
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 12 October 2023
Sec. Social Psychiatry and Psychiatric Rehabilitation
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1240703
This article is part of the Research Topic Community Series in Mental Illness, Culture, and Society: Dealing with the COVID-19 Pandemic, volume VIII View all 63 articles
 Maia Adam
Maia Adam James K. Moran
James K. Moran Yann David Kippe
Yann David Kippe Meryam Schouler-Ocak
Meryam Schouler-Ocak Felix Bermpohl
Felix Bermpohl Stefan Gutwinski
Stefan Gutwinski Thomas Goldschmidt*†
Thomas Goldschmidt*†Introduction: While numerous studies have identified an increase in symptoms of depression as well as anxiety and distress due to the COVID-19 pandemic, relatively few studies have investigated the new-onset of psychiatric diseases during the pandemic.
Methods: This study focuses on the number of psychiatric new-onset diagnoses in a psychiatric emergency department (pED) in Berlin, Germany during the second wave of the pandemic (i.e. from 09/15/2020 to 03/01/2021 = COVID-19-period) compared to pre-pandemic times (09/15/2019 to 03/01/2020 = control period). We focused on diagnostic subgroups and performed logistic regression analysis to investigate potential risk groups based on covariables such as age, gender, homelessness, attending in police custody and familial relationship.
Results: Overall, there was a 59.7% increase in new-onset psychiatric diagnoses during the COVID-19-period. Increases in the following diagnoses were observed: new-onset of substance-related and addictive disorders (+192.5%), depressive disorders (+115.8%), schizophrenia spectrum and psychotic disorders (+113.3%) and anxiety disorders (+63.6%). These diagnostic subgroups, together with attending in police custody, were found to predict pED presentations with new-onset during the COVID-19-period. Interestingly, in the group of new-onset psychiatric diseases in the COVID-19-period, higher amounts of job loss and living alone as well as a relative decrease in familial relationships were observed.
Discussion: COVID-19 infections and post-COVID-19 syndrome are unlikely to have played a substantial role in the increase of new-onset diseases in this study. Conclusion: Our findings underline the role of indirect factors in new-onset of psychiatric diseases during the pandemic and should be a caveat for future pandemic control policies.
During the global COVID-19 pandemic, first recognized in December 2019, people were exposed to the acute health risks of COVID-19 infection (1), the potential long-term consequences of infection (2, 3), and a health system on the verge of collapse. Measurements such as travel restrictions, the closure of schools and workplaces, contact limitation, quarantine, isolation and also prevention of access to public places were implemented to mitigate the spread of the COVID-19 virus (4, 5).
The impact of the pandemic on mental health has been studied thoroughly already. Studies based on online questionnaires suggest a deterioration in the general population’s mental health since the beginning of the pandemic (6–9), predominantly regarding symptoms of depression, anxiety, insomnia, and acute stress. Most studies, however, show a substantial decline in psychiatric Emergency Department (pED) presentations (10–13), especially at the beginning of the pandemic. Yet, there are indicators that the presentations were more severe (14–16). Reasons for the decline might include the fear of getting infected with the COVID-19 virus in a pED (17–19), qualms about overloading the health system (20) or the government’s appeal to stay at home (21). An increase in the prevalence of psychiatric diseases might also lead to a deterioration of preexisting somatic diseases, as for example diabetes (22).
A global study from 2019 showed that mental disorders were among the leading cause of disability (16% of disability-adjusted life-years) in the last 20 years (23, 24). It can be assumed that if there was a significant increase in new-onset psychiatric disorders during the COVID-19 pandemic, this may lead to a simultaneous increase in the burden of psychiatric disorders. Therefore, investigating if there was an increase in new-onset psychiatric disorders is of great importance as it has long-lasting implications for patients, the health system and the economy (24, 25). Only a few studies have sought to further examine psychiatric diagnoses within the COVID-19 period in terms of chronic and new-onset diagnoses.
Most studies on new-onset psychiatric disorders during the COVID-19 pandemic focus on post-COVID-19 psychiatric disorders. There is increasing evidence that psychiatric disorders, such as depression (26–28), psychosis (29–32) and anxiety disorders (27, 28) frequently occur following a COVID-19 infection, often also as new-onset diagnoses (31, 33–35). Pathophysiologically, an immune response (cytokine storm) to an initial infection or a direct viral infection of the central nervous system might be the cause (27, 28, 31, 36).
In the current study, however, we are not focusing on the direct sequelae of COVID-19 infections but the indirect effect of the pandemic and its impact on new-onset psychiatric disorders. The indirect effect could result from fear of COVID-19 infection (37, 38), social isolation during lockdown (39, 40), loss of daily routines and financial insecurity (40). Changes within the medical care system such as reduced outpatient psychiatric and psychotherapeutic care, which was seen particularly during the first lockdowns (41–44) might also have led to an increase in new-onset psychiatric disorders.
Studies on new-onset psychiatric disorders through the indirect effect of the pandemic are scarce. An online survey from Italy showed that 16.0% of participants during the first wave and 18.6% of participants during the second wave of COVID-19 met the criteria for at least one new-onset psychiatric disorder, suggesting an increase compared to pre-pandemic times (45). A study of 850 individuals attending a pED during the first wave of the pandemic in Hannover, Germany assessed more treatment-naive patients with neurotic, stress-related, and somatoform disorders, than in the comparison time period 1 year earlier. The authors argue that this may point toward an increase in the new-onset of these disorders (46). A longitudinal comparative study from Israel showed a significant increase of 38.0% of new-onset psychosis or mania in pED presentations during the first wave (March–April 2020) (47). A study from New York found an increase in new-onset psychiatric disorders during the first wave in children and adolescents but not in adults (32).
To assess the indirect effect of the COVID-19 pandemic on new-onset of psychiatric diseases, this study focuses on the number of psychiatric new-onset diagnoses in pED presentations during the second wave of the pandemic compared to pre-pandemic times. We focused on diagnostic subgroups and, based on research from early phases of the pandemic, defined risk groups by age, gender, homelessness (11), attending in police custody (48) and familial relationship (7, 32, 49) that might be especially vulnerable. We investigated all records from patients of one major pED in Berlin, Germany during the second wave of COVID-19 to validate for new-onset diagnoses.
This study was approved by the local ethics committee (Charité Universitätsmedizin, Berlin; number of approval: EA 110/20). We conducted a retrospective chart review comparing all presentations at an academic psychiatric emergency department (pED) in Berlin (St. Hedwig Hospital) during the second wave of the COVID-19 pandemic (9/15/2020–3/1/2021 = “COVID-19-period”) with all pED presentations of the same time period 1 year earlier as a baseline (“control period”).
The psychiatric department of Charité Universitätsmedizin Berlin at St. Hedwig Hospital (SHK) is responsible for providing psychiatric emergency care to the approx. 327,000 citizens of the districts Tiergarten, Wedding and Moabit. It consists of one emergency admission and seven psychiatric care units for inpatient treatment. Patients living in other districts of Berlin are usually redirected to the psychiatric clinic of their district when inpatient treatment is required.
We decided to study the second wave as it has been less studied than the first, while being more than twice as long and providing an opportunity to explore the effects of the implementation of a lockdown. The beginning of the second wave in Berlin (9/15/2020) is defined by a continuously rising 7-day-incident measure, the number of COVID-19 cases in the last 7 days per 100,000 citizens (50). The end (3/1/2021) is marked by the beginning of the relaxation of the COVID-19 policy [e.g., reopening of hairdressers (51)]. On December 16th 2020 a resolution for a “hard lockdown” came into force (52, 53). Private gatherings were limited to a maximum of five adults, the retail and gastronomic sector had to close with some exceptions, schools were closed and drinking alcohol in public spaces was forbidden. Clinical routine chart data documented in ORBIS®, the digital hospital software, from all patients from both time periods was extracted, including the pED cases and the cases with inpatient treatment.
