- 1Department of Public Health, Hangzhou Normal University, Hangzhou, Zhejiang, China
- 2Nanjing Zhiyuan Healthcare Training Center, Jiangsu SuYi Health Care Research Institute, Nanjing, Jiangsu, China
- 3Health management center, The First Affiliated Hospital of Hainan Medical University, Haiko, Hainan, China
Introduction: Cognitive Impairment (CI) in the elderly, encompassing conditions ranging from Mild Cognitive Impairment (MCI) to dementia, represents a growing public health concern globally. This study aims to investigate the prevalence and correlates of CI among individuals aged 80 and above.
Methods: The study conducts 13,027 elderly individual’s door-to-door surveys, followed by the cross-tabulation of analysis data, logistic regression analysis, and health condition assessments to examine various determinants of CI.
Results: The current study’s key findings demonstrate sub-statical correlations between CI and various factors, including educational attainment, marital status, and gender. Pronounced differences are evident between urban and rural demographics. Furthermore, aspects of social engagement, notably communication proficiency and sensory capabilities, exhibit a strong association with CI. Logistic regression analysis highlights that residing in rural areas (Odds Ratio [OR] = 0.637) and being female (OR = 0.71) are linked to a decreased risk of CI. In contrast, behavioral and health-related variables present a complex picture. Specifically, aggressive behavior (Adjusted OR = 1.881) and symptoms of depression (Adjusted OR = 0.549) contrast with conditions such as asthma (OR= 2.857) and cerebral infarction (OR=1.348), which elevate the risk of CI. Intriguingly, hyperlipidemia (OR= 0.671) appears to confer a protective effect against CI.
Conclusion: The study highlights the complexity of factors affecting CI in the elderly, advocating for a comprehensive approach to understanding and managing cognitive health.
1 Introduction
Cognitive Impairment (CI) manifests as a spectrum of cognitive deficits in the elderly, impacting essential domains such as orientation, memory, calculation, attention, language, executive function, reasoning, and visualization abilities (1). This condition is broadly classified into mild cognitive impairment (MCI) and dementia, based on severity (2). Dementia, particularly prevalent among the older population, has emerged as a significant public health concern due to its substantial socio-economic and healthcare implications. For instance, in 2010, the prevalence of dementia in the U.S. population aged over 70 was approximately 14.7% (3).
In China, the incidence rate of dementia for individuals aged 60 and above is reported to be 9.9 cases per 1000 person-years. Alzheimer’s disease and related dementia show an increasing trend with age, evidenced by an 8% prevalence in those over 65, rising sharply to about 43% in adults over 85. Projections indicate that the number of individuals in the ‘oldest old’ category (over 80 years) will triple by 2050 (4). The prevalence of MCI, a transitional state between the normal cognitive aging process and early dementia, exhibits significant variability in China, with estimates ranging from 9.7% to 23.3% (5).
CI in older adults, a condition characterized by memory deficits, learning challenges, and impaired concentration, significantly compromises their quality of life. This impairment not only elevates the risk of dementia and mortality but also stems from a multifactorial etiology, including vascular issues, neuronal degeneration, and strokes (6). Empirical evidence indicates that around 10% of individuals who suffer strokes had pre-existing dementia, a figure that increases in post-stroke scenarios, especially among recurrent stroke patients (7). Central to its progression are factors such as gender (8), advancing age (9), smoking habits (10), limited mental and physical engagement (11), and reduced social interactions, which cumulatively exacerbate cognitive decline. Moreover, cardiovascular metabolic risk factors (12), including diabetes, hypertension, metabolic syndrome, and other vascular disorders (13), are strongly correlated with an acceleration of cognitive decline. Additional factors contributing to this impairment range from atrial fibrillation and depression to obesity (14), traumatic brain injury, hearing loss, alcohol misuse (15), and exposure to air pollution (16). The spectrum of cognitive impairment in the elderly spans from mild, often undiagnosed deficits to more severe conditions like dementia.
The Mini-Cog, a concise and innovative tool for dementia screening, combines two simple cognitive tasks: recalling three words and drawing a clock. Created by Borson and colleagues in 2000 (17)., this approach improves upon the Clock Drawing Test (CDT) and the Mini-Mental State Examination (MMSE), as evidenced by multiple studies. With an average administration time of just 3 minutes, it is faster than the MMSE and is preferred by elderly patients due to its omission of potentially uncomfortable orientation questions. It has been validated as an effective tool for screening dementia and cognitive impairment in various settings, including preoperative clinic evaluations.
Understanding the trajectory of cognitive impairment over a lifetime is crucial for developing strategies to prevent its onset and slow its progression towards dementia. However, data regarding the association of cognitive impairment with demographic factors, social engagement, and disease prevalence, particularly in individuals aged 80 and above, remains sparse. Our study aims to bridge this gap by investigating whether cognitive impairment, as detected using the Mini-Cog test, correlates with demographic characteristics, social engagement levels, and disease prevalence in older adults. To this end, we have designed a cohort study targeting adults aged 80 years and above.
