
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 25 August 2023
Sec. Psychological Therapy and Psychosomatics
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1241190
 Galia Bahadori-Birgani1
Galia Bahadori-Birgani1 Shahram Molavynejad1*
Shahram Molavynejad1* Mahbobe Rashidi2
Mahbobe Rashidi2 Fereshteh Amiri2
Fereshteh Amiri2 Elham Maraghi3
Elham Maraghi3 Bahman Dashtbozorgi1
Bahman Dashtbozorgi1 Zulvikar Syambani Ulhaq4
Zulvikar Syambani Ulhaq4 Gholamreza Alizadeh-Attar5
Gholamreza Alizadeh-Attar5Introduction: The COVID-19 virus spreads at a high rate, exerting many physical, mental and psychological effects on patients. Patients with COVID-19 have been reported to have high levels of interleukin 1 and interleukin 6. Therefore, this study was conducted to determine the association of physical, mental, and psychological problems with the levels of interleukin-1 and -6 in COVID-19 patients.
Methodology: This is cross-sectional descriptive-analytical research on 121 COVID-19 patients selected using simple random sampling method. The patients were hospitalized in university hospitals affiliated to Ahvaz Jundishapur University of Medical Sciences and Amir al-Momenin Hospital. Data collection tools included the depression anxiety stress scale (DASS), a demographic questionnaire, and a checklist of physical problems. Blood sampling was also done to perform an ELISA test and measure the level of interleukin-1 and -6. Data were analyzed based on independent t-tests, chi-square, regression, and Pearson’s correlation coefficient, using SPSS ver. 22.
Results: The average age of the 121 patients participating in this study was 53.31 ± 14.09. A direct and statistically significant correlation was observed between body temperature on the first day and interleukin 1 level. A statistically significant negative correlation was observed between blood oxygen saturation level and interleukin-1 and -6 on the first, third and fifth days. Shortness of breath and coughing had a statistically significant correlation with the level of interleukin 1 on the third and fifth days. A direct and statistically significant correlation was observed between body temperature on the first, third and fifth days and interleukin 6 level. Coughing on the third and fifth days had a statistically significant relationship with interleukin 6 level. No direct and non-significant statistical correlation was found between depression and stress and the serum level of interleukin 1, but a significant correlation was observed between anxiety and serum level of interleukin 1. Finally, the results showed that depression, anxiety and stress had a direct and statistically significant correlation with the serum level of interleukin 6.
Conclusion: Given the relationship between interleukin-1 and -6 and most physical and psychological problems, level of the inflammatory biomarkers interleukin-1 and -6 can be used to estimate the severity of physical and psychological symptoms in COVID-19 patients.
SARS-CoV-2 (2019-nCoV) coronavirus is the seventh pathogenic virus in humans that can cause severe human disease along with severe acute respiratory syndrome (SARS) (1, 2). Disturbance in the body’s immune system caused by corona virus infection can lead to psychological pathology and psychiatric consequences after the outbreak of acute respiratory syndrome (3). Patients with COVID-19 are really vulnerable to stressful situations, and they have low psychological tolerance. According to the current state of the disease in the world, these individuals are highly prone to psychological disorders such as emotional changes, depression, anxiety, frustration, fear, high level of mental stress, negative thoughts, and insomnia (4, 5). Corona viruses can cause mental complications through direct viral infection of the central nervous system (CNS) or indirectly through the immune response (6). Other factors threatening the mental health of people in the community include fear of illness or death, spread of false news and rumors, disruption in daily activities, prohibition or restrictions on travel, reduced social relations, and job and financial problems, to name only a few (7). One of the most important psychological disorders that can harm the mental health of patients with COVID-19 is post-traumatic stress disorder (PTSD), which may lead to permanent consequences such as an influx of disturbing memories, avoidance behaviors, irritability, and emotional numbness (8). Other important psychological disorders that can negatively affect the mental health of patients with COVID-19 are stress, anxiety and depression. The result of a meta-analysis in patients with COVID-19 showed that the pooled prevalence of depression was 45% (95% CI: 37%–54%, I2 = 96%), the pooled prevalence of anxiety was 47% (95% CI: 37%–57%, I2 = 97%), and the pooled prevalence of sleeping disturbances was 34% (95% CI: 19%–50%, I2 = 98%) (9). The prevalence of depressive and anxiety symptoms, insufficient sleep, unsatisfactory sleep, and unsatisfactory quality of life was significantly increased. Importantly, a significant relation with all mental health outcomes considered was found for women vs. males, for current vs. never smokers, and with increasing physical activity. In addition, the use of at least one psychotropic drug increased compared to pre-lockdown (10–12). Patients infected with COVID-19 show high levels of the following cytokines: IL-1, IL-6, IFN, CXCL10, and CCL2 (13). Activation of immune cells residing in the lung through diagnostic receptors triggers the release of inflammatory cytokines and the release of blood neutrophils and monocytes into the bronchi, which will cause damage to the lung tissue and subsequently destruction of alveolar ventilation (14). Increased levels of interleukin-6 have been proven in cases of inflammatory diseases. COVID-19 is pathophysiologically characterized with severe inflammation and chemokine storm, which is associated with increased levels of interleukin-1 and 6 (15, 16). IL-6 exerts various effects other than those on hepatocytes and lymphocytes and these are frequently detected in chronic inflammatory diseases (17). The results of Zhu’s et al. (18) study showed that high levels of interleukin-6, C-reactive proteins, and high blood pressure were independent risk factors for the severity of COVID-19. Some studies have reported the relationship of mental and psychological disorders with high levels of interleukin-1 and -6 (19–21). Interleukin 6 plays a role in the development and physiological or somatic consequences of major depression, and the levels of two types of cytokines, namely interleukin 6 and tumor necrosis factor α (TNFα), are significantly higher in patients with major depression. In general, cytokine dysfunction could be associated with depression (22). Despite the prevalence of COVID-19 in the world and Iran and the numerous studies conducted so far, little is still known about this disease. In addition to physical symptoms in COVID-19 patients, psychological symptoms among hospitalized patients are of particular importance to nurses since they play a key role in the recovery process and improving the physical and mental state of these patients (23). Currently, available evidence overall argues the COVID-19 in the severe state exhibits a cytokine storm with elevated plasma levels IL-1, and IL-6. However, crucial questions remain unanswered pertaining to the physical and psychological problems with the levels of interleukin-1 and -6 in COVID-19 patients. To address these questions, we aimed to examine the association of physical and psychological problems with the levels of interleukin-1 and -6 in patients infected with COVID-19.
