Abstract
Traditional clinical diagnoses relying on symptoms may overlook latent factors that illuminate mechanisms and potentially guide treatment. The Operationalized Psychodynamic Diagnosis (OPD) system may compensate for symptom-based diagnosis by measuring psychodynamic profiles underlying mental disorders through conflicts and structure axes. However, OPD has not been widely adopted in China, and it remains unclear whether OPD can be used as an effective approach to distinguish between depression and anxiety. The current study aims to adopt the OPD system to investigate the psychodynamic profiles of major depressive disorder (MDD) and generalized anxiety disorder (GAD) in China, targeting patients with “pure” symptoms without comorbidity. We recruited 42 MDD patients, 32 GAD patients, and 31 healthy controls (HC), and assessed their self-report depression and anxiety symptoms, along with their underlying psychodynamic profiles through OPD interviews. Overall, both MDD and GAD patients showed more prominent conflict issues and lower levels of structure than HC. The MDD and GAD groups yielded different conflict profiles and conflict processing modes when processing their second conflicts. Importantly, the multi-dimensional psychodynamic profiles achieved machine learning classification of clinical groups with an accuracy of 0.84, supporting successful distinction of MDD and GAD patients. In conclusion, the OPD demonstrated sensitivity in revealing distinct psychodynamic profiles underlying “pure” depression and anxiety clinical populations in China. This work calls for future incorporation of OPD as a tool to investigate psychodynamic formulations underlying mental disorders, compensating for traditional symptom-based diagnostic approaches to guide precise individualized interventions.
1 Introduction
Major depressive disorder (MDD) and generalized anxiety disorder (GAD) are the top two mental diseases worldwide, severely impacting patients’ psychosocial functioning and quality of life (1, 2). In China, there is a comparable high prevalence of MDD and GAD, with 12-month prevalence estimates of 2.3% and 0.8% and lifetime prevalence estimates of 3.3% and 1.2%, respectively (3, 4). Currently, diagnoses of these mental disorders are based on symptomatology, which results in poor separation of clinical symptom profiles, leading to heterogeneity and comorbidity. This further complicates the identification of appropriate therapeutic interventions and increases the challenges of treatment (5).
To disentangle the intertwined symptoms, psychodynamics provides a unique perspective to investigate the hidden psychological mechanisms in MDD and GAD (6). The Operationalized Psychodynamic Diagnosis (OPD) system (7) is a clinical tool that can provide a multiaxial psychodynamic description for mental illnesses, containing in its second revision (OPD-2) five independent axes: (I) Experience of illness and prerequisites for treatment, (II) Interpersonal relations, (III) Conflict, (IV) Structure, and (V) Mental and psychosomatic disorders. Specifically, Axes III “Conflicts” and IV “Structures” are commonly the only axes being focused on when investigating the psychodynamic profiles of patients, as they align to the psychodynamic core concepts: conflict and structure (8), while interpersonal relations are not rated dimensionally, making the scientific use of OPD axis II difficult and the other two axes play as supplemental assessment from the perspectives outside the psychodynamics. Consistently, Benecke et al. also specified the conflict and structure axes of OPD to explain individual psychodynamic differences (9). Psychodynamic conflicts correspond to the internal and unconscious collision and tensions of opposed tendencies of motives, needs, and wishes. The conflict axis in OPD focuses on the contents and coping style of conflicts, indicating patients handle the following conflicts in a passive or active way: individuation (dependence vs. autonomy), control (submission vs. control), care (need for care vs. autarky), self-worth (undervaluing oneself vs. overvaluing oneself), guilt (self-blame vs. rejecting responsibility), and sexual roles (unattractiveness vs. attractiveness) and identity (lacking identities vs. adoption of identity) (10). Axis IV comprises four main parts: “perception”, “regulation”, “emotion communication” and “attachment”, where each part is rated on a self-related and an object-related dimension, describing the relationships and interaction with self and objects. Together, the OPD structure axis resembles the personality functioning concept as defined in the Alternative DSM-5 Model for Personality Disorders and ICD-11.
Together, the OPD system incorporates perspectives of psychoanalysts, psychosomatic medicine, and psychiatrists in psychotherapy research. The OPD system has become a standard tool for psychotherapy assessment in Germany and has been published and used in several research in English, Portuguese or Spanish (11, 12). Chinese clinical practitioners introduced and adapted this tool in 2009 (13), but it has not been applied in the local clinical settings due to uncertainties in distinguishing the latent psychodynamics of psychiatric illnesses and a lack of comprehensive investigations on the psychodynamic formulations of patient populations under Chinese culture.
In the previous empirical research, MDD and GAD were found to be both associated with abnormalities in low self-esteem, insecure attachment, immature defense mechanisms, common abnormal personality (such as neuroticism and introversion/extraversion), and the processing and regulation of emotion (14–22) corresponding to issues on each indicator in Axis IV structures. Along Axis III in the psychodynamic framework, MDD may be rooted in patients’ unresolved conflicts with others sharing close relationships, giving rise to unconscious feelings of anger and guilt directed towards themselves or others. MDD patients may struggle with these negative feelings due to an immature defense mechanism. Meanwhile, GAD can be attributed to the patient’s excessive worry and anxiety, potentially stemming from an overactive defense mechanism against unconscious fears and perceived threats. The threat may be rooted from insecure/conflicted attachment patterns (23), leading to deficits in self-structure and abnormal defense mechanisms. For instance, the immature defense styles “pseudo altruism” and “reaction formation” were frequently identified in Chinese GAD patients (24).
Axis IV structure level can offer valuable information to predict symptom severity and effectiveness of treatment, thereby guiding the treatment plan. Studies have shown that the greater structural vulnerability of emotional self-regulation influences the severity of depressive symptoms (25). Moreover, the structural level of personality function described in the OPD Structure Questionnaire (OPD-SQ) was found to be associated with the quality of life of depressive patients (26). Will and colleagues (27) found that better structural integration is associated with great capability of reflection, impulse control, and frustration tolerance in depressed patients. For patients with lower levels of structural integration or deficits, supportive therapy including psychoeducational interventions and advice may be necessary in therapy (8). Therefore, these patients may benefit from different intervention methods, shifting back and forth along the expressive-supportive continuum based on their conflict/structure profiles and psychotherapy phrases (8, 28). The expressive-supportive continuum intervention categories include interpretation, observation, confrontation, clarification, encouragement to elaborate, empathic validation, psychoeducational interventions, and advice and praise.
