- Indoc Research, Toronto, ON, Canada
Anxiety is common in neurodevelopmental disorders (NDD). The parent version of the Spence Children’s Anxiety Scale (SCAS-P) is a widely used measure to assess anxiety across a broad range of childhood populations. However, assessment of the measurement properties of the SCAS-P in NDDs have been limited. The present study aimed to assess the psychometric properties of the SCAS-P in children with attention-deficit/hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) using Rasch Measurement Theory. Data from the Province of Ontario Neurodevelopmental Disorders Network Registry were used in the analysis. Children (ages 6-13 years old) with a primary diagnosis of ADHD (n=146) or ASD (n=104) were administered the SCAS-P. Rasch Measurement Theory was used to assess measurement properties of the SCAS-P, including unidimensionality and item-level fit, category ordering, item targeting, person separation index and reliability and differential item functioning. The SCAS-P fit well to the Rasch model in both ADHD and ASD, including unidimensionality, satisfactory category ordering and goodness-of-fit. However, item-person measures showed poor precision at lower levels of anxiety. Some items showed differential item functioning, including items within the obsessive-compulsive, panic/agoraphobia and physical injury fears domains, suggesting that the presentation of anxiety may differ between ADHD and ASD. Overall, the results generally support the use of the SCAS-P to screen and monitor anxiety symptoms in children with ADHD and ASD. Future studies would benefit from examination of more severely anxious NDD cohort, including those with clinically diagnosed anxiety.
Introduction
Anxiety is a common mental health problem in children with attention-deficit/hyperactivity disorder (ADHD) (1–3) and 40% of children with autism spectrum disorder (ASD) (4, 5). Comorbid anxiety in children with NDDs can cause distress and is associated impaired functioning (6, 7). Accurate assessments of anxiety are therefore needed to identify and monitor symptoms of anxiety in children living with NDDs. However, there are challenges to assessing anxiety in children with NDDs, including overlapping features of NDDs and anxiety that can confound the assessment of anxiety and lead to misinterpretation of anxiety-related signs and symptoms (8, 9). Indeed, there is considerable overlap in diagnostic symptom criteria for ADHD and anxiety, including restlessness and distractibility (8). In ASD, deficits in social interactions and stereotyped, repetitive motor movements too can be misinterpreted as anxiety and vice versa (9). These challenges are particularly difficult given co-occurring intellectual disabilities and language impairments (9).
A number of scales have been developed to assess symptoms of anxiety in children, including the Revised Children’s Anxiety and Depression Scale (10), the Screen for Child Anxiety Related Emotional Disorders (11) and the Spence Children’s Anxiety Scale (SCAS) (12). However, most scales that are used to assess anxiety in NDDs were developed and validated in typically developing children and validation studies in children with NDDs have been limited (9). The SCAS was developed to assess the severity of anxiety symptoms in children that is based on six anxiety disorder dimensions, including generalized anxiety, panic, social phobia, separation anxiety, obsessive compulsive disorder and fear of injuries (12, 13). The SCAS, therefore, can be a useful tool to assess and monitor anxiety in children and has been used across a broad range of childhood populations, including children with NDDs (14). In children with ASD, the SCAS was found to have good psychometric properties (14–17). However, differences in factor structure of the SCAS between anxious children with or without ASD diagnosis have been noted, suggesting presence of ASD-related signs and symptoms may impact the presentation of anxiety (14, 16, 18). The validity of the SCAS in children with ADHD has not been addressed.
Given the high rates of comorbid anxiety and inherent challenges in assessing anxiety in NDD, is important that the psychometric properties of the SCAS be further evaluated in children with NDDs. The objective of this study was to assess the psychometric properties of the parent version of the SCAS (SCAS-P) in children with ADHD and ASD using Rasch Measurement Theory (RMT) (19, 20). RMT considers the probability of an item’s score as a function of both the person’s individual trait level (i.e., level of anxiety) and the item’s difficulty (i.e., level of anxiety that item assesses) (19). In this context, children with higher levels of anxiety have a greater chance of endorsing an anxiety item, and an item that assesses lower levels of anxiety are more likely to be endorsed than items that assess higher levels of anxiety. RMT provides fundamental criteria for objective scale measurement and determines how well the observed data approximates the Rasch measurement model. Items that do not fit the model are indication that they may be measuring more than one construct, thus calling into question the scales construct validity. RMT approach, therefore, can be particularly useful in evaluating the construct validity and generalizability of rating scales in populations that they were not originally developed. We recently used this approach to evaluate depressive symptoms in adults with neurological disorders, where the overlap between symptoms of depression and neurological disorders could potentially confound the assessment of depression (21). The same approach was used in the present study, including Rasch-based criteria to assess item-level goodness of fit, category ordering, item targeting, person separation index and reliability and item bias (differential item functioning) (21–23).
Methods
Study population
The present study used de-identified data from the Province of Ontario Neurodevelopmental Disorders Network (POND) Registry; a multi-centre research network studying the neurobiology of NDDs (24). These data are currently stored in the Brain-CODE Neuroinformatics Platform (25) and were made available for secondary use through a controlled public data release from the Ontario Brain Institute (www.braincode.ca). Data included demographic and SCAS-P assessments for children aged 6-13 years old, with a primary diagnosis of ADHD (n=146) or ASD (n=104), as well as small cohort of typically developing (TD) children (n=13). Please see (20) for POND protocol details.
Assessments
The SCAS-P is a 38-item parent-report measure that assesses the severity of anxiety-related symptoms in children (12, 26). The scale is aligned with symptom domains based on DSM-IV criteria for anxiety disorder, including separation anxiety (6 items), social phobia (6 items), obsessive-compulsive (6 items), panic (6 items)/agoraphobia (3 items), physical injury fears (5 items) and generalized anxiety (6 items). Items are scored on a 4-point scale: 0 = never, 1 = sometimes, 2 = often and 3 = always; a total score is calculated (maximum = 114), as well as for each of the six domains/subscales, with higher scores indicating greater severity of anxiety symptoms.
