- 1Department of Psychiatry, Tongji Hospital, School of Medicine, Tongji University, Shanghai, China
- 2Clinical Research Center, Tongji Hospital, School of Medicine, Tongji University, Shanghai, China
- 3Department of Medical Education, Tongji Hospital, School of Medicine, Tongji University, Shanghai, China
- 4Teaching Office, Renmin Hospital of Wuhan University, Wuhan, China
- 5Clinical Research Center for Mental Disorders, Chinese-German Institute of Mental Health, Shanghai Pudong New Area Mental Health Center, School of Medicine, Tongji University, Shanghai, China
Introduction: The Coronavirus disease 2019 (COVID-19) pandemic is a global traumatic event that has profoundly struck individuals’ mental health. However, this might potentially promote positive transformation such as posttraumatic growth (PTG). Studies have indicated that the COVID-19 pandemic negatively affected the well-being of resident physicians, but little is known about PTG among this vulnerable population in China. Therefore, this study investigated the prevalence and associated factors of PTG among Chinese resident physicians after 3-years outbreak of COVID-19.
Methods: An online survey was conducted from 9 March to 20 March in 2023. PTG was assessed using the 10-item Posttraumatic Growth Inventory-Short Form (PTGI-SF). Scores ≥30 implied moderate-to-high PTG. We also collected possible associated factors for PTG, including socio-demographic and psychological variables. Data was analyzed by applying descriptive statistics, univariable and multivariable logistic regression models.
Results: In total, 2267 Chinese resident physicians provided validated data. 38.7% of them reported moderate-to-high PTG. In the multivariable logistic regression models, age (odds ratio, OR = 1.039; 95% confidence interval, 95%CI = 1.008–1.070), female (OR = 1.383, 95%CI = 1.151–1.662), satisfied or neutral with annual income (OR = 2.078, 95%CI = 1.524–2.832; OR = 1.416, 95%CI = 1.157–1.732), sufficient support at work (OR = 1.432, 95%CI = 1.171–1.751) and resilience (OR = 1.171, 95%CI = 1.096–1.252) were significantly positively associated with moderate-to-high PTG. On the contrary, burnout (OR = 0.653, 95%CI = 0.525–0.812), depression symptoms (OR = 0.700, 95%CI = 0.552–0.889), and stress (OR = 0.757, 95%CI = 0.604–0.949) were significantly negatively associated with moderate-to-high PTG.
Discussion: Overall, resident physicians in China experienced relatively high prevalence of PTG that could be associated with several psychosocial factors. Findings may provide evidence to develop interventions for resident physicians to systematically and constructively process traumatic events related to the pandemic and foster their PTG.
Introduction
The Coronavirus disease 2019 (COVID-19) pandemic is an unforeseen and unprecedented global public health emergency that has had severe and far-reaching repercussions for health systems, economies, and societies worldwide. It is a shared global traumatic event that has profoundly threatened people’s mental health through disruptive societal changes and neuropsychiatric consequences following the infection (1, 2). Healthcare workers (HCW) experienced more adverse psychological outcomes due to the increased workload and heightened risk of infection, with prevalence rates ranging from 27.0 to 49.0% for anxiety, depression, sleep problems and post-traumatic stress disorder (3, 4).
Resident physicians constituted a crucial workforce in the healthcare system during the pandemic. In China, all medical graduates are required to undergo 3 years of systematic training, known as standardized residency training program (SRTP). As the healthcare system was strained during the COVID-19 epidemic, resident physicians inevitably assumed additional responsibilities and burdens, and had to rapidly adapt to changing pandemic management regulations (5, 6). Besides, physicians at this stage may generally experience higher levels of stress due to factors such as insufficient clinical training, financial constraints, heavy academic workload, family responsibilities and job competitions (7). Consequently, they were more susceptible to burnout, sleep disturbances and psychological distress during this challenging period (8–10). Their impaired mental health would not only interfere with their personal and professional growth but also negatively influence the quality of patient care (11).
As a global traumatic event, COVID-19 pandemic has not only caused widespread chaos and suffering, but also presented opportunities for positive transformation, a phenomenon known as posttraumatic growth (PTG). PTG is manifested in five aspects: more meaningful interpersonal relationships, new possibilities, increased sense of personal strength, deeper appreciation for life, and richer understanding of spiritual matters (12). Previously, numerous studies have demonstrated that individuals who have experienced life-threatening events such as cancer (13), natural disasters (14) and major life changes such as divorce (15) and bereavement (16) would experience PTG. And PTG encompasses extensive benefits, varying from making meaning of the adversity (17) and turning wounds into wisdom (18) to reducing the risk of psychiatric disorders and suicide intention (19, 20) and increasing personal development and life satisfaction (21).
In recent years, there has been a growing interest in PTG in the general public (22), university students (23) and HCW (24–26) during the COVID-19 pandemic. However, the existing psychological research on resident physicians during the pandemic predominantly focused on the negative impacts. Little has documented the PTG of them amidst this special stage. To fill this gap, this study aimed to evaluate the PTG and its associated factors among Chinese resident physicians after 3 years of the COVID-19 outbreak.
A recent systematic review of 27 studies on HCW demonstrated that PTG could enhance HCWs’ coping abilities in dealing with trauma, and it can be influenced by socio-demographic and psychological factors (27). Socio-demographics, such as age, gender, marital status and educational background, are assumed to be associated with PTG across diverse cohorts (27, 28). Working situations, including region, prior experience and work hours, are associated with the PTG of resident physicians during the COVID-19 pandemic (27). Psychological factors are important to the cognitive reconstruction, a necessary process in the formation of PTG (29). Income satisfaction, perceived support at work, burnout, stress, depression, anxiety, and resilience stand as pivotal variables that may influence PTG (27). Income satisfaction, as a measure of financial well-being, might influence the psychological adjustment of resident physicians (27). Support at work is anticipated to play a significant role in shaping their psychological responses (30). However, burnout, a prevalent issue among medical professionals, could hinder PTG by diminishing psychological resources and adaptive capacities (31, 32). Stress, depression, and anxiety are previously shown to be associated with PTG; however, consensus on whether these relationships are positive or negative has not been reached (33, 34). Conversely, resilience, characterized by tenacity, strength and optimism, could potentially facilitate PTG by enabling individuals to navigate the challenges on pandemic (35). To our knowledge, there is limited research on the relationship between PTG and the variables above among Chinese resident physicians.
