- 1Department of Nursing, College of Health Sciences, Woldia University, Woldia, Ethiopia
- 2Department of Public Health, College of Health Sciences, Woldia University, Woldia, Ethiopia
- 3Department of Psychiatry, College of Medicine and Health Sciences, Wollo University, Dessie, Ethiopia
- 4School of Medicine, College of Health Sciences, Woldia University, Woldia, Ethiopia
- 5Department of Pediatrics and Child Health Nursing, School of Nursing, College of Medicine and Health Science, Woldia University, Woldia, Ethiopia
- 6Department of Veterinary Parasitology, School of Veterinary Medicine, Wollo University, Dessie, Ethiopia
Background: The experience of war in recent time is very common around the world, and the impact is profound on the mental health of the victims, especially among the young population. The most implicated mental health problem is post-traumatic stress disorder, which comes after an exposure to trauma as a severe and long-term result of the traumatic event. Studies in developed countries revealed this finding, but there is insufficient information in developing countries, where much of war and conflict exist and young population live including Ethiopia. Therefore, this study aims to assess the prevalence and associated factors of post-traumatic stress disorder among high school students who experienced war.
Objective: We assessed the prevalence and factors associated with post-traumatic stress disorder among high school students who experienced war.
Methods: A multi-centered school base cross-sectional study was conducted from May 23 to June 08, 2022. Data were collected from high school students in Woldia town. Bivariable and multivariable logistic regression was used to identify the independent factors associated with post-traumatic stress disorder.
Results: A total of 338 of the 410 students participated in this study (94.5% response rate). The prevalence of post-traumatic stress disorder was 39.2%. In the multivariable analysis, poor social support (AOR = 3.40, 95% CI: 1.45, 7.95), depression (AOR = 3.24, 95% CI: 1.69,6.21), high level of perceived stress (AOR = 2.98, 95% CI: 1.61, 5.50), being in war fighting situation (AOR = 2.85, 95% CI: 1.40, 5.78), and witnessing the murder of family members or friends (AOR = 3.05, 95% CI: 1.47, 6.32) were factors significantly associated with post-traumatic stress disorder at a p-value <0.05.
Conclusions and recommendations: In this study, around two in five of high school students had post-traumatic stress disorder. Independent factors of PTSD were depression, high stress levels, poor social support, witnessing the murder of family members/friends, and being in war fighting situation. We recommend that the Ministry of Education and the Ministry of Health collaborate to integrate mental health services into schools. This focuses on the early detection of students at risk of PTSD, such as those with depression, high perceived stress levels, and exposure to murder or war, and provides necessary social support to prevent PTSD.
Introduction
Adolescence is a time period between childhood and adult. Any person between the ages of 10 and 19 is considered as an adolescent by the World Health Organization (WHO) (1). Because adolescence constitutes a unique stage of development, this population group is particularly susceptible to certain threats and risks that create specific needs and greater vulnerability (2). The WHO states that half of all mental health disorders that are fully developed during adulthood begin before the age of 14 (3).
Post-traumatic stress disorder (PTSD) is one of the trauma and stress-related disorders that develop after experiencing or witnessing a stressful, frightening, or life-threatening event like combats, disasters, or sexual assaults (4). Individuals with PTSD suffer from loneliness, irritability, guilt, difficulty concentrating, difficulty sleeping, and dreams or flashbacks that bring back the horrific incident. They also attempt to avoid circumstances, people, and places that remind them of the traumatic event (5). In general, the symptoms of PTSD in adolescents are similar to the symptoms of PTSD in adults (6). Adolescents may show specificities with extreme reactions than in adults such as becoming more aggressive, difficulty of controlling their impulses, and substances misuse (7). In addition, adolescents frequently experience nightmares, emotional insensitivity, conscious avoidance of anything that could trigger memories of the traumatic event, as well as frequent depression, antisocial behavior, physical complaints, decreased academic performance, sleeping problems, and suicidal thoughts (8).
Armed conflict, war, or insurgency that affects civilian populations increased toward the end of the 20th century. At this time, violence and attacks against civilian targets are common in wars around the world, which lead to population danger, insecurity, and anxiety. More than a billion youth worldwide live in countries where an armed conflict, war, or terrorism is common (9). In Ethiopia, Tigray People Liberation Front (TPLF) forces have been fighting an open assault against the Federal Republic Government of Ethiopia at Amhara and Afar regions since June 2021, leaving the population there in terrible economic and social circumstances. The invading force targeted a number of rural farmers, city people, teachers, and medical professionals who were not politically engaged (10). Children and adolescents are the most at risk of suffering the effects of these hostilities because they must negotiate the tasks of normal developmental growth against a backdrop of insecurity and violence, which increases their vulnerability and susceptibility (11).
After trauma, up to 36% of adolescents exposed to trauma have a risk of developing PTSD (11). A meta-analysis study from North America, Europe, Australia, and Asia revealed that approximately 16% of trauma-exposed adolescents had PTSD (12). A recent systematic review and meta-analysis study among adolescents in low- and middle-income countries (LMICs) reported that the prevalence of PTSD range from 0.2% to 87% (13). According to a meta-analysis of studies published from 1998 to 2011, the prevalence of PTSD among adolescents exposed to a traumatic event was 15.9% (12). Another meta-analysis study done among adolescents showed that the prevalence of PTSD was 19.9% after road traffic accidents (14). In addition, studies done among adolescents reported that the prevalence of PTSD after an earthquake was 58.3% in Indonesia, 66.7% in Iran, and 43.3% in Nepal (15–17). Furthermore, other studies done among school students showed that the prevalence of PTSD was 26.8% in Kenya (18), 16.4% in Palestine (19), 31% in Jordan of Syrian refuge (20), 53% in Syrian (21), 19.3%, 63.9%, and 70.4% in Morocco studies (22–24), 46.3% in China (25), 60% in Uganda (26), and 61% in Iraq (27). Some studies from Ethiopia showed that the prevalence of PTSD among individuals in war-affected areas was 59.8% in Northwest Ethiopia (28), 58.4% in South Ethiopia (29), 17.1% in West Ethiopia (30), 37.3% in Addis Ababa (31), 19.4% in Dessie town (32), and 56.28% in Woldia town (33).
Different variables can affect the prevalence of PTSD among adolescents as studies have reported. These variables—which are categorized as variables that occurred prior to the traumatic event, such as female sex (29, 34, 35), younger age, poor social support, chronic medical illness, drinking alcohol (31, 36–44), and a previous history of mental illness like depression symptoms (28, 29, 43, 45); factors which occurred during traumatic events, like witnessing the death of a family member or friends (29, 36, 46–49), type of trauma, and serious physical injury (50–52); and variables which occurred following traumatic events, for example, having a high level of perceived life stress and destruction of property—were the predictors of PTSD (28, 31, 53–55).
The effect of PTSD on school-age adolescents is profound as it will lead to low self-esteem, alcoholism, and other problems such as substance abuse, poor academic performance, poor relationship with family members, and even social isolation and self-harming behaviors (52, 56, 57). Therefore, in order to prevent more suffering, post-traumatic stress disorder symptoms need to be handled as soon as they arise (15). Even if Ethiopia is experiencing different conflicts recently, nearly around all regions, but limited studies were done on the impacts of these conflicts on the development of post-traumatic stress disorder, especially on the mental health of adolescents. Therefore, the aim of this study was to assess the level of post-traumatic stress disorder and its predictors among high school students. The research questions are as follows: 1. How much is the magnitude of PTSD among high school adolescents who experienced war? 2. Which factors are affecting the magnitude of PTSD among high school adolescents who experienced war?
Materials and methods
Study area and populations
In May 2022, a multi-centered, school-based, cross-sectional study was carried out at four high schools in Woldia town, Northeastern Ethiopia. The schools are Mesenado Secondary and Preparatory School, Millennium Secondary and Preparatory School, Genetie Secondary and Preparatory School, and Woldia Secondary and Preparatory School (58). The study area is located 521 kilometers from Addis Ababa, the capital city of Ethiopia, in the North Wollo Zone of the Amhara National Regional State. In the study area, there were 46,139 residents overall, including 23,000 men and 23,139 women. Moreover, 80.49% of the total residents are Ethiopian Orthodox Christians religion followers, while 18.46% are Muslims and the rest are Protestants. This study included all secondary and preparatory school students who had attended their classes during the period of data collection and had lived in the study area at least for the last preceding year of the war. Students who were unable to communicate, those who were acutely sick during the time of data collection, and students who lived in the study area for less than a year during the conflict were excluded from the study (58).
