- 1College of Health Science, Oda Bultum University, Chiro, Ethiopia
- 2Department of Nursing, College of Health Science, Oda Bultum University, Chiro, Ethiopia
- 3School of Nursing and Midwifery, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 4Department of Biochemistry, College of Medicine and Health Sciences, Debre Tabor University, Debre Tabor, Ethiopia
- 5Immunology and Molecular Biology Unit, Department of Medical Laboratory Sciences, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
Introduction: Despite its deleterious consequences, khat chewing is escalating worldwide. However, there is a lack of evidence about the extent of khat chewing among pregnant women in Ethiopia, particularly in the current study area. Therefore, this study aimed to assess the prevalence of current khat chewing and its associated factors among pregnant women in Chiro district, eastern Ethiopia.
Methods: This community-based cross-sectional study was conducted in Chiro district from November 1 to 30, 2022 G.C. Study participants were selected using the systematic random sampling technique. An interview-administered structured questionnaire was used to collect data through a house-to-house survey. The data were entered into EpiData version 3.1 and analyzed in STATA 14 software. Characteristics of study participants were summarized using descriptive analysis, and binary logistic regression was used to identify determinants of khat chewing.
Results: A total of 409 pregnant women participated in this study, with a response rate of 99%. The overall prevalence of khat chewing was 60.4% (95% CI: 55.5%, 65.2%). Religion (AOR: 2.08; 95% CI: 1.13, 3.82), khat cultivation (AOR: 0.43; 95% CI: 0.25, 0.77), partner khat use (AOR: 5.54; 95% CI: 3.11, 9.88), pre-pregnancy khat use (AOR: 9.95; 95% CI: 5.55, 17.81), antenatal care (ANC) visit (AOR: 2.71; 95% CI: 1.41, 5.21), and mental distress (AOR: 4.89; 95% CI: 2.38, 10.02) were significantly associated with current khat chewing.
Conclusion: The majority of pregnant women in the study area practice khat chewing. Thus, accessible and comprehensive pre-conception and pre-natal care incorporating the prevention and management of antenatal khat chewing is crucial to overcome this problem. Provision of mental healthcare involving partners of pregnant women is also important to reduce the extent and impacts of khat chewing during pregnancy. Further longitudinal studies triangulated with qualitative designs are recommended.
Introduction
Khat (Catha edulis) is an evergreen stimulant plant that is widely cultivated and consumed in East Africa and the Arabian Peninsula (1). The young buds and fresh, tender leaves are chewed to attain psycho-stimulation and euphoria (2). Cathinone and cathine, which are central nervous system stimulants with a qualitatively similar effect as amphetamine, are the principal active ingredients in fresh khat leaves (2–4). In its early stages, khat chewing results in excitement, cheerfulness, relief from fatigue, increased energy, the ability to associate ideas, and high confidence (5, 6). However, these effects are short lived and then replaced by outweighing negative consequences like depression, insomnia, and anxiety (6).
Khat chewing is increasingly becoming a global public health threat (7, 8). Advancing global market and increased production of the crop due to its ability to tolerate climate extremes have enhanced the accessibility and consumption of khat worldwide (8, 9). The practice is widely prevalent in Eastern Africa and the Middle East (1, 8). A cross-sectional study in Yemen found that three in ten adult Yemeni women practice khat chewing (10). Whereas, about 90% of adult men in Yemen exercise khat chewing (11). Another house-to-house survey in Kenya revealed that the prevalence of current khat chewing was 36.8% (12). In Ethiopia, the extent of current khat use ranges from 4 to 64.9%, yet it substantially varies between study populations and geographical areas (13–15).
Khat chewing has multiplex consequences, especially among reproductive-age women (2, 14); these problems are exceedingly escalated, and it is a potential risk for serious reproductive health problems among pregnant women (16). Such problems include preterm labor, pre-labor rupture of membranes, intrauterine fetal death, fetal distress, congenital malformations, anemia, low birth weight, and perinatal death (16–18). It is also associated with preeclampsia, induction of labor, decreased lactation, and embryotoxic effects (19, 20). Thus, indicating its numerous consequences on the health of the mother and her offspring.
Despite its deleterious consequences, khat chewing practice is escalating worldwide (1, 7); its close relation with cultural norms and lack of clear regulatory rules in many high-producing countries have made control efforts less effective, if not ineffective (21, 22). In Ethiopia, measures like increased taxation have been implemented (23), yet the problem remains substantial (24). Although the topic is better investigated among a few segments of the population (24, 25), there is a paucity of evidence about khat chewing practice among pregnant women in Ethiopia, particularly in the current study area. Therefore, this study aimed to assess the prevalence of current khat chewing and its associated factors among pregnant women in Chiro district, eastern Ethiopia.
