- 1Center for Clinical Big Data and Analytics of the Second Affiliated Hospital, and Department of Big Data in Health Science School of Public Health, The Key Laboratory of Intelligent Preventive Medicine of Zhejiang Province, Zhejiang University School of Medicine, Hangzhou, China
- 2Department of Neurology/Center for Sleep Medicine, Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, China
- 3Department of Internal Medicine of Traditional Chinese Medicine, Shaoxing Hospital of Traditional Chinese Medicine, Shaoxing, China
- 4Department of Neurology, Affiliated Hospital of Shaoxing University, Shaoxing, China
Background: Sleep disorders such as insomnia can lead to a range of health problems. The high risk of side effects and drug abuse of traditional pharmacotherapy calls for a safer non-pharmacotherapy.
Aims: To examine the use and efficacy of weighted blankets in improving sleep and related disorders in different populations and explore the possible mechanisms.
Methods: A literature search was conducted using PubMed, Embase, Web of Science, MEDLINE, Cochrane Library and CNKI databases. Eligible studies included an intervention with weighted blankets and outcomes covering sleep and/or related disorders (behavioral disturbance, negative emotions and daytime symptoms). Studies using other deep pressure, compression, or exercise-related interventions were excluded.
Conclusions: Most of the included studies showed that weighted blankets could effectively improve sleep quality and alleviate negative emotions and daytime symptoms in patients with sleep disorders, attention deficit hyperactivity disorder, autism spectrum disorder, and other related disorders, with a possible mechanism of deep pressure touch.
Recommendations: Weighted blankets might be a promising tool for sleep interventions among individuals with sleep disorders in clinical settings. More high-quality and large-scale randomized controlled trials are needed to further validate the safety and efficacy of weighted blankets and explore precise mechanisms.
1 Introduction
Quality sleep is essential for psychological, cardiovascular, metabolic, and other aspects of health (1). However, during the COVID-19 pandemic, with about 40% of people reporting sleep problems, sleep-related problems have become more severe and were particularly prominent in some populations, including children and adolescents (2, 3). Sleep disorders, such as insomnia, are common risk factors for many psychiatric disorders and may also be a symptom of mental health disorders (4, 5). In any case, effective interventions for insomnia should be provided to prevent the development of sleep disorders and alleviate other mental health problems (6, 7). Common treatments for insomnia are mainly pharmacotherapy and cognitive behavioral therapy (non-pharmacotherapy), with the latter being preferred for its safety and durability (8, 9). However, about 40% of patients with persistent insomnia do not respond to cognitive behavioral therapy combined medication treatment (10). In addition, pharmacotherapy for insomnia often leads to a high risk of side effects and drug abuse. In adverse drug reaction studies, the highest reporting odds ratios of somnolence are 7.1 and 13.3 for patients prescribed antidepressants (11) and antipsychotics (12), respectively. For patients prescribed higher dose Z-drugs, the hazard ratios of fractures, hip fractures, ischaemic stroke, and falls ranged from 1.33 to 1.96 (13). Thus, a safer non-pharmacotherapy needs to be explored.
Weighted blanket, an emerging non-pharmacotherapy, has gradually entered people’s vision. A weighted blanket is usually made of special weight-adding materials such as beads and chains, allowing it to cover the body evenly and create a pleasant hugging sensation. As a non-invasive intervention assistive device, a weighted blanket was initially suggested as a prescription or treatment option by occupational therapists for patients with sleep problems (14). To date, weighted blankets have been increasingly used in sleep interventions for different populations, such as patients with insomnia, attention deficit hyperactivity disorder (ADHD), and autism spectrum disorder (ASD), and have shown positive effects on relieving insomnia, anxiety, and fatigue (15, 16). Only one previous review has evaluated the effect of weighted blankets on decreasing anxiety and insomnia using 8 studies conducted before March 1, 2018 (17). However, the use of weighted blankets for wider targets has surged in recent years, calling for an updated and comprehensive review of the effect of weighted blankets in different populations and the in-depth mechanisms.
Therefore, this narrative review summarized the use and efficacy of weighted blankets in sleep and other related disorders (e.g., behavioral disturbance, negative emotions and daytime symptoms) in different populations and discussed the relevant mechanisms to provide a reference for a comprehensive overview of the research status of weighted blankets and make recommendations for an alternative therapy to medications of sleep and sleep-related disorders in clinical settings.
2 Materials and methods
We searched in PubMed, Embase, Web of Science, MEDLINE, Cochrane Library and CNKI using optimized search strategies up to March 10, 2023. We determine the search terms using appropriate controlled vocabulary terms. The final search terms consisted of “weighted blankets”, “gravity blankets”, “ball blankets”, “sleep”, and “sleep quality”. Studies were limited to those published in English.
A study was included if it met the following criteria: (1) it included an intervention with weighted blankets; (2) it reported parameters that assessed the sleep quality (e.g., sleep latency, sleep duration, sleep efficiency, and number of wakings) and/or related disorders (e.g., behavioral disturbance, negative emotions and daytime symptoms). A study was excluded if it used other deep pressure, compression, or exercise-related interventions. Furthermore, letters, study protocols, guidelines, dissertations, and thesis were excluded.
We read the titles and abstracts to identify all relevant studies using the inclusion and exclusion criteria above. Then, two reviewers worked independently to assess each included study and resolved any discrepancies through discussion (see flow chart in Supplementary Figure 1).
3 Results
3.1 Application of weighted blankets in improving sleep
Sleep disturbance, a symptom or harbinger of psychiatric problems, can be comorbid with psychiatric disorders and increases the risk of psychiatric relapse (18). To improve sleep quality and reduce the negative impact of sleep disturbance on psychiatric disorders, occupational therapists have attempted to use a weighted blanket as a safer physical therapy (19). A randomized controlled trial in Sweden has provided primary evidence for weighted blankets’ efficacy in relieving insomnia and daytime fatigue in patients with psychiatric disorders (16). Besides, another randomized controlled study showed that after using weight blankets, insomniacs had improved sleep quality, shorter nighttime awakenings, reduced self-reported stress, and enhanced relaxation (20). For older people living in nursing homes, weighted blankets also have positive effect on improving sleep especially concerning waking up during the night (21). Furthermore, weighted blankets have also been used to treat sleep disorders in children with ADHD, ASD, and CHARGE syndrome (22–24). Interestingly, a review on non-traditional clinical treatments for improving sleep in children and young people suggested that although the weighted blankets intervention did not result in significant differences in sleep indicators, there was positive feedback on self-reports from subjects and caregivers (23). This finding revealed a difference in the efficacy between subjective and objective sleep measurements. Non-significant effects on subjective sleepiness and total sleep duration were observed in an in-laboratory crossover study. However, the significant increase of salivary melatonin in this study provided new evidence for the sleep-promoting mechanisms of weighted blankets (25).
