
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 26 January 2024
Sec. Public Mental Health
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1332066
This article is part of the Research Topic Cognitive and Mental Health Improvement Under- and Post-COVID-19 View all 24 articles
Background: Long-COVID (LC) refers to post-acute COVID-19 symptoms that can last for months or longer after the initial infection, affecting the physical health of infected patients. This study aims to investigate the association between the symptomology of LC and the mental health of patients in China. It also aims to examine the relationship between the perceived symptom burden and mental health of these patients.
Methods: A population-based stratified cluster sample was recruited, using a standard sampling procedure, from a prefecture-level city in Northern China. Participants included patients who had tested positive for COVID-19 after December 2022. LC symptomology was assessed using a LC symptoms checklist where the perceived symptom burden was measured by the included 5-point Likert scales. Mental health of patients was measured using the Depression, Anxiety, and Stress Scale (DASS), the original Connor-Davidson Resilience Scale (CD-RISC), and the Duke-UNC Functional Social Support Questionnaire (DUFSS). Data were analysed using multiple linear regression models.
Results: About 25% of respondents, experienced COVID symptoms lasting longer than two months that could only be explained by the infection. Post-exertional malaise (22.2%) and fatigue (21.2%) were the most common symptoms. After controlling for potential confounding variables, LC symptomology was significantly and positively associated with depression (t=2.09, p=0.037) and anxiety (t=4.51, p<0.001), but not stress. Perceived symptoms burden was also positively and significantly related to depression (β=0.35, p<0.001), anxiety (β=0.54, p<0.001), and stress (β=0.35, p<0.001), suggesting a dose-response relationship between perceived symptom burden and mental ill health.
Conclusion: This study highlights the importance of recognising the risk of LC, patients’ perception of the symptom burden and its potential impact on mental health. Healthcare professionals should be aware of the complexity of psychological comorbidities among infected patients reporting prolonged symptoms, and be able to give advice regarding long-term management of the symptoms.
The COVID-19 pandemic has not only caused almost 800 million cases and 7 million deaths globally, but also the long-lasting and profound changes at the personal level, such as social interactions, lifestyles, and mental-wellbeing. It also affected the population at the social level including the global economy, healthcare system, and social inequalities (1, 2). In October 2021, the World Health Organization (WHO) defined Long-COVID (LC) as the condition typically occurs in individuals with a history of probable or confirmed SARS-CoV-2 infection, usually 3 months after onset, lasting for at least 2 months and cannot be explained by any alternative diagnosis (3). With global numbers of infections of COVID-19 exceeding 500 million, a conservative estimate of people being currently affected by LC worldwide could be more than 100 million (4). Typical acute COVID-19 cases are characterised by respiratory symptoms, fever, and neurological symptoms (5). The duration and severity of acute COVID-19 cases vary, with some patients being asymptomatic, while others require hospitalisation and mechanical ventilation. The average duration of a COVID-19 infection is typically shorter than 4 weeks (6). The new-onset conditions including cardiovascular, thrombotic/cerebrovascular disease, type 2 diabetes, myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) and dysautonomia, especially postural orthostatic tachycardia syndrome (POTS), could last for a long time even years. These symptoms could be commonly called LC. It also have different labels, such as post-acute sequelae of COVID-19, post-acute COVID-19, or post-COVID-19 condition (7).
It has been widely reported that the risk of psychiatric symptoms was associated with COVID-19 infection. A recent meta-analysis revealed that up to one in four patients experienced neuropsychiatric symptoms spanning sleep disorders, fatigue, anxiety, and post-traumatic stress (PTSD) after the onset of COVID-19 with an approximate follow-up duration of 77 days (8). Studies have further explored potential correlations between the risk of LC and mental health problems. Specifically, LC was found to be associated with increased display of depression, anxiety, PTSD, and weakened life satisfaction (9), which might be partially attributed to the persistent physical symptoms of LC (10). In China, few studies have focused on evaluating the impact of LC on COVID survivors. Zhao et al.’s study (11) found that approximately 9.6% of hospitalised patients suffering from moderate impairment reported mainly mental health and cognitive symptoms 20 months after recovery. Several factors were reported to be predictive of long-term physical and cognitive symptoms, which included age, hospital stay, sex, and comorbidities. However, the sample was recruited in 2021 and was not based on a randomised sampling method. Another study conducted in China has found that having at least one LC symptom increased the risk of depression or anxiety by 3.44-fold (12). However, the study sample was limited to hospitalised patients recruited in 2020. Given the limitations of these studies, there is a need to further study the mental health effect of LC, particularly in patients who were infected in the later period of the pandemic using a random community-based sample.
The extent of suffering from chronic illness is not just determined by the severity of the illness itself, but rather moderated by external and subjective factors (13). As The Burden of Treatment Theory posits, management of chronic conditions involves routine work for patients to control their illness. As treatment burdens accumulate, some patients become overwhelmed leading to poorer outcomes, stress on caregivers, and increased healthcare costs (14). In addition, personality factors also play an important role when patients cope with the illness. According to Leventhal’s self-regulatory model, patients’ “illness representations” (beliefs about cause, timeline, consequences, etc.), reflecting their perceived burden, affect their self-management behaviors, psychological adjustment, and mental health (15). Therefore, the perceived burden of illness of patients suffering from Long-COVID, like any other chronic conditions, may also have a direct impact on their mental health.
In terms of the relationship between the perceived severity of LC symptoms and the mental health of patients, few studies have been conducted. In the study by Sivan and colleagues, it was found a positive correlation between the perceived severity of 12 types of LC symptoms and cognitive symptoms, PTSD, depression, and anxiety (16). However, in another study of patients with LC symptoms, the perceived severity of autonomic dysfunction and anxiety, as well as emotional well-being were not positively correlated (17).
