
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychiatry, 05 July 2024
Sec. Aging Psychiatry
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1347476
This article is part of the Research TopicReviews in Psychiatry 2023: Aging PsychiatryView all 5 articles
Background: Stroke is considered the second most common cause of death and the third leading cause of disability worldwide. Frailty, characterized by increased vulnerability to stressors, is emerging as a key factor affecting outcomes in older adults and stroke patients. This study aimed to estimate the prevalence of frailty in acute stroke patients and assess its association with mortality and poor functional outcome.
Methods: Medline, Google Scholar, and Science Direct databases were systematically searched for English-language studies that included adult stroke patients (>16 years), have defined frailty, and reported mortality and functional outcomes. Meta-analysis was done using STATA 14.2, and the results were expressed as pooled odds ratios (OR) with 95% confidence intervals (CI). Heterogeneity was assessed using the I2 statistic and the Chi-square test. Study quality was evaluated using the Newcastle Ottawa Scale (NOS).
Results: Twenty-five studies were included in the analysis. Frailty prevalence in stroke patients was 23% (95% CI 22% - 23%). Unadjusted analysis showed an OR of 2.66 (95% CI: 1.93 - 3.67) for mortality and 2.04 (95% CI: 1.49 - 2.80) for poor functional outcome. Adjusted estimates indicated an OR of 1.22 (95% CI: 1.1 - 1.35) for mortality and 1.21 (95% CI: 1.04 - 1.41) for poor functional outcome, with substantial heterogeneity for both adjusted and unadjusted analyses. No publication bias was detected for the prevalence of frailty. However, there was a publication bias for the association between frailty and mortality.
Conclusions: Frailty was significantly associated with increased mortality and poorer functional outcomes in stroke patients. Our study highlights the need to focus on frailty in stroke patients to improve outcomes and quality of life. Further research should aim to standardize assessment of frailty and reduce heterogeneity in study outcomes.
Systematic review registration: https://www.crd.york.ac.uk/prospero/#searchadvanced, CRD42023470325.
Stroke is a leading cause of mortality and disability worldwide, presenting a significant public health challenge (1). It is third most common cause of disability (5.7 percent of total disability-adjusted disability years [DALYs]) and the second most common cause of death worldwide (11.6% of total deaths) (2). Stroke often leads to long-term physical, cognitive, and emotional consequences (3) which are associated with a considerable economic burden due to medical costs, lost productivity, and the need for the caregiver support. Predicting the outcomes of stroke is inherently complex due to the heterogeneity of the disease: stroke patients may experience a wide range of clinical symptoms and functional impairments that affect recovery (4). With the continuous aging of the general population, frailty is emerging as a potential key factor in the context of stroke outcomes. Frailty is characterized by multi-systemic decline that impacts the ability of cellular repair mechanisms to maintain system homeostasis, and is linked to increased mortality and higher rates of hospital admissions (5). Several studies have shown that acute stroke patients frequently present with frailty, which is linked to unfavorable outcomes (6, 7).
Many global healthcare systems are currently viewing frailty as an integral component of their acute care pathways (8). While stroke is considered one of the more common acute presentations in older patient, frailty assessment is not yet routinely included in stroke care, and stroke is rarely mentioned in best practice guidelines on frailty (9). Studies, evaluating the impact of frailty on the outcomes in stroke patients are still scarce. Previous existing meta-analyses by Bao et al. (2023), and Burton et al. (2022) included only eight and 14 studies, respectively, with an literature search up to 2020 (10, 11). While a recent study by Huang et al. updated the existing body of evidence, it focused exclusively on the burden of frailty in stroke patients (12). There is no existing research that has determined the association between frailty and mortality in this vulnerable group. This study aims to summarize the existing data, update a baseline estimation on the prevalence of frailty in stroke patients, and to assess the link between frailty and stroke outcomes.
To estimate the prevalence of frailty in patients with acute stroke and to assess the association between frailty and clinical outcomes (mortality and poor functional outcome) in this population.