3.2 Application of weighted blankets in ADHD and ASD
Several studies have used weighted blankets as an intervention for patients with neurodevelopmental disorders, including ADHD and ASD. Most of them indicated a beneficial impact of weighted blankets on the improvements in sleep quality (e.g., sleep onset latency) and ADHD/ASD-related symptoms (e.g., concentration and daily function) in patients with AHDH or ASD (Table 1).
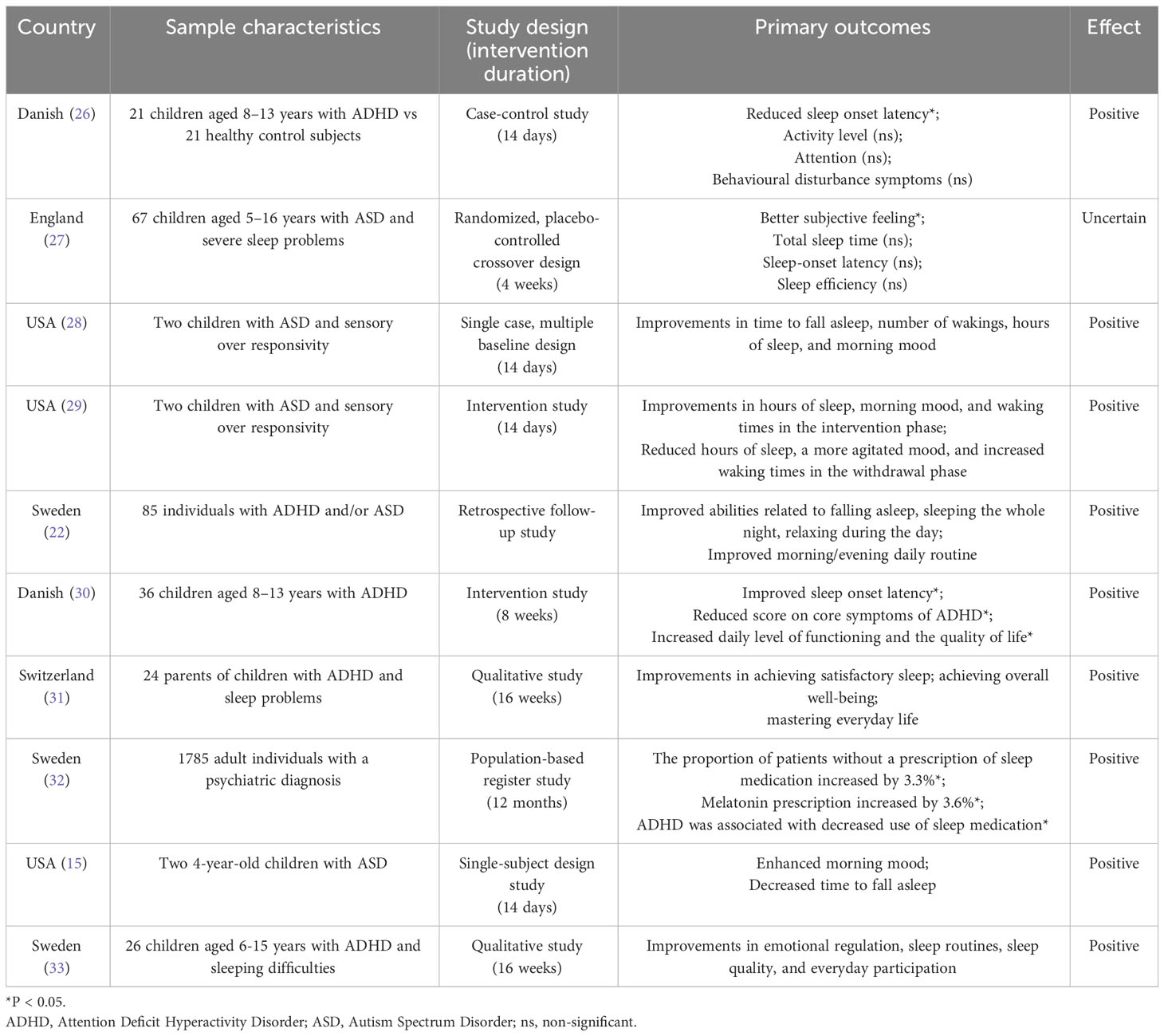
Table 1 Application of weighted blankets in attention deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD).
Specifically, a case-control study found that after using a weighted ball blanket for 14 days, children aged 8-13 years with ADHD had improvements in sleep onset latency, awakening times, concentration, and physical activities (26). Another Danish study also provided evidence for the positive effects on sleep onset latency, daily functioning levels, and quality of life in children with ADHD in the same age range after using weighted ball blankets for 8 weeks (30). Similarly, A qualitative study based on parents’ experiences of the impact of weighted blankets on children with ADHD and sleep disorders indicated that after 16 weeks of weighted blankets intervention, children could better master everyday life, and achieve satisfactory sleep and overall well-being (31). Another qualitative study based on children’s experiences revealed that the use of weighted blankets improved the emotional regulation, everyday participation and sleep quality of children with ADHD and sleeping difficulties (33). Moreover, in Idaho, USA, a single-subject design study (28) and two continuation studies (15, 29) in children with ASD and sleep disorders indicated that weighted blankets were beneficial for the improvement of overall sleep quality, especially the sleep onset latency, awakening times, sleep duration, and morning mood, although the effects were not sufficient to recommend for clinical use. However, a randomized, placebo-controlled crossover design trial observed that the use of weighted blankets did not help children aged 5-16 years with ASD and severe sleep problems obtain longer sleep duration, faster sleep onset, or fewer awakenings (27).
