
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 19 July 2024
Sec. Anxiety and Stress Disorders
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1359348
 Nader Ashraf1,2*
Nader Ashraf1,2* Tarek Ziad Arabi1
Tarek Ziad Arabi1 Alhomam Dabaliz1
Alhomam Dabaliz1 Bader Abou Shaar1
Bader Abou Shaar1 Omar Javed Baqal3
Omar Javed Baqal3 Rand Mohammad Taha1
Rand Mohammad Taha1 Eman Javed Baqal1
Eman Javed Baqal1 Mohamad Salim Alkodaymi1
Mohamad Salim Alkodaymi1 Akef Obeidat1
Akef Obeidat1 Abderrahman Ouban1
Abderrahman Ouban1Introduction: Mental health among medical students is an area that has been increasingly garnering world-wide attention. Yet, despite this increased attention, research related to anxiety disorders in Saudi Arabia remain limited. This study aims to address this gap by assessing the prevalence of generalized anxiety disorder (GAD) as well as explore its association with students’ sociodemographic factors and academic performance among medical students in a Saudi Arabian institute that has a diverse, multicultural student body.
Methods: The study takes place in a unique educational environment: a privately funded institute in Riyadh, the capital of Saudi Arabia, with 32% of its student body comprising international students from over 40 countries, during the COVID-19 pandemic. The study deploys the use of a survey that was sent to the students at this institute via their institutional emails. A survey containing 33 items assessing demographics, GAD using GAD-7 questionnaire, stress-relief measures, online learning experience during the pandemic, mental disorders, anxiety associated with the pandemic, two open-ended questions, and one item assessing sleep difficulty.
Results: The results of the survey showed that a significant majority of the responders’ scores in the GAD-7 assessment were in the range of moderate to severe anxiety. The results also suggest that low cGPA and the first academic years are significantly associated with higher GAD-7 scores. Students found severe time constraints, difficult educational content, and lack of psychological support to be major sources of stress. Furthermore, students suggested providing an in-house psychologist, personalized feedback, and guidance on study tactics as methods to reduce anxiety.
Conclusion: These findings, among others, suggest a need for further studies and research in this field to uncover broader patterns and inform targeted mental health support strategies.
Mental health among medical students is a critical area of concern, with studies indicating a high prevalence of mental health issues in this population due to the demanding nature of medical education (1). These challenges, including academic pressures, social isolation, and financial stress, contribute significantly to mental health disorders (2). While much of the focus in literature has been on depression, anxiety disorders, and specifically Generalized Anxiety Disorder (GAD), are increasingly being recognized as significant concerns (3).
GAD, characterized by persistent, excessive, and unrealistic worry (4) emerges in medical students due to various factors such as personality traits (5), academic workload (6), sleep deprivation (7), and financial pressures (7). The impact of patient deaths (8) and student mistreatment (9) are also notable. The COVID-19 pandemic has exacerbated mental health issues among medical students, highlighting the need for robust mental health support systems (10, 11). Anxiety can significantly impact academic performance and professional competence, with cognitive functions, particularly in learning environments, being adversely affected (12, 13).
Despite the increasing recognition of GAD among medical students, research in the Middle Eastern context, particularly in Saudi Arabia, remains limited (14, 15). GAD is estimated to be prevalent in approximately one-third of medical students in Saudi Arabia (14). Furthermore, this study is set against the backdrop of a region where mental health often carries a significant stigma (16–18). In Saudi Arabia, like much of the Middle East, there is a marked reluctance to discuss mental health issues openly, often viewed as a taboo subject (19, 20). This societal stigma can lead to underreporting of mental health issues and a hesitancy to seek help (19, 21). Given the diverse student body, the multicultural aspect of our institution offers an unparalleled opportunity to examine GAD in a setting that merges varied social, cultural, and educational backgrounds, potentially affecting the manifestation and perception of GAD.
This study aims to address this gap by assessing the prevalence of GAD among medical students in a Saudi Arabian institute. By exploring GAD within this unique socio-cultural milieu, this study seeks to shed light on the complexities surrounding mental health in a setting where such discussions are often limited. In doing so, we hope to contribute to the destigmatization of mental health issues in this region. The insights gained could be pivotal in developing culturally sensitive approaches to mental health care in Saudi Arabia and similar contexts.
The study takes place in a unique educational environment: a privately funded institute in Riyadh, the capital of Saudi Arabia, with 32% of its student body comprising international students from over 40 countries. This diverse cultural mix provides a distinctive setting to explore the prevalence and nuances of GAD among medical students. The multicultural aspect of our institution offers an unparalleled opportunity to examine GAD in a setting that merges varied social, cultural, and educational backgrounds, potentially affecting the manifestation and perception of GAD.
To the best of our knowledge, there was no validated questionnaire dedicated to exploring generalized anxiety disorder, especially during the COVID-19 pandemic quarantine, in Saudi Arabia. Our survey encompassed 33 items: 11 items assessing stress-relief measures, eight items from the GAD 7-item (GAD-7) scale (22), six items assessing demographics, three items exploring the online learning experience during the pandemic, two items generally assessing mental disorders, two items evaluating anxiety associated with the pandemic, two open-ended questions, and one item assessing sleep difficulty. The key topics covered in the questionnaire included the following: anxiety level changes during the quarantine, difficulty sleeping due to the pandemic, memory retention and concentration changes due to online learning, and different techniques employed for anxiety relief.
