- 1Department of Psychiatry, Vitalite Health Network, Campbellton, NB, Canada
- 2Department of Psychiatry at the Centre for Addiction & Mental Health, University of Toronto, Toronto, ON, Canada
The authors present a rare case of a family in which both the mother, and four decades later the son, committed second-degree murder while suffering from major mental illnesses. The mother had successfully used a mental disorder defence and it was likely that the son who had raised the defence would have qualified also. The mother has a history of adverse childhood experiences. The son had also experienced various severe childhood adversities, though there were no functional impairments, personality dysfunction, suicidality or violent crimes until the onset of treatment-resistant schizoaffective disorder around age 18. His earlier comorbidities included sport-related traumatic brain injuries, sickle cell trait, severe burns, and tardive dyskinesia. His comorbidities around the material time included occasional cannabis use and dementia pugilistica. While awaiting court ruling on criminal responsibility, additional stressors triggered significant deterioration of his schizoaffective disorder and the court found him unfit to stand trial. During rehabilitation, he was severely injured by another accused, which subsequently led to his demise. This case is the first report of intergenerational mental disorder defence and involved almost every facet of criminal forensic psychiatry, which highlights the need for further research on the association between intergenerational ACEs and intergenerational risk for criminal behaviour from a comprehensive and longitudinal perspective.
Introduction
Adverse childhood experiences (ACEs) are potentially traumatic or stressful events occurring in the first 18 years of life (1). The link between ACEs and impairments in health and wellbeing has been well documented (1). Many studies have also associated high parental ACE scores with child adversity (2–4). Further, there is a converging body of evidence that highlights the association between exposure to ACEs and adult criminal behaviours (5, 6). In 2021, Guina et al. published the first study on the prevalence of trauma and posttraumatic stress disorder (PTSD) among acquittees who had been adjudicated not guilty by reason of insanity (NGRI), and found that most NGRI acquittees had experienced trauma (86%, averaging 11 events) and ACEs (76%, averaging 3 types) (7). Nevertheless, a Pubmed search with keywords intergeneration and mental disorder defence, dated May 6, 2023, did not yield any relevant study. This study is the first case study on intergenerational mental disorder defence, and involves almost every facet of criminal forensic psychiatry. Given the emerging data on intergenerational transmission of ACEs and on ACEs as criminogenic risk factors among the forensic population, it has become increasingly apparent that the association between intergenerational ACEs and intergenerational risk for criminal behaviour is an important topic in forensic psychiatry.
Case presentation (patient 1)
Patient 1 had been charged with killing her 2-year-old son. Her two other children (including patient 2) were taken into care and placed in the home of her older sister. Patient 1 had been born and raised on a farm. She is from a large family and had little formal schooling. Later it was established that she had been the victim of multiple sexual assaults from various members of the family. At 16 she came to Ontario, and entered into a series of unhealthy relationships. She had three children in the next few years. She began to believe that she was possessed and that the only way to save her son was to strangle him.
Patient 1 had no psychiatric history before the offence. She was diagnosed with psychotic depression as well as alcohol abuse during her first psychiatric admission for an assessment of fitness to stand trial. Having originally been found unfit to stand trial she was treated to fitness, and was subsequently found not guilty by reason of insanity (as the term was according to the Criminal Code of Canada at the time). She was detained at the pleasure of Her Majesty (as was dictated in the Criminal Code at the time), in the forensic unit. She was treated with antipsychotics and antidepressants and she was gradually able to engage in a lengthy course of forensic rehabilitation. She was subject to a hearing of the Lieutenant Governor’s Board of Review every year (The Canadian Review Board System later replaced the Lieutenant Governor’s Board of Review in 1992 with the proclamation of Bill C-30). Although strictly speaking, the latter only had the statutory power to recommend to the Lieutenant governor whether she was ready to be released, it was developing its own policies and procedures for cascading patients into the community (i.e., gradual conditional release over some years).
