- 1College of Physical Education and Health, Guangxi Normal University, Guilin, China
- 2College of Physical Education, China Three Gorges University, Yichang, China
- 3College of Physical Education and Health, Guilin University, Guilin, China
Background: Limited research directly compares the clinical effects of different types of mind-body exercises on anxiety and depression in older adults. Therefore, we conducted a systematic review and network meta-analysis of randomized controlled trials that meet the inclusion criteria to explore the intervention effects of five different types of mind-body exercises in improving anxiety and depression in older adults.
Methods: We followed the PRISMA-NMA guidelines and conducted searches in the Web of Science, PubMed, the Cochrane Library, and Embase databases up to July 28, 2023. The language was limited to English. Two independent reviewers conducted literature screening and data extraction. Review Manager 5.4 was used to perform Pairwise meta-analysis and risk assessment, while STATA version 15 software was used for network meta-analysis.
Result: A total of 42 studies, involving 2974 participants, were included. The results of the traditional meta-analysis showed that mind-body exercises were superior to the control group in alleviating anxiety (SMD: -0.87, 95% CI: -1.43, -0.31, p<0.05, I2 = 95%) and depressive (SMD: -0.52, 95% CI: -0.71, -0.34, p<0.05, I2 = 80%). In the network meta-analysis, the ranking of treatment effects for anxiety showed that Tai Chi > Qigong > Yoga > Dance > control group, while for depression, the ranking showed Tai Chi > Pilates > Yoga > Qigong > Dance > control group.
Conclusion: This study found that mind-body exercises have positive effects on improving anxiety and depression in older adults. Among the five different types of mind-body exercise interventions, Tai Chi was considered an effective approach for improving anxiety and depression. However, we encourage older adults to choose exercise modalities that suit their interests to enhance adherence.
Systematic review registration: http://www.crd.york.ac.uk/PROSPERO/, identifier CRD42023464296.
1 Introduction
Anxiety and depression have become one of the most common mental health problems globally, affecting approximately 340 million people (1). Research by Hay et al. indicates that between 2005 and 2015, the prevalence of anxiety increased by 14.9% and the prevalence of depression increased by 18.4% (2). The old adults are the main population affected by anxiety and depression, as they often face challenges such as social isolation and lack of family support, in addition to the threat of declining physical function and chronic health issues (3). Therefore, finding the best treatment measures for anxiety and depression in old adults has become an important scientific issue of global concern. Currently, the main treatment methods for anxiety and depression include medication therapy and cognitive behavioral therapy. However, both of these treatment measures have certain limitations. On one hand, the elderly may have weaker physical health and poor medication adherence, which restricts the use of medication therapy. On the other hand, cognitive behavioral therapy requires face-to-face communication between patients and therapists, which may cause fear, anxiety, and privacy concerns for patients, thereby negatively affecting the mental and physical health of the therapist (4). Additionally, the high cost of treatment also increases the economic burden on patients. Therefore, the current treatment methods for anxiety and depression still need further improvement.
An increasing number of research and commentary reports indicate that mind-body exercise plays a positive role in alleviating anxiety and depression symptoms in older adults. “Mind-body exercise” is a fitness activity that integrates physical and psychological elements. It emphasizes the coordination of body movements and mental processes, aiming to promote physical health while also contributing to mental well-being (5, 6). This exercise typically includes various forms such as yoga, tai chi, Pilates, qigong, and dance. As a complementary and alternative therapy, mind-body exercise is prevalent among older adults due to its ease of learning and low requirements for equipment and space (7–9). For example, yoga has been proven to reduce anxiety and depression levels in older adults, while tai chi exercise also improves their psychological health (10, 11). In addition, relevant meta-analysis results have shown significant therapeutic effects of tai chi in improving anxiety and depression in older adults (12–14). However, there is a wide range of mind-body exercise forms, including differences in exercise frequency, duration, and target population, making it unclear which therapy is more suitable for older adults. Moreover, most randomized controlled trials (RCTs) and traditional meta-analysis methods usually only compare treatment effects between two interventions, without providing a comprehensive comparison of different types of mind-body exercise interventions. The use of traditional pairwise comparison methods has some major limitations.
Therefore, this study chose to use the network meta-analysis (NMA) method to comprehensively compare multiple different intervention measures. Through NMA, we can use the indirect comparison method to quantitatively evaluate the therapeutic effects of different intervention measures in similar situations, thus providing a basis for selecting the best treatment plan. At the same time, we will rank various intervention measures. This study aims to evaluate the impact of different types of mind-body exercise on anxiety and depression symptoms in old adults through network meta-analysis, to provide the best treatment plan for clinical doctors in choosing non-pharmacological treatment options.
2 Materials and methods
As this is a systematic review, ethical approval is not required. We have registered this study and network meta-analysis on the International Prospective Register of Systematic Reviews (PROSPERO) with registration number CRD42023464296, and have strictly adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Network Meta-Analysis (PRISMA-NMA) statement for reporting (15).
2.1 Data sources and search strategy
We conducted a systematic search across four databases, including PubMed, Web of Science, Cochrane Controlled Trials Register, and Embase. During the search process, we employed a combination of medical subject headings and free-text terms, encompassing topics such as mind-body exercise, Tai Chi, Qigong, Wu Qin Xi, Ba Duan Jin, Yi Jing Jin, Liu Zi Jue, Yoga, Pilates, Dance for older adults, anxiety, depression, and randomized controlled trials. The search was limited to English language publications and covered the period from the inception of the databases until July 28, 2023. Additionally, we conducted a reference search of the included articles to identify studies that met our predefined criteria. The detailed search strategy is provided in the Appendix.
2.2 Selection and exclusion criteria
Inclusion criteria: The inclusion criteria for this study are as follows: (a) The baseline characteristics of the study population included old adults aged ≥60 years, regardless of gender, duration of illness, or source of cases. Additionally, participants should not have any diseases that could impact mind-body exercise. (b) The experimental group receives various types of mind-body exercises, including Tai Chi, Qigong (such as Ba Duan Jin, Yi Jin Jing, Liu Zi Jue, and Wu Qin Xi), yoga, Pilates, and dance. The control group, on the other hand, receives a waiting list, standard care, health education, or treatment methods different from the aforementioned interventions. (c) In the included scales, only select a scale that can measure either anxiety or depression as one of the outcome indicators. However, the selected scale must present baseline values and endpoint values, or the difference between the two. If multiple scales are used to test the same indicator in a study, we will choose the results obtained from the scale that is more suitable for the study population (old adults). These scales are specifically designed to assess symptoms in old adults, have high reliability and validity, and are widely used in older adults. To reduce the differences between different scales, standardized mean differences (SMD) should be used for representation. Most anxiety measurements use self-reported anxiety scales, the Hamilton Anxiety Rating Scale, or other valid specific scales. Depression, on the other hand, is measured using self-assessment scales such as the Beck Depression Inventory, Geriatric Depression Scale, Hamilton Depression Rating Scale, or other scales considered specific. Of course, some scales assess both indicators simultaneously, such as the Hospital Anxiety and Depression Scale (HADS). (d) All studies must be randomized controlled trials.
Exclusion criteria: The following criteria will be used to exclude studies: (1) duplicate publications, case reports, clinical guidelines, review articles, and non-randomized controlled trials; (2) interventions with unclear or mixed interventions combining Tai Chi with other exercises; (3) studies without analyzable data, such as studies that do not report values (i.e., mean, standard deviation, and sample size) necessary for calculating effect sizes; (4) participants with unclear age descriptions or <60 years old.
2.3 Data extraction and quality assessment
To eliminate duplicate search results, we utilized the EndNote X9 software. Subsequently, Subsequently, two reviewers independently assessed the titles and abstracts of the articles to determine their eligibility for inclusion in the study. For studies that did not meet the inclusion criteria, no further review was conducted. The remaining studies that were not excluded underwent a full-text evaluation by the two reviewers (YD and XK). Any disagreements or ambiguities were resolved through discussion with a third reviewer (JY). The data from randomized controlled trials (RCTs) were independently extracted by two reviewers according to a standardized form. The extracted information included the first author’s name, publication year, sample size, gender ratio, age, type of mind-body exercise intervention, control group intervention, intervention duration, frequency, cycle, primary outcome measures, and measurement tools. In case of unclear or incomplete information in the studies, the first author was contacted for clarification.