2 Materials and methods
2.1 Methods
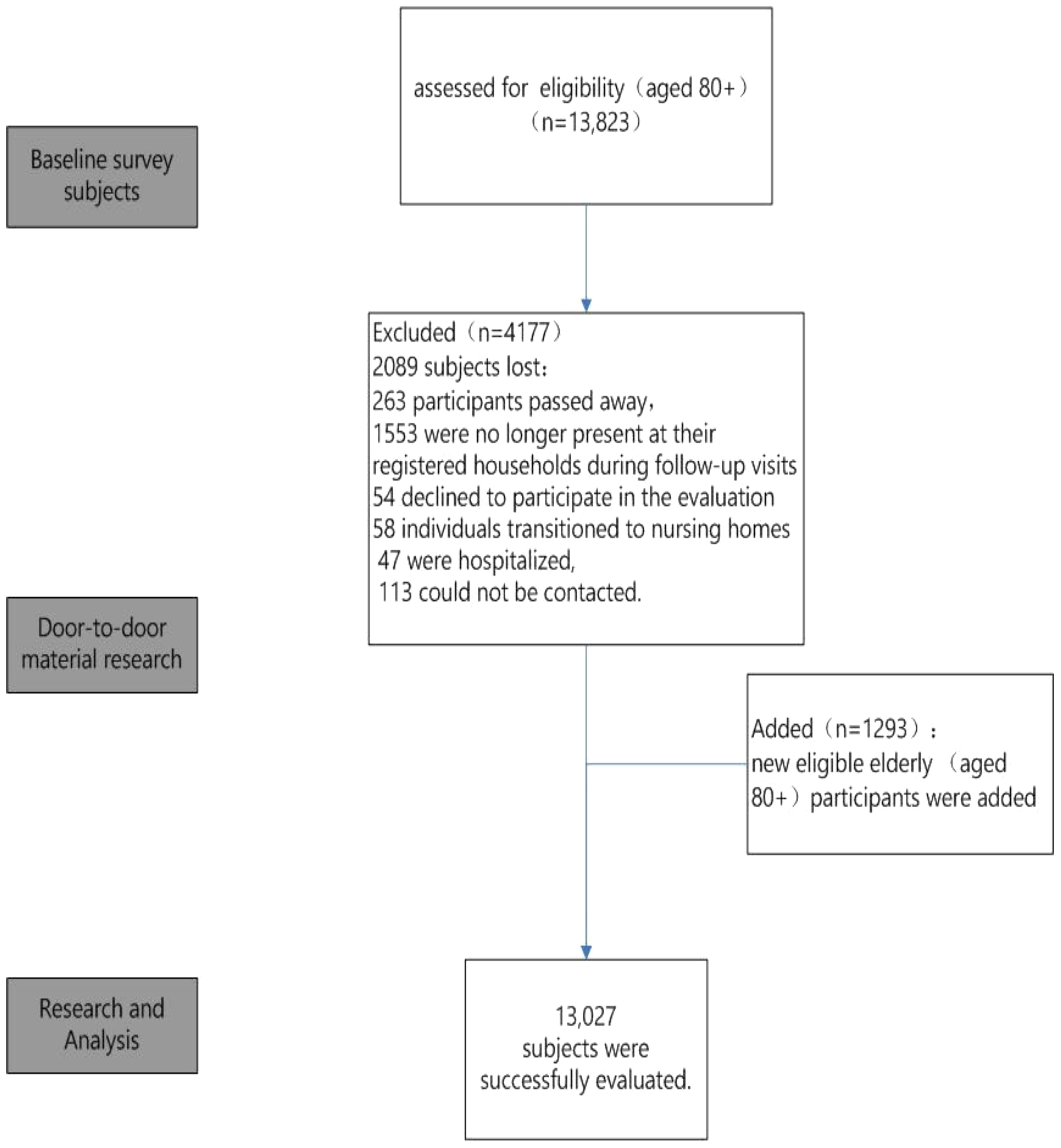
Our research was a comprehensive 8-month-long (April to December 2022) population-based, cross-sectional study conducted in Lishui District, Jiangsu, China (Figure 1). The study commenced with an initial cohort of 13,823 individuals aged 80 or older, identified with the assistance of the Lishui Civil Affairs Bureau. The research team comprised a total of 57 researchers who underwent uniform training to ensure their proficiency in basic assessment knowledge and skills. This training was essential to guarantee that each of the 57 door-to-door researchers adhered to unified assessment requirements, thereby ensuring the scientific accuracy of the research data.
As the study progressed, an additional 1,293 elderly individuals were identified and incorporated, thereby expanding our study population. However, the dynamics of participant involvement underwent notable changes over the course of the study. Specifically, of the initial participant group, 263 individuals passed away, 1,553 were not found at their registered residences during follow-up visits, 54 opted to withdraw from the study, 58 relocated to nursing homes, 47 were hospitalized, and 113 remained unreachable for various reasons. After adjusting for these participant changes, the study successfully completed evaluations with a total of 13,027 elderly participants, as shown in Figure 1.
2.2 Measurements
The equations should be inserted in editable format from the equation editor.
2.2.1 Cognitive impairment
In our study, we utilized the Mini-Cog assessment method as outlined by Borson et al. (15) to screen for cognitive impairment (18). This evaluation awards one point for each item correctly recalled and up to two points for the clock-drawing task, culminating in a maximum score of five points. Data were collected for both the recall and clock-drawing tasks for all participants. However, consistent with Borson’s scoring protocol, the clock-draw performance was scored only for patients who recalled between one and two words. ‘Cognitive Impairment’ was defined as a score of two or less, and ‘No Cognitive Impairment’ as a score greater than two, in accordance with the methodology established by Borson et al.
2.2.2 Demographic factors and social engagement
This study rigorously explores the impact of various demographic and socioeconomic factors on the prevalence of Cognitive Impairment. These factors include age, occupation, urban-rural residency, marital status, educational level, income bracket, living conditions, and health insurance status. Concurrently, the study probes into the complex interplay of changes in social engagement and functional capabilities among the subjects. A comprehensive questionnaire was utilized, covering facets such as communication, sensory perception, life skills, occupational capacity, orientation in time and space, personal orientation, and social interaction.