Among the questions assessing anxiety changes, sleeping difficulties, and online learning during the pandemic, four were close-ended questions and two were five-point Likert scale questions. In GAD-7 scale, eight items were appraised using the 4-point Likert scale. The first seven items had the following options: not at all [0], several days [1], over half the days [2], nearly every day [3]; total score (adding all numbers) provides a possible score from 0–21. GAD-7 score range of 0–4, 5–9, 10–14, and 15–21 indicate minimal, mild, moderate, and severe anxiety, respectively. The eighth item assessed the extent of the effect that the problems mentioned in the first 7 items had on the person’s daily life. It had the following options: Not Difficult at all, Somewhat Difficult, Very Difficult, Extremely Difficult. A diagnosis of GAD should not be based on the GAD-7 scores alone; however, a score of 10 or higher indicates that further evaluation is needed.
To ensure instrument validity, an extensive literature review was performed to develop the survey items. Additionally, these items underwent evaluation and validation by a panel of subject matter experts. A preliminary study involving 30 medical students from our institution was conducted to assess the tool’s clarity and face validity, as well as to identify any technical challenges. These participants were subsequently asked to refrain from completing the survey in its final iteration to prevent repeat responses. The pilot phase indicated that the average completion time for the survey was approximately 7 minutes. Based on the feedback obtained, several survey questions were refined to enhance clarity and reduce potential confusion. We also addressed several technical issues identified during the pilot phase. The final survey was then created and disseminated using Google® Forms.
The study population consisted of medical students from all academic years studying in the college of medicine at our institute. Faculty, staff, graduates, and non-medical students were excluded from the study population.
This study utilized a convenience sampling technique. A message bearing the questionnaire link was circulated via the university’s institutional email system to the target population. The survey contained an introductory paragraph that details the study’s aim and affirmed participant anonymity as well as the liberty to withdraw or decline a response entirely. We collected responses using the survey starting from August 2020 until January 2021. In March 2020, the Saudi Ministry of Education announced the closure of all schools and universities due to the pandemic, and all lectures were given using an online format. During the start of the next academic year in August 2020 and our study period, the university began implementing a hybrid teaching format, where students would take turns in small groups to attend lectures on campus, while the remainder attended the sessions online.
The accumulated data were organized and tabulated using Microsoft® Excel (Microsoft Corporation, Redmond, WA). Categorical data were described as counts. For quantitative data, the range, mean, and standard deviation were calculated. Statistical analysis was performed using GraphPad® Prism 9 version 9.4.1 (GraphPad Software, San Diego, CA). Shapiro-Wilk tests were used to determine if the data follow a Gaussian distribution. Due to the abnormal distribution of the data, comparisons between two or more groups were conducted using the Mann-Whitney, Kruskal-Willis, and chi-square tests. Statistical significance was set at P < 0.05.
In compliance with the provisions of the Saudi Law of Ethics of Research on Living Creatures and regulations, and under the guidelines of the National Committee of Bioethics, ethics approval has been acquired from the institutional review board (Reference IRB-18098). Informed consent was obtained from all students.
The calculated sample size to achieve a 95% confidence interval with a margin of error at 5% was determined to be 293, as per the methodology outlined by Pourhoseingholi et al. (23). Our survey received 431 responses comprising 37.1% (160/431) Saudi and 62.9% (271/431) non-Saudi students. The cohort included 33.4% (144/431) male and 66.6% (287/431) female students, aged between 17–28 years. First-year students were the most responsive group, comprising 34.1% (147/431) of the total responses. A majority, 66.6% (287/431), reported a cumulative GPA in the range of 3.0 to 4.0 out of 4.0. Table 1 delineates the demographic and academic characteristics of the respondents.
Starting with mental health specifics (Table 2), 14.6% (63/431) of respondents acknowledged a previous diagnosis of a mental disorder, while 39.9% (172/431) suspected they might have an undiagnosed mental health condition. In terms of specific conditions, among those diagnosed, 63.5% (40/63) had anxiety disorders and 44.4% (28/63) had depression. Within the group suspecting undiagnosed conditions, anxiety disorders and depression were suspected by 52.9% (91/172) and 37.8% (65/172), respectively.
Saudi students represented a substantial majority among both individuals diagnosed and suspected having a mental disorder (P < 0.01). First-year students notably reported suspecting undiagnosed mental health conditions more frequently (P < 0.01). Furthermore, students with lower cGPAs were significantly more likely to be diagnosed or suspect a mental health condition (P < 0.01). Living alone was associated with a higher likelihood of a diagnosed mental health condition, compared to living with spouse/family or roommate/s (P < 0.05). These associations are further detailed in Tables 3 and 4.