Current study
This study is cross-sectional and was approved by the Tongji Hospital of Tongji University Institutional Review Board (Registration Number K-W-2023-002). The study was registered with the Chinese Clinical Trial Registry (Registration Number ChiCTR2300074782). An online survey was conducted from 9 March to 20 March in 2023. The aim of this study are two folds: firstly, to provide an overview of the current status of PTG among Chinese resident physicians after 3 years outbreak of COVID-19; secondly, to explore the association between PTG and socio-demographic (e.g., age, gender) or other psychological variables (e.g., income satisfaction, support at work, burnout, depression, anxiety, stress and resilience). We hope to provide evidence to develop interventions for resident physicians to systematically and constructively process traumatic events related to the pandemic and foster their PTG.
Materials and methods
Participants and procedure
Convenience sampling was adopted to collect data. The questionnaire was designed based on literature review and group discussion. A pilot study was conducted to improve the questionnaire’s quality. It involved 20 resident physicians from our team who completed the questionnaire. Their feedback and suggestions were carefully considered, leading to revisions aimed at enhancing the clarity and comprehensibility of the questions. Then an online questionnaire was created via www.wjx.cn, an extensively utilized online-survey platform in China. Thereafter, we distributed the questionnaire link to managers of SRTP from all Chinese provinces and municipalities via WeChat group (a widely used social media in China). SRTP managers volunteered to distribute the questionnaire link to resident physicians within their own units. The inclusion criteria of the study population were: (1) registered resident physician in China, and (2) voluntarily signed the informed consent form. There was no missing data as all questions were mandatory before submission. During the completion process, participants were free to terminate any time, and all previous responses would not be saved. A total of 2,364 residents completed the questionnaire. For the sake of data quality, 97 questionnaires with a completing time of less than 3 min were excluded. The remaining 2,267 were retained in the analyses, with a validity rate of 95.9%.
Sample size
Sample size was calculated based on a recent PTG survey of Chinese nurses during the COVID-19 pandemic, which reported a moderate-to-high PTG prevalence of 39.3% (36). A desired level of precision, with an allowable error of 0.03 and a significance level (α) of 0.05, was used to calculate the required sample size, resulting in a minimum of 1,018 resident physician. The actual sample size 2,267 exceeded this requirement, thus enabling the study to be conducted with sufficient statistical power.
Materials
Outcome—post-traumatic growth
The Posttraumatic Growth Inventory-Short Form (PTGI-SF) (37) was used to assess resident physicians’ positive psychological changes following COVID-19. The PTGI-SF consisted of 10 items measuring five domains of PTG: relating to others, personal strength, appreciation of life, spiritual change, and new possibilities (e.g., “I changed my priorities about what is important in life”). It was scored using a 6-point scale (0 as I did not experience this change, 5 as I experienced this change to a very great degree), with higher scores indicating greater levels of PTG. Scores ≥ 30 imply moderate-to-high PTG (38). The PTGI-SF has been applied among Chinese nurses over the pandemic and exhibited good reliability (25). The Cronbach’s α for this sample was 0.88.
Influential factors—socio-demographic and psychological factors
Socio-demographics include age, gender (male or female), marital status (unmarried/divorced or married/cohabitation), region of work (eastern, central or western China), residential status (living in dormitory, living with family, shared housing or living alone), educational background (Bachelor’s, Master’s or Doctoral degree), years in SRTP (1st, 2nd, or 3rd year), work experience before SRTP (yes or no), training specialty and weekly working hours.
Psychological factors include annual income satisfaction, being supported at work, sleep hours per day, burnout, stress, depression and anxiety symptoms and resilience. Annual income satisfaction was classified into satisfied, neutral and unsatisfied. Being supported at work was assessed by a 5-point Likert scale and subsequently categorized as either “insufficiently (very bad/bad)” or “sufficiently (average/good/very good).” Daily sleep hours was measured as a continuous variable and was cut off by 7 h.
Burnout was measured by the 2-item Maslach Burnout Inventory (MBI-2) (39) (e.g., “I feel burned out from my work”). Responses were rated on a 7-point scale ranging from 0 (never) to 6 (every day). Answering less than once a week (scores < 4) on both questions meant low burnout, otherwise the results stood for high burnout (40). The MBI-2 has been found to be reliable among Chinese physicians (41).
Stress was measured by the “stress subscale” of Depression Anxiety Stress Scales-21 (DASS-21) (42) which comprised of 7 items (e.g., “I found it difficult to relax.”) and was scored using a 4-point scale (0 as not apply to me at all, 3 as apply to me very much). Scores of 0–7 were considered normal, while scores of ≥8 represented mild or higher levels of stress (42). Evidence of reliability of the DASS-Stress was found among healthcare workers in China during the COVID-19 pandemic (43). For the present sample, the Cronbach’s α was 0.91.
Depression symptoms was measured by the Patient Health Questionnaire-2 (PHQ-2) (44). It consists of 2 items (e.g., Feeling down, depressed or hopeless.) and was rated on a 4-point scale ranging from 0 (not at all) to 3 (nearly every day). Scores of ≥3 indicating a positive screen for depression. PHQ-2 has been validated among Chinese population and the Cronbach’s α was 0.85 in this study (45).
Anxiety symptoms was measured by the Generalized Anxiety Disorder-2 (GAD-2) (46). It consists of 2 items (e.g., Feeling nervous, anxious or on edge). Participants used a 4-point scale ranging from 0 (not at all) to 3 (nearly every day). Scores of ≥3 indicating a positive screen for anxiety. Application of GAD-2 among Chinese people showed robust validation (47). The Cronbach’s α was 0.90 in this study.
Resilience was measured by Connor Davidson Resilience Scale-2 (CD-RISC-2), which contains 2 items (e.g., “Able to adapt to change”) (48). On a five-point scale from 0 (not true at all) to 4 (true nearly all the time), a higher score suggests more resilience. The reliability is good among Chinese people (49). The Cronbach’s α was 0.82 in the current sample.
Statistical analysis
Descriptive statistics were computed using frequencies and percentages for categorical variables, means and standard deviations (SD) for continuous variables. Univariable and multivariable binary logistic regression analyses were performed. In the multivariable binary logistic regression analysis, the input variables with p < 0.05 in the univariable analysis were selected using the forward stepwise method based on the likelihood ratio (LR). Odds ratios (ORs) and their 95% confidence intervals (CIs) were calculated to estimate the magnitude and direction of the relationship between each independent variable and PTG. The variance inflation factor (VIF) was used to assess multicollinearity among independent variables, with a VIF higher than 5 to 10 presenting significant multicollinearity (50). The goodness-of-fit of the logistic regression model determined using the Hosmer-Lemeshow test. Statistical significance was defined at p < 0.05. All statistical analyses were conducted using SPSS version 25.0 (IBM Corporation, Armonk, NY, United States).