Literature search was done in Medline, Google Scholar and Science Direct databases from inception till October 2023 for articles published in English language. Data screening was performed independently by the two reviewers, and all disagreements were resolved by the principal investigator (PI). The review was reported in accordance with the latest “Preferred reporting items for systematic reviews and meta-analyses (PRISMA)” framework (13). The data extraction template was prepared by the PI, who also double checked the data entry for correctness. Ethical approval is not applicable since we extracted data from freely available sources.
Adult patients (>16 years of age) who presented with any type of stroke (except for transient ischemic attacks) were included. Only patients who presented with acute stroke were included, while patients who were undergoing rehabilitative therapy were excluded.
The exposure of interest was frailty. We accepted any recommended definition of frailty used by individual studies if that have quantified or categorized frailty levels and have confirmed its onset before the stroke event. In addition, we included studies that reported prevalence of frailty among patients with acute stroke.
Our primary outcome of interest was mortality (reported at various time points – in hospital to 1 year follow up as reported by the studies), functional outcome and length of hospital stay.
We included all analytical studies (prospective, retrospective, and cross-sectional studies).
We utilized Medical subject heading (MeSH) terms such as: “Stroke” OR “Cerebrovascular accident” AND “Fragility” OR “Elderly” AND “Mortality” OR “Death” OR “Survival” AND “functional outcome” AND “Observational studies” OR “Cohort studies” OR “Prospective studies”. The references of included studies for potentially eligible reports. The detailed search strategy is explained in Supplementary File 1.
The first and the second authors independently extracted data such as author’s details, study design, sample size, geographical location, inclusion criteria, definition of frailty and classification tools used to assess it.
STATA 14.2. was used for analysis. Inverse variance method was used for binary outcomes to combine the effects across various studies. The outcome was then expressed as pooled odds ratios (OR) with 95% confidence intervals (CIs). For each study reporting prevalence of frailty among patients with diagnosed stroke, standard error was computed by using provided prevalence and sample size. To perform the prevalence meta-analysis, we employed the “metaprop” function (14). To account for the potential influence of both large and small studies on the pooled estimates, we applied the Freeman-Tukey double arcsine transformation. The final pooled prevalence was reported, along with its corresponding 95% CI. In cases of missing data, attempts were made to contact the respective authors for the necessary information. The results were presented as pooled effect sizes and visually depicted through forest plots. Funnel plots and Egger’s test (15) were used to assess publication bias. P<0.05 indicated statistical significance.
Variability between studies was assessed by I2 statistic and Chi-square heterogeneity test. We categorized heterogeneity into three levels: mild (I2 < 25%), moderate (I2 between 25% and 75%), and considerable (I2 > 75%).
Quality of the studies included in our analysis was evaluated by the Newcastle Ottawa Scale (NOS) (16). This scale assesses study quality based on three criteria: ascertainment of outcomes, selection of study groups, and comparability. In the Selection and Outcome categories, a study can receive a maximum of one star for each numbered item. For comparability, a maximum of two stars can be assigned. Therefore, the NOS allows for a maximum score of nine for each study.
A total of 10128 articles were identified by the literature search. After primary screening, 7639 papers were removed as duplicates. Additional 2003 studies were eliminated at the stage of title and abstract screening. From the remaining 486 studies, 55 free full text articles were retrieved. Finally, 25 articles that met eligibility criteria were included in our systematic review and meta-analysis (17–41). Twenty articles reported on the prevalence of frailty among stoke patients, 17 reported on the association between mortality and frailty, and eight studies reported the association between poor functional outcome and frailty. The PRISMA 2020 flow diagram of the study is explained in Figure 1.
General characteristics of the included studies are detailed in Table 1. Of 25 included studies, 12 were from Europe, eight were from Asia, three from America and two from Australia. Included studies had sample sizes ranging from 102 to 48980. All studies reported results in English language. Studies defined frailty based on different assessment tools, with the most commonly used tool being Clinical Frailty Scale (CFS).
Of 55 full-text articles that were retrieved, 37 were excluded during the secondary screening. Of them, 24 studies did not define frailty, six were reported in languages other than English, and seven had mixed study population.