Cases were excluded if they had duplicate clinical records, if the patient left without being seen by medical staff and if they did not have a psychiatric diagnosis according to the International Classification of Diseases version 10, Clinical Modification (ICD-10-GM-2022). Further exclusion criteria were day therapy cases, as admissions to the day therapy unit were restricted as part of the measures to reduce the spread of COVID-19. Scheduled inpatient admissions (not via the pED) were also excluded. This concerns mainly scheduled detoxifications. In the case of repetitive presentations of patients within one time period, we decided to include only the first attendance (S1).
This study refers to the new-onset of the main diagnosis only, as it can be considered to be the most reliably diagnosed across different psychiatrists (54) and to have the biggest impact on the patient. Main diagnoses were defined as new-onset if they were first diagnosed in the current hospital attendance. These may be individuals who had never received a psychiatric diagnosis before or individuals who had a history of another psychiatric diagnosis. We only considered a main diagnosis as new-onset when this diagnosis did not appear in any previous records of the patient, either as a main or a secondary diagnosis. For first-time patients at SHK with no earlier psychiatric records available, patients’ description of events and medical history obtained in the pED were used to determine if the main diagnosis fulfilled the criteria of new-onset or not.
Main diagnoses were grouped into nine subgroups: substance use disorders (without nicotine dependence/harmful use), depressive disorders, schizophrenia and psychotic disorders, anxiety disorders, trauma and stress-related disorders, other neurotic disorders, personality disorders, organic mental disorders and bipolar and manic disorders (S2).
Variables of particular interest were “homelessness” i.e., individuals with no shelter or who are staying in homeless shelters, “familial relationship,” defined as people that are in a relationship or have children; and “attendance in police custody” meaning people referred by the police to the pED.
Descriptive statistical analyses were performed to assess differences between new-onset of diagnoses during the second wave of the COVID-19 pandemic and the control period. Since the metric variable “age” was not normally distributed, the median is reported. Comparison of medians between the time periods was performed using the Mann–Whitney-U-Test. For all other categorical variables, absolute numbers and percentages are reported and compared using the Chi2 test. The value of p for statistical significance was set to p < 0.05 except for the diagnostic subgroups. For these analyses, we applied a Bonferroni correction for multiple testing to control the occurrence of false positives to the significance levels as follows: p = 0.05/9 = 0.0056. The logistic regression model was conducted to explore potential influence factors on new-onset diagnoses.
We assessed for diagnostic subgroups and risk factors found in the literature and based on our hypothesis, limiting ourselves to those that were well documented in our primary data: age, gender, homelessness, attending in police custody, familial relationships and time period. As an outcome variable, we chose new-onset vs. chronic. Results from the regression models are presented as odds ratios (OR) with 95% confidence intervals (95%CI) and are tested for significance using the Wald-Chi2 tests.
Statistical analyses were performed using the SPSS statistical package, version 27.0, IBM Corporation (2020). The cross correlation was created with the tseries package (55) in R 4.1.2. Tables were created using MS Excel 365, Microsoft Corporation (2020).
A total of n = 4,010 records (patients n = 2,624) were documented during the two observed time periods (COVID-19-period: n = 1986; patients n = 1,312, control period: n = 2024; patients n = 1,312). After applying exclusion criteria, a total of n = 2,619 records (patients n = 2,445) were included in our analysis (COVID-period: n = 1,249, control period: n = 1,370; Table 1). 174 patients presented to the pED in both time periods. Eleven patients during the COVID-19-period were tested positive for COVID-19. Four patients reported a previous COVID-19 infection. For a detailed description of the demographic and clinical characteristics of all patients presenting to the pED, see Table 1.
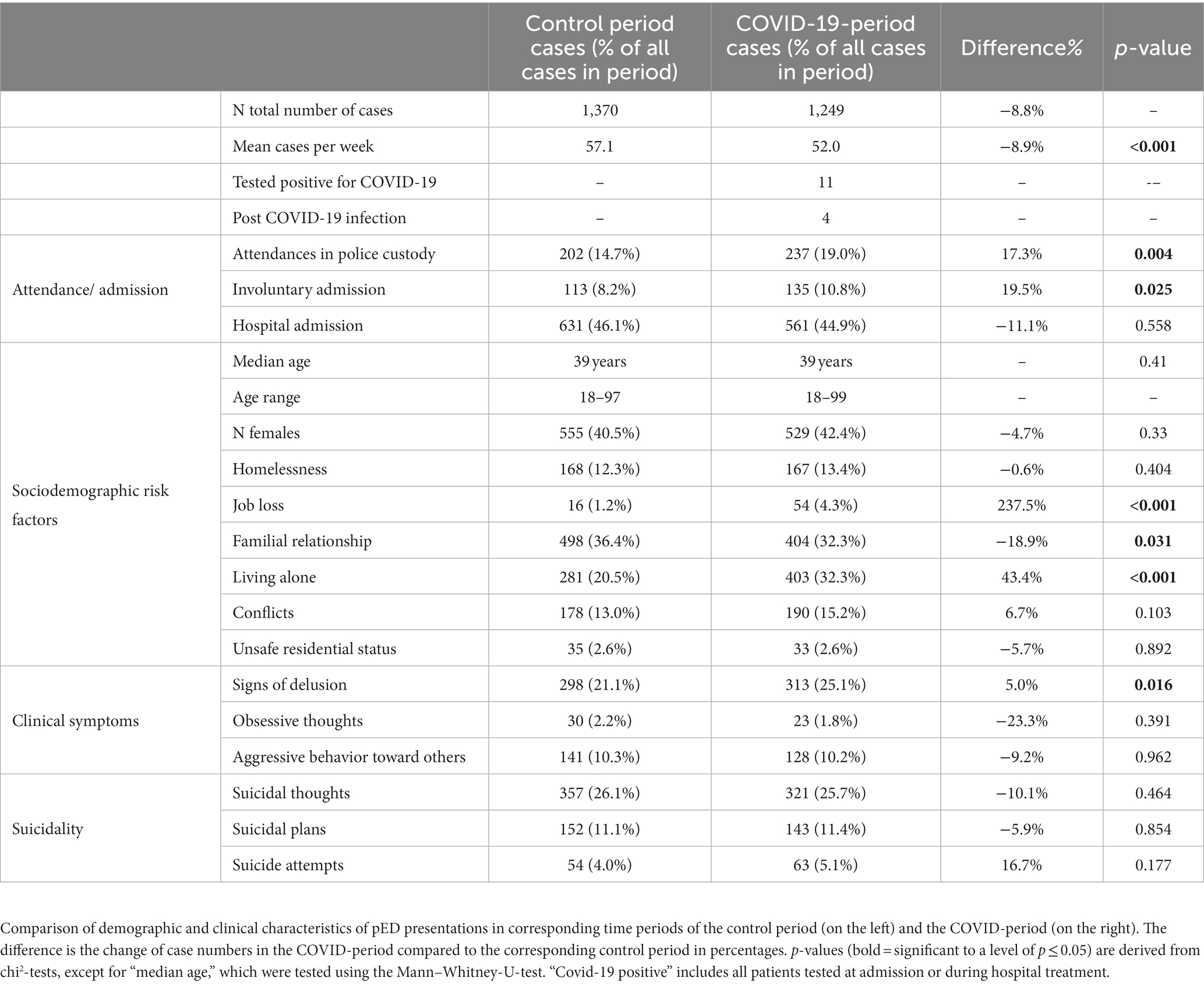
Table 1. Clinical and demographic characteristics of Psychiatric emergency department (pED) presentations.
