
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 19 October 2023
Sec. Public Mental Health
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1272959
This article is part of the Research TopicElucidating the Determinants Between the Environment and Individuals’ Behaviors Amidst the COVID-19 Pandemic and the Post-COVID EraView all 25 articles
 Carla Comacchio1
Carla Comacchio1 Maddalena Cesco1
Maddalena Cesco1 Rosita Martinelli1
Rosita Martinelli1 Marco Garzitto1
Marco Garzitto1 Rita Bianchi1
Rita Bianchi1 Nicola Innocente1
Nicola Innocente1 Emanuela Sozio2
Emanuela Sozio2 Carlo Tascini2
Carlo Tascini2 Matteo Balestrieri1
Matteo Balestrieri1 Marco Colizzi1,3*
Marco Colizzi1,3*Introduction: Vaccination against SARS-CoV-2 has been used to reduce the severity of COVID-19 disease and the incidence of new cases. However, a significant proportion of people have shown vaccination hesitancy.
Methods: This study explored psychological factors related to vaccination hesitancy in a sample of Italian COVID-19 patients (N = 54), hospitalized during 2021, after vaccines had been made available and while the vaccination campaign was on-going. Consecutive patients, aged 18 or older, admitted to the hospital with a diagnosis of COVID-19 were assessed with a set of standardized measures.
Results: In our sample, 48.1% was not vaccinated and 7.4% died within 6months after hospitalization, with a preponderance of deaths among non-vaccinated patients. Non-vaccinated participants had higher resilience scores at the CD-RISC-10 scale than vaccinated ones (33.6 ± 5.50 vs 28.6 ± 6.61; t40.2=+ 2.94, p = 0.005). No statistically significant differences were found between the two groups for any other measures.
Discussion: Higher levels of resilience among non-vaccinated patients may reflect greater identity worth and self-esteem, in turn resulting in a decrease in vaccination likelihood. This finding may have important public health implications, as it indicates that specific psychological aspects, such as resilience, may result in vaccination hesitancy, with implications for hospitalization rates, and thus healthcare costs, as well as loss of lives.
COVID-19 is the name of the disease caused by the new coronavirus SARS-CoV-2, discovered in China in December 2019. It was declared by the World Health Organization (WHO) to be a global pandemic in March 2020 (1). Over 600 million people have suffered from COVID-19 and almost 6 million have died by March 10th, 2023, because of the disease (2). The virus spread very quickly around the world, resulting in the decision to implement restrictive measures by public health services, such as social and physical distancing, travel restrictions, use of personal protective equipment, confinement (quarantine), and hygiene measures. Common symptoms of COVID-19 include a dry cough, fever or chills, shortness of breath or difficulty breathing, muscle or body aches, sore throat, loss of taste or smell, diarrhea, headache, fatigue, nausea or vomiting, and congestion or a runny nose. However, the impact of COVID-10 has not been limited to physical health. The virus itself (direct effect) (3) and the measures applied by institutions (indirect effect) (4) have contributed to worsening the quality of life and mental health of the general population (5), along with a higher risk of relapse in individuals with mental health issues before the start of the pandemic (6). Vaccination against SARS-CoV-2 has been used to reduce the severity of COVID-19 disease and the incidence of new cases, leading to a significant change in the course of the pandemic and eventually relaxing restrictions and confinements. Moreover, it has been helpful to minimize possible permanent adverse health consequences and to avoid collapse of the health care systems. However, the success of a vaccination campaign does not depend only on its efficacy and safety, but also on the level of the vaccine acceptance, that may jeopardize the successful control of an infectious disease (7). Reaching out and vaccinating people who accept vaccination is obviously crucial, however the real challenge is to convince reluctant persons to vaccinate. Another factor that influenced the success of the vaccination campaign is represented by the introduction of certain laws that have contributed to increasing the vaccination rate in certain population groups (8, 9). Analyzing data from 33 countries, a recent systematic review found significant variation in terms of COVID-19 vaccine acceptance, with Italy being one of the countries with the lowest levels (10), possibly causing delays in reaching the target population immunization rate (11). Thus, studies are needed to identify predictors of vaccination hesitancy, including psychological characteristics (12), with the goal of mitigating its detrimental effects on control of infectious disease. The aim of the present study was to evaluate the prevalence of vaccination hesitancy in a cohort of COVID-19 hospitalized patients in Italy during a later phase of the pandemic, when the vaccine was already available, and the vaccination campaign was ongoing. Furthermore, the study aimed at identifying psychological factors associated with vaccination hesitancy.
This is an observational study. It was conducted at the University hospital of Udine, a tertiary referral hospital of nearly 1,000 beds serving approximately 350,000 inhabitants, which has been appointed as regional hub for COVID-19 patients. The recruitment started on March 20th 2021 and ended December 31st 2022. All consecutive patients, aged 18 or older, admitted at the Infectious Disease Department with a diagnosis of COVID-19 confirmed by molecular swab, were considered eligible for inclusion. For those patients expressing willingness to participate, written informed consent was obtained before data collection. Since interviews were conducted via telephone, exclusion criteria included being unable to undertake a telephone interview due to any medical or psychological condition. The study was conducted in accordance with the Declaration of Helsinki and approved by the local Ethics Committee (CEUR-2021-OS-19).
