
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry , 13 February 2024
Sec. Addictive Disorders
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1347678
This article is part of the Research Topic Community Series in Novel Treatment Approaches and Future Directions in Substance Use Disorders, Volume II View all 5 articles
 Vivian W. L. Tsang1*
Vivian W. L. Tsang1* James S.H. Wong1,2
James S.H. Wong1,2 Jean N. Westenberg1
Jean N. Westenberg1 Noor H. Ramadhan1
Noor H. Ramadhan1 Hasti Fadakar1
Hasti Fadakar1 Mohammadali Nikoo1,2
Mohammadali Nikoo1,2 Victor W. Li1,2
Victor W. Li1,2 Nick Mathew1,3
Nick Mathew1,3 Pouya Azar1,2
Pouya Azar1,2 Kerry L. Jang1
Kerry L. Jang1 Reinhard M. Krausz1
Reinhard M. Krausz1Objectives: Fentanyl is a highly potent opioid and has, until recently, been considered an unwanted contaminant in the street drug supply among people who use drugs (PWUD). However, it has become a drug of choice for an increasing number of individuals. This systematic review evaluated intentional non-medical fentanyl use among PWUD, specifically by summarizing demographic variance, reasons for use, and resulting patterns of use.
Methods: The search strategy was developed with a combination of free text keywords and MeSH and non-MeSH keywords, and adapted with database-specific filters to Ovid MEDLINE, Embase, Web of Science, and PsychINFO. Studies included were human studies with intentional use of non-medical fentanyl or analogues in individuals older than 13. Only peer-reviewed original articles available in English were included.
Results: The search resulted in 4437 studies after de-duplication, of which 132 were selected for full-text review. Out of 41 papers included, it was found that individuals who use fentanyl intentionally were more likely to be young, male, and White. They were also more likely to have experienced overdoses, and report injection drug use. There is evidence that fentanyl seeking behaviours are motivated by greater potency, delay of withdrawal, lower cost, and greater availability.
Conclusions: Among PWUD, individuals who intentionally use fentanyl have severe substance use patterns, precarious living situations, and extensive overdose history. In response to the increasing number of individuals who use fentanyl, alternative treatment approaches need to be developed for more effective management of withdrawal and opioid use disorder.
Systematic review registration: https://www.crd.york.ac.uk/prospero/, identifier CRD42021272111.
Fentanyl and its analogues such as alfentanil, sufentanil and remifentanil were first introduced into clinical practice (carfentanil in veterinary medicine) as μ-opioid receptor agonists and potent relatively short-acting analgesic agents. Fentanyl is between 50-fold and 100-fold more potent than morphine, thereby offering greater ability to manage intractable pain, breakthrough cancer pain and to produce balanced intravenous (IV) anaesthesia (1). The unique pharmacological properties of fentanyl and its widespread prevalence in the current North American drug market have contributed to alarming rates of fentanyl-related overdose deaths (2).
The use of non-medical fentanyl and its analogues has changed drastically over the last ten years. (3) In the 2000s and the early years of non-medical fentanyl use, fentanyl was diverted from clinical settings, mostly in the form of transdermal patches. Fentanyl patches were “cooked into fentanyl tea” and the fluid was injected intravenously along with extracted fentanyl. (4) This was a rare occurrence, and the practice was only found in parts of Europe (e.g., in Germany). A decade later, fentanyl made its way into the street drug market. Due to its synthetic quality, high availability, and lower cost, fentanyl was commonly mixed into other desired substances to offset the cost for producers and sellers. (3) Originally a contaminant, fentanyl has now become increasingly present in street opioids, stimulants and hallucinogens. (5) Over time, people who use drugs (PWUD) have also become increasingly accustomed to fentanyl added to other illicit substances. Based on legally available precursors, fentanyl has also increasingly been produced in local private laboratories. (3) Combined with a lower cost of production, increased availability in the illicit drug market, and the rapid, intense onset of effect, these attributes have altered fentanyl’s identity from an unwanted contaminant to a desirable drug of choice. (2) However, the demographic characteristics and comorbidities common to individuals who prefer fentanyl to other substances and use it intentionally as their drug of choice are unknown in the current literature. Intentional fentanyl use has been defined in this review as seeking fentanyl in the illicit drug market or using substances that are known to contain fentanyl; in other words, having fentanyl as one’s drug of choice, seeking out fentanyl, and not using fentanyl by accident. The details around patterns of use and motivation to use are also currently unknown.
This systematic review aimed to evaluate the evidence on intentional fentanyl use among PWUD by summarizing demographic variance, reasons for use, and resulting patterns of use to inform the development of effective interventional approaches and settings and identify critical research questions.
The Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines were used to ensure the details in the methodology is comprehensive (6). A protocol for this review has been registered with PROSPERO (registration number: CRD42021272111) (7). Research ethics board review was not required as this study relies exclusively on publicly available information that is legally accessible to the public.
The search strategy in this study was developed with a combination of free text keywords and MeSH and non-MeSH keywords. Search items were adapted with database-specific filters. Four different databases: Ovid MEDLINE (1860-May 2021); Embase (1952-May 2021); Web of Science (1900-May 2021); and PsychINFO (1900-May 2021). The search strategies for Ovid MEDLINE, Embase, Web of Science, and PsychINFO are provided in the supplemental material (Supplementary Tables S1A-D). References of all included papers were hand-mined, and any additional documents were added from gray literature such as from thesis dissertations and Google Scholar. The last search was completed on May 29, 2021.
Studies were included if they reported data on the intentional use of non-medical fentanyl or any fentanyl analogues in PWUD older than 13. The term PWUD refers to those who use illicit drugs or use prescription drugs non-medically. Papers from all regions of the world were considered as long as they were written or were available in the English language. Only peer-reviewed original articles were included, including case reports/series. Letters, reviews, meta-analyses, toxicology or coroner’s reports, commentaries, and editorials were excluded. Studies that included non-human participants, did not mention explicit intentional fentanyl use, or only discussed medical indications for fentanyl were excluded. Control or other comparison groups were not relevant to this study and the outcome of interest was intentional fentanyl use.
The PRISMA flow diagram was used to review selected articles in sequential fashion (Figure 1). Titles and abstracts of studies retrieved using the search strategy were screened by at least two of five reviewers (VWLT, JSHW, JNW, HF, NR). Any inconsistencies were reviewed by a third reviewer (VWLT or JSHW). The inclusion and exclusion criteria were strictly adhered and all articles were independently screened to minimize bias. Full text documents were independently assessed by at least two of five reviewers (VWLT, JSHW, JNW, HF, NR) for inclusion and any disagreements were resolved by consensus. A standardized table with predetermined categories was used for independent data extraction by at least two reviewers. Data on patient demographics, study setting, study methods, motivations for drug use, patterns of use, and associated attributes or behaviours of participants were collected.