The weekly number of cases with new-onset diagnoses during both observation periods is presented in Figure 1 along with the timeline of the 7-day incidence of COVID-19 cases in Berlin, Germany. The average weekly number of new-onset diagnoses was 59.3% higher during the COVID-19-period compared to the control period (Table 2). The range of new-onset cases was between 7 and 16 per day in the control period and 10–26 in the COVID-19-period without any significant peaks.
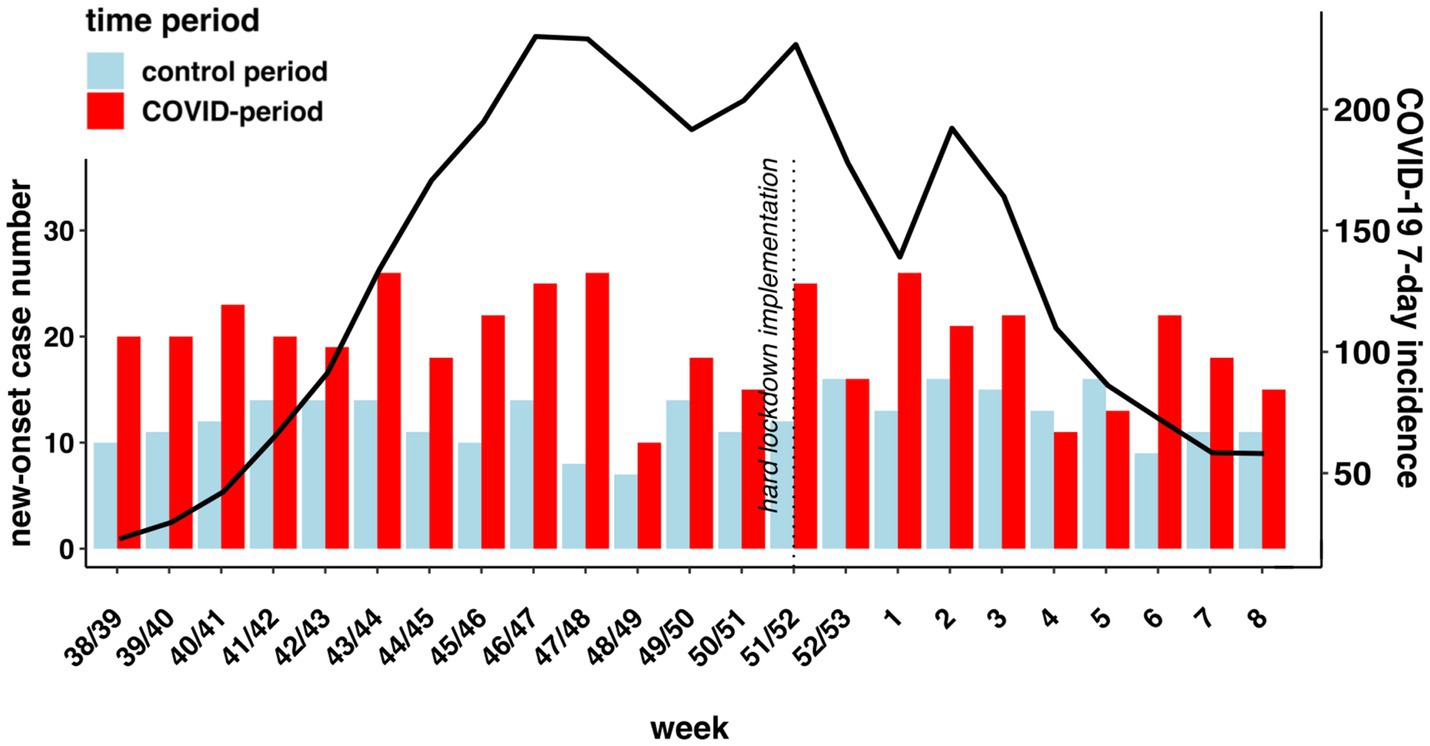
Figure 1. Displays weekly new-onset diagnoses in absolute numbers in the COVID-19-period (red bars) and control period (blue bars) and weekly 7-days incidence in Berlin (red line) in the calendar weeks 38-8 2019/2020 (control period) and 39-8 2020/2021 (COVID-19-period). Weeks 9 in both periods and 38 in the COVID-period are not displayed, as the observation periods did not include complete weeks. The vertical line indicates the enforcement of hard lockdown measures in Germany (12/16/2020). Data on Covid-19 incidence from “Landesamt für Gesundheit und Soziales”: https://www.berlin.de/lageso/gesundheit/infektionskrankheiten/corona/tabelle-indikatoren-gesamtuebersicht/; Abbreviations used: pED = psychiatric emergency department. Raw data on weekly new-onset presentations is shown in Supplementary data (S3).
To test whether the 7-day incidence of COVID-19 cases predicts diagnosis significance at different lagged time points, we implemented a cross-correlation, which measures the degree of correlation between a time series and another time series lagged at different time points. Correlations ranged from (−0.295; 0.249) none of them reached significance (S4). Thus, the lockdown on 16th of December was not accompanied by effects on the number of new-onset diagnoses.
There was a total of 295 (21.5%) cases with a new-onset of the main diagnosis in the control period and 471 (37.7%) of new-onset diagnoses during the COVID-19-period, indicating an increase of 59.7% in new-onset diagnoses during the COVID-19-period. Three patients with new-onset psychiatric diseases tested positive for COVID-19, and four had a positive history of COVID-19 infection (Table 3). The number of new-onset of substance use disorders (20.5% of new-onset cases in the COVID-19-period) was higher by 192.5% (p < 0.001), for depressive disorders (15.7% of new-onset cases in the COVID-19-period) the number was higher by 115.8% (p < 0.001), for schizophrenia spectrum and psychotic disorders (12.3% of new-onset cases in the COVID-19-period) the number was higher by 113.3% (p < 0.001) and for anxiety disorders (7.6% of new-onset cases in the COVID-19-period) the number was higher by 63.6% (p < 0.001) in comparison to the new-onset of these diagnostic subgroups during the control period. For all other diagnostic subgroups, no statistically significant differences in new-onset diagnoses were found.
Patients with new-onset diagnoses during the COVID-19-period compared to the control period were more often attending in police custody (p = 0.004; diff. +147.8%), had in absolute numbers more often, but proportionally less often, a familial relationship (p = 0.039; diff. +33.1%), were more often admitted to the hospital (p = 0.040; diff. +94.1%), more often involuntarily (p = 0.039; diff. +156.5%), had more often experienced job loss (p = 0.046; diff. +283.3%) and were more often living alone (p < 0.001; diff: +201.9%; Table 3).
Patients diagnosed with substance use disorders (p < 0.001; OR 3.28; 95% CI 1.97–5.46), depression (p < 0.001; OR 3.28; 95% CI 1.87–5.74) or anxiety disorders (p = 0.009; OR 2.83; 95% CI 1.30–6.15) had around three times higher risk of having a new-onset during the COVID-19-period (Table 4). Patients with diagnoses of schizophrenia spectrum and psychotic disorders (p = 0.034; OR 1.84; 95% CI 1.05–3.22) were also more susceptible to having a new-onset of their disease.
Individuals who came to the pED in police custody during the COVID-19-period were 1.81 times (p = 0.021; 95% CI: 1.09–3.00) more likely to present with new-onset diagnoses than their counterparts attending the pED without police. Age, gender, being homeless or having a familial relationship was not associated with the risk of having a new-onset diagnosis during the COVID-19-period.
Older age predicted a lower risk of having a new-onset of diagnoses, independently of the time period (p < 0.001; OR 0.98; 9% CI 0.97–0.99). Having a familial relationship (partnership or children) was associated with a higher risk for a new-onset diagnosis (p = 0.003; OR 1.56; 95% CI 1.17–2.09; Table 4). The diagnostic subgroups substance use disorders (p < 0.001; OR 0.18; 95% CI 0.12–0.27), depression (p < 0.001; OR 0.39; 95% CI 0.26–0.60), schizophrenia spectrum and psychotic disorders (p < 0.001; OR 0.19; 95% CI 0.12–0.29) and anxiety disorders (p = 0.048; OR 0.58; 95% CI 0.33–1.00) predicted a significantly lower risk for a new-onset diagnosis.