In addition to children, a randomized controlled study in Stockholm, Sweden, found that in adult patients with ADHD, a weighted chain blanket was also a safe and effective intervention for insomnia, which could improve adult patients’ daytime symptoms and activity levels (16). Interestingly, a population-based registry study indirectly demonstrated the positive effect of weighted blankets intervention on reducing the use of common sleep medication among ADHD patients (32). Moreover, another registry study found that patients with ADHD retained the weighted blankets longer than others, indicating a possible benefit from using weighted blankets (34). Likewise, a retrospective follow-up study in 2021 found that after interventions of a weighted chain or ball blanket, both adults and children with ADHD or ASD showed improvements in sleep, daytime relaxation, and morning/evening routine (children significantly benefited more in falling asleep than adults.) (22).
3.3 Application of weighted blankets in improving negative emotions
There are 17 studies (including one systematic review) related to weighted blankets intervention and psychological behaviors (e.g., anxiety, depression, and stress). Two single-subject design studies found that patients with nighttime weighted blanket intervention had a better morning mood, which could be agitated and unstable when the intervention was discontinued (15, 29). A retrospective follow-up study showed that weighted blankets benefited daytime relaxation in patients with ADHD/ASD (22). Furthermore, a randomized controlled study showed a positive effect of weighted chain blankets on depression and anxiety symptoms (16). However, two similar conference abstracts argued that weighted blankets could not reduce stress in patients with pain (35, 36), while another conference abstract indicated that weighted blanket could reduce self-reported stress and increase relaxation in patients with sleep disorders (20).
A few studies have focused on the effect on alleviating anxiety. A systematic review suggested that weighted blankets might be an appropriate therapeutic tool for reducing anxiety (17). Additionally, a controlled clinical trial in the United States based on a repeated crossover design found that compared to standard care, the use of weighted blankets for 30 minutes resulted in significantly lower anxiety levels (based on the visual analog scale for anxiety) in cancer patients undergoing outpatient chemotherapy infusion (37). Significant alleviation in anxiety (measured by pulse and a shortened form of the Spielberger State-Trait Anxiety Inventory [STAI: Y-6]) was also found among adult patients in mental health institutions after using weighted blankets (38). Moreover, a pilot study at a liberal arts university in the Midwest suggested that a weighted blanket may improve sleep quality and reduce anxiety among college students (39). Similar results were also found in patients with ADHD/ASD. Two qualitative studies on nursing home staff (40) and children with ADHD and sleep problems (31) also provided positive evidence that weighted blankets helped relax and reduced anxiety.
3.4 Application of weighted blankets in special populations
3.4.1 In patients with chronic pain
A total of three studies were conducted on patients with chronic pain. A randomized controlled trial showed that heavier-weighted blankets produced a greater alleviation in widespread chronic pain than the lighter-weighted blankets, and the effects were stronger in individuals with high trait anxiety (41). However, two of the Danish conference abstracts (36, 42) indicated that no difference of HbA1C, a reflection of stress, was found between patients with chronic pain in the weighted ball blanket group and the control blanket group.
3.4.2 In patients with dementia
Four studies have explored the effect of weighted blankets on patients with dementia. One intervention trial in female patients with late-stage of dementia found a significant reduction in the duration of sustained vocalizations after 10 min of weighted blanket intervention, suggesting that it was a promising non-pharmacological treatment for patients with dementia (43). Likewise, a prospective, within subjects, pre-post design study with a 4-week intervention indicated that weighted blankets were of high feasibility and acceptability for families living with dementia (44). Another case report in Japan demonstrated the effects of weighted blankets on alleviating sleep disorders in patients with Alzheimer’s and easing the caregiver’s burden (45). In addition, the longer use time of weighted blankets in patients with dementia provided indirect evidence that weighted blankets may be beneficial (34).
3.4.3 In patients with psychiatric disorders
Three studies were conducted on patients with different psychiatric disorders. A randomized controlled trial in Sweden showed that weighted blankets could improve insomnia, daytime symptoms, and activity levels in various psychiatric disorders (16). Another clinical trial concluded that weighted blankets could help patients in psychiatric hospitals better manage anxiety (38). A registry study also observed a statistically significant association between weighted blankets intervention and decreased use of common sleep medication in patients with psychiatric disorders (32).
3.4.4 Others
Several studies focused on the impact of weighted blankets on other special populations. One exploratory study showed that parents of children with CHARGE syndrome found weighted blankets slightly effective in improving children’s sleep problems (24). The positive effects of weighted blankets were also found in children under general anesthesia, indicating that weighted blankets can be safely used for hospitalized children (46). Another crossover randomized controlled trial in 16 infants with neonatal withdrawal syndrome (NAS) found no adverse events during 67 30-minute sessions with weighted blanket, confirming the safety, feasibility, and efficacy of weighted blanket in reducing NAS symptoms (47). Only one study proved that using weighted blankets for 30 minutes could reduce anxiety better than standard care among cancer patients (37).
3.5 Comparison of weighted blankets and drug therapy
Although sleep drugs have been widely used in clinical practice, the side effects of drugs (e.g., drug resistance and drug tolerance) could rebound after drug withdrawal, making it not a good option. Also, the adverse outcomes caused by drug abuse were still great troubles for patients with sleep disorders (48, 49). For these reasons, sleep drugs are not recommended for treating chronic sleep disorders and anxiety disorders, or people over 65 years old (50). Weighted blankets were considered one of the non-pharmacological approaches to alleviate sleep disorders in patients with ASD without adverse effects (51). Several studies directly compared weighted blankets with drug therapy from the rate of prescription (32), perceived efficacy (24), and economic cost (34), respectively. First, a population-based register study of 1785 adult individuals with a psychiatric diagnosis directly compared the subscription of common sleep drugs (benzodiazepine receptor agonists, antihistamines, melatonin, and mirtazapine) before and after receiving a weighted blanket prescription, and found a significant association between weighted blanket use and the reduced use of common sleep drugs except melatonin that increased slightly (32). Second, however, in a cross-sectional study of children with CHARGE syndrome, their parents rated weighted blankets less effective than melatonin in improving their sleep quality. One possible reason is that melatonin is a common treatment that is more trusted by parents when recommended by doctors (24). Besides, the cost of weighted blankets as a prescription is higher than sleep drugs, which may lead to easier use and acceptance of sleep drugs. The average cost of a weighted blanket prescription for six months is just under €190, compared with sleep medications for the same period that was slightly below €86 in western Sweden. The higher cost of weighted blankets was mainly due to the more lengthy and complex prescription process and less to the material (34). In general, a weighted blanket is a non-drug supplement nearly without side effects, which might be safer than drug therapy in sleep intervention. Due to lower adverse effects but higher economic cost, the prescription pattern of weighted blankets should be revised and systemized to reduce the costs and better identify the target populations who may benefit from weighted blankets.
