
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
PERSPECTIVE article
Front. Psychiatry, 10 June 2024
Sec. Perinatal Psychiatry
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1364845
This article is part of the Research TopicWomen in Psychiatry 2023: Perinatal PsychiatryView all 12 articles
The concept of matrescence, akin to adolescence but for mothers, has gained increasing attention in perinatal psychiatry, marking a paradigm shift towards understanding the holistic development of mothers. Matrescence encompasses the myriad psychological, social, cultural, and existential changes which occur as women transition into motherhood. Despite advances in maternal mental health, a bias towards pathologizing maternal experiences persists in research and practice. This commentary advocates for the integration of matrescence into perinatal psychiatry, drawing from the work of Dana Raphael and contemporary scholarship. Matrescence offers a strengths-based framework that acknowledges both the challenges and opportunities of motherhood, emphasizing the normative aspects of a mother’s self-development. By adopting matrescence terminology and nosology, clinicians and researchers can enhance traditional psychiatric classifications. Additionally, matrescence underscores the importance of considering ecological systems and historical factors in maternal well-being, highlighting the need for comprehensive and compassionate healthcare services. Embracing matrescence as a fundamental concept in perinatal psychiatry holds promise for improving maternal mental health outcomes and promoting the flourishing of mothers worldwide.
Since the inception of psychiatry at the end of the 19th century, its various theoretical orientations have shifted in prominence but rarely has the mother as a figure of interest for the well-being of individuals and the broader societal fabric lost her primacy. Mothers have been identified as primary agents in the developmental trajectories of their offspring and as sources of negative impact when in distress. Regrettably, this scholarly fascination has historically led to the stigmatization and medicalization of maternal experience without the same attention paid to their well-being. Over the past six decades, with the establishment of entities such as the International Society for Psychosomatic Obstetrics and Gynecology, the Marcé Society, and Postpartum Support International, the field of perinatal psychiatry has made significant contributions to recognizing the pivotal role of reproductive transitions in women’s health, facilitated by a global consortium of researchers, clinicians, educators, and advocates (1–4). This unfolded in parallel with social justice activism that ultimately led to legislative actions mandating the universal screening of new mothers for depression and their active participation in clinical research (5–8). By the turn of the 21st century, the field of maternal mental health had grown beyond its myopic focus on child outcomes to encompass a wider classification of diagnoses (e.g., perinatal mood and anxiety disorders or PMADs), clinical windows (e.g., prenatal onset), pathophysiologies (e.g., traumatic childbirth), interventions (e.g., zuranolone), and trainings (e.g., specialized curricula)— this time to alleviate the distress of the mothers themselves (9–11). Epidemiological data revealed that vulnerability in motherhood was ubiquitous with estimates between 15% to 21% of the general population experiencing depression, and up to 80% of mothers reporting distress of some kind (12). This paradigmatic shift from viewing the mother merely as a functional object to recognizing her as a psychological subject marked a belated but critical turn.
Despite these notable advancements, it is imperative to acknowledge that a deeply rooted biomedical “psychiatry bias” in maternal mental health research and practice still remains, inviting critical reflection (13). Ongoing theoretical innovation is necessary to advance bold ideas that can evolve outdated explanatory frameworks and guide scientific exploration now in the direction of building resilience. In 2018, the World Health Organization (WHO) underscored the mental health of mothers as a fundamental component of their overall health, defining maternal well-being not merely as a reductionistic absence of mental illness, but as the capacity for flourishing (14). There exists an urgent need for a strengths-based framework that studies the normative aspects of a mother’s self-development and acknowledges both the positive and negative outcomes with equal consideration. Such an expanded viewpoint provides a more comprehensive appreciation of mothers as complete individuals capable of thriving if given the optimal environmental conditions. Using a term known as matrescence from the archives of women’s health literature and, notably, from a different discipline, is a timely intervention (15). The process of becoming a mother, or matrescence, was first introduced in the 1970s by Dana Raphael, Ph.D., a female medical anthropologist who studied birth and breastfeeding and also coined the word ‘doula’. It was largely neglected until half a century later when the author revived it to complement diagnostic views in maternal mental health and expanded its definition further (15). Matrescence must once again evolve beyond its original conceptualization in order to offer a new lineage of thinking for the field of perinatal psychiatry. The larger promise of matrescence may be in its ability to reshape entrenched societal beliefs and, by extension, how health systems nurture maternal welfare by providing a more comprehensive and compassionate approach to their care.
