
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 05 February 2024
Sec. Public Mental Health
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1353088
This article is part of the Research Topic Parents with Mental and/or Substance Use Disorders and their Children, Volume III View all 33 articles
 Vanessa Seipp1*
Vanessa Seipp1* Klara Hagelweide2
Klara Hagelweide2 Rudolf Stark3
Rudolf Stark3 Sarah Weigelt2
Sarah Weigelt2 Hanna Christiansen4
Hanna Christiansen4 Meinhard Kieser5
Meinhard Kieser5 Kathleen Otto6
Kathleen Otto6 Corinna Reck7
Corinna Reck7 Ricarda Steinmayr8
Ricarda Steinmayr8 Linda Wirthwein8
Linda Wirthwein8 Anna–Lena Zietlow9
Anna–Lena Zietlow9 Christina Schwenck1 and the COMPARE-Family Research Group
Christina Schwenck1 and the COMPARE-Family Research GroupObjective: Children of parents with a mental illness are at heightened risk to develop a mental illness themselves due to genetics and environmental factors. Although parenting stress (PS) is known to be associated with increased psychopathology in parents and children, there is no study investigating PS multimodally in a sample of parents with a mental illness. This study aims to compare PS of parents with and without a mental illness and further to examine the relationship between PS and psychopathology of children.
Methods: Participants were parents with a mental illness and parents without a mental illness and their children aged four to sixteen years. We assessed PS multimodally using a questionnaire, parents’ evaluation of children’s behavior (relational schemas) and psychophysiological arousal of parents during free speech task.
Results: Self-reported PS was increased, and evaluation of children’s behavior was more negative and less positive in parents with a mental illness compared to parents without a mental illness. Children’s psychopathology was associated with self-reported PS and relational schemas of parents. Regarding psychophysiological arousal, parents with a mental illness showed reduced reactivity in heart rate from baseline to free speech task in comparison to parents without a mental illness.
Conclusions: Our findings highlight the importance of implementing intervention programs to reduce PS for parents and children. In particular, parents with a mental illness might benefit from specific intervention programs in order to interrupt the transgenerational transmission of mental disorders.
In Germany, approximately three million children live with a parent with a mental illness (1). Children of parents with a mental illness (COPMI) show three to seven times higher rates of subclinical symptoms (2), poorer health-related quality of life (3) and lower academic achievement (4) compared to children of parents without a mental illness (COPWMI). Due to genetics as well as environmental factors, COPMI are particularly at risk of developing a mental disorder themselves (5, 6). Compared to COPWMI, this risk is two to five times higher (7). Therefore, a transgenerational transmission of mental disorders (TTMD) can be assumed. The association between the parental mental illness and children’s psychopathology depends on different variables and risk constellations (8). Thus, COPMI constitute a high-risk group that needs to be identified and addressed by prevention programs in order to reduce their risk and prevent future mental disorders in this group (6). The model of the TTMD identifies five transmission mechanisms and their interaction related to parent, child, family and social environment contributing to the heightened risk of COPMI to develop a mental disorder themselves (9). Besides genetics, prenatal and social factors, parenting is considered to be a core mechanism in TTMD (9, 10). Parenting is comparably easy to address through preventive measures and interventions. However, there is a lack of studies investigating parenting in COPMI (e.g., (11)), and thus it remains open how this should be targeted optimally. In this context, parenting stress (PS) is of particular importance because it is associated with maladaptive parenting (12) and psychopathology of parents and children (13–15). One purpose of this study, therefore, is to examine PS using multimodal data in parents with and without a mental illness.
According to Bowlby’s attachment theory (16), attachment determines how children can regulate their emotions and behavior. While secure attachment is associated with positive developmental outcomes in children (17), insecure attachment is associated with negative outcomes in children and is considered a risk factor for developing a mental illness (17, 18). Positive parenting (e.g. sensitive parenting) provides the foundation for a secure parent-child bond and is considered to be the cornerstone of children’s biological, cognitive, social, and emotional development (19, 20). Stress related to parenting is a normal response experienced by all parents at times (21). It can be helpful as it prompts the use of resources to support positive parenting behaviors (22). It is rather the cumulative impact of stress that adversely affects parenting behavior, the parent-child-interaction and children’s development (21, 23–25). PS is defined as “a set of processes that leads to aversive psychological and physiological reactions arising from attempts to adapt to the demands of parenthood” resulting in negative feelings and beliefs regarding the self and the child (25). There are several theories that help explain how PS affects well-being of parents and children. Abidin (22) postulates that high level of PS reinforces the use of maladaptive parenting behavior and thus negatively influences the development of children, which is confirmed by several studies (12, 26–29). Furthermore, the model of Abidin (22) postulates that aspects of parents, children and environment affect PS. Regarding environmental aspects, several studies highlight the link between PS and social support (30), partnership satisfaction (31) and socioeconomic status (30). Regarding aspects of children, research showed that insecure attachment (26) and internalizing as well as externalizing behavior problems (32) are associated with PS. With respect to aspects of parents, several studies found that parental psychopathology plays a significant role (33–35). According to the transactional model (36), stress has an impact on a behavioral level as well as on a cognitive and affective level. In addition to behaviors, cognitions and affects can also be passed on from parents to children (10) suggesting cognitive processes play an important role how PS affects child outcomes. Additionally, psychophysiological theories can help to explain how PS leads to physiological stress responses in parents and adversely affects interacting with their children (37, 38). Another purpose of this study, therefore, is to examine how cognitive and psychophysiological aspects of PS are associated with psychopathology in children.
High levels of stress are associated with automatic and rigid rather than controlled and flexible information processing (39, 40). Thus, parents with high levels of PS are less able to understand the child’s behavior within the actual context and are more likely to evaluate the child’s behavior in a more negative way (39, 40). In line with this, studies that found that parents with high levels of PS tend to perceive their child as more difficult and subsequently display more negative affectivity towards it (41–43). A growing body of literature confirms the relation between PS and parental negative attributions of child behavior (41, 44–46). Moreover, a study found that negative attributions mediated the association between PS and maladaptive parenting behaviors (41). Relational schemas (RS) guide parent’s attributions of the intent of their child’s behaviors (47). RS are described as an overlearned and unconscious semantic schema guiding actions and reactions to interpersonal events (48). The interpretation that a child is provoking or intentionally frustrating can be called a negative RS (49). In contrast to that, the interpretation of the child’s behavior as compliant or responsive to the caregiver can be called a positive RS (49). Besides, RS include parent’s sets of implicit beliefs and affective attitudes towards their children (50). Parents’ internal representations can be assessed verbally during the Five-Minute Speech Sample (FMSS; (51)). The FMSS provides independent data that are free from biases associated with self-reports (52). Because RS are part of an unconscious, automatic cognitive process and operate largely outside of the caregiver’s awareness (49), Bullock and Dishion (50) developed the Family Affective Attitude Ratings Scale (FAARS) to identify RS expressed by parents during FMSS (51).
Besides information processing, high levels of stress also have an influence on physiological arousal. A key system of physiological arousal is the autonomic nervous system (ANS) which subdivides into the sympathic (SNS) and parasympathic nervous system (PNS; (53)). During stress, SNS produces increased physiological arousal, such as increased heart rate (HR), whereas during periods of stability PNS lowers HR. Heart rate variability (HRV) is a measure of the interplay between SNS and PNS on the HR, and a flexible HRV allows for modulation of arousal depending on situational demands (53). Since emotion regulation depends on flexible adjustment of ANS, HRV is known to be an important index (53). Regarding parent-child-interaction, stress can adversely affect the parent’s ability to regulate emotions (37) and to respond appropriately to the child’s needs (38). A “spillover effect” can decrease emotion regulation skills in children (54) and can consequently lead to increased psychopathology (55). There are some studies suggesting a relation between parenting behaviors and physiological reactivity in parents (38, 56–60). However, the direction of this relation is contradictory. On the one hand, there is evidence that increased reactivity in parents is associated with maladaptive parenting behavior (58, 59). On the other hand, studies found decreased reactivity in parents associated with maladaptive parenting behavior (38, 56, 57, 60). Reasons for the inconsistent results may be found in differences in laboratory tasks, physiological indicators or analytic strategies (60). Fundamental frequency corresponds to the perceived voice pitch and it is determined by the frequency with which the vocal folds open and close when forming sounds (61, 62). Fundamental frequency correlates strongly with established indicators of ANS (e.g. heart rate, blood pressure, and cortisol) and with self-reported emotional state (63, 64). A study confirmed that higher fundamental frequency range was associated with higher emotional arousal (64). While there are some studies examining fundamental frequency in couple relationships (61, 65, 66), there are only a few studies dealing with parent-child relationships or mental illness. A study showed that during conflict talks between adolescents and their parents, higher range of fundamental frequency was associated with higher cortisol levels and more self-reported negative emotionality of parents and adolescents (63).
According to the model of Abidin (22), PS is linked to the psychopathology of both parents and children. Psychopathology increases vulnerability to stress because it reduces access to coping skills that are necessary to decrease stress levels (67). Therefore, a mental illness diminishes the parent’s resources (68). Moreover, the use of ineffective coping strategies can lead to chronically high levels of PS in parents with a mental illness (22, 69). Several studies confirmed the relationship between PS and depression and anxiety symptoms (33–35, 70–74). Independently from psychopathology in parents, a growing body of literature found PS to be related to several negative child outcomes such as internalizing and externalizing behavior problems (75, 76). Longitudinal studies suggest that the relationship between children’s psychopathology and PS is bidirectional (13, 14). Thus, elevations in children’s behavior problems lead to increased PS, which then leads to increased behavior problems in children. Additionally, a longitudinal study found that children’s externalizing behaviors decreased if PS does and vice versa (77). Fredriksen et al. (70) found a mediating effect of PS between parental depressive symptoms and negative child outcomes in a longitudinal study. The findings suggest that PS plays an important role in TTMD. Noteworthy, the research mentioned above used self-report measures only to assess parental and child psychopathology as well as PS that can lead to biased information and compromises objectivity (11). Parents with more psychopathological symptoms might have stronger negative self-appraisals, which lead to elevated reports of PS and psychopathology of children (78). Furthermore, most studies investigated parents with sub-clinical psychopathological symptoms (33). Future research needs to investigate PS multimodally in parents with clinically relevant diagnosis (33, 69, 78). This is especially true regarding the role of PS in TTMD. Therefore, research on parental information processing, as interpretation and beliefs about their children’s behavior is of particular interest. In this term, assessing RS of parents during FMSS can provide an independent data source that is free from biases associated with self-reports (49). Recent studies found that less positive and more negative RS of parents are associated with higher psychopathology in children (49, 79, 80). Moreover, a study found an association between negative RS and increased stress and psychopathology in parents in a clinical-referred child sample (79). Besides, psychophysiological arousal of parents can provide an objective measure of PS (69, 81, 82). To the best of our knowledge, there is no study investigating RS and psychophysiological arousal of parents with a mental illness. Comparing parents with and without a mental illness allows examining psychopathology as a specific risk factor for PS. Since PS is considered a relevant factor in TTMD, it is of clinical importance to gain detailed insight in this relation. This is especially true because PS displays a target for intervention. Examining how PS relates to psychopathology in children regardless of a parental mental illness allows developing specific intervention programs to reduce the risk for negative child developmental outcomes.
The current study aims to examine parenting stress in parents with a mental illness compared to parents without a mental illness. In order to gain detailed insight into how cognitive and psychophysiological aspects of parenting stress adversely correlates to child outcomes, we investigate the relation of parenting stress and psychopathology in children regardless of a parental mental illness. We examine parenting stress multimodally by self-report, parents’ relational schemas and psychophysiological data.