Vaccination status for COVID-19 together with sociodemographic information were collected using an ad hoc form. Cognitive status was assessed with a back-translated version of the original English Telephone Interview for Cognitive Status (TICS) developed by Brandt in 1988 (13). TICS score ranges from 1 to 41 and comprises 11 items assessing orientation (personal, temporal, and spatial; score range: 0–12), attention and executive functioning (backward counting, backward calculation, abstraction; range: 0–9), language (naming to description, sentence repetition, and oral comprehension; range: 1–8), and memory (immediate recall, semantic memory; range: 0–12). Resilience was assessed with the Connor–Davidson resilience scale (CD-RISC-10). This is the abridged version of a 25-items self-report scale developed by Connor and Davidson in 2003 (14). It measures characteristics such as persistence, optimism, and confidence in ability to cope, with higher score indicating better resilience (15). Illness perception was assessed with the Brief illness perception questionnaire (IPQ-B), developed by Broadbent in 2006 (16). It is an eight-item scale that has each item rated on a scale from 0 (minimum) to 10 (maximum) and which assesses the emotional and cognitive aspects of an individual’s illness. Each item of this questionnaire examines a dimension of understanding of the disease as follows: 1. Consequences; 2. Timeline; 3. Personal control; 4. Treatment control; 5. Identity; 6. Concern; 7. Illness comprehensibility; 8. Emotions. The IPQ-B also includes a question that is answered by the patient about one’s opinion regarding the cause of illness. Items 1–5 assess the cognitive dimensions which relate to understanding of illness, its causes, and effect of treatment, while items 6 to 8 evaluate the emotional dimensions that relate to emotions such as mood, fear, anxiety, or anger. The total score of illness perception is calculated by inverting the score for items 3, 4 and 7 and added to the score of the other items. The maximum total score is 80 and the minimum total score is 0. A higher score indicates a more threatening view of the patient, while a lower score indicates a more optimistic view of the disease. Family function was assessed with the Family APGAR (17). It is a 5-item questionnaire (with each item rated on a 3-point scale) measuring five constructs: 1. Adaptability; 2. Partnership; 3. Growth; 4. Affection; and 5. Resolve. Scores range from 0 to 10 with higher scores indicating better functionality. Protective and risk factors after a potential traumatic event were assessed with the Global Psychodrama Screen (GPS, version 1.2), developed by the ‘Global Collaboration on Traumatic Stress’ (18). It consists of 22 items, 17 symptom items and 5 risk or protective factors, each to be answered in a yes/no format. The 17 symptom items assess: PTSD symptoms; affective dysregulation and negative self-concept; depression symptoms; anxiety symptoms; dissociation; sleep problems; self-injurious behavior; substance abuse; and other problems (physical, emotional, or social). The five risk or protective items assess other stressful events; social support; traumatic life events in childhood; history of psychiatric treatment; and resilience. The GPS total score is calculated using all 22 items, ranging 0–22. A total symptom score is the sum score of the 17 symptom items (range 0–17). A risk factor score is the sum score of the five risk or protective items (range 0–5). The Mini Locus of Control Scale (MLCS) has been used to assess self-perception of control over external events (19). It consists of 6 items. People were asked to state their level of agreement according to a 4-point scale: totally (4); enough (3); little (2); not at all (1). It comprises three main subscales: 1. Fatalism, the random play of external circumstances (“There are those who are born lucky and those who are not”; “Without the right opportunities, it is difficult to succeed in life”); 2. Hetero-dependence, the influence exerted by the social environment (“My life is controlled mainly by the influence of other people”; “It is others who decide whether you succeed in your life or not”); and 3. Internality, the personal wills capabilities (“People could do so much more, if only they really tried”; “It’s entirely up to me if I can take advantage of the opportunities life gives me”).
Categorical measures were summarized with percentage frequencies; mean, standard deviation (SD), and range of variation were reported for continuous measures. Fisher’s exact test was used in cross- tables with categorical measures (also reporting Odd-ratios, OR, with their 95% confidence interval, ci). In between-group comparisons, Welch’s corrected t-test (or Mann–Whitney’s test) or one-way analysis of variance were used with continuous measures (checking homoskedasticity with median-centered Levene’s test). Also, Pearson’s correlations were calculated (reporting estimated correlation with its 95% ci). Finally, multiple linear regression was fitted reporting its coefficient of determination (R2; also adjusted for the number of covariates) and statistical significance; for predictors, tolerances and standardized coefficient (β) with statistical significance were reported. Pair-wise deletion on missing data was adopted. The statistical significance was set to p < 0.050. Analyzes were conducted with R-4.2.3 (R Development Core Team, 2023).
