
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 25 April 2024
Sec. Social Psychiatry and Psychiatric Rehabilitation
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1229380
This article is part of the Research Topic Insights in Social Psychiatry and Psychiatric Rehabilitation: 2023 View all 8 articles
Background: Behavioral activation (BA) and cognitive-behavioral therapy (CBT) have shown to be efficacious treatment methods for depression. Previous studies focused mostly on the outpatient treatment either in group or individual setting. The present study aimed at comparing the efficacy of group treatment BA vs. CBT, when embedded in inpatient psychosomatic rehabilitation treatment.
Methods: 375 inpatients were randomly assigned to either BA (N = 174) or CBT (N = 201). We used established scales for depression such as the Beck Depression Inventory II (BDI-II, self-rating), the Quick Inventory of Depressive Symptomatology (QIDS; expert rating) and the Behavioral Activation for Depression Scale (BADS) to assess changes over the course of the treatment and at follow-up (4 to 6 months). In addition, we measured disability-related functioning with the Mini-ICF-APP, a rating scale built in reference to the International Classification of Functioning, Disability and Health (ICF). Multilevel models with repeated measures were conducted to examine the differences between groups in relation to change over time with patients’ random effects.
Results: Both group formats showed substantial reduction in depressive symptoms at the end of treatment (d= 0.83 BA vs. d= 1.08 CBT; BDI-II) and at follow-up after 4 to 6 months (d = 0.97 BA vs. d = 1.33 CBT, BDI-II; and d = 1.17 BA vs. d = 1.09 CBT, QIDS). There were no significant differences between treatment approaches. At least 50% symptom reduction was achieved by 53.7% and 54.2% in BA vs. CBT respectively. Reported activation levels increased from pre- to posttreatment (d = 0.76 BA vs. d = 0.70CBT), while showing loss of increment between the end of the treatment until follow up in both formats (d = 0.28 BA vs. d = 0.29 CBT).
Discussion: Both modalities led to significant improvement of symptomatology and functioning at the end of the treatment and at follow-up, thus for the first time demonstrating the practicability of BA in rehabilitation clinics. Considering its lower requirements regarding cognitive abilities and its easier implementation, BA proved to be a good alternative to other psychotherapeutic treatments.
Affective disorders are one of the three leading non-fatal health burdens across the globe (1). They are not only common and costly (e.g.; due to premature retirement), but also associated with considerable morbidity and mortality. As effective treatments are available (2) it is primarily the implementation of effective as well as efficient treatment methods for these disorders which poses a major challenge for service provision worldwide. Accordingly, there are continuing efforts to disseminate efficacious treatments into the diverse segments of health services. Furthermore, considering patient preferences it is important to make different types of efficacious treatments available to establish a more precise matching between individual patients and individual psychotherapies (3).
Psychotherapy has been found to be at least as efficacious as pharmacotherapy in mild to moderate depression (4) and many psychotherapeutic interventions could demonstrate their long-term efficacy (3). Two types of psychotherapy are exceptionally well-researched and have proven their efficacy based on many randomized and controlled studies: cognitive-behavioral therapy (CBT) and behavioral activation (BA). Despite their demonstrated and comparable efficacy (5) one advantage of BA might be that it is easier to understand (for patients) and, hence, to implement (into service structures): Cognitive-behavioral therapy for depression includes different components focusing both on behavioral as well as cognitive change, which at least some patients may find complex and time-consuming (6). Particularly its cognitive components can be more difficult to understand for marginalized populations (e.g., due to language, cognitive or economical barriers). On the other hand, there is strong evidence that a simple behavioral approach, behavioral activation (BA), is easy to administer (e.g., 7) and efficacious within many diverse patient populations (e.g., 8–10). Dimidjan et al. (11) showed in an RCT a significant amount of extreme non-responders in the CBT study arm but not in the BA. Furthermore, Jahoda et al. (12) conducted a RCT with intellectual disabilities who showed a substantial decline in depressive symptoms after BA treatment. The main focus of BA lies on activity monitoring and activity planning (13), which both aim at directly counteracting depressogenic factors such as lack of reinforcement, extinction of instrumental behavior, and excesses of aversive control. Recent research has shown that brief activity planning instructions alone can have relevant effects for emotion regulation and prevention (14). Given the clear focus and the relative simplicity of BA, we assume that it can be a viable alternative to CBT in many settings, especially when large groups of patients need to be treated in relatively condensed ways, as is the case in inpatient psychosomatic rehabilitative treatment (15).
The positive effects of CBT and BA mentioned above seem to be observable across different modalities such as individual vs. group treatment (16, 17). Group psychotherapy in particular constitutes a competing alternative to individual psychotherapy as it makes psychotherapy accessible for many patients and is clearly more economical (18). Furthermore, it is the most viable form of psychotherapy in inpatient settings, and in countries such as the UK, the USA, and Germany, group psychotherapy is the most prevalent modality of inpatient psychological care (19–21).However, as countries such as the USA are following the trend of outsourcing psychological treatment away from psychiatric wards, there is less data on inpatient than on outpatient treatment (22). This is a shortcoming of high clinical relevance, as it has been shown that inpatients do not represent the same target population as outpatients as they demonstrate more severe symptomatology, are often chronically ill, and diagnosed with higher number of comorbidities (22).Hence, the effects observed in outpatient settings may or may not be valid in inpatient contexts as well. The need of independent research on that subject, especially regarding group therapy, is obvious.
Another research requirement is the more thorough study not just of patients’ symptom reduction but also of their improvement in quality of life, functioning and participation within society (23). In order to do so, clinical research as well as clinical decision-making regarding mental health disorders must consider level and pattern of functioning (24). As a system for providing data on disability-related functioning and non-fatal health outcomes, the World Health Organization (WHO) proposed the International Classification of Functioning, Disability and Health (ICF, 25). ICF acts complementary to ICD (see ICF, 2001) and will be consistently applied in this study. The terms ICF, functioning, and disability-related functioning and non-fatal health outcomes will be used interchangeably.
Summarizing, the aim of the present study was to compare BA to cognitive-behavioral therapy, embedded in a group inpatient treatment of depressed patients with a high number of comorbidities. Firstly, we expect patients in both treatment modalities to reduce depressive symptoms with BA exhibiting a significantly larger reduction. Furthermore, we expect patients with lower education level to show steeper decline than those with higher one. Secondly, we expect both groups BA and CBT to increase in activation, especially patients with lower education level in the BA group. Thirdly, participation/impairment: We expect both groups BA and CBT to show a decrease in social and work impairment.
Given the context of a multidimensional inpatient treatment for chronic mental disorders, which focuses on life and work participation, we also examine the changes in terms of the ICF (25).
The study was conducted in the naturalistic setting of two psychosomatic rehabilitation clinics but based on the admission date of the individual patient, quasi-randomization of patients to BA vs. CBT could be established.
Psychosomatic rehabilitation is a specific treatment setting within the German health provision system. It is closely related to the ICF hence it must encompass certain treatments: treatment of symptoms (psychotherapy and/or medication), training of capacities (e.g., assertiveness, social competence), change of context, social support (e.g., pension, other monetary services), salutotherapy. The average stay is 5 weeks with the option of prolonging the stay by up to 2 weeks. All patients get individual (1x 60 min/week) and group psychotherapy (2 x 90 min special group therapy e.g., depression; 1 x 90 min interpersonal group), occupational therapy, muscular and balance training (2 x week), and aerobic exercise (2 x week). If deemed necessary, patients can also participate in occupation related either individual or group counseling. For more information on the German psychosomatic rehabilitation system and its relatedness to the ICF see Linden (19).
Within the above-described setting, we systematically varied the specific group psychotherapy component (see below 2.4 randomization), which was the main psychotherapeutic ingredient of the treatment. Groups conducted according to a BA manual (see below) with those conducted according to a standard CBT manual (see below) were compared.