This study investigated the incidence of new-onset psychiatric diagnoses as well as further contributing factors among patients presenting to a major pED in Berlin during the second wave of the COVID-19 pandemic, based on a retrospective cross-sectional study.
The current study shows an approximately consistent number of cases in both time periods, in contrast to most previous studies showing a decrease in psychiatric presentations in the early COVID-19-periods (10, 11, 13, 56, 57). This is likely due to local differences and the later observation period in comparison in the current study.
A higher number of patients with new-onset diagnoses presented to the pED during the COVID-19-period compared to the control period. During the COVID-19-period, presentations of new-onset substance use disorders, depressive disorders, schizophrenia spectrum and psychotic disorders, and anxiety disorders were more frequent than during the control period. Furthermore, the presence of these diagnostic subgroups and being referred by the police, predicted a pED presentation with new-onset diagnosis during the COVID-19-period in our logistic regression analysis.
The new-onset of substance use disorders increased by 192.5% during the COVID-19-period and substance use disorders were more than three times more likely to be new-onset (p < 0.001; OR 3.28; 95% CI 1.97–5.46). Most studies report an increase of substance use disorders in the general population during the COVID-19-period (58, 59). However, among pED presentations, the number of patients with substance use disorders decreased at the beginning of the pandemic (60, 61). This is also true for our sample: the absolute number of pED presentations with substance use disorders decreased by 5.7% (Table 1) while new-onsets increased.
In a sub-analysis (S5), we see that the most important factor in the increase in new-onset substance use disorders in our sample is the increase in pED presentations with acute alcohol intoxication (33.3% of new-onset substance use disorders during the COVID-19-period). This is in line with the literature, showing increases in alcohol consumption at the beginning of the pandemic (62, 63). Also, differences in alcohol use patterns are reported, with more binge/heavy drinking during a lockdown and an increase in alcohol-related emergencies (64).
Low-threshold services such as group meetings for people dealing with addictions were not taking place regularly anymore (65), which might have driven patients to attend the pED. Possibly, there was a shift from consumption in social situations to consumption at home, due to restrictions (4). Conceivably, this shifted the perception of users regarding their consumption from being legitimized by social activities to being pathological when alone. Loneliness, which is described as a pathogenetic factor during the COVID-19-period (40, 66), might have also triggered more heavy consumption patterns. Finally, supply shortages of drugs, due to travel restrictions, may have driven people to source supplies from unfamiliar providers, increasing the risk of exposure to contaminated substances (67).
Depressive disorders increased by 115.8% during the COVID-19-period, in comparison to the control time. Patients diagnosed with depression had an approximately three times higher risk of having a new-onset of the disorder (p < 0.001). Many studies from the beginning of the pandemic report an increase in depressive symptoms without differing between new-onset and chronic (6, 8, 9, 38, 68–71).
An online study from Italy found an increase in new-onset major depressive disorders in the first and second wave among the general population (72). A longitudinal survey among university students in Japan found that 11.8% had a new-onset of depressive symptoms, supporting our findings (73).
During the pandemic, known risk factors for depression such as social isolation/loneliness (40), job loss (74, 75) and financial insecurity were on the rise. This can also be seen in our sample: job loss and living alone were significantly more prevalent in the COVID-19-period than in the control period (Table 1). These circumstances may have led to an increase in new-onset depressions. In addition, patients with new symptoms of depression, who would normally have consulted psychiatric practices or other outpatient mental health services, instead turned to the pED (42). This mechanism likely applies to the other diagnostic subgroups as well.
Depression has the highest lifetime prevalence among psychiatric diagnoses (76). Possibly, the pandemic precipitated the onset of depression in vulnerable patients.
There was a significant increase in the prevalence of new-onset schizophrenia spectrum and psychotic disorders. Furthermore, this diagnostic subgroup was a predictor for presentations with a new-onset diagnosis during the COVID-19-period (p = 0.034). This finding is in line with prior studies that saw the number of patients with psychotic disorders rising during the pandemic, both directly via neuropsychiatric sequelae after SARS-CoV-2 infection (36, 77, 78) and indirectly (10, 14, 79, 80). In line with this, there were also significantly more cases with signs of delusion in the COVID-19-period than the control period (Table 1).
The already mentioned Israeli study shows that the increase in pED presentations with psychotic disorders and mania correlated highly with lockdown measures and not with national incidence rates (47). Their new-onset cases increased by 45.5% compared to 2019. In our sample, the increase was 113.3%. In their study, the difference in the overall proportion of new-onset diagnoses (psychosis and mania) was 5.5% in 2019 and 8% in 2020 of all diagnoses with psychosis and mania. In the current study, the rate of new-onset psychotic disorders is 10.2% in 2019 and 23.2% in 2020. In another study, also conducted in Israel, a decrease in the incidence rate for schizophrenia was found for the period from March 2020 to February 2021 compared with the years before (81). However, the decrease may rather reflect reduced utilization of medical services by chronic schizophrenic patients and is no clear evidence against a rise in new-onset cases.
While fewer patients with anxiety disorders presented to the pED in general, patients with anxiety disorders showed an increase of 63.6% of new-onset during the COVID-19-period and had a higher risk for a new-onset during the COVID-19-period. These results are in line with other studies showing an increase in symptoms of anxiety in the general population (6, 8, 9) as well as in pED presentations (17, 32). One study showed an increase of 35% in pED presentations with anxiety disorders (17), although no distinction was made between new-onset and chronic diagnoses. The study from a pED in New York found an increase in anxiety disorders in adults of 200% during the COVID-19-pandemic. Here, however, the results are probably not representative due to the insufficient sample size of a total of 16 patients with anxiety disorders (32).
A Canadian study found that fewer young patients presented to primary care with a new episode of anxiety during the first wave, albeit incidence rates were higher during the second wave than before the pandemic. Older adults were found to have higher incidence rates of anxiety disorders in both waves than before the pandemic (82). Age was not found to be a predictor of new-onset in our study. This suggests local differences in risk factors for new-onset diagnoses.
Reasons for this increase are not fully understood yet. There might be more fear in general because of the pandemic, such as fear of a COVID-19 infection (37) as well as more social fears due to social distancing (83).
While there was a decline in the absolute number of patients attending police custody, there was an increase in the relative attendance in police custody. Significantly, a high proportion of patients with a new-onset of a psychiatric disorder during the COVID-19-period attended police custody.
Other studies also show higher proportions of police referrals (48, 84, 85) but do not report if these patients had chronic or new-onset diseases. A Canadian study indicated a drastic increase of emergency police calls involving persons with perceived mental illness, especially in the second wave (86).
In the current study “attendance in police custody” was a predictor of new-onset diagnoses during the COVID-19-period, suggesting high acuity of these cases. In line with this, we found that hospital admissions and involuntary admissions did occur more often in new-onset diagnoses during the COVID-19-period than during the control period. This implies that the more severe cases were also the cases that were more likely to be newly diagnosed. People might have waited until it was too late to be able to go voluntarily to the hospital, for fear of getting infected with COVID-19, which might account for the increase in attendance in police custody. A study from London showed that patients were likely to experience a longer duration of symptoms before seeking help from mental health services during the COVID-19 pandemic (14).
We could not find a correlation between the number of new-onset diagnoses and the 7-day incidence of COVID-19 cases in Berlin (Figure 1). This is in line with a study from Israel showing no epidemiological evidence for a causal link between the number of COVID-19 cases and the increased ratio of new-onset psychosis and mania during the first and second wave of COVID-19 (47).