We aim to address the following hypotheses:
1. Parents with a mental illness report higher parenting stress than parents without a mental illness.
2. Increased self-reported parenting stress is positively correlated with psychopathology in children regardless of parents’ diagnostic status.
3. Parents with a mental illness show more negative and less positive relational schemas than parents without a mental illness.
4. Valence of relational schemas are negatively correlated with psychopathology in children regardless of parents’ diagnostic status.
5. Parents with a mental illness show reduced reactivity in heart rate variability and heart rate from baseline assessment to Five Minute Speech Sample compared to parents without a mental illness.
6. Parents with a mental illness show higher fundamental frequency range during the Five Minute Speech Sample than parents without a mental illness.
7. Psychophysiological arousal in parents is correlated with psychopathology in children regardless of parents’ diagnostic status.
The current study is part of the German prospective multicentre RCT Children of Mentally Ill Parents At Risk Evaluation (COMPARE-family; grant number: 01GL1748B) and its add on-project COMPARE-emotion (grant number: 01GL1748C and 01GL1748E). For detailed description of this study, see study protocols (5, 83). Parents with a mental illness were recruited as part of the prospective multicenter RCT COMPARE-family (5, 83). Patients were recruited from the outpatient clinics of the universities of Gießen, Bochum, Marburg and Landau. In the study centers, we used the universities’ mailing lists, mailings of families with children in the corresponding age range provided by local registry offices, and public advertisement (flyer, newspaper, online-platforms) as recruitment tools. Parents without a mental illness were recruited as part of the add-on project COMPARE-emotion in study centers Gießen and Dortmund. Parents without a mental illness and their children were recruited by mailings of children in the corresponding age range provided by local registry offices, public advertisement (flyer, online-platforms), and the research group’s database of former study participants. Inclusion criteria for COMPARE-emotion were: a) children between 4 to 16 years of age; b) parents agreeing to participate in a videotaped paradigm; c) parents seeking psychotherapeutic treatment and meeting diagnostic criteria of a mental illness according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; (84)) for parents with a mental illness; or d) parents with no mental illness and no psychotherapeutic treatment during the life of parents without a mental illness; e) children living with the participating parent for at least half of the week.
Exclusion criteria were a) insufficient German language skills; b) children presenting severe impairment requiring urgent treatment; c) parental ongoing outpatient or inpatient treatment; d) regular use of benzodiazepines as is thought to hamper cognitive behavioral therapy; e) parents without a mental illness reporting psychopathological symptoms above the cut-off value in the Brief Symptom Inventory (85); f) COPWMI meeting diagnostic criteria according to the DSM-5 (84). Local ethics committees at all participating universities approved the study. All participants provided written informed consent. For participation, each child received a gift or a financial allowance of €5. Parents without a mental illness and their children participated once, while parents with a mental illness and their children participated in repeated assessments at three measurement points (83). For the current study, we analyzed data of the first assessment point in parents with a mental illness participating in the study centers Giessen, Bochum, Marburg and Landau.
Before participating in the laboratory assessment of COMPARE-emotion, families provided written informed consent and completed several questionnaires online. Assessments took place at the laboratories of the Universities of Gießen, Dortmund, Marburg and Landau between 2018 and 2022 and lasted one hour. During the assessment, we conducted different paradigms with the dyads including the FMSS (51) for assessment of RS and fundamental frequency to measure psychophysiological arousal in parents. Due to availability of the ECG-equipment, we assessed psychophysiological arousal via HR and HRV exclusively in Gießen. Parents placed three electrodes on themselves (one over the right collarbone and one over each of the lower ribs) at the start of the assessment. Once the ECG signal was registered, parents were asked to sit quietly and describe a picture puzzle for one minute. After completion of the baseline period, parents performed the FMSS. Here, parents were asked to speak for five minutes about their thoughts and feelings regarding their child and how they get along together. We recorded baseline period and speech samples on video camera and converted them to wav-audio files for further analyses.
We conducted analyses with different sample sizes because not all families participating in laboratory assessment completed the questionnaires of parenting stress and psychopathological symptoms of children. Thus, we included all available data sets and did not exclude families of our analyses because of missing values. Besides, we assessed electrocardiographic (ECG) activity exclusively in the study center Gießen. Demographic information for sub-samples are described below.
Five Minute Speech Samples of 189 independent parent-child dyads were available (n = 91 parents with a mental illness, n = 98 parents without a mental illness). Data of the dyads were used for analyses of RS and fundamental frequency. Since not all parents returned the questionnaire, information about psychopathology of children (n = 20 in COPMI, n = 3 in COPWMI) was missing. Due to technical problems that led to the video-files not being readable, baseline-recordings of parents (n = 8) were missing. Of the parents performing the Five Minute Speech Sample, 150 were mothers (79%) and 100 children were female (53%). Children ranged from four to 16 years of age (M = 9.08, SD = 3.40). Groups did not differ in age, gender or parents’ gender but in parents’ age, parents’ and children’s psychopathological symptoms and socioeconomic status (SES; see Table 1). COPMI showed higher psychopathological symptoms than COPWMI. Parents with a mental illness were younger and their SES was lower. According to Lampert et al. (86), the SES of parents without a mental illness can be classified as high, while the SES of parents with a mental illness can be classified in the middle status group. We used a structured diagnostic interview to determine mental disorders and verify diagnostic criteria for study inclusion of parents with a mental illness. The most common disorders among parents were Depressive Disorders as primary diagnosis (42%), followed by Trauma- and Stressor-Related Disorders (28%), Anxiety Disorders (23%), Somatic Symptom and Related Disorders (3%), Feeding and Eating Disorders (1%), Personality Disorders (1%), Disturbance of Activity and Attention Disorders (1%) and Schizophrenia Spectrum and Other Psychotic Disorders (1%). The mean number of comorbid diagnosis was two (SD = 1.22, range from 1 - 5), and severity of the primary diagnosis ranged from four to eight (M = 5.88, SD = 0.91) on a 9-point-Likert-Scale. Digits in this range indicate a clinical diagnosis.
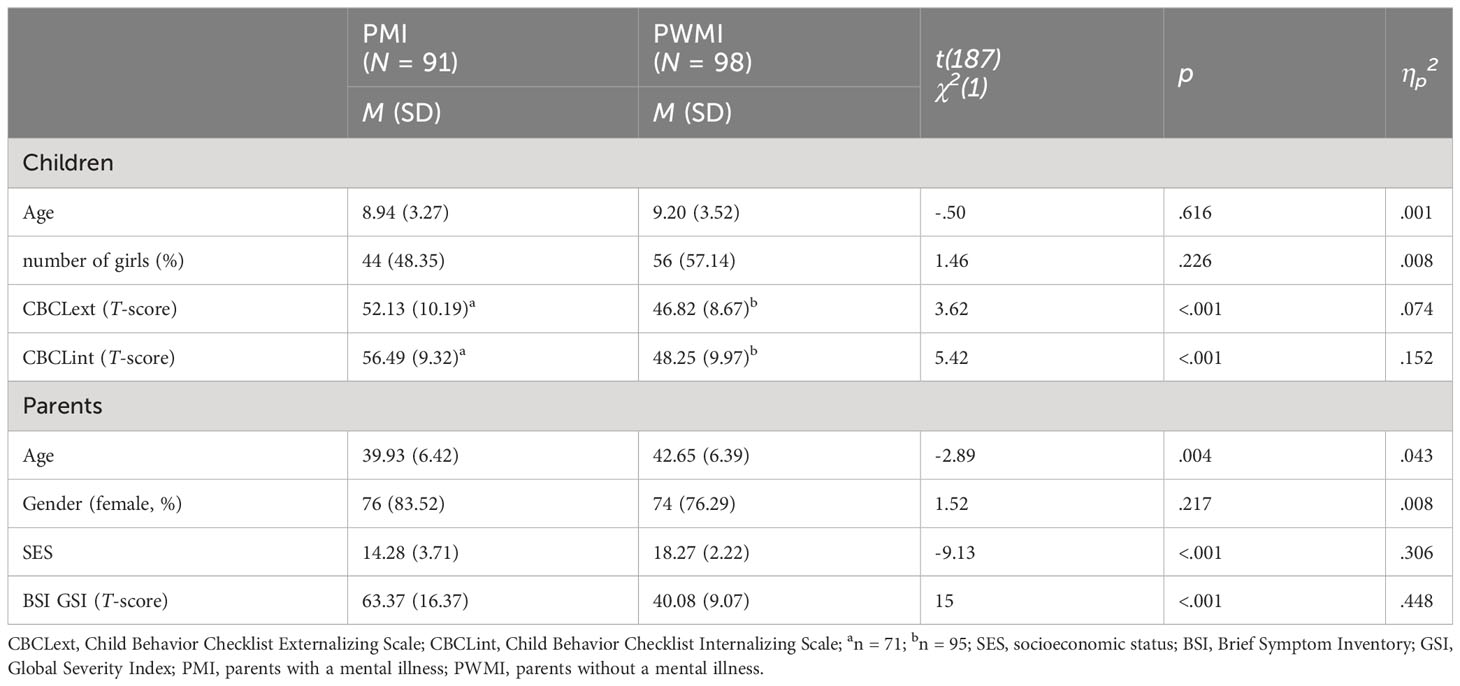
Table 1 Demographic characteristics of participants and means and standard deviations of psychopathological symptoms of children and parents for analyses with the Five Minute Speech Sample.
Self-reported PS was available from n = 54 data sets of parents with a mental illness and n = 96 data sets of parents without a mental illness. Of this sub-sample, 118 were mothers (79%) and 79 children were female (53%). Children ranged from four to 16 years of age (M = 8.67, SD = 3.23). Groups did not differed in gender of children and parents, but in age of children and parents, psychopathological symptoms of children and parents, and SES (see Table 2). In this sub-sample, COPMI were younger than COPWMI. The most common disorders among parents of this sub-sample were Depressive Disorders as primary diagnosis (39%), followed by Trauma- and Stressor-Related Disorders (31%), Anxiety Disorders (22%), Somatic Symptom and Related Disorders (4%), Feeding and Eating Disorders (2%) and Schizophrenia Spectrum and Other Psychotic Disorders (2%). The mean number of comorbid diagnosis was two (SD = 1.26, range from 1 - 5), and severity of the primary diagnosis ranged from four to eight (M = 5.80, SD = 0.98).