In her pioneering yet overlooked work, Becoming a Mother, A New/Old Rite de Passage in Reproduction, Power, and Change (1975), Raphael stated,
“The critical transition period which has been missed is matrescence, the time of mother-becoming … Giving birth does not automatically make a mother out of a woman … The amount of time it takes to become a mother needs study” (16, p.65-70).
Raphael’s words serve as a call to inquire further into the nature of maternal psychological maturation and to integrate these insights into modern psychiatric theory and practice. The delayed explication of matrescence may be due, in part, to the lack of language available to describe new motherhood as a “life crisis” without cloaking it entirely in negative terminology. Like the term adolescence from the Latin word “adolescere”, meaning “to emerge, grow, or mature”, it may share similar defining features of developmental growth or regression true of any life transition. The more common terms of postpartum or perinatal are borrowed from the obstetric establishment and as such form a natural pairing with words of infirmity (e.g., postpartum depression). It illuminates how over time the study of maternal development has been saddled with a conceptual basis that has shaped it into a ‘curative discipline’ based on the medical model of disease, and to which some argue it largely owes its transformation into the subfield of perinatal psychiatry (17). Establishing its own unique nosology instead may help matrescence gain similar recognition and relevance. A standardized framework would also enable systematic investigation by others, enhance the quality and comparability of studies, and could play a vital role in education and awareness efforts.
The act of transcending disciplinary boundaries to adapt concepts from other fields is a key strategy for theoretical innovation. This approach not only enriches our understanding but also broadens our interpretative frameworks for the better (see reproductive identity) (18, 19). It is also an opportune moment as the classification of PMADs is currently being subjected to greater scrutinty (1). While more studies aim to distinguish conditions like postpartum depression from nonpuerperal major depression, comparisons to non-pathological human development remain curiously sparse. This discrepancy highlights a fundamental lack of understanding about what is normative during this life stage. More attention is needed as to whether general maternal distress is a distinct affective state, a subclinical presentation, or part of a normal continuum across the spectrum of illnesses from “baby blues” to psychosis (20). The utility of a developmental orientation such as matrescence is in helping to discern between normal and abnormal reactions to common experiences like fatigue or mood changes when interpreting the concerns of new mothers. For example, the term “perinatal distress” often serves as a vague catch-all that may incorrectly suggest impending illness (21). Recognizing it instead as a universal phenomenon of psychological disorientation to a major life change could clarify its meaning and reduce its potential overuse. In such an acute time of flux, distinguishing between psychiatric disorders and developmentally appropriate reactions can become challenging and potentially obscure the theoretical and practical boundaries between them (see Figure 1).
This conceptual “fuzziness” also extends into the history of nonspecific constructs often used to describe maternal psychology such as “transition to motherhood”, “becoming a mother”, “maternal role attainment”, or “maternal identity formation” (22). Using agreed-upon, succinct and clear terms such as Raphael’s matrescence and matrescents may reduce confusion, improve communication, and assist keyword searches when exploring these diverse bodies of literature. In terms of its timing and scope, precocious puberty and assisted reproductive technologies have widened the reproductive window and made it possible to become a mother even younger and older than previous generations. The exact length of matrescence is therefore individual, recurs with each child, and may last a lifetime with no clear endpoint. Integrating additional terminology from the field of developmental psychology could further improve cohesiveness and distinguish the various ages and stages of motherhood, similar to what is noted for young adulthood: emerging motherhood (infants to school-aged offspring), middle motherhood (adolescent offspring), and late motherhood (adult offspring). Notably, most research on maternal psychology predominantly centers around the early years of motherhood, leaving a gap in our understanding of late motherhood or the dynamics of parenting during menopause, especially considering the rising trend of delayed childbearing. This lack of comprehensive exploration suggests potential areas for future research to delve into the various phases of motherhood. For example, borrowing insights from the literature on grief could shed light on topics such as mourning the loss of one's former self or the emotional impact of the empty nest syndrome.
