
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 10 September 2024
Sec. Digital Mental Health
Volume 15 - 2024 | https://doi.org/10.3389/fpsyt.2024.1181739
This article is part of the Research TopicMental Health, Epidemiology and Machine LearningView all 16 articles
 Ava J. C. Mason1*
Ava J. C. Mason1* Vishal Bhavsar1,2
Vishal Bhavsar1,2 Riley Botelle1
Riley Botelle1 David Chandran1
David Chandran1 Lifang Li1
Lifang Li1 Aurelie Mascio1
Aurelie Mascio1 Jyoti Sanyal2
Jyoti Sanyal2 Giouliana Kadra-Scalzo1
Giouliana Kadra-Scalzo1 Angus Roberts1
Angus Roberts1 Marcus Williams2,3
Marcus Williams2,3 Robert Stewart1,2
Robert Stewart1,2Introduction: Experiences of violence are important risk factors for worse outcome in people with mental health conditions; however, they are not routinely collected be mental health services, so their ascertainment depends on extraction from text fields with natural language processing (NLP) algorithms.
Methods: Applying previously developed neural network algorithms to routine mental healthcare records, we sought to describe the distribution of recorded violence victimisation by demographic and diagnostic characteristics. We ascertained recorded violence victimisation from the records of 60,021 patients receiving care from a large south London NHS mental healthcare provider during 2019. Descriptive and regression analyses were conducted to investigate variation by age, sex, ethnic group, and diagnostic category (ICD-10 F chapter sub-headings plus post-traumatic stress disorder (PTSD) as a specific condition).
Results: Patients with a mood disorder (adjusted odds ratio 1.63, 1.55-1.72), personality disorder (4.03, 3.65-4.45), schizophrenia spectrum disorder (1.84, 1.74-1.95) or PTSD (2.36, 2.08-2.69) had a significantly increased likelihood of victimisation compared to those with other mental health diagnoses. Additionally, patients from minority ethnic groups (1.10 (1.02-1.20) for Black, 1.40 (1.31-1.49) for Asian compared to White groups) had significantly higher likelihood of recorded violence victimisation. Males were significantly less likely to have reported recorded violence victimisation (0.44, 0.42-0.45) than females.
Discussion: We thus demonstrate the successful deployment of machine learning based NLP algorithms to ascertain important entities for outcome prediction in mental healthcare. The observed distributions highlight which sex, ethnicity and diagnostic groups had more records of violence victimisation. Further development of these algorithms could usefully capture broader experiences, such as differentiating more efficiently between witnessed, perpetrated and experienced violence and broader violence experiences like emotional abuse.
Interpersonal violence is defined as threatened or actual use of physical force or power against another person, involving one or more perpetrators and victims (1). Violence can be categorised in a variety of ways (e.g., physical, sexual, emotional, domestic) but all cause significant physical and mental morbidity within general populations (2–4). Individuals with a severe mental illness have been found to be significantly more likely to experience domestic, physical, and sexual violence compared to the general population (5–8). Despite this, data on violence (all forms) has been inadequately available from healthcare records. This is partly due to the lack of routine enquiry by professionals at points of clinical contact, and partly because instances of violence are difficult to identify in healthcare data in the absence of specific coding systems (9, 10).
Inconsistencies are also present between different mental health services. For instance, individuals from inpatient settings are more likely to have structured data collected on violent incidents, although the form of data collection also varies depending on the type of violence experienced (11). Electronic healthcare records data could help researchers and clinicians understand the occurrence of interpersonal violence (when disclosed), its risk factors, and the level of treatment and support provided. However, research has focused mainly on recorded incidents within inpatient settings, such as using specific violence definitions to examine the prevalence of recorded experiences of physical assault (12). Because most instances are likely to be recorded as unstructured text data, violence experiences across mental healthcare settings cannot be adequately captured without natural language processing (NLP).
A general challenge for using health records data for research is that the most valuable and granular information is frequently contained in text fields (e.g., routine case notes, clinical correspondence) rather than in pre-structured fields; this includes mentions of violence whether experienced as a victim or perpetrated. NLP has been used increasingly to extract information automatically from unstructured text in electronic health records, particularly in mental healthcare, on clinical entities such as diagnosis, symptoms, and treatment (11–14). However, few of these studies have applied NLP to investigate mentions of violence across different clinical samples. One study using NLP reported greater odds of physical victimisation within groups who had an ICD-10 diagnosis of F2x (schizophrenia, schizotypal and delusional disorder), F6x (disorders of adult personality and behaviour), F7x (mental retardation) and F3x (mood disorders) diagnostic groups vs those with an organic syndrome. However, this was specifically examined within an inpatient setting, where victimisation would be expected to be mentioned more regularly than in outpatient samples (11). Another study using NLP found individuals with victimisation to be most commonly diagnosed with psychotic disorders (20.4%) or mood disorders (16.3%) (12). However, this study specifically investigated physical victimisation, rather than other types of experienced victimisation. From these findings, it could be suggested that physical victimisation may be more prevalent in individuals with a diagnosis of a psychotic or mood disorder.