Although psychodynamic profiles have been widely investigated and reported under the western culture, we cannot directly adopt those conclusions to guide our clinical settings due to the impact of cultural factors on clinical presentations. The World Health Organization stated that cross-cultural applicability was a very high priority during the process of revising the symptom-based clinical diagnosis system (29), indicating the existence of culture-specific symptoms. This phenomenon was observed in the variation of the core symptoms of depression and anxiety. Rumination was found to be the core symptom in western culture, while worry instead of rumination plays a central role in the eastern culture (30, 31). Chinese GAD patients were found to use the defense style “pseudo altruism”, and “reaction formation” significantly more than other cultures, manifesting as coping more with repressed rage (24). In addition, the variations in clinical presentations also indicate the possible difference in psychodynamic formulations. Based on OPD, German patients suffered from more frequent conflicts including “need for care vs. autarky” and “guilt conflict”, while Chinese patients had more frequent “dependence vs. individuation” conflicts (32). Although Xu & Cierpka’s study provides insights into the cultural variations in the Conflicts axis, it lacks the psychodynamic profiles of two groups and specific clinical features of the two groups. Therefore, to facilitate the application of the OPD system in MDD and GAD clinical diagnosis and treatment planning, it is necessary to investigate the comprehensive psychodynamic profiles of these two groups in Chinese culture, and a comparison with western findings can help refine the treatments.
In the current study, we aim to examine the sensitivity of Axis III and IV in the OPD system and explore the psychodynamic profiles of MDD and GAD patients in China. Aiming to reveal psychodynamic profiles specifically for each mental disorder, we only recruited patients with a single or “pure” diagnosis, avoiding comorbidity conditions. In the current study, we hypothesize that data will yield similar conflict profiles, such as conflicts in self-worth and guilt, in both MDD and GAD. Additionally, we hypothesize that the strategies for coping with conflicts will be different between clinical groups based on existing research evidence, where MDD individuals may employ more passive coping style (32, 33), and GAD individuals may adopt more active coping style such as “reaction formation” and “pseudo altruism” (24, 33). For the structure levels, we hypothesize that both MDD and GAD patients will demonstrate lower levels of structural integration compared to healthy controls. We further expect MDD patients to exhibit the lowest levels of structural integration due to their utilization of passive conflict processing models, which are more associated with personality functioning impairments (10) in contrast to those with GAD.
2 Method
2.1 Participants
The total sample contains 42 MDD patients (29 female, mean age = 35.05 years, SD = 11.00) including 7 inpatients, 32 GAD outpatients (21 female, mean age = 39.97 years, SD = 11.12), and 31 healthy controls (20 female, mean age = 37.87 years, SD = 10.22). Both MDD and GAD patients were diagnosed by experienced psychiatrists based on the DSM-IV-TR criteria (American Psychiatric Association, 2000), and they were recruited in two independent research projects and in a multi-sited way. They had no other comorbid psychiatric or organic illness that could impact cognitive functions. Healthy controls were excluded if they had any history of psychiatric or neurological disorders, history, or current use of any psychoactive medication. The three groups are matched in marriage status, educational attainment, and occupation status, except for patient care (Table 1). This study was approved by the ethics committee of Peking University Sixth Hospital (Institute of Mental Health) in China, and all participants gave their informed written consent in accordance with the Declaration of Helsinki.
Table 1
| Variables | MDD group (n=42) | GAD group (n=32) | Control group (n=31)) | H/F/χ2 | p | |
|---|---|---|---|---|---|---|
| Age (years) (M ± SD) | 35.05 ± 11.00 | 39.97 ± 11.12 | 37.87 ± 10.22 | 1.927 | 0.151 | |
| Gender N (%) | Male | 13(31.0) | 11(34.4) | 11(35.5) | 0.186 | 0.911 |
| Female | 29(69.0) | 21(65.6) | 20(64.5) | |||
| Marital status N (%) | single | 10(23.8) | 5(15.6) | 9(29.0) | 1.261 | 0.532 |
| married | 24(57.1) | 24(75.0) | 19(61.3) | |||
| divorce | 6(14.3) | 3(9.4) | 3(9.7) | |||
| widowed | 2(4.8) | 0 | 0 | |||
| Educational attainment N (%) | Lower than undergraduate | 27(64.3) | 22(68.8) | 15(48.4) | 0.906 | 0.636 |
| Undergraduate or higher | 15(35.7) | 10(31.2) | 16(51.6) | |||
| Occupation status N (%) | retired | 5(11.9) | 7(21.9) | 2(6.5) | 0.818 | 0.664 |
| employed | 30(71.4) | 20(62.5) | 27(87.1) | |||
| unemployed | 7(16.7) | 5(15.6) | 2(6.5) | |||
| Age of onset (M ± SD) | 31.62 ± 11.72 | 35.66 ± 12.39 | – | -1.43 | 0.156 | |
| Patient care N (%) | inpatient | 7(16.7) | 0(0) | – | 11.250 | 0.004** |
| outpatient | 35(83.3) | 32(100) | – |
Demographic characteristics of the participants.
* p < 0.05 ** p < 0.01 *** p < 0.001. MDD, major depressive disorder; GAD, generalized anxiety disorder; M, mean; SD, standard deviation; N, number.
2.2 Clinical assessments
2.2.1 Hamilton depression rating scale
Depression severity was measured by HAMD-17 (The 17-item Hamilton Depression Rating Scale, Hamilton, 1967), which is a widely used clinician-administered depression assessment tool utilizing a scale of 0 (not present) to 4 (severe). It was developed by Hamilton, where high scores indicate more serious depressive symptoms. The Chinese version has high inter-rater reliability with r = 0.88–0.99 (34).