Therefore, this study aims to describe the common symptoms related to LC and to quantify the prevalence of these symptoms among community-dwelling COVID patients. It also aims to examine the relationship between the LC symptomology and the mental health status of these patients, as well as the relationship between the perceived burden of the LC symptoms and the level of mental health problems. It is hypothesised that LC symptomatology is associated with the mental health of patients and that there is a positive dose-response relationship between the perceived burden of LC symptomatology and the severity of mental health problems.
This was a population-based cross-sectional health survey using a stratified cluster random sample recruited from Shijiazhuang, a prefecture-level city in Northern China. Since residents of the city were housed in compounds in China, two compounds from the list of compounds within each jurisdiction in the city were randomly selected in accordance with the population size of jurisdictions. In total, eight compounds were selected as the sample frame. Two buildings were then randomly selected from each compound for the recruitment of the sample. Additional buildings will be selected if the sample size does not reach the expected level. The researchers joined the WeChat group of the selected buildings to distribute the online questionnaire with the permission of the compound’s management. The online survey was designed using the Tencent platform which could be easily distributed through social media platforms. For participants who were not familiar with mobile technologies, a printed questionnaire was delivered by post and collected through a neighbourhood collection point designated by the researchers.
The survey was conducted in May and June 2023, approximately 5 months after the peak of COVID-19 infection in December 2022. Only participants aged 25-54 years were included to reduce potential age-related biases (18, 19). Participants who were not diagnosed as positive (hospital or self-tested antigen) in China after December 2022 were excluded. Participant’s participation in the survey implied their consent, which was stated in the promotional materials and on the survey’s front page. The study was approved by the Macau University of Science and Technology Medical Ethics Committee (MUST-HSS-20230505001).
Based on the literature, it was estimated that the prevalence of unresolved COVID-19-related symptoms at about 4 months among COVID-19 survivors was 45% (20). Using the prevalence-based calculation of the sample size with a precision of 5% and a confidence interval of 95% was estimated that a sample of at least 380 would be required to provide sufficient power for the study (21). Given an estimated 20% of invalidation rate, the final required sample size was estimated to be about 460.
Mental Health status was assessed using the Depression, Anxiety, and Stress Scale (DASS) (22). The DASS designed to assess the severity of symptoms related to depression, anxiety, and stress. Participants are asked to rate the extent to which they have experienced each symptom over the past week using a 4-point Likert scale ranging from 0 (Did not apply to me at all) to 3 (Applied to me very much or most of the time). The final scores will be for depression (7 items, range 0-21), anxiety (7 items, range 0-21) and stress (7 items, range 0-21).
The LC symptomology was assessed by the Long-COVID Symptoms Checklist of 15 questions on symptoms commonly identified with patients with LC symptoms. Patients were asked if the symptoms persisted for at least two months after diagnosis of COVID-19, or if they had developed any new symptoms that had been present for a minimum of two months following their initial diagnosis. In this study, LC symptomatology was defined as having at least one of the symptoms reported on the Symptom Checklist. The validity of the Long-COVID Symptoms Checklist was tested by 10 global experts from cardiology, respiratory medicine, intensive care, and internal medicine. The content validity of the scale was calculated using the item-level content validity index (I-CVI) and the average scale-level content validity index (S-CVI/Ave). An I-CVI ≥ 0.78 and an S-CVI/Ave ≥ 0.90 were considered acceptable (23). Additionally, to evaluate the internal consistency of the items measuring Long-COVID with respect to the underlying construct, Cronbach’s α reliability coefficient was computed using SPSS software (SPSS 26.0: SPSS; Chicago, IL, USA). The I-CVI of each item of the Checklist ranged from 0.8 to 1.0, and the S-CVI/Ave was 0.87 with an I-CVI ≥ 0.78 and an S-CVI/Ave ≥ 0.90 considered acceptable (23). For internal consistency, Cronbach’s alpha coefficient was calculated as 0.80 with a value exceeding 0·7 regarded as acceptable (24).
To assess the burden of LC symptoms, patients were asked to rate each symptom on the Long-COVID Symptom Checklist the degree to which it interfered with their daily activities (including work and household duties) on a 5-point Likert scale ranging from 0 (Not at all) to 4 (Very much). The total perceived burden was assessed using the total score summing the responses on each item.
Resilience was examined by using the shortened version of the Connor-Davidson Resilience Scale (CD-RISC2) (25). The scale is based on two items that they believed captured the essence of resilience conceptually from the 25-item the Connor-Davidson Resilience Scale. It uses 5-point Likert-type response scale, ranging from “not at all” (0 points) to “almost completely” (4 points) (26). Participants rated each item based on their experiences during the past month. Higher scores indicate higher levels of resilience.
Social Support was assessed using The Duke-UNC Functional Social Support Questionnaire (DUFSS), which is a multidimensional social support scale consisting of 8 items used to measure an individual’s perceived social support (27). The DUFSS is a reliable and valid self-report tool that has been used in research with medical patients (28). Scores range from 8 to 40, with higher scores indicating greater perceived social support.
Other information collected included demographics, pre-COVID-19 health status, vaccination history, date of their first COVID-19 symptom onset, symptoms in the acute infection phase, hospitalisation during the acute symptomatic period, and how they confirmed their COVID-19 infection.
The statistical analyses were performed in STATA 15.1 (StataCorp LLC, TX, USA). Descriptive analyses were performed to examine the participants’ demographic and health-related profiles, the prevalence of symptoms, and scores on psychological scales. Continuous variables are expressed as the mean (SD), while binary and categorical variables are presented as counts and percentages. Bivariate analyses were conducted between LC symptomology, demographic, health-related and other study variables, and the three mental health variables, namely depression, anxiety, and stress separately. For the selection of variables to be included in further multiple linear regression analyses, a criterion of p<0.1 was applied. For the association between LC symptomology and mental health, multiple linear regression analyses were employed since the raw scores of the DASS were used as the outcome measures. The possible moderating effect of resilience and social support between LC symptomology and poor mental health was checked by testing their corresponding interaction terms in the regression models. The analyses of the relationship between the perceived burden of LC and mental health were only conducted in the subgroup of patients with LC symptomology; namely, patients responded positively to the question “experienced lingering symptoms at least lasting for 2 months that cannot be explained except due to the infection.”. A similar approach to the aforementioned analyses for the association between LC symptomology and mental health was adopted. A type I error rate of 5% was used for all 2-tailed hypotheses testing for independent variables and 1% for the interaction terms.