Sample size determination
The sample size was determined by taking a single population proportion formula assumption. We calculated the sample size using the proportion from a previous study with proportion (p) of 58.4% (29), with 95% confidence interval (CI) and margin of error 5%, and 10% non-response rate. Then, the final sample size was 410.
Student recruitment procedures
Before the actual data collection time, the students were first stratified by their grade level as grade 9, grade 10, grade 11, and grade 12, considering each grade level as strata. The data we get on education of the study region showed that there were a total of 5,100 high school students (58). Among these, grade 9 accounts for 1,606, grade 10 accounts for 1,230, grade 11 accounts for 1,179, and grade 12 accounts for 1,085 of the students from the total number of high school students. Then, we made a proportional allocation for each stratum (grade levels), and as a result, 129 students from grade 9, 99 students from grade 10, 95 students from grade 11, and 87 students from grade 12 were drawn. Finally, a computer-generated lottery method using the students’ identification number was applied to select the study participants from each stratum. In the end, the selected students in each stratum were taken to one hall, which has a separate entry and exit for the study participants, and each study participant was entered and filled the questionnaire and went out through the exit of the hall without contacting another study participant to ensure no information sharing and secure their anonymity. Then, the questionnaires were administered after orientation through direct contact with the study participants but keeping their anonymity, and all the filled questionnaires were collected by the data collectors.
Measurement and data collection
PTSD was measured by using a 20-item Post-Traumatic Checklist (PCL-5) with scores ranging from 0 to 80 with a five-point Likert scale (0 = not at all, 1 = a little bit, 2 = moderately, 3 = quite a bit, 4 = extremely). The participants were asked based on their experiences over the last month. Then, summing up all points, those participants scoring ≥33 were considered as having PTSD. PCL-5’s validity and reliability have been examined and demonstrated and were used to assess PTSD. PCL-5 was used and validated in Rwanda students to have internal consistency (Cronbach alpha) of 0.934, sensitivity of 88.7%, and specificity of 88.9% (59). The internal consistency (Cronbach alpha) of PCL-5 in this study was 0.89. In the present study, the nine-item Patient Health Questionnaire (PHQ-9), with scores ranging from 0 to 27 with four-point Likert scale (0 = not at all, 1 = several days, 2 = more than half the days, 3 = nearly every day), was used to assess depression, with a score of 10 or higher indicating depression. The participants were asked based on their experiences over the past 2 weeks. PHQ-9 was validated in Nigerian students, and the internal consistency (Cronbach alpha) was 0.85, the sensitivity was 87.9%, and the specificity was 98.9%, respectively (60). The internal consistency (Cronbach alpha) of (PHQ-9) in this study was 0.84.
Perceived life stress was assessed using Perceive Stress Scale (PSS) scale, which is widely used as a psychological instrument to measure the perception of stress. PSS has a five-point Likert scale (0 = never, 1 = almost never, 2 = sometimes, 3 = fairly often, 4 = very often) with 0–40 range. The participants were asked based on their experiences over the last month. Respondents with scores between 0 and 13 were considered to have a low level of perceived stress, those between 14 and 26 were considered to have a moderate level of perceived stress, and participants who scored between 27 and 40 were considered to have a high level of perceived stress. A study done in Bhutan showed the internal consistency of this PSS as 0.90 (61). The internal consistency (Cronbach alpha) of Perceived Stress Scale (PSS) in this study was 0.82.
The three-item Oslo (Oslo-3) tool was used to assess the level of social support of the participants with a score range of 3–14. Participants with a score of 3–8 were categorized as having a poor social support level, those with a score of 9–11 were categorized as having a moderate social support level, and participants with a score between 12 and 14 were categorized as having a strong social support level (62). A study done in Nigeria showed that the internal consistency (Cronbach alpha) of Oslo-3 social support was 0.5 (63), and the internal consistency (Cronbach alpha) of Oslo-3 social support in this study was 0.79.
Substance use history of the participants including Khat, tobacco, and alcohol was assessed using yes/no (yes = 1, no = 0) questionnaires adapted from the ASSIST (Alcohol, Smoking, and Substance Involvement Screening Test) (64). The questions include about ever substance use history as well as current substance use history. Ever substance use history asks about any history of substance use in the individual’s life, and current substance use history asks about history of substance use in the past 3 months. Anxiety was assessed using GAD-7, which is a self-administered questionnaire designed for screening and measuring the severity of generalized anxiety disorder. GAD-7 consists of seven items that respondents respond to base on their experiences over the past 2 weeks. GAD-7 had a four-point Likert scale, with each item scored from 0 (not at all) to 3 (nearly every day) and with the score ranging from 0 to 21; individuals who scored 10 and above were considered as having anxiety (65). GAD-7 has a sensitivity of 89% and a specificity of 82% (66). The internal consistency of GAD-7 in this study was 0.90. Socio-demographic characteristics such as age, sex, and grade level were collected by using structured socio-demographic questionnaires (sex of participants: male = 1, female = 0, urban residence = 1, rural residence = 0). Factors like family history of mental illness, trauma-related factors, and history of chronic medical illness were assessed using a structured yes/no (yes = 1, no = 0) questionnaire.
The collected data were coded, edited, entered, and checked into the computer using EPI data version 4.6.02 and imported to STATA version 14.0 to generate descriptive statistics like means, standard deviation, frequency, and percentages. To determine an association between dependent and independent variables, adjusted odds ratios were used using logistic regression, and the significance level was determined using a confidence interval of 95%. Bivariable and multivariable logistic regression, respectively, was used to identify the independent predictors of PTSD. Each independent variable was separately entered in the bivariable analysis. Then, variables with a p-value <0.2 on bivariable analysis were entered into multivariate analysis. Then, variables that showed a statistically significant association with a p-value <0.05 on multi-variable analysis were considered to be the predictors of PTSD.
Statistical analysis
Parametric properties of data collection tools
As checked by Shapiro–Wilk test for PCL-5 (p = 0.39), PHQ-9 (p = 0.25), PSS (p = 0.48), Oslo-3 (p = 0.65), and GAD-7 (p = 0.92), the revealed p-values were insignificant for each tool; this indicated a normal distribution. Because the data were normally distributed, we calculated the mean for each independent variable: PCL-5 (mean = 29.6, standard deviation = 2.35), PHQ-9 (mean = 11.5, standard deviation = 1.99), PSS (mean =25.4, standard deviation = 2.21), Oslo-3 (mean = 9.405, standard deviation = 2.54), and GAD-7 (mean = 10.3, standard deviation = 2.35). The skewness test of these tools indicated the following: PCL-5 = 0.0730, PHQ-9 = 0.078, PSS = 0.060, Oslo-3 = 0.62, and GAD-7 = 0.082. Multi-collinearity was assessed for the independent variables, and VIF was less than 10.
Data quality control
To control the quality of data, the questionnaire was translated appropriately into the local Amharic language with a local language expert. The training was given to data collectors and supervisors, and each completed questionnaire was checked and the necessary feedback was also offered to data collectors each following morning. The questionnaire was pretested 1 week before the actual data collection time on 5% (n = 21) of the study participants who were not included in the main study.
