
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 05 February 2024
Sec. Aging Psychiatry
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1305945
 Vanessa Giffoni M. N. P. Peixoto1,2*
Vanessa Giffoni M. N. P. Peixoto1,2* Lucas Alves Facci3
Lucas Alves Facci3 Thiago C. S. Barbalho3
Thiago C. S. Barbalho3 Raíssa Nascimento Souza3
Raíssa Nascimento Souza3 Alice Mendes Duarte3
Alice Mendes Duarte3 Katie Moraes Almondes1,4
Katie Moraes Almondes1,4Introduction: Sleep problems are one of the most persistent symptoms of post-COVID syndrome in adults. However, most recent research on sleep quality has relied on the impact of the pandemic, with scarcely any data for older adults on the long-term consequences of COVID infection. This study aims to understand whether older individuals present persistently impaired sleep quality after COVID-19 infection and possible moderators for this outcome.
Methods: This is a cross-sectional analysis of a longitudinal cohort study with 70 elders with 6-month-previous SARS-CoV-2 infection and 153 controls. The Pittsburgh Sleep Quality Index (PSQI) was used to assess sleep quality; Geriatric Depression Scale and Geriatric Anxiety Inventory for screening depression and anxiety. Demographics and comorbid conditions were collected.
Results: The mean age of participants was 66,97 ± 4,64 years. There were no statistical differences in depression and anxiety between groups. Poor sleep quality was found in 52,9% and 43,8% of the COVID and control groups (p=.208). After controlling for multiple variables, all the following factors resulted in greater chances of poor sleep quality: female gender (OR, 2.12; p=.027), memory complaints (OR, 2.49; p=.074), insomnia (OR, 3.66; p=.032), anxiety (OR, 5.46; p<.001), depression (OR, 7.26; p=.001), joint disease (OR, 1.80; p=.050), glucose intolerance (OR, 2.20; p=.045), psychoactive drugs (OR, 8.36; p<.001), diuretics (OR, 2.46; p=.034), and polypharmacy (OR, 2.84; p=.016).
Conclusion: Psychosocial burden in the context of the COVID-19 pandemic and pre-existing conditions seems to influence the sleep quality of older adults more than SARS-CoV-2 infection.
Although the COVID-19 pandemic was declared over in May 2023 (1), it remains the most devastating disease in recent history, with unprecedented global spread leading to social and economic crises worldwide. For over two years, strict policy responses, including social distancing interventions, were adopted to prevent COVID transmission and protect the most vulnerable. Older adults were considered highly susceptible to COVID-19 complications and have consequently suffered more severe and prolonged social isolation (2), leading to deleterious impacts on their mental and physical health (3). On the other hand, some studies have pointed toward better adaptation and lower psychological distress in this age group compared to younger individuals (4, 5), possibly reflecting higher levels of resilience mediating COVID-19 stressors (5, 6).
Sleep has restorative and regulatory functions (7), being crucial to memory and other neurocognitive functions (8), hormone production (9), support of the immune system (10), metabolic control (7), and cardiovascular protection (11). Indeed, sufficient evidence links poor sleep health to a variety of adverse outcomes (12, 13). As a result, the American Heart Association has recently updated its ‘Life Essential’ guidelines to include sleep health as the newest crucial factor in optimizing cardiovascular health (14). Meanwhile, aging is associated with physiological changes in sleep architecture, circadian rhythm shifts, chronic medical and psychiatric illnesses, and polypharmacy (9, 15, 16), all concurring for a higher prevalence of sleep disorders (16, 17). As such, pre-existing sleep problems have been hypothesized to partially explain the unfavorable outcomes in the older age group during COVID infection (18).
Adequate sleep depends on various behavioral factors, including sunlight exposure, outdoor physical activities, sleeping schedules, nocturnal use of digital gadgets, and psychosocial issues (15, 19). Economic uncertainties, fear of getting infected, and loneliness are examples of the psychological distress that arose from the COVID-19 outbreak, not to mention social isolation and home confinement, which intensely disrupted daily routines, daylight exposure, and circadian rhythms (18, 20).
Given these facts, most recent research on sleep quality has addressed the impact of the pandemic itself on the quality of sleep of the overall population (19, 21, 22). After the first year of the COVID-19 pandemic, two systematic reviews and meta-analyses reported pooled prevalence of sleep problems between 18% to 37,5% in the general population, contrasting with 57% to 74,8% among patients who recently recovered from infection (19, 23), therefore suggesting that SARS-CoV-2 infection might implicate future sleep problems. With a look at post-COVID syndrome, Chen et al. (24) reported the prevalence of sleep problems of 11% (95% CI, 0.05–0.23) up to 120 days post-infection in a meta-analysis that gathered information from 1,680,003 COVID‐19 patients. Interestingly, Huang et al. (25) followed up on 1,119 adult Chinese patients (median age of 57 years) 2 years after recovering from SARS‐CoV‐2 infection and found at least one persistent symptom in as much as 55% of patients, fatigue and sleep disturbances being the most common complaints. Remarkably, older age was one of the strongest predictors of symptom persistence in this cohort. Nonetheless, concerning older patients, few studies have specifically investigated whether sleep might be persistently disturbed long after COVID infection (26). Hence, this study aims to understand whether older individuals have long-term impacts on sleep quality after COVID-19 infection and which factors may influence this outcome.
