- Department of Psychiatry, College of Medicine and Health Sciences, University of Gondar, Gondar, Ethiopia
Background: Coronavirus disease 2019 (COVID-19) outbreak is one of the public health problems that pose a serious mental health concern due to its high morbidity and mortality rate. The healthcare workers are at risk of developing mental health symptoms like depression and anxiety because they are the first point of contact in the diagnosis, treatment, and care of patients with COVID-19. This study aimed to systematically review the prevalence and the associated factors of depression and anxiety disorders among healthcare workers amid COVID-19 pandemic in Ethiopia.
Method: A systematic review and meta-analysis study was conducted. Different primary studies that assessed the depressive and anxiety disorders during amid COVID-19 pandemic in the Ethiopian healthcare workers were extracted by Microsoft Excel and exported to STATA version 11 for further analysis. Random-effects model meta-analysis was used to the estimate pooled effect size and the effect of each study with their 95% confidence interval. Funnel plot analysis and Egger regression tests were conducted to detect the presence of publication bias. Subgroup analysis and sensitivity analysis were conducted.
Results: Thirteen studies with 5,174 participants were included in this systematic review and meta-analysis study. The pooled prevalence of depression and anxiety disorders was 40.39% (95% CI: 28.54, 52.24) and 44.93% (95% CI: 31.39, 58.46), respectively. Being a woman, being married, working in the frontline, and having high perceived susceptibility were significantly associated with depression among the Ethiopian healthcare workers. Similarly, being a woman, being older in age, working in the frontline, and having high perceived susceptibility were the factors associated with anxiety disorder among the Ethiopian healthcare workers during the COVID-19 pandemic.
Conclusion: The prevalence of depression and anxiety disorders in the Ethiopian healthcare workers was high. The timely detection and appropriate management of mental health problems is essential for the quality of healthcare services, and proactive support methods for the female, married, and older-age healthcare professionals could result in these outcomes.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/, identifier CRD42022299074.
Introduction
Coronavirus disease 2019 (COVID-19) is a family of ribonucleic acid (RNA) viruses that results in infections for humans with respiratory syndrome, causing unprecedented numbers of deaths and substantial psychological distress to the global community (1, 2). The diseases rapidly propagated, and, in a realm of less than a month, it rapidly disseminated in other parts of the world; hence, the detected cases were reported in nine countries (3), and, then, it spread and nocked the door of the majority of countries. Since then, a staggering number of new cases are pouring into the case box every single minute, and death toll is climbing overwhelmingly high with a growth factor above 1 indicating an exponential increase (4). Ethiopia has faced the pandemic and reported the case of COVID-19 in March 2020 (5). The shock wave of information regarding the pandemic in the country is more than ever since the first case was confirmed.
The outbreak of the COVID-19 pandemic results in a huge mental health concern such as depression, anxiety, adjustment disorder, panic attacks, and insomnia because of the fear of getting sick and/or dying (6–8). The psychological fear reaction results from the infection and death of higher numbers of people by COVID-19 infection in the general public (9). The healthcare workers (HCWs) are at risk of developing mental health symptoms like depression and anxiety because they are the first point of contact in the diagnosis, treatment, and care of patients with COVID-19 (10, 11). Recent literature studies reported that the disease outbreak causes a higher level of mental health impacts particularly depression and anxiety symptoms among HCWs compared to those in the general population (12–14). In regard to the types of mental health impact, depression, anxiety, stress, and insomnia were ranging from 10.6% to 58%, 11.1% to 100%, 5.2% to 100%, and 28.75% to 34%, respectively (10, 15–17). Factors, such as gender, age, educational level, work experience, psychological/medical comorbidity, perceived social support, perceived susceptibility, working environment, and personal/family exposure, were the factors associated with the negative mental state of HCWs due to COVID-19 (10, 18–20).
Higher levels of depressive and anxiety symptoms are also associated with the perceived susceptibility to the disease and perceived severity of disease (21, 22) and loneliness (23, 24). World Health Organization reports that depression, anxiety, panic disorder, suicide, and sleep disturbances increased because of the burden of psychological distress in the world (25). Furthermore, it reports that COVID‐19 pandemic–related long‐lasting depression and anxiety problems are becoming a serious public health concern (26). These mental health problems can prevent the HCWs from fulfilling their duties and reduce the quality of healthcare services to patients (27, 28).
In Ethiopia, there are inconsistent primary studies on mental health problems and its correlates amid COVID-19 outbreak on HCWs, which need comprehensive evidence for decision-making, and, yet, there is no systematic review and meta-analysis. Studying the mental health impacts of COVID-19 gives vital information on its prevalence of depression and anxiety symptoms and enables us to discover HCWs dynamics of strong resilience. This information helps to the planning and provision of preventive strategies and effective treatment modalities to strengthen its positive outcomes and health policy of the country to address the HCWs’ mental health outcomes of pandemic. Thus, the aim of this systematic review and meta-analysis was to assess the prevalence of depression and anxiety symptoms and its potential correlates on HCWs during the COVID-19 response in Ethiopia.
Methods
We conducted a systematic review to identify the prevalence of depressive and anxiety symptoms and its correlates in low-resource settings using the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines (29). The checklist of meta-analysis of observational study in epidemiology was also followed. The project’s protocol was prepared, registered, and published on Prospero with the registration number CRD42022299074.
Search strategy
We rigorously searched the peer-reviewed literature studies that were found from PubMed, Medline, ScienceDirect, and Google Scholar. The electronic databases were searched for all the published articles until 15 March 2022. In addition to these searching databases, the reference lists of relevant articles were manually searched. PubMed database was searched using the search term ((Mental health symptoms [MeSH Terms]) OR (negative mental outcomes) OR (Depression) OR (depressive symptoms) OR (anxiety) OR (anxiety symptoms) OR (Anxiety disorders) OR (panic attack) OR (stress)) AND ((healthcare workers) [MeSH Terms]) OR (healthcare professionals)) AND (corona-virus disease 2019) [MeSH Terms]) OR (COVID-19) OR COVID-19 pandemic)) AND Ethiopia. Again, Medline and ScienceDirect databases were searched using similar search terms as applied in PubMed. Google Scholar was also searched for gray literature and published paper in unindexed journals.
Selection of the studies
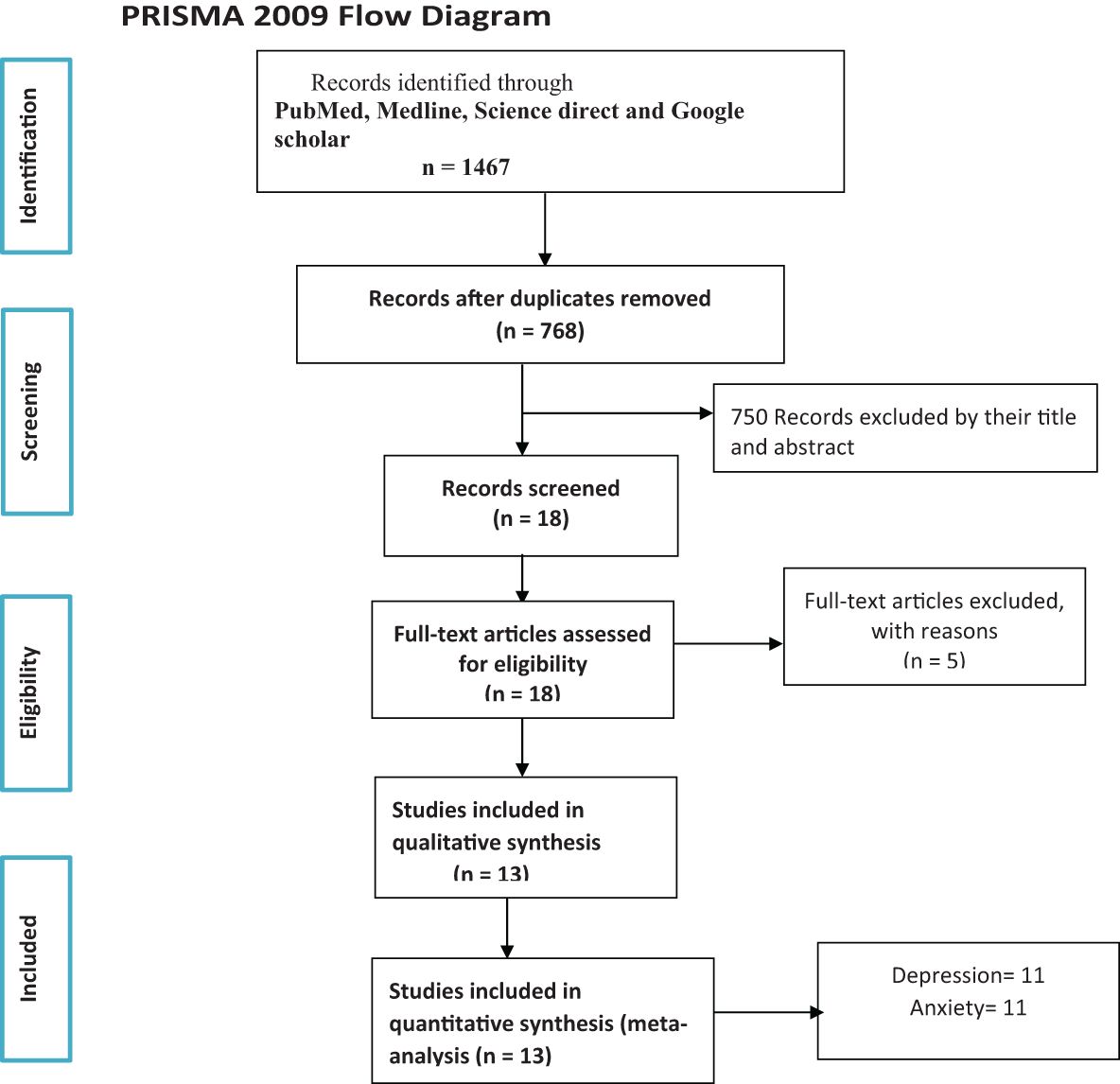
Two blinded researchers (TK and MM) searched for the published articles. All citations (N = 13) identified in the search process using their titles and abstracts were imported into Endnote X7.8 reference management software. This software was also used to eliminate any duplicates. Wherever there was a disagreement of relevancy of the included studies during the review, the reviewers have discussed together to reach consensus. A flow diagram (Figure 1) was used to show the included studies.