Prevalence of frailty in stroke patients was reported in 20 studies (n=90118). After adjusting for population weights, the overall pooled prevalence of frailty in stroke patients was 23% (95%CI 22% - 23%) with no heterogeneity (I2 = 0.0). (Figure 2) A subgroup analysis analyzing the difference in prevalence estimates with respect to region of the included studies showed that the prevalence was lower in studies from the Asian continent (15%, 95%CI 13% - 16%), (Supplementary File 2).
Seventeen studies reported the unadjusted association between frailty and mortality. We saw that patients with frailty and stroke had 2.66 higher odds of mortality when compared to stroke patients without frailty (pooled OR of 2.66, 95% CI: 1.93 - 3.67), with very high heterogeneity (I2 = 95.1, p-value <0.001). (Figure 3) Eight studies reported on the unadjusted association between frailty and poor functional outcome. Frail patients had 2.04-higher odds of having poor functional outcome when compared to patients without frailty (pooled OR of 2.04, 95% CI: 1.49 - 2.80), with high heterogeneity (I2 = 88.3, p value <0.001). (Figure 4) Subgroup analysis based on the region of included studies for mortality and poor functional outcome is shown in Supplementary File 3 and Supplementary File 4 respectively.
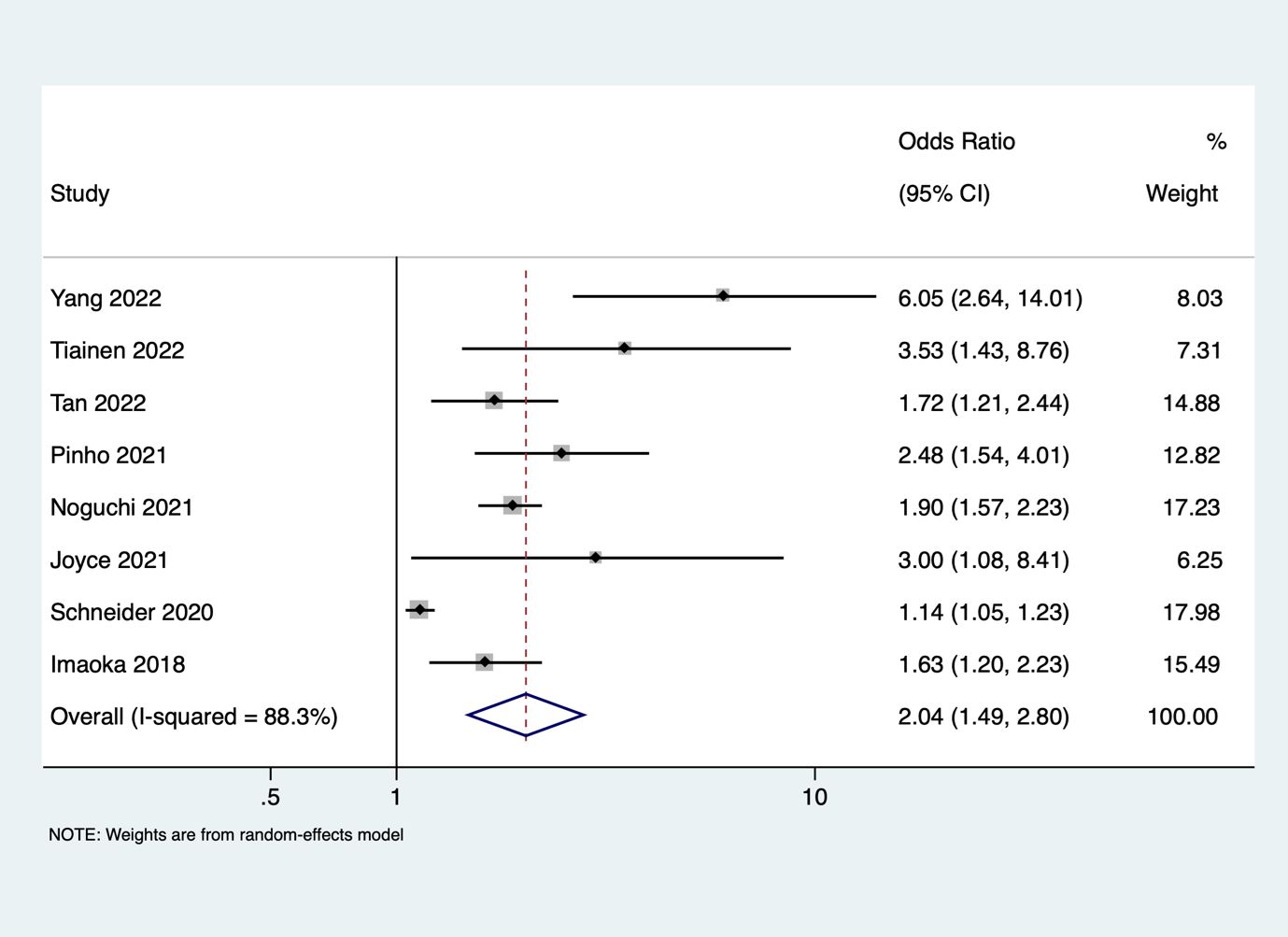
Figure 4 Forest plot showing the association between frailty and poor functional outcome (unadjusted).
