
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Psychiatry , 17 November 2023
Sec. Psychological Therapy and Psychosomatics
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1260664
This article is part of the Research Topic Community Series in Psychocardiology: Exploring the Brain-Heart Interface, volume II View all 10 articles
 Britta Stapel1†
Britta Stapel1† Nicole Scharn1†
Nicole Scharn1† Tim Halling1
Tim Halling1 Steffen Akkermann1
Steffen Akkermann1 Ivo Heitland1
Ivo Heitland1 Mechthild Westhoff-Bleck2
Mechthild Westhoff-Bleck2 Kai G. Kahl1*
Kai G. Kahl1*Objective: Adult congenital heart disease (ACHD) is a growing disease entity, posing questions concerning psychosocial outcomes across the lifespan. Spousal relationships were shown to benefit cardiovascular and mental health in the general population. We assessed the association of relationship status with anxiety and depression in ACHD patients and determined whether patients considered disease-related concerns potential mediators of relationship problems.
Methods: N = 390 ACHD patients were included. Self-report questionnaires were used to assess relationship status, ACHD-related relationship problems, socio-demographic variables, and depression and anxiety scores. Further, clinical parameters concerning the heart condition were determined.
Results: N = 278 (71%) patients were currently in a relationship, while N = 112 (29%) were not in a relationship. Groups did not significantly differ regarding age, sex, and cardiovascular parameters. Two-way MANCOVA with relationship status and sex as independent variables, controlling for age, NYHA class, and NT-proBNP, showed an association of relationship status with depression, while sex was associated with anxiety. N = 97 (25%) patients reported disease-related adverse effects on a current or prior relationship. In detail, worries about body image (N = 57, 61%), own fears (N = 51, 54%), problems arising from wish to have children (N = 33, 35%), fears regarding a joint future (N = 29, 31%), partner’s fears or lack of understanding (N = 28, 30%), and sexual problems (N = 21, 22%) were cited.
Conclusion: Relationships status was associated with depression, while sex was associated with anxiety in ACHD patients. Relationship status as well as potential relationship problems, and the importance of social support for mental and physical well-being, should be considered when treating ACHD patients.
With a reported prevalence of 0.9–1% of live birth worldwide, congenital heart disease (CHD) represents the most commonly diagnosed congenital malformation in newborns (1, 2). With recent innovations in early diagnostic, interventional, and surgical procedures, the number of CHD patients that survive childhood and adolescence is steadily increasing. With up to 90% of patients reaching adulthood, factors that impact long-term cardiovascular disease (CVD) risk become increasingly important in patients with adult CHD (ACHD) (3, 4). In this regard, a current meta-analysis that assessed CVD risk of CHD survivors in later life found an increased risk for overall CVD, albeit the study was unable to pinpoint whether CHD constituted an independent risk factor or whether the association was confounded by a CVD risk factor profile among ACHD patients (5).
Next, to the increased CVD risk, ACHD patients display a significantly higher prevalence of psychiatric disorders when compared to the general population, with mood- and anxiety disorders being the most frequent (6–8). As psychiatric disorders are in turn associated with a heightened risk for CVD in the general population and symptomatic depression and anxiety are associated with adverse outcome measures, including rehospitalization and mortality, in patients with established CVD (9, 10), it is of clinical importance to identify modifiable factors that might negatively impact mental well-being in ACHD patients.
Various studies have evaluated the impact of (marital) relationship status on CV parameters and CVD risk in the general population. A twin study conducted in Sweden showed that living alone was associated with an increased CVD risk (11). Similar findings were reported in other countries and cultural regions (12). This association is further supported by a recent meta-analysis, which concluded that individuals that were not in a relationship had a higher CVD risk compared to married individuals (13). Next to the association with CVD risk, relationship status has also been shown to be associated with the outcome following a cardiac event, as individuals that lived alone were found to have an increased risk for all-cause mortality, CVD death, and myocardial infarction compared to individuals that lived in a marital relationship (14). While data regarding underlying mechanisms are limited, social support received from the partner is thought to reduce psychosocial stress and to thereby play an important role in mediating the beneficial effect of spousal relationships (15). Additionally, individuals in a relationship are thought to seek healthcare earlier and more often, to show better adherence to prescribed treatment, and to be more susceptible to healthier lifestyle behaviors (15).
Next, to CV parameters, relationship status has been associated with mental health measures. In this regard, spousal relationships have been described to be associated with protection from depression and anxiety in the general population (16, 17).
While research regarding relationship status in the context of ACHD is currently limited, a study assessing quality of life (QOL) in ACHD patients showed that next to older age, lack of employment, and higher New York Heart Association (NYHA) functional class, no marriage history was associated with lower QOL (18). Furthermore, feeling of loneliness was found as a common predictor of depression and anxiety in patients with ACHD (7).
As ACHD has been associated with an increased risk for CVD as well as for mood and anxiety disorders (5–8) and relationship status has been found to impact CV parameters and CVD risk as well as mental well-being in the general population (13), relationship status presents a relevant issue in the growing population of ACHD patients. Nevertheless, the association of relationship status with depression and anxiety has not been previously examined in ACHD patients and disease-related factors that might affect relationship quality and thereby stability of a spousal relationship have not been previously assessed.
Therefore, we examined relationship status and its impact on symptoms of anxiety and depression in a sample of ACHD patients. Additionally, we describe frequency and characteristics of disease-related relationship problems in these patients.