Analyses
Demographic and clinical characteristics were calculated and compared across cohorts; ANOVA was used for comparison of continuous variables (age) and chi-squared for comparison of categorical variables (sex). Analyses were performed using SPSS V27. A level of p < 0.05 was regarded as statistically significant. RMT was used to assess performance of the SCAS-P in NDD. Rasch analyses were carried out using WinSteps Version 5.1.
Unidimensionality was examined by principal component analysis of the residuals derived from the Rasch model. The scale was considered unidimensional if > 40% of variance was explained by the measurement variable and unexplained variance of the first contrast accounts for < 10 % (27–29).
Item-level goodness of fit statistics were calculated as an index of how much the observed score for a given item within the scale deviates from the expected score of the Rasch model. Items that did not fit the Rasch model (misfits) do not contribute to measurement of the underlying construct and likely add unwanted noise to the scale. Item “infit” mean square (MNSQ) values provide a fit index for each item that are in close proximity to the person’s severity level, and “outfit” MNSQ values for differences between observed and expected values for items that are far from the person’s severity level. MNSQ values between 0.5 and 1.5 were considered to be acceptable fit, with values between 1.5 and 2 considered to underfit the model, but do not distort the results, and values greater than 2.0 flagged as misfits that can distort the scale (30).
Category threshold ordering determined whether participants can discriminate between the ordered response options (i.e., never, sometimes, often, always) with fit values between 0.5 and 1.5 considered to be acceptable fit, and values greater than 2.0 flagged as misfitting (30).
Person-item maps plot individual participants and items on a single continuum to compare the range and position of the person measure distribution to that of the item measure distribution. Both item “difficulty” (i.e., the level of anxiety that item assesses) and person “ability” (i.e., level of symptom severity) are visualized together on a logit scale (i.e., log of the odds); with the right side of the map displaying the items from most difficult (top) to least difficult (bottom) and the left side plotting the individual participants, with those at the top having the highest trait level (symptom severity) and those at the bottom the least. The targeting of the scale is assessed by comparing mean person and mean item logit locations, with good measurement targeting evidenced when mean persons and items that are in close proximity to one another (within 1 logit) (31, 32). The clinical utility of summing individual items from a scale to form a total score of overall severity requires that the items be spread out across the severity level of a broad range of persons. Gaps between items impact the scale’s sensitivity, as persons falling within those gaps cannot be differentiated from one another.
To assess potential item biases, differential item functioning (DIF) was used to determine whether items show differences in item difficulty between groups (i.e., whether subgroups with similar levels of anxiety have the same probability of endorsing a given item). In the present study, DIF are indications that the expression of anxiety may differ between subgroups. The existence of DIF was assessed by cohort (ADHD vs ASD) and sex (male vs female), with mean differences in person measures > 0.64 logits (with p<0.05 in Rasch-Welch test statistic) as indications of significant and meaningful DIF (31, 32).
Reliability of the SCAS-P was evaluated using item and person separation indices and reliability derived from the Rasch model (30). The person separation index provides an estimate of spread of participants that reflect the number of distinct levels of severity that can be distinguished (strata), with person separation indices of > 1.5 considered acceptable(minimum required to divide sample into two distinct strata). Person reliability is analogous to Cronbach’s alpha as a measure of internal constancy, with values of >0.70 as indication of acceptable internal consistency. That is, confirmation that a person with higher levels of the underlying trait do indeed score higher on the scale than those with lower levels of the underlying trait, and vice versa. The item separation index was used to confirm hierarchy of items, with item separation indices of > 2 and reliability >0.8 considered acceptable to support the scales construct validity (30).
Results
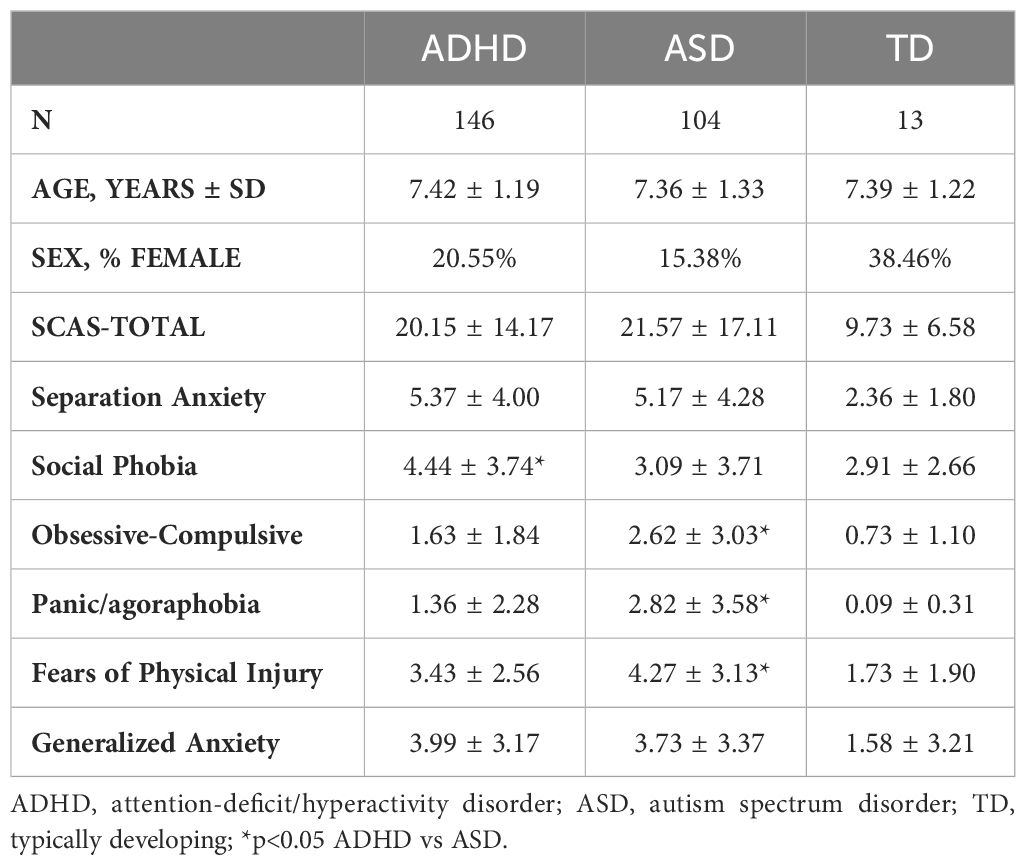
Demographic and clinical characteristics are shown in Table 1. The ADHD and ASD cohorts were predominately male (79.45 and 84.62%, respectively) and that is consistent with the higher rates reported by males (33, 34). The ADHD cohort reported greater social phobia than ASD, whereas the ASD cohort reported greater obsessive-compulsive behaviors, panic/agoraphobia and fears of physical injury than the ADHD cohort (see Table 1). SCAS-P total scores did not differ between NDD cohorts. Demographic and clinical characteristics for the TD cohort are also shown in Table 1 for comparison (statistical comparisons to the TD cohort were not reported given the small sample size).