4 Discussion
Our review summarized all available studies examining the use and efficacy of weighted blankets in improving sleep quality, ADHD/ASD-related symptoms, negative emotions, and other related disorders in different populations, indicating a variability in the results, but a majority of studies showed positive results. Although the efficacy in individuals with sleep disorders and ADHD/ASD showed stronger supporting evidence, further validations are still needed due to the non-significant or negative results reported by a few studies. Meanwhile, due to the differences in the populations, outcomes, and intervention strategies (e.g., duration and frequency) in the included studies, particular caution is required when generalizing the findings to other populations.
4.1 Mechanisms of weighted blankets
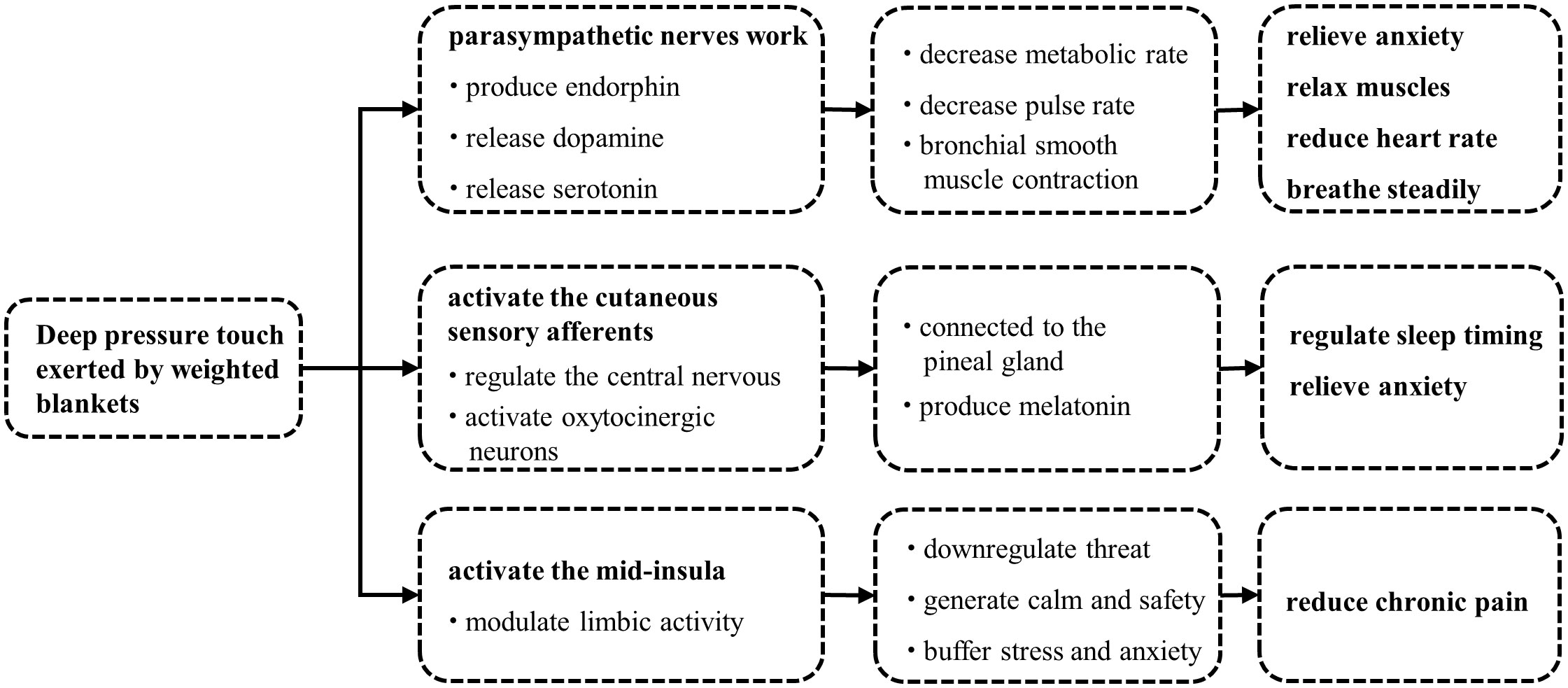
Deep pressure touch (DPT) is the most recognized mechanism of weighted blankets by researchers (Figure 1) (52, 53). DPT is a form of tactile input which can be provided by holding, touching, embracing, stepping, and squeezing (14). A weighted blanket can cause changes in sensory nerve endings through continuous mechanical stimulations such as touch and pressure to the skin, leading to the opening of mechanically gated sodium channels, Na+ influx, and the generation of receptor potentials. The sympathetic nerve deals with the body’s decision to fight or flight; if it takes over, individuals can experience nervousness, anxiety, fear, irritability, poor sleep, and even digestive problems (54). The parasympathetic nervous system has a calming effect, which determines the “rest and digestion” of the body (55). A weighted blanket is a typical application of DPT, and can stimulate the parasympathetic nervous system, which has been supported by previous physiological studies (53, 56). When the parasympathetic nerve works, it can produce endorphins and release dopamine and serotonin (57), while endorphins and dopamine can result in reduced heart rate, relieved anxiety, relaxed muscles, and steady breath (58), and consequently, conducing to staying asleep. In a study of various tactile stimulations ending apnea in preterm infants, deep pressure stimulation was effective in helping preterm infants return to spontaneous breathing quickly (59).
Furthermore, a recent in-laboratory crossover study found that weighted blankets increased pre-sleep salivary concentrations of melatonin in young, healthy adults (25), providing new evidence for the sleep-promoting mechanisms of weighted blankets. Melatonin is released by the pineal gland and plays a critical role in sleep timing and anti-anxiety (60, 61). One explanation could be that the deep pressure provided by the weighted blankets activates cutaneous sensory afferents that transmit sensory information to the nucleus tractus solitarius through the spinal cord. The nucleus tractus solitarius projects to the paraventricular nucleus of the hypothalamus, which hosts parvocellular oxytocinergic neurons (62). They subsequently connect to the pineal gland to affect the release of melatonin (63). Notably, a previous study showed that a total loss of afferent sensory signals was related to a complete absence of nocturnal melatonin increase, reinforcing that the peripheral sensory nervous system plays a critical role in regulating the release of melatonin from central nervous system (64).