2.2.3 Disease survey questionnaire
To elucidate the correlation between CI and diverse medical conditions, a survey encompassing various diseases was executed. The surveyed conditions included hypertension, hyperglycemia, hyperlipidemia, cardiac disorders, cerebral infarction, leg and foot discomfort, pain, gastrointestinal diseases, back pain, stroke, pulmonary ailments, asthma, gout, osseous disorders, cancer, ocular conditions, renal diseases, gallstones, rheumatism, among others.
2.2.4 Data analysis
In this investigation, we utilized SPSS software (IBM Corp., Armonk, NY, USA; Version 25.0.0.0) for a comprehensive analysis of the data. The threshold for statistical significance was established at p < 0.05. Depending on the nature of the measurement scales, group comparisons were executed using either Student’s t-tests for continuous variables or chi-square tests for categorical variables.
In our univariate analyses, we scrutinized variations in mini-cog scores across diverse demographic categories within the population aged 80 years and older. This analysis revealed significant disparities, highlighting the diversity within this age group. Moreover, the study assessed the predictive capability of mini-cog scores for the likelihood of disease onset using binary logistic regression analysis, applying a Forward Stepwise method. The significance level for this analysis was maintained at p < 0.05.
3 Results
3.1 Demographic factors in CI
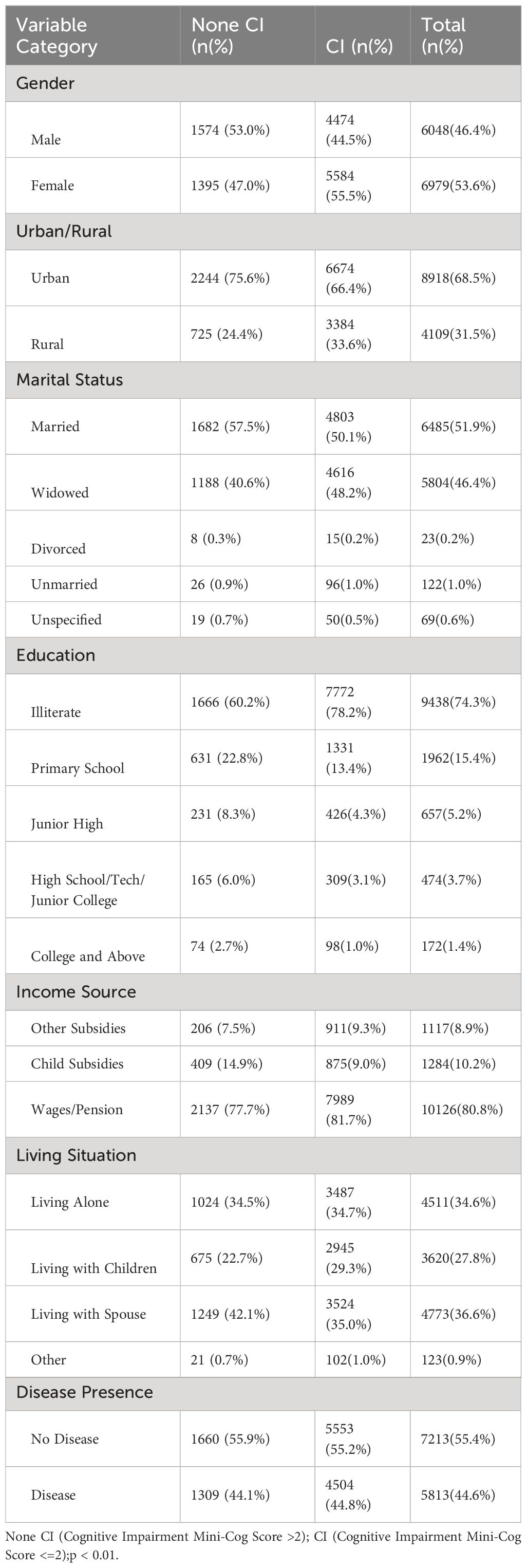
These figures indicate the necessity for targeted approaches to address CI within various demographic segments (Table 1). The table details demographics and health characteristics of individuals with and without CI. In urban areas, 2244 individuals (75.6%) have no CI, while 6674 (66.4%) do. Rural areas have 725 (24.4%) without impairment and 3384 (33.6%) with it. Regarding marital status, the majority of non-impaired individuals are married (57.5%), while a significant proportion of impaired individuals are widowed (48.2%). For education, a notable 78.2% of cognitively impaired individuals are illiterate. In terms of income, most in both groups rely on wages/pension. Living situations show 34.5% of non-impaired and 34.7% of impaired individuals living alone. Gender-wise, more females (55.5%) have CI compared to males. Disease presence is nearly equal in both groups, and mental illness is found only among the cognitively impaired (4.1%).
