- 1Department of Neuropsychiatry, College of Korean Medicine, Kyung Hee University, Seoul, Republic of Korea
- 2Department of Neuropsychiatry, Kyung Hee University Korean Medicine Hospital at Gangdong, Seoul, Republic of Korea
Background: Hwabyung is a Korean culture-bound syndrome characterized by anger-related physical and psychological symptoms. Depressive disorder is a common mental illness occurring worldwide, and has been reported to have a high comorbidity rate with Hwabyung. For patients with depressive disorders, differential diagnosis and combined treatment for Hwabyung should be considered. Mindfulness and Qigong may be effective alternatives for regulating emotions such as depression, anxiety, and anger. This study aims to investigate whether Mindfulness and Qigong Training for Self-Healing (MQT-SH) would improve emotional problems in patients with Hwabyung and depressive disorder.
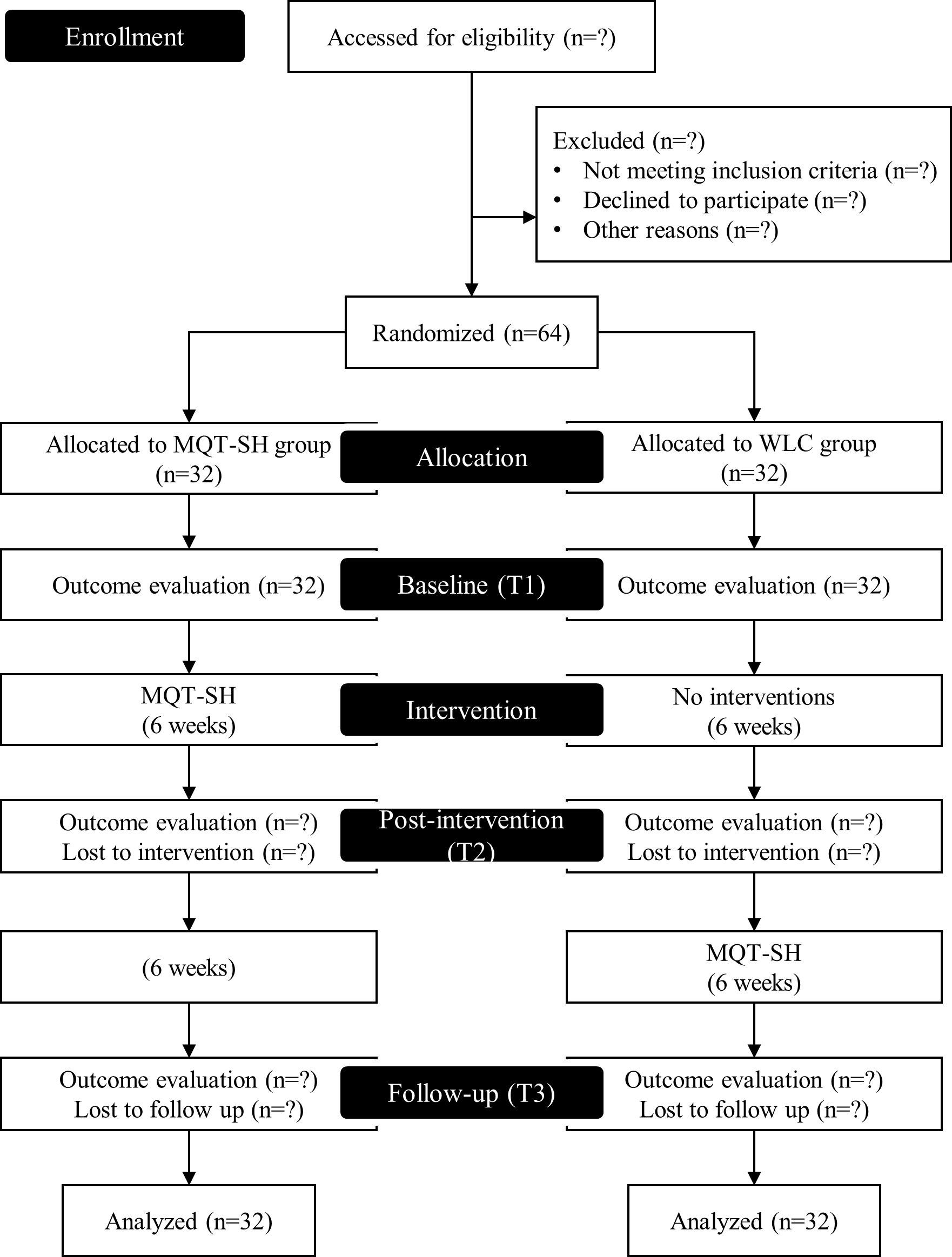
Methods: This study will be a two-arm block randomized controlled trial. A total of 64 participants will be recruited and randomly assigned to either experimental or control group. While the experimental group will perform MQT-SH for the first six weeks, the control group will receive no treatment. During the next six weeks, the control group will perform MQT-SH for ethical equity. Assessments will be conducted at baseline, post-intervention (6 weeks) and follow-up (12 weeks). The primary outcomes would be Hwabyung and depression, while the secondary outcomes would include anxiety, anger, and vitality.