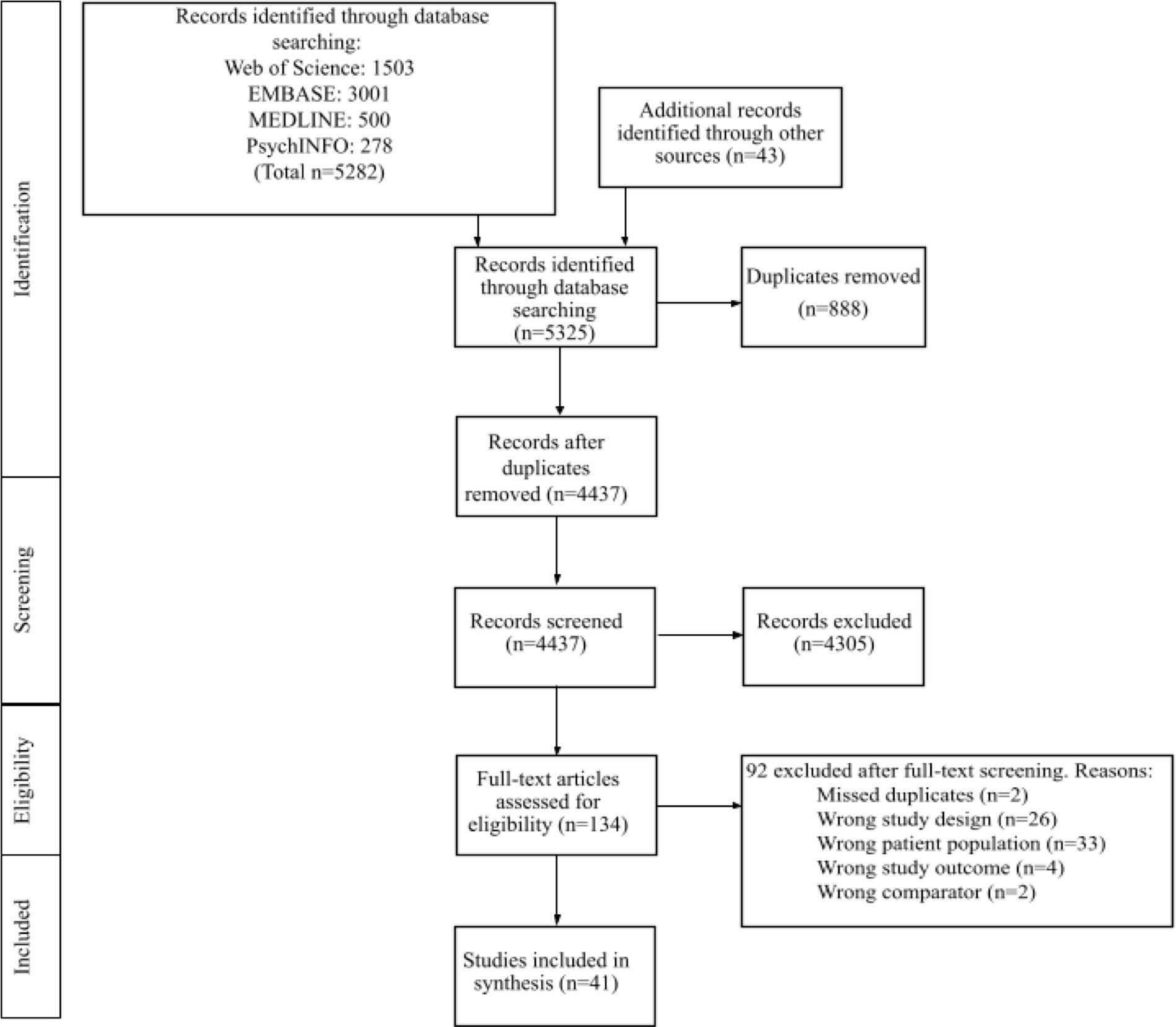
Figure 1 Flow of literature search. (MEDLINE, Medical Literature Analysis and Retrieval System Online; EMBASE, Excerpta Medica database) Legend. Wrong comparator: original study had not included a group or population with intentional fentanyl use for comparison or analysis within the study text.
Quality synthesis and evaluation of bias for article inclusion was completed in alignment with
the Newcastle-Ottawa Quality Assessment scale for cohort and case-controlled studies (8). Cross-sectional studies were evaluated with the modified Newcastle-Ottawa Quality Assessment scale for comparable results (9). Qualitative studies were appraised with the Critical Appraisal Skills Program (CASP) checklist (10). For case studies and series, we noted the following criteria for assessing methodological quality: timeline of recruitment, prospective or retrospective recruitment. Meta-analyses and reviews were not included in this study and there were no randomized controlled trials found.
Any inconsistencies were brought up to VWLT for review and final decision. The approach for analysis was conducted by separation of studies into three categories: studies discussing intentional fentanyl use with other substance use but where data were not distinguishable, studies with intentional fentanyl use only, and studies comparing intentional fentanyl using cohorts with non-intentional fentanyl using cohorts. This was conducted by three reviewers (NR, JSHW, JNW) with a second reviewer for each grouped analysis. Details of interest captured for each category of studies include demographic descriptors such as mean age, gender distribution, racial background, and socioeconomic status. Other relevant details captured include years of substance use, substance use patterns, overdose history, motivation for substance use, and usage patterns. In order to calculate pooled means for age, we estimated means from studies which only reported medians by using Luo et al., 2018’s model (11, 12).
The search resulted in 4437 studies after de-duplication, 132 were selected for full-text review, and 41 were included (Figure 1). Of the 41 studies included, 23 were in the United States (13–35); seven in Canada; (36–42) two in Sweden; (43, 44) one each in Australia, (45) Germany, (46) Denmark, (47) France, (48) Estonia, (49) the UK, (50) and Turkey. (51) Two studies were done online with no note of specific country involvement (Table 1) (52, 53). A mean of 62·63% of participants were male and 64·05% were White. The mean of average age was 41·36 (SD=10·86).
Outcomes were analyzed in three groups. Nineteen studies discussed intentional fentanyl use with other substance use where data were not distinguishable (Table 2), 13 studies discussed intentional fentanyl use only (Table 3), and 9 studies compared intentional fentanyl using cohorts with non-intentional fentanyl using cohorts (Table 4). It should be noted that there was little data to extract from studies examining intentional fentanyl use only, as 11 of the 13 studies were case reports/series. Moreover, of the 11 case reports/series, 3 were post-mortem analyses, all of which reported illicit intentional use of fentanyl. (34, 42, 43) More comprehensive details are available as online supplements (Supplementary Tables S2–S4).
