- 1Research Department, George Institute for Global Health, New Delhi, India
- 2Centre for Global Mental Health and Centre for Implementation Science, Health Service and Population Research Department, Institute of Psychiatry, Psychology & Neuroscience, King’s College London, London, United Kingdom
- 3Department of Global Health, School of Health, Georgetown University, Washington, DC, United States
- 4Center for Global Mental Health Equity, The George Washington University School of Medicine and Health Sciences, Washington, DC, United States
- 5Faculty of Medicine, University of New South Wales, Sydney, NSW, Australia
- 6Department of Brain Sciences, Imperial College London, London, United Kingdom
- 7Department of Public Health, Prasanna School of Public Health, Manipal Academy of Higher Education, Manipal, India
Background: The International Study of Discrimination and Stigma Outcomes (INDIGO) Partnership is a multi-country international research program in seven sites across five low- and middle-income countries (LMICs) in Africa and Asia to develop, contextually adapt mental health stigma reduction interventions and pilot these among a variety of target populations. The aim of this paper is to report on the process of culturally adapting these interventions in India using an established framework.
Methods: As part of this larger program, we have contextualized and implemented these interventions from March 2022 to August 2023 in a site in north India. The Ecological Validity Model (EVM) was used to guide the adaptation and contextualization process comprising eight dimensions.
Findings: Six dimensions of the Ecological Validity Model were adapted, namely language, persons, metaphors, content, methods, and context; and two dimensions, namely concepts and goals, were retained.
Conclusion: Stigma reduction strategies with varied target groups, based on culturally appropriate adaptations, are more likely to be acceptable to the stakeholders involved in the intervention, and to be effective in terms of the program impact.
1 Introduction
Stigma and discrimination towards people with mental health conditions are universally reported across the world (1). People with mental health conditions experience stigma, prejudice, and discrimination from a variety of different sources and settings. Such stigma can come, for example, from the public and local communities where people with mental health conditions live (2, 3), from primary care workers and the healthcare system (4, 5), or from specialist mental health professionals (6). Stigma has wide-ranging consequences on people with mental health conditions, who have described stigma as worse than the mental health condition itself (1, 7). Stigma from different sources can have a range of deleterious impacts on people with mental health conditions, who can be excluded from social participation, with negative impacts on wellbeing, reduced employment opportunities, greater risk of poverty, difficulties in maintaining personal relationships (8), and limited access to health care because of barriers to help seeking (9, 10).
There is limited research conducted in low-and middle-income countries (LMICs) that evaluates the effectiveness of interventions to reduce mental health stigma and discrimination among groups that have the potential to stigmatize (11–14). There are studies in some of these countries that have shown an increase in the uptake of mental health services following an anti-stigma and awareness campaign (15, 16). There is also emerging evidence that basic mental health services can be provided by trained non-specialists (e.g., primary care providers and community health workers, peers, and other lay persons) in LMICs (17, 18). However, there is an absence of studies on anti-stigma interventions that target mental health professionals in LMICs (12), with relevant studies mostly taking place in high-income countries (19, 20). Recent studies and systematic reviews examining interventions to reduce mental health stigma and discrimination have shown that there is an increasing number of effective interventions being reported from LMICs (11–14). There is more evidence on interventions to change mental health knowledge, but fewer that addresses the critical areas of attitudes and behavior (11, 12). Extant evidence on stigma interventions has shown the effectiveness of social contact-based interventions in reducing mental health stigma, with regard to changes in discriminatory behaviors across different target groups (1). However, this evidence is less robust from LMICs (4, 11, 21) where the cultural contexts and stigmatizing groups can be very diverse.
The ways in which stigma and discrimination are expressed by different groups at the community, primary healthcare, and mental health system levels, as well as how they are experienced by people with mental health conditions, varies a great deal across countries and cultures (22–25). Dominant local beliefs about mental health conditions co-exist along with western biomedical models in LMICs with a pluralistic health system (26, 27). Labels, stereotypes, and causal attributions attached to mental health conditions vary considerably across different cultures (22, 28), and may mediate the extent to which people with mental health conditions are stigmatized and seek treatment (29). A study conducted in North India showed that the most commonly used labels for people with severe mental illness were “Aalsi” (lazy), “sustt” (lethargic), “paagal” (mad), and “darpok” (coward). About one third of the participants with these illnesses reported experiencing these labels were significantly associated with discontinuing treatment or a desire to do so (29). Despite such cultural variations, promising research shows that evidence-based psychological interventions are effective for the treatment of mental health conditions among diverse populations (30, 31). A recent review that examined incorporating cultural elements into anti-stigma programs in LMICs found that only a fifth of the studies considered cultural values, meanings, and practices in their interventions with healthcare professionals, community members and people with lived experiences (32).
In this context, the International Study of Discrimination and Stigma Outcomes (INDIGO) Partnership is a multi-country international research program in seven sites across five LMICs in Africa and Asia to develop, test and contextually adapt mental health stigma reduction interventions among a variety of target populations (33). The three interventions that are being piloted target community members and community health workers (CHWs) (Indigo-Local) (34), primary care providers (PCPs) (Indigo-Primary) (35), and mental health professionals (Indigo-READ) (36). As part of this larger program, we have contextualized and implemented these interventions in a site in north India. The aim of this paper is to report the process of culturally adapting these interventions using an established framework.
2 Methods
2.1 Study implementation and design
Implementation of the Indigo-Primary intervention among PCPs was the first of the three interventions to be implemented. This included two site staff (MD and SK), i.e. researchers involved in mental health projects, being trained in the RESHAPE (REducing Stigma among HealthcAre ProvidErs) manual (35, 37), a social-contact based stigma reduction intervention, in which five mental health service users (MHSUs) and two caregivers were trained in the photovoice technique over a period of two-and-a-half months. This is a participatory photography narrative technique to visually develop and narrate recovery stories and testimonials (38). The intervention included training primary health care providers on mental health where social contact of photovoice trained MHSUs was integrated. Two health workers were trained in the WHO mhGAP-Intervention Guide (depression and suicide modules) (39) where the two MHSUs and their caregivers narrated their recovery stories using the photovoice technique, along with a model aspirational figure (primary healthcare facility doctor) who had experience of managing people with common mental disorders. The aspirational figure shared her reflections and learnings from providing treatment for common mental disorders in a primary health care setting.
