
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry , 30 May 2024
Sec. Sleep Disorders
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1365463
 Afework Edmealem1*
Afework Edmealem1* Belachew Tegegne2
Belachew Tegegne2 Girma Alem3
Girma Alem3 Haymanot Zeleke1
Haymanot Zeleke1 Temesgen Ayenew1
Temesgen Ayenew1 Setarg Ayenew1
Setarg Ayenew1 Ayenew Sisay Gebeyew3
Ayenew Sisay Gebeyew3 Bereket Tomiso4
Bereket Tomiso4 Abuneh Getahun5
Abuneh Getahun5 Tirusew Wondie1
Tirusew Wondie1 Tiliksew Liknaw1
Tiliksew Liknaw1Background: Poor sleep quality impedes the progression of chronic illnesses, while chronic illnesses themselves are caused by poor sleep quality. Despite this fact, there is no research that has been conducted in Ethiopia that provides a thorough estimate of the self-reported sleep quality among patients with chronic illnesses. In order to present a complete picture of poor sleep quality among diabetes, hypertension, heart failure, cancer, HIV/AIDS and epilepsy patients, this systematic review and meta-analysis was carried out.
Methods: Systematic review and meta-analysis was conducted to estimate the quality of sleep among patients with chronic illness in Ethiopia. The Preferred Reporting Items for Systematic Review and Meta Analysis standard was followed in the reporting of this systematic review and meta-analysis. An extensive exploration of digital repositories, including PubMed, EMBASE, Cochrane, Africa Journal of Online, Google Scholar, and an advanced Google search, was conducted to obtain published studies until December 1st, 2023 detailing poor sleep quality of patients with chronic illness. STATA version 17 commands were used to create the pooled estimate. The I2 test and Egger’s test, respectively, were used to identify the presence of heterogeneity and publication bias. To manage heterogeneity, a subgroup analysis and random effect model were used.
Results: A total 21 articles with a total of 7393 participants were included in the final systematic review and meta-analysis. The pooled estimate of poor sleep quality among patients with chronic illness was 52% (95% of CI: 48%, 59%; I2 = 97.26%). In subgroup analysis, the highest pooled estimate of poor sleep quality was observed in cancer patients 63% (95% CI: (95% CI: 45% - 80%). Regarding to data collection period, the highest pooled estimate of poor sleep quality was seen during spring 68% (95% CI: 42% - 94%).
Conclusions: Patients with chronic illnesses in Ethiopia had a high pooled estimate of poor sleep quality. Patients with cancer had the highest pooled estimate of poor-quality sleep compared with other patients. Patients with chronic illnesses had trouble sleeping in the spring, according to this systematic review and meta-analysis. Therefore, attention and intervention should be given to enhance the quality of sleep for patients with chronic illnesses.
Sleep is one of the most important aspects of life, as one-third of our lives are dedicated to sleep (1). It is vital to everyone’s life because it helps people unwind, revitalize their bodies, minds, and emotions, mend their physical bodies to enhance and preserve overall health, solidify their learning and memory, and refuel psychologically to preserve emotional equilibrium and well-being (1–3). The importance of maintaining adequate sleep quality and quantity has relevance beyond reducing healthcare spending, improving morale, and improving productivity (4). In terms of preserving general health, sleep is just as crucial as diet or exercise (3). Poor sleep quality has been linked to a lower chance of living a longer life (5), along with other risk factors such obesity and weight gain, high blood pressure, high cholesterol, diabetes, atherosclerosis, poor mental health, alcoholism, smoking, bad eating habits, and sedentary behavior (6–8). Additionally, sleep plays a significant role in brain activities that are critical for work, such as decision-making, attentiveness, and drowsiness (9).
Chronic illness patients face several challenges. The primary complaint among them is sleep disorders (10). Sleep problems included inadequate sleep duration, insomnia, snoring, poor sleep quality, obstructive sleep apnea and restless legs syndrome (1, 11). Patients with chronic illnesses have been shown in studies to go years without getting enough sleep (12) which impaired their quality of life (13). Poor sleep quality impedes the progression of chronic illnesses, while chronic illnesses themselves are caused by poor sleep quality (14). For instance, a comprehensive review found that individuals living with HIV/AIDS are at risk to develop poor sleep quality (15). The hypothalamic-pituitary-adrenal axis, disturbed circadian rhythms, proinflammatory reactions, elevated sympathetic nervous system activity, and metabolic impacts are some of the mechanisms behind the multifaceted relationship between poor sleep quality and chronic illness (2, 16).
Poor sleep quality has become an increasing public health problem in modern society, and there is a high correlation between poor sleep quality and the development of late-chronic diseases (2). The magnitude of poor sleep quality is high among patients with chronic illnesses. A systematic review of 20 studies among patients with chronic kidney diseases showed that the prevalence of poor sleep quality was 11% to 97% (17). Another systematic review of 24 studies among hypertension patients in China revealed that poor sleep quality ranges from 14.9% to 85.7% (18). Furthermore, the prevalence of poor sleep quality among cancer patients ranges from 16% to 93% (19).
Poor sleep quality has a negative effect on self-rated health or one’s perception of his or her health (20), life expectancy (5), quality of life (13), impaired immune system, hampered physical performance, affected cell growth and repair, deteriorated neuronal connections and neuronal malfunctions (9), deleterious health consequences, including an increased risk of hypertension, diabetes, atherosclerosis, obesity, depression, heart attack, and stroke (8, 10), results in vehicle and fall accidents (9), high health care expenditure (10), absenteeism from the workplace, presenteeism/productivity loss (2, 10), and in general, it increases the disease burden (3). The impact of poor sleep quality on the patients’ quality of life is much in African population due to the rapid increment of aging population and chronic disease conditions.