Materials and methods
Study setting
This study was conducted in Chiro district, which is located in West Hararghe Zone, Oromia Regional State, Ethiopia. The district is 326 km away from the national capital, Addis Ababa, in the east direction. It is bordered by Tullo district on the east, Meiso district on the north, Gemechis district on the south, and Guba Koricha on the west. Administratively, Chiro district is divided into 42 kebeles (three urban and thirty-nine rural kebeles). The total estimated population of the district is 314,056 people, of which 10,898 are pregnant women. The district is known for its high production and consumption of khat (9).
Study design and period
We employed a community-based cross-sectional study from November 1 to 30, 2022 G.C.
Population
Source population: all pregnant women in Chiro District.
Study population: all pregnant women in the selected kebeles of Chiro district.
Eligibility criteria
All pregnant women who lived in Chiro district for at least 6 months before the survey were eligible for this study. However, pregnant women who were seriously ill and/or had difficulties to communicate were excluded from the study.
Sample size and sampling procedure
The sample size was estimated using the single population proportion formula with the assumptions of a 95% confidence interval, 5% margin of error, and Khat chewing prevalence of 37.2% from a previous study in eastern Ethiopia (18). Accordingly, the calculated sample size was 359. After adding a 15% non-response rate, the final sample size was estimated to be 413.
After estimating the sample size, it was allocated proportionally to eight randomly selected kebeles within the district. Then, study participants were selected systematically by using the pregnancy screening registration book of health posts as a sampling frame.
Data collection and quality control
An interview-administered structured questionnaire that was adapted by reviewing previous literature was utilized to collect the data (5, 14, 26). The questionnaire was first prepared in English and then finalized and administered in Oromiffa. A house-to-house survey was employed to collect the data through face-to-face interview by eight clinical nurses, who are fluent in the local language (Oromiffa), and they were supervised by four B.Sc. nurses.
To ensure the quality of the collected data, 2 days training was given to data collectors and supervisors about the study’s aims and how to approach and interview pregnant women. The questionnaire was also pretested on 30 pregnant women in one of the kebeles of Chiro district, which was not included in the study. In addition, the collected data were verified every day for quality, completeness, and consistency.
Variables of the study
Dependent variable: our outcome variable of interest was the current khat chewing practice of pregnant women, which was a categorical variable with a yes or no response.
Independent variables: the independent variables include socio-demographic, reproductive, and behavioral characteristics of pregnant women, such as age, residence, religion, educational status, antenatal care (ANC) visit, history of abortion, pre-pregnancy khat use, alcohol use, etc.
Operational definitions
Current khat chewing: a woman who chewed khat at least once in the last month (14, 27).
Alcohol use: a woman who had ever used alcoholic drinks in her lifetime (27).
Mental distress: the level of mental distress was measured using a contextually validated self-reporting questionnaire (28). A woman was screened as positive for mental distress if she had seven or more yes responses out of the total 20 questions (26, 29).
Data processing and analysis
After checking for completeness, the data were coded and entered into EpiData version 3.1 software. Then, it was exported to STATA 14 statistical software for further analysis. Descriptive analysis like frequency and percentage was performed and presented in tables. Binary logistic regression was used to identify the determinants of khat chewing. Bi-variable logistic regression with a P-value less than 0.25 was used to select candidate variables for multivariable analysis. In the multivariable logistic regression model, the association between khat chewing and predictor variables was summarized using the adjusted odds ratio (AOR) and its 95% confidence intervals (CI). Besides, the fitness of the final model was verified using the Hosmer-Lemeshow goodness-of-fit test and classification table.