The presented data were generated as part of the ongoing PSYConHEART study that aims to establish morbidity and mortality factors in ACHD patients (19–22). Data collection took place from August 2020 to February 2021 at the outpatient clinic of the Department of Cardiology at Hannover Medical School. The study was conducted in accordance to the ethical guidelines of the 1975 Declaration of Helsinki and ethical approval was obtained from the local ethics committee at Hannover Medical School. All participants gave their written informed consent before entering the study. Inclusion criteria were a structural CHD, the ability to read and agree to the consent form and to read and answer the German versions of the relevant questionnaires, and an age ≥ 18 years. Exclusion criteria were pregnancy and instability of the cardiac condition. For our analyses that focused on the effect of spousal relationships, we considered respective literature that indicates that the main source for social support in adults are spousal relationships while in adolescents parental support was found to be the most important with regards to parameters of mental well-being (23). As data from the German Federal Statistical Office indicate a mean age of 23.6 years for young adults to leave their parental home in Germany in 2021 (24) we only included patients with an age ≥ 25 years in the analyses.
Data from N = 575 patients were obtained. After exclusion of cases with an age < 25 years, and cases that were missing data regarding relationship status, NYHA class, NT-proBNP, and/or hospital anxiety and depression scale (HADS) score. N = 390 cases were included in the study sample. Supplementary Figure 1 shows the sample selection process.
A senior cardiologist examined all patients included in the study during their routine check-up. The functional status of patients was determined by use of NYHA class. Cardiac morphology and function, including LVEF, were assessed by echocardiography. To classify the complexity of the underlying heart condition, the Bethesda scale was used to divide the congenital defect into “simple,” “moderate,” or “complex” (25). Additionally, number of thoracotomies was documented.
All participants answered a demographic survey that included relationship status (defined as an intimate spousal relationship that was marriage-like). Symptoms of depression and anxiety were assessed using the HADS, with the anxiety (HADS-A) and the depression (HADS-D) subscores being used (26). Additionally, patients were asked whether their heart defect had ever negatively impacted their relationship and to determine potential underlying issues, participants were asked to check either “yes” or “no” to the following suggested reasons: (1) negative body image, (2) own fears, (3) problems arising from wish to have children, (4) fears regarding a joint future, (5) fear or lack of understanding by the partner, and (6) sexual problems.
All statistical analyses were performed in SPSS 28 (IBM, Armonk, NY, United States). Shapiro Wilk Test was used for assessment of normality of data distribution. For group comparisons regarding anthropometric- and demographic data and CV parameters based on relationship status, non-parametric Mann–Whitney U-Test was used. Chi square test was performed for group comparisons of nominal data. To assess the association of relationship status and sex with depression and anxiety scores, two-way multivariate analysis of covariance (MANCOVA) was performed; HADS-D score and HADS-A score were imputed as dependent variables, relationship status and sex as independent variables, and age, NYHA class, and NT-proBNP as covariates. Sex was included as an independent variable based on dedicated