An NLP approach was previously developed to ascertain violence according to its presence, agent (i.e., patient as perpetrator or victim) and certain subtypes (physical, domestic, sexual) (15). This method provided a potential way of furthering research on how professionals and services respond to violence, as well as provide opportunities for monitoring recorded violence victimisation in different groups (16). For example, one application of these NLP algorithms included their use in a study investigating associations of victimisation with adverse mental healthcare outcomes during the early stages of the COVID-19 pandemic (17). Having run these previously developed algorithms across a large mental healthcare data resource, we sought to describe the distribution of interpersonal violence ascertained in this way across different psychiatric settings and diagnostic groups. The output presented here examined the distribution of any recorded violence victimisation, with secondary analysis examining the distribution of specific victimisation types: physical, domestic, and sexual violence. This was a descriptive study testing victimisation seeking primarily to estimate the prevalence of recorded victimisation using the aforementioned NLP algorithm across a large mental health resource. Therefore, we did not have specific hypotheses relating to which diagnostic groups would have higher prevalence of specific victimisation types. However, it was anticipated from the previous studies mentioned, that physical victimisation may be higher in patients with an ICD-10 diagnosed psychotic or mood disorder (F2x, F3x).
The study reported in this paper analysed information about violence extracted from the English language text portions of a de-identified secondary care psychiatric electronic health record (EHR), from the South London and Maudsley NHS Foundation Trust. The text consisted of a mix of document types from several EHR fields, including correspondence between clinicians, event notes written by clinicians in day-to-day clinical care, and discharge summaries (18, 19).
The method by which violence information was extracted from the text is in routine at the UK’s National Institute for Health Research Maudsley Biomedical Research Centre, where it is regularly run over the dataset. The full method, and its evaluation, has been previously reported (15). We provide a summary here for convenience.
As a first step, a list of violence-related keywords based on literature, clinical experience and informatics expertise was created. Seventeen keywords were assembled in this respect. Next, a technique called sequence classification, a common sub-task in NLP, was implemented. This involves obtaining text sequences that contain one of the listed violence-related key words, and manually labelling them as being indicative or not of five binary classes (a mention of victimisation, perpetration of violence, or general mention (as victim, witness or perpetrator) of domestic violence, physical violence or sexual violence) by multiple annotators. Guidelines were then developed on how to annotate further text sequences based on discussions with these annotators of their experiences (e.g., what text sequences would be more indicative of victimisation vs other text sequences). Inter-annotator agreement was estimated on a subset of the data labelled, giving agreements in this case of 82%-96%, and Cohen’s kappa coefficients of 60%-85% (15). As previously stated, the selection of keywords, labelling guidelines, characteristics of the labelled text and the labelling process are fully described in a previous (open access) publication (15). After measuring inter-annotator agreement on what would be classed as one of the five binary classes, separate binary classification models were trained from the labelled data, one for each of these five classes. Models were built by adapting a widely used transformer model (a type of neural network model), BioBERT (20). BioBERT was adapted using the Hugging Face Bert-For-Sequence-Classification interface (21) adding a single classification layer to the standard transformer model. Cross entropy loss with custom weight parameters was used to account for dataset imbalance. Each model created in this way classifies a text sequence as being a member or not a member of a class, such as physical violence or domestic violence. We refer to these as “instance level” mentions of violence. These instance level text sequences are derived from documents, such as clinician notes. The final algorithm labels any document that contains one or more text sequence instance of a given class with that same class, thus creating a “document level” label. For example, if a document contains two sequences labelled as being in the physical violence class, and three sequences in the domestic violence class, then the document will be labelled as being in the physical violence and domestic violence classes. As documents are written about and linked to patients, we are then able to draw conclusions about those patients. Blind testing of the final NLP algorithms on 1411 random documents gave document level F1 statistics of 0.90, 0.85, 0.98, 0.93, and 0.93 for victimisation, perpetration, physical, domestic, or sexual attributes respectively (15).
As with the NLP development, data for the analyses presented here were extracted from the case register of the South London and Maudsley NHS Foundation Trust (SLaM). SLaM is a large secondary care mental healthcare provider, serving around 1.3 million residents of a defined catchment of four London boroughs (Croydon, Lambeth, Lewisham, and Southwark). SLaM care covers all specialist mental health care, including liaison and crisis teams, community and inpatient services and early intervention services. Electronic health records (EHRs) have been used for all SLaM services since 2006, and the Maudsley Clinical Record Interactive Search (CRIS) platform was established in 2008 in order to retrieve de-identified data from records of patients previously or currently receiving SLaM care (18). The EHR source includes structured fields coding demographic information (e.g., ethnicity, sex, age), and unstructured free text fields from case notes, mental health examinations, personal histories, management plans and correspondence. Within the last decade, a range of NLP algorithms have been developed, whose detailed performance data and descriptions can be found in an open-access catalogue (22). CRIS has a robust, patient-led governance and data security model and has approval as a data resource for secondary analysis (Oxford Research Ethics Committee C, reference 18/SC/0372).
For the analyses within this paper, data were extracted for all individuals receiving SLaM services at any point during 2019, defining their demographic and diagnostic status on or as closest as possible to an index date of 1st July 2019 and ascertaining any recorded violence victimisation from the full record up to the end of 2019. The NLP algorithm can assess for a mention of violence victimisation, but it cannot accurately indicate the frequency with which that victimisation has occurred (e.g., three mentions of victimisation in different documents highlighted by the NLP could refer to the same event). As this study is interested in whether individuals have a mention of recorded victimisation in general, patients were classified within two groups based on whether they had one or more mention of recorded violence victimisation in any free text fields occurring within the study period. Records describing the violence victimisation were then further evaluated for the presence or not of physical, domestic, or sexual violence. Because the violence app in its current version does not identify the intersection of violence type and violence victimisation specifically at instance level, performance was re-checked by extracting documents to analyse accordance of each recorded victimisation and type combination. Based on 50 randomly selected positive instances for each, evaluated for the analyses presented in this report, the precision statistics for victimisation for physical violence, domestic violence, and sexual violence were 0.72, 0.72 and 0.62 respectively.