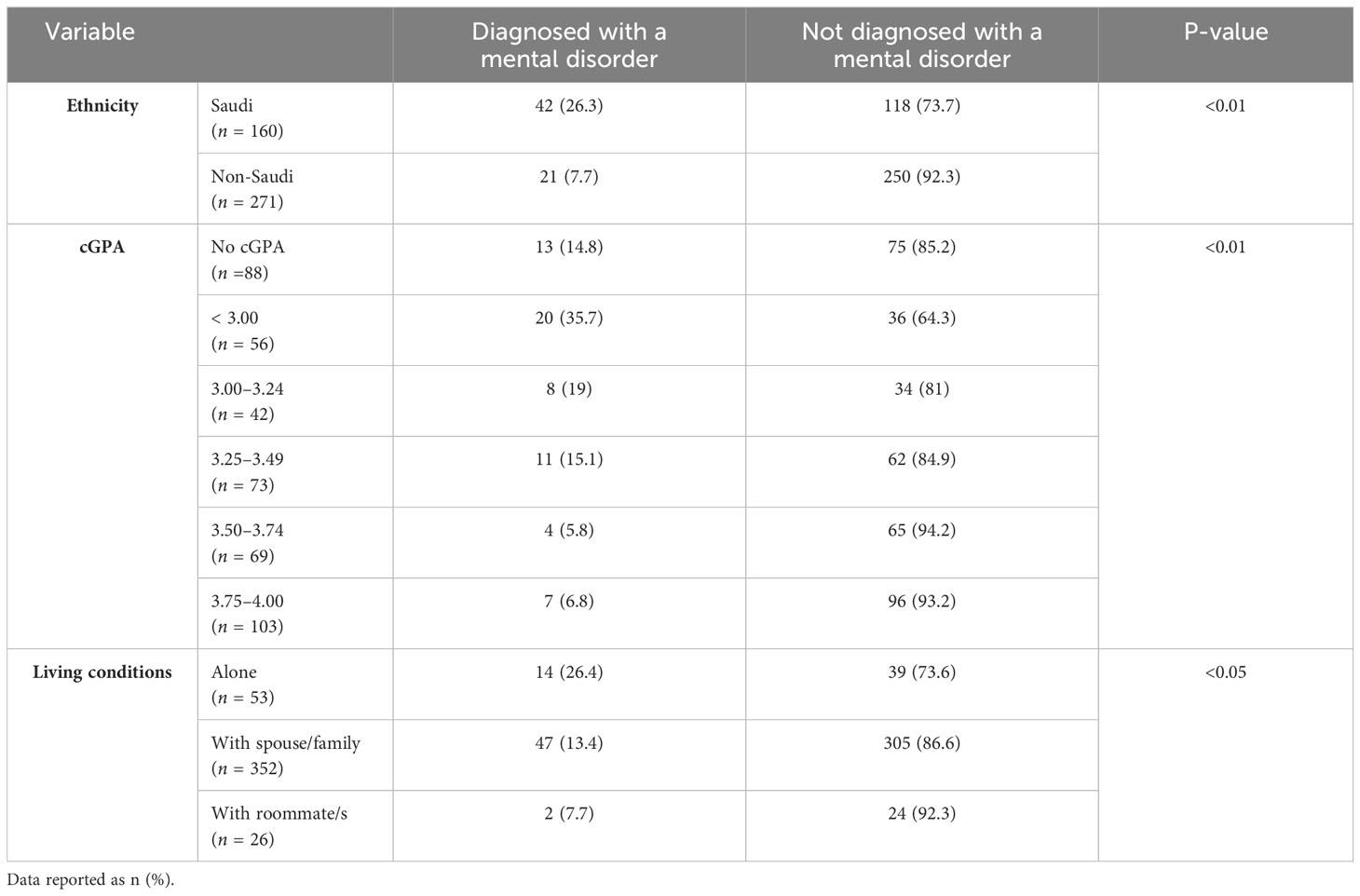
Table 3 Significant results of Chi-square test for factors associated with being diagnosed with a mental disorder (N = 431).
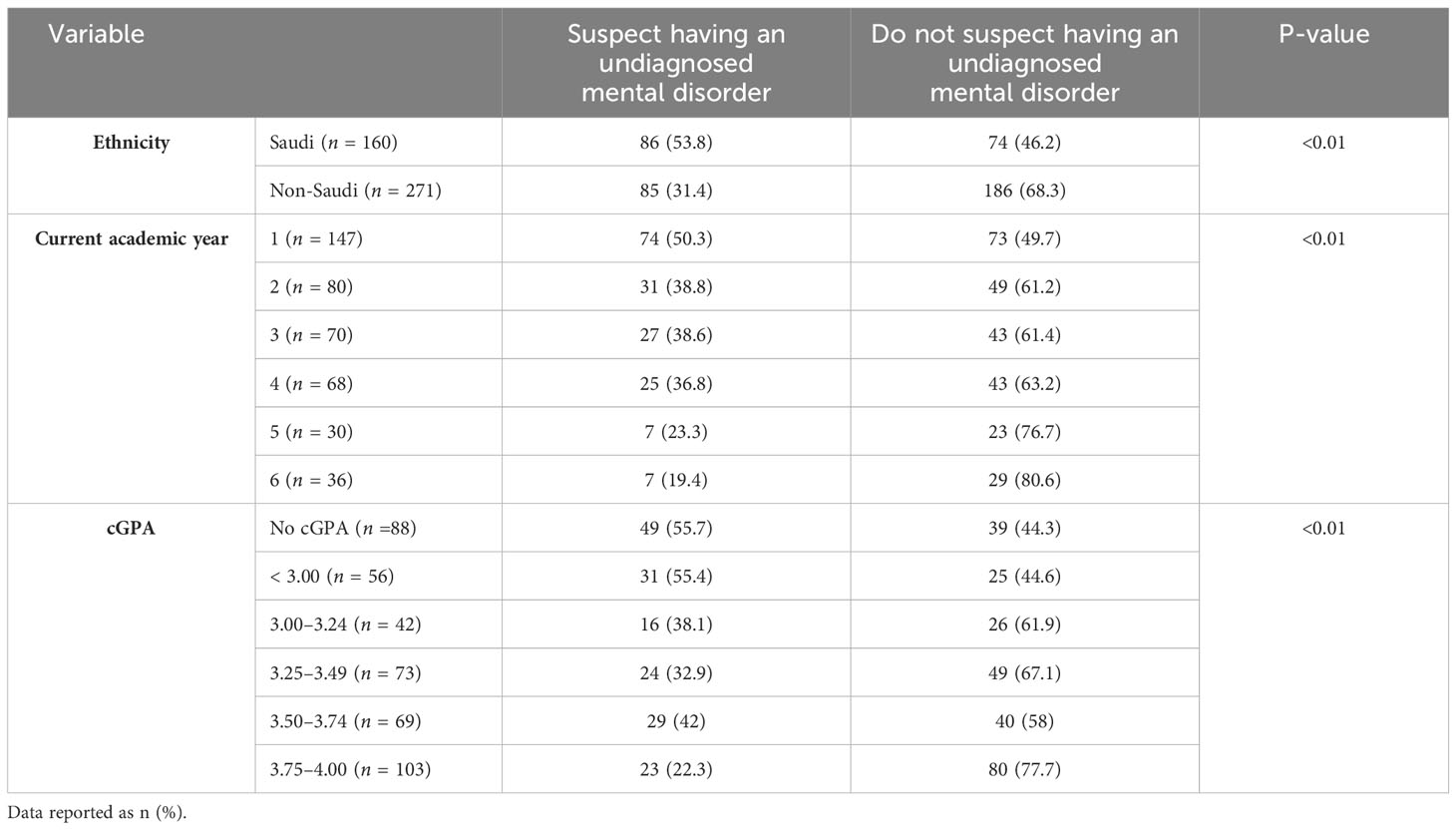
Table 4 Significant results of Chi-square test for factors associated with being suspicious of having an undiagnosed mental disorder (N = 431).
The distribution of GAD-7 scores shows that the majority of students experience moderate to severe anxiety levels, with 31.6% (136/431) in the severe range (14–20) and 19.7% (85/431) in the moderate range (10–14) (Figure 1). Several factors were found to be associated with GAD-7 scores among medical students (Table 5). Being a female (11.7 ± 6.4 vs. 7.8 ± 6.4, P < 0.01), Saudi (12.1 ± 6.6 vs. 9.4 ± 6.5, P < 0.01), or a first-year student (13.1 ± 6.3, P < 0.01) correlated significantly with higher GAD-7 scores. Students with no cGPA or a cGPA lower than 3.00 displayed higher GAD-7 scores (13.4 ± 6.2 for no cGPA, 13.0 ± 6.6 for < 3.00 cGPA, P < 0.01). Students clinically diagnosed with a mental disorder reported higher GAD-7 scores (13.6 ± 6.3, P < 0.01), as did those suspecting an undiagnosed mental disorder (14.7 ± 5.3, P < 0.01).
The pandemic’s impact was reflected in the increased anxiety levels during quarantine, reported by 51.0% (220/431) of respondents, while a decrease was noted by 13.0% (56/431) only (Figure 2). When asked why it increased, medical students attributed this to a variety of factors. Key reasons include the stress of being confined at home, often in a toxic environment, and the fear of COVID-19 exposure or transmitting the virus to loved ones. The academic stress of constantly studying, especially for board exams, was compounded by the lack of social interaction and outdoor activities. Other factors contributing to heightened anxiety include the monotonous and repetitive nature of staying at home, overthinking due to increased