- 1Clinical Psychology Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy
- 2Department of Psychiatry, Department of Neuroscience, Head, Neck and Thorax, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy
- 3NESMOS Department (Neurosciences, Mental Health, and Sensory Organs), University of Rome “La Sapienza”, Rome, Italy
- 4Catholic University of the Sacred Heart–Rome, Rome, Italy
- 5Center for Metacognitive Interpersonal Therapy, Turin, Italy
- 6Center for Metacognitive Interpersonal Therapy, Rome, Italy
- 7Department of Mental Health, Rome, Italy
- 8Pediatric Neuropsychiatry Unit, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome, Italy
- 9Institute of Psychiatry, Department of Neuroscience, Catholic University of the Sacred Heart–Rome, Rome, Italy
- 10Department of Life Sciences and Public Health Department, Catholic University of Sacred Heart, Rome, Italy
Introduction: Psychological distress may result in impairment and difficulty understanding oneself and others. Thus, addressing metacognitive issues in psychotherapy may improve psychopathology in adolescents and young adults (AYAs). We aimed to compare metacognitive interpersonal therapy (MIT)-informed psychotherapy with other treatment-as-usual (TAU) therapies.
Methods: We administered the Global Assessment of Functioning (GAF) scale, the Clinical Global Impressions–Severity (CGI-S) scale, and the Brief Psychiatric Rating Scale (BPRS) at baseline (BL) and at treatment termination (the endpoint was at 6 months and any last results obtained before that term were carried forward in analyzes). Patients received concomitant psychiatric and psychological treatment.
Results: Sixty AYAs were involved in the study. There was a significant reduction in symptomatology after the intervention. Twelve patients (17%) dropped out; treatment adherence was 83%. In the MIT group, 2 patients dropped out (11%), and in the TAU group, 9 patients dropped out (19%). All scales showed a significant reduction in symptoms between baseline (BL) and the 6-month endpoint: GAF (χ2 = 6.61, p < 0.001), BPRS (χ2 = 6.77, p < 0.001), and CGI (χ2 = 7.20, p < 0.001). There was a greater efficacy for the MIT group in terms of symptom reduction on the BPRS (t = 2.31; p < 0.05).
Conclusion: The study confirmed the efficacy of early and integrated care in adolescence and suggested greater symptom reduction for a psychotherapeutic intervention focused on stimulating mentalization skills. The study indicates the usefulness of this type of approach in the treatment of adolescent psychopathology. Due to the small sample size, the results need replication.
1. Introduction
The World Health Organization (WHO) (1) reported that 10–20% of children and adolescents had mental health problems prior to the COVID-19 outbreak. The onset of about half of mental disorders occurs within 14 years of age, with three-fourths having their onset before age 18 (2, 3). Generalized anxiety disorder and depression are the most common disorders (4), and their prevalence among young people has risen in the last 25 years (5). Depression and anxiety impact adolescent development negatively, including lower academic performance, school dropout, strained social relationships, increased risk of substance abuse, self-harm, and suicide (6–9).
The COVID-19 emergency caused a health alert and sudden changes in daily life and mental disorders (10–12). In children, depression and anxiety were among the most common mental disorders (13, 14). Young people suffer behavioral and emotional changes, such as sleep problems, phobias, increased drug and alcohol use, isolation, loss of interest, and irritability (15). Although in this study we will not focus on the effects of the pandemic on adolescent and young adult patients’ (AYA) treatment, the pandemic affected patient recruitment and service access. Several studies aimed to identify effective interventions suiting adolescents’ needs during the pandemic (16–21).
Greater accuracy and definition of care pathways would possibly combine emerging evidence with proven pharmacological (22, 23), psychotherapeutic (23–25), and combined interventions (26, 27).
Cognitive behavior therapy (CBT) is effective in treating anxiety and depression (28). However, outcomes are not yet entirely satisfactory, mainly due to high dropout and insufficient remission rates. Studies reported low response and premature psychotherapy termination, especially for adolescents with moderate to severe anxiety and depression. Concerning dropout, one study of 406 patients reported it to be 37% (29), a meta-analysis reported 23% (30), and other studies reported lower rates [12.2% (31)–13.3% (32)].
Another issue is remission. A meta-analysis of CBT in childhood and adolescence (28) showed remission to occur in only 53.2% of adolescents with depressive and 50.7% of adolescents with anxiety disorders. Against this background, current protocols clearly need improvement.
Since the capacity to reflect on mental states and use psychological knowledge for purposeful problem-solving is reduced in many patients, it is reasonable to consider it a relevant treatment target (33). One of the underlying reasons for adopting the metacognitive interpersonal therapy (MIT)-informed approach is that many adolescents have difficulties understanding and naming what they feel or considering their negative views about themselves and others are not matter of fact, but just ideas. As a consequence, psychotherapy with adolescents is likely to benefit from focusing on their capacity to understand mental states and use this knowledge adaptively.
Several studies showed that skills related to metacognition (33, 34) and mentalizing (35) are important in helping adolescents to understand themselves and others. Mentalization is the ability to think and reflect on one’s own experiences and formulate interpretations of one’s and others’ behavior (33, 36). It involves socio-cognitive functions, including the recognition of emotions, theory of mind, mind-reading, and reflective function (37).
In adolescents with borderline (confused mentalizing) and narcissistic (excessive certainty about others’ mental states) personality traits, abnormal mentalizing was found to mediate the effects of adverse childhood experiences on their development (38).
Poor metacognition was found in various mental conditions (39–41), and significant increases in adolescents’ metacognitive abilities were observed after completing MIT (42, 43). An intervention that combines symptom-focused work with MIT (42–44) holds promise to improve treatment adherence and outcomes in adolescents with a wide array of symptoms and behavioral problems.
MIT for adults with personality disorders (PDs) has received empirical support from a series of case studies (45–47), pilot non-controlled studies (48), and randomized controlled trials (RCTs) (48). In adolescence, it has been successfully applied in early psychosis (41) and an RCT of adolescents with avoidant PD. (49) MIT combined with mentalization-based treatment improved outcomes and was associated with low dropout rates in avoidant PD. (50) Some aspects of MIT were included in a DBT-based protocol for PD requiring hospitalization; results were satisfactory (51). An RCT of group-MIT for PDs obtained large effect sizes for the MIT vs. treatment-as-usual (TAU) group on alexithymia, mastery, and self- and other-related metacognition (48). A pilot non-inferiority RCT of metacognitive and compassion treatment vs. CBT + medication for schizotypal PD yielded larger reductions in general symptomatology (η2 = 0.558) and larger increases in metacognition (η2 = 0.734) in the experimental group vs. CBT + medication (52). Overall, MIT has shown effectiveness on symptoms and social dysfunctions.
The current preliminary observational study aimed to examine treatment adherence, safety, and efficacy of MIT treatment in adolescents. To meet this goal, we compared the outcomes of an AYA group with anxiety and/or depressive disorders receiving MIT therapy with another receiving TAU (consisting of other psychotherapies not focused on metacognition but well-established in our service).
Here, we tested whether the group receiving MIT-informed psychotherapy, i.e., a combination of symptom work promoting metacognition and counteracting maladaptive interpersonal schemas was able to (a) guarantee treatment adherence as assessed with a number of dropouts; (b) be effective in terms of global psychopathology and functioning. We compared the group receiving MIT-informed therapy with TAU as routinely delivered in our unit.