Discussion: This study will provide a basis for assessing the effectiveness of mindfulness and Qigong training in patients with Hwabyung and depressive disorder.
Ethics and dissemination: This study was approved by the Institutional Review Board of Kyung-Hee University Oriental Medicine Hospital in Gangdong (KHNMCOH 2023-09-003). The results will be disseminated through peer-reviewed publications.
Trial registration: This trial was registered with the Clinical Research Information Service (CRIS), Republic of Korea, No. KCT0008937 and was registered on November 10, 2023.
1 Introduction
Hwabyung is a disorder that is culturally specific to Korea (1). It is a syndrome in which negative emotions such as anger cannot be resolved and explode. According to previous research, physical symptoms include chest stuffiness, heat, feeling of something pushing up, and the feeling of a lump in the throat or pit of the stomach (2). Psychological symptoms include feelings of unfairness, resentment, and anger (2). Symptoms have been reported to be associated with specific stressful events (3). Research on the diagnosis of Hwabyung commenced in the 2000s, and the diagnostic criteria were first established by Kim et al. (2). When standardized diagnostic criteria are applied, the prevalence of Hwabyung in Koreans has been reported to range between 4.2-13.3% (4–7). Treatment for Hwabyung is generally provided by Korean medicine doctors (3).
In Korean medicine, it is believed that Hwabyung manifests as a result of problems with the circulation and regulation of ‘Qi.’ According to Donguibogam, a classic in Korean medicine literature, physical and psychological problems occur when Qi is not properly circulated (通卽不痛 不通卽痛) (8). Hwabyung is understood as a state of psychological blockage caused by persistent unresolved resentment in which the emotion of anger is biased upward and, as a consequence, Qi cannot circulate properly (9). To treat these symptoms, Korean medicine aims to achieve balance and harmony between the mind and body through the optimal circulation of Qi.
Depression is a mental health problem characterized by absence of positive emotions such as interest and pleasure, and a depressed mood (10). It is a mental illness that not only negatively affects an individual's quality of life, but also their overall occupational and social functioning (11). Depressive disorder is a common disease occurring worldwide. More than 185 million people were diagnosed with depression in 2019, and its prevalence is reportedly higher among women (3.07%) than men (1.89%) (12). In the 2019 Global Burden of Disease Study, the disease burden of depressive disorder ranked 13th among the top 25 diseases, showing a disease burden similar to that of AIDS, cirrhosis, lung cancer, and headache (13). In particular, it can be said that symptoms of depression have become more serious due to the recent impact of COVID-19 (14).
Hwabyung and depressive disorder have a high comorbidity rate. Epidemiological surveys have shown that 44% of the patients with Hwabyung have depressive disorder (15). Considering the fact that previous research (16) has demonstrated that 28.5% of patients with depressive disorder have generalized anxiety disorder as a comorbidity, it can be considered that Hwabyung and depressive disorder have a very high comorbidity rate. Therefore, in patients with depressive disorder, differential diagnosis and combined treatment for Hwabyung should be considered.
Recently, various mind-body interventions, such as mindfulness and Qigong, have been proposed as alternatives for treating mental disorders while minimizing the side effects of drugs. Mindfulness, which based on traditional Buddhist practices, is operationally defined as “paying attention in a particular way: on purpose, in the present moment, and nonjudgmentally” (17). Mindfulness, a non-judgmental concentration on the present moment, results in a relaxation response associated with activation of the parasympathetic nervous system (18). Mindfulness helps patients with depression or Hwabyung stay in the present moment and not trapped in negative thoughts or past resentment (19, 20). Based on these principles of mindfulness, a standardized program has been developed for emotional regulation, including stress reduction and prevention of depressive relapse (19, 21). In fact, mindfulness-based programs have been shown to improve depression in patients with depressive disorders and university students (22, 23), as well as Hwabyung in middle-aged females (20).
Qigong, which has its basis in the Taoist tradition, is a system of practices intended to cultivate control over life energy, known as Qi, through various body postures and movements, deep breathing, and mental concentration (24). Qigong is a broad concept that includes both static and movement-based practices, and is classified into various methods depending on tradition, such as Ba Duan Jin, Liu Zi Jue, Wu Qin Xi, and Kouksundo (25). The broad concept of Qigong and its diverse methods make it difficult to standardize programs. To compensate for these limitations and increase reproducibility in follow-up studies, this study defined Qigong operationally as feeling, accumulating, and utilizing Qi. Previous studies have shown that Qigong improves depression and Hwabyung (26, 27). The effects of Qigong on emotional regulation are explained by mindfulness. Qigong, along with Tai Chi and yoga, is referred to as meditative or mindful movement (28, 29), and is considered to share the therapeutic mechanisms of mindfulness meditation for emotional regulation (30). From a Korean medicine perspective, Qigong is believed to ameliorate Hwabyung and depression through the regulation of Qi (8, 9).
This study aims to investigate the effectiveness of Mindfulness and Qigong Training for Self-Healing (MQT-SH) from the comorbidity of depression and Hwabyung. The MQT-SH is a standardized Korean medicine mind-body intervention that aims to achieve a healthy balance between the mind and body (9). The primary hypothesis is that MQT-SH significantly reduces Hwabyung and depression in comparison to the control group. The secondary hypothesis is that MQT-SH reduces anxiety and anger while increasing vitality compared to the control group.