free time, and concerns about the future, including career opportunities and board exams. Additionally, concerns about uncertainty, boredom, and lack of control over their lives were common themes. Despite these challenges, some students found positive aspects in the situation, such as the comfort of studying from home, reduced social and academic pressures, and more time for family and personal growth. The transition to online learning and a change in routine provided a more relaxed environment and opportunities for introspection and pursuing hobbies, which contributed to decreased anxiety for these individuals.
Interestingly, a larger portion of students (53.8%, 232/431) reported not experiencing stress due to the fear of contracting COVID-19. Most students (68.9%, 297/431) indicated difficulties in concentrating on their studies due to the transition to online teaching. More than three-quarters of students (77.0%, 332/431) reported difficulty sleeping due to the pandemic. Responses regarding exam environment preferences were fairly evenly distributed (Table 6).
In Figure 3, 59.8% (258/431) of students reported a decrease in information retention due to online learning, with 34.1% (147/431) specifically reporting a significant decrease. Further analysis revealed that first-year students were significantly more negatively affected compared to other years (P < 0.01).
Figure 4 lists various methods of stress relief reported by the respondents. The most used methods are ‘Sleeping’, ‘Going to a psychiatrist’, ‘Talking to family/friends’, and ‘Religion’, each reported by approximately 75% of participants. Figure 5 correlates the average GAD-7 scores with the methods of stress relief. The highest average GAD-7 scores were associated with ‘Taking medications’ (13.66) and ‘Smoking’ (12.72), while ‘Exercise/Sports’ (9.4) and ‘Religion’ (9.71) are associated with the lowest average GAD-7 scores.