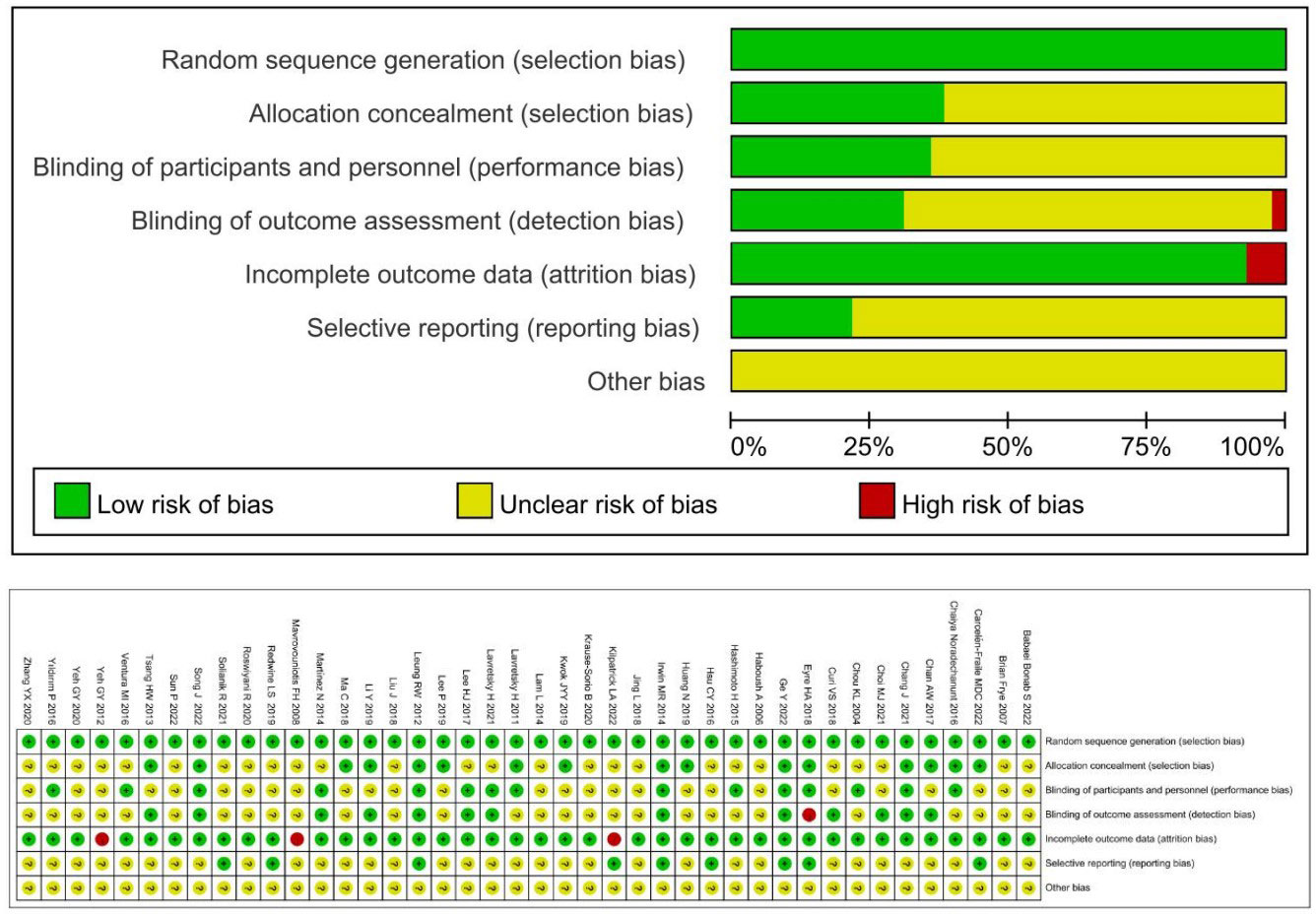
The two reviewers (DY and KX) assessed the quality of the included RCTs using the Cochrane risk of bias tool (16) in the following domains: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessors, (5) incomplete outcome data, (6) selective reporting, and (7) other biases. Each domain was evaluated as having a high risk of bias, an uncertain risk of bias, or a low risk of bias. Disagreements were resolved through discussion between the two reviewers, and if no consensus was reached, a third reviewer was consulted for final decision-making.
2.4 Data synthesis and analysis
During the data analysis process, statistical analysis was performed using Stata 15 software. To address the differences in anxiety and depression assessment scales used in different studies, standardized mean differences (SMD) were used as the measure of effect size for summarizing the results. Considering that SMD computed using Cohen’s d in small-scale studies may introduce slight bias and overestimate the effect size, our study utilized Hedges’ g as a summary measure to control for this bias (17). Network meta-analysis (NMA) was employed to explore the comparative relationships between different mind-body exercise interventions. For each outcome, SMDs, mean values, and 95% confidence intervals were calculated, with P<0.05 indicating statistical significance. Heterogeneity was assessed using statistical tests, where P>0.10 and I2<50% indicated low heterogeneity and a common-effect model was used; while P<0.10 and I2>50% indicated high heterogeneity and a random-effects model was used, simultaneously, we employ grouping analysis and meta-regression methods to explore the latent variables that lead to heterogeneity, while the REML method is used for testing heterogeneity (18). A network plot was created to visually depict the connections between different mind-body exercise interventions. The net-meta command in Stata 15 was used in conjunction with frequency analysis methods to perform the network meta-analysis. To assess potential inconsistency between direct and indirect evidence, a global consistency test was conducted, and node splitting was used to determine local consistency. If the analysis yielded a P>0.05, indicating no significant differences between direct and indirect comparisons, a consistency model was used to analyze the effect sizes of multiple treatment comparisons. Otherwise, an inconsistency model was employed. In cases where closed loops were present in the comparative studies, a test for inconsistency in the loops was conducted, with a 95% confidence interval (CI) containing 0 indicating that no significant loop inconsistency (19, 20).
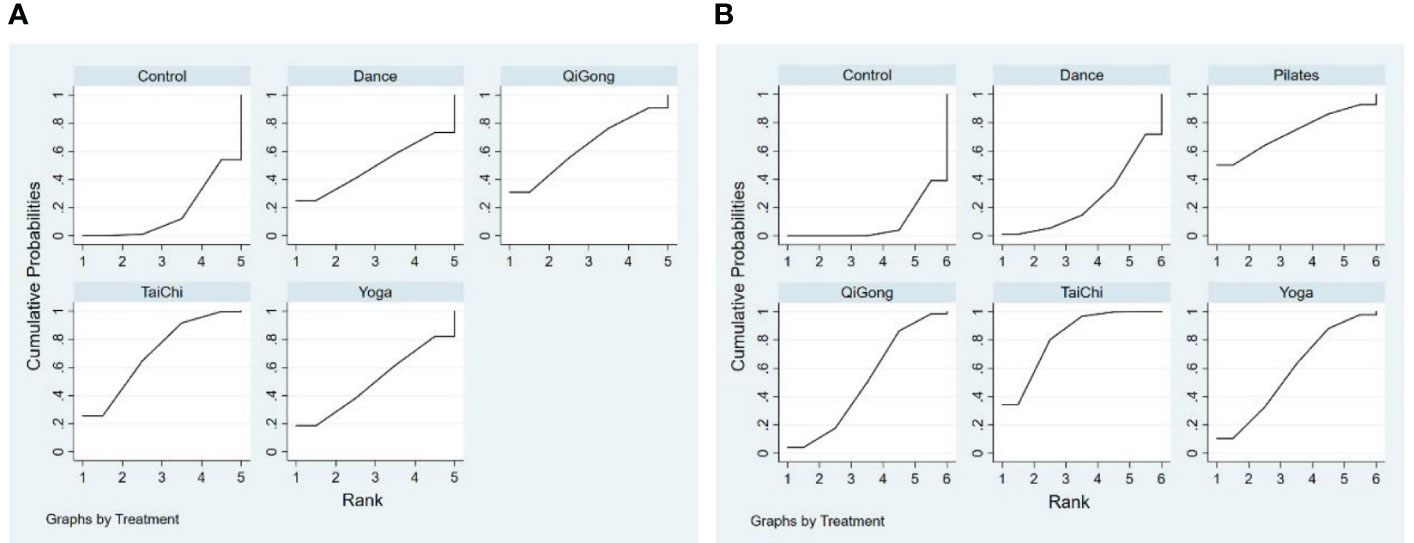
We utilize a joint analysis table to compare the results of different intervention measures based on network meta-analysis. Additionally, by examining the area under the cumulative probability curve, we can rank the interventions, with a higher SUCRA value indicating a more effective intervention (21). Furthermore, to assess publication bias, we employ a comparison-adjusted funnel plot to detect potential publication bias risks. If the effect sizes of the included studies exhibit a symmetrical distribution, it suggests minimal publication bias in the network meta-analysis (22, 23).
3 Results
3.1 Study inclusion and selection
Through systematic retrieval, we have collected a total of 42 randomized controlled trials (RCTs) from 4 databases, encompassing 2974 old adults, and provided a detailed description of the literature screening process. After excluding 325 duplicate articles, we conducted a preliminary review of titles and abstracts, excluding 681 irrelevant articles and 206 meta-analyses. Finally, 160 articles were included for full-text reading. After a comprehensive review, 108 articles were excluded, including 2 conference abstracts, 1 clinical guideline, 2 inappropriate intervention measures, 57 articles with unavailable data, 7 articles without full-text access, 8 review articles, and 41 articles with participants’ average age below 60 years. In the end, we included 42 published randomized controlled trials in this network meta-analysis to compare the effects of different types of mind-body exercise interventions with the control group on improving anxiety and depression in older adults.
