
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 08 March 2024
Sec. Mood Disorders
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1366191
 Annekatrin Groh1
Annekatrin Groh1 Lydia Bahlmann1,2
Lydia Bahlmann1,2 Lejla Colic1,3
Lejla Colic1,3 Alexandra Schulz4
Alexandra Schulz4 Ulrich W. Kastner5
Ulrich W. Kastner5 Udo Polzer6
Udo Polzer6 Martin Walter1,3
Martin Walter1,3 Thomas Sobanski2,4
Thomas Sobanski2,4 Gerd Wagner1,2,7*
Gerd Wagner1,2,7*Background: The COVID-19 pandemic and related restrictions may have led to increased stress, particularly in people with mental health problems. Since stress factors play important role in the emergence of suicide attempts (SA) and suicidal ideation (SI), they may have been exacerbated by the pandemic, which could have led to an increased number of suicide attempts. Thus, we first investigated whether the pandemic affected personal stress experiences and appraisal of coping potential in individuals with and without SA and SI. In a second step, we analyzed the frequency and dynamics of SAs by patients admitted to a psychiatric university clinic over a period of four years.
Methods: We examined stress experiences and appraisal of coping resources of inpatients recruited between March 2021 and February 2022 with SA (n=38), SI (n=27), and with mood disorder without SA or SI (n=45). In the second study, we investigated the time course of prospectively recorded patients with a suicide attempt (n=399) between January 1st 2018 and December 31st 2021 using interrupted time-series Poisson regression models.
Results: There was a significant main effect of group (F[2,107]=6.58, p=0.002) regarding psychological stress levels, which was significantly higher in the SA and SI groups than in the psychiatric control group. No significant differences were found in the appraisal of coping resources or in the frequency of SAs before and during pandemic. However, the pandemic had a significant impact on the seasonal pattern of SAs.
Conclusions: The pandemic increased psychological stress levels in individuals with SA and SI, which may be related to SI and do not necessarily result in SA. The pandemic did not affect the overall frequency of SA between March 2020 and December 2021, but interfered with the seasonal pattern of SA occurrence. Effective intervention strategies during a pandemic should include programs to strengthen the psychological resilience of people who are susceptible to mental health problems.
● Inpatients with suicide attempts (SA) and suicidal ideation (SI) reported similar levels of psychological distress.
● SAs and SIs reported higher psychological stress symptoms compared to psychiatric controls.
● No group differences were observed in the appraisal of coping resources.
● The frequency of SA during the pandemic did not differ from that before the pandemic.
● We found differences in the seasonality of SA during the pandemic compared to pre-pandemic.
On March 20th, 2020, the World Health Organization (WHO) declared the spread of the novel ‘Severe acute respiratory syndrome coronavirus 2’ (SARS-CoV-2) and the resulting coronavirus disease (COVID-19) a global pandemic [World Health Organization, (1)].
The pandemic and associated preventive measures increased stressors that have affected individuals and communities in different ways. One major source of stress has been uncertainty about the future, e.g., worries about individual health and about the well-being of relatives (2, 3). Social distancing measures and lockdowns (4) have led to increased loneliness and lack of social support for many people, in particular individuals with psychiatric disorders (5, 6). Furthermore, the pandemic has created additional challenges related to caregiving responsibilities (7). Thus, all of these factors have led to increased stress levels in many people around the world (8).
For example, several German cross-sectional studies with online surveys in the general population investigated the effects of pandemic-related restrictions on the extent of psychosocial stress and on mental health in the early phase of the pandemic and reported a significantly increased prevalence of psychological distress, e.g., from 39% before to 65.2% during the pandemic as well as of depressive and anxiety symptoms (6, 9, 10). Studies from other countries, e.g., the US, also reported an increase in psychological distress as a possible consequence of the pandemic itself and the preventive measures (11). It is assumed that the increase in stress experiences also leads in vulnerable people to an increase in mental health problems such as negative mood, hopelessness, anxiety, irritability or suicidal ideation (12). In a systematic review of data collected mainly in the early phase of the pandemic (between March and May 2020), Santomauro, Herrera (13) reported a 27.6% increase in the global prevalence of major depressive disorder and a 25.6% increase in anxiety disorders. As a consequence, psychiatrists and the media proclaimed at the onset of the pandemic that the global population would experience a “mental health tsunami” (14, 15). However, recent systematic reviews of a larger number of high-quality study data collected over a longer period of the pandemic showed that there was only a small increase in mental health symptoms in the general population (16–18). This means that the impact of the pandemic on mental health appears to be much more nuanced than was assumed at the beginning of the pandemic. It also appears that factors such as the appraisal of one’s own coping potential and the use of specific coping strategies have had a significant influence on mental health during the pandemic (19).
Notwithstanding, there were only few robust studies with vulnerable groups, such as people with pre-existing mental disorders or with previous suicide attempts, and it may be that some groups experience psychological distress and mental health issues differently from the general population. For example, in an Australian study individuals with mental disorders experienced higher levels of stress as a result of the pandemic than people without mental disorders (20). In that context, an especially vulnerable group in terms of experiencing stress may be individuals with a diathesis for suicidal behavior (SB) and/or suicidal ideation (SI). SB encompasses a spectrum of behaviors from suicide attempt to completed suicide. Mental disorders, in particular mood disorders, are considered a significant stress factor that significantly increases the risk of suicidal behavior (21). Previous studies reported a lifetime SA rate ranging from 19% to 50% for bipolar disorder (BD) and between 21% and 40% in MDD (22). A recent meta-analysis found a pooled estimate of suicide rate of 237.0 per 100,000 person-years for BD and 534.3 per 100,000 person-years for MDD, which is the highest suicide rate among mental disorders (23) and considerably higher than the global suicide rate of 9.0 per 100,000 inhabitants in 2019 (24).
Amplification of psychological stress due to pandemic-related factors such as social distancing, financial worries and increased worries about health and lack of adaptive coping have been discussed as possible triggers for SB, e.g., in people with mood disorders or substance use disorder (4, 25, 26). Similarly, it has also been shown that increased perceived stress during the pandemic was strongly correlated with the occurrence of suicidal ideation (27, 28). Thus, it is not clear if perceived stress, but also appraisal of coping skills during the pandemic is related to the occurrence of SB, or whether this applies more to the occurrence of SI. Even if previous epidemics (29) or socioeconomic crises (30) seems to have some influence on suicide rates, there is still too little knowledge about the factors that facilitate the transition from suicidal ideation to suicidal action (31).
Most studies on the potential triggers for SB during the Covid-19 pandemic were based on online surveys or meta-regression with extrapolation (13, 32, 33). A face-to-face interview with clinically well-characterized patients using standardized and comprehensive clinical assessment may therefore provide a more accurate evaluation of the possible interaction between SA and experienced stress during the pandemic.
One of the few studies based on structured face-to-face interview found that family problems such as marginalization, domestic violence and personal/health concerns such as fear or uncertainty were frequently cited as reasons for a suicide attempt during the Covid-19 pandemic (34). Tanaka and Okamoto (35) also described a simultaneous increase in the suicide rate and the number of calls about domestic violence in the first month of the pandemic. Following this line of reasoning, some authors have argued that the pandemic could lead to an increase in SB (36).
However, thus far, the studies on the occurrence of suicide attempts (SA) and suicides during the pandemic have been inconsistent. Studies from Germany analyzing suicide rates or the number of SA over several years have shown no significant increase in suicidal behavior in the first two years (37, 38) or even decreased number of SAs (39) in the first wave of the pandemic compared to the period before the pandemic. These results are supported by studies from Australia or Spain, for example (40–42). On the other hand, there are studies from Japan, India, Brazil, Czech Republic, and the United Kingdom that describe increased suicide rates (43–46), indicating country specific variability. In addition, in our recently published study (37), we found that the seasonal pattern of suicide attempts is significantly influenced by the pandemic.
Thus, in the present two-part mixed methods study we investigated perceived stress level, appraisal of coping skills during the pandemic and areas of life affected by the pandemic in individuals who have recently attempted suicide. We hypothesized that individuals with SA will exhibit higher level of stress and lower appraisal of coping skills due to pandemic-related factors compared to patients with a mood disorder and suicidal ideation as well as compared to patients with a mood disorder, but without SA/SI (Hypothesis #1).