Several key themes emerged from the 233 student responses to our open-ended question regarding reasons that may be responsible for the prevalence of anxiety in medical students studying in Saudi Arabia. A significant factor contributing to anxiety is the academic and financial pressure, particularly due to the high cost and competitive nature of private medical colleges, leading to concerns about family financial burdens, delayed graduation, and fears of academic failure. Students also cited high expectations set by universities, with a rigorous and dense curriculum that offers little time for relaxation, leading to an exam-centric learning environment that lacks enjoyment. The curriculum’s misalignment with crucial future examinations like the United States Medical Licensing Examination, continuous assessments, and irrelevant elective courses further exacerbate stress levels. The COVID-19 pandemic has notably impacted students’ anxiety, primarily due to reduced clinical exposure and hands-on experience, preparing them inadequately for future professional challenges. Social and personal factors, such as family pressure, fear of failure, comparison with peers, and the challenges of living alone, especially for non-local students, significantly contribute to the students’ anxiety. Online learning, adopted due to the pandemic, has led to decreased information retention and concentration, with freshmen facing particular difficulties due to limited peer interaction. The responses also pointed to a pervasive stigma around mental health in the country, making it challenging for students to seek help. A lack of institutional support, including insufficient mental health counseling, lack of recreational activities, and the absence of necessary breaks in the academic schedule, was a recurring theme. Finally, the intense academic competition, stress about future career prospects, and general pressures of medical education compound the anxiety experienced by these students.
Finally, 215 students provided their input regarding what can be changed to improve mental wellbeing. The most suggested method was providing on-campus psychologists and psychiatrists for in-house student support. Key suggestions include academic adjustments such as offering second chances for improved grades, reducing the number and clustering of exams, and revising the GPA system towards a more lenient Pass/Fail approach. Enhanced support and counseling are crucial, with an increased role for mentors, more accessible counseling services, and faculty training in mental health awareness. Students advocate for curricular reforms that lessen exam difficulty and introduce leisure and relaxation events, alongside reevaluating fee structures and expanding scholarships. The establishment of wellness-focused infrastructure, like gyms and recreational spaces, is seen as vital for stress alleviation. Systemic changes are also recommended, including policy reforms for more student-friendly exam schedules and a participatory approach in academic decision-making. Additionally, there’s a call for psychological support through increased mental health awareness and professional psychiatric assistance, coupled with organizing activities for relaxation and fostering a positive, flexible academic environment.
While this study initially aimed simply to assess the prevalence of mental health conditions in medical students, the results have unveiled intriguing patterns that contribute to our understanding of the relationship between mental health conditions and various demographic and academic factors. The overall impact of the pandemic on students’ mental health, encompassing a mix of academic, social, and personal challenges. highlight its complex and multifaceted nature. The recommendations brought up by the students highlight the necessity for universities to adopt a holistic approach in addressing student mental health, balancing academic rigor with supportive and student-centric policies and resources.
In alignment with the data from the Saudi National Mental Health Survey on Saudi youth (24), our results indicate a higher prevalence of GAD and mean GAD-7 scores among Saudi students compared to non-Saudis. Additionally, Saudi students were more likely to be diagnosed with or suspect undiagnosed mental disorders, which resonates with the broader context of mental health in Saudi Arabia (25). The idea that Saudis have a higher-than-average prevalence of mental health conditions is supported by multiple studies that reveal an abnormally high rate of mental health conditions in the Saudi population. For instance, one study found a 28.5% prevalence of mental disorders in primary healthcare patients (26), and another reported a 48% prevalence in a suburban population (27). In fact, a meta-analysis on global prevalence of anxiety among medical students showed that Middle Eastern countries had higher prevalence estimates compared to others (3). The Saudi National Mental Health Survey also highlighted that nearly two in five Saudi youth meet criteria for a mental health condition at some point in their lives, with only a small fraction (13.6%) seeking treatment annually (28).
Conversely, Alyami et al. (2021) found higher rates of depression and anxiety among non-Saudi working-class individuals, suggesting that socioeconomic and living conditions, particularly during the COVID-19 pandemic, might influence mental health (29). These contradicting results may be explained by the difference in the study sample, as Alyani et al.’s study had far more participants from the working class compared to university students, and a large amount of employed non-Saudis are working in the labor force and may live in heavily crowded areas. These living conditions during the COVID-19 pandemic were associated with higher rates of infections, which may explain the high prevalence of anxiety and depression reported in this study (30).
The association between mental health conditions and academic performance was also noteworthy. Students with cGPAs below 3.00 were more likely to have diagnosed or suspect having undiagnosed mental disorder, consistent with Bruffaerts et al. (2013), who observed a 0.2–0.3 drop in cGPA among students with mental health conditions (31). Additionally, first-year students, who typically experience heightened stress and pressure and do not have a cGPA yet, showed higher GAD-7 scores and prevalence of suspected undiagnosed conditions, aligning with findings that college freshmen are more susceptible to mental health issues (32–34). This can potentially be attributed to transitional stress, as students go directly from high school to medical school, and adjustment to a new academic and social environment (35). Table 6 reveals several associations with GAD-7 scores, including higher scores in female students, aligning with existing literature that suggests females are generally more prone to anxiety disorders than males (36, 37).