Eleven out of seventeen studies that reported on association between frailty and mortality reported adjusted estimates. After adjusting for potential confounders, our analysis demonstrated that frailty in stroke patients was associated with 1.22-higher odds of mortality when compared to stroke patients without frailty (pooled OR of 1.22, 95% CI: 1.1 - 1.35), with high heterogeneity (I2 = 83.3, p-value <0.001). (Supplementary File 5) Six out of eight studies reported on the adjusted association between frailty and poor functional outcome. The pooled evidence showed that after adjusting for potential confounders, frailty was associated with 1.21-higher odds of ending up with poor functional outcomes (pooled OR of 1.21, 95% CI: 1.04 - 1.41, with high heterogeneity I2 = 80.8, p value <0.001). (Supplementary File 6). Supplementary Files 7 and 8 describes the subgroup analysis based on the region of included studies for mortality and poor functional outcome.
We evaluated the presence of publication bias for prevalence and the association between frailty and mortality (both adjusted and unadjusted) as they had more than 10 studies. We noted that the funnel plots were symmetrical for prevalence estimates, confirming the absence of publication bias (Egger coefficient -0.23, p value 0.91). (Figure 5) However, we observed clear asymmetry in funnel plot for both unadjusted (Supplementary File 9), and adjusted estimates (Supplementary File 10) for association between frailty and mortality.
As shown in Table 1, most included studies had low risk of bias, with the NOS scores of 6 to 8. The difference in effect estimates for various outcomes with respect to risk of bias scores is expressed in Supplementary Files 11-15. Subgroup analysis based on the tool used is described in Supplementary File 16. We did not detect any difference in the mortality prevalence, except for three studies that had used Faurot frailty index, pre stroke modified Rankin scale, 5 item simplified frailty scale, and frailty phenotype – all of which showed mortality less than 15%. Comparison of the length of hospital stay in patients with and without frailty is described in Supplementary File 17. Subgroup analyses based on the study design of the included studies for unadjusted mortality estimates are included in Supplementary File 18.
Our meta-analysis that included 25 studies showed that the prevalence of frailty among patients with stroke was 23% (95%CI 22% - 23%). Our results detected a significant association between frailty and mortality (adjusted OR 1.22, 95% CI: 1.1 - 1.35) and poor functional outcome (adjusted OR 1.21, 95% CI: 1.04 - 1.41) even after adjusting for potential confounders. The findings of our review further emphasize the importance of frailty assessment in predicting outcomes after stroke.
Our results showed that the pooled prevalence of frailty in stroke patients was 23 percent, as reported by 20 studies from various study settings. This is consistent with the growing understanding that frailty is a common problem among elderly stroke patients (11, 12). Previous studies have shown that factors such as type of assessment method and geographic location can affect the prevalence of frailty (42). This is supported by our subgroup analysis, which reveals that the prevalence of frailty in Asian studies was 15% lower than that in non-Asian populations.