In a second part of the study, we investigated the temporal course of the prospectively and systematically recorded number of suicide attempts from January 2018 to December 2021 from a large psychiatric university clinic in Jena, Germany. We hypothesized that, despite the negative results of some previous studies, the number of suicide attempts will increase during the COVID-19 pandemic and the dynamics of their occurrence will change (Hypothesis #2).
To investigate the first hypothesis, a sample of 110 adult inpatients with a recent SA or current SI or without SA/SI was recruited from March 2021 to February 2022 in the Departments of Psychiatry and Psychotherapy of Jena University Hospital and Thüringen-Kliniken “Georgius Agricola” in Saalfeld.
Inclusion criteria for the SAs were based on the Diagnostic and Statistical Manual of Mental Disorders (DSM)-5 criteria for the current suicide behavior disorder (SBD), which is one of eight conditions for further study included in Section III of the DSM-5 (47). The criteria explicitly define suicide attempt as “a self-initiated sequence of behaviors by an individual who, at the time of initiation, expected that the set of actions would lead to his or her death” (47, p. 801). Since mood disorders were the most frequently found mental disorders associated with suicidal behavior and suicidal ideation (23, 48, 49), we included only inpatients with or without suicidal ideation who also had a mood disorder. Thus, inclusion criteria for the inpatients with SI were presence of a mood disorder and current suicidal ideation but no current/past SBD. Inclusion criteria for the inpatients without SI/SA (psychiatric control group) were presence of a mood disorder, no current suicidal ideation and no current/past SBD. Exclusion criteria for all groups were acute psychosis, foreign language barriers, dementia, lack of compliance, and age <18 years. All participants consented in writing to participate in the study.
Thus, the sample included three groups of inpatients: individuals with a recent SA (n=38), individuals with a mood disorder and SI (n=27), and individuals with a mood disorder but without current SI and current or past SA (n=45). The majority of inpatients with SA (76%) have been diagnosed with a mood disorder (Table 1). Recruitment and data collection were conducted in parallel for all groups. For 5 individuals in the SA group, scores for the SI intensity were missing. The third psychiatric control group comprised individuals with a mood disorder and without current SI and current or past SBD. The local ethics committee of the Friedrich Schiller University, Jena, Germany, approved this part of the study.
Data collection involved a structured face-to-face interview, clinician- and patient-rated questionnaires, which were carried out by trained members of the study team (A.G., L.B., A.S.) under hygienic conditions. The interview included the assessment of sociodemographic data (age, gender, number of school years, family status), recording of previous and current SAs and the presence and intensity of SI, number of previous SAs, method and “intent to die” of the last SA, as well as the main diagnosis of mental disorder according to the criteria included in Chapter V(F) of the International Statistical Classification of Diseases (ICD-10). The average time between the SA and clinical interview was 31 days. The total duration of the clinical assessment was approximately 90 minutes, depending on the study participant. The data from the clinical interview are summarized in Table 1.
The intent to die, which is an important criterion for the definition of an SBD in DSM-5, was systematically evaluated in suicide attempters using the Pierce Suicide Intent Scale [SIS; (50)]. In this clinician-rated questionnaire, the objective circumstances (6 items) and the patient’s evaluation (4 items) related to the recent SA are recorded. In addition, there are two items that assess the potential lethality of SA. Each item is rated on an ordinal scale of 0, 1, or 2, with the total score ranging from 0 to 24. The higher the total score, the higher the patient’s intention to die. The questionnaire takes approx. 15 min.
The presence of suicide attempts and suicidal ideation was assessed using the clinician-rated Columbia Suicide Severity Rating Scale [C-SSRS; (51)]. C-SSRS systematically asks a series of questions about suicidal thoughts, e.g., about the desire to be dead, thoughts about the suicide method or the existence of a specific plan and their intensity. In addition, C-SSRS scale systematically assess current and past SB encompassing actual attempts and following the definition of SBD in DSM-5, but also interrupted or aborted attempts [C-SSRS; (51)]. The questionnaire takes approx. 15 min.
Symptoms of stress in the past 4 weeks related to pandemic, as explicitly stated in the instruction, were assessed by the Subclinical Stress Symptom Questionnaire [SSQ-25; (52)]. This self-report questionnaire comprises 25 items evaluating psychological and physical stress symptoms, ranging from 1 (not at all) to 5 (very intense). Psychological stress is measured by 15 questions about internal tension, nervousness, central issues and concerns (e.g., “I was easily irritated, annoyed or moody.”). Physical stress is assessed with 10 questions aimed at pain, weight changes, circulatory problems, insomnia (e.g., “I had trouble falling asleep, sleeping through or sleeping late “). SSQ-25 has good internal consistency and is suitable to differentiate different stress profiles even in samples with non-clinically significant mental health symptoms (52).
Individual appraisal of the threat posed by the pandemic and the associated measures as well as of the individual coping skills were assessed using the Primary Appraisal Secondary Appraisal (PASA) questionnaire (53). It is a 16-item self-report questionnaire specifically designed to measure cognitive appraisal processes in a stressful situation like Covid-19 pandemic (54). The two PASA subscales used in the present study measure primary appraisal, i.e., the person’s appraisal of the significance of the pandemic, e.g., as threatening, controllable or challenging and secondary appraisal, i.e., “self-concept of own competence” and “control expectancy”, which assesses coping resources available. Another PASA subscale used is the stress index, which is the difference between the values of the primary and secondary appraisal and provides a measure of stress perception. Higher score on the stress index indicates higher stress. Completing the SSQ-25 and PASA questionnaires takes about 5-10 minutes, respectively.
Individual stressful life events during the COVID-19 pandemic and their perceived stress were assessed using a structured interview in the following key life domains: Family/Partnership, Apartment, Social Life, Job, Finances, Leisure time, Health, Regeneration, and Life Perspective based on Satow (55). The patients were asked to indicate whether and, if so, which specific factors/burdens in the systematically surveyed life domains had led to an increased perception of stress during pandemic. With regard to life perspectives, for example, they were asked: “What factors have made you feel burdened in the area of life goals/life planning during the COVID-19 pandemic?” Subjects have to name these factors briefly and use the Likert scale from 1 (low) to 7 (high) provided to estimate the respective degree of stress. 11 persons of the SA group had missing values in the interview for the domains “Social Life” and “Regeneration”. This interview lasted about 20 minutes.
To investigate overall differences between the three groups in stress perceptions and appraisal of coping resources, analyses of variance (ANOVA) tests were done with the subscales of SSQ-25 and PASA questionnaires as dependent variables. To investigate the differences between the group means, post-hoc t-tests were performed, which were adjusted for multiple comparisons. For nominal variables, such as presence of stress in certain life domains, a Fisher’s exact test and for ordinal variables, a Kruskal-Wallis test were performed. Missing values were imputed with the overall mean values of the respective individual questions across all groups. Alpha threshold was set to 0.05.
This study was part of a suicide prevention project (“Network for Suicide Prevention in Thuringia”), funded by the Federal Ministry of Health (BMG). We prospectively collected unique data on adults, 18 years or older, (n=399; mean age=41.88, standard deviation (SD)=19.36; 206 (51.63%) women) admitted after a suicide attempt to the Department of Psychiatry and Psychotherapy, Jena University Hospital. The study was conducted between January 1th, 2018 and December 31th, 2021. A suicide attempt was defined based on the DSM-5 criteria for the current SBD (47). Exclusion criteria were self-harm behavior in an altered mental state such as delirium or confusion, or if the act was ideologically motivated. The current diagnosis of SBD was also clearly delineated from the ‘non-suicidal self-injury.’ Based on the above criteria, 95 participants with SA were included in the study for 2018, 107 for 2019, 111 for 2020, and 86 for 2021. Six participants were excluded because the precise date of SA was not recorded. Prospective and systematic data collection within this project was additionally retrospectively checked for completeness via the hospital’s internal documentation system.