Results
Participant characteristics
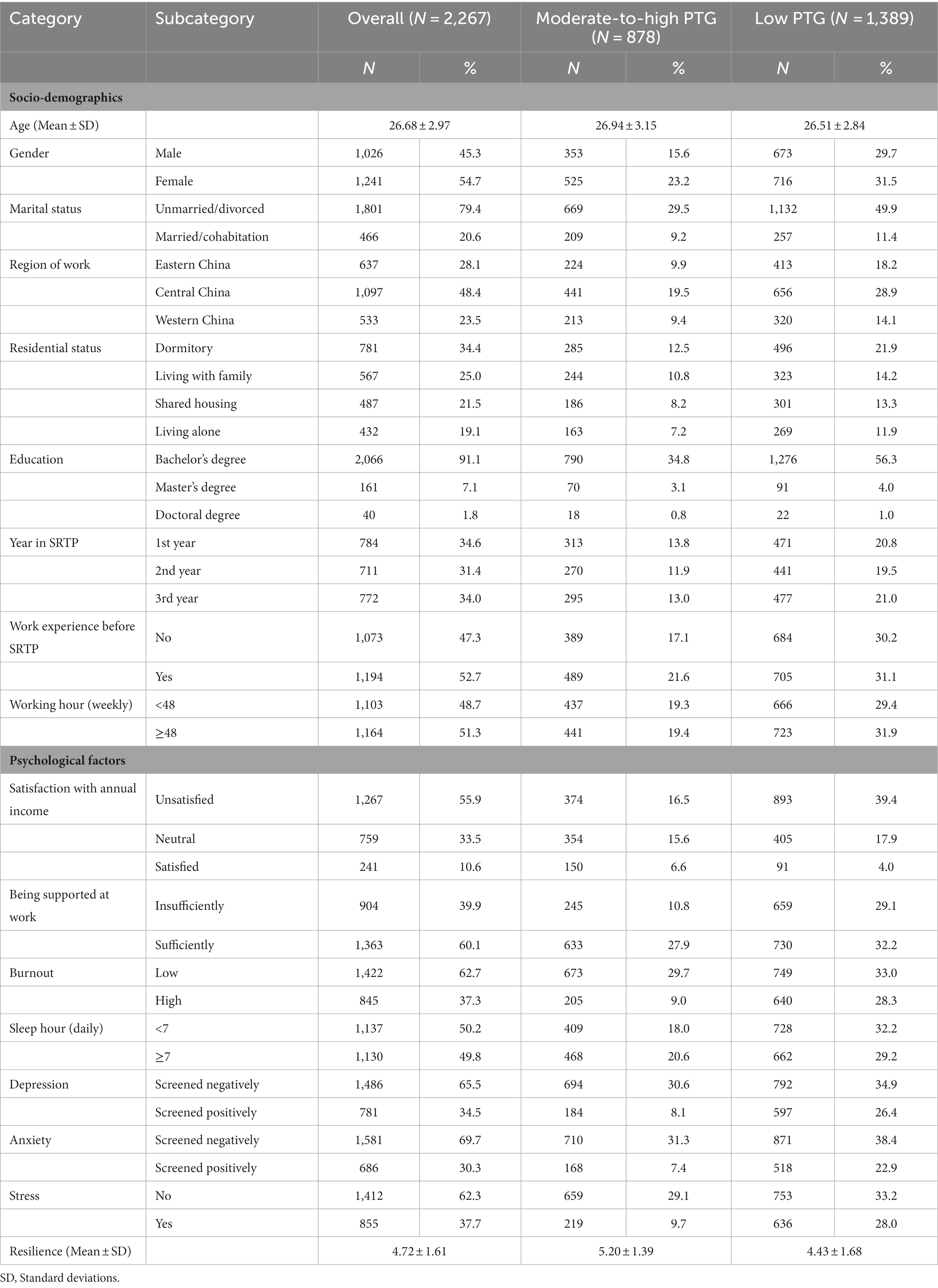
Our investigation covered 24 provinces and municipalities in China, such as Shanghai, Jiangsu, Zhejiang in eastern China, Hebei, Hunan, Anhui in central China; and Guangxi, Shaanxi, Sichuan in western China. The average age of the respondents was 26.68 years (range = 20–39; SD = 2.97). The majority of participants were female (1,241, 54.7%), single (1,801, 79.4%), working in central China (1,097, 48.4%), living in dormitory (781, 34.5%) and bachelors (2,066, 91.1%). 557 (23.6%) respondents were from internal medicine, 390 (16.5%) were from surgery, 359 (15.2%) were from family medicine, 158 (6.7%) were from anesthesiology, 155 (6.6%) were from medical imaging and nuclear medicine, 153 (6.5%) were from pediatrics, 122 (5.2%) were from obstetrics and gynecology, and the remaining respondents were from Dentistry (106, 4.7%), emergency medicine (64, 2.8%), neurology (59, 2.6%), psychiatry (36, 1.6%), dermatology (28, 1.2%), Otolaryngology (25, 1.1%), medical laboratory (22, 1.0%), ophthalmology (21, 0.9%), rehabilitation (9, 0.4%) and intensive care unit (3, 0.1%). Approximately half of the resident physicians had work experience before SRTP (52.7%), worked over 48 h per week (51.3%) and slept less than 7 h per day (50.2%). Three fifths thought they got sufficient support at work while merely one tenth were satisfied with their annual income. The proportion of high burnout, positively screened depression, positively screened anxiety, mild or higher stress were 37.3%, 34.5%, 30.3%, and 37.7%, respectively. The average score of resilience was 4.72 ± 1.61. Other details of participant characteristics were shown in Table 1.