Interestingly, weighted blankets also contributed to relieving perceived bodily pain (41). This may result from several mechanisms. First, given that chronic pain is determined in part by social and/or emotional factors (65, 66), we speculate that the deep pressure provided by a weighted blanket may downregulate threat and generate calm and safety through activation of the insula, thereby alleviating stress and anxiety and ultimately reducing perception of bodily pain (67, 68). Second, the deep pressure can increase local tissue oxygenation and blood flow. These peripheral effects may account for the antinociceptive function of the weighted blankets (69, 70).Third, studies have reported that deep pressure sensation is transmitted by A-beta afferents (71), which was found to suppress laser pain in the same dermatome at the spinal cord level (72), suggesting that deep pressure provided by a weighted blanket might reduce bodily pain through A-beta stimulation.
4.2 Current research gaps and potential developments
This review reflects several current research gaps in weighted blankets therapy. First, the sample size of most existing studies did not reach 100, calling for more large-scale studies. Second, there was a lack of prospective, parallel and controlled studies, with many existing studies being poor clinical trials or observational studies, indicating a huge evidence gap. High-quality randomized controlled trials with longer intervention duration are required to strengthen the level of evidence. Third, sleep measurements were mostly subjective, hence, the results lack credibility. Objective measurements such as actigraphy covering multiple sleep outcomes should be applied. In addition, it is necessary to distinguish between subjective and objective effects of the weighted blankets. For instance, a review on non-traditional sleep treatments in children and young people reported that the subjects and caregivers using weighted blankets had positive feedbacks, despite a lack of significant differences in their objective sleep indicators (23). Forth, a few studies were relatively weak in statistical analysis, such as uncontrolled confounding factors, inappropriate use of statistical methods, etc. Moreover, several studies were qualitative, and these conclusions need to be further confirmed by empirical research with rigorous statistical methods. Fifth, the limited evidence of how weighted blankets work indicates a need for more research into the potential mechanisms. Future research could explore how weighted blankets can improve sleep through its effects on the brain using objective measurements such as electroencephalogram. Sixth, future studies could try to test the effects of weighted blankets in healthy people without insomnia or to test the non-inferiority of weighted blankets using a well-recognized sleep medication as a positive control.
4.3 Clinical implications
The efficacy of weighted blankets in sleep quality in different populations provides scientific recommendations for a non-pharmacotherapy of sleep disorders such as insomnia in clinical settings. Nevertheless, given the limited evidence available, the clinical application should be especially cautious. Clinicians should help patients make a reasonable decision by informing them of the uncertainty of the efficacy and other alternative approaches, considering the patients’ core needs and preferences. In practice, clinicians should evaluate whether the patients have characteristics unsuitable for using weighted blankets, such as a history of serious diseases including coronary heart disease, cerebral infarction, respiratory problems, and cancer; active abuse of sleeping pills; severe cognitive dysfunction, etc. Once a patient starts using, it is better for clinicians to monitor closely, collect the feedbacks in time, and discontinue immediately if the patient feels uncomfortable. It is important to note that weighted blankets can be dangerous, especially for children and the elderly. The higher weight of weighted blankets may cause pain, anxiety, and panic to a few children (33, 73). In general, children under 3 years of age or weighing less than 50 pounds should not use weighted blankets due to the risk of suffocation or entrapment. It is best for children to use a weighted blanket under the supervision of their parents and will need to go through a period of adaptation. We advise parents to avoid covering the children’s face with a blanket. For the elderly, it is worth emphasizing that they should have the physical capacity to remove the weighted blanket from the head if needed to avoid the risk of suffocation. If the blanket is too heavy that they have to struggle to get it off, they could end up injuring themselves. Therefore, if the elderly have frailty, limited mobility, or severe dementia, they should use the lightest weighted blanket possible after consulting medical doctors (45).
In summary, weighted blankets might be a safe and effective intervention for insomnia and various sleep disturbances and psychiatric disorders, with fewer side effects than drug therapy. More research is needed further to explore the application of weighted blankets in a wider range of populations. At present, deep pressure touch has been recognized as an essential mechanism of weighted blankets. Further studies aiming at identifying more mechanisms of weighted blankets are needed. The long-term safety and efficacy of weighted blankets must be further validated in high-quality, large-scale randomized controlled trials.
Author contributions