Beyond reducing health care costs, sleep intervention has relevance to improving morale and productivity (21). Studying the prevalence of poor sleep quality at the national level warrants health care providers and policymakers to give more attention and prepare themselves for intervention. The quality of sleep among Ethiopian patients with cancer, HIV/AIDS, diabetes, heart failure, hypertension, and epilepsy is not consistent. Moreover, no research has been conducted in Ethiopia that provides a thorough estimate of the pooled prevalence of poor sleep quality among patients with chronic illnesses. In order to present a complete picture of poor sleep quality among Ethiopian patients with chronic illnesses, this systematic review and meta-analysis was carried out.
Systematic review and meta-analysis of both published articles conducted in Ethiopia to estimate the quality of sleep among patients with chronic illness. Ethiopia is one the developing country in East part of Africa. It has 13 regions and 2 city administrations. The regions are Tigray, Afar, Amhara, Oromo, Ethiosomali, Benshangul gumz, Central Ethiopia, Sidama, South West Ethiopia, South Ethiopia, Gambela, and Hareri. The two city administrations are Addis Ababa and Dredawa (22).
In this systematic review and meta-analysis, all published articles that were done in Ethiopia were included. All studies that reported the quality of sleep among patients with chronic illnesses such as diabetes, heart failure, hypertension, cancer, HIV/AIDS and epilepsy were included. All types of studies that were published in English and conducted among all stages of chronic illness and published until December 1st, 2023, were included.
Studies that failed to report sleep quality based on the Pittsburgh Sleep Quality Index (PSQI) tool were excluded from this review. Studies that were conducted among patients who were taking sleep medication were excluded. Additionally, studies such as case reports, case studies, editorial letters, reports, and qualitative studies were excluded from the study.
Before going to the extensive searching, the presence of systematic review and meta-analysis protocol on sleep quality among patients with chronic illness at PROSPERO was checked. After that, both published articles and grey literatures that assessed sleep quality among patients with chronic illness in all regions of Ethiopia were used as sources of data. The review was conducted by using the Preferred Reporting Items for Systematic Review and Meta Analysis (PRISMA) guideline (23). The search strategy was developed using the Population (Patients with chronic illness), Intervention, Comparison (patients without chronic illness), and Outcome (sleep quality) searching guide. For published articles, an intensive search of online databases such as PubMed (MEDLINE), EMBASE, Cochrane, Africa Journal of Online, Google Scholar, and an advanced Google search was made. During systematic search, the word ((((((((“sleep quality”) OR “poor sleep quality”) AND patients) OR “chronic illness patients”) OR “patients with hypertension”) OR “patients with diabetes”) OR “patients with heart failure”) OR “patients with HIV/AIDS”) OR “patients with cancer”) OR “patients with epilepsy”) AND Ethiopia) was used. All articles in reference lists were searched to include additional studies and reports in the review and analysis. A systematic search of the literature was made from November 11, 2023, until December 1, 2023.
There are various ways to quantify the quality of sleep. Nonetheless, the Pittsburg Sleep Quality Index (PSQI) was the most often utilized instrument. Its validity was assessed in Ethiopia among community-dwelling adults (24). The PSQI evaluates sleep quality by asking questions regarding, e.g., the respondent’s self-reported duration of sleep, sleep latency, and sleep arousals for the 1 month preceding the time of evaluation. The 19 questions that make up the PSQI are divided into seven categories. Each questionnaire response is assigned a number between 0 and 3, where 0 denotes no problems and 3 denotes serious problems. The sum of the response ratings from each of the seven question groupings makes up the final score. The total score (global score) can range from 0 to 21. The lower scores indicate better sleep quality, and the higher scores indicate poor sleep quality. Chronic illnesses are disease conditions that include diabetes, hypertension, heart failure, HIV/AIDS, cancer, and epilepsy.
In this systematic review and meta-analysis, included studies were cross sectional studies. There is only one case control study. Hence, the quality of included studies were assessed by a 8 item critical appraisal tool adopted from Joanna Briggs Institute (JBI) (25) and considered high quality when the sum of JBI items is above 70%. This is a tool used for the evaluation of prevalence studies. AE and TA assessed the methodological quality of eligible articles independently. The difference in extraction was managed through discussion and the third author. All articles scored above half of the score were included in the systematic review and meta-analysis.
A Microsoft Excel spread sheet was used to generate the pre-piloted format in which AE, BT, SA, and AS extracted the data from the included literature. First author names, year of publication, region, sample size, population categories, study design, study area (institution vs. community), PSQI cut-off point, data collecting time, and prevalence of poor sleep quality were retrieved from each article. Following a conversation among the authors to resolve the disagreement, AE collated the data that had been extracted from the authors.
The extracted data were exported from the Microsoft Excel spreadsheet and entered the STATA version 17 command window (26). Using the I-squared statistic, the presence of statistical heterogeneity within the included papers was evaluated prior to conducting the primary meta-analysis. I2 value ranges between 0 and 100% whereby I2 > =75% indicate high heterogeneity across the studies. Additionally, Egger’s tests and a funnel plot were used to determine whether publication bias existed. Following that, STATA meta set command was used to complete the pooled estimate. To control heterogeneity, a subgroup analysis of the included studies was conducted based on the categories of populations and the cutoff point. Additional advanced statistical analyses, such as meta-regression to identify the potential sources of heterogeneity and sensitivity analysis to investigate the influence of a single study on the overall pooled estimate, were performed. The trim and fill test were done to minimize publication bias. The findings of this study were presented using tables and forest plots with 95% confidence intervals (CI).