This is a cross-sectional analysis of a longitudinal cohort study with a total follow-up of two years, comprising two groups of older adults, either previously infected by the novel coronavirus or healthy peers. Recruitment took place in March 2021, during the second wave of the pandemic, in which the Gamma variant was circulating. Eligible participants were those aged 60 to 80 with a formal education of over four years. COVID (+) participants were recruited from a private laboratory in Natal, Brazil, among all 527 patients in this age group diagnosed with SARS-CoV-2 infection by RT-PCR technique this month. Healthy controls, which means those who had never been infected by SARS-CoV-2, were engaged through social media announcements, in whom the serologic status was tested through the ELISA technique to rule out previously unknown disease. Of note, these subjects had not received any COVID vaccine yet. Individuals with previous cognitive decline, uncontrolled psychiatric conditions, recent stroke, heart attack, or cardiac arrest were excluded. The general inclusion and exclusion criteria were applied to both cohorts. After inclusion and exclusion criteria were applied and due to the longitudinal nature of the study and the anticipated proportion of controls to contract COVID-19 during the follow-up, a final of 70 COVID and 153 control participants comprised the initial sample. They were submitted to three comprehensive in-person interviews by a certified geriatrician, neuropsychologist, and trained research assistants. The data presented in this paper was collected between May and September 2021 and relates to the first of three assessments of the prospective follow-up. In the COVID group, six months elapsed from the COVID-19 diagnosis to the assessment.
A structured questionnaire was used to record data on demographics and self-report of comorbid conditions. Depression was screened by the Geriatric Depression Scale (GDS-15), ranging from 0 to 15, with higher scores indicating higher depression probability (27). Anxiety was suggested by scores higher than 10 on the Geriatric Anxiety Inventory (GAI) (28). The Pittsburgh Sleep Quality Index (PSQI) (29, 30) was used to assess sleep quality within the last month. It is a 19-item questionnaire addressing seven components of sleep quality: subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, sleep medication intake, and daytime dysfunction. Each component score is rated on a 0–3 scale, where 3 on the Likert scale corresponds to a negatively extreme response. The total score leads to a sum of up to 21 points, in which PSQI scores > 5 indicate poor sleep quality and ≤ 5 indicate good sleep quality.
Statistical analyses were performed with the IBM® Statistical Package for Social Sciences (SPSS) version 23. Descriptive and inferential analyses were completed for demographic and clinical data, GDS-15, GAI, and PSQI. According to the Shapiro-Wilk test, normally distributed continuous variables were analyzed by Student’s t-test or Mann–Whitney test for non-normally distributed variables. Pearson’s chi-square or Fisher’s tests were used for group comparisons on nominal variables. A p-value <.05 was considered statistically significant. All categorical variables with p-values <.20 were tested through a multivariate logistic regression, identifying poor sleep quality predictors.
The study was conducted by ethical guidelines after approval by the local Research Ethics Committee of UFRN – Campus Central, Natal, Brazil, under process number 44011221.8.0000.5537. Written informed consent was collected from all participants before conducting the study. All information was kept confidential.
A total of 223 older adults aged 60 to 78 participated in the study (70 with previous exposure to SARS-CoV-2 - COVID (+) and 153 healthy controls). The mean age of participants was 66,97 ± 4,64 years. The female gender accounted for approximately 70% of participants. Other sociodemographic characteristics of the sample are summarized in Table 1. Frequencies of the leading clinical conditions and the medications in use are summarized in Table 2. Most participants reported exercising regularly (Table 1). Depression estimate, according to the GDS-15 was approximately 8% in both groups; anxiety measured by GAI was 17.1% and 11.1% in the COVID and control groups, respectively. There were no statistically significant differences in depression and anxiety between groups (Table 3).
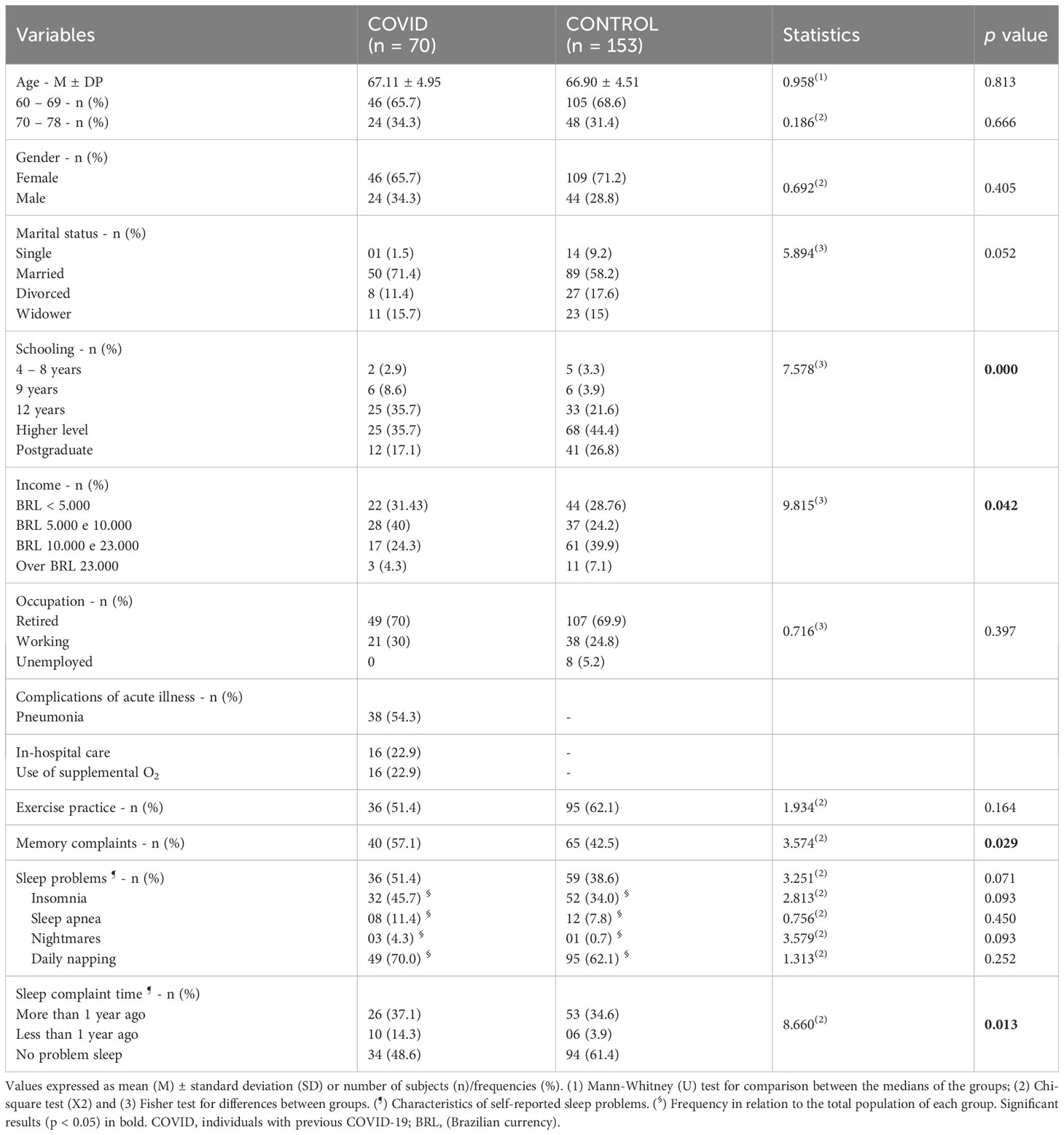
Table 1 Comparison of sociodemographic and clinical characteristics between COVID and CONTROL groups during the second wave of COVID-19.