literature that suggests distinct effects of relationship status on mental wellbeing in men and women in the general population (16). The respective covariates were included as prior studies reported conflicting results with regard to a potential association of disease severity and prognosis on psychological distress in ACHD patients (7, 27), and additionally an association of age, relationship status, and depression has previously been reported based on data from the general population (16). Two-tailed p-values are depicted and p ≤ 0.050 was considered statistically significant.
An overview regarding sociodemographic factors and cardiac parameters of the study sample is provided in the Supplementary Results. Table 1 compares sociodemographic variables and CV measures in patients that reported to be currently in a relationship (N = 278 [71%]) to those that reported to be not in a relationship (N = 112 [29%]). Both groups did not significantly differ in any of the reported parameters.
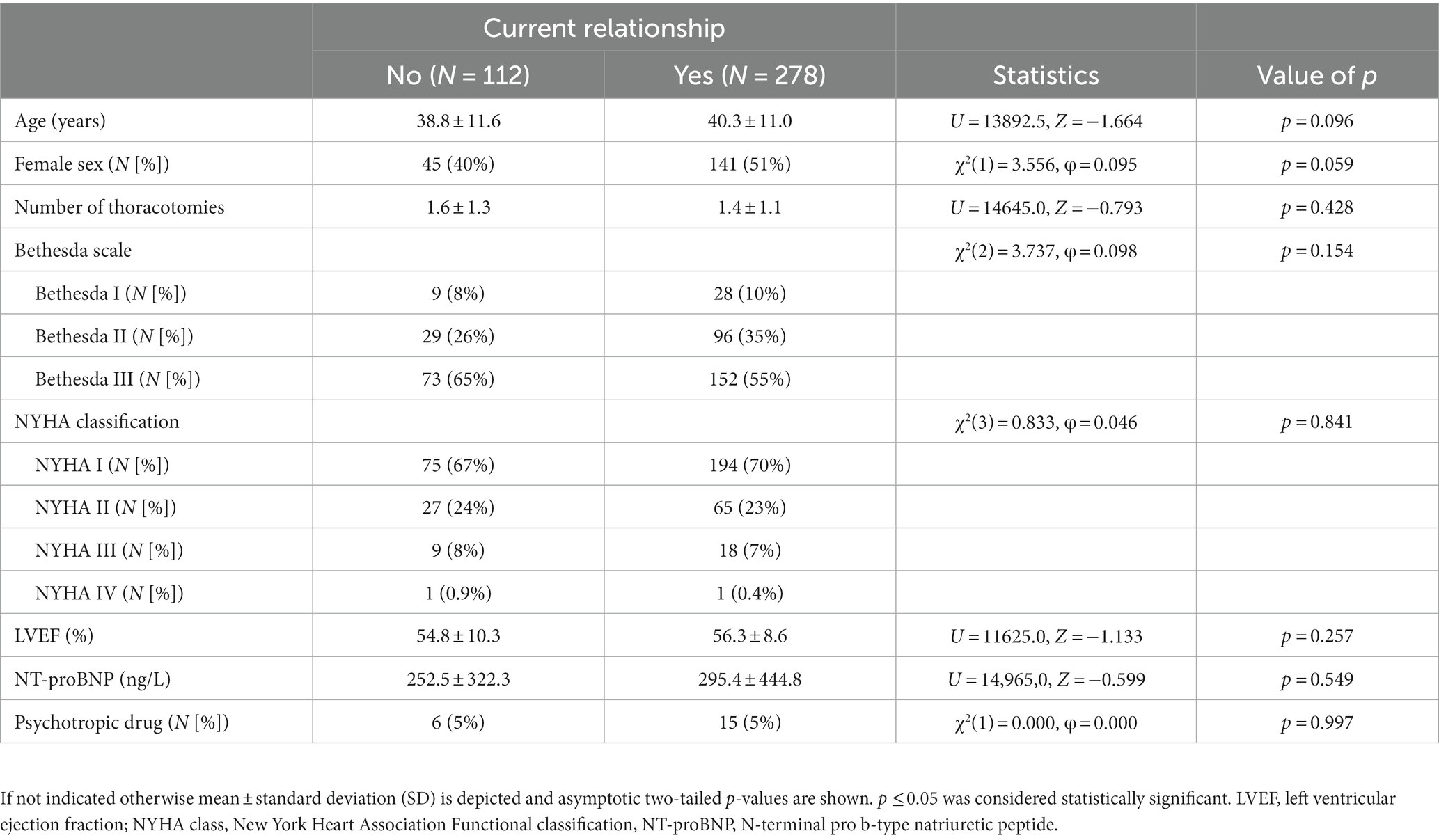
Table 1. Comparison of sociodemographic variables and CV measures in ACHD patients based on current relationship status.
Based on research indicating sex-specific effects of relationship status and social support on mental well-being (16), we assessed the association of relationship status and sex with HADS-D and HADS-A scores using two-way MANCOVA. To account for potential effects of age and disease severity, age, NYHA class, and NT-proBNP were included as covariates (7, 27). Two-way MANCOVA showed a statistically significant difference between relationship groups on the combined dependent variables [F(2, 382) = 4.352, p = 0.014, Wilk’s Λ = 0.978]. Additionally, sex had a statistically significant effect on the combined term [F(2, 382) = 4.371, p = 0.013, Wilk’s Λ = 0.978], while no significant interaction effect was found [F(2, 382) = 1.217, p = 0.297, Wilk’s Λ = 0.994]. Post hoc univariate ANCOVAs were conducted for both dependent variables. Results show a statistically significant difference between relationship groups for HADS-D scores [F(1, 383) = 6.330, p = 0.012, η2 = 0.016], while no significant difference for HADS-A score was found [F(1, 383) = 0.383, p = 0.537, η2 = 0.001]. Contrarily, a statistically significant difference between sexes was found for HADS-A scores [F(1, 383) = 5.020, p = 0.026, η2 = 0.013], while HADS-D scores did not significantly differ [F(1, 383) = 0.022, p = 0.882, η2 < 0.001]. Pairwise comparisons based on estimated marginal means using Bonferroni-corrected post hoc test showed a significant difference of HADS-D scores based on relationship status only in women (p = 0.015, MDiff = 1.30, 95%-CI [0.255, 2.345]) but not in men (p = 0.308, MDiff = 0.478, 95%-CI [−0.442, 1.398]). Additionally, increased anxiety scores in women compared to men were only observed in the no relationship group (p = 0.026, MDiff = 1.575, 95%-CI [0.192, 2.957]), but not in the relationship group (p = 0.527, MDiff = 0.279, 95% -CI [−0.586, 1.144]). Results are visualized in Figures 1A,B.
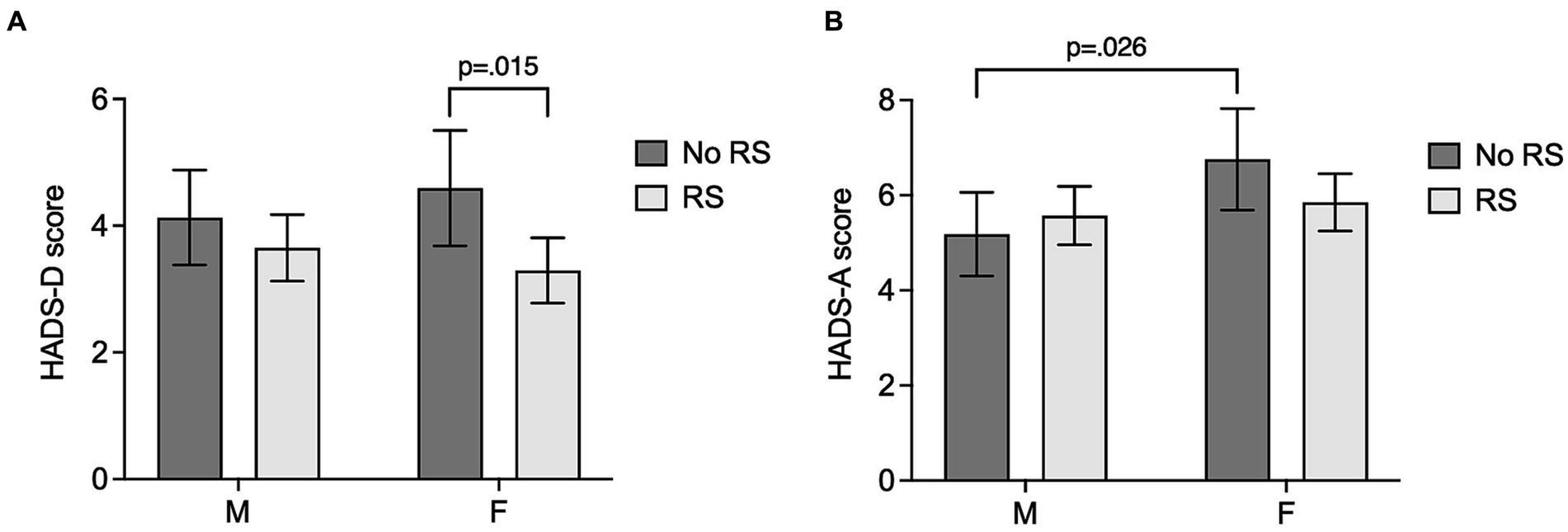
Figure 1. Depression and anxiety scores in ACHD patients in relation to relationship status and sex. Bar graphs depict estimated marginal means and 95% confidence intervals (calculated with age = 39.85, NYHA class = 1.39, and NT-proBNP = 283.12) of depressive symptoms measured by HADS-D score (A), and anxiety symptoms indicated by HADS-A score (B), dependent on relationship problems (No RS: no current relationship; RS: current relationship) and sex (M: male; F: female). Bonferroni-corrected two-tailed p-values for statistically significant pairwise group comparisons are depicted. p ≤ 0.050 was considered statistically significant.