Demographic variables extracted were age, sex, and ethnicity. Age at the index date was categorised and entered in 10-year increments. Ethnicity was categorised into six groups for analysis compiled using census categories (23): ‘Asian’ (Indian, Bangladeshi, Pakistani, Chinese or any other Asian background), ‘Black’ (Caribbean, African or any other black background), ‘White British’ (British), ‘White other’ (Irish or any other white background), ‘Other/mixed’ (White and Asian, White and Black Caribbean, White and Black African, any other ethnic group) and ‘Not stated’. Diagnoses are coded in structured fields in the source record according to the International Classification of Diseases, 10th Edition (ICD-10). Participants were categorised by ICD-10 codes (24) for primary diagnosis (recorded closest to 01.07.2019) as follows: F0x (organic mental disorders), F1x (psychoactive substance use), F2x (schizophrenia, schizotypal and delusional disorders), F3x (mood disorders), F4x (neurotic, stress-related and somatoform disorders), F5x (behaviour syndromes associated with physiological and physical factors), F6x (disorders of adult personality and behaviour), F7x (mental retardation), F8x (disorders of psychological development), F9x (behavioural and emotional disorders with onset during childhood and adolescence), ‘unspecified’ and ‘no axis 1’. In addition, post-traumatic stress disorder (PTSD; F43.1) was ascertained as an individual disorder of interest.
All analysis was conducted in R (version 4.1.2) using various packages (readr (25); dplyr (26); ggplot2 (27);). Descriptive statistics (means, standard deviations, frequencies, and percentages) of age, sex, ethnicity, and victimisation mentions were provided. Patients without any of the sociodemographic data were excluded from analysis. Chi square tests were also conducted to investigate victimisation differences between different demographic groups (age, sex, ethnicity) and diagnostic groups, supplemented by Cramér’s V effect sizes. These results were reported for any recorded violence victimisation, as well as specifically for domestic, physical, and sexual victimisation. Logistic regression analysis was conducted to investigate whether being part of a specific diagnostic group predicted mention of any recorded violence victimisation. Diagnostic groups were defined as separate binary variables for each diagnosis, (e.g., F0x diagnoses vs all other categories). Unadjusted models assessed age, sex, ethnicity, and each binary diagnostic group comparison in relation to presence or not of recorded experiences of recorded violence victimisation. Each of these models (for each sociodemographic variable and separate diagnostic group comparison) was then adjusted for age, sex, and ethnicity. The adjusted models were also conducted within males and female subsamples independently. For secondary analysis, unadjusted and adjusted regressions were conducted to measure whether being part of a specific diagnostic group predicted mention of physical, domestic, and sexual victimisation specifically. Bonferroni correction was used to adjust for multiple comparisons, whereby the alpha value was lowered to account for the number of comparisons performed (0.05 divided by number of tests conducted). P values from the regression analysis were considered significant if they were lower than the adjusted value. Multicollinearity tests using the R function vif() within the [car package] were undertaken to avoid issues with overlapping predictor variables. The predictor of being of age 91-100 was not added to the adjusted regressions, as it was highly correlated with other predictor age groups (with a VIF value above five (28)).
We present results of the violence prevalence analysis based on information extracted using NLP. A full evaluation of the NLP itself can be found in the previously published paper (15). The cohort comprised 60,021 individuals: 56,482 with a F0-F9 diagnosis, 3527 with an unspecified disorder and 12 with no axis 1 disorder recorded. Of the 56,482 individuals with a F0-F9 diagnosis, there were 27,191 (46.3%) with at least one victimisation mention: 26,038 (46.1%) with a mention of physical violence, 22,396 (39.7%) with domestic violence, and 13,558 (24.0%) with sexual violence. The mean (SD) age of the cohort was 37.6 (20.4) years. Distribution frequencies and Chi squared test results for associations with demographic variables and diagnostic group can be found in Table 1. Age, sex, ethnicity, and diagnostic group were all significantly associated with any victimisation, physical, domestic, and sexual victimisation mentions. For age groups, violence prevalence showed an inverted-U-shaped pattern of association with highest proportions in the 41-60y groups for all types. All victimisation types were more commonly recorded in women than men. For ethnicity, the highest prevalence of overall victimisation was within the Black ethnic group (62.3%), which was also observed for recorded physical and sexual violence victimisation specifically, but the highest prevalence of domestic victimisation was in the Other/Mixed group. For diagnostic groups, overall recorded violence victimisation prevalence was highest in patients with schizophrenia and related disorders (F2x) or personality disorders (F6x), the same being observed for physical violence. Recorded domestic and sexual violence victimisation prevalence were highest in those with personality disorder diagnoses. Considering effect sizes, as quantified by Cramér’s V statistic, these were moderate (0.2-0.6) for ethnicity and diagnosis and small (<0.2) for age and sex. Most did not vary substantially by violence category apart from sex which had higher effect sizes for domestic and sexual than physical violence, and ethnicity which was strongest for physical violence.