Sociodemographic and clinical characteristics of the sample, including details about vaccination status, are described in Table 1. Considering the overall sample, 48.1% of patients were not vaccinated. 7.4% of participants died within 6 months after hospitalization [3.2 ± 1.78 (1.2, 5.0) months]. It was observed a preponderance of deaths in the non-vaccinated group (16.7%) when compared with the vaccinated group [2.8%; OR = 6.727 (IC 95% 0.495, 376.765)]. No statistically significant differences were observed between participants who have been vaccinated and those who were not for age at hospitalization (U = 276.0, p = 0.944), sex [OR = 1.528 (IC 95% 0.360, 7.842)], being single [OR = 1.118 (IC 95% 0.304, 4.044)], living alone [OR = 1.898 (IC 95% 0.385, 9.073)], having a low-level of schooling [OR = 0.468 (IC 95% 0.092, 1.948)], working [OR = 0.705 (IC 95% 0.175, 2.612)], having physical comorbidities [OR = 1.000 (IC 95% 0.181, 7.039)], being under psychopharmacological treatment [OR = 2.699 (IC 95% 0.269, 137.102)], and duration of hospitalization (t27.4 = +0.23, p = 0.821).
Results of the self-assessment tests are provided in Table 2. Non-vaccinated participants had higher total scores at the CD-RISC-10 than vaccinated ones (33.6 ± 5.50 vs. 28.6 ± 6.61; t40.2 = +2.94, p = 0.005), in particular they were less represented in the lower quartile [16.6% vs. 83.3%; OR = 0.235 (IC 95% 0.047, 0.943)], without statistically significant differences for distribution in other quartiles (all with p ≥ 0.273; Table 3). Instead, no statistically significant differences resulted between the two groups for having an internal locus of control [MLCS: OR = 1.488 (IC 95% 0.352, 6.024)], for cognitive status (I-TIC: t47.8 = +0.68, p = 0.498), for having a dysfunctional family [Family-Apgar: OR = 1.488 (IC 95% 0.352, 6.024)], for illness perception (Brief-IPQ total score: t37.0 = +0.06, p = 0.954; with p ≥ 0.091, for single items), and for presenting with psycho-traumatic symptoms (GPS symptoms: t33.8 = −0.55, p = 0.587; with p ≥ 0.083, for sub-scales and specific symptoms). Going into more detail (see Figure 1), the number of vaccine doses was significantly associated to the total CD- RISC-10 score (F3,50 = 3.91, p = 0.014), lowering from those who had not been vaccinated (33.6 ± 5.50) to those who had received three doses [27.0 ± 6.33; in post-hoc: Δ = +6.6 (+1.3, +11.9), p = 0.009]. Consistently, considering the distinction between