
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 15 August 2023
Sec. Schizophrenia
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1196760
 Na Hu1
Na Hu1 Wei Li1
Wei Li1 Hu Deng1
Hu Deng1 Jiaqi Song1
Jiaqi Song1 Hanxue Yang2
Hanxue Yang2 Jiabao Chai1
Jiabao Chai1 Wenqian Huang1
Wenqian Huang1 Hong Wang1
Hong Wang1 Xuanzi Zhou3
Xuanzi Zhou3 Pan Zhang4
Pan Zhang4 Sushuang He1
Sushuang He1 Yonghua Cui5*
Yonghua Cui5* Tengteng Fan6*
Tengteng Fan6* Ying Li5*
Ying Li5*Background: Chronic schizophrenia is significantly influenced by negative symptoms, with several known contributors to secondary negative symptoms. However, the impact of these factors and negative symptoms on social functioning warrants further exploration.
Methods: We assessed the clinical symptoms, antipsychotic adverse reactions, and social functioning of 283 hospitalized patients with chronic schizophrenia using various standardized interviews and scales. We conducted multiple regression and mediation analyses to elucidate the impact of secondary factors on negative symptoms, and the relationship among these “secondary factors,” negative symptoms, and social functioning.
Results: Our findings identified depressive symptoms, extrapyramidal symptoms, and positive symptoms as significant contributors to secondary negative symptoms. We found that negative symptoms play a notable mediating role in the effect of depressive and positive symptoms on social functioning. However, the relationship between positive symptoms, negative symptoms, and social functioning proved to be intricate.
Conclusion: Our findings propose that negative symptoms act as pivotal mediators in the correlation between “secondary factors” (including the depressive symptoms and positive symptoms) and social functioning. The treatment of chronic schizophrenia necessitates focusing on key factors such as depressive and positive symptoms, which might significantly contribute to the development of secondary negative symptoms. Further research is essential to clarify the complex relationship among positive symptoms, negative symptoms, and social functioning in schizophrenia.
Negative symptoms, characterized by deficits in motivation, communication, emotion, and social functioning (1), are considered a core feature of schizophrenia—a chronic and debilitating mental disorder (2). These symptoms significantly deteriorate the functioning and quality of life of patients with schizophrenia (2–5), imposing a substantial burden on patients, their families, and the healthcare system (6). Negative symptoms primarily denote the decrease or absence of typical behaviors (such as indulgence, anhedonia, and social engagement) or expressions (such as emotional dullness, apathy) associated with motivation and interest (7, 8). The current consensus classifies negative symptoms into five domains: Blunted affect, characterized by a reduction in emotional expression, demonstrated by decreased facial and vocal expressions, and physical movements; Alogia, referring to a decrease in the quantity of speech and spontaneous elaboration; Asociality, indicating a diminished drive to engage in interpersonal relationships, leading to reduced social interactions; Anhedonia, describing a decreased capacity to derive pleasure from current activities or anticipate enjoyment from future engagements; Avolition, representing a diminished ability to initiate and maintain goal-oriented activities due to a lack of motivation (9).
Negative symptoms have been differentiated into either primary symptom intrinsic to schizophrenia, or secondary symptom resultant from other underlying factors (6). Primary negative symptoms, considered inherent aspects of schizophrenia’s core pathology, are thus direct manifestations of the disorder (10). Secondary negative symptoms, however, are thought to arise from exogenous factors, they are typically transient and more prevalent than primary negative symptoms (11). Given their clear causative factors, secondary negative symptoms are generally more responsive to treatment compared to primary negative symptoms (11, 12). Secondary negative symptoms in schizophrenia can stem from a variety of sources, including positive symptoms, depressive symptoms, side effects of antipsychotic medication (such as extrapyramidal symptoms), or prolonged social isolation due to extended hospitalization (2, 13–15). According to the European Psychiatric Association (EPA) guidance on assessment of negative symptoms in schizophrenia, there are three key factors that might serve as “secondary factors” which include depressive symptoms, positive symptoms, and extrapyramidal symptoms (7). For instance, extrapyramidal symptoms can lead to a blunted affect and alogia, both of which form part of the negative symptoms (2). However, it remains unclear whether these secondary factors impede social functioning by exacerbating negative symptoms.