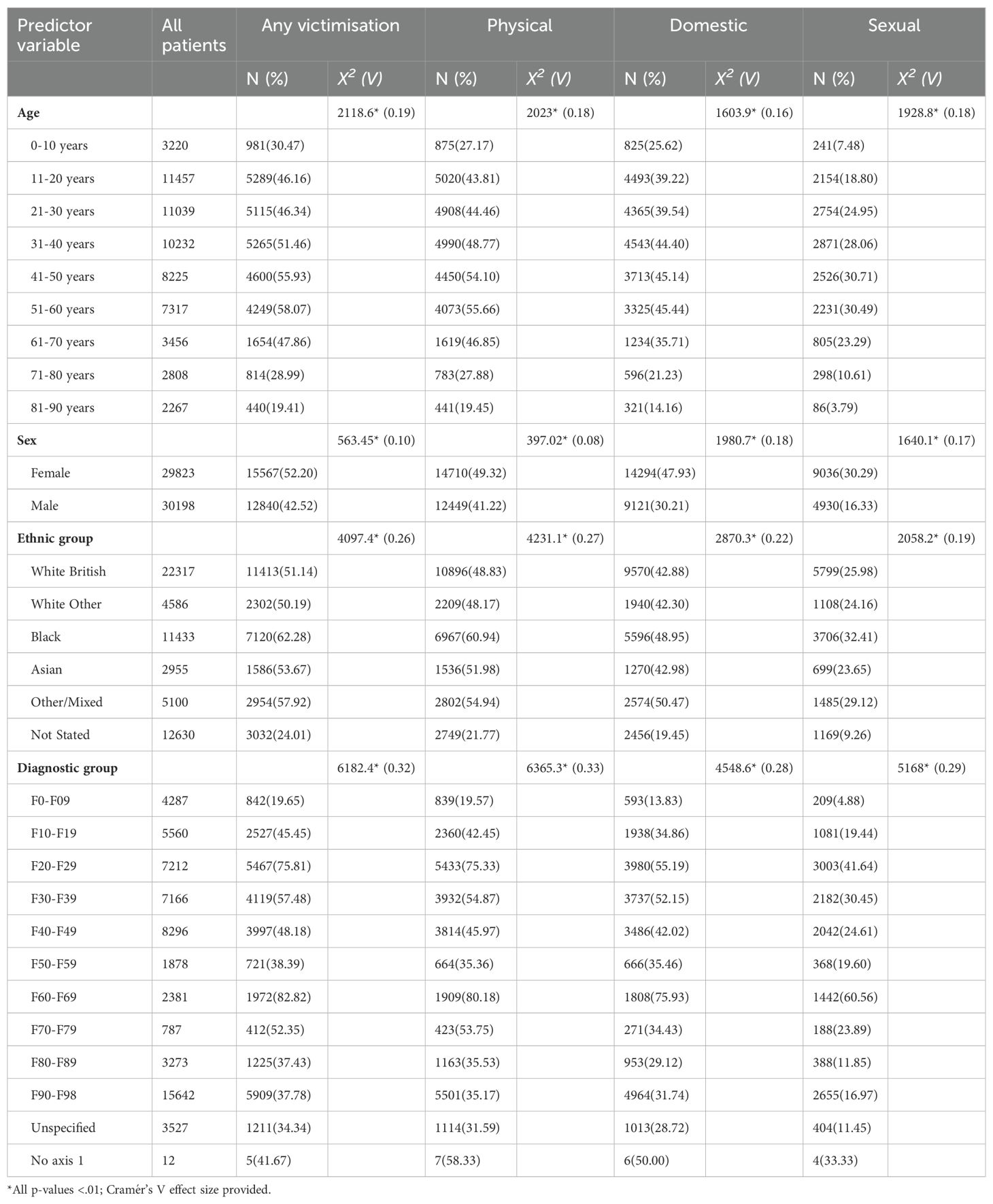
Table 1. Distribution frequencies (N(%)) and chi square test statistics measuring group differences in recorded violence victimization or specific physical, domestic, or sexual victimisation in 2019 for each age category, sex, ethnicity, and diagnostic group.
For overall recorded violence victimisation, results from unadjusted and adjusted logistic regression models are displayed in Table 2. In adjusted models, the same mid-life peaks in age distribution were observed as in unadjusted analyses, as were associations with female sex and with Black, Asian, and Other/Mixed ethnic groups compared to the White British reference. Additional analysis conducted in males and females separately found few differences between the sex of patients (Supplementary Table 1). For diagnoses, when analysed individually against all other diagnostic groups, significantly higher odds of recorded violence victimisation were observed in patients with schizophrenia and related disorders (F2x), affective disorders (F3x), PTSD, and personality disorders (F6x). In secondary analyses of specific violence types, findings were similar for physical and domestic violence (Supplementary Tables 2, 3, respectively). Findings for sexual violence differed in that no association was found with Asian ethnic groups compared to the White British reference; they were similar in all other respects (Supplementary Table 4).