2.2.2 Hamilton anxiety rating scale
The severity of anxiety symptoms was clinician-rated by a 14-item Hamilton Anxiety Rating Scale (HAMA, Hamilton, 1959). Each item is scored on a scale of 0 (not present) to 4 (severe), with a total score range of 0–56, where < 17 indicates mild severity, 18–24 mild to moderate severity, and 25–30 moderate to severe. The HAMA has high reliability in China with r = 0.93 (35).
2.2.3 Operationalized psychodynamic diagnosis interview
Psychodynamic diagnosis of conflicts (Axis III) and structures (Axis IV) were clinically assessed by two experienced clinicians using the Chinese OPD interview, which was introduced and translated in 2009 (13). In Jiang’s study, the interrater reliabilities for the conflict and structure axes were acceptable, with values of 0.65 and 0.51, respectively, and the 3–5 weeks retest reliabilities were high, with values of 0.81 for the conflict axis and 0.93 for the structure axis. The inter-rater reliability was also verified through prior practice by the same team, and a good agreement between the two raters was found for the conflict axis, with a value of 0.81, and a moderate agreement was found for the structure axis, with a value of 0.58. These results indicate that the psychodynamic diagnosis of conflicts and structures using the Chinese OPD interview in the current study is reliable and valid for use in clinical practice and research.
2.3 Statistical analysis
Statistical analysis was performed by IBM Statistical Package for the Social Sciences (SPSS V20.0). To examine the characteristics of different groups, demographic data, HAMD and HAMA scores, and OPD dimensions among the three groups were compared respectively, by applying one-way ANOVAs and repeated measures ANOVAs for continuous variables and Kruskal-Wallis test or chi-square test for categorical variables, the effect of patient care (inpatient vs. outpatient) was controlled as a covariate.
To further evaluate whether we can use psychodynamic profiles to guide clinical prediction and classification, we utilized the Least Absolute Shrinkage Selection Operator (LASSO) regression, using the glmnet package (36)in R. We used all 20 OPD indicators as predictive variables (see Supplementary Table 2), and groups (MDD, GAD, or HC) as the outcome variable. Data were split into 80% vs. 20% for training and testing respectively. Nested cross-validation with 5 folders was employed during training. The sampling, training, and testing procedures were repeated 100 times as a bootstrapping strategy to examine the confidence interval of the predictive accuracy. Furthermore, to examine the effectiveness of OPD Axes III and IV in group classification, we summarized the frequency of each feature being selected as an effective predictor across 100 iterations of model fitting.
3 Results
3.1 Demographic information
The effectiveness of the grouping was examined and found to be reasonable (Table 1), as there were significant differences among groups in both HAMD (F(2, 102)=94.402, p<0.001) and HAMA (F(2, 98)=114.712, p<0.001). The post-hoc test revealed that MDD (M±SD = 17.67±6.80) group had significantly higher HAMD scores than those in both the GAD (M±SD = 14.06±4.67, p=0.026) and HC (M±SD=1.45±1.72, p<0.001) groups, and individuals in the GAD group (M±SD=23.46±7.45) exhibited the most severe anxiety symptoms as assessed by HAMA when compared to those in the MDD (M ± SD=12.05 ± 5.57, p<0.001) and HC groups (M±SD=2.10±1.83, p <0.001). Both patient groups yielded significantly greater scores on HAMD and HAMA as compared to HCs (ps<0.001).
3.2 Psychodynamic profiles across groups
Axis III Conflicts. After controlling the effect of patient care (inpatient vs. outpatient), the repeated measures ANOVA determined that Axis III “conflict” significantly differed both among groups, F(2, 101)=145.709, p<0.001, η2 =0.743, and among conflict indicators (F(6, 606)=29.802, p<0.001, η2 =0.228) (Figure 1A). The interaction effect between conflict indicators and groups was also significant (F(6, 606)=4.546, p < 0.001, η2 =0.083). However, no significant main of patient care or its interactive effects with other variables has been found (ps>0.05). One-way ANOVAs performed on each “conflict” indicator revealed significant group differences among three groups on the first six indicators (ps<0.015). Specifically, post hoc analysis revealed that individuals in the MDD group demonstrated stronger conflicts than HC on dimensions of “individuation vs. dependence”, “submission vs. control”, “need for care vs. autarky”, and “self-worth conflict”, “guilt conflict” and “oedipal conflict” (ps<0.010, Figures 1B-G). Comparing MDD and GAD, the MDD group yielded stronger conflicts on “individuation vs. dependence” (p=0.025, Figure 1B) and milder “self-worth conflict” (p=0.043, Figure 1E). The GAD group exhibited stronger conflicts than HC on “submission vs. control”, “need for care vs. autarky”, “self-worth conflict” and “guilt conflict” (ps<0.022, Figures 1C-F).