In total, 781 patients tested positive with COVID-19 were recruited. Of these 482 respondents provided useful information for data analyses, after removing 299 questionnaires having inconsistent answers on geographical information or confirmation date of infection. A comparison between the respondents and non-respondents indicated no differences in demographic variables. Table 1 presents patients’ demographics, basic health information, and scores on mental health measures. Of the total 482 respondents, there were 195 (40.5%) males, with 374 (77.6%) receiving three or more doses of vaccine, and the most commonly received vaccine was the domestically produced inactivated vaccine (66.8%), followed by the domestically produced recombinant protein vaccine (30.5%). The most prevalent symptom of acute-phase infection reported by participants was fever (87.1%), followed by muscle and joint pain (56.0%), cough (47.9%), fatigue (42.7%), headache (41.9%), ENT abnormalities (25.1%), and finally shortness of breath (12.4%). Seven (n=7, 1.5%) of the respondents reported pre-morbid mental health problems, and 6 (1.2%) were hospitalised during the acute phase of the infection, with half (50%) of these hospitalised patients receiving treatment in the ICU. In terms of the outcome measures of the study, namely the mental health status, 61 (12.7%) exhibited symptoms of severe to extremely severe depression symptoms (mean=15.9, s.d=4.7), 26.8% (n=129) anxiety (mean=12.2, s.d=4.8), and 25.1% (n=121) stress (mean=17.2, s.d=3.8).
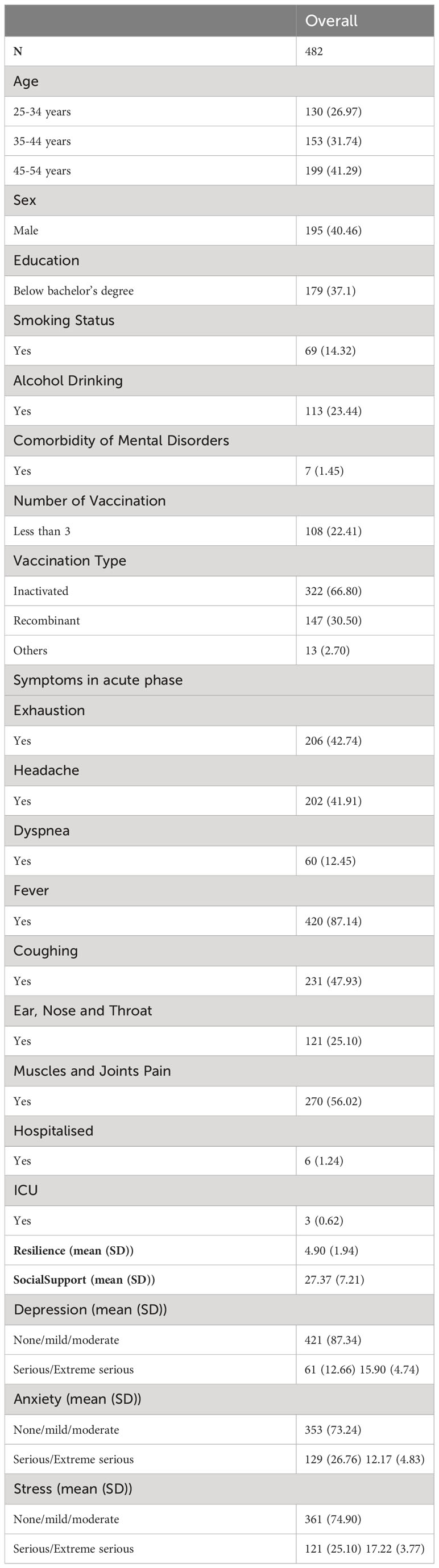
Table 1 Descriptive information on the demographics, premorbid health, vaccination, hospitalisation, resilience, social support, and mental health symptoms (N=482).
The results of LC symptomology were summarised in Table 2. As shown, among all respondents, 25.5% had symptoms that persisted for more than two months and could not be explained by causes other than COVID-19 infection. In addition, the top five common symptoms were postexertional malaise (22.2%), fatigue (21.2%), brain fog (14.3%), sleep (11.6%), shortness of breath (11.4%), and palpitations (10.2%).
The unadjusted bivariate relationships between LC symptomology, other study variables, and depression, anxiety, and stress were summarised in Table 3. As shown, a few variables were related to the mental health variables. LC symptomology, resilience, social support, and premorbid mental health problems were significantly related to all three aspects of mental health of interest. In addition, education level was significantly associated with stress and marginally related to anxiety. All other variables were insignificantly related to the mental health variables with a p-value much greater than 0.1. Hence, they were not included in further analyses. The results obtained from the multiple linear regression analyses were presented in Table 4. After adjusting for other variables in the model, the LC symptomology was still positively and significantly associated with depression (t=2.09, p=0.037) and anxiety (t=4.51, p<0.001), but not stress. The regression coefficient of LC symptomology was 1.13 (s.e. = 0.54) for depression suggesting a difference in the depression score of more than 1 unit between patients with LC symptomology and those without. The regression coefficient of LC symptomology for anxiety was 2.35 (s.e. = 0.52) indicating a difference of more than 2.3 units in the anxiety score between groups. In terms of the interaction terms between LC symptomology and resilience, as well as social support, the results indicated that none were significant even at the 5% types I error rate.