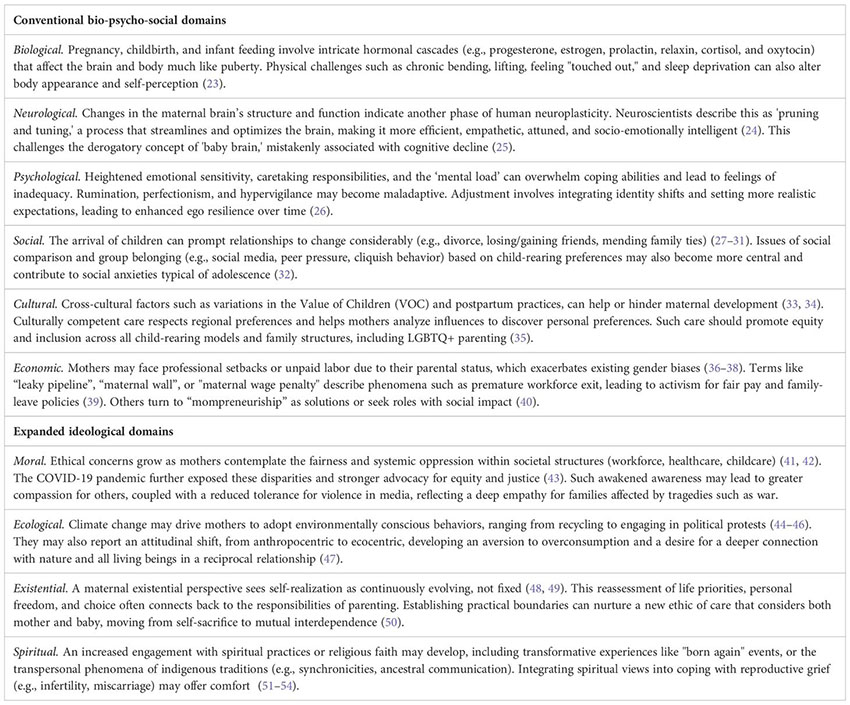
Raphael (16) gave us another clue that motherhood was a holistic experience with multidimensional significance: “The matrescent rite de passage can be examined as a biological fact, as a cultural event … The physiological stage of matrescence begins at the moment a female delivers a live infant. But, human beings are never limited by biological fact!” (16, pg. 66). Adolescence is widely recognized as a significant developmental period between childhood and adulthood that shares these equivalent all-encompassing changes. Although the comparison to adolescence is imperfect, theories from this field can provide valuable guidance in understanding the unique and distinct aspects of matrescence. Still, many questions remain unanswered. Is it a discrete life transition like adolescence or a complex life-long experience? If acute, what are the anticipated developmental tasks, and how does it then shape later adult development across the lifespan of a mother (and perhaps even into grandmothering)? What has been evidenced to date is that people who experience preconception, pregnancy, birth, surrogacy, adoption, and early parenting, undergo alterations not only in the few domains Raphael initially proposed but across all of the domains of human existence. With this in mind, the updated definition of matrescence for the 21st century offered here, as a first step in this longer inquiry process, is: a lifespan, developmental transformation that is biological, neurological, psychological, social, cultural, economic, political, moral, ecological, existential, and spiritual in nature. Furthermore, creating a comprehensive nosology for matrescence should also involve classifying both the developmental challenges and opportunities possible within each of these domains (see Box 1).