2. Methods
2.1. Study design and procedure
This study was a longitudinal, prospective, naturalistic, observational study, conducted in a hospital psychiatric service dedicated to Adolescents and Young Adults (AYA). The Fondazione Policlinico Universitario A. Gemelli IRCCS ‘Early Intervention for Adolescents and Young Adults’ service provides outpatient visits and day-hospital admissions. Help-seeking patients were referred by external practitioners and other institutions. They were visited by psychiatrists of the AYA service, who assessed them in terms of diagnosis and study eligibility. Either patients or, if underage, their parents or legal tutors received adequate information regarding study aims and procedures and provided consent to participate. They were informed they could receive 16–24 weekly sessions of individual psychotherapy (but at least 8 sessions were required for being included in the study), each lasting 50 min, along with the possibility of receiving pharmacotherapy. The total duration of psychotherapy could vary from 2 to 6 months. Patients who adhered to the study received baseline assessment by their treating psychiatrists and were introduced to their psychotherapists. Treatments started within 2 weeks after assessment. The assessment carried out at baseline was repeated at the end of treatment. When this occurred earlier than the 6-month endpoint, results were carried forward for statistical purposes.
Psychotherapy could be carried out at AYA service, but patients could opt for private psychotherapy.
2.2. Participants
Patients referred to the service from May 2020 to March 2022 (which happened to be during the COVID-19 pandemic) were screened for eligibility. Participants had to be at least moderately proficient in Italian. Among the 111 patients screened, 60 (54%) met inclusion criteria and completed baseline and endpoint assessments. Recruitment implied assignment to MIT or TAU on the basis of patient preference and therapist availability, with both treatments being presented as potentially equivalent and no effort being made to persuade patients (or their legal tutors/parents, if patients were not of legal age) to prefer one or another. Hence, any difference that might arise in sociodemographic parameters between MIT and TAU would only be attributed to chance.
2.3. Exclusion criteria
Exclusion criteria were the presence of severe systemic diseases, intellectual disability or borderline functioning, psychosis, psychoactive substance use or severe eating disorders needing inpatient treatment, traumatic cranial injury, severe neurological disorders, failure to provide informed consent, and current or past psychotherapy experience. Patients were free to withdraw consent at any moment. Those withdrawing consent were instantly assessed upon withdrawal, and their results were carried forward in the analyzes. Patients who failed to initiate treatment within 2 weeks from baseline and patients/parents who refused treatment or participation in the study were excluded.
2.4. Assessments and outcome measures
A baseline assessment was conducted at the first visit. Endpoint assessment was set at 6 months after baseline; when assessments were made before this term, they were carried forward to the endpoint. Patients’ developmental and family histories were investigated at baseline with a semi-structured interview. Primary outcomes were the reduction of psychometric scale scores and the increase in the functioning assessment.
The Global Assessment of Functioning (GAF) scale (53) rates social, occupational, and psychological functioning. Scores range from 1 (“severely impaired”) to 100 (“extremely high functioning”). In this study, we used the Italian version of the scale included in the DSM-IV-TR (54), which showed good psychometric properties in Italian populations of adolescents and young adults (55, 56). Cronbach’s alpha was found to be 0.74, indicating good reliability (57).
Clinical Global Impression–Severity (CGI-S) scale (58) is a frequently used 7-point Likert scale (59). Higher scores indicate worse psychopathology. CGI-S measures the severity of patients’ illness and its improvement over treatment. Cronbach’s alpha was 0.998, which indicates excellent reliability (60).
Brief Psychiatric Rating Scale (BPRS) is a 7-point Likert scale (plus the option of considering an item not rated) used in order to assess the level of general psychopathology around a broad range of symptoms. A higher score indicates more severe psychopathology. It has been consistently used also as a measure of treatment change (61). The purpose of BPRS is to broaden the symptom spectrum investigated, for a psychopathological profile definition (62). Cronbach’s alpha was found to be 0.87, indicating good reliability (63).
A response was considered an at least 50% decrease from the baseline of BPRS scores, and at least a 2-point drop from baseline on the CGI-S or a CGI-S score of ≤3, while a score of 1 or 2 on the CGI-S was considered a remission.
2.5. Interventions
2.5.1. Metacognitive interpersonal therapy
MIT aims to help patients improve their ability to understand their mental states, so they become a ground for more adaptive strategies to deal with symptoms and improve social functioning. Maladaptive interpersonal schemas encompass images of self and self-with-other and are common in PDs. They include negative core self-images (“I am unlovable” or “I have no value”) and reactions to others, e.g.: “if I express my need to be appreciated, the other person will be critical, and I will become sad, confirming my idea of having no value.” From early MIT stages, therapists help patients become aware of the schemas that guide them, gain distance from their underlying negative self-images, and promote initial access to more benevolent representations of self and others. In the manualized form applied here (43), MIT-informed treatment included a joint formulation of shared goals, helping patients recognize and pursue their needs/desires for attachment, appreciation, exploration, and group inclusion (42, 43). MIT-informed psychotherapy attempted to engage adolescents in practices such as guided imagery, chairwork, bodywork (64), and role-playing to encourage their involvement in activities, aimed at modifying their maladaptive schemata and creating new ways to derive meaning from social interactions.
Importantly, during this protocol, MIT-informed treatment included symptom-specific, empirically supported techniques, e.g., behavioral activation for depression or graded exposure to different forms of anxiety (42). One MIT-certified therapist with 1-year MIT experience treated all MIT-informed patients and received 1-h supervision fortnightly by one of the MIT developers.
2.5.2. Treatment-as-usual (TAU)
The control group received TAU that consisted of individual psychotherapy delivered according to practitioners’ preferred orientation, mostly psychoanalytic/psychodynamic. Most psychotherapists conducting TAU had a psychoanalytic/psychodynamic orientation and were supervised by senior colleagues.
2.5.3. Patient assignment to groups
All patients were offered integrated multidisciplinary care. Patients were assigned to MIT or TAU according to their preference and therapist availability. All patients who started psychotherapy received sufficient information about both types of therapeutic approaches and additional information about the psychotherapy they chose. In some cases, psychological therapy and medication were administered together, while in other cases, patients refrained from taking medication or they dropped out of therapy immediately and were not included in the MIT-TAU comparison. Three patients later dropped out, one from MIT and two from TAU. Psychotherapy sessions at the service’s premises or in private locations lasted 50 min each. At least eight sessions were required to include the patient in data analysis; assessments were processed through the last observation carried forward (LOCF) method.
2.5.4. Other interventions
Concurrent psychiatric counseling was delivered in order to evaluate the need for medication or dose changes for some participants. Psychiatric visits (not psychotherapy sessions) were scheduled weekly for 2 weeks, then monthly for another two visits, and then bi-monthly. Visits were scheduled based on the patient’s clinical conditions and in agreement with the patient/family, but other visits could be added at patients’/tutors’ requests. Parents in both groups of patients were offered family or couple psychotherapy delivered by therapists working in the community.
2.6. Safety assessment
We assessed safety with spontaneous reporting of adverse events weekly. The caring physicians filled in a list of possible adverse events, especially focusing on the common side effects of medications used in this study, but also including items on suicidal thinking and attempts, self-harm ideation, and acts. These were labeled “severe,” “moderate,” or “mild.” Participants were not provided with the list to avoid being overconcerned about adverse events and being influenced in their perceptions. Safety data collection was identical for the two groups.
2.6.1. Ethics statement
The study was approved by the ethics committee of Fondazione Policlinico Universitario A. Gemelli IRCCS, ID 5025 Prot. N 0020268/22 of June 14, 2022. All patients and parents were informed and signed informed consent.