Results
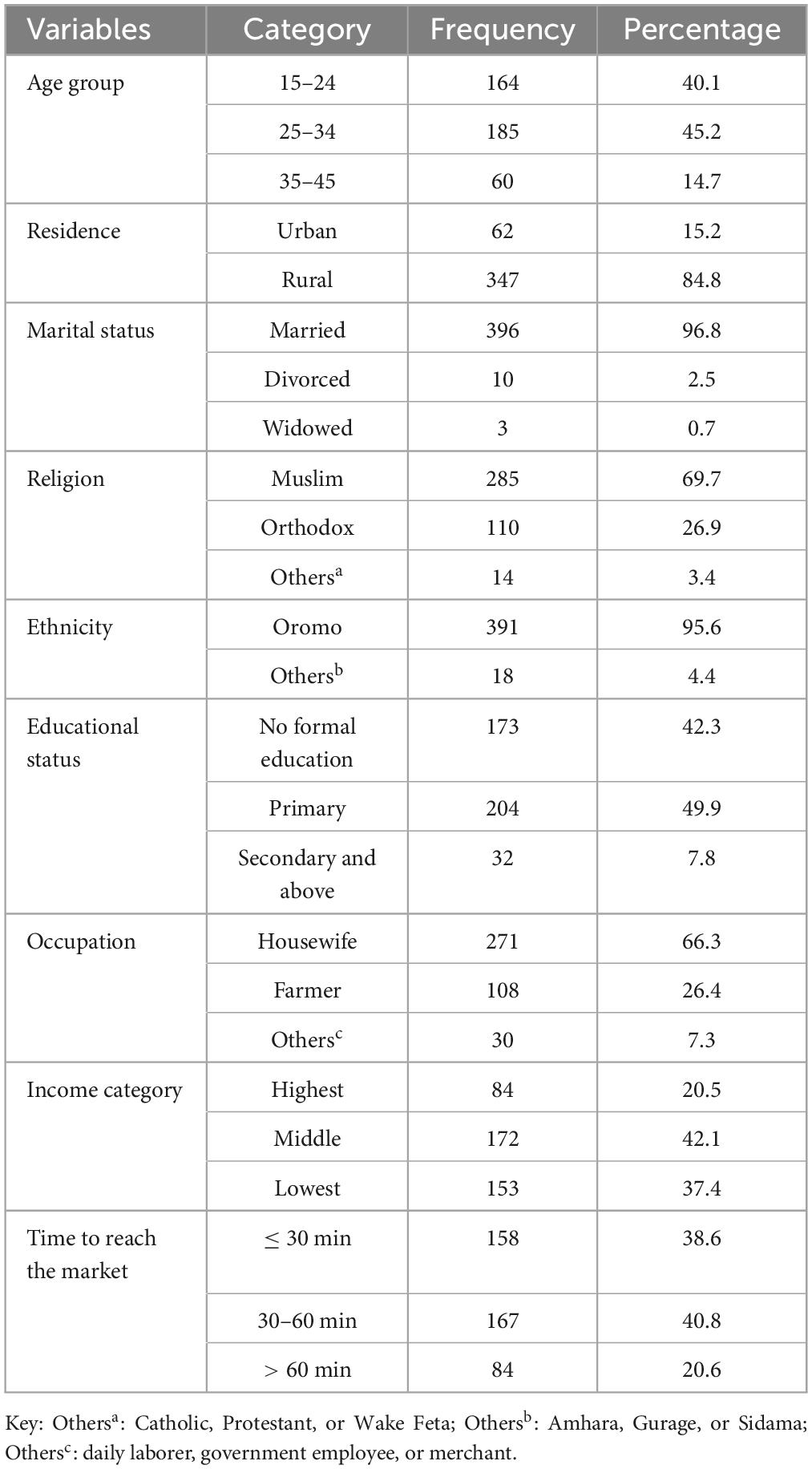
Scio-demographic characteristics of respondents
A total of 409 pregnant women participated in the study, with a response rate of 99%. The median age of the study participants was 26 years (IQR ± of 9 years). The majority of the respondents were rural dwellers (84.8%), married (96.8%), and Muslim religion followers (69.7%), (Table 1).
Reproductive features of pregnant women
Most (73.1%) of pregnant women had at least one ANC follow-up during their current pregnancy. More than half (53.3%) of women were in their second trimester, and about one in ten (12.0%) women had a history of abortion (Table 2).
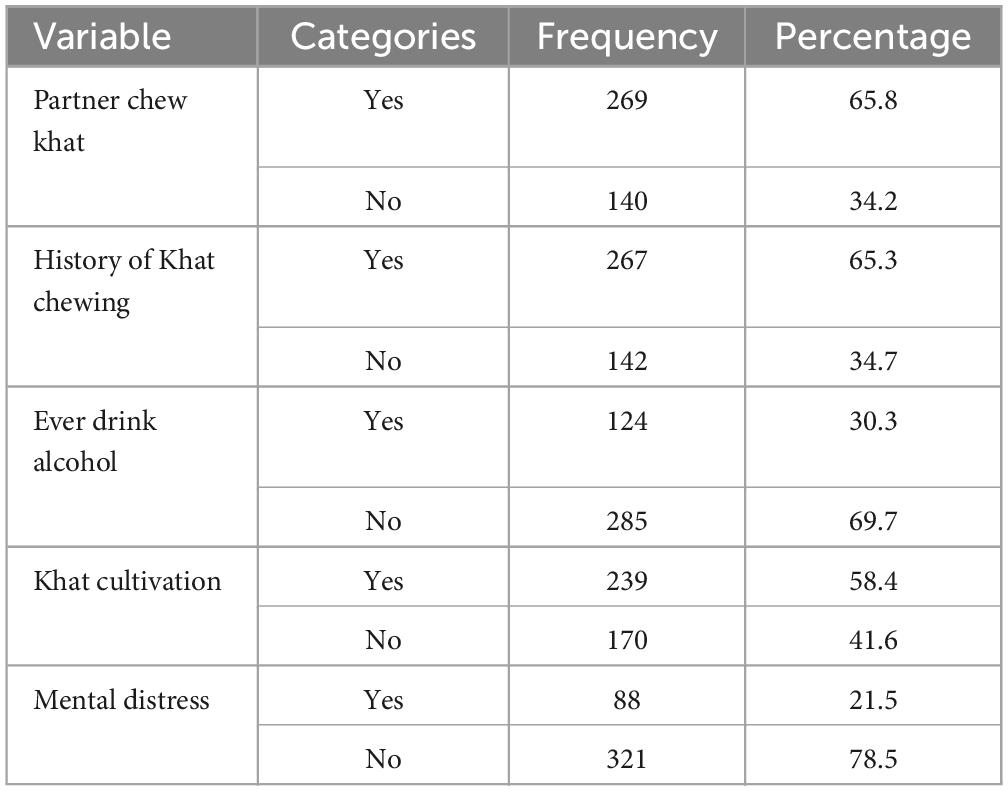
Behavioral characteristics of pregnant women
About two-thirds of pregnant women had partners who practiced khat chewing. Most of the respondents exercised khat cultivation (58.4%), and had a pre-pregnancy khat chewing history (65.3%), (Table 3).