Using advanced searching, 142 articles were found in Pubmed, EMBASE, Google Scholar, and Google. Reference tracing was used to add two articles to the overall number of articles. One hundred and six papers were screened using their title and abstract after 36 duplicate articles were eliminated. A total of 28 articles were screened for their full text. Following that, a total of 21 articles that passed the eligibility requirements and quality assessment were included in the final systematic review and meta-analysis (Figure 1).
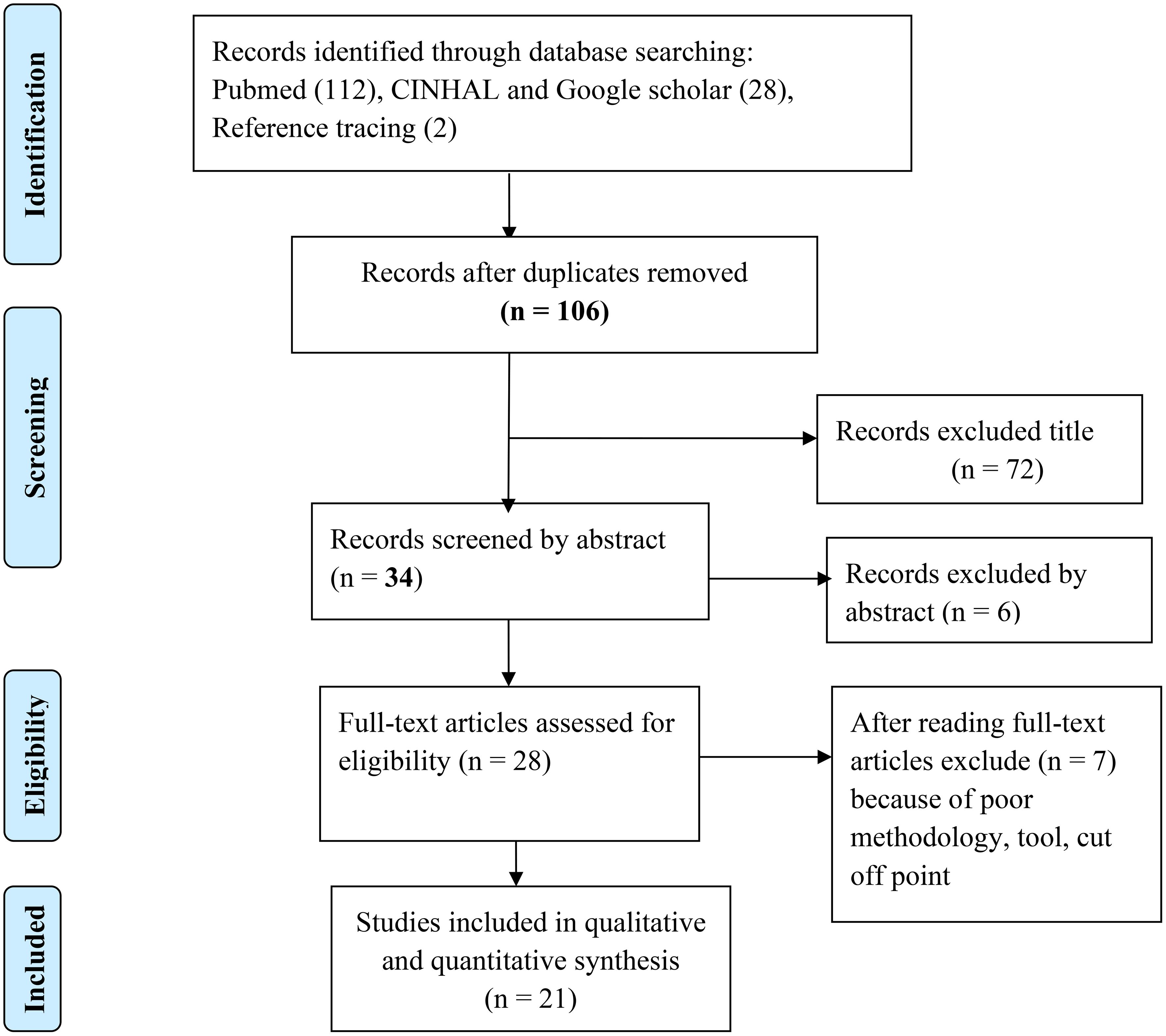
Figure 1 PRISMA flow diagram that shows study selection for meta-analysis of sleep quality among patients with chronic illness.
A total of 21 articles with 7393 study participants were included in the final systematic review and meta-analysis. All the articles were published from 2015 till 2023. All of the articles were done at institutional level. From the total included studies, 4 of them were done in Addis Ababa (27–30) and 11 studies were done in the Amhara region (29, 31–40). The other five articles were conducted in the Oromia region (41–45), and one article was done in the Sidama region (46). Regarding the study population, five studies were conducted on diabetes patients (29, 32–34, 41), and the other six studies were conducted on HIV/AIDS patients (29, 38, 39, 44, 46, 47). One of the articles used case control as a study design (32). Three articles used non-probability sampling, such as convenient sampling (32, 41, 42). Five of the articles reported poor sleep quality for those patients whose PSQI score was ‗ 5 (28, 37, 42, 43). The rest 16 studies used PSQI score >5 to declare the presence of poor sleep quality. The largest sample size was 565, which was obtained from a study conducted in the Amhara region among epileptic patients in 2021 (37). The data for three studies were collected during the winter season (34, 35, 38), and similarly the data for three studies were collected during the summer season (29, 32, 45) (Table 1).