Our results do not show a concordant increase in pED presentations with new-onset psychiatric disorders along with the implementation of a hard lockdown (Figure 1). This is in contrast to the above-mentioned Israeli study, which did report a correlation between lockdown and an increase in new-onset of psychosis and mania (47). This finding may indicate different lockdown implications in different countries or different populations. In Turkey, for example, there is evidence even for improvement of mental health symptoms during the first lockdown in college students (87). Heterogeneities like this, stress the potential impact of local differences. In addition, differences in the extent of lockdown measures may be an explanatory factor (88).
If post-COVID-19 was the driving factor behind the increase in new-onset pED presentations, one would expect an increase in new-onset cases over time as the virus continued spreading. This was not the case in our sample. Furthermore, in the current study we report an increase in new-onset psychiatric disorders not only in depression disorders, anxiety disorders and schizophrenia spectrum and psychotic disorders, which are also reported as being caused by COVID-19 infections (26–32), but also in substance use disorders, which up until now, have not been linked to COVID-19 infections. In summary, we posit that the increases in new-onset psychiatric disorders reported in this study are for the most part not due to a prior COVID-19 infection but due to the indirect effect of the pandemic.
This study is the first to systematically investigate the prevalence of new-onset psychiatric diagnoses in pED presentations during the second wave of COVID-19, together with associated risk factors. The current study covers a relatively long observation period with a comparably large number of assessed pED presentations. Indicators of mental health were based on clinical diagnoses rather than self-reports. In addition, our detailed clinician-led review of each case was based on thorough clinical documentation and gave detail to elucidate the changes during the COVID-19-period.
The following limitations need to be considered: the control data is limited to the previous year only. We cannot rule out the possibility that the control year had an unusual low ratio of new-onset diagnoses. Furthermore, the study only reflects mental health during a part of the pandemic and may thus miss rebound effects in post-lockdown periods or long-time effects. The study is based on clinical routine data which can differ in quality and extent which may introduce bias. We cannot completely rule out the possibility of an interrater bias. However, to limit this bias we implemented the following measures: consulting all available data and scheduling regular meetings to discuss pressing questions, resolving them in consensus.
A further limitation is that we only gathered information about patients presenting with new-onset diagnoses in a single-center psychiatric emergency department. Extrapolation of results should therefore be done with caution. Besides, taking into account all diagnostic subgroups, our study does not provide information on whether there was a complete new-onset of symptoms or whether a decompensation of prior “subthreshold” psychiatric symptoms has occurred.
Only very few patients presented with a COVID-19 infection or a history of COVID-19 infection. Asymptomatic infections and underreporting are likely.
Psychiatric emergency department presentations with new-onset diagnoses of substance use disorders, depressive disorders, schizophrenia spectrum and psychotic disorders and anxiety disorders strongly increased during the COVID-19-period. These diagnoses and attendance in police custody were predictors of new-onset diagnoses during the second wave of the pandemic.
The current study provides evidence suggesting that the underlying factors affecting these increases in new-onset diseases at this phase of the pandemic were generally not directly linked to COVID-19 infections, but rather to other indirect sequelae of the pandemic. The current study reports greater job loss, living alone, and a relative decrease in familial relationships in patients with new-onset psychiatric diseases in the COVID-19-period as compared to the control period. These factors might have contributed to the increase in new-onset psychiatric diseases. Further studies are needed to assess the respective effects and other potential pathogenic factors. However, to date it is evident that some pathogenic factors are man-made and unintended sequelae of strict lockdown policies. Therefore, our findings should be taken into account for future pandemic control policies.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving humans were approved by the local ethics committee (Charité Universitätsmedizin, Berlin; number of approval: EA 110/20). The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants’ legal guardians/next of kin in accordance with the national legislation and institutional requirements.
TG and SG conceptualized this study. MA wrote the original draft, edited and critically revised the manuscript. TG, SG, MS-O, YK, and JM edited and critically revised the manuscript. MA and YK extracted data from clinical documentation records. MA conceptualized and executed statistical analyses together with JM. All authors contributed to the article and approved the submitted version.
We acknowledge financial support for the publication fee from the Open Access Publication Fund of Charité – Universitätsmedizin Berlin and the German Research Foundation (DFG).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1240703/full#supplementary-material
1. Rahman, S, Montero, MTV, Rowe, K, Kirton, R, and Kunik, F. Epidemiology, pathogenesis, clinical presentations, diagnosis and treatment of COVID-19: a review of current evidence. Expert Rev Clin Pharmacol. (2021) 14:601–21. doi: 10.1080/17512433.2021.1902303
2. Fahriani, M, Ilmawan, M, Fajar, JK, Maliga, HA, Frediansyah, A, Masyeni, S, et al. Persistence of long COVID symptoms in COVID-19 survivors worldwide and its potential pathogenesis - a systematic review and meta-analysis. Narra J. (2021) 1:1–14. doi: 10.52225/narraj.v1i2.36
3. Fajar, JK, Ilmawan, M, Mamada, SS, Mutiawati, E, Husnah, M, Yusuf, H, et al. Global prevalence of persistent neuromuscular symptoms and the possible pathomechanisms in COVID-19 recovered individuals: a systematic review and meta-analysis. Narra J. (2021) 1:27–43. doi: 10.52225/narra.v1i3.48
4. Chronik zum Coronavirus SARS-CoV-2. Maßnahmen - Bundesgesundheitsministerium. (2022). Available at: https://www.bundesgesundheitsministerium.de/coronavirus/chronik-coronavirus.html
5. Cheng, C, Barceló, J, Hartnett, AS, Kubinec, R, and Messerschmidt, L. COVID-19 government response event dataset (CoronaNet v.1.0). Nat Hum Behav. (2020) 4:756–68. doi: 10.1038/s41562-020-0909-7
6. Shi, L, Lu, ZA, Que, JY, Huang, XL, Liu, L, Ran, MS, et al. Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw Open. (2020) 3:e2014053:221–5. doi: 10.1001/jamanetworkopen.2020.14053
7. Pierce, M, Hope, H, Ford, T, Hatch, S, Hotopf, M, John, A, et al. Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry. (2020) 7:883–92. doi: 10.1016/S2215-0366(20)30308-4
8. Özdin, S, and Bayrak, ÖŞ. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: the importance of gender. Int J Soc Psychiatry. (2020) 66:504–11. doi: 10.1177/0020764020927051
9. Kunzler, AM, Röthke, N, Günthner, L, Stoffers-Winterling, J, Tüscher, O, Coenen, M, et al. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Glob Health. (2021) 17:34. doi: 10.1186/s12992-021-00670-y
10. Rodriguez-Jimenez, R, Rentero, D, Romero-Ferreiro, V, and García-Fernández, L. Impact of outbreak COVID-19 pandemic on psychiatry emergencies in Spain. Psychiatry Res. (2021) 295:113581. doi: 10.1016/j.psychres.2020.113581