Khat chewing and associated factors
In this study, 60.4% (95% CI: 55.5%, 65.2%) of pregnant women practice khat chewing (Figure 1). The bi-variable analysis indicated that residence, income, ANC visit, ethnicity, religion, educational status, partner khat use, pre-pregnancy khat chewing, khat cultivation, history of abortion, and mental distress had a P-value less than 0.25. Whereas, the multivariable logistic regression showed that religion, ANC visit, partner khat use, pre-pregnancy khat chewing, khat cultivation, and mental distress were significantly associated with current khat chewing with a P-value less than 0.05.
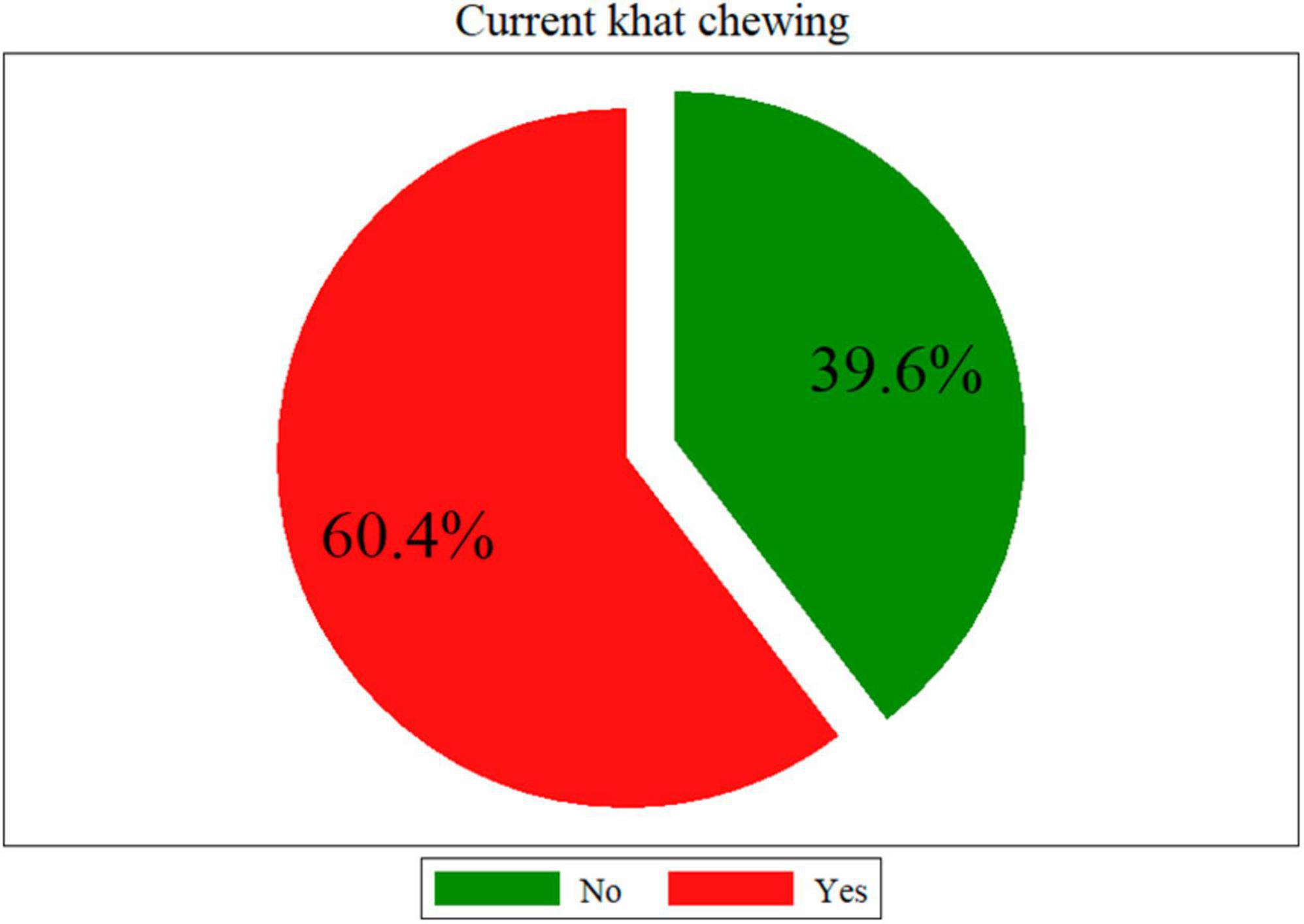
Figure 1. Prevalence of current khat chewing among pregnant women in Chiro district, eastern Ethiopia.