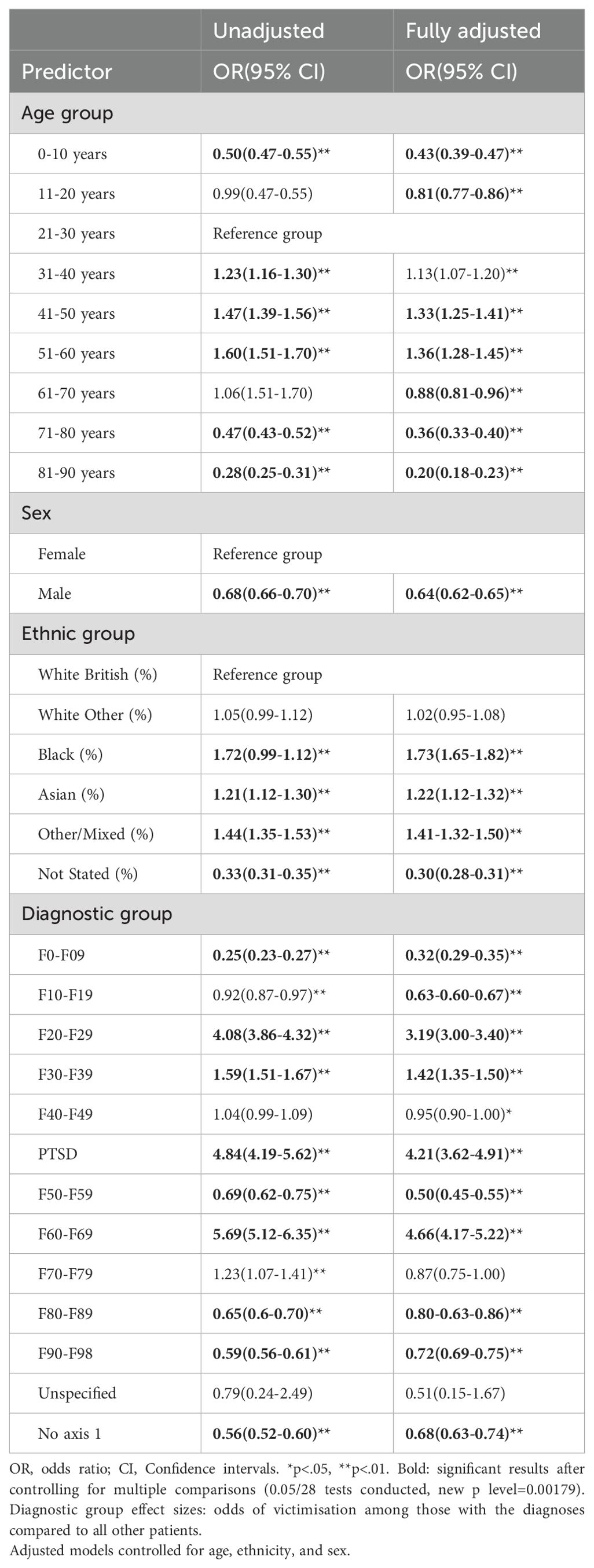
Table 2. Unadjusted and fully adjusted logistic regression models for having at least one record of violence victimisation (any type) in 2019.
To our knowledge, this is the first application of NLP algorithms to characterise recorded violence in a large corpus of mental health electronic health records. Considering distribution, violence was most commonly recorded in mid-life age groups, in women compared to men, in patients from minority ethnic groups compared to White groups, and among people diagnosed with schizophrenia and related disorders, affective disorders, PTSD and personality disorders, compared to those with other diagnoses.
The reported prevalence of violence in individuals with a severe mental illness has varied between 4% to 35% (5),, with prevalence of violence in patients with a general mental disorder being 15.2% (compared to 6.9% in those without) (29). Physical, domestic, and sexual violence were recorded in 46%, 40% and 24% of our sample of individuals with a diagnosis of a F0-F9 disorder. These absolute levels should be viewed cautiously in light of the performance levels of the algorithms, which we intend to develop further to improve characterisation accuracy. In particular, it should be borne in mind that status combinations (i.e., between ‘victimisation’ and each violence type) could only be applied at document level. It was therefore conceivable that the victimisation status applied to a different experience of violence in the same document (e.g., sexual violence might have been recorded as a perpetration event in the same document as physical violence received as victimisation, resulting in a false positive ascertainment for recorded sexual violence victimisation). Sub-optimal precision (positive predictive value) will have resulted in an over-estimation of exposure due to false positive instances, while sub-optimal recall (sensitivity) will have resulted in an under-estimation of exposure due to missed instances. Under-estimation will also clearly result from failure to ascertain or record experiences of violence in the source clinical record. Despite this, the associations with demographic and clinical factors, in the directions anticipated, support the applicability of these algorithms, at least as proxy markers of exposure, for analysis over large datasets, even if the performance levels achieved to date do not yet support their use for individual clinical decision support. Importantly, to our knowledge, there are currently no adequate means for quantifying recorded violence victimisation in mental healthcare records (or clinical records for any specialty), so we feel that the approach here at least represents a step towards more inclusive data capture. Relatively high prevalence of recorded violence is consistent with the 17% prevalence for any victimisation ascertained in case notes from a shorter (3-month) period early in the COVID-19 pandemic, a feature that was found to be prospectively associated with increased risk of acute care, emergency referrals, and mortality (30).
Recorded violence was ascertained most frequently in people with diagnoses of schizophrenia and related disorders, affective disorders, PTSD, and personality disorders. The vulnerability of patients within these diagnostic groups to experiences of interpersonal violence has been strongly supported in previous literature
(31–34). Therefore, our results support the notion of having increased screening (for all victimisation types) and victimisation support for these vulnerable groups. Unexpectedly, patients diagnosed with an organic disorder, substance misuse disorder, stress disorder (excluding PTSD), developmental disorder or a disorder with physiological disturbances had significantly less victimisation mentions than other disorders. Previous research has found at least some of these disorders to be risk factors for victimisation, such as research reporting higher rates of victimisation with a substance use disorder compared to those without (32). However, the observed low effect sizes may suggest that disorders such as schizophrenia should be considered a stronger risk factor. In interpreting these findings, it is important to bear in mind the purpose of the algorithm – namely to ascertain violence that has been clinically recorded. It is possible that the nature of some diagnoses encourages the ascertainment and recording of violence; for example, the diagnosis of PTSD would require identification and recording of an index traumatic event, and diagnoses of affective or personality disorders may prompt (and/or result from) a detailed enquiry as to relevant aetiology. In addition, it is important to bear in mind that longer and/or more intensive clinical contact, accompanied by more extensive health records, will increase the likelihood of events being recorded, something which was not adjusted for in these analyses. Patients with briefer contacts with mental healthcare are likely to have less detailed records, which might account for the lack of association with substance use disorder diagnoses. Of note, it is important to bear in mind that the diagnostic categories used in this analysis are very broad ones. There may well be within-category heterogeneity in associations, particularly within the larger groupings of patients with schizophrenia and related disorders, and mood disorders. Evaluation of more specific diagnostic sub-groups was not attempted in this study, aside from PTSD, and we feel that this would demand more specific investigation within broadly defined clinical groups (e.g., mood disorders) rather than across all mental health service users. However, more granular clinical phenotypes might be better ascertained via recorded symptom profiles than specific diagnostic codes, given the potential variability with which coding is likely to be applied in routine practice.