The government introduced significant measures in Germany and Thuringia State to contain the COVID-19 pandemic with the first restrictions starting in March 2020, strongly affecting social and public life. As a result, people reduced their private contacts substantially to a minimum. We used this time point to compare the frequency and the time course of SA before (Jan, 2018 to Feb, 2020; 220 suicide attempters included) and during the COVID-19 pandemic (Mar, 2020 to Dec, 2021; 179 suicide attempters included). The local ethics committee of the Friedrich Schiller University, Jena, Germany, also approved this part of the study.
The data collection included prospectively collected sociodemographic data such as age and gender, the ICD-10 diagnosis of the concomitant psychiatric disorder, and SA-related information such as intent to die using SIS questionnaire, the date of the current suicide attempt, the current SA method, and the location of the SA.
To model changes in SA frequency before and during the COVID-19 pandemic, we applied an interrupted time-series Poisson regression model using SPSS version 29.0 (https://www.ibm.com/de-de/analytics/spss-statistics-software). We modeled the impact of the pandemic, while controlling for the seasonal pattern and trend. We explored the interaction effects between the factor pandemic and seasonal patterns and trends. For modeling both covariates, i.e. seasonal pattern and trend, the time series of suicide attempts were decomposed using the additive model as implemented in the seasonal decomposition procedure in SPSS version 29.0 (https://www.ibm.com/docs/en/spss-statistics/29.0.0?topic=forecasting-seasonal-decomposition). The smoothed trend-cycle component was used as a covariate for the Poisson regression. This method was previously used for modeling the count time series (40, 56). The alpha threshold was 0.05.
SSQ-25. As shown in Table 2, the ANOVA indicated an overall significant difference across three groups in the levels of psychological stress symptoms (F[2,107]=6.58, p=0.002; Figure 1), but not regarding levels of physical stress symptoms (F[2,107]=0.01, p=0.99; Figure 1). Post-hoc t-tests revealed that the groups with SA (t[81]=3.23, p=0.005, Bonferroni-adjusted) and SI (t[70]=2.69, p=0.02, Bonferroni-adjusted) had significantly higher level of psychological stress symptoms during the pandemic than the psychiatric control group (Table 2). Suicide attempts and suicidal ideation did not differ significantly from each other, as shown in Table 2.
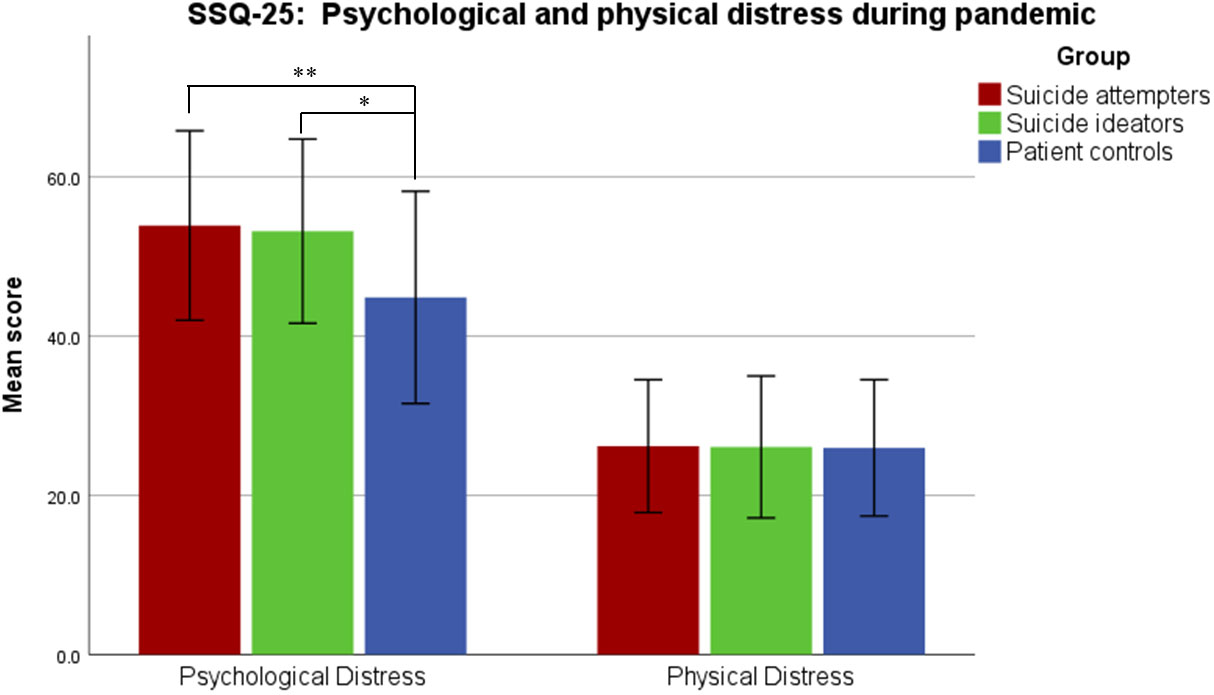
Figure 1 Psychological and physical stress symptoms experienced due to the COVID-19 pandemic, assessed with Subclinical Stress Symptom Questionnaire (SSQ-25). Error bars correspond to the first standard deviation. Patients with SA and SI reported significantly higher levels of psychological stress symptoms compared to the control patients. (*, p<0.05; **, p<0.01).
PASA. There were no group differences regarding primary appraisal of the pandemic (F[2,107]=1.18, p=0.31), secondary appraisal of coping resources (F[2,107]=1.27, p=0.28), as well as the stress index (F[2,107]=0.84, p=0.43, Table 2). Thus, regarding the primary appraisal, groups with SA and SI did not evaluate the overall pandemic situation as significantly more threatening or challenging than a psychiatric control group. In addition, all groups rated the expectation of available coping skills similarly.
The SA group was significantly more likely than the psychiatric control group to experience stress from the pandemic-related measures in the area “Family/Partnership” than psychiatric control group (Fischer’s exact test, p = .025) and on a trend level compared to the SI group (Fischer’s exact test, p = .068), see Table 2 and Figure 2. Interestingly, patient controls felt more burdened by the pandemic than patients with SA in the area of “Life Perspectives/Life Planning” (Fischer’s exact test, p = .002) (Table 2, Figure 2). The SA group was also significantly more likely than the SI group to experience stress in the area “Regeneration” (Fischer’s exact test, p = .046). No significant differences were detected in other investigated life domains when comparing the SA group to both other groups. In addition, the psychiatric control group was significantly more likely to experience stress from the pandemic-related measures in the area “Social Life” (Fischer’s exact test, p = .005) and “Regeneration” (Fischer’s exact test, p = .046) than the SI group (Table 2).