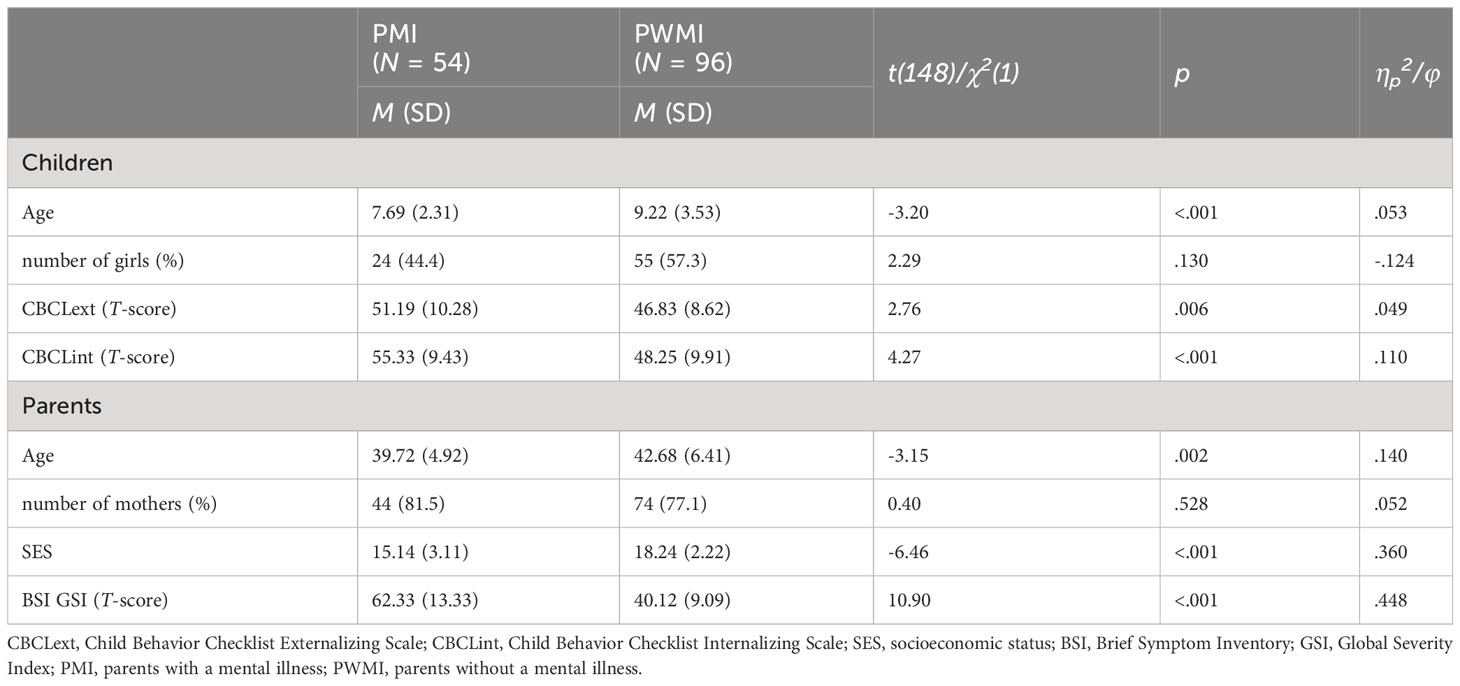
Table 2 Demographic characteristics of participants and means and standard deviations of psychopathological symptoms of children and parents for analyses of self-reported parenting stress.
ECG recordings were available from n = 30 data sets of parents with a mental illness and n = 33 data sets of parents without a mental illness. Data of this sample were used for analyses of HR and HRV. Of this sub-sample, 48 were mothers (76%) and 36 children were female (57%). Parents ranged from 24 to 56 years of age (M = 41.72, SD = 7). Groups did not differed in children’s age, children’s gender or parent’s gender but in age and psychopathological symptoms of parents and SES (see Table 3). In this sub-sample, COPMI did not differed in externalizing psychopathological symptoms. The most common disorders among parents of this sub-sample were Depressive Disorders as primary diagnosis (37%), followed by Trauma- and Stressor-Related Disorders (27%) and Anxiety Disorders (27%), Somatic Symptom and Related Disorders (3%), Personality Disorders (3%) and Schizophrenia Spectrum and Other Psychotic Disorders (3%). The mean number of comorbid diagnosis was two (SD = 1.97, range from 1 - 5), and severity of the primary diagnosis ranged from four to eight (M = 5.93, SD = 0.79).
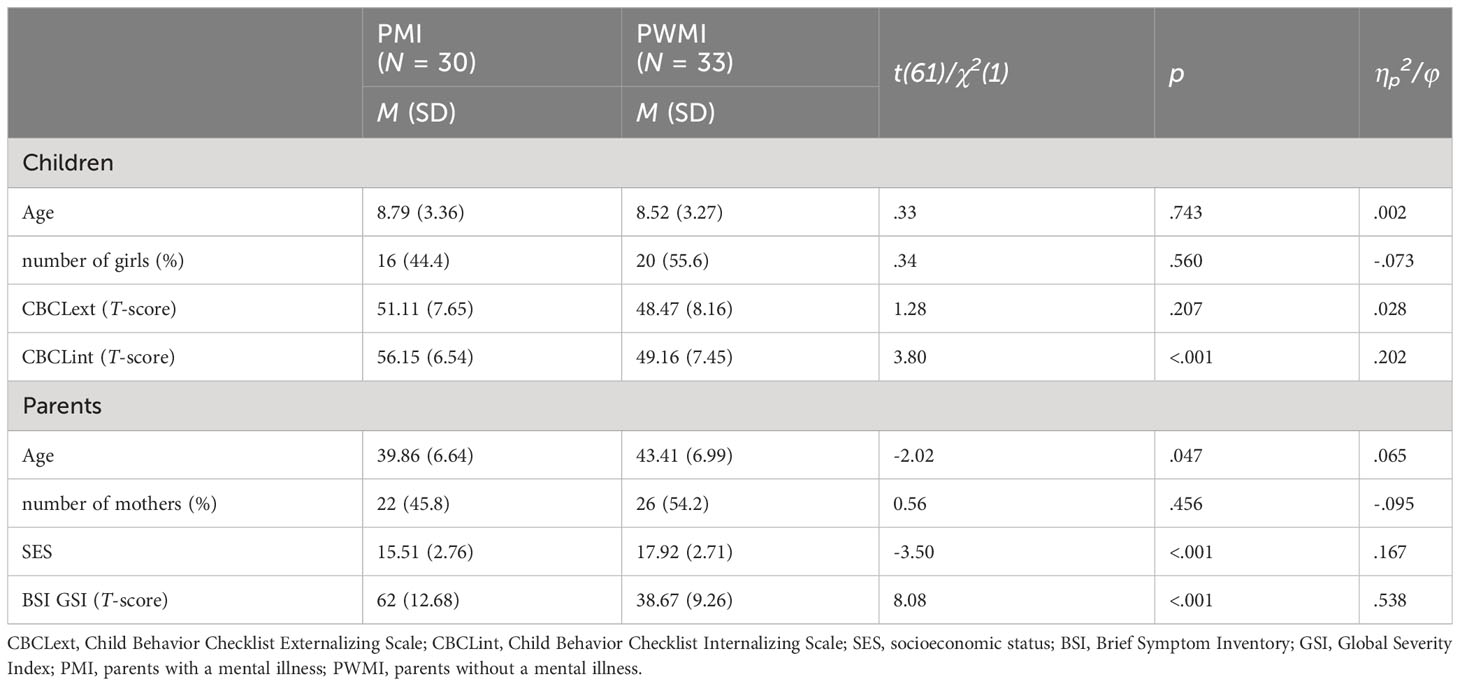
Table 3 Demographic characteristics of participants and means and standard deviations of psychopathological symptoms of children and parents for analyses of electrocardiographic activity.
We assessed parental RS using the Family Affective Attitude Rating Scale (FAARS; (87)). The FAARS is an extension and re-formulation of the original FMSS coding system (51) for parents of children in childhood and adolescence (50). The measures of RS consist of items reflecting negative and positive attitudes relevant for parent-child-relationship. Respective items score on a 9-Point-Likert-Scale from 1 (not present) to 5 (one concrete example) to 9 (multiple examples). Following the methodology of Bullock and Dishion (50), we averaged respective items reflecting positive RS and negative RS. The scale for positive RS derived from the mean of the five items: parent is positive regarding the child’s behavior, parent is positive regarding the child’s traits, parent reports a positive relationship with the child, parent attributes positive intentions of the child, parent makes statements of caring and loving. For computing the scale of negative RS, we used the mean of the five items: parent is critical of the child’s behavior, parent is critical of the child’s traits, parent reports a negative relationship with the child, parent attributes negative intentions of the child, parent reports of conflict or anger. To assess inter-rater reliability, two raters coded speech samples independently and blind to parental diagnostic status. As recommended by Bullock et al. (87), for our study we calculated inter-rater reliability ratings from 25% of analyzed samples. Indicating good consensus among the coders, intraclass correlations ranged from 0.86 to 0.91 (M = 0.89) for negative RS and from 0.95 to 0.97 (M = 0.96) for positive RS. Cronbach’s alpha values indicate good internal consistency with negative RS (α = 0.83) and positive RS (α = 0.80). Our results are similar to those reported in previous FAARS validation studies (50, 79, 80).
We assessed parents’ fundamental frequency during a baseline period and FMSS. Prior to calculating fundamental frequency, baseline and FMSS wav-audio files were cleaned for artefacts (experimenter speaking, laughter, etc.) using a cutting program (Audacity, Version 3.0.0). We included the normal range of speech in our analyses by setting the floor at 75 Hz and the ceiling at 300 Hz (88). Using the voice analysis program Praat (Version, 6.1.56; (89)), we assessed minimum and maximum values in 0.25 second intervals. Fundamental frequency range was calculated by subtracting minimum from maximum values for each data set.
We used the BIOPAC system MP160 (90) and the portable bionomadix modules for assessing electrocardiographic (ECG) activity with an acquisition sample rate of 1000 Hz. 3-point ECG using Ag/AgCl electrodes (one over the right collarbone and one over each of the lower ribs) were installed on parents’ thoraxes. The physiological data were processed using the Acqknowledge software (Version 5.0.8; (90)). We inspected the ECG signals using Kubios HRV Scientific software (Version 4.0.1). The software identified successive R spikes via an automatic beat detection algorithm, we visually inspected and corrected for artefacts. Mean HR was calculated in beats per minute (bpm) based on the ECG channel. We used the time-domain index “root mean square of successive differences between normal heartbeats” (RMSSD) for calculating HRV. We choose RMSSD, because it is less affected by respiratory rate (91). For detailed description of RMSSD see Shaffer and Ginsberg (92).
To assess parental stress experience, we used the German “Parenting-Stress-Questionnaire” versions for children in kindergarten, preschool and school (ESF; (93)). The ESF consists of 38 items rated on a 4-point Likert Scale from 0 (disagree) to 3 (fully agree). Items are aggregated into the four scales, parenting stress (e.g. perceived parenting skills, stress in interaction with the child), role restriction (perceived limitations associated with raising the child), social support (perceived support from relatives, friends and close environment) and partnership (e.g. perceived support from the partner, agreement on parenting issues). For partnership, the respective items were answered only if the parent was currently living with a partner. Domsch and Lohaus (93) reported internal consistencies ranging from acceptable (Cronbach’s alpha = 0.76 for social support) to very good (Cronbach’s alpha = 0.92 for parental stress).
We used the German versions of the parent-reported questionnaire Child Behaviour Checklist (CBCL). Depending upon the children’s age to assess psychopathology of COPMI and COPWMI, we applied the CBCL 1½-5 (94) or the CBCL 6-18R (95). The German version of the CBCL 1½-5 (94) assesses problems of children between 1,5 and 5 years of age. It includes 99 items rated on a 3-point Likert Scale from 0 (never or not true) to 2 (often or very true). The German version of CBCL 6-18R captures problems of children and adolescents ageing from 6 to 18 years. It includes 120 items rated on a 3-point Likert Scale from 0 (never or not true) to 2 (often or very true). In both versions, items are aggregated into three superordinate scales (externalizing problems, internalizing problems and total problems). Achenbach and Rescorla (94) reported good to very good internal consistencies for CBCL 1½-5 (Cronbach’s alpha = 0.89 - 0.95) as well as Döpfner et al. (95) for CBCL 6-18R (Cronbach’s alpha = 0.82 - 0.93).