3.2 The characteristics of studies
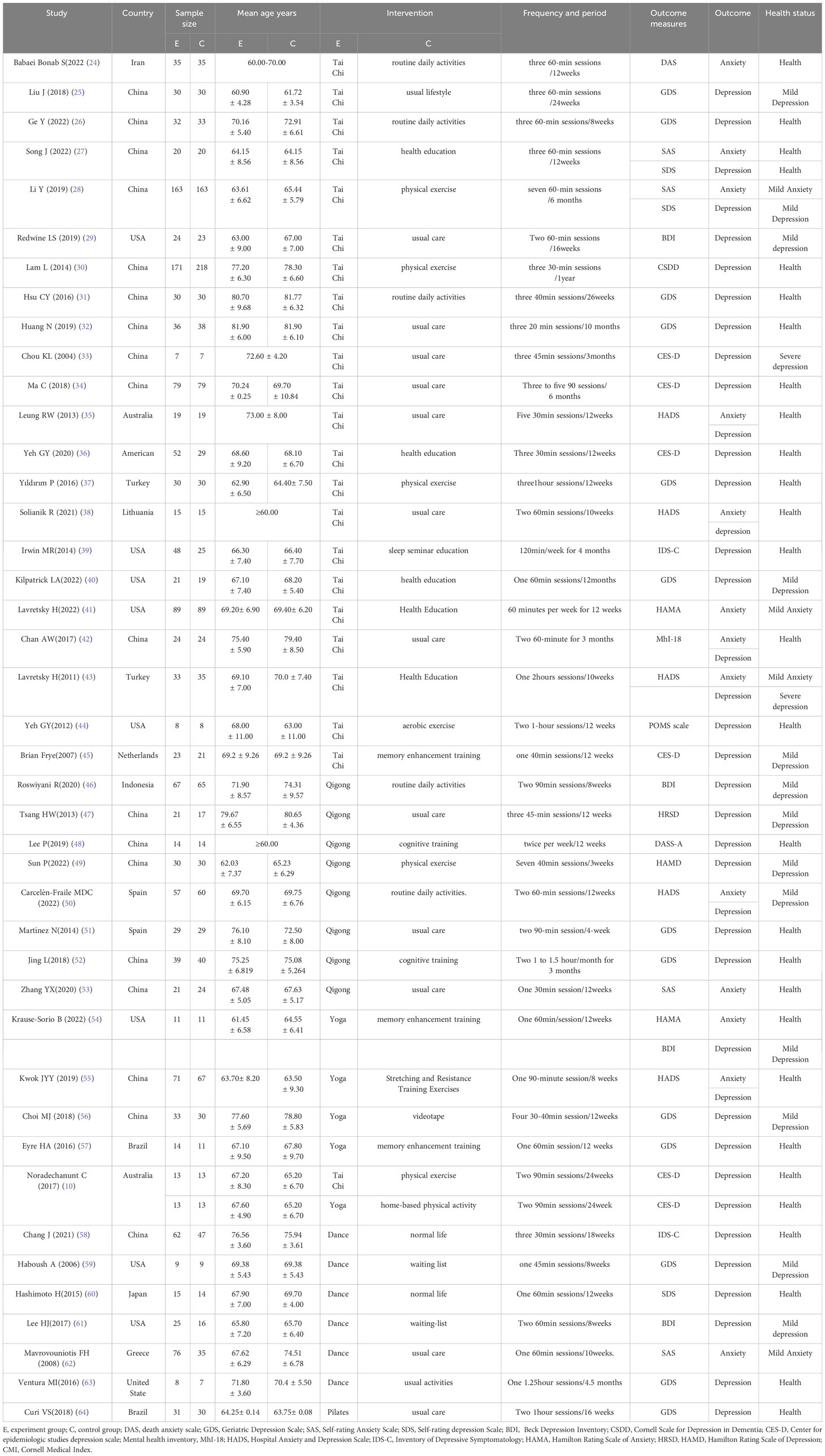
This study covers 42 studies, including a total of 2974 old adults. All participants were randomly assigned to the experimental group and control group according to a predetermined protocol. The experimental group included five different intervention modalities (Tai Chi, Qigong, Yoga, Dance, and Pilates), including 23 studies involving Tai Chi, 8 involving Qigong, 5 involving Yoga, 6 involving Dance, and 1 involving Pilates. The duration of each intervention ranged from 20 to 90 minutes, and the frequency ranged from once a week to seven times a week. The control group received interventions such as routine daily activities, health education, physical exercise, and routine care. These studies are mainly distributed in China and the United States, with the publication years mainly concentrated between 2016 and 2022. Anxiety was evaluated using the Death anxiety scale, Self-rating Anxiety Scale, Hospital Anxiety and Depression Scale, and Hamilton Rating Scale of Anxiety, while depression was assessed using the Geriatric Depression Scale, Self-rating depression Scale, The 21-item Beck Depression Inventory−1A, Cornell Scale for Depression in Dementia, Center for epidemiologic studies depression scale, Hospital Anxiety and Depression Scale, Inventory of Depressive Symptomatology, Hamilton Rating Scale of Depression, Hamilton Rating Scale of Depression, and Cornell Medical Index. Within these 42 randomized controlled trials, the process of selecting eligible studies is shown in Figure 1, and the characteristics of the selected studies for this network meta-analysis are summarized in Table 1.
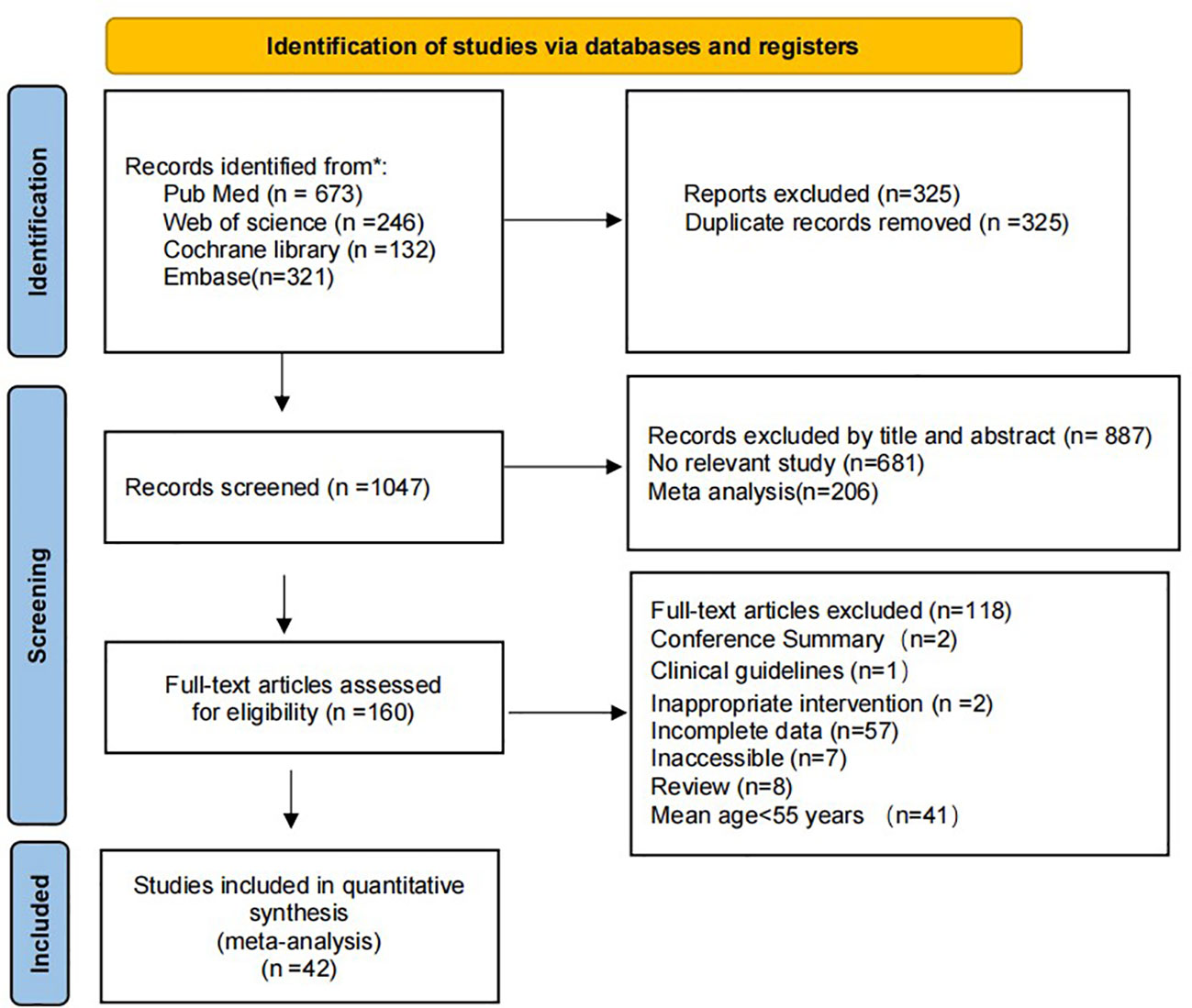
Figure 1 The process of slection of the eligible studies. * means reporting the number of records identified from each database or register searched (rather than the total number across all databases/registers).
3.3 Quality assessment
The quality assessment of the selected studies was conducted using the Cochrane risk of bias tool, and the assessment results are shown in Figure 2. 41 studies were two-arm studies, with one being a three-arm study, all involving descriptions of randomization. Among them, 27 studies described in detail the methods of generating random sequences, while only 8 studies mentioned specific allocation concealment methods. Due to the nature of physical exercise interventions, most experiments did not use blinding, with only a few experiments using a single-blinding design. The majority of experiments reported in detail the data missing during the experimental process, with 2 studies not specifying the specific reasons for participant loss during the experiment, thus being judged as high risk of bias. All studies did not report other biases.