2 Methods
2.1 Trial design
This study is designed as a two-arm block randomized controlled trial. Patients will be assigned to either the experimental or the control group. The trial will be conducted for a duration of 12 weeks. During the first six weeks, the experimental group will receive MQT-SH, while the control group will receive no treatment as a waiting list control (WLC). During the next six weeks, the control group will receive MQT-SH with consideration for ethical equity. Assessments will be performed at three points: baseline (T1), post-intervention (T2; 6 weeks), and follow-up (T3; 12 weeks).
This trial was registered with the Clinical Research Information Service (CRIS), Republic of Korea (KCT0008937). This trial complies with the SPIRIT guidelines and will be conducted in accordance with the tenets of Declaration of Helsinki. Figure 1 presents a flow chart representing the overview of the study design.
2.2 Study setting
This trial will be conducted at Kyung Hee University Korean Medicine Hospital in Gangdong, South Korea. Participants will be recruited through advertisements in hospital and subways. Potential participants interested in participating will be informed about the study. If they agree to participate, they will be screened to assess the inclusion and exclusion criteria.
2.3 Eligibility criteria
Participants will be included if they i) have simultaneously been diagnosed with Hwabyung and depressive disorder by the Hwa-Byung Diagnostic Interview Schedule (HBDIS) (2) and Structured Clinical Interview for DSM-5 (SCID-5) (31); ii) are ≥ 19 years of age; and iii) can participate in the study by considering the timetable.
2.4 Interventions
Participants will be randomly assigned to either MQT-SH or WLC.
2.4.1 Mindfulness and Qigong training for self-healing
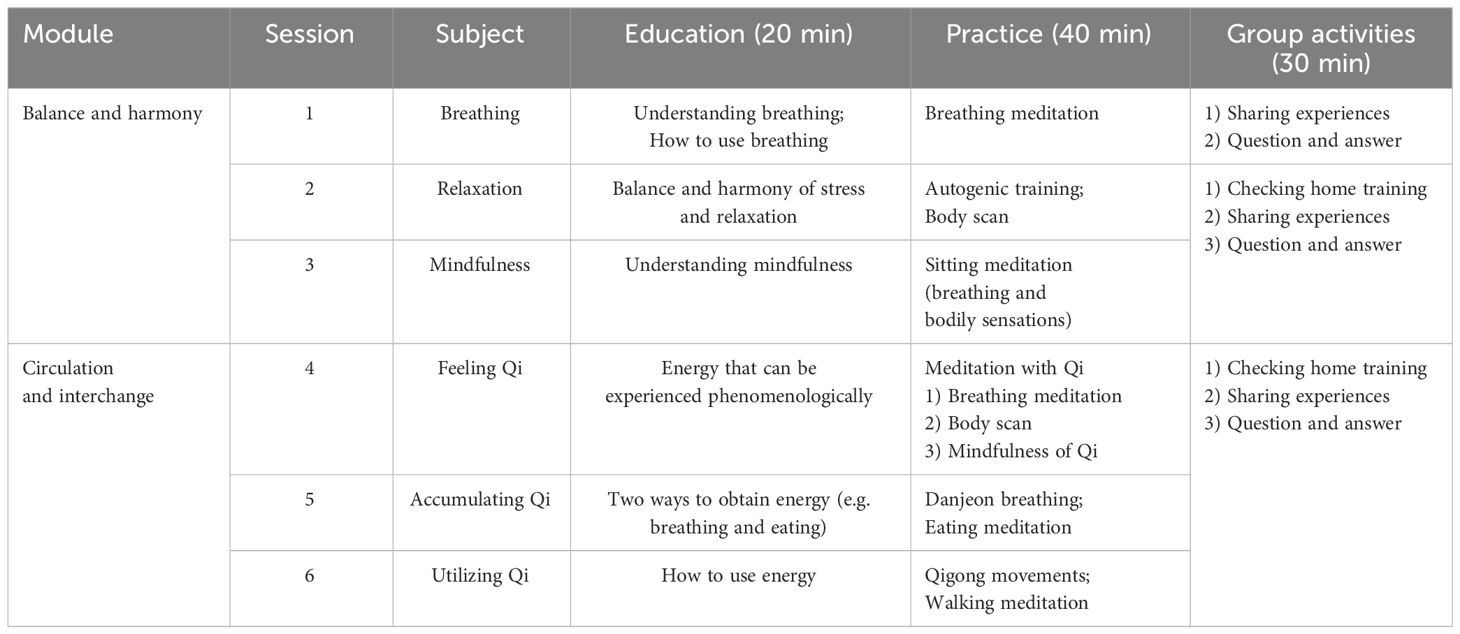
The experimental group will perform MQT-SH for the first six weeks. MQT-SH is a standardized mindfulness- and Qigong-based program to enhance self-healing (9). The goal of MQT-SH is to achieve optimal physical and psychological conditions. To achieve this goal, MQT-SH consists of two modules: i) balance and harmony, and ii) circulation and interchange. According to the traditional Oriental medicine, excessive emotions cause physical and psychological problems (32), and these imbalanced problems can be solved through circulation and interchange of energy (33). Balance and harmony have recently become the core principles of health and well-being across various cultures (34–36).