2.7. Statistical analyses
We performed descriptive statistics to assess the sample age, sex, psychopathological diagnosis, drug therapy, and type of psychotherapeutic delivered. For the main study variables, the observed median, mean, and standard deviation were calculated. Primary outcome measures were pre–post GAF, BPRS, and CGI changes. To test sample normality of distribution, we used the Shapiro–Francia and Anderson–Darling tests that yielded W′ = 0.977 (p = 0.037) and W 0.766 (p = 0.045), respectively, both ruling out normality. Hence, we turned to non-parametric tests. To analyze overall treatment response (changes in symptoms and functioning over time), we conducted non-parametric repeated-measures ANOVA. Spearman’s correlations between the scores of the 3 scales were analyzed in the two-time measures. To compare groups of patients who had undergone different types of psychotherapy, we used the repeated-measures ANOVA and post-hoc t-test. Statistical analysis was performed using the R 4.1 version (65). p-values were two-tailed; statistical significance was set at p < 0.05.
3. Results
Participants were in the age range of 13–23 years. Supplementary Figure S1 shows the flowchart of participants throughout the study. The total sample (mean age 16.7 ± 2.59) consisted of 40 female participants (66.67%) and 20 male participants (33.33%). In total, 30 participants were diagnosed with mood disorders (50%), including 13 with depressive disorders and 17 with bipolar disorders; 15 (25%) had anxiety disorders; 5 (8%) had diagnosed adjustment disorder; 4 (7%) had disruptive, impulse-control, and conduct disorders; 3 (5%) had non-underweight eating disorders; and 3 (5%) had diagnosed obsessive-compulsive disorder. Table 1 illustrates demographic characteristics, baseline tests, and between-group differences, suicidal, and self-harm symptoms.
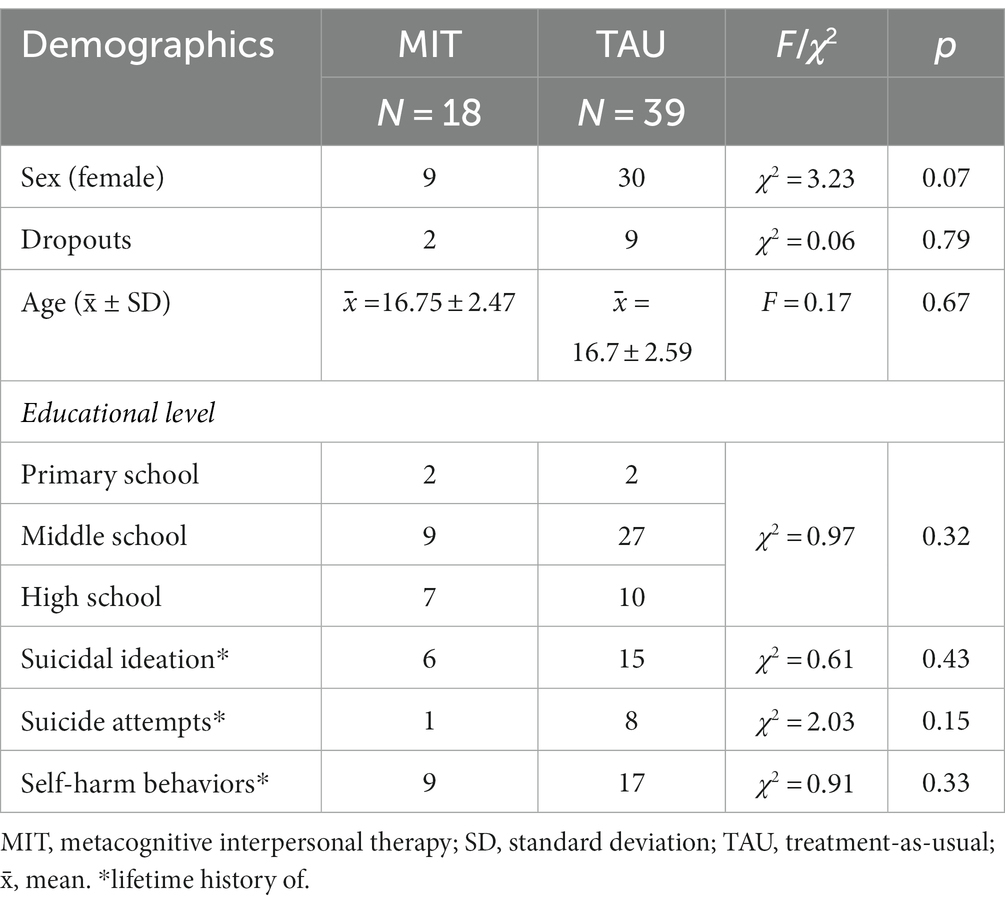
Table 1. Sociodemographic characteristics of our sample subdivided according to the treatment received.
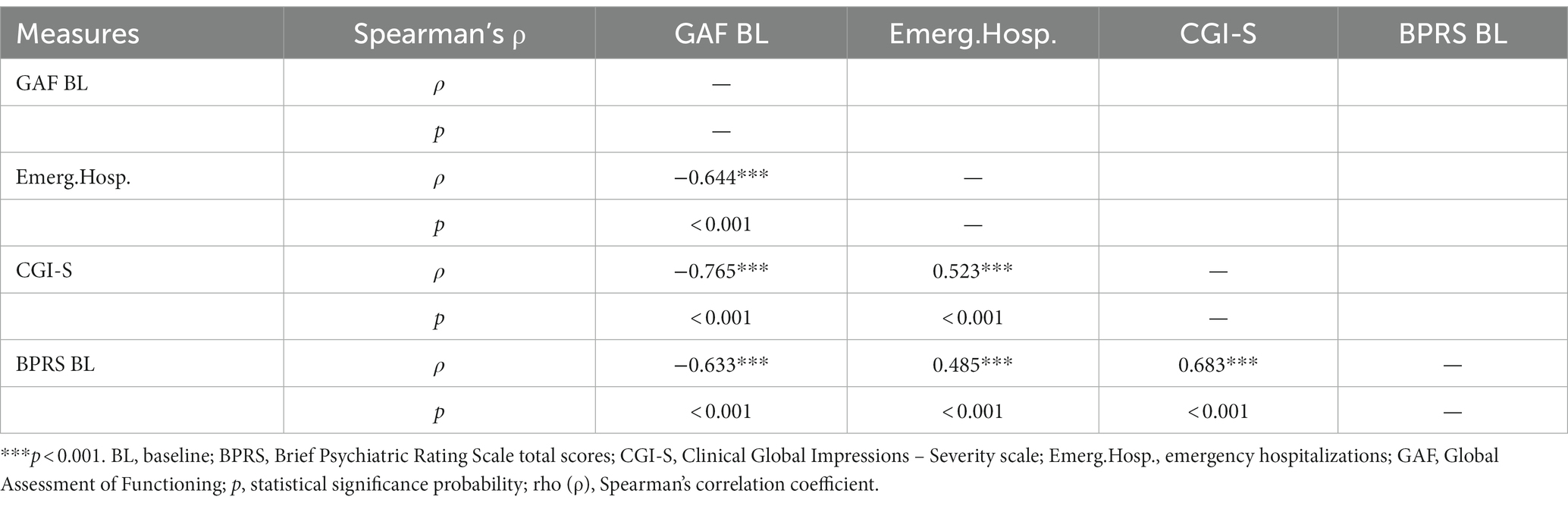
All participants were born in Italy; 27% (n = 16) were second-generation immigrants and had at least one parent born in a foreign country. No significant baseline differences were found regarding all variables. Spearman matrix correlations between scores on the psychometric scales (GAF, CGI, and BPRS) and a high number of emergency unit access confirmed that the instruments were capable of detecting the severity of patients’ symptoms (Table 2).