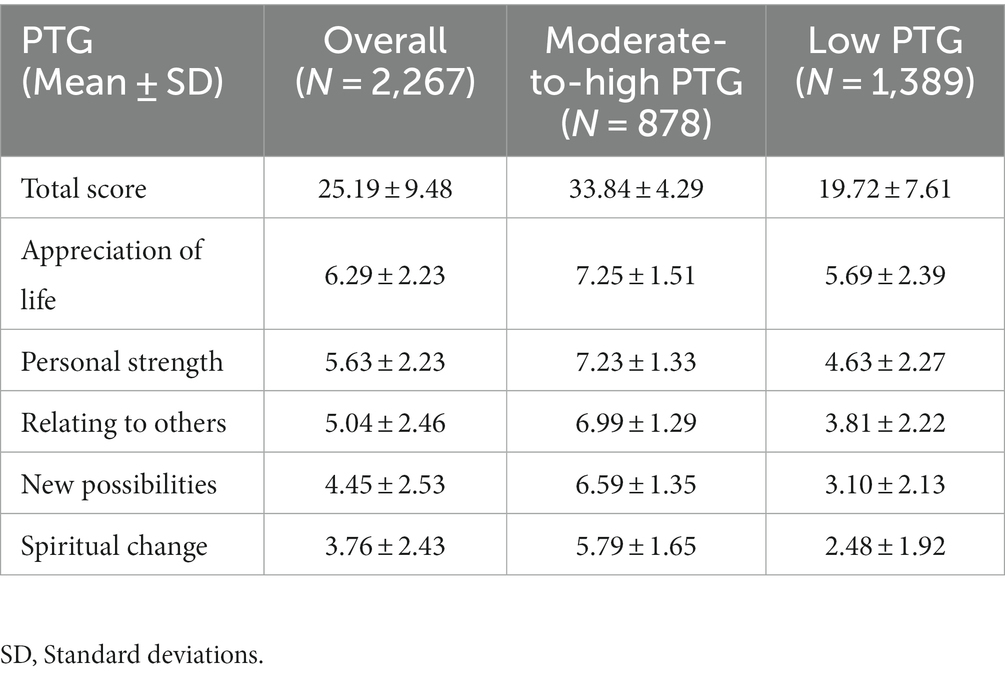
A total of 878 (38.7%) participants met the criteria of moderate-to-high level of PTG (scores ≥30). Shown in Table 2, the Mean ± SD scores of PTG total score, appreciation of life, personal strength, relating to others, spiritual change, and new possibilities were 25.19 ± 9.48, 6.29 ± 2.23, 5.63 ± 2.23, 5.04 ± 2.46, 4.45 ± 2.53, and 3.76 ± 2.43, respectively.
Logistic regression models
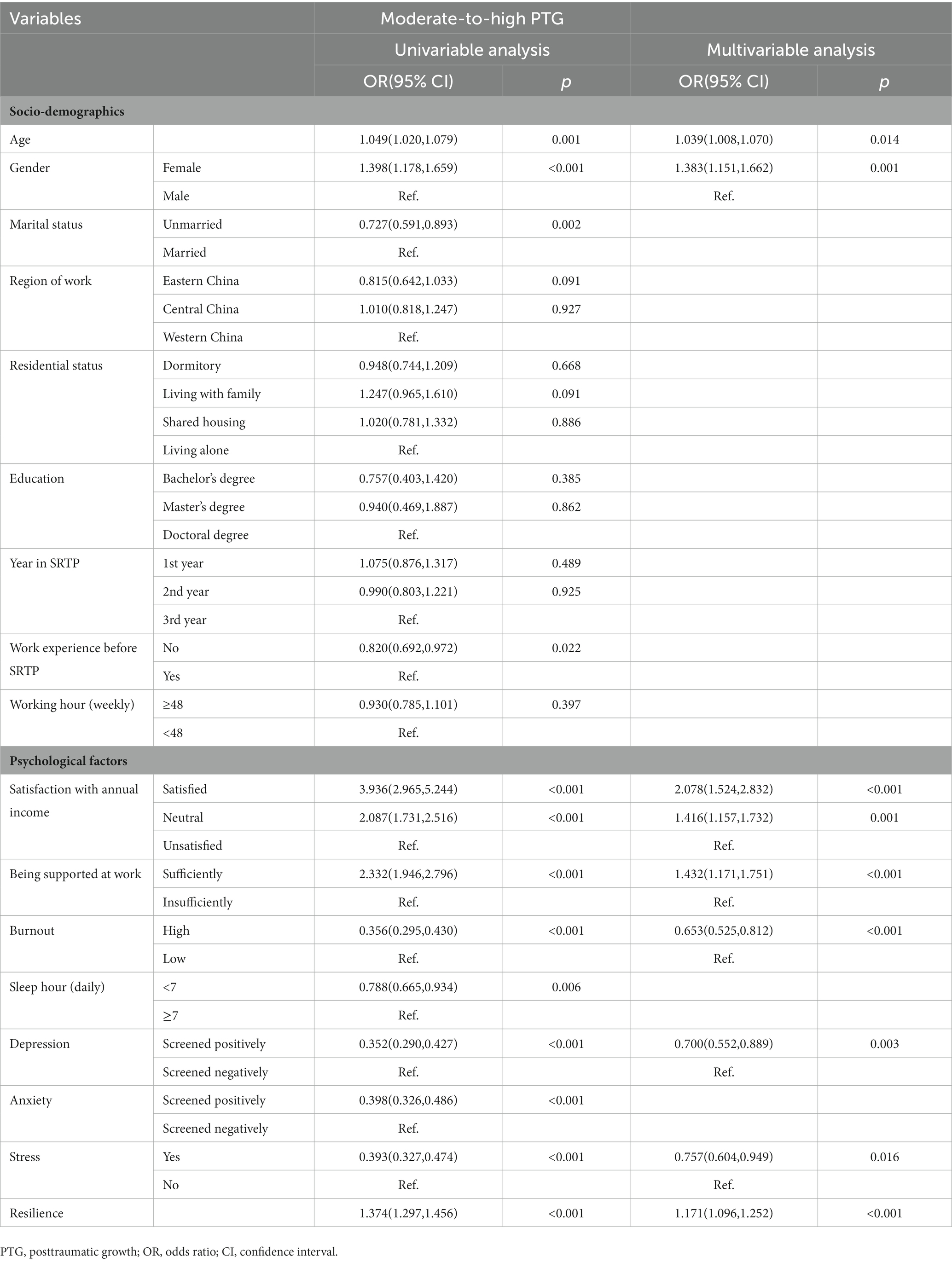
Table 3 demonstrates the univariable and multivariable binary logistic regression analyses of PTG. The VIFs among independent variables were between 1.027 and 2.197. According to the univariable regression model, age, gender, marital status, work experience before SRT, satisfaction with annual income, being supported at work, burnout, sleeping hours, depression and anxiety symptoms, stress and resilience were significant correlates of moderate-to-high PTG (p < 0.050). Multivariable binary logistic regression showed that age (OR = 1.039, 95%CI = 1.008–1.070, p = 0.014), female (OR = 1.383, 95%CI = 1.151–1.662, p = 0.001), satisfied with annual income (OR = 2.078, 95%CI = 1.524–2.832, p < 0.001), neutral in annual income (OR = 1.416, 95%CI = 1.157–1.732, p = 0.001), sufficient support at work (OR = 1.432, 95%CI = 1.171–1.751, p < 0.001) and resilience (OR = 1.171, 95%CI = 1.096–1.252, p < 0.001) were significant positive correlates of moderate-to-high PTG. On the contrary, burnout (OR = 0.653, 95%CI = 0.525–0.812, p < 0.001), depression symptoms (OR = 0.700, 95%CI = 0.552–0.889, p = 0.003), and stress (OR = 0.757, 95%CI = 0.604–0.949, p = 0.016) were significant negative correlates of moderate-to-high PTG. The Hosmer-Lemeshow goodness of fit test was χ2 = 7.313, df = 8, p = 0.503.