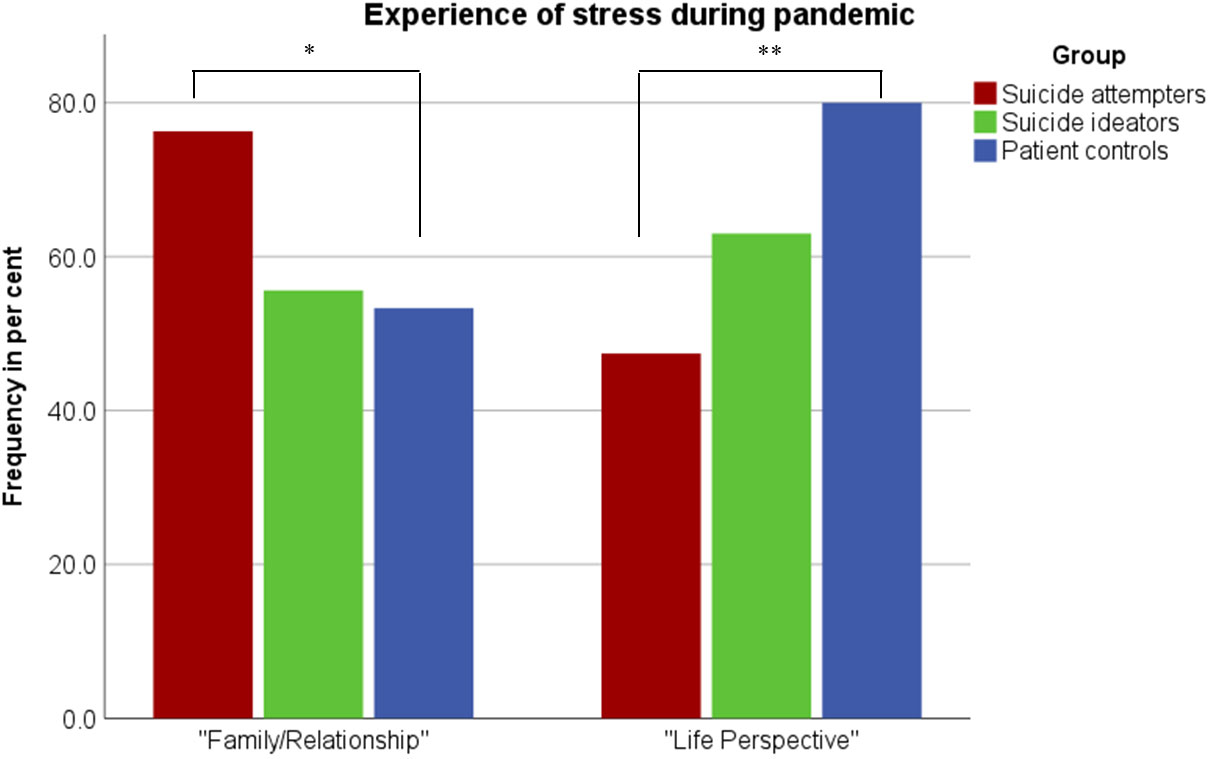
Figure 2 Frequencies of subjects reporting stress due to the COVID-19 pandemic in the domains of “family/partnership” and “life perspectives” (*, p<0.05; **, p<0.01).
The three groups did not show significant differences in the intensity of the experienced stress in the examined life domains, as the analysis with the Kruskal-Wallis-H test showed.
We did not observe a significant effect of the pandemic on the frequency of SA (Wald χ²=0.07, p=0.8). However, there was a significant interaction between the pandemic and the seasonal component (Wald χ²=15.14, p<0.001). The Goodness of Fit for the Pearson Chi-Square statistic resulted in the Value/df of 0.95 indicating no serious violation of the equidispersion. We additionally used time series modeler procedure in SPSS to predict the number of SA during the pandemic based on the pre-pandemic data. The simple seasonal model showed the best model fit of the pre-pandemic data. However, as illustrated in the Figure 3, this model did not have a good forecast (R²=0.03) for the actual numbers of SA during the pandemic, which supports the assumption of a changing seasonal pattern of SA occurrence.
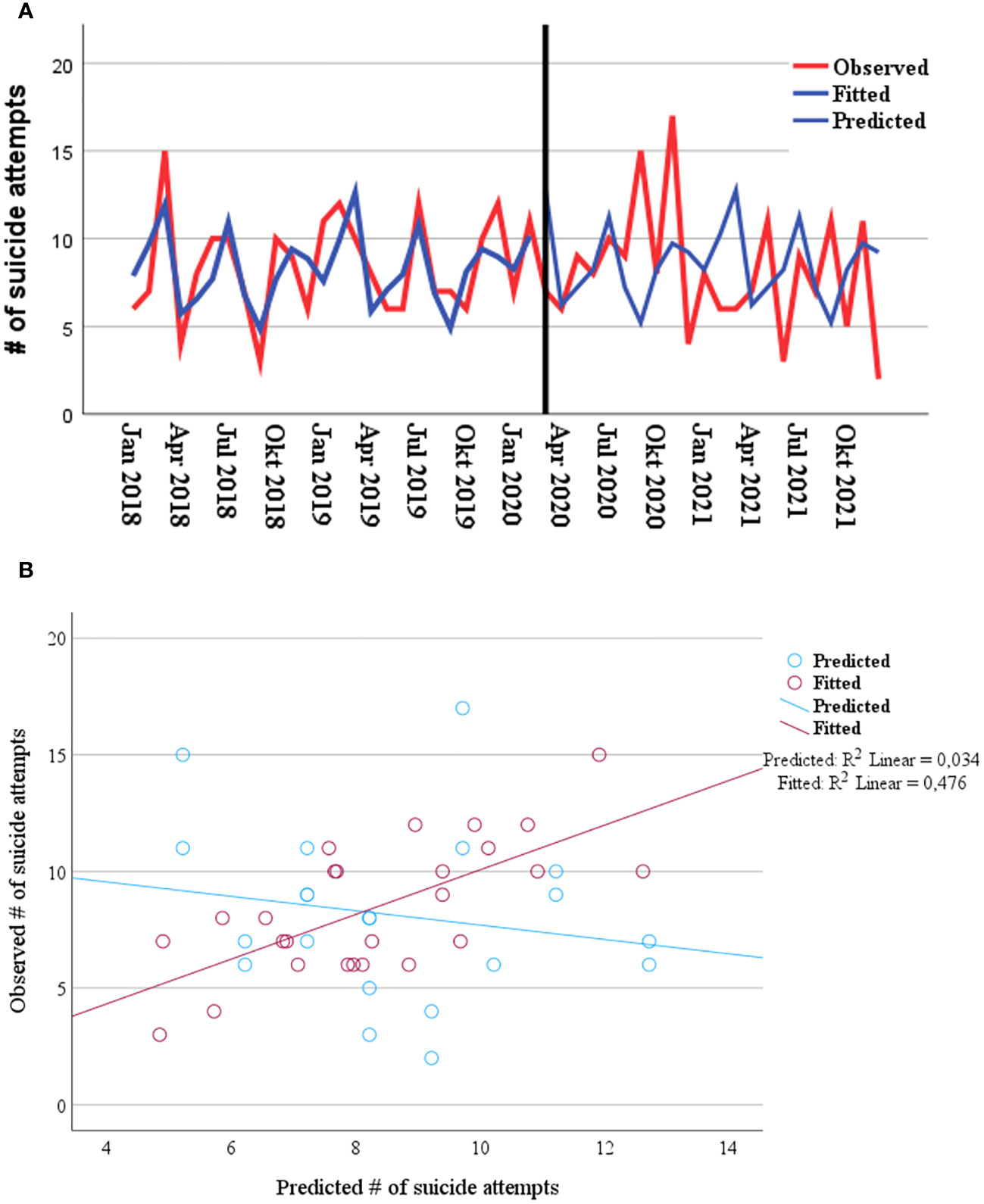
Figure 3 (A) Observed, fitted and predicted (during pandemic) values by applying simple seasonal model regarding the frequency of suicide attempts from 01 Jan 2018, until 31 Dec 2021. (B) Scatter plot and R-squared with observed data, fitted (R²=0.48) and predicted data (R²=0.03) for pre-pandemic (red dots) and pandemic (blue dots).
Since the COVID-19 outbreak in March 2020, a variety of pandemic response actions took place. The contact minimization measures may have had a tremendous impact on people’s stress experiences, especially in individuals with mental disorders, which may consequently lead to an increase in suicidal ideation and suicide attempts. However, the differences between patients with SA and SI and patients without SA/SI in terms of perceived stress and appraisal of coping resources have not yet been investigated. In addition, previous findings on the possible increase in SA frequency during pandemic have been mixed. To answer these questions, in the first study, we investigated stress experiences and appraisal of personal coping skills via in-person structural clinical interviews and validated questionnaires across well-defined psychiatric groups. We, additionally, in the second study, examined the impact of the pandemic and associated measures on the number of suicide attempts by analyzing their time course from January 2018 to December 2021 in a large psychiatric university clinic in Germany.