Descriptive and statistical analyzes were carried out to assess whether MIT was feasible in terms of adherence and preliminary outcomes vs. TAU. We describe first the results at the level of the total sample, and then, we compare those who received MIT (n = 18) with those undergoing TAU (n = 39). Participants (n = 3) who refused psychotherapy were excluded from these analyzes.
As regards overall intervention adherence, 12 patients (17%) dropped out. There were 2 patients in the MIT group (11%) and nine patients (19%) in the TAU group. Concerning overall treatment response, repeated-measures ANOVA (non-parametric) was performed to assess changes in symptoms and functioning over time: GAF BL vs. GAF at the 6-month endpoint (<χ2 = 6.61, p < 0.001), BPRS BL vs. BPRS at the 6-month endpoint (χ2 = 6.77, p < 0.001), and CGI BL vs. CGI at the 6-month endpoint (χ2 = 7.20, p < 0.001). All differences in psychometric scores from baseline to the 6-month endpoint were significant and in the improvement direction in all groups. Scores on psychometric scales are shown in Table 3.
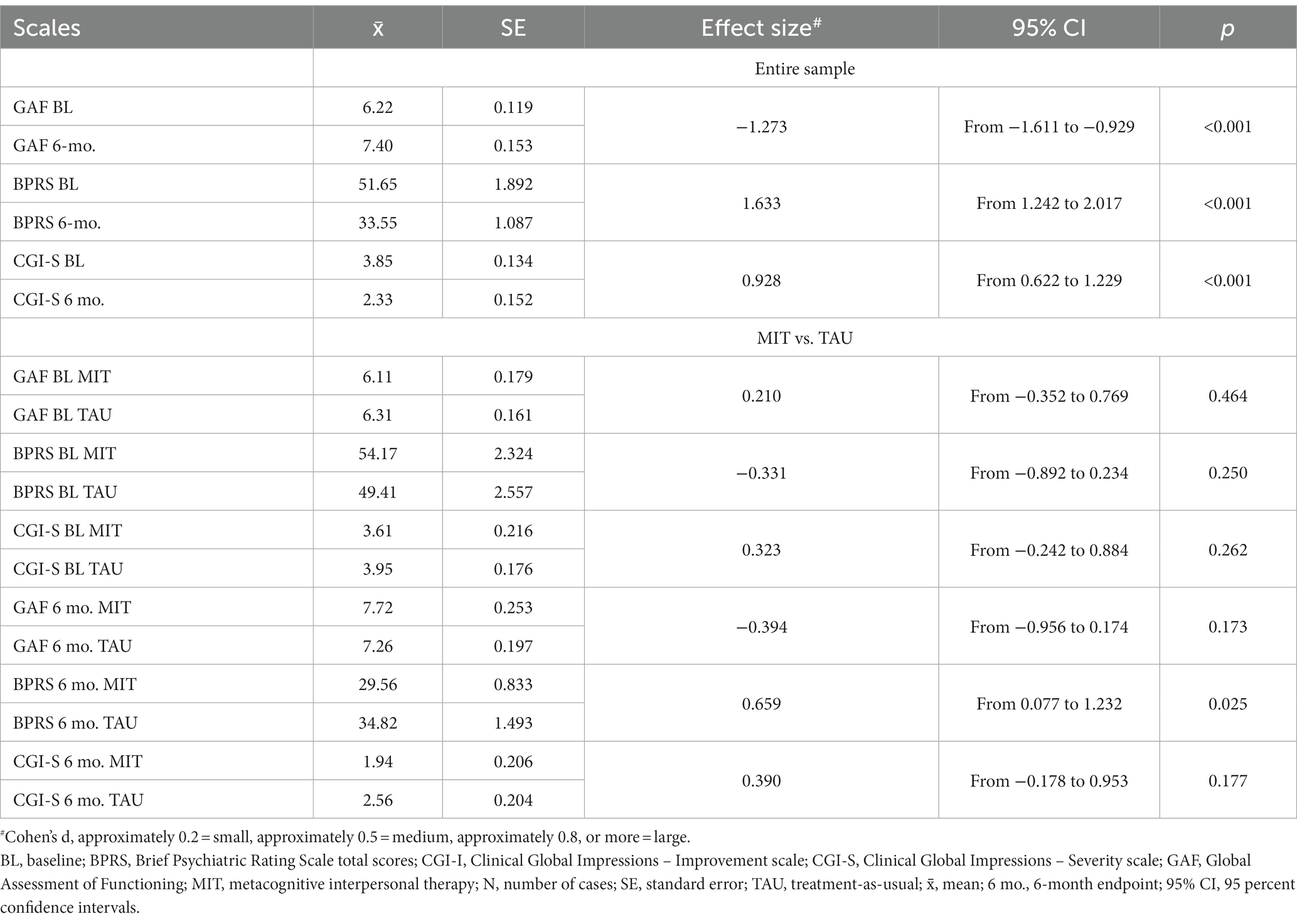
Table 3. Scores on the psychometric scales at baseline and 6-month endpoint of the entire sample (N = 60) and of the sample subdivided according to psychotherapy received [MIT (n = 18) vs. TAU (n = 39)].
Of the 18 MIT patients, 4 were responders according to the at least 50% drop of BPRS scores from baseline (vs. 1 of the 38 TAU patients, χ2 = 5.765; p = 0.016, χ2 = 3.607 after Yates’ correction, p = 0.057, not significant [ns]) and 17 were responders according to the CGI-S ≥ 2-point drop from baseline or a final score of ≤3 criterion (vs. 27 of TAU patients, χ2 = 3.969; p = 0.046, χ2 = 2.702 after Yates’ correction, p = 0.100, ns). All comparisons favored MIT. According to the final CGI-S score of 1 or 2 criteria, there were 10 remitters in the MIT group vs. 21 remitters in the TAU group (χ2 = 0.0004; p = 0.98, ns).
In the entire group of treated AYAs, the effect size was very large for the BPRS (Cohen’s d = 1.515, Hedges’ g = 1.515) and for the CGI-S (Cohen’s d = 1.209, Hedges’ g = 1.209). For the individual groups, effect sizes were very large (“huge” according to Sawilowsky, Cohen’s d and Hedges’ g = 3.3236) for the BPRS and very large for the CGI-S (Cohen’s d and Hedges’ g = 1.518) in the MIT group, while in the TAU group, the effect sizes were large (Cohen’s d and Hedges’ g = 1.125) for the BPRS and also for the CGI-S (Cohen’s d and Hedges’ g = 1.132).
As regards MIT vs. TAU, we compared outcome results on the GAF scale, BPRS, and CGI scale (BL to 6 months). On the GAF scale, the increase for the MIT group was greater than for the TAU group, F = 6.73, p = 0.01. Moreover, on the BPRS, MIT was superior to TAU, F = 11.8, p = 0.001 (Figure 1).

Figure 1. Comparison of the MIT and TAU groups as concerns the baseline–6-month comparison of BPRS scores.
Concerning the CGI-S, the difference between MIT and TAU, although present, did not reach statistical significance. The t-test post-hoc analysis confirmed a significant difference between MIT and TAU after 6 months of treatment on the BPRS (t = 2.31; p < 0.05). Differences on the CGI scale did not reach significance. Separate scores by MIT and TAU groups are shown in Table 3.
3.1. Safety issues
Adverse events did not differ between MIT and TAU. None of the adverse events was rated “severe”; there were only three mild and transient events in the MIT group (two headaches and one gastrointestinal upset) and six in the TAU group (two headaches, two constipation, one nausea, and one vomiting). No patient developed suicidal or self-harming thinking or committed attempts or self-cutting.
