- 1Department of Environmental and Global Health, University of Florida, Gainesville, FL, United States
- 2Denver Zoological Foundation, Denver, CO, United States
- 3Department of Clinical and Health Psychology, University of Florida, Gainesville, FL, United States
- 4Unconditional Love, Inc., Melbourne, FL, United States
- 5School of Social Work, Virginia Commonwealth University, Richmond, VA, United States
- 6Department of Psychology, University of Florida, Gainesville, FL, United States
- 7Department of Epidemiology, University of Florida, Gainesville, FL, United States
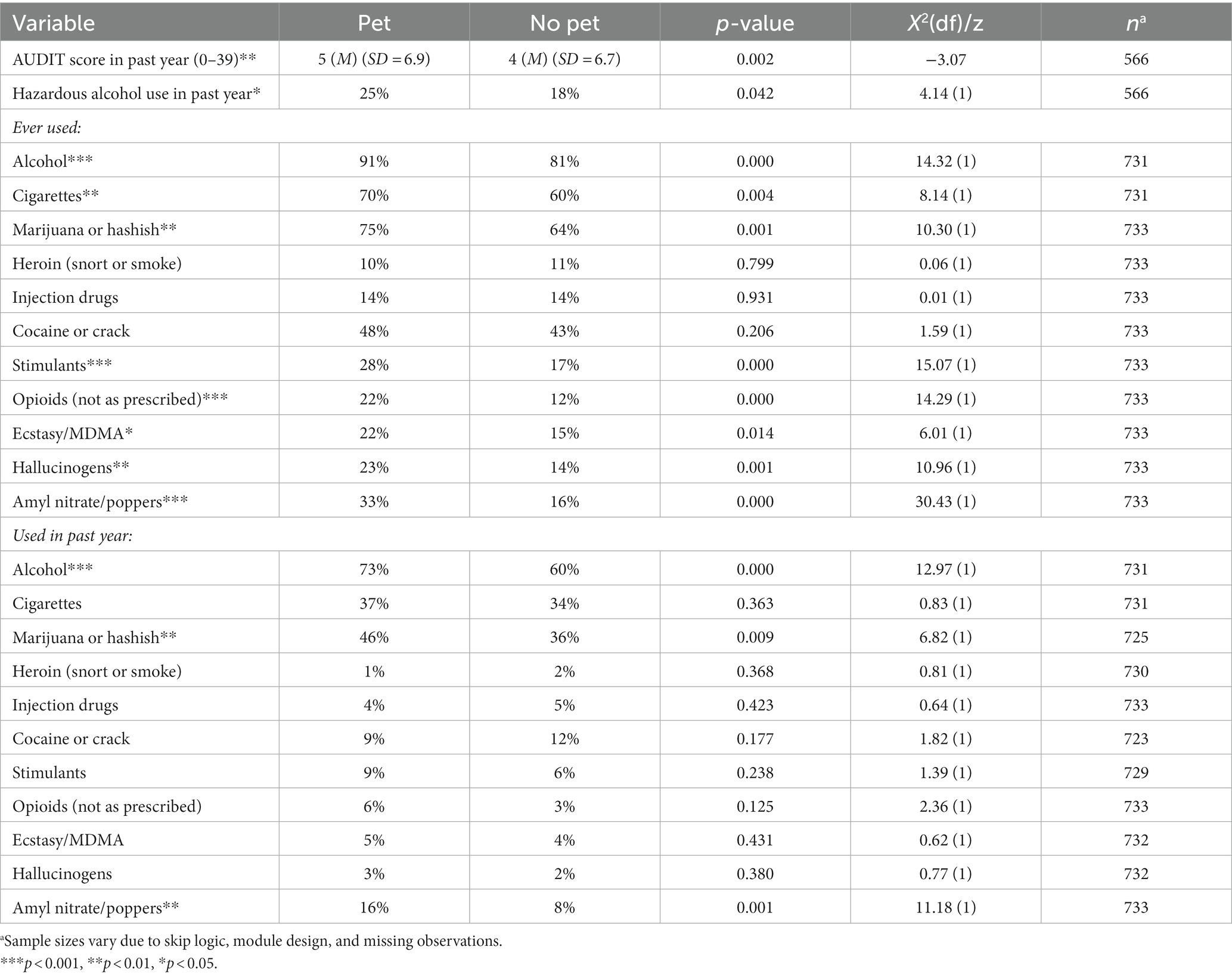
Research suggests that people with HIV (PWH), who are at high risk for alcohol and substance use, may rely on relationships with pets for companionship and stress relief. There may be common mechanisms underlying both substance use and attachment to pets. The purpose of this brief research report was to compare alcohol and substance use behaviors between pet owners and non-owners among a cohort of PWH. Participants (n = 735) in a survey study of PWH in Florida were asked about their alcohol and substance use behaviors, whether they owned a pet, and their sociodemographic characteristics. We used bivariate analyses and logistic regression to examine differences in alcohol and substance use behaviors between pet owners and non-owners. Pet owners had higher mean AUDIT scores than non-owners (Mpet = 5, Mnopet = 4, z = −3.07, p = 0.002). Pet owners were more likely than non-owners to use alcohol in a harmful or hazardous way (AUDIT score ≥ 8), above and beyond sociodemographic characteristics (OR = 1.65, p = 0.052). Pet owners were more likely to have ever used most substances than non-owners, and more likely to currently use alcohol (X2(1) = 12.97, p = 0.000), marijuana or hashish (X2(1) = 6.82, p = 0.009), and amyl nitrate/poppers (X2(1) = 11.18, p = 0.001). Pet owners may be more likely to use alcohol and other substances at higher rates than non-owners. Reasons for owning a pet and using substances may be similar, such as coping with stress.
1. Introduction
Alcohol and substance use are highly prevalent among people with HIV (PWH) and are determinants of medication adherence and secondary transmission risk (1, 2). Identifying psychosocial correlates of alcohol and substance use among PWH is of critical importance both for public health and individual prognosis (1, 3, 4). Although a majority of U.S. households have at least one pet in the home (5–7), no prior