Figure 1
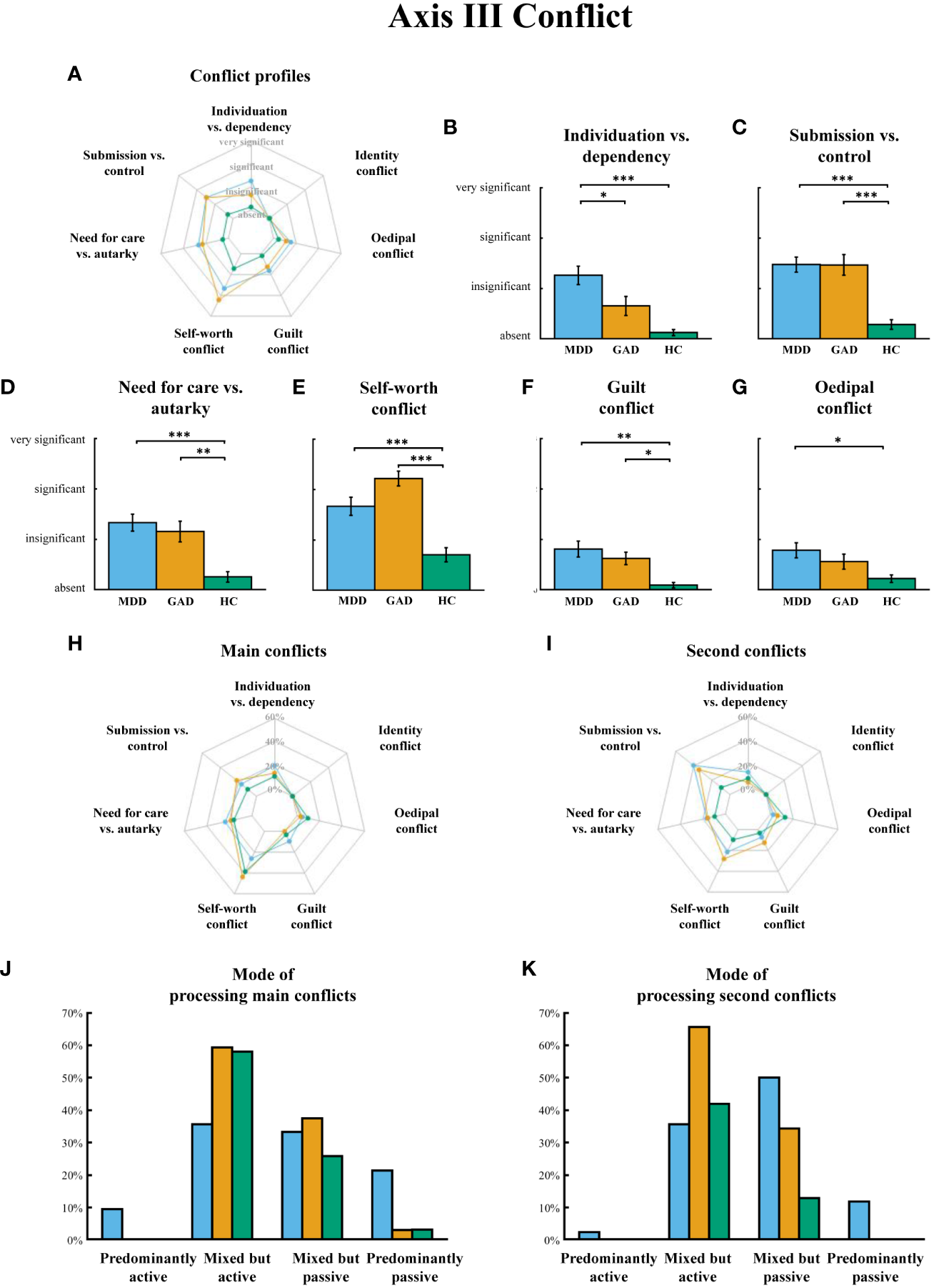
(A) OPD Axis III “conflict” profiles in MDD, GAD and H. (B–G) Significant group differences on conflict dimensions. (H) The composition of main conflict in three groups, expressed as the percentage of the group population. (I) The composition of second conflict in three groups, expressed as the percentage of the group population. (J, K) Their mode of processing main conflicts and second conflicts. MDD = major depressive disorder, GAD = generalized anxiety disorder, HC = healthy controls. Error bars indicate standard errors of the average across participants. * p < 0.05, ** p < 0.01, *** p < 0.001.
It is worth noting that a large proportion of patients in both the MDD (26.2%) and GAD (43.8%) groups identified “self-worth conflict” as their main conflict, with “submission vs. control” being the second most common conflict dimension (MDD: 40.5%; GAD: 34.4%) (Figures 1H, I). However, the assessments of the main and second conflict were independent, i.e., one patient may have “self-worth” as the main conflict but may have a different conflict dimension as their second conflict. Furthermore, one-way ANOVAs found that three groups had no differences in processing mode to main conflicts (F(2,98)=1.578, p=0.212), while they had significant differences in processing mode to second conflicts (F(2,88)=5.560, p=0.005), with MDD group exhibited a “mixed but passive” processing mode, which is significantly different from both GAD (p=0.027) and HC (p=0.018), who tend to process conflicts in a “mixed but positive” way (Figures 1J, K).
Axis IV Structures. Significant differences in the overall structure level among groups were found reflected by the total structure score (F(2,102)=202.512, p<0.001, Figure 2B). Consistently, after controlling the effect of patient care (inpatient vs. outpatient), we used a repeated measures ANOVA to examine the effect of group and structure indicators, with group as between-subject factor and structure indicators as within-subject factor. Results showed that the main effect of group was significant, F(2, 101)=209.164, p<0.001, η2 =0.806, as well as the main effect of structure indicators, F(7, 707)=13.523, p<0.001, η2 =0.118. The interaction effect between structure indicators and groups was also significant, F(14, 707)=2.278, p=0.005, η2 =0.043. Patient care did not show a significant main effect or interactive effect (ps>0.05). One-way ANOVAs on structure indicators further indicated the significant group differences (ps<0.001). Post hoc analysis revealed that both GAD (p.s. < 0.001) and MDD (ps<0.001) had overall lower structure level than HC, and MDD had the lowest structure levels (p.s. < 0.001) in all indicators (Figure 2A). All conflicts and structures profiles of groups were reported in See Supplementary Table 1.