The Indigo-Local intervention comprised of a community-based, multi-component, public awareness-raising activities designed to reduce stigma and discrimination and to increase referrals of people with mental health conditions. Implementation of the intervention among community members and CHWs involved organizing two stakeholder meetings where a total of more than 50 participants were present, comprising local administrative officials of different political parties, schoolteachers, CHWs, health workers, and community members. Eleven CHWs and two MHSUs participated in the intervention trainings. A media campaign for this study was rolled out in the community using printed materials and lived experience videos developed as a part of the SMART mental health study, where a large anti-stigma campaign was implemented in a similar setting (40). This campaign as a part of INDIGO Local, was implemented for three months and covered 1185 community members with majority (70%) being women.
The Indigo-READ intervention assesses the feasibility, potential effectiveness and costs of responding to experienced and anticipated discrimination training for health professionals working in mental health care. This intervention included in-person training of six mental health professionals of the district mental health program comprising of two psychiatric nurses, one psychologist, one psychiatrist, a data entry personnel, and an intern. In addition to a service user who presented her personal testimony as an expert by experience, a short video of a person with lived experience was screened in the training.
All three interventions employed an uncontrolled design with evaluations pre-and post-intervention, and a later follow up point at three, six- or 12-months’ time. These are small scale feasibility studies that test a particular proof-of-principle largely employing mixed methods approaches (41). Box 1 describes the different program details and key components of each of the Indigo interventions. Table 1 provides further details on the methodological aspects of each intervention in the North Indian site. All the three interventions have been completed and there is a plan to bring out separate site-specific publication following the main and combined publication of each of these interventions by the work package leads.
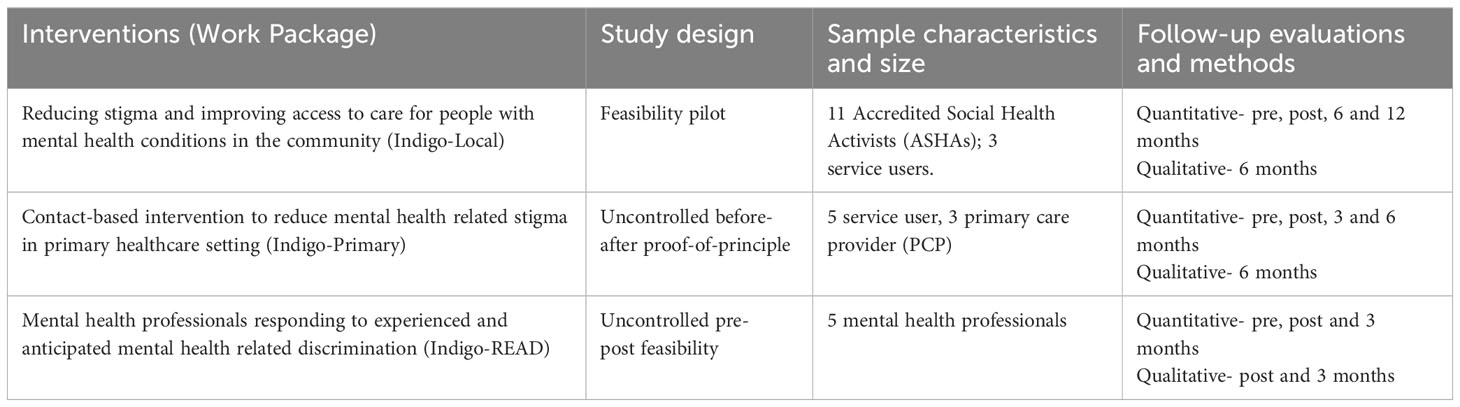
Table 1 Study design, sample size, follow-up evaluations and methods for Indigo interventions in North India.
Box 1. Program details and key components of Indigo interventions.
Indigo-Local
● Aim- to develop, implement, and evaluate a community-based, multi-component, public awareness-raising intervention designed to reduce stigma and discrimination and to increase referrals of people with mental health conditions for assessment and treatment.
● Key components- stakeholder group workshop; a stepped training programme of CHWs and MHSUs with repeated supervision and booster sessions; awareness raising activities in the community; and a media campaign.
● Social contact and service user involvement are instrumental to all components.
● Evaluation- mixed-methods pre-post design; quantitative assessment of stigma outcomes measuring knowledge, attitudes, and behaviour; quantitative evaluation of mental health service utilization rates; qualitative assessment of effectiveness and impact of the intervention; process evaluation; implementation evaluation; and evaluation of implementation costs.
● Sample size- 11-86 CHWS, 3-5 MHSUs, and 5-20 stakeholders. Participants were sampled purposively and based on feasibility and availability of local resources and size of the site.
Indigo-Primary
● Aim- to adapt and evaluate cross-cultural feasibility and acceptability of a social contact-based primary healthcare intervention.
● Key components- collaboration MHSUs with lived experience of mental health conditions, their family members, and aspirational figures (PCPs who have demonstrated high motivation to integrate mental health services). MHSUs and their family members are trained in a participatory technique, PhotoVoice, to visually depict and narrate recovery stories. Aspirational figures conduct myth busting exercises and share their experiences treating MHSUs.
● Evaluation- uncontrolled before-after study design; outcomes among PCPs will include stigma knowledge, explicit and implicit attitudes, and mental healthcare competencies; qualitative interviews with MHSUs, family members, and aspirational figures, PhotoVoice trainers, mental health specialists co-leading the primary care trainings, and PCPs receiving mental health training; generate evidence regarding feasibility, acceptability, recruitment, retention, fidelity, safety, and usefulness of the intervention.
● Sample size- 6-20 MHSUs, 1-8 aspirational figure, and 2-36 PCPs. The sample size were determined by the number of participants available and feasibility to include them in the study.
Indigo-READ
● Aim- assess feasibility, potential effectiveness, and costs of Responding to Experienced and Anticipated Discrimination training for health professionals working in mental health care.
● Key components- training draws upon evidence bases for stigma reduction, health advocacy and medical education and is tailored to sites through situational analyses; content, delivery methods and intensity were agreed upon through a consensus exercise with site research teams; delivered to health professionals working in mental health care.
● Evaluation- uncontrolled pre-post mixed methods feasibility study; baseline data collection; outcome measures at post-training and 3 months post-baseline, followed by qualitative data collection; fidelity rated during intervention delivery; data on training costs; qualitative data to identify feedback about training methods and content, including the implementability of the knowledge and skills learned; pooled and site-specific training costs per trainee and per session.
● Sample size- 4-30 mental health professionals. As this is a feasibility study without any control group the sample size is not designed to determine effectiveness.
