- 1Flinders Health and Medical Research Institute, College of Medicine and Public Health, Flinders University, Adelaide, SA, Australia
- 2Behavioural Research Unit, Cancer Council SA, Adelaide, SA, Australia
- 3National Centre for Education and Training on Addiction, Flinders University, Bedford Park, SA, Australia
As tobacco smoking prevalence is unacceptably high for the one in five Australians reporting a mental health condition in the past year, multiple cessation supports are needed to reduce tobacco-related disease. Nicotine vaping product (NVP)-facilitated smoking cessation is one option requiring a medical prescription in Australia. Yet, people easily obtain NVPs via non-prescription channels. As mental health impacts quitting intentions and health system engagement, this study examined how presence of anxiety and depression symptoms may be associated with perceived health risk of using NVPs from prescription or non-prescription sources for smoking cessation. We used cross-sectional South Australian (15 years +) 2022 survey data on vaping, smoking, anxiety, and depression. Robust linear regression was used to examine the association of anxiety and depression symptoms and nicotine addiction concern on perceived health risk of using NVPs from prescription or non-prescription sources. For prescription NVPs, vaping was associated with lower perceived health risk (b=−0.732). Higher perceived addiction risk was associated with higher perceived health risk from prescription NVPs (b=0.784). For non-prescription NVPs, vaping (b=−0.661) or smoking (b=−0.310) was associated with lower perceived health risk, and higher perceived addiction risk (b=0.733) was associated with a higher perceived health risk. Although anxiety and depression were not directly associated with NVP health risk perceptions, vaping while having depression symptoms was associated with higher perceived health risk ratings for prescription (b=0.700) but not non-prescription sources. People with depression who vape may see health risk barriers in NVP prescription access for smoking cessation, a smoking cessation support gap.
1 Introduction
Despite successful tobacco control efforts in Australia, smoking rates continue to be unacceptably high at 11% in the general population and up to 84% among some population groups (1). There is high-level evidence of the effectiveness of nicotine vaping products (NVP) to assist people to stop smoking (2). Current evidence supports the use of NVPs as a second-line therapy for treating tobacco use and dependence (2) after the established route of combination nicotine replacement therapy (i.e., long-acting transdermal, rapid-acting oromucosal) with behavioural counselling has been attempted (3). Despite this, public sentiment studies show regulated NVP-facilitated cessation to be an acceptable approach to tobacco cessation (4, 5) despite some health organisations holding cautious positions regarding the evidence and safety (6, 7).
Australians have access to NVPs through a variety of sources despite this being one of the most highly regulated environments for these products. The legally accepted route for accessing NVPs is through a medical prescription for purchase access or personal importation, specifically for tobacco cessation purposes. However, the more commonly used route is to identify non-legal sources for NVPs due to the relatively fewer barriers in obtaining devices this way. Importantly, the public is also exposed to a variety of media addressing known and potential health risks of NVP use (8), which can inform these types of consumer health behaviours. Recent preventive health campaigns describe the potential physical health and addiction risks associated with vaping amongst youth (9).
The physical health of people with mental health conditions is a priority in Australia’s National Preventive Health Strategy (10) given their markedly higher smoking prevalence than the wider population at 20.2% versus 9.9% of those without one in 2019 (11). Moreover, 21.0% of Australians reported a mental health condition in the past 12 months (12), including anxiety (16.8%) and affective disorders (8.0%) such as depressive episodes (4.6%) (13). Together, this indicates a population at high risk of tobacco-related illnesses.
Mental and physical illness can increase our attention to health concerns as uncontrollable contributing to reduced motivation and unhealthy behaviour (14). For example, models of depression emphasise low likelihood of positive outcomes and high probability of aversive outcomes—or pessimistic judgement bias (15). Depression and anxiety can lower quitting intentions particularly for depression (16). As depression (17) and anxiety (18) are also associated with poorer adherence to current smoking cessation approaches (e.g., transdermal patches), acceptability of alternatives, such as NVPs, warrant exploration in relation to these mental health factors.
Perceived health risks of NVP use can be influenced by socioeconomic gradient, gender, ethnicity, and sexual orientation (19), as well as by mental health status (20, 21). A study in England found that sizable proportion of people who used e-cigarettes still considered these to be equally (35%) or more (6%) (2) addictive than tobacco cigarettes with 77% reporting that they felt addicted to vaping (22). These perceptions may also influence willingness to engage with healthcare professionals who themselves weigh the prescribing risks regarding NVP safety (23). Early US research found that prescription medications can be judged as riskier than over-the-counter medications for reasons including drug familiarity, prescriber interaction, and uncertainty around health risk (24). Given these considerations, it follows that health risk perceptions of accessing NVPs via both prescription and informal routes may inform willingness to engage with this alternative to established smoking cessation methods [e.g., patch Nicotine Replacement Therapy (NRT)] among people with mental health symptoms. Understanding this further can help in framing health communication about NVP sourcing decisions and prescription access for people with anxiety and depression symptoms.
This study aims to examine how the presence of anxiety and depression symptoms may be associated with perceived health risk associated with sourcing NVPs via both routes, as well as the association of media exposure and general nicotine addiction concerns regarding NVP use. We examine the association of demographic and depression and anxiety characteristics with perceived health risk of sourcing NVPs from prescription versus non-prescription sources.