A significant association between living alone and the presence of mental health conditions was also observed, resonating with studies on older adults that link solitary living to increased depressive (33) and anxiety (38) symptoms. This suggests a potential correlation even in younger populations (39).
Regarding the pandemic’s impact (Table 6 and Figure 2), most students reported increased anxiety levels, yet this did not directly translate to anxiety over COVID-19 infection. The fact that more students did not report experiencing stress related to COVID-19 infection fears is a notable finding, as it may suggest effective coping mechanisms or a degree of desensitization to the ongoing pandemic situation. This contrasts with the commonly observed trend of heightened fear and stress due to the pandemic in broader populations (40). This implies that the pandemic’s effects on daily life and rapid adjustments might have been the primary anxiety sources, particularly loneliness and social distancing (41).
The online learning effects during the pandemic highlighted challenges in information retention and concentration, particularly among freshmen. This subjective worsening may be due to the decrease in peer-to-peer interactions both between colleagues and with seniors, which especially affects freshmen and leaves them feeling more lost than they would be otherwise (42). Online learning’s efficacy is supported in literature, especially in pre-clerkship years (43, 44). In fact, a systematic review found online learning to be superior to face-to-face learning in certain situations (44). Nonetheless, our findings suggest that subjective measures like focus and memory retention might differ from objective outcomes like cGPA. This discrepancy underscores the need for more nuanced research into online learning’s impacts, particularly in adapting to its benefits without losing face-to-face learning’s advantages. Online learning remains a relatively new system that needs rigorous studying to optimize the learning methods and materials and maximize the effectiveness without compromising the benefits associated with face-to-face learning (45).
Interestingly, the methods of stress relief (Figures 4, 5) showed that medication and smoking, though less frequently used, were linked to higher GAD-7 scores. In contrast, exercise, religious activities, and leisure, more commonly reported, were associated with lower scores, underscoring the potential effectiveness of these methods in mitigating stress and anxiety. This observation aligns with the studies by Steptoe et al. (46), who found that exercise and leisure activities are effective in reducing anxiety and improving mental health, and Khantzian et al. (47), who noted the potential risks associated with self-medication practices like smoking for stress relief. These results may be indicative of the effectiveness of these methods for alleviating stress and anxiety and warrant further investigation with studies that target the association between stress relief methods and mental disorders to understand it more extensively.
This study has several limitations that should be considered. As a single-institution study conducted during the COVID-19 pandemic, the generalizability of our findings may be limited. The reliance on self-reported data and the use of the GAD-7 as a screening tool, rather than clinical interviews, may affect the accuracy of our prevalence estimates. Additionally, the cross-sectional design precludes establishing causal relationships between the factors examined and GAD prevalence. Cultural factors and stigma surrounding mental health in Saudi Arabia may have also influenced participants’ responses. Despite these limitations, this study provides valuable preliminary data on GAD prevalence among medical students in Saudi Arabia and highlights areas for future research.
Our study revealed a higher prevalence of Generalized Anxiety Disorder (GAD) and associated mental health conditions among Saudi medical students, those living alone, and students with lower cumulative GPAs. Notably, female students, freshmen, and Saudis exhibited elevated GAD-7 scores, particularly those with a history of diagnosed mental health conditions. Stress relief methods such as exercise, religious activities, and leisure were linked to lower GAD-7 scores, suggesting their effectiveness in mitigating anxiety. The transition to online learning was perceived to negatively impact students’ focus and information retention. Given these findings, we advocate for expansive research across Saudi Arabia’s medical student population to uncover broader patterns and inform targeted mental health support strategies.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Alfaisal University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
NA: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. TA: Formal analysis, Writing – original draft, Writing – review & editing. AD: Data curation, Writing – original draft. BA: Data curation, Writing – original draft. OB: Data curation, Investigation, Writing – review & editing. RT: Data curation, Writing – review & editing. EB: Data curation, Writing – review & editing. MA: Data curation, Investigation, Writing – review & editing. AOb: Data curation, Writing – review & editing. AOu: Data curation, Investigation, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1359348/full#supplementary-material
Supplementary File 1 | The survey circulated to medical students at Alfaisal University.
1. Brazeau CM, Shanafelt T, Durning SJ, Massie FS, Eacker A, Moutier C, et al. Distress among matriculating medical students relative to the general population. Acad Med. (2014) 89:1520–5. doi: 10.1097/acm.0000000000000482
2. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. (2006) 81:354–73. doi: 10.1097/00001888-200604000-00009
3. Quek TT, Tam WW, Tran BX, Zhang M, Zhang Z, Ho CS, et al. The global prevalence of anxiety among medical students: A meta-analysis. Int J Environ Res Public Health. (2019) 16. doi: 10.3390/ijerph16152735
4. Diagnostic and statistical manual of mental disorders, fifth edition, text revision (Dsm-5-tr). 5 ed. Amer Psychiatric Pub Inc (2023).