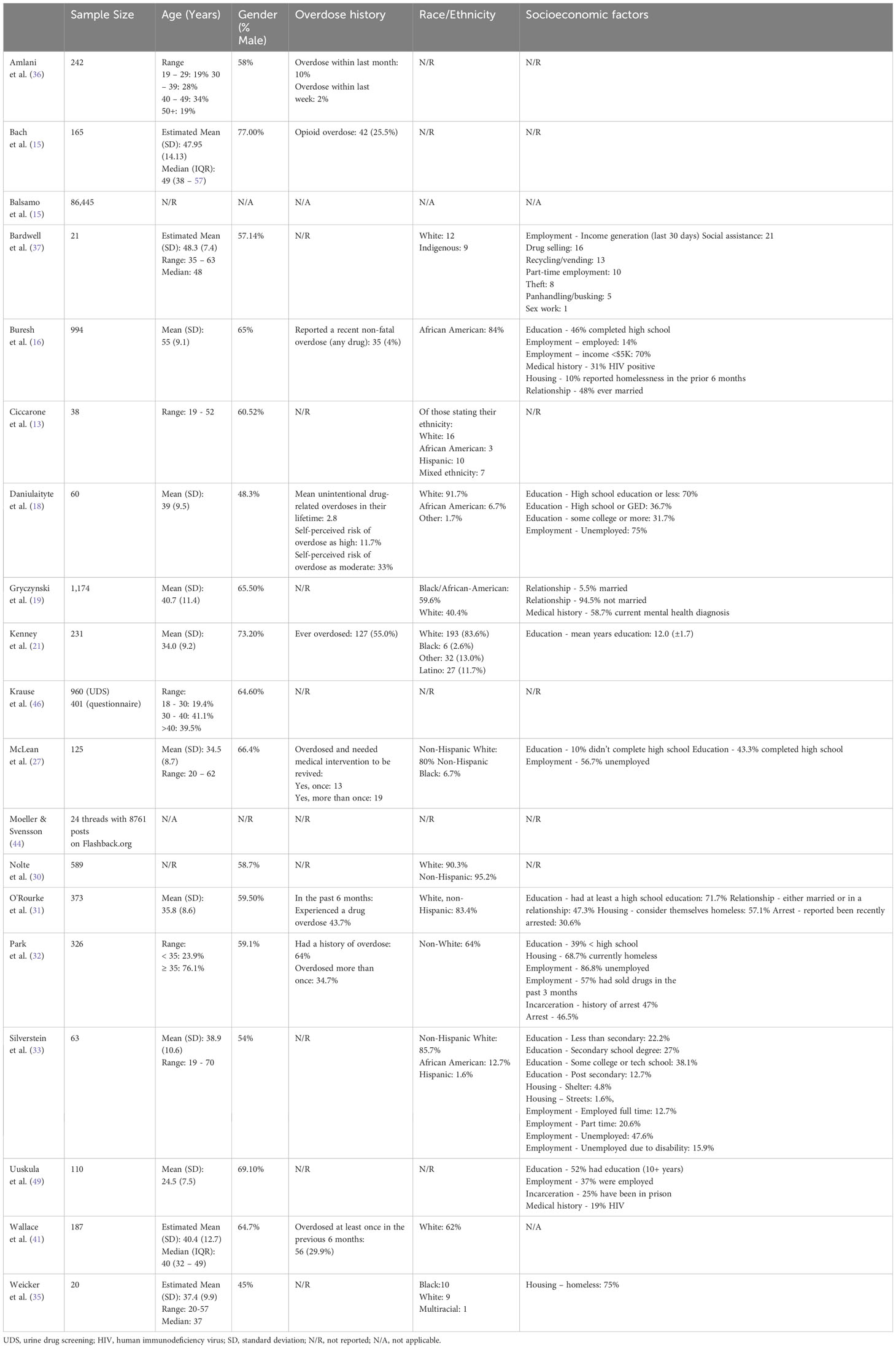
Table 2 Comprehensive description of studies involving intentional fentanyl use that is undistinguishable from other substance use (N=19).
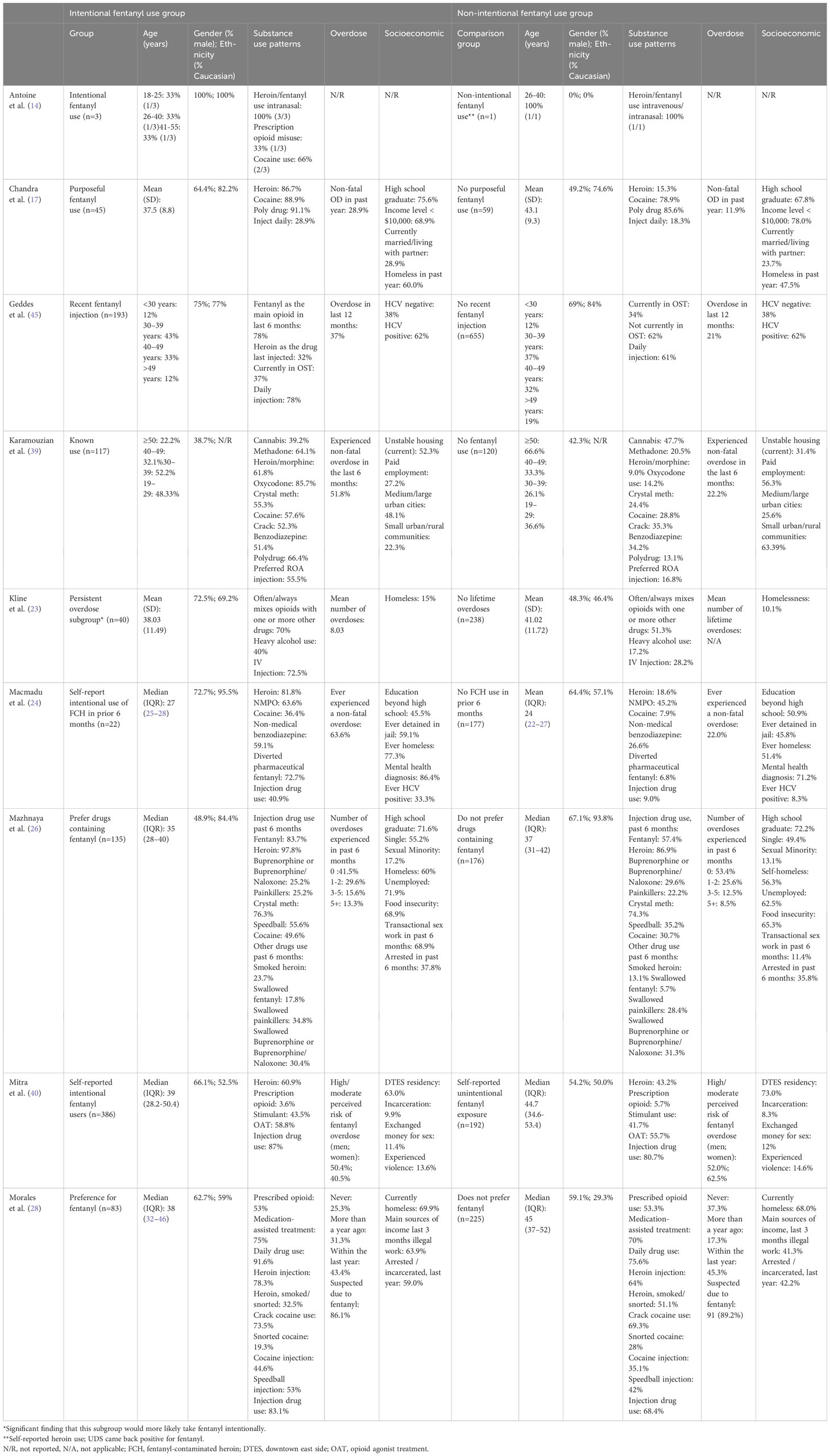
Table 4 Comprehensive description of the intentional fentanyl using subpopulations among studies comparing intentional fentanyl and non-intentional fentanyl use (N=9).