2.2 Setting
The interventions were conducted in and around two Urban Primary Health Centres (UPHCs) of Atmadpur and Mewla Maharajpur, covering the areas of Rajeev nagar, Harkesh nagar, Santosh nagar, Dheeraj nagar part 1, Dheeraj nagar part 2, under the former UPHC and Mewla Maharajpur, Ghandhi colony, Fatehpur Chandela, under the latter UPHC. These UPHCs fall under the district of Faridabad, Haryana state where the intervention with mental health professionals took place at the district hospital. The UPHCs and district hospital were chosen as they were near the central office and field offices of the implementing site of Delhi, and we had a well-established relationship with the state and district health departments. Study participants across all interventions were selected using a qualitative technique akin to convenience sampling as they were easily accessible, and such a technique is generally applied for pilot testing (41).
The activities across all the three anti-stigma interventions started in July 2022 with the integrated training of PCPs beginning first. However, the preparation for this intervention started much before in March 2022 with the training of service users on the photovoice technique. All intervention activities have been completed with a final quantitative evaluation of CHWs done in late August 2023.
2.3 Cultural adaptation framework
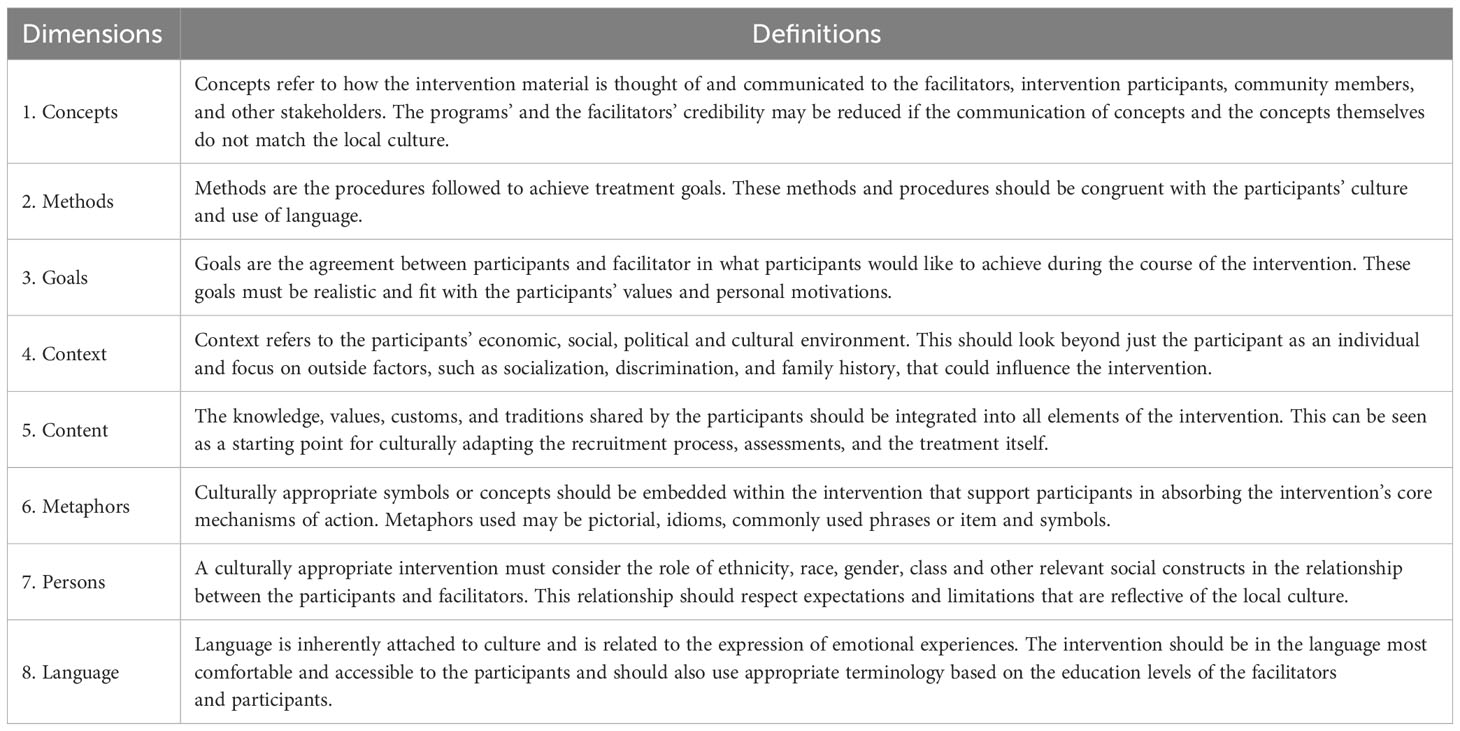
Each of the Indigo interventions went through a process of adaption. The adaptations were specifically made keeping in mind the local cultural context in which the interventions were implemented. The Ecological Validity Model (42) was used to document the adaptation and contextualization process. This documentation took place either during the preparatory phase of planning the interventions or during and after certain intervention activities were completed. The EVM outlines eight contextualization dimensions, with operational definitions provided in Table 2.
Across each of these dimensions six domains of contextualization were recorded: 1) original content changed, 2) pages/location in the intervention manual or materials, 3) description of contextualization, 4) rationale of change and what it would accomplish, 5) evidence for change, and 6) the source of this evidence. Characteristics of team members who conducted the contextualization procedure were also recorded. This included indicating relevant educational qualifications and work experience of the team members, and any other relevant demographic information. Additionally, it was critically important to mention whether team members spoke the local language and had experience working in settings where the intervention was rolled out.
2.4 Characteristics of team conducting cultural adaptation and contextualization
A total of three staff members were involved in the cultural adaptation process with diverse educational qualifications, experience, genders, and capability of speaking in the local language of study participants. The educational qualifications of the team members varied from Masters to Post-doctoral level in social work or public health. Experience of working in the field of mental health also varied among the team members between 5-20 years. All the members involved in the cultural adaptation process had varying capabilities of reading, writing, and speaking the local language of study participants. Two of the team members (SK and SC) could read, write, and speak the local language and were involved in the translation of training materials from English to Hindi and conducting the training sessions.1 MD adapted the training materials as per the need and context of the interventions that were provided in English by the work package leads. These were then handed over to SC who was primarily involved in translating the materials to Hindi. This was then cross checked and finalized by SK. If any disagreements on the translation arose, then it was consensually decided by both SC and SK. One team member (MD) who could speak the local language was involved in conducting the training sessions.1 All team members had the experience of directly engaging with MHSUs from an ongoing project (40, 43).
3 Results
3.1 Cultural adaptation and contextualization
The processes of culturally adapting the interventions are documented and presented in a matrix under each contextual dimension and across the different domains (Table 3). All materials used in the training of MHSUs and CHWs that were presented in the form of power point slides were originally developed in English and then translated into Hindi (the local vernacular language spoken in the area). These changes have been indicated in the pages of the original training manuals and the adapted manuals or power point slides. Training materials for mental health professionals (MHPs) were however retained in the original English language and used as such, though much of the discussion around the content of the training were done in the local Hindi language.