Our results demonstrated that stroke patients with frailty are at significantly higher risk of mortality compared to patients without frailty (OR of 2.66). Moreover, after accounting for potential confounders, frailty remained independently associated with increased mortality in stroke patients (OR of 1.22). These findings are consistent with the previous reports (11, 37) which further strengthen the prognostic significance of frailty in stroke patients. The observed high heterogeneity in both unadjusted and adjusted estimates underscores the need for further investigation into factors contributing to this variability (43).
Both unadjusted and adjusted estimates in our study showed that frailty was significantly associated with poor functional outcomes post-stroke. These results have crucial implications for rehabilitation and allocation of resources to support functional recovery of stroke survivors.
In Europe, the prevalence of frailty in persons 65 years of age or older is currently estimated to be over 15% (42), rising to over 25% (44) in adults 85 years of age or older. These estimates are in line with our subgroup analysis findings. Studies showed that clinical frailty positively correlated with stroke severity in older patients and with 28-day mortality following ischemic stroke (45). We may speculate that these findings can be partially explained by the multifaceted nature of frailty. The term “frailty” refers to a range of psychological, social, and physiological characteristics that, together with stroke-related factors, may affect outcomes of stroke patients. Frailty is defined physiologically as a reduced reserve and increased susceptibility to stressors. In stroke patients, these stressors include the cerebrovascular event itself and subsequent complications. Reduced physiological resilience of frail patients may, therefore, translate into poorer outcomes. Frailty is often accompanied by psychological, cognitive and emotional challenges that can worsen after the stroke, impairing self-care and rehabilitation compliance. Additionally, while social networks are essential for stroke rehabilitation, their availability may be restricted by frailty. Stroke patients with frailty may, therefore, face challenges in accessing caregiving resources and rehabilitation services, potentially affecting the effectiveness of their recovery.
Our results have substantial clinical implications. By recognizing frailty as a key predictor of stroke outcomes, clinicians can refine risk stratification and individualize care plans. Early interventions targeting frailty, such as physical therapy, nutrition support, and psychosocial interventions, can be integrated into stroke management protocols. These measures may improve post-stroke recovery and reduce the burden of frailty-related complications. Moreover, policymakers and healthcare systems should consider the inclusion of frailty assessments in stroke care guidelines. This could lead to improved resource allocation, including the provision of rehabilitation services and social support tailored to the needs of frail stroke survivors.
Our review is one of the few studies that attempted to find the link between frailty and stroke outcomes. The increased power of our review due to the large sample size is another major strength. We have also assessed the risk of publication bias and showed that our summary estimates were robust across various subgroup and sensitivity analyses. However, our study has several limitations. First, most included studies were observational with a retrospective design, which might have biased our results. Second, we were unable to adjust for all confounding variables. Finally, not all studies used the same frailty assessment tools, resulting in differences in estimates and high clinical heterogeneity. Additionally, we could not completely exclude the possibility of language and publication bias.
In conclusion, this systematic review and meta-analysis showed that approximately fifth of older stroke patients are frail, which could potentially influence their clinical outcome. Our study underscores the importance of addressing frailty in the context of stroke. By recognizing and managing frailty, healthcare providers and policymakers have an opportunity to improve outcomes and quality of life of this vulnerable population. Future studies should aim to reduce heterogeneity by standardizing frailty assessment. We recommend incorporation of frailty assessment in elderly stroke management. Clinicians should consider specific rehabilitation interventions targeting nutritional and psychosocial needs, based on the frailty status of stroke survivors.
The original contributions presented in the study are included in the article/Supplementary Materials. Further inquiries can be directed to the corresponding author.