This was a cross-sectional descriptive-analytical research conducted on 121 COVID-19 patients hospitalized in Amir al-Momenin Hospital and university hospitals affiliated to Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
The participants of the present study were selected using convenient sampling from among COVID-19 patients hospitalized in the general wards of Amir al-Momenin Hospital and university hospitals affiliated to Ahvaz Jundishapur University of Medical Sciences.
The sample size was calculated using PASS version 15 based on the Multiple Regression using Effect Size procedure. Assuming age and gender as control variables, interleukin level as the test variable, type 1 error of 0.05, power of 80%, and an effect size of 0.08, the final sample size was calculated to be 121.
Patients were eligible to enter the study if they: were diagnosed with COVID-19 and in the severe stage of the disease (positive PCR test), aged between 18–65 years, were hospitalized in either Amir al-Momenin Hospital or university hospitals affiliated to Ahvaz Jundishapur University of Medical Sciences, and gave informed written consent to participate in the study. Exclusion criteria were: inadequate completion of the questionnaires or unwillingness to continue participation.
The data collection tools used in this study were the depression, anxiety and stress scale (DASS-21) and a demographic questionnaire inquiring information about age, sex, history of neurological and psychiatric diseases, history of taking neuropsychiatric drugs, history of suicide attempts, marital status, employment status, and level of education. Also, a checklist was used to record the values of interleukin-1 and -6 in the patients’ tests. Physical problems (i.e., abnormal body temperature and blood oxygen saturation levels, shortness of breath, coughing, weakness, and lethargy) were also recorded in a separate checklist. Body temperature was measured using a non-contact thermometer (Beurer Company, Germany) and oxygen saturation level was measured using a pulse oximeter (Beurer Company, Germany). Shortness of breath, coughing, weakness, and lethargy were assessed based on examination, observation, and patient report.
Persian version of depression, anxiety, and stress scale is a set of three self-measurement subscales to assess negative affective states of depression, anxiety and stress. Each of the three subscales of DASS-21 contains 7 items (depression; items 3, 5, 10, 13, 16, 17, and 21; anxiety; items 2, 4, 7, 9, 15, 19, and 20; stress; items 1, 6, 8, 11, 12, 14, and 18). The depression scale assesses dysphoria, hopelessness, devaluation of life, self-deprecation, lack of interest/involvement, anhedonia and inertia. The anxiety scale assesses autonomic arousal, skeletal muscle effects, situational anxiety, and subjective experience of anxious affect. The stress scale is sensitive to levels of chronic nonspecific arousal. It assesses difficulty relaxing, nervous arousal, and being easily upset/agitated, irritable/over-reactive and impatient. Scores for depression, anxiety and stress are calculated by summing the scores for the relevant items. Participants were asked to rate each item’s applicability based on their past week experience on a four-point scale ranged from 0 (“does not apply to me at all”) to 3 (“applies to me most of the time”). In each scale, total scores were calculated by summing the scores into seven items and then multiplied by two. Total scores ranged between 0 and 42 (24). Also, the test does not have reverse scores. The original study reported the high reliability of DASS-21, Cronbach’s alpha coefficients for depression, anxiety, and stress were reported as 0.91, 0.84, and 0.90, respectively (25). Numerous studies have evaluated the psychometric properties of this scale in medical and non-medical populations to determine its validity and reliability (26, 27). In Iran, Kakemam et al. (28) prepared the Persian version of DASS and validated it. The internal reliability of DASS scales was calculated using Cronbach’s alpha and the following results were obtained: 0.93 for the depression scale, 0.79 for the anxiety scale, and 0.91 for the stress scale.
On the first day of hospitalization, questionnaires and checklists were completed in full compliance with health precautionary measures during the COVID-19 pandemic. Physical problems were also recorded using the above-mentioned tools. Afterwards, using venous blood sampling, the clot test was taken by staff nurses, and in compliance with the health regulations and standards for maintaining the test tubes, the blood samples were sent to Imam Khomeini Hospital to perform ELISA test and measure the level of interleukin-1 and -6. Finally, the measured values of these two factors were recorded in the checklist of each patient. In the following days until the end of the hospitalization period, physical and mental problems were measured every other day and the patient’s final condition was also recorded. The human IL-6 ELISA kit (Carmania Pars Gene Company, Iran), manufactured according to the standards of Mitrogen and R&D companies, uses an immunoassay method based on sandwich ELISA protocols. In this method, both a special monoclonal antibody against IL-6 and the biotin-streptavidin system are used. This gives the kit very high sensitivity and specificity in measuring interleukin 6. The detection range of this kit is 6.25–200 pg/mL. The main advantages of this method include a sensitivity or detection limit of around 5 pg/mL as well as high specificity and accuracy. This kit can detect natural and human recombinant IL-6. The results were reported in pg/mL (29). The level of IL-β1 was measured in picograms per milliliter based on ELISA method using the quantitative detection kit (Carmania Pars Gene, Iran) manufactured according to the standard of Mitrogen and R&D companies.
This study was approved by the Ethics Committee of Ahvaz Jundishapur University of Medical Sciences (Ref. ID: IR.AJUMS.REC.1400.050). The study was conducted according to the Declaration of Helsinki. Written informed consent was obtained from the patients who were already told that they have the right to withdraw from the research at any stage. The participants and their families had the right to ask any questions to resolve any ambiguity. They were also assured that no cost was imposed on them, that their information would remain confidential, and that the results would be published only for research purposes.
Chi-square test (or Fisher’s exact test) was used to examine the relationship between qualitative variables, and independent t-test and repeated measure analysis was used to compare quantitative variables between two independent groups. Correlation coefficient and multivariate regression models were used to determine the relationship between interleukin level and psychological problems. The significance level of the above tests was set at 0.05. Data analysis was done using SPSS version 22. The normality of the distribution of the variables was checked using the Kolmogorov–Smirnov test.