The exploration of the positive psychology of motherhood represents an essential aspect of matrescence that warrants further investigation into the opportunities for personal growth available to mothers. Perinatal patients often challenge clinical interpretations that solely pathologize their maternal experiences. Intolerance for this one-sidedness is gaining momentum as more mothers publicly share their stories and global public health initiatives such as Maternal Mental Health awareness campaigns increasingly use empowering and destigmatizing language (5). Today, Positive Youth Approaches (PYA) teach adolescents that they can adopt a growth mindset during their time of identity difussion. The "disorienting dilemma" of matrescence should be similarly viewed as a fertile period of self-discovery, experimentation, and subsequent mastery for mothers (55). For example, managing a central preoccupation like the desire for autonomy versus healthy interdependence can be reframed as an occasion to explore their personal values and to become more clear in their direction, meaning, and purpose. This may herald a more pivotal turning in their overall worldview, a metanoia that is more akin to an existential conversion-- a fundamentally transformed outlook in life, or a moral evolution.
To that end, the repackaging of the nosology outlined in Box 1. into an innovative self-assessment tool that acknowledges the bivalent, dual, or paradoxical nature of motherhood would help identify not only areas of vulnerability and symptoms as is the convention in a psychiatric evaluation but also the coexistence of self-perceived virtues and strengths. Unfortunately, explicitly “probing for the positive” is not how mental health practitioners are commonly trained, and as such they likely miss accounting for the subtle psychological gains (e.g., tolerance for ambiguity) experienced by mothers alongside the more obvious losses (e.g., sleeplessness). This "benign neglect" could be considered an ethical violation as the psychological and philosophical literature has validated a range of indicators for maternal subjective well-being and post-traumatic growth, and even the presence of perinatal flourishing (18). Denying the full range of maternal experience may have unforeseen consequences such as too many false positive diagnoses of depression in light of widespread screening. It may also unwittingly lead mothers to believe their failures are more important than their achievements. Designing a more comprehensive “positive and negative” assessment would be a useful adjunct to the widely used Whooley Screening Questions or Edinburgh Postnatal Depression Scale (EPDS). Such an innovation would also be in keeping with John Cox’s recommendation that organizations such as the Marcé Scientific Society or Global Alliance for Maternal Mental Health create forums for thinking about new scale development (56). Interestingly, in the appendix of Cox’s ten updated recommendations for the optimal administration of the EPDS are instructions on how to thoroughly ask and listen to answers:
“When used to assess a mother in the community, the practitioner should discuss the responses with her, listen to her story, ascertain whether clinical depression or another mental disorder is present – and consider referral and/or further listening visits” (25, p.128).
Perhaps swapping out “another mental disorder” with “matrescence” would be a step in the right direction for a more mother-centered, supportive, and developmentally-informed attitude. An interesting challenge moving forward, therefore, is how to best build the capacity of professionals to help mothers integrate the transformative effects of matrescence into their overall self-understanding while also preparing to assist them through impaired functioning when warranted.
Box 1. Developmental domains of matrescence.
In conclusion, it is important to emphasize this stage of development as a critical window for establishing lifelong positive health behaviors. Developmental factors such as the timing of the first pregnancy or whether a mother has been given a proper 'head start,' by equipping her with comprehensive matrescence education and not just childbirth preparation, can profoundly impact the course of motherhood. Future maternal functioning depends in part on past exposures, with each stage affecting the next and leading to a weathering effect of cumulative distress over time. This developmental cascade requires redesigning healthcare services to include prevention and early intervention programs, seamless linkages to professionals—especially during peak times of need—and sequential, stepwise care. Such a life course perspective must also extend its focus beyond individual-level assets and consider the broader ecological systems in which mothers are situated. It should critique the quality of their own holding environment and incorporate historical factors (e.g., COVID-19). Just as with adolescence, the experiences of matrescence can be severely altered by how well or poorly a mother is socially or economically resourced, placing her on a vastly different trajectory in terms of her well-being (57).