Given the observed protective effect of a spousal relationship on depressive symptomology in our sample, we assessed whether the underlying heart defect could have potential, adverse effects on a patient’s relationship. When asked, N = 97 (25%) of all ACHD patients in our sample reported that their heart disease had ever negatively impacted their relationship or prevented them from committing to a relationship, while N = 292 (75%) of patients reported no prior or current negative effect. Table 2 summarizes sociodemographic variables and CV measures of patients that had ever experienced a disease-associated adverse impact on their relationship compared to those who reported no previous or current impact. Patients that reported an adverse impact of their disease on their relationship did not significantly differ from those that were not affected with regard to current relationship status, age, or sex. However, patients that reported an adverse impact on their relationship presented with a higher disease severity indicated by a more complex underlying heart defect based on Bethesda class, a higher number of thoracotomies, a higher NYHA class and decreased LVEF. Additionally, patients that reported disease-related relationship problems had a prescription for at least one psychotropic drug more frequently.
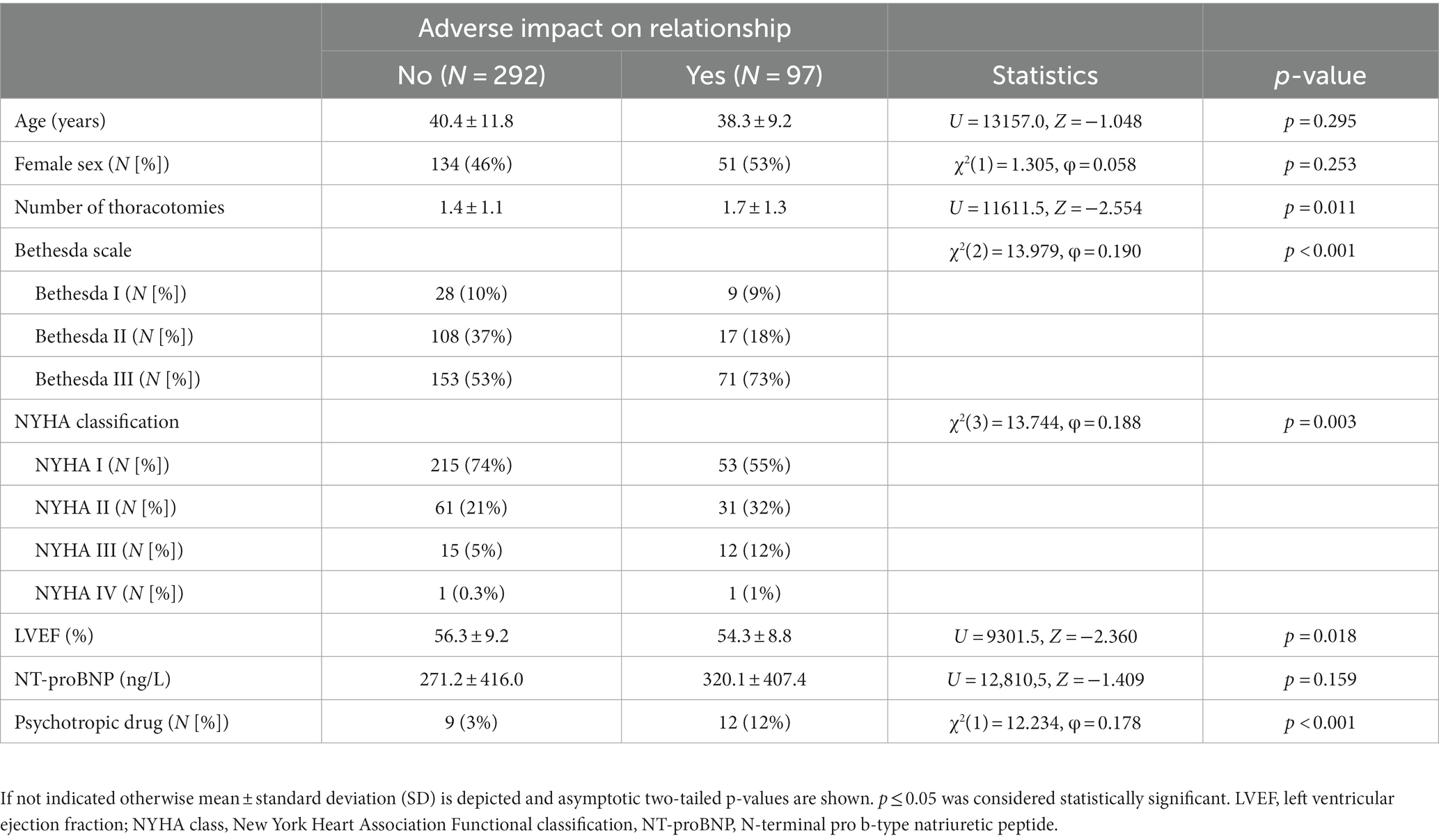
Table 2. Comparison of sociodemographic variables and CV measures in ACHD patients based on reported disease-related relationship problems.