Before pooling the estimated effect, the presence of heterogeneity and publication bias were evaluated. Heterogeneity between included articles was assessed statistically by using I-squared statistic. According to the result, there was high heterogeneity between the included studies (I2 = 97.26; P = 0.000). The presence of publication bias was statistically assessed by Egger’s weighted regression, Begg’s method and funnel plot. P value of Egger’s and Begg’s test was 0.209 and 0.349 respectively, which indicates that there is no publication bias. However, the funnel plot showed asymmetrical distribution of studies inside the funnel which implies that there is a publication bias (Figure 2).
After testing heterogeneity and the presence of publication bias, the effect size was pooled by using STATA version 17. Since there is considerable heterogeneity between the studies (I2 = 97.26; P = 0.000), the main meta-analysis was performed using a random effect model. As it is shown in Figure 3, the pooled estimate of poor sleep quality for patients with chronic illness was 52% (95% CI: 46 - 59%) (Figure 3).
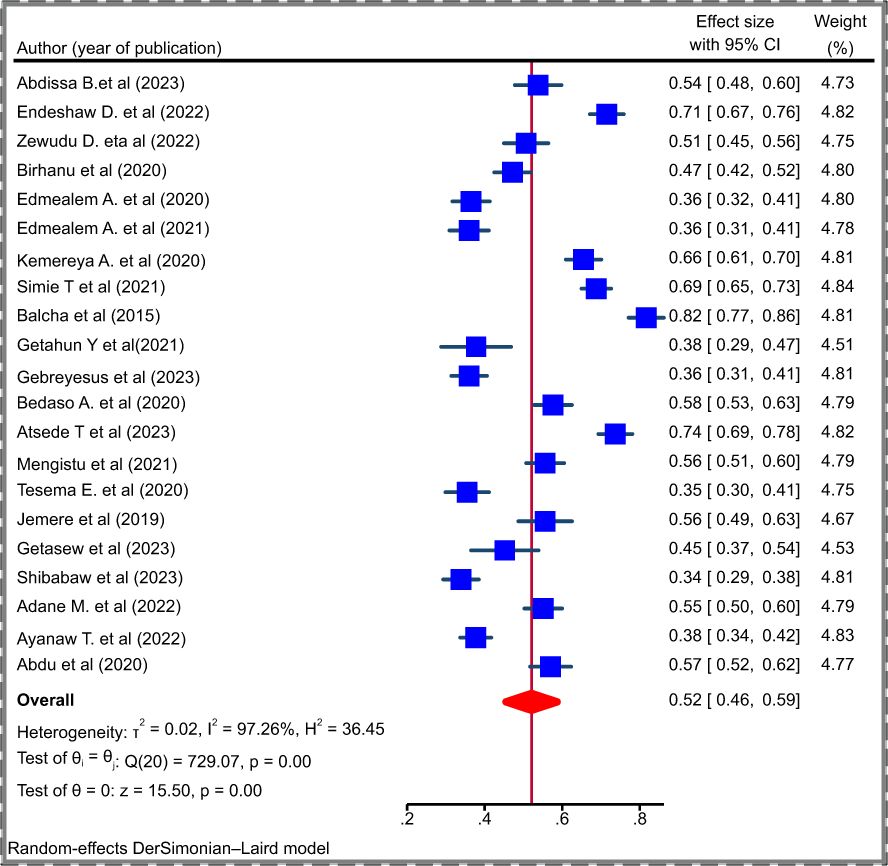
Figure 3 Forest plot depicting the pooled prevalence of poor sleep quality among patients with chronic illness, 2023.
Meta regression was performed to identify the sources of heterogeneity between the studies. In this systematic review and meta-analysis, meta regression was performed by type population, cut off point for PSQI score, data collection period and region to evaluate whether these variables are sources of heterogeneity between the studies. However, none of them were sources of heterogeneity, in which the P value was above 0.05 (Table 2).
Subgroup analysis is done by type of population, season of data collection and cutoff point of PSQI to minimize heterogeneity between the included studies. As it is shown in Table 3, the highest pooled estimate poor sleep quality was seen among patients’ cancer patients 67% (95% CI: 64%-71%). The pooled estimate of poor sleep quality among diabetes patients was 36% (95% CI: 33% - 40%). Moreover, the pooled estimate of poor sleep quality among people living with HIV/AIDS was 56% (95% CI: 48 – 68%). The highest poor sleep quality was seen among studies whose data was collected during spring (68%: 95% (42% - 94%) (Table 3).
Sensitivity analysis was done to evaluate whether the pooled effect size was influenced by individual studies or not. As it is shown in Figure 4, there is no any study which influences the overall pooled estimate of poor sleep quality among patients with chronic illness. The pooled effect size after omitting the individual study was inside the confidence interval of the overall pooled effect size (all the effect sizes after omitting a single study were between 48% and 59%) (Figure 4).