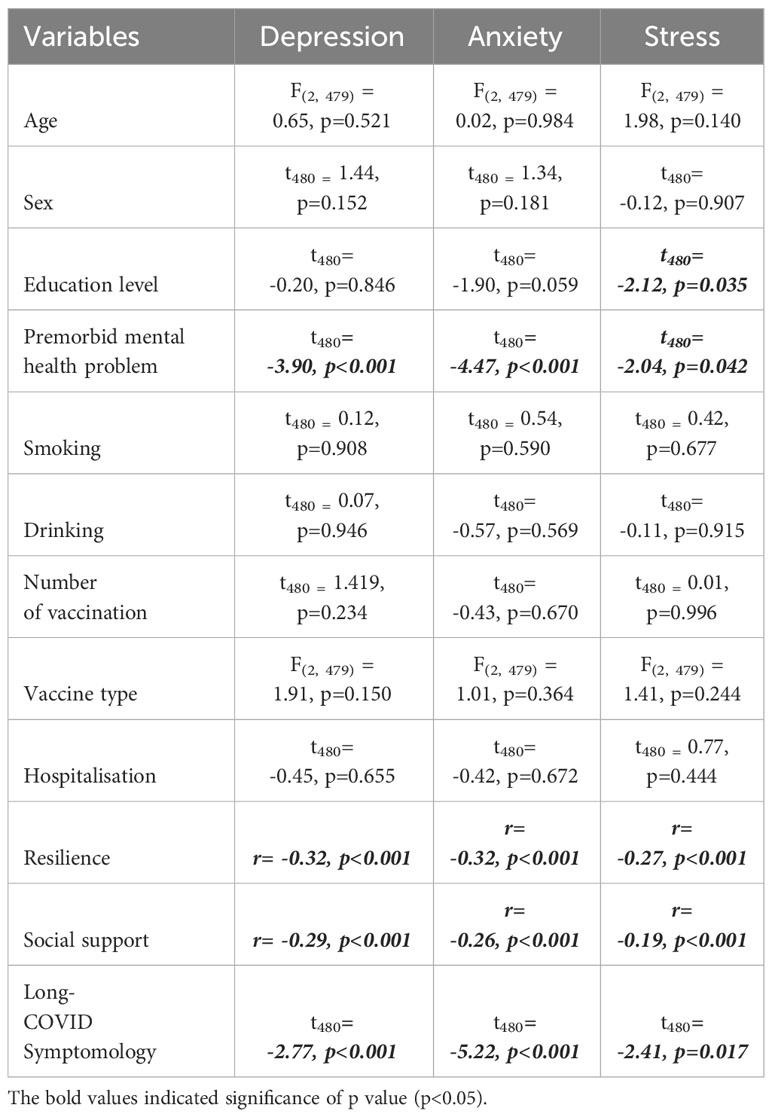
Table 3 Unadjusted association between Long-Covid Symptomology, demographics, premorbid health, vaccination, hospitalisation, resilience, social support, and mental health symptoms.
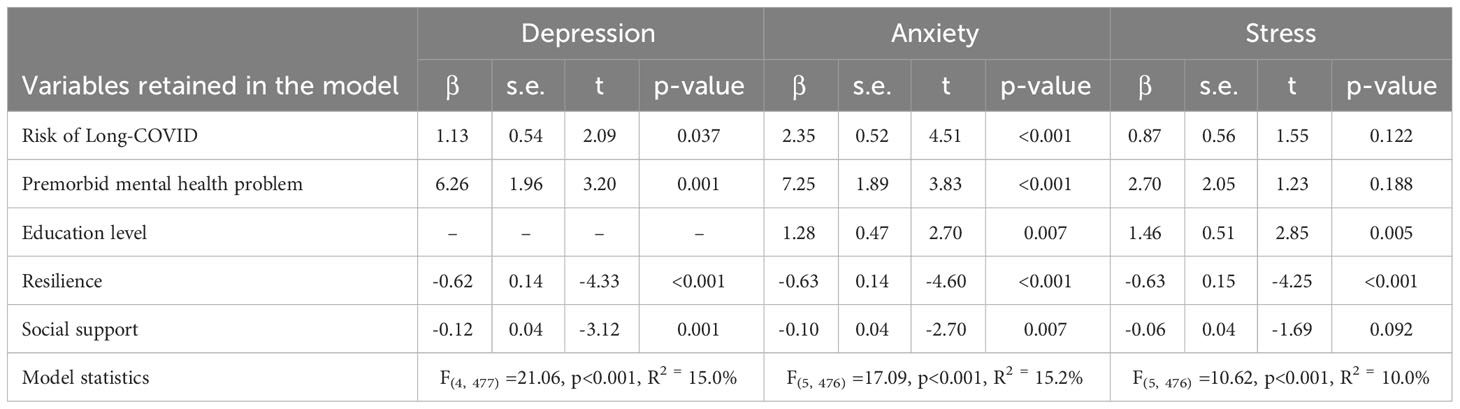
Table 4 Result of the adjusted association between the Long-COVID Symptomology and mental health (N=482).
For the relationships between the perceived burden of LC symptoms and mental health, the results were presented in Table 5. As shown, after adjusting for variables including premorbid mental health problem, education level, resilience, and social support, positive and significant associations were found between the perceived burden of LC and depression, anxiety, and stress. The regression coefficients of the perceived burden of LC for depression and stress were 0.38 (s.e. = 0.07) and 0.35 (s.e. = 0.08) respectively, indicating, on average, for each increase in 1 unit of perceived burden measure there was a corresponding increase of 0.38 units in the depression and 0.35 in the stress scores. Among the three mental health variables, anxiety had the largest increase in the score with an increase of each unit of perceived burden of LC there was an increase of 0.54 units (s.e. = 0.07, t=8.24, p<0.001). These results suggested a positive dose-response relationship between the perceived burden of LC symptoms and mental health problems. As in the previous analyses, none of the interaction terms between perceived burden and resilience, as well as social support were significant.