This research was conducted on 121 patients with an average age of 53.31 ± 14.09, of whom, 51.4% were women and the majority (52.1%) were unemployed. Other demographic characteristics are listed in Table 1.
Results of independent t-test and chi-square showed that there was no statistically significant difference between male and female patients in terms of marital status, educational attainment, history of neuropsychiatric disease, history of taking neuropsychiatric drugs, and history of suicide attempts (p > 0.05). A statistically significant difference was observed between the two groups only in terms of occupation (p < 0.0001). Also, regarding interleukin-1 and -6 variables, no statistically significant difference was observed between the two sexes (p > 0.05) (Table 2).
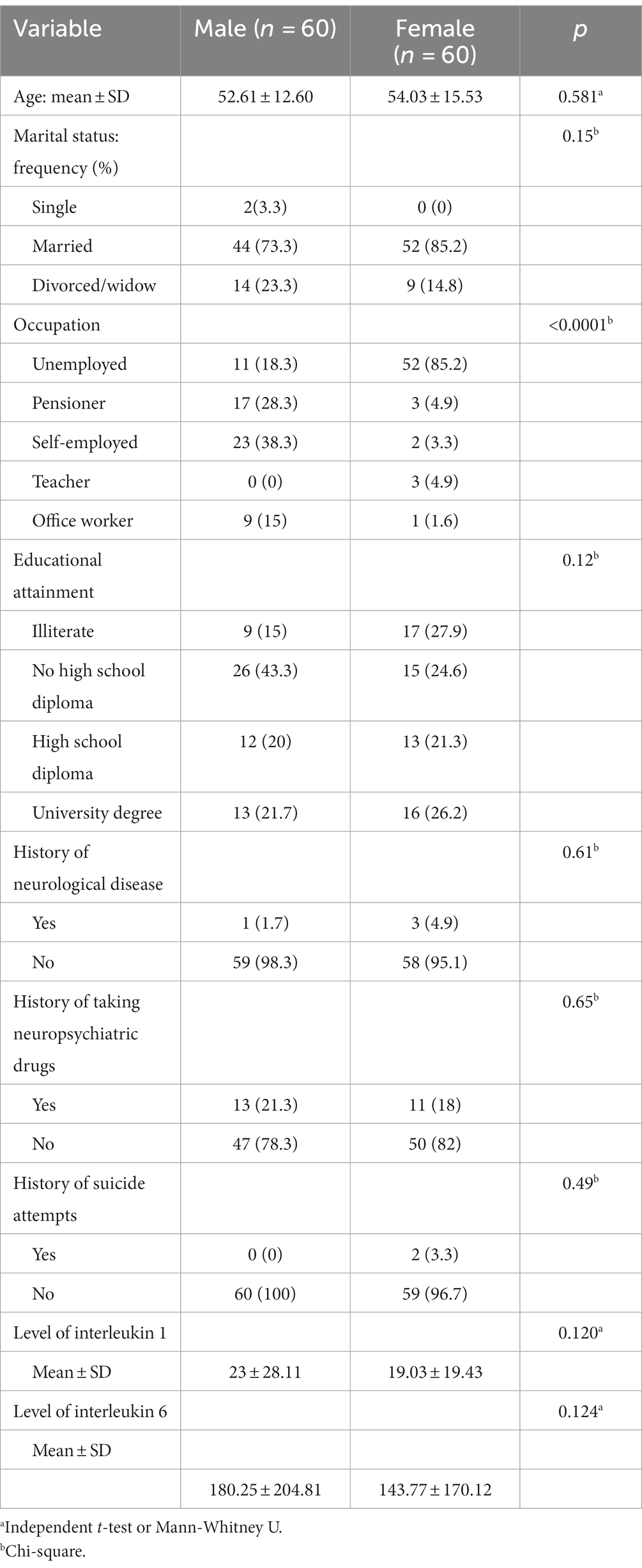
Table 2. Demographic characteristics of the COVID-19 patients included in the study according to their gender.
The results showed that the mean and standard deviation of the patients’ temperature on the first, third, and fifth days was 37.94 ± 0.88, 37.57 ± 0.66, and 37.28 ± 0.48, respectively which showed a significant difference between the days based on Friedman test (p < 0.0001). The mean and standard deviation of the percentage of oxygen saturation in patients on the first, third, and fifth days was 92.36 ± 2.73, 92.76 ± 3.40, and 93.08 ± 3.77, respectively which showed a significant difference between the days based on Friedman test (p < 0.0001). According to the results of Cochran’s Q test, the rate of shortness of breath on the first, third, and fifth days was 90.1%, 54.5%, and 32.2%, respectively which showed a downward trend and a statistically significant difference between the 3 days (p < 0.0001). The rate of coughing on the first, third, and fifth days was 76.9%, 67.8%, and 50.4%, respectively which showed a downward trend and a statistically significant difference between the 3 days (p < 0.0001). As far as weakness and lethargy were concerned, their rate was 97.5%, 97.5%, and 96.7% on the first, third, and fifth days, respectively which showed a downward trend but no statistically significant difference (p = 0.368) (Table 3).
The results showed that the mean and standard deviation of interleukin 1 level in the studied patients was 21.007 ± 12.24. Pearson’s correlation test showed that there was a direct and statistically significant correlation between body temperature on the first day and interleukin 1 level (r = 0.186, p = 0.041). However, no such correlation was observed between body temperature on the third (r = 0.130, p = 155, p = 0.0) and fifth days (r = 0.070, p = 0.447) and interleukin 1 level. A negative and statistically significant correlation was observed between blood oxygen saturation level and level of interleukin-1 on the first (r = −0.214, p = 0.018), third (r = −0.285, p = 0.002) and fifth days (r = −0.236, p = 0.009). According to the results of the statistical test, shortness of breath and coughing on the third and fifth days were significantly correlated with the level of interleukin 1 (p < 0.05) (Table 4).