We used the German version of the self-reported questionnaire Brief Symptom Inventory (BSI (85);) to assess psychopathology of parents with and without a mental illness. The BSI contains 53 items rated on a 5-point Likert Scale from 0 (not at all) to 4 (very much). We aggregated items into Global Severity Index (GSI). Derogatis (85) reported internal consistency of GSI to be very good (Cronbach’s Alpha = .97). We invited parents without a mental illness to further diagnostic examination and excluded them of our analyses if the GSI was above the cut-off value (TGSI ≥ 62). The Diagnostic Interview for Mental Disorders (DIPS; (96)) is a structured diagnostic interview to determine mental disorders according to the DSM-5 (84). We used the DIPS to verify diagnostic criteria for study inclusion of parents with a mental illness. The interview has a good to very good inter-rater reliability (97). The Diagnostic Interview for Mental Disorders During Childhood and Adolescence (Kinder-DIPS; (98)) and the Structured Interview for Preschool Age (SIVA; (99)) are structured diagnostic interviews to determine mental disorders from age of six to adulthood (Kinder-DIPS) as well as in preschool children (SIVA) according to DSM-5 (84). We used the parent-report versions of both for children’s diagnostic assessment. Good to very good interrater reliabilities are reported for both the Kinder-DIPS (100) and SIVA (99). In COPMI, we conducted diagnostic interviews by default. In COPWMI, we conducted diagnostic interviews if total problem scale of CBCL was above the cut-off value (TCBCLSum ≥ 60).
We assessed SES of parents with and without a mental illness according to the KiGGS study (101). The SES-index was calculated as a point-sum score from 1 to 7 based on parents’ information on their schooling and occupational qualifications (1 = not finished school and professional training to 7 = high school SAT-level and university degree), occupational status (1 = in professional training or unskilled employee to 7 = executive or self-employed), and net equivalent income (1 = less than €1250 net income per month to 7 = more than €5000 net income per month). This allows to calculate a multidimensional SES-index ranging between 3.0 and 21.0 (86). Alternatively, SES can be categorized into status groups from low (range: 3.2 -8.7) to high (range: 17.0 – 21.0), each including 20% of children and adolescents of a representative German sample. The more broadly defined middle status group (range: 8.8 – 16.9) includes 60% of children and adolescents of a representative sample (86). We used this categorization to compare the SES of our study’s samples with a representative sample. Based on the mean SES of our samples, parents with a mental illness and their children can be assigned to the middle status group, whereas the mean SES of parents without a mental illness and their children can be categorized as high (see Tables 1–3).
We performed statistical analyses using SPSS version 28.0 (102). To address the need for confounding variables in further analyses, we examined possible differences in demographic characteristics between groups (two-sample t-test or chi-square test, respectively; see Tables 1–3). Since groups differed on SES, parents’ and child age, we conducted correlation analyses with all dependent variables. Since studies have shown that PS is associated with SES (30) and because of significant correlations with self-reported PS (p <.05), we included SES as a covariate in respective analyses. Furthermore, we found significant correlations of child age and self-reported PS (p <.05). Since studies produced mixed findings regarding the association of age of children and PS (30, 77), we decided to include child age as a covariate in respective analyses to minimize potential biases in our results.
We applied an alpha level of 0.05 (two-tailed) and calculated effect sizes (ηp2) for all statistical analyses. As multiple testing leads to an inflation of the alpha error and hence an increased likelihood of type 1 errors, we used Bonferroni-Holm correction for hypotheses 1 to 4, 6 and 7. The described p-values for the inferential statistical tests are already adjusted and can be compared with the applied alpha level. Due to missing values in questionnaires, we examined if parents reporting higher psychopathological symptoms during the DIPS (96) were more likely not to return the questionnaires. For that, we conducted a t-test for independent samples in corresponding analyses. In addition, we performed analyses of questionnaire data with multiple imputations in order to test the robustness of our results. In general, results did not differ between analyses with and without multiple imputations.
To test for differences in self-reported PS between groups (Hypothesis 1), we conducted a multivariate analysis of covariance (MANCOVA) with group (parents with vs. without a mental illness) as a between-subject variable. SES and age of children were included as covariates. Scales of self-reported PS were dependent variables. We used Pillai’s trace as the statistic measure to test for significance. Significant effects were decomposed using univariate ANCOVAs.
To examine the association of self-reported PS and children’s psychopathology (Hypothesis 2), we applied a partial correlation analysis with group, SES and age of children as control variables. We used Pearson’s r correlation coefficients as statistic measures.
To test for differences in parental RS in both groups (Hypothesis 3), we conducted a multivariate analysis of variance (MANOVA) with group (parents with vs. without a mental illness) as a between-subject variable and parents’ positive and negative RS as dependent variables. We used Pillai’s trace as the statistic measure to test for significance. Significant effects were decomposed using univariate ANOVAs.
To examine the association of parental RS and children’s psychopathology (Hypothesis 4), we conducted a partial correlation analysis with group as a control variable. We used Pearson’s r correlation coefficients as statistic measures.
To test for differences in fundamental frequency range in both groups (Hypothesis 5), we applied an ANOVA with repeated measures with group (parents with vs. without a mental illness) as between-subject factor and fundamental frequency range of phase (baseline, FMSS) as dependent variable, which we entered as a within-subject factor. We used the F-statistic as a statistic measure to test for significance.
To test for differences in HR and HRV in both groups (Hypothesis 6), we conducted a MANOVA with repeated measures with group (parents with vs. without a mental illness) as between-subject factor. Mean HR and HRV of each phase (baseline, FMSS) were dependent variables, which we entered as within-subject factors. We used Pillai’s trace as the statistic measure to test for significance. Significant effects were decomposed using univariate ANOVAs.
To examine the association of parent’s psychophysiological arousal and children’s psychopathological symptoms (Hypothesis 7), we applied a partial correlation analysis with group as a control variable. We included parents’ psychophysiological arousal during FMSS (fundamental frequency range, HR and HRV) and children’s psychopathological symptoms in partial correlation analysis. We used Pearson’s r correlation coefficients as statistic measures.
Regarding self-reported PS, a significant group difference with a large effect size was found in MANCOVA, V = 0.19, F(4, 143) = 8.33, p <.001, ηp2 = .189. However, univariate ANCOVAs on the outcome variables revealed non-significant group differences on PS, F(1, 146) = 0.21, p = .644, and on role restriction, F(1, 146) = 2.39, p = .124. We found a significant group difference on social support, F(1, 146) = 28.42, p <.001, and support in parental relationship, F(1, 146) = 6.10, p = .045, with parents with a mental illness reporting less social support and less support in parental relationship (for means and standard deviations, see Table 4). 15% of parents with a mental illness (n = 8) reported living without a partner, whereas this was reported by 4% of parents without a mental illness (n = 4). Due to missing values of self-reported PS in parents with a mental illness (n = 54, 41% missing), we examined if parents reporting higher psychopathological symptoms during the diagnostic interview were more likely not to complete the questionnaire. For that, we conducted a t-test for independent samples with group (questionnaire complete vs. missing) as independent and severity of primary diagnosis as dependent variable. Results indicated that groups do not differ in severity of psychopathological symptoms, t(89) = -1.056, p = .294, ηp2 = 012.
We conducted partial correlation analyses of self-reported PS, CBCLint, and CBCLext with group, age of children and SES as control-variables (see Table 5). We found significant correlations of CBCLext with self-reported PS. All significant correlation coefficients were in the expected direction with positive associations between psychopathological symptoms and PS. Significant correlation coefficients can be classified as moderate (103).
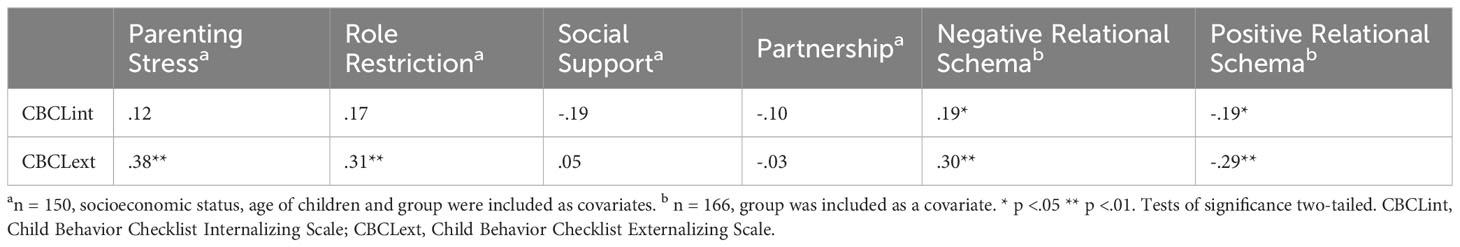
Table 5 Partial correlation analysis of self-reported parenting stress, parent’s relational schema, and children’s psychopathological symptoms.
To test for differences in talking time during FMSS, we conducted a t-test for independent samples with group (parents with vs. without a mental illness) as independent and talking time (in minutes) as dependent variable. There was a significant group difference (t(187) = -2.59, p = .010). Parents with a mental illness talked for a shorter time (M = 2.96, SD = .90) compared to parents without a mental illness (M = 3.31, SD = .92). Since parents differed in terms of their talking time during FMSS, we conducted correlation analyses with the dependent variables. Because of non-significant correlations with negative RS (p = .357) and positive RS (p = .887), we did not include parents’ talking time as a covariate in analyses of RS.
Results of MANOVA indicated that parents with a mental illness differed from parents without a mental illness regarding parents’ RS with a large effect size (V = 0.29, F(2, 186) = 38.50, p <.001; ηp2 = .293). Univariate ANOVAs revealed significant group differences on negative RS, F(1, 187) = 66.47, p <.001, and positive RS, F(1, 187) = 52.01, p <.001, with parents with a mental illness reporting more negative and less positive RS (for means and standard deviations, see Table 6).
We conducted partial correlation analyses of negative and positive RS, CBCLint and CBCLext with group as control-variable (see Table 5). We found significant correlations of CBCLext and CBCLint with parents’ RS. All significant correlation coefficients were in the expected direction with valence of RS associated with higher psychopathological symptoms and can be classified as low (103). Due to missing values of psychopathological symptoms in COPMI (n = 20, 22% missing), we examined if parents reporting higher psychopathological symptoms during the diagnostic interview were more likely to not complete the CBCL. For that, we conducted a t-test for independent samples with group (CBCL complete vs. missing) as independent and severity of primary diagnosis as dependent variable. Results indicated that groups do not differ in severity of psychopathological symptoms, t(89) = -.956, p = .342, ηp2 = 010.
Results of mixed ANOVA revealed a significant effect of phase, F(1, 178) = 24.50, p <.001, ηp2 = .121, indicating that fundamental frequency ranges differed between baseline period and FMSS, with higher fundamental frequency ranges during baseline period. Groups did not differ in fundamental frequency ranges, F(1, 178) = 1.66, p = .199, ηp2= .009, nor did we find an interaction effect between group and phase, F(1, 178) = 1.10, p = .297, ηp2 = .006. Since baseline-period was missing in n = 8 data sets, this analysis was conducted with a slightly reduced sample sizes. For means and standard deviations, see Table 7.
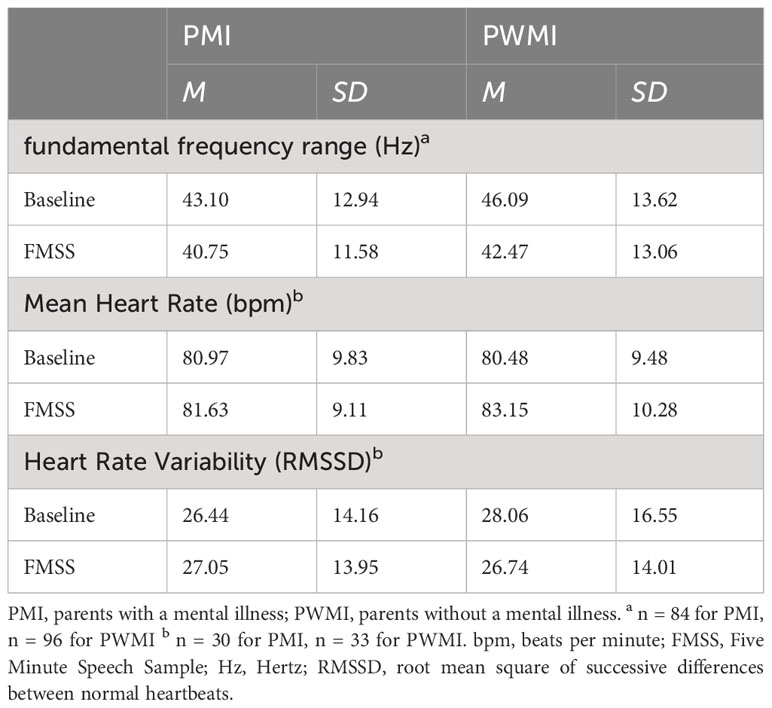
Table 7 Mean scores and standard deviations of parent’s fundamental frequency range, HR and HRV per phase.