Correspondingly, women who were Muslim religion followers had 2.08 (95% CI: 1.13, 3.82) times higher odds of khat chewing as compared to Orthodox religion followers. Similarly, khat cultivation increases the likelihood of khat chewing by 57% (AOR: 0.43; 95% CI: 0.25, 0.77). The risk of khat chewing was 5.54 (95% CI: 3.11, 9.88) times higher among women who have khat chewer partners. The likelihood of current khat chewing was 9.95 (95% CI: 5.55, 17.81) times higher among women who were pre-pregnancy khat chewers than their counterparts. Pregnant women who had no ANC visit had a 2.71 (95% CI: 1.41, 5.21) times higher chance of khat chewing than women with at least one ANC visit for their current pregnancy. The odds of khat chewing were 4.89 (95% CI: 2.38, 10.02) times higher among women with mental distress than women without mental distress (Table 4).
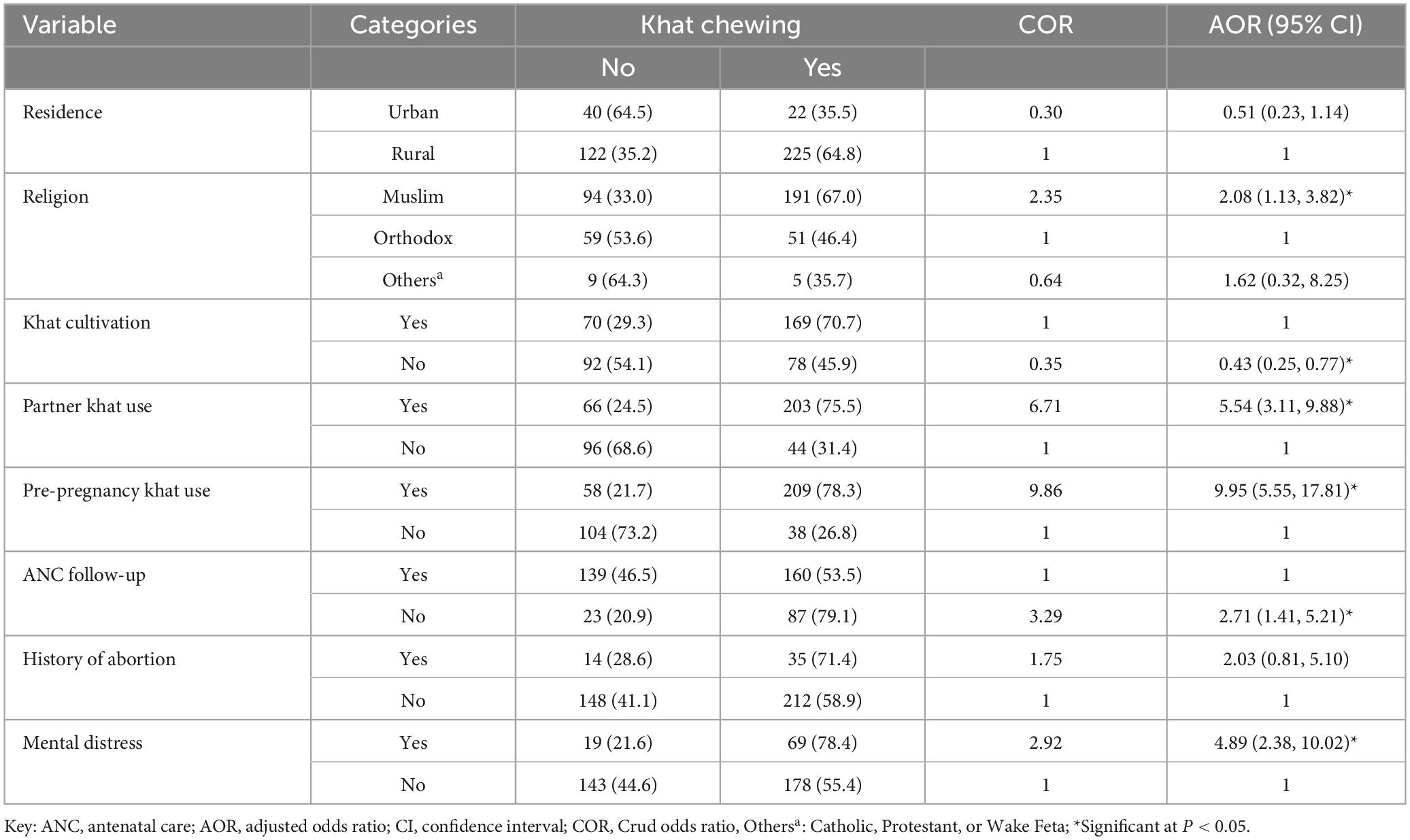
Table 4. Factors associated with khat chewing among pregnant women in Chiro district, eastern Ethiopia.