We observed that both inpatients with SA and SI reported higher levels of psychological stress symptoms due to the pandemic than the psychiatric control group. Given that patients with SA also experience SI, the similarly high level of psychological stress symptoms would suggest that it is related to the development of suicidal thoughts rather than behavior. In support, population surveys indicate that psychological distress is a strong correlate of SI both in the pandemic (57, 58) as well as in the pre-pandemic period (59). In addition, current theories emphasize that clinical risk factors for suicidal ideation and suicidal acts partly overlap, but also have some unique features (60–63). Indeed, SI usually precedes SA, although a recent study reported that a larger number of individuals who had recently attempted suicide denied any suicidal thoughts (64). Nonetheless, given the marked differences in the prevalence of suicide ideation compared to action, most individuals with SI will not attempt suicide (65). In other words, it is relevant to consider suicidal ideation and attempted suicide as linked but also different phenotypes. This is also the main premise of current theories of suicidal behavior, e.g. the Three Step Theory (3ST) (66) that suicidal ideation is only one component of suicide risk and by itself is unlikely to lead to SB. The 3ST emphasizes that a combination of psychological pain and hopelessness as well as disrupted feeling of connectedness is the main cause for SI, but that transition from SI to SA is only possible if the capability to do so exists (67). Such a capability could be based on previous SA or non-suicidal self-harm.
Thus, the present findings suggest that although the COVID-19 pandemic and related restrictions might be a strong psychological stressor associated with an increase in suicidal ideation, other vulnerability factors such as cognitive, psychological or neurobiological vulnerability contribute to the transition from suicidal ideation to the manifest suicidal act. A converging body of evidence suggests specific differences in the so-called “suicide capability” among attempters compared to ideators (61).
In contrast to the SSQ-25 we did not find any significant differences in the PASA questionnaire assessing threats and challenges posed by the pandemic and the appraisal of personal coping resources. One suggested explanation for this result, which may seem contradictory at first glance, is that the questions of the SSQ-25 ask for stress symptoms in the last four weeks, whereas the PASA inquiries about symptoms and coping resources for the entire duration of the pandemic period. A recency effect can therefore not be ruled out in terms that more recent short-term experiences of the pandemic were described more challenging by the individuals with SI and SA, whereas the stress and coping level for the entire pandemic period were similarly described across groups. Furthermore, due to the cross-sectional nature of our study, we cannot discern if the groups experiencing SI would generally tend to experience and report higher levels of psychological distress also in the pre-pandemic time, i.e., in the sense that this association is unspecific to the pandemic context.
When asked systematically for stressful life events in various areas of life, individuals with SA were significantly more likely to experience stress in the area of “Family/Partnership” than the psychiatric control group and at the trend level than the SI group. There is some evidence from previous studies that pandemic-related lockdowns exacerbated existing difficulties in the relationship and familial cohabitation, leading to mental health difficulties and strained family relationships (68, 69). This last factor led to the onset or further exacerbation of domestic violence for some, especially those who were already at risk before (70). In our previous study we observed that by far most common motive given for a suicide attempt, especially for suicide re-attempts, was an interpersonal conflict (71). A longitudinal study, which investigated type and number of stressful life events in a 3-year follow-up period, observed that interpersonal conflicts, but also financial problems were the most robust predictors of a suicide attempt after adjusting for several demographic and clinical parameters (72). Also, the influential Interpersonal Psychological Theory of Suicide (IPTS) emphasizes the interpersonal problems in the emergence of suicidal desire (73). Our present finding also confirms the observation of the two previous studies, from India (34) and Japan (35), which reported an association between the increase in domestic violence and suicidal behavior during pandemic.
Thus, social disconnections and the intensification of existing inequalities in relationship quality might be one proximal factor responsible for the potential association between pandemic-related stay-at-home orders and suicidal behavior in vulnerable individuals, at least in the first waves of the pandemic. This finding further indicates that the amelioration of interpersonal relationships should be viewed as a key factor in suicide prevention - be it in its universal, selective or indicated form.
Surprisingly, the psychiatric control group with a mood disorder reported to be more affected by the pandemic regarding their life perspectives, such as future career plans or vacation trips. We do not know exactly why they perceived pandemic-related restrictions on life perspectives as particularly stressful. However, one reason might be that patients with SA and SI had already reduced life perspectives or life goals which was thus not affected by the pandemic to the same extent as it was in control patients, who did not develop suicidal ideations or showed suicidal behavior.
The other areas of life did not differ significantly between the groups. However, in almost all areas of life surveyed, with the exception of “finances”, most patients in all three groups reported pandemic-related burdens (Table 2). The overall stress level reported in the questionnaires was also relatively high, indicating that people with a mood disorder, regardless of the presence of SA/SI, were similarly affected by the pandemic and the associated restrictions (74, 75). Interestingly, all three groups reported relatively high level of appraisal of coping potential, which could be due at least in part to government assistance measures during pandemic, such as financial support.
Contrary to our hypothesis, there was no significant increase in suicide attempt numbers during the pandemic compared with the pre-pandemic time. This result is consistent with studies from high and upper-middle-income countries that also found no increase in the number of suicide attempts and deaths by suicide during the pandemic (37, 42, 76). There are a number of reasons for this lack of increase in SA frequency. The widely reported increases in psychological distress and mental health problems may have indeed increased suicidal ideation, which in turn does not necessarily lead to increases in suicide attempts (21, 61). In support, previous studies have described the association between acute stress and anxiety and an increase in suicidal ideation in the general population (32, 77) but not suicide attempts. Suicidal behavior is related not only to proximal factors, such as increased experience of stress, but also to predisposing factors, such as genetic and/or neurocognitive factors (21, 31). Together with the results of the first part of our study, we may therefore speculate that the psychological distress would not directly lead to SA unless there is an already present high vulnerability, e.g., poor decision-making (78). Lastly, some studies report stable levels not only for SA but also for SI during the pandemic (75). However, it cannot be ruled out that the varying strength of the restriction measures, the different levels of state support and the cultural differences in the individual countries have a specific negative but also protective influence on people at risk of suicidal behavior (79). Future global efforts could help to identify the systemic protective factors.
In our analysis, we did observe a significant interaction between the pandemic and seasonal components, where the seasonality of the SA trends was interrupted. Before the pandemic, the highest frequency of suicide attempts was in spring and late summer. During the pandemic, on the other hand, most suicide attempts occurred in fall 2020, with the start of the second wave of the pandemic. Our previous study (37) in the same federal state (Thuringia), but in a rural area, also showed similar frequencies of suicide attempts before and during the pandemic, but significant changes in seasonality. Previous studies have shown that there are seasonal clusters in the occurrence of suicides (80, 81), but these are heterogeneous in form, amplitude, as well as in the seasonal patterns of specific subgroups and between countries (82). We speculate that the observed changes in the seasonal variation in SA may be related to limited access to suicide means due to pandemic-related measures, such as stay-at-home orders, and/or due to changes in outdoor/indoor spent time [i.e., reported effect of daily sunshine on suicide frequency (83)] and/or pandemic-related changes in personal relationships, employment status and media reporting (84). Future prospective studies should collect corroborating data for activity patterns of individuals vulnerable to SA.
To sum up, SB is a complex and multifaceted phenomenon that encompasses biological, psychological and environmental factors, which interact in such an unfavorable way that a person decides to end their life. Although the pandemic has brought with it all the putative risk factors to trigger suicidal behavior, we have not seen an increase in SA numbers over a period of almost two years of the pandemic. This means that individual risk factors that constitute “suicidal capability” are necessary for suicidal thoughts to be acted upon. Further studies in subjects with SA are therefore needed to better understand this capability.
Participation in the face-to-face interview was voluntary, making it more likely that individuals who were open about their SA or SI and experienced distress were preferentially included in the study. Individuals who did not choose to participate may thus have exhibited higher levels of distress. Moreover, the study was conducted cross-sectionally over the second to fifth wave of the pandemic, which took place from the end of September 2020 to February 2022 (85). These waves differed in their severity of contact measures and it may be that various waves were perceived as differently “dangerous.” Thus, the recorded stress levels may have differed between participants due to the different survey periods. Regarding the time series analysis, it seems conceivable that individuals received initial care in an emergency department after a suicide attempt without being referred to psychiatry for further treatment. However, this would be in contrast to the situation before the pandemic began, where it was common for almost every patient to be referred to a psychiatric clinic for further evaluation of the suicide risk. In addition, 5 subjects in the SA group had missing values for the intensity of suicidal thoughts.