studies to our knowledge have examined pet ownership as a potential psychosocial correlate of alcohol and substance use among PWH, despite research linking pet ownership with a variety of human health outcomes (6, 8–11). It is unclear whether pet ownership and substance use may be correlated in PWH or in what direction, owing to the complex physical, social, and economic challenges of living with HIV.
One possibility is that pet ownership may be linked with lower rates of alcohol and substance use in this population. There is some evidence that pets serve as meaningful relationships for PWH. Specifically, previous studies on pet ownership among PWH suggest that for some, pets offer companionship and a nonjudgmental source of emotional support (12–18). Moreover, caring for pets can provide a meaningful social role that promotes effective self-management of HIV via stress reduction and daily caregiving tasks (18). Thus, it is possible that pet ownership may be associated with lower alcohol and substance use among PWH by providing opportunities to engage in positive coping behaviors.
Alternatively, it is also plausible that pet ownership is associated with higher rates of alcohol and substance use among PWH. At a socioemotional level, people may engage in substance use for coping with distressing emotional states and symptoms (e.g., depression, internalized HIV stigma/self-stigma) social enhancement and intoxication (i.e., to feel good and fit in), and improvement of internal emotional and physical states (19–21). Research suggests that people seek out pet ownership for similar reasons: to foster relationships, experience companionship, and to provide stress relief and psychological benefits (22, 23). At a biological level, neuromodulators that impact responses to stressful experiences as well as social affiliative behavior such as OXTR are implicated in both alcohol misuse and interactions with companion animals. For example, OXTR rs53576 is recognized as a potential genetic locus for sensitivity to the social environment, and A-carriers at this locus have been reported to engage in more substance use among males (24, 25) and engage in more petting behavior during human-animal interaction (26). For PWH, a pet may provide social and emotional comfort, but may not fully alleviate anxiety and stress. Therefore, it is possible that motivations to manage negative affectivity and cope with stress may contribute to high degrees of overlap between pet ownership and substance use.