Discussion
Determining the extent and risk factors of khat chewing among pregnant women is important for public health planning and care. In reference to this, we assessed the prevalence and factors associated with current khat chewing among pregnant women in Chiro district, eastern Ethiopia. Accordingly, 60.4% of pregnant women practice khat chewing. Religion, khat cultivation, having a khat chewer partner, pre-pregnancy khat chewing, ANC visit, and mental distress were significantly associated with current khat chewing.
The overall prevalence of current khat chewing among pregnant women in the present study was in agreement with a previous report from Hossana, southern Ethiopia, 58% (22). However, the magnitude of khat chewing in this study was quite higher than previous reports from eastern Ethiopia, 15.5% (5); and southern Ethiopia, 9.9% (26). This might be due to the high production of khat in the current study area, thereby enhancing its accessibility and consumption (9). On the other hand, the prevalence of khat chewing in our study was lower than previous reports from Yemen, 90% (11); and Kenya, 81% (30). The possible explanation for this variation could be due to the difference in study population: that the estimate in Yemen and Kenya was among the general adult population, including men, and it is evidenced elsewhere that men had a higher risk of khat chewing than women (15).
In line with previous studies (14, 22), our analysis indicated that Muslim religion followers had higher odds of khat chewing. This might be due to the utilization of khat during religious rituals, as evidenced by a previous qualitative exploration (31). The likelihood of khat chewing was also higher among pregnant women who are from households that cultivate khat as compared to their counterparts. The possible explanation could be due to the easy availability and frequent exposure to the crop among women who cultivate it.
The present study found higher odds of khat chewing among pregnant women who had a khat chewer partner than their counterparts. This association was also detected by previous studies (22, 26), and might be due to the need for increasing intimacy and socialization with their partners (1). Similar to previous reports (32), the likelihood of khat chewing was higher among pregnant women with a history of pre-pregnancy khat chewing than among women without such a history. This might be due to the development of psychological dependency and addiction among khat chewers (33). Poor knowledge about the feto-neonatal and maternal consequences of antenatal khat chewing could also be another reason (16).
Our analysis found that attending ANC reduces the likelihood of khat chewing during pregnancy. Accordingly, pregnant women who had no ANC visit for the current pregnancy were more likely to practice khat chewing than women who had at least one ANC visit. This could be partly because women who do not attend ANC may not be informed about the harmful consequences of khat chewing. Hence, indicating the comprehensive role of ANC on maternal and child health. Consistent with previous studies (26, 34), the odds of khat chewing were higher among pregnant women with mental distress as compared to those without it. This might be to use the early euphoric and psycho-stimulant effect of khat as a remedy for the experienced mental distress, yet not understanding or ignoring its enormous negative consequences (16, 35). On the other hand, this might be due to the psychiatric consequences of khat chewing (21). Hence, calling for mental health and psychosocial support for khat chewers.
This study has certain limitations. The cross-sectional nature of the study makes it difficult to establish a causal association. Feto-maternal outcomes of pregnant women were not assessed in relation to their khat chewing pattern. Besides, despite the close tie between khat chewing and cultural norms, our study was not triangulated with a qualitative design.
Conclusion
The majority of pregnant women in the study area practice khat chewing. Religion, khat cultivation, partner khat use, pre-pregnancy khat use, ANC visit, and mental distress were significantly associated with current khat chewing. Thus, accessible and comprehensive pre-conception and pre-natal care incorporating the prevention and management of antenatal khat chewing is crucial to overcome this problem. Provision of mental healthcare involving partners of pregnant women is also important to reduce the extent and impacts of khat chewing during pregnancy. Further longitudinal studies triangulated with qualitative designs are recommended.
Data availability statement
The original contributions presented in this study are included in this article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
Ethical approval was granted by the Oda Bultum University Ethical Review Committee. The study was performed in accordance with the declaration of Helsinki’s ethical principles for medical research involving human subjects. Informed consent was obtained from all pregnant women who participated in this study after a detailed explanation of the purpose of the research and the right to withdraw from the study at any time. Besides, confidentiality of the collected information was assured by not recording women’s personal identifiers.