2 Materials and methods
2.1 Study design
A cross-sectional population computer-assisted telephone interview survey with the SA Health Population Health Survey Module System (PHSMS) was used. Participants were eligible if aged ≥15 years and residing in South Australia. Surveying occurred from November to December 2022. This study was part of the larger PHSMS annual omnibus telephone survey. The PHSMS used random digit dialing and multistage systematic sampling of metropolitan and regional South Australian residential centres, with approximately 3,000 respondents and up to 80 questions each year (25). Items relating to this study included question on demographics, anxiety and depression symptoms, smoking and vaping behaviour, and NVP health risk perceptions. The full bank of items can be requested from Wellbeing SA (26).
2.2 Participants
Of the eligible people contacted (n=3,741), non-participation (n=749) resulted from refusal (n=216), discontinued contact (n=36), physical or mental capacity (n=275), or language option unavailability (n=212). There was an 80.2% participation rate and a final sample of 3,002 respondents. Parental consent was obtained for participants aged 15 to 17 years.
2.3 Measures
2.3.1 Sociodemographic
Sociodemographic factors included age, sex, education [range: 1 low (no schooling) to 8 high (tertiary)], and relative socioeconomic advantage in ascending deciles via socio-economic index for areas (SEIFA) (27). Primary language at home, income [range: 1 low (≤20,000) to 8 high (>150,000)], and metropolitan versus country residence were also recorded. Current smoking was determined by asking whether participants “currently smoke cigarettes, cigars, pipes, or other tobacco products” on a “daily,” “at least weekly,” “less often than weekly” basis, or “not at all.” Participants who smoked daily, at least weekly, or less often than weekly, were coded as people who smoked. Similarly, current vaping was determined by asking whether participants “currently use e-cigarettes” on a “daily,” “at least weekly,” “less often than weekly” basis, or “not at all.” Those who vaped daily, at least weekly, or less often than weekly, were coded as people who currently vaped.
2.3.2 Anxiety and depression symptoms
Mental health was measured via the Patient Health Questionnaire 4 (PHQ-4), a short four-item mental health screening scale for anxiety and depression symptoms (28). Items for anxiety symptoms were as follows: 1) Over the last 2 weeks, how often have you been bothered by feeling nervous, anxious, or on edge? 2) Over the last 2 weeks, how often have you been bothered by not being able to stop or control worrying? Items for depression symptoms were as follows: 1) Over the last 2 weeks, how often have you been bothered by little interest or pleasure in doing things? 2) Over the last 2 weeks, how often have you been bothered by feeling down, depressed, or hopeless? Items are rated 0 not at all to 3 nearly every day summing two items each for depression and anxiety (range: 0–6, cutoff ≥3) symptom severity. Binary variables were created for PHQ-4 indicating likely presence of depression and anxiety. Overall mental health symptom severity score ranged from 0 to 12, with symptom cutoffs of 0–2 none, 3–5 mild, 6–8 moderate, and 9–12 severe.
2.3.3 Risk perception
The perceived addiction risk of vaping was recorded by asking, “If a person uses a nicotine e-cigarette or vaping device to reduce or quit smoking, how much risk of addiction to vaping is there after they stop smoking tobacco?,” rated 1 no risk to 5 extreme risk or do not know or prefer not to say. This was categorised as 1 low, 2 moderate, or 3 high for the regressions. Perceived health risk exposure when using NVPs obtained via the non-prescription versus prescription sources was recorded by asking, “If a person is using a non-prescription nicotine e-cigarette or vaping device to reduce or quit smoking, how much health risk do you feel they are exposed to?” and “If a person is using a prescription nicotine e-cigarette or vaping device to reduce or quit smoking, how much health risk do you feel they are exposed to?” Both items were rated from 1 no risk to 5 extreme risk or do not know or prefer not to say. Exposure to vaping-related media was recorded via the item, “How often do you see media that presents scientific evidence about the use of e-cigarette or vaping devices?,” rated from 1 never (e.g., every 6 months) to 5 very frequently (e.g., multiple times per week).
2.4 Procedure
Project approval was obtained from the Department for Health and Wellbeing Human Research Ethics Committee (HREC/18/SAH/78/AM10), and all participants provided informed consent. An external research provider contacted participants by random digit dialing, provided a study summary, and sought consent for surveying by phone. Parental consent was obtained for those aged <18 years to participate. Languages other than English, and male or female interviewers could be chosen, where interviewers were available for this.
3 Data analysis
Descriptive analyses were conducted with R v.4.1.3, (29) using the packages “corrplot,” (30) “psych,” (31) and “olsrr” (32) to inspect diagnostic plots with weighted robust linear regression performed using the “robustbase” (33) package for outlier and normality considerations. Two linear regression models were fitted for the association of PHQ-4 anxiety and depression symptom presence with level of perceived health risk of prescription versus non-prescription NVPs, including variables for age, sex, social advantage, primary language, education, income, and metropolitan versus country residential classification. Interaction terms were included for tobacco smoking, vaping, and media exposure to vaping-related media, with indicators for presence of anxiety and depression symptoms, as use of nicotine products and media exposure related to this is highly likely to influence risk perceptions related to NVP use.