Discussion
The present study shows that, among Chinese resident physicians after 3 years outbreak of COVID-19, the prevalence of moderate-to-high PTG in this population was 38.7%. We report a similar prevalence and mean score among Chinese nurses in response to COVID-19 pandemic (36). The average score in our sample is higher than those reported in Hong Kong (25) and Australian (51) nurses, mental and community healthcare workers in the UK (52) and psychotherapists in the US (53). One possible explanation for the observed discrepancies in PTG scores could be the timing of investigation. As Zhou and Wu (54) showed, increased time elapsed after trauma allowed individuals more opportunity for deliberate rumination, which led to higher PTG. Our investigation was conducted 3 years after the outbreak of COVID-19, during which time resident physicians were faced with less challenging clinical work situations, providing them with more opportunities to restore inner harmony and facilitate positive changes. Additionally, disparities in PTG scores might also be linked to differences in the management of the pandemic across countries and variations in the responsibilities of healthcare workers.
Interestingly, appreciation of life is the highest scoring PTG domain, followed by personal strength, which suggested that the focus of resident physicians’ PTG is more internal and self-centered. In contrast, more experienced healthcare professionals might have a broader perspective on the pandemic, leading to a greater emphasis on relationships and new opportunities for personal and professional development, as evidenced by highest scores in domains of new possibilities and relating to others in a previous study of senior physicians and nurses (55).
Female resident physicians report greater PTG than males, which is in line with previous research findings (56). It is conceivable that females were more likely to seek out social resources and use emotion-focused coping strategies than males, which may facilitate PTG (57). However, it should be noted that the gender differences in PTG were not consistent across studies that varied in populations, types of trauma, and PTG measurement tools (58, 59). Age is weakly positively associated with PTG, implying that older resident physicians with more life experiences and coping skills might have a slightly greater capacity for positive adjustment in response to the pandemic.
Being supported at work and having high income satisfaction are two significant positive correlates of moderate-to-high PTG in resident physicians. PTG theoretical model by Tedeschi RG and Calhoun LG asserted that social support was instrumental in the development of PTG (29). Support at work and income are regarded as two forms of social support from workplace. On the one hand, being supported at work can provide resident physicians with a sense of belonging and assistance in coping with the demands and stressors of their job. When they perceived adequate support from colleagues, supervisors, or the organization as a whole, they might feel more valued and validated, thereby promoting cognition processing and contributing to PTG (60). On the other hand, high income satisfaction could mitigate financial stress and provide a sense of security and stability (61), which might enable resident physicians to adopt more positive coping strategies, such as seeking psychotherapy or participating in leisure activities. Notwithstanding, it is worth noting that a majority of resident physicians in our study reported low satisfaction with their annual income, in accordance with our earlier investigation of Shanghai resident physicians (62). Therefore, hospitals can implement interventions aimed at fostering and maintaining a supportive workplace environment and improving the work compensation for resident physicians to promote PTG.
Burnout is negatively associated with resident physicians’ PTG. This is congruent with a study conducted among Chinese nurses showing higher level of burnout were negatively associated with PTG (36). According to the effort-reward imbalance model by Johannes and colleagues (63), the additional workload, health risks, and relatively low income during the pandemic might increase the risk of burnout among resident physicians. Notably, burnout can trigger a range of detrimental consequences, including psychological issues such as depression and suicidal ideation, physical manifestations such as pain and fatigue, alongside challenges within the healthcare system such as strained doctor-patient relationships and medical errors (64–66), all of which might impede the experience of PTG. Although ours is one of the earliest studies to provide evidence on the relationship between burnout and PTG, further research is needed to fully understand the underlying mechanisms of this relationship.
Depression symptoms and stress are negatively associated with PTG, whereas resilience may catalyze it. The findings concur with former studies showing significant negative relationships between depression and PTG, stress and PTG (30) and a positive association between resilience and PTG (67). The negative effects of depression symptoms and stress on PTG may be attributed to the impact on cognitive processing, such as negative automatic thoughts and intrusive rumination, which can impede the meaning-construction process necessary for PTG (29). In contrast, resilience may ignite positive coping strategies and adaptive problem-solving skills in the face of trauma, leading to a more positive outlook and greater capacity for PTG (35). However, affective-cognitive processing model of PTG proposed by Joseph et al. (57) posited that high distress would challenge individuals’ understanding of the world, leading them to reflect extensively on their core beliefs and create new schemas and meanings, thus spurring the process of PTG. Although this theoretical framework is substantiated by prior research conducted with cancer patients (68) and earthquake survivors (69), our findings appear to contradict it. A possible account for this may be our study was cross-sectional designed and the depression and stress screening measurements only evaluated the current distress. At the time of assessment, the negative automatic thoughts and intrusive rumination caused by depression and stress had a more intense influence on PTG.
To our knowledge, this study represents the first attempt to adopt a positive perspective to investigate the favorable factors of PTG among resident physicians in China following the 3-years outbreak of COVID-19. The study also sheds light on psychological factors that may influence resident physicians’ PTG, addressing several under-researched questions, such as the relationship between burnout and PTG. Another notable strength of this study is the large sample size and coverage of the majority of the provinces and municipalities in China.
This study has some limitations. Firstly, the cross-sectional design of the study limits our ability to establish causality between the examined factors and outcome. Secondly, the use of online convenience sampling as a recruitment method may introduce response biases and affect the generalization of the results. Finally, the use of brief screening measurements to assess burnout, depression and anxiety may have limited the ability to explore complex relationships between variables, highlighting the need for more in-depth measurement tools in future research.
Based on the perspective of positive psychology, this study examined the associated factors of PTG among resident physicians in the wake of the COVID-19 pandemic. Practically, findings of this study implied that fostering a supportive workplace environment and improving the work compensation for resident physicians might be important to promote PTG among resident physicians. For those experiencing burnout, depression and stress, interventions based on positive psychology principles, such as emotional regulation training and narrative therapy, may potentially facilitate PTG (70). Future research should conduct a longitudinal design to investigate the trajectories of PTG over time and to explore the temporal relationships between PTG and other psychological characteristics among resident physicians.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Tongji Hospital of Tongji University Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
ZZ was responsible for study design, recruitment of respondents, and manuscript writing. YZ, RC, and XZ collected data and performed the data analyses. HW, ZL, and YL provided critical revisions. LH contributed to manuscript revision and research supervision. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Shanghai Pujiang Program, grant number: 2020PJC097, Key Projects of the Ministry of Education in 2019 under “The 13th Five-year Plan” for National Educational Science, grant number: DIA190409, Psychosomatic Medicine Project of Key Developing Disciplines of Shanghai Municipal Health Commission, grant number: 2019ZB0202.