The outcome of the patient’s forensic rehabilitation has been successful. After 8 years, she had worked her way up to having privileges for up to 12 h passes per day from the unit. Independently, to the surprise of the multidisciplinary team, 1 day she returned to say she had got a job working nights at a manual job. After much discussion, the team agreed that she could take the job, and she started working every night for the next 20 years, until physical problems intervened and she had to go on disability. 41 years since the senior author (GG) first met her, the former continues to see the latter as an outpatient, now only on an occasional, as-needed basis and she has not required rehospitalization. She shares an apartment with her partner of 20 years, plays bingo regularly, and supports her daughter and grandchildren who live in the same apartment block.
Case presentation (patient 2)
The index offences took place when patient 2 was around 50 years of age. He passed away in the following year. He was single and had no dependents at the material time. Prior to the index offences, he resided in an apartment and worked part-time in a restaurant. He was financially supported by disability benefits. His mother (patient 1) and sister were living in another province and he maintained regular contact with them.
The patient has a significant history of ACEs and scored positive on almost every item of the ACE questionnaire. He has a significant family history of mental illnesses. His mother suffered from psychotic depression, and his sister was diagnosed with bipolar disorder. The mother was financially supported by welfare when the patient was born. During pregnancy, she experienced domestic violence from the father, and they broke up at the time. Before the age of eight, the patient was sexually abused by his grandparent. The patient had two siblings. When he was 7 years old, his mother (patient 1) was charged with killing his 2-year-old brother. Following that incident, the patient and his sister were adopted by family members. The patient was physically and sexually abused by his adoptive family members from age eight to 14. At the age of 15, he went back to live with his mother, while his sister stayed with the adoptive family who sexually abused her as well. Through the intervention of the Children’s Aid Society (child welfare), the sister eventually reunited with the family. The patient had a good relationship with his mother who financially supported him when he had difficulty providing for himself, and he had little contact with his father.
The rest of the patient’s background and personal history did not note further concerns until the onset of his mental illness. The patient’s family described him as an honest person when clinically stable. There was no history of conduct-disordered behaviours in his childhood or teenage years. There were no initial learning difficulties and the patient went to study in university. Nevertheless, he had to discontinue his university studies 2 years later due to the onset of his schizoaffective disorder. He had also been a former boxer, and he had to discontinue his career in boxing as a result of the impact of his severe mental illness as well. He had several romantic relationships up and until 2 years before the material time, which all ended during his relapses.
With regards to the patient’s medical history and substance use history, aside from sickle cell traits diagnosed early on, sport-related concussions during his boxing career, coma induced by hypothermia in his twenties, and severe burns, there was no other reported significant medical history. He endorsed marijuana use as well as alcohol use from age 13 to 15, and denied any other history of substance use.
With the onset of schizoaffective disorder at age 18, aside from the mood episodes, the patient’s symptoms mainly consisted of religious delusions and auditory hallucinations. Although he had always believed in religion, his religious beliefs reached delusional intensity following the onset of his mental illness. The patient’s prior run-ins with the police all took place in the context of florid psychosis. He also used to call the police to bring him to the hospital during his relapses. From age 18 to 42, with various psychiatric admissions and treatment adjustments, his psychotic symptoms significantly improved after initiating treatment with olanzapine and lorazepam. He was overall able to remain active and was teaching boxing in a gym. The side effects at the time included weight gain and gynecomastia. He was referred to a plastic surgeon, though he decided to hold off until further weight loss. He had access to relevant and appropriate community care, and there were no substance use or medication compliance issues. Around age 42, he decided to move to another province to stay closer to his mother’s side of the family.
The patient presented with a fluctuating course of illness after he had moved to another province. He continued to suffer from his well-described chronic major mental illness of psychotic proportions. He had repeated psychiatric admissions and developed tardive dyskinesia. His relapse pattern typically consisted of psychotic decompensation associated with non-adherence to medication. When discharged from the hospital, he generally lived in his own apartment and was followed by the flexible assertive community treatment (FACT) team. His treatment mainly consisted of antipsychotic medications and mood stabilizers, and involved several medication adjustments in the context of treatment resistance. Prior to the index offences around age 50, his medications included lamotrigine 50 mg at bedtime, quetiapine 200 mg at bedtime, haloperidol 5 mg daily, olanzapine 20 mg twice daily, temazepam 30 mg at bedtime, and lorazepam 1 mg daily, and tertrabenazine.