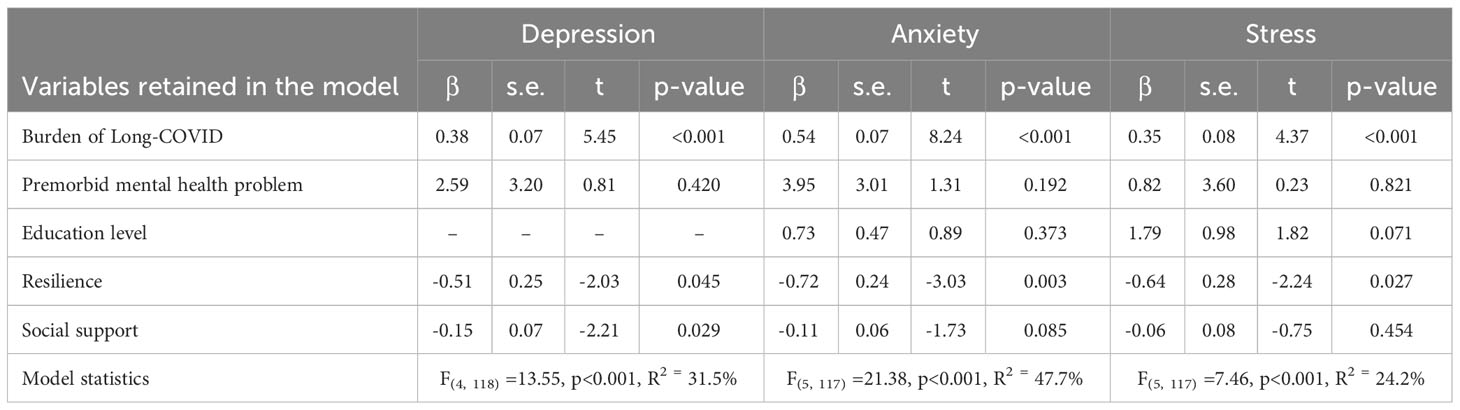
Table 5 Result of the association between the perceived symptom burden of Long-COVID and depression, anxiety, and stress (N=123).
This study aimed to investigate the prevalence of common symptoms of LC, and the propensity of LC in a community sample of COVID-19 patients. It also aimed to examine the relationship between LC symptomology and the mental health status, as well as the relationship between the perceived symptom burden of LC and mental health problems. The results suggested that patients exhibited the overall LC symptomology was about 25% among patients who had tested positive for COVID-19 after December 2022. Postexertional malaise and fatigue were the most prevalent LC symptoms, accounting for 22.2% and 21.2% of all LC patients, followed by cognitive impairment including brain frog (14.3%), and sleep problems (11.6%). The results further suggest a positive and significant association between LC symptomatology and poor mental health, particularly depression and anxiety. In terms of the perceived burden of LC symptoms, it is related to the mental health of patients also demonstrating a positive dose-response relationship with depression, anxiety, and stress.
The results on symptomatology, in general, are consistent with those reported in the literature, though some minor discrepancies are found in other less commonly reported symptoms, such as headaches and muscle aches that have been ranked less prevalent in the current study (29, 30). Furthermore, some differences in the prevalence of symptoms have also been identified compared to previous studies on COVID-19 patients one-year post-infection in China (12, 31). In Zhang’s study, the prevalence of muscle and joint pain was 11.8%, whereas in the current study, it was 8.3% (12). While the prevalence of brain fog and palpitations were 14.3% and 10.2% in this study, they are higher than that reported in the literature of 2.2% and 5.8% (31) This study also found that patients with LC symptomology scored significantly higher in depression and anxiety, but not stress. In terms of the propensity of these symptoms, these patients reported postexertional malaise, fatigue, brain fog, shortness of breath, and insomnia, as the most common symptoms, indicating that these symptoms had a greater impact on people’s lives and work. In the present study, postexertional malaise (PEM), a distinguishing feature of chronic fatigue syndrome (CFS) (32), was most prevalent and reported to be the most burdensome among other symptoms identified as post-COVID-19 sequelae. There could be many explanations for this result. One possible reason may relate to the potential physiological responses for the infection in different body parts including the brain, such as neuroinflammation (33). This has highlighted how the chronic and debilitating fatigue associated with CFS can significantly impact patients’ work productivity and quality of life, posing psychological distress (34). Moreover, symptoms related to CFS are relatively difficult to diagnose in hospitals to receive appropriate rehabilitation recommendations (35).
For the relationship of LC and mental health, the changes to routine happened due to pandemic, such as financial instability, social distance and mask wearing, have been challenging people’s psychological needs that previously fulfilled for about 3 years (36–38). Moreover, as for patients developed LC symptoms, they might experience additional symptoms related to brain function leading to a worse mental health outcome compared to those who recovered well from COVID-19 infection (39). The perceived burden of LC symptoms further exhibits the impact of the disease on the mental health of patients. There could be many reasons attributing to the interplay between the actual severity of the physical illness, treatment demands and individuals’ perceptions of their ability to adapt (40). According to the Burden of Treatment Theory (14), the perceived disease burden in LC patients may be aggregated by the difficulties of managing the symptoms. Overall, medical expenses on the treatment, which was estimated at $9,000 per person annually, could be a stress for many people (41). Moreover, the increased stringency of containment measures during the pandemic resulted in unemployment also exerted additional pressure on patients (42). As a result, patients who would like to retain their jobs are more likely to keep working and not take any medical leaves, thus becoming an additional layer of burden.
The findings highlight the need to provide mental health support for those severely affected by COVID-19 infection, particularly those who developed LC symptoms. In 2020, the National Health Commission of China issued “Rehabilitation Program for Discharged COVID-19 Patients” (43) recommending respiratory training, physical exercises, psychological support, and activities to regain daily living abilities to address residual respiratory, physical, and psychological dysfunctions like cough, fatigue, and anxiety that may persist post-hospitalisation. To date, the treatment strategies for LC in designated clinics or outpatient services mainly focused on symptom relief (44), with both Western and Chinese medicine focusing on physical rehabilitation (45, 46). In terms of mental health services in general, and particularly for patients with LC symptoms, it is a lacking area. China has very few numbers of mental health professionals relative to its large population (47). There is also a lack of mental health rehabilitation services, and the utilisation of telemedicine is also low mainly due to the limited access to facilities (47). With such limited resources, well-designed and validated preventive programs using a mHealth approach for early detection, intervention, treatment and management are urgently needed for the patient population with LC symptoms (48, 49).