Acknowledgments
The authors gratefully thank all the resident physicians who generously shared their time to participate in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1228259/full#supplementary-material
References
1. Penninx, B, Benros, ME, Klein, RS, and Vinkers, CH. How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med. (2022) 28:2027–37. doi: 10.1038/s41591-022-02028-2
3. Hu, N, Deng, H, Yang, H, Wang, C, Cui, Y, Chen, J, et al. The pooled prevalence of the mental problems of Chinese medical staff during the COVID-19 outbreak: a meta-analysis. J Affect Disord. (2022) 303:323–30. doi: 10.1016/j.jad.2022.02.045
4. Saragih, ID, Tonapa, SI, Saragih, IS, Advani, S, Batubara, SO, Suarilah, I, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud. (2021) 121:104002. doi: 10.1016/j.ijnurstu.2021.104002
5. Ey, S, Soller, M, and Moffit, M. Protecting the well-being of medical residents and faculty physicians during the COVID-19 pandemic: making the case for accessible, comprehensive wellness resources. Glob Adv Health Med. (2020) 9:2164956120973981. doi: 10.1177/2164956120973981
6. Seehusen, DA, Kost, A, Barr, WB, Theobald, M, Harper, DM, and Eden, AR. Family medicine Residents' experience during early phases of the COVID-19 pandemic. PRiMER. (2021) 5:18. doi: 10.22454/PRiMER.2021.909862
7. Levey, RE. Sources of stress for residents and recommendations for programs to assist them. Acad Med. (2001) 76:142–50. doi: 10.1097/00001888-200102000-00010
8. Jia, SZ, Zhao, YZ, Liu, JQ, Guo, X, Chen, MX, Zhou, SM, et al. Study of mental health status of the resident physicians in China during the COVID-19 pandemic. Front Psychol. (2022) 13:764638. doi: 10.3389/fpsyg.2022.764638
9. Steil, A, Pereira Tokeshi, AB, Bernardo, LS, da Silva Neto, GP, Júnior, DRF, Bárbara, A, et al. Medical residents' mental distress in the COVID-19 pandemic: an urgent need for mental health care. PLoS One. (2022) 17:e0266228. doi: 10.1371/journal.pone.0266228
10. Khalafallah, AM, Lam, S, Gami, A, Dornbos, DL, Sivakumar, W, Johnson, JN, et al. A national survey on the impact of the COVID-19 pandemic upon burnout and career satisfaction among neurosurgery residents. J Clin Neurosci. (2020) 80:137–42. doi: 10.1016/j.jocn.2020.08.012
11. Brunsberg, KA, Landrigan, CP, Garcia, BM, Petty, CR, Sectish, TC, Simpkin, AL, et al. Association of Pediatric Resident Physician Depression and Burnout with Harmful Medical Errors on inpatient services. Acad Med. (2019) 94:1150–6. doi: 10.1097/ACM.0000000000002778
12. Tedeschi, RG, and Calhoun, LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. (1996) 9:455–71. doi: 10.1007/BF02103658
13. Nik Jaafar, NR, Abd Hamid, N, Hamdan, NA, Rajandram, RK, Mahadevan, R, Mohamad Yunus, MR, et al. Posttraumatic growth, positive psychology, perceived spousal support, and psychological complications in head and neck cancer: evaluating their Association in a Longitudinal Study. Front Psychol. (2022) 13:920691. doi: 10.3389/fpsyg.2022.920691
14. Marshall, EM, Frazier, P, Frankfurt, S, and Kuijer, RG. Trajectories of posttraumatic growth and depreciation after two major earthquakes. Psychol Trauma. (2015) 7:112–21. doi: 10.1037/tra0000005
15. Kaleta, K, and Mróz, J. Posttraumatic growth and subjective well-being in men and women after divorce: the mediating and moderating roles of self-esteem. Int J Environ Res Public Health. (2023) 20:20. doi: 10.3390/ijerph20053864
16. Zhou, N, Yu, W, Tang, S, Wang, J, and Killikelly, C. Prolonged grief and post-traumatic growth after loss: latent class analysis. Psychiatry Res. (2018) 267:221–7. doi: 10.1016/j.psychres.2018.06.006
17. Davis, CG, Wohl, MJ, and Verberg, N. Profiles of posttraumatic growth following an unjust loss. Death Stud. (2007) 31:693–712. doi: 10.1080/07481180701490578
18. Nijdam, MJ, van der Meer, C, van Zuiden, M, Dashtgard, P, Medema, D, Qing, Y, et al. Turning wounds into wisdom: posttraumatic growth over the course of two types of trauma-focused psychotherapy in patients with PTSD. J Affect Disord. (2018) 227:424–31. doi: 10.1016/j.jad.2017.11.031
19. Park, SR, and Im, SY. Is posttraumatic growth helpful in overcoming mental health disorders due to COVID-19?: the moderating effect of posttraumatic growth in the relationship between COVID-19 and psychological health. Front Psychol. (2021) 12:773326. doi: 10.3389/fpsyg.2021.773326
20. Yasdiman, MB, Townsend, E, and Blackie, L. Examining the protective influence of posttraumatic growth on interpersonal suicide risk factors in a 6-week longitudinal study. Front Psychol. (2022) 13:998836. doi: 10.3389/fpsyg.2022.998836
21. Mostarac, I, and Brajković, L. Life after facing cancer: posttraumatic growth, meaning in life and life satisfaction. J Clin Psychol Med Settings. (2022) 29:92–102. doi: 10.1007/s10880-021-09786-0
22. Feng, LS, Dong, ZJ, Wu, XQ, Zhang, L, Yan, RY, Ma, J, et al. COVID-19-related post-traumatic growth in the general public: a cross-sectional study from Yunnan, China. Psychol Health Med. (2022) 27:925–30. doi: 10.1080/13548506.2021.1966700
23. Xu, Y, Yang, G, Liu, L, and Wu, X. The influence of deliberate rumination on the post-traumatic growth of college students during the COVID-19 pandemic and the moderating role of self-efficacy. Front Public Health. (2023) 11:1043402. doi: 10.3389/fpubh.2023.1043402
24. Yan, Z, Wenbin, J, Bohan, L, Qian, W, Qianqian, L, Ruting, G, et al. Post-traumatic growth trajectories among frontline healthcare workers during the COVID-19 pandemic: a three-wave follow-up study in mainland China. Front Psych. (2022) 13:945993. doi: 10.3389/fpsyt.2022.945993