Principal component analysis of the residuals revealed unidimensionality of the SCAS-P that supported a single dominant factor (29, 30), with variances explained by the measurement variables of 48.6% and 40.7% and unexplained variance of the first residual of 4.3% and 5.9% in ADHD and ASD cohorts, respectively.
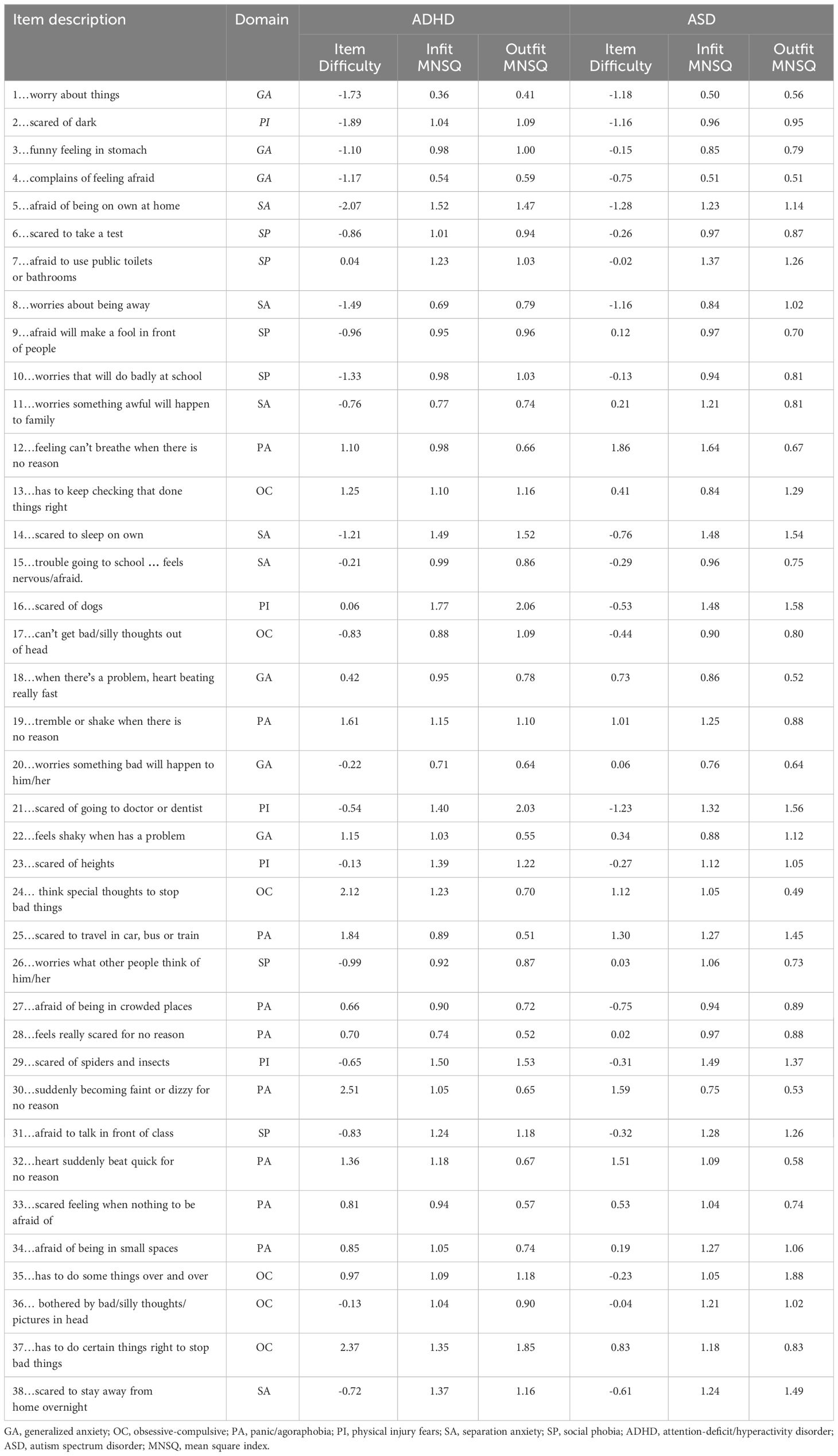
Item difficulty estimates and fit statistics are shown in Table 2. In both cohorts, Item 5 (“My child would feel afraid of being on his/her own at home”) was the least difficult/most endorsed item (ADHD: -2.07 logits; ASD: -1.63 logits) and item 30 (“My child suddenly becoming faint or dizzy for no reason”) the most difficult/least endorsed item (ADHD: 2.51 logits; ASD: 1.99 logits). Most items showed acceptable goodness-of-fit statistics, although some underfitting was noted (MNSQs >1.5, see Table 2). In particular, item 16 (“My child is scared of dogs”) was identified as a possible misfit item in the ADHD cohort with infit MNSQ = 1.77 and outfit MNSQ = 2.06, thus questioning the construct validity of this item as a measure of anxiety. This is not surprising given the potential positive impact child-dog interactions can have on wellbeing and can serve as a source of reduced stress (35).