Pets (i.e., dogs) can also act as social lubricants (27); accordingly, pet ownership may increase opportunities for social engagement, and while reduced perceived social isolation has been associated with negative mental health outcomes (e.g., anxiety and depression), alcohol and other substances of abuse are often used in social situations and may also be impacted by this same mechanism. Finally, due to the level of responsibility required to adequately care for pets, as well as associated economic stressors (e.g., veterinary care), PWH who own pets may experience a higher level of stress than non-owners, which could contribute to higher rates of negative coping strategies such as alcohol and substance use in this population (28).
Given that pet owners are systematically different from non-pet owners with regard to several demographic and contextual characteristics (e.g., gender, race, income), it is important that research accounts for these factors when comparing health outcomes for PWH and how they may vary by pet ownership status (6, 29, 30). The purpose of this brief research report was to report comparisons in alcohol and substance use behaviors between pet owners and non-owners among a cohort of PWH while adjusting for the potential confounding effects of sociodemographic characteristics.
2. Methods
Data were from Wave 3 of the Florida Cohort, a survey of PWH in Florida, run by the Southern HIV and Alcohol Research Consortium (SHARC) in 2021–2023. Wave 2 of the Florida Cohort is described in Ibanez et al. (31) and had a similar methodology and goals to Wave 3. Participants were recruited at HIV care providers, patient registries, participant referrals, and remotely via advertising. Participants completed several survey modules, available in English, Spanish, and Haitian Creole, regarding general health, health care utilization, behavioral and social factors, alcohol and substance use, mental health, and pet ownership. Participants were compensated for each module they completed. The study was approved by the University of Florida Internal Review Board.
2.1. Measures
Alcohol use: The Alcohol Use Disorders Identification Test (AUDIT) is a validated 10-item questionnaire measuring alcohol consumption, drinking behavior, and alcohol-related problems (32). Possible scores on the AUDIT range from 0–40; based on AUDIT scoring criteria, participants who scored eight or above were coded as using alcohol in a harmful or hazardous way.
Other substances: Participants were asked if they had ever used several substances, including tobacco, marijuana, heroin, cocaine, stimulants, MDMA, opioids, hallucinogens, and amyl nitrate. Those who endorsed ever having used each substance were asked if they had used the substance in the past 12 months.
Pet ownership: Participants were asked, “do you have any pets?” Possible responses were “yes” or “no.”
Sociodemographic characteristics: Participants self-reported their age, race, Hispanic ethnicity, yearly family income, educational attainment, gender, and marital or relationship status.
2.2. Analytic procedures
We present bivariate analyses (Wilcoxon signed rank tests, chi-squared tests, and t-tests) to compare alcohol and substance use behaviors between pet owners and non-owners. We estimate a multivariate logistic regression to isolate the association between pet ownership and harmful or hazardous alcohol use above and beyond sociodemographic characteristics. We control for characteristics with known associations to alcohol use behaviors and/or pet ownership.
Of the 735 total participants, 546 both completed the AUDIT and had complete information on all variables of interest and are thus included in the multivariate analyses. Bivariate analyses and descriptive information are included for all non-missing observations.