Patient acquisition and treatment took place in two inpatient psychosomatic rehabilitation hospitals (Seehof in Teltow, and Clinic Bavaria in Kreischa, both in Germany). Both belong to a larger network of hospitals run by the German Pension Insurance (19). Access is open to the public and costs are covered either by the German Pension Insurance or by the general healthcare system in Germany. Due to differences in the interpretation of federal state requirements on public hospitals by hospital CEOs, one methodological difference needs to be mentioned. Group sessions could only be videotaped in hospital 1, whereas in hospital 2 adherence was checked in regular supervisions. Furthermore, different hospital policies and organizational processes, stuff shortages during the COVID-19 pandemic led to following differences: the Mini-ICF-APP was conducted as an external rating at T0 and T3 in hospital 1 and self-rating at T4. In hospital 2, Mini-ICF APP was only conducted as self-rating at T0, T3, T4. Furthermore, QIDS-C was conducted at T0 and T4 at the hospital 1, and at T0, T3 and T4 at hospital 2.
Adults undergoing psychosomatic rehabilitation between February 2019 and November 2020 with a diagnosis of a depressive syndrome (assessed with M.I.N.I. and QIDS, 26, 27) were recruited into the study (N= 375, women= 76%). Additionally, 56% of the patients in BA and 63% in TAU also showed particularly problematic occupational problems at admission, assessed via SIMBO-C (28). A total score of SIMBO-C (based on 6 scales: age, motivation/expectation, subjective occupational prognosis, socio-medical problems, health-related occupational impairments) was used to assess whether additional occupation counselling was needed. Exclusion criteria were a history of or current psychotic symptoms, substance dependence or abuse, or a severe comorbid anxiety disorder with pronounced avoiding behavior. Also, patients with organic brain disorders and/or severe untreated sleeping apnea were excluded from the study. All participants provided oral and written consent to be included in the study. Patients were blinded to the purpose and study hypothesis. Informed consent included the information that participants would participate in a treatment condition expected to offer an effective treatment for depression.
All patients considered eligible for the study purposes were randomized into either BA or CBT The randomization was conducted as following: The study nurse responsible for the general coordination of all treatments conducted the randomization. The study nurse was blinded for the purposes of the study as well as the content of group modalities. Upon inclusion in the study, patients were assigned to the category “the group therapy for depression” in the computer system of the hospital. From this group, the nurse then assigned them either to BA or CBT based on the odd or even number of the week.
Data was collected from February 2019 until September 2020 under the project title “Behavioral activation for depressive syndromes in rehabilitation”. The study was approved by the local ethics committee of the Technische Universität Dresden (Germany; EK 327082018) and preregistered at the German Clinical Trials Register (DRKS 00016495). Patients were randomly assigned either to a behavioral activation group (BA, N = 174) or a cognitive-behavioral group-psychotherapy (CBT, N = 201) for depressive syndromes. Based on clinical expertise of the medical director or assistant medical director, if deemed inevitable for the achievement of therapy goals, the stay was prolonged by up to two weeks. In order to fulfill the rehabilitation-guidelines (29) of the German Pension Insurance Union, group therapy is mandatory throughout the whole stay. Therefore, patients attended a psychological group treatment with the focus on relaxation/mindfulness exercises and problem-solving exercises after the prolongation of their stay. CBT group therapy format adhered to the well-established and scientifically evaluated methods of the cognitive-behavioral therapy manual by Hautzinger (30). The group therapy comprised psychoeducation, cognitive therapy, session(s) on social skills, and (restricted to one session) behavioral activation with pleasant activities. The behavioral activation (BA) group was based on the manual on behavioral activation in groups by Hoyer and Vogel (31), which focuses strongly on value-based activity monitoring and planning. Sessions took place twice a week, each lasting 90 min. In total, 75 groups (each consisting of 3-12 patients) were analyzed.
All sessions of hospital 1 were videotaped, and the adherence was checked by regular supervision. In addition, we conducted a formal analysis of the adherence with the respective treatment manual. For this purpose, the rating scale AVADIR (32) was developed. The scale was created using a rational-deductive approach from various instruments evaluated in practice to assess manual adherence for the two treatment conditions (BA vs. CBT). AVADIR is a 64-items 7-point Likert scale with four subscales: behavioral activation techniques, cognitive techniques, generic group-psychotherapeutic techniques, and extraneous techniques. Based on these items, a total sum score is calculated. In addition, it is possible to map a differentiated representation of individual treatment techniques in the context of the therapy sessions to be evaluated. Each video included in the analysis was rated by 3 trained members of the study, and interrater reliability was calculated. The adherence in hospital 2 was provided by regular supervision meetings.
Diagnoses were established according to the following procedures:
All patients that were checked for eligibility in the study participated in a diagnostic interview, which was conducted by trained interviewers. Training was comprised of 3 components: a) shadowing of project coordinator (a clinical psychologist in an advanced psychotherapeutic training), b) participation in an online training on QIDS, c) performance of the interview in front of the project coordinator. The diagnostic instruments used in this study were the Quick Inventory of Depressive Symptomatology (QIDS, 27) and the Mini-International Neuropsychiatric Interview (M.I.N.I., 26). Patients were considered eligible when they reached minimum 8 points in QIDS and were screened for psychosis, alcohol abuse, and bipolar disorder with the M.I.N.I.
Depressive symptoms’ severity was measured via the Beck Depression Inventory (BDI-II, 33). The BDI-II is a widely used 21-item self-report inventory measuring severity of depressive symptoms. Activation was measured with the Behavioral Activation for Depression Scale (BADS), via a 25-item (T0, T3, T4) (34) and 9-item (T2, T3) form (35). Additionally, QIDS-C scores were analyzed at Pre and T3 (hospital 2) vs. T4/Follow up (both hospitals).
Disability related functioning was measured via Mini-ICF-APP (Mini-ICF-Rating für Aktivitäts- und Partizipationsstörungen bei psychischen Erkrankungen/Mini-ICF-Rating of impairment in activation and participation for mental illnesses) which measures either as a 13-item self-report (36) or 13-item external rating (37) following the 13 areas of ICF: adherence to regulations, planning and structuring of tasks, flexibility, applying expertise, competence to judge and decide, endurance, assertiveness, contact with others, group integration, intimate relationships, non-work activities, self-care, and mobility. Depression and activation scores were measured prior to the treatment and then in the 2nd, 3rd and 4th week of the treatment (see Figure 1), before the respective group session started (Pre, T1, T2, T3).