JY: Methodology, Visualization, Writing – original draft, Writing – review & editing. ZY: Methodology, Writing – original draft. SS: Methodology, Visualization, Writing – original draft. KS: Investigation, Writing – review & editing. WC: Investigation, Writing – review & editing. LMZ: Investigation, Writing – review & editing. JX: Investigation, Writing – review & editing. QX: Investigation, Writing – review & editing. ZL: Conceptualization, Funding acquisition, Supervision, Writing – review & editing. JK: Investigation, Writing – review & editing. LSZ: Supervision, Writing – review & editing. YZ: Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by funding from Damian Health Tech (Hangzhou) CO., LTD (Kheng-20220141, to ZL) and Key Laboratory of Intelligent Preventive Medicine of Zhejiang Province (2020E10004). The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1333015/full#supplementary-material
References
1. Consensus Conference P, Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, et al. Joint consensus statement of the American academy of sleep medicine and sleep research society on the recommended amount of sleep for a healthy adult: methodology and discussion. Sleep. (2015) 38:1161–83. doi: 10.5665/sleep.4886
2. Jahrami HA, Alhaj OA, Humood AM, Alenezi AF, Fekih-Romdhane F, AlRasheed MM, et al. Sleep disturbances during the Covid-19 pandemic: A systematic review, meta-analysis, and meta-regression. Sleep Med Rev. (2022) 62:101591. doi: 10.1016/j.smrv.2022.101591
3. Sharma M, Aggarwal S, Madaan P, Saini L, Bhutani M. Impact of Covid-19 pandemic on sleep in children and adolescents: A systematic review and meta-analysis. Sleep Med. (2021) 84:259–67. doi: 10.1016/j.sleep.2021.06.002
4. Palagini L, Hertenstein E, Riemann D, Nissen C. Sleep, insomnia and mental health. J Sleep Res. (2022) 31:e13628. doi: 10.1111/jsr.13628
5. Plante DT. The evolving nexus of sleep and depression. Am J Psychiatry. (2021) 178:896–902. doi: 10.1176/appi.ajp.2021.21080821
6. Cheng P, Kalmbach DA, Tallent G, Joseph CL, Espie CA, Drake CL. Depression prevention via digital cognitive behavioral therapy for insomnia: A randomized controlled trial. Sleep. (2019) 42. doi: 10.1093/sleep/zsz150
7. Gee B, Orchard F, Clarke E, Joy A, Clarke T, Reynolds S. The effect of non-pharmacological sleep interventions on depression symptoms: A meta-analysis of randomised controlled trials. Sleep Med Rev. (2019) 43:118–28. doi: 10.1016/j.smrv.2018.09.004
8. Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Clinical guidelines committee of the American college of P. Management of chronic insomnia disorder in adults: A clinical practice guideline from the American college of physicians. Ann Intern Med. (2016) 165:125–33. doi: 10.7326/M15-2175
9. Beaulieu-Bonneau S, Ivers H, Guay B, Morin CM. Long-term maintenance of therapeutic gains associated with cognitive-behavioral therapy for insomnia delivered alone or combined with Zolpidem. Sleep. (2017) 40. doi: 10.1093/sleep/zsx002
10. Morin CM, Vallières A, Guay B, Ivers H, Savard J, Mérette C, et al. Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia: A randomized controlled trial. JAMA. (2009) 301:2005–15. doi: 10.1001/jama.2009.682
11. Eugene AR. Association of sleep among 30 antidepressants: A population-wide adverse drug reaction study, 2004-2019. PeerJ. (2020) 8:e8748. doi: 10.7717/peerj.8748
12. Eugene AR, Eugene B, Masiak M, Masiak JS. Head-to-head comparison of sedation and somnolence among 37 antipsychotics in schizophrenia, bipolar disorder, major depression, autism spectrum disorders, delirium, and repurposed in Covid-19, infectious diseases, and oncology from the Faers, 2004-2020. Front Pharmacol. (2021) 12:621691. doi: 10.3389/fphar.2021.621691
13. Richardson K, Loke YK, Fox C, Maidment I, Howard R, Steel N, et al. Adverse effects of Z-drugs for sleep disturbance in people living with dementia: A population-based cohort study. BMC Med. (2020) 18:351. doi: 10.1186/s12916-020-01821-5
14. Reynolds S, Lane SJ, Mullen B. Effects of deep pressure stimulation on physiological arousal. Am J Occup Ther. (2015) 69:6903350010p1–5. doi: 10.5014/ajot.2015.015560
15. Gee BM, Lloyd K, Sutton J, McOmber T. Weighted blankets and sleep quality in children with autism spectrum disorders: A single-subject design. Children (Basel). (2020) 8:10. doi: 10.3390/children8010010
16. Ekholm B, Spulber S, Adler M. A randomized controlled study of weighted chain blankets for insomnia in psychiatric disorders. J Clin Sleep Med. (2020) 16:1567–77. doi: 10.5664/jcsm.8636
17. Eron K, Kohnert L, Watters A, Logan C, Weisner-Rose M, Mehler PS. Weighted blanket use: A systematic review. Am J Occup Ther. (2020) 74:7402205010p1–p14. doi: 10.5014/ajot.2020.037358
18. Freeman D, Sheaves B, Waite F, Harvey AG, Harrison PJ. Sleep disturbance and psychiatric disorders. Lancet Psychiatry. (2020) 7:628–37. doi: 10.1016/S2215-0366(20)30136-X
20. Danoff-Burg S, Rus HM, Cruz Martir L, Raymann RJ. 1203 worth the weight: weighted blanket improves sleep and increases relaxation. Sleep. (2020) 43:A460. doi: 10.1093/sleep/zsaa056.1197
21. Hjort Telhede E, Arvidsson S, Karlsson S, Ivarsson A. Weighted blankets' Effect on the health of older people living in nursing homes. Geriatrics (Basel). (2022) 7:79. doi: 10.3390/geriatrics7040079
22. Bolic Baric V, Skuthalla S, Pettersson M, Gustafsson PA, Kjellberg A. The effectiveness of weighted blankets on sleep and everyday activities - a retrospective follow-up study of children and adults with attention deficit hyperactivity disorder and/or autism spectrum disorder. Scand J Occup Ther. (2023) 30:1357–67. doi: 10.1080/11038128.2021.1939414
23. France KG, McLay LK, Hunter JE, France MLS. Empirical research evaluating the effects of non-traditional approaches to enhancing sleep in typical and clinical children and young people. Sleep Med Rev. (2018) 39:69–81. doi: 10.1016/j.smrv.2017.07.004
24. Kennert BA, Harshorne TS, Kanouse S, Johnson C. Parent survey of sleep problems among children with charge syndrome. Res Dev Disabil. (2020) 101:103614. doi: 10.1016/j.ridd.2020.103614