In relation to sociodemographic factors, patients from most minority ethnic groups had significantly higher risk of recorded violence victimisation compared to White British patients. While patients from minority ethnic groups face more barriers that reduce instances of disclosing victimisation in healthcare settings (35), the findings of higher recorded victimisation in these groups has been consistently highlighted in previous literature (36). Also supporting previous research (37), male patients were at a lower risk of victimisation mentions compared to females; this was consistent within all victimisation types. Future research could helpfully investigate whether incidents of victimisations differ between men and women within different diagnostic groups, to ascertain vulnerability and target further support.
The study described here has important strengths. Firstly, it provides novel findings on how sociodemographic factors and mental health diagnosis associate with the distribution of recorded violence victimisation within clinical record data. The 12-month time period for assessment allowed victimisation to be assessed across a representative sample of patients receiving secondary mental healthcare services, circumventing seasonal variation of victimisation (38, 39). In addition, 2019 was chosen as a recent time period, but one which preceded the COVID-19 pandemic and consequent disruption to services and, potentially, healthcare records. The large sample size increased the precision for the estimate of prevalence of violence mentions and allowed distributions to be investigated across a wide range of disorders. The development of the NLP victimisation application demonstrated the application of machine learning to unlock a complex but clinically important construct, utilising rich and diverse free-text data from a wide array of clinical professionals and groups (15). This approach helps to automate the measurement of victimisation, increasing the number of cases that can be investigated and providing a method that could be used more routinely to monitor victimisation in patients.
One of the important limitations of the NLP algorithm at its current stage of development is the requirement to combine features at document rather than instance level. This means that the algorithm could be raising documents with mixed experiences, e.g. a document raised by the algorithm as having a positive mention of violence victimisation may also include recorded instances of perpetrated violence. Therefore, prevalence of recorded victimisation should be considered with caution and further development of the NLP algorithm is needed to increase precision and recall. In addition, NLP can only be used to ascertain violence which, if it is recorded at all, is done so using terminology that can be reliably ascertained. This will inevitably underestimate true exposure where this is not enquired about and/or not reported by the patient and/or not recorded by the reviewing clinician (9, 40). Finally, the analyses presented here focused on relatively few characteristics as exposures, and only considered the primary diagnosis of the patient (and, as mentioned, within relatively broad diagnostic groupings), not including the additive effects of comorbid disorders that may strengthen or weaken the risk of victimisation.
Considering future directions, clearly further development is required to construct accurate NLP algorithms to allow combinations of features at instance level, and to differentiate more efficiently between witnessed, perpetrated, and experienced violence, as well as encompassing broader experiences (e.g., including emotional abuse). This would aid in our understanding of the complex relationship between violence and mental health diagnoses. Future research into the clinical benefits of synthesizing previous interpersonal violence experienced by patients could aid in the real time decision making of clinicians, although ethical challenges of using NLP methods in practice need to be considered (15).
The datasets presented in this article are not readily available due to the terms of Ethics and Information Governance approvals and clinical source of the data, CRIS datasets must remain within the SLaM firewall. All data used from this study can remade accessible on request fromcmlzLmFkbWluaXN0cmF0b3JAc2xhbS5uaHMudWs=with an appropriate research passport or appropriate SLaM honorary contract. Requests to access the datasets should be directed tocmlzLmFkbWluaXN0cmF0b3JAc2xhbS5uaHMudWs=.
The studies involving humans were approved by CRIS has a robust, patient-led governance and data security model and has approval as a data resource for secondary analysis (Oxford Research Ethics Committee C, reference 18/SC/0372). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
AM: Conceptualisation, Formal analysis, Writing - original draft, Writing - review & editing. VB: Writing - original draft, Writing - review & editing. RB: Resources, Methodology, Writing - original draft. DC: Methodology, Resources, Writing - original draft. LL: Methodology, Resources, Writing - original draft, Writing - review & editing. AM: Methodology, Resources, Writing - original draft. JS: Resources, Writing - original draft, GKS: Writing - original draft, Writing - review & editing. AR: Methodology, Resources, Writing - original draft. MW: Writing - original draft, Writing - review & editing. RS: Funding acquisition, Methodology, Resources, Supervision, Writing - original draft, Writing - review & editing.