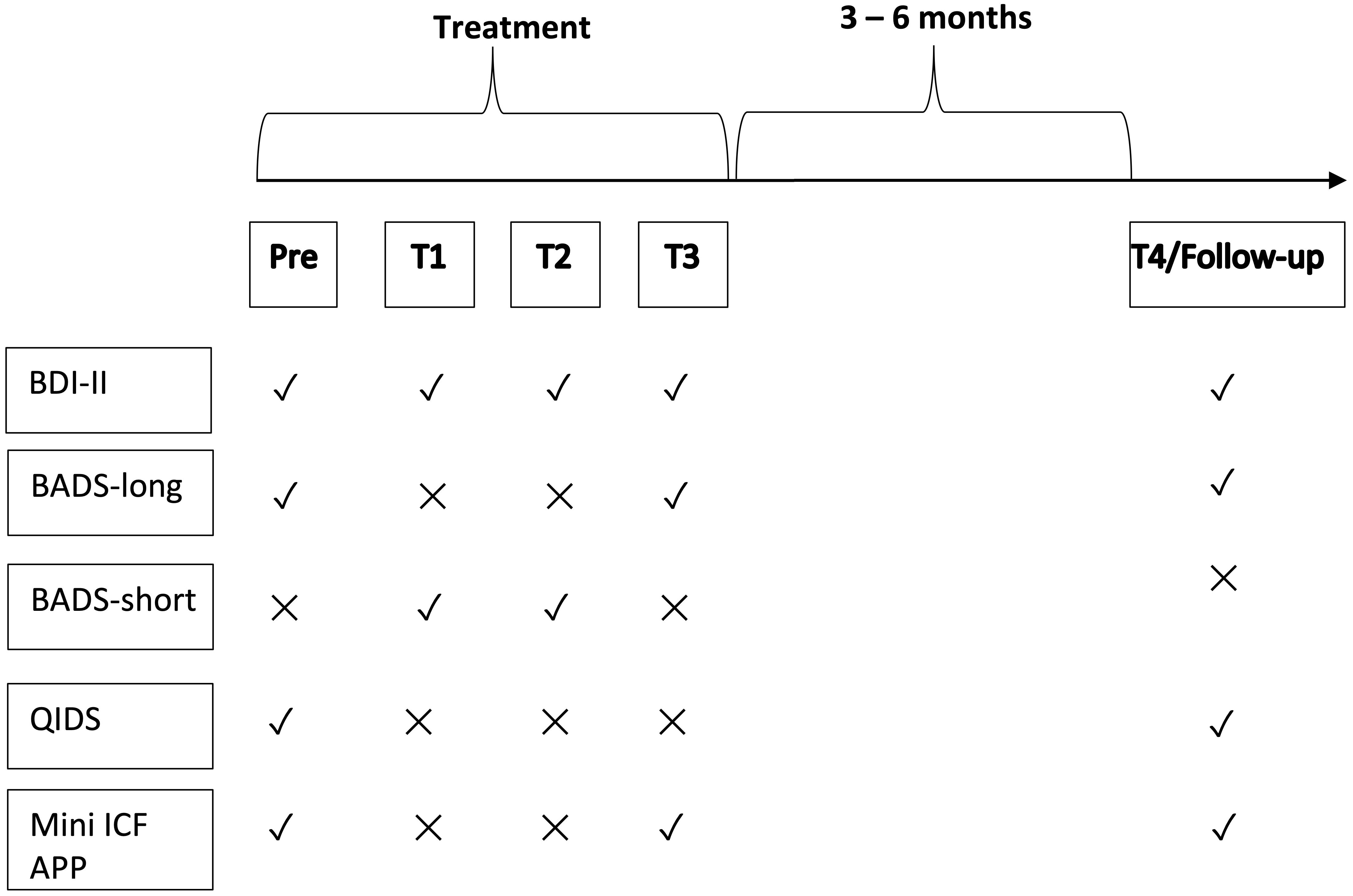
Figure 1 Study timeline. The figure depicts the order in which the questionnaires were administered to the patients. Time point Pre took place prior to the beginning of the treatment. T1, T2, and T3 were administered in the subsequent weeks. Follow up took place at 3 to 6 months. Check marks indicate that the questionnaire was administered and crosses that it was not. Due to differences in organizational processes, only in one hospital QIDS-C was conducted at T3. We did not include this data in the main analysis.
Follow-up took place at 3 to 6 months after the discharge from the hospital (T4). Both clinics followed the same procedure: 3 up to 6 months after the discharge from the clinic, patients were contacted by the trained study team via telephone. After oral consent was given, qualitative interviews concerning symptoms and work status, as well as the QIDS-C were conducted. Patients were then asked to fill BDI-II and BADS online, in pen-and-pencil form, or directly on the telephone, as has been done similarly by Senior, Kunik (38). Patients who did not complete the questionnaires received a maximum of five reminder phone calls (pen-and-pencil) or emails (online) after one and two weeks.
A total number of 35 therapists (hospital 1, n= 25) were recruited to participate in the study. All therapists were either clinical psychologists (holding a master’s degree in psychology) or physicians (specialization in psychosomatic medicine), either fully approved in psychotherapy (CBT) or in an advanced postgraduate training in CBT. The training for both psychologists and for physicians specializing in psychosomatic medicine and psychotherapy are equivalent in Germany. Accumulated over both hospitals the mean clinical experience was 4.98 years (SD= 5.34), mean age 36.91 years (SD= 5.9). In hospital 1 68% were women vs. 90% in hospital 2. All therapists had participated in the workshop on CBT specific techniques for groups that are required for the psychotherapeutic training. In particular, as CBT is an integral component of the psychotherapeutic curriculum, all therapists took part in it. In addition, all therapists also participated in a specific training for the application of the manual for the study. The latter comprised of two lectures (with an average duration of 3 hours) that introduced the theory and specific techniques of the modality to which they were allocated. The allocation was not random as both therapists’ and hospital schedule had to be accounted for. Throughout the duration of the study regular supervision was available. In a nutshell, all therapists had received basic training in CBT prior to the study. However, only BA therapists received training in BA. CBT therapists also attended additional workshop on CBT right before they were allocated to this treatment modality.
Figure 2 shows the study flow chart. Due to high dropout rates, especially at follow up, multilevel models were carried out as intent-to-treat analysis.
Based on the combined assumption that BA might only be marginally more efficacious in typical patients (d = .20) but more efficacious to a moderate degree in those being less well educated (d = .50) and that both groups will constitute about 50% of the sample, we deduced a potential effect of d = .35. In addition, we corrected the a priori sample size for potential cluster effects following the proposals by Rutterford, Copas and Eldridge (2015) and which resulted in a priori sample size N= 500 (250 in each arm).
Due to lockdown during the first two COVID-19-waves, group treatment was unexpectedly cancelled which led to a significantly smaller sample size (see flow chart). Since the estimated sample size was not met, we interpreted the results based on the confidence intervals (CI, see Supplementary Figure 1) as described elsewhere (39, 40). CIs are a more sound alternative to post-hoc power analysis, which has been criticized for only giving tautological and non-informative results as all studies with non-significant results will always show low power (41).
Both outcome variables have a hierarchical structure in which BDI-II and BADS (scales: activation, avoidance, social and work impairment) responses (level 1) are nested within participants (level 2), who are nested within groups/therapists (level 3) and within hospitals (level 4). Mixed effect models (also called multilevel models or hierarchical linear models) are a more appropriate method than conventional unilevel analysis for such nested data (42). We used a mixed effects models approach with full information maximum likelihood estimation. Furthermore, mixed effect models are able to accommodate missing data and integrate time-varying factors (43). In particular, linear mixed models are also robust to violations of distributional assumptions (42). We report the results according to Luo et al. (44).
Data preparation and statistical analyses were carried out with RStudio (Version 1.3.109, RRID : SCR_000432) with R 4.0.3 and diverse additional packages available under: the reserved DOI: 10.6084/m9.figshare.22815773. Prior to the analysis, the differences in demographic variables between the group formats were tested via non parametric tests (Pearson’s Chi-squared test, Wilcoxon rank sum test or Fisher’s exact test), see Table 1.
To model the development of BDI-II scores between the two group therapy formats, a linear multi-level model was used. To analyze the BADS, the following steps were conducted. Scales activation, avoidance, social and work impairment were calculated with the scoreItems function from the psych package. See vignette of the package for more information. Each scale was quantified as a sum of items of BADS-Scales for each patient. For the BDI-II we used the total scores as outcome variable. Data was analyzed as a function of treatment, time, and education level as fixed effects and the interaction term was treatment, time and education level. To incorporate the dependency among observations within a person and a hospital, random intercept person nested within a location (hospital) were specified. We used the log likelihood test and the AIC criterion to determine whether the inclusion of each term improved the model fit, and the function cohen.d from the package effsize to calculate Cohen’s d effect size (45). Also, QIDS at follow-up scores were analyzed as a function of baseline score, treatment and education level via multilevel models. Random intercepts of groups nested within a location were included, too. Further details and R code are available in the Supplementary Materials.
Secondary outcome measure: As Mini-ICF-APP consists of ordinal data, one sample Wilcoxon signed-rank tests were conducted for each scale. Furthermore, due to high number of zeros in data set causing non-normal distribution, zero-inflation Poisson regression was conducted with interaction term Time x Treatment (46). Therefore, the Cohen´s d could not be calculated. The effect size (ES) r is calculated as Z statistic divided by square root of the sample size (47). Due to differences in data collection between the two hospitals, only one hospital was able to provide a clinician-administered scale rather than a self-rating, which were analyzed. The descriptive statistics of the self-rating from the second hospital are available in the Supplementary Materials.