3.4 Pairwise meta-analysis
Pairwise meta-analyses showed that the intervention group significantly reduced anxiety (SMD: -0.87, 95% CI: -1.43, -0.31, p<0.05) and depression (SMD: -0.52, 95% CI: -0.71, -0.34, p<0.05) scores compared to the control group. In addition, our findings also showed a high degree of heterogeneity in anxiety (I2 = 95%) and depression (I2 = 80%) after the meta-merger. For detailed results of the meta-analysis, please refer to the Appendix. To further explore the sources of heterogeneity, we conducted subgroup and meta-regression analyses based on moderating variables.
The moderating variables were categorized into 3 main areas. The first is the population characteristics moderating variable, which mainly includes the age and health status of the subjects. The second is the interventions, mainly including the experimental group interventions and control group interventions. The third is the evaluation scale. Subgroup analyses in this study showed that subgroup analyses based on moderator variables did not significantly reduce the heterogeneity of anxiety and depression outcome indicators. For anxiety indicators, in the subgroup with age >70 years, mind-body exercise had no significant effect. In the experimental group, different intervention methods also showed that qigong had no significant effect. As for the indicators of depression, the subgroup analysis of different intervention methods in the experimental group showed that dance had no significant effect, while in the control group, different intervention measures of physical exercise showed that mind-body exercise had no significant effect on depression. Among the different subgroups using different evaluation scales, BDI showed that mind-body exercise also had no significant effect on depression. Meta-regression analyses showed that differences in the evaluation scales were a significant contributor to heterogeneity in the anxiety outcome indicators (P=0.035), while the remaining moderator variables did not affect heterogeneity; please see Appendix Tables S2, S3 for detailed subgroup analyses, and Appendix Tables S4, S5 for meta-regression results.
3.5 Network meta-analysis
In the included 42 studies, a network diagram (Figure 3) was established between different forms of mind-body exercises in the intervention of anxiety and depression in older adults. The lines between the points in the diagram represent studies with direct comparisons, while points without lines indicate randomized controlled trials that have not been directly compared. The thicker the line between two points in the network diagram, the more studies have compared these two intervention measures. A consistency test was conducted for the anxiety and depression outcome indicators included in the studies. The results show that the PSRF parameter values are all greater than 0.05, close to 1.00, indicating good convergence of the model. Therefore, a network meta-analysis was conducted under the assumption of consistency.
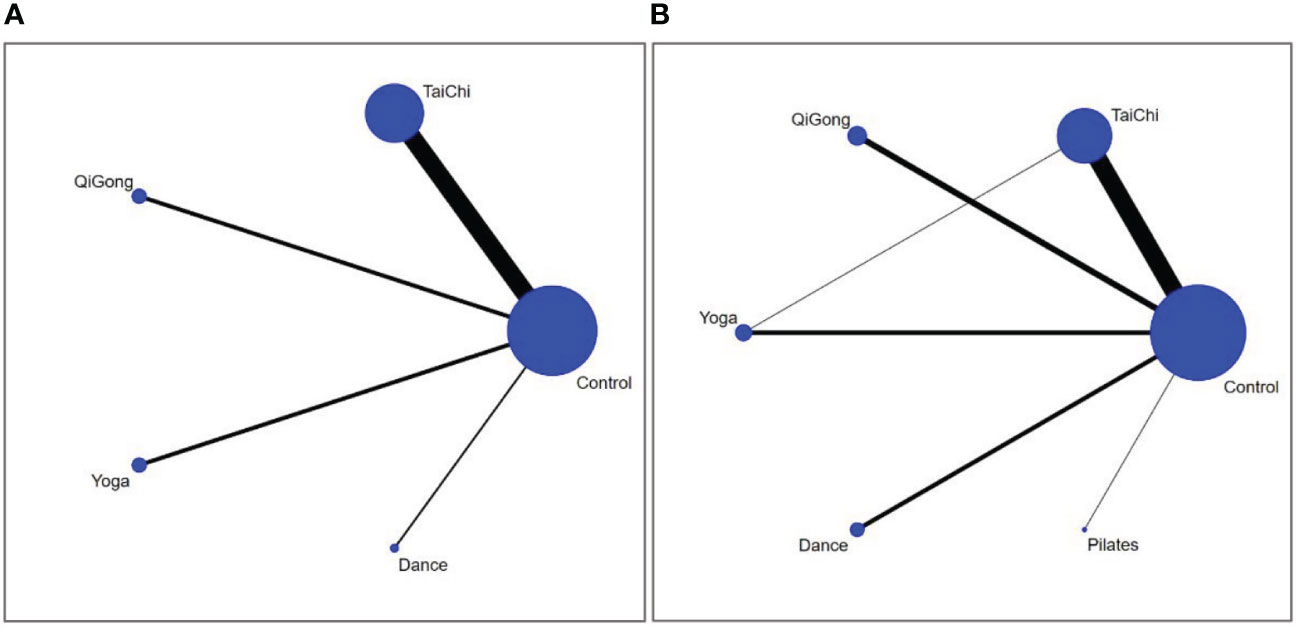
Figure 3 The network structure of the analysed treatment comparisons for the outcome of anxiety (A) and depression (B).
Network meta-analyses covered changes in anxiety for 4 different types of mind-body exercise interventions versus a control group (Figure 3A). Since there is no direct and indirect comparison in the network plot, we used the consistency model to compare different interventions. The specific results are shown in Figure 4A, compared with the control group, Tai Chi (SMD: -0.93, 95% CI: -1.66, -0.20), Qigong (SMD: -0.88, 95%CI: -2.42,0.67), Yoga (SMD: -0.57, 95%CI: -2.14, 0.99), Dance (SMD: -0.56,95% CI: -2.71, 1.60) all showed better effects. In the probability ranking table in Figure 5A, Tai Chi exercise is considered to be the most likely intervention for anxiety in older adults, with a probability of 70.4%, followed by Qigong (63.4%). Therefore, according to this ranking, the intervention effects of the four mind-body exercises on anxiety in older adults are as follows: Tai Chi > Qigong > Yoga > Dance > Control group.
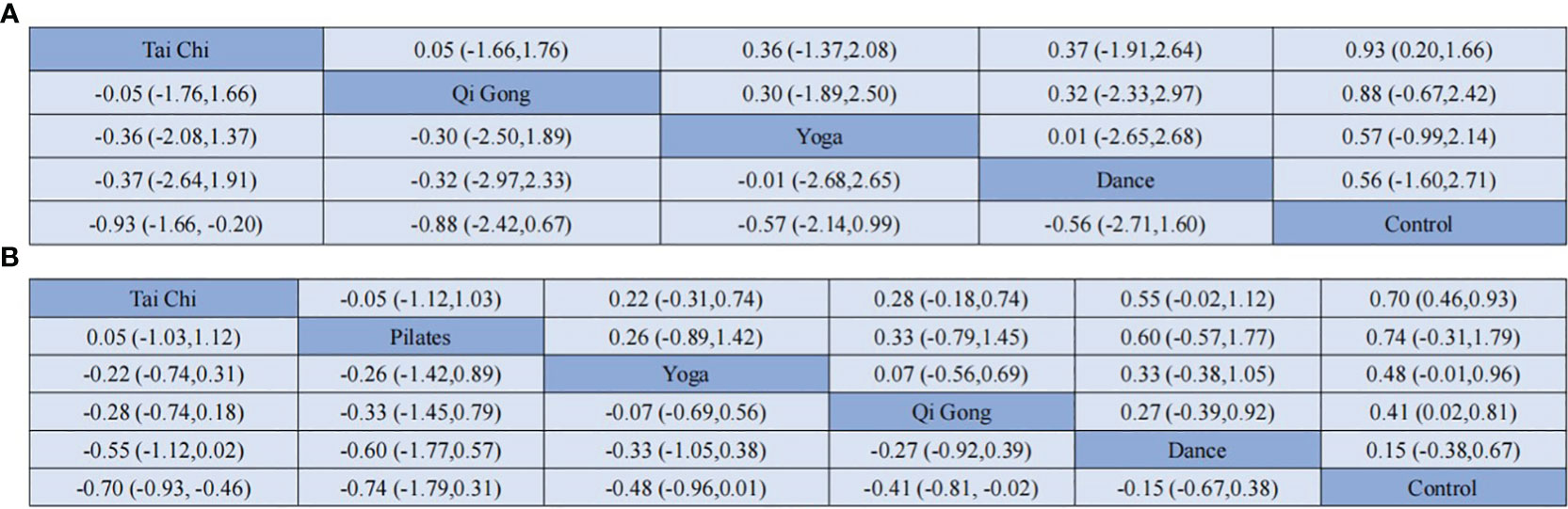
Figure 4 Results of the network meta-analysis (SMD vs 95% CI) of the effects different mind-body exercise on anxiety (A) and depression (B) in the adults.
The depression network diagram shown in Figure 3B), was compared between the 5 different mind-body exercise interventions and the control group. Considering the presence of both direct and indirect comparisons in the network diagram, we first performed an inconsistency test. The results showed good convergence. In addition, considering that a triangle loop was formed by a multi-arm trial in this study, the consistency of the I2 quadratic loop was tested if they were inconsistent. The 95% confidence interval (CI) of the closed loop was 0, indicating a significant inconsistency. Therefore, a consistency model was adopted to compare different interventions. The results in Figure 4B showed that in comparison with the control group, Tai Chi (SMD: -0.70, 95% CI: -0.93, -0.46), Pilates (SMD: -0.74, 95% CI: -1.79, 0.31), Yoga (SMD: -0.48, 95% CI: -0.96, -0.01), Qigong (SMD: -0.41, 95% CI: -0.81, -0.02), and Dance (SMD: -0.15, 95% CI: -0.67, 0.38) showed better efficacy. In the probability ranking table in Figure 5B, Tai Chi was considered to be the most likely best intervention for old adults with depression with a probability of 83.7%, followed by Pilates (73.9%). Therefore, according to this ranking, the intervention effects of the five mind-body exercises on depression in older adults are as follows: Tai Chi > Pilates > Yoga > Qigong > Dance > control group.