Regarding age among studies comparing intentional fentanyl using cohorts with non-intentional fentanyl using cohorts, participants were a pooled mean of 37·65 years (SD=13·77) in the intentional fentanyl-using cohort compared to 38·89 years (SD=10·53) in the non-intentional fentanyl-using cohort. This compared with 32·32 years (SD=9·73) in studies examining intentional fentanyl use only, and 43·34 years (SD=10·34) in studies examining intentional fentanyl use with other substance use.
Regarding gender distribution, studies comparing the two groups reported a mean of 62·52% male participants in the intentional fentanyl-using cohort and 60·54% in the non-intentional fentanyl-using cohort. This compares with 58·93% in studies on intentional fentanyl use only and 63·64% in studies on fentanyl with other substance use. Only one study comparing the two groups directly reported non-binary or gender non-conforming prevalence, which was 37·5% in both the fentanyl using cohort and non-intentional fentanyl using cohort (39). There were no mentions of non-binary or gender nonconformity in the fentanyl use only studies, and one study in the studies on fentanyl with other substance use (31).
Among studies comparing intentional fentanyl using cohorts with non-intentional fentanyl substance using cohorts, individuals who intentionally use fentanyl were more likely to be male and young (17, 23, 28, 40). In Krause et al., 2017, it was reported that a significant difference was found between younger age and fentanyl consumption (p=0·003) (46). In contrast, self-reported unintentional exposure to fentanyl was positively associated with women and older age (40, 49).
Elaborating on racial differences, studies comparing the two cohorts reported a pooled mean of 66·47% participants who were White in the intentional fentanyl cohort and 65·74% participants who were White in the non-intentional fentanyl cohort. This compared with a pooled percentage of 72·43% in studies with intentional fentanyl use only and 62·12% in studies on fentanyl with other substance use. In a study from Baltimore, Boston, and Providence, fentanyl preference was associated with non-Hispanic white race among PWUD (N=308) (32). Similarly, from a case-series that describes buprenorphine/naloxone inductions of four individuals who tested positive for fentanyl, three intentional-using individuals were male and White, while the unintentionally-using individual was female and non-White (14). One study further showed that African American respondents were less likely to report having ever used fentanyl (16). Only one study reported the opposite - that participants preferring drugs containing fentanyl were less likely to be White and non-Hispanic (26).
Among the three groups of studies, each group reported at least one study with either unemployment or educational attainment as a socioeconomic factor. Unemployment was considered as a socioeconomic factor in seven out of 19 studies where intentional fentanyl use and other substance use was not distinguishable (Table 2) (16, 18, 27, 32, 33, 37, 49). The only studies of the 13 that reported on intentional fentanyl use only was a case report that included unemployment as a socioeconomic factor (Table 3) (51). Three of nine studies comparing intentional fentanyl and non-intentional fentanyl using cohorts reported unemployment or illegal work as main source of income as being more common with the intentional fentanyl using group (Table 4) (26, 28, 39).
Educational attainment was reported in eight of 19 studies which did not distinguish fentanyl use and other substance use (Table 2) (16, 18, 21, 27, 31–33, 49). Three studies in the group comparing intentional fentanyl using cohorts with non-intentional fentanyl using cohorts (Table 4) and one study in the intentional fentanyl use only group (Table 3) reported educational attainment as a socioeconomic characteristic (17, 22, 24, 26). In Macmadu et al., 2017, the group of individuals with intentional fentanyl-contaminated heroin use also had a lower proportion who had attained education beyond high school (24).
Among six studies in the group comparing intentional fentanyl using cohorts with non-intentional fentanyl using cohorts, it was reported that individuals who intentionally used fentanyl were more commonly homeless and experiencing unstable housing (Table 4) (17, 23, 24, 28, 39). However only three studies demonstrated this association to be significant (17, 24, 39). Additionally, only three of 19 studies in the group which looked at fentanyl use with other substance use reported the majority of individuals being homeless (Table 2) (31, 32, 35). Homelessness was not reported in any of the 13 studies which examined intentional fentanyl use only (Table 3).
Incarceration and arrest were reported in three of the 19 studies which looked at fentanyl use with other substances (Table 2) (31, 32, 49). Moreover, in the group of studies that compared intentional fentanyl using cohorts with non-intentional fentanyl using cohorts, four studies reported higher rates of incarceration and arrest in cohorts who use fentanyl intentionally (Table 4) (24, 26, 28, 40). However, only two studies found the association to be significant (24, 28). Incarceration and arrest were not reported in the 13 studies that discussed intentional fentanyl use only (Table 3).
Overdose history was reported in eight of the 19 studies which did not distinguish fentanyl use and other substance use (Table 2) (15, 16, 21, 27, 31, 32, 36, 41). Compared to persons who did not use fentanyl in the prior six months, those that reported fentanyl use were nine times more likely to report a recent overdose following the use of any drug (16). Fentanyl injection and public injection were associated with an increased likelihood of non-fatal overdose (41). Among the group of 13 studies which looked at intentional fentanyl use only, overdose history was reported in six of the 13 studies (Table 3) (20, 34, 42, 50, 51, 53).