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. AM, JS, DC, and RS are part-funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust and King’s College London. RS is additionally funded by i) the National Institute for Health Research (NIHR) Applied Research Collaboration South London (NIHR ARC South London) at King’s College Hospital NHS Foundation Trust; ii) the DATAMIND HDR UK Mental Health Data Hub (MRC grant MR/W014386); iii) the UK Prevention Research Partnership (Violence, Health and Society; MR-VO49879/1), an initiative funded by UK Research and Innovation Councils, the Department of Health and Social Care (England) and the UK devolved administrations, and leading health research charities. The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care. VB is funded by an NIHR Advanced Fellowship NIHR302243 administered by KCL. GK-S has received salary support from the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London; and has also received funding from a researcher-initiated grant from the Violence and Abuse Mental Health Network (VAMHN) UKRI.
RS declares research support received in the last 3 years from Janssen, GSK, and Takeda. GK-S has received research funding from Janssen and H Lundbeck.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2024.1181739/full#supplementary-material
1. Krug GE, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet. (2002) 360:1083–88. doi: 10.1016/S0140-6736(02)11133-0
2. Reza A, Mercy JA, Krug E. Epidemiology of violent deaths in the world. Injury Prev. (2001) 7:104–11. doi: 10.1136/ip.7.2.104
3. Olofsson N, Lindqvist K, Shaw BA, Danielsson I. Long-term health consequences of violence exposure in adolescence: A 26–year prospective study. BMC Public Health. (2012) 12:1–11. doi: 10.1186/1471-2458-12-411
4. López-Martínez AE, Serrano-Ibáñez ER, Ruiz-Párraga GT, Gómez-Pérez L, Ramírez-Maestre C, Esteve R. Physical health consequences of interpersonal trauma: A systematic review of the role of psychological variables. Trauma Violence Abuse. (2018) 19:305–22. doi: 10.1177/1524838016659488
5. Maniglio R. Severe mental illness and criminal victimization: a systematic review. Acta Psychiatrica Scandinavica. (2009) 119:180–91. doi: 10.1111/j.1600-0447.2008.01300.x
6. Khalifeh H, Moran P, Borschmann R, Dean K, Hart C, Hogg J, et al. Domestic and sexual violence against patients with severe mental illness. psychol Med. (2015) 45:875–86. doi: 10.1017/S0033291714001962
7. Khalifeh H, Johnson S, Howard LM, Borschmann R, Osborn D, Dean K, et al. Violent and non-violent crime against adults with severe mental illness. Br J Psychiatry. (2015) 206:275–82. doi: 10.1192/bjp.bp.114.147843
8. Mullen PE. Schizophrenia and violence: from correlations to preventive strategies. Adv Psychiatr Treat. (2006) 12:239–48. doi: 10.1192/apt.12.4.239
9. Howard LM, Trevillion K, Agnew-Davies R. Domestic violence and mental health. Int Rev Psychiatry. (2010) 22:525–34. doi: 10.3109/09540261.2010.512283
10. Hildersley R, Easter A, Bakolis I, Carson L, Howard LM. Changes in the identification and management of mental health and domestic abuse among pregnant women during the COVID-19 lockdown: regression discontinuity study. BJPsych Open. (2022) 8:e96. doi: 10.1192/bjo.2022.66
11. Robson D, Spaducci G, McNeill A, Stewart D, Craig TJ, Yates M, et al. Effect of implementation of a smoke-free policy on physical violence in a psychiatric inpatient setting: an interrupted time series analysis. Lancet Psychiatry. (2017) 4:540–6. doi: 10.1016/S2215-0366(17)30209-2
12. Bhavsar V, Sanyal J, Patel R, Shetty H, Velupillai S, Stewart R, et al. The association between neighbourhood characteristics and physical victimisation in men and women with mental disorders. BJPsych Open. (2020) 6:e73. doi: 10.1192/bjo.2020.52
13. Cullen AE, Bowers L, Khondoker M, Pettit S, Achilla E, Koeser L, et al. Factors associated with use of psychiatric intensive care and seclusion in adult inpatient mental health services. Epidemiol Psychiatr Sci. (2018) 27:51–61. doi: 10.1017/S2045796016000731
14. Wang Y, Wang L, Rastegar-Mojarad M, Moon S, Shen F, Afzal N, et al. Clinical information extraction applications: a literature review. J Biomed Inf. (2018) 77:34–49. doi: 10.1016/j.jbi.2017.11.011
15. Botelle R, Bhavsar V, Kadra-Scalzo G, Mascio A, Williams MV, Roberts A, et al. Can natural language processing models extract and classify instances of interpersonal violence in mental healthcare electronic records: an applied evaluative study. BMJ Open. (2022) 12:e052911. doi: 10.1136/bmjopen-2021-052911
16. Florence C, Shepherd J, Brennan I, Simon T. Effectiveness of anonymised information sharing and use in health service, police, and local government partnership for preventing violence related injury: experimental study and time series analysis. BMJ. (2011) 342:1–9. doi: 10.1136/bmj.d3313
17. Kadra-Scalzo G, Kornblum D, Stewart R, Howard LM. Adverse outcomes associated with recorded victimization in mental health electronic records during the first UK COVID-19 lockdown. Soc Psychiatry Psychiatr Epidemiol. (2023) 58:431–40. doi: 10.1007/s00127-022-02393-w
18. Stewart R, Soremekun M, Perera G, Broadbent M, Callard F, Denis M, et al. The South London and Maudsley NHS foundation trust biomedical research centre (SLAM BRC) case register: development and descriptive data. BMC Psychiatry. (2009) 9:1–12. doi: 10.1186/1471-244X-9-51
19. Perera G, Broadbent M, Callard F, Chang C-K, Downs J, Dutta R, et al. Cohort profile of the South London and Maudsley NHS Foundation Trust Biomedical Research Centre (SLaM BRC) case register: current status and recent enhancement of an electronic mental health record-derived data resource. BMJ Open. (2016) 6:e008721. doi: 10.1136/bmjopen-2015-008721
20. Lee J, Yoon W, Kim S, Kim D, Kim S, So CH, et al. BioBERT: a pre-trained biomedical language representation model for biomedical text mining. Bioinformatics. (2020) 36:1234–40. doi: 10.1093/bioinformatics/btz682
21. Hugging_face, Read Rectangular Text Data . Available online at: https://huggingface.co/docs/transformers/en/model_doc/bert (Accessed 26 April 2024).