participants who were vaccinated before hospitalization (i; CD-RISC-10: 28.1 ± 6.41), those vaccinated after hospitalization (ii; 30.3 ± 7.48), and those never vaccinated (iii; 33.6 ± 5.50), we observed a statistically significant difference (F2,51 = 4.17, p = 0.021), in particular between those vaccinated before hospitalization and those never vaccinated [Δ = +5.5 (+0.9, +10.1), p = 0.015].
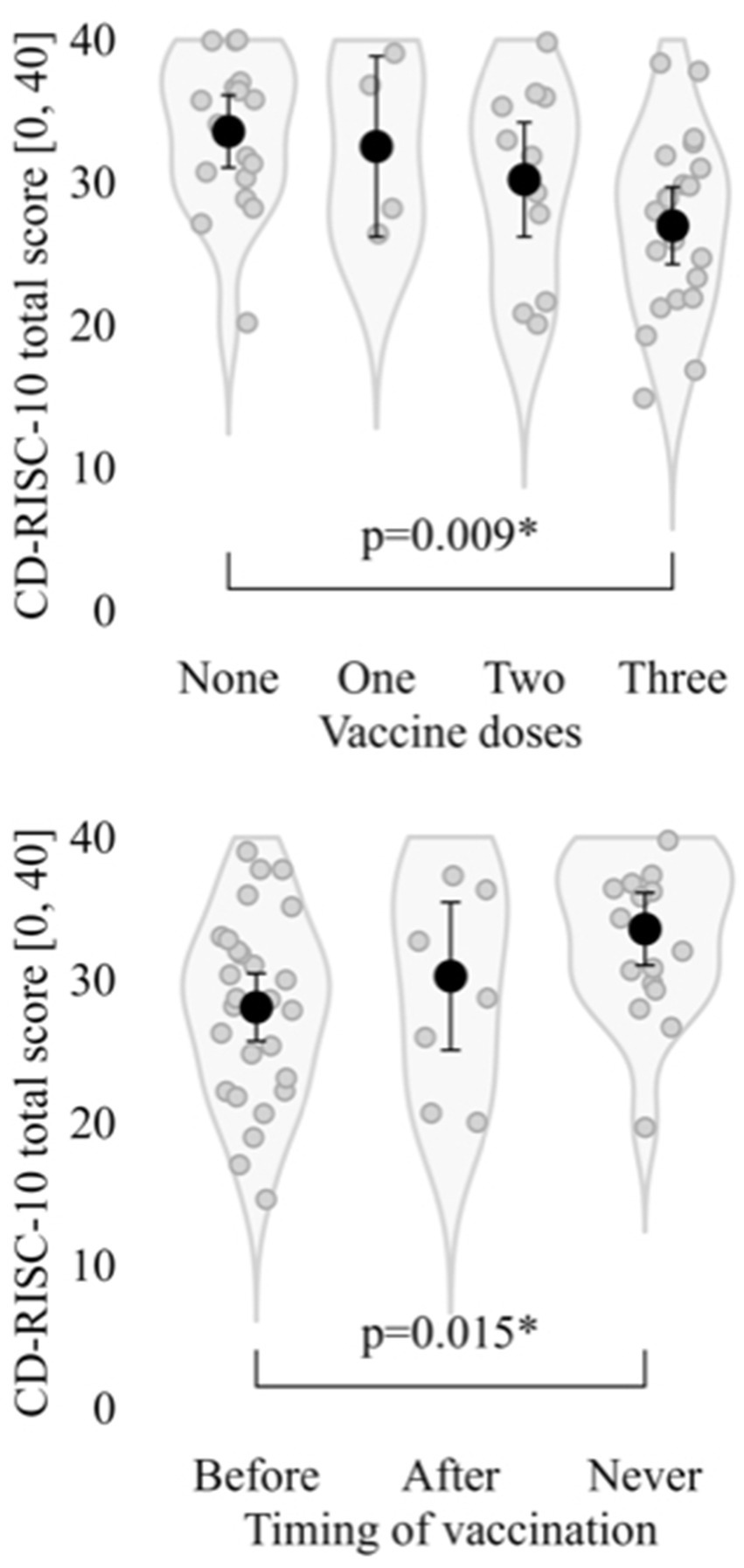
Figure 1. Total score at CD-RISC-10 by number of vaccine doses and timing of vaccination with reference to hospitalization. CD-RISC-10: Connor-Davidson’s Resilience Scale, 10-items. *: Statistically significant with p.
The CD-RISC-10 total score was not associated with age at hospitalization [r = −0.130 (−0.392, +0.151)], being single (t44.4 = +0.09), living alone (t13.4 = +1.04), having a low-level of schooling (t28.3 = +0.81), working (t46.1 = −1.77), having physical comorbidities (t11.3 = −1.42), being under psychopharmacological treatment (U = 126.0) and duration of hospitalization [r = −0.049 (−0.326, +0.235)]. Resilience was also not significantly associated with internal locus of control at the MLCS (t33.5 = −0.70) or symptoms at the GPS [r = −0.198 (−0.442, +0.074)]. Instead, males scored higher than females (31.4 ± 6.47 vs. 27.1 ± 6.30; t26.1 = −2.22) and the resilience score was found to be associated with the I-TIC score [r = +0.407 (+0.151, +0.612)], having a dysfunctional family according to the Family-Apgar questionnaire (t7.5 = +2.62) and the Brief-IPQ score [r = −0.293 (−0.520, −0.028)]. When statistically significant moderators were considered together (tolerance ranging between 0.819 and 0.976), the multiple regression was statistically significant (R2 = 0.568, adjusted to 0.510; F5,37 = 9.75). As can be seen in Figure 2, not being vaccinated was still shown to have a statistically significant association with resilience score (β = +0.771), cognitive status (I-TIC score: β = +0.412) and having a dysfunctional family (Family-Apgar: β = −1.062). The introduction of covariates reduced the β of vaccination by 7.9%.
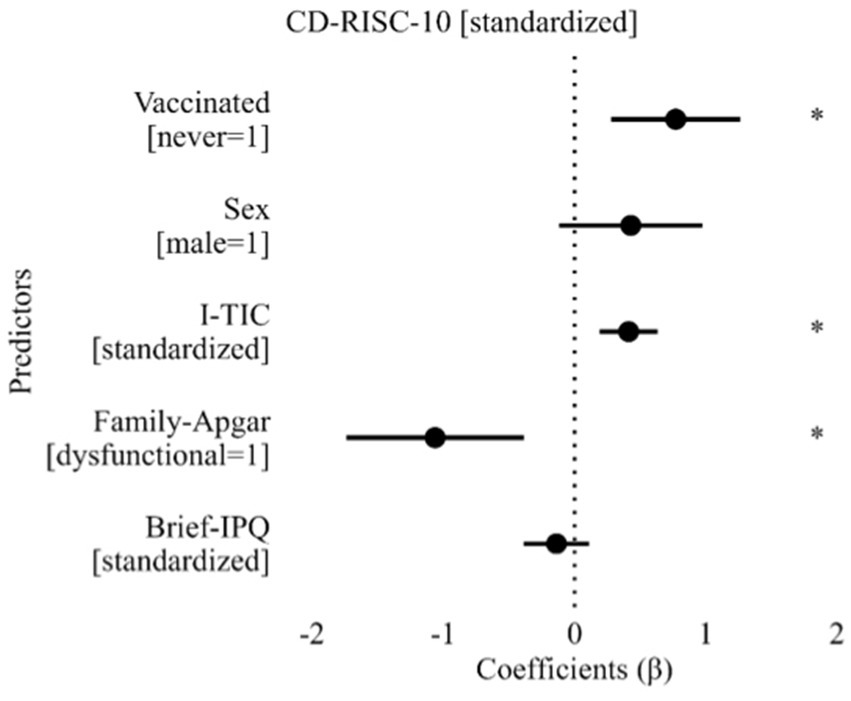
Figure 2. Results of multiple linear regression for CD-RISC-10 score. Brief-IPQ: Brief Illness Perception Questionnaire; CD-RISC-10: Connor-Davidson’s Resilience Scale, 10-items; Family-Apgar: Family Apgar; I-TIC: Telephone Interview for Cognitive Status, Italian version. *: Statistically significant predictor with p.