Results
Socio-demographic characteristics of participants
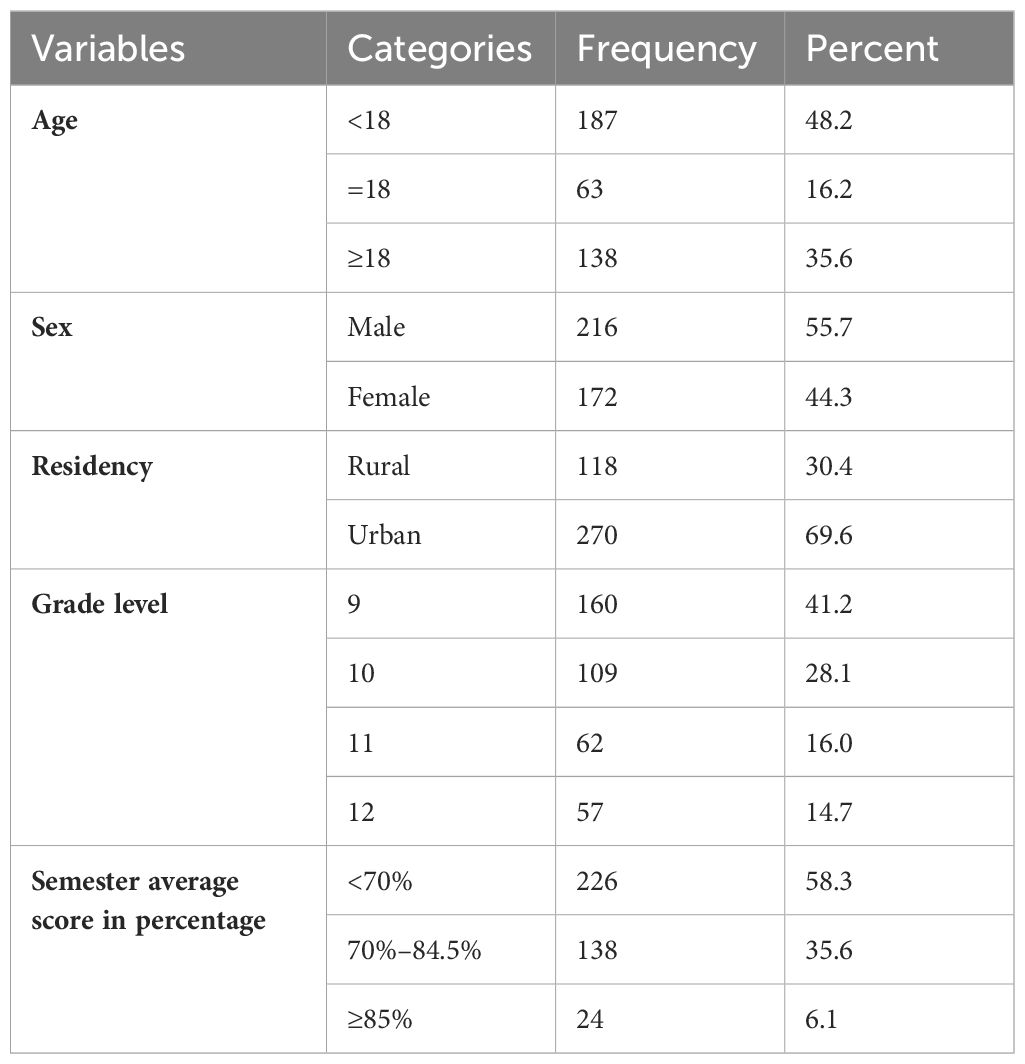
Data were obtained from 388 high school students, with a response rate of 94.5%. The mean age of the participants was 17.82 ± 1.66, ranging from 14 to 25 years old, and the majority of the ages of 48.2% of the participants was ranging between 14 and 18 years old. More than half of the number (55.67%) of the participants were male, and 69.59% of them were from urban areas, while the rest were from rural areas as shown in Table 1.
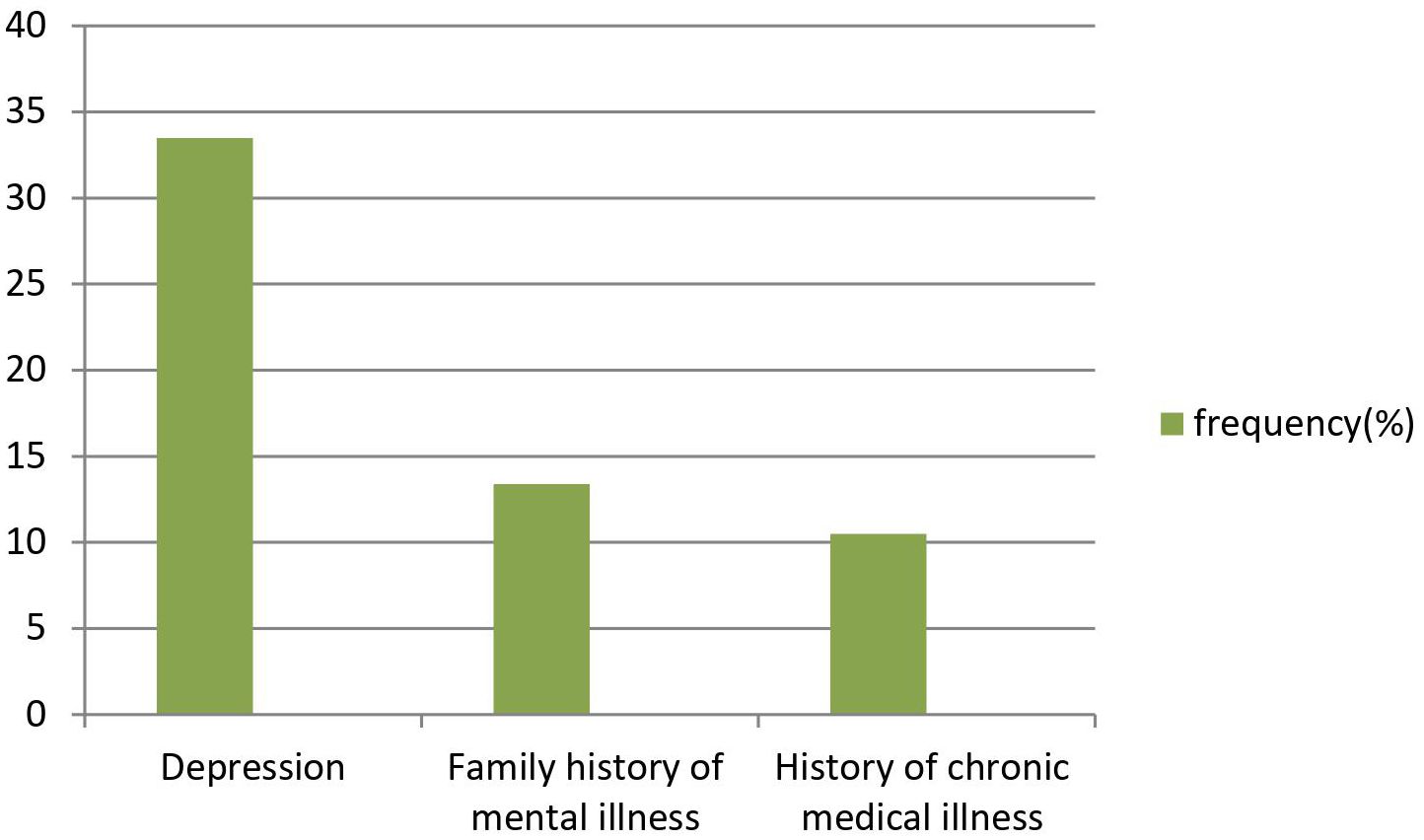
Clinical characteristics of the respondents
Out of the total participants, 10.57% of students had a history of chronic medical illness, 13.40% of students had a family history of mental illness, and 33.51% had depression as seen in Figure 1.