The mean age in the study was 51.92 years (SD=8.65); 76% were women. For a comparison between the treatment groups see Table 1. In the present sample, most of the patients completed vocational training. All patients were diagnosed with depressive disorders and 66% were diagnosed with a comorbid mental disorder (see Table 1). Comparison of the socio-demographic variables did not reveal any significant differences between completers vs. non-completers of follow-up (see Supplementary Table 1 in Supplementary Materials).
8% of the video tapes were of sufficient recording quality and could be selected for adherence checks according to the AVADIR scale. The adherence check was conducted after 13.5 months (out of 24 months). At this time in the hospital 1, 448 group therapy sessions were conducted (56 group therapies conducted x 8 sessions). Of the 448 group therapy sessions conducted, video excerpts of at least 30 minutes were available for 218 sessions. According to Dennhag, Gibbons (48), at least three group therapy sessions of six sessions each should be assessed per therapist to provide sufficient assessment of adherence. For a total of 15 therapists (BA=7; CBT= 8) at least one complete group therapy (8 sessions per run) was available. 22 complete group therapies (56%) were led by more than one therapist, so that these had to be excluded from analysis.
From this sample, a random sample was drawn from three different strata: 1) one of the three group therapies per therapist per condition (BA; CBT), 2) session number per group therapy (one from session 1-4 and one from session 5-8), and 3) session phase (beginning, middle, or end of session). Thirty-six therapy excerpts (duration: 30 minutes; BA: 18; CBT: 18) from each of six therapists (BA: 3;CBT: 3) were included in the analysis.
The overall adherence to the group manuals was measured via the total score. No differences were found between the therapists of both groups (BA: M= 3.94, CBT: M=3.57). The results indicate an average adherence based on the 7-point Likert scale of the AVADIR. The inter-rater-reliability was average (ICC5= .46 (95% K [.07,.71], p = .013). Furthermore, rated video segments conducted by BA therapists contained 66% behavioral techniques (M = 9.80, SD = 5.98); 34% generic group techniques (5.02, SD = 3.37) and 1% cognitive ones (M = 0.13, SD = 0.38). Rated video segments conducted by CBT therapists were found to contain 66% cognitive (M = 7.89, SD = 5.81), 22% generic (M = 2.65, SD = 2.40), and 12% behavioral techniques (M = 1.48, SD = 2.53). This indicates a good adherence to both manuals and a small proportion of overlapping therapeutic interventions.
Depression scores in both groups significantly decreased from T0 (M=27.12, SD=11.81) to T3 (M= 14.06, SD=11.69), t (797) =15.99, p <.001, d= 1.13 and also from T0 to follow up (M= 11.02, SD=15.11), t (625) =16.96, p <.001, d= 1.28. The results of the comparison tests between the treatment groups are aggregated in Table 2. Response rates were calculated according to Hiller and Schindler (49, see Table 3). The model that was found to have the best fit based on Akaike Information Criterion (AIC) for BDI-II-score was the one with fixed effects treatment (BA vs. CBT), time, and education level, the interaction term treatment x time x education level, and random intercept of patients nested within location (see Supplementary Table 3 in the Supplementary Material).
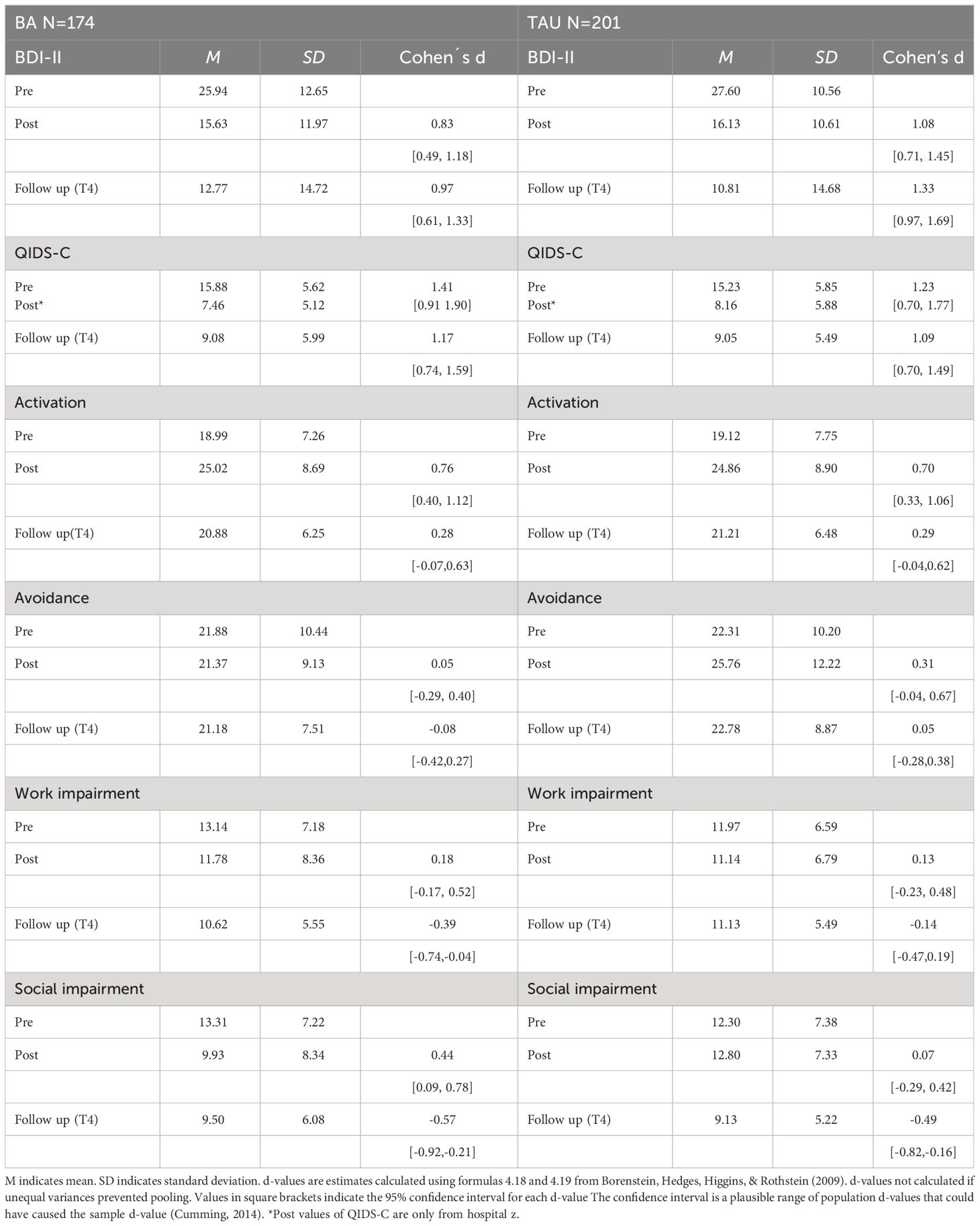
Table 2 Means, standard deviations, and d-values with confidence intervals of depression and activation measures.
The estimated variance of patients’ random effects was statistically significant (p <.000), indicating that the within patient variance significantly contributed to the outcome. The ICC for the patients’ random effects nested within a location was 0.48 indicating that 49% of the variance in the outcome was explained by the individual differences between patients and their respective locations.
The effect of time on the outcome was significant in both subgroups, β= -3.78, 95% CI [-4.61; -2.95], p <.001 indicating that patients in both treatment groups significantly reduced their symptomatology. Effects of education level (completed vocation training) β= 5.21, 95% CI [0.76;9.65], p = .022 and education level (University degree) β= -7. 03, 95% CI [-12.98; -1.07], p = .021, were also statistically significant. However, the interaction between time, education level and treatment were not (p=.116). For more detailed information see Supplementary Table 3 in the Supplementary Material.
Models that were found to have the best fit based on Akaike Information Criterion (AIC) for BADS Scales (activation, avoidance, social, and work impairments) were the ones with fixed effects treatment (BA vs. CBT), time, education level, and random intercept of person nested within a location, see Supplementary Table 5 in the Supplementary Material.