3.6 Publication bias
In the final inclusion of the 42 studies, 13 studies provided detailed descriptions of the intervention effects of different types of mind-body exercises on anxiety in older adults, while the other 38 studies reported intervention effects on depression. These studies all achieved a moderate to high level of quality assessment. In addition, we used anxiety and depression as outcome indicators and generated a funnel plot using STATA software version 15. The results showed that the funnel plot of depression (Figure 6B) presented a basic stacking pattern, indicating no apparent publication bias for the depression indicator. However, the funnel plot of anxiety (Figure 6A) exhibited some degree of asymmetry, which may be related to the relatively little literature on the included types of mind-body exercises and the relatively insufficient overall sample size. Therefore, there is a possibility of publication bias.
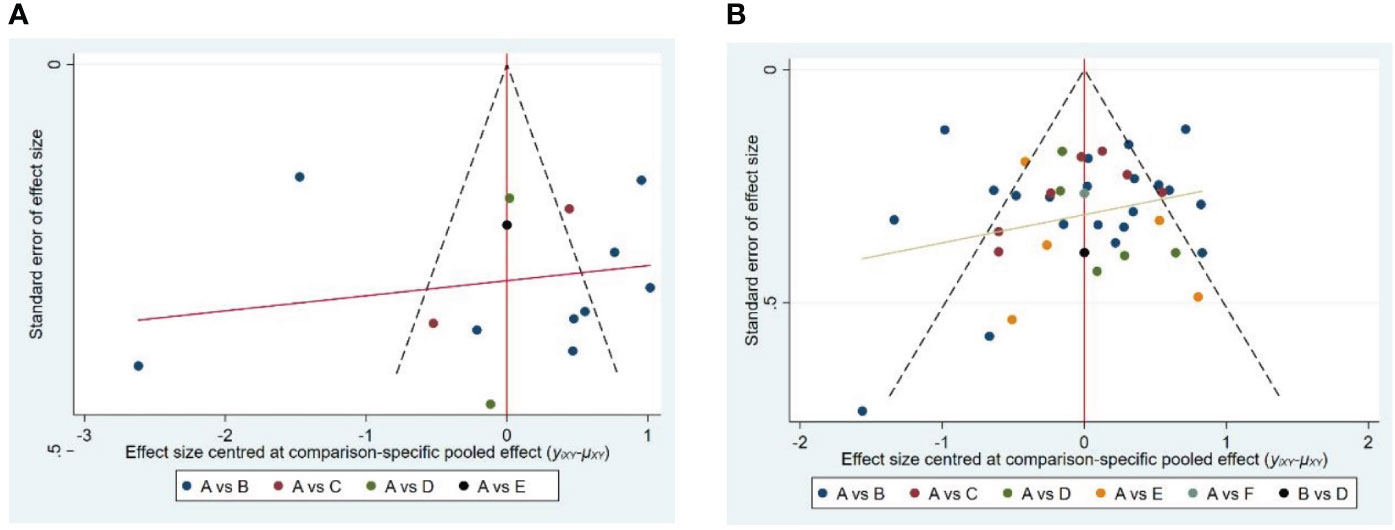
Figure 6 Publication bias of four tyles of mind-body exercise on anxiety (A) and depression (B). In the picture (A), A is control group, B is Tai Chi, C is Qigong, D is Yoga, and E is Dance. In picture (B), A is control group, B is Tai Chi, C is Qigong, D is Yoga, E is Dance, and F is Pilates.
3.7 Sensitivity analysis
By excluding individual studies, sensitivity analysis demonstrated that there was no significant change in the statistical significance of all primary or secondary outcomes. This further validates the robustness of the results and the heterogeneity of the study.
4 Discussion
Mental health issues are increasingly gaining attention in the old adult population, with anxiety and depression, although common, often going unnoticed. This study employed a network meta-analysis approach, incorporating 42 articles with a total of 2,000 participants. Among these articles, 13 focused on anxiety, while 38 addressed Depression. We systematically explored mind-body exercises, including Tai Chi, Qigong, yoga, Dance, and Pilates, among various physical exercise modalities, by conducting direct and indirect comparative analyses of their interventions on anxiety and depression in older adults. In Pairwise meta-analysis, it is evident that mind-body exercises have significant effects on anxiety (SMD: -0.84, 95% CI: -1.37, -0.31, p<0.05, I2 = 94%) and depression (SMD: -0.52, 95% CI: -0.71, -0.34, p<0.05, I2 = 80%) among older adults. In the network meta-analysis, Tai Chi ranked highest in terms of SUCRA values for anxiety, followed by Qigong, yoga, Dance, and the control group. Similarly, for depression, Tai Chi demonstrated the most favorable outcomes, followed by Pilates, yoga, Qigong, Dance, and the control group.
A mind-body exercise is a comprehensive form of health practice, including Tai Chi, Qigong, yoga, dance, and Pilates, among others. It can alleviate physical and mental tension, improve mental health, and establish a healthier lifestyle to reduce anxiety and depression. It can also stimulate the synthesis of tryptophan hydroxylase, thereby promoting the production of serotonin (65). In addition, mind-body exercise can activate the endocannabinoid system, alter the function of the hypothalamic-pituitary-adrenal axis, increase levels of norepinephrine, decrease the expression of glucocorticoid receptors, and promote the regeneration of hippocampal neurons (66, 67). Interestingly, this study demonstrates that physical and mental exercise has a significant intervention effect on anxiety and depression in older adults. However, traditional meta-analyses have shown high levels of statistical heterogeneity. By including population characteristics (age and health status) as well as the classification of the experimental and control groups, and using different scales as moderating variables, it was found that the use of different scales is the cause of heterogeneity in anxiety indicators. This difference may be due to the variations in the assessment of anxiety indicators by different measurement scales, including question settings and scoring criteria, which leads to heterogeneity in the results. However, we cannot rule out other potential influencing factors, such as cultural and racial differences among the included population, or other variables that have not been considered.
Tai Chi, a traditional Chinese fitness practice, is well-known for its unique exercise approach, characterized by slow, fluid movements, deep breathing, and elements of meditation (68). These distinctive features contribute to lowering stress levels, reducing tension, and enhancing relaxation in the body, thus positively affecting mental well-being (69). Our research findings reveal that Tai Chi ranks highly in SUCRA values for addressing anxiety and depression in older adults, indicating its effectiveness as one of the primary methods. This is attributed to Tai Chi’s capacity to heighten bodily awareness and relaxation, which aids in mitigating tension and anxiety, ultimately raising levels of psychological well-being. Tai Chi underscores meditation and the connection between body and mind, facilitating superior emotional management (70). During Tai Chi practice, the emphasis on fluid body postures enhances concentration and self-harmony, critical factors in alleviating anxiety and depression (71). The deep breathing exercises in Tai Chi play a vital role in managing anxiety by stabilizing the autonomic nervous system, transitioning the body from a state of stress to one of calm, and reducing tension and anxiety, thereby enabling individuals to respond to stressors with greater composure (24). Additionally, Tai Chi’s meditation components help individuals focus, enhance self-awareness, and reduce negative thinking. This meditation practice strengthens emotional regulation, enabling better coping with depressive emotions (72).
Our study also compared other forms of mind-body exercises, including Qigong, Yoga, and Dance, to explore their effects on anxiety and depression intervention. Despite falling within the category of mind-body exercises, these interventions exhibit differences in their methods and practices, potentially resulting in varying outcomes in alleviating anxiety and depression. Qigong emphasizes the regulation of breath and the balance of internal energy. Deep breathing and specific movements (73) have shown some effectiveness in addressing anxiety and depression in older adults. Research results indicate that Qigong practice can significantly reduce anxiety and depression levels in older adults (74). However, what is even more crucial is Qigong’s focus on cultivating emotional management and self-regulation. By enhancing emotional stability, older adults can more effectively cope with anxious emotions, thereby reducing their severity (74). This improvement in emotional management plays a pivotal role in the treatment of anxiety and depression in older adults.
Yoga focuses on the practice of asanas (physical postures) and breath control techniques, which can lead to various physiological and psychological effects, thereby influencing the outcomes of anxiety interventions (75). The meditation and body posture exercises in yoga improve emotional stability and psychological well-being in older adults (76). A study has shown that yoga practice can significantly improve depression in family caregivers (77). However, more importantly, yoga emphasizes cultivating emotional management and self-awareness. By enhancing emotional stability, older adults are better able to cope with anxiety and depressive emotions, thereby reducing their severity (78). Improving emotional management skills is crucial for the psychological well-being of older adults.
Although Pilates primarily focuses on physical training, it still incorporates elements of deep breathing and body awareness in its practice (79). Research findings suggest that Pilates ranks high in interventions for reducing depression in older adults, which may be attributed to its emphasis on the connection between the body and emotions, thus aiding in improving emotional management and alleviating depression (80). However, it is important to note that this study only included one research article on Pilates, thus potential biases exist. Further research is needed to gain a more comprehensive understanding of the mechanisms of Pilates and its relationship with emotional management.