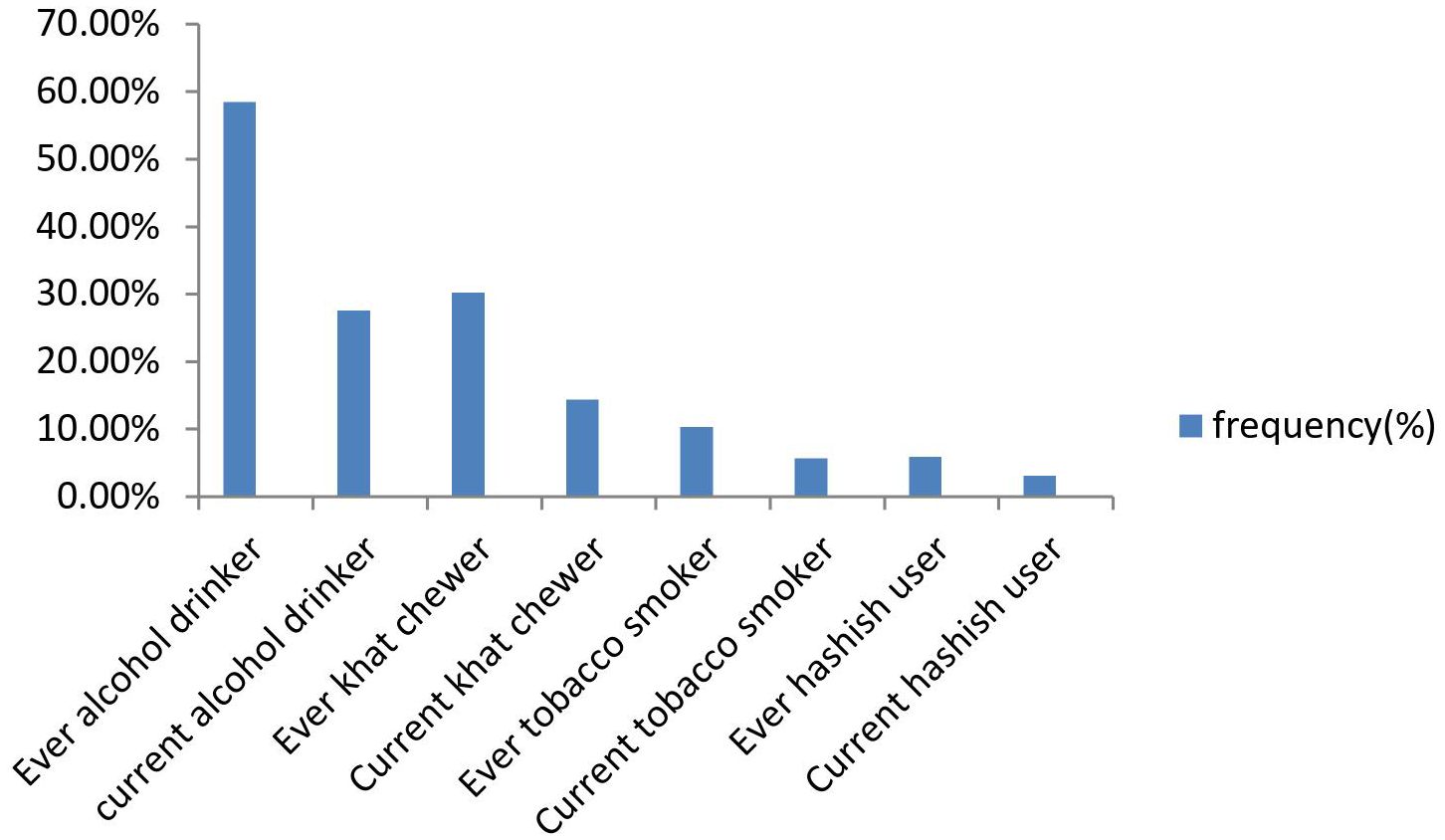
Substance-related characteristics of the participants
Regarding substance use, out of the total participated students, 58.5% were ever alcohol drinkers, whereas Khat and cigarette ever users were 30.2% and 10.3%, respectively, and 27.6% of them were current alcohol drinkers as shown in Figure 2.
Individual trauma type and psychosocial-related characteristics of participants
Among the study participants, 52.8% were in a war fighting situation, 16.5% had a destruction of property, 19.1% witnessed the murder of family or friends, 16% had ill health without medical care, 13.1% had a strong social support, 28.6% had a moderate social support, and 58.3% had a poor social support, and 37.1%, 20.9%, and 42.0%, of the respondents had a high, moderate, and low level of perceived stress, respectively.
Prevalence and associated factors of post-traumatic stress disorder
In this study, the overall prevalence of post-traumatic stress disorder among high school students was 39.2% (95% CI: 34.4, 44.1). Having depression, high and moderate levels of perceived stress level, witnessing the murder of family or friends, having ill health without medical care, being tortured or beaten, witnessing the murder of a stranger, imprisonment against will, forced separation from the family, having moderate and poor social support levels, and being in a war fighting situation were factors associated with post-traumatic stress disorder at p < 0.2 in binary logistic regression.
Finally, in the analysis of multivariable logistic regression model, this study showed that having depression, high and moderate levels of perceived stress level, witnessing the murder of family members or friends, being in a war fighting situation, and having poor social support were found to be significantly associated with post-traumatic stress disorder, with 95% of CI and at p-value <0.05 as shown in Table 2.

Table 2 Bivariable and multivariable analysis of factors associated with post-traumatic disorder among high school students in Woldia town, 2022 (n = 388).
Students who had poor social support were 3.4 times more likely to have post-traumatic stress disorder compared to students who had a strong social support (AOR = 3.40, 95% CI: 1.45, 7.95). Students who witnessed the murder of family members or friends were about 3.1 times more likely to have post-traumatic stress disorder than students who did not witness the murder of family members/friends (AOR = 3.05, 95% CI: 1.47, 6.32).
Students who were in a war fighting situation had 2.9 times higher post-traumatic stress disorder than students who were not in a war fighting situation (AOR = 2.85, 95% CI: 1.40, 5.78). Students who had depression reported 3.2 times higher post-traumatic stress disorder than students who had not depression (AOR = 3.24, 95% CI: 1.69, 6.21). Students with a high level of perceived stress level had three times higher post-traumatic stress disorder than students who have a low level of perceived stress (AOR = 2.98, 95% CI: 1.61, 5.50).
Discussion
The findings of the current study showed that the prevalence of post-traumatic stress disorder among high school students in Woldia town was 39.2% (95% CI: 34.4, 44.1), which is similar with studies done in Palestine, Turkey, Nepal, and Ethiopia with a reported prevalence of 36%, 40.6%, 43.3%, and 36.5%, respectively (67–69).
However, the prevalence of post-traumatic stress disorder in this study was higher than studies done in Ukraine 28% (48), Jordan 31% (20), Kenya 26.8% (18), Saudi Arabia 24.8% (70), and Morocco 19.3% (22). The possible reason for this difference may be due to the difference in the instruments that they used—for example, a study done in Ukraine was conducted using the Harvard Trauma Questionnaire tool; in the Kenya study, UCLA PTSD-RI (UCLA PTSD Reaction Index) tool was used; and in the Jordan study, the Child Post-traumatic Stress Disorder Symptom Scale (CPSS) tool was used; whereas in this study, the PCL-5 with extended criteria A modified and having better internal consistency was used (71). Different studies evidenced that the difference in the instrument tool affects the prevalence of post-traumatic stress disorder (29, 31, 40). Another reason might be due to the difference in the timing of these studies when conducted after the study participants faced a traumatic event—for example, a study done in Ukraine was conducted 2 years after Russia invaded areas of Eastern Ukraine, a study done among Syrian refugees in Jordan was conducted after 3 years of conflict, but the current study was conducted 12 months after the participants experienced traumatic events. If studies are conducted long after the traumatic events, the participants will have a probability of decreased severity perception about the traumatic events due to recall bias, which may affect the participants’ report (72). Furthermore, the difference in the prevalence rate could be explained by the difference in trauma type and socio-cultural difference among study participants of these studies. On the other hand, the current prevalence was lower than the prevalence of studies done in China with 46.3% (25), Syria with 53% (21), and Uganda with 60% (26), respectively. The difference may be attributed to the varying proportions of study participants with a comorbid mental illness in these studies—for instance, in studies conducted in Uganda and Syria, 58% and 51.5% of the participants, respectively, had depression. In contrast, our study found that only 33.5% of the participants had comorbid depression. Various studies have shown that having comorbid depression can elevate the risk of developing post-traumatic stress disorder (28, 29, 73–75). Another reason for this discrepancy could be the differences in the assessment tools, study designs, and the type and degree of exposure experienced by the participants in these studies.