Definition of the variables
In this review, depression was a variable that was assessed using the validated standardized screening tools on the Ethiopian HCWs during COVID-19 pandemic. The tools used for measurement of depression in the included studies were the Depression, Anxiety and Stress Scale–21 (DASS-21) scale (30, 31) and Patient Health Questionnaire 9 (PHQ-9) (32). In addition, anxiety was also an outcome variable that was measured using DASS-21 (30, 31) and the seven-item Generalized Anxiety Disorder–7 (GAD-7) (33) in the included studies.
Eligibility criteria
The studies fulfilling the following criteria were included for the review: cross-sectional studies that assess one or more mental health symptoms (depression and anxiety) due to the current COVID-19 pandemic; the articles published in English language; and the studies interested on data of the Ethiopian HCWs. The articles with the unclear outcome of interest, case reports, reviews, and qualitative studies were excluded. The Joanna Briggs Institute study quality checker was used to evaluate the quality of the paper included (34). A quality appraisal criterion was used to check studies conducted by using cross-sectional research and prevalence data. The final reviewed paper was five or above out of a total of nine rating scales. This quality appraisal score was assessed by two investigators (TK and MM), and disagreements were solved by discussion.
Data extraction and synthesis
The required data of the included articles were extracted by using a structured and customized data abstraction sheet and stored in a Microsoft Excel spreadsheet. The data were extracted by two independent researchers (TK and DA) and checked for accuracy by the two independent reviewers and by MW and WM as a mediator. The extracted data include the author’s name, year of publication, study area, study design, aims, sample size, methods of data collection, primary outcomes (depression and anxiety), and their correlates. Magnitude of depression and anxiety symptoms amid COVID-19 and the associated factors with 95% confidence intervals (CIs) were also extracted. A narrative synthesis was employed to describe the studies design, implementation, and findings.
Data processing and analysis
The extracted data were entered into Microsoft Excel and then exported to STATA version 14 for further analysis. Random-effects model meta-analysis was used to estimate the pooled effect size and the effect of each study with their 95% CI. A forest plot was used to determine the pooled effect size and magnitude of each recruited study with 95% CI to indicate a graphic summary of the data. The index of heterogeneity (I2 statistics) was used to measure the degree of heterogeneity among the included studies (35). The potential sources of heterogeneity were identified through subgroup analysis by (region, study setting, and measurement tool), and a sensitivity analysis was also conducted to determine the potential source of heterogeneity. Funnel plot analysis and Egger-weighted regression tests were conducted to detect the presence of publication bias. P-value < 0.05 in Egger’s test was considered evidence of statistically significant publication bias (36, 37).
Results
Search results
The articles were searched from PubMed, Medline, ScienceDirect, and Google Scholar. From the searching databases, 1,467 articles were found initially. A total of 699 articles were removed because of duplication; later, 768 articles were left. After seeing their titles and abstracts, 750 articles were removed. Therefore, only 18 articles underwent a full-text review. Finally, we included 13 articles that fulfilled the inclusion criteria to conduct this systematic review and meta-analysis, whereas five studies were excluded from the review as they did not satisfy the eligibility criteria (Figure 1).
Characteristics of the included studies
After screening, 13 studies (13, 14, 38–48) with a total of 5,174 participants were included in the analysis. All of the studies were cross-sectional and reported on the prevalence and/or associated factors of depression and anxiety disorders on the Ethiopian HCWs during the COVID-19 pandemic. From the included studies, 11 studies that assessed depression and/or associated factors were included in this systematic review and meta-analysis (Table 2). Similarly, 11 studies that assessed the anxiety disorders and/or the associated factors were included in this systematic review and meta-analysis as indicated in Table 1. Nine of the studies assessed the outcome variable with a self-administered questionnaire, two studies with a face-to-face interview, and two studies using an online survey method of data collection. PHQ-9 (13, 39, 41, 43, 46) and DASS-21 (14, 40, 42, 44, 45, 47) were the frequently used tools for the screening of depression. On the other hand, GAD-7 (13, 38, 39, 43, 46, 48) and DASS-21 (14, 40, 44, 45, 47) were the two most common assessment instruments for the assessment of anxiety.
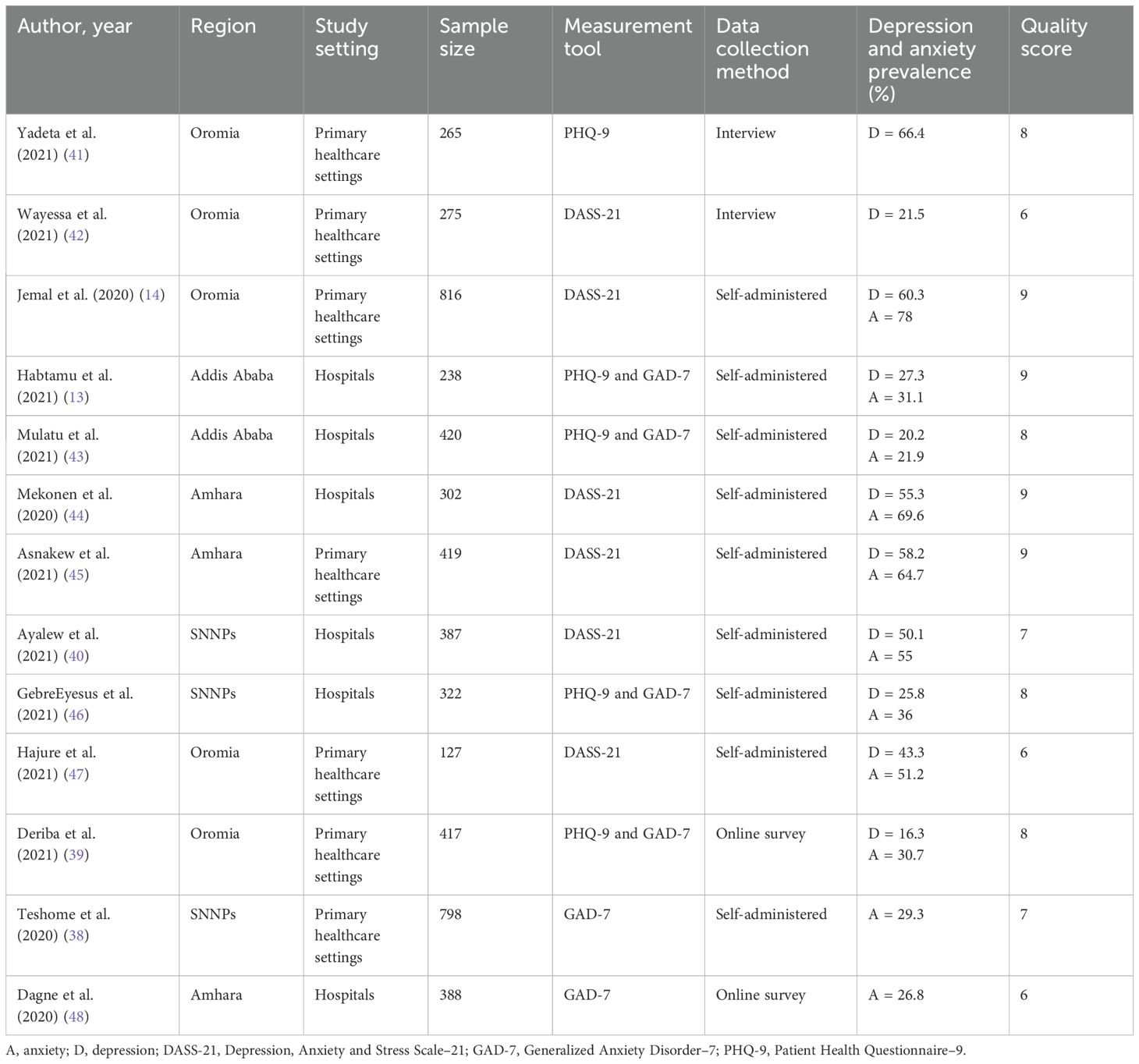
Table 1. Characteristics of the included studies on depression and anxiety disorders amid COVID-19 pandemic on the Ethiopian healthcare workers.