Figure 2
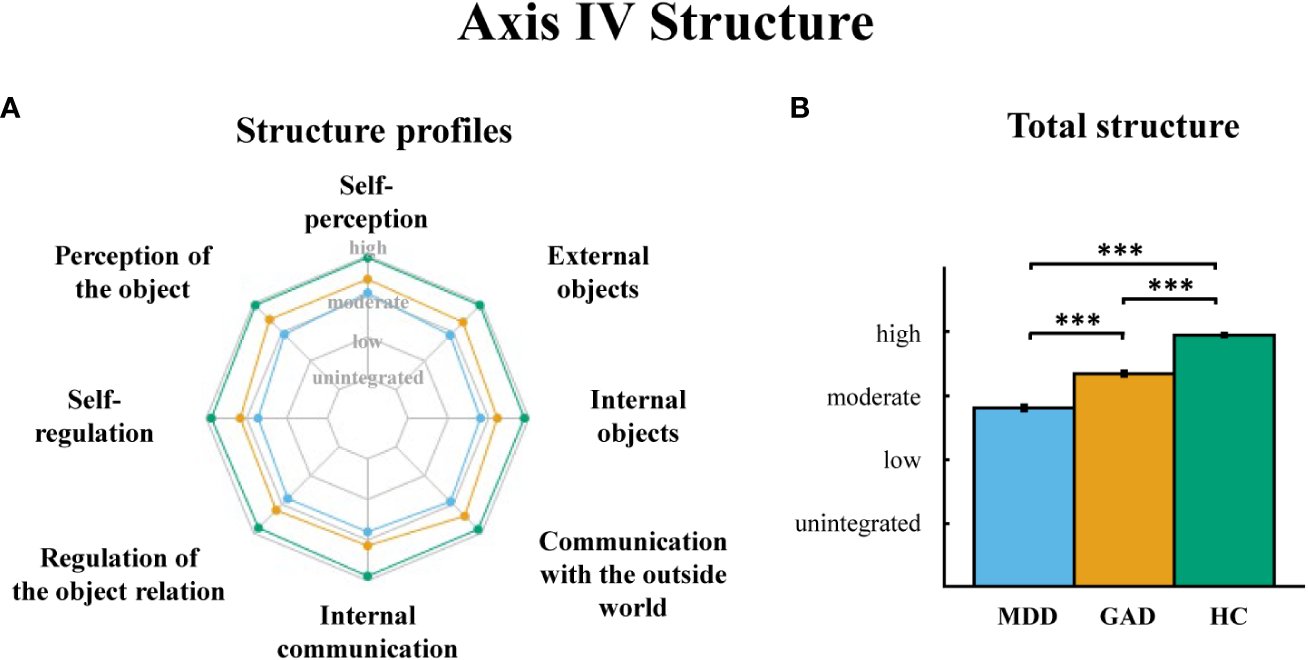
(A) OPD Axis IV “structure” profiles in MDD, GAD, and HC. (B) The total structure score comparisons among three groups. MDD = major depressive disorder, GAD = generalized anxiety disorder, HC = healthy controls. Error bars indicate standard errors of the average across participants. *** p < 0.001.
3.3 Group classification based on psychodynamic profiles
The results of the LASSO regression analysis showed that the OPD Axis III and IV had high predictive and discrimination ability to classify three groups, with the predictive accuracy (M = 0.844, CI [0.650, 1.000]) and the mean area under the curve (AUC) was 0.920 CI [0.833, 1.000].
Looking at feature selections across iterations of model training (Supplementary Table 2), “self-worth conflict” and “total structure” were 100% and 99% selected as effective predictors in the LASSO regression model, followed by two structure indicators “self-regulation” and “attachment to internal objects” with frequencies of 96% and 98% respectively. It is important to note that although there was heterogeneity among the predictive OPD indicators in 100 model iterations, all iterations consistently suggested the OPD profiles can consistently predict and distinguish between clinical groups. For detailed statistical reports, see Supplementary Table 2.
4 Discussion
In the current study, we identified distinct psychodynamic profiles in MDD and GAD, manifesting as more prominent conflicts and lower levels of psychological structure as revealed by OPD Axes III and IV, compared to HC. These results serve as empirical support to the classic psychodynamic theories that MDD and GAD patients have more unconscious conflicts and intrapsychic structure deficits than healthy individuals (8, 26, 37, 38), extending previous evidence that distinguished the psychodynamic profiles between panic disorder patients and MDD patients (39), and studies that suggested different psychodynamic profiles between various anxiety disorders (37, 38).
For Axis III of conflicts, MDD and GAD groups yielded significantly different conflict profiles and conflict processing modes. First, the MDD group demonstrated stronger conflicts on “individuation vs. dependence”, whereas the GAD group yielded stronger conflicts on “self-worth conflict”. The results are consistent with previous evidence where lower self-esteem, insecure attachment and autonomy/independence conflict were found in MDD and GAD (6, 37, 40), and further provide evidence on the differences between MDD and GAD. Second, MDD patients tended to process major conflicts in a “mixed but passive” manner, while GAD patients tended to process them in a “mixed but positive” way when responding to their conflicts. By reviewing evidence-based unified psychodynamic protocol for depressive and anxiety disorders, Leichsenring and Steinert (6) found that different treatments may fit MDD and GAD better separately. Empowering patients to become active participants in the treatment may be specifically relevant for the treatment of depressive patients, while the inner dialogue may have a more calming tone and function for patients with GAD. The significantly different conflict models of MDD and GAD found in our study support these suggestions. Empowerment could alter the relatively passive conflict model in depression, while calming inner dialogue may reduce the active conflict model in anxiety.
Beyond Axis III of conflicts, MDD and GAD also demonstrated significant differences on Axis IV of structure. Specifically, both patient groups demonstrated lower psychological structure levels than the healthy controls, while individuals with MDD demonstrated all the lowest structural profiles. The finding of lower psychological structure in two clinical patient groups may reflect the group difference in immature defense mechanisms. Colovic et al. (41) found that depressive patients more frequently used immature defense mechanisms than anxiety patients. Therefore, MDD patients tend to have more deficits of intrapsychic structure than GAD patients. These lower-than-moderate structure level of MDD patients may be associated with the fact that the patients in the current study were purely diagnosed with MDD in this study, instead of other depressive disorders belonging to neurosis, such as dysthymia or depressive neurosis. MDD is more likely to bring worse symptoms than dysthymia or depressive neurosis. The lower the level of personality functioning or structure level, the higher the severity of depressive symptoms (26). Especially, MDD group and GAD group had significantly different patient care, where the MDD group included 7 inpatients, who often had worse symptoms than outpatients. The current results are also consistent with the previous studies showing structure levels of GAD between moderate and high, along with most clinical neuroses (7). The finding supports the idea that psychodynamic treatment for anxiety focuses on unconscious conflicts and the defense use (23, 42), such as expressive interventions (6). However, structure levels of GAD between moderate and high in the present study are different from findings revealed by Doering and colleagues (22), where they found GAD spanning across all levels of personality organization, from high to low level. Their patients were recruited from both inpatient and outpatient care settings. While the GAD patients in the present study were only in outpatient care settings. Patients from different mental health care settings would have found different personality functioning (22). It is possible GAD outpatients would have better structure levels than GAD inpatients.