There are several limitations to our study that should be noted. First, our sample was limited to individuals who self-reported LC symptoms, which may not be representative of all patients with LC symptoms. Out of the total sample, only 7 patients reported pre-morbid mental problems, which could limit the generalisation of correlation found between pre-morbid mental problems and mental illness severity after COVID-19 infection. Second, due to the study design being a cross-sectional survey, it would be difficult to draw any conclusion on the causality of the results obtained. Longitudinal studies could undoubtedly provide more powerful data for interpreting causality. While many other countries have established app-based COVID-19 syndromic surveillance systems (50, 51), a similar tracking platform has not yet been deployed in China (52). In addition, our study was conducted in a single city in the northern part of China. This may not be representative of the whole country due to possible geographical differences across the land, thus making it difficult to generalise the findings. For better evidence of the effect of LC on the mental health of infected patients’ studies of a stronger design, such as a cohort study, should be conducted. Furthermore, the study should also be expanded to a wider geographical region with more diverse populations.
However, despite these limitations, our study also has important contributions. To our knowledge, this is one of the first studies to investigate the impacts of perceived LC burden on mental health in China through a standardised assessment procedure. While larger and more rigorous studies are still needed, our findings provide valuable preliminary insights into how LC may be associated with increased mental illness severity.
The present study provides evidence that LC symptomology is associated with mental health problems of patients and that there is a dose-response relationship between the burden of LC symptoms and mental health problems. Long-term management and rehabilitation are essential in providing support to these patients. Continued investigation of how LC may influence mental well-being may also provide insights to guide targeted interventions and management strategies.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The informed consent and study protocol was confirmed by the Macau University of Science and Technology Medical Ethics Committee (MUST-HSS-20230505001).
YL: Conceptualization, Formal analysis, Methodology, Visualization, Writing – original draft. LL: Formal analysis, Supervision, Writing – review & editing. YX: Conceptualization, Supervision, Writing – review & editing. ZQ: Investigation, Validation, Writing – original draft. YZ: Investigation, Validation, Writing – original draft.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This research received funding from Guangdong-Hong Kong-Macao Joint Laboratory for Contaminants Exposure and Health (2020B1212030008/Science and Technology Planning Project of Guangdong Province).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
CD-RISC, Connor-Davidson Resilience Scale; CFS, chronic fatigue syndrome; COVID-19, coronavirus disease 2019; DASS-21, 21-item Depression, Anxiety and Stress Scale; DUFSS, Duke-UNC Functional Social Support Questionnaire; ICU, Intensive Care Unit; I-CVI, item-level content validity index; IQR, Interquartile Range; LASSO, least absolute shrinkage and selection operator; LC, Long-COVID; OR, odds ratio; PEM, postexertional malaise; S-CVI/Ave, average scale-level content validity index.
1. Müller SA, Isaaka L, Mumm R, Scheidt-Nave C, Heldt K, Schuster A, et al. Prevalence and risk factors for long COVID and post-COVID-19 condition in Africa: a systematic review. Lancet Glob Health (2023) 11:e1713–24. doi: 10.1016/S2214-109X(23)00384-4
2. Ventriglio A, Castaldelli-Maia JM, Torales J, Chumakov EM, Bhugra D. Personal and social changes in the time of COVID-19. Ir J Psychol Med (2021) 38:315–7. doi: 10.1017/ipm.2021.23
3. World Health Organization (WHO). A clinical case definition of post COVID-19 condition by a Delphi consensus (2021). Available at: https://www.who.int/publications-detail-redirect/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1 (Accessed Mar 21, 2023).
4. Byambasuren O, Stehlik P, Clark J, Alcorn K, Glasziou P. Effect of covid-19 vaccination on long covid: systematic review. BMJ Med (2023) 2:e000385. doi: 10.1136/bmjmed-2022-000385
5. Ahmad I, Rathore FA. Neurological manifestations and complications of COVID-19: A literature review. J Clin Neurosci (2020) 77:8–12. doi: 10.1016/j.jocn.2020.05.017
6. Nalbandian A, Sehgal K, Gupta A, Madhavan MV, McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med (2021) 27(4):601–15. doi: 10.1038/s41591-021-01283-z
7. Parotto M, Gyöngyösi M, Howe K, Myatra SN, Ranzani O, Shankar-Hari, et al. Post-acute sequelae of COVID-19: understanding and addressing the burden of multisystem manifestations. Lancet Respir Med (2023) 11(8):739–54. doi: 10.1016/S2213-2600(23)00239-4
8. Schou TM, Joca S, Wegener G, Bay-Richter C. Psychiatric and neuropsychiatric sequelae of COVID-19 - A systematic review. Brain Behav Immun (2021) 97:328–48. doi: 10.1016/j.bbi.2021.07.018
9. Goodman ML, Molldrem S, Elliott A, Robertson D, Keiser P. Long COVID and mental health correlates: a new chronic condition fits existing patterns. Health Psychol Behav Med (2023) 11(1):2164498. doi: 10.1080/21642850.2022.2164498
10. Matsumoto K, Hamatani S, Shimizu E, Käll A, Andersson G. Impact of post-COVID conditions on mental health: a cross-sectional study in Japan and Sweden. BMC Psychiatry (2022) 22(1):237. doi: 10.1186/s12888-022-03874-7
11. Zhao Y, Shi L, Jiang Z, Zeng N, Mei H, Lu Y, et al. The phenotype and prediction of long-term physical, mental and cognitive COVID-19 sequelae 20 months after recovery, a community-based cohort study in China. Mol Psychiatry (2023) 28(4):1793–801. doi: 10.1038/s41380-023-01951-1
12. Zhang L, Lei J, Zhang J, Yin L, Chen Y, Xi Y, et al. Undiagnosed long COVID-19 in China among non-vaccinated individuals: identifying persistent symptoms and impacts on patients' Health-related quality of life. J Epidemiol Glob Health (2022) 12(4):560–71. doi: 10.1007/s44197-022-00079-9