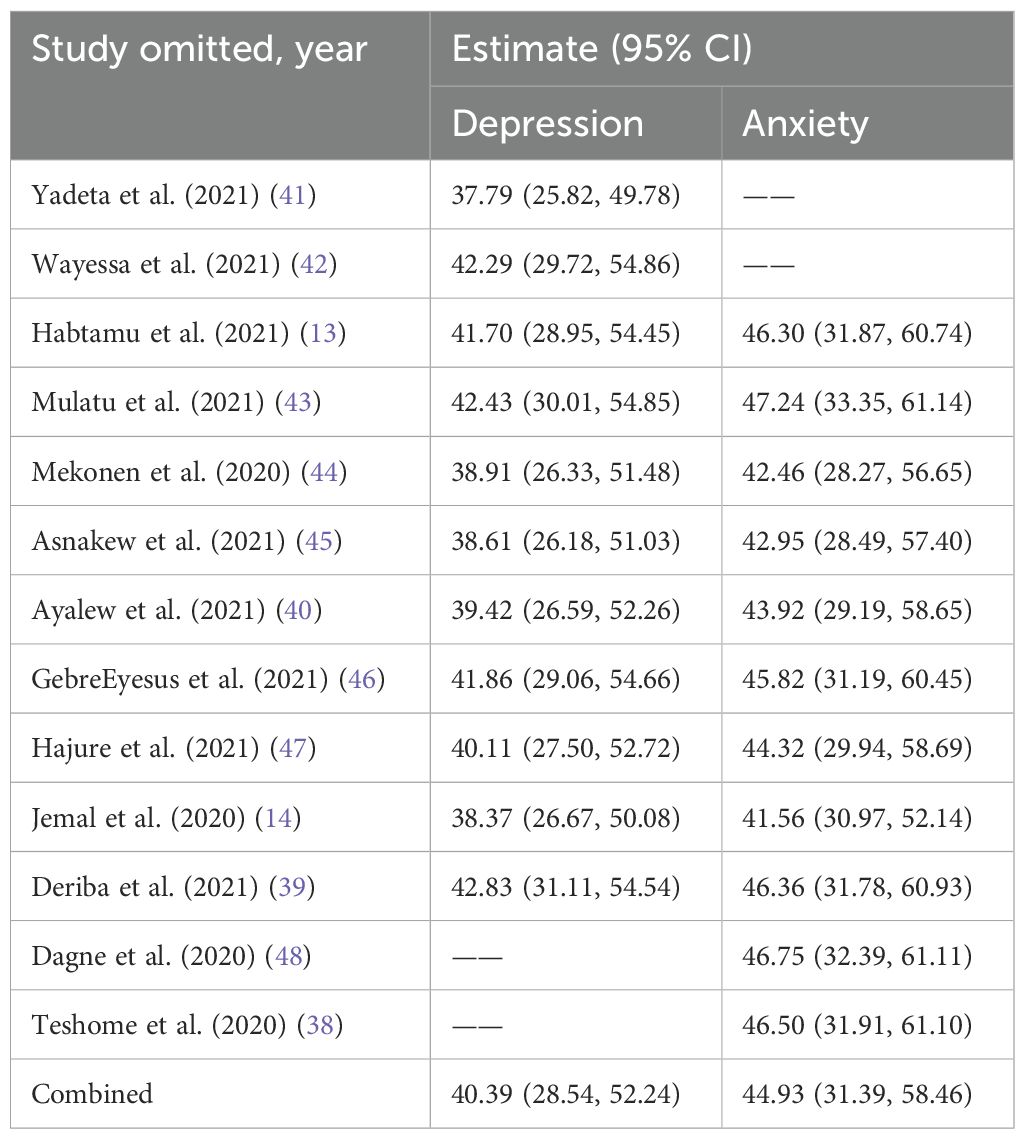
Table 2. Sensitivity analysis on prevalence of depression and anxiety in HCWs during COVID-19 pandemic in Ethiopia.
A summary of the characteristics of the included studies based on the author’s name and year of publication, region, study setting, sample size, measurement tool, methods of data collection, and main findings is provided in Table 1.
The prevalence of depression
In the 11 included studies, the pooled prevalence of depression in HCWs during COVID-19 pandemic was 40.39% (95% CI: 28.54, 52.24) as indicated in Figure 4. There was a significant level of heterogeneity among the included studies (I2 = 9 8.6%, p ≤ 0.001) (Figure 2). A sensitivity analysis was performed by omitting each study individually to see whether each one affected the average prevalence because of the significant level of heterogeneity of the meta-analysis. This illustrates that the omission of any one of the studies from this systematic review and meta-analysis does not change the overall pooled prevalence of depression, as all point values are within the overall 95% CI (Table 2).
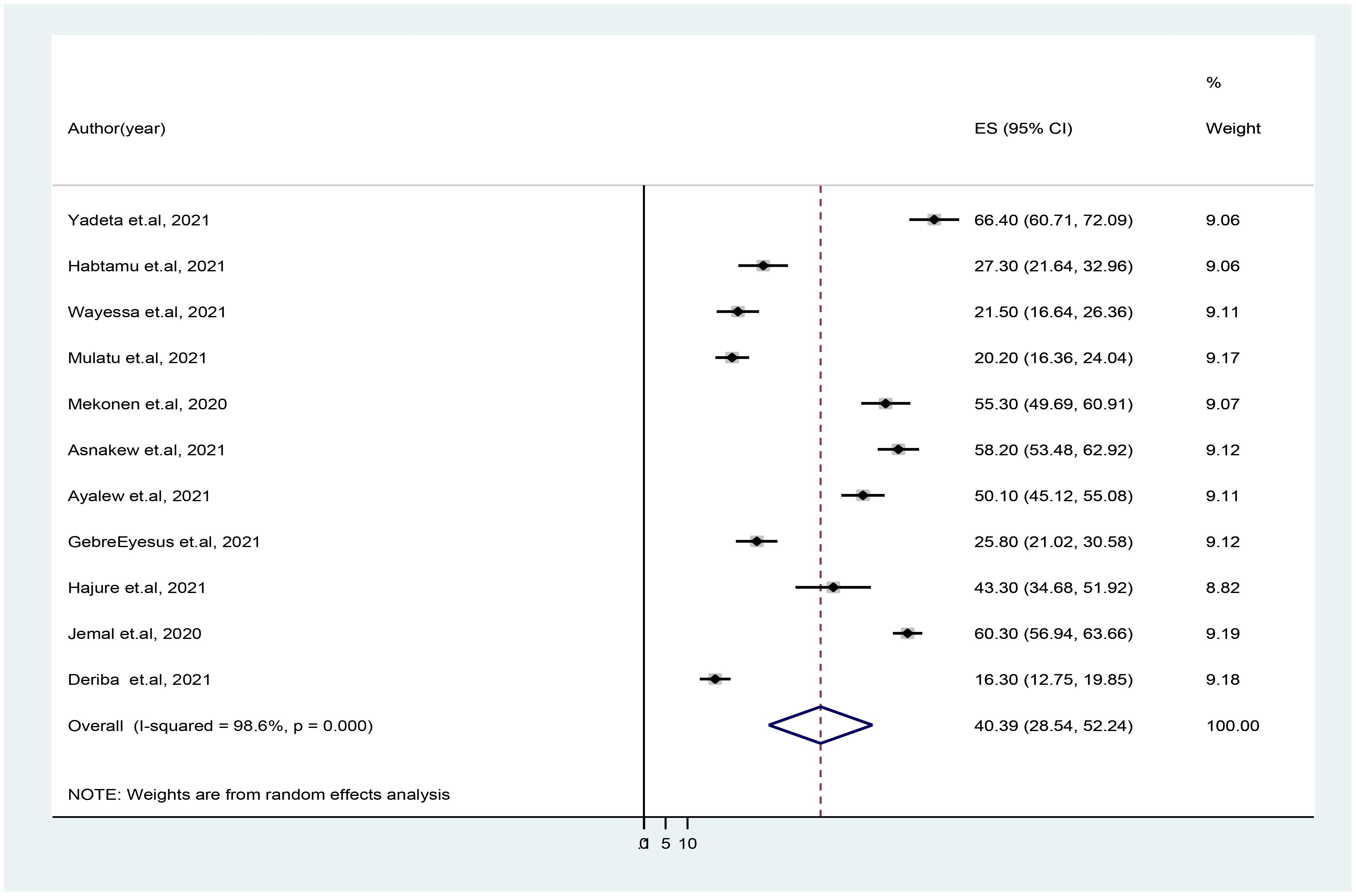
Figure 2. Forest plot showing the pooled prevalence of depression in healthcare workers during COVID-19 pandemic in Ethiopia. Note: The midpoint and the length of each segment indicate prevalence and a 95% confidence interval (CI), whereas the diamond shape shows the combined prevalence of all studies.
A subgroup analysis by region, measurement tool, and study setting was performed to identify the source of heterogeneity. Accordingly, five studies were conducted in Oromia region, and the pooled prevalence of depression in these studies was 41.53% (95% CI: 19.57, 63.49, I2 = 99.1%). The prevalence of depression was higher in studies conducted at the primary healthcare settings (44.31%) than that in studies conducted at referral and/or specialized hospitals (35.69%). Furthermore, the average prevalence of depression of HCWs amid COVID-19 was 48.18%, as it is measured by using DASS-21 measurement tool. The level of heterogeneity among studies included in each subgroup analysis was high (p < 0.05), except that among the studies conducted in Amhara region as illustrated in Table 3. The funnel plot test is symmetric (Figure 3), and the Eggers test for publication bias was insignificant [B = 5.91 (95% CI: −19.74, 31.56), SE = 11.34, and P = 0.62], illustrating that there was no evidence of publication bias for the prevalence of depression.