The balance and harmony module consists of the 1st to 3rd sessions. This module emphasizes the balance of inhalation/exhalation, sympathetic/parasympathetic nervous systems, and past/future/present for health. This module teaches various mindfulness-based training for healthy balance. In the first session, the participants will be taught the meaning of breathing and how to use it. Subsequently, breathing meditation will be performed. Breathing meditation involves counting numbers or adding words while concentrating on breathing. In the second session, participants will be educated about the balance and harmony of stress and relaxation. After educating the patients, body scan and autogenic training will be performed. In the third session, the participants would be educated on the meaning of mindfulness, and sitting meditation will be performed subsequently. Sitting meditation focuses on the awareness of breathing and bodily sensations.
The circulation and interchange module consists of the 4th to 6th sessions. This module teaches Qigong to encourage proper circulation and interchange of Qi. In MQT-SH, Qigong is operationally defined in three ways: feeling, accumulating, and utilizing Qi. In the fourth session, participants will be educated about the energy that could be experienced phenomenologically, and after education, meditation with Qi will be performed. The goal of meditating with Qi is to sensuously experience Qi in a comfortable and calm state. Meditation with Qi consists of breathing meditation, body scan, and mindfulness of the energy called Qi. In the fifth session, two ways of obtaining energy (e.g., breathing and eating) would be taught to the participants. Moreover, Danjeon breathing and eating meditations will be performed. In the sixth session, participants will be taught to use energy, and simple Qigong movements and walking meditation will be performed. Table 1 provides the detailed structure by session.
The MQT-SH period may vary depending on the setting (9). A manual for researchers and participants was developed to improve compliance to the intervention protocol. In this study, the MQT-SH will be conducted once a week for 1.5 h for a total of six weeks. Each session will consist of 20 min of education, 40 min of practice (i.e., meditation), and 30 min of group activities, such as checking home training and sharing practice experiences. This intervention will be conducted as a group program, with a maximum of 12 people per group. Participants will be asked to perform home training five times a week for at least 30 min each day. Participants will receive guided audio materials for home training. Dropouts will be defined as i) individuals attending three or less out of six sessions, ii) those who complain of physical or psychological discomfort and want to give up because of such discomfort, or iii) those who would want to give up for reasons other than discomfort.
2.4.2 Wait-list control
The control group will be assigned to WLC and will receive no treatment for the first six weeks. Considering ethical equity, the control group will undergo the same MQT-SH over the next six weeks.
2.5 Sample size
The sample size was estimated using G*power (37). The sample size calculation is based on a power of 80% and a type I error of 5%, as well as a moderate effect size for the intervention (partial η2 = 0.04). A minimum sample size of 25 participants per group is estimated (50 participants in total). This number was obtained by performing a simulation procedure using repeated-measures ANOVA, considering the existence of a significant 2 (group: experimental vs. control) × 2 (time: T1 vs. T2) interaction effect. Considering a dropout rate of 20%, we aim to include 32 participants per group (64 participants in total).
2.6 Randomization
Participants will be randomly allocated to either the experimental or the control group (1:1 ratio, block size = 4). Random numbers for allocation will be generated by the computer and managed by the researcher (YSI). Before enrollment, the participants and other researchers will be unaware of the allocation. After enrollment, YSI will allocate participants to the experimental or control group according to random numbers, and the results of the allocation will be shared only with the clinical research coordinator.
2.7 Blinding
In this clinical trial, assessors will be blinded. However, participants and practitioners will not be blinded. The assessors will be blinded to the intervention group and prevented from speaking with the participants, except during the clinical interviews.