In summary, we found increased pandemic-related psychological stress levels in vulnerable groups of inpatients with suicide attempt and suicidal ideation compared to a psychiatric control group, but no differences in the appraisal of coping resources. We also found that suicide attempters were more affected by the pandemic in the area of family and partnerships than the other two patient groups. These effects should be carefully investigated in further studies in order to draw final conclusions. Furthermore, the Covid-19 pandemic and its restriction measures have no direct effect on the SA frequency overall, but on the seasonal fluctuations. However, the long-term consequences of the pandemic and associated measures could have an impact on suicidal behavior in the future, as shown by a trend reversal in suicide rates in 2022 among older people in a recent study (86). It is therefore imperative to set up real-time and reliable monitoring of suicides and attempted suicides in order to implement targeted and timely measures and thus accelerate suicide prevention.
Finally, given the significance of suicidal behavior, there is undoubtedly an urgent need for the further development of effective psychosocial/psychotherapeutic therapies that have a specific focus on the prevention of suicidal behavior and on dealing with suicidal ideation. In our recent systematic review, such interventions were shown to be effective in preventing suicide re-attempts and suicide (87).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by ethics committee of the Friedrich Schiller University, Jena, Germany. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
AG: Data curation, Formal Analysis, Investigation, Writing – original draft, Writing – review and editing. LB: Data curation, Investigation, Writing – original draft, Writing – review and editing. LC: Writing – original draft, Writing – review and editing. AS: Investigation, Writing – original draft, Writing – review and editing. UK: Writing – original draft, Writing – review and editing. UP: Writing – original draft, Writing – review and editing. MW: Supervision, Writing – original draft, Writing – review and editing. TS: Project administration, Supervision, Writing – original draft, Writing – review and editing. GW: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Supervision, Writing – original draft.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The present work was supported by a research grant from the Bundesministerium für Gesundheit to GW (BMG; Federal Ministry of Health, ZMVI1-2517FSB143).The present work was supported by the Interdisciplinary Center of Clinical Research of the Medical Faculty Jena (LC). We acknowledge support by the German Research Foundation Projekt-Nr. 512648189 and the Open Access Publication Fund of the Thueringer Universitaets- und Landesbibliothek Jena. Funding sources had no role in the study design, data collection, analysis, and interpretation, the writing of the report, and the decision to submit the article for publication.
We thank our participants for their participation in our studies.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Organization WH. Listings of WHO´s response to COVID-19 2020, June 29. Available online at: https://www.who.int/news/item/29-06-2020-covidtimeline.
2. Ahmed F, Sifat RI. Strategic assessment of mental health and suicide amid COVID-19 pandemic in Bangladesh. Int J Health Plann Manage. (2021) 36:980–5. doi: 10.1002/hpm.3121
3. Almaghrebi AH. Risk factors for attempting suicide during the COVID-19 lockdown: Identification of the high-risk groups. J Taibah Univ Med Sci. (2021) 16:605–11. doi: 10.1016/j.jtumed.2021.04.010
4. Ganesan B, Al-Jumaily A, Fong KNK, Prasad P, Meena SK, Tong RK. Impact of coronavirus disease 2019 (COVID-19) outbreak quarantine, isolation, and lockdown policies on mental health and suicide. Front Psychiatry. (2021) 12:565190. doi: 10.3389/fpsyt.2021.565190
5. Banerjee D, Rai M. Social isolation in Covid-19: The impact of loneliness. Int J Soc Psychiatry. (2020) 66:525–7. doi: 10.1177/0020764020922269
6. Benke C, Autenrieth LK, Asselmann E, Pane-Farre CA. Lockdown, quarantine measures, and social distancing: Associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. (2020) 293:113462. doi: 10.1016/j.psychres.2020.113462
7. Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. Am Psychol. (2020) 75:631–43. doi: 10.1037/amp0000660
8. Wiegelmann H, Hess M, Domhoff D, Heinze F, Schmidt A, Seibert K, et al. [The situation of informal caregivers of working age in the COVID-19 pandemic-results of an online survey in Germany]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. (2023) 66:265–74. doi: 10.1007/s00103-023-03659-7
9. Wechsler TF, Schmidmeier M, Biehl S, Gerczuk J, Guerrero-Cerda FM, Muhlberger A. Individual changes in stress, depression, anxiety, pathological worry, posttraumatic stress, and health anxiety from before to during the COVID-19 pandemic in adults from Southeastern Germany. BMC Psychiatry. (2022) 22:528. doi: 10.1186/s12888-022-04148-y
10. Bauerle A, Teufel M, Musche V, Weismuller B, Kohler H, Hetkamp M, et al. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J Public Health (Oxf). (2020) 42:672–8. doi: 10.1093/pubmed/fdaa106
11. Tull MT, Edmonds KA, Scamaldo KM, Richmond JR, Rose JP, Gratz KL. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res. (2020) 289:113098. doi: 10.1016/j.psychres.2020.113098
12. Troisi A. Social stress and psychiatric disorders: Evolutionary reflections on debated questions. Neurosci Biobehav Rev. (2020) 116:461–9. doi: 10.1016/j.neubiorev.2020.07.016
13. Santomauro DF, Herrera AMM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. (2021) 398:1700–12. doi: 10.1016/S0140-6736(21)02143-7
14. Roxby P. Psychiatrists fear “tsunami” of mental illness after lockdown. United Kingdom: BBC News (2020).
15. Holmes EA, O’Connor RC, Perry VH, Tracey I, Wessely S, Arseneault L, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. (2020) 7:547–60. doi: 10.1016/S2215-0366(20)30168-1
16. Kunzler AM, Lindner S, Rothke N, SchSfer SK, Metzendorf MI, Sachkova A, et al. Mental health impact of early stages of the COVID-19 pandemic on individuals with pre-existing mental disorders: A systematic review of longitudinal research. Int J Env Res Pub He. (2023) 20. doi: 10.3390/ijerph20020948
17. Salanti G, Peter N, Tonia T, Holloway A, White IR, Darwish L, et al. The impact of the COVID-19 pandemic and associated control measures on the mental health of the general population: A systematic review and dose-response meta-analysis. Ann Intern Med. (2022) 175:1560–71. doi: 10.7326/M22-1507
18. Sun Y, Wu Y, Fan SQ, Dal Santo T, Li LT, Jiang XW, et al. Comparison of mental health symptoms before and during the covid-19 pandemic: evidence from a systematic review and meta-analysis of 134 cohorts. Bmj-Brit Med J. (2023) 380. doi: 10.1136/bmj-2022-074224
19. Kirby LD, Qian W, Adiguzel Z, Afshar Jahanshahi A, Bakracheva M, Orejarena Ballestas MC, et al. Appraisal and coping predict health and well-being during the COVID-19 pandemic: An international approach. Int J Psychol. (2022) 57:49–62. doi: 10.1002/ijop.12770
20. Newby JM, O’Moore K, Tang S, Christensen H, Faasse K. Acute mental health responses during the COVID-19 pandemic in Australia. PloS One. (2020) 15:e0236562. doi: 10.1371/journal.pone.0236562
21. Mann JJ, Rizk MM. A brain-centric model of suicidal behavior. Am J Psychiatry. (2020) 177:902–16. doi: 10.1176/appi.ajp.2020.20081224
22. Xu YE, Barron DA, Sudol K, Zisook S, Oquendo MA. Suicidal behavior across a broad range of psychiatric disorders. Mol Psychiatry. (2023) 28:2764–810. doi: 10.1038/s41380-022-01935-7
23. Fu XL, Qian Y, Jin XH, Yu HR, Wu H, Du L, et al. Suicide rates among people with serious mental illness: a systematic review and meta-analysis. Psychol Med. (2023) 53:351–61. doi: 10.1017/S0033291721001549
24. WHO. Suicide in the worldwide 2019: Global Health Estimates. (2021).World Health Organization, United Nation, Suicide in the worldwide 2019:Genf, Switzerland: Global Health Estimates.