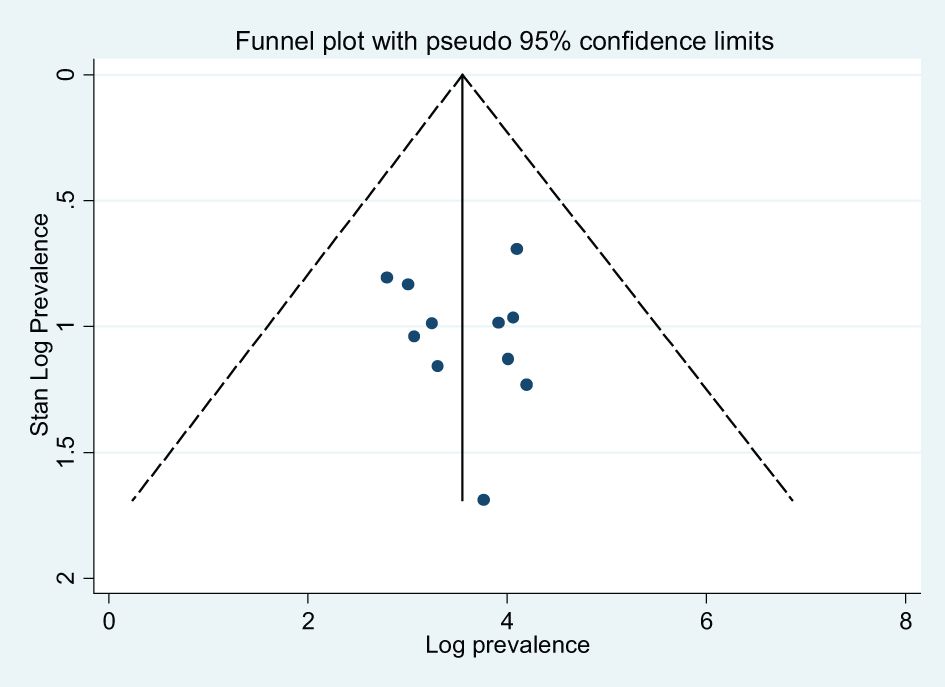
Figure 3. Funnel plots for publication bias of the studies that were included in the prevalence of depression in Ethiopia.
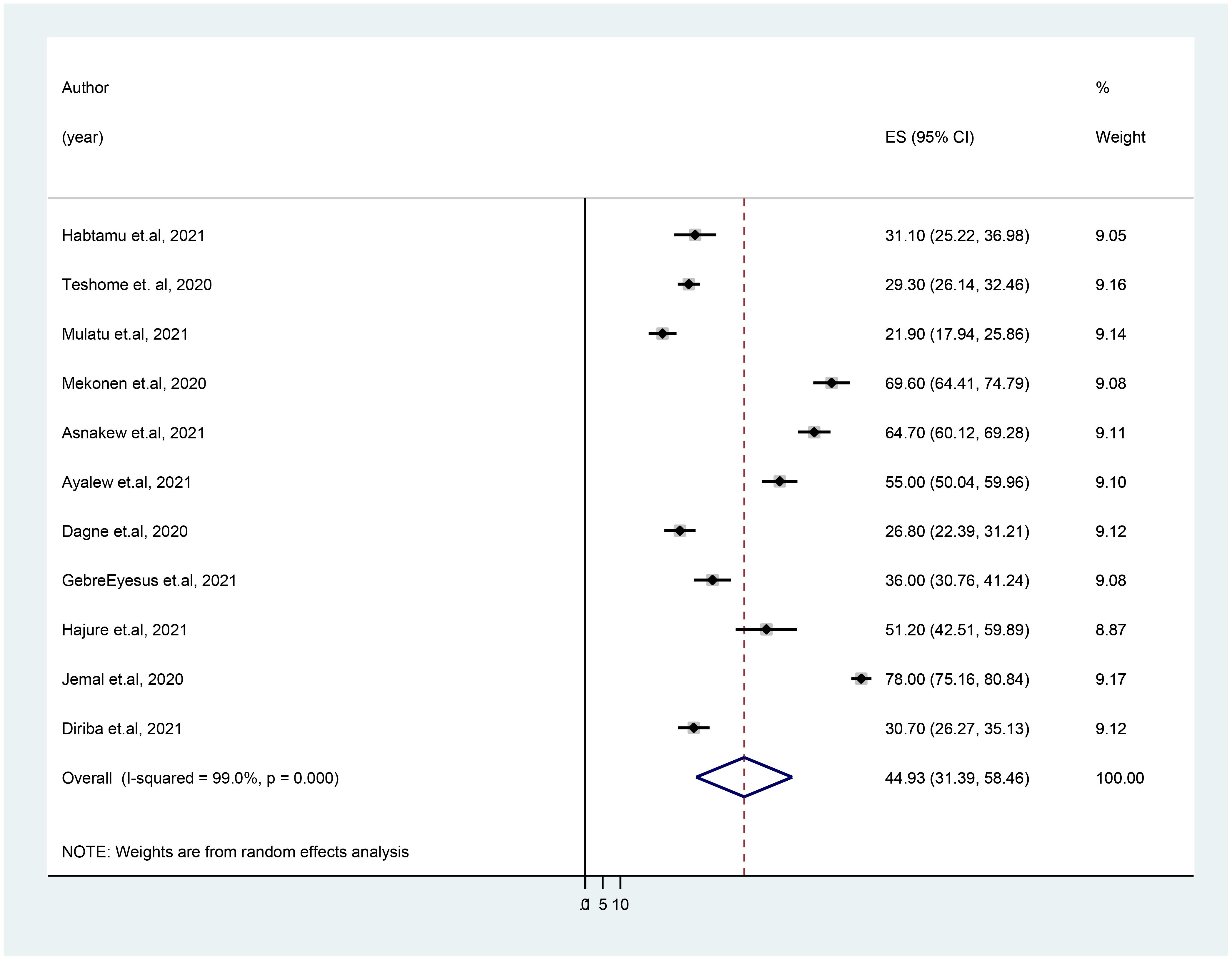
Figure 4. Forest plot showing the pooled prevalence of anxiety disorder in healthcare workers during COVID-19 pandemic in Ethiopia.
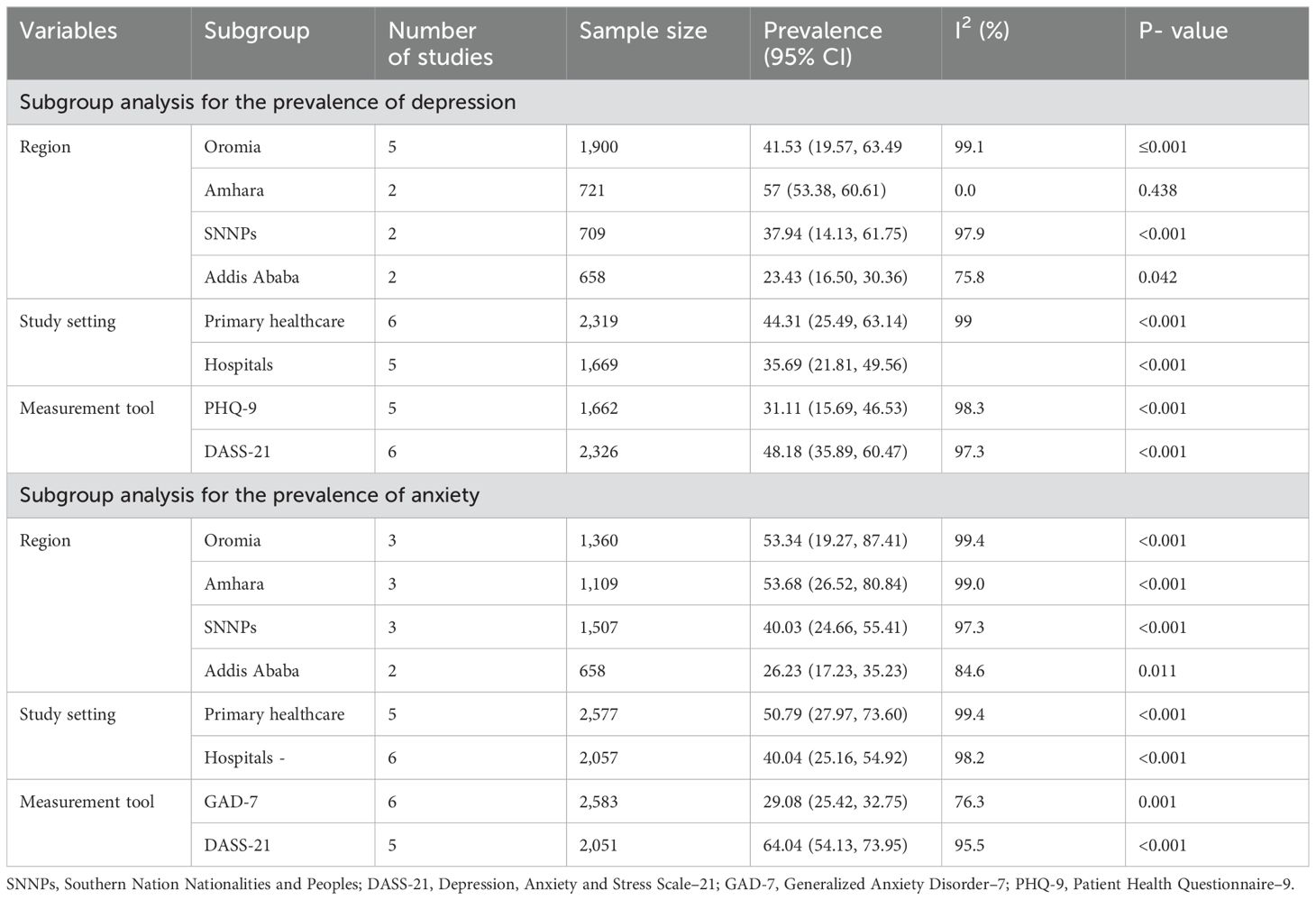
Table 3. The subgroup analysis on the prevalence of depressive and anxiety disorders in HCWs during COVID-19 in Ethiopia.