4. Discussion
In this study, we obtained satisfactory efficacy and safety, in terms of psychometric scale drops from baseline, as well as high adherence to treatment and a low dropout rate (18.33%) in the entire group of AYA. However, MIT-informed psychotherapy was associated with a lower dropout rate than TAU (11.11% vs. 23.08%), but also lower than most dropout rates reported in literature. Both treatments proved to be efficacious, but MIT-informed psychotherapy superseded TAU on the BPRS, although not on the CGI-S.
AYA mental health services often manage symptomatologically variable and complex patients (1, 16). The importance of multidisciplinary care is now recognized in these settings (57). The present study reflects a currently growing trend in the literature to conduct studies on identifying effective psychotherapeutic interventions in AYA populations (18, 19). Treating adolescents with more effective methods is currently important, due to the general increase in global individual suffering (66). Furthermore, this population has been given particular attention after the pandemic event (10–12) due to the higher impact of the restrictions compared with other age ranges (67). The increased recognition that psychopathology in the general population received [due to a purported stress-related increased occurrence of mental disorders (68)] prompted the establishment and spread of early intervention services throughout the world (69), aiming at preventing the development of severe mental conditions or reducing the onset-detection and treatment interval. Our study carried out in a dedicated adolescent mental health service active during the pandemic involved 60 adolescents who deserved clinical attention and associated pharmacological and psychotherapeutic treatment. Obviously, psychiatric evaluation to initiate the patient to possible pharmacological (22, 23) or combined (26, 27) interventions, remains central in the psychotherapeutic intake. Overall, the study showed good efficacy of integrated care at 6-month follow-up. From this perspective, it seems interesting to explore therapeutic approaches that consider prerequisites related to knowledge of self and others’ mental states that are effective in counteracting maladaptive interpersonal patterns, which are typical of PDs (70). Among these, MIT is particularly focused on the ability to make sense of one’s own mental states and those of others. Theoretically, this approach, when provided early, could increase emotional awareness in AYAs with psychiatric symptomatology, thus allowing them to provide meaning to their emotional experience and experience and manage interpersonal relationships. This could increase the general psychological wellbeing of young people and consequently affect the reduction of anxiety-depressive psychopathology, which is very common in the AYA population (22–24). This preliminary naturalistic study showed a low dropout rate and good efficacy in patients with various psychiatric symptoms who received MIT-informed psychotherapy.
Metacognitive interpersonal therapy (MIT) (42–44) is in fact a treatment directed at increasing awareness of mental states and becoming aware of maladaptive interpersonal patterns. This treatment is applied along with empirically supported CBT techniques to promote symptom management. In our study, MIT was compared with routinely administered TAU in our unit. Consistent with previous studies (41, 47, 48, 71, 72), the results of MIT-informed psychotherapy confirmed low absolute dropout rates and higher efficacy and lower dropout compared with TAU, as well as lower dropout than other studies in the literature. Regarding efficacy, the results were good and significantly superior to TAU in terms of both symptoms and functioning; the only scale that did not reach significance was CGI.
Both treatments were safe, with only mild and transient adverse events developing in 3 patients of the MIT groups and in 5 patients of the TAU group (one patient in this group developed two symptoms). The large to very large effect sizes we observed in both groups and the entire sample indicate that help-seeking AYAs benefitted from psychotherapy.
4.1. Limitations
Our study confirmed previously obtained results of MIT in AYAs (41, 48, 72) but had limitations. The sample size was low and diagnostically heterogeneous to prevent us from accurately identifying and quantifying which symptoms responded to treatment. We did not assess PDs or measure metacognition using a valid scale, which constitutes the main target of MIT-informed psychotherapy. Female participants were twice as many as males. However, despite few studies reported better psychotherapy outcomes in the female sex (73, 74), others found no sex-based differences (75), and in any case, as the sex distribution in our sample did not differ significantly between MIT and TAU, it is unlikely that our results could be affected by a gender bias. Half of our sample consisted of patients with mood disorders; this probably does not reflect the proportions found in the general adolescent population (76). Furthermore, parents in both groups of patients were encouraged to consult relational psychotherapists in the community, who provided them with couple or family therapy. The progress made by parents could have affected the responses of their children to both MIT and TAU. The possible effect of the psychological adaptation of one family member on other family members’ psychological status could not be explored with this design, but it would need a design where parents of one group were exposed to relational psychotherapy and parents of another were not. This should be controlled in future studies. However, in this study, taking into account that parent psychotherapy could affect children’s outcomes and responses, these could not be affected differentially in the two groups as parents from both groups all accepted to endorse couple or family therapy. Future studies should focus on MIT-informed psychotherapy in comparison with other CBT techniques or with individual standardized psychodynamically informed psychotherapies.
In spite of the above limitations, our naturalistic study suggests that MIT is a promising treatment with the potential to help adolescents with mental health problems reduce their suffering and find their way in social life.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Fondazione Policlinico A. Gemelli IRCCS, Catholic University of Sacred Heart, Rome, Italy. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin.
Author contributions
EM, LM, GF, and DC conceived the study. EM, LM, GF, DJ, VZ, DV, and MS were engaged in the clinical activities of the study patient population. DJ, VZ, DV, MS, and SP directed and conducted the data collection. EM, LM, SP, and GK organized and collected the material and wrote the first draft of the manuscript. EP, GD, and RP performed literature searches. EM, LM, GF, FM, and GK wrote the Methods and decided eligibility criteria. DC, GK, RP, and GD supervised the writing of the manuscript. DC, CV, GK, and GS revised the final version of the manuscript. All authors contributed to the writing of the manuscript, read, and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1221158/full#supplementary-material
References
1. World Health Organization. Global diffusion of eHealth: Making universal health coverage achievable: Report of the third global survey on eHealth. Geneva: World Health Organization (2016).
2. Kessler, RC, Merikangas, KR, and Wang, PS. Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the twenty-first century. Annu Rev Clin Psychol. (2007) 3:137–58. doi: 10.1146/annurev.clinpsy.3.022806.091444
3. Kim-Cohen, J, Caspi, A, Moffitt, TE, Harrington, H, Milne, BJ, and Poulton, R. Prior juvenile diagnoses in adults with mental disorder: developmental follow-back of a prospective-longitudinal cohort. Arch Gen Psychiatry. (2003) 60:709–17. doi: 10.1001/archpsyc.60.7.709
4. Stansfeld, S, Clark, C, Bebbington, P, King, M, Jenkins, R, and Hinchliffe, S. Common mental disorders In: S McManus, P Bebbington, R Jenkins, and T Brugha, editors. Mental health and wellbeing in England: Adult psychiatric morbidity survey 2014. Leeds: NHS Digital (2016)
5. Royal Society for Public Health. Royal Society for public health and young health movement. #StatusOfMind. Social media and young people’s mental health and wellbeing. London, UK: Royal Society for Public Health (2017).