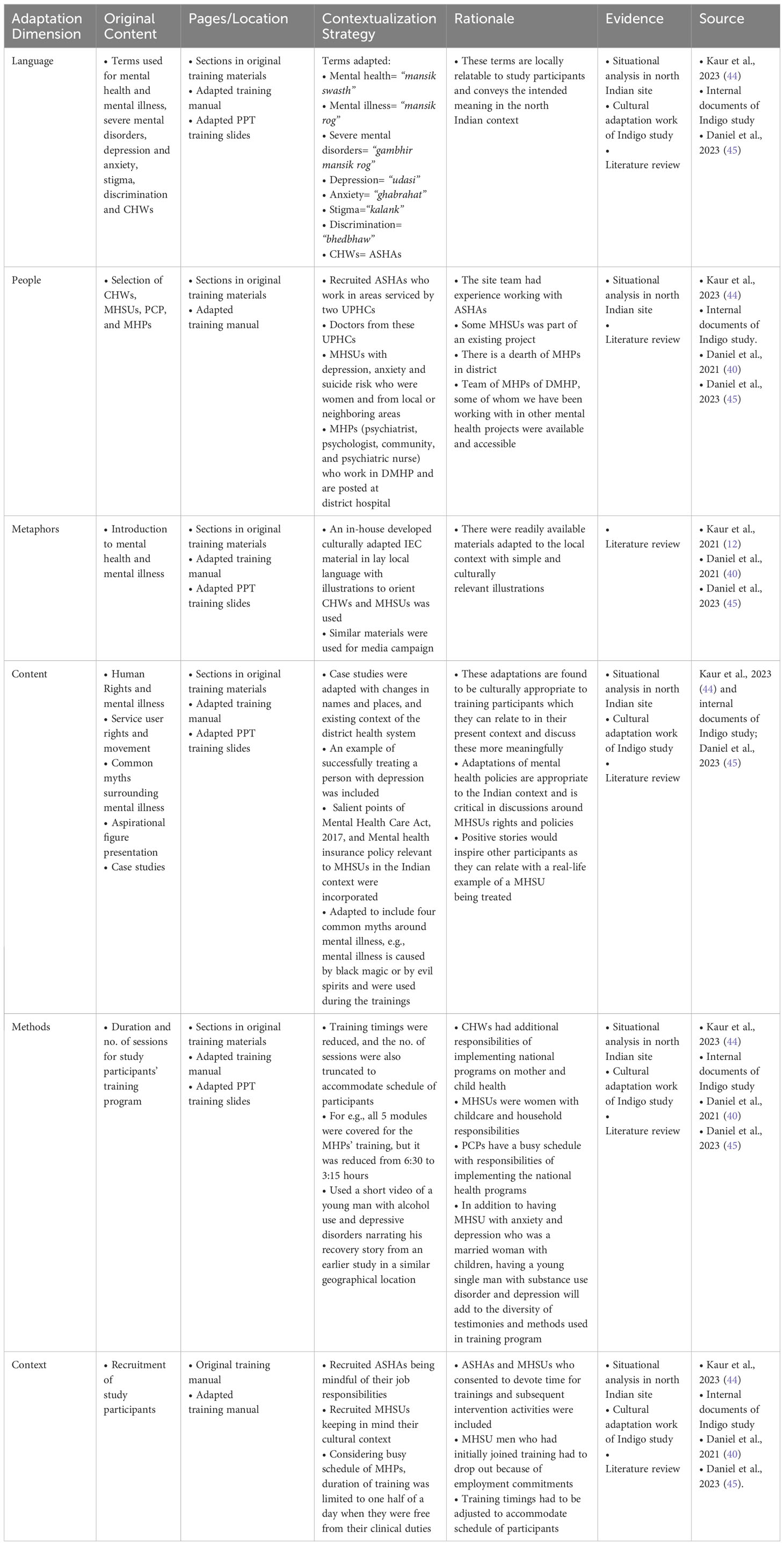
Table 3 Cultural adaptation of Indigo study interventions using an ecological validity model matrix.
3.2 Language
The adaptation of language in the training and intervention materials included terms used for mental health and mental illness, severe mental disorders, depression and anxiety, stigma, and discrimination. The translated Hindi terms used for these are further described in Table 3. The contextualization process considered previous research that was conducted in similar geographical locations and cultural context (40, 45) to where the Indigo interventions were implemented. Additionally, MHSUs were asked to elucidate derogatory terms used for people with mental health conditions that either they have been referred to or have heard somewhere. These terms were “besahoor” (creep), “chatka huaa” (cracked), “paagal” (mad), “nasamaj” (foolish), “budhiheen” (brainless), mental, “ganwar” (uneducated), “bewakoof” (idiot). It was necessary to bring out culturally dominant and derogatory stereotypes that MHSUs experienced to provide alternative destigmatizing terms to challenge these. These terms were adapted to the local context as they are more relatable to ASHAs and MHSUs and convey the desired meaning in the local context.
3.3 Persons
Participants who were recruited for the interventions were CHWs known as Accredited Social Health Activists (ASHAs) in India. As this was a pilot intervention, only few ASHAs who worked in select areas serviced by two UPHCs were included. ASHAs are an all women cadre of primary health workers and act as a link between the community and the health system (40, 46). The project team had experience working with ASHAs for a considerable period in mental health projects that also utilized an anti-stigma campaign (16, 40). The research team had experience working with MHSUs (40, 43). MHSUs with depression, anxiety, and suicide risk who were receiving treatment from either a public or private facility and those from an ongoing project were included in the interventions. Doctors from the UPHCs and mental health professionals who are a part of the District Mental Health Program (DMHP) at the district hospital were included in the trainings.
3.4 Metaphors
Culturally adapted materials in a lay local language that were used in an ongoing mental health study were used for the training of CHWs and MHSUs to orient them on mental health, types of mental disorders, causes of mental disorders, identifying mental disorders, treatment of common mental disorders (like depression, anxiety and suicide risk), ways to manage people with CMDs and ways to overcome stigma (45, 47). As part of a media campaign for the intervention with community members (Indigo Local), we used existing culturally adapted materials like a flipbook and a video of a person with lived experience. The flipbook included simple illustrations of what CMDs are and what can be done to overcome and live with CMDs. In the training with MHPs, we used materials in English as training participants and trainers spoke both English and Hindi. However, the discussions during the training were done in the local language, where for example local metaphors were used to explain the idea of empathy in a culturally relevant way by one of the participants.