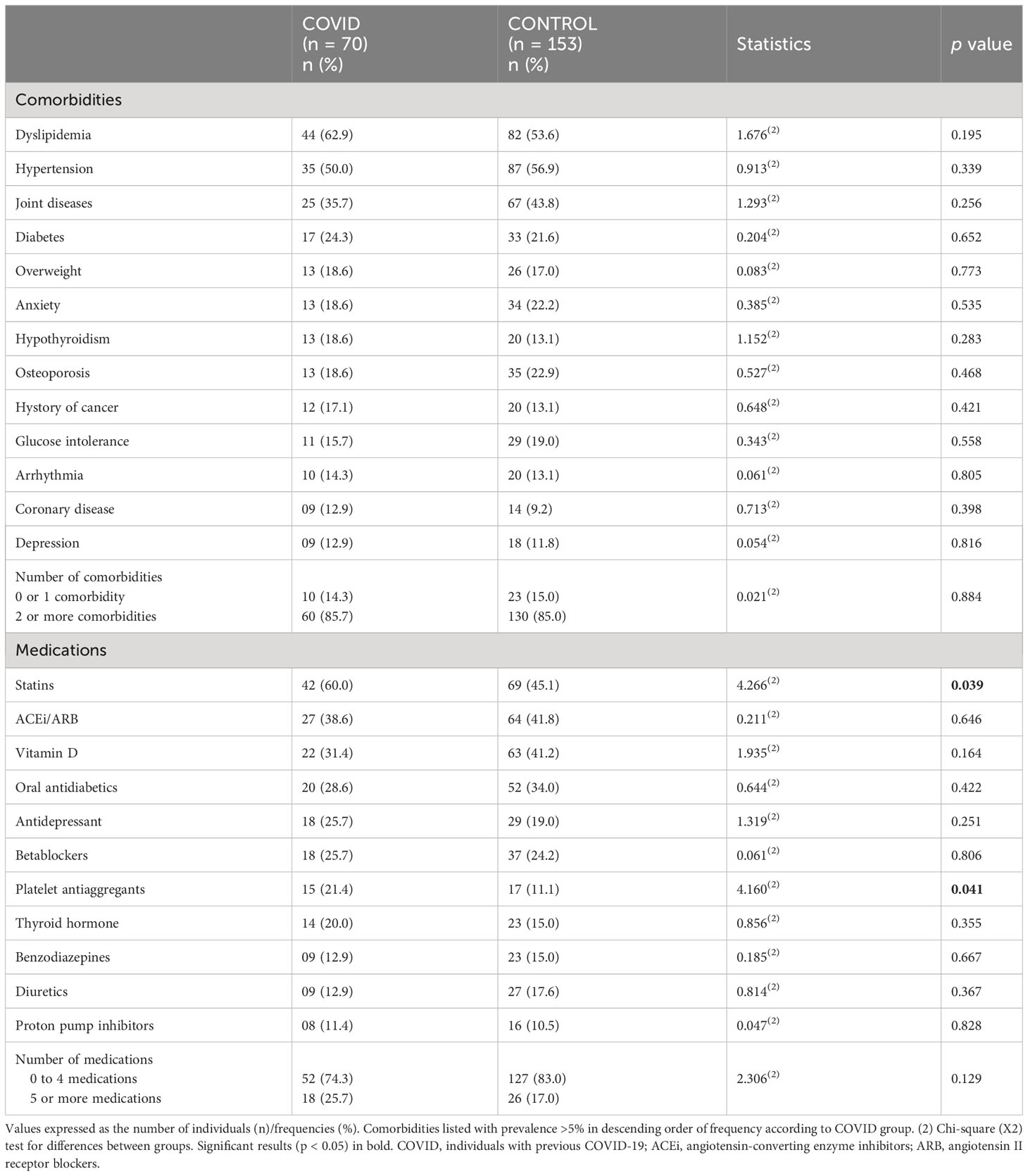
Table 2 Comparison of the prevalence of self-reported comorbidities and medications in use between the COVID (at the time of collection) and CONTROL groups.