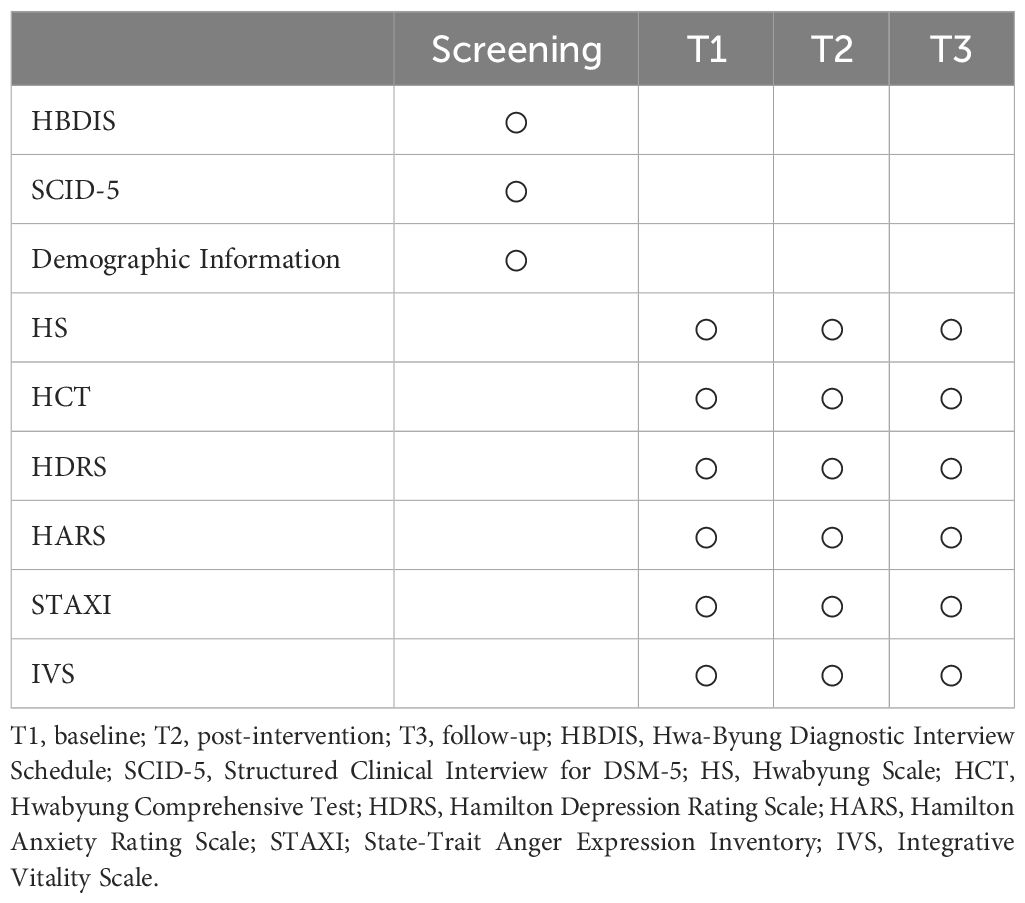
2.8 Assessment
Assessments are scheduled at baseline (T1), post-intervention (six weeks; T2), and follow-up (12 weeks; T3). Assessments include observer ratings (conducted by blinded clinicians) and self-report ratings. A structured interview manual will be used to increase the reliability of observer ratings (e.g., 38, 39). If participants drop out, they will not be assessed further. Missing data will be statistically imputed. Table 2 summarizes the assessment time points.
2.9 Primary outcomes
2.9.1 Hwabyung scale
The Hwabyung scale (40) will be used to assess Hwabyung-related personality and symptoms. This scale comprises 16 items on Hwabyung personality and 15 items on Hwabyung symptoms. This is a self-reported 5-point Likert scale. The total score ranges from 0 to 64 for Hwabyung personality, and from 0 to 60 for Hwabyung symptoms. Higher scores indicate higher Hwabyung personality and symptoms. In a previous study (40), the Cronbach's alpha for the Hwabyung scale was .85 for Hwabyung personality, .93 for Hwabyung symptoms, and .93 overall.
2.9.2 Hwabyung comprehensive test
The Hwabyung Comprehensive Test (41) will be used to assess Hwabyung-related symptoms and psychological characteristics. This test consists of 13 items on Hwabyung symptoms, 5 items on the incident questionnaire, and 21 items on Hwabyung psychological characteristics. Hwabyung symptoms and psychological characteristics will be used to interpret scores. This test is a self-reported 5-point Likert scale. The total score ranges from 0 to 52 for Hwabyung symptoms, and from 0 to 84 for Hwabyung psychological characteristics. Higher score indicates more severe Hwabyung symptoms and vulnerability. In a previous study (41), the Cronbach's alpha for the Hwabyung Comprehensive Test was .89 for Hwabyung symptoms and .95 for Hwabyung psychological characteristics.
2.9.3 Hamilton depression rating scale
In this study, a structured interview manual will be used to increase inter-rater reliability.
The Korean version of the Hamilton Depression Rating Scale (42) will be used to assess depression. This is an observer rating scale consisting of 17 items. Each item is scored from 0 to 2 or from 0 to 4. The total score ranges from 0 to 52. Higher scores indicate more depressive symptoms. In this study, a structured interview manual will be used to increase the inter-rater reliability (39).
2.10 Secondary outcomes
2.10.1 Hamilton anxiety rating scale
The Hamilton Anxiety Rating Scale (43) will be used to assess anxiety. This is an observer rating scale consisting of 14 items. Each item is scored from 0 to 4. The total score ranges from 0 to 56. Higher scores indicate higher anxiety symptoms. In this study, a structured interview manual will be used to increase the inter-rater reliability (38).
2.10.2 State-trait anger expression inventory
The Korean Adaptation of the State-Trait Anger Expression Inventory (44) will be used to assess anger experiences and expression. This scale consists of 10 items for state anger, 10 items for trait anger, and 24 items for anger expression. This is a self-reported 4-point Likert scale. The total score ranges from 10 to 40 for state anger, 10 to 40 for trait anger, and 24 to 96 for anger expression. Anger expression consists of three factors: anger-out, anger-in, and anger control. Anger control is considered a functional expression of anger and will be reverse calculated. A higher score indicates experiencing and expressing more anger. In a previous study (44), Cronbach's alpha was .90 for state anger, .75 for trait anger, .70 for anger-out, .66 for anger-in and, .79 for anger-control.
2.10.3 Integrative vitality scale
The Integrative Vitality Scale is a self-reported questionnaire that is under development to measure physical and psychological vitality. This scale consists of 11 items on physical vitality (e.g., My body is full of energy) and 11 items on psychological vitality (e.g., I have a passion for life). This is a self-reported 5-point Likert scale. The total score ranges from 0 to 44 for physical vitality and from 0 to 44 for psychological vitality. One item (e.g., My head feels heavy and achy) will be reverse-calculated. Higher scores indicate higher subjective vitality. In a survey of 348 people, Cronbach's alpha was .91 for physical vitality, .91 for psychological vitality, and .94 overall (preparing for publication).