The COVID-19 global health emergency officially started on January 30th 2020 and ended on May 5th 2023. Incidence rates fluctuated over time and in Italy have been divided into four waves (20). The first wave happened during February–May 2020, the second during October–December 2020, the third during January–May 2021 and the fourth during November 2021–March 2022. The vaccination campaign started on December 27th 2020 and is still ongoing. This study has been conducted between the third and the fourth wave, when the percentage of vaccinated people increased from 24 to 80% (21), achieving the target population immunization rate (22). In the overall sample, 48.1% of patients were not vaccinated (i.e., with a ratio of 1.1 vaccinated persons for every non-vaccinated person), against an expectation of 15.9% (i.e., expected ratio: 5.3) (23). Such finding is in line with the higher risk of suffering from a form of COVID-19 requiring hospitalization among non-vaccinated individuals found in the relevant literature (24). A clinically significant higher mortality was also observed among non-vaccinated individuals (24). In a study conducted in 26 European countries in the same time period, the percentage of people declining COVID-19 vaccination was around 26% (25). Despite vaccination being among the key strategies implemented to limit the spread of the virus and improve health outcomes and life expectancy (26), a significant proportion of people have shown high levels of hesitancy. Vaccine hesitancy is a complex phenomenon, and it is influenced by several factors, including perceived need for the vaccine, accessibility of the vaccine, and perceived benefits and safety of the vaccine (25). Reduced vaccination intentions have been associated with female gender (27–33), high trust in media information sources (29, 34), low levels of trust in information from government sources, high conspiracy-mindedness (29), fear of side effects, and preference for a natural lifestyle (35). On the contrary, willingness to receive the vaccine has been associated with high education, high economic status, high perceived risk of infection (36–38), living with people with poor health, viewing vaccinations as a moral norm (39), positive attitude toward vaccines and previous vaccination (40), fear of COVID-19 and high levels of resilience (41). This study did not find any association between vaccination hesitancy and gender, economic status, and level of education. However, higher levels of resilience were found among non-vaccinated people, and such a result is worth of attention. Resilience refers to the process of bouncing back from difficult experiences and adapting well in the face of adversity, trauma, tragedy, threats, or significant sources of stress (42). It can be conceptualized at the individual (i.e., a stable trajectory of healthy functioning after a highly adverse event) (43), community (i.e., the success of the community to provide for the needs of its members and the extent to which individuals are helped by their community) (44), and societal (i.e., the perceived ability of the society to successfully deal with adversities and quickly recover after the threat has been removed) (45) levels. Individual resilience is closely related to identity resilience, that reflects the individual’s subjective belief in their capacity to understand and overcome challenges, their self-worth and value, their positive distinctiveness from others, and their certainty about who they have been and will remain (46). Identity resilience has two key components, which are identity worth, comprising self-efficacy, self-esteem, and positive distinctiveness, and identity continuity, depending upon feeling that the uniqueness and meaning of their identity persists over time (46). Regarding COVID-19, it has been found that identity worth is associated with less COVID-19 fear and less perceived COVID-19 risk, which could possibly result in a decrease in vaccination likelihood. One of the elements that define identity worth is self-esteem, and high levels of self-esteem have been associated with both healthy behaviors (47) and reduced probability of influenza vaccination (48). This has been explained by the tendency of individuals with high self-esteem to ignore disagreeable information and assume that calamities cannot happen, which can lead to declining vaccination (47). Thus, we can speculate that high levels of resilience among non-vaccinated people in our sample may be explained by high levels of identity worth and self-esteem.
It is worth mentioning that the high levels of vaccination hesitancy in our sample may result from the complex Italian sociopolitical situation during the pandemic. Italy was the first European country to be hit by the COVID-19 and since then several television personalities, politicians, media outlets, and even scientists have contributed to spreading conflicting and misleading information (49). This has generated a climate of uncertainty that has compromised trust in institutions, whose non- pharmacological interventions were often cataloged as exaggerated, and altered the risk perception of the population (50). The lack for trust in institutions has been related with an increase in vaccination hesitancy (51).
Limitations of this study include the single assessment performed during COVID-19-related hospitalization. In the absence of resilience information obtained outside of such a context, a confounding effect of hospitalization for COVID-19 cannot be ruled out. This may be particularly relevant for vaccinated individuals, whose resilience may have suffered a reduction for failing to avoid hospitalization despite having received one or more vaccine doses. Nevertheless, the current work may have important public health implications, as it indicates that specific psychological aspects, such as resilience, may modulate vaccination hesitancy, with implications for hospitalization rates, and thus healthcare costs, as well as loss of lives.