In the period of time leading up to the index offences, the patient presented as paranoid and disorganized in his behaviour and thinking, with associated odd behaviours and thoughts. He presented with commanding auditory hallucinations, with reference to religious, grandiose, and trauma-related themes. He began to believe he was Messiah and that he needed to sacrifice himself to save the world. To achieve this purpose, he was planning to buy a weapon from the victim. The patient recalled the following auditory hallucinations, which he perceived as voices emanating from the unrelated victim around the material time with reference to his history of ACEs: “The voices of devil – voices of my uncle who sexually abused me. My cousin also sexually abused my sister, and I told her I would protect her. My cousin and uncle saying that I should murder myself, I’m no good.” The patient reported having the following thoughts at the time: “Thoughts of revenge, beating them…” He also recalled feeling obliged to cleanse the world of wickedness as Messiah and repeatedly talked about Armageddon. He acknowledged that these psychotic features had led to the alleged use of the purchased weapon toward the victim and the subsequent charge of second-degree murder.
Following the index offence and after being found fit to stand trial, the patient (he was an accused at the time) and his lawyers raised the not criminally responsible (NCR) defence. The court-ordered psychiatric assessment of criminal responsibility at the time revealed the initial diagnoses of schizoaffective disorder, bipolar type, non-compliance with medication, possible neurocognitive disorder and occasional cannabis use, though the urine drug screen was negative. Despite his history of sickle cell traits, the initial medical assessment did not find sufficient evidence to support any related correlation with his symptomatology at the time. Following his clinical stabilization in an inpatient forensic assessment facility, neurology assessment noted the diagnosis of dementia pugilistica, though cognitive testing suggested that the ability to retain and recall information was intact.
The final comprehensive forensic psychiatric assessment found that the patient likely would not have been able to access the rational choice about his behaviours at the time as a result of the burden of his religious and grandiose delusions, as well as his auditory hallucinations, and the decompensation of his schizoaffective disorder was more likely than not the primary driving factor. As laid out in R. v. Oomen (Supreme Court of Canada ruling in 1994), the crux of the inquiry is whether the accused lacks the capacity to rationally decide whether the act is right or wrong and hence to make a rational choice about whether to do it or not. Accordingly, from a purely psychiatric perspective and on the balance of probabilities, a defence of not criminally responsible on account of mental disorder likely would have been available to him on that basis.
At the initial court hearing on criminal responsibility, the Court decided to admit the findings of the above-mentioned forensic psychiatric assessment as expert witness evidence, and the Crown did not challenge the mental disorder defence by calling in second opinion. The Crown prosecutor was planning, however, to have the co-author (YCY) who had completed the forensic assessments testify in court given the high-profile nature of this case. While awaiting the next court hearing on criminal responsibility, additional stressors at the correctional centre had triggered significant deterioration of the patient’s schizoaffective disorder and the Court ordered another fitness-to-stand-trial assessment. The co-author (YCY) completed this assessment and testified in court. The judge admitted the expert witness evidence and rendered a verdict of unfit to stand trial, as the patient’s persistent suicidal ideation in the context of religious delusions, the related impairment in concentration and the associated defect in his capacity for self-preservation had caused significant impairments in his ability to meaningfully participate in proceedings. The judge indicated at the end of the hearing that the Court would arrange another hearing on the NCR defence if the patient’s fitness could be eventually restored through rehabilitation. During rehabilitation, the patient was severely injured by another accused, which subsequently led to his demise (Figures 1A,B).