2.11 Adverse events
Adverse events will be assessed after each session of MQT-SH. The results section will describe the type, frequency, and severity of the adverse events. Severity will be assessed according to three grades (mild, moderate, or severe). Mild is defined as an adverse reaction that does not interfere with daily life. Moderate is defined as an adverse reaction that interferes with daily life but is not dangerous. Severe is defined as an adverse reaction that is severe and interferes with basic daily activities (e.g., eating, changing clothes).
2.12 Data management
All the data will be encrypted and stored on the researcher's computer. Personally identifiable information will not be included in publications. Personal information will be stored together with the data for a maximum of 10 years, after which they will be destroyed.
2.13 Statistical analyses
Analyses based on the Intention-To-Treat (ITT) principle will be conducted, with missing data imputed using expectation-maximization (EM) algorithm.
To investigate the effect of MQT-SH, 2 (group: MQT-SH vs. WLC) × 2 (time: T1 vs. T2) repeated measures ANOVA will be performed. If the interaction between the group and time is significant, a simple main effect analysis will be performed.
Additional analyses will be performed. First, to investigate the follow-up effect of the MQT-SH, a paired t-test will be performed to compare T3 and T1 and T3 and T2 in the experimental group alone. Second, a paired t-test comparing T3 and T2 in the control group will be performed to investigate the effects of MQT-SH. Third, a subgroup analysis will be performed to investigate the difference in effectiveness depending on the amount of home training. For this purpose, 2 (amount: top 30% vs. bottom 30%) × 2 (time: pre-intervention vs. post-intervention) repeated-measures ANOVA will be performed. Data from both the experimental and control groups will be used for subgroup analysis.
3 Discussion
The purpose of this study is to investigate the effectiveness of a mindfulness and Qigong program for patients with depression and Hwabyung. This study is designed as a two-armed block randomized controlled trial. This study will primarily investigate the effectiveness of MQT-SH on Hwabyung, depression, anxiety, anger, and vitality. Additionally, this study will investigate the follow-up effect of MQT-SH and perform a subgroup analysis to compare the differences in the effect according to the amount of home training.
While depression is characterized by a sad mood or absence of joy or interest (10), Hwabyung is characterized by a combination of physical (chest tightness, heat, etc.) and psychological (resentment, resentment, etc.) symptoms related to anger (2). Although depression and Hwabyung have different diagnostic criteria, they have a high likelihood of comorbidity (15). In fact, 44.1% of patients with Hwabyung were diagnosed with depressive disorder, and 18.3% were diagnosed with both depressive and anxiety disorders (45). This suggests that Hwabyung is not only related to depression, but also to anxiety. Therefore, interventions are needed to comprehensively deal with various emotional problems such as depression, anxiety, and anger.
Mindfulness and Qigong can be used as transdiagnostic approaches for improving emotion regulation. Previous studies have shown that mind-body interventions, such as mindfulness and Qigong, improve depression, anxiety, and anger (27, 46–48). Mindfulness is a basic factor in several mind-body interventions and is considered a Qigong therapeutic mechanism for emotional regulation (20). This study investigates whether mindfulness and Qigong interventions improve emotional regulation in patients with Hwabyung and depressive disorder. MQT-SH is a standardized mind-body intervention that combines mindfulness and Qigong (9). This study adhered to the standard procedure of MQT-SH, but made some modifications to the period and content in consideration of the study setting and participants.
The control group in this study is a non-active group. For ethical reasons, the control group will perform MQT-SH for six weeks between the T2 and T3 assessments. Therefore, the main statistical analysis is a comparison of the two groups for T1 and T2 assessments. Additionally, a follow-up effect analysis will be conducted in the experimental group alone, and a single-arm pre-post effect analysis will be conducted in the control group. Finally, a subgroup analysis will be conducted based on the amount of home training.
3.1 Limitations
The results of this study may have several limitations. First, the participants and intervention instructor are not blinded. The control group is a non-active group; therefore, the participants are not blinded. In addition, due to the nature of the intervention, where meditation and Qigong are directly guided, the intervention instructor also cannot be blinded. However, the researchers conducting observer ratings will be blinded. Second, this study is a single-center trial. A single-center approach has the advantage of complying with the study protocol in comparison to a multicenter trial. However, this may have implications for generalizability and external validity.
3.2 Conclusion
In conclusion, this study will provide empirical results on the effectiveness of a standardized mindfulness and Qigong program for patients with Hwabyung and depressive disorder. This study will be an opportunity to investigate the possibility of a low-risk practical treatment for emotional problems in clinical settings.
3.3 Trial status
Recruitment, enrollment and treatment of participants has started. Follow-up assessments for the last participant are expected to be completed by September 2024.
Ethics statement
This study was approved by the Institutional Review Board (IRB) of Kyung-Hee University Oriental Medicine Hospital in Gangdong (KHNMCOH 2023-09-003). Written informed consent will be obtained from all the participants prior to their inclusion in the study. If the study protocol is changed, it will be reviewed by the IRB. The results of this study will be disseminated through publication submissions in peer-reviewed journals.