Individuals in the studies that compared intentional fentanyl using cohorts with non-intentional fentanyl using cohorts showed that individuals who use fentanyl intentionally experienced more overdoses (reported in seven out of 9 studies) (17, 23, 24, 26, 28, 39, 45). Among people who used heroin or prescription opioids from Baltimore, Boston, and Providence, fentanyl preference was associated with overdose more than a year ago (28). This is in contrast to a study by Chandra et al., 2021 where a cross-sectional survey found that those who purposefully used fentanyl any time in the past were significantly more likely to have experienced an overdose in the past 12 months (17). This finding is also supported by a study on the Australian Needle Syringe Program Survey (45). In British Columbia, Canada, even within the last 6 months, there were higher levels of non-fatal overdose in the last 6 months reported in individuals who intentionally use fentanyl compared to those who do not (39).
By nature of the categorization used in this review, in the group of studies that looked at fentanyl use with other substance use but where fentanyl use data were not distinguishable from other substances, it is implied that these studies included individuals who used other substances (Table 2). Among the group of studies that looked at intentional fentanyl use only, polysubstance use was common among participants as it was reported in nine of the 13 studies (Table 3) (22, 34, 38, 42, 43, 47, 48, 51, 53). This is supported by the group of studies comparing intentional fentanyl using cohorts with non-intentional fentanyl, substance using cohorts, where individuals who intentionally use fentanyl are more likely to report polysubstance use, including cocaine, heroin, and methamphetamine use (reported in eight of 9 studies) (14, 17, 23, 24, 26, 28, 39, 40). In one study, young adults who reported non-medical fentanyl use were associated with regular heroin and cocaine use, diverted pharmaceutical fentanyl use in the prior six months, regular injection drug use and prior overdose, when compared to individuals that reported non-intentional fentanyl-contaminated heroin use (24). Similarly, a population estimation study reported individuals who prefer fentanyl to have recently smoked or injected heroin and more likely to report recent injection of speedball and cocaine (26).
Among participants from studies on fentanyl with other substance use, five out of 19 studies reported motivations for fentanyl use (13, 27, 33, 37, 44). Motivations included seeking out fentanyl due to their high tolerance levels, (13, 27, 37) higher potency, (13, 27, 33, 37) delaying the onset of withdrawal, (27) and intense rush and feelings of euphoria (13, 44). Among the studies which looked at intentional fentanyl use only, motivations for fentanyl use were reported in six of the 13 studies (Table 3) (22, 38, 47, 48, 50, 51). Motivations included relieving stress/anxiety and pain (22, 38, 51). Among studies that compared intentional fentanyl using cohorts with non-intentional fentanyl substance using cohorts (Table 4), only one study described the motivations for fentanyl use among the sample: among participants who reported intentional fentanyl-contaminated heroin use, the majority (59%) reported that it provided a better high (24).
Among the 41 studies included in this review, injection as a route of administration was preferred or common in more than half of the studies. This was reported in 11 of 19 studies which did not distinguish fentanyl use and other substance use. (13, 18, 21, 27, 30–32, 35, 46, 49, 52) Similarly, this was reported in four of 13 studies which looked at intentional fentanyl use only, (22, 34, 38, 53) and seven of the nine studies which differentiated intentional fentanyl using cohorts and non-intentional fentanyl use cohorts. (17, 23, 26, 28, 39, 40, 45) Fentanyl preference was also associated with documented daily illicit drug use, (28) and injection in a public location in the last month, (45) as well as daily injection use. (16)
Independent correlates of any purposeful fentanyl use included moderate/severe depression. (17) In Macmadu et al., 2017, the group of individuals with intentional fentanyl-contaminated heroin use also had a higher proportion of ever testing positive for HCV and having a mental health diagnosis. (24) Among the studies which looked at intentional fentanyl use only, only 4 had reported concurrent disorders among participants: depression, (51) mental problems, (43) lifetime history of mental illness diagnosis, (22) and depression with psychosis. (34)
Out of the 41 papers included in this systematic review, 19 were cross-sectional studies; three were case-control, cohort, or qualitative studies. Most of the cross-sectional studies were of good methodological quality (a score of 6 or above out of 10). Six were of moderate quality (a score of 5) due to the lack of comparability based on the study design (Supplementary material). All the 12 qualitative studies were of good quality, the only flaw being not considering the relationship between the researcher and the participants for all studies except for one. This systematic review includes 11 case reports, of which nine were of good methodological quality, and two were of low quality. One flaw they all had in common was not including patients’ perspectives or experiences. However, this was not possible for some of the papers as the subjects were deceased (Supplementary material).
This systematic review found demographic indicators that were associated with fentanyl use. These include identifying as White, male, and young. Individuals who report intentional use of fentanyl also have higher likelihood of risky substance use behaviours and patterns, such as injection as their preferred route of administration, use of multiple substances, recent overdose history, daily substance use, and use of substances in public spaces. This group was also associated with socioeconomic risks such as homelessness, higher rates of unemployment, and incarceration. The scaling-up of interventions to effectively address such social and structural factors is direly needed to improve the health and well-being of individuals with fentanyl use.
Health care systems currently struggle with adapting treatment strategies to individuals with fentanyl use and severe opioid use disorder (OUD). Some novel approaches to opioid agonist treatment (OAT) have emerged in recent years, but have not seen appropriate and sustainable implementation, despite the need for it. For instance, Health Canada in 2019 approved injectable diacetylmorphine and hydromorphone for treatment of severe OUD in adults (injectable opioid agonist treatment: iOAT), (54) but the number of patients receiving iOAT is still low (149 diacetylmorphine and 28 hydromorphone clients in British Columbia in November 2022) (55). High doses of buprenorphine have been found to be effective in patients who use fentanyl in some studies due to its high potency and affinity for μ-opioid receptors (27, 56). However, the lipophilicity of fentanyl leads to its accumulation in peripheral tissues, resulting in an increased risk of precipitated withdrawal and difficulty with the buprenorphine induction process (57). One such innovation may be the use of low-dose buprenorphine inductions, which has been reported only in case series but has been successfully utilized to avoid precipitated withdrawal among fentanyl-using patients (14, 58). As there is overall limited experience with OAT approaches to suit fentanyl-using individuals, further timely research is needed to explore alternative treatment strategies, which include high-dose methadone and slow-release oral morphine protocols and fentanyl iOAT (59–62).
Current guidelines recommend the use of methadone, buprenorphine, and non-opioids for managing opioid withdrawal, however, these medications can often be insufficient in alleviating withdrawal among patient using fentanyl (63–65). Patients with undertreated withdrawal may use their illicit substances and self-discharge against medical advice, which are strongly associated with adverse outcomes and mortality (66–68). Some physicians have employed the use of short-acting opioids, like IV hydromorphone and fentanyl, to support patients to stay in hospital and initiate them on OAT (60, 65). Although these approaches have been successful, they have not yet been formally recognized as alternatives for withdrawal management in hospitalized patients. Further research is needed to determine the efficacy for these strategies.