11. Beghi, M, Brandolini, R, Casolaro, I, Beghi, E, Cornaggia, CM, Fraticelli, C, et al. Effects of lockdown on emergency room admissions for psychiatric evaluation: an observational study from 4 centres in Italy. Int J Psychiatry Clin Pract. (2021) 25:135–9. doi: 10.1080/13651501.2020.1859120
12. Kratochvil, D, Hill, H, and Moylan, S. The impact of stage 3 COVID-19 lockdown on psychiatric presentations at a regional Victorian emergency department. Australas Psychiatry. (2021) 29:105–6. doi: 10.1177/1039856220968390
13. Holland, KM, Jones, C, Vivolo-Kantor, AM, Idaikkadar, N, Zwald, M, Hoots, B, et al. Trends in US emergency department visits for mental health, overdose, and violence outcomes before and during the COVID-19 pandemic. JAMA Psychiatry. (2021) 78:372–9. doi: 10.1001/jamapsychiatry.2020.4402
14. Mukadam, N, Sommerlad, A, Wright, J, Smith, A, Szczap, A, Solomou, S, et al. Acute mental health presentations before and during the COVID-19 pandemic. BJPsych Open. (2021) 7:e134. doi: 10.1192/bjo.2021.970
15. Ambrosetti, J, Macheret, L, Folliet, A, Wullschleger, A, Amerio, A, Aguglia, A, et al. Psychiatric emergency admissions during and after COVID-19 lockdown: short-term impact and long-term implications on mental health. BMC Psychiatry. (2021) 21:465. doi: 10.1186/s12888-021-03469-8
16. Kippe, YD, Adam, M, Finck, A, Moran, JK, Schouler-Ocak, M, Bermpohl, F, et al. Suicidality in psychiatric emergency department situations during the first and the second wave of COVID-19 pandemic. Eur Arch Psychiatry Clin Neurosci. (2022) 273:311–23. doi: 10.1007/s00406-022-01486-6
17. McAndrew, J, O’Leary, J, Cotter, D, Cannon, M, MacHale, S, Murphy, KC, et al. Impact of initial COVID-19 restrictions on psychiatry presentations to the emergency department of a large academic teaching hospital. Ir J Psychol Med. (2021) 38:108–15. doi: 10.1017/ipm.2020.115
18. Håkansson, A, and Grudet, C. Decreasing psychiatric emergency visits, but stable addiction emergency visits, during COVID-19—a time series analysis 10 months into the pandemic. Front Psych. (2021) 12:1122. doi: 10.3389/fpsyt.2021.664204
19. Butler, M, Delvi, A, Mujic, F, Broad, S, Pauli, L, Pollak, TA, et al. Reduced activity in an inpatient liaison psychiatry service during the first wave of the COVID-19 pandemic: comparison with 2019 data and characterization of the SARS-CoV-2 positive cohort. Front Psych. (2021) 12:619550. doi: 10.3389/fpsyt.2021.619550
20. Gonçalves-Pinho, M, Mota, P, Ribeiro, J, Macedo, S, and Freitas, A. The impact of COVID-19 pandemic on psychiatric emergency department visits – a descriptive study. Psychiatry Q. (2021) 92:621–31. doi: 10.1007/s11126-020-09837-z
21. Federal Government Germany. Corona-Pandemie: Merkel fordert nationale Kraftanstrengung. (2020). Available at: https://www.bundesregierung.de/breg-de/suche/bund-laender-beschluss-1805264 (Accessed December 6, 2022).
22. Zahra, Z, Ramadhani, CT, Mamfaluti, T, Pamungkas, SR, and Firdausa, S. Association between depression and HbA1c levels in the elderly population with type 2 diabetes mellitus during COVID-19. pandemic Narra J. (2022) 2:49–55. doi: 10.52225/narra.v2i1.51
23. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatry. (2022) 9:137–50. doi: 10.1016/S2215-0366(21)00395-3
24. Arias, D, Saxena, S, and Verguet, S. Quantifying the global burden of mental disorders and their economic value. eClinicalMedicine. (2022) 54:101675. doi: 10.1016/j.eclinm.2022.101675
25. Vindegaard, N, and Benros, ME. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav Immun. (2020) 89:531–42. doi: 10.1016/j.bbi.2020.05.048
26. Ma, YF, Li, W, Deng, HB, Wang, L, Wang, Y, Wang, PH, et al. Prevalence of depression and its association with quality of life in clinically stable patients with COVID-19. J Affect Disord. (2020) 275:145–8. doi: 10.1016/j.jad.2020.06.033
27. Iosifescu, AL, Hoogenboom, WS, Buczek, AJ, Fleysher, R, and Duong, TQ. New-onset and persistent neurological and psychiatric sequelae of COVID-19 compared to influenza: a retrospective cohort study in a large new York City healthcare network. Int J Methods Psychiatr Res. (2022) 31:e1914. doi: 10.1002/mpr.1914
28. Hu, Y, Chen, Y, Zheng, Y, You, C, Tan, J, Hu, L, et al. Factors related to mental health of inpatients with COVID-19 in Wuhan, China. Brain Behav Immun. (2020) 89:587–93. doi: 10.1016/j.bbi.2020.07.016
29. Mourani, SC, Khoury, R, and Ghossoub, E. Mechanisms of new-onset psychosis during the COVID-19 pandemic: what ignited the fire? Ann Clin Psychiatry. (2022) 34:123–35. doi: 10.12788/acp.0065
30. Yalçın, M, Baş, A, Bilici, R, Özdemir, YÖ, Beştepe, EE, Kurnaz, S, et al. Psychiatric emergency visit trends and characteristics in a mental health epicenter in Istanbul during COVID-19 lockdown. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:2299–310. doi: 10.1007/s00127-021-02171-0
31. Parra, A, Juanes, A, Losada, CP, Álvarez-Sesmero, S, Santana, VD, Martí, I, et al. Psychotic symptoms in COVID-19 patients. A retrospective descriptive study. Psychiatry Res. (2020) 291:113254. doi: 10.1016/j.psychres.2020.113254
32. Ferrando, SJ, Klepacz, L, Lynch, S, Shahar, S, Dornbush, R, Smiley, A, et al. Psychiatric emergencies during the height of the COVID-19 pandemic in the suburban new York City area. J Psychiatr Res. (2021) 136:552–9. doi: 10.1016/j.jpsychires.2020.10.029
33. Coleman, B, Casiraghi, E, Blau, H, Chan, L, Haendel, MA, Laraway, B, et al. Risk of new-onset psychiatric sequelae of COVID-19 in the early and late post-acute phase. World Psychiatry. (2022) 21:319. doi: 10.1002/wps.20992
34. Kim, J, Seo, YE, Sung, HK, Park, HY, Han, MH, and Lee, SH. Predictors of the development of mental disorders in hospitalized COVID-19 patients without previous psychiatric history: a single-Center retrospective study in South Korea. Int J Environ Res Public Health. (2022) 19:1092. doi: 10.3390/ijerph19031092
35. Taquet, M, Luciano, S, Geddes, JR, and Harrison, PJ. Bidirectional associations between COVID-19 and psychiatric disorder: retrospective cohort studies of 62 354 COVID-19 cases in the USA. Lancet Psychiatry. (2021) 8:130–40. doi: 10.1016/S2215-0366(20)30462-4
36. Ferrando, SJ, Klepacz, L, Lynch, S, Tavakkoli, M, Dornbush, R, Baharani, R, et al. COVID-19 psychosis: a potential new neuropsychiatric condition triggered by novel coronavirus infection and the inflammatory response? Psychosomatics. (2020) 61:551–5. doi: 10.1016/j.psym.2020.05.012
37. Winkler, JG, Jalilzadeh Masah, D, Moran, JK, Bretz, J, Tsagkas, I, Goldschmidt, T, et al. Psychische Belastung während der COVID-19-Pandemie: Konsequenzen für psychiatrisch Erkrankte und therapeutische Implikationen. Nervenarzt. (2021) 92:243–51. doi: 10.1007/s00115-020-01056-y
38. Yasmin, F, Dapke, K, Khalid, MR, Naz, H, Naz, F, Admani, B, et al. Generalized anxiety disorder and depressive symptoms among Pakistani population during the second wave of the COVID-19 pandemic: a regression analysis. Am J Trop Med Hyg. (2021) 105:915–23. doi: 10.4269/ajtmh.21-0380
39. O'Connor, RC, Wetherall, K, Cleare, S, McClelland, H, Melson, AJ, Niedzwiedz, CL, et al. Mental health and well-being during the COVID-19 pandemic: longitudinal analyses of adults in the UK COVID-19 Mental Health & Wellbeing study. Br J Psychiatry. (2021) 218:326–33. doi: 10.1192/bjp.2020.212
40. Liu, S, Heinzel, S, Haucke, MN, and Heinz, A. Increased psychological distress, loneliness, and unemployment in the spread of COVID-19 over 6 months in Germany. Medicina (Kaunas). (2021) 57:1–11. doi: 10.3390/medicina57010053
41. Krings, A, Steffen, G, and Germershausen, C. Zimmermann R. Auswirkungen der COVID-19-Krise auf Präventionsangebote zu durch Blut und sexuell übertragenen Infektionen bei Drogengebrauchenden. Basel, Switzerland: MDPI (2020).