Social functioning, defined as the capacity to comprehend and partake in social activities, thus facilitating effective and regular involvement in social life (16), constitutes a crucial facet of the rehabilitation journey for individuals diagnosed with schizophrenia (17). It is important to highlight that impaired social functioning is a typical characteristic of those with schizophrenia, with negative symptoms serving as a major contributor to such deficits (18). Notably, the co-occurrence of depressive symptoms is another influential factor, as it has been found to result in markedly detrimental consequences on social functioning in patients with schizophrenia (19). It is also noteworthy that positive symptoms have been identified as influencing social functioning in patients with this disorder. Furthermore, existing literature has established that patients presenting more severe motor impairments, such as extrapyramidal symptoms, often correspondingly display worsened social functioning (20). Motor abnormalities, such as extrapyramidal symptoms, are believed to result from a combination of brain dysfunction and the side effects of antipsychotic medication (20, 21). Despite these observations, the interrelationships among these secondary factors (which contribute to secondary negative symptoms), negative symptoms themselves, and social functioning call for further exploration.
The main objective of this study is 2-fold. Firstly, we aimed to investigate several potential “secondary factors” that might lead to negative symptoms in chronic schizophrenia. Secondly, by employing mediation analysis, the relationship among (1) negative symptoms, (2) secondary factors (including positive symptoms, depressive symptoms, and extrapyramidal symptoms), and (3) social functioning were explored. For this study, our hypothesis suggests that the “secondary factors” has an impact on social functioning by a mediator of the severity of negative symptoms.
The present study employed a cross-sectional design and conducted a sampling survey at the one of the Mental Health Centers of Beijing from March 1, 2018, to September 30, 2018. A total of 283 hospitalized patients between the ages of 18 and 60, who had been diagnosed with schizophrenia by two psychiatrists according to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), were recruited as participants. Eligible participants had a course of schizophrenia lasting more than 5 years and had been hospitalized for at least 5 years.
Inclusion criteria of this study were as followed: (1) diagnosed with schizophrenia by the DSM-5 diagnostic criteria; (2) having a disease duration of more than 5 years; (3) hospitalized for longer than 5 years; (4) aged between 18 and 60; (5) had not have any changes in antipsychotic medication for at least 6 weeks; and (6) voluntary participation with informed consent. Exclusion criteria were: (1) having comorbid mental disorders; (2) having brain diseases or serious/unstable physical illnesses; (3) being pregnant or lactating; (4) having drug or alcohol abuse/dependence; (5) having received modified electroconvulsive therapy within the past 3 months; and (6) were unable to complete all surveys. Informed consent obtained from all patients and their guardians. The study protocol was approved by the Ethics Committee of the one Mental Health Center of Beijing (protocol number: 109).
The positive and negative syndrome scale (PANSS) is a widely used tool designed to evaluate the severity of schizophrenia symptoms (22). The PANSS has a Chinese version which comprises of 30 items and is divided into three subscales: positive, negative, and general psychopathology. The severity of each item is rated on a Likert scale from 1 (absent) to 7 (extreme), with higher scores indicating more severe symptoms. The Chinese version of the PANSS has been shown to be a reliable and effective assessment tool for evaluating the severity of psychopathology in hospitalized, stable patients with schizophrenia (23).
The scale for assessment of negative symptoms (SANS) is a well-established instrument in evaluating negative symptoms across five domains, including affective flattening, alogia, avolition apathy, anhedonia-asociality, and attention. The scale consists of 25 items, which are rated on a six-point Likert scale ranging from 0 to 5 points, with higher scores indicating greater impairment (24). The Chinese versions of the SANS have good reliability and validity (25).
Factor analysis of the general psychopathological rating scales found that some items in SANS did not belong to the category of negative symptoms, including attentional impairment (SANS global rating of attention), inappropriate affect (SANS item 6), and poverty of content of speech (SANS item 10) (7, 8). Therefore, we have excluded the above three items in the data related to SANS in the article.