3.5 Content
The intervention and training content used several case studies to substantiate and prompt discussions on aspects related to mental health and mental health stigma. The case examples were adapted with changes in names, places, and health system context to assist study participants relate to these in a more meaningful way. For instance, a real-life example of successfully treating a person with a mental health condition was narrated by a primary care provider. Based on a situational analyses study and earlier formative research, common myths of mental illness prevalent in the study area were adapted (44, 45) and included in the intervention trainings. Policies relevant to MHSUs in the Indian context were included and discussed in the trainings, which is critical in any discussion around MHSUs representation and rights.
3.6 Methods
There was no major change in the methods of imparting trainings for study participants as per the intervention protocol templates, which included didactic lectures, group exercises, case studies, and individual presentations. However, the duration of the trainings was reduced with the number of sessions shortened. The timings of the trainings were also scheduled in a way that accommodated the caring and household responsibilities of MHSUs, community outreach work of ASHAs, and clinical commitments of PCPs and MHPs. Trainings with participants who were extremely busy with their day-to-day work were conducted at the end of the program. In addition to using lived experience testimonies of MHSUs, we included a short video of a lived experience testimony to add to the diversity of the methods used in the intervention trainings.
3.7 Context
The research team conducting the interventions with different groups of study participants were mindful of their background, which included both their personal and professional context. Only those participants who gave their consent and agreed to take part and continue in the trainings were recruited. MHSUs who were men, for instance, could not continue in the trainings and intervention as they had to take care of their job commitments. The context of the study participants across all categories, i.e., mental health service users, primary care providers, community health workers, and mental health professionals, to a large extent had a bearing on the training methods employed in the intervention (Table 3).
3.8 Concepts and goals
While six dimensions of the intervention were adapted to the local context, the dimensions of ‘concepts’ and ‘goals’ were not changed and retained as they were. It was not necessary to change the different concepts that went into the Indigo interventions. The idea to engage with key community stakeholders prior to intervention activities to gain buy-in has been integral to the work that we do. During the stakeholders meetings we took feedback from community members on the strategies for the Indigo-Local media campaign. The social contact element was incorporated into all the interventions (33). The social-contact based concept of engagement in Indigo-Primary where PCPs interacted with SUs and aspirational figures in reducing potential survival, social and professional threats (37) also applied in our setting. Additionally, the concept of reflective practice, intergroup contact theory, and mechanisms that sustain social distance remained the same in the Indigo-READ intervention that involved mental health professionals (48, 49). There was no change in the goals of stigma reduction across all study groups, especially in terms of integrating a social contact element in the interventions.
4 Discussion
This study used a cultural framework to contextually adapt mental health stigma reduction interventions among community members and community health workers, PCPs, and mental health professionals in a north Indian site as part of the larger Indigo Partnership study. Guided by the EVM framework, six dimensions (language, persons, metaphors, content, methods, context) were adapted either before, during or after the interventions were implemented. However, two dimensions, (concepts and goals) were retained and used as they were in the original training materials. The team members involved in the adaptation process had experience working in mental health and could read, write, and speak the local language of study participants.
4.1 Elements of cultural adaptation
The purpose of using a validated cultural adaptation framework – that is, the EVM framework (42) - in this study was twofold. Firstly, to document the entire intervention adaptation processes; and secondly, to increase the cultural acceptability and effectiveness of the intervention strategies used among different target groups. We did this by making certain changes in different dimensions of the interventions that align with the culture of the study participants and the context of the health system, while retaining the core elements of the intervention that are backed by evidence informed practices (32, 42, 50, 51). While encouraging adaptations that are receptive to the requirements of study participants, it is also necessary to implement the intervention as intended. The methods dimension was adapted whereby the duration of the interventions were truncated while not making any changes to the concepts and goals. This reflects what researchers have termed the balance between fidelity and fit elements of an intervention that promotes cultural relevance of the intervention while also adhering to evidence-based practices to increase effectiveness (52, 53).
The eight dimensions that were used in the EVM framework are based on cultural adaptation facets proposed by Bernal and Rodriguez (54) in documenting the adaptation process while conceptually adhering to the intervention’s primary mechanisms of actions. Like other researchers who have pointed out that the dimensions of content and context overlap with each other (42), we also found this to be similar in the Indian setting. We found considerable commonalities across these dimension groups: language, metaphor, and content; and persons and context. While using the language dimension in the adaptation process of this study, stigmatizing labels associated to mental health conditions that emerged were quite similar to those reported from the same north Indian region (29). Under the two latter dimensions, we considered the role of gender, age, caste, and class that go into the relationships among study participants and with researchers, where social constructs such as these largely influence cultural practices (45). In one of our mixed methods formative research in the adjoining rural areas of where this present study was conducted, we found caste-based marginalization among community members and gender and age related cultural practices (45). The metaphor dimension was adapted by using a pre-existing adapted print material from an ongoing study with simple culturally relevant illustrations that were informed by formative research (45, 47). Researchers involved in cultural adaptation of psychological interventions have observed that using ethnically relevant pictorial materials identical to the study participants context improved their retention, which is referred to as surface level adaptations (55). This highlights the importance of simple, yet crucial, cultural adaptation processes (56). Engagement with participants at various stages of the study to understand their experiences and overall acceptability of these stigma reductions interventions were possible because of the cultural adaptations. However, it is critical to keep in mind that while contextually adapting complex community and health system-based interventions, some of these cultural adaptations processes are not as straightforward as they may initially appear. An important aspect of any cultural adaptation of stigma and discrimination reduction strategies should consider that the processes of contextualizing different cultural elements do not in turn reinforce or increase perceptions of stigma among study participants and service users in particular.
4.2 Need for cultural adaptation
The nature and extent of stigma and discrimination expressed by different groups and experienced by people with mental health conditions is greatly influenced by their cultural beliefs and practices (22–25). Despite these cultural influences, research on stigma and discrimination reduction interventions have noted that almost all interventions that are implemented in LMICs have predominantly been developed in high-income countries (HICs) based on western principles, values, and frameworks (57). This ignores how existing diverse local health systems and practices might influence the ways in which stigma and discrimination around mental health conditions are socially constructed, perceived and expressed, across culturally heterogeneous global settings (26, 27, 58). Programs in reducing stigma and discrimination of mental health conditions have made phenomenal global progress over the past few decades (1). However, unfortunately most programs are carried out in HICs (59). Most of these interventions are resource intensive and complex, and not suitable to the sociocultural contexts and health systems in LMICs making it a challenge to introduce these programs in low resource settings (32). Although it is encouraging that several interventions to address stigma and discrimination among people with mental health conditions are being implemented in LMICs (1, 60), little is known on the extent to which of these interventions have been effective, and whether these have used culturally appropriate approaches (32).