Key variables in the models included tobacco smoking, use of NVPs, exposure to media that presents scientific evidence about the use of e-cigarette or vaping devices, perceived risk of addiction to vaping once a person stops smoking tobacco, PHQ-4-indicated anxiety and depression symptoms, and interactions of tobacco smoking, vaping, and exposure to media about e-cigarettes and vaping, with anxiety and depression symptoms. To avoid error rate inflation, false discovery adjusted p-values using “p.adjust” in the “stats” (34) package are reported with unadjusted values and confidence intervals. Data were weighted by inverse selection probability, then by age group, by sex, and by metropolitan or country residence using 2016 Australian Census data for consistency with previous PHSMS datasets. Figures are weighted unless otherwise specified. This study was not preregistered, as no hypotheses were tested in this exploratory analysis (35).
4 Results
Among the participants who proceeded beyond the demographic component of the survey, those stating they were not familiar with NVPs were excluded from answering questions related to them (n=401). This exclusion led to approximately 13% of missing data for the items used in the two regression models. Selection of the items “prefer not to say” and “don’t know” accounted for further reduction in cases included in both models. A small number of influential cases were downweighted in “robustbase” based on Mahalanobis distance for the first (n=33) and second regression (n=40).
4.1 Sociodemographic
Sociodemographic, nicotine use, and mental health characteristics in Table 1 show that the overall sample (N=3,002) averaged 47.90 ± 18.97 years of age, around half were female (50.82%), lived mostly in metropolitan areas (70.73%), and were well educated with a medium level of average social advantage. Low levels of current tobacco smoking (11.16%) and e-cigarette use (3.70%) were seen with many viewing vaping as a nicotine addiction risk (81.81%) and half (54.91%) reporting exposure to media that presents scientific evidence about the use of e-cigarette or vaping devices. Most participants reported no PHQ-4 mental health symptoms (69.57%), while the remaining participants reported mild (18.07%), moderate (7.10%), or severe (5.26%) overall mental health symptoms. PHQ-4 scores indicated anxiety (16.90%) and depression (12.00%) symptoms for some participants.
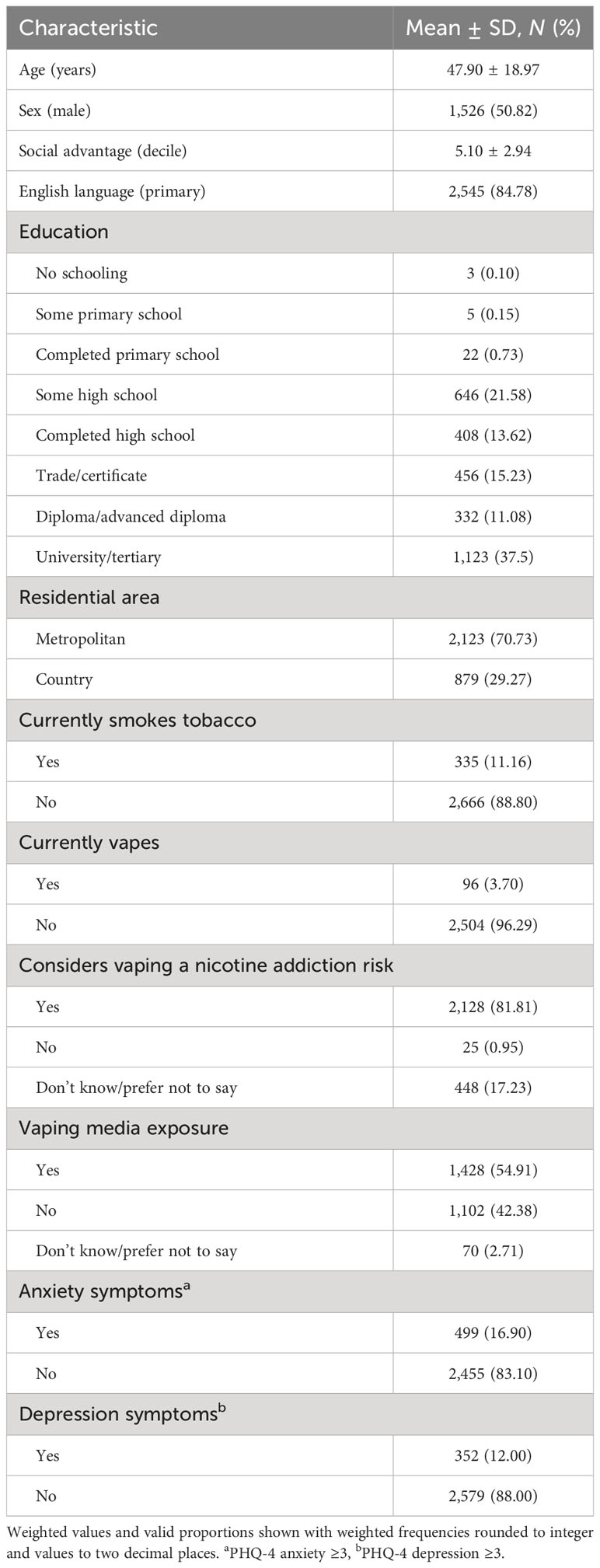
Table 1 Sociodemographic and mental health characteristics of total sample, aged ≥15 years (N=3,002).
4.2 Perceived health risk of NVPs from prescription sources for tobacco cessation
Table 2 shows the associations between demographic, nicotine use (i.e., smoking, vaping), nicotine addiction risk perception, and anxiety and depression characteristics with perceived health risk of using prescription NVPs. The model indicated that vaping (beta=−0.732, 95% CI=−0.984, −0.480), but not smoking (beta=−0.214, 95% CI=−0.414, −0.015), was associated with lower perceived health risk of prescription NVPs. Exposure to media presenting scientific evidence about vaping was not associated with perceived prescription NVP risk (beta=−0.128, 95% CI=−0.002, 0.257). However, perceived risk of nicotine addiction from vaping to quit smoking was associated with higher perceived health risk of prescription NVPs (beta=0.784, 95% CI=0.690, 0.787).