Activation was significantly predicted by time β= 1.04, 95% CI [0.35; 1.72], p= .003, indicating that patients in both treatment groups increased their activity levels. Social impairment β= - 0.99, 95% CI [-1.57; - -0.41], p<.001 significantly decreased over time, whereas work impairment β= - 0.48, 95% CI [-1.03; - 0.07], p= .089 did not. Educational level (completed vocational training) had significant effect on avoidance β= 3.89, 95% CI [0.31; 7.47], p= .033. The interaction between time, educational level and treatment was not statistically significant for any of the scales, see Supplementary Table 5 in the Supplementary Material.
Descriptive analysis revealed that both groups significantly decreased from T0 (M=15.03, SD=5.47) to follow up (M= 8.01, SD=5.91), t(292.44) = 10.43, p <.001, d = 1.21. Additionally, in hospital 2 QIDS-C scores decreased from T0 (M=12.33, SD=4.13) to T3 (M= 7.76, SD=5.40), t(50.15) = 3.79, p <.001, d = 0.91.
Multilevel models: After adjusting for the baseline differences in QIDS scores, no significant impact of treatment on depressive symptoms was found β= - 4.27, 95% CI [-12.94; 4.40], p= .333. The interaction between time, education level and treatment was not statistically significant p=.116. For more detailed information see Supplementary Table 4 in the Supplementary Material.
All but few scales significantly changed from pre to follow up. The scales endurance (BA: r = 60 vs. CBT: r =53), assertiveness (BA: r= 39 vs. CBT: r=63), contact with others (BA: r= 43 vs. CBT: r=52), flexibility (BA: r= 44), and group integration (CBT: r= 50) showed increase through higher scores at the end of the treatment (T3). As visual inspection showed increased number of zeros in the data set, we conducted zero-inflated Poisson regression. This analysis confirmed only statistically significant influence of factor time on endurance. Among those who scored minimum 1 point on the MINI-ICF-APP scale, the score changed by a factor of 0.7 from pre to post, and this is statistically significant p=.018. For more information see Tables 4 and 5.
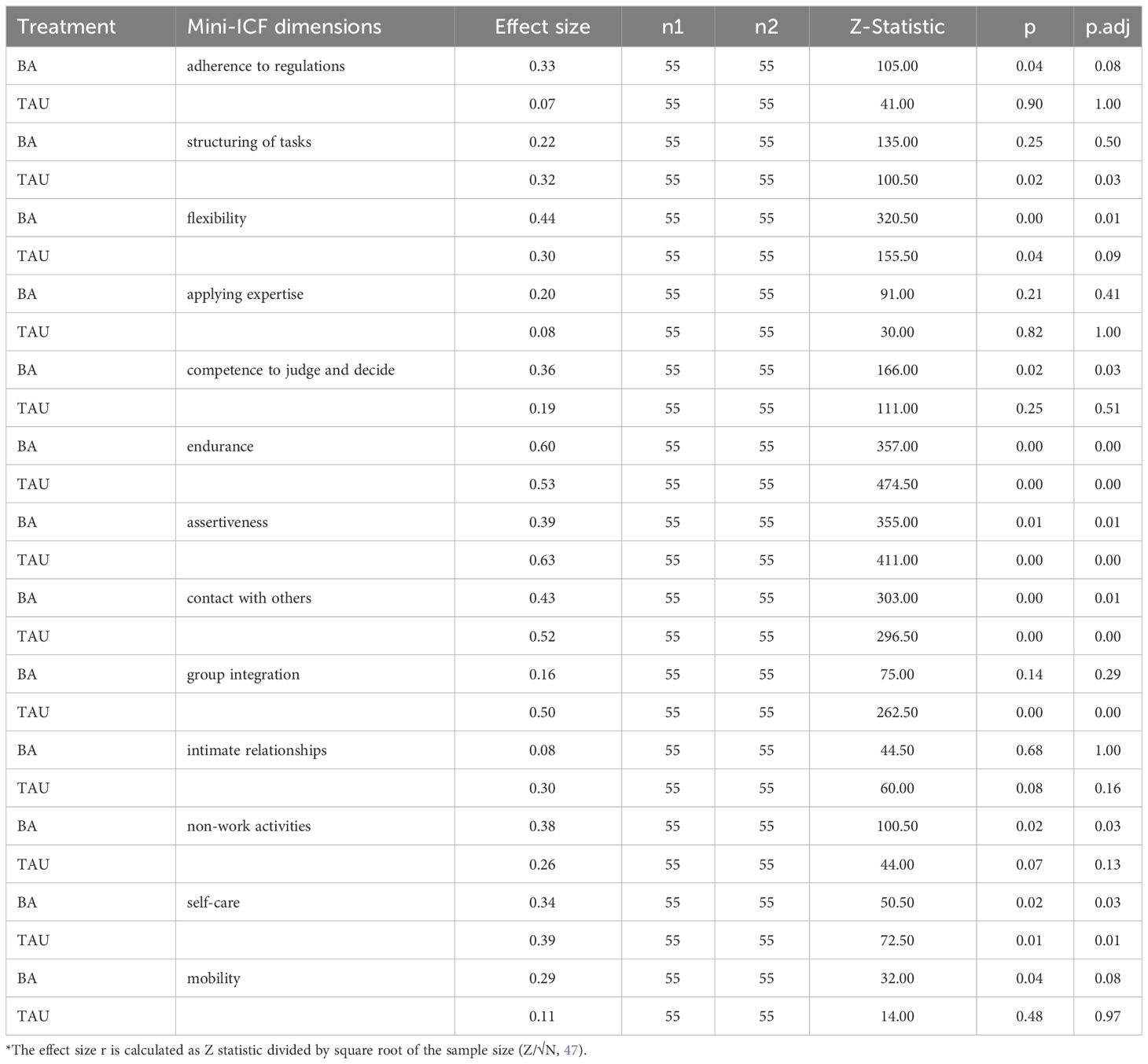
Table 5 Wilcoxon test results of pre to post change: Z-statistics, p values and effect sizes of Mini-ICF-APP scale.
In the present quasi randomized-controlled study, the effects of behavioral activation in a group setting versus cognitive-behavioral group therapy were compared as nested treatment components within a psychosomatic rehabilitation treatment in Germany. Given the large sample and the robust statistical analyses, the study significantly contributes to the rather scarce pool of literature on inpatient group psychotherapy. In line with Folke, Hursti (9), it shows that inpatient psychotherapy is beneficial for the treatment of depression, which is of relevant knowledge as it refers to a clientele for which treatment success was not deemed promising in the outpatient setting (e.g., multi-morbid, belongs to marginalized social groups, or is chronically ill).
Our results showed large within-group effect sizes in the decline of depressive symptoms in both treatment groups of about d = 1.24 at follow-up. Furthermore, there were highly favorable response and remission rates in CBT and BA (53.7% and 54.2%, respectively). These effects are among the largest when compared to previous reports on depression treatment in rehabilitation (50) and these results clearly demonstrate the effectiveness of depression treatment within the context of psychosomatic rehabilitation. Compared to outpatient treatment, inpatient treatment is of higher intensity, but also more time-condensed in terms of the duration of stay, which is limited to 5 weeks and can be prolonged to up to 7 weeks. Our results demonstrate that such short-term inpatient psychotherapy programs can be highly effective.