A scoping review conducted to examine the role of culture in programs to reduce stigma towards people with mental health conditions in LMICs found that only a handful of studies considered cultural elements of mental health stigma in the design and implementation of such programs (32). More importantly, the studies also lacked a systematic way of comparing cultural dimensions across and within countries. The larger Indigo Partnership study in seven sites across five LMICs (33), within which the work reported on in this study is conducted, has a dedicated work stream of culturally contextualizing interventions to reduce stigma and discrimination among people with mental health conditions. As such it will be able to provide insights into many of these research gaps. Moreover, using the EVM framework for the three interventions in the larger Indigo Partnership study provides a method to evaluate and compare cultural adaptation strategies across the seven contextually and culturally varied sites. Overall, it would be important to assess how these adaptations might possibly have an impact on the intervention outcomes, so as to identify which modifications appear to enhance intervention acceptability and effectiveness.
5 Conclusion
In this study stigma reduction interventions were implemented as a small-scale proof of principle interventions across different target groups in one of the North Indian sites of the Indigo collaborative research. We documented the process of culturally adapting these strategies across different dimensions and domains. Unlike previous work, we used the well validated Ecological Validity Model framework to capture these modifications and to inform the cultural adaptation and implementation science research. Stigma reduction strategies encompassing varied target groups, based on culturally appropriate adaptations and evidence, will be more applicable to stakeholders involved in the intervention in the future to achieve program acceptability and effectiveness, and possibly in taking these anti-stigma interventions to scale.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material. Further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by The George Institute Ethics Committee, The George Institute for Global Health (18/2020 dated 04.09.2020). Approval from the Health Ministry Screening Committee, Department of Health Research/ICMR was also sought (HMSC- 2020-10098). The studies were approved by by the KCL PNM Research Ethics Subcommittee (HR-19/20-17252). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
MD: Writing – original draft. SK: Writing – review & editing. PCG: Writing – review & editing. SW: Writing – review & editing. BK: Writing – review & editing. GT: Writing – review & editing. PKM: Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research is funded by the UK Medical Research Council (MRC) [MR/R023697/1]. The funding body had no role in the design of the study, its data collection, analysis, and interpretation, or the writing of this manuscript. For the purpose of open access, the author has applied a Creative Commons Attribution (CC BY) licence (where permitted by UKRI, ‘Open Government Licence’ or ‘Creative Commons Attribution No-derivatives (CC BY-ND) licence’ may be stated instead) to any Author Accepted Author Manuscript version arising from this submission. MD and PCG are supported by the UK Medical Research Council (UKRI) for the Indigo Partnership (MR/R023697/1) award. PKM and SK are partially or wholly supported by the UKRI/MRC grant (MR/S023224/1) Adolescents’ Resilience and Treatment Needs for Mental health in Indian Slums (ARTEMIS) grant and NHMRC/GACD SMART Mental Health grant (APP1143911). GT is supported by the National Institute for Health and Care Research (NIHR) Applied Research Collaboration South London (NIHR ARC South London) at King’s College Hospital NHS Foundation Trust. GT is also supported by the UK Medical Research Council (UKRI) for the Indigo Partnership (MR/R023697/1) awards.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The George Institute has a part-owned social enterprise, George Health Enterprises, which has commercial relationships involving digital health innovations.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Footnotes
- ^ Mercian Daniel (MD), Senior Research Fellow, Sudha Kallakuri (SK), Research Fellow, and Santosh Chouhan Project Supervisor, The George Institute for Global Health, India.
References
1. Thornicroft G, Sunkel C, Alikhon Aliev A, Baker S, Brohan E, El Chammay R, et al. The Lancet Commission on ending stigma and discrimination in mental health. Lancet (2022) 400(10361):1438–80. doi: 10.1016/S0140-6736(22)01470-2
2. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol (2001) 27(1):363–85. doi: 10.1146/annurev.soc.27.1.363
3. Pescosolido BA. The public stigma of mental illness: what do we think; what do we know; what can we prove? J Health Soc Behav (2013) 54(1):1–21. doi: 10.1177/0022146512471197
4. Heim E, Kohrt B, Koschorke M, Milenova M, Thornicroft G. Reducing mental health-related stigma in primary health care settings in low-and middle-income countries: a systematic review. Epidemiol Psychiatr Sci (2020) 29:e3. doi: 10.1017/S2045796019000349
5. Vistorte AOR, Ribeiro WS, Jaen D, Jorge MR, Evans-Lacko S, Mari J. Stigmatizing attitudes of primary care professionals towards people with mental disorders: A systematic review. Int J Psychiatry Med (2018) 53(4):317–38. doi: 10.1177/0091217418778620
6. Sartorius N. Stigma: what can psychiatrists do about it? Lancet (1998) 352(9133):1058–9. doi: 10.1016/S0140-6736(98)08008-8
7. Henderson C, Thornicroft G. Stigma and discrimination in mental illness: Time to Change. Lancet (2009) 373(9679):1928–30. doi: 10.1016/S0140-6736(09)61046-1
8. Thornicroft G, Brohan E, Rose D, Sartorius N, Leese M, Group IS. Global pattern of experienced and anticipated discrimination against people with schizophrenia: a cross-sectional survey. Lancet (2009) 373(9661):408–15. doi: 10.1016/S0140-6736(08)61817-6
9. Clement S, Schauman O, Graham T, Maggioni F, Evans-Lacko S, Bezborodovs N, et al. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol Med (2015) 45(1):11–27. doi: 10.1017/S0033291714000129
10. Corrigan PW, Druss BG, Perlick DA. The impact of mental illness stigma on seeking and participating in mental health care. Psychol Sci Public Interest (2014) 15(2):37–70. doi: 10.1177/1529100614531398
11. Clay J, Eaton J, Gronholm PC, Semrau M, Votruba N. Core components of mental health stigma reduction interventions in low- and middle-income countries: a systematic review. Epidemiol Psychiatr Sci (2020) 29:e164. doi: 10.1017/S2045796020000797