5. Kawamura KY, Hunt SL, Frost RO, DiBartolo PM. Perfectionism, anxiety, and depression: are the relationships independent? Cogn Ther Res. (2001) 25:291–301. doi: 10.1023/A:1010736529013
6. Guthrie EA, Black D, Shaw CM, Hamilton J, Creed FH, Tomenson B. Embarking upon a medical career: psychological morbidity in first year medical students. Med Educ. (1995) 29:337–41. doi: 10.1111/medu.1995.29.issue-5
7. Wolf TM, Faucett JM, Randall HM, Balson PM. Graduating medical students' Ratings of stresses, pleasures, and coping strategies. J Med Educ. (1988) 63:636–42. doi: 10.1097/00001888-198808000-00008
8. Williams CM, Wilson CC, Olsen CH. Dying, death, and medical education: student voices. J Palliative Med. (2005) 8:372–81. doi: 10.1089/jpm.2005.8.372
9. Richman JA, Flaherty JA, Rospenda KM, Christensen ML. Mental health consequences and correlates of reported medical student abuse. JAMA. (1992) 267:692–4. doi: 10.1001/jama.1992.03480050096032
10. Meherali S, Punjani N, Louie-Poon S, Abdul Rahim K, Das JK, Salam RA, et al. Mental health of children and adolescents amidst covid-19 and past pandemics: A rapid systematic review. Int J Environ Res Public Health. (2021) 18. doi: 10.3390/ijerph18073432
11. Lyons Z, Wilcox H, Leung L, Dearsley O. Covid-19 and the mental well-being of Australian medical students: impact, concerns and coping strategies used. Australas Psychiatry. (2020) 28:649–52. doi: 10.1177/1039856220947945
12. Moutinho IL, Maddalena NC, Roland RK, Lucchetti AL, Tibiriçá SH, Ezequiel OD, et al. Depression, stress and anxiety in medical students: A cross-sectional comparison between students from different semesters. Rev Assoc Med Bras (1992). (2017) 63:21–8. doi: 10.1590/1806-9282.63.01.21
13. Meyer C, ACdA Guimarães, MaChado Z, Parcias SR. Qualidade de vida E estresse ocupacional em estudantes de medicina. Rev Bras Educação Médica. (2012) 36. doi: 10.1590/S0100-55022012000600007
14. AlShamlan NA, AlOmar RS, Al Shammari MA, AlShamlan RA, AlShamlan AA, Sebiany AM. Anxiety and its association with preparation for future specialty: A cross-sectional study among medical students, Saudi Arabia. J Multidiscip Healthcare. (2020) 13:581–91. doi: 10.2147/JMDH.S259905
15. Almojali AI, Almalki SA, Alothman AS, Masuadi EM, Alaqeel MK. The prevalence and association of stress with sleep quality among medical students. J Epidemiol Glob Health. (2017) 7:169–74. doi: 10.1016/j.jegh.2017.04.005
16. Andrade G, Bedewy D, Elamin ABA, Abdelmonem KYA, Teir HJ, Alqaderi N. Attitudes towards mental health problems in a sample of United Arab Emirates’ Residents. Middle East Curr Psychiatry. (2022) 29:88. doi: 10.1186/s43045-022-00255-4
17. Khatib HE, Alyafei A, Shaikh M. Understanding experiences of mental health help-seeking in Arab populations around the world: A systematic review and narrative synthesis. BMC Psychiatry. (2023) 23:324. doi: 10.1186/s12888-023-04827-4
18. Zolezzi M, Alamri M, Shaar S, Rainkie D. Stigma associated with mental illness and its treatment in the Arab culture: A systematic review. Int J Soc Psychiatry. (2018) 64:597–609. doi: 10.1177/0020764018789200
19. Zarbah AA, Al Alfard HA, Alamri HS, Al Edrees N, Alshahrani NS, Alshehri AF. Prevalence of internalized stigma in patients with psychiatric illness in abha, Southern Region, Saudi Arabia. J Family Community Med. (2023) 30:103–8. doi: 10.4103/jfcm.jfcm_222_22
20. AlAteeq D, AlDaoud A, AlHadi A, AlKhalaf H, Milev R. The experience and impact of stigma in Saudi people with a mood disorder. Ann Gen Psychiatry. (2018) 17:51. doi: 10.1186/s12991-018-0221-3
21. Alattar N, Felton A, Stickley T. Mental health and stigma in Saudi Arabia: A scoping review. Ment Health Rev J. (2021) 26:180–96. doi: 10.1108/MHRJ-08-2020-0055
22. Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Internal Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
23. Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. (2013) 6:14–7.