With regards to the comparison of BA vs. CBT, no differences were found between both treatments, neither in the change of depressive symptoms nor in the change of any other main outcomes. For example, activity levels increased throughout the stay, independent of the form of group treatment applied. These findings are in line with a recent meta-analysis, in which BA compared to an active control group yielded only marginal effect sizes in reduction of depression symptoms as well as increase in activation (51). In line with previous research (52) both treatment modalities showed significant improvement in measures of functional impairment ICF, which, however, did not significantly differ between treatments. This finding does not surprise, as psychosomatic rehabilitations in Germany are packaged treatments that are fine-tuned towards individual assessment and rehabilitation of functional impairments. Differences between BA and CBT regarding ICF were highly improbable, and we did not expect them. Furthermore, patients’ level of education did not moderate the outcome variables. Contrary to our hypothesis, patients with a low education level did not benefit more than other patients from the BA component. However, patients with low education showed higher avoidance rates, and social as well as work-related impairments. Interestingly, these findings did not correlate with depression scores as we did not find education level to significantly predict either of the depression measures. Contrary to previous research (53–55), patients with lower education status did not appear to be more depressed. However, psychosomatic rehabilitation clinics not only offer inpatient psychotherapeutic treatment, but they also conduct psychosocial assessment. The results of psychosocial assessment can then lead to measures for further outpatient occupational rehabilitation or even early retirement. Since persons with lower education level (LEL) tend to work in occupations with higher exposure to risks and tend to discharge from work life earlier (54), the above-mentioned results could mirror the fact that for persons with LEL, psychosomatic inpatient psychotherapeutic treatment is as important as psychosocial assessment and occupational therapy.
Overall, the findings suggest that using BA in the context of psychosomatic rehabilitation does not have any add-on effects on treatment outcome. Neither is it inferior to CBT in the present sample. Hence, the evidence of the present study leaves it open which of the two approaches should be preferred in treatment. As both have the same average effects, therapists as well as patients can freely decide which of the two approaches is more convenient and convincing for them. Even if these “weaker” reasons for choosing a treatment approach may not moderate the treatment outcome, they should not be neglected as they are central for what is perceived as a “quality treatment” from the patients’ perspective (56). For many patients, it is of importance how complex, feasible, cost-extensive, comprehensible, fast etc. a treatment is, independent of the outcome (56). Against the backdrop of the advances in personalized medicine, research on psychotherapy has started examining potential of patient-centered treatment. Making a larger variety of treatment modalities available, that can be then tailored towards individual patient’s needs, could lead to better outcomes in the future (57–60). Such development will mirror multi-optional treatment in other medical fields, where patients can e.g., express their wish for or against adjunctive pharmacotherapy. Accommodating individuals’ preferences for psychotherapy type could further catalyze the treatment due to a better fit between patient and intervention(s).
At this point, we would like to elaborate on the differences between inpatient psychosomatic rehabilitation and outpatient psychotherapy in Germany. Public insurance companies in Germany reimburse outpatient psychotherapeutic treatment (behavioral therapy), independent of the clinical diagnosis, with up to 60 sessions per case. However, in the practice, the median therapy length is 15,9 months (SD=0.64) and the median number of sessions is 40 (SD= 2 sessions) sessions (1). Since the therapeutic sessions occur on average 1x week, interventions can be precisely tailored towards the demands of the person´s natural environment. On the other hand, inpatient psychosomatic rehabilitation lasts 5 weeks, occasionally up to 7 weeks. This is a very condensed and intense therapeutic treatment package. In particular, it can be very effective for patients that would not be able to make a progress when treated in outpatient setting e.g. due to the severity of the symptoms (2). The challenge than is the transfer and application of newly acquired competencies and skills in the broader contexts of everyday life (e.g. at home, at work etc., 2).
In this respect, it must be emphasized that, behavioral activation is an especially simple and parsimonious method, that is easier to understand for cognitively impaired patients (61). Moreover, it does not require sophisticated therapeutic skills that take years of training (for the therapists of this study applying BA was new). The present study demonstrates that it can be easily integrated into an established and complex treatment program without any negative consequences for the overall effectiveness.
Although specifically targeted, the inpatient setting of this study limits the interpretation of the results. All patients participated in an extensive inpatient treatment program of approximately 25 hrs/week (e.g., occupational therapy, sports, etc.), of which group therapy lasted only 180 min/week. Hence, we could not dismantle the effects of the group therapy modality by itself. Our results should rather be interpreted as a comparison of two treatment packages of which one includes BA and the other CBT. Future studies should direct their attention towards this aspect. Also, the pre-registered sample size of N= 500 could not be achieved due to restrictions of the COVID-19 pandemic. Since we did not conceptualize this study as an equivalence trial, we did not set a margin to which we would compare the difference in treatment effects, hence we cannot conclude whether these two methods (BA vs. CBT) are equivalent. However, visual inspection of the mean scores showed no substantial differences between the treatment methods, and CIs overlap to a great extent, which is in line with previous research (7). Due to the design of the study, we cannot rule out other factors that might have played a role, such as other treatments (e.g. physical exercise 62), medication, and social environment of the hospital (63). As group therapy is only one aspect of the treatment package within inpatient care, a substantially larger sample or a completely different design (e.g., one arm of the study without any group treatment) would be necessary to detect a possibly small effect. Given the great overlap of the CIs, future researcher should also target the comparison between BA and CBT in terms of an equivalence study.
A further limitation is the number of videotaped sessions of the hospital 1 (8%) that could be used for the adherence check. We chose to follow the well-researched procedure suggested by Dennhag, Gibbons (48). Due to its strictness (e.g., only group sessions led by one therapist, etc.), a large number of group sessions had to be excluded. Considering the context in which this procedure was developed, outpatient addiction treatment in one-to-one setting, it is understandable that such rules have to be followed. However, in inpatient setting of psychosomatic rehabilitation, substitutes lead sessions that would be canceled in outpatient setting. Hence, groups are bound to experience more than one therapist. On the other hand, we can speculate that due to close proximity of team members, and regular meetings such as supervisions, head physician’s weekly rounds etc., adherence can be monitored and maintained better than in an outpatient setting despite sessions being substituted. Since there are no studies focusing on the number of sessions per therapist to check adherence of inpatient group therapies, we decided to choose a rather conservative rule suggested above. However, this is a research gap of clinical relevance that future studies should aim at.
Despite our great effort in contacting patients multiple times by multiple means (e.g. by phone, E-mail, mail), we could not prevent high dropout rates at follow up. This is in line with previous research conducted in inpatient settings. Particularly in psychosomatic rehabilitation, response rates have been found to be very low (50). Nevertheless, this reduces the chance to detect differences between the treatments. As the allocation was quasi-randomized, however, neither the researchers nor the patients could influence drop-out rates in any systematic way. Also, limited ethnical and cultural variability of the sample prevents this study from generalizing the results to other ethnical and cultural contexts. Additionally, use of self-reports for testing the main criteria poses a limitation of this study as there are typical risks of biases (e.g., response bias) inherent in the self-report approach. Nevertheless, it has economical and practical advantages for standard use in the inpatient setting and the expert rating measure (QIDS-C) that was conducted at follow up (T4) mirrored the results on the self-report level. Having to interview patients multiple times throughout the study might have additionally reduced the number of participants willing to partake.
Summarizing, this large data set demonstrates behavioral activation to provide a good alternative to cognitive-behavioral therapy in groups especially in fields with a chronically ill, multi-morbid clientele.
The original contributions presented in the study are included in the article/Supplementary Materials. Further inquiries can be directed to the corresponding author.
The studies involving humans were approved by the local ethics committee of the Technische Universität Dresden (Germany; EK 327082018). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
UM and TS collected and participated in data preparation. TS overseen and conducted the manual adherence measurement. UM wrote the code and analyzed the data. VK and JH, as senior authors, together with UM conceptualized the study and wrote the manuscript. All authors extensively reviewed the manuscript, supplementary materials, and all tables and graphs. All authors contributed to the article and approved the submitted version.
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded by Grant No. DRV 8011-106-31/31.127 from the German Pension Insurance Union.