12. Kaur A, Kallakuri S, Kohrt BA, Heim E, Gronholm PC, Thornicroft G, et al. Systematic review of interventions to reduce mental health stigma in India. Asian J Psychiatr (2021) 55:102466. doi: 10.1016/j.ajp.2020.102466
13. Maulik PK, Devarapalli S, Kallakuri S, Tewari A, Chilappagari S, Koschorke M, et al. Evaluation of an anti-stigma campaign related to common mental disorders in rural India: a mixed methods approach. Psychol Med (2017) 47(3):565–75. doi: 10.1017/S0033291716002804
14. Maulik PK, Devarapalli S, Kallakuri S, Tripathi AP, Koschorke M, Thornicroft G. Longitudinal assessment of an anti-stigma campaign related to common mental disorders in rural India. Br J Psychiatry (2019) 214(2):90–5. doi: 10.1192/bjp.2018.190
15. Eaton J, Agomoh AO. Developing mental health services in Nigeria: the impact of a community-based mental health awareness programme. Soc Psychiatry Psychiatr Epidemiol (2008) 43(7):552–8. doi: 10.1007/s00127-008-0321-5
16. Maulik PK, Devarapalli S, Kallakuri S, Bhattacharya A, Peiris D, Patel A. The systematic medical appraisal referral and treatment mental health project: quasi-experimental study to evaluate a technology-enabled mental health services delivery model implemented in rural India. J Med Internet Res (2020) 22(2):e15553. doi: 10.2196/15553
17. Patel V, Weiss HA, Chowdhary N, Naik S, Pednekar S, Chatterjee S, et al. Lay health worker led intervention for depressive and anxiety disorders in India: impact on clinical and disability outcomes over 12 months. Br J Psychiatry (2011) 199(6):459–66. doi: 10.1192/bjp.bp.111.092155
18. Patel V, Weobong B, Weiss HA, Anand A, Bhat B, Katti B, et al. The Healthy Activity Program (HAP), a lay counsellor-delivered brief psychological treatment for severe depression, in primary care in India: a randomised controlled trial. Lancet (2017) 389(10065):176–85. doi: 10.1016/S0140-6736(16)31589-6
19. Arboleda-Flórez J, Stuart H. From sin to science: fighting the stigmatization of mental illnesses. Can J Psychiatry (2012) 57(8):457–63. doi: 10.1177/070674371205700803
20. Ungar T, Knaak S, Szeto AC. Theoretical and practical considerations for combating mental illness stigma in health care. Community Ment Health J (2016) 52(3):262–71. doi: 10.1007/s10597-015-9910-4
21. Morgan AJ, Reavley NJ, Ross A, Too LS, Jorm AF. Interventions to reduce stigma towards people with severe mental illness: Systematic review and meta-analysis. J Psychiatr Res (2018) 103:120–33. doi: 10.1016/j.jpsychires.2018.05.017
22. Littlewood R. Cultural variation in the stigmatisation of mental illness. Lancet (1998) 352(9133):1056–7. doi: 10.1016/S0140-6736(98)07471-6
23. Yang LH, Kleinman A, Link BG, Phelan JC, Lee S, Good B. Culture and stigma: adding moral experience to stigma theory. Soc Sci Med (2007) 64(7):1524–35. doi: 10.1016/j.socscimed.2006.11.013
24. Pescosolido BA, Medina TR, Martin JK, Long JS. The “backbone” of stigma: identifying the global core of public prejudice associated with mental illness. Am J Public Health (2013) 103(5):853–60. doi: 10.2105/AJPH.2012.301147
25. Bracke P, Delaruelle K, Verhaeghe M. Dominant cultural and personal stigma beliefs and the utilization of mental health services: A cross-national comparison. Front Sociol (2019) 4:40. doi: 10.3389/fsoc.2019.00040
26. Kakar S. Shamans, mystics and doctors: a psychological inquiry into India and its healing traditions. Philosophy East West (1993) 43(2):352. doi: 10.2307/1399636
27. Gureje O, Appiah-Poku J, Bello T, Kola L, Araya R, Chisholm D, et al. Effect of collaborative care between traditional and faith healers and primary health-care workers on psychosis outcomes in Nigeria and Ghana (COSIMPO): a cluster randomised controlled trial. Lancet (2020) 396(10251):612–22. doi: 10.1016/S0140-6736(20)30634-6
28. Fabrega H Jr. Psychiatric stigma in the classical and medieval period: a review of the literature. Compr Psychiatry (1990) 31(4):289–306. doi: 10.1016/0010-440X(90)90036-R
29. Grover S, Shouan A, Sahoo S. Labels used for persons with severe mental illness and their stigma experience in North India. Asian J Psychiatr (2020) 48:101909. doi: 10.1016/j.ajp.2019.101909
30. Cuijpers P, Karyotaki E, Reijnders M, Purgato M, Barbui C. Psychotherapies for depression in low- and middle-income countries: a meta-analysis. World Psychiatry (2018) 17(1):90–101. doi: 10.1002/wps.20493
31. Singla DR, Kohrt BA, Murray LK, Anand A, Chorpita BF, Patel V. Psychological treatments for the world: lessons from low- and middle-income countries. Annu Rev Clin Psychol (2017) 13:149–81. doi: 10.1146/annurev-clinpsy-032816-045217
32. Mascayano F, Toso-Salman J, Ho YCS, Dev S, Tapia T, Thornicroft G, et al. Including culture in programs to reduce stigma toward people with mental disorders in low- and middle-income countries. Transcult Psychiatry (2020) 57(1):140–60. doi: 10.1177/1363461519890964
33. Gronholm PC, Bakolis I, Cherian AV, Davies K, Evans-Lacko S, Girma E, et al. Toward a multi-level strategy to reduce stigma in global mental health: overview protocol of the Indigo Partnership to develop and test interventions in low- and middle-income countries. Int J Ment Health Syst (2023) 17(1):2. doi: 10.1186/s13033-022-00564-5
34. Semrau M, Gronholm PC, Eaton J, Maulik PK, Ayele B, Bakolis I, et al. Reducing stigma and improving access to care for people with mental health conditions in the community: protocol for a multi-site feasibility intervention study (Indigo-Local). Res Sq (2023). doi: 10.21203/rs.3.rs-3237562/v1
35. Gurung D, Kohrt BA, Wahid SS, Bhattarai K, Acharya B, Askri F, et al. Adapting and piloting a social contact-based intervention to reduce mental health stigma among primary care providers: Protocol for a multi-site feasibility study. SSM - Ment Health (2023) 4:100253. doi: 10.1016/j.ssmmh.2023.100253
36. Henderson C, Ouali U, Bakolis I, Berbeche N, Bhattarai K, Brohan E, et al. Training for mental health professionals in responding to experienced and anticipated mental health-related discrimination (READ-MH): protocol for an international multisite feasibility study. Pilot Feasibility Stud (2022) 8(1):257. doi: 10.1186/s40814-022-01208-8
37. Kohrt BA, Jordans MJD, Turner EL, Rai S, Gurung D, Dhakal M, et al. Collaboration with people with lived experience of mental illness to reduce stigma and improve primary care services: A pilot cluster randomized clinical trial. JAMA Netw Open (2021) 4(11):e2131475. doi: 10.1001/jamanetworkopen.2021.31475
38. Mizock L, Russinova Z, Shani R. New roads paved on losses: photovoice perspectives about recovery from mental illness. Qual Health Res (2014) 24(11):1481–91. doi: 10.1177/1049732314548686
39. World Health Organisation. WHO mental health gap action programme (mhGAP). Geneva: World Health Organization (2021). Available at: http://www.who.int/mental_health/mhgap/en/index.html.