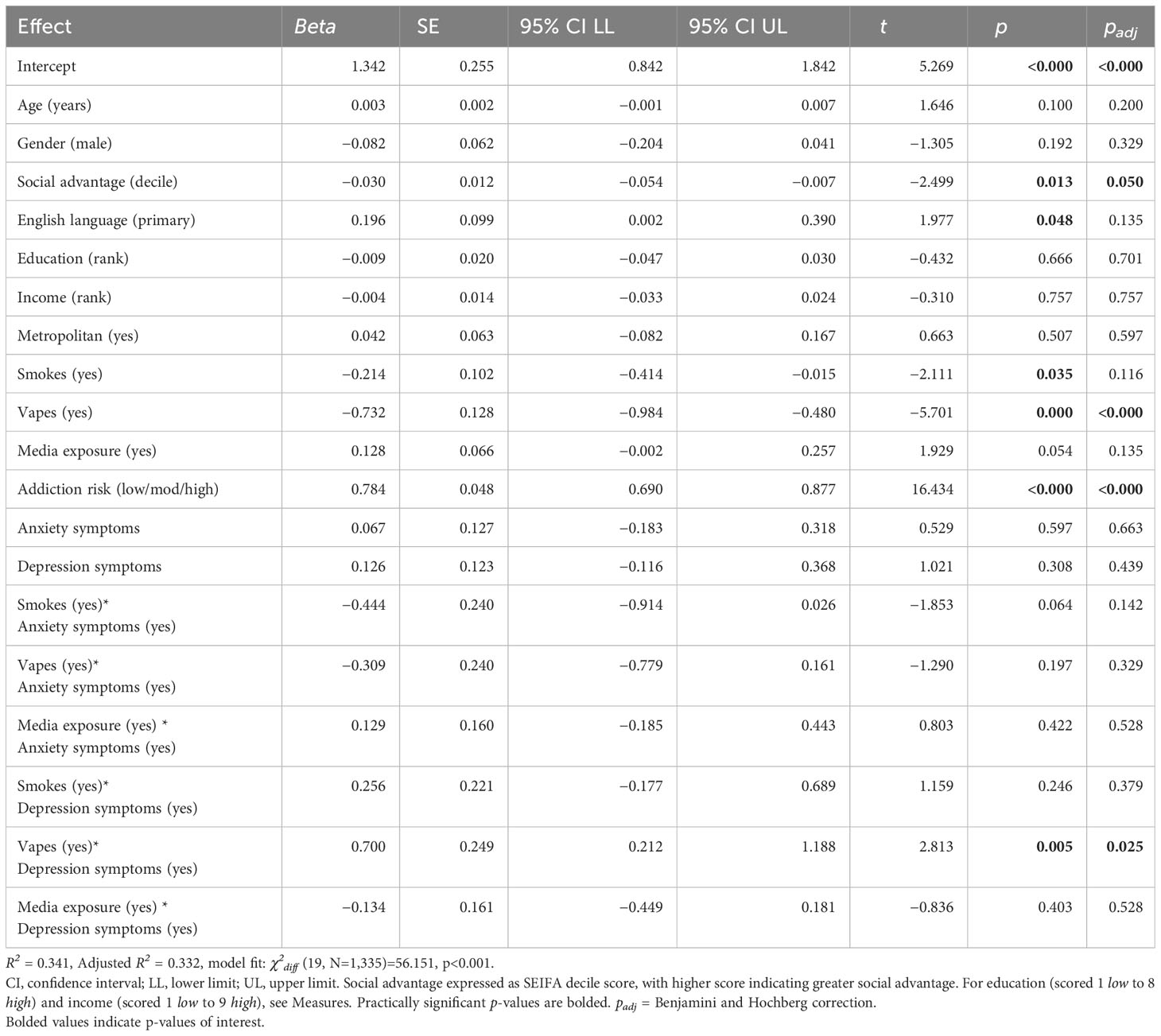
Table 2 Robust linear regression summary for demographic factors and presence of anxiety and depression symptoms predicting perceived health risk associated with accessing NVPs through prescription sources (N=1,336).
Mental health symptoms were not associated with health risk views on prescription NVPs when indicating presence of anxiety (beta=0.067, 95% CI=−0.183, 0.318) or depression (beta=0.126, 95% CI=−0.116, 0.368). Associations of smoking, vaping, and media exposure with health risk views on prescription NVPs were not modified by the presence of anxiety symptoms. Similarly, associations of smoking and media exposure with health risk views on prescription NVPs were not modified by the presence of depression symptoms. However, vaping was associated with a higher perceived risk of prescription NVPs among people with depression symptoms (beta=0.700, 95% CI=0.212, 1.118) (see Table 2).
4.3 Perceived health risk of NVPs from non-prescription sources for tobacco cessation
Table 3 shows the associations between demographic, nicotine use (i.e., smoking, vaping), nicotine addiction risk perception, and anxiety and depression characteristics with perceived health risk of using non-prescription NVPs. Both vaping and smoking were associated with lower perceived health risk of non-prescription NVPs with this being stronger for vaping (beta=−0.661, 95% CI=−1.196, −0.126) than for smoking (beta=−0.310, 95% CI=−0.558, −0.062). Exposure to media on scientific evidence about vaping was not associated with perceived non-prescription NVP risk. Perceived risk of nicotine addiction from vaping to quit smoking was associated with higher perceived health risk of non-prescription NVPs (beta=0.733, 95% CI=0.602, 0.865).