Special acknowledgment goes towards Christine Kühn for her immeasurable help with the data collection. We thank Christoph Julian von Borell du Vernay, Technical University of Dresden, for his assistance in language editing. We also thank Lilia Papst, PhD for her review of our code and statistical methods. We would also like to extend our gratitude to all physicians, psychologists, psychotherapists, and student assistants who participated in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1229380/full#supplementary-material
1. James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990; 2013; 2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2018) 392:1789–858. doi: 10.1016/S0140-6736(18)32279-7
2. Cuijpers P, Noma H, Karyotaki E, Vinkers CH, Cipriani A, Furukawa TA. A network meta-analysis of the effects of psychotherapies, pharmacotherapies and their combination in the treatment of adult depression. World Psychiatry. (2020) 19:92–107. doi: 10.1002/wps.20701
3. Cuijpers P, Ciharova M, Miguel C, Harrer M, Ebert DD, Brakemeier E-L, et al. Psychological treatment of depression in institutional settings: A meta-analytic review. J Affect Disord. (2021) 286:340–50. doi: 10.1016/j.jad.2021.03.017
4. Cuijpers P, Sijbrandij M, Koole SL, Andersson G, Beekman AT, Reynolds CF III. The efficacy of psychotherapy and pharmacotherapy in treating depressive and anxiety disorders: a meta-analysis of direct comparisons. World Psychiatry. (2013) 12:137–48. doi: 10.1002/wps.20038
5. Driessen E, Cuijpers P, de Maat SC, Abbass AA, de Jonghe F, Dekker JJ. The efficacy of short-term psychodynamic psychotherapy for depression: a meta-analysis. Clin Psychol Rev. (2010) 30:25–36. doi: 10.1016/j.cpr.2009.08.010
6. Kazantzis N, Luong HK, Usatoff AS, Impala T, Yew RY, Hofmann SG. The processes of cognitive behavioral therapy: A review of meta-analyses. Cogn Ther Res. (2018) 42:349–57. doi: 10.1007/s10608-018-9920-y
7. Richards DA, Ekers D, McMillan D, Taylor RS, Byford S, Warren FC, et al. Cost and Outcome of Behavioural Activation versus Cognitive Behavioural Therapy for Depression (COBRA): a randomised, controlled, non-inferiority trial. Lancet. (2016) 388:871–80. doi: 10.1016/S0140-6736(16)31140-0
8. Alexopoulos GS, O'Neil R, Banerjee S, Raue PJ, Victoria LW, Bress JN, et al. "Engage" therapy: Prediction of change of late-life major depression. J Affect Disord. (2017) 221:192–7. doi: 10.1016/j.jad.2017.06.037
9. Folke F, Hursti T, Tungstrom S, Soderberg P, Kanter JW, Kuutmann K, et al. Behavioral activation in acute inpatient psychiatry: a multiple baseline evaluation. J Behav Ther Exp Psychiatry. (2015) 46:170–81. doi: 10.1016/j.jbtep.2014.10.006
10. Xie J, He G, Ding S, Pan C, Zhang X, Zhou J, et al. A randomized study on the effect of modified behavioral activation treatment for depressive symptoms in rural left-behind elderly. Psychother Res. (2019) 29:372–82. doi: 10.1080/10503307.2017.1364444
11. Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, Addis ME, et al. Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in the acute treatment of adults with major depression. J Consulting Clin Psychol. (2006) 74:658–70. doi: 10.1037/0022-006X.74.4.658
12. Jahoda A, Hastings R, Hatton C, Cooper SA, Dagnan D, Zhang R, et al. Comparison of behavioural activation with guided self-help for treatment of depression in adults with intellectual disabilities: a randomised controlled trial. Lancet Psychiatry. (2017) 4:909–19. doi: 10.1016/S2215-0366(17)30426-1
13. Kanter JW, Manos RC, Bowe WM, Baruch DE, Busch AM, Rusch LC. What is behavioral activation? A review of the empirical literature. Clin Psychol Rev. (2010) 30:608–20. doi: 10.1016/j.cpr.2010.04.001
14. Hoyer J, Dechmann JCG, Stender T, Čolić J. Selecting and imagining rewarding activities during the COVID-19 lockdown: Effects on mood and what moderates them. Int J Psychol. (2021) 56:585–93. doi: 10.1002/ijop.12759
15. Simmonds-Buckley M, Kellett S, Waller G. Acceptability and efficacy of group behavioral activation for depression among adults: A meta-analysis. Behav Ther. (2019) 50:864–85. doi: 10.1016/j.beth.2019.01.003
16. Burlingame GM, Fuhriman A, Mosier J. The differential effectiveness of group psychotherapy: A meta-analytic perspective. Group Dynamics: Theory Research Practice. (2003) 7:3–12. doi: 10.1037/1089-2699.7.1.3
17. Cuijpers P, Karyotaki E, de Wit L, Ebert DD. The effects of fifteen evidence-supported therapies for adult depression: A meta-analytic review. Psychother Res. (2019) 30:279–93. doi: 10.1080/10503307.2019.1649732
18. Burlingame GM, Seebeck JD, Janis RA, Whitcomb KE, Barkowski S, Rosendahl J, et al. Outcome differences between individual and group formats when identical and nonidentical treatments, patients, and doses are compared: A 25-year meta-analytic perspective. Psychotherapy. (2016) 53:446–61. doi: 10.1037/pst0000090
19. Linden M. Psychosomatic inpatient rehabilitation: The german model. Psychother psychosomatics. (2014) 83:205–12. doi: 10.1159/000358852
20. Substance Abuse and Mental Health Services Administration S, National Mental Health Services Survey (N-MHSS). Data on Mental Health Treatment Facilities Vol. 2019. . Rockville: MD: Substance Abuse and Mental Health Services Administration (2018). p. 2020.
21. Royal College of Psychiatrists RCoP. National Clinical Audit of Anxiety and Depression: technical report for the core audit 2017-2018. CCQI 308. Lengerich, London: Healthcare Quality Impovement Partnership (2019).
22. Kösters M, Burlingame GM, Nachtigall C, Strauss B. A meta-analytic review of the effectiveness of inpatient group psychotherapy. In: Group Dynamics: Theory, Research, and Practice, vol. 10. Washington DC: American Psychological Association. (2006). p. 146–63.
23. Reed GM, Spaulding WD, Bufka LF. The relevance of the International Classification of Functioning, Disability and Health (ICF) to mental disorders and their treatment. Alter. (2009) 3:340–59. doi: 10.1016/j.alter.2008.11.003
24. Linden M. Definition and assessment of disability in mental disorders under the perspective of the international classification of functioning disability and health (ICF). Behav Sci Law. (2017) 35:124–34. doi: 10.1002/bsl.2283
25. Üstün TB, Chatterji S, Bickenbach J, Kostanjsek N, Schneider M. The International Classification of Functioning, Disability and Health: a new tool for understanding disability and health. Disabil Rehabil. (2003) 25:565–71. doi: 10.1080/0963828031000137063
26. Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. (2003) 54:573–83. doi: 10.1016/S0006-3223(02)01866-8
27. Roniger A, Späth C, Schweiger U, Klein JP. A psychometric evaluation of the German version of the quick inventory of depressive symptomatology (QIDS-SR16) in outpatients with depression. Fortschr Neurologischer Psychiatrie. (2015) 83:e17–22. doi: 10.1055/s-00000019
28. Streibelt M. Validität und Reliabilität eines Screening-Instruments zur Erkennung besonderer beruflicher Problemlagen bei chronischen Krankheiten (SIMBO-C). Rehabilitation. (2009) 48:135–44. doi: 10.1055/s-0029-1220742
29. Farin E, Wirth A, Quaschning K, Meyer T, Nowik D, Block I, et al. Die Aktualisierung der Reha-Therapiestandards der Deutschen Rentenversicherung. Rehabilitation. (2018) 57:48–54. doi: 10.1055/s-0043-124309
31. Hoyer J, Vogel D. Verhaltensaktivierung: techniken der verhaltenstherapie. Praxis der Kinderpsychologie und Kinderpsychiatrie. (2018) 68:163–7.
32. Eickschen M, Schott T, Hoyer J. ARVADIR-Adhärenzrating in der Studie zur Verhaltensaktivierung depressiver Syndrome in der Rehabilitation. (2020). Unpublished questionnaire.
33. Hautzinger M, Keller F, Kühner C. Das Beck Depressionsinventar II. Deutsche Bearbeitung und Handbuch zum BDI II. Frankfurt a.M: Harcourt Test Services (2006).