As one of our most important findings, the LASSO regression analysis showed that “self-worth conflict” and “total structure” were the most effective predictors, and two structure components “self-regulation” and “attachment capacity internal objects” were the second most effective predictors for distinguishing between the three groups. These results were consistent with the above-mentioned empirical evidence of MDD and GAD associated with lower self-esteem and insecure attachment. In addition, the results serve as evidence of distinct patterns of MDD/GAD-specific psychodynamic profiles, and therefore show the promise that the OPD could be used to assist the more precise diagnosis and interventions of depressive and anxiety patients in the clinics. Based on our data, various transdiagnostic and disorder-specific psychodynamic strategies about conflicts and structure could be designed for an evidence-based intervention for MDD and GAD. For instance, the psychodynamic therapy could consider expressive interventions of self-worth conflict for self-exploration to enhance self-esteem in GAD (6, 42, 43). Meanwhile, the psychodynamic therapy of MDD may focus more on structured and supportive interventions (6, 44, 45), such as promoting self-regulation ability, which was found as the lowest level among dimensions of substructures of MDD participants in our study. However, this only applies to patients on a group level, and each patient needs individualized treatment based on their precise OPD profiles. Moreover, the two substructures “self-regulation” and “attachment capacity internal objects” were found to be the most effective predictors when classifying groups. To a certain extent, our current results are consistent with the finding of Nowak and his team (37). They also found GAD outpatients tended to have impaired self-regulation. Additionally, the current profiles of conflicts in patients may be related to the characteristics of collective Chinese culture. The Chinese culture encourages emotional suppression and encourages people to “experience more other-focused emotions (e.g., sympathy and shame) rather than ego-focused emotions (e.g., anger, frustration, pride)” (46). Thus, the substructure levels of regulation of object-relationships and attachment capacity external objects could be enhanced in the Chinese culture, whereas, the substructure levels of “self-regulation” and “attachment capacity internal objects could be weakened among the Chinese.
Our research is not without limitations. First, the current study enrolled patients with no known comorbidity to aim for higher sample homogeneity, however ending up with a small sample size. Future studies should further expand the sample size to examine the reliability of psychodynamic profiles in China. Second, the effects of inpatient and outpatient subgroups and medicine on their psychodynamics among MDD and GAD patients in this study were not covered, inspiring future studies to further investigate. Third, it would be beneficial to include cultural characteristic assessments to explore the cultural influence on psychodynamic profiles for evidence-based and culture-specific psychotherapy approaches. Fourth, current results reveal psychodynamic patterns of MDD and GAD on a group-level, with limited ability to draw inferences on an individual-level. Together, OPD assessments compensate for the current clinical diagnosis of symptom-based diagnoses of MDD and GAD by revealing hidden psychodynamics and also provide a more economical approach to reveal subtypes of clinical populations in comparison to neuroimaging-based biotype models (47). Future studies should further expand the sample size, collect cultural characteristics, and investigate the impacts of inpatient/outpatient and medicine on psychodynamic profiles, and include self-assessed measures about psychodynamic profiles compensating other OPD assessments (48, 49).
5 Conclusions
In the current study, we used the OPD system to examine the multi-dimensional psychodynamics profiles of MDD, GAD patients, and health participants from China based on a small sample with relatively “pure” clinical symptoms. Results showed good inter-rater reliabilities of the OPD conflict and structure axes and revealed contrasts of conflict models and structure levels in MDD and GAD, promoting the understanding of psychodynamic profiles of MDD and GAD in China. The OPD system may serve as a complementary tool in addition to the classic symptom-based diagnosis system through revealing latent factors that indicate hidden causes of mental disorders and potentially guide treatment for therapists. In clinical practice, the understanding of psychodynamic profiles of a patient may serve as a useful indicator when carrying out clinical therapy intervention, facilitating personalized therapeutic interventions and more effective treatments.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the ethics committee of Peking University Sixth Hospital (Institute of Mental Health) in China. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JX: Conceptualization, Data curation, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing. YW: Formal analysis, Methodology, Writing – review & editing. YP: Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The study was supported by National Natural Science Foundation of China 32200854 and Young Elite Scientists Sponsorship Program 2021QNRC00 to YP.
Acknowledgments
We thank all of the participants for their willingness to participate in the study and the time that they devoted to the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1312980/full#supplementary-material
References
1
Malhi GS Mann JJ . Depression. Lancet (London England) (2018) 392(10161):2299–312. doi: 10.1016/S0140-6736(18)31948-2
2
Penninx BW Pine DS Holmes EA Reif A . Anxiety disorders. Lancet (London England) (2021) 397(10277):914–27. doi: 10.1016/S0140-6736(21)00359-7
3
Gu L Xie J Long J Chen Q Chen Q Pan R et al . Epidemiology of major depressive disorder in mainland China: a systematic review. PloS One (2013) 8(6):e65356. doi: 10.1371/journal.pone.0065356
4
Ma X Xiang YT Cai ZJ Lu JY Li SR Xiang YQ et al . Generalized anxiety disorder in China: prevalence, sociodemographic correlates, comorbidity, and suicide attempts. Perspect Psychiatr Care (2009) 45(2):119–27. doi: 10.1111/j.1744-6163.2009.00212.x
5
Zhou Y Cao Z Yang M Xi X Guo Y Fang M et al . Comorbid generalized anxiety disorder and its association with quality of life in patients with major depressive disorder. Sci Rep (2017) 7:40511. doi: 10.1038/srep40511
6
Leichsenring F Steinert C . Towards an evidence-based unified psychodynamic protocol for emotional disorders. J Affect Disord (2018) 232:400–16. doi: 10.1016/j.jad.2017.11.036
7
Force OT . Operationalized psychodynamic diagnosis OPD-2: Manual of diagnosis and treatment planning. (2008).