Author contributions
HG conceived the study. HG, FK, AN, MM, and DG designed the study, supervised data collection, analyzed the data, wrote the first draft, and critically reviewed the manuscript. All authors have read and approved the final manuscript.
Acknowledgments
We acknowledge Oda Bultum University for approving the study proposal. We are also grateful for the study participants, data collectors, and supervisors.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Fiidow O, Minhat H, Zulkefli N, Ahmad N. A systematic review on risk factors for khat chewing among adolescents in the African continent and Arabian Peninsula. PLoS One. (2022) 17:e0263372. doi: 10.1371/journal.pone.0263372
2. Ageely H. Health and socio-economic hazards associated with khat consumption. J Fam Commun Med. (2008) 15:3–11.
3. Mohamed Abdoul-Latif F, Ainane A, Houmed Aboubaker I, Merito Ali A, El Montassir Z, Kciuk M, et al. Chemical composition of the essential oil of catha edulis forsk from djibouti and its toxicological investigations in vivo and in vitro. Processes. (2023) 11:1324.
4. Graziani M, Milella M, Nencini P. Khat chewing from the pharmacological point of view: an update. Subst Use Misuse. (2008) 43:762–83.
5. Misgana T, Tesfaye D, Alemu D, Gebremichael B, Tamiru D, Tariku M, et al. Khat use and associated factors during pregnancy in eastern Ethiopia: a community-based cross-sectional study. Front Glob Womens Health. (2022) 3:941300. doi: 10.3389/fgwh.2022.941300
7. Ardabili H, Akbari A, Rafei P, Butner J, Khan R, Khazaal Y, et al. Tramadol, captagon and khat use in the Eastern Mediterranean Region: opening Pandora’s box. BJPsych Int. (2022) 19:58–62.
8. Ye S, Hu J, Liu Z, Liang M. Progress and research trends on Catha Edulis (Vahl) Endl. (Catha Edulis): a review and bibliometric analysis. Front Pharmacol. (2021) 12:705376. doi: 10.3389/fphar.2021.705376
9. Tofu D, Wolka K. Climate change induced a progressive shift of livelihood from cereal towards Khat (Chata edulis) production in eastern Ethiopia. Heliyon. (2023) 9:e12790.
10. Sutan R, Al-Dubai S, Aljunid S. Family context and Khat chewing among adult Yemeni women: a cross-sectional study. Biomed Res Int. (2014): 2014:505474.
12. Ongeri L, Kirui F, Muniu E, Manduku V, Kirumbi L, Atwoli L, et al. Khat use and psychotic symptoms in a rural Khat growing population in Kenya: a household survey. BMC Psychiatry. (2019) 19:137. doi: 10.1186/s12888-019-2118-3
13. Hagos E, Asfeha G, Berihu B. Prevalence of substance abuse among regular degree health science students in Sheba University College in Mekelle Town, Tigray-Ethiopia. J Neurosci Rural Pract. (2016) 7:200–5.
14. Yitayih Y, van Os J. Prevalence and determinants of chewing khat among women in Ethiopia: data from Ethiopian demographic and health survey 2016. BMC Psychiatry. (2021) 21:127. doi: 10.1186/s12888-021-03136-y
15. Adugna F, Jira C, Molla T. Khat chewing among Agaro secondary school students, Agaro, southwestern Ethiopia. Ethiopian Med J. (1994) 32:161–6.
16. Yitayih Y, Vanderplasschen W, Vandewalle S, Rita V, Gilbert L. The effects of khat use during pregnancy on perinatal and maternal outcomes: a meta-analysis. Arch Womens Ment Health. (2023) 26:11–27.
17. Abdel-Aleem M. Khat chewing during pregnancy: an insight on an ancient problem. Impact of chewing Khat on maternal and fetal outcome among Yemeni pregnant women. J Gynecol Neonatal Biol. (2015) 1:1–04.
18. Yadeta T, Egata G, Seyoum B, Marami D. Khat chewing in pregnant women associated with prelabor rupture of membranes, evidence from eastern Ethiopia. Pan Afr Med J. (2020) 36:1.
19. Mekonnen A, Hordofa A, Kitila T, Sav A. Modifiable risk factors of congenital malformations in bale zone hospitals, Southeast Ethiopia: an unmatched case-control study. BMC Pregn Childbirth. (2020) 20:129. doi: 10.1186/s12884-020-2827-0
20. Hunde A, Demissie D, Garado T, Feyisa J, Kitila K. Caffeine consumption, khat chewing, and associated factors among pregnant mothers in Illu Aba Bor Zone, South West Ethiopia. Int J Afr Nurs Sci. (2023) 18:100559.