The odds of post-traumatic stress disorder were 3.3 times higher among high school students who had poor social support compared to those who had strong social support. This finding was supported by studies done in Ethiopia (31, 40), Nigeria (39),US (37), China (36), and UK (38). The reason for this finding may be due to the fact that individuals with poor social support may lack the emotional and practical assistance needed to cope with the aftermath of traumatic events. Without support from friends, family, or community, they are more likely to experience heightened levels of stress and anxiety, which can contribute to the development of PTSD. Another reason could be explained by the lack of social support which may be expressed through a perception of being unsupported, which can exacerbate feelings of isolation and helplessness. When individuals believe that they have no one to turn to, their ability to process and recover from traumatic experiences diminish, which increases the likelihood of PTSD (76, 77). The finding of this particular relationship between social support and the risk of PTSD underscoring the importance of fostering strong social support systems and supportive environment within schools and communities by promoting positive relationships among students, teachers, families, and community members is essential to mitigate the risk of PTSD. In addition, counseling services and mental health resources are offered to students, particularly those who may be at risk due to limited social support. This can include individual counseling, support groups, and access to mental health professionals.
The odds of post-traumatic stress disorder were three times higher among students who witnessed the murder of family members or friends compared to those who had not. Studies done in Ethiopia (29, 46), Canada (49), China (36), Ukraine (48), and Turkey (47) supported this finding. The reason for this finding may be due to the fact that witnessing the murder of a loved one is an extremely distressing and traumatic experience. The intensity and severity of this trauma can significantly impact the individual’s psychological well-being, increasing their vulnerability to PTSD. Another reason might be due to the fact that witnessing the murder of a family member or friend can shatter a person’s sense of safety and security in the world. This loss of trust in their environment and the people around them can contribute to the development of PTSD symptoms, as individuals may constantly feel on the edge or hyper-vigilant to potential threats. Moreover, this finding may be attributed to the intertwining of grief resulting from the loss of a loved one and trauma stemming from witnessing their murder. This combination creates a complex and lasting psychological burden, intensifying PTSD symptoms and complicating the healing and recovery process for individuals (78, 79). This implies offering immediate access to mental health professionals trained in trauma-focused therapy to provide support and intervention for students who have witnessed such traumatic events. Adopt trauma-informed approaches in schools, ensuring that all interactions and interventions are sensitive to the needs of students who have experienced trauma. This may involve modifying disciplinary practices, providing accommodations for academic performance, and creating a supportive school environment.
The odds of developing post-traumatic stress disorder (PTSD) were 3.5 times higher in students who had been in war fighting situations compared to those who had not. This finding was supported by studies done in Ethiopia (80), US (38), Iraq (81), and Turkey (82). The possible explanation for this finding could be that individuals in war zones are frequently exposed to highly traumatic events such as violence, death, and destruction. This exposure significantly increases their risk of developing PTSD (83). Another reason for this finding might be that persistent threat to life and the constant state of alertness required in war fighting situations can lead to chronic stress, which is a known contributor to PTSD (84). Additionally, the possible reason behind this finding might be that, during war situations, individuals often witness or directly experience severe violence, including injuries and deaths of fellow soldiers, civilians, and even family members. Such experiences can profoundly impact their psychological health (85). Furthermore, the chaotic nature of war can result in the loss of family members and friends, disrupting social support systems. The disintegration of these support networks leaves individuals more vulnerable to PTSD (86). Thus, it is essential to create a safe environment where affected students can share their experiences, feelings, and concerns with peers who have undergone similar trauma. Peer support can be invaluable in the healing process. In addition, it is imperative to teach students resilience-building skills and coping strategies to help them manage stress, regulate emotions, and navigate challenging situations. This may include mindfulness exercises, relaxation techniques, and problem-solving skills training.
Students with depression were 3.2 times more likely to develop post-traumatic stress disorder (PTSD) compared to those without depression. Similar studies conducted in Greece (87), Indonesia (15), and Ethiopia (28) supported this finding. The reason for this might be due to the fact that individuals with depression are more likely to have encountered traumatic events, which subsequently increases their risk of developing PTSD (88). Another explanation for this finding might be due to individuals who have currently depression and may have a previous history of this depression or other psychological problems, both of which can increased the risk of PTSD (89, 90). This finding implies implementing routine mental health screenings to identify students who may be experiencing depression. This can be done through surveys, questionnaires, or discussions with school counselors or mental health professionals. It is also advisable to work closely with mental health professionals, including therapists, psychologists, and psychiatrists, to develop comprehensive treatment plans for students with depression and PTSD. This may involve coordinating care, sharing information, and ensuring continuity of services. Additionally, any underlying traumatic experiences that may be contributing to both depression and PTSD are explored and addressed.
Students with high levels of perceived stress were three times more likely to develop post-traumatic stress disorder (PTSD) compared to those with low levels of perceived stress. This finding was supported by studies conducted in Ethiopia (31), Qatar (54), China (55), Bosnia, and Herzegovina (53). The possible explanation for this finding might be due to the fact that the negative perceptions regarding the harmful consequences of continuous threats can expedite the onset and continuation of PTSD (91). Practicing stress management programs or workshops teaches students coping skills and resilience-building techniques, including relaxation exercises, mindfulness practices, and time management strategies. Healthy lifestyle habits like engaging in regular physical activity, maintaining a balanced diet, getting adequate sleep, and practicing self-care techniques to help reduce stress levels are also promoted.
Limitations of the study
This study is conducted with some limitations. One of the limitations of this study was that there may be recall bias since the study collected retrospective data of 12 months. Because of limited resources and funding, using self-report, sometimes adolescents may exaggerate their responses and report more severe symptoms; this may overestimate the finding of this study. Adolescents repeatedly discuss their experiences with each other, and this sharing of stories might influence their reports of their own experiences.
Conclusions and recommendations
This study revealed that around two out of five high school students in the sample had experienced post-traumatic stress disorder. The independent variables that affect post-traumatic stress disorder among high school students are depression, high perceived level of stress, poor social support, witnessing the murder of family members or friends, and being in a war fighting situation. Therefore, we recommend that the Ministry of Education shall work with the Ministry of Health to include mental health professionals in addition to counseling psychologists and implement mental health services in high schools. They should implement mental health services, including the early detection of students at risk of PTSD, such as those who have depression, a high level of perceived stress, been exposed to war, or witnessed the murder of family members or friends. Providing social support to students is essential to prevent PTSD.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
All procedures were conducted according to the ethical standards of the Declaration of Helsinki. The study was approved by the Institutional Review Board (IRB) of the University of Gondar. Information about the study was explained to each study participant in the information sheet. Written informed consent from the study participants who were greater than 18 years old and assent from those less than 18 years old from parents/caregiver/guardians were obtained. The right to refuse or discontinue participation at any time and the chance to ask anything about the study was given. The privacy and confidentiality of the study participants’ information were kept at every stage of data processing by not including any personal identifiers in the questionnaire. Students were not forced to participate and receive any monetary incentive, and it was solely voluntary-based.
Author contributions
MK: Conceptualization, Data curation, Methodology, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SF: Conceptualization, Data curation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. TA: Conceptualization, Data curation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. NT: Conceptualization, Data curation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. AZ: Conceptualization, Data curation, Supervision, Validation, Visualization, Writing – review & editing. GK: Conceptualization, Data curation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. BA: Conceptualization, Data curation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. ES: Conceptualization, Data curation, Methodology, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to express our thanks to the University of Gondar for giving us the chance to conduct this research. The authors’ appreciation also goes to the study participants, data collectors, and supervisors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Csikszentmihalyi M . “adolescence”. Encyclopedia Britannica. (2024). Available at: https://www.britannica.com/science/adolescence. (Accessed 20 June 2024).
2. World Health O. Global Accelerated Action for the Health of Adolescents (AA-HA)!: guidance to support country implementation. Geneva, Swetherland: World Health Organization (2017).
3. Hewlett E, Moran V. Making mental health count: the social and economic costs of neglecting mental health care: OECD. (2014), 1–246. doi: 10.1787/2074319x
4. Levin AP, Kleinman SB, Adler JS. DSM-5 and posttraumatic stress disorder. J Am Acad Psychiatry Law Online. (2014) 42:146–58.