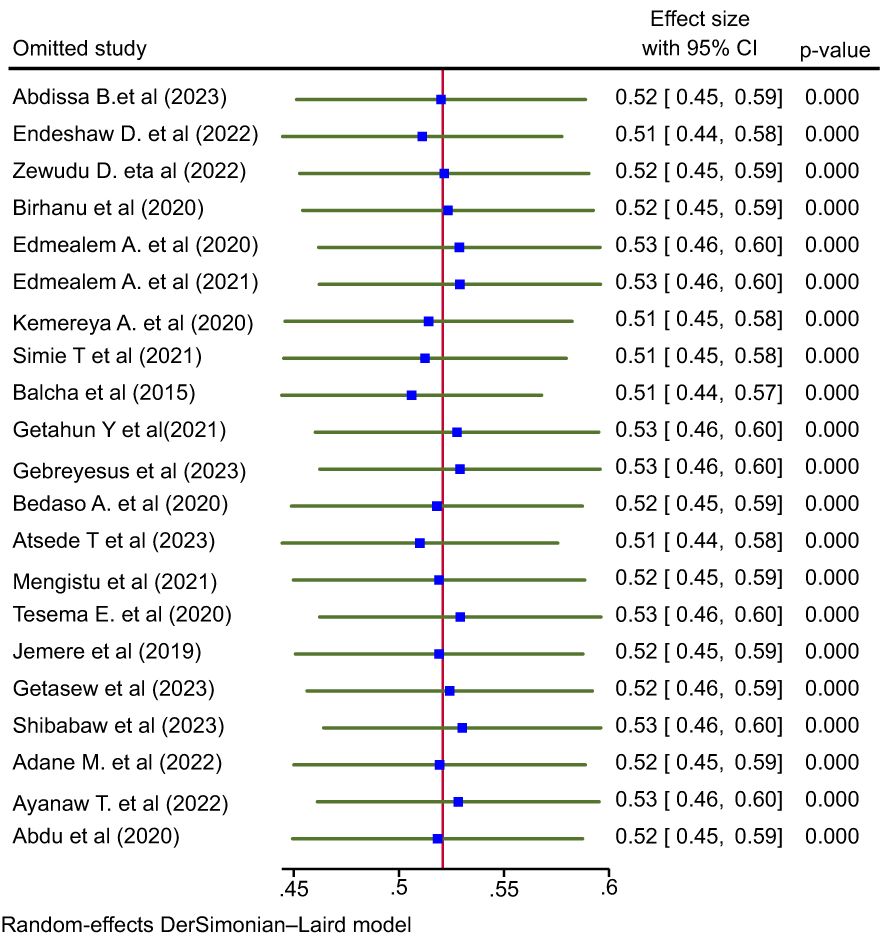
Figure 4 Leave - one- out meta- analysis to see the influence of the single study on the pooled effect size, 2023.
The prevalence of poor sleep quality among patients with chronic illness in Ethiopia is not known. However, understanding the overall quality of sleep among patients with chronic illness is valuable for different stake holders including health care providers to tackle the adverse prognosis and decrease the burden of the diseases. This systematic review and meta-analysis revealed that the pooled estimate of poor sleep quality among patients with chronic illness in Ethiopia was 52% (95% CI: 48% -59%). The prevalence of sleep quality in this study when compared to other studies, it is in line with the finding of the pooled estimate of poor sleep quality among chronic kidney disease patients (59%) (17) and a single study in Nigeria among chronic kidney disease patients (54). Additionally, the pooled prevalence of poor sleep quality for patients with chronic illness in this study is comparable to the global prevalence of poor sleep quality among cancer patients(57.4%) (19), and the pooled prevalence of poor sleep quality among stroke patients (53%) (55). On the contrary, the finding of this review is higher than the pooled prevalence of poor sleep quality among patients with Inflammatory bowel disease (19). Moreover, the finding of this systematic review and meta-analysis is lower than the pooled prevalence poor sleep quality among HIV/AIDS patients (63%) (44). The possible justification for this discrepancy might be the difference in study population, eligibility criteria, the treatment modality and the cutoff point in the PSQI score. Most of the studies pooled the prevalence of poor sleep quality for a single type of population in their analysis unlike to this study which pooled the prevalence poor sleep quality for different types of chronic illnesses. The quality of sleep quality is different for different disease conditions.
According to the subgroup analysis, the highest pooled estimate of poor sleep quality was seen among cancer patients. This might be occurred due to the treatment effect and pain (56). According to a systematic review, the treatment given to cancer patients affects the sleep quality (57). The pooled estimate of poor sleep quality among cancer patients was 63% (95% CI: 45% - 80%). In this subgroup analysis, the lowest pooled estimate of poor sleep quality was observed among hypertension patients. Hypertension is a silent killer, and it has no any suffering symptoms in contrast to cancer, HIV/AIDS, diabetes, epilepsy and other chronic illnesses. As a result, there is no significant factor that hinder and interfere sleep quality of hypertension patients. The difference in socioeconomic status, pathogenies of the disease condition, environmental factors, treatment modality, study period and life style of patients might be the other justifications for the discrepancy between the highest and lowest pooled estimates.
Seasonal variations and environmental factors have an impact on the quality of sleep. This systematic review and meta-analysis found that studies using data gathered in the spring had the highest pooled estimate of poor sleep quality 68% (95% CI: 42% - 94%). The chilly weather in Ethiopia throughout the spring may be the cause of this. The pooled estimate of poor sleep quality was lowest among patients with chronic diseases who were interviewed in the summer 37% (95% CI: 32% - 43%). This could be because of the high temperatures that make Ethiopia’s summertime more comfortable.
This systematic review and meta-analysis has its own limitations. The presence of high level of heterogeneity among included studies is the main limitation. Included studies use different cut off point to estimate the prevalence of poor sleep quality.