To determine potential underlying reasons for disease-related relationship problems, patients were asked to answer “yes” or “no” to six suggested potential reasons as detailed in section 2.5. N = 94/97 patients that had report prior or current disease-related adverse effects on their relationship completed the respective questionnaire. Patients that reported problems in their relationship indicated underlying reasons with the following frequencies: negative body image (N = 57 [61%]), own fears (N = 51 [54%]), problems arising from wish to have children (N = 33 [35%]), fears regarding a joint future (N = 29 [31%]), fear or lack of understanding by the partner (N = 28 [30%]), and sexual problems [N = 21 (22%)]. N = 29 (31%) patients cited only one of these reasons to be applicable, however, most patients reported more than one reason for their relationship problems (N = 64 [68%]) (Supplementary Figure 2).
One main result of our study is the finding that patients without a current relationship reported higher depression scores. Additionally, woman that were not in a current relationship also reported higher anxiety scores compared to men without a current relationship.
The second main finding of our study is that one fourth of patients in the present sample reported a negative impact of their CHD on a prior or current relationship. These patients were characterized by a more complex underlying heart condition and a more severe heart disease.
Our data indicate that patients with ACHD may benefit from a spousal relationship. In particular, our results suggest a greater benefit of being in a spousal relationship for women compared to men. In this regard, post hoc groupwise comparisons showed significant effects of relationship status on depression scores only in women but not in men and additionally, higher anxiety scores were detected in women that were not in a relationship compared to men with the same relationship status, while no effect of sex on anxiety scores was found in the relationship group.
While survival rates in patients have increased significantly over the last decades, ACHD patients with a moderate or complex underlying heart defect are often not cured and are confronted with medical complications and a shortened life expectancy (28–30). This might be associated with additional psychosocial challenges, which is reflected by the high frequency of depression and anxiety disorders in this patient population (6–8). In this regard, a study Kovacs and colleagues found that 50% of ACHD patients in the respective sample fulfilled criteria for at least one lifetime mood or anxiety disorder (7). Similarly, a prior study by our group found a prevalence of any mood disorder of 31% and of any anxiety disorder of 28% based on structured clinical interview in accordance to DSM-IV criteria (6). Therefore, the identification of factors that might protect from mood and anxiety symptoms is of importance.
Beneficial effects of spousal relationships on mental and on physical well-being have frequently been reported in the literature (31, 32). With regard to depression and depressive symptoms, various studies have found beneficial effects of marital relationships in the general population (16). An important factor that appears to confer beneficial effects of spousal relationships on protection from depression is perceived social support (23, 33). Perceived social support constitutes a subjective perspective of how individuals perceive the availability of material, psychological, and overall support offered by others (34). Perceived social support correlates well with various measures of mental health (35, 36). Of importance, social support is also characterized by the individuals that provide the support. In this regard, it is assumed that protective effects of social support vary depending on the provider, i.e., a spouse, relatives, or friends (23). A dedicated meta-analysis that reported on the association between social support and protection from depression found the strongest evidence for spousal support as a protective factor from depression in the adult population and especially emotional support was consistently found to be a protective factor (23).
Previous studies have found that ACHD patients experience mental health disorders, including depression and anxiety, with a higher prevalence than the general population (6–8). A study by Kovacs and colleagues found potential predictors for symptoms of depression and anxiety in these patients to be limited to feelings of loneliness and fear of negative evaluation as factors of social functioning, disease severity or functional class were not predictive (7). Contrarily, a recent publication reported a positive association of NYHA class and psychological distress (27). Our results are in line with the study by Kovacs et al. as no significant association of either NYHA class or NT-proBNP that were included as potential confounders in the MANCOVA, on HADS-D scores were detected in the present sample. While the impact of relationship status on depression and anxiety has not been previously evaluated in ACHD patients, prior studies have assessed relationship status in the context of quality of life in this patient population. Importantly, quality of life has been found to be significantly associated with anxiety and depression in ACHD patients (6). Previous studies have reported heterogenous effects regarding an association of marital relationship with QOL in patients with ACHD, with some studies reporting a significant association (18, 37, 38) while others failed to detect a significant effect (39). In line with our findings, a prior study reported that parameters of subjective functional status were only associated with the physical but not with the psychological domain of quality of life, while family support and psychological distress were common denominators for most quality of life domains including the psychological domain (40).
Of note, our data suggest greater effects of relationship status on depressive symptoms in women with ACHD compared to male patients. This is in contrast to data from the general population that suggest a greater benefit from marital relationships for men when compared to women. A study conducted with data from a series of cross-sectional national health surveys in Canada found modifying effects of age and sex on the relationship of marital status and depression (16). In this study, women that were single, widowed, or divorced were found to be less vulnerable to depression than men (16). The authors hypothesized that women more frequently utilize larger and stronger networks of social support while men often appear to rely on spousal support (16). However, this might not be the case in patients with CVD, as data from patients post acute myocardial infarction suggest that women experience lower levels of social support compared to men (41). Additionally, our results are in line with findings from Chen and colleagues that assessed determinants of quality of life in ACHD patients. The authors found sex-specific differences in the psychological domain of quality of life, which could be attributed to underlying psychosocial factors (40). Whether the observed sex-differences regarding the association of relationship status on protection from depressive symptoms are a specific feature of ACHD patients or whether other factors not investigated in our sample, including relationship satisfaction and the quality of social support by the spouse as well as other sources of social support, contribute to the observed effect will be subject of follow-up studies.