8
Gabbard GO . Psychodynamic psychiatry in clinical practice, 5th ed Vol. 639-xiv. . Arlington, VA, US: American Psychiatric Publishing, Inc (2014).
9
Benecke C Remmers C Henkel M Zimmermann J . Oops, I did it again: The role of motivational conflicts and impaired psychological capacities in explaining the persistence of maladaptive behavior. Eur J Personality (2018) 32(5):525–624. doi: 10.1002/per.2174
10
Remmers C Wester R Repnik LG Plumbohm M Unger S Jauk E . Psychodynamic theory meets HiTOP: The nomological network between motivational conflicts and dimensions of the hierarchical taxonomy of psychopathology (HiTOP). J Res Personality (2023) 106:104418. doi: 10.1016/j.jrp.2023.104418
11
Vicente CS Oliveira RA Silva F Ferrajão P Augusto S Oliveira S et al . Cross-cultural adaptation of the operationalized psychodynamic diagnosis (OPD-2) in Portugal. Trends Psychiatry Psychother (2012) 34(3):129–38. doi: 10.1590/S2237-60892012000300004
12
Both L Bastos A Freitas L . Operationalized psychodynamic diagnosis: a systematic review of the literature. Trends Psychiatry Psychother (2019) 41(2):201–10. doi: 10.1590/2237-6089-2018-0020
13
Jiang WH Xiao ZP Wang X Zhang HY Qiu JY . The reliability and validity of operationalized psychodynamic diagnostics system. Chin J Behav Med Brain Sci (2009) 18(6):561–5. doi: 10.3760/cma.j.issn.1674-6554.2009.06.030
14
Clark LA Watson D Mineka S . Temperament, personality, and the mood and anxiety disorders. J Abnorm Psychol (1994) 103(1):103–16. doi: 10.1037/0021-843X.103.1.103
15
Gamez W Watson D Doebbeling BN . Abnormal personality and the mood and anxiety disorders: Implications for structural models of anxiety and depression. J Anxiety Disord (2007) 21(4):526–39. doi: 10.1016/j.janxdis.2006.08.003
16
Marganska A Gallagher M Miranda R . Adult attachment, emotion dysregulation, and symptoms of depression and generalized anxiety disorder. Am J Orthopsychiatry (2013) 83(1):131–41. doi: 10.1111/ajop.12001
17
Martinez R Senra C Fernandez-Rey J Merino H . Sociotropy, autonomy and emotional symptoms in patients with major depression or generalized anxiety: the mediating role of rumination and immature defenses. Int J Environ Res Public Health (2020) 17(16):5716. doi: 10.3390/ijerph17165716
18
Prince EJ Siegel DJ Carroll CP Sher KJ Bienvenu OJ . A longitudinal study of personality traits, anxiety, and depressive disorders in young adults. Anxiety Stress Coping (2021) 34(3):299–307. doi: 10.1080/10615806.2020.1845431
19
Schrier AC de Wit MA Krol A Fassaert TJ Verhoeff AP Kupka RW et al . Similar associations between personality dimensions and anxiety or depressive disorders in a population study of Turkish-Dutch, Moroccan-Dutch, and native Dutch subjects. J Nerv Ment Dis (2013) 201(5):421–8. doi: 10.1097/NMD.0b013e31828e110d
20
Spinhoven P Kooiman CG . Defense style in depressed and anxious psychiatric outpatients: an explorative study. J Nerv Ment Dis (1997) 185(2):87–94. doi: 10.1097/00005053-199702000-00004
21
Lyon K Elliott R Ware K Juhasz G Brown L . Associations between facets and aspects of big five personality and affective disorders:A systematic review and best evidence synthesis. J Affect Disord (2021) 288:175–88. doi: 10.1016/j.jad.2021.03.061
22
Doering S Blüml V Parth K Feichtinger K Gruber M Aigner M et al . Personality functioning in anxiety disorders. BMC Psychiatry (2018) 18(1):294. doi: 10.1186/s12888-018-1870-0
23
Crits-Christoph P Connolly MB Azarian K Crits-Christoph K Shappell S . An open trial of brief supportive-expressive psychotherapy in the treatment of generalized anxiety disorder. Psychother: Theory Res Practice Training (1996) 33(3):418–30. doi: 10.1037/0033-3204.33.3.418
24
Xiao B Xie W Zhang F Shi Z Qiu C Qiu K . investigation on the defense style, social support and family function in patients with depression and anxiety. Chin J Behav Med Sci (2006) 15(9):797–9.
25
Dagnino P Pérez C Gómez A Gloger S Krause M . Depression and attachment: how do personality styles and social support influence this relation? Res Psychother (Milano) (2017) 20(1):237. doi: 10.4081/ripppo.2017.237
26
Crempien C Grez M Valdés C López MJ de la Parra G Krause M . Role of personality functioning in the quality of life of patients with depression. J Nerv Ment Dis (2017) 205(9):705–13. doi: 10.1097/NMD.0000000000000676
27
Will H Grabenstedt Y Völkl G Banck G . Depression. Psychodynamik und Therapie. Auflage: 3., überarbeitete und erweiterte Auflage. Stuttgart: W. Kohlhammer GmbH. (2008).
28
Centonze A Ottavi P MacBeth A Popolo R Dimaggio G . Modular treatment for complex depression according to metacognitive interpersonal therapy. In: de la ParraGDagninoPBehnA, editors. Depression and Personality Dysfunction: An Integrative Functional Domains Perspective. Cham: Springer International Publishing (2021). p. 245–76.