The prevalence of anxiety disorder
Figure 4 shows that, among Ethiopian healthcare professionals during the COVID-19 pandemic, the pooled prevalence of anxiety disorder was 44.93% (95% CI: 31.39, 58.46) across the 11 studies that were included. This meta-analysis revealed heterogeneity (I2 = 98.6%, p = 0.001); as a result, a sensitivity analysis was carried out by omitting each study independently to determine whether doing so had an impact on the average prevalence. This illustrates that the omission of any one of the studies from this systematic review and meta-analysis does not influence the overall pooled prevalence of anxiety disorder, as all point values are within the overall 95% CI (Table 2).
A subgroup analysis by region, study setting, and measurement tool was performed to identify the source of heterogeneity. Accordingly, the pooled prevalence of anxiety disorder in the Amhara region studies was 53.68% (95% CI: 26.52, 80.84), whereas, in Addis Ababa, it was 26.23% (95% CI: 17.23, 35.23). The prevalence of anxiety disorder was higher in studies conducted at the primary health settings (health centers and primary hospitals) (50.79%) than that in studies conducted at referral and specialized hospitals (40.04%). Furthermore, the average prevalence of anxiety disorder in HCWs amid COVID-19 was 64.04% as measured by using the DASS-21 measurement tool. The level of heterogeneity among studies included in each subgroup analysis was high (p < 0.01) as illustrated in Table 3. The funnel plot test is symmetric (Figure 5), and the Eggers test for publication bias was insignificant [B = −7.19 (95% CI: −34.01, 19.62), SE = 11.83, and P = 0.56], indicating that there was no evidence of publication bias for the prevalence of anxiety symptoms.
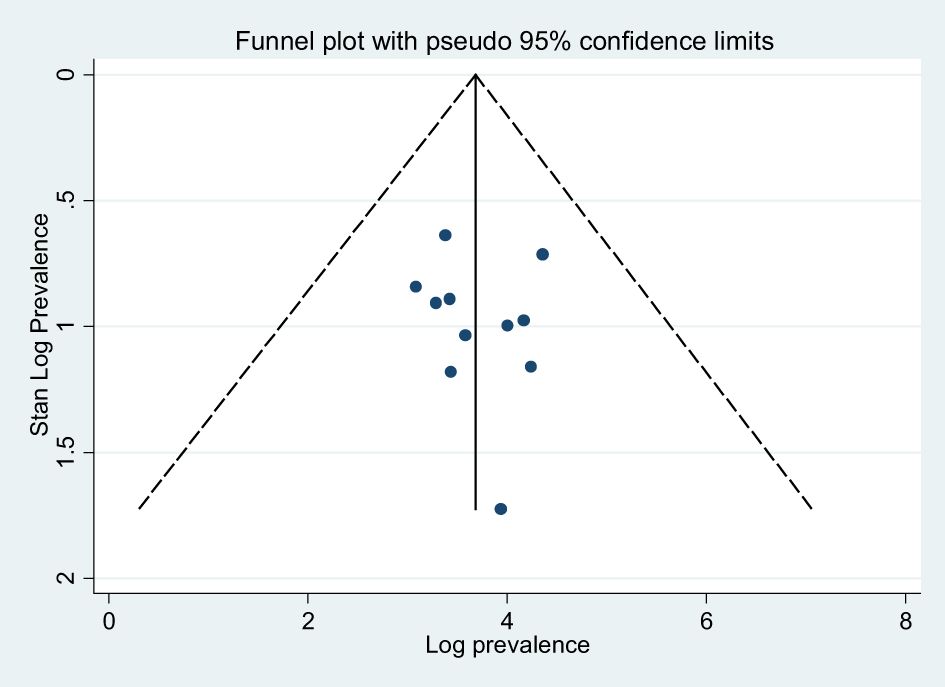
Figure 5. Funnel plots for publication bias of the studies that were included in the prevalence of disorder in Ethiopia.
Factors associated with depressive and anxiety disorders
In this meta-analysis study, five factors (being a woman, being married, working in the frontline, having high perceived susceptibility, and having poor social support) and four factors (being a woman, being older in age, working in the frontline, and having high perceived susceptibility) were extracted to evaluate the determinant factors with depression and anxiety, respectively. Female participants were 2.5 and 2.11 times more likely to have depressive and anxiety disorders than male participants [adjusted OR (AOR) = 2.50 (95% CI: 1.89–3.31)] and [AOR = 2.11 (95% CI: 1.69–2.64)], respectively. Participants who worked at the frontline during COVID-19 were 2.22 and 2.84 times more likely to have depressive and anxiety symptoms than participants who work other than frontline healthcare activities [AOR = 2.22 (95% CI: 1.57–3.15) and AOR = 2.84 (95% CI: 2.19–3.69)], respectively. The odds of depressive and anxiety disorders, respectively, were 3.25 and 2.34 times higher among HCWs with high perceived susceptibility to COVID-19 infection than those with low perceived susceptibility. Furthermore, the odds of depressive disorder was three times higher among married participants than unmarried HCWs [AOR = 3.02 (95% CI: 2.19–4.16)], and older participants [AOR = 3.87 (95% CI: 1.72–8.71)] were significantly more likely to have anxiety disorder amid COVID-19 pandemic than young HCWs (Table 4).
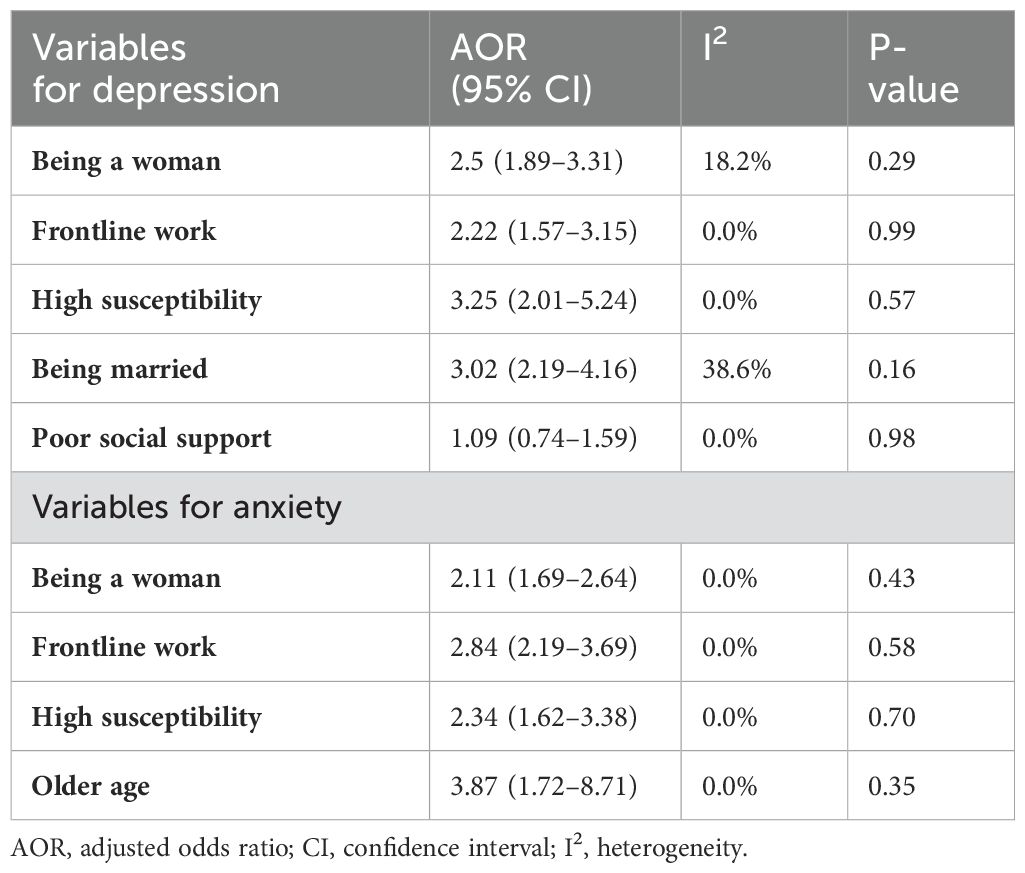
Table 4. Odds ratio of factors associated with depressive and anxiety disorders in Ethiopian healthcare workers amid COVID-19.