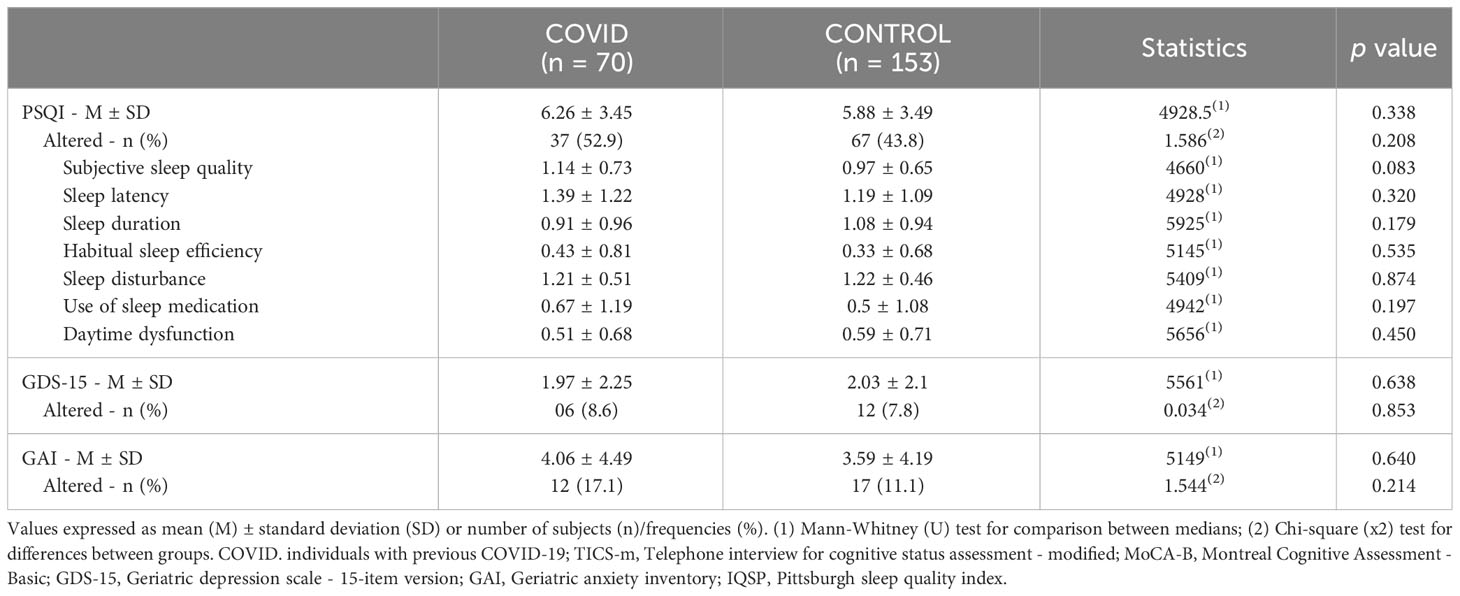
Table 3 Comparison of the results of screening tests for poor sleep quality, depression, and anxiety (PSQI/GDS-15/GAI) between the COVID group (at the time of collection) and the control group (absolute values and respective binary classification according to cut-off points when available).
Participants from the COVID group reported more sleep difficulties (51.4%) compared to the control group (38.6%), although this difference was not statistically significant (X2 = 3.251, gl=1, p= .071). Insomnia and sleep apnea were the most cited sleep problems during the second wave of the pandemic. Regarding individuals who reported sleep-related conditions, 72% of the COVID group and 90% of the control group already presented this complaint for over a year. Daily naps were reported by 70% of the COVID group and 62.1% of the control group (Table 1). Mean PSQI scores were 6,26 ± 3,45 in the COVID group and 5,88 ± 3,49 in the control group (U=4928,5; p= .338). According to a cut-off point of 5 in the PSQI, 52,9% and 43,8% of the COVID and control groups had poor sleep quality (X2 = 1,586, df= 1, p= .208 - Table 3).
After controlling for multiple variables, logistic regression analysis identified some factors associated with greater chances of having poor quality of sleep according to the PSQI scale: female gender (OR, 2.12; 95% CI, 1.09–4.11; p= .027), individuals with memory complaints (OR, 2.49; 95% CI, 0.92–6.76; p= .074), insomnia (OR, 3.66; 95% CI, 1.12–11.96, p= .032), self-reported anxiety (OR, 5.46; 95% CI, 2.46–12.11; p<.001), self-reported depression (OR, 7.26; 95% CI, 2.30–22.88, p= .001), joint disease (OR, 1.80; 95% CI, 0.99–3.26; p= .050), and glucose intolerance (OR, 2.20; 95% CI, 1.02–4.76; p= .045). Also, those in use of psychoactive drugs (OR, 8.36; 95% CI, 4.14–16.87; p<.001), diuretics (OR, 2.46; 95% CI, 1.07–5.66; p= .034), and polypharmacy (OR, 2.84; 95% CI, 1.22–6.63; p= .016) were more likely to have poor sleep quality (Table 4).
Sleep problems seem to be one of the most persistent symptoms of post-COVID syndrome in adults older than 18 years, with a variety of predisposing factors, such as older age, female gender, the severity of the acute illness, the time of follow-up from recovery, and premorbid conditions (24, 25). Our study demonstrated a high proportion of sleep complaints among older adults during the second wave of the pandemic, regardless of previous SARS-CoV-2 infection. Nearly half of the participants reported poor sleep quality according to PSQI. Although PSQI mean score and its ‘subjective sleep quality’, ‘latency’ and ‘efficiency’ components were higher in the COVID group, no statistically significant difference was found when comparing them to healthy controls (Table 3).
Contrary to what we expected, previous SARS-CoV-2 infection did not influence sleep quality in persons 60 and over six months after infection. We have hypothesized some explanations for this finding: (1) the older age group has been assumed to be the most at-risk population for COVID-19, and most of them were submitted to more prolonged and strict social isolation. As so, the psychosocial burden and confinement measures due to the COVID-19 pandemic per se might have been the primary responsible for sleep problems in both groups, including that of healthy controls (19, 21); (2) it is intuitive that the severity of SARS-CoV-2 infection possibly implicates further neurological sequelae (24, 31). In our study, only one in every four patients of the COVID (+) group needed in-hospital care (Table 1), leading us to extrapolate that most of this cohort experienced mild illness, resulting in less probable post-COVID symptoms; (3) there is scarcely any data on the Gamma variant post-COVID syndrome, and it is plausible that this strain causes less disturbed sleep like the Delta variant (32); (4) higher formal schooling (33) and income (34) have been associated with better-coping strategies (24) and pointed as protective factors against worsening sleep quality. Surprisingly, both cohorts in this study have been mainly composed of subjects with high income and at least a higher degree of education, which could have prevented participants from experiencing worse sleep complaints; (5) finally, as mentioned elsewhere in this article, the aging process is associated with greater resilience to stressful events, possibly resulting in less deleterious impacts on the sleep when compared to younger individuals (5, 6).