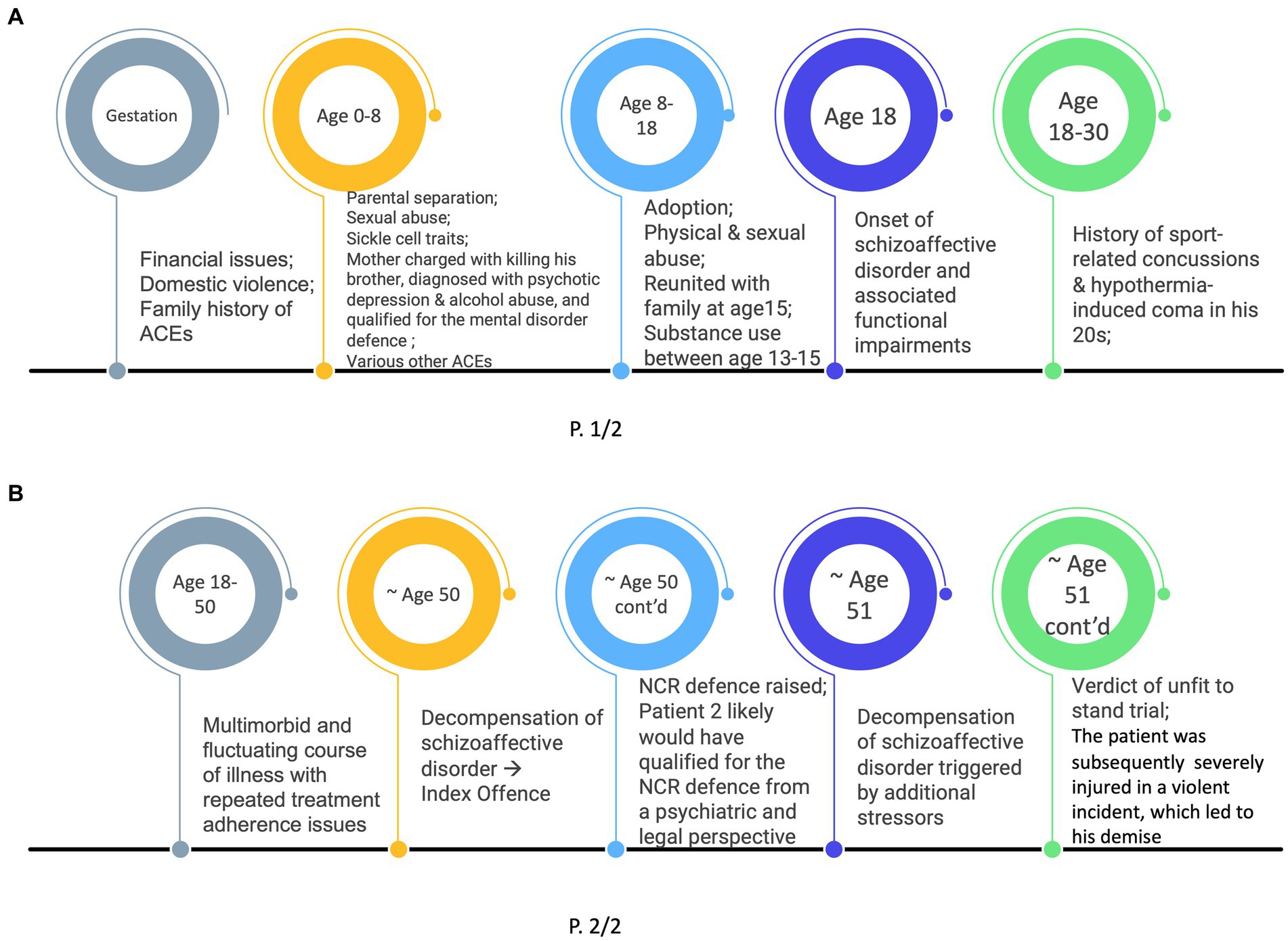
Figure 1. (A) Timeline of Patient 2’s History – Gestation to Age 30. (B) Timeline of Patient 2’s History – Age 18 (cont’d) to Age 51.
Patient perspective
Please refer to the case presentation on patient 2 for his perspective, and the conclusion for the perspective of patient 1.