3.2 Association between social engagement aspects and CI
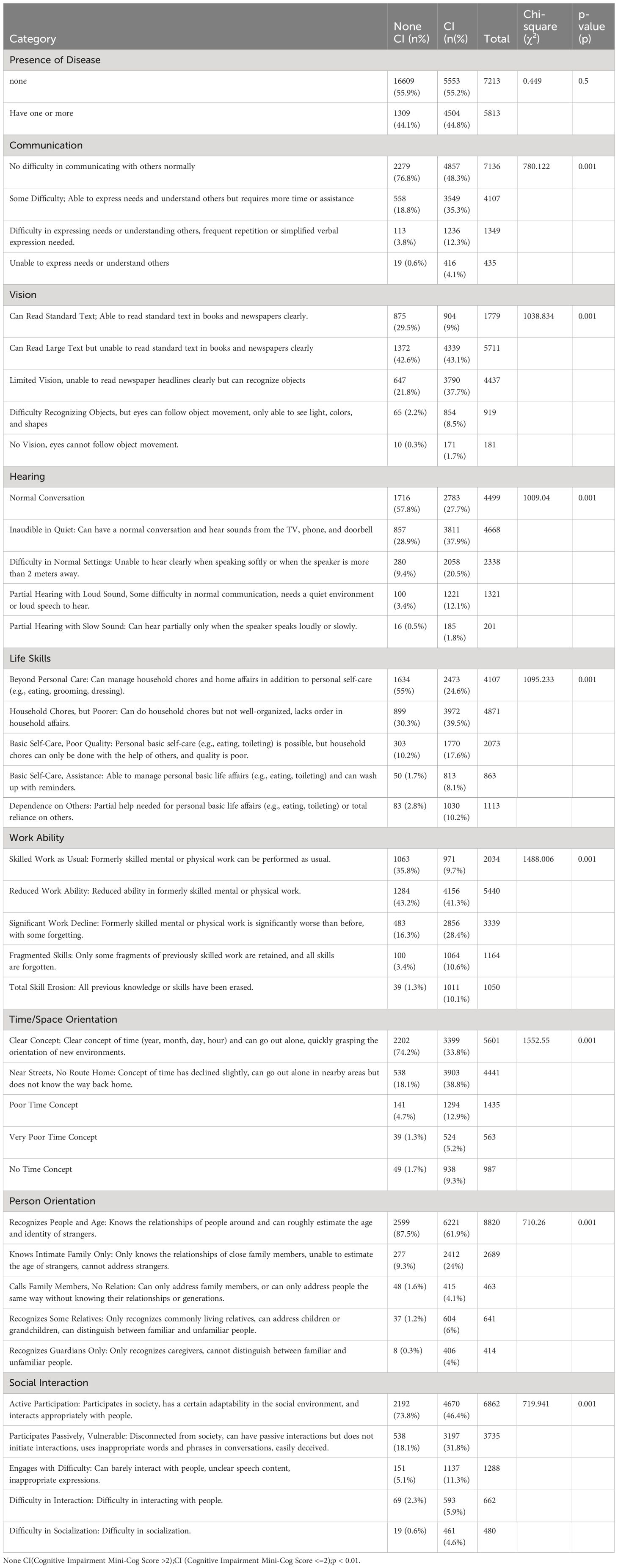
Table 2 explored the association between various Social Engagement aspects and CI. We utilized a cross-tabulation approach, categorizing CI based on a scoring system. The findings revealed significant associations in several domains: Communication abilities (χ² = 780.122, p < 0.001), Vision (χ² = 1038.834, p < 0.001), Hearing (χ² = 1009.04, p < 0.001), Life Skills (χ² = 1095.233, p < 0.001), Work Ability (χ² = 1488.006, p < 0.001), Time/Space Orientation (χ² = 1552.55, p < 0.001), Person Orientation (χ² = 710.26, p < 0.001), and Social Interaction (χ² = 719.941, p < 0.001). No significant association was observed between the presence of disease and CI (χ² = 0.449, p = 0.5).
3.3 Demographic, economic, social CI influences
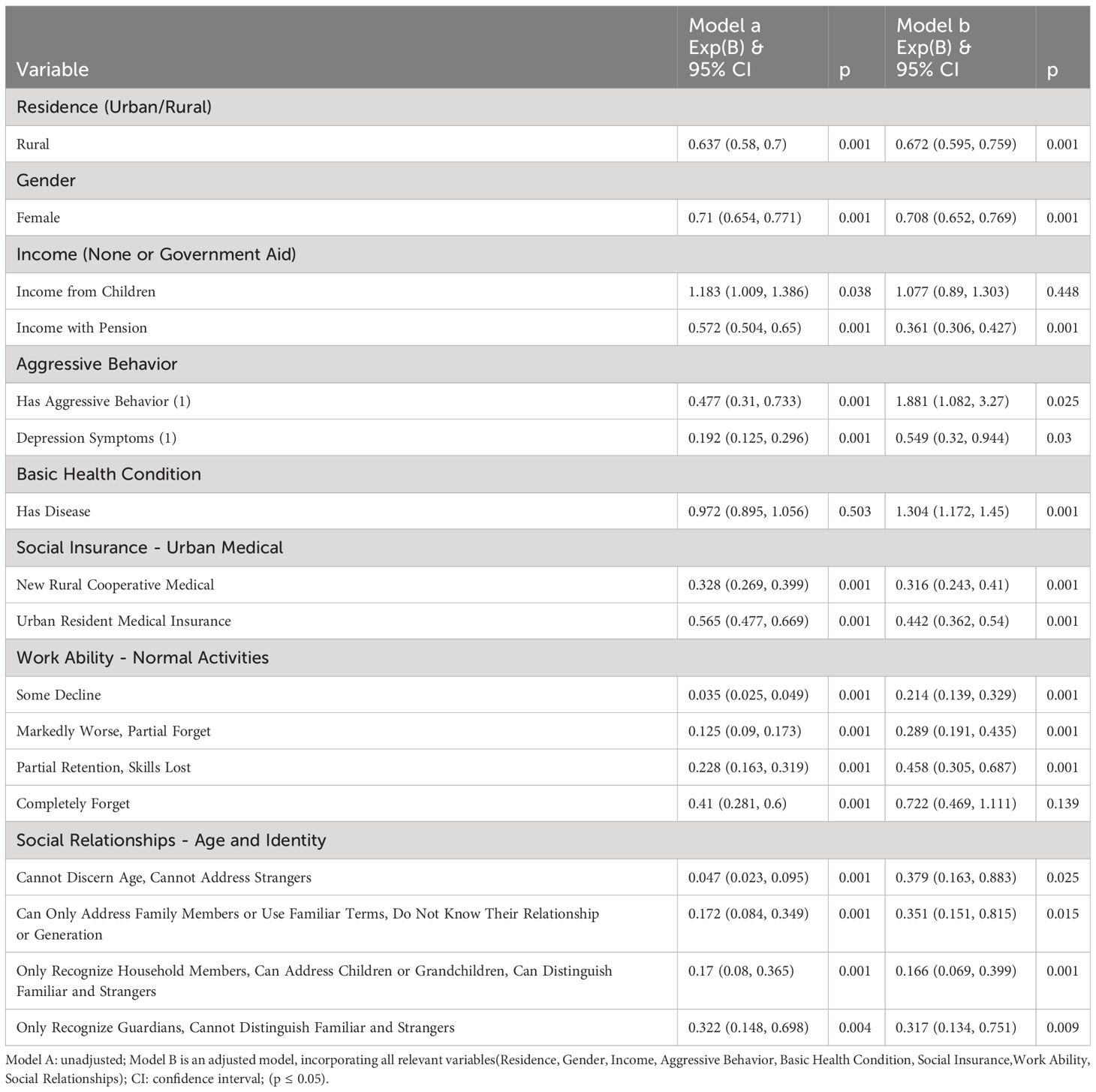
In our logistic regression analysis examining the impact of various factors on CI (Table 3), significant associations were found across demographic, behavioral, health, insurance, work ability, and social relationship variables. Residence in a rural area was associated with a decreased likelihood of the outcome, as evidenced in both unadjusted (OR = 0.637, 95% CI (0.58, 0.7) and adjusted models (OR = 0.672, 95% CI (0.595, 0.759), with statistical significance (p < 0.001). Similarly, female gender was significantly linked to a lower likelihood of the outcome in both models (Unadjusted: OR = 0.71, 95% CI (0.654, 0.771); Adjusted: OR = 0.708, 95% CI (0.652, 0.769), p < 0.001). Income sources showed varying impacts; income for children was significant only in the unadjusted model (OR = 1.183, 95% CI (1.009, 1.386), p = 0.038), while pension income showed a strong negative association in both models.