25. Meth EMS, Brandao LEM, van Egmond LT, Xue P, Grip A, Wu J, et al. A weighted blanket increases pre-sleep salivary concentrations of melatonin in young, healthy adults. J Sleep Res. (2023) 32:e13743. doi: 10.1111/jsr.13743
26. Hvolby A, Bilenberg N. Use of ball blanket in attention-deficit/hyperactivity disorder sleeping problems. Nord J Psychiatry. (2011) 65:89–94. doi: 10.3109/08039488.2010.501868
27. Gringras P, Green D, Wright B, Rush C, Sparrowhawk M, Pratt K, et al. Weighted blankets and sleep in autistic children–a randomized controlled trial. Pediatrics. (2014) 134:298–306. doi: 10.1542/peds.2013-4285
28. Gee BM, Peterson TG, Buck A, Lloyd KG. Improving sleep quality using weighted blankets among young children with an autism spectrum disorder. Int J Ther Rehabil. (2016) 23:173–81. doi: 10.12968/ijtr.2016.23.4.173
29. Gee B, McOmber T, Sutton J, Lloyd K. Efficacy of weighted blankets for children with autism spectrum disorder, sensory overresponsivity, and sleep disturbance. Am J Occup Ther. (2017) 71:7111515242p1. doi: 10.5014/ajot.2017.71S1-PO4116
30. Hvolby A. The application of ball blankets in the treatment of sleeping difficulties in children with attention deficit or hyperactivity disorder. Effect on quality of life and daily functioning. J Sleep Med Disord. (2020) 6:1100. doi: 10.47739/2379-0822/1100
31. Larsson I, Aili K, Nygren JM, Jarbin H, Svedberg P. Parents' Experiences of weighted blankets' Impact on children with attention-deficit/hyperactivity disorder (Adhd) and sleep problems-a qualitative study. Int J Environ Res Public Health. (2021) 18:12959. doi: 10.3390/ijerph182412959
32. Steingrimsson S, Odeus E, Cederlund M, Franzen S, Helgesson C, Nystrom K, et al. Weighted blanket and sleep medication use among adults with psychiatric diagnosis - a population-based register study. Nord J Psychiatry. (2022) 76:29–36. doi: 10.1080/08039488.2021.1931713
33. Lönn M, Aili K, Svedberg P, Nygren J, Jarbin H, Larsson I. Experiences of using weighted blankets among children with Adhd and sleeping difficulties. Occup Ther Int. (2023) 2023:1945290. doi: 10.1155/2023/1945290
34. Odeus E, Pauli E, Steingrimsson S, Cederlund M, Franzen S, Helgesson C, et al. Weighted blankets for sleep problems - prescription, use and cost analysis. Scand J Occup Ther. (2023) 30:211–21. doi: 10.1080/11038128.2022.2066017
35. Joergensen ME, Nielsen IK, Olesen AS, Pedersen V. Sleep quality, pain, hba1c levels and quality of life in chronic non-malignant pain patients: A randomised double-blinded clinical study. Pain Pract. (2012) 12:47. doi: 10.1111/j.1533-2500.2011.00528.x
36. Joergensen ME, Nielsen IK, Olesen AS, Pedersen V. 997 Hba1c levels and health related quality of life (Sf-36) in non-malignant chronic pain patients supplied with a ball-or placebo-blanket. Eur J Pain. (2009) 13:S280a–S. doi: 10.1016/S1090-3801(09)61000-4
37. Vinson J, Powers J, Mosesso K. Weighted blankets: anxiety reduction in adult patients receiving chemotherapy. Clin J Oncol Nurs. (2020) 24:360–8. doi: 10.1188/20.CJON.360-368
38. Becklund AL, Rapp-McCall L, Nudo J. Using weighted blankets in an inpatient mental health hospital to decrease anxiety. J Integr Med. (2021) 19:129–34. doi: 10.1016/j.joim.2020.11.004
39. Clapp A. Effects of Weighted Blankets on College Students’ Anxiety. Berkeley, United States: Illinois Wesleyan University (2019).
40. Hjort Telhede E, Arvidsson S, Karlsson S. Nursing staff's experiences of how weighted blankets influence resident's in nursing homes expressions of health. Int J Qual Stud Health Well-being. (2022) 17:2009203. doi: 10.1080/17482631.2021.2009203
41. Baumgartner JN, Quintana D, Leija L, Schuster NM, Bruno KA, Castellanos JP, et al. Widespread pressure delivered by a weighted blanket reduces chronic pain: A randomized controlled trial. J Pain. (2022) 23:156–74. doi: 10.1016/j.jpain.2021.07.009
42. Nielsen IK, Joergensen ME, Olesen AS, Pedersen V. Pb62 does a ball blanket influence hba1c levels in patients with chronic non-malignant pain? Preliminary results of a controlled, randomized, and doubleblinded clinical trial. Pain Pract. (2009) 9:110. doi: 10.1111/j.1533-2500.2009.00267.x
43. Dyon NA, Sue JL, Tchakerian N, Fisher K. The use of weighted blankets as a novel approach for treatment of persistent vocalizations in late stage dementia. Geriatr Nurs. (2021) 42:1253–6. doi: 10.1016/j.gerinurse.2021.08.004
44. Harris ML, Titler MG. Feasibility and acceptability of a remotely delivered weighted blanket intervention for people living with dementia and their family caregivers. J Appl Gerontol. (2022) 41:2316–28. doi: 10.1177/07334648221111123
45. Nakamura M, Yamauchi N. A case of effective usage of a weighted blanket for a person with severe dementia. Psychogeriatrics. (2021) 21:239–42. doi: 10.1111/psyg.12656
46. Eull D, Zachrison B, Nickel A. Feasibility trial of weighted blankets as an intervention for emergence delirium in postoperative pediatric patients. J Pediatr Nurs. (2022) 62:30–5. doi: 10.1016/j.pedn.2021.11.022
47. Summe V, Baker RB, Eichel MM. Safety, feasibility, and effectiveness of weighted blankets in the care of infants with neonatal abstinence syndrome: A crossover randomized controlled trial. Adv Neonatal Care. (2020) 20:384–91. doi: 10.1097/ANC.0000000000000724
48. Atkin T, Comai S, Gobbi G. Drugs for insomnia beyond benzodiazepines: pharmacology, clinical applications, and discovery. Pharmacol Rev. (2018) 70:197–245. doi: 10.1124/pr.117.014381
50. Chapoutot M, Peter-Derex L, Bastuji H, Leslie W, Schoendorff B, Heinzer R, et al. Cognitive behavioral therapy and acceptance and commitment therapy for the discontinuation of long-term benzodiazepine use in insomnia and anxiety disorders. Int J Environ Res Public Health. (2021) 18:10222. doi: 10.3390/ijerph181910222