The category thresholds were ordered indicating that the SCAS-P scale options functioned in sequential order in capturing increases levels of severity, with children with higher levels of anxiety endorsing higher SCAS-P options. Average measures increased in scale categories from -2.74 logits (“never”) to 0.08 logits (“always”) in the ADHD cohort and from -2.33 logits (“never”) to 0.42 logits (“always”) in the ASD cohort. All infit/outfit MNSQ were acceptable (MNSQ < 1.5).
Person-item locations (Wright maps) for the SCAS are shown in Figure 1. The mean person measures were -2.00 and -1.71 logits in ADHD and ASD cohorts, respectively. Therefore, although the SCAS had a wide range of items and no large gaps were noted between items, no items targeted children with anxiety levels below -2.07 logits in ADHD and -1.63 logits in ASD (see Figure 1, Table 2).
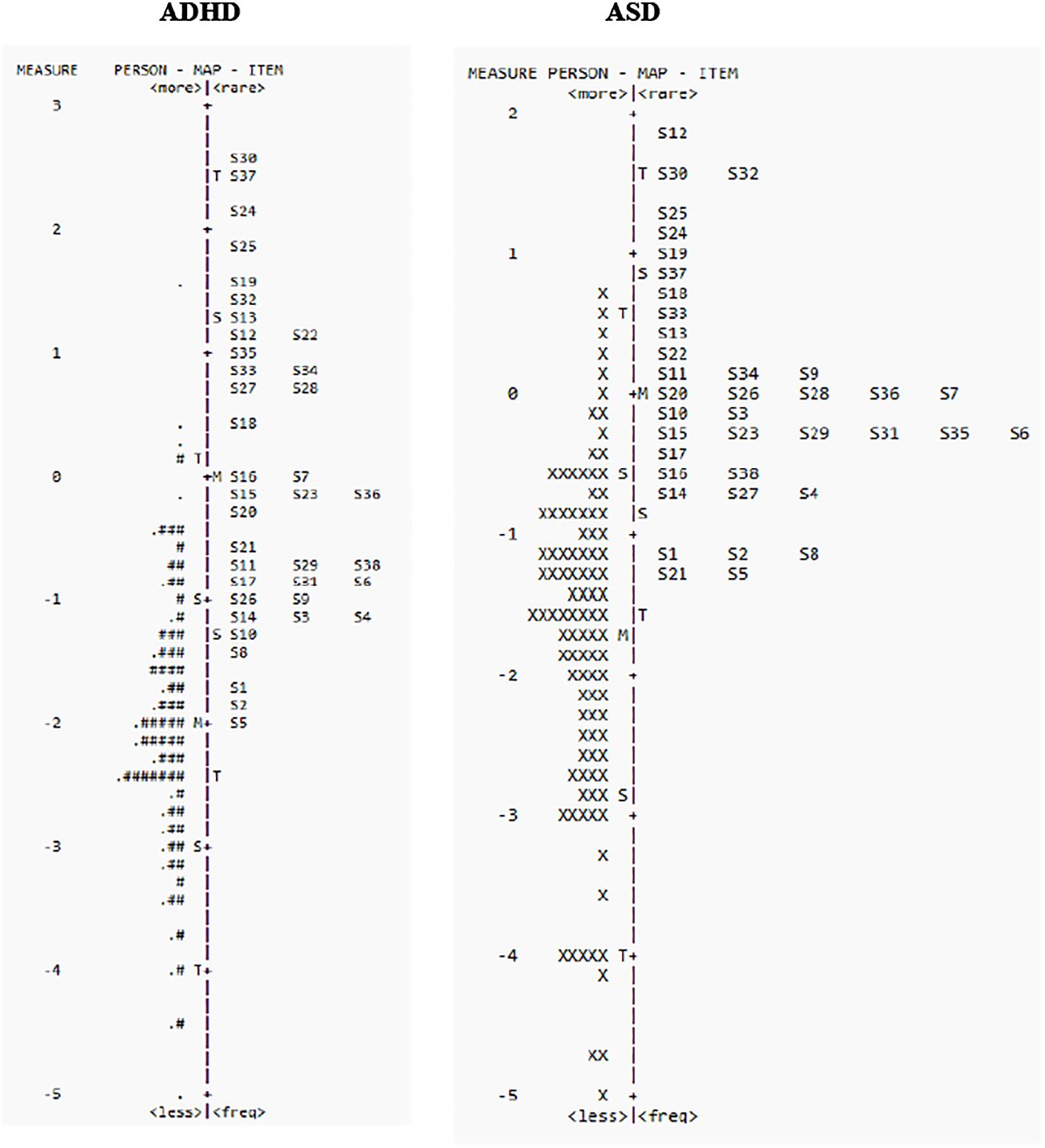
Figure 1 Person-item location (Wright maps) for SCAS-P items in ADHD (left panel) and ASD (right panel). The right side of the map displays the items from most difficult (top) to least difficult (bottom), and the left side plots the individual participants, with those at the top having the highest trait level (depression) and those that the bottom the least. M, mean difficulty; S, one standard deviation; T, two standard deviations.