Behavioral and health factors presented contrasting associations with the outcome. Aggressive behavior increased the likelihood of the outcome (Adjusted OR = 1.881, 95% CI (1.082, 3.27), p = 0.025), whereas depression symptoms were inversely associated (Adjusted OR = 0.549, 95% CI (0.32, 0.944), p = 0.03). Basic health conditions, specifically having a disease, were not significant in the unadjusted model but showed a significant positive association after adjustment (OR = 1.304, 95% CI (1.172, 1.45), p < 0.001). Participants with New Rural Cooperative Medical Insurance or Urban Resident Medical Insurance were notably less likely to experience the outcome, with the New Rural Cooperative Medical group showing the most substantial effect (Adjusted OR = 0.316, 95% CI (0.243, 0.41), p < 0.001).
Work ability and social relationships also demonstrated significant impacts. A marked decline in work ability and deterioration in social relationships were strongly associated with the outcome. The most pronounced effects were observed in participants with markedly worse work ability (Adjusted OR = 0.214, 95% CI (0.139, 0.329), p < 0.001) and those only able to recognize household members (Adjusted OR = 0.166, 95% CI (0.069, 0.399), p < 0.001). These findings emphasize the multifaceted nature of CI and the importance of considering a broad range of factors in its understanding and management.
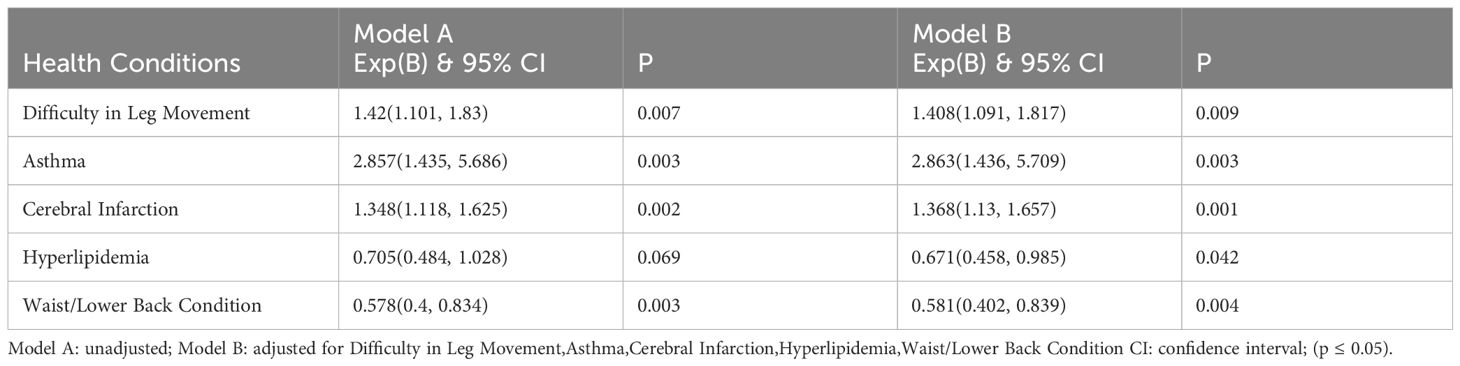
3.4 Disease factors influencing CI
Our analysis identified significant associations between multiple health conditions and CI, as presented in Table 4. Asthma and Cerebral Infarction showed a strong positive association with the CI. In both unadjusted and adjusted models, individuals with asthma had approximately 2.86 times higher odds of experiencing CI (OR= 2.857, 95% CI(1.435, 5.686); OR =2.863, 95% CI(1.436, 5.709). Similarly, cerebral infarction was linked to an increased likelihood of CI (Unadjusted OR=1.348, 95% CI(1.118, 1.625); Adjusted OR=1.368, 95% CI(1.13,1.657).