JL: Conceptualization, Data curation, Investigation, Supervision, Writing – original draft, Writing – review & editing. JW: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Validation, Writing – original draft. HW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1347476/full#supplementary-material
1. Kamalakannan S, Gudlavalleti ASV, Gudlavalleti VSM, Goenka S, Kuper H. Incidence & prevalence of stroke in India: A systematic review. Indian J Med Res. (2017) 146:175–85. doi: 10.4103/ijmr.IJMR_516_15
2. GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. (2021) 20:795–820. doi: 10.1016/S1474-4422(21)00252-0
3. Strong K, Mathers C, Bonita R. Preventing stroke: saving lives around the world. Lancet Neurol. (2007) 6:182–7. doi: 10.1016/S1474-4422(07)70031-5
4. Emberson J, Lees KR, Lyden P, Blackwell L, Albers G, Bluhmki E, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of individual patient data from randomised trials. Lancet Lond Engl. (2014) 384:1929–35. doi: 10.1016/S0140-6736(14)60584-5
5. Quinn TJ, Taylor-Rowan M, Coyte A, Clark AB, Musgrave SD, Metcalf AK, et al. Pre-stroke modified Rankin scale: evaluation of validity, prognostic accuracy, and association with treatment. Front Neurol. (2017) 8:275. doi: 10.3389/fneur.2017.00275
6. Bruno A, Switzer JA, Durkalski VL, Nichols FT. Is a prestroke modified Rankin Scale sensible? Int J Stroke Off J Int Stroke Soc. (2011) 6:414–5. doi: 10.1111/j.1747-4949.2011.00661.x
7. Burton JK, Ferguson EEC, Barugh AJ, Walesby KE, MacLullich AMJ, Shenkin SD, et al. Predicting discharge to institutional long-term care after stroke: A systematic review and metaanalysis. J Am Geriatr Soc. (2018) 66:161–9. doi: 10.1111/jgs.15101
8. Visvanathan A, Graham C, Dennis M, Lawton J, Doubal F, Mead G, et al. Predicting specific abilities after disabling stroke: Development and validation of prognostic models. Int J Stroke Off J Int Stroke Soc. (2021) 16:935–43. doi: 10.1177/1747493020982873
9. Quinn TJ, Dawson J, Walters MR, Lees KR. Functional outcome measures in contemporary stroke trials. Int J Stroke Off J Int Stroke Soc. (2009) 4:200–5. doi: 10.1111/j.1747-4949.2009.00271.x
10. Bao Q, Huang X, Wu X, Chen S, Yang J, Zhang J, et al. Implications of frailty in acute ischemic stroke receiving endovascular treatment: systematic review and meta-analysis. Aging Clin Exp Res. (2023) 35:969–78. doi: 10.1007/s40520-023-02383-1
11. Burton JK, Stewart J, Blair M, Oxley S, Wass A, Taylor-Rowan M, et al. Prevalence and implications of frailty in acute stroke: systematic review & meta-analysis. Age Ageing. (2022) 51:afac064. doi: 10.1093/ageing/afac064
12. Huang YN, Yan FH, Wang XY, Chen XL, Chong HY, Su WL, et al. Prevalence and risk factors of frailty in stroke patients: A meta-analysis and systematic review. J Nutr Health Aging. (2023) 27:96–102. doi: 10.1007/s12603-023-1879-z
13. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71. doi: 10.1136/bmj.n71
14. Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health Arch Belg Sante Publique. (2014) 72:39. doi: 10.1186/2049-3258-72-39
15. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
16. Lo CKL, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. (2014) 14:45. doi: 10.1186/1471-2288-14-45
17. Taylor-Rowan M, Hafdi M, Drozdowska B, Elliott E, Wardlaw J, Quinn TJ. Physical and brain frailty in ischaemic stroke or TIA: Shared occurrence and outcomes. A cohort study. Eur Stroke J. (2023) 8:23969873231186480. doi: 10.1101/2023.02.15.23286006