21. Malasevskaia I, Al-Awadhi A, Mohammed L. Tea in the morning and khat afternoon: health threats due to khat chewing. Cureus. (2020) 12:e12363.
22. Rather R, Berhanu S, Abaynah L, Sultan M. Prevalence of Khat (Catha edulis) chewing and its determinants: A respondent-driven survey from Hossana, Ethiopia. Subst Abuse Rehabil. (2021) 12:41–8.
23. Akalu T, Baraki A, Wolde H, Lakew A, Gonete K. Factors affecting current khat chewing among male adults 15–59 years in Ethiopia, 2016: a multi-level analysis from Ethiopian Demographic Health Survey. BMC Psychiatry. (2020) 20:21. doi: 10.1186/s12888-020-2434-7
24. Ayano G, Ayalew M, Bedaso A, Duko B. Epidemiology of Khat (Catha edulis) chewing in ethiopia: a systematic review and meta-analysis. J Psychoact Drugs. (2022) [Epub ahead of print].
25. Alemu W, Zeleke T, Takele W, Mekonnen S. Prevalence and risk factors for khat use among youth students in Ethiopia: systematic review and meta-analysis, 2018. Ann Gen Psychiatry. (2020) 19:16.
26. Mekuriaw B, Belayneh Z, Yitayih Y. Magnitude of Khat use and associated factors among women attending antenatal care in Gedeo zone health centers, southern Ethiopia: a facility based cross sectional study. BMC Public Health. (2020) 20:110. doi: 10.1186/s12889-019-8026-0
27. Yeshaw Y, Zerihun M. Khat chewing prevalence and correlates among university staff in Ethiopia: a cross-sectional study. BMC Res Notes. (2019) 12:673. doi: 10.1186/s13104-019-4706-1
28. Hanlon C, Medhin G, Alem A, Araya M, Abdulahi A, Hughes M, et al. Detecting perinatal common mental disorders in Ethiopia: validation of the self-reporting questionnaire and Edinburgh postnatal depression scale. J Affect Disord. (2008) 108:251–62.
29. Scholte W, Verduin F, van Lammeren A, Rutayisire T, Kamperman A. Psychometric properties and longitudinal validation of the self-reporting questionnaire (SRQ-20) in a Rwandan community setting: a validation study. BMC Med Res Methodol. (2011) 11:116. doi: 10.1186/1471-2288-11-116
30. Hassan H, Guyo S, Ndemwa M, Karama M, Mwaniki P. Health effects and association of demographic characteristics with khat chewing for residents between 18-50 years in moyale sub-county, Kenya. East Afr Med J. (2021) 98:3590–98.
31. Mihretu A, Fekadu A, Habtamu K, Nhunzvi C, Norton S, Teferra S. Exploring the concept of problematic khat use in the Gurage community, South Central Ethiopia: a qualitative study. BMJ Open. (2020) 10:e037907.
32. Fetene M, Teji K, Assefa N, Bayih W, Tsehaye G, Hailemeskel H. Magnitude and associated factors of substance use among pregnant women attending antenatal care in public hospitals of eastern Ethiopia. BMC Psychiatry. (2021) 21:96. doi: 10.1186/s12888-021-03078-5
33. El-Setouhy M, Alsanosy R, Alsharqi A, Ismail A. Khat dependency and psychophysical symptoms among chewers in Jazan Region, Kingdom of Saudi Arabia. Biomed Res Int. (2016) 2016:2642506.
34. Damena T, Mossie A, Tesfaye M. Khat chewing and mental distress: a community based study, in Jimma city, southwestern Ethiopia. Ethiopian J Health Sci. (2011) 21:37–45.
Keywords: prevalence, khat chewing, addiction, pregnant women, Ethiopia
Citation: Geremew H, Kebede FA, Negash A, Mengstie MA and Geremew D (2023) Khat chewing and its associated factors among pregnant women in Chiro district, eastern Ethiopia: a community-based study. Front. Psychiatry 14:1253128. doi: 10.3389/fpsyt.2023.1253128
Received: 05 July 2023; Accepted: 27 October 2023;
Published: 15 November 2023.
Edited by:
Berihun Dachew, Curtin University, AustraliaReviewed by:
Taiwo Lateef Sheikh, Ahmadu Bello University, NigeriaVahid Farnia, Kermanshah University of Medical Sciences, Iran
Copyright © 2023 Geremew, Kebede, Negash, Mengstie and Geremew. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Habtamu Geremew, aGFidGVnMjlAZ21haWwuY29t
 Habtamu Geremew
Habtamu Geremew Fekadu Abera Kebede
Fekadu Abera Kebede Abraham Negash
Abraham Negash Misganaw Asmamaw Mengstie
Misganaw Asmamaw Mengstie Demeke Geremew
Demeke Geremew