13. Klis S, Vingerhoets AJ, de Wit M, Zandbelt N, Snoek FJ. Pictorial Representation of Illness and Self Measure Revised II (PRISM-RII): a novel method to assess perceived burden of illness in diabetes patients. Health Qual Life Outcomes (2008) 6:104. doi: 10.1186/1477-7525-6-104
14. May CR, Eton DT, Boehmer K, Gallacher K, Hunt K, MacDonald S, et al. Rethinking the patient: using Burden of Treatment Theory to understand the changing dynamics of illness. BMC Health Serv Res (2014) 14:281. doi: 10.1186/1472-6963-14-281
15. Hale ED, Treharne GJ, Kitas GD. The common-sense model of self-regulation of health and illness: how can we use it to understand and respond to our patients' needs? Rheumatol (Oxford) (2007) 46:904–6. doi: 10.1093/rheumatology/kem060
16. Sivan M, Parkin A, Makower S, Greenwood DC. Post-COVID syndrome symptoms, functional disability, and clinical severity phenotypes in hospitalized and nonhospitalized individuals: A cross-sectional evaluation from a community COVID rehabilitation service. J Med Virol (2022) 94:1419–27. doi: 10.1002/jmv.27456
17. Larsen NW, Stiles LE, Shaik R, Schneider L, Muppidi S, Tsui CT, et al. Characterization of autonomic symptom burden in long COVID: A global survey of 2,314 adults. Front Neurol (2022) 13:1012668. doi: 10.3389/fneur.2022.1012668
18. World Health Organization (WHO). Young people’s health – a challenge for society Report of a Study Group on Young People and Health for All by the Year 2000, Technical Report Series, No 731 (1986). Geneva: World Health Organization. Available at: http://whqlibdoc.who.int/trs/WHO_TRS_731.pdf (Accessed Apr 5, 2023).
19. Patton GC, Coffey C, Romaniuk H, Mackinnon A, Carlin JB, Degenhardt L, et al. The prognosis of common mental disorders in adolescents: a 14-year prospective cohort study. Lancet (2014) 383:1404–11. doi: 10.1016/S0140-6736(13)62116-9
20. O'Mahoney LL, Routen A, Gillies C, Ekezie W, Welford A, Zhang A, et al. The prevalence and long-term health effects of Long Covid among hospitalised and non-hospitalised populations: A systematic review and meta-analysis. EClinicalMedicine (2022) 55:101762. doi: 10.1016/j.eclinm.2022.101762
21. Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench (2013) 6:14–7. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4017493/.
22. Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales. 2nd. Ed. Sydney: Psychology Foundation (1995). Available at: https://maic.qld.gov.au/wp-content/uploads/2016/07/DASS-21.pdf.
23. Almanasreh E, Moles R, Chen TF. Evaluation of methods used for estimating content validity. Res Soc Adm Pharm (2019) 15:214–21. doi: 10.1016/j.sapharm.2018.03.066
24. Gliner JA, Morgan G. A. Research methods in applied settings: An integrated approach to design and analysis. New York: Routledge (2011) p. 101–10.
25. Ni MY, Li TK, Yu NX, Pang H, Chan BH, Leung GM, et al. Normative data and psychometric properties of the Connor-Davidson Resilience Scale (CD-RISC) and the abbreviated version (CD-RISC2) among the general population in Hong Kong. Qual Life Res (2016) 25:111–6. doi: 10.1007/s11136-015-1072-x
26. Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety (2003) 18:76–82. doi: 10.1002/da.10113
27. Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH. The Duke-UNC Functional Social Support Questionnaire. Measurement of social support in family medicine patients. . Med Care (1988) 26:709–23. doi: 10.1097/00005650-198807000-00006
28. Applebaum AJ, Stein EM, Lord-Bessen J, Pessin H, Rosenfeld B, Breitbart W. Optimism, social support, and mental health outcomes in patients with advanced cancer. Psychooncology (2014) 23:299–306. doi: 10.1002/pon.3418
29. Davis HE, Assaf GS, McCorkell L, Wei H, Low RJ, Re'em Y, et al. Characterizing long COVID in an international cohort: 7 months of symptoms and their impact. EClinicalMedicine (2021) 38:101019. doi: 10.1016/j.eclinm.2021.101019
30. Mclaughlin M, Cerexhe L, Macdonald E, Ingram J, Sanal-Hayes NEM, Meach R, et al. A cross-sectional study of symptom prevalence, frequency, severity, and impact of long-COVID in Scotland: part I. Am J Med (2023). doi: 10.1016/j.amjmed.2023.07.009
31. Liu T, Wu D, Yan W, Wang X, Zhang X, Ma K, et al. Twelve-month systemic consequences of coronavirus disease 2019 (COVID-19) in patients discharged from hospital: A prospective cohort study in Wuhan, China. Clin Infect Dis (2022) 74:1953–65. doi: 10.1093/cid/ciab703
32. Azcue N, Gómez-Esteban JC, Acera M, Tijero B, Fernandez T, Ayo-Mentxakatorre N, et al. Brain fog of post-COVID-19 condition and Chronic Fatigue Syndrome, same medical disorder? J Transl Med (2022) 20:569. doi: 10.1186/s12967-022-03764-2
33. Tate W, Walker M, Sweetman E, Helliwell A, Peppercorn K, Edgar C, et al. Molecular mechanisms of neuroinflammation in ME/CFS and long COVID to sustain disease and promote relapses. Front Neurol (2022) 13:877772. doi: 10.3389/fneur.2022.877772
34. May M, Milrad SF, Perdomo DM, Czaja SJ, Fletcher MA, Jutagir DR, et al. Post-exertional malaise is associated with greater symptom burden and psychological distress in patients diagnosed with Chronic Fatigue Syndrome. J Psychosom Res (2020) 129:109893. doi: 10.1016/j.jpsychores.2019.109893
35. Lehman AM, Lehman DR, Hemphill KJ, Mandel DR, Cooper LM. Illness experience, depression, and anxiety in chronic fatigue syndrome. J Psychosom Res (2002) 52:461–5. doi: 10.1016/s0022-3999(02)00318-5
36. Kämpfen F, Kohler IV, Ciancio A, Bruine de Bruin W, Maurer J, Kohler HP. Predictors of mental health during the Covid-19 pandemic in the US: Role of economic concerns, health worries and social distancing. PloS One (2020) 15:e0241895. doi: 10.1371/journal.pone.0241895
37. Scheid JL, Lupien SP, Ford GS, West SL. Commentary: physiological and psychological impact of face mask usage during the COVID-19 pandemic. Int J Environ Res Public Health (2020) 17:6655. doi: 10.3390/ijerph17186655
38. World Health Organization (WHO). Coronavirus disease (COVID-19) pandemic (2023). Available at: https://www.who.int/europe/emergencies/situations/covid-19 (Accessed April 5, 2023).