This systematic review has several limitations. Of note are the heterogeneity of the included studies. In particular, it was important for this study to identify and focus on the intentionality of fentanyl use. Therefore, other variability was accepted in the inclusion criteria. In order to present data as granular as possible, studies where fentanyl use specifically was separated from other substances were grouped separately from studies where fentanyl use was included but not separable from the use of other substances. In addition, due to the novelty of this paper, and its focus on qualitative outcomes and breadth of data, it was difficult to screen for sufficient homogeneity to allow for a meta-analysis. Finally, this review specifically reported on intentional non-medical fentanyl use among PWUD, as opposed to among people with OUD, in order to increase the breadth of studies included and the generalizability of the findings.
The growing tendency to use fentanyl as drug of choice is extremely concerning. Our review has found that individuals who intentionally use fentanyl have severe substance use patterns, precarious living situations, and extensive overdose histories. With the street supply of opioids increasing in toxicity and an increasing number of individuals intentionally seeking fentanyl, more effective withdrawal management and OAT approaches must be developed. This paper calls for healthcare providers, researchers, and government advocates to develop alternative approaches for OUD and put in place policies allowing increased availability for fentanyl-based treatment options based on further research, which will result in a paradigm shift in the system of care.
The original contributions presented in the study are included in the article/Supplementary Materials, further inquiries can be directed to the corresponding author.
VT: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. JW: Data curation, Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. JWe: Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. NR: Data curation, Formal analysis, Writing – review & editing. HF: Data curation, Formal analysis, Writing – review & editing. MN: Writing – review & editing. VL: Writing – review & editing. NM: Writing – review & editing. PA: Writing – review & editing. KJ: Writing – review & editing. RK: Conceptualization, Resources, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authorship team would like to thank members of the research team including Rachael Reinders for her work on this manuscript. The team would also like to thank the patients at affiliated hospitals for their inspiration and motivation to carry out this project and advocate for improvements to the current health system.
PA is a consultant on Indivior-led buprenorphine extended-release studies, which are unrelated to this systematic review.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be constructed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1347678/full#supplementary-material
1. Kelly E, Sutcliffe K, Cavallo D, Ramos-Gonzalez N, Alhosan N, Henderson G. The anomalous pharmacology of fentanyl. Br J Pharmacol (2023) 180(7):797–812. doi: 10.1111/bph.15573
2. Krausz RM, Westenberg JN, Ziafat K. The opioid overdose crisis as a global health challenge. Curr Opin Psychiatry (2021) 34(4):405–12. doi: 10.1097/YCO.0000000000000712
3. Krausz RM, Westenberg JN, Mathew N, Budd G, Wong JSH, Tsang VWL, et al. Shifting North American drug markets and challenges for the system of care. Int J Ment Health Systems. (2021) 15(1):1–8. doi: 10.1186/s13033-021-00512-9
4. Barrueto F, Howland MA, Hoffman RS, Nelson LS. The fentanyl tea bag. Veterinary Hum toxicology. (2004) 46(1):30–1. Available at: https://pubmed.ncbi.nlm.nih.gov/14748415/
5. Mars SG, Rosenblum D, Ciccarone D. Illicit fentanyls in the opioid street market: desired or imposed? Addiction (2019) 114(5):774–80. doi: 10.1111/add.14474
6. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ (2021) 88:105906. doi: 10.1136/bmj.n71
7. Tsang V, Wong J, Westenberg J, Ramadhan N, Fadakar H. Systematic Review on Intentional Illicit Fentanyl Use. Available at: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021272111.
8. Wells G, Shea B, O’Connell D, et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandomised Studies in Meta-Analyses. Available at: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp.
9. Modesti PA, Reboldi G, Cappuccio FP, Agyemang C, Remuzzi G, Rapi S, et al. Panethnic differences in blood pressure in europe: A systematic review and meta-analysis. PloS One (2016) 11(1):e0147601. doi: 10.1371/journal.pone.0147601
10. Critical Appraisal Skills Programme. CASP qualitative studies checklist. Available at: https://casp-uk.net/casp-tools-checklists/.
11. Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat Methods Med Res (2018) 27(6):1785–805. doi: 10.1177/0962280216669183
12. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res methodology. (2014) 14(1):1–13. doi: 10.1186/1471-2288-14-135
13. Ciccarone D, Ondocsin J, Mars SG. Heroin uncertainties: Exploring users’ perceptions of fentanyl-adulterated and-substituted ‘heroin’. Int J Drug Policy. (2017) 46:146–55. doi: 10.1016/j.drugpo.2017.06.004
14. Antoine D, Huhn AS, Strain EC, et al. Method for successfully inducting individuals who use illicit fentanyl onto buprenorphine/naloxone. Am J Addictions. (2021) 30(1):83–7. doi: 10.1111/ajad.13069
15. Bach H, Jenkins V, Aledhaim A, Moayedi S, Schenkel S, Kim H. Prevalence of fentanyl exposure and knowledge regarding the risk of its use among emergency department patients with active opioid use history at an urban medical center in Baltimore, Maryland. Clin Toxicology. (2020) 58(6):460–5. doi: 10.1080/15563650.2019.1657583
16. Buresh M, Genberg BL, Astemborski J, Kirk GD, Mehta SH. Recent fentanyl use among people who inject drugs: results from a rapid assessment in Baltimore, Maryland. Int J Drug Policy. (2019) 74:41–6. doi: 10.1016/j.drugpo.2019.08.006
17. Chandra DK, Altice FL, Copenhaver MM, Zhou X, Didomizio E, Shrestha R. Purposeful fentanyl use and associated factors among opioid-dependent people who inject drugs. Subst Use Misuse. (2021) 56(7):979–87. doi: 10.1080/10826084.2021.1901931