Conversely, Hyperlipidemia and Waist/Lower Back Condition were associated with a reduced likelihood of CI. Hyperlipidemia showed a significant protective effect in the adjusted model (OR= 0.671, 95% CI(0.458,0.985), though it was not significant in the unadjusted model. The waist/lower back condition consistently showed a negative association in both models (Unadjusted OR=0.578, 95% CI(0.4, 0.834); Adjusted OR=0.581, 95% CI(0.402,0.839). Difficulty in Leg Movement was also found to moderately increase the likelihood of CI (Unadjusted OR=1.42, 95% CI(1.101,1.83); Adjusted OR=1.408, 95% CI(1.091,1.817). These findings highlight the varied influence of different health conditions on the risk of CI, underscoring the need for tailored approaches in its management and prevention.
4 Discussion
These figures highlight key differences and potential correlations between gender and various such as social (19), educational, and health factors with CI (20), where social factors (21) include urban-rural residence, marital status, income source, living conditions. The urban-rural divide (22) in cognitive scores could be attributed to differences in access to healthcare, educational opportunities, and lifestyle factors. Marital status, particularly being married, seems to confer a protective effect on cognitive health, potentially due to social support and shared responsibilities (23).
The strong link between educational attainment (24) and cognitive function underscores the importance of education in cognitive health. Higher education levels may provide better cognitive stimulation and access to information on health-promoting behaviors. Income source, particularly from pensions or wages, suggests a possible link between financial stability and cognitive health (25).
Living arrangements’ influence on cognitive function highlights the role of social interactions and support systems in maintaining cognitive health (26). The gender differences observed point towards potential biological and social factors influencing cognitive health.
There is a complex relationship between health condition and functional abilities among the study participants. While certain domains, such as communication, vision, hearing, life skills, work ability, time/space orientation, person orientation, and social interaction, showed significant associations with functional abilities, the presence of disease did not exhibit a significant impact. These findings highlight the multifaceted nature of functional abilities and the need for a comprehensive assessment.
CI or dementia refers to a clinical syndrome characterized by challenges in memory, language, and behavior, resulting in limitations in performing daily activities. Moreover, the results of this study reveal that the capacity to execute daily life skills (27), maintain occupational effectiveness, and preserve orientation in time and space emerged as notable determinants of functional abilities.
The significant association of rural residence with a decreased likelihood of the outcome contrasts with common perceptions and may reflect underlying socioeconomic and healthcare disparities (28). Gender differences, particularly the lower likelihood of the outcome among females, align with previous studies suggesting gender-specific risk factors and resilience mechanisms. The differential impact of income sources, notably the significant negative association of pension income, could be indicative of socioeconomic stability’s influence on health outcomes.
The contrasting associations of behavioral factors, such as aggressive behavior (29) and depression (30) symptoms, with the outcome underscore the complexity of behavioral health’s role. The significant association after adjustment for having a disease highlights the importance of considering comorbid conditions in evaluating health outcomes.
The substantial impact of social insurance types, especially the New Rural Cooperative Medical Insurance, suggests that healthcare accessibility and quality are critical determinants of health outcomes. These findings emphasize the importance of functional and social aspects in health, going beyond mere clinical or behavioral considerations. This aligns with the growing recognition of holistic health approaches, integrating physical, mental, and social well-being.
The results of this study underscore that respiratory and circulatory conditions (31), such as asthma (32) and cerebral infarction (33), significantly elevate the risk of CI. The observed increase in odds ratios for asthma and cerebral infarction emphasizes the need for vigilant monitoring and management in patients with these conditions.
Conversely, our study revealed a notable protective effect of hyperlipidemia and waist/lower back conditions (34) against CI. This counterintuitive finding, particularly for hyperlipidemia, which is often considered a risk factor for various health issues (35), suggests a potential area for further investigation. It raises questions about the underlying mechanisms that might confer this protection and how these might be leveraged in clinical practice.
The moderate increase in the likelihood of CI associated with difficulty in leg movement (36) could be indicative of broader mobility or lifestyle-related factors impacting health outcomes. This observation aligns with studies emphasizing the importance of physical mobility in overall health (37).
This study conducted an extensive door-to-door survey, meticulously targeting individuals aged over 80 years within a specific locale, with the objective of performing a thorough evaluation. The investigation revealed a range of demographic, social, and health challenges prevalent among older adults living in their own homes and examined their association with CI. This research thus offers a foundational dataset for future studies. It is crucial to acknowledge the limitations of this study, notably its focused demographic and methodological approach. Further investigation into the health status disparities between elderly individuals residing independently and those in nursing homes or healthcare facilities is essential. Additionally, the selection of participants should incorporate considerations of regional differences.
5 Conclusion
The study reveals correlation between CI and demographic and health factors. Urban-rural differences are evident, for social engagement playing a significant role. Logistic regression analysis highlights rural residence and female gender as protective against CI, while behavioral and health factors present a complex picture. Hyperlipidemia shows a protective effect. These findings underscore the multifaceted nature of CI and the importance of comprehensive assessment and intervention strategies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
Approval for this study was granted by the Ethical Committee of Jiangsu SuYi Health Care Research Institute (1/4/2022). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SB: Writing – review & editing, Writing – original draft, Resources, Methodology, Investigation, Formal Analysis, Data curation, Conceptualization. XT: Writing – review & editing, Supervision, Project administration, Investigation, Funding acquisition, Conceptualization. FM: Writing – review & editing, Methodology, Conceptualization. CX: Writing – review & editing, Project administration, Investigation, Data curation. YZ: Writing – review & editing, Investigation. QG: Writing – review & editing, Investigation. CB: Writing – review & editing, Investigation.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research was supported by the ability assessment project of the elderly aged 80 and above in Lishui District in 2022, project number CPZC-2022010. This research was supported by the National Natural Science Foundation of China-“ A study on the development of a digital therapy-based assessment tool for evaluating the sleep quality of middle-aged individuals and researching the O2O (Online to Offline) health management pathway”, project number 72364013.