Results of mixed MANOVA indicated a significant effect of phase with a large effect size, V = .25, F(2, 60) = 9.90, p <.001, ηp2= .248, but no significant effect of group, V = .00, F(2, 60) = .089, p = .915, ηp2 = .003. However, we found a significant interaction between group and phase with a moderate effect size, V = .10, F(2, 60) = 3.44, p = .039, ηp2 = .103.
Results of univariate ANOVA revealed a significant effect of phase in mean HR, F(1, 61) = 18.49, p <.001, ηp2 = .233, indicating that mean HR differed between baseline and FMSS, with a higher mean HR during FMSS. We found a significant interaction between group and phase, F(1, 61) = 6.66, p = .024, ηp2 = .098, indicating reduced reactivity in mean HR from baseline to FMSS in parents with a mental illness compared to parents without a mental illness (see Figure 1). For means and standard deviations, see Table 7.
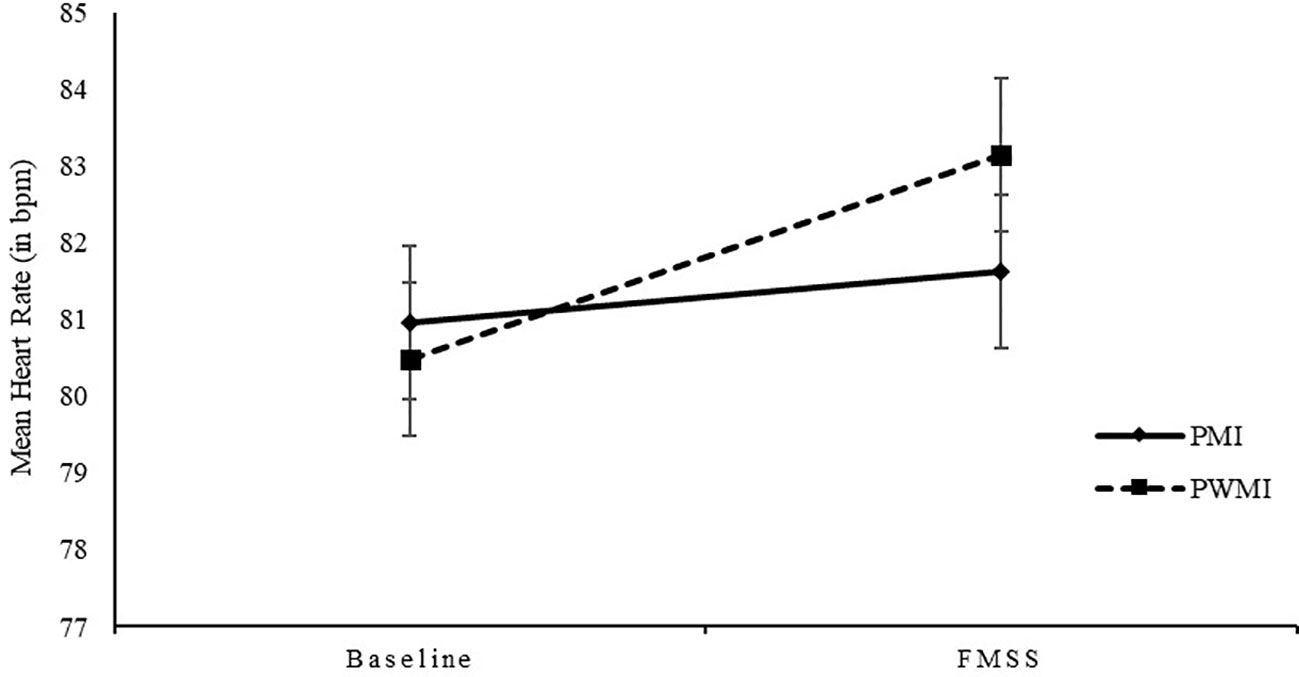
Figure 1 Mean heart rate (bpm) and standard deviations for parents with and without a mental illness at baseline and during FMSS. bpm, beats per minute; PMI, parents with a mental illness; PWMI, parents without a mental illness; FMSS, Five Minute Speech Sample.
Results of univariate ANOVA for HRV revealed no significant effect of phase, F(1, 61) = 0.34, p = .564, ηp2 = .005, no significant effect of group, F(1, 61) = 0.03, p = .858, ηp2 = .001, nor a significant interaction of group and phase, F(1, 61) = 2.48, p = .121, ηp2 = .039. For means and standard deviations, see Table 7.
We conducted partial correlation analyses of fundamental frequency range, mean HR and HRV, CBCLint and CBCLext with group as control-variable. We did not find any significant correlations of parent’s psychophysiological arousal and children’s psychopathological symptoms.
In this study, we investigated PS using multimodal data in parents with and without a mental illness. We expected parents with a mental illness to report higher levels of PS than parents without a mental illness. Since PS is considered a mechanism in TTMD, we aimed to examine how PS affects psychopathological symptoms in children. We expected self-reported PS to be positively correlated with children’s psychopathological symptoms regardless of a parental mental illness. Regarding the way parents think about their children, we expected parents with a mental illness to show more negative and less positive RS. We expected negative RS to be positively correlated with children’s psychopathological symptoms and positive RS to be negatively correlated with children’s psychopathological symptoms. Furthermore, we expected parents with a mental illness to show reduced reactivity from the baseline-period to FMSS in mean HR and HRV and higher fundamental frequency ranges during FMSS. Finally, we examined whether psychophysiological arousal in parents is correlated with psychopathological symptoms in children.
Our study is the first to compare PS using multimodal data in a sample of parents with and without a mental illness and investigating the relationship of PS with psychopathological symptoms of their children. Confirming our hypothesis, we found parents with a mental illness to report higher levels of PS than parents without a mental illness. This is in line with previous studies on parents with depression and anxiety symptoms (30, 33–35, 70–74, 88). Taking a closer look at the questionnaire’s scales, we found parents with a mental illness to perceive less social support and less support in parental relationship. This is in line with findings that suggest that parents with a mental illness report a below-average extent of social support (104). Additionally, over 50% of parents in this study reported a need for help, mostly with childcare. The extent of social support and need for help were moderated by sociodemographic differences (104). That is, in general, mothers report a higher extend of needed help compared to fathers, and unmarried patients report less social support than married ones (104). This could also be the case in our sample as 79% of the participants were female. Moreover, 15% of parents with a mental illness versus 4% of parents without a mental illness reported living without a partner. Besides, social support was found to increase parenting qualities in parents with a mental illness and therefore reducing the risk for TTMD in COPMI (for review see (105). According to Bowlby’s attachment theory (16), positive parenting provides the foundation for a secure attachment, which is linked to positive developmental outcomes in children. Thus, specific programs to increase social support in parents may be useful to support the use of positive parenting and to reduce the heightened risk for TTMD in COPMI. In line with our hypothesis, we found associations between PS and children’s psychopathological symptoms regardless of parents’ diagnostic status. This is in line with theories of PS (22) that PS has an influence on the development of children. Taking a closer look, we found significant associations between children’s externalizing psychopathological symptoms and PS as well as role restriction. Correlation coefficients were in the expected direction with higher psychopathological symptoms associated with higher PS and role restriction. This is in line with previous research finding PS to be related to externalizing problems in children (75, 76). However, we did not find any associations with children’s internalizing symptoms. Since we assessed age of children as a covariate, it could be that the relation between PS and children’s internalizing symptoms is more relevant for a particular age group. It is important to note that longitudinal studies suggest a bidirectional relation between children’s psychopathology and PS (13, 14), and that due to our cross-sectional study design, we cannot draw causal conclusions. Nevertheless, a longitudinal study found that children’s externalizing problems decreases if PS does (77). Thus, interventions for parents to reduce PS may indeed be useful to reduce psychopathology in children and the risk for TTMD.
Confirming our hypothesis, parents with a mental illness showed more negative and less positive RS than parents without a mental illness. This is in line with findings suggesting that parental psychopathological symptoms were positively associated with negative RS. Moreover, we found that parents with a mental illness showed less positive RS. A high extent of negative and a low extent of positive RS may discriminate between sub-clinical and clinically relevant psychopathological symptoms in parents, indicating this constellation as a potential risk factor for TTMD. Since means of self-reported PS in our sample were within the average range, differences in RS may not exclusively be due to heightened PS (39, 40). More likely, parents with a mental illness evaluated their children’s behavior in a more negative and less positive way due to their own psychopathology. This is in line with research suggesting that depressive symptoms in mothers lead to increased negative appraisals of their children (106), and a reduced threshold for tolerating aversive child behaviors (107). In line with our hypothesis, we found expected associations between RS and children’s psychopathological symptoms regardless of parents’ diagnostic status. This is consistent with previous findings on RS and psychopathological symptoms in children (49, 79, 80). In contrast to our study, the described studies examined clinically-referred child samples with externalizing behavior problems. We found that RS are associated with externalizing and internalizing symptoms as well although children’s psychopathology was within a normal range. In sum, our results support the idea that parental information processing can provide an explanation for how PS affects child outcomes. We need to mention again that the relation between children’s psychopathology and PS is bidirectional (13, 14), and that due to our cross-sectional study design, we cannot draw causal conclusions.
To our knowledge, this is the first study examining psychophysiological arousal in parents with a mental illness. We did not differences between parents with and without a mental illness during baseline assessments or the FMSS in fundamental frequency range, rejecting our hypothesis. This could be due to several reasons. First, bivariate correlation analysis showed no significant associations between HR, HRV and fundamental frequency range. This is contrary to findings that fundamental frequency is a valid indicator of arousal correlating strongly with established indicators of ANS (63, 64). However, we found a significant difference between the baseline-period and FMSS, with parents showing higher fundamental frequency ranges during the baseline-period. Thus, arousal in parents differed between phases indicating a physiological stress response. Second, previous studies examined fundamental frequency during conflict tasks between couples or parents and their children. We assessed fundamental frequency during free speech in which parents talk freely about their child for five minutes, without the child being present. It could be that the arousal provoked in this task was not strong enough to elicit potential differences. We were not able to find any associations between fundamental frequency and children’s psychopathology either. This could be due to the described methodological reasons. Nevertheless, future studies should examine fundamental frequency in parents with a mental illness considering our limitations. Partially confirming our hypothesis, we found an interaction effect between group and phase in mean HR, indicating reduced reactivity in parents with a mental illness. As an indication of a physiological stress response, we found significant differences in mean HR between baseline-period and FMSS, with parents showing higher mean HR during FMSS. This is in line with findings on high-risk parents showing reduced reactivity in response to a stress task (56, 57). Contrary to previous studies, we were not able to find differences in HR between parents with and without a mental illness during baseline and FMSS. Comparing the mean HR during baseline with previous studies (56, 57), we need to mention that parents’ mean HR in our study was quite high (M = 80.71, SD = 9.58). We asked parents to describe a hidden object picture resulting in higher arousal compared to baseline obtained by asking parents to sit quietly. Speculatively, this makes it harder to detect any group differences. We did not detect reduced reactivity on HRV in parents with a mental illness, either. This could be due to further methodological reasons. First, we assessed HRV during FMSS to provoke a stress response, which is in contrast to studies using established stress tasks, such as a cry paradigm (57). In fact, we were not able to find significant changes in parents’ HRV in the baseline-period compared to FMSS. Probably, by using FMSS we did not induce enough stress to detect any changes in HRV. Unfortunately, we did not assess subjective stress response via questionnaire. Second, in contrast to previous studies, parents in our study were talking during the assessment of HRV. On the one hand, breathing and physical activity can affect HRV (108). On the other hand, we used RMSSD for calculating HRV because it is less affected by respiration (92). Third, we had a reduced sample size regarding HR and HRV. Since HRV is an important index for emotion regulation (53), we cannot conclude that emotion regulation is reduced in parents with a mental illness on a psychophysiological level. We were not able to detect significant associations between parents’ psychophysiological arousal and children’s psychopathological symptoms rejecting our hypothesis. This could be due to described methodological issues. Thus, the role of parents’ psychophysiological arousal in how PS affects child outcomes and in the TTMD remains unclear and should further be investigated.