Today, a growing number of scientists are studying reproductive health issues, driven by advancements in women’s representation in the sciences, as well as their increased economic and political influence. These efforts are the unfinished work of generations of scientists, many of whom were mothers themselves, who were not afforded protected time from family life or adequate funding to pursue their hypotheses in earnest. Meanwhile, matrescence has also come a long way since its initial introduction to the scientific community in the 1970s, gaining significant traction and recognition. Its resurgence has catalyzed fresh discoveries across various fields, from neuroscience to economics and has been embraced by contemporary scholars as a good fit for reframing their inquiries (58). However, this has also led to fragmentation, with numerous disconnected discussions lacking a centralized platform for a more fruitful exchange of complementary perspectives. Lewis Gordon, as cited by Mantuori, notes that
“The emergence of disciplines has often led to the forgetting of their impetus in living human subjects” (59, p.45).
The prospect of matrescence serving as an academic container to consolidate its disparate strands of scholarship into a newly named specialization is promising. E.O. Wilson similarly advocated for ‘a unification of knowledge … a consilience,’ since bridging the gaps between disciplines can enhance the depth and diversity of understanding of any subject (60). A parallel process to what was done for adolescence more than a century ago, now for matrescence, could promulgate the same progress (61). Cross-disciplinary collaboration is also essential for maintaining checks and balances, especially for more dominant disciplines like psychiatry that may inadvertently skew scientific discourse, social trends, or grant allocations towards its own objectives. Efforts should be inquiry-driven rather than discipline-driven as a reminder that the priority should be a common commitment to improving the well-being of mothers.
Matrescence has also captured the interest of the private sector, leading to the development of various profitable outputs such as beauty products, luxury wellness services, trade books, and expensive online educational programs. This trend has opened up avenues for its commercialization with little ethical oversight. It is therefore necessary to protect and ensure robust support for all new mothers, not just the privileged few. The evolving science of matrescence, combined with grassroots activism and a reproductive justice perspective, demands a radical reimagination of our collective obligation to empower every mother to thrive, regardless of their socioeconomic status. This will require a multi-pronged approach: 1) establishing foundational knowledge of its unique developmental tasks and coping mechanisms; (2) identifying environmental factors that either facilitate or impede its optimal progression; (3) overhauling healthcare systems to ensure greater integration of services; (4) enforcing ethical guidelines for the treatment of mothers as a protected group; 5) expanding access to public health education initiatives; 6) training competent professionals in the specialization of maternal well-being. As was once said of adolescents, until society embraces this responsibility, the promise of matrescence will remain unfulfilled for millions of women. These issues will only continue to gain importance, and with them, the need for bold ideas like matrescence that can better sustain the reproductive life satisfaction of parents and the future environmental conditions that support them.
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
AA: Conceptualization, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Stowe ZN. Perinatal mental health: advances and opportunities. Am J Psychiatry. (2023) 180:874–7. doi: 10.1176/appi.ajp.20230822
2. Quatraro RM, Grussu P. Handbook of perinatal clinical psychology: from theory to practice. Routledge (2020). doi: 10.4324/9780429351990
3. Krohn H, Meltzer-Brody S. The history of perinatal psychiatry. In: Women's mood disorders: A clinician’s guide to perinatal psychiatry. Springer International Publishing, Cham (2021). p. 1–4.
