait time in the emergency department by facilitating psychiatric discharges. J Psychosocial Nurs Ment Health Services. (2015) 53:20–7. doi: 10.3928/02793695-20151020-02
82. Vakkalanka JP, Nataliansyah MM, Merchant KAS, Mack LJ, Parsons S, Mohr NM, et al. Telepsychiatry services across an emergency department network: a mixed methods study of the implementation process. Am J Emergency Med. (2022) 59:79–84. doi: 10.1016/j.ajem.2022.06.053
83. Wand T, Happell B. The mental health nurse: contributing to improved outcomes for patients in the emergency department. Accident Emergency Nursing. (2001) 9:166–76. doi: 10.1054/aaen.2000.0248
84. Wand T, Collett G, Cutten A, Stack A, Dinh M, Bein K, et al. Evaluating an emergency department-based mental health liaison nurse service: A multi-site translational research project. Emergency Med Australasia. (2021) 33:74–81. doi: 10.1111/1742-6723.13583
85. Woo BKP, Chan VT, Ghobrial N, Sevilla CC. Comparison of two models for delivery of services in psychiatric emergencies. Gen Hosp Psychiatry. (2007) 29:489–91. doi: 10.1016/j.genhosppsych.2007.07.004
86. Zeitz K, Watson D. Principles of capacity management, applied in the mental health context. Aust Health Review. (2018) 42:438–44. doi: 10.1071/AH17007
87. Zwank MD, Rupp PE, Salzman JG, Gudjonsson HP, LeFevere RC, Isenberger KM. Elimination of routine screening laboratory tests for psychiatric admission: a quality improvement initiative. Psychiatr Services. (2020) 71:1252–9. doi: 10.1176/appi.ps.202000121
88. Coles E, Anderson J, Maxwell M, Harris FM, Gray NM, Milner G, et al. The influence of contextual factors on healthcare quality improvement initiatives: A realist review. Systematic Rev. (2020) 9:94. doi: 10.1186/s13643-020-01344-3
89. Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ Br Med J. (2014) 348:g1687. doi: 10.1136/bmj.g1687
90. Quintana JM, González N, Bilbao A, Aizpuru F, Escobar A, Esteban C, et al. Predictors of patient satisfaction with hospital health care. BMC Health Serv Res. (2006) 6:102. doi: 10.1186/1472-6963-6-102
91. International Consortium for Health Outcomes Measurement. Patient-centred outcome measures USA. ICHOM (2023). Available at: https://www.ichom.org/patient-centered-outcome-measures/#MentalHealth.
92. Austin E, Blakely B, Salmon P, Braithwaite J, Clay-Williams R. Identifying constraints on everyday clinical practice: applying work domain analysis to emergency department care. Hum Factors. (2021) 64:74–98. doi: 10.1177/0018720821995668
93. Pfaff H, Braithwaite J. A parsonian approach to patient safety: transformational leadership and social capital as preconditions for clinical risk management—the GI factor. Int J Environ Res Public Health. (2020) 17:3989. doi: 10.3390/ijerph17113989
94. Flavel M-J, Holmes A, Ellen S, Khanna R. Evaluation of consultation liaison psychiatry in Australian public hospitals (AU-CLS-1). Australas Psychiatry. (2022) 31:95–8. doi: 10.1177/10398562221143930
95. Hopkins J, Sundram F, Cullum S. The multi-dimensional matrix for consultation-liaison psychiatry (mMAX-LP). Australas Psychiatry. (2019) 28:66–74. doi: 10.1177/1039856219875069
Keywords: healthcare quality, quality improvement, mental health, process re-design, equity, equality, acute care, emergency department
Citation: Austin EE, Cheek C, Richardson L, Testa L, Dominello A, Long JC, Carrigan A, Ellis LA, Norman A, Murphy M, Smith K, Gillies D and Clay-Williams R (2024) Improving emergency department care for adults presenting with mental illness: a systematic review of strategies and their impact on outcomes, experience, and performance. Front. Psychiatry 15:1368129. doi: 10.3389/fpsyt.2024.1368129
Received: 09 January 2024; Accepted: 08 February 2024;
Published: 29 February 2024.
Edited by:
Getinet Ayano, Curtin University, AustraliaReviewed by:
Liliya Gershengoren, New York University, United StatesHoward Ryland, University of Oxford, United Kingdom
Copyright © 2024 Austin, Cheek, Richardson, Testa, Dominello, Long, Carrigan, Ellis, Norman, Murphy, Smith, Gillies and Clay-Williams. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elizabeth E. Austin, RWxpemFiZXRoLmF1c3RpbkBtcS5lZHUuYXU=
 Elizabeth E. Austin
Elizabeth E. Austin Colleen Cheek
Colleen Cheek Lieke Richardson1
Lieke Richardson1 Amanda Dominello
Amanda Dominello Janet C. Long
Janet C. Long Louise A. Ellis
Louise A. Ellis Alicia Norman
Alicia Norman Robyn Clay-Williams
Robyn Clay-Williams