Overall, our findings expand data from previous studies that found that being in a (marital) relationship was associated with higher levels of psychological well-being, indicated by lower rates of depression and substance abuse in the general population as well as in patients that suffer from mental health problems, to ACHD patients (42).
In our sample, 71% of ACHD patients reported to be currently in a spousal relationship, which is comparable to a study from the Netherlands that reported 69% of patients to be in a spousal relationship (43). In that study, the rate of individuals in a relationship was significantly lower in the ACHD group than that observed in the respective control sample, in which relationship rate was 89% (43).
Given the association of relationship status and depressive symptomology in ACHD patients, and considering findings by others that commonly reported an effect of relationship quality, i.e., marriage dissatisfaction or conflict, on cardiovascular parameters, CVD risk, and mental well-being (15, 44, 45), it is of importance to identify potential disease-related problems that ACHD patients might experience with regard to their spousal relationship.
Our data show that one fourth of the ACHD patients in our sample reported that their disease had previously negatively impacted their relationship and those patients were characterized by a more complex underlying heart condition and a more severe heart disease.
When asked for reasons underlying their perceived relationship problems, most patients cited one of the suggested reasons. However, more than half of the patients cited more than one reason. Contrarily, to the finding that disease-related relationship problems were more frequent in patients with a more severe underlying heart disease, the frequency with which the different suggested reasons for these perceived problems were cited did not depend on disease severity. Additionally, the respective reasons were cited with similar frequencies by male and female patients, with the exception of “problems arising from wish to have children” that was reported significantly more often by women (data not shown).
Overall, our data suggest protective effects of being in a spousal relationship on depressive symptoms in patients with ACHD. In light of literature that reports that ACHD patients are in spousal relationships at a lower rate than the general population (43), it appears of importance to identify factors, including those associated with the underlying cardiac defect, that might adversely affect relationship quality and stability. Our data show that a considerable percentage of patients has previously found their heart disease to adversely impact their relationship or prevented them from entering a relationship. Most patients cited at least one disease-related reason that could be attributed to the patient. Therefore, it might be considered to address relationship status as well as potential relationship problems, and the importance of social support for mental and physical well-being, when treating patients with ACHD.
Our study has several limitations that should be considered. We only present cross-sectional data, which does not allow for temporal or causal inference. We did not assess whether patients that were not in a relationship were single, separated, or widowed. Therefore, we did not investigate any potential differences in these subgroups with regards to depression and anxiety scores, which is of importance, as literature suggests distinct effects on depression scores (16). Additionally, data regarding quality of social support by the spouse, as well as other sources of social support were not assessed in our sample. Finally, we did not assess current relationship quality, which could have impacted depression scores as literature suggests adverse effects of relationship conflict or dissatisfaction on mental health parameters (46–48).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the local Ethics Committee at Hannover Medical School. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
BS: Formal analysis, Visualization, Writing – original draft. NS: Formal analysis, Writing – original draft. TH: Investigation, Writing – review & editing. SA: Investigation, Writing – review & editing. IH: Formal analysis, Writing – review & editing. MW-B: Conceptualization, Formal analysis, Project administration, Supervision, Writing – review & editing. KK: Conceptualization, Formal analysis, Project administration, Supervision, Writing – review & editing.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
KK received speaker honoraria and travel grants from EliLilly, Janssen, Takeda, Medice, Servier, Schwabe, and Idorsia.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1260664/full#supplementary-material
1. Liu, Y, Chen, S, Zuhlke, L, Black, GC, Choy, MK, Li, N, et al. Global birth prevalence of congenital heart defects 1970-2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol. (2019) 48:455–63. doi: 10.1093/ije/dyz009
2. van der Linde, D, Konings, EE, Slager, MA, Witsenburg, M, Helbing, WA, Takkenberg, JJ, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol. (2011) 58:2241–7. doi: 10.1016/j.jacc.2011.08.025
3. Moons, P, Bovijn, L, Budts, W, Belmans, A, and Gewillig, M. Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation. (2010) 122:2264–72. doi: 10.1161/CIRCULATIONAHA.110.946343