Discussion
The current review is the first quantitative epidemiological review of depression and anxiety disorders among HCWs during the COVID-19 pandemic in Ethiopia. We systematically identified 13 cross-sectional studies and quantitatively synthesized the pooled prevalence of depressive and anxiety symptoms. The overall prevalence of depression and anxiety was 40.39% and 44.93%, respectively. This study confirmed the presence of a high prevalence of depression and anxiety problems among HCWs in Ethiopia. It is common to observe higher mental health problems in healthcare providers due to the widespread occurrence of COVID-19 pandemic and increased number of cases and deaths and more vulnerable to becoming infected or even transmitting the disease to their family members (49–53). This study’s value for the prevalence of anxiety and depressive disorders was in line with other reviews and meta-analyses. For instance, according to a review by Hossain et al. (2021), during the COVID-19 pandemic, the prevalence of depression and anxiety disorders among HCWs was higher in Pakistan (depression, 41.6%; and anxiety, 50.4%) and Bangladesh (depression, 48.2%; and anxiety, 43.6%) (54). Similarly, the global estimated prevalence of depression and anxiety disorders among HCWs was predicted to be 37% and 40%, respectively, according to the review and meta-analysis by Saragih et al. (2021) (55). The prevalence of depression and anxiety among nurses was also reported by Al Maqbali et al. (2021) to be 35% and 37%, respectively (56).
The estimated prevalence of depression and anxiety disorders in this study was higher than that in the earlier review and meta-analysis conducted in high resources settings. For example, in a review and meta-analysis done by Pappa et al. (2020) on healthcare professionals, the estimated prevalence of depression and anxiety was 22.8% and 23.2%, respectively (57). The findings in this study are also higher than those in the recently published meta-analysis findings, with the estimated prevalence of depression of 21.7% (58), 24% (59), 26% (60), and 24.83% (61), in which most of the participants were from high-resource settings. Furthermore, the estimated prevalence of anxiety in this study also is higher than that in the earlier published meta-analysis findings with the estimated prevalence ranging from 22.1% to 30% (58, 61–63).
The possible reason for these different prevalences might be due to the dissimilarities in infrastructural facilities of healthcare systems and the level of attention given to the mental wellbeing of HCWs by policymakers and health authorities. This variation may be due to the difference in study period. The earlier review and meat-analyses were done in the early period of the COVID-19 pandemic during which there were limited studies in the low-resource settings (53). A variety of rating scales used the studies are the other possible reason for the source of variability among study findings. It is evident by the results of the subgroup analysis that the prevalence of depression and anxiety disorders in studies measured via DASS-21 (48.18% and 64.04%, respectively) was higher than those measured using PHQ-9 and GAD-7 scales. The variation in sensitivity and specificity of the rating scales to screen out depression and anxiety could be responsible for this. On the other hand, an increasing trend of infected and hospitalized patients leads to a heavier workload, threatening the mental health of the Ethiopian HCWs. Furthermore, the shortage of personal protective equipment frequently reported in the low-resource settings like Ethiopia can increase the mental health impacts and lead to stress reactions of HCWs during the COVID-19 pandemic (64, 65). This indicates the importance of empowering healthcare professionals to successfully deal with the emotions rising from such difficult circumstances.
The HCWs in Addis Ababa had a lower prevalence of both conditions (depression, 23.43%; and anxiety, 26.23%) compared to those studies held in other regions of the country in this review and meta-analysis. For instance, the HCWs in Amhara region had a higher prevalence of both conditions (depression, 57%; and anxiety, 53.68%) compared to those in Addis Ababa (depression, 23.43%; and anxiety, 26.23%). The possible explanation for this epidemiological variation of depression and anxiety disorders across regions may be attributed to the variation in personal protective equipment, workload related to increased infected and hospitalized cases, and concept of the illness (66, 67). There were limited infrastructural facilities of healthcare system in other regions than that in Addis Ababa during the earlier period of the pandemic. Moreover, the average prevalence of depression and anxiety of HCWs was higher (44.31% and 50.79%, respectively) in the studies held in the primary healthcare settings than those done in hospitals.
Our review suggested that being a woman is the determinant factor for depression and anxiety disorders among HCWs during COVID-19. This finding is in line with other systematic review and meta-analysis studies (68–70). In another study by Han et al. (2020) on HCWs, the estimated prevalence of depression in women was higher than that in men (71). A possible reason might be the greater number of female workers employed globally in lower status roles within healthcare systems, which put them in greater risk of exposure to patients with COVID-19 and bring negative outcomes on mental wellbeing (60). Women are more burdened with different tasks of giving care in the office and at home than men, which brings mental health impact related to the COVID pandemic (70). It is also the fact that women had negative feeling and emotion and that the effect of hormonal difference could contribute a great role for the adverse effects of mental wellbeing (69, 72).
Being older in age was the potential risk factor for anxiety disorders among HCWs during COVID-19. Previous studies also affirmed that older-aged HCWs had the greatest anxiety disorders due to considerable changes in physical health and their responsibilities of taking care of family members and organizing their work affairs (73, 74). The other associated factor with depression in HCWs at the time of the COVID pandemic is being married. This finding is consistent with other studies in China (75, 76). The possible explanation could be the fear of contaminating and loss their loved ones due to the pandemic and separation from the family members (77, 78).
Furthermore, frontline work and high perceived susceptibility to COVID-19 infection were significant risk factors for depression and anxiety disorders among health workers. Because they are the initial point of contact in the diagnosis, treatment, and care of patients with COVID-19, HCWs are at risk for acquiring depression and anxiety (10, 11). The frontline HCW may be more susceptible to depression and anxiety disorders due to exposure to unpredictable daily caseloads, the burden of making decisions, many deaths, bans on family visits, and ongoing changes to clinical guidelines (62). This might be due to the lack of personal protective equipment, the fear of being infected or infecting family members, having chronic medical condition, contact with infected person, and feeling of helplessness that can render the work environment dangerous, leading to a feeling of insecurity and vulnerability to the infection that could have a mental health impact on HCWs (79–81). This demonstrated the necessity of providing healthcare personnel with proper personal protection equipment and psychosocial support to improve their mental wellbeing.
Limitations
This review and meta-analysis has some limitations. First, the current research did not include mental disorders other than depression and anxiety, such as distress, trauma, and sleep disorders, which limited our findings. Second, the studies included in this review were cross-sectional studies that could not show the causal relationship of the potential risk factors with depression and anxiety disorders. Furthermore, using the broad phrase “healthcare worker” prevents us from drawing conclusions about particular occupations like that of a doctor or nurse.
Conclusion
Our study revealed that the prevalence of depression and anxiety disorders in Ethiopian HCWs was high. Being a woman, being married, being older in age, working in the frontline, and having high perceived susceptibility were the factors associated with depressive and anxiety disorders amid COVID-19 pandemic in HCWs. Findings also provided health policymaker’s evidence-based information to improve the mental health of HCWs through earlier detection of high-risk groups based on their demographic and working characteristics, as well as the provision of emotional support programs. The timely detection and appropriate management of mental health problems is essential for the quality of healthcare services, and proactive support methods for the female, married, and older-age healthcare professionals could result in these outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
DA: Writing – review & editing, Writing – original draft, Methodology, Formal analysis, Data curation, Conceptualization. TK: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. MM: Writing – review & editing, Writing – original draft, Methodology, Investigation, Formal analysis, Data curation, Conceptualization. MW: Writing – original draft, Methodology, Data curation, Conceptualization. WM: Writing – original draft, Methodology, Data curation, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1342002/full#supplementary-material
Abbreviations
AOR, adjusted odd ratio; COVID-19, Coronavirus disease 2019; HCWs, healthcare workers; SNNPs, South Nation Nationality and Peoples; DASS-21, Depression, Anxiety and Stress Scale–21; GAD-7, Generalized Anxiety Disorder–7; PHQ-9, Patient Health Questionnaire–9; WHO, World Health Organization.
References
1. Zhu N, Zhang D, Wang W, China Novel Coronavirus Investigating and Research Team. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:(8). doi: 10.1056/NEJMoa2001017
2. Organization WH. Mental health and psychosocial considerations during the COVID-19 outbreak. Geneva: WHO (2020).
3. Munster VJ, Koopmans M, van Doremalen N, van Riel D, de Wit E. A novel coronavirus emerging in China—key questions for impact assessment. New Engl J Med. (2020) 382:692–4. doi: 10.1056/NEJMp2000929
4. Worldometer. COVID-19 CORONAVIRUS / DEATH TOLL (2020). Available online at: https://www.worldometers.info/coronavirus/coronavirus-death-toll/.