25. Berardelli I, Sarubbi S, Rogante E, Cifrodelli M, Erbuto D, Innamorati M, et al. The impact of the COVID-19 pandemic on suicide ideation and suicide attempts in a sample of psychiatric inpatients. Psychiatry Res. (2021) 303:114072. doi: 10.1016/j.psychres.2021.114072
26. Yip PS, Cheung YT, Chau PH, Law YW. The impact of epidemic outbreak: the case of severe acute respiratory syndrome (SARS) and suicide among older adults in Hong Kong. Crisis. (2010) 31:86–92. doi: 10.1027/0227-5910/a000015
27. Okubo R, Yoshioka T, Nakaya T, Hanibuchi T, Okano H, Ikezawa S, et al. Urbanization level and neighborhood deprivation, not COVID-19 case numbers by residence area, are associated with severe psychological distress and new-onset suicidal ideation during the COVID-19 pandemic. J Affect Disord. (2021) 287:89–95. doi: 10.1016/j.jad.2021.03.028
28. Tasnim R, Islam MS, Sujan MSH, Sikder MT, Potenza MN. Suicidal ideation among Bangladeshi university students early during the COVID-19 pandemic: Prevalence estimates and correlates. Child Youth Serv Rev. (2020) 119. doi: 10.1016/j.childyouth.2020.105703
29. Chan SM, Chiu FK, Lam CW, Leung PY, Conwell Y. Elderly suicide and the 2003 SARS epidemic in Hong Kong. Int J Geriatr Psychiatry. (2006) 21:113–8. doi: 10.1002/(ISSN)1099-1166
30. Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. Effects of the 2008 recession on health: a first look at European data. Lancet. (2011) 378:124–5. doi: 10.1016/S0140-6736(11)61079-9
31. Sobanski T, Peikert G, Kastner UW, Wagner G. Suicidal behavior-advances in clinical and neurobiological research and improvement of prevention strategies. World J Psychiatry. (2022) 12:1115–26. doi: 10.5498/wjp.v12.i9.1115
32. Ammerman BA, Burke TA, Jacobucci R, McClure K. Preliminary investigation of the association between COVID-19 and suicidal thoughts and behaviors in the U.S. J Psychiatr Res. (2021) 134:32–8. doi: 10.1016/j.jpsychires.2020.12.037
33. Kasal A, Kuklova M, Kagstrom A, Winkler P, Formanek T. Suicide risk in individuals with and without mental disorders before and during the COVID-19 pandemic: an analysis of three nationwide cross-sectional surveys in Czechia. Arch Suicide Res. (2023) 27:671–85. doi: 10.1080/13811118.2022.2051653
34. Prabhakar K, Aswathanarayana A, Kumar Reddy KH. Reasons for suicide attempts in south India during the COVID-19 pandemic. Clin Med Res. (2022) 20:34–9. doi: 10.3121/cmr.2022.1704
35. Tanaka T, Okamoto S. Increase in suicide following an initial decline during the COVID-19 pandemic in Japan. Nat Hum Behav. (2021) 5:229–38. doi: 10.1038/s41562-020-01042-z
36. Fountoulakis KN, Karakatsoulis G, Abraham S, Adorjan K, Ahmed HU, Alarcon RD, et al. Results of the COVID-19 mental health international for the general population (COMET-G) study. Eur Neuropsychopharmacol. (2022) 54:21–40. doi: 10.1016/j.euroneuro.2021.10.004
37. Kastner UW, Javaheripour N, Arand J, Schonherr D, Sobanski T, Fehler SW, et al. Effects of the COVID-19 pandemic on suicide attempts in a rural region in Germany, a 5-year observational study. J Affect Disord. (2022) 318:393–9. doi: 10.1016/j.jad.2022.09.022
38. Radeloff D, Genuneit J, Bachmann CJ. Suicides in Germany during the COVID-19 pandemic. Dtsch Arztebl Int. (2022) 119:502–3. doi: 10.3238/arztebl.m2022.0198
39. Reif-Leonhard C, Lemke D, Holz F, Ahrens KF, Fehr C, Steffens M, et al. Changes in the pattern of suicides and suicide attempt admissions in relation to the COVID-19 pandemic. Eur Arch Psychiatry Clin Neurosci. (2023) 273:357–65. doi: 10.1007/s00406-022-01448-y
40. Leske S, Kolves K, Crompton D, Arensman E, de Leo D. Real-time suicide mortality data from police reports in Queensland, Australia, during the COVID-19 pandemic: an interrupted time-series analysis. Lancet Psychiatry. (2021) 8:58–63. doi: 10.1016/S2215-0366(20)30435-1
41. Perez V, Elices M, Vilagut G, Vieta E, Blanch J, Laborda-Serrano E, et al. Suicide-related thoughts and behavior and suicide death trends during the COVID-19 in the general population of Catalonia, Spain. Eur Neuropsychopharmacol. (2022) 56:4–12. doi: 10.1016/j.euroneuro.2021.11.006
42. Pirkis J, John A, Shin S, DelPozo-Banos M, Arya V, Analuisa-Aguilar P, et al. Suicide trends in the early months of the COVID-19 pandemic: an interrupted time-series analysis of preliminary data from 21 countries. Lancet Psychiatry. (2021) 8:579–88. doi: 10.1016/S2215-0366(21)00091-2
43. Acharya B, Subedi K, Acharya P, Ghimire S. Association between COVID-19 pandemic and the suicide rates in Nepal. PloS One. (2022) 17:e0262958. doi: 10.1371/journal.pone.0262958
44. Kasal A, Kuklova M, Kagstrom A, Winkler P, Formanek T. Suicide risk in individuals with and without mental disorders before and during the COVID-19 pandemic: an analysis of three nationwide cross-sectional surveys in Czechia. Arch Suicide Res. (2022), 1–15. doi: 10.1080/13811118.2022.2051653
45. Liem A, Prawira B, Magdalena S, Siandita MJ, Hudiyana J. Predicting self-harm and suicide ideation during the COVID-19 pandemic in Indonesia: a nationwide survey report. BMC Psychiatry. (2022) 22:304. doi: 10.1186/s12888-022-03944-w
46. Sakamoto H, Ishikane M, Ghaznavi C, Ueda P. Assessment of suicide in Japan during the COVID-19 pandemic vs previous years. JAMA Netw Open. (2021) 4:e2037378. doi: 10.1001/jamanetworkopen.2020.37378
47. APA. Diagnostic and Statistical Manual of Mental Disorders (DSM-5). Washington, DC: American Psychiatric Association (2013).
48. Bertolote JM, Fleischmann A. Suicide and psychiatric diagnosis: a worldwide perspective. World Psychiatry. (2002) 1:181–5.
49. Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, et al. Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychol Bull. (2017) 143:187–232. doi: 10.1037/bul0000084
50. Pierce DW. The predictive validation of a suicide intent scale: a five year follow-up. Br J Psychiatry. (1981) 139:391–6. doi: 10.1192/bjp.139.5.391
51. Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. (2011) 168:1266–77. doi: 10.1176/appi.ajp.2011.10111704
52. Helms E, Wetzel E, Weierstall R. [Development and validation of the subclinical stress symptom questionnaire SSQ-25]. Nervenarzt. (2017) 88:1050–7. doi: 10.1007/s00115-016-0181-2
53. Gaab J. PASA-Primary Appraisal Secondary Appraisal - Ein Fragebogen zur Erfassung von situationsbezogenen kognitiven Bewertungen. Karger. (2009), 114–5. doi: 10.1159/000223610
54. Carpenter R. A review of instruments on cognitive appraisal of stress. Arch Psychiatr Nurs. (2016) 30:271–9. doi: 10.1016/j.apnu.2015.07.002
55. Satow L. Stress- und Coping-Inventar (SCI): Test- und Skalendokumentation. Available online at: http://www.drsatow.de2012.