18. Daniulaityte R, Carlson RR, Juhascik MP, Strayer KE, Sizemore IE. Street fentanyl use: Experiences, preferences, and concordance between self-reports and urine toxicology. Int J Drug Policy. (2019) 71:3–9. doi: 10.1016/j.drugpo.2019.05.020
19. Gryczynski J, Nichols H, Schwartz RP, Mitchell SG, Hill P, Wireman K. Fentanyl exposure and preferences among individuals starting treatment for opioid use disorder. Drug Alcohol dependence. (2019) 204:107515. doi: 10.1016/j.drugalcdep.2019.06.017
20. Gunn CM, Maschke A, Harris M, Schoenberger SF, Sampath S, Walley AY, et al. Age-based preferences for risk communication in the fentanyl era: ‘A lot of people keep seeing other people die and that’s not enough for them’. Addiction (2021) 116(6):1495–504. doi: 10.1111/add.15305
21. Kenney SR, Anderson BJ, Conti MT, Bailey GL, Stein MD. Expected and actual fentanyl exposure among persons seeking opioid withdrawal management. J Subst Abuse Treat (2018) 86:65–9. doi: 10.1016/j.jsat.2018.01.005
22. Kilwein TM, Hunt P, Looby A. A descriptive examination of nonmedical fentanyl use in the United States: Characteristics of use, motives, and consequences. J Drug Issues. (2018) 48(3):409–20. doi: 10.1177/0022042618765726
23. Kline A, Mattern D, Cooperman N, et al. Opioid overdose in the age of fentanyl: risk factor differences among subpopulations of overdose survivors. Int J Drug Policy. (2021) 90:103051. doi: 10.1016/j.drugpo.2020.103051
24. Macmadu A, Carroll JJ, Hadland SE, Green TC, Marshall BD. Prevalence and correlates of fentanyl-contaminated heroin exposure among young adults who use prescription opioids non-medically. Addictive behaviors. (2017) 68:35–8. doi: 10.1016/j.addbeh.2017.01.014
25. Marquardt KA, Steven Tharratt R. Inhalation abuse of fentanyl patch. J Toxicology: Clin Toxicology. (1994) 32(1):75–8. doi: 10.3109/15563659409000433
26. Mazhnaya A, O’Rourke A, White RH, et al. Fentanyl preference among people who inject drugs in West Virginia. Subst Use misuse. (2020) 55(11):1774–80. doi: 10.1080/10826084.2020.1762653
27. McLean K, Monnat SM, Rigg K, Sterner GE III, Verdery A. “You never know what you’re getting”: opioid users’ perceptions of fentanyl in southwest Pennsylvania. Subst Use misuse. (2019) 54(6):955–66. doi: 10.1080/10826084.2018.1552303
28. Morales KB, Park JN, Glick JL, Rouhani S, Green TC, Sherman SG. Preference for drugs containing fentanyl from a cross-sectional survey of people who use illicit opioids in three United States cities. Drug Alcohol dependence. (2019) 204:107547. doi: 10.1016/j.drugalcdep.2019.107547
29. Mrvos R, Feuchter AC, Katz KD, Duback-Morris LF, Brooks DE, Krenzelok EP. Whole fentanyl patch ingestion: a multi-center case series. J Emergency Med (2012) 42(5):549–52. doi: 10.1016/j.jemermed.2011.05.017
30. Nolte K, Drew AL, Friedmann PD, Romo E, Kinney LM, Stopka TJ. Opioid initiation and injection transition in rural northern New England: A mixed-methods approach. Drug Alcohol dependence. (2020) 217:108256. doi: 10.1016/j.drugalcdep.2020.108256
31. O’Rourke A, White RH, Park JN, Rodriguez K, Kilkenny ME, Sherman SG, et al. Acceptability of safe drug consumption spaces among people who inject drugs in rural West Virginia. Harm Reduction J (2019) 16(1):1–7. doi: 10.1186/s12954-019-0320-8
32. Park JN, Sherman SG, Rouhani S, Morales KB, McKenzie M, Allen ST, et al. Willingness to use safe consumption spaces among opioid users at high risk of fentanyl overdose in Baltimore, Providence, and Boston. J urban Health (2019) 96(3):353–66. doi: 10.1007/s11524-019-00365-1
33. Silverstein SM, Daniulaityte R, Martins SS, Miller SC, Carlson RG. “Everything is not right anymore”: buprenorphine experiences in an era of illicit fentanyl. Int J Drug Policy. (2019) 74:76–83. doi: 10.1016/j.drugpo.2019.09.003
34. Tharp AM, Winecker RE, Winston DC. Fatal intravenous fentanyl abuse: four cases involving extraction of fentanyl from transdermal patches. Am J forensic Med pathology. (2004) 25(2):178–81. doi: 10.1097/01.paf.0000127398.67081.11
35. Weicker NP, Owczarzak J, Urquhart G, et al. Agency in the fentanyl era: Exploring the utility of fentanyl test strips in an opaque drug market. Int J Drug Policy. Oct (2020) 84:102900. doi: 10.1016/j.drugpo.2020.102900
36. Amlani A, McKee G, Khamis N, Raghukumar G, Tsang E, Buxton JA. Why the FUSS (Fentanyl Urine Screen Study)? A cross-sectional survey to characterize an emerging threat to people who use drugs in British Columbia, Canada. Harm Reduction J 2015/11/14 (2015) 12(1):54. doi: 10.1186/s12954-015-0088-4
37. Bardwell G, Small W, Lavalley J, McNeil R, Kerr T. “People need them or else they’re going to take fentanyl and die”: A qualitative study examining the ‘problem’of prescription opioid diversion during an overdose epidemic. Soc Sci Med (2021) 279:113986. doi: 10.1016/j.socscimed.2021.113986
38. Firestone M, Goldman B, Fischer B. Fentanyl use among street drug users in Toronto, Canada: behavioural dynamics and public health implications. Int J Drug Policy. (2009) 20(1):90–2. doi: 10.1016/j.drugpo.2008.02.016
39. Karamouzian M, Papamihali K, Graham B, et al. Known fentanyl use among clients of harm reduction sites in British Columbia, Canada. Int J Drug Policy. (2020) 77:102665. doi: 10.1016/j.drugpo.2020.102665
40. Mitra S, Boyd J, Wood E, et al. Elevated prevalence of self-reported unintentional exposure to fentanyl among women who use drugs in a Canadian setting: a cross-sectional analysis. Int J Drug Policy. (2020) 83:102864. doi: 10.1016/j.drugpo.2020.102864
41. Wallace B, Kennedy MC, Kerr T, Pauly B. Factors associated with nonfatal overdose during a public health emergency. Subst Use misuse. (2019) 54(1):39–45. doi: 10.1080/10826084.2018.1491051
42. Woodall KL, Martin TL, McLellan BA. Oral abuse of fentanyl patches (Duragesic®): seven case reports. J forensic Sci (2008) 53(1):222–5. doi: 10.1111/j.1556-4029.2007.00597.x
43. Guerrieri D, Rapp E, Roman M, Thelander G, Kronstrand R. Acrylfentanyl: another new psychoactive drug with fatal consequences. Forensic Sci Int (2017) 277:e21–9. doi: 10.1016/j.forsciint.2017.05.010