51. Tayyar Iravanlou F, Soltani M, Alsadat Rahnemaei F, Abdi F, Ilkhani M. Non- pharmacological approaches on the improvement of sleep disturbances in patients with autism spectrum disorder (Asd). Iran J Child Neurol. (2021) 15:79–91. doi: 10.22037/ijcn.v15i2.25539
52. Mullen B, Champagne T, Krishnamurty S, Dickson D, Gao RX. Exploring the safety and therapeutic effects of deep pressure stimulation using a weighted blanket. Occup Ther Ment Health. (2008) 24:65–89. doi: 10.1300/J004v24n01_05
53. Chen H-Y, Yang H, Chi H-J, Chen H-M. Physiological effects of deep touch pressure on anxiety alleviation: the weighted blanket approach. J Med Biol Eng. (2013) 33:463–70. doi: 10.5405/jmbe.1043
54. Chanques G, Constantin JM, Devlin JW, Ely EW, Fraser GL, Gelinas C, et al. Analgesia and sedation in patients with Ards. Intensive Care Med. (2020) 46:2342–56. doi: 10.1007/s00134-020-06307-9
55. de Looff PC, Cornet LJM, Embregts P, Nijman HLI, Didden HCM. Associations of sympathetic and parasympathetic activity in job stress and burnout: A systematic review. PLoS One. (2018) 13:e0205741. doi: 10.1371/journal.pone.0205741
56. Chen HY, Yang H, Meng LF, Chan PS, Yang CY, Chen HM. Effect of deep pressure input on parasympathetic system in patients with wisdom tooth surgery. J Formos Med Assoc. (2016) 115:853–9. doi: 10.1016/j.jfma.2016.07.008
57. Huang JH, Chang HA, Fang WH, Ho PS, Liu YP, Wan FJ, et al. Serotonin receptor 1a promoter polymorphism, Rs6295, modulates human anxiety levels via altering parasympathetic nervous activity. Acta Psychiatr Scand. (2018) 137:263–72. doi: 10.1111/acps.12853
58. Kastenberger I, Lutsch C, Herzog H, Schwarzer C. Influence of sex and genetic background on anxiety-related and stress-induced behaviour of prodynorphin-deficient mice. PLoS One. (2012) 7:e34251. doi: 10.1371/journal.pone.0034251
59. Martin S, Thome UH, Grunwald M, Mueller SM. Light or deep pressure: medical staff members differ extensively in their tactile stimulation during preterm Apnea. Front Pediatr. (2020) 8:102. doi: 10.3389/fped.2020.00102
60. Brzezinski A, Vangel MG, Wurtman RJ, Norrie G, Zhdanova I, Ben-Shushan A, et al. Effects of exogenous melatonin on sleep: A meta-analysis. Sleep Med Rev. (2005) 9:41–50. doi: 10.1016/j.smrv.2004.06.004
61. Brzezinski A. Melatonin in humans. N Engl J Med. (1997) 336:186–95. doi: 10.1056/nejm199701163360306
62. Saper CB, Loewy AD, Swanson LW, Cowan WM. Direct hypothalamo-autonomic connections. Brain Res. (1976) 117:305–12. doi: 10.1016/0006-8993(76)90738-1
63. Møller M. Chapter 2 - vasopressin and oxytocin beyond the pituitary in the human brain. In: Swaab DF, Kreier F, Lucassen PJ, Salehi A, Buijs RM, editors. Handbook of Clinical Neurology, vol. 180 . Amsterdam, Netherlands: Elsevier (2021). p. 7–24.
64. Verheggen RJHM, Jones H, Nyakayiru J, Thompson A, Groothuis JT, Atkinson G, et al. Complete absence of evening melatonin increase in Tetraplegics. FASEB J. (2012) 26:3059–64. doi: 10.1096/fj.12-205401
65. Martinez-Calderon J, Flores-Cortes M, Morales-Asencio JM, Luque-Suarez A. Pain-related fear, pain intensity and function in individuals with chronic musculoskeletal pain: A systematic review and meta-analysis. J Pain. (2019) 20:1394–415. doi: 10.1016/j.jpain.2019.04.009
66. Ploghaus A, Narain C, Beckmann CF, Clare S, Bantick S, Wise R, et al. Exacerbation of pain by anxiety is associated with activity in a hippocampal network. J Neurosci. (2001) 21:9896–903. doi: 10.1523/jneurosci.21-24-09896.2001
67. Case LK, Liljencrantz J, McCall MV, Bradson M, Necaise A, Tubbs J, et al. Pleasant deep pressure: expanding the social touch hypothesis. Neuroscience. (2021) 464:3–11. doi: 10.1016/j.neuroscience.2020.07.050
68. Krauss KE. The effects of deep pressure touch on anxiety. Am J Occup Ther. (1987) 41:366–73. doi: 10.5014/ajot.41.6.366
69. Messere A, Ceravolo G, Franco W, Maffiodo D, Ferraresi C, Roatta S. Increased tissue oxygenation explains the attenuation of hyperemia upon repetitive pneumatic compression of the lower leg. J Appl Physiol (1985). (2017) 123:1451–60. doi: 10.1152/japplphysiol.00511.2017
70. Monteiro Rodrigues L, Rocha C, Ferreira HT, Silva HN. Lower limb massage in humans increases local perfusion and impacts systemic hemodynamics. J Appl Physiol (1985). (2020) 128:1217–26. doi: 10.1152/japplphysiol.00437.2019
71. Case LK, Liljencrantz J, Madian N, Necaise A, Tubbs J, McCall M, et al. Innocuous Pressure Sensation Requires a-Type Afferents but Not Functional Pιϵζo2 Channels in Humans. Nat Commun. (2021) 12:657. doi: 10.1038/s41467-021-20939-5
72. Valeriani M, Pazzaglia C, Rizzo V, Quartarone A, Vollono C. Laser evoked potential amplitude and laser-pain rating reduction during high-frequency non-noxious somatosensory stimulation. Clin Neurophysiol. (2018) 129:920–5. doi: 10.1016/j.clinph.2018.02.004
Keywords: weighted blanket, sleep disorder, insomnia, deep pressure, occupational therapy, psychiatric disorder
Citation: Yu J, Yang Z, Sun S, Sun K, Chen W, Zhang L, Xu J, Xu Q, Liu Z, Ke J, Zhang L and Zhu Y (2024) The effect of weighted blankets on sleep and related disorders: a brief review. Front. Psychiatry 15:1333015. doi: 10.3389/fpsyt.2024.1333015
Received: 04 November 2023; Accepted: 27 March 2024;
Published: 15 April 2024.
Edited by:
Guanhu Yang, Ohio University, United StatesReviewed by:
Steinn Steingrimsson, Sahlgrenska University Hospital, SwedenAndy R. Eugene, Larned State Hospital, United States
Copyright © 2024 Yu, Yang, Sun, Sun, Chen, Zhang, Xu, Xu, Liu, Ke, Zhang and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yubo Zhu, eWlzaGFubWFtYTEzMTIwNEAxNjMuY29t; Lisan Zhang, emxzMDlAemp1LmVkdS5jbg==; Zuyun Liu, WnV5dW4ubGl1QG91dGxvb2suY29t
†These authors have contributed equally to this work and share first authorship
 Jie Yu
Jie Yu Zhenqing Yang
Zhenqing Yang Sudan Sun1†
Sudan Sun1† Zuyun Liu
Zuyun Liu Lisan Zhang
Lisan Zhang Yubo Zhu
Yubo Zhu