6. Copeland, WE, Angold, A, Shanahan, L, and Costello, EJ. Longitudinal patterns of anxiety from childhood to adulthood: the Great Smoky Mountains study. J Am Acad Child Adolesc Psychiatry. (2014) 53:21–33. doi: 10.1016/j.jaac.2013.09.017
7. Gore, FM, Bloem, PJ, Patton, GC, Ferguson, J, Joseph, V, Coffey, C, et al. Global burden of disease in young people aged 10-24 years: a systematic analysis. Lancet. (2011) 377:2093–102. doi: 10.1016/S0140-6736(11)60512-6
8. Hetrick, SE, Cox, GR, Witt, KG, Bir, JJ, and Merry, SN. Cognitive behavioural therapy (CBT), third-wave CBT and interpersonal therapy (IPT) based interventions for preventing depression in children and adolescents. Cochrane Database Syst Rev. (2016) 8:CD003380. doi: 10.1002/14651858.CD003380.pub4
9. Morgan, PL, Farkas, G, Hillemeier, MM, and Maczuga, S. Replicated evidence of racial and ethnic disparities in disability identification in US schools. Educ Res. (2017) 46:305–22. doi: 10.3102/0013189X17726282
10. Vigo, D, Patten, S, Pajer, K, Krausz, M, Taylor, S, Rush, B, et al. Mental health of communities during the COVID-19 pandemic. Can J Psychiatr. (2020) 65:681–7. doi: 10.1177/0706743720926676
11. Lessard, LM, and Puhl, RM. Adolescent academic worries amid COVID-19 and perspectives on pandemic-related changes in teacher and peer relations. Sch Psychol. (2021) 36:285–92. doi: 10.1037/spq0000443
12. World Health Organization. Disability inclusion in health responses to COVID-19 in the eastern Mediterranean region: Results of a rapid assessment. Geneva, CH: World Health Organization (2022).
13. Breaux, R, Dvorsky, MR, Marsh, NP, Green, CD, Cash, AR, Shroff, DM, et al. Prospective impact of COVID-19 on mental health functioning in adolescents with and without ADHD: protective role of emotion regulation abilities. J Child Psychol Psychiatry. (2021) 62:1132–9. doi: 10.1111/jcpp.13382
14. Murata, S, Rezeppa, T, Thoma, B, Marengo, L, Krancevich, K, Chiyka, E, et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. (2021) 38:233–46. doi: 10.1002/da.23120
15. Manzar, MD, Albougami, A, Usman, N, and Mamun, MA. Suicide among adolescents and youths during the COVID-19 pandemic lockdowns: a press media reports-based exploratory study. J Child Adolesc Psychiatr Nurs. (2021) 34:139–46. doi: 10.1111/jcap.12313
16. Courtney, D, Watson, P, Battaglia, M, Mulsant, BH, and Szatmari, P. COVID-19 impacts on child and youth anxiety and depression: challenges and opportunities. Can J Psychiatr. (2020) 65:688–91. doi: 10.1177/0706743720935646
17. Garcia, I, and O’Neil, J. Anxiety in adolescents. Nurse Pract. (2021) 17:49–53. doi: 10.1016/j.nurpra.2020.08.021
18. Krause, K, Midgley, N, Edbrooke-Childs, J, and Wolpert, M. A comprehensive mapping of outcomes following psychotherapy for adolescent depression: the perspectives of young people, their parents and therapists. Eur Child Adolesc Psychiatry. (2021) 30:1779–91. doi: 10.1007/s00787-020-01648-8
19. Bahji, A, Pierce, M, Wong, J, Roberge, JN, Ortega, I, and Patten, S. Comparative efficacy and acceptability of psychotherapies for self-harm and suicidal behavior among children and adolescents: a systematic review and network meta-analysis. JAMA Netw Open. (2021) 4:e216614. doi: 10.1001/jamanetworkopen.2021.6614
20. Berny, LM, and Tanner-Smith, EE. Differential predictors of suicidal ideation and suicide attempts: internalizing disorders and substance use in a clinical sample of adolescents. J Dual Diagn. (2022) 18:59–69. doi: 10.1080/15504263.2021.2016343
21. Morese, R, Palermo, S, Torello, C, and Sechi, F. Social withdrawal and mental health: an interdisciplinary approach In: R Morese, S Palermo, and R Fiorella, editors. Social isolation - an interdisciplinary view. London, UK: IntechOpen Ltd. (2020)
22. Carr, V, and Boyd, C. Efficacy of treatments for depression in children and adolescents. Behav Change. (2003) 20:103–8. doi: 10.1375/bech.20.2.103.24842
23. Michael, KD, and Crowley, SL. How effective are treatments for child and adolescent depression? Clin Psychol Rev. (2002) 22:247–69. doi: 10.1016/s0272-7358(01)00089-7
24. Berryhill, B, Carlson, C, Hopson, L, Culmer, N, and Williams, N. Adolescent depression and anxiety treatment in rural schools: a systematic review. J Rural Ment Health. (2022) 46:13. doi: 10.1037/rmh0000183
25. Vitiello, B, Correll, C, Van Zwieten-Boot, B, Zuddas, A, Parellada, M, and Arango, C. Antipsychotics in children and adolescents: increasing use, evidence for efficacy and safety concerns. Eur Neuropsychopharmacol. (2009) 19:629–35. doi: 10.1016/j.euroneuro.2009.04.008
26. Brent, D, Emslie, G, Clarke, G, Wagner, KD, Asarnow, JR, Keller, M, et al. Switching to another SSRI or to venlafaxine with or without cognitive behavioral therapy for adolescents with SSRI-resistant depression: the TORDIA randomized controlled trial. JAMA. (2008) 299:901–13. doi: 10.1001/jama.299.8.901
27. Zhou, Y, Wang, W, Sun, Y, Qian, W, Liu, Z, Wang, R, et al. The prevalence and risk factors of psychological disturbances of frontline medical staff in China under the COVID-19 epidemic: workload should be concerned. J Affect Disord. (2020) 277:510–4. doi: 10.1016/j.jad.2020.08.059
28. Wergeland, GJ, Riise, EN, and Öst, LG. Cognitive behavior therapy for internalizing disorders in children and adolescents in routine clinical care: a systematic review and meta-analysis. Clin Psychol Rev. (2021) 83:101918. doi: 10.1016/j.cpr.2020.101918
29. Goodyear, RK, Wampold, BE, Tracey, TJ, and Lichtenberg, JW. Psychotherapy expertise should mean superior outcomes and demonstrable improvement over time. Counsel Psychol. (2017) 45:54–65. doi: 10.1177/0011000016652691
30. Rohden, AI, Benchaya, MC, Camargo, RS, Moreira, TC, Barros, HMT, and Ferigolo, M. Dropout prevalence and associated factors in randomized clinical trials of adolescents treated for depression: systematic review and meta-analysis. Clin Ther. (2017) 39:971–92.e4. doi: 10.1016/j.clinthera.2017.03.017
31. Butollo, W, Karl, R, König, J, and Rosner, R. A randomized controlled clinical trial of dialogical exposure therapy versus cognitive processing therapy for adult outpatients suffering from PTSD after type I trauma in adulthood. Psychother Psychosom. (2016) 85:16–26. doi: 10.1159/000440726
32. Skar, AS, Braathu, N, Jensen, TK, and Ormhaug, SM. Predictors of nonresponse and drop-out among children and adolescents receiving TF-CBT: investigation of client-, therapist-, and implementation factors. BMC Health Serv Res. (2022) 22:1212. doi: 10.1186/s12913-022-08497-y
33. Semerari, A, Carcione, A, Dimaggio, G, Falcone, M, Nicolò, G, Procacci, M, et al. How to evaluate metacognitive functioning in psychotherapy? The metacognition assessment scale and its applications. Clin Psychol Psychother. (2003) 10:238–61. doi: 10.1002/cpp.362
34. Lysaker, PH, and Lysaker, JT. Disturbances in dialogue and metacognition: a renewed way to understand and respond to alterations in self-experience in psychosis. Theory Psychol. (2021) 31:335–54. doi: 10.1177/0959354320973752