Acknowledgments
We would like to thank De Hua Shi, You Shun Wang (Jiangsu SuYi Health Care Research Institute) for the statistics consultation.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ding D, Zhao Q, Guo Q, Liang X, Luo J, Yu L, et al. Progression and predictors of mild cognitive impairment in chinese elderly: A prospective follow-up in the shanghai aging study. Alzheimer's Dementia: Diagnosis Assess Dis Monit. (2016) 4:28–36. doi: 10.1016/j.dadm.2016.03.004
2. Deng Y, Zhao S, Cheng G, Yang J, Li B, Xu K, et al. The prevalence of mild cognitive impairment among chinese people: A meta-analysis. Neuroepidemiology. (2021) 55:79–91. doi: 10.1159/000512597
3. Shami A, Brennan M, Marie PS, Lindenauer PK, Stefan MS. The association of cognitive impairment as screened by the mini-cog with long term post-hospitalization outcomes. Arch Gerontology Geriatrics. (2019) 85:103916. doi: 10.1016/j.archger.2019.103916
4. Pais R, Ruano L P, Carvalho O, Barros H. Global cognitive impairment prevalence and incidence in community dwelling older adults—a systematic review. Geriatrics. (2020) 5:84. doi: 10.3390/geriatrics5040084
5. Ding D, Zhao Q, Guo Q, Meng H, Wang B, Luo J, et al. Prevalence of mild cognitive impairment in an urban community in China: A cross-sectional analysis of the shanghai aging study. Alzheimer's Dementia. (2015) 11:300–9.e2. doi: 10.1016/j.jalz.2013.11.002
6. Rujing R, Jinlei Q, Shaohui L, Xinya L, Peng Y, Zhihui W, et al. The China alzheimer report 2022. Gen Psychiatry. (2022) 35:e100751. doi: 10.1136/gpsych-2022-100751
7. Stewart R, Qu Y, Zhuo L, Li N, Hu Y, Chen W, et al. Prevalence of post-stroke cognitive impairment in China: A community-based, cross-sectional study. PloS One. (2015) 10(4):e0122864. doi: 10.1371/journal.pone.0122864
8. Artero S, Ancelin M-L, Portet F, Dupuy A, Berr C, Dartigues J-F, et al. Risk profiles for mild cognitive impairment and progression to dementia are gender specific. J Neurology Neurosurg Psychiatry. (2008) 79:979–84. doi: 10.1136/jnnp.2007.136903
9. Morley JE. An overview of cognitive impairment. Clin Geriatr Med. (2018) 34:505–13. doi: 10.1016/j.cger.2018.06.003
10. Zhong G., Wang Y., Zhang Y., Guo JJ., Zhao Y. Smoking is associated with an increased risk of dementia: a meta-analysis of prospective cohort studies with investigation of potential effect modifiers. PloS one. (2015) 10(3):e0118333. doi: 10.1002/alz.12068
11. Demurtas J, Schoene D, Torbahn G, Marengoni A, Grande G, Zou L, et al. Physical activity and exercise in mild cognitive impairment and dementia: an umbrella review of intervention and observational studies. J Am Med Directors Assoc. (2020) 21:1415–22.e6. doi: 10.1016/j.jamda.2020.08.031
12. Gottesman RF, Albert MS, Alonso A, Coker LH, Coresh J, Davis SM, et al. Associations between midlife vascular risk factors and 25-year incident dementia in the atherosclerosis risk in communities (Aric) cohort. JAMA Neurol. (2017) 74:1246–54. doi: 10.1001/jamaneurol.2017.1658
13. Solfrizzi V, Panza F, Colacicco A, D’introno A, Capurso C, Torres F, et al. Vascular risk factors, incidence of mci, and rates of progression to dementia. Neurology. (2004) 63:1882–91. doi: 10.1212/01.WNL.0000144281.38555.E3
14. Doi T, Verghese J, Shimada H, Makizako H, Tsutsumimoto K, Hotta R, et al. Motoric cognitive risk syndrome: prevalence and risk factors in Japanese seniors. J Am Med Directors Assoc. (2015) 16:1103.e21–.e25. doi: 10.1016/j.jamda.2015.09.003
15. Rost NS, Meschia JF, Gottesman R, Wruck L, Helmer K, Greenberg SM, et al. Cognitive impairment and dementia after stroke: design and rationale for the discovery study. Stroke. (2021) 52(8):e499–e516. doi: 10.1161/strokeaha.120.031611
16. Gao Q, Zang E, Bi J, Dubrow R, Lowe SR, Chen H, et al. Long-term ozone exposure and cognitive impairment among chinese older adults: A cohort study. Environ Int. (2022) 160:107072. doi: 10.1016/j.envint.2021.107072
17. Tiwary N, Treggiari MM, Yanez ND, Kirsch JR, Tekkali P, Taylor CC, et al. Agreement between the mini-cog in the preoperative clinic and on the day of surgery and association with postanesthesia care unit delirium: A cohort study of cognitive screening in older adults. Anesth Analgesia. (2021) 132:1112–9. doi: 10.1213/ane.0000000000005197
18. Chan CCH, Fage BA, Burton JK, Smailagic N, Gill SS, Herrmann N, et al. Mini-cog for the diagnosis of alzheimer’s disease dementia and other dementias within a secondary care setting. Cochrane Database Systematic Rev. (2019) 9. doi: 10.1002/14651858.CD011414.pub2
19. Han R, Tang Z, Ma L. Related factors of cognitive impairment in community-dwelling older adults in beijing longitudinal study of aging. Aging Clin Exp Res. (2019) 31:95–100. doi: 10.1007/s40520-018-0943-8