4. Mandalenakis, Z, Giang, KW, Eriksson, P, Liden, H, Synnergren, M, Wahlander, H, et al. Survival in children with congenital heart disease: have we reached a peak at 97%? J Am Heart Assoc. (2020) 9:e017704. doi: 10.1161/JAHA.120.017704
5. Wang, T, Chen, L, Yang, T, Huang, P, Wang, L, Zhao, L, et al. Congenital heart disease and risk of cardiovascular disease: a Meta-analysis of cohort studies. J Am Heart Assoc. (2019) 8:e012030. doi: 10.1161/JAHA.119.012030
6. Westhoff-Bleck, M, Briest, J, Fraccarollo, D, Hilfiker-Kleiner, D, Winter, L, Maske, U, et al. Mental disorders in adults with congenital heart disease: unmet needs and impact on quality of life. J Affect Disord. (2016) 204:180–6. doi: 10.1016/j.jad.2016.06.047
7. Kovacs, AH, Saidi, AS, Kuhl, EA, Sears, SF, Silversides, C, Harrison, JL, et al. Depression and anxiety in adult congenital heart disease: predictors and prevalence. Int J Cardiol. (2009) 137:158–64. doi: 10.1016/j.ijcard.2008.06.042
8. Bromberg, JI, Beasley, PJ, D'Angelo, EJ, Landzberg, M, and DeMaso, DR. Depression and anxiety in adults with congenital heart disease: a pilot study. Heart Lung. (2003) 32:105–10. doi: 10.1067/mhl.2003.26
9. Angermann, CE, and Ertl, G. Depression, anxiety, and cognitive impairment: comorbid mental health disorders in heart failure. Curr Heart Fail Rep. (2018) 15:398–410. doi: 10.1007/s11897-018-0414-8
10. Chaddha, A, Robinson, EA, Kline-Rogers, E, Alexandris-Souphis, T, and Rubenfire, M. Mental health and cardiovascular disease. Am J Med. (2016) 129:1145–8. doi: 10.1016/j.amjmed.2016.05.018
11. Chen, R, Zhan, Y, Pedersen, N, Fall, K, Valdimarsdottir, UA, Hagg, S, et al. Marital status, telomere length and cardiovascular disease risk in a Swedish prospective cohort. Heart. (2020) 106:267–72. doi: 10.1136/heartjnl-2019-315629
12. Dhindsa, DS, Khambhati, J, Schultz, WM, Tahhan, AS, and Quyyumi, AA. Marital status and outcomes in patients with cardiovascular disease. Trends Cardiovasc Med. (2020) 30:215–20. doi: 10.1016/j.tcm.2019.05.012
13. Wong, CW, Kwok, CS, Narain, A, Gulati, M, Mihalidou, AS, Wu, P, et al. Marital status and risk of cardiovascular diseases: a systematic review and meta-analysis. Heart. (2018) 104:1937–48. doi: 10.1136/heartjnl-2018-313005
14. Schultz, WM, Hayek, SS, Samman Tahhan, A, Ko, YA, Sandesara, P, Awad, M, et al. Marital status and outcomes in patients with cardiovascular disease. J Am Heart Assoc. (2017) 6:5890. doi: 10.1161/JAHA.117.005890
15. O'Keefe, J, Torres-Acosta, N, and Lavie, CJ. Living alone makes the heart more vulnerable. Heart. (2020) 106:246–7. doi: 10.1136/heartjnl-2019-316042
16. Bulloch, AGM, Williams, JVA, Lavorato, DH, and Patten, SB. The depression and marital status relationship is modified by both age and gender. J Affect Disord. (2017) 223:65–8. doi: 10.1016/j.jad.2017.06.007
17. LaPierre, TA . Marital status and depressive symptoms over time: age and gender variations. Fam Relat. (2009) 58:404–16. doi: 10.1111/j.1741-3729.2009.00562.x
18. Apers, S, Kovacs, AH, Luyckx, K, Thomet, C, Budts, W, Enomoto, J, et al. Quality of life of adults with congenital heart disease in 15 countries: evaluating country-specific characteristics. J Am Coll Cardiol. (2016) 67:2237–45. doi: 10.1016/j.jacc.2016.03.477
19. Proskynitopoulos, PJ, Heitland, I, Glahn, A, Bauersachs, J, Westhoff-Bleck, M, and Kahl, KG. Prevalence of Child maltreatment in adults with congenital heart disease and its relationship with psychological well-being, health behavior, and current cardiac function. Front Psych. (2021) 12:686169. doi: 10.3389/fpsyt.2021.686169
20. Halling, T, Akkermann, S, Loffler, F, Groh, A, Heitland, I, Haefeli, WE, et al. Factors that influence adherence to medication in adults with congenital heart disease (ACHD). Front Psych. (2021) 12:788013. doi: 10.3389/fpsyt.2021.788013
21. Akkermann, S, Halling, T, Loffler, F, Silber-Peest, AS, Kruger, T, Bleich, S, et al. Impact of COVID-19 on medical supply in adults with congenital heart disease. Front Psych. (2022) 13:812611. doi: 10.3389/fpsyt.2022.812611
22. Westhoff-Bleck, M, Lemke, LH, Bleck, JS, Bleck, AC, Bauersachs, J, and Kahl, KG. Depression associated with reduced heart rate variability predicts outcome in adult congenital heart disease. J Clin Med. (2021) 10:1554. doi: 10.3390/jcm10081554
23. Gariepy, G, Honkaniemi, H, and Quesnel-Vallee, A. Social support and protection from depression: systematic review of current findings in Western countries. Br J Psychiatry. (2016) 209:284–93. doi: 10.1192/bjp.bp.115.169094
24. Destatis (SB) . Press release no. N 049 of 1 August 2022. (2022). Available at: https://www.destatis.de/EN/Press/2022/08/PE22_N049_12.html.
25. Warnes, CA, Liberthson, R, Danielson, GK, Dore, A, Harris, L, Hoffman, JI, et al. Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. (2001) 37:1170–5. doi: 10.1016/S0735-1097(01)01272-4
26. Snaith, RP . The hospital anxiety and depression scale. Health Qual Life Outcomes. (2003) 1:29. doi: 10.1186/1477-7525-1-29
27. Lebherz, C, Frick, M, Panse, J, Wienstroer, P, Brehmer, K, Kerst, G, et al. Anxiety and depression in adults with congenital heart disease. Front Pediatr. (2022) 10:906385. doi: 10.3389/fped.2022.906385
28. Khajali, Z, Maleki, M, Amin, A, Saedi, S, Arabian, M, Moosazadeh, M, et al. Prevalence of cardiac dysfunction among adult patients with congenital heart disease: a single-center investigation. Iran Heart J. (2019) 20:12–9.