Author contributions
S-IY: Conceptualization, Writing – original draft. H-YP: Writing – original draft. HL: Writing – review & editing. CP: Writing – review & editing. S-YC: Conceptualization, Writing – review & editing. JWK: Conceptualization, Funding acquisition, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study is financially supported by the Korea Health Industry Development Institute (KHIDI) in Korea (Project number: HF20C0079). The funding did not and will not have any implication on the design of the study, collection, analysis, and interpretation of data, or in writing the manuscript.
Acknowledgments
We would like to express our gratitude to all the patients and research assistants who would be participating in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1336656/full#supplementary-material
References
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. Arlington, VA: American Psychiatric Press Inc (2000).
2. Kim JW, Kwon JH, Lee MS, Park DG. Development of Hwa-Byung diagnostic interview schedule (HBDIS) and its validity test. Korean J Health Psychol. (2004) 9:321–31.
3. The Korean Society of Oriental Neuropsychiatry. Korean Medicine Clinical Practice Guideline for Hwabyung. Seoul, Republic of Korea: National Institute for Korean Medicine Development Clinical Practice Guideline of Korean Medicine Development Project Group (2021). p. 3.
5. Min SK, Kim JH. A study on Hwabyung in Bokil island. J Korean Neuropsychiatr Assoc. (1986) 25:459–66.
6. Kim H-K, Park J-Y. Prevalence and related factors of Hwabyung for the aged woman in rural community. J Korean Public Health Nurs. (2004) 18:234–42.
7. Lee J-G, Lee J-H. Study on the prevalence of Hwa-Byung diagnosed by HBDIS in general population in Kang-won province. J Orient Neuropsychiatry. (2008) 19:133–9.
9. Kim JW, Suh HW, Yoon SI. Mindfulness and Qigong Training for Self-Healing: Korean Medicine Counselling Workbook 1. Seoul: Jipmoondang (2022).
10. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5. Washington, DC: American Psychiatric Association (2013). doi: 10.1176/appi.books.9780890425596
11. Adler DA, McLaughlin TJ, Rogers WH, Chang H, Lapitsky L, Lerner D. Job performance deficits due to depression. Am J Psychiatry. (2006) 163:1569–76. doi: 10.1176/ajp.2006.163.9.1569
12. Institute for Health Metrics and Evaluation (IHME). GBD Results (2020). Available online at: https://vizhub.healthdata.org/gbd-results/ (Accessed September 19, 2023).
13. GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
14. Sun Y, Wu Y, Fan S, Dal Santo T, Li L, Jiang X, et al. Comparison of mental health symptoms before and during the covid-19 pandemic: Evidence from a systematic review and meta-analysis of 134 cohorts. BMJ. (2023) 380:e074224. doi: 10.1136/bmj-2022-074224
15. The Korean Society of Oriental Neuropsychiatry Hwabyung research center. Korean Medicine Clinical Practice Guideline for Hwabyung. Seoul, Republic of Korea: National Institute for Korean Medicine Development Clinical Practice Guideline of Korean Medicine Development Project Group (2013).
16. King-Kallimanis B, Gum AM, Kohn R. Comorbidity of depressive and anxiety disorders for older Americans in the national comorbidity survey-replication. Am J Geriatric Psychiatry. (2009) 17:782–92. doi: 10.1097/JGP.0b013e3181ad4d17
17. Kabat-Zinn J. Wherever you go there you are: Mindfulness meditation in everyday life. NY: Hyperion (1994).
19. Teasdale JD, Segal ZV, Williams JMG, Ridgeway VA, Soulsby JM, Lau MA. Prevention of relapse/recurrence in major depression by mindfulness-based cognitive therapy. J consulting Clin Psychol. (2000) 68:615. doi: 10.1037/0022-006X.68.4.615
20. You SY, Kim M, Kim JH. Effects of mindfulness meditation on symptoms of depression, anxiety, stress, and hwa-byung among middle-aged women with hwa-byung disorders. Korean J Health Psychol. (2014) 19:83–98. doi: 10.17315/kjhp.2014.19.1.005
22. Piet J, Hougaard E. The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clin Psychol Rev. (2011) 31:1032–40. doi: 10.1016/j.cpr.2011.05.002
23. González-Martín AM, Aibar-Almazán A, Rivas-Campo Y, Castellote-Caballero Y, Carcelen-Fraile MDC. Mindfulness to improve the mental health of university students. A systematic review and meta-analysis. Front Public Health. (2023) 11:1284632. doi: 10.3389/fpubh.2023.1284632
24. Tsang HWH, Cheung L, Lak DCC. Qigong as a psychosocial intervention for depressed elderly with chronic physical illnesses. Int J Geriatr Psych. (2002) 17:1146–54. doi: 10.1002/gps.739
25. Choi WY, Suh H-W, Kim JW. Analysis of clinical study trends on ‘Qigong’: A preliminary scoping review. J Oriental Neuropsychiatry. (2021) 32:207–17. doi: 10.7231/jon.2021.32.3.207
26. Oh BS, Choi SM, Inamori A, Rosenthal D, Yeung A. Effects of qigong on depression: A systemic review. Evidence-Based Complementary Altern Med. (2013) 2013:8. doi: 10.1155/2013/134737
27. Hwang E-Y, Chung S-Y, Cho J-H, Song M-Y, Kim S, Kim J-W. Effects of a Brief Qigong-based Stress Reduction Program (BQSRP) in a distressed Korean population: a randomized trial. BMC Complementary Altern Med. (2013) 13:113. doi: 10.1186/1472-6882-13-113
28. Payne P, Crane-Godreau MA. Meditative movement for depression and anxiety. Front Psychiatry. (2013) 4:71. doi: 10.3389/fpsyt.2013.00071
29. Pölönen P, Lappi O, Tervaniemi M. Effect of meditative movement on affect and flow in Qigong practitioners. Front Psychol. (2019) 10:2375. doi: 10.3389/fpsyg.2019.02375
30. Yeung A, Chan JS, Cheung JC, Zou L. Qigong and Tai-Chi for mood regulation. Focus. (2018) 16:40–7. doi: 10.1176/appi.focus.20170042
31. First MB, Williams JBW, Karg RS, Spitzer RL. Structured Clinical Interview for DSM-5, Clinician Version (SCID-5-CV). Arlington, VA: American Psychiatric Association (2015).