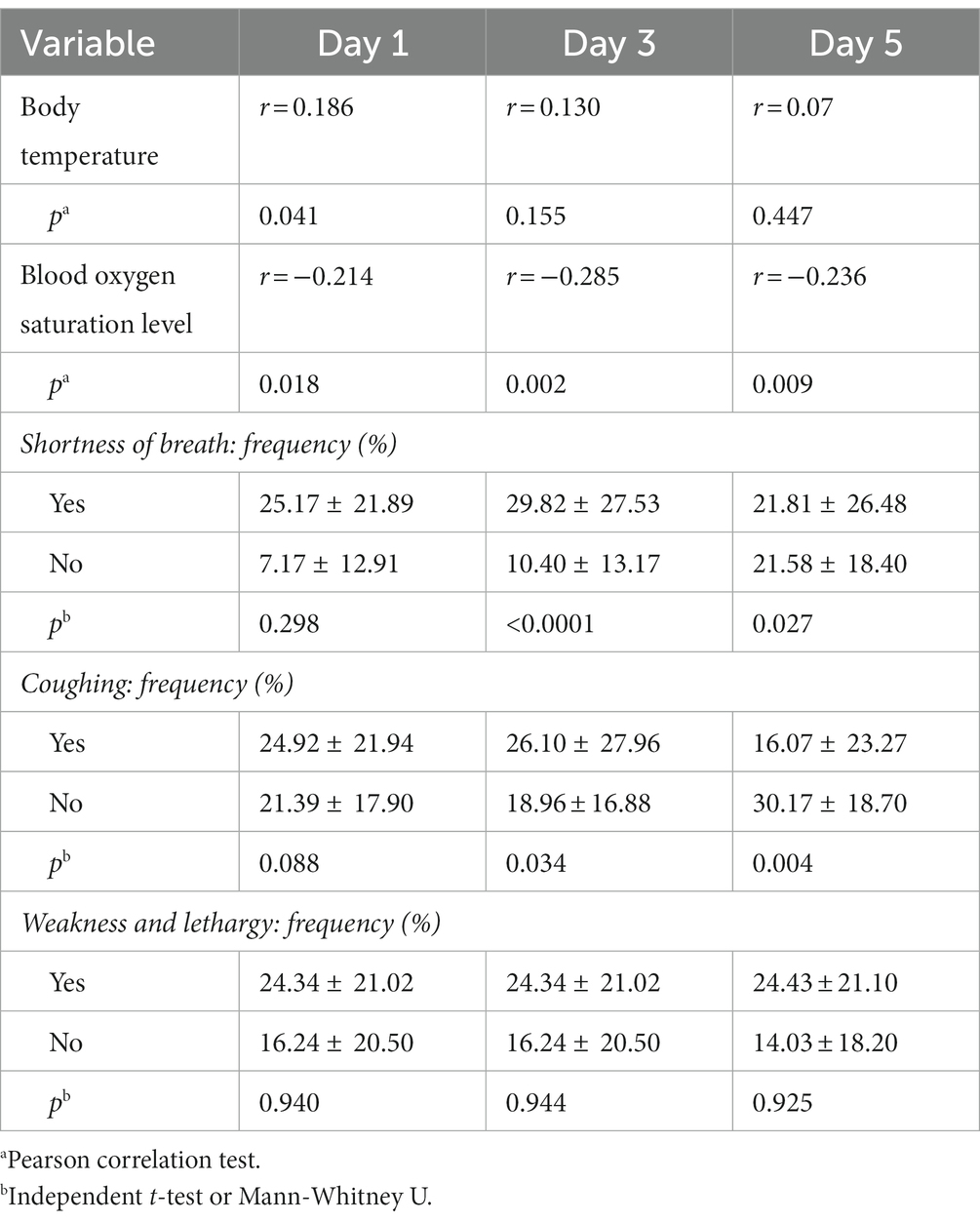
Table 4. The relationship between physical problems (body temperature, blood oxygen saturation level, shortness of breath, coughing, weakness, and lethargy) and interleukin 1 level in patients with COVID-19.
According to the results of the Pearson correlation coefficient test, a direct and statistically significant correlation was observed between body temperature on the first (r = 0.339, p < 0.0001), third (r = 0.336, p < 0.0001) and fifth days (r = 0.244, p < 0.007, p = 0) and interleukin 6 level. Also, a negative and statistically significant correlation was observed between the percentage of blood oxygen saturation level on the first (r = −0.472, p < 0.0001), third (r = −0.598, p < 0.0001) and fifth days (r = −0.511, p < 0.0001) and interleukin 6 level. Coughing on the third and fifth days had a statistically significant relationship with the level of interleukin 6 (p < 0.05). According to the results of the statistical test, coughing on the third and fifth days had a statistically significant correlation with the level of interleukin 6 (p < 0.05) (Table 5).