44. Moeller K, Svensson B. “Shop Until You Drop”: Valuing fentanyl analogs on a Swedish internet forum. J Drug Issues. (2021) 51(1):181–95. doi: 10.1177/0022042620964129
45. Geddes L, Iversen J, Memedovic S, Maher L. Intravenous fentanyl use among people who inject drugs in Australia. Drug Alcohol review. (2018) 37:S314–22. doi: 10.1111/dar.12668
46. Krause D, Plörer D, Koller G, et al. High concomitant misuse of fentanyl in subjects on opioid maintenance treatment. Subst Use Misuse. (2017) 52(5):639–45. doi: 10.1080/10826084.2016.1246571
47. Kimergård A, Dunne J, Bøgen A, Hindersson P, Breindahl T. Characteristics of opioid-maintained clients smoking fentanyl patches: The importance of confirmatory drug analysis illustrated by a case series and mini-review. Drug testing analysis. (2018) 10(6):917–26. doi: 10.1002/dta.2397
48. Eiden C, Mathieu O, Donnadieu-Rigole H, Marrot C, Peyrière H. High opioids tolerance due to transmucosal fentanyl abuse. Eur J Clin Pharmacol (2017) 73(9):1195–6. doi: 10.1007/s00228-017-2272-9
49. Uusküla A, Raag M, Marsh K, Talu A, Vorobjov S, Des Jarlais D. HIV prevalence and gender differences among new injection-drug-users in Tallinn, Estonia: A persisting problem in a stable high prevalence epidemic. PloS One (2017) 12(2):e0170956. doi: 10.1371/journal.pone.0170956
50. Lyttle MD, Verma S, Isaac R. Transdermal fentanyl in deliberate overdose in pediatrics. Pediatr Emergency Care (2012) 28(5):463–4. doi: 10.1097/PEC.0b013e31825358b4
51. Gecici O, Gokmen Z, Nebioglu M. Fentanyl dependence caused by the non-medical use: a case report. Klinik Psikofarmakoloji Bülteni-Bulletin Clin Psychopharmacology. (2010) 20(3):255–7. doi: 10.1080/10177833.2010.11790668
52. Balsamo D, Bajardi P, Salomone A, Schifanella R. Patterns of routes of administration and drug tampering for nonmedical opioid consumption: data mining and content analysis of Reddit discussions. J Med Internet Res (2021) 23(1):e21212. doi: 10.2196/21212
53. Reeves MD, Ginifer CJ. Fatal intravenous misuse of transdermal fentanyl. Med J Australia. (2003) 178(10):526–6. doi: 10.5694/j.1326-5377.2003.tb05342.x
54. Government of Canada Approves New Treatment Options for Opioid Use Disorder and Supports Research, Treatment and Harm Reduction Projects in Ontario. Health Canada. Available at: https://www.Canada.ca/en/health-Canada/news/2019/05/government-of-Canada-approves-new-treatment-options-for-opioid-use-disorder-and-supports-research-treatment-and-harm-reduction-projects-in-ontario.html (Accessed July 18, 2022).
55. Opioid Agonist Treatment Indicators. British Columbia Centre for Disease Control (BCCDC). Available at: http://www.bccdc.ca/health-professionals/data-reports/overdose-response-indicators#OAT (Accessed October 3, 2022).
56. Baca-Atlas MH, Williams JB. Treatment of opioid use disorder attributed to fentanyl with high-dose buprenorphine: A case report. J Clin Psychopharmacology. (2021) 41(1):83–5. doi: 10.1097/JCP.0000000000001308
57. Shearer D, Young S, Fairbairn N, Brar R. Challenges with buprenorphine inductions in the context of the fentanyl overdose crisis: A case series. Drug Alcohol Review. (2022) 41(2):444–8. doi: 10.1111/dar.13394
58. Klaire S, Zivanovic R, Barbic SP, Sandhu R, Mathew N, Azar P. Rapid micro-induction of buprenorphine/naloxone for opioid use disorder in an inpatient setting: A case series. Am J Addict. Jul (2019) 28(4):262–5. doi: 10.1111/ajad.12869
59. Krausz RM, Westenberg JN, Vogel M. Addressing fentanyl use disorder with fentanyl-assisted treatment. Lancet Psychiatry (2022) 9(2):103–5. doi: 10.1016/S2215-0366(21)00393-X
60. Azar P, Westenberg JN, Ignaszewski MJ, Wong JSH, Isac G, Mathew N, et al. Case report: acute care management of severe opioid withdrawal with IV fentanyl. Addict Sci Clin Practice. (2022) 17(1):1–6. doi: 10.1186/s13722-022-00305-6
61. Socias ME, Wood E, Dong H, et al. Slow release oral morphine versus methadone for opioid use disorder in the fentanyl era (pRESTO): Protocol for a non-inferiority randomized clinical trial. Contemp Clin Trials (2020) 91:105993. doi: 10.1016/j.cct.2020.105993
62. Buresh M, Nahvi S, Steiger S, Weinstein ZM. Adapting methadone inductions to the fentanyl era. J Subst Abuse Treat (2022) 141:108832. doi: 10.1016/j.jsat.2022.108832
63. American Society of Addiction Medicine. The ASAM national practice guideline for the treatment of opioid use disorder: 2020 focused update. J Addict Med (2020) 14(2S):1–91. doi: 10.1097/adm.0000000000000633
64. Canadian Research Initiative on Substance Misuse (CRISM). CRISM National Guideline for the Clinical Management of Opioid use Disorder (2018). Available at: https://crism.ca/projects/opioid-guideline/ (Accessed 2022-11-30).
65. Kleinman RA, Wakeman SE. Treating opioid withdrawal in the hospital: A role for short-acting opioids. Ann Internal Med Feb (2022) 175(2):283–4. doi: 10.7326/m21-3968
66. Simon R, Snow R, Wakeman S. Understanding why patients with substance use disorders leave the hospital against medical advice: A qualitative study. Subst Abuse. 2020/10/01 (2020) 41(4):519–25. doi: 10.1080/08897077.2019.1671942
67. Southern WN, Nahvi S, Arnsten JH. Increased risk of mortality and readmission among patients discharged against medical advice. Am J Med (2012) 125(6):594–602. doi: 10.1016/j.amjmed.2011.12.017
Keywords: addiction, fentanyl, overdose crisis, substance use, opioid use disorder
Citation: Tsang VWL, Wong JSH, Westenberg JN, Ramadhan NH, Fadakar H, Nikoo M, Li VW, Mathew N, Azar P, Jang KL and Krausz RM (2024) Systematic review on intentional non-medical fentanyl use among people who use drugs. Front. Psychiatry 15:1347678. doi: 10.3389/fpsyt.2024.1347678
Received: 01 December 2023; Accepted: 18 January 2024;
Published: 13 February 2024.
Edited by:
Marc Walter, University of Basel, SwitzerlandReviewed by:
Brian J. Piper, Geisinger Commonwealth School of Medicine, United StatesCopyright © 2024 Tsang, Wong, Westenberg, Ramadhan, Fadakar, Nikoo, Li, Mathew, Azar, Jang and Krausz. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vivian W. L. Tsang, dml2aWFud2x0c2FuZ0BhbHVtbmkudWJjLmNh
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.