In addition, two meta-analytic studies have shown that Dance interventions do not have a significant effect on anxiety and depression (81, 82), which is consistent with our research findings. Dance emphasizes the body’s dynamism and the sense of rhythm in music, which may make it challenging for many older adults to adapt to its specific rhythms and demands (83). Apart from differences in intervention methods, the quality and quantity of research may also influence the relative effectiveness of these mind-body exercises. For example, some studies may have a small sample size or inadequate control over individual differences, all of which can impact the reliability and generalizability of the research.
Furthermore, it is imperative to consider the individual differences and intervention preferences of older adults, as they can significantly impact the effectiveness of mind-body exercise. Each older adult possesses unique physical conditions, health needs, and varying levels of acceptance toward different types of exercise modalities. Consequently, a particular mind-body exercise may prove more efficacious for certain individuals, while being less suitable for others, thereby elucidating the observed variations in outcomes. For instance, some older adults may find it easier to embrace the slow and gentle movements of Tai Chi, while being more receptive to the breath-regulation techniques of Qigong, thereby manifesting superior outcomes in anxiety and depression interventions. Conversely, there may be individuals who lean towards the mind-body balance offered by yoga or the muscle conditioning provided by Pilates, consequently exhibiting enhanced results in terms of psychological well-being. These factors of individual differences and intervention preferences necessitate further exploration in future research endeavors, to formulate personalized and precise mental health intervention plans.
There are several limitations to our study. First, we observed significant heterogeneity in the traditional meta-analysis phase, and although we used subgroup analysis and meta-regression to explore the sources of heterogeneity, we were not able to pinpoint the sources of heterogeneity, and future research could validate the results of this study by expanding the study sample size and using experimental studies with different interventions as well as different evaluation scales. Second, only one Pilates study was included in this study, which may also introduce bias in the findings. It is recommended that future studies expand the search and increase the number of study interventions to further validate the results of this study.
5 Conclusion
The network meta-analysis results of this study show that mind-body exercises have significant positive effects on improving anxiety and depression in older adults. Among the five different types of mind-body exercises included in the research, Tai Chi and Qigong showed better improvement in reducing anxiety. For older patients who wish to improve depression, we recommend considering Tai Chi and Pilates as treatment options. However, to scientifically select suitable exercise programs, individual differences of patients need to be fully considered. Therefore, this study provides evidence and references for clinical doctors regarding non-pharmacological treatment options for improving anxiety and depression in older adults.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material. Further inquiries can be directed to the corresponding author.
Author contributions
YD: Writing – original draft, Validation, Software, Methodology, Data curation. JY: Writing – review & editing, Supervision, Formal analysis. XK: Writing – original draft, Validation, Software, Methodology, Data curation. RZ: Writing – review & editing, Methodology, Formal analysis. LC: Writing – original draft, Software, Methodology, Data curation. XZ: Writing – review & editing, Methodology, Supervision, Formal analysis.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1305295/full#supplementary-material
References
1. Bernabe E, Marcenes W, Hernandez CR, Bailey J, Abreu LG, Alipour V, et al. Global, regional, and national levels and trends in burden of oral conditions from 1990 to 2017: A systematic analysis for the global burden of disease 2017 study. J Dental Res (2020) 99(4):362–73. doi: 10.1177/0022034520908533
2. Hay SI, Jayaraman SP, Truelsen T, Sorensen RJD, Millear A, Giussani G, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015 (vol 388, pg 1545, 2016). Lancet (2017) 389(10064):E1–1.
3. Huang Y, Wang Y, Wang H. Prevalence of mental disorders in China: a cross-sectional epidemiological study (vol 6, pg 211, 2019). Lancet Psychiatry (2019) 6(4):E11–1. doi: 10.1016/s2215-0366(19)30074-4
4. Koufakis T, Grammatiki M, Kotsa K. Type 2 diabetes management in people aged over seventy-five years: targets and treatment strategies. Maturitas (2021) 143:118–26. doi: 10.1016/j.maturitas.2020.10.005
5. Zhang YJ, Loprinzi PD, Yang L, Liu J, Liu SJ, Zou LY. The beneficial effects of traditional chinese exercises for adults with low back pain: A meta-analysis of randomized controlled trials. Medicina-Lithuania (2019) 55(5):118. doi: 10.3390/medicina55050118
6. Zou LY, Zhang YJ, Yang L, Loprinzi PD, Yeung AS, Kong J, et al. Are mindful exercises safe and beneficial for treating chronic lower back pain? A systematic review and meta-analysis of randomized controlled trials. J Clin Med (2019) 8(5):628. doi: 10.3390/jcm8050628
7. Zhou SW, Zhang YJ, Kong ZW, Loprinzi PD, Hu Y, Ye JJ, et al. The effects of tai chi on markers of atherosclerosis, lower-limb physical function, and cognitive ability in adults aged over 60: A randomized controlled trial. Int J Environ Res Public Health (2019) 16(5):753. doi: 10.3390/ijerph16050753
8. Zou LY, Sasaki JE, Wei GX, Huang T, Yeung AS, Neto OB, et al. Effects of mind-body exercises (Tai chi/yoga) on heart rate variability parameters and perceived stress: A systematic review with meta-analysis of randomized controlled trials. J Clin Med (2018) 7(11):404. doi: 10.3390/jcm7110404
9. Liu SJ, Ren ZB, Wang L, Wei GX, Zou LY. Mind-body (Baduanjin) exercise prescription for chronic obstructive pulmonary disease: A systematic review with meta-analysis. Int J Environ Res Public Health (2018) 15(9):1830. doi: 10.3390/ijerph15091830
10. Noradechanunt C, Worsley A, Groeller H. Thai Yoga improves physical function and well-being in older adults: a randomised controlled trial [Journal article]. J Sci Med Sport (2017) 20(5):494–501. doi: 10.1016/j.jsams.2016.10.007
11. Chou KL, Lee PW, Yu EC, Macfarlane D, Cheng YH, Chan SS, et al. Effect of Tai Chi on depressive symptoms amongst Chinese older patients with depressive disorders: a randomized clinical trial [Journal article]. Int J Geriatric Psychiatry (2004) 19(11):1105–7. doi: 10.1002/gps.1178
12. Zou LY, Yeung A, Li CX, Wei GX, Chen KW, Kinser PA, et al. Effects of meditative movements on major depressive disorder: A systematic review and meta-analysis of randomized controlled trials. J Clin Med (2018) 7(8):95. doi: 10.3390/jcm7080195
13. Zou LY, Yeung A, Zeng N, Wang CY, Sun L, Thomas GA, et al. Effects of mind-body exercises for mood and functional capabilities in patients with stroke: an analytical review of randomized controlled trials. Int J Environ Res Public Health (2018) 15(4):721. doi: 10.3390/ijerph15040721
14. Zou LY, Yeung A, Quan XF, Hui SSC, Hu XY, Chan JSM, et al. Mindfulness-based baduanjin exercise for depression and anxiety in people with physical or mental illnesses: A systematic review and meta-analysis. Int J Environ Res Public Health (2018) 15(2):321. doi: 10.3390/ijerph15020321
15. Lai X, Wen H, Li Y, Lu LM, Tang CZ. The comparative efficacy of multiple interventions for mild cognitive impairment in alzheimer’s disease: A bayesian network meta-analysis. Front Aging Neurosci (2020) 12:121. doi: 10.3389/fnagi.2020.00121
16. Cumpston MS, McKenzie JE, Welch VA, Brennan SE. Strengthening systematic reviews in public health: guidance in the Cochrane Handbook for Systematic Reviews of Interventions, 2nd edition. J Public Health (2022) 44(4):E588–92. doi: 10.1093/pubmed/fdac036
17. Lin LF, Aloe AM. Evaluation of various estimators for standardized mean difference in meta-analysis. Stat Med (2021) 40(2):403–26. doi: 10.1002/sim.8781
18. Tanriver-Ayder E, Faes C, van de Casteele T, McCann SK, Macleod MR. Comparison of commonly used methods in random effects meta-analysis: application to preclinical data in drug discovery research. BMJ Open Sci 2021 (2021) 5(1):e100074–e100074. doi: 10.1136/bmjos-2020-100074
19. Lei HH, Ma Z, Tian KX, Liu K, Wang JY, Zhu XY, et al. The effects of different types of Tai Chi exercises on motor function in patients with Parkinson’s disease: A network meta-analysis. Front Aging Neurosci (2022) 14:936027. doi: 10.3389/fnagi.2022.936027
20. Su KQ, Yuan J, Liu HH, Luo M, Li Q, Liu ST, et al. The comparative effectiveness of traditional chinese medicine exercise therapies in elderly people with mild cognitive impairment: A systematic review and network meta-analysis. Front Neurol (2022) 13:775190. doi: 10.3389/fneur.2022.775190
21. Salanti G, Ades AE, Ioannidis JPA. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol (2011) 64(2):163–71. doi: 10.1016/j.jclinepi.2010.03.016
22. Wu C, Ge YL, Zhang XY, Du YL, He SZ, Ji ZH, et al. The combined effects of Lamaze breathing training and nursing intervention on the delivery in primipara A PRISMA systematic review meta-analysis. Medicine (2021) 100(4):e2920. doi: 10.1097/md.0000000000023920
23. Sterne JAC, Gavaghan D, Egger M. Publication and related bias in meta-analysis: Power of statistical tests and prevalence in the literature. J Clin Epidemiol (2000) 53(11):1119–29. doi: 10.1016/s0895-4356(00)00242-0
24. Bonab SB, Parvaneh M. The effect of twelve weeks of tai chi exercises on sleep quality, pain perception, and death anxiety in elderly women. Annales Medico-Psychologiques (2022) 180(9):905–11. doi: 10.1016/j.amp.2022.01.019
25. Liu J, Xie H, Liu M, Wang Z, Zou L, Yeung AS, et al. The effects of tai chi on heart rate variability in older chinese individuals with depression. Int J Environ Res Public Health (2018) 15(12):2771. doi: 10.3390/ijerph15122771
26. Ge Y, Liu H, Wu Q, Chen A, Gao Z, Xing F, et al. Effects of a short eight Tai Chi-forms for the pre-frail elderly people in senior living communities [Journal article]. Physiother Theory Pract (2022) 38(12):1928–36. doi: 10.1080/09593985.2021.1926023
27. Song J, Wei L, Cheng K, Lin Q, Xia P, Wang X, et al. The effect of modified tai chi exercises on the physical function and quality of life in elderly women with knee osteoarthritis [Journal article]. Front Aging Neurosci (2022) 14:860762. doi: 10.3389/fnagi.2022.860762
28. Li Y, Zhang H, Wang Y. Tai Chi Ameliorates Coronary Heart Disease by Affecting Serum Levels of miR-24 and miR-155. Front Physiol (2019) 10:587. doi: 10.3389/fphys.2019.00587
29. Redwine LS, Pung MA, Wilson K, Bangen KJ, Delano-Wood L, Hurwitz B. An exploratory randomized sub-study of light-to-moderate intensity exercise on cognitive function, depression symptoms and inflammation in older adults with heart failure [Journal article]. J Psychosomatic Res (2020) 128:109883. doi: 10.1016/j.jpsychores.2019.109883
30. Lam L. Effectiveness of Tai Chi in maintenance of cognitive and functional abilities in mild cognitive impairment: a randomised controlled trial. Hong Kong Med J (2014) 20(3 Suppl 3):20–3.