Discussion
This case study is the first report of intergenerational mental disorder defence. Both subjects went through comprehensive forensic psychiatric assessments and court proceedings within the framework of Canada’s Criminal Justice System supported by extensive objective data and evaluations by qualified medico-legal experts, which significantly limited recall bias and interviewer bias. The limitations of this study included the absence of similar cases in literature and the absence of control for potential confounding factors.
This case illustrates the findings from recent studies on intergenerational ACEs and on the association between ACEs and risk for criminal behaviours. The 2021 longitudinal study published by Schickedanz et al. found that among the 2,205 parent–child dyads, children of parents with four or more ACEs had 3.25-fold higher risk of experiencing four or more ACEs themselves, compared to children of parents without ACEs, and mothers’ ACE counts were more strongly associated with their children’s ACE counts than were fathers’ ACE counts (8). The 2023 prospective cohort study by Bolhuis et al. found that the intergenerational transmission of childhood adversity could be relevant in the aetiology of psychosis vulnerability (9). The 2023 retrospective cohort study by Moog et al. suggested that children of mothers exposed to childhood maltreatment were more likely to exhibit a diagnostic pattern characterized by higher risk for multimorbidity (10). In addition to the growing evidence that has highlighted the association between exposure to ACEs and adult criminality (5, 6), the 2021 cross-sectional study by Guina et al. found a high prevalence (76%) of ACEs among the 107 NGRI acquittees, and noted a higher prevalence of trauma in the forensic population than what had been reported in the general population (7).
The specific mechanism underlying the intergenerational transmission of the effects of ACEs remains unknown, though several mechanisms have been hypothesized, including epigenetic inheritance, pathways involving variations in gestational biology, and shared biopsychosocial challenges across generations (10, 11). Emerging data has also suggested an association between maternal ACEs and newborn brain development (12, 13). The 2018 prospective longitudinal study by Moog et al. also found an association between maternal exposure to childhood maltreatment and lower child intracranial volume (13). The 2022 longitudinal study by Demers et al. demonstrated that higher maternal ACEs were associated with smaller neonatal left amygdala volume (12). However, further studies will be needed to investigate their potential correlation or causation.
This first case study on intergenerational mental disorder defence noted significant intergenerational continuity of ACEs, psychopathologies, and criminogenic risk factors, and involved almost every facet of criminal forensic psychiatry. Further research is needed to investigate the correlation between intergenerational ACEs and intergenerational risk for criminal behaviour in the forensic setting, as well as the mechanisms underlying this intergenerational transmission of risk that could serve as potential targets for clinical intervention.
Conclusion
The circle game, a song by Joni Mitchell, resonates well the theme of this study, “And the seasons, they go round and round and the painted ponies go up and down. We’re captive on the carousel of time… And go round and round and round, in the circle game.” Nevertheless, the mother of the patient chose to take a step further through her decision to contribute her family’s case to scientific research with the hope of helping find measures that could mitigate the risk factors perpetuating the intergenerational cycle of trauma and its associated adverse outcomes. She gave informed consent as well as informed substitute consent (on behalf of patient 2) authorizing the publication of this case study. Her contribution struck a note of resolution and allowed the preparation of this case study. As highlighted by Theodor Mommsen’s closing remark in the first paragraph of the History of Rome, “The grandest system of civilization has its orbit, and may complete its course but not so the human race, to which, just when it seems to have reached its goal, the old task is ever set anew with a wider range and with a deeper meaning.”
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: Due to the strictly confidential nature of medico-legal file information in Canada, data analyzed during this study is not publicly available. Requests to access these datasets should be directed to YY, eXUueXVlQHZpdGFsaXRlbmIuY2E=.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article. Written informed consent was obtained from the participant/patient(s) for the publication of this case report.
Author contributions
GG contributed to the conceptualization, project administration, supervision, writing – review, editing, manuscript revision, as well as the reading and approval of the submitted version. YY performed the search of literature and prepared the first draft of the manuscript. YY and GG contributed to writing the draft of the case presentations. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Centers for Disease Control and Prevention. Preventing adverse childhood experiences: leveraging the best available evidence. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention (2019).