29
International Advisory Group for the Revision of ICD-10 Mental and Behavioural Disorders . A conceptual framework for the revision of the ICD-10 classification of mental and behavioural disorders. World Psychiatry (2011) 10(2):86–92. doi: 10.1002/j.2051-5545.2011.tb00022.x
30
Yook K Kim K-H Suh SY Lee KS . Intolerance of uncertainty, worry, and rumination in major depressive disorder and generalized anxiety disorder. J Anxiety Disord (2010) 24(6):623–8. doi: 10.1016/j.janxdis.2010.04.003
31
Yang MJ Kim BN Lee EH Lee D Yu BH Jeon HJ et al . Diagnostic utility of worry and rumination: a comparison between generalized anxiety disorder and major depressive disorder. Psychiatry Clin Neurosci (2014) 68(9):712–20. doi: 10.1111/pcn.12193
32
Xu J Cierpka M . P-441 - The psychodynamic profiles of Chinese and German depressed patients. Eur Psychiatry (2012) 27:1. doi: 10.1016/S0924-9338(12)74608-4
33
Vierl L Juen F Benecke C Hörz-Sagstetter S . Exploring the associations between psychodynamic constructs and psychopathology: A network approach. Pers Ment Health (2022) 17(1):40–54. doi: 10.1002/pmh.1559
34
Tang Y. H. Zhang M. Y. Hamilton Depression Rating Scale (HAMD). Shanghai Archives of Psychiatry (1984) 2 (3):61–4.
35
Tang YH Zhang MY . Hamilton anxiety rating scale (HAMA). Shanghai Arch Psychiatry (1984) 2(3):64–5.
36
Friedman J Hastie T Tibshirani R . Regularization paths for generalized linear models via coordinate descent. J Stat Software (2010) 33(1):1–22. doi: 10.18637/jss.v033.i01
37
Nowak J Nikendei C Rollmann I Orth M Friederich HC Kindermann D . Characterization of different types of anxiety disorders in relation to structural integration of personality and adverse and protective childhood experiences in psychotherapy outpatients - a cross-sectional study. BMC Psychiatry (2023) 23(1):501. doi: 10.1186/s12888-023-04988-2
38
Gruber M Doering S Bluml V . Personality functioning in anxiety disorders. Curr Opin Psychiatry (2020) 33(1):62–9. doi: 10.1097/YCO.0000000000000556
39
Almeida YA Nardi AE . Psychological features in panic disorder: A comparison with major depression. Arquivos Neuro-Psiquiatria (2002) 60(3-A):553–7. doi: 10.1590/S0004-282X2002000400007
40
Milrod B Shapiro T Gross C Silver G Preter S Libow A et al . Does manualized psychodynamic psychotherapy have an impact on youth anxiety disorders? Am J Psychother (Association Advancement Psychother) (2013) 67(4):359–66. doi: 10.1176/appi.psychotherapy.2013.67.4.359
41
Colovic O Lecic Tosevski D Perunicic Mladenovic I Milosavljevic M Munjiza A . Defense mechanisms in “Pure” Anxiety and “Pure” Depressive disorders. J Nerv Ment Dis (2016) 204(10):746–51. doi: 10.1097/NMD.0000000000000559
42
Slavin-Mulford J Hilsenroth MJ . Evidence-based psychodynamic treatments for anxiety disorders: A review. In: LevyRAAblonJSKächeleH, editors. Psychodynamic Psychotherapy Research: Evidence-Based Practice and Practice-Based Evidence. Totowa, NJ: Humana Press (2012). p. 117–37.
43
Crits-Christoph P Crits-Christoph K Wolf-Palacio D Fichter M Rudick D . Brief supportive-expressive psychody. Dynamic Therap Psychiat Disord (Axis I) (1995), 43–83. doi: 10.1002/jclp.20435
44
Molenaar PJ Dekker J Van R Hendriksen M Vink A Schoevers RA . Does adding psychotherapy to pharmacotherapy improve social functioning in the treatment of outpatient depression? Depress Anxiety (2007) 24(8):553–62. doi: 10.1002/da.20254
45
de Maat S Dekker J Schoevers R van Aalst G Gijsbers-van Wijk C Hendriksen M et al . Short psychodynamic supportive psychotherapy, antidepressants, and their combination in the treatment of major depression: a mega-analysis based on three randomized clinical trials. Depress Anxiety (2008) 25(7):565–74. doi: 10.1002/da.20305
46
Dwairy M . Foundations of psychosocial dynamic personality theory of collective people. Clin Psychol Rev (2002) 22(3):345–62. doi: 10.1016/S0272-7358(01)00100-3
47
Williams LM . Defining biotypes for depression and anxiety based on large-scale circuit dysfunction: a theoretical review of the evidence and future directions for clinical translation. Depress Anxiety (2017) 34(1):9–24. doi: 10.1002/da.22556
48
Dinger U Schauenburg H Hörz S Rentrop M Komo-Lang M Klinkerfuß M et al . Self-report and observer ratings of personality functioning: A study of the OPD system. J Pers Assessment (2014) 96(2):220–5. doi: 10.1080/00223891.2013.828065
49
Obbarius A Ehrenthal JC Fischer F Liegl G Obbarius N Sarrar L et al . Applying item response theory to the OPD structure questionnaire: identification of a unidimensional core construct and feasibility of computer adaptive testing. J Pers Assessment (2021) 103(5):645–58. doi: 10.1080/00223891.2020.1828435
Summary
Keywords
operationalized psychodynamic diagnosis, major depressive disorder (MDD), generalized anxiety disorder (GAD), psychodynamic profile, personality organization
Citation
Xu J, Wang Y and Peng Y (2024) Psychodynamic profiles of major depressive disorder and generalized anxiety disorder in China. Front. Psychiatry 15:1312980. doi: 10.3389/fpsyt.2024.1312980
Received
11 October 2023
Accepted
08 January 2024
Published
23 January 2024
Volume
15 - 2024
Edited by
Emanuel Jauk, Medical University of Graz, Austria
Reviewed by
Larissa Vierl, University of Kassel, Germany
Casimiro Cabrera Abreu, Queen’s University, Canada
Anna-Lisa Schuler, Max Planck Institute for Human Cognitive and Brain Sciences, Germany
Updates
Copyright
© 2024 Xu, Wang and Peng.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jia Xu, dr_xujia@163.com; Yujia Peng, yujia_peng@pku.edu.cn
†These authors share last authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.