24. Altwaijri Y, Kazdin AE, Al-Subaie A, Al-Habeeb A, Hyder S, Bilal L, et al. Lifetime prevalence and treatment of mental disorders in Saudi youth and adolescents. Sci Rep. (2023) 13:6186. doi: 10.1038/s41598-023-33005-5
25. Carlisle J. Mental health law in Saudi Arabia. BJPsych Int. (2018) 15:17–9. doi: 10.1192/bji.2017.10
26. Alghadeer SM, Alhossan AM, Al-Arifi MN, Alrabiah ZS, Ali SW, Babelghaith SD, et al. Prevalence of mental disorders among patients attending primary health care centers in the capital of Saudi Arabia. Neurosci (Riyadh). (2018) 23:239–43. doi: 10.17712/nsj.2018.3.20180058
27. Al-Sughayr AM, Ferwana MS. Prevalence of mental disorders among high school students in National Guard Housing, Riyadh, Saudi Arabia. J Family Community Med. (2012) 19:47–51. doi: 10.4103/2230-8229.94015
28. Al-Subaie AS, Al-Habeeb AH, Altwaijri YA. Overview of the Saudi national mental health survey. Int J Methods Psychiatr Res. (2020) 29:e1835. doi: 10.1002/mpr.1835
29. Alyami HS, Naser AY, Dahmash EZ, Alyami MH, Alyami MS. Depression and anxiety during the covid-19 pandemic in Saudi Arabia: A cross-sectional study. Int J Clin Pract. (2021) 75:e14244. doi: 10.1111/ijcp.14244
30. Joseph R, Lucca JM, Alshayban D, Alshehry YA. The immediate psychological response of the general population in Saudi Arabia during covid-19 pandemic: A cross-sectional study. J Infection Public Health. (2021) 14:276–83. doi: 10.1016/j.jiph.2020.11.017
31. Bruffaerts R, Mortier P, Kiekens G, Auerbach RP, Cuijpers P, Demyttenaere K, et al. Mental health problems in college freshmen: prevalence and academic functioning. J Affect Disord. (2018) 225:97–103. doi: 10.1016/j.jad.2017.07.044
32. Lu W, Bian Q, Song YY, Ren JY, Xu XY, Zhao M. Prevalence and related risk factors of anxiety and depression among chinese college freshmen. J Huazhong Univ Sci Technolog Med Sci. (2015) 35:815–22. doi: 10.1007/s11596-015-1512-4
33. Ebert DD, Buntrock C, Mortier P, Auerbach R, Weisel KK, Kessler RC, et al. Prediction of major depressive disorder onset in college students. Depress Anxiety. (2019) 36:294–304. doi: 10.1002/da.22867
34. Pedrelli P, Nyer M, Yeung A, Zulauf C, Wilens T. College students: mental health problems and treatment considerations. Acad Psychiatry. (2015) 39:503–11. doi: 10.1007/s40596-014-0205-9
35. Tan GXD, Soh XC, Hartanto A, Goh AYH, Majeed NM. Prevalence of anxiety in college and university students: an umbrella review. J Affect Disord Rep. (2023) 14:100658. doi: 10.1016/j.jadr.2023.100658
36. McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. (2011) 45:1027–35. doi: 10.1016/j.jpsychires.2011.03.006
37. Remes O, Brayne C, van der Linde R, Lafortune L. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav. (2016) 6:e00497. doi: 10.1002/brb3.497
38. Yu J, Choe K, Kang Y. Anxiety of older persons living alone in the community. Healthcare (Basel). (2020) 8. doi: 10.3390/healthcare8030287
39. Hawkley LC, Cacioppo JT. Loneliness matters: A theoretical and empirical review of consequences and mechanisms. Ann Behav Med. (2010) 40:218–27. doi: 10.1007/s12160-010-9210-8
40. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
41. Kupcova I, Danisovic L, Klein M, Harsanyi S. Effects of the covid-19 pandemic on mental health, anxiety, and depression. BMC Psychol. (2023) 11:108. doi: 10.1186/s40359-023-01130-5
42. Alghalyini B, Albeyahi A, Abou Shaar B, Salah M. Perception of the covid-19 pandemic among members of saudi society: solidarity, humility, and connectivity. Cureus. (2021) 13:e19427. doi: 10.7759/cureus.19427
43. McCutcheon K, Lohan M, Traynor M, Martin D. A systematic review evaluating the impact of online or blended learning vs. Face-to-face learning of clinical skills in undergraduate nurse education. J Adv Nurs. (2015) 71:255–70. doi: 10.1111/jan.12509
44. Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online. (2019) 24:1666538. doi: 10.1080/10872981.2019.1666538
45. Almakadma AS, Fawzy NA, Baqal OJ, Kamada S. Perceptions and attitudes of medical students towards student evaluation of teaching: A cross-sectional study. Med Educ Online. (2023) 28:2220175. doi: 10.1080/10872981.2023.2220175
46. Steptoe A, Edwards S, Moses J, Mathews A. The effects of exercise training on mood and perceived coping ability in anxious adults from the general population. J Psychosom Res. (1989) 33:537–47. doi: 10.1016/0022-3999(89)90061-5
Keywords: generalized anxiety disorder, mental health, medical student, Middle East, medical education
Citation: Ashraf N, Arabi TZ, Dabaliz A, Abou Shaar B, Baqal OJ, Taha RM, Baqal EJ, Alkodaymi MS, Obeidat A and Ouban A (2024) Assessing the prevalence of generalized anxiety disorder in a multicultural medical education setting in Saudi Arabia during the COVID-19 pandemic. Front. Psychiatry 15:1359348. doi: 10.3389/fpsyt.2024.1359348
Received: 21 December 2023; Accepted: 08 July 2024;
Published: 19 July 2024.
Edited by:
Gaia Sampogna, University of Campania “L. Vanvitelli”, ItalyReviewed by:
Mohamad Golitaleb, Arak University of Medical Sciences, IranCopyright © 2024 Ashraf, Arabi, Dabaliz, Abou Shaar, Baqal, Taha, Baqal, Alkodaymi, Obeidat and Ouban. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nader Ashraf, bmFkZXIuYXNocmFmQGxpdmUuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.