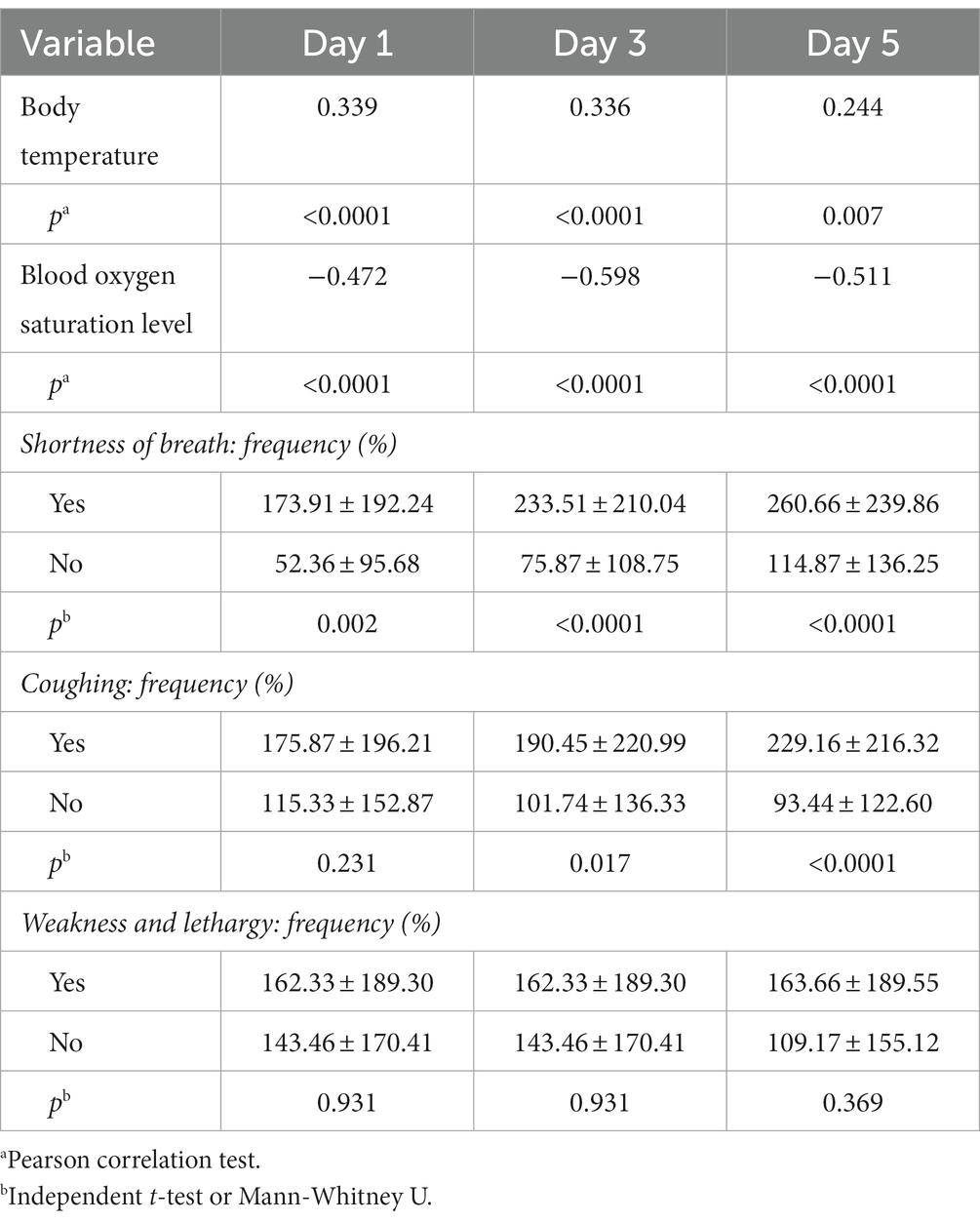
Table 5. The correlation between physical problems (body temperature, blood oxygen saturation level, shortness of breath, coughing, weakness, and lethargy) and interleukin-6 level in COVID-19 patients.
The results of the generalized estimating equations showed that with the increase in interleukin-1 (after adjusting for age and gender), the percentage of oxygen saturation decreases significantly (p = 0.014). Also, with the increase in interleukin-1 (after adjusting for age and gender), body temperature, shortness of breath, coughing, and weakness increase non-significantly (p < 0.05). The results of the generalized estimating equations showed that with the increase in interleukin 6 (after adjustment of age and gender), the percentage of oxygen saturation decreases significantly (p < 0.0001). The results also showed that with the increase in interleukin 6 (after adjusting for age and gender), temperature (p < 0.0001), shortness of breath (p < 0.0001) and coughing increase significantly (p = 0.023). Also, with the increase in interleukin-1 (with adjustment of age and gender), the rate of weakness and lethargy increases non-significantly (p = 0.971) (Table 6).
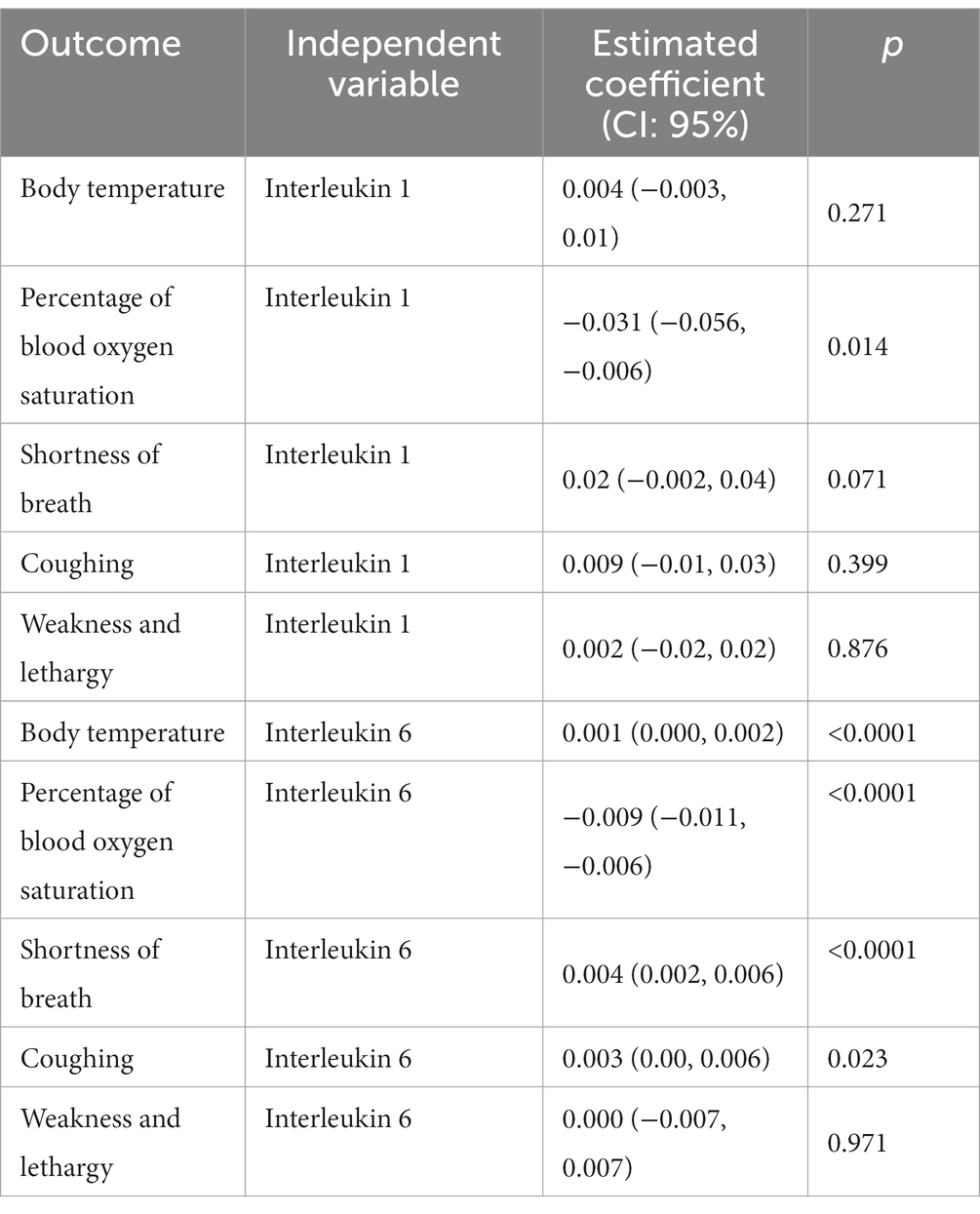
Table 6. Investigating the relationship between the severity of physical problems (i.e., body temperature, blood oxygen saturation percentage, shortness of breath, coughing, and weakness and lethargy) and the serum level of interleukin 1 and 6 in patients with COVID-19.