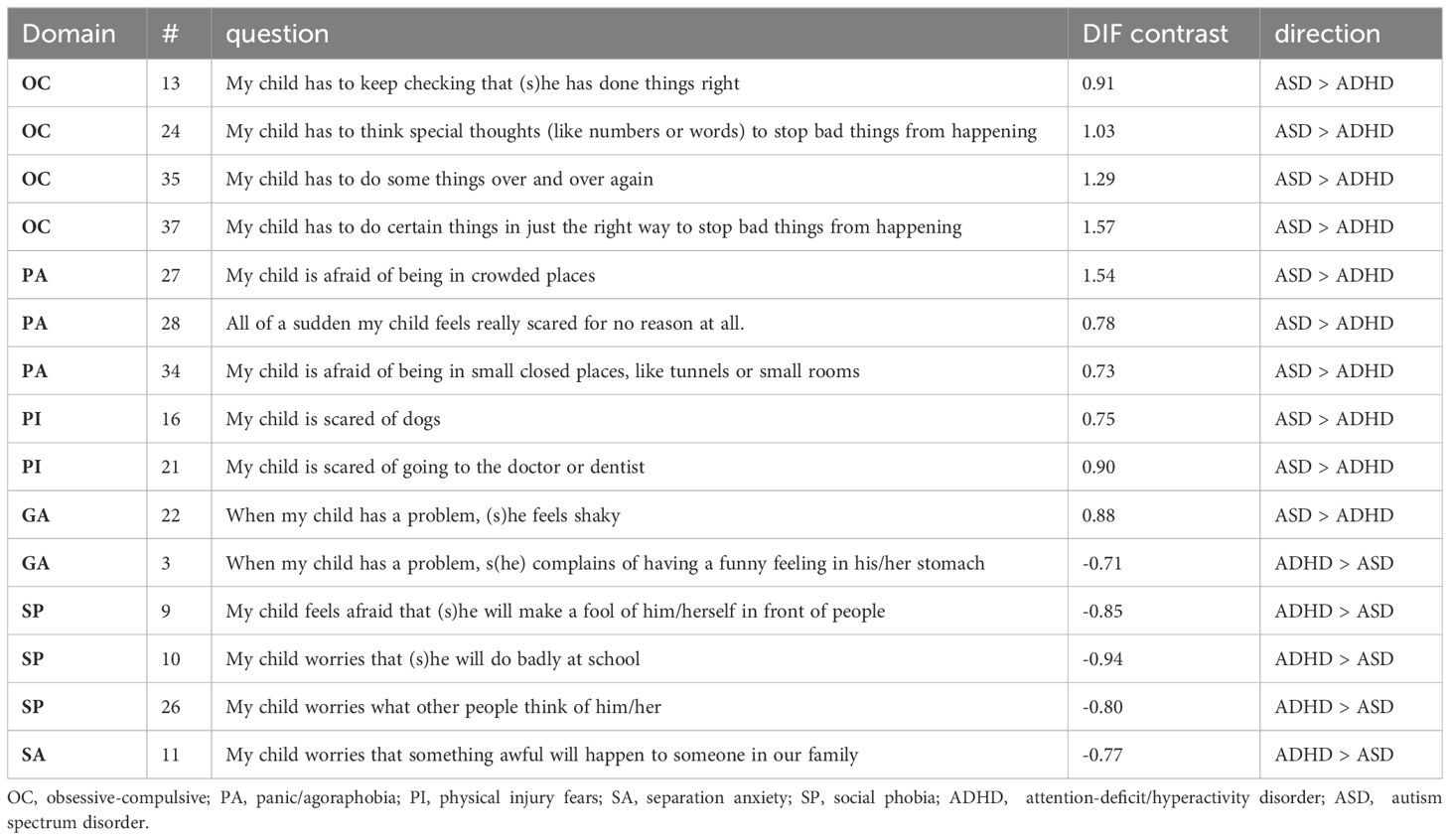
Meaningful DIF (>0.64 logits) between ASD and ADHD was noted for 15 of the 39 items, including multiple items within the “obsessive-compulsive,” “panic-agoraphobia” and “physical injury fears” domains more likely to be endorsed in the ASD than the ADHD cohort, and items within the “social phobia” domain more likely to be endorsed in the ADHD than the ASD cohort (Table 3). No DIF was noted based on sex.
Person separation indices and reliability were acceptable in both cohorts, indicating the SCAS-P could stratify NDD participants into at least 3 separate groups, with person separation indices and reliability of 2.83 and 0.89 in the ADHD cohort, respectively and 2.73 and 0.88 in the ASD cohort, respectively. Internal consistency was also good, with Cronbach’s alpha of 0.97 (ADHD) and 0.94 (ASD), consistent with previous reports in ASD of 0.94 (15). The scales construct validity and hierarchy of items was also supported, with acceptable item separation indices and reliability of 6.07 and 0.97 for ADHD and 4.08 and 0.94 for ASD, respectively.
Discussion
The present study used RMT to evaluate the psychometric properties of the SCAS-P in children with ADHD and ASD. The results generally support the use of the SCAS-P to assess anxiety in children with ADHD and ASD, including unidimensionality and acceptable item-level goodness-of-fit statistics, suggesting that all items contributed to the same underlying construct. However, item difficulty estimates and person-item maps showed poor item targeting at lower levels anxiety (see Figure 1). This is not surprising as POND participants were recruited based on primary NDD diagnosis and not presence (or absence) of comorbid anxiety (24). None-the-less, person separation indices and reliability indicated that in the present cohort the SCAS-P can effectively discriminate different levels of anxiety and can therefore be a useful tool screen and monitor anxiety in children with NDDs.
The present study also compared the presentation of anxiety-related symptoms between ADHD and ASD cohorts. DIF revealed that children with ASD were more likely to endorse anxiety symptoms related to OC behaviours, panic/agoraphobia and physical fear-related behaviours, than the ADHD cohort (see Table 3). These results are consistent with those reported by Toscano et al. (18) that children with ASD and comorbid anxiety show higher levels of anxiety related to fears of physical injuries and OC behaviours, as compared to children with anxiety without an ASD diagnosis. On the other hand, DIF revealed that children in the ADHD cohort were more likely to endorse anxiety related to social phobias, than the ASD cohort, including afraid that (s)he will make a fool of him/herself in front of people (item 9), worries that (s)he will do badly at school (item 10) and worries what other people think of him/her (item 26). Indeed, previous studies have demonstrated that anxiety in children with ADHD is associated with poorer social functioning (36). Taken together, these results suggest the expression of anxiety may be different across NDDs and should be considered in the assessment of anxiety-related behaviours.