5. Kebede Y, Birhanu Z. Myths, beliefs, and perceptions about COVID-19 in Ethiopia: A need to address information gaps and enable combating efforts. Plos One (2020) 15(11):e0243024. doi: 10.1371/journal.pone.0243024
6. Schäfer SK, Sopp MR, Schanz CG, Staginnus M, Göritz AS, Michael T. Impact of COVID-19 on public mental health and the buffering effect of a sense of coherence. Psychother Psychosomatics. (2020) 89:386–92. doi: 10.1159/000510752
7. Ahorsu DK, Lin C-Y, Pakpour AH. The association between health status and insomnia, mental health, and preventive behaviors: the mediating role of fear of COVID-19. Gerontology Geriatric Med. (2020) 6:2333721420966081. doi: 10.1177/2333721420966081
8. Kang L, Ma S, Chen M, Yang J, Wang Y, Li R, et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behavior Immunity. (2020) 87:11–7. doi: 10.1016/j.bbi.2020.03.028
9. Yu H, Li M, Li Z, Xiang W, Yuan Y, Liu Y, et al. Coping style, social support and psychological distress in the general Chinese population in the early stages of the COVID-19 epidemic. BMC Psychiatry. (2020) 20:1–11. doi: 10.1186/s12888-020-02826-3
10. Bekele F, Hajure M. Magnitude and determinants of the psychological impact of COVID-19 among health care workers: A systematic review. SAGE Open Med. (2021) 9:20503121211012512. doi: 10.1177/20503121211012512
11. Bekele M, Getnet M, Getachew A, Shewamene Z, Abraha M, Simegn W. Depression, anxiety, stress and their associated factors among Ethiopian University students during an early stage of COVID-19 pandemic: An online-based cross-sectional survey. PloS One. (2021) 16:e0251670. doi: 10.1371/journal.pone.0251670
12. Krishnamoorthy Y, Nagarajan R, Saya GK, Menon V. Prevalence of psychological morbidities among general population, healthcare workers and COVID-19 patients amidst the COVID-19 pandemic: A systematic review and meta-analysis. Psychiatry Res. (2020) 293:113382. doi: 10.1016/j.psychres.2020.113382
13. Habtamu Y, Admasu K, Tullu M, Damene W, Birhanu A, Beyero T, et al. Mental Health Outcomes among Frontline Health-Care Workers at Eka Kotebe National COVID-19 Treatment Center, Addis Ababa, Ethiopia, 2020: A Cross-Sectional Study. Neuropsychiatr Dis Treat. (2021) 17:2831–40. doi: 10.2147/NDT.S311949
14. Jemal K, Deriba BS, Geleta TA, Tesema M, Awol M, Mengistu E, et al. Self-reported symptoms of depression, anxiety, and stress among healthcare workers in Ethiopia during the COVID-19 pandemic: A cross-sectional study. Neuropsychiatr Dis Treat. (2021) 17:1363. doi: 10.2147/NDT.S306240
15. Tan BY, Chew NW, Lee GK, Jing M, Goh Y, Yeo LL, et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Internal Med. (2020) 173:317–20. doi: 10.7326/M20-1083
16. Shaukat N, Ali DM, Razzak J. Physical and mental health impacts of COVID-19 on healthcare workers: a scoping review. Int J Emergency Med. (2020) 13:1–8. doi: 10.1186/s12245-020-00299-5
17. de Pablo GS, Vaquerizo-Serrano J, Catalan A, Arango C, Moreno C, Ferre F, et al. Impact of coronavirus syndromes on physical and mental health of health care workers: Systematic review and meta-analysis. J Affect Disord. (2020) 275:48–57. doi: 10.1016/j.jad.2020.06.022
18. Sharma R, Saxena A, Magoon R, Jain MK. A cross-sectional analysis of prevalence and factors related to depression, anxiety, and stress in health care workers amidst the COVID-19 pandemic. Indian J Anaesthesia. (2020) 64:S242. doi: 10.4103/ija.IJA_417_19
19. Agberotimi SF, Akinsola OS, Oguntayo R, Olaseni AO. Interactions between socioeconomic status and mental health outcomes in the Nigerian context amid COVID-19 pandemic: a comparative study. Front Psychol. (2020) 11. 2655. doi: 10.3389/fpsyg.2020.559819
20. Khanal P, Devkota N, Dahal M, Paudel K, Joshi D. Mental health impacts among health workers during COVID-19 in a low resource setting: a cross-sectional survey from Nepal. Globalization Health. (2020) 16:1–12. doi: 10.1186/s12992-020-00621-z
21. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public–A systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
22. Venema TA, Pfattheicher S. Perceived susceptibility to COVID-19 infection and narcissistic traits. Pers Individ Differences. (2021) 175:110696. doi: 10.1016/j.paid.2021.110696
23. Chew NW, Lee GK, Tan BY, Jing M, Goh Y, Ngiam NJ, et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behavior Immunity. (2020) 88:559–65. doi: 10.1016/j.bbi.2020.04.049
24. Inbar L, Shinan-Altman S. Emotional reactions and subjective health status during the COVID-19 pandemic in Israel: the mediating role of perceived susceptibility. Psychology Health Med. (2021) 26:75–84. doi: 10.1080/13548506.2020.1858490
25. Zhou J, Liu L, Xue P, Yang X, Tang X. Mental health response to the COVID-19 outbreak in China. Am J Psychiatry. (2020) 177:574–5. doi: 10.1176/appi.ajp.2020.20030304
26. Usher K, Durkin J, Bhullar N. The COVID-19 pandemic and mental health impacts. Int J Ment Health Nursing. (2020) 29:315. doi: 10.1111/inm.12726
27. She R, Wang X, Zhang Z, Li J, Xu J, You H, et al. Mental health help-seeking and associated factors among public health workers during the COVID-19 outbreak in China. Front Public Health. (2021) 9. doi: 10.3389/fpubh.2021.622677
28. Sun Y, Song H, Liu H, Mao F, Sun X, Cao F. Occupational stress, mental health, and self-efficacy among community mental health workers: a cross-sectional study during COVID-19 pandemic. Int J Soc Psychiatry. (2021) 67:737–46. doi: 10.1177/0020764020972131
29. Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Reprint—preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Phys Ther. (2009) 89:873–80. doi: 10.1093/ptj/89.9.873
30. Bottesi G, Ghisi M, Altoè G, Conforti E, Melli G, Sica C. The Italian version of the Depression Anxiety Stress Scales-21: Factor structure and psychometric properties on community and clinical samples. Compr Psychiatry. (2015) 60:170–81. doi: 10.1016/j.comppsych.2015.04.005
31. Chan RC, Xu T, Huang J, Wang Y, Zhao Q, Shum DH, et al. Extending the utility of the Depression Anxiety Stress scale by examining its psychometric properties in Chinese settings. Psychiatry Res. (2012) 200:879–83. doi: 10.1016/j.psychres.2012.06.041
32. Manea L, Gilbody S, McMillan D. A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. Gen Hosp Psychiatry. (2015) 37:67–75. doi: 10.1016/j.genhosppsych.2014.09.009
33. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Internal Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
34. Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evidence-Based Healthcare. (2015) 13:147–53. doi: 10.1097/XEB.0000000000000054
35. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58. doi: 10.1002/sim.1186
36. Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
37. Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. (2001) 54:1046–55. doi: 10.1016/S0895-4356(01)00377-8
38. Teshome A, Glagn M, Shegaze M, Tekabe B, Getie A, Assefa G, et al. Generalized anxiety disorder and its associated factors among health care workers fighting COVID-19 in Southern Ethiopia. Psychol Res Behav Management. (2020) 13:907. doi: 10.2147/PRBM.S282822
39. Jemal K, Deriba BS, Geleta TA. Psychological distress, early behavioral response, and perception toward the COVID-19 pandemic among health care workers in North Shoa zone, Oromiya region. Front Psychiatry. (2021) 12. doi: 10.3389/fpsyt.2021.628898
40. Ayalew M, Deribe B, Abraham Y, Reta Y, Tadesse F, Defar S, et al. Prevalence and determinant factors of mental health problems among healthcare professionals during COVID-19 pandemic in southern Ethiopia: multicentre cross-sectional study. BMJ Open. (2021) 11:e057708. doi: 10.1136/bmjopen-2021-057708
41. Yadeta TA, Dessie Y, Balis B. Magnitude and predictors of health care workers depression during the COVID-19 pandemic: health facility-based study in Eastern Ethiopia. Front Psychiatry. (2021) 12:654430. doi: 10.3389/fpsyt.2021.654430
42. Wayessa ZJ, Melesse GT, Amaje Hadona E, Wako WG. Prevalence of depressive symptoms due to COVID-19 and associated factors among healthcare workers in Southern Ethiopia. SAGE Open Med. (2021) 9:20503121211032810. doi: 10.1177/20503121211032810
43. Mulatu HA, Tesfaye M, Woldeyes E, Bayisa T, Fisseha H, Kassu RA. The prevalence of common mental disorders among healthcare professionals during the COVID-19 pandemic at a tertiary Hospital in Addis Ababa, Ethiopia. J Affect Disord Rep. (2021) 6:100246. doi: 10.1016/j.jadr.2021.100246
44. Mekonen E. The psychological impact of COVID-19 outbreak on nurses working in the northwest of Amhara Regional State referral hospitals, northwest Ethiopia. Infection Drug Resistance. (2020) 13:1353–64. doi: 10.2147/PRBM.S291446
45. Asnakew S, Amha H, Kassew T. Mental health adverse effects of COVID-19 pandemic on health care workers in North West Ethiopia: A multicenter cross-sectional study. Tylor and Francis (2021) 17:1375–84. doi: 10.2147/NDT.S306300