29. Warnes, C, Williams, R, Bashore, T, Child, J, Connolly, H, Dearani, J, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to develop guidelines on the Management of Adults with Congenital Heart Disease). Developed in collaboration with the American Society of Echocardiography, Heart Rhythm Society, International Society for Adult Congenital Heart Disease, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. J Am Coll Cardiol. (2008) 118:e1–e121. doi: 10.1161/CIRCULATIONAHA.108.190690
30. Verheugt, CL, Uiterwaal, CS, van der Velde, ET, Meijboom, FJ, Pieper, PG, van Dijk, AP, et al. Mortality in adult congenital heart disease. Eur Heart J. (2010) 31:1220–9. doi: 10.1093/eurheartj/ehq032
31. Jaffe, DH, Manor, O, Eisenbach, Z, and Neumark, YD. The protective effect of marriage on mortality in a dynamic society. Ann Epidemiol. (2007) 17:540–7. doi: 10.1016/j.annepidem.2006.12.006
32. Manzoli, L, Villari, P, MP, G, and Boccia, A. Marital status and mortality in the elderly: a systematic review and meta-analysis. Soc Sci Med. (2007) 64:77–94. doi: 10.1016/j.socscimed.2006.08.031
33. Dean, A, Kolody, B, and Wood, P. Effects of social support from various sources on depression in elderly persons. J Health Soc Behav. (1990) 31:148–61. doi: 10.2307/2137169
34. Barrera, M Jr . Distinctions between social support concepts, measures, and models. Am J Community Psychol. (1986) 14:413–45. doi: 10.1007/BF00922627
35. Lakey, B, and Cronin, A. Low social support and major depression: Research, theory and methodological issues. Risk factors in depression. San Diego, CA, US: Elsevier Academic Press; (2008). p. 385–408.
36. Liang, J, Krause, NM, and Bennett, JM. Social exchange and well-being: is giving better than receiving? Psychol Aging. (2001) 16:511–23. doi: 10.1037/0882-7974.16.3.511
37. Moons, P, and Luyckx, K. Quality-of-life research in adult patients with congenital heart disease: current status and the way forward. Acta Paediatr. (2019) 108:1765–72. doi: 10.1111/apa.14876
38. Truong, TH, Kim, NT, Nguyen, MT, Do, DL, Nguyen, HT, Le, TT, et al. Quality of life and health status of hospitalized adults with congenital heart disease in Vietnam: a cross-sectional study. BMC Cardiovasc Disord. (2021) 21:229. doi: 10.1186/s12872-021-02026-1
39. Khajali, Z, Sayyadi, A, Ansari, Z, and Aliramezany, M. Quality of life in adult patients with congenital heart disease: results of a double-center study. Front Psych. (2022) 13:1062386. doi: 10.3389/fpsyt.2022.1062386
40. Chen, CA, Liao, SC, Wang, JK, Chang, CI, Chiu, IS, Chen, YS, et al. Quality of life in adults with congenital heart disease: biopsychosocial determinants and sex-related differences. Heart. (2011) 97:38–43. doi: 10.1136/hrt.2010.200709
41. Naqvi, TZ, Naqvi, SS, and Merz, CN. Gender differences in the link between depression and cardiovascular disease. Psychosom Med. (2005) 67:S15–8. doi: 10.1097/01.psy.0000164013.55453.05
42. Frech, A, and Williams, K. Depression and the psychological benefits of entering marriage. J Health Soc Behav. (2007) 48:149–63. doi: 10.1177/002214650704800204
43. Zomer, AC, Vaartjes, I, Uiterwaal, CS, van der Velde, ET, Sieswerda, GJ, Wajon, EM, et al. Social burden and lifestyle in adults with congenital heart disease. Am J Cardiol. (2012) 109:1657–63. doi: 10.1016/j.amjcard.2012.01.397
44. Nealey-Moore, JB, Smith, TW, Uchino, BN, Hawkins, MW, and Olson-Cerny, C. Cardiovascular reactivity during positive and negative marital interactions. J Behav Med. (2007) 30:505–19. doi: 10.1007/s10865-007-9124-5
45. Isiozor, NM, Kunutsor, SK, Laukkanen, T, Kauhanen, J, and Laukkanen, JA. Marriage dissatisfaction and the risk of sudden cardiac death among men. Am J Cardiol. (2019) 123:7–11. doi: 10.1016/j.amjcard.2018.09.033
46. Whisman, MA, and Uebelacker, LA. Impairment and distress associated with relationship discord in a national sample of married or cohabiting adults. J Fam Psychol. (2006) 20:369–77. doi: 10.1037/0893-3200.20.3.369
47. Goldfarb, MR, and Trudel, G. Marital quality and depression: a review. Marriage Fam Rev. (2019) 55:737–63. doi: 10.1080/01494929.2019.1610136
Keywords: adult congenital heart disease, depression, anxiety, relationship status, cardiovascular disease
Citation: Stapel B, Scharn N, Halling T, Akkermann S, Heitland I, Westhoff-Bleck M and Kahl KG (2023) Impact of relationship status on psychological parameters in adults with congenital heart disease. Front. Psychiatry. 14:1260664. doi: 10.3389/fpsyt.2023.1260664
Received: 18 July 2023; Accepted: 06 November 2023;
Published: 17 November 2023.
Edited by:
Preethi Premkumar, London South Bank University, United KingdomReviewed by:
Zahra Khajali, Shaheed Rajaei Cardiovascular Medical and Research Center, IranCopyright © 2023 Stapel, Scharn, Halling, Akkermann, Heitland, Westhoff-Bleck and Kahl. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kai G. Kahl, a2FobC5rYWlAbWgtaGFubm92ZXIuZGU=
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.