22. Maudsley, CRIS NLP service . Available online at: https://www.maudsleybrc.nihr.ac.uk/media/325736/applications-library-v13.pdf (Accessed 26 April 2024).
23. GOV.UK, List of ethnic groups: GOV.UK (2022). Available online at: https://www.ethnicity-facts-figures.service.gov.uk/style-guide/ethnic-groups#2021-census (Accessed 26 April 2024).
24. WHO. The ICD-10 classification of mental and behavioural disorders. Geneva, Switzerland: World Health Organization (1993).
25. Wickham H, et al. Package ‘readr’. Read Rectangular Text Data . Available online at: https://cran.r-project.org/web/packages/readr/readr.pdf (Accessed 23 August 2023).
26. Wickham H, François R, Henry L, Müller K. dplyr: A Grammar of Data Manipulation. R package version 0.7. 6. (2018). https://github.com/tidyverse/dplyr.
28. Hair JF, Risher JJ, Sarstedt M, Ringle CM. When to use and how to report the results of PLS-SEM. Eur Business Rev. (2019) 31:2–24. doi: 10.1108/EBR-11-2018-0203
29. Silver E, Arseneault L, Langley J, Caspi A, Moffitt TE. Mental disorder and violent victimization in a total birth cohort. Am J Public Health. (2005) 95:2015–21. doi: 10.2105/AJPH.2003.021436
30. Kadra G, Dean K, Hotopf M, Hatch SL. Investigating exposure to violence and mental health in a diverse urban community sample: data from the South East London Community Health (SELCoH) survey. PloS One. (2014) 9(4):e93660. doi: 10.1371/journal.pone.0093660
31. Kooyman I, Dean K, Harvey S, Walsh E. Outcomes of public concern in schizophrenia. Br J Psychiatry. (2007) 191:s29–36. doi: 10.1192/bjp.191.50.s29
32. Fazel S, Gulati G, Linsell L, Geddes JR, Grann M. Schizophrenia and violence: systematic review and meta-analysis. PloS Med. (2009) 6:e1000120. doi: 10.1371/journal.pmed.1000120
33. Labrum T, Solomon P, Marcus S. Victimization and perpetration of violence involving persons with mood and other psychiatric disorders and their relatives. Psychiatr Serv. (2020) 71:498–501. doi: 10.1176/appi.ps.201900384
34. Mazza M, Marano G, Del Castillo AG, Chieffo D, Monti L, Janiri D, et al. Intimate partner violence: A loop of abuse, depression and victimization. World J Psychiatry. (2021) 11:215. doi: 10.5498/wjp.v11.i6.215
35. Heron RL, Eisma MC, Browne K. barriers and facilitators of disclosing domestic violence to the UK health service. J Family Violence. (2022) 37:533–43. doi: 10.1007/s10896-020-00236-3
36. Policastro C, Teasdale B, Daigle LE. The recurring victimization of individuals with mental illness: a comparison of trajectories for two racial groups. J Quantitative Criminology. (2016) 32:675–93. doi: 10.1007/s10940-015-9271-8
37. Yapp E, Booth T, Davis K, Coleman J, Howard LM, Breen G, et al. Sex differences in experiences of multiple traumas and mental health problems in the UK Biobank cohort. Soc Psychiatry Psychiatr Epidemiol. (2021) 58(12):1819–31. doi: 10.1007/s00127-021-02092-y
38. Koutaniemi EM, Einiö E. Seasonal variation in seeking help for domestic violence based on Google search data and Finnish police calls in 2017. Scandinavian J Public Health. (2021) 49:254–9. doi: 10.1177/1403494819834098
39. Farrell G, Pease P. CRIM SEASONALITY: domestic disputes and residential burglary in Merseyside 1988–90. Br J Criminology. (1994) 34:487–98. doi: 10.1093/oxfordjournals.bjc.a048449
Keywords: natural language processing, victimisation, mental health records, CRIS, violence
Citation: Mason AJC, Bhavsar V, Botelle R, Chandran D, Li L, Mascio A, Sanyal J, Kadra-Scalzo G, Roberts A, Williams M and Stewart R (2024) Applying neural network algorithms to ascertain reported experiences of violence in routine mental healthcare records and distributions of reports by diagnosis. Front. Psychiatry 15:1181739. doi: 10.3389/fpsyt.2024.1181739
Received: 07 March 2023; Accepted: 14 August 2024;
Published: 10 September 2024.
Edited by:
Farhad Soleimanian Gharehchopogh, Hacettepe University, TürkiyeReviewed by:
Zhihao Ma, Nanjing University, ChinaCopyright © 2024 Mason, Bhavsar, Botelle, Chandran, Li, Mascio, Sanyal, Kadra-Scalzo, Roberts, Williams and Stewart. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ava J. C. Mason, YXZhLm1hc29uLjIwQHVjbC5hYy51aw==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.