4. Payne JL. Reproductive psychiatry: giving birth to a new subspecialty. Int Rev Psychiatry. (2019) 31:207–9. doi: 10.1080/09540261.2018.1579991
5. Elliott GK, Millard C, Sabroe I. The utilization of cultural movements to overcome stigma in narrative of postnatal depression. Front Psychiatry. (2020) 11:532600. doi: 10.3389/fpsyt.2020.532600
6. Miller ES, Wisner KL, Gollan J, Hamade S, Gossett DR, Grobman WA. Screening and treatment after implementation of a universal perinatal depression screening program. Obstet Gynecol. (2019) 134:303–9. doi: 10.1097/AOG.0000000000003369
7. Price SK, Corder-Mabe J, Austin K. Perinatal depression screening and intervention: enhancing health provider involvement. J Womens Health. (2012) 21:447–55. doi: 10.1089/jwh.2011.3172
8. Rhodes AM, Segre LS. Perinatal depression: a review of US legislation and law. Arch Womens Ment Health. (2013) 16:259–70. doi: 10.1007/s00737-013-0359-6
9. Erdly C, Etyemez S, Standeven LR, Nagle-Yang S, Osborne LM. Setting common standards for reproductive psychiatry education: effectiveness of the national curriculum in reproductive psychiatry. Acad Psychiatry. (2023) 47:63–8. doi: 10.1007/s40596-022-01663-8
10. Horan A, Kondas C, Dinsell V. Integrating peripartum mental health education into the psychiatry clerkship: a multimodal approach. Acad Psychiatry. (2022) 46:175–9. doi: 10.1007/s40596-021-01501-3
11. Osborne LM, MacLean JV, Barzilay EM, Meltzer-Brody S, Miller L, Yang SN. Reproductive psychiatry residency training: a survey of psychiatric residency program directors. Acad Psychiatry. (2018) 42:197–201. doi: 10.1007/s40596-017-0672-x
12. Rohr J, Vahidy FS, Bartek N, Bourassa KA, Nanavaty NR, Antosh DD, et al. Reducing psychiatric illness in the perinatal period: A review and commentary. World J Psychiatry. (2023) 13:149. doi: 10.5498/wjp.v13.i4.149
13. Blehar MC. Women's mental health research: The emergence of a biomedical field. Annu Rev Clin Psychol. (2006) 2:135–60. doi: 10.1146/annurev.clinpsy.2.022305.095344
14. World Health Organization. Strengthening resilience: A priority shared by Health 2020 and the sustainable development goals. Copenhagen: WHO Regional Office for Europe (2018).
15. Athan A, Reel HL. Maternal psychology: Reflections on the 20th anniversary of Deconstructing Developmental Psychology. Feminism & Psychology. (2016) 25(3):311–25.
16. Raphael D. Matrescence, becoming a mother, a “new/old” rite de passage. . In: Raphael D, editor. Being female: Reproduction power Change. Berlin: De Gruyter Mouton. (1975), 65–71. doi: 10.1515/9783110813128
17. Wood AM, Tarrier N. Positive clinical psychology: A new vision and strategy for integrated research and practice. Clin Psychol Rev. (2010) 30:819–29. doi: 10.1016/j.cpr.2010.06.003
18. Athan AM. Reproductive identity: An emerging concept. Am Psychol. (2020) 75:445. doi: 10.1037/amp0000623
19. Brookfield SD. Theoretical frameworks for understanding the field. In: Kasworm CE, Rose AD, Ross-Gordon JM, editors. Handbook of adult and continuing education. Sage, Los Angeles, CA (2010), 71–81.
20. Matthey S. Are we overpathologising motherhood? J Affect Disord. (2010) 120:263–6. doi: 10.1016/j.jad.2009.05.004
21. Rallis S, Skouteris H, McCabe M, Milgrom J. The transition to motherhood: towards a broader understanding of perinatal distress. Women Birth. (2014) 27:68–71. doi: 10.1016/j.wombi.2013.12.004
22. Hwang WY, Choi SY, An HJ. Concept analysis of transition to motherhood: a methodological study. Korean J Women Health nursing. (2022) 28:8–17. doi: 10.4069/kjwhn.2022.01.04
23. van Raalte LJ, Burke TJ, DeGroot JM, Mellow AJ. Examining changes in affection and “Feeling touched out” after the birth of a child. J Fam Commun. (2023) 23:52–62. doi: 10.1080/15267431.2022.2142229
24. Pawluski JL, Hoekzema E, Leuner B, Lonstein JS. Less can be more: Fine tuning the maternal brain. Neurosci Biobehav Rev. (2022) 133:104475. doi: 10.1016/j.neubiorev.2021.11.045
25. McCormack C, Callaghan BL, Pawluski JL. It’s time to rebrand “Mommy brain”. JAMA Neurol. (2023) 80:335–6. doi: 10.1001/jamaneurol.2022.5180
26. Gross Spector M, Cinamon RG. Identity exploration during the transition to motherhood: facilitating factors and outcomes. Career Dev Int. (2017) 22:829–43. doi: 10.1108/CDI-01-2017-0021
27. Cronin AM. ‘Domestic friends’: women's friendships, motherhood and inclusive intimacy. Sociol Rev. (2015) 63:662–79. doi: 10.1111/1467-954X.12255
28. Doss BD, Rhoades GK. The transition to parenthood: Impact on couples’ romantic relationships. Curr Opin Psychol. (2017) 13:25–8. doi: 10.1016/j.copsyc.2016.04.003
29. Hartup WW. Friendships and their developmental significance. In: McGurk H, editor. Childhood Social Development: Contemporary Perspectives. 1st ed. Psychology Press, London (1992), p. 175–205.