3. Results
3.1. Descriptive information
Among the 735 Florida Cohort participants, 43% were pet owners. Participants were aged 20–80 years; the mean age for pet owners was slightly younger (M = 48, SD = 12.5) than non-owners (M = 51, SD = 13.6; t (733) = 2.93, p = 0.004). Race, Hispanic ethnicity, income, education, and marital status varied significantly between pet owners and non-owners. Sixty-two percent of pet owners identified their race as White, 33% Black, and 5% other races,1 while 21% of non-owners identified as White, 70% as Black, and 9% as other races (X2 (2)=124.46, p = 0.000). Twenty-one percent of pet owners endorsed Hispanic ethnicity, versus 12% of non-owners (X2 (1)=12.53, p = 0.000). Among pet owners, 26% made less than $10,000 per year, 38% made $10,000-29,999, 22% made $30,000-49,999, and 14% made $50,000 and above; among non-owners, 44% made less than $10,000, 35% made $10,000-29,999, 13% made $30,000-49,999, and 8% made $50,000 and above (X2 (3)=31.03, p = 0.000). Sixteen percent of pet owners reported less than a high school education, 32% reported high school or GED attainment, and 52% reported some college and above; 32% of non-owners had less than high school education, 27% had high school or GED, and 41% reported some college and above (X2 (2)=24.76, p = 0.000). Among pet owners, 48% were single, 9% were living with a long-term partner, 16% were married, and 26% were divorced, separated, or widowed; among those who did not own pets, 56% were single, 4% were living with a long-term partner, 12% were married, and 28% were divorced, separated, or widowed (X2 (3)=11.92, p = 0.008). Gender did not vary significantly between pet owners and non-owners: 60% of pet owners were male versus 55% of non-owners, 38% of pet owners were female, versus 43% of non-owners, and 3% of pet owners reported other genders, versus 1% of non-owners (X2 (2)=3.87, p = 0.144).
3.2. Differences in alcohol and substance use behaviors between pet owners and non-owners
Pet owners had significantly higher AUDIT scores and were more likely to use alcohol in a hazardous or harmful manner (≥8 AUDIT score) than non-owners. Pet owners were significantly more likely to have ever used alcohol, cigarettes, marijuana or hashish, stimulants, unprescribed opioids, ecstasy or MDMA, hallucinogens, and amyl nitrate or poppers than non-owners. In the past 12 months, pet owners were more likely than non-owners to have used alcohol, marijuana or hashish, and amyl nitrate. See Table 1 for statistical information.
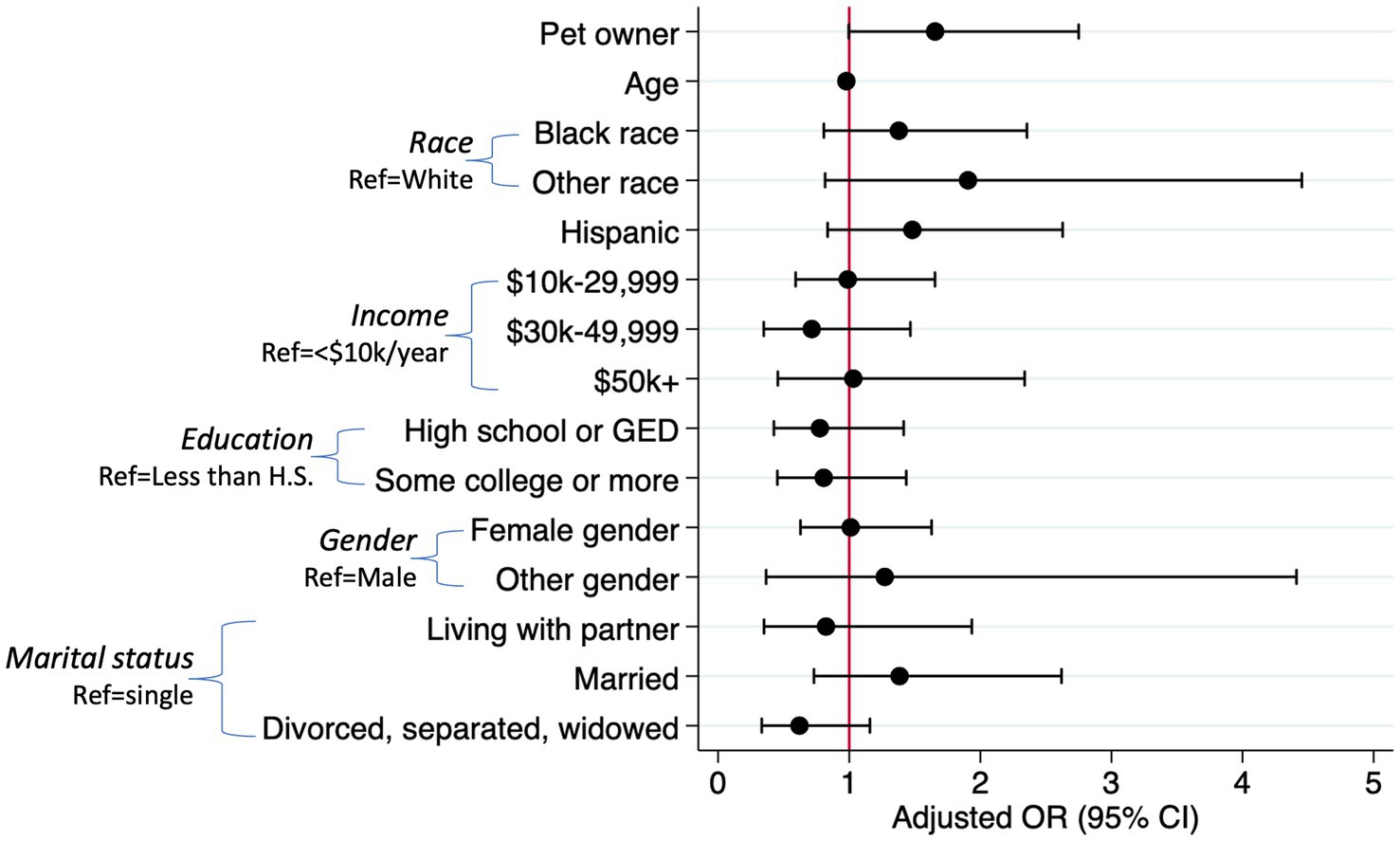
In the logistic regression model (LR X2 (15)=29.44, p = 0.014), pet ownership was marginally significantly associated with harmful or hazardous alcohol use (≥8 AUDIT score) above and beyond the effects of age, race, Hispanic ethnicity, income, education, gender, and marital status (OR = 1.65, p = 0.052). Age was the only other significant variable in the model: older participants were less likely to be harmful or hazardous alcohol users than younger participants (OR = 0.98, p = 0.015). Figure 1 displays the odds ratios and confidence intervals for each variable in the model.