39. de Erausquin GA, Snyder H, Carrillo M, Hosseini AA, Brugha TS, Seshadri S, et al. The chronic neuropsychiatric sequelae of COVID-19: The need for a prospective study of viral impact on brain functioning. Alzheimer's Dementia (2021) 17:1056–65. doi: 10.1002/alz.12255
40. Haydon KC, Salvatore JE. Self-regulation predicts mental health and well-being during the Covid-19 pandemic: a prospective study. J Soc Clin Psychol (2022), 41(1):1–29. doi: 10.1521/jscp.2021.40.6.1
41. Cutler DM. The costs of long COVID. JAMA Health Forum (2022) 3:e221809. doi: 10.1001/jamahealthforum.2022.1809
42. Morris W, Correa A, Leiva R. Impact of COVID-19 containment measures on unemployment: A multi-country analysis using a difference-in-differences framework. Int J Health Policy Manag (2023) 12:7036. doi: 10.34172/ijhpm.2022.7036
43. General Office of the National Health Commission(China). Rehabilitation Program for discharged COVID-19 Patients (Trial) (2020). Available at: http://www.nhc.gov.cn/xcs/zhengcwj/202003/d4558d2cc35e44d5b9adba7c911e0b4c.shtml (Accessed 2023 April 3).
44. Tang J, Song T, Kuang M, Feng Y, Liu G, Liu H. Recent advancements on long COVID in China: A narrative review. Int J Gen Med (2023) 16:2585–93. doi: 10.2147/IJGM.S417692
45. Zhong LL, Wong YP, Leung CY, Peng B, Lin ZX, Wong Taam VC, et al. COVID-19 CM Research Working Group. Effects of Chinese medicine for COVID-19 rehabilitation: a multicenter observational study. Chin Med (2022) 17:99. doi: 10.1186/s13020-022-00654-z
46. Sum CH, Ching JYL, Song T, Cheong PK, Lo CW, Lai MK, et al. Chinese medicine for residual symptoms of COVID-19 recovered patients (long COVID)-A double-blind, randomized, and placebo-controlled clinical trial protocol. Front Med (Lausanne) (2023) 9:990639. doi: 10.3389/fmed.2022.990639
47. Xiao Y, Chen TT, Liu L, Zong L. China ends its zero-COVID-19 policy: New challenges facing mental health services. Asian J Psychiatr (2023) 82:103485. doi: 10.1016/j.ajp.2023.103485
48. Mansouri F, Darvishpour A. Mobile health applications in the COVID-19 pandemic: A scoping review of the reviews. Med J Islam Repub Iran (2023) 37:8. doi: 10.47176/mjiri.37.8
49. Stewart C, Ranjan Y, Conde P, Sun S, Rashid Z, Sankesara H, et al. Presentation of long COVID and associated risk factors in a mobile health study. medRxiv (2022) 9:1–24. doi: 10.2196/47294
50. Russell D, Spence NJ, Chase JD, Schwartz T, Tumminello CM, Bouldin E. Support amid uncertainty: Long COVID illness experiences and the role of online communities. SSM Qual Res Health (2022) 2:100177. doi: 10.1016/j.ssmqr.2022.100177
51. Kennedy B, Fitipaldi H, Hammar U, Maziarz M, Tsereteli N, Oskolkov N, et al. App-based COVID-19 syndromic surveillance and prediction of hospital admissions in COVID Symptom Study Sweden. Nat Commun (2022) 13:2110. doi: 10.1038/s41467-022-29608-7
Keywords: Long-COVID, depression, anxiety, stress, mental health, post-COVID conditions
Citation: Li Y, Lam LT, Xiao Y, Qiu Z and Zhang Y (2024) The association between Long-COVID symptomology, perceived symptom burden and mental health in COVID-19 patients in Shijiazhuang, China: a population-based health survey. Front. Psychiatry 15:1332066. doi: 10.3389/fpsyt.2024.1332066
Received: 02 November 2023; Accepted: 10 January 2024;
Published: 26 January 2024.
Edited by:
Gabriele Nibbio, University of Brescia, ItalyReviewed by:
Renata Kochhann, Moinhos de Vento Hospital, BrazilCopyright © 2024 Li, Lam, Xiao, Qiu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Xiao, eXhpYW9AbXVzdC5lZHUubW8=; Lawrence T. Lam, dG1sYW1AbXVzdC5lZHUubW8=
†ORCID: Yufei Li, orcid.org/0000-0002-8015-897X
Lawrence T. Lam, orcid.org/0000-0001-6183-6854
Ying Xiao, orcid.org/0000-0001-5178-1706
Zhengqi Qiu, orcid.org/0000-0003-0033-0512
Yanming Zhang, orcid.org/0000-0003-1181-1629
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.