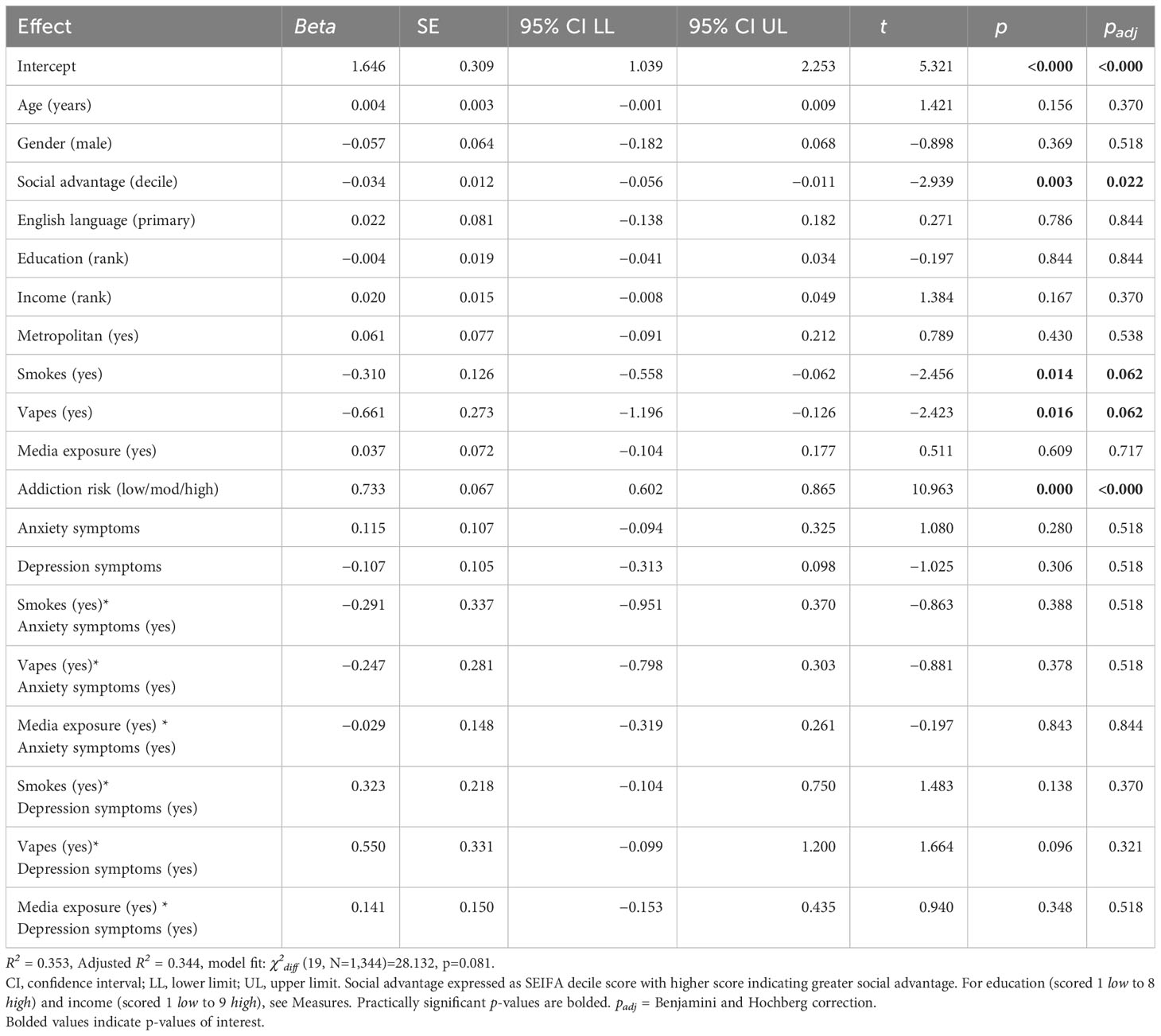
Table 3 Robust linear regression summary for demographic factors and presence of anxiety and depression symptoms predicting perceived health risk associated with accessing NVPs through non-prescription sources (N=1345).
Mental health symptoms were again not associated with risk views on non-prescription NVPs when indicating presence of anxiety (beta=0.115, 95% CI=−0.094, 0.325) or depression (beta=-0.107, 95% CI=−0.313, 0.098). However, associations of smoking, vaping, and media exposure with risk views on non-prescription NVPs were not modified by the presence of anxiety or depression symptoms.
5 Discussion
This study found that there is little difference between how people view health risk of vaping-facilitated tobacco smoking cessation when NVPs are sourced via medical prescription versus non-prescription sources (e.g., other people, illegal sales). This latter category encompasses illegal NVP markets, a source of vaping products that Australia is moving to further restrict access to (36). As this leaves only prescription access for smokers opting for NVP-facilitated cessation, preventive health communications about this process consider how mental health symptoms can factor into this process.
Concern about the potential risk of nicotine addiction from vaping being related to increased health risk concern about using NVPs from either source is consistent with other findings that stronger perceptions of addictiveness are inversely related to the use of e-cigarettes (37).