42. Reich, H, Czaplicki, A, Gravert, C, and Hegerl, U. Negative effects of COVID-19 measures on the care of people with depression: results of a representative population survey. Nervenarzt. (2022) 93:305–8. doi: 10.1007/s00115-021-01148-3
43. Ärzteblatt. Psychotherapie während der Coronapandemie: Selbstfürsorge und Reflexion. (2020). Available at: https://www.aerzteblatt.de/archiv/213962/Psychotherapie-waehrend-der-Coronapandemie-Selbstfuersorge-und-Reflexion (Accessed November 9, 2022).
44. Fasshauer, JM, Schomerus, G, and Stengler, K. COVID-19 pandemic and psychiatry - how much have the interests of people with psychiatric disorders been considered in German Laws? Psychiatr Prax. (2021) 48:309–15. doi: 10.1055/a-1353-1774
45. Caldirola, D, Cuniberti, F, Daccò, S, Grassi, M, Torti, T, and Perna, G. Predicting new-onset psychiatric disorders throughout the COVID-19 pandemic: a machine learning approach. J Neuropsychiatry Clin Neurosci. (2022) 34:233–46. doi: 10.1176/appi.neuropsych.21060148
46. Seifert, J, Meissner, C, Birkenstock, A, Bleich, S, Toto, S, Ihlefeld, C, et al. Peripandemic psychiatric emergencies: impact of the COVID-19 pandemic on patients according to diagnostic subgroup. Eur Arch Psychiatry Clin Neurosci. (2021) 271:259–70. doi: 10.1007/s00406-020-01228-6
47. Segev, A, Hirsch-Klein, E, Kotz, G, Kamhi-Nesher, S, Halimi, S, Qashu, K, et al. Trends of new-onset psychosis or mania in psychiatric emergency departments during the COVID19 pandemic: a longitudinal comparative study. Sci Rep. (2021) 11:21002. doi: 10.1038/s41598-021-00310-w
48. Goldschmidt, T, Kippe, Y, Finck, A, Adam, M, Hamadoun, H, Winkler, JG, et al. Psychiatric presentations and admissions during the first wave of Covid-19 compared to 2019 in a psychiatric emergency department in Berlin, Germany: a retrospective chart review. BMC Psychiatry. (2023) 23:38. doi: 10.1186/s12888-023-04537-x
49. Henssler, J, Stock, F, van Bohemen, J, Walter, H, Heinz, A, and Brandt, L. Mental health effects of infection containment strategies: quarantine and isolation—a systematic review and meta-analysis. Eur Arch Psychiatry Clin Neurosci. (2021) 271:223–34. doi: 10.1007/s00406-020-01196-x
50. Office for Health and Social Affairs Berlin (LAGeSo). COVID-19 in Berlin, Fallzahlen und Indikatoren – Gesamtübersicht. (2020). Available at: https://www.berlin.de/lageso/gesundheit/infektionskrankheiten/corona/tabelle-indikatoren-gesamtuebersicht/ (Accessed April 23, 2022).
51. Tagesspiegel. Erste Lockerung: Friseure öffnen am 1. März – das müssen Kunden wissen. (2021). Available at: https://www.tagesspiegel.de/berlin/erste-lockerung-friseure-oeffnen-am-1-maerz-das-muessen-kunden-wissen/26956438.html (Accessed April 23, 2022).
52. City of Berlin. Lockdown in Berlin offiziell. (2020). Available at: https://www.berlin.de/aktuelles/berlin/6386726-958092-lockdown-in-berlin-offiziell.html (Accessed April 23, 2022).
53. Federal Government Germany. Telefonkonferenz der Bundeskanzlerin mit den Regierungschefinnen und Regierungschefs der Länder am 13. Dezember 2020. (2020). Available at: https://www.bundesregierung.de/resource/blob/975226/1827366/69441fb68435a7199b3d3a89bff2c0e6/2020-12-13-beschluss-mpk-data.pdf (Accessed April 23, 2022).
54. Grove, WM, Andreasen, NC, McDonald-Scott, P, Keller, MB, and Shapiro, RW. Reliability studies of psychiatric diagnosis: theory and practice. Arch Gen Psychiatry. (1981) 38:408–13.
55. Trapletti, A, Hornik, K, and LeBaron, B. Time series analysis and computational finance. (2023). Available at: https://cran.r-project.org/package=tseries (Accessed May 23, 2023).
56. Capuzzi, E, Di Brita, C, Caldiroli, A, Colmegna, F, Nava, R, Buoli, M, et al. Psychiatric emergency care during coronavirus 2019 (COVID 19) pandemic lockdown: results from a Department of Mental Health and Addiction of northern Italy. Psychiatry Res. (2020) 293:113463. doi: 10.1016/j.psychres.2020.113463
57. Di Lorenzo, R, Frattini, N, Dragone, D, Farina, R, Luisi, F, Ferrari, S, et al. Psychiatric emergencies during the Covid-19 pandemic: a 6-month observational study. Neuropsychiatr Dis Treat. (2021) 17:1763. doi: 10.2147/NDT.S307128
58. Roberts, A, Rogers, J, Mason, R, Siriwardena, AN, Hogue, T, Whitley, GA, et al. Alcohol and other substance use during the COVID-19 pandemic: a systematic review. Drug Alcohol Depend. (2021) 229:109150. doi: 10.1016/j.drugalcdep.2021.109150
59. Czeisler, M, Wiley, JF, Facer-Childs, ER, Robbins, R, Weaver, MD, Barger, LK, et al. Mental health, substance use, and suicidal ideation during a prolonged COVID-19-related lockdown in a region with low SARS-CoV-2 prevalence. J Psychiatr Res. (2021) 140:533–44. doi: 10.1016/j.jpsychires.2021.05.080
60. Dragovic, M, Pascu, V, and Waters, F. Psychiatrydragovic a. emergency department mental health presentations before and during the COVID-19 outbreak in Western Australia 960673A PY COVID-19 pandemic. Clin Res Cent. (2020) 28:627–31. doi: 10.1177/1039856220960673
61. Gómez-Ramiro, M, Fico, G, Anmella, G, Vázquez, M, Sagué-Vilavella, M, Hidalgo-Mazzei, D, et al. Changing trends in psychiatric emergency service admissions during the COVID-19 outbreak: report from a worldwide epicentre. J Affect Disord. (2021) 282:26–32. doi: 10.1016/j.jad.2020.12.057
62. Jacob, L, Smith, L, Armstrong, NC, Yakkundi, A, Barnett, Y, Butler, L, et al. Alcohol use and mental health during COVID-19 lockdown: a cross-sectional study in a sample of UK adults. Drug Alcohol Depend. (2021) 219:108488. doi: 10.1016/j.drugalcdep.2020.108488
63. Niedzwiedz, CL, Green, MJ, Benzeval, M, Campbell, D, Craig, P, Demou, E, et al. Mental health and health behaviours before and during the initial phase of the COVID-19 lockdown: longitudinal analyses of the UK household longitudinal study. J Epidemiol Community Health. (2021) 75:224–31. doi: 10.1136/jech-2020-215060
64. Murthy, P, and Narasimha, VL. Effects of the COVID-19 pandemic and lockdown on alcohol use disorders and complications. Curr Opin Psychiatry. (2021) 34:376–85. doi: 10.1097/YCO.0000000000000720
65. Tagesspiegel. Suchtexperten schlagen Alarm: Coronakrise treibt immer mehr Menschen zum Alkohol. (2021). Available at: https://www.tagesspiegel.de/politik/coronakrise-treibt-immer-mehr-menschen-zum-alkohol-7728853.html (Accessed October 5, 2022).