20. Wu M-S, Lan T-H, Chen C-M, Chiu H-C, Lan T-Y. Socio-demographic and health-related factors associated with cognitive impairment in the elderly in Taiwan. BMC Public Health. (2011) 11:22. doi: 10.1186/1471-2458-11-22
21. Arber S. Gender, marital status, and ageing: linking material, health, and social resources. J Aging Stud. (2004) 18:91–108. doi: 10.1016/j.jaging.2003.09.007
22. Xiang Y, Zare H, Guan C, Gaskin D. The impact of rural-urban community settings on cognitive decline: results from a nationally-representative sample of seniors in China. BMC Geriatrics. (2018) 18:323. doi: 10.1186/s12877-018-1003-0
23. Kelly ME, Duff H, Kelly S, McHugh Power JE, Brennan S, Lawlor BA, et al. The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: A systematic review. Systematic Rev. (2017) 6:259. doi: 10.1186/s13643-017-0632-2
24. Knopman DS, Gottesman RF, Sharrett AR, Wruck LM, Windham BG, Coker L, et al. Mild cognitive impairment and dementia prevalence: the atherosclerosis risk in communities neurocognitive study. Alzheimer's Dementia: Diagnosis Assess Dis Monit. (2016) 2:1–11. doi: 10.1016/j.dadm.2015.12.002
25. Johnston DW, Kassenboehmer SC, Shields MA. Financial decision-making in the household: exploring the importance of survey respondent, health, cognitive ability and personality. J Economic Behav Organ. (2016) 132:42–61. doi: 10.1016/j.jebo.2016.09.014
26. Goveas JS, Espeland MA, Woods NF, Wassertheil-Smoller S, Kotchen JM. Depressive symptoms and incidence of mild cognitive impairment and probable dementia in elderly women: the women's health initiative memory study. J Am Geriatrics Soc. (2011) 59:57–66. doi: 10.1111/jgs.2011.59.issue-1
27. Strömbäck C, Lind T, Skagerlund K, Västfjäll D, Tinghög G. Does self-control predict financial behavior and financial well-being? J Behav Exp Finance. (2017) 14:30–8. doi: 10.1016/j.jbef.2017.04.002
28. Dennison EM, Laskou F, Westbury LD, Bevilacqua G, Fuggle NR, Iidaka T, et al. Do lifestyle, anthropometric and demographic factors associated with muscle strength differ in a uk and Japanese cohort? An exploratory analysis. Aging Clin Exp Res. (2023) 35(12):3097–104. doi: 10.1007/s40520-023-02614-5
29. Margari F, Sicolo M, Spinelli L, Mastroianni F, Pastore A, Craig F, et al. Aggressive behavior, cognitive impairment, and depressive symptoms in elderly subjects. Neuropsychiatr Dis Treat. (2012) 8:347–53. doi: 10.2147/ndt.S33745
30. Lam RW, Kennedy SH, McLntyre RS, Khullar A. Cognitive dysfunction in major depressive disorder: effects on psychosocial functioning and implications for treatment. Can J Psychiatry. (2014) 59:649–54. doi: 10.1177/070674371405901206
31. Tsai N-C, Lee R-M. Interaction between cardiovascular system and respiration. Appl Math Model. (2011) 35:5460–9. doi: 10.1016/j.apm.2011.04.033
32. Anke H, Andrea V, Dorothea S, Michael JA, Ulrich R, Ursula K, et al. The role of air pollution and lung function in cognitive impairment. Eur Respir J. (2018) 51:1701963. doi: 10.1183/13993003.01963-2017
33. Saczynski JS, Sigurdsson S, Jonsdottir MK, Eiriksdottir G, Jonsson PV, Garcia ME, et al. Cerebral infarcts and cognitive performance. Stroke. (2009) 40:677–82. doi: 10.1161/STROKEAHA.108.530212
34. Wirick DM, Teufel-Prida LA. Chronic lower back pain: cognitive behavioral therapy with family therapy interventions. Family J. (2018) 26:86–9. doi: 10.1177/1066480718756845
35. Dai L, Zhong LLD, Cao Y, Chen W, Cheng Y, Lin X-F, et al. Efficacy and safety of yirui capsule in patients with hyperlipidemia: study protocol for a multicenter, randomized, double-blind, placebo-controlled trial. Trials. (2016) 17:291. doi: 10.1186/s13063-016-1419-9
36. Donaghy PC, Barnett N, Olsen K, Taylor JP, McKeith IG, O'Brien JT, et al. Symptoms associated with lewy body disease in mild cognitive impairment. Int J Geriatric Psychiatry. (2017) 32:1163–71. doi: 10.1002/gps.4742
Keywords: socio-economic, social interaction, diabetes, cognition function, mini-cog
Citation: Bian S, Tian X, Meng F, Xu C, Zhao Y, Gao Q and Bian C (2024) Assessing cognitive impairment in home-dwelling Chinese elders aged 80+: a detailed survey of 13,000 participants focusing on demographic factors, social engagement, and disease prevalence. Front. Psychiatry 15:1355708. doi: 10.3389/fpsyt.2024.1355708
Received: 15 December 2023; Accepted: 19 March 2024;
Published: 02 April 2024.
Edited by:
Madia Lozupone, University of Bari Aldo Moro, ItalyReviewed by:
Andrea Ballini, University of Foggia, ItalyRenata Kochhann, Moinhos de Vento Hospital, Brazil
Copyright © 2024 Bian, Tian, Meng, Xu, Zhao, Gao and Bian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fanli Meng, bWZsMTIwNkAxMjYuY29t
 Sensen Bian
Sensen Bian Xiaobing Tian2
Xiaobing Tian2