2. Narayan, AJ, Kalstabakken, AW, Labella, MH, Nerenberg, LS, Monn, AR, and Masten, AS. Intergenerational continuity of adverse childhood experiences in homeless families: unpacking exposure to maltreatment versus family dysfunction. Am J Orthopsychiatry. (2017) 87:3–14. doi: 10.1037/ort0000133
3. Randell, KA, O’Malley, D, and Dowd, MD. Association of parental adverse childhood experiences and current child adversity. JAMA Pediatr. (2015) 169:786. doi: 10.1001/jamapediatrics.2015.0269
4. Skolnick, VG, Lynch, BA, Smith, L, Romanowicz, M, Blain, G, and Toussaint, L. The association between parent and child ACEs is buffered by forgiveness of others and self-forgiveness. J Child Adolesc Trauma. (2023):1–9. doi: 10.1007/s40653-023-00552-y
5. Basto-Pereira, M, Gouveia-Pereira, M, Pereira, CR, Barrett, EL, Lawler, S, Newton, N, et al. The global impact of adverse childhood experiences on criminal behavior: a cross-continental study. Child Abuse Negl. (2022) 124:105459. doi: 10.1016/j.chiabu.2021.105459
6. Reavis, JA, Looman, J, Franco, KA, and Rojas, B. Adverse childhood experiences and adult criminality: how long must we live before we possess our own lives? Perm J. (2013) 17:44–8. doi: 10.7812/TPP/12-072
7. Guina, J, Audu, AK, Cameron, J, Lemmen, A, Mamidipaka, A, and Kletzka, N. Prevalence of traumas and PTSD among individuals adjudicated not guilty by reason of insanity. J Am Acad Psychiatry Law. (2021) 49:194–201. doi: 10.29158/JAAPL.200062-20
8. Schickedanz, A, Escarce, JJ, Halfon, N, Sastry, N, and Chung, PJ. Intergenerational associations between parents’ and children’s adverse childhood experience scores. Children. (2021) 8:747. doi: 10.3390/children8090747
9. Bolhuis, K, Steenkamp, LR, Tiemeier, H, Blanken, L, Pingault, J-B, Cecil, CAM, et al. A prospective cohort study on the intergenerational transmission of childhood adversity and subsequent risk of psychotic experiences in adolescence. Schizophr Bull. (2023) 49:799–808. doi: 10.1093/schbul/sbac195
10. Moog, NK, Cummings, PD, Jackson, KL, Aschner, JL, Barrett, ES, Bastain, TM, et al. Intergenerational transmission of the effects of maternal exposure to childhood maltreatment in the USA: a retrospective cohort study. Lancet Public Health. (2023) 8:e226–37. doi: 10.1016/S2468-2667(23)00025-7
11. Moog, NK, Heim, CM, Entringer, S, Simhan, HN, Wadhwa, PD, and Buss, C. Transmission of the adverse consequences of childhood maltreatment across generations: focus on gestational biology. Pharmacol Biochem Behav. (2022) 215:173372. doi: 10.1016/j.pbb.2022.173372
12. Demers, CH, Hankin, BL, Hennessey, E-MP, Haase, MH, Bagonis, MM, Kim, SH, et al. Maternal adverse childhood experiences and infant subcortical brain volume. Neurobiol Stress. (2022) 21:100487. doi: 10.1016/j.ynstr.2022.100487
Keywords: adverse childhood experiences, intergeneration, mental disorder defence, NCRMD, unfit to stand trial, forensic, complex care and recovery, criminogenic risks
Citation: Yue YC and Glancy G (2023) Case report: The Circle Game. Front. Psychiatry. 14:1241540. doi: 10.3389/fpsyt.2023.1241540
Edited by:
Heng Choon (Oliver) Chan, University of Birmingham, United KingdomReviewed by:
Märta Wallinius, Lund University, SwedenCharles Saldanha, University of California, San Francisco, United States
Copyright © 2023 Yue and Glancy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yu Chen Yue, eXVjaGVuLnl1ZUBtYWlsLnV0b3JvbnRvLmNh
 Yu Chen Yue
Yu Chen Yue Graham Glancy
Graham Glancy