18. Zhang XM, Jiao J, Xu T, Wu XJ. The association between frailty of older stroke patients during hospitalization and one-year all-cause mortality: A multicenter survey in China. Int J Nurs Sci. (2023) 9:162–8. doi: 10.1016/j.ijnss.2022.02.001
19. Ng CC, Lim WC, Tan KM, Wong KY, Kanagarajah RR, Singh HSAK, et al. Is pre-stroke frailty as determined by the Clinical Frailty Scale version 2.0 associated with stroke outcomes? Singapore Med J. (2023), 1–4. doi: 10.4103/singaporemedj.SMJ-2021-187
20. Vazquez S, Stadlan Z, Lapow JM, Feldstein E, Shah S, Das A, et al. Frailty and outcomes in lacunar stroke. J Stroke Cerebrovasc Dis. (2023) 32:106942. doi: 10.1016/j.jstrokecerebrovasdis.2022.106942
21. Hanlon P, Burton JK, Quinn TJ, Mair FS, McAllister D, Lewsey J, et al. Prevalence, measurement, and implications of frailty in stroke survivors: An analysis of three global aging cohorts. Int J Stroke. (2023) 18:720–7. doi: 10.1177/17474930231151847
22. Yang F, Li N, Yang L, Chang J, Yan A, Wei W. Association of pre-stroke frailty with prognosis of elderly patients with acute cerebral infarction: A cohort study. Front Neurol. (2022) 13:855532. doi: 10.3389/fneur.2022.855532
23. Nozoe M, Noguchi M, Kubo H, Kanai M, Shimada S. Association between the coexistence of premorbid sarcopenia, frailty, and disability and functional outcome in older patients with acute stroke. Geriatr Gerontol Int. (2022) 22:642–7. doi: 10.1111/ggi.14432
24. Miranda LA, Luvizutto GJ, Stephan BCM, de Souza JT, da Silva TR, Winckler FC, et al. Evaluating the performance of the PRISMA-7 frailty criteria for predicting disability and death after acute ischemic stroke. J Stroke Cerebrovasc Dis. (2022) 31:106837. doi: 10.1016/j.jstrokecerebrovasdis.2022.106837
25. Noguchi M, Kubo H, Kanai M, Nozoe M, Shimada S. Relationship between pre-stroke frailty status and short-term functional outcome in older patients with acute stroke -A mediation analysis-. Arch Gerontol Geriatr. (2021) 94:104370. doi: 10.1016/j.archger.2021.104370
26. Kilkenny MF, Phan HT, Lindley RI, Kim J, Lopez D, Dalli LL, et al. Utility of the hospital frailty risk score derived from administrative data and the association with stroke outcomes. Stroke. (2021) 52:2874–81. doi: 10.1161/STROKEAHA.120.033648
27. Joyce N, Atkinson T, Mc Guire K, Wiggam MI, Gordon PL, Kerr EL, et al. Frailty and stroke thrombectomy outcomes—an observational cohort study. Age Ageing. (2022) 51:1–24. doi: 10.1093/ageing/afab260
28. Pinho J, Küppers C, Nikoubashman O, Wiesmann M, Schulz J, Reich A, et al. Frailty is an outcome predictor in patients with acute ischemic stroke receiving endovascular treatment. Age Ageing. (2021) 50:1785–91. doi: 10.1093/ageing/afab092
29. Schnieder M, Bähr M, Kirsch M, Maier I, Behme D, Riedel CH, et al. Analysis of frailty in geriatric patients as a prognostic factor in endovascular treated patients with large vessel occlusion strokes. J Clin Med. (2021) 10:2171. doi: 10.3390/jcm10102171
30. Wæhler I, Saltvedt I, Lydersen S, Fure B, Askim T, Einstad MS, et al. Association between in-hospital frailty and health-related quality of life after stroke: the Nor-COAST study. BMC Neurol. (2021) 21:1–12. doi: 10.1186/s12883-021-02128-5
31. Zhang W, Anderson CS, Kilkenny MF, Kim J, Dewey HM, Andrew NE, et al. Hospital admissions prior to primary intracerebral haemorrhage and relevant factors associated with survival. J Stroke Cerebrovasc Dis. (2020) 29:105026. doi: 10.1016/j.jstrokecerebrovasdis.2020.105026
32. Kanai M, Noguchi M, Kubo H, Nozoe M, Kitano T, Izawa KP, et al. Pre-stroke frailty and stroke severity in elderly patients with acute stroke. J Stroke Cerebrovasc Dis. (2020) 29:105346. doi: 10.1016/j.jstrokecerebrovasdis.2020.105346