The results of the generalized estimation equations showed that with the increase in interleukin-1 (after adjusting for age and gender), psychological problems (depression, anxiety, and stress) increase. Meanwhile, the increase in anxiety is statistically significant (p = 0.043). The results showed that with the increase in interleukin-6 (after adjusting for age and gender), psychological problems (depression, anxiety, and stress) increase significantly (p < 0.05) (Table 7).
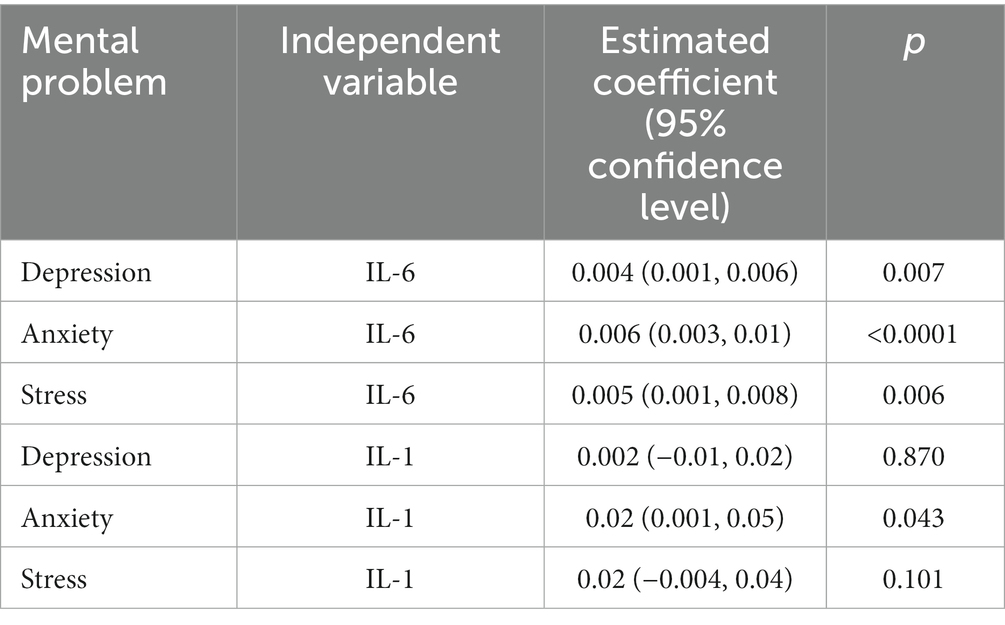
Table 7. The relationship between the severity of psychological problems (depression, anxiety and stress) and the serum level of interleukin 6 in patients with COVID-19.
The results of the present study showed that there was a direct and statistically significant correlation between body temperature on the first day and interleukin 1 level. A negative and statistically significant correlation was also observed between blood oxygen saturation level and interleukin-1 level on the first, third and fifth days. Shortness of breath and coughing on the third and fifth days had a statistically significant correlation with the level of interleukin 1.
Previous studies have shown that release of inflammatory cytokines and the release of blood neutrophils and monocytes into the bronchi will cause damage to the lung tissue and subsequently lead to destruction of alveolar ventilation (14). Based on these results and those of the present study, it can be argued that an increase in interleukin level is associated with reduced levels of blood oxygen saturation. Also, this alveolar destruction is followed by shortness of breath and coughing, which is in line with the results of the present study. As far as body temperature is concerned, it can be said that an increase in inflammatory mediators can lead to a further increase in the activity of the immune system.
The results of the current study also showed a direct and statistically significant correlation between body temperature on the first, third and fifth days and interleukin 6 level. A negative and statistically significant correlation was observed between blood oxygen saturation level on the first, third, and fifth days and interleukin 6 level. Coughing on the third and fifth days had a statistically significant relationship with the level of interleukin 6.
In a study aimed at determining the level of interleukin 6 in patients with COVID-19, Coomes et al. (30) found that the level of interleukin 6 in patients with COVID-19 significantly increased and was associated with adverse clinical outcomes, and that inhibition of interleukin 6 is a possible therapeutic target for managing dysregulated responses in patients with COVID-19. In COVID-19, interleukin-6 level is elevated (15, 16), and due to its mediating role in the lung and destruction of pulmonary alveoli (14), side effects such as drop in blood oxygen saturation level and coughing are expected, which is consistent with the results of the present study.