30. Kluwer ES. From partnership to parenthood: A review of marital change across the transition to parenthood. J Fam Theory Rev. (2010) 2:105–25. doi: 10.1111/j.1756-2589.2010.00045.x
31. Leonhardt ND, Rosen NO, Dawson SJ, Kim JJ, Johnson MD, Impett EA. Relationship satisfaction and commitment in the transition to parenthood: A couple-centered approach. J Marriage Fam. (2022) 84:80–100. doi: 10.1111/jomf.12785
32. Berndt TJ. Transitions in friendship and friends' influence. In: Adams GR, Berzonsky MD, editors. Transitions through adolescence: Interpersonal domains and context. 2nd ed. Routledge, New York, NY (2016). p. 57–84.
33. Bina R. The impact of cultural factors upon postpartum depression: a literature review. Health Care Women Int. (2008) 29:568–92. doi: 10.1080/07399330802089149
34. Withers M, Kharazmi N, Lim E. Traditional beliefs and practices in pregnancy, childbirth and postpartum: A review of the evidence from Asian countries. Midwifery. (2018) 56:158–70. doi: 10.1016/j.midw.2017.10.019
35. Roosevelt LK, Pietzmeier S, Reed R. Clinically and culturally competent care for transgender and nonbinary people: A challenge to providers of perinatal care. J Perinat Neonatal Nurs. (2021) 35:142–9. doi: 10.1097/JPN.0000000000000560
36. Cukrowska-Torzewska E, Matysiak A. The motherhood wage penalty: A meta-analysis. Soc Sci Res. (2020) 88:102416. doi: 10.1016/j.ssresearch.2020.102416
37. Delacruz AY, Speer AB. Maternal wall biases and the maybe baby effect. Ind Organ Psychol. (2023) 16:221–4. doi: 10.1017/iop.2023.3
38. Williams JC. The glass ceiling and the maternal wall in academia. New Dir High Educ. (2005) 130):91–105. doi: 10.1002/he.181
39. Ysseldyk R, Greenaway KH, Hassinger E, Zutrauen S, Lintz J, Bhatia MP, et al. A leak in the academic pipeline: Identity and health among postdoctoral women. Front Psychol. (2019) 10:1297. doi: 10.3389/fpsyg.2019.01297
40. Yang T, Kacperczyk A, Naldi L. The motherhood wage penalty and female entrepreneurship. Organ Sci. (2023) 35(1):27–51. doi: 10.1287/orsc.2023.1657
41. Mendoza EFO. Maternal activism in comparative perspective: Past, present, and future. Sociol Compass. (2023) 17:e13088. doi: 10.1111/soc4.13088
42. Poe D. Maternal activism: Mothers confronting injustice. State University of New York Press, Albany, NY (2015). doi: 10.1353/book39135
43. Adams EL, Smith D, Caccavale LJ, Bean MK. Parents are stressed! Patterns of parent stress across COVID-19. Front Psychiatry. (2021) 12:626456. doi: 10.3389/fpsyt.2021.626456
44. Davis AC. Untangling the double bind of carework in green motherhood: An ecofeminist developmental path forward. Women's Stud Int Forum. (2023) 98:102730. doi: 10.1016/j.wsif.2023.102730
45. Logsdon-Conradsen SC, Allred SL. Motherhood and environmental activism: A developmental framework. Ecopsychology. (2010) 2:141–6. doi: 10.1089/eco.2010.0027
46. Shrum TR, Platt NS, Markowitz E, Syropoulos S. A scoping review of the green parenthood effect on environmental and climate engagement. Wiley Interdiscip Reviews: Climate Change. (2023) 14:e818. doi: 10.1002/wcc.818
47. Davis A, Athan A. Ecopsychological development and maternal ecodistress during matrescence. Ecopsychology. (2023) 15(3):281–93. doi: 10.1089/eco.2022.0084
48. Arnold-Baker C. editor. The existential crisis of motherhood. 1st ed. Palgrave Macmillan, Cham (Switzerland) (2020), 346 p.