31. Hsu CY, Moyle W, Cooke M, Jones C. Seated Tai Chi versus usual activities in older people using wheelchairs: a randomized controlled trial [Journal article]. Complementary Ther Med (2016) 24:1–6. doi: 10.1016/j.ctim.2015.11.006
32. Huang N, Li W, Rong X, Champ M, Wei L, Li M, et al. Effects of a modified tai chi program on older people with mild dementia: a randomized controlled trial [Journal article]. J Alzheimer’s Dis (2019) 72(3):947–56. doi: 10.3233/JAD-190487
33. Chou K-L, Lee PWH, Yu ECS, Macfarlane D, Cheng Y-H, Chan SSC, et al. Effect of Tai Chi on depressive symptoms amongst Chinese older patients with depressive disorders: a randomized clinical trial [Clinical Trial; Randomized Controlled Trial; Research Support, Non-U.S. Gov’t]. Int J Geriatric Psychiatry (2004) 19(11):1105–7. doi: 10.1002/gps.1178
34. Ma C, Zhou W, Tang Q, Huang S. The impact of group-based Tai chi on health-status outcomes among community-dwelling older adults with hypertension [Journal article]. Heart Lung (2018) 47(4):337–44. doi: 10.1016/j.hrtlng.2018.04.007
35. Leung RWM, McKeough ZJ, Peters MJ, Alison JA. Short-form Sun-style t’ai chi as an exercise training modality in people with COPD [Article]. Eur Respir J (2013) 41(5):1051–7. doi: 10.1183/09031936.00036912
36. Yeh GY, Litrownik D, Wayne PM, Beach D, Klings ES, Reyes Nieva H, et al. BEAM study (Breathing, Education, Awareness, Movement): a randomised controlled feasibility trial of tai chi exercise in patients with COPD [Journal article]. BMJ Open Respir Res (2020) 7(1):e000697. doi: 10.1136/bmjresp-2020-000697
37. Yıldırım P, Ofluoglu D, Aydogan S, Akyuz G. Tai Chi vs. combined exercise prescription: a comparison of their effects on factors related to falls. J Back Musculoskeletal Rehabil (2016) 29(3):493–501. doi: 10.3233/BMR-150645
38. Solianik R, Mickeviciene D, Zlibinaite L, Cekanauskaite A. Tai chi improves psychoemotional state, cognition, and motor learning in older adults during the COVID-19 pandemic. Exp Gerontol (2021) 150:111363. doi: 10.1016/j.exger.2021.111363
39. Irwin MR, Olmstead R, Carrillo C, Sadeghi N, Breen EC, Witarama T, et al. Cognitive behavioral therapy vs. Tai Chi for late life insomnia and inflammatory risk: a randomized controlled comparative efficacy trial. Sleep (2014) 37(9):1543–52. doi: 10.5665/sleep.4008
40. Kilpatrick LA, Siddarth P, Milillo MM, Krause-Sorio B, Ercoli L, Narr KL, et al. Impact of Tai Chi as an adjunct treatment on brain connectivity in geriatric depression. J Affect Disord (2022) 315:1–6. doi: 10.1016/j.jad.2022.07.049
41. Lavretsky H, Milillo MM, Kilpatrick L, Grzenda A, Wu P, Nguyen SA, et al. A randomized controlled trial of tai chi chih or health education for geriatric depression. Am J Geriatric Psychiatry (2022) 30(3):392–403. doi: 10.1016/j.jagp.2021.07.008
42. Chan AW, Yu DS, Choi KC. Effects of tai chi qigong on psychosocial well-being among hidden elderly, using elderly neighborhood volunteer approach: a pilot randomized controlled trial. Clin Interventions Aging (2017) 12:85–96. doi: 10.2147/cia.S124604
43. Lavretsky H, Alstein LL, Olmstead RE, Ercoli LM, Riparetti-Brown M, Cyr NS, et al. Complementary use of tai chi chih augments escitalopram treatment of geriatric depression: a randomized controlled trial [Journal article]. Am J Geriatric Psychiatry (2011) 19(10):839–50. doi: 10.1097/JGP.0b013e31820ee9ef
44. Yeh GY, Wood MJ, Wayne PM, Quilty MT, Stevenson LW, Davis RB, et al. Tai chi in patients with heart failure with preserved ejection fraction. Congestive Heart Failure (2013) 19(2):77–84. doi: 10.1111/chf.12005
45. Frye B, Scheinthal S, Kemarskaya T, Pruchno R. Tai chi and low impact exercise: Effects on the physical functioning and psychological well-being of older people. J Appl Gerontol (2007) 26(5):433–53. doi: 10.1177/0733464807306915
46. Roswiyani R, Hiew CH, Witteman CLM, Satiadarma MP, Spijker J. Art activities and qigong exercise for the well-being of older adults in nursing homes in Indonesia: a randomized controlled trial. Aging Ment Health (2020) 24(10):1569–78. doi: 10.1080/13607863.2019.1617239
47. Tsang HW, Tsang WW, Jones AY, Fung KM, Chan AH, Chan EP, et al. Psycho-physical and neurophysiological effects of qigong on depressed elders with chronic illness. Aging Ment Health (2013) 17(3):336–48. doi: 10.1080/13607863.2012.732035
48. Lee P, Cai S, Lu EY, Ng BFL, Jensen MP, Tsang HWH. Qigong reduces depressive symptoms of Taiwanese elderly with chronic physical illness: A randomized controlled trial. J Altern Complement Med (2020) 26(1):76–8. doi: 10.1089/acm.2019.0354
49. Sun P. Yijinjing Qigong intervention shows strong evidence on clinical effectiveness and electroencephalography signal features for early poststroke depression: A randomized, controlled trial. Front Aging Neurosci (2022) 14:956316. doi: 10.3389/fnagi.2022.956316
50. Carcelén-Fraile MDC, Aibar-Almazán A, Martínez-Amat A, Jiménez-García JD, Brandão-Loureiro V, García-Garro PA, et al. Qigong for mental health and sleep quality in postmenopausal women: A randomized controlled trial [Article]. Med (United States) (2022) 101(39):E30897. doi: 10.1097/MD.0000000000030897
51. Martínez N, Martorell C, Espinosa L, Marasigan V, Domènech S, Inzitari M. Impact of Qigong on quality of life, pain and depressive symptoms in older adults admitted to an intermediate care rehabilitation unit: a randomized controlled trial. Aging Clin Exp Res (2015) 27(2):125–30. doi: 10.1007/s40520-014-0250-y
52. Jing L, Jin Y, Zhang X, Wang F, Song Y, Xing F. The effect of Baduanjin qigong combined with CBT on physical fitness and psychological health of elderly housebound. Medicine (2018) 97(51):e13654. doi: 10.1097/md.0000000000013654
53. Zhang YX, Quan Y, Chen MH, Zhang D, Zhang Y, Zhu ZG. Does Liuzijue Qigong affect anxiety in patients with chronic obstructive pulmonary disease, even during the COVID-19 outbreak? a randomized, controlled trial [Article]. Traditional Med Res (2020) 5(4):216–28. doi: 10.12032/TMR20200528183
54. Krause-Sorio B, Siddarth P, Kilpatrick L, Milillo MM, Aguilar-Faustino Y, Ercoli L, et al. Yoga prevents gray matter atrophy in women at risk for alzheimer’s disease: A randomized controlled trial [Article]. J Alzheimers Dis (2022) 87(2):569–81. doi: 10.3233/jad-215563
55. Kwok JYY, Kwan JCY, Auyeung M, Mok VCT, Lau CKY, Choi KC, et al. Effects of mindfulness yoga vs stretching and resistance training exercises on anxiety and depression for people with parkinson disease A randomized clinical trial [Article]. JAMA Neurol (2019) 76(7):755–63. doi: 10.1001/jamaneurol.2019.0534
56. Choi MJ, Sohng KY. The effects of floor-seated exercise program on physical fitness, depression, and sleep in older adults: A cluster randomized controlled trial. Int J Gerontol (2018) 12(2):116–21. doi: 10.1016/j.ijge.2017.06.003
57. Eyre HA, Acevedo B, Yang HY, Siddarth P, Van Dyk K, Ercoli L, et al. Changes in neural connectivity and memory following a yoga intervention for older adults: A pilot study. J Alzheimers Dis (2016) 52(2):673–84. doi: 10.3233/jad-150653