Our findings also showed no direct and non-significant statistical correlation between depression and stress and the serum level of interleukin 1. However, a significant correlation was observed between anxiety and the serum level of interleukin 1. Mazza et al. (6) studied anxiety and depression in COVID-19 survivors and the role of inflammatory and clinical predictors in this disease. They reported that the levels of peripheral lymphocytes, neutrophils, and platelets are associated with depression and anxiety scores in the follow-up stage. Although their study was on other factors related to inflammation, it seems that mental problems including anxiety can affect the production of inflammatory mediators by affecting the immune system. Additional studies on other viral diseases are recommended to provide more solid evidence for such conclusions.
According to the results of the present study, depression, anxiety and stress had a direct and statistically significant correlation with the serum level of interleukin 6. In a review study, Sepehrinezhad et al. (22) reported that chronic stress by inducing the production of pro-inflammatory cytokines such as interleukin-6 can lead to an increase in various chronic diseases, which confirms the results of the present study. O’Donovan’s et al. (31) study showed significantly higher levels of interleukin-6 in participants with clinical anxiety compared to non-anxious participants. Although their study population is different from that of the present study, both studies came up with similar results. Also, another study showed that the level of interleukin 6 in women having positive social relationships and a purpose for life is lower compared with other women (19), suggesting that people experiencing anxiety, depression and anxiety have a higher level of interleukins in their bodies. This has important implications for nurses and health officials, because nurses, as the main caregivers of patients, especially during the COVID-19 pandemic, play an important role in reducing mental stress caused by this pandemic. In fact, nurses’ care measures to reduce these symptoms can play an effective role in reducing inflammatory mediators. Of course, additional studies in this regard can help to provide clinical evidence for this.
A limitation of this study is the self-reporting of symptoms that might bias the analysis, since participants with ongoing symptoms and higher subjective symptom load may be select. Second, we used IL-6 and IL-1 level as a biomarker of inflammatory cytokines. Future studies should consider other inflammatory cytokines such as C-reactive protein, L-7, IL-8, and granulocyte colony stimulating factor and TNF-α. Finally, it was not possible to examine and eliminate other confounding factors related to mental problems in these patients.
Given the relationship between levels of interleukin-1 and -6 and most physical and mental problems, it seems that the level of these inflammatory biomarkers can be used to estimate the severity of physical and psychological symptoms in COVID-19 patients. Furthermore, researchers should develop a scoring system including IL-1 and IL-6 to assist clinicians in early recognition of patients at risk for developing severe disease.
The datasets presented in this article are not readily available because these data were used under license for the current study, and so are not publicly available. Data are, however available from the authors upon reasonable request. Requests to access the datasets should be directed to SM, c2hhaHJhbWJhcmF6QGFqdW1zLmFjLmly.
The studies involving humans were approved by Ahvaz Jundishapur University of Medical Sciences. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
GB-B, SM, MR, FA, EM, BD, ZU, and GA-A: investigation, wrote the manuscript, and writing—review and editing. GB-B, SM, MR, FA, EM, and BD: conceptualization methodology and writing—review and editing. GB-B, SM, BD, EM, MR, and ZU: writing—review and editing. All authors contributed to the article and approved the submitted version.
This study was drawn from a research project (U-00046) sponsored by Deputy of Research and Technology of AJUMS. The payment was spent on the design and implementation of the study.
We are grateful to the Deputy for Research and Technology, Ahvaz Jundishapur University of Medical Science, for cooperating in this research. We thank all the participants in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Ulhaq, ZS, and Soraya, GV. Interleukin-6 as a potential biomarker of COVID-19 progression. Med Mal Infect. (2020) 50:382–3. doi: 10.1016/j.medmal.2020.04.002
2. Zurlo, MC, Cattaneo Della Volta, MF, and Vallone, F. COVID-19 student stress questionnaire: development and validation of a questionnaire to evaluate students’ stressors related to the coronavirus pandemic lockdown. Front Psychol. (2020) 11:576758. doi: 10.3389/fpsyg.2020.576758
3. Xiang, YT, Yang, Y, Li, W, Zhang, L, Zhang, Q, Cheung, T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. (2020) 7:228–9. doi: 10.1016/S2215-0366(20)30046-8
4. Li, Y, Qin, Q, Sun, Q, Sanford, LD, Vgontzas, AN, and Tang, X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J Clin Sleep Med. (2020) 16:1417–8. doi: 10.5664/jcsm.8524
5. Yao, H, Chen, JH, and Xu, YF. Patients with mental health disorders in the COVID-19 epidemic. Lancet Psychiatry. (2020) 7:e21. doi: 10.1016/S2215-0366(20)30090-0
6. Mazza, MG, De Lorenzo, R, Conte, C, Poletti, S, Vai, B, Bollettini, I, et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav Immun. (2020) 89:594–600. doi: 10.1016/j.bbi.2020.07.037
7. Freckelton Qc, I. COVID-19: fear, quackery, false representations and the law. Int J Law Psychiatry. (2020) 72:101611. doi: 10.1016/j.ijlp.2020.101611
8. Bo, H-X, Li, W, Yang, Y, Wang, Y, Zhang, Q, Cheung, T, et al. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. (2021) 51:1052–3. doi: 10.1017/S0033291720000999