The main strength of this study is the assessment of PS by using multimodal data. In this way, we used parents’ self-report, parents’ RS and psychophysiological measures to extend previous literature that is limited to studies using mainly parental self-report to assess PS (69). Another strength is the sample of parents with a mental illness with clinically verified diagnosis. Preventing reporter bias, our study can contribute to objectivity in research on PS and psychopathology in parents. Further, this was the first study examining the relation between PS in parents with a mental illness and psychopathological symptoms in children allowing the conclusion that PS seems to be relevant for TTMD. The large sample size and the representativeness of our clinical sample should also be mentioned. Aside from these strengths, several limitations warrant consideration when interpreting the findings from the present study. One limitation is that parents reported their children’s psychopathology. On the one hand, parents could overestimate their children’s psychopathological symptoms due to their own psychopathology (106). On the other hand, psychopathology of children was within the normal range. Moreover, parent-report has been shown to be more valid for externalizing symptoms than child-report (100, 109). Future research should consider this by using teacher-report for instance. Another limitation is the paradigm we used for the assessment of psychophysiological arousal. The FMSS is an established paradigm to assess RS, but it is not known as a stress paradigm to assess psychophysiological arousal. Future research should consider this by using an established stress paradigm, such as conflict tasks with parents and their children. This would allow assessing psychophysiological arousal in children as well. A final limitation of the study is that the data is cross-sectional and therefore does not allow causal conclusions. Therefore, longitudinal studies are needed to investigate how PS affects child outcomes. With respect to the role of PS in TTMD, longitudinal studies are needed as well to identify PS as a risk factor for TTMD. Given the longitudinal design of the COMPARE-study, this will be explored in a further study.
Our findings suggest that parents with a mental illness perceive increased PS, especially a lower extent of social support and less support in parental relationships, and that they evaluate their children in a more negative and less positive manner than parents without a mental illness. Regarding psychophysiological arousal, parents with a mental illness show a reduced reactivity in stress response, indicating a less flexible response of SNS. Beyond that, our findings suggest that perceived PS and the way, parents talk about their children are associated with children’s psychophysiological symptoms regardless of parental diagnostic status. Therefore, our results support the idea that parents and children benefit from specific (preventive) intervention programs to reduce PS (30). In this context, parenting programs have shown to be effective in reducing PS (110). In addition, our results support the idea, that these programs should consider how parents evaluate their children’s behavior. Besides, our results have several implications for clinical practice with parents with a mental illness. First, they indicate that therapeutic professionals should focus on interventions to increase social support (also in parental relationship) in parents with a mental illness. Such support should probably be differentiated between the amount of social support and perceived social support leading to different implications for interventions increasing social support. Furthermore, our result support the idea to facilitate access to support services, for example parenting programs. Second, the parent-child-relationship should be considered in therapeutic contexts. Since RS play a critical role in how parents read their children’s behavior, reframing caregiver’s beliefs about their children may be an important tool to modulate RS. Third, parents with a mental illness may profit from strategies to reduce stress and to increase coping skills, such as relaxation or biofeedback trainings. In sum, parents with a mental illness benefit from intervention programs to reduce PS and thus the risk for TTMD in their children.
The datasets presented in this article are not readily available because of patient confidentiality and restrictions by law. Requests to access the datasets should be directed to Y2hyaXN0aW5hLnNjaHdlbmNrQHBzeWNob2wudW5pLWdpZXNzZW4uZGU=.
The studies involving humans were approved by ethics committee from Justus-Liebig-University Giessen, Philipps-University Marburg and Technical University Dortmund. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
VS: Data curation, Formal analysis, Investigation, Writing – original draft, Validation. KH: Investigation, Writing – review & editing. RuS: Funding acquisition, Project administration, Writing – review & editing. SW: Funding acquisition, Methodology, Project administration, Writing – review & editing. HC: Funding acquisition, Methodology, Project administration, Writing – review & editing. MK: Funding acquisition, Project administration, Writing – review & editing. KO: Funding acquisition, Project administration, Writing – review & editing. CR: Funding acquisition, Project administration, Writing – review & editing. RiS: Funding acquisition, Project administration, Writing – review & editing. LW: Funding acquisition, Project administration, Writing – review & editing. AZ: Funding acquisition, Project administration, Writing – review & editing. CS: Funding acquisition, Methodology, Project administration, Supervision, Writing – review & editing.
Study management: Stracke, Gilbert, Eitenmüller. Biometry and data management: Awounvo, Kirchner, Klose. Clinical study monitoring: Buntrock, Ebert. Recruiting center Bielefeld: Schlarb. Recruiting center Bochum: Margraf, Schneider, Friedrich, Teismann. Recruiting center Giessen: Stark, Metzger. Recruiting center Greifswald: Brakemeier, Wardenga, Hauck. Recruiting center Landau: Glombiewski, Schröder, Heider. Recruiting center Mainz: Jungmann, Witthöft. Recruiting center Marburg: Rief, Eitenmüller.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the Federal Ministry of Education and Research (BMBF) under grant # 01GL1748B, # 01GL1748C and # 01GL1748E.
We would like to thank all the families who participated in the COMPARE-study and its sub-project COMPARE-emotion.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Wiegand-Grefe S. Unterstützung für Kinder und Jugendliche mit psychisch erkrankten Eltern im “Children of mentally ill parents –network”. Psychotherapeut (2022) 67:34–41. doi: 10.1007/s00278-021-00565-8
2. Wiegand-Grefe S, Geers P, Plaß A, Petermann F, Riedesser P. Kinder psychisch kranker Eltern: Zusammenhänge zwischen subjektiver elterlicher Beeinträchtigung und psychischer Auffälligkeit der Kinder aus Elternsicht. Kindheit Und Entwicklung (2009) 18(2):111–21. doi: 10.1026/0942-5403.18.2.111
3. Radicke A, Barkmann C, Adema B, Daubmann A, Wegscheider K, Wiegand-Grefe S. Children of parents with a mental illness: predictors of health-related quality of life and determinants of child-parent agreement. Int J Environ Res Public Health (2021) 18(2):379. doi: 10.3390/ijerph18020379
4. Kersten-Alvarez LE, Hosman CMH, Riksen-Walraven JM, van Doesum KTM, Smeekens S, Hoefnagels C. Early school outcomes for children of postpartum depressed mothers: comparison with a community sample. Child Psychiatry Hum Dev (2012) 43(2):201–18. doi: 10.1007/s10578-011-0257-y
5. Christiansen H, Reck C, Zietlow A-L, Otto K, Steinmayr R, Wirthwein L, et al. Children of mentally III parents at risk evaluation (COMPARE): design and methods of a randomized controlled multicenter study-part I. Front Psychiatry (2019) 10:128. doi: 10.3389/fpsyt.2019.00128
6. Leijdesdorff S, van Doesum K, Popma A, Klaassen R, van Amelsvoort T. Prevalence of psychopathology in children of parents with mental illness and/or addiction: an up to date narrative review. Curr Opin Psychiatry (2017) 30(4):312–7. doi: 10.1097/YCO.0000000000000341
7. Wiegand-Grefe S, Sell M, Filter B, Plass-Christl A. Family functioning and psychological health of children with mentally ill parents. Int J Environ Res Public Health (2019) 16(7):1278. doi: 10.3390/ijerph16071278
8. Reupert AE, Maybery D J, Kowalenko NM. Children whose parents have a mental illness: prevalence, need and treatment. Med J Aust (2013) 199(3 Suppl):S7–9. doi: 10.5694/mja11.11200
9. Hosman CMH, van Doesum KTM, van Santvoort F. Prevention of emotional problems and psychiatric risks in children of parents with a mental illness in the Netherlands: I. The scientific basis to a comprehensive approach. Aust e-J Advancement Ment Health (2009) 8(3):250–63. doi: 10.5172/jamh.8.3.250
10. Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev (1999) 106(3):458–90. doi: 10.1037/0033-295X.106.3.458
11. Zahn-Waxler C, Duggal S, Gruber R, Bornstein MH. Parental psychopathology. Mahwah, NJ: Lawrence Erlbaum Associates (2002).
12. Villarreal DL, Smith OA, Nelson JA. Child behavior problems related to inconsistency and average negativity in mother–child conflict characteristics: the mediating role of parenting stress. J Child Fam Stud (2022) 31(7):1859–68. doi: 10.1007/s10826-021-02146-4
13. Baker BL, McIntyre LL, Blacher J, Crnic K, Edelbrock C, Low C. Pre-school children with and without developmental delay: behaviour problems and parenting stress over time. J Intellect Disabil Res (2003) 47(Pt 4-5):217–30. doi: 10.1046/j.1365-2788.2003.00484.x
14. Neece CL, Green SA, Baker BL. Parenting stress and child behavior problems: a transactional relationship across time. Am J Intellect Dev Disabil (2012) 117(1):48–66. doi: 10.1352/1944-7558-117.1.48
15. Orsmond GI, Seltzer MM, Krauss MW, Hong J. Behavior problems in adults with mental retardation and maternal well-being: examination of the direction of effects. Am J Ment Retard (2003) 108(4):257. doi: 10.1352/0895-8017(2003)108<257:BPIAWM>2.0.CO;2
16. Bowlby J. Attachment and loss. Volume II. In: Separation, anxiety and anger. New York, NY: Basic Books (1973) p. 429.
17. Hong YR, Park JS. Impact of attachment, temperament and parenting on human development. Korean J Pediatr (2012) 55(12):449–54. doi: 10.3345/kjp.2012.55.12.449
18. Sroufe LA. Attachment and development: A prospective, longitudinal study from birth to adulthood. Attachment Hum Dev (2005) 7(4):349–67. doi: 10.1080/14616730500365928
19. Feldman R. Mother-infant synchrony and the development of moral orientation in childhood and adolescence: direct and indirect mechanisms of developmental continuity. Am J Orthopsychiatry (2007) 77(4):582–97. doi: 10.1037/0002-9432.77.4.582
20. Leckman JF, Carter CS, Hennessy MB, Hrdy SB, Keverne EB, Klann-Delius G, et al. Group report: biobehavioral processes in attachment and bonding. In: Carter CS, Ahnert L, editors. Attachment and bonding: A new synthesis. Cambridge, MA, US: Boston Review (2005). p. 301–48.