Patients with chronic illnesses in Ethiopia had a high pooled estimate of poor sleep quality. Patients with cancer had the highest pooled estimate of poor-quality sleep compared with other patients. Patients with chronic illnesses had trouble sleeping in the spring, according to this systematic review and meta-analysis. Therefore, healthcare professionals, the ministry of health, and other stakeholders should give attention and intervention to enhance the quality of sleep for patients with chronic illnesses.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
AE: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. BTe: Writing – original draft, Writing – review & editing. GA: Writing – original draft, Writing – review & editing. HZ: Writing – original draft, Writing – review & editing. TA: Writing – original draft, Writing – review & editing. SA: Writing – original draft, Writing – review & editing. AS: Writing – original draft, Writing – review & editing. BTo: Writing – original draft, Writing – review & editing. AG: Writing – original draft, Writing – review & editing. TW: Writing – original draft, Writing – review & editing. TL: Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
We acknowledge all the authors of included studies. We want also acknowledge authors who gave us comments in research gate.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
JBI, Joanna Briggs Institute; PRISMA, Preferred Reporting Items for Systematic Review and Meta Analysis; PICO, Population Intervention Comparison Outcome; PSQI, Pittsburgh Sleep Quality Index.
1. Foster R. A good introduction to sleep and sleep disorders. Lancet Neurol. (2012) 11:848. doi: 10.1016/S1474-4422(12)70222-3
2. Berryman P, Lukes E, Ohlmann KK, O'sullivan MI. The costs of short sleep. AAOHN J. (2009) 57(9):381–5. doi: 10.3928/08910162-20090817-02
3. Grandner MA. The cost of sleep lost: Implications for health, performance, and the bottom line. Los Angeles, CA: Sage Publications Sage CA (2018) p. 1629–34.
4. Hillman D, Mitchell S, Streatfeild J, Burns C, Bruck D, Pezzullo L. The economic cost of inadequate sleep. Sleep. (2018) 41(8):zsy083. doi: 10.1093/sleep/zsy083
5. Stenholm S, Head J, Kivim�ki M, Magnusson Hanson LL, Pentti J, Rod NH, et al. Sleep duration and sleep disturbances as predictors of healthy and chronic disease–free life expectancy between ages 50 and 75: a pooled analysis of three cohorts. Journals Gerontology: Ser A. (2019) 74(2):204–10. doi: 10.1093/gerona/gly016
6. Wang J, Qin W, Pang M, Zhao B, Xu J, Li S, et al. The effect of chronic disease and mental health on sleep quality among migrant elderly following children in Weifang City, China. Int J Environ Res Public Health. (2022) 19(19):12734. doi: 10.3390/ijerph191912734
7. Lian Y, Yuan Q, Wang G, Tang F. Association between sleep quality and metabolic syndrome: A systematic review and meta-analysis. Psychiatry Res. (2019) 274:66–74. doi: 10.1016/j.psychres.2019.01.096
8. Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. (2010) 71:1027–36. doi: 10.1016/j.socscimed.2010.05.041
9. Hudson AN, Van Dongen HP, Honn KA. Sleep deprivation, vigilant attention, and brain function: a review. Neuropsychopharmacology. (2020) 45:21–30. doi: 10.1038/s41386-019-0432-6
10. Ancoli-Israel S. The impact and prevalence of chronic insomnia and other sleep disturbances associated with chronic illness. Am J Managed Care. (2006) 12:S221.
11. Zhou Y, Jin Y, Zhu Y, Fang W, Dai X, Lim C, et al. Sleep problems associate with multimorbidity: A systematic review and meta-analysis. Public Health Rev. (2023) 44:1605469. doi: 10.3389/phrs.2023.1605469
12. Kemple M, O'Toole S, O'Toole C. Sleep quality in patients with chronic illness. J Clin Nurs. (2016) 25:3363–72. doi: 10.1111/jocn.13462
13. Lee S, Kim JH, Chung JH. The association between sleep quality and quality of life: a population-based study. Sleep Med. (2021) 84:121–6. doi: 10.1016/j.sleep.2021.05.022
14. Hyyppä MT, Kronholm E. Quality of sleep and chronic illnesses. J Clin Epidemiol. (1989) 42:633–8. doi: 10.1016/0895-4356(89)90006-1
15. Uch�a LR, Oliveira MD, De AU, Da Silva A, Veras VS, De Sousa DF, et al. Poor sleep quality in persons living with HIV: a systematic review and meta-analysis. Journal of Nursing and Health Science. (2018) 4(2):8.
16. Ruan W, Yuan X, Eltzschig HK. Circadian rhythm as a therapeutic target. Nat Rev Drug Discovery. (2021) 20:287–307. doi: 10.1038/s41573-020-00109-w
17. Tan LH, Chen PS, Chiang HY, King E, Yeh HC, Hsiao YL, et al. Insomnia and poor sleep in CKD: a systematic review and meta-analysis. Kidney Med. (2022) 4(5):100458. doi: 10.1016/j.xkme.2022.100458
18. Li L, Li L, Chai L, Xiao L, Ng L, Ungvari L, et al. Prevalence of poor sleep quality in patients with hypertension in china: a meta-analysis of comparative studies and epidemiological surveys. Front Psychiatry. (2020) 11:591. doi: 10.3389/fpsyt.2020.00591
19. Chen MY, Zheng WY, Liu YF, Li XH, Lam MI, Su Z, et al. Global prevalence of poor sleep quality in cancer patients: A systematic review and meta-analysis. Gen Hosp Psychiatry. (2023). doi: 10.37766/inplasy2023.4.0036
20. Štefan L, Sporiš G, Krističević T. The associations between sleep duration and sleep quality with self-rated health in young adults: a population-based study. Int J Adolesc Med Health. (2020) 32. doi: 10.1515/ijamh-2018-0007
21. Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Internal Med. (2016) 165(2):125–33. doi: 10.7326/M15-2175
23. PRISMA. Preferred Reporting Items for Systematic Reviews and MetaAnalyses. PRISMA (2009). Available at: http://www.prismastatement.org/.