Interestingly, DIF revealed that within the OC domain, children with ASD were more likely to express compulsive-like thoughts/behaviours, including checking that (s)he has done things right (item 13), think special thoughts to stop bad things from happening (item 24), do things over and over again (item 35) and do certain things in just the right way to stop bad things from happening (item 37), whereas the cohorts did not differ in obsessive-like thoughts, such as bad/silly thoughts in head (items 17 and 36). As obsessions are intrusive, recurring thoughts that cause anxiety and distress, compulsions are in response to these intrusive thoughts that are meant to control anxiety (13). This is consistent with the compulsive behaviors in ASD as being a way of reducing anxiety and managing intrusive thoughts and overwhelming sensory inputs (37). However, although compulsions in OCD are unwanted and distressing, compulsive behaviours in ASD can provide comfort (38). Furthermore, the similarity between ASD-related repetitive behaviours and OCD-related behaviours can make it difficult to differentiate their underlying motivation (37, 38). This should be considered in the assessment of OC behaviours in ASD, as obsessions and compulsions in ASD may have different dynamics than OCD that can lead to misinterpretation of OC features in ASD.
It is important to note that in the present study only the parent version of the SCAS was used. Although previous studies have demonstrated generally good concordance between parent and child versions of the SCAS in typically developing children (26, 39), concordance is reduced in children with ASD (36). Given the intellectual and verbal challenges in children with ASD and other NDDs, it is possible that reduced parent-child concordance is related to the child’s difficulty in communicating anxiety-related thoughts and feelings (39). Indeed, child’s verbal ability is associated with greater parent-child concordance, suggesting that better verbal skills facilitate communication of anxiety-related feelings and reduce ambiguity between anxiety and NDD-related signs and symptoms (39, 40). Moreover, parent-child concordance is higher for observable symptoms, such as separation anxiety, as compared to internalized symptoms, such as generalized anxiety (39, 40). It is possible therefore that compulsive behaviours in ASD are more easily recognized by the parent, than internal obsessive thoughts. In the present study this may have led to a bias towards observable behaviours and underrepresentation of internalized symptoms of anxiety. Assessment of anxiety in children with NDDs based on the SCAS-P therefore should be interpreted with caution, as it relies on interpretation of a child’s behaviour and recognition of internalized symptoms of anxiety. Furthermore, as the SCAS-P is based on the parent’s own conceptualizations of anxiety and interpretation of symptoms, it is important that other sources of information also be considered. To get a more complete picture, assessment of anxiety in children with NDDs would benefit from inclusion of multi-informant information (9, 40).
The POND Network is part of the Ontario Brain Institute’s Integrated Discovery programs (41). These programs generate diverse data types that are integrated within the Brain-CODE platform to support cross-disease comparisons (25). In particular, the establishment of common data elements provides consistency in data collection and optimizes pooling of data and cross-disorder comparisons (42). In the present study, demographic information and SCAS-P were collected consistently across cohorts, thus allowing us to pool and compare ADHD and ASD cohorts. Overall, the present study supports the SCAS-P as a valid instrument to screen and monitor anxiety-related symptoms in children with ADHD and ASD, including children without formally diagnosed anxiety disorders. As a screening tool for comorbid anxiety disorders in children with NDDs, therefore, the SCAS-P can provide important information about the presence of anxiety-related symptoms that may warrant clinical follow-up (9). However, there still remains inherent challenges to assessing anxiety in children with NDDs, including communication difficulties, overlapping features of anxiety and NDD, as well as potential differences in the presentation of anxiety across NDDs (6, 8, 9). These factors will add unwanted noise the measurement tool and reduce its sensitivity to screen and monitor for anxiety.
Limitations and future directions
As the present study involved secondary use of data, some limitations were noted. SCAS-P items were found to target more severe anxiety than experienced in the present NDD cohorts, which was not surprising as comorbid anxiety was not considered a selection criterion for participation in POND (24). The performance of the SCAS-P in more severely anxious cohorts would require additional studies, including examination in those with clinically diagnosed anxiety. Furthermore, although previous studies have shown that anxiety is a common mental health issue in children with NDDs (1–5), the relatively small sample size of the typically developing children limited comparisons with the ASD and ADHD cohorts. Larger sample size of typically developing children would be needed to support any statistical inferences with respect to the higher levels of anxiety in children with NDDs observed this study.
The present study shows that the SCAS-P can be a valuable tool to assess and monitor anxiety in children with NDD and has implications regarding presentation of anxiety-related symptoms across NDDs and challenges in assessing these symptoms, including confounding NDD-related symptoms, and language and intellectual challenges. Future research should address these challenges, including the modification of existing scales or development of new fit-for-purpose anxiety measures designed specifically for children with NDDs (9). This, of course, will require a better understanding of anxiety-related behaviours in children with NDDs and challenges in assessing those behaviours.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: Participants’ data used in this study are currently stored in the Brain-CODE Neuroinformatics Platform (https://www.braincode.ca/) managed by the Ontario Brain Institute. Requests to access these datasets should be directed to Ontario Brain Institute ataW5mb0BicmFpbmluc3RpdHV0ZS5jYQ==.