46. GebreEyesus FA, Tarekegn TT, Amlak BT, Shiferaw BZ, Emeria MS, Geleta OT, et al. Levels and predictors of anxiety, depression, and stress during COVID-19 pandemic among frontline healthcare providers in Gurage zonal public hospitals, Southwest Ethiopia, 2020: A multicenter cross-sectional study. PloS One. (2021) 16:e0259906. doi: 10.1371/journal.pone.0259906
47. Hajure M, Dibaba B, Shemsu S, Desalegn D, Reshad M, Mohammedhussein M. Psychological distress among health care workers in health facilities of mettu town during COVID-19 outbreak, South West Ethiopia, 2020. Front Psychiatry. (2021) 12:1049. doi: 10.3389/fpsyt.2021.574671
48. Dagne H, Atnafu A, Alemu K, Azale T, Yitayih S, Dagnew B, et al. Anxiety and associated factors among Ethiopian health professionals at early stage of COVID-19 pandemic in Ethiopia. PloS One. (2021) 16:e0252664. doi: 10.1371/journal.pone.0252664
49. Dimitriu MC, Pantea-Stoian A, Smaranda AC, Nica AA, Carap AC, Constantin VD, et al. Burnout syndrome in Romanian medical residents in time of the COVID-19 pandemic. Med Hypotheses. (2020) 144:109972. doi: 10.1016/j.mehy.2020.109972
50. Lian X, Huang J, Huang R, Liu C, Wang L, Zhang T. Impact of city lockdown on the air quality of COVID-19-hit of Wuhan city. Sci Total Environment. (2020) 742:140556. doi: 10.1016/j.scitotenv.2020.140556
51. Huang Y, Zhao N. Chinese mental health burden during the COVID-19 pandemic. Asian J Psychiatry. (2020) 51:102052. doi: 10.1016/j.ajp.2020.102052
52. Huang Y, Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: Who will be the high-risk group? Psychology Health Med. (2021) 26:23–34. doi: 10.1080/13548506.2020.1754438
53. Necho M, Tsehay M, Birkie M, Biset G, Tadesse E. Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Int J Soc Psychiatry. (2021) 67:892–906. doi: 10.1177/00207640211003121
54. Hossain MM, Rahman M, Trisha NF, Tasnim S, Nuzhath T, Hasan NT, et al. Prevalence of anxiety and depression in South Asia during COVID-19: a systematic review and meta-analysis. Heliyon. (2021) 7:e06677. doi: 10.1016/j.heliyon.2021.e06677
55. Saragih ID, Tonapa SI, Saragih IS, Advani S, Batubara SO, Suarilah I, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud. (2021) 121:104002. doi: 10.1016/j.ijnurstu.2021.104002
56. Al Maqbali M, Al Sinani M, Al-Lenjawi B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and meta-analysis. J Psychosomatic Res. (2021) 141:110343. doi: 10.1016/j.jpsychores.2020.110343
57. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behavior Immunity. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
58. Li Y, Scherer N, Felix L, Kuper H. Prevalence of depression, anxiety and post-traumatic stress disorder in health care workers during the COVID-19 pandemic: A systematic review and meta-analysis. PloS One. (2021) 16:e0246454. doi: 10.1371/journal.pone.0246454
59. Olaya B, Pérez-Moreno M, Bueno-Notivol J, Gracia-García P, Lasheras I, Santabárbara J. Prevalence of depression among healthcare workers during the COVID-19 outbreak: a systematic review and meta-analysis. J Clin Med. (2021) 10:3406. doi: 10.3390/jcm10153406
60. Rezaei S, Hoseinipalangi Z, Rafiei S, Dolati Y, Hosseinifard H, Asl MT, et al. The global Prevalence of Depression among Health Workers during the COVID-19 pandemic: a Systematic review and Meta-analysis. J Affect Disord Rep. (2022) 8:100326. doi: 10.1016/j.jadr.2022.100326
61. Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Prog Neuropsychopharmacol Biol Psychiatry. (2021) 107:110247. doi: 10.1016/j.pnpbp.2021.110247
62. Marvaldi M, Mallet J, Dubertret C, Moro MR, Guessoum SB. Anxiety, depression, trauma-related, and sleep disorders among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Neurosci Biobehav Rev. (2021) 126:252–64. doi: 10.1016/j.neubiorev.2021.03.024
63. Adibi A, Golitaleb M, Farrahi-Ashtiani I, Pirani D, Yousefi K, Jamshidbeigi Y, et al. The prevalence of generalized anxiety disorder among health care workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front Psychiatry. (2021) 12:658846. doi: 10.3389/fpsyt.2021.658846
64. Dai H, Zhang SX, Looi KH, Su R, Li J. Perception of health conditions and test availability as predictors of adults’ mental health during the COVID-19 pandemic: A survey study of adults in Malaysia. Int J Environ Res Public Health. (2020) 17:5498. doi: 10.3390/ijerph17155498
65. Cai Q, Feng H, Huang J, Wang M, Wang Q, Lu X, et al. The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. J Affect Disord. (2020) 275:210–5. doi: 10.1016/j.jad.2020.06.031
66. Deng Y, Chen Y, Zhang B. Different prevalence trend of depression and anxiety among healthcare workers and general public before and after the peak of COVID-19 occurred in China: A meta-analysis. Asian J Psychiatry. (2021) 56:102547. doi: 10.1016/j.ajp.2021.102547
67. Delgado D, Wyss Quintana F, Perez G, Sosa Liprandi A, Ponte-Negretti C, Mendoza I, et al. Personal safety during the COVID-19 pandemic: realities and perspectives of healthcare workers in Latin America. Int J Environ Res Public Health. (2020) 17:2798. doi: 10.3390/ijerph17082798
68. Bekele F, Mechessa DF, Sefera B. Prevalence and associated factors of the psychological impact of COVID-19 among communities, health care workers and patients in Ethiopia: A systematic review. Ann Med Surgery. (2021) 66:102403. doi: 10.1016/j.amsu.2021.102403
69. Wang Y, Kala MP, Jafar TH. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PloS One. (2020) 15:e0244630. doi: 10.1371/journal.pone.0244630
70. Elvira SD, Lamuri A, Lukman PR, Malik K, Shatri H, Abdullah M. Psychological distress among Greater Jakarta area residents during the COVID-19 pandemic and community containment. Heliyon. (2021) 7:e06289. doi: 10.1016/j.heliyon.2021.e06289
71. Han L, Wong FKY, She DLM, Li SY, Yang YF, Jiang MY, et al. Anxiety and depression of nurses in a north west province in China during the period of novel coronavirus pneumonia outbreak. J Nurs Scholarship. (2020) 52:564–73. doi: 10.1111/jnu.12590
72. Ching SM, Ng KY, Lee KW, Yee A, Lim PY, Ranita H, et al. Psychological distress among healthcare providers during COVID-19 in Asia: Systematic review and meta-analysis. PloS One. (2021) 16:e0257983. doi: 10.37766/inplasy2021.4.0043
73. Bailey L, Ward M, DiCosimo A, Baunta S, Cunningham C, Romero-Ortuno R, et al. Physical and mental health of older people while cocooning during the COVID-19 pandemic. QJM: Int J Med. (2021) 114:648–53. doi: 10.1093/qjmed/hcab015
74. Seid A, Metaferia Y. Factors associated with treatment delay among newly diagnosed tuberculosis patients in Dessie city and surroundings, Northern Central Ethiopia: a cross-sectional study. BMC Public Health. (2018) 18:1–13. doi: 10.1186/s12889-018-5823-9
75. Du J, Dong L, Wang T, Yuan C, Fu R, Zhang L, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen Hosp Psychiatry. (2020) 67:144. doi: 10.1016/j.genhosppsych.2020.03.011
76. Zhang H, Li W, Li H, Zhang C, Luo J, Zhu Y, et al. Prevalence and dynamic features of psychological issues among Chinese healthcare workers during the COVID-19 pandemic: a systematic review and cumulative meta-analysis. Gen Psychiatry. (2021) 34. doi: 10.1136/gpsych-2020-100344
77. Feng Z, Xu L, Cheng P, Zhang L, Li L-J, Li W-H. The psychological impact of COVID-19 on the families of first-line rescuers. Indian J Psychiatry. (2020) 62:S438. doi: 10.1002/wps.2076810.4103/psychiatry.IndianJPsychiatry_1057_20
78. Ghebreyesus TA. Addressing mental health needs: an integral part of COVID-19 response. World psychiatry: Off J World Psychiatr Assoc (WPA). (2020) 19:129. doi: 10.1002/wps.20768
79. Boyraz G, Legros DN, Tigershtrom A. COVID-19 and traumatic stress: The role of perceived vulnerability, COVID-19-related worries, and social isolation. J Anxiety Disord. (2020) 76:102307. doi: 10.1016/j.janxdis.2020.102307
80. Wang Y, Shi L, Que J, Lu Q, Liu L, Lu Z, et al. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol Psychiatry. (2021) 26:4813–22. doi: 10.1038/s41380-021-01019-y
Keywords: anxiety, depression, COVID-19 pandemic, meta-analysis, systematic review, Ethiopia
Citation: Kassew T, Melkam M, Minichil W, Wondie M and Ali D (2024) Depressive and anxiety symptoms amid COVID-19 pandemic among healthcare workers in a low-resource setting: a systematic review and meta-analysis from Ethiopia. Front. Psychiatry 15:1342002. doi: 10.3389/fpsyt.2024.1342002
Received: 21 November 2023; Accepted: 24 July 2024;
Published: 22 October 2024.
Edited by:
Wulf Rössler, Charité University Medicine Berlin, GermanyReviewed by:
Aislinn Joanmarie Williams, The University of Iowa, United StatesMohamad Golitaleb, Arak University of Medical Sciences, Iran
Copyright © 2024 Kassew, Melkam, Minichil, Wondie and Ali. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tilahun Kassew, dGlsYWh1bmthc3NldzEyM0BnbWFpbC5jb20=
 Tilahun Kassew*
Tilahun Kassew* Dawed Ali
Dawed Ali