56. Islam N, Sharp SJ, Chowell G, Shabnam S, Kawachi I, Lacey B, et al. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. (2020) 370:m2743. doi: 10.1136/bmj.m2743
57. Shi L, Que JY, Lu ZA, Gong YM, Liu L, Wang YH, et al. Prevalence and correlates of suicidal ideation among the general population in China during the COVID-19 pandemic. Eur Psychiatry. (2021) 64:e18. doi: 10.1192/j.eurpsy.2021.5
58. Ide K, Asami T, Suda A, Yoshimi A, Fujita J, Shiraishi Y, et al. The psychological distress and suicide-related ideation in hospital workers during the COVID-19 pandemic: Second results from repeated cross-sectional surveys. PloS One. (2022) 17:e0277174. doi: 10.1371/journal.pone.0277174
59. Eskin M, Sun JM, Abuidhail J, Yoshimasu K, Kujan O, Janghorbani M, et al. Suicidal behavior and psychological distress in university students: A 12-nation study. Arch Suicide Res. (2016) 20:369–88. doi: 10.1080/13811118.2015.1054055
60. Klonsky ED, May AM. Differentiating suicide attempters from suicide ideators: a critical frontier for suicidology research. Suicide Life Threat Behav. (2014) 44:1–5. doi: 10.1111/sltb.12068
61. Klonsky ED, Qiu T, Saffer BY. Recent advances in differentiating suicide attempters from suicide ideators. Curr Opin Psychiatry. (2017) 30:15–20. doi: 10.1097/YCO.0000000000000294
62. Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: results from the National Comorbidity Survey Replication. Mol Psychiatry. (2010) 15:868–76. doi: 10.1038/mp.2009.29
63. Nock MK, Millner AJ, Joiner TE, Gutierrez PM, Han G, Hwang I, et al. Risk factors for the transition from suicide ideation to suicide attempt: Results from the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). J Abnormal Psychol. (2018) 127:139–49. doi: 10.1037/abn0000317
64. Wastler HM, Bryan AO, Bryan CJ. Suicide attempts among adults denying active suicidal ideation: An examination of the relationship between suicidal thought content and suicidal behavior. J Clin Psychol. (2022) 78:1103–17. doi: 10.1002/jclp.23268
65. Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. (2008) 192:98–105. doi: 10.1192/bjp.bp.107.040113
66. Tsai M, Lari H, Saffy S, Klonsky ED. Examining the three-step theory (3ST) of suicide in a prospective study of adult psychiatric inpatients. Behav Ther. (2021) 52:673–85. doi: 10.1016/j.beth.2020.08.007
67. Klonsky ED, Dixon-Luinenburg T, May AM. The critical distinction between suicidal ideation and suicide attempts. World Psychiatry. (2021) 20:439–41. doi: 10.1002/wps.20909
68. Evans S, Mikocka-Walus A, Klas A, Olive L, Sciberras E, Karantzas G, et al. From “It has stopped our lives” to “Spending more time together has strengthened bonds”: the varied experiences of Australian families during COVID-19. Front Psychol. (2020) 11:588667. doi: 10.3389/fpsyg.2020.588667
69. Long E, Patterson S, Maxwell K, Blake C, Boso Perez R, Lewis R, et al. COVID-19 pandemic and its impact on social relationships and health. J Epidemiol Community Health. (2022) 76:128–32. doi: 10.1136/jech-2021-216690
70. McNeil A, Hicks L, Yalcinoz-Ucan B, Browne DT. Prevalence & Correlates of intimate partner violence during COVID-19: A rapid review. J Fam Violence. (2023) 38:241–61. doi: 10.1007/s10896-022-00386-6
71. Lübbert M, Bahlmann L, Josfeld S, Bürger J, Schulz A, Bär K-J, et al. Identifying distinguishable clinical profiles between single suicide attempters and re-attempters. Front Psychiatry. (2021). doi: 10.3389/fpsyt.2021.754402
72. Wang Y, Sareen J, Afifi TO, Bolton SL, Johnson EA, Bolton JM. A population-based longitudinal study of recent stressful life events as risk factors for suicidal behavior in major depressive disorder. Arch Suicide Res. (2015) 19:202–17. doi: 10.1080/13811118.2014.957448
73. Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The interpersonal theory of suicide. psychol Rev. (2010) 117:575–600. doi: 10.1037/a0018697
74. Sole B, Verdolini N, Amoretti S, Montejo L, Rosa AR, Hogg B, et al. Effects of the COVID-19 pandemic and lockdown in Spain: comparison between community controls and patients with a psychiatric disorder. Preliminary results from the BRIS-MHC STUDY. J Affect Disord. (2021) 281:13–23. doi: 10.1016/j.jad.2020.11.099
75. Oppenauer C, Burghardt J, Kaiser E, Riffer F, Sprung M. Psychological distress during the COVID-19 pandemic in patients with mental or physical diseases. Front Psychol. (2021) 12:703488. doi: 10.3389/fpsyg.2021.703488
76. Radeloff D, Papsdorf R, Uhlig K, Vasilache A, Putnam K, von Klitzing K. Trends in suicide rates during the COVID-19 pandemic restrictions in a major German city. Epidemiol Psychiatr Sci. (2021) 30:e16. doi: 10.1017/S2045796021000019
77. Killgore WDS, Cloonan SA, Taylor EC, Allbright MC, Dailey NS. Trends in suicidal ideation over the first three months of COVID-19 lockdowns. Psychiatry Res. (2020) 293:113390. doi: 10.1016/j.psychres.2020.113390
78. Jollant F, Bellivier F, Leboyer M, Astruc B, Torres S, Verdier R, et al. Impaired decision making in suicide attempters. Am J Psychiatry. (2005) 162:304–10. doi: 10.1176/appi.ajp.162.2.304
79. Nochaiwong S, Ruengorn C, Thavorn K, Hutton B, Awiphan R, Phosuya C, et al. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: a systematic review and meta-analysis. Sci Rep-Uk. (2021) 11. doi: 10.1038/s41598-021-89700-8
80. Christodoulou C, Douzenis A, Papadopoulos FC, Papadopoulou A, Bouras G, Gournellis R, et al. Suicide and seasonality. Acta Psychiatr Scand. (2012) 125:127–46. doi: 10.1111/j.1600-0447.2011.01750.x
81. Coimbra DG, Pereira ESAC, de Sousa-Rodrigues CF, Barbosa FT, de Siqueira Figueredo D, Araujo Santos JL, et al. Do suicide attempts occur more frequently in the spring too? A systematic review and rhythmic analysis. J Affect Disord. (2016) 196:125–37. doi: 10.1016/j.jad.2016.02.036
82. Yu J, Yang D, Kim Y, Hashizume M, Gasparrini A, Armstrong B, et al. Seasonality of suicide: a multi-country multi-community observational study. Epidemiol Psychiatr Sci. (2020) 29:e163. doi: 10.1017/S2045796020000748
83. Vyssoki B, Kapusta ND, Praschak-Rieder N, Dorffner G, Willeit M. Direct effect of sunshine on suicide. JAMA Psychiatry. (2014) 71:1231. doi: 10.1001/jamapsychiatry.2014.1198
84. Clapperton A, Spittal MJ, Dwyer J, Garrett A, Kolves K, Leske S, et al. Patterns of suicide in the context of COVID-19: evidence from three Australian states. Front Psychiatry. (2021) 12:797601. doi: 10.3389/fpsyt.2021.797601
85. Robert-Koch-Institut. Epidemiologisches Bulletin. Robert-Koch-Institut. Berlin, Germany: Epidemiologisches Bulletin. (2022).
86. Radeloff D, Papsdorf R, White L, Genuneit J. Suicide trends in Germany during the COVID-19 pandemic and the war in Ukraine. Psychiat Res. (2023) 330. doi: 10.1016/j.psychres.2023.115555
Keywords: suicide, suicide attempts, suicidal ideation, COVID-19, interrupted time series analysis, psychological stress, coping resources, mental health
Citation: Groh A, Bahlmann L, Colic L, Schulz A, Kastner UW, Polzer U, Walter M, Sobanski T and Wagner G (2024) Psychological distress among individuals with a suicide attempt or suicidal ideation and suicide attempts patterns: first two years of the pandemic. Front. Psychiatry 15:1366191. doi: 10.3389/fpsyt.2024.1366191
Received: 05 January 2024; Accepted: 21 February 2024;
Published: 08 March 2024.
Edited by:
Tasuku Hashimoto, International University of Health and Welfare (IUHW), JapanReviewed by:
Claudia Oppenauer, Karl Landsteiner University of Health Sciences, AustriaCopyright © 2024 Groh, Bahlmann, Colic, Schulz, Kastner, Polzer, Walter, Sobanski and Wagner. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gerd Wagner, d2FnbmVyLmdlcmRAdW5pLWplbmEuZGU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.