24. Salahuddin M, Maru TT, Kumalo A, Pandi-Perumal SR, Bahammam AS, Manzar MD. Validation of the Pittsburgh sleep quality index in community dwelling Ethiopian adults. Health Qual Life outcomes. (2017) 15:1–7. doi: 10.1186/s12955-017-0637-5
25. Institute, J.B, J.B. Institute. Checklist for analytical cross sectional studies Vol. 7. Adelaide: The Joanna Briggs Institute (2017).
27. Abebe E, Giru BW, Boka A. Sleep quality and associated factors among adult cancer patients on treatments at tikur anbessa specialized hospital oncology unit, Addis Ababa, Ethiopia, 2021. Cancer Control. (2023) 30:10732748231160129. doi: 10.1177/10732748231160129
28. Adem K, Kassew T, Birhanu A, Abate A. Sleep quality and associated factors among peoples with epilepsy who have a follow-up at Amanuel Mental Specialized Hospital, Addis Ababa, Ethiopia, 2019: an institutional based cross-sectional study. Psychiatry J. (2020) 2020:1–9. doi: 10.1155/2020/1402712
29. Shibabaw YY, Dejenie TA, Tesfa KH. Glycemic control and its association with sleep quality and duration among type 2 diabetic patients. Metab Open. (2023) 18:100246. doi: 10.1016/j.metop.2023.100246
30. Mengistu N, Azale T, Yimer S, Fikreyesus M, Melaku E, Shumye S. Quality of Sleep and Associated Factors among People Living with HIV/AIDS on Follow up at Zewditu Memorial Hospital, Ethiopia: An Institution-Based Cross-Sectional Study. Perspective Recent Adv Med Res. (2022) 2:1–15.
31. Endeshaw D, Biresaw H, Asefa T, Yesuf NN, Yohannes S. Sleep quality and associated factors among adult cancer patients under treatment at oncology units in Amhara region, Ethiopia. Nat Sci Sleep. (2022), 1049–62. doi: 10.2147/NSS.S356597
32. Mersha GA, Alemu DS, Ferede MG, Tegegn MT, Tilahun MM, Lorato MM, et al. Association of Poor Quality of Sleep with Vision-Threatening Diabetic Retinopathy: A Matched Case–Control Study. Ophthalmol Ther. (2023) 12(2):1141–53. doi: 10.1007/s40123-023-00663-7
33. Zewdu D, Gedamu H, Beyene Y, Tadesse M, Tamirat M, Muluken S. Sleep quality and associated factors among type 2 Dm patients and non-Dm individuals in Bahir Dar governmental hospitals: comparative cross-sectional study.... Sleep Sci Pract. (2022) 6(1):10. doi: 10.1186/s41606-022-00079-5
34. Birhanu TT, Hassen Salih M, Abate HK. Sleep quality and associated factors among diabetes mellitus patients in a follow-up clinic at the University of Gondar comprehensive specialized hospital in Gondar, Northwest Ethiopia: a cross-sectional study. Diabetes Metab Syndrome Obes. (2020), 4859–68. doi: 10.2147/DMSO.S285080
35. Edmealem A, Ademe S, Andualem A. Sleep quality and associated factors among patients with chronic illness at South Wollo Zone Public Hospitals, Northeast Ethiopia. Clin J Nurs Care Pract. (2021) 5:043–50. doi: 10.29328/journal.cjncp.1001036
36. Edmealem A, Degu SG, Haile D, Gedfew M, Bewket B, Andualem A. Sleep quality and associated factors among diabetes, hypertension, and heart failure patients at Debre Markos Referral Hospital, Northwest Ethiopia. Sleep Disord. (2020) 2020. doi: 10.1155/2020/6125845
37. Simie Tsega S, Yazew BG, Mekonnen K. Sleep quality and associated factors among adult patients with epilepsy attending follow-up care at referral hospitals in Amhara region, Ethiopia. PLoS One. (2021) 16:e0261386. doi: 10.1371/journal.pone.0261386
38. GebreEyesus FA, Degu FS, Yohanes YB, Azagew AW. Sleep quality and associated factors among adult people living with HIV on follow-up at Dessie Town Governmental Health Facilities Antiretroviral Therapy Clinics, Northeast, Ethiopia, 2020, a multicenter cross-sectional study. BMC Psychiatry. (2023) 23(1):1–13. doi: 10.1186/s12888-023-04619-w
39. Adane M, Amha H, Tafere Y, Alem G. Poor sleep quality and associated factors among people attending anti-retroviral treatment clinic at Finote selam general hospital, Amhara, Ethiopia. Sleep Medicine: X. (2022) 4:100054. doi: 10.1016/j.sleepx.2022.100054
40. Ayanaw T, Temesgen M, Azagew AW, Ferede YM. Sleep quality and associated factors among adult hypertensive patients attending a chronic follow up care clinic in northwest Amhara regional state referral hospitals, Northwest Ethiopia. PloS One. (2022) 17(7):e0271072. doi: 10.1371/journal.pone.0271072
41. Jemere T, Mossie A, Berhanu H, Yeshaw Y. Poor sleep quality and its predictors among type 2 diabetes mellitus patients attending Jimma University Medical Center, Jimma, Ethiopia. BMC Res Notes. (2019) 12:1–6. doi: 10.1186/s13104-019-4531-6
42. Balcha A.A.T.T.F., Nemera G. Perceived sleep quality of heart failure patients at Jimma university specialized hospital (JUSH) chronic follow up clinic south west Ethiopia, 2015. J Health Medicine Nurs. (2015) 20:34–44.