Ethics statement
The studies involving humans were approved by Canadian SHIELD Ethics Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
AV and AS: study design and analysis, SE, MJ, BL, EM, AS, RV: data management and curation. AV, AS, IV: manuscript preparation. All authors contributed to the article and approved the submitted version.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We would like to acknowledge the individuals and organizations that have made Data used for this research available including the Province of Ontario Neurodevelopmental Network, the Ontario Brain Institute, the Brain-CODE platform, the Government of Ontario, as well as Autism Speaks, Autism Ontario, Circle 21, Community Living Toronto, Ontario Rett Syndrome Association, Totally ADD, and Sick Kids Down Syndrome Clinic. Thanks also to Dr Joseph Fernando for helpful discussions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jarrett MA, Ollendick TH. A conceptual review of the comorbidity of attention-deficit/hyperactivity disorder and anxiety: implications for future research and practice. Clin Psychol Rev. (2008) 28:1266–80. doi: 10.1016/j.cpr.2008.05.004
2. Overgaard KR, Aase H, Torgersen S, Zeiner P. Co-occurrence of ADHD and anxiety in preschool children. J Atten Disord. (2016) 20:573–80. doi: 10.1177/1087054712463063
3. Souza I, Pinheiro MA, Mattos P. Anxiety disorders in an attention-deficit/hyperactivity disorder clinical sample. Arq Neuropsiquiatr. (2005) 63:407–9. doi: 10.1590/s0004-282x2005000300008
4. Mattila ML, Hurtig T, Haapsamo H, Jussila K, Kuusikko-Gauffin S, Kielinen M, et al. Comorbid psychiatric disorders associated with Asperger syndrome/high-functioning autism: a community- and clinic-based study. J Autism Dev Disord. (2010) 40:1080–93. doi: 10.1007/s10803-010-0958-2
5. van Steensel FJ, Bögels SM, de Bruin EI. Psychiatric comorbidity in children with autism spectrum disorders: A comparison with children with ADHD. J Child Fam Stud. (2013) 22:368–76. doi: 10.1007/s10826-012-9587-z
6. Ozsivadjian A, Knott F, Magiati I. Parent and child perspectives on the nature of anxiety in children and young people with autism spectrum disorders: a focus group study. Autism. (2012) 6:107–21. doi: 10.1177/1362361311431703
7. White SW, Oswald D, Ollendick T, Scahill L. Anxiety in children and adolescents with autism spectrum disorders. Clin Psychol Rev. (2009) 29:216–29. doi: 10.1016/j.cpr.2009.01.003
8. Koyuncu A, Ayan T, Ince Guliyev E, Erbilgin S, Deveci E. ADHD and anxiety disorder comorbidity in children and adults: diagnostic and therapeutic challenges. Curr Psychiatry Rep. (2022) 24:129–40. doi: 10.1007/s11920-022-01324-5
9. Mingins JE, Tarver J, Waite J, Jones C, Surtees AD. Anxiety and intellectual functioning in autistic children: A systematic review and meta-analysis. Autism. (2021) 25:18–32. doi: 10.1177/1362361320953253
10. Chorpita BF, Yim L, Moffitt C, Umemoto LA, Francis SE. Assessment of symptoms of DSM-IV anxiety and depression in children: A revised child anxiety and depression scale. Behav Res Ther. (2000) 38:835–55. doi: 10.1016/S0005-7967(99)00130-8
11. Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, et al. The Screen for Child Anxiety Related Emotional Disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry. (1997) 36:545–53. doi: 10.1097/00004583-199704000-00018
12. Spence SH. A measure of anxiety symptoms among children. Behav Res Ther. (1998) 36:545–66. doi: 10.1016/S0005-7967(98)00034-5
13. American Psychiatric Association, DSM-5 Task Force. Diagnostic and statistical manual of mental disorders: DSM-5™ (5th ed.). American Psychiatric Publishing, Inc. (2013). doi: 10.1176/appi.books.9780890425596
14. Jitlina K, Zumbo B, Mirenda P, Ford L, Bennett T, Georgiades S, et al. Psychometric properties of the spence children's anxiety scale: parent report in children with autism spectrum disorder. J Autism Dev Disord. (2017) 47:3847–56. doi: 10.1007/s10803-017-3110-8
15. Carruthers S, Kent R, Hollocks MJ, Simonoff E. Brief report: testing the psychometric properties of the spence children's anxiety scale (SCAS) and the screen for child anxiety related emotional disorders (SCARED) in autism spectrum disorder. J Autism Dev Disord. (2020) 50:2625–32. doi: 10.1007/s10803-018-3774-8
16. Magiati I, Lerh JW, Hollocks MJ, Uljarevic M, Rodgers J, McConachie H, et al. The measurement properties of the spence children's anxiety scale-parent version in a large international pooled sample of young people with autism spectrum disorder. Autism Res. (2017) 10:1629–52. doi: 10.1002/aur.1809
17. Zainal H, Magiati I, Tan JW, Sung M, Fung DS, Howlin P. A preliminary investigation of the Spence Children's Anxiety Parent Scale as a screening tool for anxiety in young people with autism spectrum disorders. J Autism Dev Disord. (2014) 44:1982–94. doi: 10.1007/s10803-014-2075-0
18. Toscano R, Baillie AJ, Lyneham HJ, Kelly A, Kidd T, Hudson JL. Assessment of anxiety in children and adolescents: A comparative study on the validity and reliability of the Spence Children's Anxiety Scale in children and adolescents with anxiety and Autism Spectrum Disorder. J Affect Disord. (2020) 260:569–76. doi: 10.1016/j.jad.2019.09.055
19. Andrich D. Rating scales and Rasch measurement. Expert Rev Pharmacoecon Outcomes Res. (2011) 11:571–85. doi: 10.1586/erp.11.59
20. Petrillo J, Cano SJ, McLeod LD. Using classical test theory, item response theory, and Rasch measurement theory to evaluate patient-reported outcome measures: a comparison of worked examples. Value Health. (2015) 18:25–34. doi: 10.1016/j.jval.2014.10.005