4. Discussion
In this brief research report, we described differences in alcohol and substance use behaviors between pet owners and non-owners among a cohort of PWH. We found that pet owners were more likely to be current alcohol users than non-owners, tended to score higher on a standard assessment of harmful or hazardous alcohol use, and this association remained marginally statistically significant when adjusting for the effects of sociodemographic covariates in the model. Additionally, pet owners were more likely to have ever used most substances than non-owners and more likely to be current users of marijuana or hashish, and amyl nitrate.
The higher likelihood of harmful alcohol use among pet owners (compared to non-owners) in this study, at a surface level, may be somewhat counter-intuitive in the context of previous research among this population suggesting that pets may contribute to well-being and motivate PWH to maintain healthy lifestyles (13–16, 18). However, some research among PWH and other populations has shown that pet owners with strong attachment bonds may have poorer mental health than those with weaker bonds (9, 13, 34), suggesting that reliance on a pet for emotional support could be indicative of a greater need for coping mechanisms. Additionally, this study is cross-sectional and did not account for the participants’ duration of pet ownership, years living with HIV, and duration of alcohol and substance use; other research has suggested that the mental health effects of pet ownership could emerge over time (35). Future research should account for these factors.
If both pet ownership (i.e., attachment to pets) and substance and alcohol use serve similar coping roles, it may be possible to harness the human-animal bond to reduce the harmful or hazardous use of alcohol and other substances. For example, if a pet owner uses substances to relieve stress, creating interventions to strengthen the human-animal bond (e.g., engaging in activities that are mutually beneficial for both human and pet) may help to reduce substance use behaviors via pet-associated stress reduction. Importantly, broader public and community-based support for pet ownership among marginalized populations, such as PWH, is pertinent in order to relieve some of the stress of pet caregiving and thus encourage healthy coping via pet support, versus unhealthy coping with substances. Pet ownership, without broader support for the human-animal bond, may serve to create more stress and thus encourage substance use, rather than reduce it. Future research should assess whether programs to support pet ownership among PWH may encourage healthy coping and thus reduce alcohol and substance use.