43. Getahun Y, Demissie WR, Amare H. Sleep quality among cardiac patients on follow up at Jimma Medical Center, southwestern Ethiopia. Sleep Sci. (2021) 14:11.
44. Abdu Z, Dule A. Poor quality of sleep among HIV-positive persons in Ethiopia. HIV/AIDS-Research Palliative Care. (2020), 621–8. doi: 10.2147/HIV.S279372
45. Birhanu TE, Getachew B, Gerbi A, Dereje D. Prevalence of poor sleep quality and its associated factors among hypertensive patients on follow up at Jimma University Medical Center. J Hum hypertension. (2021) 35(1):94–100. doi: 10.1038/s41371-020-0320-x
46. Bedaso A, Abraham Y, Temesgen A, Mekonnen N. Quality of sleep and associated factors among people living with HIV/AIDS attending ART clinic at Hawassa University comprehensive specialized Hospital, Hawassa, SNNPR, Ethiopia. PloS One. (2020) 15(6):e0233849. doi: 10.1371/journal.pone.0233849
47. Mengistu N, Azale T, Yimer S, Fikreyesus M, Melaku E, Shumye S. Quality of sleep and associated factors among people living with HIV/AIDS on follow up at Ethiopian Zewditu Memorial Hospital, 2018. Sleep Sci Pract. (2021) 5:1–8. doi: 10.1186/s41606-020-00056-w
48. Abebe E, B.W Giru, A Boka. Sleep quality and associated factors among adult cancer patients on treatments at tikur anbessa specialized hospital oncology unit, addis ababa, ethiopia, 2021. Cancer Contro. (2023) 301073274823116012. doi: 10.1177/10732748231160129
49. Zewdu D, Gedamu H, Beyene Y, et al. Sleep quality and associated factors among type 2 Dm patients and non-Dm individuals in Bahir Dar governmental hospitals: comparative cross-sectional study. Sleep Science Practice. (2022) 6:10. doi: 10.1186/s41606-022-00079-5
50. Adem K, Kassew T, Birhanu A, Abate A. Sleep Quality and Associated factors among peoples with epilepsy who have a follow-up at amanuel mental specialized hospital, addis ababa, ethiopia, 2019: an institutional based cross-sectional study. Psychiatry J. (2020) 2020:1402712. doi: 10.1155/2020/1402712
51. GebreEyesus F.A, Degu F.S, Yohanes Y.B, Azagew A.W. Sleep quality and associated factors among adult people living with HIV on follow-up at dessie town governmental health facilities antiretroviral therapy clinics, northeast, ethiopia, 2020, a multicenter cross-sectional study. BMC Psych. (2023) 23(1):1–13. doi: 10.1186/s12888-023-04619-w
52. Bedasos A, Abraham Y, Temesgen A, Mekonnen N. Quality of sleep and associated factors among people living with HIV/AIDS attending ART clinic at Hawassa University comprehensive specialized Hospital, Hawassa, SNNPR, Ethiopi. PLoS One. (2020) 15(6):e0233849.
53. Birhanu T.E, Getachew B, Gerbi A, Dereje D. Prevalence of poor sleep quality and its associated factors among hypertensive patients on follow up at Jimma University Medical Center. J Hum Hypertens. (2021) 35(1):94–100. doi: 10.1038/s41371-020-0320-x
54. Adejumo OA, Edeki IR, Mamven M, Oguntola OS, Okoye OC, Akinbodewa AA, et al. Sleep quality and associated factors among patients with chronic kidney disease in Nigeria: a cross-sectional study. BMJ Open. (2023) 13(12):e074025. doi: 10.1136/bmjopen-2023-074025
55. Luo Y, Yu G, Liu Y, Zhuge C, Zhu Y. Sleep quality after stroke: A systematic review and meta-analysis. Medicine. (2023) 102(20):e33777. doi: 10.1097/MD.0000000000033777
56. Sun Y, Laksono I, Selvanathan J, Saripella A, Nagappa M, Pham C, et al. Prevalence of sleep disturbances in patients with chronic non-cancer pain: a systematic review and meta-analysis. Sleep Med Rev. (2021) 57:101467. doi: 10.1016/j.smrv.2021.101467
57. Divani A, Heidari ME, Ghavampour N, Parouhan A, Ahmadi S, Narimani Charan O, et al. Effect of cancer treatment on sleep quality in cancer patients: A systematic review and meta-analysis of Pittsburgh Sleep Quality Index. Supportive Care Cancer. (2022) 30(6):4687–97. doi: 10.1007/s00520-021-06767-9
Keywords: hypertension, diabetes, cancer, sleep quality, chronic illness, Ethiopia
Citation: Edmealem A, Tegegne B, Alem G, Zeleke H, Ayenew T, Ayenew S, Sisay Gebeyew A, Tomiso B, Getahun A, Wondie T and Liknaw T (2024) Sleep quality among patients with chronic illness in Ethiopia: systematic review and meta-analysis. Front. Psychiatry 15:1365463. doi: 10.3389/fpsyt.2024.1365463
Received: 24 January 2024; Accepted: 16 May 2024;
Published: 30 May 2024.
Edited by:
Tarak Driss, Université Paris Nanterre, FranceReviewed by:
Francesc Xavier Gomez-Olive, University of the Witwatersrand, South AfricaCopyright © 2024 Edmealem, Tegegne, Alem, Zeleke, Ayenew, Ayenew, Sisay Gebeyew, Tomiso, Getahun, Wondie and Liknaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Afework Edmealem, YWZld29ya2VkbWVhbGVtQGRtdS5lZHUuZXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.