9. Deng, J, Zhou, F, Hou, W, Silver, Z, Wong, CY, Chang, O, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. (2021) 1486:90–111. doi: 10.1111/nyas.14506
10. Ambrosetti, J, Macheret, L, Folliet, A, Wullschleger, A, Amerio, A, Aguglia, A, et al. Impact of the COVID-19 pandemic on psychiatric admissions to a large Swiss emergency department: an observational study. Int J Environ Res Public Health. (2021) 18:1174. doi: 10.3390/ijerph18031174
11. Amerio, A, Lugo, A, Stival, C, Fanucchi, T, Gorini, G, Pacifici, R, et al. COVID-19 lockdown impact on mental health in a large representative sample of Italian adults. J Affect Disord. (2021) 292:398–404. doi: 10.1016/j.jad.2021.05.117
12. Nobari, H, Fashi, M, Eskandari, A, Villafaina, S, Murillo-Garcia, Á, and Pérez-Gómez, J. Effect of COVID-19 on health-related quality of life in adolescents and children: a systematic review. Int J Environ Res Public Health. (2021) 18:18. doi: 10.3390/ijerph18094563
13. Coperchini, F, Chiovato, L, and Rotondi, M. Interleukin-6, CXCL10 and infiltrating macrophages in COVID-19-related cytokine storm: not one for all but all for one! Front Immunol. (2021) 12:668507. doi: 10.3389/fimmu.2021.668507
14. Risitano, AM, Mastellos, DC, Huber-Lang, M, Yancopoulou, D, Garlanda, C, Ciceri, F, et al. Complement as a target in COVID-19? Nat Rev Immunol. (2020) 20:343–4. doi: 10.1038/s41577-020-0320-7
15. Qin, C, Zhou, L, Hu, Z, Zhang, S, Yang, S, Tao, Y, et al. Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in Wuhan, China. Clin Infect Dis. (2020) 71:762–8. doi: 10.1093/cid/ciaa248
16. Liu, Z, Long, W, Tu, M, Chen, S, Huang, Y, Wang, S, et al. Lymphocyte subset (CD4+, CD8+) counts reflect the severity of infection and predict the clinical outcomes in patients with COVID-19. J Infect. (2020) 81:318–56. doi: 10.1016/j.jinf.2020.03.054
17. Tanaka, T, Narazaki, M, and Kishimoto, T. IL-6 in inflammation, immunity, and disease. Cold Spring Harb Perspect Biol. (2014) 6:a016295. doi: 10.1101/cshperspect.a016295
18. Zhu, Z, Cai, T, Fan, L, Lou, K, Hua, X, Huang, Z, et al. Clinical value of immune-inflammatory parameters to assess the severity of coronavirus disease 2019. Int J Infect Dis. (2020) 95:332–9. doi: 10.1016/j.ijid.2020.04.041
19. Friedman, EM, Hayney, M, Love, GD, Singer, BH, and Ryff, CD. Plasma interleukin-6 and soluble IL-6 receptors are associated with psychological well-being in aging women. Health Psychol. (2007) 26:305. doi: 10.1037/0278-6133.26.3.305
20. Osimo, EF, Pillinger, T, Rodriguez, IM, Khandaker, GM, Pariante, CM, and Howes, OD. Inflammatory markers in depression: a meta-analysis of mean differences and variability in 5,166 patients and 5,083 controls. Brain Behav Immun. (2020) 87:901–9. doi: 10.1016/j.bbi.2020.02.010
21. Solmi, M, Suresh Sharma, M, Osimo, EF, Fornaro, M, Bortolato, B, Croatto, G, et al. Peripheral levels of C-reactive protein, tumor necrosis factor-α, interleukin-6, and interleukin-1β across the mood spectrum in bipolar disorder: a meta-analysis of mean differences and variability. Brain Behav Immun. (2021) 97:193–203. doi: 10.1016/j.bbi.2021.07.014
22. Sepehrinezhad, A, Momeni, J, Gorji, A, and Sahab, NS. Stress-induced immune dysfunction: implications for intrapersonal and interpersonal processes. Neurosci J Shefaye Khatam. (2020) 8:93–106. doi: 10.29252/shefa.8.2.93
23. Yıldırım, N, Dayılar Candan, H, and İnan, AH. Psychological distress in patients with COVID-19 during hospitalization. Clin Nurs Res.. (2022) 31:376–384. doi: 10.1177/10547738211040322
24. Lovibond, SH, and Lovibond, PF. Manual for the depression anxiety & stress scales. 2nd ed. Sydney: Psychology Foundation (1995).
25. Lovibond, PF, and Lovibond, SH. The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behav Res Ther. (1995) 33:335–43. doi: 10.1016/0005-7967(94)00075-U
26. Ali, AM, Ahmed, A, Sharaf, A, Kawakami, N, Abdeldayem, SM, and Green, J. The Arabic version of the depression anxiety stress scale-21: cumulative scaling and discriminant-validation testing. Asian J Psychiatr. (2017) 30:56–8. doi: 10.1016/j.ajp.2017.07.018
27. Jiang, LC, Yan, YJ, Jin, ZS, Hu, ML, Wang, L, Song, Y, et al. The depression anxiety stress scale-21 in Chinese hospital workers: reliability, latent structure, and measurement invariance across genders. Front Psychol. (2020) 11:247. doi: 10.3389/fpsyg.2020.00247
28. Kakemam, E, Navvabi, E, Albelbeisi, AH, Saeedikia, F, Rouhi, A, and Majidi, S. Psychometric properties of the Persian version of depression anxiety stress scale-21 items (DASS-21) in a sample of health professionals: a cross-sectional study. BMC Health Serv Res. (2022) 22:111. doi: 10.1186/s12913-022-07514-4
29. Sharif, N, and Agha, YA. Analysis of the relation between coping ways with stress and IL-6 immunologic biomarker in coronary heart disease when faced with a stressful event. J Sabzevar Univ Med Sci. (2016) 22:1088–98.
30. Coomes, EA, and Haghbayan, H. Interleukin-6 in COVID-19: a systematic review and meta-analysis. Rev Med Virol. (2020) 30:1–9. doi: 10.1002/rmv.2141
Keywords: interleukin 1, interleukin 6, inflammatory mediator, COVID-19, depression, anxiety, stress, physiological indicators
Citation: Bahadori-Birgani G, Molavynejad S, Rashidi M, Amiri F, Maraghi E, Dashtbozorgi B, Ulhaq ZS and Alizadeh-Attar G (2023) Investigating the association of physical and psychological problems with the levels of interleukin-1 and -6 in COVID-19 patients. Front. Psychiatry. 14:1241190. doi: 10.3389/fpsyt.2023.1241190
Received: 19 June 2023; Accepted: 04 August 2023;
Published: 25 August 2023.
Edited by:
Massimo Tusconi, University of Cagliari, ItalyReviewed by:
Serdar M. Dursun, University of Alberta, CanadaCopyright © 2023 Bahadori-Birgani, Molavynejad, Rashidi, Amiri, Maraghi, Dashtbozorgi, Ulhaq and Alizadeh-Attar. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shahram Molavynejad, c2hhaHJhbWJhcmF6QGFqdW1zLmFjLmly
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.