Our study identified no main effect of anxiety or depression on perceptions of health risks of NVP-facilitated smoking cessation—whether via the prescription or non-prescription route. However, a key finding related to depression symptoms and being a person who vapes. Findings showed that being either a person who smokes or who vapes was associated with seeing lower health risk in NVP-facilitated quitting, irrespective of sourcing NVPs via prescription or elsewhere. Though when mental health symptoms indicated depression in a person, being a person who uses a vape was associated with seeing greater health risk in NVP-facilitated quitting—though only for prescription-sourced NVPs.
If this effect is meaningful—and further research is necessary to test this—it may mean that people experiencing depression who vape have a low likelihood of engaging with the prescription access system for quitting—something they may benefit from in the future if availability of non-prescription NVPs becomes more difficult under tightened Australian tobacco and vaping regulations. Alternatively, this finding could arise from the assumption that the way a person currently accesses NVPs will continue to be available in the future. As noted, there is a low likelihood that this source is prescription access given research showing proportions for this (7%) compared to other sources (e.g., vape shop, 53%; friend over 18, 39%; tobacconist, 33%; online, 30%) (37).
A further possible reason could relate to pessimistic judgement bias present in models of depression (15), where a person might anticipate poorer outcomes regarding health risks of prescription access NVPs. This may limit intentions to use this approach for smoking cessation or for switching from non-prescription to prescription NVPs. Studies of clients of psychiatric services indicate complex relationships with nicotine use and cessation, including overall declining health and pessimism about success of nicotine replacement (38). Australia has mental health-specific support for quitting smoking (39, 40), a suitable avenue for addressing barriers to NVP-facilitated cessation by people living with depression.
It may also be the case that population-specific supported or subsidised access for people experiencing depression, coupled with targeted education on health risk evidence, may support access to a wider range of cessation pharmacotherapies in this group. As with tobacco cessation (41), health messaging focused on benefits to mental health could be tested, though in this case in relation to the benefits of accessing or switching to prescription NVPs versus via other unregulated sources.
6 Limitations
Limitations to the current study included, first, that a large number of respondents selected opt-out responses for key variables (i.e., “I don’t know,” “prefer not to say”). This was seen, for example, with considering vaping a nicotine addiction risk. However, excluding this, respondents still provided sufficient data for the models to be run. Second, as the overall sample was structured to be representative of the South Australian population, the prevalence of vaping, tobacco smoking, and respondents with high anxiety depression symptoms was relatively low. Third, the item used to ask about “exposure to scientific evidence about the use of e-cigarettes’” did not account for individual level of scientific literacy as a factor in the perceived and actual robustness of evidence that respondents considered for this item. Extensions of this study should factor in a measure of scientific literacy. Further research is needed that solely recruits people with clinically meaningful anxiety or depression symptoms, and potentially symptoms of other conditions. Fourth, both models should be replicated with a national Australian sample and be paired with qualitative comments to capture why people may see differing levels of addiction risk for both NVP source categories.
7 Conclusions
This study provides a brief and exploratory snapshot of how mental health symptoms of South Australians may affect perceptions of health risk of the NVP prescription access model versus via other non-prescription sources. General concern about nicotine addiction risk in NVP-facilitated smoking cessation was related to heath concerns of NVP use, irrespective of prescription or non-prescription source. People who vape and experience depression symptoms may see greater health risk in using the NVP prescription access model compared with those without depression symptoms. This has potential implications for this priority population in accessing prescription-sourced NVPs as part of a wider range of smoking cessation pharmacotherapies given that non-prescription sources are more highly restricted in Australia. Qualitative interviews with tobacco smokers with and without clinically meaningful anxiety or depression symptoms are needed to identify how health risk perceptions in this population can inform mental health-tailored smoking and vaping cessation programs.
Data availability statement
The data analysed in this study is subject to the following licenses/restrictions: Permission is required from Wellbeing SA and SA Health to access this South Australian population health data (42). Requests to access these datasets should be directed to am9zaHVhLnRyaWdnQGZsaW5kZXJzLmVkdS5hdQ==.
Ethics statement
This study was approved by SA Health Department for Health and Wellbeing Human Research Ethics Committee (HREC/18/SAH/78/AM10). The study was conducted in accordance with the local legislation and institutional requirements. Informed consent for participation in this study was provided by participants, and was provided by participants’ legal guardians were required.
Author contributions
JT: Conceptualization, Data curation, Formal Analysis, Methodology, Writing – original draft, Writing – review & editing. RC: Conceptualization, Investigation, Writing – original draft, Writing – review & editing. PA: Conceptualization, Writing – review & editing. JB: Writing – review & editing. BB: Conceptualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was conducted with data collected for Cancer Council SA and the South Australian Health and Medical Research Institute via research agreement with SA Health. Publication was supported by The Australian Prevention Partnership Centre. The Australian Prevention Partnership Centre is funded by the NHMRC, Australian Government Department of Health, ACT Health, Cancer Council Australia, NSW Ministry of Health, Wellbeing SA, Tasmanian Department of Health, and VicHealth. The Australian Government has also contributed funding through the Medical Research Future Fund. In 2022, Queensland Health joined the Prevention Centre as a financial contributor and valued partner. The Prevention Centre is administered by the Sax Institute. This work was funded by Cancer Council SA. JT was also supported by Australian National Health and Medical Research Council grant GNT1198301.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Author disclaimer
The authors are responsible for the content and writing of the paper, and do not necessarily represent the views of Cancer Council SA, SA Health, or the National Centre for Education and Training on Addiction.