After controlling for multiple variables, our results indicated greater chances of inadequate sleep in women, people with self-reported anxiety and depression, arthritis, glucose intolerance, cognitive complaints, psychoactive drugs, diuretics, and polypharmacy. Although men are more susceptible to severe forms of acute COVID-19, women seem to be disproportionally affected by long COVID symptoms (35, 36), also in sleep issues (37). Biological and psychosocial factors might explain such differences, starting with women being more likely to report somatic symptoms (38). Additionally, traditional social roles in low and middle-income countries, such as caring for family members and domestic duties, might have overwhelmed women during COVID-19 pandemic and implicated greater stress levels and poorer sleep quality (39). Biological sex differences in structure and hormones also justify discrepancies in sleep architecture and disorders (see Mallampalli and Carter for detailed review) (40).
Importantly, participants suffering from depression and anxiety experienced chances of poor sleep 5 to 7 times higher, in line with the entire body literature on the reciprocal relationship between sleep disturbances and psychiatric comorbidities (19, 41–43). In keeping with this view, taking psychoactive drugs also hugely impacted on worse sleep quality, probably through different mechanisms. First, psychoactive compounds potentialize monoaminergic transmission and receptors’ activity, affecting sleep integrity (44); second, some antidepressants may exacerbate primary sleep disturbances such as restless legs syndrome and periodic limb movement, whereas benzodiazepines and opioids may accentuate obstructive sleep apnea (44); finally, the relationship between psychoactive drugs and sleep quality might indirectly reflect the link between pre-existing neuropsychiatric conditions and sleep issues. However, our study has neither identified a single pharmacological agent underlying this association nor explored whether these drugs may have been prescribed as sleeping aids.
Diuretic drugs also doubled the chances of poor sleep in our sample of elders. Nocturia was the main reason for disturbed sleep in a sample of 1424 older individuals (45) and implicates reduced quality of life, diurnal somnolence, and falls during awakenings (46). Polypharmacy - the regular use of at least five drugs - also increased the chances of bad sleep quality in our sample, as was described in previous studies (47, 48). Conversely, a study conducted with elders living in care facilities in Malaysia found no statistical relationship between polypharmacy and sleep quality, although individuals with poor sleep used more drugs compared to those with good sleep (49). In the last few decades, polypharmacy has been on the rise among the geriatric population, with current estimates varying from 26,3 to 39,8% across European countries and Israel (50). The risk of potential drug-drug interactions increases dramatically with the number of drugs used, as do drug-disease interactions, resulting in unfavorable outcomes including falls, hospitalization, a decline in physical function, frailty, more sleep problems, and mortality (51).
Nonetheless, it is hard to disentangle the side effects of multiple drugs from the underlying comorbidities for which the drugs were prescribed, including in the context of sleep (15). This was particularly relevant in our sample, as people with chronic conditions like arthritis and glucose intolerance also exhibited greater chances of disturbed sleep. Much is known regarding the somewhat reciprocal association between sleep disturbance and chronic pain, in which psychological factors play an essential role (52). Osteoarthritis-related pain has also been previously associated with decreased sleep quality (53). Disturbed sleep has been recognized as a risk factor for metabolic and cardiovascular diseases (54); vice versa, sleep duration and quality directly impact glycemic control (55).
Surprisingly though, patients with subjective cognitive complaints had twice higher chances of poor sleep; however, given the transversal nature of our preliminary analysis, it is possible that the natural direction of this relationship might be inverse. Links between sleep and cognitive decline have been increasingly debated in the last few years (56, 57) and seem to be bidirectional (56). Sleep disturbances might be implicated in higher risks of subjective cognitive decline (57, 58), mild cognitive impairment (MCI), and Alzheimer’s disease (AD) (59, 60). On the other hand, sleep disturbances frequently co-occur in neurodegenerative disorders from the earliest through late stages, as seen, for instance, in AD, in which patients may present sleep fragmentation, shorter duration and changes in architecture, diurnal somnolence and sleep-wake cycle inversion (61). In some neurodegenerative conditions, such derangements start in preclinical stages, as observed in REM sleep behavior disorder and synucleinopathies (62).
An important strength of this study resides in the older age target. In times of social restriction measures, we could conduct personal interviews with a significant number of senior volunteers and follow up with them using validated assessment scales to evaluate sleep quality and psychiatric morbidity. Soon, the longitudinal nature of our data will help to add crucial information about the long-term effects of SARS-CoV-2 infection on the sleep quality of older people. Having healthy controls with no previous COVID-19 infection (as verified through serological exams) is another strength of our work, as well as recruiting volunteers and collecting data before COVID vaccination. Finally, researchers were blind to the previous exposure of participants to SARS-CoV-2, which helped to reduce bias. However, we recognize some limitations of this research. First, since it covers people aged 60 and over, the results may not be generalizable to younger populations. Second, participants’ high educational level and income possibly reflected their more significant interest in research volunteering and may represent a selection bias. In this perspective, education might have acted as a protective factor toward better sleep quality, as discussed above. Third, participants, not medical records, informed clinical data concerning comorbidities, medications, and COVID infection. Fourth, regarding psychiatric morbidity, data was either extracted from participants’ self-report on their comorbidities or through validated questionnaires (GDS-15 and GAI). It is possible that under the high prevalence of psychoactive compounds in our sample, current depressive and anxious symptoms were somewhat controlled, and the screening questionnaires were less effective than the self-report of pre-existing depression and anxiety. Finally, although PSQI is a validated and widespread instrument to assess sleep quality, participants were not submitted to polysomnography to investigate detailed sleep parameters.