66. Baarck, J, d’Hombres, B, and Tintori, G. Loneliness in Europe before and during the COVID-19 pandemic. Health Policy. (2022) 126:1124–9. doi: 10.1016/j.healthpol.2022.09.002
67. United Nations Office on Drugs and Crime. COVID-19 and the drug supply chain: from production and trafficking to use. (2020). Available at: https://www.unodc.org/documents/data-and-analysis/covid/Covid-19-and-drug-supply-chain-Mai2020.pdf (Accessed December 30, 2022).
68. Lee, J, Solomon, M, Stead, T, Kwon, B, and Ganti, L. Impact of COVID-19 on the mental health of US college students. BMC Psychol. (2021) 9:95. doi: 10.1186/s40359-021-00598-3
69. Schecke, H, Fink, M, Bäuerle, A, Skoda, EM, Schweda, A, Musche, V, et al. Changes in substance use and mental health burden among women during the second wave of COVID-19 in Germany. Int J Environ Res Public Health. (2021) 18:9728. doi: 10.3390/ijerph18189728
70. Marzo, RR, Vinay, V, Bahari, R, Chauhan, S, Ming, DAF, Nelson Fernandez, SFA, et al. Depression and anxiety in Malaysian population during third wave of the COVID-19 pandemic. Clin Epidemiol Glob Heal. (2021) 12:100868. doi: 10.1016/j.cegh.2021.100868
71. Zhang, Z, Feng, Y, Song, R, Yang, D, and Duan, X. Prevalence of psychiatric diagnosis and related psychopathological symptoms among patients with COVID-19 during the second wave of the pandemic. Glob Health. (2021) 17:44. doi: 10.1186/s12992-021-00694-4
72. Caldirola, D, Daccò, S, Cuniberti, F, Grassi, M, Alciati, A, Torti, T, et al. First-onset major depression during the COVID-19 pandemic: a predictive machine learning model. J Affect Disord. (2022) 310:75–86. doi: 10.1016/j.jad.2022.04.145
73. Nomura, K, Yamazaki, T, Maeda, E, Hirayama, J, Ono, K, Fushimi, M, et al. Longitudinal survey of depressive symptoms among university students during the COVID-19 pandemic in Japan. Front Psychol. (2022) 13:863300. doi: 10.3389/fpsyg.2022.863300
74. Mazure, CM, Bruce, ML, Maciejewski, PK, and Jacobs, SC. Adverse life events and cognitive-personality characteristics in the prediction of major depression and antidepressant response. Am J Psychiatry. (2000) 157:896–903. doi: 10.1176/appi.ajp.157.6.896
75. Corona-Krise: Monatliche Arbeitslosenquote bis 2021 | Statista [Internet]. (2023). Available from: https://de.statista.com/statistik/daten/studie/1290076/umfrage/corona-krise-arbeitslosenquote-in-deutschland/
76. Kessler, RC, Angermeyer, M, Anthony, JC, de Graaf, R, Demyttenaere, K, Gasquet, I, et al. Lifetime prevalence and age-of-onset distributions of mentaldisorders in the World Health Organization’s world mental health survey initiative. World Psychiatry. (2007) 6:168–76.
77. Kozato, N, Mishra, M, and Firdosi, M. New-onset psychosis due to COVID-19. BMJ Case Rep. (2021) 14:242538. doi: 10.1136/bcr-2021-242538
78. Moccia, L, Kotzalidis, GD, Bartolucci, G, Ruggiero, S, Monti, L, Biscosi, M, et al. COVID-19 and new-onset psychosis: a comprehensive review. J Pers Med. (2023) 13:104. doi: 10.3390/jpm13010104
79. Agostino, D, Angelo, S, Giordano, B, Cigognini, AC, Chirico, ML, Redaelli, C, et al. Brief psychotic disorder during the National Lockdown in Italy: an emerging clinical phenomenon of the COVID-19 pandemic. Schizophr Bull. (2021) 47:15–22. doi: 10.1093/schbul/sbaa112
80. Brooks, V. COVID-19’s effects on emergency psychiatry. Curr Psychiatr Ther. (2020) 19:33–9. doi: 10.12788/cp.0013
81. Travis-Lumer, Y, Kodesh, A, Goldberg, Y, Reichenberg, A, Frangou, S, and Levine, SZ. Biopsychosocial exposure to the COVID-19 pandemic and the relative risk of schizophrenia: interrupted time-series analysis of a nationally representative sample. Eur Psychiatry. (2022) 65:e7. doi: 10.1192/j.eurpsy.2021.2245
82. Stephenson, E, O’Neill, B, Kalia, S, Ji, C, Crampton, N, Butt, DA, et al. Effects of COVID-19 pandemic on anxiety and depression in primary care: a retrospective cohort study. J Affect Disord. (2022) 303:216–22. doi: 10.1016/j.jad.2022.02.004
83. Santini, ZI, Jose, PE, York Cornwell, E, Koyanagi, A, Nielsen, L, Hinrichsen, C, et al. Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): a longitudinal mediation analysis. Lancet Public Health. (2020) 5:e62–70. doi: 10.1016/S2468-2667(19)30230-0
84. Ng, L, Narayanan, N, Diamond, D, and Pitigala, N. Audit of acute psychiatric presentations during New Zealand’s first COVID-19 national lockdown. Australas Psychiatry. (2022) 30:223–8. doi: 10.1177/10398562211052918
85. Liu, CH, Chen, PC, Chen, JH, and Yeh, CC. Changes in self-harm- and violence-related urgent psychiatric consultation in the emergency department during the different stages of the COVID-19 pandemic. BMC Psychiatry. (2022) 22:384. doi: 10.1186/s12888-022-04029-4
86. Koziarski, J. The effect of the COVID-19 pandemic on mental health calls for police service. Crime Sci. (2021) 10:22. doi: 10.1186/s40163-021-00157-6
87. Dogan, AE, Kebapci, D, Ertan, O, Kalay, Z, Caki, NK, Sar, V, et al. Decreased psychiatric symptomatology after the onset of COVID-19 in a longitudinal college mental health study. npj Ment Heal Res. (2022) 1:1–8. doi: 10.1038/s44184-022-00017-4
Keywords: COVID-19, mental health, psychiatric disorder, new-onset, lockdown, psychiatric emergency department
Citation: Adam M, Moran JK, Kippe YD, Schouler-Ocak M, Bermpohl F, Gutwinski S and Goldschmidt T (2023) Increase in presentations with new-onset psychiatric disorders in a psychiatric emergency department in Berlin, Germany during the second wave of the COVID-19 pandemic – a retrospective cross-sectional study. Front. Psychiatry. 14:1240703. doi: 10.3389/fpsyt.2023.1240703
Received: 15 June 2023; Accepted: 25 September 2023;
Published: 12 October 2023.
Edited by:
Renato de Filippis, University Magna Graecia of Catanzaro, ItalyReviewed by:
Atefeh Zandifar, Alborz University of Medical Sciences, IranCopyright © 2023 Adam, Moran, Kippe, Schouler-Ocak, Bermpohl, Gutwinski and Goldschmidt. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thomas Goldschmidt, dGhvbWFzLmdvbGRzY2htaWR0QGNoYXJpdGUuZGU=
†ORCID: Thomas Goldschmidt, https://orcid.org/0000-0003-2948-0362
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.