5. American Psychiatric Association D, American Psychiatric A. Diagnostic and statistical manual of mental disorders: DSM-5. Washington, DC: American psychiatric association (2013). doi: 10.1176/appi.books.9780890425596
6. Dyregrov A, Yule W. A review of PTSD in children. Child Adolesc Ment Health. (2006) 11:176–84. doi: 10.1111/j.1475-3588.2005.00384.x
7. Pelcovitz D, Kaplan S. Post-traumatic stress disorder in children and adolescents. Child Adolesc Psychiatr Clinics. (1996) 5:449–70. doi: 10.1016/S1056-4993(18)30375-4
8. Bui E, Ohye B, Palitz S, Olliac B, Goutaudier N, Raynaud J-P, et al. Acute and chronic reactions to trauma in children and adolescents. Geneva: IACAPAP International Association for Child and Adolescents Psychiatry and Allied Professions (2014).
9. Chrisman AK, Dougherty JG. Mass trauma: Disasters, terrorism, and war. Child Adolesc Psychiatr Clinics. (2014) 23:257–79. doi: 10.1016/j.chc.2013.12.004
10. Engida AE. The scene of Wollo university during the invasion of TPLF led force. Abyssinia J Business Soc Sci. (2022) 7:1–18. doi: 10.20372/ajbs.2022.7.1.527
11. Frounfelker RL, Islam N, Falcone J, Farrar J, Ra C, Antonaccio CM, et al. Living through war: Mental health of children and youth in conflict-affected areas. Int Rev Red Cross. (2019) 101:481–506. doi: 10.1017/S181638312000017X
12. Alisic E, Zalta AK, Van Wesel F, Larsen SE, Hafstad GS, Hassanpour K, et al. Rates of post-traumatic stress disorder in trauma-exposed children and adolescents: meta-analysis. Br J Psychiatry. (2014) 204:335–40. doi: 10.1192/bjp.bp.113.131227
13. Yatham S, Sivathasan S, Yoon R, da Silva TL, Ravindran AV. Depression, anxiety, and post-traumatic stress disorder among youth in low and middle income countries: a review of prevalence and treatment interventions. Asian J Psychiatry. (2018) 38:78–91. doi: 10.1016/j.ajp.2017.10.029
14. Dai W, Liu A, Kaminga AC, Deng J, Lai Z, Wen SW. Prevalence of posttraumatic stress disorder among children and adolescents following road traffic accidents: a meta-analysis. Can J Psychiatry. (2018) 63:798–808. doi: 10.1177/0706743718792194
15. Marthoenis M, Ilyas A, Sofyan H, Schouler-Ocak M. Prevalence, comorbidity and predictors of post-traumatic stress disorder, depression, and anxiety in adolescents following an earthquake. Asian J Psychiatry. (2019) 43:154–9. doi: 10.1016/j.ajp.2019.05.030
16. Sharma A, Kar N. Posttraumatic stress, depression, and coping following the 2015 Nepal earthquake: a study on adolescents. Disaster Med Public Health preparedness. (2019) 13:236–42. doi: 10.1017/dmp.2018.37
17. Ziaaddini H, Nakhaee N, Behzadi K. Prevalence and correlates of PTSD among high school students after the earthquake disaster in the city of Bam, Iran. Am J Appl Sci. (2009) 6:130–2. doi: 10.3844/ajassp.2009.130.132
18. Mbwayo AW, Mathai M, Harder VS, Nicodimos S, Vander Stoep A. Trauma among Kenyan school children in urban and rural settings: PTSD prevalence and correlates. J Child Adolesc trauma. (2020) 13:63–73. doi: 10.1007/s40653-019-00256-2
19. Qeshta H, Hawajri AMA, Thabet AM. The relationship between war trauma, PTSD, anxiety and depression among adolescents in the Gaza Strip. Health Sci J. (2019) 13:621. doi: 10.21767/1791-809X.1000621
20. Beni Yonis O, Khader Y, Jarboua A, Al-Bsoul MM, Al-Akour N, Alfaqih MA, et al. Post-traumatic stress disorder among Syrian adolescent refugees in Jordan. J Public Health. (2020) 42:319–24. doi: 10.1093/pubmed/fdz026
21. Kakaje A, Al Zohbi R, Alyousbashi A, Abdelwahed RNK, Aldeen OH, Alhalabi MM, et al. Post-traumatic stress disorder (PTSD), anger and mental health of school students in Syria after nine years of conflict: a large-scale school-based study. psychol Med. (2022) 52:1923–33. doi: 10.1017/S0033291720003761
22. Astitene K, Barkat A. Prevalence of posttraumatic stress disorder among adolescents in school and its impact on their well-being: a cross-sectional study. Pan Afr Med J. (2021) 39:1–11. doi: 10.11604/pamj.2021.39.54.27419
23. Astitene K, Aguenaou H, Lahlou L, Barkat A. Prevalence of post-traumatic stress disorder among school-age adolescent. Int Neuropsychiatr Dis J. (2020) 14:40–9. doi: 10.9734/indj/2020/v14i130121
24. Astitene K, Lahlou L, Barkat A. Post traumatic stress disorder among adolescents schooled in public schools. Open Access Library J. (2018) 5:1–25. doi: 10.4236/oalib.1105019
25. Qi J, Yang X, Tan R, Wu X, Zhou X. Prevalence and predictors of posttraumatic stress disorder and depression among adolescents over 1 year after the Jiuzhaigou earthquake. J Affect Disord. (2020) 261:1–8. doi: 10.1016/j.jad.2019.09.071
26. Ainamani HE, Weierstall-Pust R, Bahati R, Otwine A, Tumwesigire S, Rukundo GZ. Post-traumatic stress disorder, depression and the associated factors among children and adolescents with a history of maltreatment in Uganda. Eur J Psychotraumatol. (2022) 13:2007730. doi: 10.1080/20008198.2021.2007730
27. Al-Hadethe A, Hunt N, Thomas S, Al-Qaysi A. Prevalence of traumatic events and PTSD symptoms among secondary school students in Baghdad. Eur J Psychotraumatol. (2014) 5:23928. doi: 10.3402/ejpt.v5.23928
28. Ali D, Azale T, Wondie M, Tadesse J. About six in ten survivors of the november 2020 Maikadra massacre suffer from posttraumatic stress disorder, northwest Ethiopia. Psychol Res Behav Manage. (2022) 15:251–60. doi: 10.2147/PRBM.S338823
29. Madoro D, Kerebih H, Habtamu Y, G/Tsadik M, Mokona H, Molla A, et al. Post-traumatic stress disorder and associated factors among internally displaced people in South Ethiopia: a cross-sectional study. Neuropsychiatr Dis Treat. (2020), 2317–26. doi: 10.2147/NDT.S267307
30. Golja EA, Labata BG, Mekonen GF, Dedefo MG. Post-traumatic stress disorder and associated factors among traumatic patients attended in four government hospitals, West Ethiopia. Open Public Health J. (2020) 13:1–6. doi: 10.2174/1874944502013010576
31. Asnakew S, Shumet S, Ginbare W, Legas G, Haile K. Prevalence of post-traumatic stress disorder and associated factors among Koshe landslide survivors, Addis Ababa, Ethiopia: a community-based, cross-sectional study. BMJ Open. (2019) 9:e028550. doi: 10.1136/bmjopen-2018-028550
32. Anbesaw T, Zenebe Y, Asmamaw A, Shegaw M, Birru N. Post-traumatic stress disorder and associated factors among people who experienced traumatic events in dessie town, Ethiopia, 2022: a community based study. Front Psychiatry. (2022) 13:1026878. doi: 10.3389/fpsyt.2022.1026878
33. Kassaye A, Demilew D, Fanta B, Mulat H, Ali D, Seid J, et al. Post-traumatic stress disorder and its associated factors among war-affected residents in Woldia town, North East Ethiopia, 2022; community based cross-sectional study. PloS One. (2023) 18:e0292848. doi: 10.1371/journal.pone.0292848
34. Afana AH, Dalgard OS, Bjertness E, Grunfeld B, Hauff E. The prevalence and associated socio-demographic variables of post-traumatic stress disorder among patients attending primary health care centres in the Gaza Strip. J Refugee Stud. (2002) 15:283–95. doi: 10.1093/jrs/15.3.283