25. Yeung, NC, Wong, EL, Cheung, AW, Leung, CS, Yeoh, EK, and Wong, SY. Finding the positives from the COVID-19 pandemic: factors associated with posttraumatic growth among nurses in Hong Kong. Eur J Psychotraumatol. (2022) 13:2005346. doi: 10.1080/20008198.2021.2005346
26. Cui, PP, Wang, PP, Wang, K, Ping, Z, Wang, P, and Chen, C. Post-traumatic growth and influencing factors among frontline nurses fighting against COVID-19. Occup Environ Med. (2021) 78:129–35. doi: 10.1136/oemed-2020-106540
27. O'Donovan, R, and Burke, J. Factors associated with Post-traumatic growth in healthcare professionals: a systematic review of the literature. Healthcare. (2022) 10:10. doi: 10.3390/healthcare10122524
28. Titlestad, KB, Kristensen, P, O'Connor, M, Hystad, S, and Dyregrov, K. Paths to positive growth in parents bereaved by drug-related death: a mixed-method study. Front Psychol. (2022) 13:982667. doi: 10.3389/fpsyg.2022.982667
29. Tedeschi, RG, and Calhoun, LG. TARGET ARTICLE: posttraumatic growth: conceptual foundations and empirical evidence. Psychol Inq. (2004) 15:1–18. doi: 10.1207/s15327965pli1501_01
30. Dominick, W. Changes in posttraumatic growth, core belief disruption, and social support over the first year of the COVID-19 pandemic. Front Psychol. (2022) 13:1019273. doi: 10.3389/fpsyg.2022.1019273
31. Zhou, AY, Hann, M, Panagioti, M, Patel, M, Agius, R, Van Tongeren, M, et al. Cross-sectional study exploring the association between stressors and burnout in junior doctors during the COVID-19 pandemic in the United Kingdom. J Occup Health. (2022) 64:e12311. doi: 10.1002/1348-9585.12311
32. Teo, I, Chay, J, Cheung, YB, Sung, SC, Tewani, KG, Yeo, LF, et al. Healthcare worker stress, anxiety and burnout during the COVID-19 pandemic in Singapore: a 6-month multi-Centre prospective study. PLoS One. (2021) 16:e0258866. doi: 10.1371/journal.pone.0258866
33. Groarke, A, Curtis, R, Groarke, JM, Hogan, MJ, Gibbons, A, and Kerin, M. Post-traumatic growth in breast cancer: how and when do distress and stress contribute. Psychooncology. (2017) 26:967–74. doi: 10.1002/pon.4243
34. Morrill, EF, Brewer, NT, O'Neill, SC, Lillie, SE, Dees, EC, Carey, LA, et al. The interaction of post-traumatic growth and post-traumatic stress symptoms in predicting depressive symptoms and quality of life. Psychooncology. (2008) 17:948–53. doi: 10.1002/pon.1313
35. Blom, DM, Sulkers, E, Post, WJ, Schroevers, MJ, and Ranchor, AV. Sub-groups (profiles) of individuals experiencing post-traumatic growth during the COVID-19 pandemic. Front Psychol. (2022) 13:969253. doi: 10.3389/fpsyg.2022.969253
36. Chen, R, Sun, C, Chen, JJ, Jen, HJ, Kang, XL, Kao, CC, et al. A large-scale survey on trauma, burnout, and posttraumatic growth among nurses during the COVID-19 pandemic. Int J Ment Health Nurs. (2021) 30:102–16. doi: 10.1111/inm.12796
37. Cann, A, Calhoun, LG, Tedeschi, RG, Taku, K, Vishnevsky, T, Triplett, KN, et al. A short form of the posttraumatic growth inventory. Anxiety Stress Coping. (2010) 23:127–37. doi: 10.1080/10615800903094273
38. Wu, X, Kaminga, AC, Dai, W, Deng, J, Wang, Z, Pan, X, et al. The prevalence of moderate-to-high posttraumatic growth: a systematic review and meta-analysis. J Affect Disord. (2019) 243:408–15. doi: 10.1016/j.jad.2018.09.023
39. West, CP, Dyrbye, LN, Sloan, JA, and Shanafelt, TD. Single item measures of emotional exhaustion and depersonalization are useful for assessing burnout in medical professionals. J Gen Intern Med. (2009) 24:1318–21. doi: 10.1007/s11606-009-1129-z
40. Van Wert, MJ, Gandhi, S, Gupta, I, Singh, A, Eid, SM, Haroon Burhanullah, M, et al. Healthcare worker mental health after the initial peak of the COVID-19 pandemic: a US medical Center cross-sectional survey. J Gen Intern Med. (2022) 37:1169–76. doi: 10.1007/s11606-021-07251-0
41. Cheng, Y, Wang, F, Zhang, L, Zhang, P, Ye, B, Sun, Y, et al. Effects of organisational and patient factors on doctors' burnout: a national survey in China. BMJ Open. (2019) 9:e024531. doi: 10.1136/bmjopen-2018-024531
42. Henry, JD, and Crawford, JR. The short-form version of the depression anxiety stress scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. (2005) 44:227–39. doi: 10.1348/014466505X29657
43. Guo, F, Han, R, Sun, Y, Sun, L, Luo, T, Zheng, L, et al. The associations between COVID-19 vaccination and psychological disorders among healthcare workers in China. J Affect Disord. (2022) 318:40–7. doi: 10.1016/j.jad.2022.08.080
44. Kroenke, K, Spitzer, RL, and Williams, JB. The patient health Questionnaire-2: validity of a two-item depression screener. Med Care. (2003) 41:1284–92. doi: 10.1097/01.MLR.0000093487.78664.3C
45. Yin, L, Teklu, S, Pham, H, Li, R, Tahir, P, and Garcia, ME. Validity of the Chinese language patient health questionnaire 2 and 9: a systematic review. Health Equity. (2022) 6:574–94. doi: 10.1089/heq.2022.0030
46. Löwe, B, Wahl, I, Rose, M, Spitzer, C, Glaesmer, H, Wingenfeld, K, et al. A 4-item measure of depression and anxiety: validation and standardization of the patient health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord. (2010) 122:86–95. doi: 10.1016/j.jad.2009.06.019
47. Luo, Z, Li, Y, Hou, Y, Zhang, H, Liu, X, Qian, X, et al. Adaptation of the two-item generalized anxiety disorder scale (GAD-2) to Chinese rural population: a validation study and meta-analysis. Gen Hosp Psychiatry. (2019) 60:50–6. doi: 10.1016/j.genhosppsych.2019.07.008
48. Vaishnavi, S, Connor, K, and Davidson, JR. An abbreviated version of the Connor-Davidson resilience scale (CD-RISC), the CD-RISC2: psychometric properties and applications in psychopharmacological trials. Psychiatry Res. (2007) 152:293–7. doi: 10.1016/j.psychres.2007.01.006