References
1. Guydish J, Passalacqua E, Pagano A, Martínez C, Le T, Chun J, et al. An international systematic review of smoking prevalence in addiction treatment. Addiction (2016) 111:220–30. doi: 10.1111/add.13099
2. Hartmann-Boyce J, Lindson N, Butler AR, McRobbie H, Bullen C, Begh R, et al. Electronic cigarettes for smoking cessation. Cochrane Database Systematic Rev (2022) 11:CD010216. doi: 10.1002/14651858.CD010216.pub7
3. RACGP. Supporting smoking cessation: A guide for health professionals. Available online at: https://www.racgp.org.au/getattachment/c07241b0-9dc1-41bd-b25b-764389a675c9/Pharmacotherapy-for-smoking-cessation.aspx (Accessed 01 August 2021).
4. Jongenelis MI, Kameron C, Rudaizky D, Pettigrew SC. Support for e-cigarette regulations among Australian young adults. BMC Public Health (2019) 19:67. doi: 10.1186/s12889-019-6410-4
5. Erku DA, Gartner CE, Tengphakwaen U, Morphett K, Steadman K. Nicotine vaping product use, harm perception and policy support among pharmacy customers in Brisbane, Australia. Drug Alcohol Rev (2019) 38:703–11. doi: 10.1111/dar.12984
6. Cancer Council Australia. E-cigarettes: What are hey and are they harmful? Sydney, NSW: Cancer Council Australia (2022).
7. McDonald CF, Jones S, Beckert L, Bonevski B, Buchanan T, Bozier J, et al. Electronic cigarettes: A position statement from the Thoracic Society of Australia and New Zealand*. Respirology (2020) 25:1082–9. doi: 10.1111/resp.13904
8. Burton S, Soboleva A, Dadich A, Garlin F. Promoting e-cigarettes: media discussion of e-cigarettes before and after vaping deaths. J Strategic Marketing (2023) 2023:1–10. doi: 10.1080/0965254X.2023.2236110
9. Marcella HB, Nora S, Whitney B, Kresovich A, Sutfin E, Sheeran P, et al. Perceived effectiveness of objective elements of vaping prevention messages among adolescents. Tobacco Control (2023) 32:e228. doi: 10.1136/tobaccocontrol-2021-057151
10. Australian Government Department of Health. National Preventive Health Strategy 2021-2030 Canberra, ACT: Australian Government (2021).
11. Australian Institute of Health and Welfare. Mental Health Services in Australia: Physical Health of People with Mental Illness (2023). Available online at: https://www.aihw.gov.au/reports/mental-health-services/physical-health-of-people-with-mental-illness.
12. Australian Institute of Health and Welfare. Mental Health Services in Australia: Mental Health: Prevalence and Impact (2023). Available online at: https://www.aihw.gov.au/reports/mental-health-services/mental-health#Common.
13. Australian Bureau of Statistics. National Study of Mental Health and Wellbeing (2023). Available online at: https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/2020-21.
14. Savioni L, Triberti S. Cognitive biases in chronic illness and their impact on patients’ Commitment. Front Psychol (2020) 11:579455. doi: 10.3389/fpsyg.2020.579455
15. Noworyta K, Cieslik A and Rygula R. Neuromolecular underpinnings of negative cognitive bias in depression. Cells (2021) 10:3157. doi: 10.3390/cells10113157
16. Yang X, Zhang L, Lin H, Lin H, Cao W, Chang C. Psychiatric symptoms and intentions to quit smoking: How regularity and volume of cigarette consumption moderate the relationship. Tob Induc Dis (2023) 21:78. doi: 10.18332/tid/163258
17. Schnoll R, Barrila GM, Dalsimer S, Hosie Quinn M, Bauer A, Fox E, et al. Treatment adherence in a smoking cessation clinical trial for individuals with current or past major depressive disorder: Predictors and association with cessation. Addictive Behav (2023) 143:107686. doi: 10.1016/j.addbeh.2023.107686
18. Handschin J, Hitsman B, Blazekovic S, Veluz-Wilkins A, Wileyto E, Leone F, et al. Factors associated with adherence to transdermal nicotine patches within a smoking cessation effectiveness trial. J Smok Cessat (2018) 13:33–43. doi: 10.1017/jsc.2017.2
19. Vu T-HT, Groom A, Hart JL, Tran H, Landry R, Ma J, et al. Socioeconomic and demographic status and perceived health risks of E-cigarette product contents among youth: results from a national survey. Health Promotion Pract (2020) 21:148S–56S. doi: 10.1177/1524839919882700
20. Spears CA, Jones DM, Weaver SR, Pechacek T, Eriksen M. Motives and perceptions regarding electronic nicotine delivery systems (ENDS) use among adults with mental health conditions. Addictive Behav (2018) 80:102–9. doi: 10.1016/j.addbeh.2018.01.014
21. Spears CA, Jones DM, Weaver SR, Yang B, Pechacek T, Eriksen M. Use of and perceptions about electronic nicotine delivery systems (ENDS) among people with mental health conditions or serious psychological distress, 2018. Drug Alcohol Depend (2020) 212:108049. doi: 10.1016/j.drugalcdep.2020.108049
22. Lohner V, McNeill A, Schneider S, Vollstädt-Klein S, Andreas M, Szafran D, et al. Understanding perceived addiction to and addictiveness of electronic cigarettes among electronic cigarette users: a cross-sectional analysis of the International Tobacco Control Smoking and Vaping (ITC 4CV) England Survey. Addiction (2023) 118:1359–69. doi: 10.1111/add.16162
23. Selamoglu M, Erbas B, Kasiviswanathan K, Barton C. General practitioners’ knowledge, attitudes, beliefs and practices surrounding the prescription of e-cigarettes for smoking cessation: a mixed-methods systematic review. BMC Public Health (2022) 22:2415. doi: 10.1186/s12889-022-14696-3
24. Droege M, Maniscalco M, Daniel KL, Baldwin H. Consumers’ Risk perceptions of prescription and over-the-counter medications. J Pharm Technol (2007) 23:142–7. doi: 10.1177/875512250702300303
25. SA Health. The South Australian Population Health Survey: Population Health Survey Module System (2024) Adelaide, South Australia: SA Health.