Psychosocial burden in the context of the COVID-19 pandemic and pre-existing illness seems to have influenced the sleep quality of older adults more than the Gamma variant of SARS-CoV-2 infection per se. It is crucial to stress the multifactorial interference of diseases and medications in the sleep of older adults. Healthcare providers should be aware of potential drug-drug and drug-disease interactions and specific drugs affecting sleep. Our longitudinal data will help clarify further aspects concerning the trajectory of SARS-CoV-2 infection recovery, covering sleep quality.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Comitê de Ética em Pesquisa (Campus Central) UFRN. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
VP: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing. LF: Data curation, Investigation, Resources, Writing – original draft. TB: Data curation, Investigation, Resources, Writing – original draft. RS: Data curation, Investigation, Resources, Writing – original draft. AD: Data curation, Investigation, Resources, Writing – original draft. KA: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision, Visualization, Writing – review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This study was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
We thank Professor Selma Jerônimo and the Institute of Tropical Medicine of UFRN for helping conduct this study. We thank Marina Bruxel dos Santos for helping with data curation.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. World Health Organization. Statement on the fifteenth meeting of the IHR (2005) Emergency Committee on the COVID-19 pandemic. World Health Organization, Geneve, Switzerland: WHO Press (2023).
2. Plagg B, Engl A, Piccoliori G, Eisendle K. Prolonged social isolation of the elderly during COVID-19: Between benefit and damage. Arch gerontology geriatrics (2020) 89:104086. doi: 10.1016/j.archger.2020.104086
3. Sepúlveda-Loyola W, Rodríguez-Sánchez I, Pérez-Rodríguez P, Ganz F, Torralba R, Oliveira DV, et al. Impact of social isolation due to COVID-19 on health in older people: mental and physical effects and recommendations. J nutrition Health Aging (2020) 24(9):938–47. doi: 10.1007/s12603-020-1500-7
4. Lebrasseur A, Fortin-Bedard N, Lettre J, Raymond E, Bussieres EL, Lapierre N, et al. Impact of the COVID-19 pandemic on older adults: rapid review. JMIR Aging (2021) 4(2):e26474. doi: 10.2196/26474
5. Varma P, Junge M, Meaklim H, Jackson ML. Younger people are more vulnerable to stress, anxiety and depression during COVID-19 pandemic: A global cross-sectional survey. Prog Neuropsychopharmacol Biol Psychiatry (2021) 109:110236. doi: 10.1016/j.pnpbp.2020.110236
6. Rossi R, Jannini TB, Socci V, Pacitti F, Lorenzo GD. Stressful life events and resilience during the COVID-19 lockdown measures in Italy: association with mental health outcomes and age. Front Psychiatry (2021) 12:635832. doi: 10.3389/fpsyt.2021.635832
7. Assefa SZ, Diaz-Abad M, Wickwire EM, Scharf SM. The functions of sleep. AIMS Neurosci (2015) 2(3):155–71. doi: 10.3934/Neuroscience.2015.3.155
8. Scullin MK, Bliwise DL. Sleep, cognition, and normal aging: integrating a half century of multidisciplinary research. Perspect psychol Sci (2015) 10(1):97–137. doi: 10.1177/1745691614556680
9. Li J MV, Vitiello, Gooneratne NS. Sleep in normal aging. Sleep Med Clin (2018) 13(1):1–11. doi: 10.1016/j.jsmc.2017.09.001
10. De Mello MT, Silva A, de Carvalho Guerreiro R, Da-Silva FR, Esteves AM, Poyares D, et al. Sleep and COVID-19: considerations about immunity, pathophysiology, and treatment. Sleep Sci (2020) 13(3):199. doi: 10.5935/1984-0063.20200062
11. Wang D, Li W, Cui X, Meng Y, Zhou M, Xiao L, et al. Sleep duration and risk of coronary heart disease: a systematic review and meta-analysis of prospective cohort studies. Int J Cardiol (2016) 219:231–9. doi: 10.1016/j.ijcard.2016.06.027
12. He M, Deng X, Zhu Y, Huan L, Niu W. The relationship between sleep duration and all-cause mortality in the older people: an updated and dose-response meta-analysis. BMC Public Health (2020) 20:1–18. doi: 10.1186/s12889-020-09275-3
13. St-Onge MP, Grandner MA, Brown D, Conroy MB, Jean-Louis G, Coons M, et al. Sleep duration and quality: impact on lifestyle behaviors and cardiometabolic health: a scientific statement from the American Heart Association. Circulation (2016) 134(18):e367–86. doi: 10.1161/CIR.0000000000000444
14. Lloyd-Jones DM, Allen NB, Anderson CA, Black T, Brewer LC, Foraker RE, et al. Life’s essential 8: updating and enhancing the American Heart Association’s construct of cardiovascular health: a presidential advisory from the American Heart Association. Circulation (2022) 146(5):e18–43. doi: 10.1161/CIR.0000000000001078
15. Miner B, Kryger MH. Sleep in the aging population. Sleep Med Clin (2020) 15(2):311–8. doi: 10.1016/j.jsmc.2020.02.016
16. Suzuki K, Miyamoto M, Hirata K. Sleep disorders in the elderly: Diagnosis and management. J Gen Fam Med (2017) 18(2):61–71. doi: 10.1002/jgf2.27
18. Pires GN, Ishikura IA, Xavier SD, Petrella C, Piovezan RD, Xerfan EMS, et al. Sleep in older adults and its possible relations with COVID-19. Front Aging Neurosci (2021) 13:647875. doi: 10.3389/fnagi.2021.647875
19. Alimoradi Z, Brostrom A, Tsang HWH, Griffiths MD, Haghayegh S, Ohayon MM, et al. Sleep problems during COVID-19 pandemic and its’ association to psychological distress: A systematic review and meta-analysis. EClinicalMedicine (2021) 36:100916. doi: 10.1016/j.eclinm.2021.100916