40. Daniel M, Maulik PK, Kallakuri S, Kaur A, Devarapalli S, Mukherjee A, et al. An integrated community and primary healthcare worker intervention to reduce stigma and improve management of common mental disorders in rural India: protocol for the SMART Mental Health programme. Trials (2021) 22(1):179. doi: 10.1186/s13063-021-05136-5
41. Lancaster GA. Pilot and feasibility studies come of age! Pilot Feasibility Stud (2015) 1(1):1. doi: 10.1186/2055-5784-1-1
42. Sangraula M, Kohrt BA, Ghimire R, Shrestha P, Luitel NP, van’t Hof E, et al. Development of the mental health cultural adaptation and contextualization for implementation (mhCACI) procedure: a systematic framework to prepare evidence-based psychological interventions for scaling. Global Ment Health (2021) 8:e6. doi: 10.1017/gmh.2021.5
43. Kaur A, Kallakuri S, Daniel M, Yatirajula SK, Devarapalli S, Maulik PK. Directly engaging with People with lived experiences of mental illness from the communities in India. SSM - Ment Health (2021) 1:100024. doi: 10.1016/j.ssmmh.2021.100024
44. Kaur A, Kallakuri S, Mukherjee A, Wahid SS, Kohrt BA, Thornicroft G, et al. Mental health related stigma, service provision and utilization in Northern India: situational analysis. Int J Ment Health Syst (2023) 17(1):10. doi: 10.1186/s13033-023-00577-8
45. Daniel M, Kaur A, Mukherjee A, Bhattacharya A, Tewari A, Sagar R, et al. The systematic medical appraisal, referral and treatment (SMART) mental health programme: Formative research informing a cluster randomized controlled trial. SSM - Ment Health (2023) 3:100223. doi: 10.1016/j.ssmmh.2023.100223
46. Daniel M, Maulik PK. Incentivizing community health workers for scaling up mental health care in rural communities in India: A critical look at principles that work. Front Health Serv (2023) 3:1119213. doi: 10.3389/frhs.2023.1119213
47. Maulik PK, Tewari A, Devarapalli S, Kallakuri S, Patel A. The systematic medical appraisal, referral and treatment (SMART) mental health project: development and testing of electronic decision support system and formative research to understand perceptions about mental health in rural India. PloS One (2016) 11(10):e0164404. doi: 10.1371/journal.pone.0164404
49. Pettigrew TF. Intergroup contact theory. Annu Rev Psychol (1998) 49:65–85. doi: 10.1146/annurev.psych.49.1.65
50. Dinos S. Culturally adapted mental healthcare: evidence, problems and recommendations. BJPsych Bull (2015) 39(4):153–5. doi: 10.1192/pb.bp.115.050872
51. Fisher J, Nguyen H, Mannava P, Tran H, Dam T, Tran H, et al. Translation, cultural adaptation and field-testing of the Thinking Healthy Program for Vietnam. Global Health (2014) 10:37. doi: 10.1186/1744-8603-10-37
52. Castro FG, Barrera M Jr., Martinez CR Jr. The cultural adaptation of prevention interventions: resolving tensions between fidelity and fit. Prev Sci (2004) 5(1):41–5. doi: 10.1023/B:PREV.0000013980.12412.cd
53. Kilbourne AM, Neumann MS, Pincus HA, Bauer MS, Stall R. Implementing evidence-based interventions in health care: application of the replicating effective programs framework. Implement Sci (2007) 2:42. doi: 10.1186/1748-5908-2-42
54. Bernal GE, Domenech Rodríguez MM. Cultural adaptations: Tools for evidence-based practice with diverse populations. Am psychol Assoc (2012). doi: 10.1037/13752-000
55. Kumpfer KL, Alvarado R, Smith P, Bellamy N. Cultural sensitivity and adaptation in family-based prevention interventions. Prev Sci (2002) 3(3):241–6. doi: 10.1023/A:1019902902119
56. Chowdhary N, Jotheeswaran AT, Nadkarni A, Hollon SD, King M, Jordans MJ, et al. The methods and outcomes of cultural adaptations of psychological treatments for depressive disorders: a systematic review. Psychol Med (2014) 44(6):1131–46. doi: 10.1017/S0033291713001785
57. Yang LH, Thornicroft G, Alvarado R, Vega E, Link BG. Recent advances in cross-cultural measurement in psychiatric epidemiology: utilizing ‘what matters most’ to identify culture-specific aspects of stigma. Int J Epidemiol (2014) 43(2):494–510. doi: 10.1093/ije/dyu039
58. Kirmayer L, Pedersen D. Toward a new architecture for global mental health. Transcultural Psychiatry (2014) 51:759–76. doi: 10.1177/1363461514557202
59. Evans-Lacko S, Corker E, Williams P, Henderson C, Thornicroft G. Effect of the Time to Change anti-stigma campaign on trends in mental-illness-related public stigma among the English population in 2003-13: an analysis of survey data. Lancet Psychiatry (2014) 1(2):121–8. doi: 10.1016/S2215-0366(14)70243-3
Keywords: indigo, cultural adaptation, mental health, stigma reduction, discrimination, India
Citation: Daniel M, Kallakuri S, Gronholm PC, Wahid SS, Kohrt B, Thornicroft G and Maulik PK (2024) Cultural adaptation of INDIGO mental health stigma reduction interventions using an ecological validity model in north India. Front. Psychiatry 15:1337662. doi: 10.3389/fpsyt.2024.1337662
Received: 13 November 2023; Accepted: 11 January 2024;
Published: 31 January 2024.
Edited by:
Piper Meyer-Kalos, University of Minnesota, United StatesReviewed by:
Lionel Wininger, University of Minnesota, United StatesJulia Browne, United States Department of Veterans Affairs, United States
Copyright © 2024 Daniel, Kallakuri, Gronholm, Wahid, Kohrt, Thornicroft and Maulik. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mercian Daniel, bWRhbmllbEBnZW9yZ2VpbnN0aXR1dGUub3JnLmlu
 Mercian Daniel
Mercian Daniel Sudha Kallakuri
Sudha Kallakuri Petra C. Gronholm
Petra C. Gronholm Syed Shabab Wahid3
Syed Shabab Wahid3 Brandon Kohrt
Brandon Kohrt Pallab K. Maulik
Pallab K. Maulik