26. Wellbeing SA. Population Health Survey Module System (2023). Available online at: https://www.wellbeingsa.sa.gov.au/evidence-data/about-our-data-collections/population-health-survey-module-system.
27. Australian Bureau of Statistics. Socio-economic Indexes for Areas (SEIFA) (2016). Available online at: https://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001 (Accessed 11 February 2022).
28. Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics (2009) 50:613–21. doi: 10.1016/S0033-3182(09)70864-3
29. R Core Team. R: A language and environment for statistical computing Vienna, Austria: R Foundation for Statistical Computing (2023).
30. Wei T, Simko VR. package ‘corrplot’: visualization of a correlation matrix (version 0.90), Vol. 2021. (2021). Available online at: https://cran.r-project.org/web/packages/corrplot/corrplot.pdf.
31. Revelle W. psych: Procedures for Psychological, Psychometric, and Personality Research (version 2.3.6), Vol. 2023. (2023). Available online at: https://cran.r-project.org/web/packages/psych/psych.pdf.
32. Hebbali A. olsrr: Tools for Building OLS Regression Models (version 0.5.3), Vol. 2020. (2020). Available online at: https://cran.r-project.org/web/packages/olsrr/index.html.
33. Maechler M, Rousseeuw P, Croux C, Todorov V, Ruckstuhl A, Salibian-Barrera M, et al. robustbase: Basic Robust Statistics (version 0.99.0) (2023). Available online at: https://cran.r-project.org/web/packages/robustbase/index.html.
34. R Core Team, contributors worldwide. The R Stats Package (version 4.4.0) (2023). Available online at: https://stat.ethz.ch/R-manual/R-devel/library/stats/html/stats-package.html.
36. Cohen JE, Gartner C, Edwards R, Hammond D. Australia tightens its prescription-only regulation of e-cigarettes. BMJ (2023) 381:1216. doi: 10.1136/bmj.p1216
37. Pettigrew S, Miller M, Alvin Santos J, Raj T, Brown K, Jones A. E-cigarette attitudes and use in a sample of Australians aged 15–30 years. Aust New Z J Public Health (2023) 47:100035. doi: 10.1016/j.anzjph.2023.100035
38. Lawn SJ, Pols RG and Barber JG. Smoking and quitting: a qualitative study with community-living psychiatric clients. Soc Sci Med (2002) 54:93–104. doi: 10.1016/S0277-9536(01)00008-9
39. Baker AL, McCarter K, Turner A, Segan C, Castle D, Brophy L, et al. ‘Quitlink’: Outcomes of a randomised controlled trial of peer researcher facilitated referral to a tailored quitline tobacco treatment for people receiving mental health services. Aust New Z J Psychiatry (2023) 2023:48674231181039. doi: 10.1177/00048674231181039
40. Quit Victoria. Training and resources for mental health services (2023). Available online at: https://www.quit.org.au/training-and-resources-mental-health-services.
41. Steinberg ML, Rosen RL, Ganz O, Wackowski O, Jeong M, Delnevo C, et al. Communicating the benefits of quitting smoking on mental health increases motivation to quit in people with anxiety and/or depression: A randomized trial of two health messages. medRxiv (2023) 21:2023.02.17.23286103. doi: 10.1101/2023.02.17.23286103
42. Wellbeing SA. SA Population Health Survey (2023). Available online at: https://www.wellbeingsa.sa.gov.au/evidence-data/sa-population-health-survey (Accessed 19/01 2023).
Keywords: vaping, smoking, mental health, prescription access, Australia, E-cigarette (e-cig), anxiety, depression
Citation: Trigg J, Calabro R, Anastassiadis P, Bowden J and Bonevski B (2024) Association of anxiety and depression symptoms with perceived health risk of nicotine vaping products for smoking cessation. Front. Psychiatry 15:1277781. doi: 10.3389/fpsyt.2024.1277781
Received: 15 August 2023; Accepted: 05 February 2024;
Published: 29 February 2024.
Edited by:
Anne Eden Evins, Massachusetts General Hospital and Harvard Medical School, United StatesReviewed by:
Robert J. Wellman, UMass Chan Medical School, United StatesHua Yong, Deakin University, Australia
Copyright © 2024 Trigg, Calabro, Anastassiadis, Bowden and Bonevski. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joshua Trigg, am9zaHVhLnRyaWdnQGZsaW5kZXJzLmVkdS5hdQ==
 Joshua Trigg
Joshua Trigg Ryan Calabro2
Ryan Calabro2 Billie Bonevski
Billie Bonevski