20. Semyachkina-Glushkovskaya O, Mamedova A, Vinnik V, Klimova M, Saranceva E, Ageev V, et al. Brain mechanisms of COVID-19-sleep disorders. Int J Mol Sci (2021) 22(13):6917. doi: 10.3390/ijms22136917
21. AlRasheed MM, Alkadir AM, Bin Shuqiran KI, Al-Aqeel S, Jahrami HA, BaHammam AS. The impact of quarantine on sleep quality and psychological distress during the COVID-19 pandemic. Nat Sci Sleep (2021) 13:1037–48. doi: 10.2147/NSS.S313373
22. de Almondes KM, Castro E de AS, Paiva T. Sleep habits, quality of life and psychosocial aspects in the older age: before and during COVID-19. Front Neurosci (2022) 16. doi: 10.3389/fnins.2022.694894
23. Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV. Sleep problems during the COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med (2021) 17(2):299–313. doi: 10.5664/jcsm.8930
24. Chen C, Haupert SR, Zimmermann L, Shi X, Fritsche LG, Mukherjee B. Global prevalence of post COVID-19 condition or long COVID: A meta-analysis and systematic review. J Infect Dis (2022) 226(9):1593–607. doi: 10.1093/infdis/jiac136
25. Huang L, Li X, Gu X, Zhang H, Ren L, Guo L, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respir Med (2022) 10(9):863–76. doi: 10.1016/S2213-2600(22)00126-6
26. Zhang D, Chung VCH, Chan DCC, Xu Z, Zhou W, Tam KW, et al. Determinants of post-COVID-19 symptoms among adults aged 55 or above with chronic conditions in primary care: data from a prospective cohort in Hong Kong. Front Public Health (2023) 11:1138147. doi: 10.3389/fpubh.2023.1138147
27. Sheikh JI, Yesavage JA. Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontologist: J Aging Ment Health (1986) 5(1-2):165–73. doi: 10.1016/0022-3956(82)90033-4
28. Pachana NA, Byrne GJ, Siddle H, Koloski N, Harley E, Arnold E. Development and validation of the geriatric anxiety inventory. Int psychogeriatrics (2007) 19(1):103–14. doi: 10.1017/S1041610206003504
29. Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res (1989) 28(2):193–213. doi: 10.1016/0165-1781(89)90047-4
30. Bertolazi AN, Fagondes SC, Hoff LS, Dartora EG, da Silva Miozzo IC, de Barba MEF, et al. Validation of the Brazilian Portuguese version of the Pittsburgh sleep quality index. Sleep Med (2011) 12(1):70–5. doi: 10.1016/j.sleep.2010.04.020
31. Huang C, Huang L, Wang Y, Li X, Ren L, Gu X, et al. 6-month consequences of COVID-19 in patients discharged from hospital: a cohort study. Lancet (2021) 397(10270):220–32. doi: 10.1016/S0140-6736(20)32656-8
32. Du M, Ma Y, Deng J, Liu M, Liu J. Comparison of long COVID-19 caused by different SARS-coV-2 strains: A systematic review and meta-analysis. Int J Environ Res Public Health (2022) 19(23):16010. doi: 10.3390/ijerph192316010
33. de Almondes KM, Castro E, Paiva T. Morbidities worsening index to sleep in the older adults during COVID-19: Potential moderators. Front Psychol (2022) 3686. doi: 10.3389/fpsyg.2022.913644
34. Bajaj S, Blair KS, Schwartz A, Dobbertin M, Blair RJR. Worry and insomnia as risk factors for depression during initial stages of COVID-19 pandemic in India. PloS One (2020) 15(12):e0243527. doi: 10.1371/journal.pone.0243527
35. Sylvester SV, Rusu R, Chan B, Bellows M, O’Keefe C, Nicholson S. Sex differences in sequelae from COVID-19 infection and in long COVID syndrome: a review. Curr Med Res Opin (2022) 38(8):1391–9. doi: 10.1080/03007995.2022.2081454
36. Pelà G, Goldoni M, Solinas E, Cavalli C, Tagliaferri S, Ranzieri S, et al. Sex-related differences in long-COVID-19 syndrome. J Women’s Health (2022) 31(5):620–30. doi: 10.1089/jwh.2021.0411
37. Massion SP, Howa AC, Zhu Y, Kim A, Halasa N, Chappell J, et al. Sex differences in COVID-19 symptom severity and trajectories among ambulatory adults. Influenza Other Respir Viruses (2023) 17(12):e13235. doi: 10.1111/irv.13235
38. Ballering AV, Bonvanie IJ, Hartman TCO, Monden R, Rosmalen JG. Gender and sex independently associate with common somatic symptoms and lifetime prevalence of chronic disease. Soc Sci Med (2020) 253:112968. doi: 10.1016/j.socscimed.2020.112968
39. Vogel B, Acevedo M, Appelman Y, Merz CNB, Chieffo A, Figtree GA, et al. The Lancet women and cardiovascular disease Commission: reducing the global burden by 2030. Lancet (2021) 397(10292):2385–438. doi: 10.1016/S0140-6736(21)00684-X
40. Mallampalli MP, Carter CL. Exploring sex and gender differences in sleep health: a Society for Women’s Health Research Report. J women’s Health (2014) 23(7):553–62. doi: 10.1089/jwh.2014.4816
41. Freeman D, Sheaves B, Waite F, Harvey AG, Harrison PJ. Sleep disturbance and psychiatric disorders. Lancet Psychiatry (2020) 7(7):628–37. doi: 10.1016/S2215-0366(20)30136-X
42. de Sousa GM, Tavares VD de O, de Meiroz Grilo MLP, Coelho MLG, de Lima-Araújo GL, Schuch FB, et al. Mental health in COVID-19 pandemic: a meta-review of prevalence meta-analyses. Front Psychol (2021) 12:703838. doi: 10.3389/fpsyg.2021.703838
43. Yu J, Rawtaer I, Fam J, Jiang M, Feng L, Kua EH, et al. Sleep correlates of depression and anxiety in an elderly A sian population. Psychogeriatrics (2016) 16(3):191–5. doi: 10.1111/psyg.12138
44. Barczi SR, Teodorescu MC. Psychiatric and medical comorbidities and effects of medications in older adults. In: Principles and practice of sleep medicine. (2017) Elsevier, Philadelphia, PA. p. 1484–95.