We carried out an observational study in order to explore psychological factors related to vaccination hesitancy in a sample of patients hospitalized for COVID-19 in a later phase of the pandemic when vaccines had been made fully available to the general population. We found higher resilience scores in non-vaccinated patients compared to vaccinated ones. This result may be explained by high levels of identity worth and self-esteem among non-vaccinated people, making them less prone to vaccination. Future studies will have to focus not only on psychological but also on broader socio-behavioral determinants of compliance with health and mental care recommendations (e.g., lack of trust in institutions), in order to better understand the vaccination hesitancy phenomenon.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by Unique Regional Ethics Commitee (CEUR-2021-OS-19). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
CC: Conceptualization, Data curation, Methodology, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. MCe: Conceptualization, Data curation, Investigation, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. RM: Conceptualization, Data curation, Investigation, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. MG: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Validation, Visualization, Writing – original draft, Writing – review & editing. RB: Conceptualization, Data curation, Investigation, Validation, Visualization, Writing – review & editing. NI: Conceptualization, Data curation, Investigation, Resources, Validation, Visualization, Writing – review & editing. ES: Conceptualization, Resources, Validation, Visualization, Writing – review & editing. CT: Conceptualization, Resources, Supervision, Validation, Visualization, Writing – review & editing. MB: Conceptualization, Data curation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – review & editing. MCo: Conceptualization, Data curation, Methodology, Project administration, Resources, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The authors would like to thank the Biobehavioral Investigation in Neuropsychiatric and neurodevelopmental Disorders (BIND) team for support with data collection and for the fruitful discussion on the topic as well as acknowledge infrastructure from the University of Udine and the Friuli Centrale Health University Authority.
CT has received grants in the last 2 years from Correvio, Biotest, Biomerieux, Gilead, Angelini, Pfizer, Thermofisher, Zambon, Shionogi, Avir Pharma, and Hikma, outside of this work. MCo has been a consultant/advisor to GW Pharma Limited, GW Pharma Italy SRL, and F. Hoffmann-La Roche Limited, outside of this work.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Cucinotta, D, and Vanelli, M. WHO declares COVID-19 a pandemic. Acta Biomed. (2020) 91:157–60. doi: 10.23750/abm.v91i1.9397
2. Coronavirus Research Center. John Hopkins university 2023. (2023). Available at: https://coronavirus.jhu.edu/map.html.
3. Colizzi, M, Peghin, M, De Martino, M, Bontempo, G, Gerussi, V, Palese, A, et al. Mental health symptoms one year after acute COVID-19 infection: prevalence and risk factors. Rev Psiquiatr Salud Ment. (2022) 16:38–46. doi: 10.1016/j.rpsm.2022.05.008
4. Pigaiani, Y, Zoccante, L, Zocca, A, Arzenton, A, Menegolli, M, Fadel, S, et al. Adolescent lifestyle behaviors, coping strategies and subjective wellbeing during the COVID-19 pandemic: an online student survey. Healthcare (Basel). (2020) 8:472. doi: 10.3390/healthcare8040472
5. Kazan Kizilkurt, O, Dilbaz, N, and Noyan, CO. Psychological impact of COVID-19 pandemic on general population in Turkey: risk factors. Asia Pac J Public Health. (2020) 32:519. doi: 10.1177/1010539520964276
6. Colizzi, M, Sironi, E, Antonini, F, Ciceri, ML, Bovo, C, and Zoccante, L. Psychosocial and behavioral impact of COVID-19 in autism Spectrum disorder: an online parent survey. Brain Sci. (2020) 10:341. doi: 10.3390/brainsci10060341
7. Reno, C, Maietti, E, Fantini, MP, Savoia, E, Manzoli, L, Montalti, M, et al. Enhancing COVID-19 vaccines acceptance: results from a survey on vaccine Hesitancy in northern Italy. Vaccines (Basel). (2021) 9:378. doi: 10.3390/vaccines9040378
8. Fazio, N, Caporale, M, Fazio, V, Delogu, G, and Frati, P. Italian law no. 1/2021 on the subject of vaccination against Covid-19 in people with mental disabilities within the nursing homes. Clin Ter. (2021) 172:414–9. doi: 10.7417/CT.2021.2349
9. Paterlini, M. Covid-19: Italy makes vaccination mandatory for healthcare workers. BMJ. (2021) 6:n905. doi: 10.1136/bmj.n905
10. Sallam, M. COVID-19 vaccine Hesitancy worldwide: a concise systematic review of vaccine acceptance rates. Vaccines (Basel). (2021) 9:160. doi: 10.3390/vaccines9020160
11. Pourrazavi, S, Fathifar, Z, Sharma, M, and Allahverdipour, H. COVID-19 vaccine hesitancy: a systematic review of cognitive determinants. Health Promot Perspect. (2023) 13:21–35. doi: 10.34172/hpp.2023.03
12. Maietti, E, Reno, C, Sanmarchi, F, Montalti, M, Fantini, MP, and Gori, D. Are psychological status and trust in information related to vaccine hesitancy during COVID-19 pandemic? A latent class and mediation analyses in Italy. Hum Vaccin Immunother. (2022) 18:2157622. doi: 10.1080/21645515.2022.2157622
13. Brandt, J, Specter, M, and Folstein, MF. The telephone interview for cognitive status. Neuropsychiatry, Neuropsychol Behavioral Neurol. (1988) 1:111–7.