33. Evans NR, Wall J, To B, Wallis SJ, Romero-Ortuno R, Warburton EA. Clinical frailty independently predicts early mortality after ischaemic stroke. Age Ageing. (2020) 49:588–91. doi: 10.1093/ageing/afaa004
34. Myint PK, Bachmann MO, Loke YK, Musgrave SD, Price GM, Hale R, et al. Important factors in predicting mortality outcome from stroke: Findings from the Anglia Stroke Clinical Network Evaluation Study. Age Ageing. (2017) 46:83–90. doi: 10.1093/ageing/afw175
35. Seamon BA, Simpson KN. The effect of frailty on discharge location for medicare beneficiaries after acute stroke. Arch Phys Med Rehabil. (2019) 100:1317–23. doi: 10.1016/j.apmr.2019.02.006
36. Taylor-Rowan M, Cuthbertson G, Keir R, Shaw R, Drozdowska B, Elliott E, et al. The prevalence of frailty among acute stroke patients, and evaluation of method of assessment. Clin Rehabil. (2019) 33:1688–96. doi: 10.1177/0269215519841417
37. Tiainen M, Martinez-Majander N, Virtanen P, Räty S, Strbian D. Clinical frailty and outcome after mechanical thrombectomy for stroke in patients aged ≥ 80 years. J Stroke Cerebrovasc Dis. (2022) 31:106816. doi: 10.1016/j.jstrokecerebrovasdis.2022.106816
38. Tan BYQ, Ho JSY, Leow AS, Chia MLJ, Sia CH, Koh YY, et al. Effect of frailty on outcomes of endovascular treatment for acute ischaemic stroke in older patients. Age Ageing. (2022) 51:afac096. doi: 10.1093/ageing/afac096
39. Patel K, Shrier WEJ, Sengupta N, Hunt DCE, Hodgson LE. Frailty, assessed by the rockwood clinical frailty scale and 1-year outcomes following ischaemic stroke in a non-specialist UK stroke centre. J Stroke Cerebrovasc Dis. (2022) 31:106451. doi: 10.1016/j.jstrokecerebrovasdis.2022.106451
40. Imaoka Y, Kawano T, Hashiguchi A, Fujimoto K, Yamamoto K, Nishi T, et al. Modified frailty index predicts postoperative outcomes of spontaneous intracerebral hemorrhage. Clin Neurol Neurosurg. (2018) 175:137–43. doi: 10.1016/j.clineuro.2018.11.004
41. Pilotto A, Brass C, Fassbender K, Merzou F, Morotti A, Kämpfer N, et al. Premorbid frailty predicts short- and long-term outcomes of reperfusion treatment in acute stroke. J Neurol. (2022) 269:269. doi: 10.1007/s00415-022-10966-7
42. Shaharudin MI, Abd Rahman NFN. Prevalence of frailty and its standardised assessment tools among Malaysian older person: A systematic review. Malays J Med Sci. (2022) 29:34–45. Academy of Language Studies, Universiti Teknologi MARA, Melaka, Malaysia, Physiotherapy Programme, Faculty of Health Sciences, Universiti Teknologi MARA, Pulau Pinang, Malaysia. doi: 10.21315/mjms
43. O’Caoimh R, Galluzzo L, Rodríguez-Laso Á, der Heyden JV, Ranhoff AH, Lamprini-Koula M, et al. Prevalence of frailty at population level in European ADVANTAGE Joint Action Member States: a systematic review and meta-analysis. Ann DellIstituto Super Sanità. (2018) 54:226–38. doi: 10.4415/ANN_18_03_10
44. Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. (2012) 60:1487–92. doi: 10.1111/j.1532-5415.2012.04054.x
Keywords: frailty, stroke, mortality, poor functional outcome, meta-analysis
Citation: Li J, Wan J and Wang H (2024) Role of frailty in predicting outcomes after stroke: a systematic review and meta-analysis. Front. Psychiatry 15:1347476. doi: 10.3389/fpsyt.2024.1347476
Received: 31 December 2023; Accepted: 03 June 2024;
Published: 05 July 2024.
Edited by:
Francesco Panza, University of Bari Aldo Moro, ItalyReviewed by:
Marzia Baldereschi, National Research Council (CNR), ItalyCopyright © 2024 Li, Wan and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jing Li, bGoxODE2NzI1Nzc4MkAxMjYuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.