49. Zhang, X, Mo, Y, Yan, C, Li, Y, and Li, H. Psychometric properties of two abbreviated Connor-Davidson resilience scales in Chinese infertile couples. Qual Life Res. (2021) 30:2405–14. doi: 10.1007/s11136-021-02820-6
50. Kim, JH. Multicollinearity and misleading statistical results. Korean J Anesthesiol. (2019) 72:558–69. doi: 10.4097/kja.19087
51. Aggar, C, Samios, C, Penman, O, Whiteing, N, Massey, D, Rafferty, R, et al. The impact of COVID-19 pandemic-related stress experienced by Australian nurses. Int J Ment Health Nurs. (2022) 31:91–103. doi: 10.1111/inm.12938
52. Barnicot, K, McCabe, R, Bogosian, A, Papadopoulos, R, Crawford, M, Aitken, P, et al. Predictors of Post-traumatic growth in a sample of United Kingdom mental and community healthcare workers during the COVID-19 pandemic. Int J Environ Res Public Health. (2023) 20:20. doi: 10.3390/ijerph20043539
53. Aafjes-van Doorn, K, Békés, V, Luo, X, Prout, TA, and Hoffman, L. Therapists' resilience and posttraumatic growth during the COVID-19 pandemic. Psychol Trauma. (2022) 14:S165–73. doi: 10.1037/tra0001097
54. Zhou, X, and Wu, X. The relationship between rumination, posttraumatic stress disorder, and posttraumatic growth among Chinese adolescents after earthquake: a longitudinal study. J Affect Disord. (2016) 193:242–8. doi: 10.1016/j.jad.2015.12.076
55. Prekazi, L, Hajrullahu, V, Bahtiri, S, Kryeziu, B, Hyseni, B, Taganoviq, B, et al. The impact of coping skills in Post-traumatic growth of healthcare providers: when mental health is deteriorating due to COVID-19 pandemic. Front Psychol. (2021) 12:791568. doi: 10.3389/fpsyg.2021.791568
56. Cohen-Louck, K. Differences in post-traumatic growth: individual quarantine, COVID-19 duration and gender. Front Psychol. (2022) 13:920386. doi: 10.3389/fpsyg.2022.920386
57. Joseph, S, Murphy, D, and Regel, S. An affective-cognitive processing model of post-traumatic growth. Clin Psychol Psychother. (2012) 19:316–25. doi: 10.1002/cpp.1798
58. Prati, G, and Pietrantoni, L. Optimism, social support, and coping strategies as factors contributing to posttraumatic growth: a meta-analysis. J Loss Trauma. (2009) 14:364–88. doi: 10.1080/15325020902724271
59. Li, L, Mao, M, Wang, S, Yin, R, Yan, H, Jin, Y, et al. Posttraumatic growth in Chinese nurses and general public during the COVID-19 outbreak. Psychol Health Med. (2022) 27:301–11. doi: 10.1080/13548506.2021.1897148
60. Wolff, MB, O'Connor, PJ, Wilson, MG, and Gay, JL. Differences in work and non-work support associations with job stress, burnout, and well-being between types of healthcare workers. J Occup Environ Med. (2021) 63:e145–52. doi: 10.1097/JOM.0000000000002134
61. Wang, J, Yan, W, and Zhang, J. Relative income and subjective well-being of urban residents in China. J Fam Econ Iss. (2019) 40:673–80. doi: 10.1007/s10834-019-09636-0
62. Huang, L, Caspari, JH, Sun, X, Thai, J, Li, Y, Chen, FZ, et al. Risk and protective factors for burnout among physicians from standardized residency training programs in Shanghai: a cross-sectional study. BMC Health Serv Res. (2020) 20:965. doi: 10.1186/s12913-020-05816-z
63. Johannes, S, Dagmar, S, Tarani, C, Isabelle, G, Michael, M, Isabelle, N, et al. The measurement of effort-reward imbalance at work: European comparisons. Soc Sci Med. (2004) 58:1483–99. doi: 10.1016/S0277-9536(03)00351-4
64. Sun, X, Zhang, M, Lu, Z, Zhang, Z, Zheng, JC, Cheng, L, et al. Turnover intention and related factors among resident physicians in China under the standardised residency training programme: a cross-sectional survey. BMJ Open. (2022) 12:e061922. doi: 10.1136/bmjopen-2022-061922
65. Kwah, J, Weintraub, J, Fallar, R, and Ripp, J. The effect of burnout on medical errors and professionalism in first-year internal medicine residents. J Grad Med Educ. (2016) 8:597–600. doi: 10.4300/JGME-D-15-00457.1
66. West, CP, Dyrbye, LN, and Shanafelt, TD. Physician burnout: contributors, consequences and solutions. J Intern Med. (2018) 283:516–29. doi: 10.1111/joim.12752
67. Luo, C, Santos-Malave, G, Taku, K, Katz, C, and Yanagisawa, R. Post-traumatic growth and resilience among American medical students during the COVID-19 pandemic. Psychiatry Q. (2022) 93:599–612. doi: 10.1007/s11126-022-09981-8
68. Schroevers, MJ, Kraaij, V, and Garnefski, N. Cancer patients' experience of positive and negative changes due to the illness: relationships with psychological well-being, coping, and goal reengagement. Psychooncology. (2011) 20:165–72. doi: 10.1002/pon.1718
69. Liao, J, Ma, X, Gao, B, Zhang, M, Zhang, Y, Liu, M, et al. Psychological status of nursing survivors in China and its associated factors: 6 years after the 2008 Sichuan earthquake. Neuropsychiatr Dis Treat. (2019) 15:2301–11. doi: 10.2147/NDT.S203909
Keywords: China, COVID-19 pandemic, physicians, posttraumatic growth, standardized residency training program
Citation: Zeng Z, Wang H, Zhou Y, Lu Z, Ci R, Lin Y, Zeng X and Huang L (2023) The prevalence and factors associated with posttraumatic growth after 3-years outbreak of COVID-19 among resident physicians in China: a cross-sectional study. Front. Psychiatry. 14:1228259. doi: 10.3389/fpsyt.2023.1228259
Edited by:
Chong Chen, Yamaguchi University Graduate School of Medicine, JapanReviewed by:
Nitikorn Phoosuwan, Kasetsart University, ThailandPaweł Larionow, Kazimierz Wielki University, Poland
Florim Gallopeni, Heimerer College, Albania
Copyright © 2023 Zeng, Wang, Zhou, Lu, Ci, Lin, Zeng and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lei Huang, aHVhbmdsZWlAdG9uZ2ppLmVkdS5jbg==
 Zixuan Zeng
Zixuan Zeng Huan Wang
Huan Wang Yaxing Zhou3
Yaxing Zhou3 Yezhe Lin
Yezhe Lin Lei Huang
Lei Huang