35. Shalev A, Liberzon I, Marmar C. Post-traumatic stress disorder. N Engl J Med. (2017) 376:2459–69. doi: 10.1056/NEJMra1612499
36. Cheng Y, Wang F, Wen J, Shi Y. Risk factors of post-traumatic stress disorder (PTSD) after Wenchuan earthquake: a case control study. PloS One. (2014) 9:e96644. doi: 10.1371/journal.pone.0096644
37. Hourani L, Williams J, Bray RM, Wilk JE, Hoge CW. Gender differences in posttraumatic stress disorder and help seeking in the US Army. J women’s Health. (2016) 25:22–31. doi: 10.1089/jwh.2014.5078
38. Iversen AC, Fear NT, Ehlers A, Hughes JH, Hull L, Earnshaw M, et al. Risk factors for post-traumatic stress disorder among UK Armed Forces personnel. psychol Med. (2008) 38:511–22. doi: 10.1017/S0033291708002778
39. Mosaku K, Akinyoola A, Olasinde A, Orekha O. Predictors of posttraumatic stress in patients admitted to a trauma unit following road traffic accident (RTA). J Psychiatry. (2014) 17:121. doi: 10.4172/Psychiatry.1000121
40. Yohannes K, Gebeyehu A, Adera T, Ayano G, Fekadu W. Prevalence and correlates of post-traumatic stress disorder among survivors of road traffic accidents in Ethiopia. Int J Ment Health sys. (2018) 12:1–8. doi: 10.1186/s13033-018-0229-8
41. Bedaso A, Kediro G, Ebrahim J, Tadesse F, Mekonnen S, Gobena N, et al. Prevalence and determinants of post-traumatic stress disorder among road traffic accident survivors: a prospective survey at selected hospitals in southern Ethiopia. BMC Emergency Med. (2020) 20:1–10. doi: 10.1186/s12873-020-00348-5
42. Cohen S, Kamarck T, Mermelstein R. Perceived stress scale. Measuring stress: A guide Health Soc scientists. (1994) 10:1–2. doi: 10.2307/2136404
43. Eytan A, Gex-Fabry M, Toscani L, Deroo L, Loutan L, Bovier PA. Determinants of postconflict symptoms in Albanian Kosovars. J nervous Ment dis. (2004) 192:664–71. doi: 10.1097/01.nmd.0000142029.96703.57
44. Stupar D, Stevanovic D, Vostanis P, Atilola O, Moreira P, Dodig-Curkovic K, et al. Posttraumatic stress disorder symptoms among trauma-exposed adolescents from low-and middle-income countries. Child Adolesc Psychiatry Ment Health. (2021) 15:26. doi: 10.1186/s13034-021-00378-2
45. Jenkins R, Othieno C, Omollo R, Ongeri L, Sifuna P, Mboroki JK, et al. Probable post traumatic stress disorder in Kenya and its associated risk factors: a cross-sectional household survey. Int J Environ Res Public Health. (2015) 12:13494–509. doi: 10.3390/ijerph121013494
46. Bethelehem T. Prevalence of post-traumatic stress, depression symptoms and associated factors in post-conflict areas, North Shoa Zone, Ethiopia: A community based cross sectional study. (2022).
47. Gormez V, Kılıç HN, Orengul AC, Demir MN, Demirlikan Ş, Demirbaş S, et al. Psychopathology and associated risk factors among forcibly displaced Syrian children and adolescents. J immigr minor Health. (2018) 20:529–35. doi: 10.1007/s10903-017-0680-7
48. Osokina O, Silwal S, Bohdanova T, Hodes M, Sourander A, Skokauskas N. Impact of the Russian invasion on mental health of adolescents in Ukraine. J Am Acad Child Adolesc Psychiatry. (2023) 62:335–43. doi: 10.1016/j.jaac.2022.07.845
49. Van Ameringen M, Mancini C, Patterson B, Boyle MH. Post-traumatic stress disorder in Canada. CNS Neurosci Ther. (2008) 14:171–81. doi: 10.1111/j.1755-5949.2008.00049.x
50. Amir M, Kaplan Z, Kotler M. Type of trauma, severity of posttraumatic stress disorder core symptoms, and associated features. J Gen Psychol. (1996) 123:341–51. doi: 10.1080/00221309.1996.9921286
51. Hsu C-C, Chong M-Y, Yang P, Yen C-F. Posttraumatic stress disorder among adolescent earthquake victims in Taiwan. J Am Acad Child Adolesc Psychiatry. (2002) 41:875–81. doi: 10.1097/00004583-200207000-00022
52. Nooner KB, Linares LO, Batinjane J, Kramer RA, Silva R, Cloitre M. Factors related to posttraumatic stress disorder in adolescence. Trauma Viol Abuse. (2012) 13:153–66. doi: 10.1177/1524838012447698
53. Jeftić A, Ikizer G, Tuominen J, Chrona S, Kumaga R. Connection between the COVID-19 pandemic, war trauma reminders, perceived stress, loneliness, and PTSD in Bosnia and Herzegovina. Curr Psychol (New Brunswick NJ). (2023) 42:8582–94. doi: 10.1007/s12144-021-02407-x
54. Kader N, Elhusein B, Chandrappa NSK, Nashwan AJ, Chandra P, Khan AW, et al. Perceived stress and post-traumatic stress disorder symptoms among intensive care unit staff caring for severely ill coronavirus disease 2019 patients during the pandemic: a national study. Ann Gen Psychiatry. (2021) 20:38. doi: 10.1186/s12991-021-00363-1
55. Mei S, Liang L, Ren H, Hu Y, Qin Z, Cao R, et al. Association between perceived stress and post-traumatic stress disorder among medical staff during the COVID-19 epidemic in Wuhan City. Front Public Health. (2021) 9:666460. doi: 10.3389/fpubh.2021.666460
56. Perry BD, Azad I. Posttraumatic stress disorders in children and adolescents. Curr Opin pedia. (1999) 11:310–6. doi: 10.1097/00008480-199908000-00008
57. Al-Hemiary NJ, Hashim MT, Al-Shawi AF, Al-Diwan JK. Effect of post-traumatic stress disorder on school achievement among secondary school students in Baghdad, Iraq. J Faculty Med Baghdad. (2016) 58:146–8. doi: 10.32007/jfacmedbagdad.2016.582
58. Kassa MA, Srahbzu M, Nenko G, Nakie G, Mekuria K, Feleke SF, et al. Suicidal ideation and attempts among high school students of war-affected area at Woldia town, Northeast, Ethiopia, 2022. BMC Psychiatry. (2023) 23:1–12. doi: 10.1186/s12888-023-04889-4
59. Niyonsenga J, Sengesho DN, Mutabaruka J. Psychometric validation of post-traumatic stress disorder checklist for DSM–5 (PCL-5) among Rwandan undergraduate students. (2021) 15(3):207–12. doi: 10.30491/IJBS.2021.279520.1519
60. Adewuya AO, Ola BA, Afolabi OO. Validity of the patient health questionnaire (PHQ-9) as a screening tool for depression amongst Nigerian university students. (2006) 96(1-2):89–93. doi: 10.1016/j.jad.2006.05.021
61. Nidup Y, Chetri DR, Wangchuk S, Jamtsho T, Bhandari B. Perceived stress of high school students. J Res Soc Sci Language. (2022) 2:95–107. doi: 10.20375/0000-000F-7399-3
62. Dalgard OS, Dowrick C, Lehtinen V, Vazquez-Barquero JL, Casey P, Wilkinson G, et al. Negative life events, social support and gender difference in depression: a multinational community survey with data from the ODIN study. Soc Psychiatry Psychiatr Epidemiol. (2006) 41:444–51. doi: 10.1007/s00127-006-0051-5
63. Abiola T, Udofia O, Zakari M. Psychometric properties of the 3-item oslo social support scale among clinical students of Bayero University Kano, Nigeria. Malay J Psychiatry. (2013) 22:32–41. doi: 10.4236/ojpsych.2013.33027
64. Humeniuk R, Ali R. Validation of the alcohol, smoking and substance involvement screening test (ASSIST) and pilot brief intervention: a technical report of phase II findings of the WHO ASSIST Project2006. (2008), 1–9. doi: 10.1111/j.1360-0443.2007.02114.x
65. Terlizzi EP, Villarroel MA. Symptoms of generalized anxiety disorder among adults: United States, 2019: US Department of Health and Human Services, Centers for Disease Control and …. (2020) 1–8.
66. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Internal Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
67. Biset G, Goshiye D, Melesse N, Tsehay M. Post-traumatic stress disorders among children and adolescents in conflict-affected zones of Amhara region, February 2022. Front Psychol. (2023) 13:8170. doi: 10.3389/fpsyg.2022.1052975
68. Agbaria N, Petzold S, Deckert A, Henschke N, Veronese G, Dambach P, et al. Prevalence of post-traumatic stress disorder among Palestinian children and adolescents exposed to political violence: A systematic review and meta-analysis. PloS One. (2021) 16:e0256426. doi: 10.1371/journal.pone.0256426
69. Kadak MT, Nasıroğlu S, Boysan M, Aydın A. Risk factors predicting posttraumatic stress reactions in adolescents after 2011 Van earthquake. Compr Psychiatry. (2013) 54:982–90. doi: 10.1016/j.comppsych.2013.04.003
70. Alshehri FS, Alatawi Y, Alghamdi BS, Alhifany AA, Alharbi A. Prevalence of post-traumatic stress disorder during the COVID-19 pandemic in Saudi Arabia. Saudi Pharm J. (2020) 28:1666–73. doi: 10.1016/j.jsps.2020.10.013
71. Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, Keane TM. The life events checklist for DSM-5 (LEC-5) Vol. 31. National Center for PTSD (2013). Available at: www.ptsd.va.gov.
72. Arora D, Belsiyal CX, Rawat VS. Prevalence and determinants of posttraumatic stress disorder and depression among survivors of motor vehicle accidents from a hilly Indian state. Indian J Psychiatry. (2021) 63:250–7. doi: 10.4103/psychiatry.IndianJPsychiatry_1059_20
73. Tesfaye AH, Sendekie AK, Kabito GG, Engdaw GT, Argaw GS, Desye B, et al. Post-traumatic stress disorder and associated factors among internally displaced persons in Africa: A systematic review and meta-analysis. PloS One. (2024) 19:e0300894. doi: 10.1371/journal.pone.0300894
74. APA. Post-traumatic stress disorder (PTSD). (2022). Available Online at: https://www.Mayoclinic.org/Diseases-Conditions/Post-Traumatic-Stress-Disorder/Symptoms-Causes/Syc-20355967. (Retrieved December 12, 2023).
75. Melkam M, Tinsae T, Andualem F, Nakie G. Post-traumatic stress disorder and associated factors among adults exposed to stress in Ethiopia: A meta-analysis and systematic review. SAGE Open Med. (2023) 11:20503121231160884. doi: 10.1177/20503121231160884
76. Calhoun CD, Stone KJ, Cobb AR, Patterson MW, Danielson CK, Bendezú JJ. The role of social support in coping with psychological trauma: An integrated biopsychosocial model for posttraumatic stress recovery. Psychiatr Quarter. (2022) 93:949–70. doi: 10.1007/s11126-022-10003-w
77. Simon N, Roberts NP, Lewis CE, van Gelderen MJ, Bisson JI. Associations between perceived social support, posttraumatic stress disorder (PTSD) and complex PTSD (CPTSD): implications for treatment. Eur J Psychotraumatol. (2019) 10:1573129. doi: 10.1080/20008198.2019.1573129
78. APA. Post-traumatic stress disorder (PTSD). (2020). Available Online at: https://www.apa.org/topics/ptsd//. (Retrieved December 11, 2023).
79. Çakır E. Witnessing the homicide of a loved one: the effect of witnessing a homicide on PTSD symptom severity and the moderating role of relationship to victim. (2019), 1–23.
80. Teshome AA, Abebe EC, Mengstie MA, Seid MA, Yitbarek GY, Molla YM, et al. Post-traumatic stress disorder and associated factors among adult war survivors in Northwest Ethiopia: Community-based, cross-sectional study. Front Psychiatry. (2023) 14:622. doi: 10.3389/fpsyt.2023.1083138
81. Polusny MA, Erbes CR, Murdoch M, Arbisi PA, Thuras P, Rath M. Prospective risk factors for new-onset post-traumatic stress disorder in National Guard soldiers deployed to Iraq. psychol Med. (2011) 41:687–98. doi: 10.1017/S0033291710002047
82. Chung MC, AlQarni N, AlMazrouei M, Al Muhairi S, Shakra M, Mitchell B, et al. The impact of trauma exposure characteristics on post-traumatic stress disorder and psychiatric co-morbidity among Syrian refugees. Psychiatry Res. (2018) 259:310–5. doi: 10.1016/j.psychres.2017.10.035
83. Carpiniello B. The mental health costs of armed conflicts-A review of systematic reviews conducted on refugees, asylum-seekers and people living in war zones. Int J Environ Res Public Health. (2023) 20:1–16. doi: 10.3390/ijerph20042840
84. Maeng LY, Milad MR. Post-traumatic stress disorder: the relationship between the fear response and chronic stress. Chronic Stress (Thousand Oaks Calif). (2017) 1:2470547017713297. doi: 10.1177/2470547017713297
85. Rivara F, Adhia A, Lyons V, Massey A, Mills B, Morgan E, et al. The effects of violence on health. Health Affairs. (2019) 38:1622–9. doi: 10.1377/hlthaff.2019.00480
86. Allen L, Jones C, Fox A, Copello A, Jones N, Meiser-Stedman R. The correlation between social support and post-traumatic stress disorder in children and adolescents: A meta-analysis. J Affect Disord. (2021) 294:543–57. doi: 10.1016/j.jad.2021.07.028
87. Kolaitis G. Trauma and post-traumatic stress disorder in children and adolescents. Eur J Psychotraumatol. (2017) 8:1351198. doi: 10.1080/20008198.2017.1351198
88. Richards A, Ospina-Duque J, Barrera-Valencia M, Escobar-Rincón J, Ardila-Gutiérrez M, Metzler T, et al. Posttraumatic stress disorder, anxiety and depression symptoms, and psychosocial treatment needs in Colombians internally displaced by armed conflict: A mixed-method evaluation. psychol Trauma: Theory Res Practice Policy. (2011) 3:384. doi: 10.1037/a0022257
89. Sheikh TL, Mohammed A, Agunbiade S, Ike J, Ebiti WN, Adekeye O. Psycho-trauma, psychosocial adjustment, and symptomatic post-traumatic stress disorder among internally displaced persons in Kaduna, Northwestern Nigeria. Front Psychiatry. (2014) 5:127. doi: 10.3389/fpsyt.2014.00127
90. Ranasinghe PD, Levy BR. Prevalence of and sex disparities in posttraumatic stress disorder in an internally displaced Sri Lankan population 6 months after the 2004 Tsunami. Disaster Med Public Health Preparedness. (2007) 1:34–41. doi: 10.1097/DMP.0b013e318068fbb7
Keywords: post-traumatic stress disorder, high school students, adolescents, war, conflict, Ethiopia
Citation: Kassa MA, Fenta S, Anbesaw T, Tesfa NA, Zemariam AB, Kassaw GM, Abate BB and Semagn EG (2024) Post-traumatic stress disorder and associated factors among high school students who experienced war in Woldia town. Front. Psychiatry 15:1359370. doi: 10.3389/fpsyt.2024.1359370
Received: 21 December 2023; Accepted: 31 May 2024;
Published: 16 July 2024.
Edited by:
Aleksandra Maria Rogowska, University of Opole, PolandReviewed by:
Sintayehu Asnakew, Debre Tabor University, EthiopiaSri Warsini, Gadjah Mada University, Indonesia
Copyright © 2024 Kassa, Fenta, Anbesaw, Tesfa, Zemariam, Kassaw, Abate and Semagn. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mulat Awoke Kassa, bXVsYXRhd29rZTQ1QGdtYWlsLmNvbQ==
 Mulat Awoke Kassa
Mulat Awoke Kassa Sefineh Fenta
Sefineh Fenta Tamrat Anbesaw
Tamrat Anbesaw Natnael Amare Tesfa4
Natnael Amare Tesfa4 Alemu Birara Zemariam
Alemu Birara Zemariam Genanew Mulugeta Kassaw
Genanew Mulugeta Kassaw Biruk Beletew Abate
Biruk Beletew Abate