49. Garland V. Existential responsibility of motherhood. In: The existential crisis of motherhood. Palgrave Macmillan, Cham, Switzerland (2020), p. 57–76. doi: 10.1007/978-3-030-56499-5_4
50. Prinds C, Hvidt NC, Mogensen O, Buus N. Making existential meaning in transition to motherhood—a scoping review. Midwifery. (2014) 30:733–41. doi: 10.1016/j.midw.2013.06.021
51. Athan A, Chung S, Sawyer Cohen J. Spiritual beliefs of mothers with potentially distressing pregnancies. Spirituality Clin Practice. (2015) 2:216. doi: 10.1037/scp0000069
52. Attard J. Spirituality and spiritual care in the transition to motherhood. In: Perspectives on midwifery and parenthood. pringer International Publishing, Cham (2023). p. 181–92.
53. Curtis C, Morgan J, Laird L. Mothers’ gardens in arid soil: A study of religious and spiritual coping among marginalized US mothers with depression. J Spirituality Ment Health. (2018) 20:293–320. doi: 10.1080/19349637.2018.1428139
54. Molina N. The liminal space in motherhood: spiritual experiences of first-time mothers. In: The faith lives of women and girls. Routledge (2016). p. 207–20.
55. Mälkki K. Rethinking disorienting dilemmas within real-life crises: The role of reflection in negotiating emotionally chaotic experiences. Adult Education Quarterly. (2012) 62(3):207–29.
56. Cox J. Thirty years with the Edinburgh Postnatal Depression Scale: voices from the past and recommendations for the future. Br J Psychiatry. (2019) 214:127–9. doi: 10.1192/bjp.2018.245
57. Bonnie RJ, Backes EP, Alegria M, Diaz A, Brindis CD. Fulfilling the promise of adolescence: realizing opportunity for all youth. J Adolesc Health. (2019) 65:440–2. doi: 10.1016/j.jadohealth.2019.07.018
58. Orchard ER, Rutherford HJ, Holmes AJ, Jamadar SD. Matrescence: lifetime impact of motherhood on cognition and the brain. Trends Cognit Sci. (2023) 27(3). doi: 10.1016/j.tics.2023.06.002
59. Montuori A. The complexity of transdisciplinary literature reviews. Complicity: Int J Complexity Educ. (2013) 10:45–55. doi: 10.29173/cmplct20399
Keywords: matrescence, transition to motherhood, maternal mental health, perinatal psychiatry, Perinatal Mood and Anxiety Disorders (PMADs), reproductive health education
Citation: Athan AM (2024) A critical need for the concept of matrescence in perinatal psychiatry. Front. Psychiatry 15:1364845. doi: 10.3389/fpsyt.2024.1364845
Received: 03 January 2024; Accepted: 06 May 2024;
Published: 10 June 2024.
Edited by:
Alison Hermann, Cornell University, United StatesReviewed by:
Ingrid Nkongho, Seleni Institute, United StatesCopyright © 2024 Athan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Aurelie M. Athan, YW1hODFAdGMuY29sdW1iaWEuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.