14. Connor, K, and Davidson, J. Development of a new resilience scale: the Connor-Davidson resilience scale (CD-RISC). Depress Anxiety. (2003) 18:76–82. doi: 10.1002/da.10113
15. Campbell-Sills, L, and Stein, M. Psychometric analysis and refinement of the Connor-Davidson resilience scale (CD-RISC): validation of a 10-item measure of resilience. J Trauma Stress. (2007) 20:1019–28. doi: 10.1002/jts.20271
16. Broadbent, E, Petrie, KJ, Main, J, and Weinman, J. The brief illness perception questionnaire. J Psychosom Res. (2006) 60:631–7. doi: 10.1016/j.jpsychores.2005.10.020
17. Smilkstein, G. The family APGAR: a proposal for a family function test and its use by physicians. J Fam Pract. (1978) 6:1231–9.
18. Frewen, P, McPhail, I, Schnyder, U, Oe, M, and Olff, M. Global Psychotrauma screen (GPS): psychometric properties in two internet-based studies. Eur J Psychotraumatol. (2021) 12:1881725. doi: 10.1080/20008198.2021.1881725
19. Perussia, F, and Viano, R. Mini locus of control scale. In: S NuovoDi and G Sprini. Teorie e metodi della psicologia italiana. Tendenze attuali. Milan, Italy: Franco Angeli (2008).
20. Bonetti, M, and La Melani, C. diffusione della pandemia COVID-19 a livello ospedaliero nella Provincia Autonoma di Bolzano: uno studio descrittivo (febbraio 2020-marzo 2022). Boll Epidemiol Naz. (2022) 2022:17–21. doi: 10.53225/BEN_055
21. Istituto Superiore di Sanità. (2021). Available at: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_21-aprile-2021.pdf; https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino-sorveglianza-integrata-COVID-19_21-dicembre-2022.pdf.
22. Britton, T, Ball, F, and Trapman, P. A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science. (2020) 369:846–9. doi: 10.1126/science.abc6810
23. Istituto Superiore di Sanità. (2022). Available at: https://www.epicentro.iss.it/coronavirus/bollettino/Bollettino- sorveglianza-integrata-COVID-19_21-dicembre-2022.pdf.
24. Hippisley-Cox, J, Coupland, CA, Mehta, N, Keogh, RH, Diaz-Ordaz, K, Khunti, K, et al. Risk prediction of covid-19 related death and hospital admission in adults after covid-19 vaccination: national prospective cohort study. BMJ. (2021) 374:n2244. doi: 10.1136/bmj.n2244
25. MacDonald, NE, SAGE Working Group on Vaccine Hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
26. Harrison, EA, and Wu, JW. Vaccine confidence in the time of COVID-19. Eur J Epidemiol. (2020) 35:325–30. doi: 10.1007/s10654-020-00634-3
27. Daly, M, Jones, A, and Robinson, E. Public trust and willingness to vaccinate against COVID-19 in the US from October 14, 2020, to march 29, 2021. JAMA. (2021) 325:2397–9. doi: 10.1001/jama.2021.8246
28. Lazarus, J, Wyka, K, Rauh, L, Rabin, K, Ratzan, S, Gostin, L, et al. Hesitant or not? The Association of age, gender, and education with potential acceptance of a COVID-19 vaccine: a country-level analysis. J Health Commun. (2020) 25:799–807. doi: 10.1080/10810730.2020.1868630
29. Murphy, J, Vallieres, F, Bentall, R, Shevlin, M, McBride, O, Hartman, T, et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nature. Communications. (2021) 12:29. doi: 10.1038/s41467-020-20226-9
30. Robertson, E, Reeve, KS, Niedzwiedz, CL, Moore, J, Blake, M, Green, M, et al. Predictors of COVID-19 vaccine hesitancy in the UK household longitudinal study. Brain Behav Immun. (2021) 94:41–50. doi: 10.1016/j.bbi.2021.03.008
31. Schwarzinger, M, Watson, V, Arwidson, P, Alla, F, and Luchini, S. COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. (2021) 6:E210–21. doi: 10.1016/S2468-2667(21)00012-8
32. Soares, P, Rocha, JV, Moniz, M, Gama, A, Laires, PA, Pedro, AR, et al. Factors associated with COVID-19 vaccine Hesitancy. Vaccines (Basel). (2021) 9:300. doi: 10.3390/vaccines9030300
33. Ishimaru, T, Okawara, M, Ando, H, Hino, A, Nagata, T, Tateishi, S, et al. Gender differences in the determinants of willingness to get the COVID-19 vaccine among the working-age population in Japan. Hum Vaccin Immunother. (2021) 17:3975–81. doi: 10.1080/21645515.2021.1947098
34. Reno, C, Maietti, E, Di Valerio, Z, Montalti, M, Fantini, MP, and Gori, D. Vaccine Hesitancy towards COVID-19 vaccination: investigating the role of information sources through a mediation analysis. Infect Dis Rep. (2021) 13:712–23. doi: 10.3390/idr13030066
35. Martin, L, and Petrie, K. Understanding the dimensions of anti-vaccination attitudes: the vaccination attitudes examination (VAX) scale. Ann Behav Med. (2017) 51:652–60. doi: 10.1007/s12160-017-9888-y