21. Crnic KA, Greenberg MT. Minor parenting stresses with young children. Child Dev (1990) 61(5):1628. doi: 10.2307/1130770
22. Abidin RR. The determinants of parenting behavior. J Clin Child Psychol (1992) 21(4):407–12. doi: 10.1207/s15374424jccp2104_12
23. Deater-Deckard K. 1 Hello Baby, Hello Stress: Introduction and Overview. In: Parenting Stress. New Haven, Yale: University Press (2008) p. 1–26. doi: 10.12987/9780300133936-003
24. Guajardo NR, Snyder G, Petersen R. Relationships among parenting practices, parental stress, child behaviour, and children’s social-cognitive development. Infant Child Dev (2009) 18(1):37–60. doi: 10.1002/icd.578
26. Anthony LG, Anthony BJ, Glanville DN, Naiman DQ, Waanders C, Shaffer S. The relationships between parenting stress, parenting behaviour and preschoolers’ social competence and behaviour problems in the classroom. Inf Child Dev (2005) 14(2):133–54. doi: 10.1002/icd.385
27. Putnick DL, Bornstein MH, Hendricks C, Painter KM, Suwalsky JTD, Collins WA. Parenting stress, perceived parenting behaviors, and adolescent self-concept in European American families. J Fam Psychol (2008) 22(5):752–62. doi: 10.1037/a0013177
28. Prinzie P, Onghena P, Hellinckx W. Reexamining the parenting scale. Eur J psychol Assess (2007) 23(1):24–31. doi: 10.1027/1015-5759.23.1.24
29. Reitman D, Currier RO, Hupp SD, Rhode PC, Murphy MA, O’Callaghan PM. Psychometric characteristics of the Parenting Scale in a head start population. J Clin Child Psychol (2001) 30(4):514–24. doi: 10.1207/S15374424JCCP3004_08
30. Fang Y, Luo J, Boele M, Windhorst D, van Grieken A, Raat H. Parent, child, and situational factors associated with parenting stress: a systematic review. Eur Child Adolesc Psychiatry (2022). doi: 10.1007/s00787-022-02027-1
31. de Stasio S, Boldrini F, Ragni B, Gentile S. Predictive factors of toddlers’ Sleep and parental stress. Int J Environ Res Public Health (2020) 17(7):2494. doi: 10.3390/ijerph17072494
32. Barroso NE, Mendez L, Graziano PA, Bagner DM. Parenting stress through the lens of different clinical groups: a systematic review & Meta-analysis. J Abnorm Child Psychol (2018) 46(3):449–61. doi: 10.1007/s10802-017-0313-6
33. Gerdes AC, Hoza B, Arnold LE, Pelham WE, Swanson JM, Wigal T, et al. Maternal depressive symptomatology and parenting behavior: exploration of possible mediators. J Abnorm Child Psychol (2007) 35(5):705–14. doi: 10.1007/s10802-007-9134-3
34. Gray PH, Edwards DM, O’Callaghan MJ, Cuskelly M. Parenting stress in mothers of preterm infants during early infancy. Early Hum Dev (2012) 88(1):45–9. doi: 10.1016/j.earlhumdev.2011.06.014
35. Kötter C, Stemmler M, Bühler A, Lösel F. Mütterliche Depressivität, Erziehung und kindliche Erlebens- und Verhaltensprobleme. Kindheit Und Entwicklung (2010) 19(2):109–18. doi: 10.1026/0942-5403/a000006
36. Lazarus RS. From psychological stress to the emotions: A history of changing outlooks. Annu Rev Psychol (1993) 44(1):1–22. doi: 10.1146/annurev.ps.44.020193.000245
37. Porges SW. The polyvagal perspective. Biol Psychol (2007) 74(2):116–43. doi: 10.1016/j.biopsycho.2006.06.009
38. Niehaus CE, Chaplin TM, Turpyn CC, Gonçalves SF. Maternal emotional and physiological reactivity: implications for parenting and the parenting-adolescent relationship. J Child Fam Stud (2019) 28:812–83. doi: 10.1007/s10826-018-01318-z
39. Milner JS. Social information processing and physical child abuse. Clin Psychol Rev (1993) 13(3):275–94. doi: 10.1016/0272-7358(93)90024-G
40. Milner JS. Social information processing in high-risk and physically abusive parents. Child Abuse Negl (2003) 27(1):7–20. doi: 10.1016/S0145-2134(02)00506-9
41. Beckerman M, van Berkel SR, Mesman J, Alink LRA. The role of negative parental attributions in the associations between daily stressors, maltreatment history, and harsh and abusive discipline. Child Abuse Negl (2017) 64:109–16. doi: 10.1016/j.chiabu.2016.12.015
42. Crawford AM, Manassis K. Familial predictors of treatment outcome in childhood anxiety disorders. J Am Acad Child Adolesc Psychiatry (2001) 40(10):1182–9. doi: 10.1097/00004583-200110000-00012
43. Crnic KA, Gaze C, Hoffman C. Cumulative parenting stress across the preschool period: relations to maternal parenting and child behaviour at age 5. Inf Child Dev (2005) 14(2):117–32. doi: 10.1002/icd.384
44. Beckerman M, van Berkel SR, Mesman J, Huffmeijer R, Alink LRA. Are negative parental attributions predicted by situational stress?: from a theoretical assumption toward an experimental answer. Child Maltreat (2020) 25(3):352–62. doi: 10.1177/1077559519879760
45. Clément M-È, Chamberland C. The role of parental stress, mother’s childhood abuse and perceived consequences of violence in predicting attitudes and attribution in favor of corporal punishment. J Child Fam Stud (2009) 18(2):163–71. doi: 10.1007/s10826-008-9216-z
46. Mouton B, Weeland J, Leijten P, Overbeek G. When parents wear dark glasses: an experimental study on parental negative attributions and parenting behavior. J Child Fam Stud (2022) 31(12):3468–84. doi: 10.1007/s10826-022-02446-3
47. Fonagy P, Target M. Attachment and reflective function: Their role in self-organization. Dev Psychopathol (1997) 9(4):679–700. doi: 10.1017/S0954579497001399
48. Hayes SC, Barnes-Holmes D, Roche B. Relational frame theory: a post-Skinnerian account of human language and cognition. Adv Child Dev Behav (2001) 28:101–38. doi: 10.1007/b108413
49. Smith JD, Dishion TJ, Shaw DS, Wilson MN. Negative relational schemas predict the trajectory of coercive dynamics during early childhood. J Abnorm Child Psychol (2015) 43(4):693–703. doi: 10.1007/s10802-014-9936-z
50. Bullock BM, Dishion TJ. Family processes and adolescent problem behavior: integrating relationship narratives into understanding development and change. J Am Acad Child Adolesc Psychiatry (2007) 46(3):396–407. doi: 10.1097/chi.0b013e31802d0b27
51. Magaña AB, Goldstein JM, Karno M, Miklowitz DJ, Jenkins J, Falloon IR. A brief method for assessing expressed emotion in relatives of psychiatric patients. Psychiatry Res (1986) 17(3):203–12. doi: 10.1016/0165-1781(86)90049-1
52. Weston S, Hawes DJ, Pasalich D. The five minute speech sample as a measure of parent–child dynamics: evidence from observational research. J Child Fam Stud (2017) 26(1):118–36. doi: 10.1007/s10826-016-0549-8
53. Appelhans BM, Luecken LJ. Heart rate variability as an index of regulated emotional responding. Rev Gen Psychol (2006) 10(3):229–40. doi: 10.1037/1089-2680.10.3.229
54. Higgins GE, Kirchner EE, Ricketts ML, Marcum CD. Developing self-control: the role of parental stress. Criminal Justice Stud (2011) 24(2):183–98. doi: 10.1080/1478601X.2011.561647
55. Cavicchioli M, Tobia V, Ogliari A. Emotion regulation strategies as risk factors for developmental psychopathology: a meta-analytic review of longitudinal studies based on cross-lagged correlations and panel models. Res Child Adolesc Psychopathol (2023) 51(3):295–315. doi: 10.1007/s10802-022-00980-8
56. Crouch JL, Hiraoka R, McCanne TR, Reo G, Wagner MF, Krauss A, et al. Heart rate and heart rate variability in parents at risk for child physical abuse. J Interpers Violence (2018) 33(10):1629–52. doi: 10.1177/0886260515619169
57. Joosen KJ, Mesman J, Bakermans-Kranenburg MJ, Pieper S, Zeskind PS, van IJzendoorn MH. Physiological reactivity to infant crying and observed maternal sensitivity. Infancy (2013) 18(3):414–31. doi: 10.1111/j.1532-7078.2012.00122.x
58. Lorber MF, O’leary SG. Mediated paths to over-reactive discipline: mothers’ experienced emotion, appraisals, and physiological responses. J Consult Clin Psychol (2005) 73(5):972–81. doi: 10.1037/0022-006X.73.5.972
59. Manczak EM, McLean KC, McAdams DP, Chen E. Physiological reactivity during parent-adolescent discussions: associations with scaffolding behaviors and relationship quality. Ann Behav Med (2015) 49(4):522–31. doi: 10.1007/s12160-014-9680-1
60. Zhang X, Cui L, Han ZR, Yan J. The heart of parenting: Parent HR dynamics and negative parenting while resolving conflict with child. J Fam Psychol (2017) 31(2):129–38. doi: 10.1037/fam0000285
61. Bulling LJ, Bertschi IC, Stadelmann CC, Niederer T, Bodenmann G. Messung der Stimmfrequenz im Paargespräch – Chancen für Diagnostik und Intervention in der Paartherapie. Z Für Psychiatrie Psychol Und Psychother (2020) 68(4):217–27. doi: 10.1024/1661-4747/a000420
62. Juslin PN, Scherer KR. Vocal expression of affect. In: Harrigan JA, Scherer KR, Rosenthal R, editors. The new handbook of methods in nonverbal behavior research. New York, NY, US: Oxford University Press (2005). p. 65–135. Series in Affective Science.
63. Baucom BR, Saxbe DE, Ramos MC, Spies LA, Iturralde E, Duman S, et al. Correlates and characteristics of adolescents’ encoded emotional arousal during family conflict. Emotion (2012) 12(6):1281–91. doi: 10.1037/a0028872
64. Weusthoff S, Baucom BR, Hahlweg K. Fundamental frequency during couple conflict: an analysis of physiological, behavioral, and sex-linked information encoded in vocal expression. J Fam Psychol (2013) 27(2):212–20. doi: 10.1037/a0031887
65. Baucom BR, Atkins DC, Simpson LE, Christensen A. Prediction of response to treatment in a randomized clinical trial of couple therapy: a 2-year follow-up. J Consult Clin Psychol (2009) 77(1):160–73. doi: 10.1037/a0014405
66. Kliem S, Weusthoff S, Hahlweg K, Baucom KJW, Baucom BR. Predicting long-term risk for relationship dissolution using nonparametric conditional survival trees. J Fam Psychol (2015) 29(6):807–17. doi: 10.1037/fam0000134
67. Webster-Stratton C. Stress: A potential disruptor of parent perceptions and family interactions. J Clin Child Psychol (1990) 19(4):302–12. doi: 10.1207/s15374424jccp1904_2
68. Christiansen H. Kinder von Eltern mit psychischen Erkrankungen: State of the Art für Psychotherapeutinnen, Pädiaterinnen, Pädagoginnen. Wiesbaden: Springer, Springer Fachmedien Wiesbaden (2020). Essentials (Springer).