21. Vaccarino L, Black SE, Gilbert SE, Frey BN, Javadi M, Kennedy SH, et al. Rasch analyses of the Quick Inventory of Depressive Symptomatology Self-Report in neurodegenerative and major depressive disorders. Front Psychiatry. (2023) 14:1154519. doi: 10.3389/fpsyt.2023.1154519
22. Boone WJ. Rasch analysis for instrument development: why, when, and how? CBE life. Sci Educ. (2016) 15:rm4. doi: 10.1187/cbe.16-04-0148
23. Uygur OF, Ahmed O, Bahar A, Hursitoglu O, Aydın EF, Chung S, et al. Adaptation and validation of the turkish version of the ford insomnia response to stress test in university students. Nat Sci sleep. (2023) 15:139–49. doi: 10.2147/NSS.S398489
24. Baribeau DA, Dupuis A, Paton TA, Hammill C, Scherer SW, Schachar RJ, et al. Structural neuroimaging correlates of social deficits are similar in autism spectrum disorder and attention-deficit/hyperactivity disorder: analysis from the POND Network. Transl Psychiatry. (2019) 9:72. doi: 10.1038/s41398-019-0382-0
25. Vaccarino AL, Dharsee M, Strother S, Aldridge D, Arnott SR, Behan B, et al. Brain-CODE: a secure neuroinformatics platform for management, federation, sharing and analysis of multi-dimensional neuroscience data. Front Neuroinform. (2018) 12:28. doi: 10.3389/fninf.2018.00028
26. Nauta MH, Scholing A, Rapee RM, Abbott M, Spence SH, Waters A. A parent-report measure of children's anxiety: psychometric properties and comparison with child-report in a clinic and normal sample. Behav Res Ther. (2004) 42:813–39. doi: 10.1016/S0005-7967(03)00200-6
27. Mallinson T, Kozlowski AJ, Johnston MV, Weaver J, Terhorst L, Grampurohit N, et al. Rasch reporting guideline for rehabilitation research (RULER): the RULER statement. Arch Phys Med Rehabil. (2022) 103:1477–86. doi: 10.1016/j.apmr.2022.03.013
28. Kim S, Ouellet LJ, Mazza J, Spaulding AC. Rasch analysis and differential item functioning of a social support measure in jail inmates with HIV infection. Eval Health Prof. (2016) 40:33–60. doi: 10.1177/0163278716644954
29. Reckase MD. Unifactor latent trait models applied to multifactor tests: results and implications. J Educ Stat. (1979) 4:207–30. doi: 10.3102/10769986004003207
31. Boone W, Staver JR, Yale MS. Rasch analysis in the human sciences. Kindle, editor. Berlin: Springer (2014). doi: 10.1007/978-94-007-6857-4
32. Jiraniramai S, Wongpakaran T, Angkurawaranon C, Jiraporncharoen W, Wongpakaran N. Construct validity and differential item functioning of the PHQ-9 among health care workers: Rasch analysis approach. Neuropsychiatr Dis Treat. (2021) 17:1035–45. doi: 10.2147/NDT.S271987
33. Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA. The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry. (2007) 164:942–8. doi: 10.1176/ajp.2007.164.6.942
34. Werling DM, Geschwind DH. Sex differences in autism spectrum disorders. Curr Opin Neurol. (2013) 26:146–53. doi: 10.1097/WCO.0b013e32835ee548
35. Giraudet CSE, Liu K, McElligott AG, Cobb M. Are children and dogs best friends? A scoping review to explore the positive and negative effects of child-dog interactions. PeerJ. (2022) 1910:e14532. doi: 10.7717/peerj.14532
36. D'Agati E, Curatolo P, Mazzone L. Comorbidity between ADHD and anxiety disorders across the lifespan. Int J Psychiatry Clin Pract. (2019) 23:238–44. doi: 10.1080/13651501.2019.1628277
37. Pazuniak M, Pekrul SR. Obsessive-compulsive disorder in autism spectrum disorder across the lifespan. Child Adolesc Psychiatr Clin N Am. (2020) 29:419–32. doi: 10.1016/j.chc.2019.12.003
38. Postorino V, Kerns CM, Vivanti G, Bradshaw J, Siracusano M, Mazzone L. Anxiety disorders and obsessive-compulsive disorder in individuals with autism spectrum disorder. Curr Psychiatry Rep. (2017) 19:92. doi: 10.1007/s11920-017-0846-y
39. May T, Cornish K, Rinehart NJ. Parent-child agreement using the spence children's anxiety scale and a thermometer in children with autism spectrum disorder. Autism Res Treat. (2015) 1:1–9. doi: 10.1155/2015/315495
40. Ooi YP, Weng SJ, Magiati I, Ang RP, Goh TJ, Fun DS, et al. Factors influencing agreement between parent and child reports of anxiety symptoms among children with high-functioning autism spectrum disorders. J Dev Phys Disabil. (2016) 28:407–24. doi: 10.1007/s10882-016-9481-5
41. Stuss DT. From silos to systems: an integrated approach to neuroscience innovation. Nat Rev Drug Discovery. (2015) 14:295–6. doi: 10.1038/nrd4615
Keywords: ADHD (attention-deficit/hyperactivity disorder), autism spectrum disorder, anxiety, Rasch analyses, validity, rating scale, neurodevelopmental disorders
Citation: Sparks A, Gilbert Evans S, Javadi M, Lasalandra B, Martens E, Venkatesh R, Vaccarino IT and Vaccarino AL (2024) Assessment of anxiety in children with neurodevelopment disorders: Rasch analysis of the Spence Children’s Anxiety Scale. Front. Psychiatry 15:1240357. doi: 10.3389/fpsyt.2024.1240357
Received: 14 June 2023; Accepted: 10 April 2024;
Published: 29 April 2024.
Edited by:
Leandro Fernandes Malloy-Diniz, Federal University of Minas Gerais, BrazilReviewed by:
Ayşe Kılınçaslan, Independent researcher, Istanbul, TürkiyeÖmer Faruk Uygur, Atatürk University, Türkiye
Celeste-Marie Combrinck, University of Pretoria, South Africa
Copyright © 2024 Sparks, Gilbert Evans, Javadi, Lasalandra, Martens, Venkatesh, Vaccarino and Vaccarino. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Anthony L. Vaccarino, YXZhY2Nhcmlub0BpbmRvY3Jlc2VhcmNoLm9yZw==
†Present address: Izzy T. Vaccarino, Steve Hicks School of Social Work, University of Texas at Austin, TX, United States
 Alana Sparks
Alana Sparks Susan Gilbert Evans
Susan Gilbert Evans Mojib Javadi
Mojib Javadi Bianca Lasalandra
Bianca Lasalandra Emily Martens
Emily Martens Anthony L. Vaccarino
Anthony L. Vaccarino