34. Kanter JW, Mulick PS, Busch AM, Berlin KS, Martell CR. The Behavioral Activation for Depression Scale (BADS): psychometric properties and factor structure. J Psychopathol Behav Assessment. (2007) 29:191. doi: 10.1007/s10862-006-9038-5
35. Manos RC, Kanter JW, Luo W. The behavioral activation for depression scale–short form: development and validation. Behav Ther. (2011) 42:726–39. doi: 10.1016/j.beth.2011.04.004
36. Linden M, Keller L, Noack N, Muschalla B. Self-rating of capacity limitations in mental disorders: The Mini-ICF-APP-S. Lengerich, London: Praxis Klinische Verhaltensmedizin und Rehabilitation (2018) p. 14–22.
37. Linden M, Baron S, Muschalla B. Mini-ICF-APP: Mini-ICF-Rating für Aktivitäts- und Partizipationsstörungen bei psychischen Erkrankungen ; ein Kurzinstrument zur Fremdbeurteilung von Aktivitäts- und Partizipationsstörungen bei psychischen Erkrankungen in Anlehnung an die Internationale Klassifikation der Funktionsfähigkeit, Behinderung und Gesundheit (ICF) der Weltgesundheitsorganisation ; Manual: Huber. Hogrefe, Göttingen, (2009).
38. Senior AC, Kunik ME, Rhoades HM, Novy DM, Wilson NL, Stanley MA. Utility of telephone assessments in an older adult population. Psycholy Aging. (2007) 22:392–7. doi: 10.1037/0882-7974.22.2.392
39. Heckman MG, Davis JM 3rd, Crowson CS. Post hoc power calculations: an inappropriate method for interpreting the findings of a research study. J Rheumatol. (2022) 49:867–70. doi: 10.3899/jrheum.211115
40. Lakens D, Scheel AM, Isager PM. Equivalence testing for psychological research: A tutorial. Adv Methods Practices psychol Science. (2018) 1:259–69. doi: 10.1177/2515245918770963
41. Goodman SN, Berlin JA. The use of predicted confidence intervals when planning experiments and the misuse of power when interpreting results. Ann Internal Med. (1994) 121:200–6. doi: 10.7326/0003-4819-121-3-199408010-00008
42. Schielzeth H, Dingemanse NJ, Nakagawa S, Westneat DF, Allegue H, Teplitsky C, et al. Robustness of linear mixed-effects models to violations of distributional assumptions. Methods Ecol Evolution. (2020) 11:1141–52. doi: 10.1111/2041-210X.13434
43. Tasca GA, Gallop R. Multilevel modeling of longitudinal data for psychotherapy researchers: I. The basics. Psychother Res. (2009) 19:429–37. doi: 10.1080/10503300802641444
44. Luo W, Li H, Baek E, Chen S, Lam K, Semma B. Reporting practice in multilevel modeling: A revisit after 10 years. Rev Educ Res. (2021) 91:003465432199122. doi: 10.3102/0034654321991229
45. Torchiano M. _effsize: Efficient Effect Size Computation_. R package version 0.8.1. Available at: https://CRAN.R-project.org/package=effsize.
46. Green JA. Too many zeros and/or highly skewed? A tutorial on modelling health behaviour as count data with Poisson and negative binomial regression. Health Psychol Behav Med. (2021) 9:436–55. doi: 10.1080/21642850.2021.1920416
47. Rosenthal R. Parametric measures of effect size. In: Cooper H, Hedges LV, editors. he handbook of research synthesis. Russell Sage Foundation, New York (1994). p. 231–44.
48. Dennhag I, Gibbons MB, Barber JP, Gallop R, Crits-Christoph P. How many treatment sessions and patients are needed to create a stable score of adherence and competence in the treatment of cocaine dependence? Psychother Res. (2012) 22:475–88. doi: 10.1080/10503307.2012.674790
49. Hiller W, Schindler A. Response and remission in psychotherapy research. Psychotherapie Psychosomatik medizinische Psychologie. (2011) 61:170–6. doi: 10.1055/s-0030-1255040
50. Steffanowski A, Löschmann C, Schmidt J, Wittmann WW, Nübling R. Meta-Analyse der Effekte stationärer psychosomatischer Rehabilitation: Meta-Studie: Huber Bern. Berlin: Springer Science and Business Media LLC (2007).
51. Stein AT, Carl E, Cuijpers P, Karyotaki E, Smits JAJ. Looking beyond depression: a meta-analysis of the effect of behavioral activation on depression, anxiety, and activation. Psychol Med. (2021) 51:1491–504. doi: 10.1017/S0033291720000239
52. Baron S, Linden M. Analyzing the effectiveness of inpatient psychosomatic rehabilitation using the mini-ICF-APP. Rehabil (Stuttg). (2009) 48:145–53. doi: 10.1055/s-0029-1220740
53. Evans-Lacko S, Aguilar-Gaxiola S, Al-Hamzawi A, Alonso J, Benjet C, Bruffaerts R, et al. Socio-economic variations in the mental health treatment gap for people with anxiety, mood, and substance use disorders: results from the WHO World Mental Health (WMH) surveys. psychol Med. (2018) 48:1560–71. doi: 10.1017/S0033291717003336
54. du Prel J-B, Schrettenbrunner C, Hasselhorn HM. Vertikale und horizontale soziale Ungleichheit und Motivation zum vorzeitigen Erwerbsausstieg. Z für Gerontologie und Geriatrie. (2019) 52:3–13. doi: 10.1007/s00391-018-1450-4
55. Toczek L, Bosma H, Peter R. Early retirement intentions: the impact of employment biographies, work stress and health among a baby-boomer generation. Eur J Ageing. (2022) 19:1479–91. doi: 10.1007/s10433-022-00731-0
56. Cougle JR. What makes a quality therapy? A consideration of parsimony, ease, and efficiency. Behav Ther. (2012) 43:468–81. doi: 10.1016/j.beth.2010.12.007
57. Cuijpers P, Ebert DD, Acarturk C, Andersson G, Cristea IA. Personalized psychotherapy for adult depression: A meta-analytic review. Behav Ther. (2016) 47:966–80. doi: 10.1016/j.beth.2016.04.007
58. Norcross J, Wampold B. What works for whom: tailoring psychotherapy to the person. J Clin Psychol. (2011) 67:127–32. doi: 10.1002/jclp.20764
59. Longmore RJ, Worrell M. Do we need to challenge thoughts in cognitive behavior therapy? Clin Psychol Rev. (2007) 27:173–87. doi: 10.1016/j.cpr.2006.08.001
60. Lorenzo-Luaces L, Keefe JR, DeRubeis RJ. Cognitive-behavioral therapy: nature and relation to non-cognitive behavioral therapy. Behav Ther. (2016) 47:785–803. doi: 10.1016/j.beth.2016.02.012
61. Stein AT, Carl E, Cuijpers P, Karyotaki E, Smits JAJ. Looking beyond depression: a meta-analysis of the effect of behavioral activation on depression, anxiety, and activation. Psychol Med. (2020) 51(9), 1–14. doi: 10.31234/osf.io/bhyg9
62. Papst L, Köllner V. Using machine learning to investigate earning capacity in patients undergoing psychosomatic rehabilitation—A retrospective health data analysis. Front Psychiatry. (2022) 13. doi: 10.3389/fpsyt.2022.1039914
Keywords: behavioral activation, cognitive-behavioral therapy, group therapy, inpatient setting, psychosomatic rehabilitation, international classification of functioning, depression
Citation: Melicherova U, Schott T, Köllner V and Hoyer J (2024) Behavioral activation for depression in groups embedded in psychosomatic rehabilitation inpatient treatment: a quasi-randomized controlled study. Front. Psychiatry 15:1229380. doi: 10.3389/fpsyt.2024.1229380
Received: 26 May 2023; Accepted: 10 April 2024;
Published: 25 April 2024.
Edited by:
Thomas Jamieson Craig, King’s College London, United KingdomReviewed by:
Beate Muschalla, Technical University of Braunschweig, GermanyCopyright © 2024 Melicherova, Schott, Köllner and Hoyer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jürgen Hoyer, anVlcmdlbi5ob3llckB0dS1kcmVzZGVuLmRl
†These authors share senior authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.