58. Chang J, Zhu W, Zhang J, Yong L, Yang M, Wang J, et al. The effect of chinese square dance exercise on cognitive function in older women with mild cognitive impairment: the mediating effect of mood status and quality of life [Article]. Front Psychiatry (2021) 12:711079. doi: 10.3389/fpsyt.2021.711079
59. Haboush A, Floyd M, Caron J, LaSota M, Alvarez K. Ballroom dance lessons for geriatric depression: An exploratory study [Article]. Arts Psychother (2006) 33(2):89–97. doi: 10.1016/j.aip.2005.10.001
60. Hashimoto H, Takabatake S, Miyaguchi H, Nakanishi H, Naitou Y. Effects of dance on motor functions, cognitive functions, and mental symptoms of Parkinson’s disease: A quasi-randomized pilot trial [Article]. Complementary Therapies Med (2015) 23(2):210–9. doi: 10.1016/j.ctim.2015.01.010
61. Lee HJ, Kim SY, Chae Y, Kim MY, Yin C, Jung WS, et al. Turo (Qi Dance) Program for Parkinson’s Disease Patients: randomized, Assessor Blind, Waiting-List Control, Partial Crossover Study [Journal article]. Explore (New York NY) (2018) 14(3):216–23. doi: 10.1016/j.explore.2017.11.002
62. Mavrovouniotis FH, Argiriadou EA, Papaioannou CS. Greek traditional dances and quality of old people’s life. J Bodywork Movement Ther (2010) 14(3):209–18. doi: 10.1016/j.jbmt.2008.11.005
63. Ventura MI, Barnes DE, Ross JM, Lanni KE, Sigvardt KA, Disbrow EA. A pilot study to evaluate multi-dimensional effects of dance for people with Parkinson’s disease [Journal article]. Contemp Clin Trials (2016) 51:50–5. doi: 10.1016/j.cct.2016.10.001
64. Curi VS, Vilaca J, Haas AN, Fernandes HM. Effects of 16-weeks of Pilates on health perception and sleep quality among elderly women [Journal article]. Arch Gerontol Geriatrics (2018) 74:118–22. doi: 10.1016/j.archger.2017.10.012
65. Brucki S, Zheng G, Li S, Huang M, Liu F, Tao J, et al. The effect of tai chi training on cardiorespiratory fitness in healthy adults: A systematic review and meta-analysis. PloS One (2015) 10(2):e0117360. doi: 10.1371/journal.pone.0117360
66. D’Ascola A, Bruschetta G, Zanghì G, Campo S, Medica P, Campana S, et al. Changes in plasma 5-HT levels and equine leukocyte SERT expression in response to treadmill exercise. Res Vet Sci (2018) 118:184–90. doi: 10.1016/j.rvsc.2018.02.012
67. Wegner M, Helmich I, MaChado S, Nardi AE, Arias-Carrión O, Budde H. Effects of exercise on anxiety and depression disorders: review of meta-analyses and neurobiological mechanisms. CNS Neurol Disorders-Drug Targets (2014) 13(6):1002–14. doi: 10.2174/1871527313666140612102841
68. Wang HR, Wei AK, Lu YZ, Yu B, Chen WH, Lu Y, et al. Simplified tai chi program training versus traditional tai chi on the functional movement screening in older adults. Evidence-Based Complementary Altern Med (2016) 2016. doi: 10.1155/2016/5867810
69. Qin JW, Chen YN, Guo S, You Y, Xu Y, Wu JS, et al. Effect of tai chi on quality of life, body mass index, and waist-hip ratio in patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Front Endocrinol (2021) 11:543627. doi: 10.3389/fendo.2020.543627
70. Jiang W, Liao SJ, Chen XK, Lundborg CS, Marrone G, Wen ZH, et al. TaiChi and qigong for depressive symptoms in patients with chronic heart failure: A systematic review with meta-analysis. Evidence-Based Complementary Altern Med (2021) 2021. doi: 10.1155/2021/5585239
71. Huang ZG, Feng YH, Li YH, Lv CS. Systematic review and meta-analysis: Tai Chi for preventing falls in older adults. BMJ Open (2017) 7(2):e013661. doi: 10.1136/bmjopen-2016-013661
72. Yeung A, Lepoutre V, Wayne P, Yeh G, Slipp LE, Fava M, et al. Tai chi treatment for depression in chinese americans A pilot study. Am J Phys Med Rehabil (2012) 91(10):863–70. doi: 10.1097/PHM.0b013e31825f1a67
73. Cheung BMY, Lo JLF, Fong DYT, Chan MY, Wong SHT, Wong VCW, et al. Randomised controlled trial of qigong in the treatment of mild essential hypertension. J Hum Hypertension (2005) 19(9):697–704. doi: 10.1038/sj.jhh.1001884
74. Chang PS, Knobf T, Oh B, Funk M. Physical and psychological health outcomes of qigong exercise in older adults: A systematic review and meta-analysis. Am J Chin Med (2019) 47(2):301–22. doi: 10.1142/s0192415x19500149
75. Saeed SA, Cunningham K, Bloch RM. Depression and anxiety disorders: benefits of exercise, yoga, and meditation. Am Family Phys (2019) 99(10):620–7.
76. Ko KY, Kwok ZCM, Chan HYL. Effects of yoga on physical and psychological health among community-dwelling older adults: A systematic review and meta-analysis. Int J Older People Nursing (2023) 18(5):e12562. doi: 10.1111/opn.12562
77. Lavretsky H, Epel ES, Siddarth P, Nazarian N, St Cyr N, Khalsa DS, et al. A pilot study of yogic meditation for family dementia caregivers with depressive symptoms: effects on mental health, cognition, and telomerase activity. Int J Geriatric Psychiatry (2013) 28(1):57–65. doi: 10.1002/gps.3790
78. Taylor J, McLean L, Korner A, Stratton E, Glozier N. Mindfulness and yoga for psychological trauma: systematic review and meta-analysis. J Trauma Dissociation (2020) 21(5):536–73. doi: 10.1080/15299732.2020.1760167
79. Meikis L, Wicker P, Donath L. Effects of pilates training on physiological and psychological health parameters in healthy older adults and in older adults with clinical conditions over 55 years: A meta-analytical review. Front Neurol (2021) 12:724218. doi: 10.3389/fneur.2021.724218
80. Curi VS, Vilaca J, Haas AN, Fernandes HM. Effects of 16-weeks of Pilates on health perception and sleep quality among elderly women. Arch Gerontol Geriatrics (2018) 74:118–22. doi: 10.1016/j.archger.2017.10.012
81. Wang LL, Sun CJ, Wang Y, Zhan TT, Yuan J, Niu CY, et al. Effects of dance therapy on non-motor symptoms in patients with Parkinson’s disease: a systematic review and meta-analysis. Aging Clin Exp Res (2022) 34(6):1201–8. doi: 10.1007/s40520-021-02030-7
82. Zhang Q, Hu JN, Wei LJ, Jia YB, Jin Y. Effects of dance therapy on cognitive and mood symptoms in people with Parkinson’s disease: A systematic review and meta-analysis. Complementary Ther Clin Pract (2019) 36:12–7. doi: 10.1016/j.ctcp.2019.04.005
Keywords: mind-body exercise, anxiety, depression, older adults, network meta-analysis
Citation: Dong Y, Zhang X, Zhao R, Cao L, Kuang X and Yao J (2024) The effects of mind-body exercise on anxiety and depression in older adults: a systematic review and network meta-analysis. Front. Psychiatry 15:1305295. doi: 10.3389/fpsyt.2024.1305295
Received: 01 October 2023; Accepted: 23 January 2024;
Published: 07 February 2024.
Edited by:
Júlio Belo Fernandes, Egas Moniz Center for Interdisciplinary Research (CiiEM), PortugalReviewed by:
Paola Longo, University of Turin, ItalyYipeng Wang, University of Florida, United States
Copyright © 2024 Dong, Zhang, Zhao, Cao, Kuang and Yao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoqin Kuang, a3Vhbmd4cTIwMjNAMTYzLmNvbQ==; Jiwei Yao, eWp3ZHhzMDkxNDEwMjBAMTYzLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Yangjian Dong
Yangjian Dong Xinxin Zhang1†
Xinxin Zhang1† Xiaoqin Kuang
Xiaoqin Kuang