45. Bliwise DL, Foley DJ, Vitiello MV, Ansari FP, Ancoli-Israel S, Walsh JK. Nocturia and disturbed sleep in the elderly. Sleep Med (2009) 10(5):540–8. doi: 10.1016/j.sleep.2008.04.002
46. Akhavizadegan H, Locke JA, Stothers L, Kavanagh A. A comprehensive review of adult enuresis. Can Urological Assoc J (2019) 13(8):282. doi: 10.5489/cuaj.5485
47. Argyropoulos K, Damka P, Argyropoulou A. Is polypharmacy risk factor for insomnia later in life? A cross-sectional study in Greece. EC Psychol Psychiatry (2020) 9:01–5.
48. Küçükdağlı P. Polypharmacy and related factors in geriatric outpatients. Eur J Geriatrics Gerentology (2019) 1(2):56–60. doi: 10.4274/ejgg.galenos.2019.144
49. Kumar S, Wong PS, Hasan SS, Kairuz T. The relationship between sleep quality, inappropriate medication use and frailty among older adults in aged care homes in Malaysia. PloS One (2019) 14(10):e0224122. doi: 10.1371/journal.pone.0224122
50. Midão L, Giardini A, Menditto E, Kardas P, Costa E. Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch gerontology geriatrics (2018) 78:213–20. doi: 10.1016/j.archger.2018.06.018
51. Wastesson JW, Morin L, Tan ECK, Johnell K. An update on the clinical consequences of polypharmacy in older adults: a narrative review. Expert Opin Drug Saf (2018) 17(12):1185–96. doi: 10.1080/14740338.2018.1546841
52. Keilani M, Crevenna R, Dorner TE. Sleep quality in subjects suffering from chronic pain. Wien Klin Wochenschr (2018) 130(1–2):31–6. doi: 10.1007/s00508-017-1256-1
53. Martinez R, Reddy N, Mulligan EP, Hynan LS, Wells J. Sleep quality and nocturnal pain in patients with hip osteoarthritis. Med (Baltimore) (2019) 98(41):e17464. doi: 10.1097/MD.0000000000017464
54. Cappuccio FP, Miller MA. Sleep and cardio-metabolic disease. Curr Cardiol Rep (2017) 19(11):110. doi: 10.1007/s11886-017-0916-0
55. Lee SWH, Ng KY, Chin WK. The impact of sleep amount and sleep quality on glycemic control in type 2 diabetes: A systematic review and meta-analysis. Sleep Med Rev (2017) 31:91–101. doi: 10.1016/j.smrv.2016.02.001
56. Abbott SM, Videnovic A. Chronic sleep disturbance and neural injury: links to neurodegenerative disease. Nat Sci sleep (2016) 8:55. doi: 10.2147/NSS.S78947
57. Kim JH, Ahn JH, Min CY, Yoo DM, Choi HG. Association between sleep quality and subjective cognitive decline: evidence from a community health survey. Sleep Med (2021) 83:123–31. doi: 10.1016/j.sleep.2021.04.031
58. Gamaldo AA, Wright RS, Aiken-Morgan AT, Allaire JC, Thorpe RJ Jr., Whitfield KE. The association between subjective memory complaints and sleep within older African American adults. Journals Gerontology: Ser B (2019) 74(2):202–11. doi: 10.1093/geronb/gbx069
59. Borges CR, Poyares D, Piovezan R, Nitrini R, Brucki S. Alzheimer’s disease and sleep disturbances: a review. Arquivos neuro-psiquiatria (2019) 77:815–24. doi: 10.1590/0004-282x20190149
60. Bubu OM, Andrade AG, Umasabor-Bubu OQ, Hogan MM, Turner AD, de Leon MJ, et al. Obstructive sleep apnea, cognition and Alzheimer’s disease: a systematic review integrating three decades of multidisciplinary research. Sleep Med Rev (2020) 50:101250. doi: 10.1016/j.smrv.2019.101250
61. Peter-Derex L, Yammine P, Bastuji H, Croisile B. Sleep and Alzheimer’s disease. Sleep Med Rev (2015) 19:29–38. doi: 10.1016/j.smrv.2014.03.007
Keywords: sleep quality, older adults, COVID-19, SARS-CoV-2, long-term, post-COVID syndrome
Citation: Peixoto VGMNP, Facci LA, Barbalho TCS, Souza RN, Duarte AM and Almondes KM (2024) The context of COVID-19 affected the long-term sleep quality of older adults more than SARS-CoV-2 infection. Front. Psychiatry 15:1305945. doi: 10.3389/fpsyt.2024.1305945
Received: 02 October 2023; Accepted: 18 January 2024;
Published: 05 February 2024.
Edited by:
Serena Sabatini, University of Nottingham, United KingdomReviewed by:
Camilla Sculco, University of Italian Switzerland, SwitzerlandCopyright © 2024 Peixoto, Facci, Barbalho, Souza, Duarte and Almondes. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vanessa Giffoni M. N. P. Peixoto, dmFuZXNzYS5naWZmb25pQHVmcm4uYnI=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.