36. Babicki, M, and Mastalerz-Migas, A. Attitudes toward vaccination against COVID-19 in Poland. A longitudinal study performed before and two months after the commencement of the population vaccination Programme in Poland. Vaccines (Basel). (2021) 9:503. doi: 10.3390/vaccines9050503
37. Butter, S, McGlinchey, E, Berry, E, and Armour, C. Psychological, social, and situational factors associated with COVID-19 vaccination intentions: a study of UK key workers and non-key workers. Br J Health Psychol. (2022) 27:13–29. doi: 10.1111/bjhp.12530
38. Paul, E, Steptoe, A, and Fancourt, D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. Lancet Regional Health- Europe. (2021) 1:100012. doi: 10.1016/j.lanepe.2020.100012
39. Griva, K, Tan, K, Chan, F, Periakaruppan, R, Ong, B, Soh, A, et al. Evaluating rates and determinants of COVID-19 vaccine Hesitancy for adults and children in the Singapore population: strengthening our Community's resilience against threats from emerging infections (SOCRATEs) cohort. Vaccine. (2021) 9:1415. doi: 10.3390/vaccines9121415
40. Chu, H, and Liu, S. Integrating health behavior theories to predict American's intention to receive a COVID-19 vaccine. Patient Educ Couns. (2021) 104:1878–86. doi: 10.1016/j.pec.2021.02.031
41. Caserotti, M, Gavaruzzi, T, Girardi, P, Tasso, A, Buizza, C, Candini, V, et al. Who is likely to vacillate in their COVID-19 vaccination decision? Free-riding intention and post-positive reluctance. Prev Med. (2022) 154:106885. doi: 10.1016/j.ypmed.2021.106885
42. American Psychological Association. (2022). Available at: https://www.apa.org/topics/resilience.
43. Bonanno, GA. Loss, trauma, and human resilience: have we underestimated the human capacity to thrive after extremely aversive events? Am Psychol. (2004) 59:20–8. doi: 10.1037/0003-066X.59.1.20
44. Bonanno, G, Romero, S, and Klein, S. The temporal elements of psychological resilience: an integrative framework for the study of individuals, families, and communities. Psychol Inq. (2015) 26:139–69. doi: 10.1080/1047840X.2015.992677
45. Ben-Dor, G, Pedahzur, A, Canetti-Nisim, D, and Zaidise, E. The role of public opinion in Israel’s national security. Am Jewish Congress. (2002) 69:13–5.
46. Breakwell, G, Jaspal, R, and Wright, D. Identity resilience, science mistrust, COVID-19 risk and fear predictors of vaccine positivity and vaccination likelihood: a survey of UK and Portuguese samples. J Health Psychol. (2023). doi: 10.1177/13591053231161891
47. Arsandaux, J, Montagni, I, Macalli, M, Bouteloup, V, Tzourio, C, and Galera, C. Health risk behaviors and self-esteem among college students: systematic review of quantitative studies. Int J Behav Med. (2020) 27:142–59. doi: 10.1007/s12529-020-09857-w
48. Bock, JO, Hajek, A, and König, HH. Psychological determinants of influenza vaccination. BMC Geriatr. (2017) 17:194. doi: 10.1186/s12877-017-0597-y
49. Roccetti, M, Marfia, G, Salomoni, P, Prandi, C, Zagari, RM, Gningaye Kengni, FL, et al. Attitudes of Crohn's disease patients: Infodemiology case study and sentiment analysis of Facebook and twitter posts. JMIR Public Health Surveill. (2017) 3:e51. doi: 10.2196/publichealth.7004
50. Rovetta, A, and Bhagavathula, A. COVID-19-related web search behaviors and Infodemic attitudes in Italy: Infodemiological study. JMIR Public Health Surveill. (2020) 6:e19374. doi: 10.2196/19374
Keywords: mental health, vaccination, vaccination hesitancy, COVID-19, resilience
Citation: Comacchio C, Cesco M, Martinelli R, Garzitto M, Bianchi R, Innocente N, Sozio E, Tascini C, Balestrieri M and Colizzi M (2023) Psychological factors associated with vaccination hesitancy: an observational study of patients hospitalized for COVID-19 in a later phase of the pandemic in Italy. Front. Psychiatry. 14:1272959. doi: 10.3389/fpsyt.2023.1272959
Received: 04 August 2023; Accepted: 04 October 2023;
Published: 19 October 2023.
Edited by:
Erum Rehman, Nazarbayev University, KazakhstanReviewed by:
Nicola Di Fazio, Sapienza University of Rome, ItalyCopyright © 2023 Comacchio, Cesco, Martinelli, Garzitto, Bianchi, Innocente, Sozio, Tascini, Balestrieri and Colizzi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marco Colizzi, bWFyY28uY29saXp6aUB1bml1ZC5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.