35. Fonagy, P, and Target, M. Early intervention and the development of self-regulation. Psychoanal Inq. (2002) 22:307–35. doi: 10.1080/07351692209348990
36. Lysaker, PH, and Dimaggio, G. Metacognitive capacities for reflection in schizophrenia: implications for developing treatments. Schizophr Bull. (2014) 40:487–91. doi: 10.1093/schbul/sbu038
37. Fonagy, P, Steele, M, Steele, H, Moran, GS, and Higgitt, AC. The capacity for understanding mental states: the reflective self in parent and child and its significance for security of attachment. Infant Ment Health J. (1991) 12:201–18. doi: 10.1002/1097-0355(199123)12:3<201::AID-IMHJ2280120307>3.0.CO;2-7
38. Duval, J, Ensink, K, Normandin, L, and Fonagy, P. Mentalizing mediates the association between childhood maltreatment and adolescent borderline and narcissistic personality traits. Adolesc Psychiatry. (2018) 8:156–73. doi: 10.2174/2210676608666180829095455
39. Lysaker, PH, Carcione, A, Dimaggio, G, Johannesen, JK, Nicolò, G, Procacci, M, et al. Metacognition amidst narratives of self and illness in schizophrenia: associations with neurocognition, symptoms, insight and quality of life. Acta Psychiatr Scand. (2005) 112:64–71. doi: 10.1111/j.1600-0447.2005.00514.x
40. Semerari, A, Colle, L, Pellecchia, G, Buccione, I, Carcione, A, Dimaggio, G, et al. Metacognitive dysfunctions in personality disorders: correlations with disorder severity and personality styles. J Personal Disord. (2014) 28:751–66. doi: 10.1521/pedi_2014_28_137
41. Inchausti, F, García-Mieres, H, García-Poveda, NV, Fonseca-Pedrero, E, MacBeth, A, Popolo, R, et al. Recovery-focused metacognitive interpersonal therapy (MIT) for adolescents with first-episode psychosis. J Contemp Psychother. (2023) 53:9–17. doi: 10.1007/s10879-022-09569-0
42. Dimaggio, G. Integrated treatment for personality disorders: an introduction. J Psychother Integr. (2015) 25:1. doi: 10.1037/a0038765
43. Dimaggio, G, Ottavi, P, Popolo, R, and Salvatore, G. Metacognitive interpersonal therapy: Body, imagery and change. London, UK: Routledge (2020).
44. Dimaggio, G, Semerari, A, Carcione, A, Nicolò, G, and Procacci, M. Psychotherapy of personality disorders: Metacognition, states of mind and interpersonal cycles. London, UK: Routledge (2007).
45. Cheli, S, Lysaker, PH, and Dimaggio, G. Metacognitively oriented psychotherapy for schizotypal personality disorder: a two-case series. Personal Ment Health. (2019) 13:155–67. doi: 10.1002/pmh.1447
46. Dimaggio, G, Maillard, P, MacBeth, A, and Kramer, U. Effects of therapeutic alliance and metacognition on outcome in a brief psychological treatment for borderline personality disorder. Psychiatry. (2019) 82:143–57. doi: 10.1080/00332747.2019.1610295
47. Gordon-King, K, Schweitzer, RD, and Dimaggio, G. Metacognitive interpersonal therapy for personality disorders: the case of a man with obsessive–compulsive personality disorder and avoidant personality disorder. J Contemp Psychother. (2019) 49:39–47. doi: 10.1097/NMD.0000000000000789
48. Popolo, R, MacBeth, A, Canfora, F, Rebecchi, D, Toselli, C, Salvatore, G, et al. Metacognitive interpersonal therapy in group (MIT-G) for young adults with personality disorders: a pilot randomized controlled trial. Psychol Psychother. (2019) 92:342–58. doi: 10.1111/papt.12182
49. Inchausti, F, Velázquez-Basterra, G, Fonseca-Pedrero, E, MacBeth, A, Popolo, R, and Dimaggio, G. Metacognitive interpersonal group therapy for adolescents with avoidant personality disorder: the case of Sofia. J Clin Psychol. (2022) 78:1579–89. doi: 10.1002/jclp.23356
50. Simonsen, S, Popolo, R, Juul, S, Frandsen, FW, Sørensen, P, and Dimaggio, G. Treating avoidant personality disorder with combined individual metacognitive interpersonal therapy and group mentalization-based treatment: a pilot study. J Nerv Ment Dis. (2022) 210:163–71. doi: 10.1097/NMD.0000000000001432
51. Prunetti, E, Magrin, C, Zavagnin, M, Bodini, L, Bateni, M, and Dimaggio, G. Short-term inpatient DBT combined with metacognitive interventions for personality disorders: a pilot acceptability and effectiveness study. J Contemp Psychother. (2022) 52:173–80. doi: 10.1007/s10879-022-09536-9
52. Cheli, S, Cavalletti, V, Lysaker, PH, Dimaggio, G, Petrocchi, N, Chiarello, F, et al. A pilot randomized controlled trial comparing a novel compassion and metacognition approach for schizotypal personality disorder with a combination of cognitive therapy and psychopharmacological treatment. BMC Psychiatry. (2023) 23:113. doi: 10.1186/s12888-023-04610-5
53. Endicott, J, Spitzer, RL, Fleiss, JL, and Cohen, J. The global assessment scale. A procedure for measuring overall severity of psychiatric disturbance. Arch Gen Psychiatry. (1976) 33:766–71. doi: 10.1001/archpsyc.1976.01770060086012
54. American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Publishing, Inc (2000).
55. Pelizza, L, Azzali, S, Paterlini, F, Garlassi, S, Scazza, I, Pupo, S, et al. The Italian version of the 16-item prodromal questionnaire (IPQ-16): field-test and psychometric features. Schizophr Res. (2018) 199:353–60. doi: 10.1016/j.schres.2018.03.023
56. Ruggeri, M, Bonetto, C, Lasalvia, A, Fioritti, A, De Girolamo, G, Santonastaso, P, et al. Feasibility and effectiveness of a multi-element psychosocial intervention for first-episode psychosis: results from the cluster-randomized controlled get up piano trial in a catchment area of 10 million inhabitants. Schizophr Bull. (2015) 41:1192–203. doi: 10.1093/schbul/sbv058
57. Söderberg, P, Tungström, S, and Armelius, BÅ. Special section on the GAF: reliability of global assessment of functioning ratings made by clinical psychiatric staff. Psychiatr Serv. (2005) 56:434–8. doi: 10.1176/appi.ps.56.4.434
58. Guy, W. ECDEU assessment manual for psychopharmacology, revised (DHEW Publ. No. ADM 76–338). Rockville, MD: U.S. Dept. of Health, Education, and Welfare, Public Health Service, Alcohol, Drug Abuse, and Mental Health Administration, National Institute of Mental Health, Psychopharmacology Research Branch, Division of Extramural Research Programs, pp. 217–222. (1976).
59. Forkmann, T, Scherer, A, Boecker, M, Pawelzik, M, Jostes, R, and Gauggel, S. The clinical global impression scale and the influence of patient or staff perspective on outcome. BMC Psychiatry. (2011) 11:83. doi: 10.1186/1471-244x-11-83
60. Targum, SD, Pestreich, L, Reksoprodjo, P, Pereira, H, Guindon, C, and Hochfeld, M. A global measure to assess switching antipsychotic medications in the treatment of schizophrenia. Hum Psychopharmacol. (2012) 27:455–63. doi: 10.1002/hup.2247
61. Varner, RV, Chen, YR, Swann, AC, and Moeller, FG. The brief psychiatric rating scale as an acute inpatient outcome measurement tool. J Clin Psychiatry. (2000) 61:418–21. doi: 10.4088/jcp.v61n0605
62. Ventura, J, Green, MF, Shaner, A, and Liberman, RP. Training and quality assurance with the brief psychiatric rating scale: the drift busters. Int J Methods Psychiatr Res. (1993) 3:221–44.