Though attachment to pets was not assessed in this study, previous research suggests there are common biological, psychological, and social mechanisms underlying both heavy alcohol use and strong attachments to pets. For example, recent experiences of stress, state or trait anxiety, and adverse childhood experiences coupled with neurobiological predispositions to experience altered responses to stress and social interaction including but not limited to the oxytocinergic system may all play common roles in both substance use and attachment to pets (36). These factors, both individually and in combination, should be assessed in future research on pet ownership and alcohol and substance use, particularly among PWH and other marginalized populations.
Data availability statement
The datasets for this article are not publicly available due to concerns regarding participant/patient anonymity. Requests to access the datasets should be directed to the corresponding author.
Author contributions
JA: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Software, Visualization, Writing – original draft, Writing – review & editing. SM: Conceptualization, Funding acquisition, Writing – original draft, Writing – review & editing. EP: Conceptualization, Writing – review & editing. MW: Data curation, Investigation, Writing – review & editing. HF: Data curation, Writing – review & editing. DK: Writing – review & editing. RC: Conceptualization, Funding acquisition, Investigation, Resources, Supervision, Writing – review & editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. The Southern HIV and Alcohol Research Consortium NIH/NIAAA U24 AA022002, R01AA030481, and pilot funding from the SHARC Center for Translational HIV Research provided funding for this study.
Conflict of interest
SM was employed by Denver Zoological Foundation. MW was employed by Unconditional Love, Inc.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
1. ^This approach was employed for analytic purposes, as small group sizes are not compatible with the methodologies used in this paper. There are limitations to grouping racial and ethnic groups; for a discussion of the issues this approach can raise (see 33).
References
1. Pence, BW, Thielman, NM, Whetten, K, Ostermann, J, Kumar, V, and Mugavero, MJ. Coping strategies and patterns of alcohol and drug use among HIV-infected patients in the United States southeast. AIDS Patient Care STDs. (2008) 22:869–77. doi: 10.1089/apc.2008.0022
2. Welch, KJ. Correlates of alcohol and/or drug use among HIV-infected individuals. AIDS Patient Care STDs. (2000) 14:317–23. doi: 10.1089/10872910050046340
3. Gerbi, GB, Habtemariam, T, Robnett, V, Nganwa, D, and Tameru, B. Psychosocial factors as predictors of HIV/AIDS risky behaviors among people living with HIV/AIDS. J AIDS HIV Res. (2012) 4:8–16. doi: 10.5897/jahr11.057
4. Mellins, CA, Kang, E, Leu, CS, Havens, JF, and Chesney, MA. Longitudinal study of mental health and psychosocial predictors of medical treatment adherence in mothers living with HIV disease. AIDS Patient Care STDs. (2003) 17:407–16. doi: 10.1089/108729103322277420
5. Applebaum, JW, Peek, CW, and Zsembik, BA. Examining U.S. pet ownership using the general social survey. Soc Sci J. (2020) 60:110–9. doi: 10.1080/03623319.2020.1728507
6. Mueller, MK, King, EK, Callina, K, Dowling-Guyer, S, and McCobb, E. Demographic and contextual factors as moderators of the relationship between pet ownership and health. Health Psychol Behav Med. (2021) 9:701–23. doi: 10.1080/21642850.2021.1963254