69. Deater-Deckard K. Parenting stress and child adjustment: Some old hypotheses and new questions. Clin Psychol: Sci Pract (1998) 5(3):314–32. doi: 10.1111/j.1468-2850.1998.tb00152.x
70. Fredriksen E, von Soest T, Smith L, Moe V. Parenting stress plays a mediating role in the prediction of early child development from both parents’ Perinatal depressive symptoms. J Abnorm Child Psychol (2019) 47(1):149–64. doi: 10.1007/s10802-018-0428-4
71. Prino LE, Rollè L, Sechi C, Patteri L, Ambrosoli A, Caldarera AM, et al. Parental relationship with twins from pregnancy to 3 months: the relation among parenting stress, infant temperament, and well-being. Front Psychol (2016) 7:1628. doi: 10.3389/fpsyg.2016.01628
72. Rollè L, Prino LE, Sechi C, Vismara L, Neri E, Polizzi C, et al. Parenting stress, mental health, dyadic adjustment: A structural equation model. Front Psychol (2017) 8:839. doi: 10.3389/fpsyg.2017.00839
73. Reck C, Zietlow A-L, Müller M, Dubber S. Perceived parenting stress in the course of postpartum depression: the buffering effect of maternal bonding. Arch Womens Ment Health (2016) 19(3):473–82. doi: 10.1007/s00737-015-0590-4
74. Stracke M, Heinzl M, Müller AD, Gilbert K, Thorup AAE, Paul JL, et al. Mental health is a family affair-systematic review and meta-analysis on the associations between mental health problems in parents and children during the COVID-19 pandemic. Int J Environ Res Public Health (2023) 20(5):4485. doi: 10.3390/ijerph20054485
75. Lohaus A, Chodura S, Möller C, Symanzik T, Ehrenberg D, Job A-K, et al. Children’s mental health problems and their relation to parental stress in foster mothers and fathers. Child Adolesc Psychiatry Ment Health (2017) 11:43. doi: 10.1186/s13034-017-0180-5
76. Sher-Censor E, Shulman C, Cohen E. Associations among mothers’ representations of their relationship with their toddlers, maternal parenting stress, and toddlers’ internalizing and externalizing behaviors. Infant Behav Dev (2018) 50:132–9. doi: 10.1016/j.infbeh.2017.12.005
77. Keyser D, Ahn H, Unick J. Predictors of behavioral problems in young children 3 to 9 years old: The role of maternal and child factors. Children Youth Serv Rev (2017) 82:149–55. doi: 10.1016/j.childyouth.2017.09.018
78. Biondic D, Wiener J, Martinussen R. Parental psychopathology and parenting stress in parents of adolescents with attention-deficit hyperactivity disorder. J Child Fam Stud (2019) 28(8):2107–19. doi: 10.1007/s10826-019-01430-8
79. Pasalich DS, Dadds MR, Hawes DJ, Brennan J. Assessing relational schemas in parents of children with externalizing behavior disorders: reliability and validity of the Family Affective Attitude Rating Scale. Psychiatry Res (2011) 185(3):438–43. doi: 10.1016/j.psychres.2010.07.034
80. Waller R, Gardner F, Viding E, Shaw DS, Dishion TJ, Wilson MN, et al. Bidirectional associations between parental warmth, callous unemotional behavior, and behavior problems in high-risk preschoolers. J Abnorm Child Psychol (2014) 42(8):1275–85. doi: 10.1007/s10802-014-9871-z
81. Le Y, Fredman SJ, Feinberg ME. Parenting stress mediates the association between negative affectivity and harsh parenting: A longitudinal dyadic analysis. J Fam Psychol (2017) 31(6):679–88. doi: 10.1037/fam0000315
82. Jones JH, Call TA, Wolford SN, McWey LM. Parental stress and child outcomes: the mediating role of family conflict. J Child Fam Stud (2021) 30(3):746–56. doi: 10.1007/s10826-021-01904-8
83. Stracke M, Gilbert K, Kieser M, Klose C, Krisam J, Ebert DD, et al. COMPARE family (Children of mentally ill parents at risk evaluation): A study protocol for a preventive intervention for children of mentally ill parents (Triple P, evidence-based program that enhances parentings skills, in addition to gold-standard CBT with the mentally ill parent) in a multicenter RCT-part II. Front Psychiatry (2019) 10:54. doi: 10.3389/fpsyt.2019.00054
84. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Fifth. Arlington: American Psychiatric Association (2013).
85. Derogatis Leonard R, Brähler E, Kliem S. BSI® - Brief Symptom Inventory (Kurzform der Symptom-Checkliste-90-R): Manual. 1. Auflage. Frankfurt am Main, Germany: Pearson Deutschlang GmbH (2017).
86. Lampert T, Hoebel J, Kuntz B, Muters S, Kroll LE. Messung des sozioökonomischen Status und des subjektiven sozialen Status in KiGGS Welle 2. (2018). doi: 10.17886/RKI-GBE-2018-016
87. Bullock B, Schneiger A, Dishion T. Manual for Coding Five-Minute Speech Samples Using the Family Affective Attitude Rating Scale (FAARS). Bullock B, editor. 195 W. 12th Ave., Eugene, OR 97401: Child and Family Center (2005).
88. Owren MJ, Bacharowski J. Measuring emotion-related vocal acoustins. In: Handbook of emotion elicitation and assessment. New York, NY, US: Oxford University Press (2007).
89. Boersma P, Weenink D. Praat: doing phonetics by computer. Version Version 6.2.22. Amsterdam: University of Amsterdam (2021).
90. MP systems hardware guide. (2021). Available at: https://www.biopac.com/manual/mp-hardware-guide/.
91. Hill L, Siebenbrock A. Are all measures created equal? Heart rate variability and respiration. Biomed Sci Instrumentation (2009) 45:71–6.
92. Shaffer F, Ginsberg JP. An overview of heart rate variability metrics and norms. Front Public Health (2017) 5:258. doi: 10.3389/fpubh.2017.00258
93. Domsch H, Lohaus A. Elternstressfragebogen (ESF). Göttingen: Hogrefe (2010). Available at: https://www.testzentrale.de/shop/elternstressfragebogen.html.
94. Achenbach TM, Rescorla L. A. Manual for the ASEBA preschool forms and profiles. University of Vermont, Research Center for Children, Youth, & Families. (2000).
95. Döpfner M, Plück J, Kinnen, Achenbach C, Thomas M. Deutsche Schulalter-Formen der Child Behavior Checklist von Thomas M. AchenbachCBCL 6-18R, TRF 6-18R, YSR 11-18R; Elternfragebogen über das Verhalten von Kindern u. Jugendlichen (CBCL/6-18R), Lehrerfragebogen über das Verhalten von Kindern u. Jugendlichen (TRF/6-18R), Fragebogen für Jugendliche (YRS/11-18R). Göttingen: Hogrefe (2014). Available at: http://slubdd.de/katalog?TN_libero_mab2.
96. Margraf J, Cwik JC, Suppiger A, Schneider S. DIPS Open Access: Diagnostisches Interview bei psychischen Störungen. (2017). doi: 10.13154/rub.100.89
97. Margraf J, Cwik JC, Pflug V, Schneider S. Strukturierte klinische Interviews zur Erfassung psychischer Störungen über die Lebensspanne. Z Für Klin Psychol Und Psychother (2017) 46(3):176–86. doi: 10.1026/1616-3443/a000430
98. Schneider S, Pflug V, Margraf J, In-Albon T. Kinder-DIPS: Diagnostisches Interview bei psychischen Störungen im Kindes- und Jugendalter. (2017). doi: 10.13154/rub.101.90
99. In-Albon T, Equit M, von Gontard A, Schwarz D, Müller JM, Bolten M. Das Strukturierte Interview für das Vorschulalter (SIVA: 0 – 6). Kindheit Und Entwicklung (2020) 29(4):209–20. doi: 10.1026/0942-5403/a000319
100. Neuschwander M, In-Albon T, Adornetto C, Roth B, Schneider S. Interrater-Reliabilität des Diagnostischen Interviews bei psychischen Störungen im Kindes- und Jugendalter (Kinder-DIPS). Z Kinder Jugendpsychiatr Psychother (2013) 41(5):319–34. doi: 10.1024/1422-4917//a000247
101. Lange M, Kamtsiuris P, Lange C, Schaffrath Rosario A, Stolzenberg H, Lampert T. Messung soziodemographischer Merkmale im Kinder- und Jugendgesundheitssurvey (KiGGS) und ihre Bedeutung am Beispiel der Einschätzung des allgemeinen Gesundheitszustands. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz (2007) 50(5):578–89. doi: 10.1007/s00103-007-0219-5
103. Cohen J. Statistical power analysis for the behavioral sciences. 2nd. Hillsdale, N.J: L. Erlbaum Associates (1988).
104. Höller I, Forkmann T, Hündlings A, Specka M, Scherbaum N. Hilfsbedarf und soziale Unterstützung bei psychisch erkrankten Elternteilen mit minderjährigen Kindern. Psychiatr Prax (2023) 50(1):20–8. doi: 10.1055/a-1704-6391
105. Seeger FR, Neukel C, Williams K, Wenigmann M, Fleck L, Georg AK, et al. Parental mental illness, borderline personality disorder, and parenting behavior: the moderating role of social support. Curr Psychiatry Rep (2022) 24(11):591–601. doi: 10.1007/s11920-022-01367-8
106. Dix T, Meunier LN. Depressive symptoms and parenting competence: An analysis of 13 regulatory processes. Dev Rev (2009) 29(1):45–68. doi: 10.1016/j.dr.2008.11.002
107. Dix T, Moed A, Anderson ER. Mothers’ depressive symptoms predict both increased and reduced negative reactivity: aversion sensitivity and the regulation of emotion. Psychol Sci (2014) 25(7):1353–61. doi: 10.1177/0956797614531025
108. Laborde S, Mosley E, Thayer JF. Heart rate variability and cardiac vagal tone in psychophysiological research - recommendations for experiment planning, data analysis, and data reporting. Front Psychol (2017) 8:213. doi: 10.3389/fpsyg.2017.00213
109. Adornetto C, In-Albon T, Schneider S. Diagnostik im Kindes- und Jugendalteranhand strukturierter Interviews: Anwendung und Durchfuhrung des Kinder-DIPS. Klin Diagnostik Und Eval (2008) 1(4):363–77.
110. Schrott B, Kasperzack D, Weber L, Becker K, Burghardt R, Kamp-Becker I. Effectiveness of the stepping stones triple P group parenting program as an additional intervention in the treatment of autism spectrum disorders: effects on parenting variables. J Autism Dev Disord (2019) 49(3):913–23. doi: 10.1007/s10803-018-3764-x
Keywords: parents with a mental illness, parenting stress, multimodal, relational schema, psychopathology of children, psychophysiological arousal, fundamental frequency, heart rate
Citation: Seipp V, Hagelweide K, Stark R, Weigelt S, Christiansen H, Kieser M, Otto K, Reck C, Steinmayr R, Wirthwein L, Zietlow A–L, Schwenck C and the COMPARE-Family Research Group (2024) Parenting stress in parents with and without a mental illness and its relationship to psychopathology in children: a multimodal examination. Front. Psychiatry 15:1353088. doi: 10.3389/fpsyt.2024.1353088
Received: 09 December 2023; Accepted: 18 January 2024;
Published: 05 February 2024.
Edited by:
Geneviève Piché, University of Quebec in Outaouais, CanadaReviewed by:
André Luiz Monezi Andrade, Pontifical Catholic University of Campinas, BrazilCopyright © 2024 Seipp, Hagelweide, Stark, Weigelt, Christiansen, Kieser, Otto, Reck, Steinmayr, Wirthwein, Zietlow, Schwenck and the COMPARE-Family Research Group. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vanessa Seipp, dmFuZXNzYS5zZWlwcEBwc3ljaG9sLnVuaS1naWVzc2VuLmRl
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.