32. Choi WJ. A study on psychophysiology and psychopathology of korean medicine -focus on emotion and thought in huangdineijing. J Oriental Neuropsychiatry. (2018) 29:21–34. doi: 10.7231/jon.2018.29.1.021
34. Hodge DR, Limb GE, Cross TL. Moving from colonization toward balance and harmony: A Native American perspective on wellness. Soc Work. (2009) 54:211–9. doi: 10.1093/sw/54.3.211
35. Lomas T. Life balance and harmony. Int J Wellbeing. (2021) 11:50–68. doi: 10.5502/ijw.v11i1.1477
36. Lomas T, Ishikawa Y, Diego-Rosell P, Daly J, English C, Harter J, et al. Balance and harmony in the Gallup World Poll: The development of the Global Wellbeing Initiative module. Int J Wellbeing. (2022) 12:1–19. doi: 10.5502/ijw.v12i4.2655
37. Faul F, Erdfelder E, Lang AG, Buchner A. G* Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. (2007) 39:175–91. doi: 10.3758/BF03193146
38. Bruss GS, Gruenberg AM, Goldstein RD, Barber JP. Hamilton Anxiety Rating Scale Interview guide: joint interview and test-retest methods for interrater reliability. Psychiatry Res. (1994) 53:191–202. doi: 10.1016/0165-1781(94)90110-4
39. Williams JB. A structured interview guide for the Hamilton Depression Rating Scale. Arch Gen Psychiatry. (1988) 45:742–7. doi: 10.1001/archpsyc.1988.01800320058007
40. Kwon JH, Kim JW, Park DG, Lee MS, Min SG, Kwon HI. Development and validation of the hwa-byung scale. Korean J Clin Psychol. (2008) 27:237–52. doi: 10.15842/kjcp.2008.27.1.014
42. Yi JS, Bae SO, Ahn YM, Park DB, Noh KS, Shin HK, et al. Validity and reliability of the Korean version of the Hamilton Depression Rating Scale (K-HDRS). J Korean Neuropsychiatr Assoc. (2005) 44:456–65.
43. Hamilton MAX. The assessment of anxiety states by rating. Br J Med Psychol. (1959) 32:50–5. doi: 10.1111/j.2044-8341.1959.tb00467.x
45. Kim JW, Chung SY, Suh HU, Jung IC, Lee SG, Kim BK, et al. The characteristics of Hwa-byung patients based on Hwa-byung epidemiologic data. J Oriental Neuropsychiatry. (2010) 21:157–69.
46. Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. J Consulting Clin Psychol. (2010) 78:169–83. doi: 10.1037/a0018555
47. Liu X, Clark J, Siskind D, Williams GM, Byrne G, Yang JL, et al. A systematic review and meta-analysis of the effects of Qigong and Tai Chi for depressive symptoms. Complementary Therapies Med. (2015) 23:516–34. doi: 10.1016/j.ctim.2015.05.001
Keywords: Hwabyung, depressive disorder, mindfulness, Qigong, randomized controlled trial
Citation: Yoon S-I, Park H-Y, Lee HW, Park C, Chung S-Y and Kim JW (2024) Effectiveness of mindfulness and Qigong training for self-healing in patients with Hwabyung and depressive disorder: a protocol for a randomized controlled trial. Front. Psychiatry 15:1336656. doi: 10.3389/fpsyt.2024.1336656
Received: 11 November 2023; Accepted: 05 April 2024;
Published: 17 April 2024.
Edited by:
Todd Knowlton Favorite, University of Michigan, United StatesReviewed by:
James Svensson, University of Michigan, United StatesCiro Conversano, University of Pisa, Italy
Copyright © 2024 Yoon, Park, Lee, Park, Chung and Kim. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jong Woo Kim, aromaqi@khu.ac.kr
 Seok-In Yoon
Seok-In Yoon Hui-Yeong Park
Hui-Yeong Park Hyun Woo Lee2
Hyun Woo Lee2