63. Hofmann, AB, Schmid, HM, Jabat, M, Brackmann, N, Noboa, V, Bobes, J, et al. Utility and validity of the brief psychiatric rating scale (BPRS) as a transdiagnostic scale. Psychiatry Res. (2022) 314:114659. doi: 10.1016/j.psychres.2022.114659
64. Centonze, A, Inchausti, F, MacBeth, A, and Dimaggio, G. Changing embodied dialogical patterns in metacognitive interpersonal therapy. J Constr Psychol. (2021) 34:123–37. doi: 10.1080/10720537.2020.1717117
65. R Core Team. R: A language and environment for statistical computing. (version 4.1) [computer software]. (2021).. Available at: https://cran.r-project.org. (R packages retrieved from MRAN snapshot 2022-01-01).
66. Twenge, JM, Cooper, AB, Joiner, TE, Duffy, ME, and Binau, SG. Age, period, and cohort trends in mood disorder indicators and suicide-related outcomes in a nationally representative dataset, 2005-2017. J Abnorm Psychol. (2019) 128:185–99. doi: 10.1037/abn0000410
67. De Figueiredo, CS, Sandre, PC, Portugal, LCL, Mázala-de-Oliveira, T, Da Silva, CL, Raony, Í, et al. COVID-19 pandemic impact on children and adolescents' mental health: biological, environmental, and social factors. Prog Neuro-Psychopharmacol Biol Psychiatry. (2021) 106:110171. doi: 10.1016/j.pnpbp.2020.110171
68. Davis, MT, Holmes, SE, Pietrzak, RH, and Esterlis, I. Neurobiology of chronic stress-related psychiatric disorders: evidence from molecular imaging studies. Chronic Stress (Thousand Oaks). (2017) 1:10916. doi: 10.1177/2470547017710916
69. Shah, JL, Jones, N, van Os, J, McGorry, PD, and Gülöksüz, S. Early intervention service systems for youth mental health: integrating pluripotentiality, clinical staging, and transdiagnostic lessons from early psychosis. Lancet Psychiatry. (2022) 9:413–22. doi: 10.1016/S2215-0366(21)00467-3
70. Kovacs, M, Rottenberg, J, and George, C. Maladaptive mood repair responses distinguish young adults with early-onset depressive disorders and predict future depression outcomes. Psychol Med. (2009) 39:1841–54. doi: 10.1017/S0033291709005789
71. Dimaggio, G, Salvatore, G, MacBeth, A, Ottavi, P, Buonocore, L, and Popolo, R. Metacognitive interpersonal therapy for personality disorders: a case study series. J Contemp Psychother. (2017) 47:11–21. doi: 10.1007/s10879-016-9342-7
72. Popolo, R, MacBeth, A, Lazzerini, L, Brunello, S, Venturelli, G, Rebecchi, D, et al. Metacognitive interpersonal therapy in group versus TAU + waiting list for young adults with personality disorders: randomized clinical trial. Personal Disord. (2022) 13:619–28. doi: 10.1037/per0000497
73. Barber, JP, Barrett, MS, Gallop, R, Rynn, MA, and Rickels, K. Short-term dynamic psychotherapy versus pharmacotherapy for major depressive disorder: a randomized, placebo-controlled trial. J Clin Psychiatry. (2012) 73:66–73. doi: 10.4088/JCP.11m06831
74. Deter, HC, Weber, C, Herrmann-Lingen, C, Albus, C, Juenger, J, Ladwig, KH, et al. Gender differences in psychosocial outcomes of psychotherapy trial in patients with depression and coronary artery disease. J Psychosom Res. (2018) 113:89–99. doi: 10.1016/j.jpsychores.2018.08.005
75. Kushner, SC, Quilty, LC, McBride, C, and Bagby, RM. A comparison of depressed patients in randomized versus nonrandomized trials of antidepressant medication and psychotherapy. Depress Anxiety. (2009) 26:666–73. doi: 10.1002/da.20566
76. Ospina-Ospina Fdel, C, Hinestrosa-Upegui, MF, Paredes, MC, Guzmán, Y, and Granados, C. Síntomas de ansiedad y depresión en adolescentes escolarizados de 10 a 17 años en Chía, Colombia [symptoms of anxiety and depression in adolescents between 10 to 17 year-old attending schools in Chía, Colombia]. Rev Salud Publica (Bogota). (2011) 13:908–20. doi: 10.1590/s0124-00642011000600004
Keywords: metacognitive interpersonal therapy, psychotherapy, adolescence, treatment adherence, general psychopathology, drop-out rate, functioning
Citation: Marconi E, Monti L, Fredda G, Kotzalidis GD, Janiri D, Zani V, Vitaletti D, Simone MV, Piciollo S, Moriconi F, Di Pietro E, Popolo R, Dimaggio G, Veredice C, Sani G and Chieffo DPR (2023) Outpatient care for adolescents’ and young adults’ mental health: promoting self- and others’ understanding through a metacognitive interpersonal therapy-informed psychological intervention. Front. Psychiatry. 14:1221158. doi: 10.3389/fpsyt.2023.1221158
Edited by:
Espen Jan Folmo, Sorbonne Universités, FranceReviewed by:
Benjamin Hummelen, Oslo University Hospital, NorwayPhoebe Barnett, University College London, United Kingdom
Copyright © 2023 Marconi, Monti, Fredda, Kotzalidis, Janiri, Zani, Vitaletti, Simone, Piciollo, Moriconi, Di Pietro, Popolo, Dimaggio, Veredice, Sani and Chieffo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elisa Marconi, ZWxpc2EubWFyY29uaUBwb2xpY2xpbmljb2dlbWVsbGkuaXQ=
†ORCID: Elisa Marconi https://orcid.org/0000-0001-6722-8390
Laura Monti https://orcid.org/0000-0001-8339-265X
Giulia Fredda https://orcid.org/0000-0003-0321-5827
Georgios D. Kotzalidis https://orcid.org/0000-0002-0281-6324
Delfina Janiri https://orcid.org/0000-0003-2485-6121
Zani Valentina https://orcid.org/0009-0004-3987-0705
Debora Vitaletti https://orcid.org/0009-0002-6386-014X
Maria Velia Simone https://orcid.org/0009-0003-0256-7430
Simone Piciollo https://orcid.org/0009-0000-0924-7227
Federica Moriconi https://orcid.org/0000-0003-1593-0043
Emanuela Di Pietro https://orcid.org/0009-0006-5518-163X
Raffaele Popolo https://orcid.org/0000-0003-4903-8977
Giancarlo Dimaggio https://orcid.org/0000-0002-9289-8756
Chiara Veredice https://orcid.org/0000-0003-2267-8077
Gabriele Sani https://orcid.org/0000-0002-9767-8752
Daniela Pia Rosaria Chieffo https://orcid.org/0000-0002-0130-6584
 Elisa Marconi
Elisa Marconi Laura Monti1†
Laura Monti1† Georgios D. Kotzalidis
Georgios D. Kotzalidis Maria Velia Simone
Maria Velia Simone Emanuela Di Pietro
Emanuela Di Pietro Giancarlo Dimaggio
Giancarlo Dimaggio Gabriele Sani
Gabriele Sani Daniela Pia Rosaria Chieffo
Daniela Pia Rosaria Chieffo