7. American Pet Products Association. (2023). Pet industry market size, Trends & Ownership Statistics. Available at: https://www.americanpetproducts.org/
8. Applebaum, JW, McDonald, SE, and Zsembik, BA. Longitudinal associations between allostatic load, pet ownership, and socioeconomic position among U.S. adults aged 50+. SSM Popul Health. (2023) 21:101344. doi: 10.1016/j.ssmph.2023.101344
9. McDonald, SE, O’Connor, KE, Matijczak, A, Tomlinson, CA, Applebaum, JW, Murphy, JL, et al. Attachment to pets moderates transitions in latent patterns of mental health following the onset of the COVID-19 pandemic: results of a survey of U.S Adults. Animals. (2021) 11:895. doi: 10.3390/ani11030895
10. Rodriguez, KE, Herzog, H, and Gee, NR. Variability in human-animal interaction research. Front Vet Sci. (2021) 7:619600. doi: 10.3389/fvets.2020.619600
11. Wells, DL. The state of research on human–animal relations: implications for human health. Anthrozoös. (2019) 32:169–81. doi: 10.1080/08927936.2019.1569902
12. Castelli, P, Hart, LA, and Zasloff, RL. Companion cats and the social support Systems of men with Aids. Psychol Rep. (2001) 89:177–87. doi: 10.2466/pr0.2001.89.1.177
13. Hutton, VE. Companion animals and wellbeing when living with HIV in Australia. Anthrozoös. (2014) 27:407–21. doi: 10.2752/175303714X14023922797823
14. Hutton, VE. Social provisions of the human—animal relationship amongst 30 people living with HIV in Australia. Anthrozoös. (2015) 28:199–214. doi: 10.1080/08927936.2015.11435397
15. Hutton, VE. A reason to live: HIV and animal companions. West Lafayette, Indiana: Purdue University Press (2019).
16. Kabel, A, Khosla, N, and Teti, M. The dog narratives: benefits of the human–animal bond for women with HIV. J HIVAIDS Soc Serv. (2015) 14:405–16. doi: 10.1080/15381501.2013.860069
17. Siegel, JM, Angulo, FJ, Detels, R, Wesch, J, and Mullen, A. AIDS diagnosis and depression in the Multicenter AIDS cohort study: the ameliorating impact of pet ownership. AIDS Care. (1999) 11:157–70. doi: 10.1080/09540129948054
18. Webel, AR, and Higgins, PA. The relationship between social roles and self-management behavior in women living with HIV/AIDS. Womens Health Issues. (2012) 22:e27–33. doi: 10.1016/j.whi.2011.05.010
19. Berry, K, Haddock, G, Barrowclough, C, and Gregg, L. The role of attachment, coping style and reasons for substance use in substance users with psychosis. Clin Psychol Psychother. (2022) 29:725–32. doi: 10.1002/cpp.2666
20. Cherenack, EM, Stein, MD, Abrantes, AM, Busch, A, Pinkston, MM, Baker, JV, et al. The relationship between substance use and physical activity among people living with HIV, chronic pain, and symptoms of depression: a cross-sectional analysis. AIDS Care. (2023) 35:170–81. doi: 10.1080/09540121.2022.2136349
21. Thornton, LK, Baker, AL, Lewin, TJ, Kay-Lambkin, FJ, Kavanagh, D, Richmond, R, et al. Reasons for substance use among people with mental disorders. Addict Behav. (2012) 37:427–34. doi: 10.1016/j.addbeh.2011.11.039
22. Bibbo, J, Curl, AL, and Johnson, RA. Pets in the lives of older adults: a life course perspective. Anthrozoös. (2019) 32:541–54. doi: 10.1080/08927936.2019.1621541
23. Green, JD, Coy, AE, and Mathews, MA. Attachment anxiety and avoidance influence pet choice and pet-directed behaviors. Anthrozoös. (2018) 31:475–94. doi: 10.1080/08927936.2018.1482117
24. Vaht, M, Kurrikoff, T, Laas, K, Veidebaum, T, and Harro, J. Oxytocin receptor gene variation rs53576 and alcohol abuse in a longitudinal population representative study. Psychoneuroendocrinology. (2016) 74:333–41. doi: 10.1016/j.psyneuen.2016.09.018
25. Cleveland, HH, Griffin, AM, Wolf, PSA, Wiebe, RP, Schlomer, GL, Feinberg, ME, et al. Transactions between substance use intervention, the oxytocin receptor (OXTR) gene, and peer substance use predicting youth alcohol use. Prev Sci. (2018) 19:15–26. doi: 10.1007/s11121-017-0749-5
26. Kertes, DA, Hall, N, and Bhatt, SS. Children’s relationship with their pet dogs and OXTR genotype predict child–pet interaction in an experimental setting. Front Psychol. (2018) 9:157–70. doi: 10.3389/fpsyg.2018.01472
27. McNicholas, J, and Collis, GM. Dogs as catalysts for social interactions: robustness of the effect. Br J Psychol Lond Engl. (1953) 91:61–70. doi: 10.1348/000712600161673
28. Applebaum, JW, MacLean, EL, and McDonald, SE. Love, fear, and the human-animal bond: on adversity and multispecies relationships. Compr Psychoneuroendocrinol. (2021) 7:100071. doi: 10.1016/j.cpnec.2021.100071
29. Marsa-Sambola, F, Williams, J, Muldoon, J, Lawrence, A, Connor, M, Roberts, C, et al. Sociodemographics of pet ownership among adolescents in Great Britain: findings from the HBSC study in England, Scotland, and Wales. Anthrozoös. (2016) 29:559–80. doi: 10.1080/08927936.2016.1228756
30. Miles, JNV, Parast, L, Babey, SH, Griffin, BA, and Saunders, JM. A propensity-score-weighted population-based study of the health benefits of dogs and cats for children. Anthrozoös. (2017) 30:429–40. doi: 10.1080/08927936.2017.1335103
31. Ibañez, GE, Zhou, Z, Cook, CL, Slade, TA, Somboonwit, C, Morano, J, et al. The Florida cohort study: methodology, initial findings and lessons learned from a multisite cohort of people living with HIV in Florida. AIDS Care. (2020) 33:516–24. doi: 10.1080/09540121.2020.1748867
32. Saunders, JB, Aasland, OG, Babor, TF, De La Fuente, JR, and Grant, M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. (1993) 88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x
33. Jenkins, JL, and Rudd, ML. Decolonizing animal welfare through a social justice framework. Front Vet Sci. (2022) 8:787555. doi: 10.3389/fvets.2021.787555
34. Ratschen, E, Shoesmith, E, Shahab, L, Silva, K, Kale, D, Toner, P, et al. Human-animal relationships and interactions during the Covid-19 lockdown phase in the UK: investigating links with mental health and loneliness. Triberti S, editor. PLoS One. (2020) 15:e0239397. doi: 10.1371/journal.pone.0239397
35. Applebaum, JW, Shieu, MM, McDonald, SE, Dunietz, GL, and Braley, TJ. The impact of sustained ownership of a pet on cognitive health: a population-based study. J Aging Health. (2023) 35:230–41. doi: 10.1177/08982643221122641
Keywords: pets, companion animals, people with HIV, alcohol use, substance use, HIV/AIDS, pet owners, human-animal interaction
Citation: Applebaum JW, McDonald SE, Porges EC, Widmeyer M, Fabelo HE, Kertes DA and Cook RL (2023) Pet ownership is associated with harmful alcohol use among a cohort of people with HIV: a brief research report. Front. Psychiatry. 14:1258850. doi: 10.3389/fpsyt.2023.1258850
Edited by:
Roxanne D. Hawkins, University of Edinburgh, United KingdomReviewed by:
Ana Lilia Cerda Molina, Instituto Nacional de Psiquiatría "Ramón de la Fuente Muñiz", MexicoAnnalyse Ellis, University of Edinburgh, United Kingdom
Copyright © 2023 Applebaum, McDonald, Porges, Widmeyer, Fabelo, Kertes and Cook. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer W. Applebaum, amVubnlhcHBsZWJhdW1AdWZsLmVkdQ==
 Jennifer W. Applebaum
Jennifer W. Applebaum Shelby E. McDonald
Shelby E. McDonald Eric C. Porges
Eric C. Porges Maya Widmeyer4
Maya Widmeyer4 Darlene A. Kertes
Darlene A. Kertes