The scale for the assessment of positive symptoms (SAPS) scale is comprised of 34 items that evaluate positive symptoms of schizophrenia across four domains: hallucinations, delusions, bizarre behavior, and positive formal thought disorder (24). Each item is scored on a severity scale from 0 (absent) to 5 (extremely severe). Every subscale has its own global score, which ranges from 0 (absent) to 5 (extremely severe), assessing the overall severity of each symptom domain. The SAPS total score is the sum of all items except the global items, while the SAPS summary score is the sum of the four global items. The Chinese version of the SAPS scale has demonstrated good reliability and validity (25).
The Simpson–Angus scale (SAS) is a validated sensitive tool to evaluate extrapyramidal side effects caused by neuroleptic drugs (26), including 10 items that are graded on a five-point Likert scale, with each item scored from 0 to 4. A higher score on the SAS scale indicates the presence of more severe extrapyramidal side effects.
The Calgary depression scale for schizophrenia (CDSS) was developed to evaluate depressive symptoms in individuals with schizophrenia. It consists of nine items, each rated on a Likert scale of 0–3, with higher scores indicate more severe symptoms (27).
The Global Assessment of Functioning (GAF) is a widely used scale in both research and clinical practice for assessing the overall functioning of patients with schizophrenia, focusing on psychological, social, and occupational well-being (28). The total score ranges from 1 to 100, with higher scores indicating better retained functions and milder symptoms. The GAF is subdivided into 10 10-point intervals. The reliability and validity of the GAF as a valuable objective indicator of overall patient functioning has been strongly suggested (29).
Four professional psychiatrists who had undergone training and consistency evaluation (the Intraclass Correlation Coefficient is 0.90) were recruited to evaluate the schizophrenia scale on site, and the survey results were collected. Each eligible patient was assessed by two psychiatrists on the same day. The first psychiatrist evaluated the patients and collected data on their sociodemographic information, clinical data, and psychiatric history through a questionnaire. The second psychiatrist administered all six scales to the patient.
Data analysis was performed using SPSS for Windows 23.0. Descriptive statistics were used to summarize continuous variables in terms of mean and standard deviation. Firstly, multiple linear regression was used to explore the factors that may significantly impact negative symptoms, with the total SANS score as the dependent variable and the common factors of secondary negative symptoms as independent variables. Secondly, we utilized a linear regression model to separately explore: (1) The prediction of social function as evaluated by Global Assessment of Functioning (GAF), by the extrapyramidal symptoms evaluated by SAS, depressive symptoms evaluated by CDSS, and positive symptoms evaluated by SAPS; (2) The combined prediction of these three factors (SAS, CDSS, and SAPS) for negative symptoms; (3) The prediction of social function (GAF) by negative symptoms, evaluated by Scale for the Assessment of Negative Symptoms (SANS), after excluding items not related to negative symptoms. Furthermore, the impact of each negative symptom factor on social functioning was further studied using multiple linear regression, with the GAF score as the dependent variable and the SANS score on the five subscales as independent variables. Finally, mediation analysis was carried out using packages in R (Mediation) (30) to investigate the relationship between depressive symptoms, extrapyramidal symptoms, positive symptoms, and social functioning, with a focus on the role of negative symptoms. All tests were two-tailed, and the significance level was set at p < 0.05.
A total of 283 long-term hospitalized patients with chronic schizophrenia participated in this study, with an age range of 29–60 and an average age of 43.83 ± 8.19. The mean age of onset was 24.57 ± 8.042, the mean course of disease was 8.92 ± 5.075 years, and the mean length of hospital stay was 6.30 ± 4.535 years. Participants exhibited significant negative symptoms (mean SANS score of 19.548 ± 10.541), and relatively mild positive (mean SAPS score of 3.15 ± 4.466) and depressive symptoms (mean CDSS score of 1.70 ± 2.00). Moreover, their social functioning was impaired, as evidenced by a mean GAF score of 68.16 ± 7.345 (see Table 1).
The multiple linear regression analysis revealed that negative symptoms, as assessed by the SANS, significantly predict social function as evaluated by the GAF scale (p < 0.001). Moreover, the scores from the CDSS (p = 0.001), SAS (p = 0.007), and the SAPS (p = 0.048) significantly predict the SANS score. However, only the CDSS (p = 0.019) and SAPS (p = 0.045) scores significantly predict the GAF score (see Table 2).
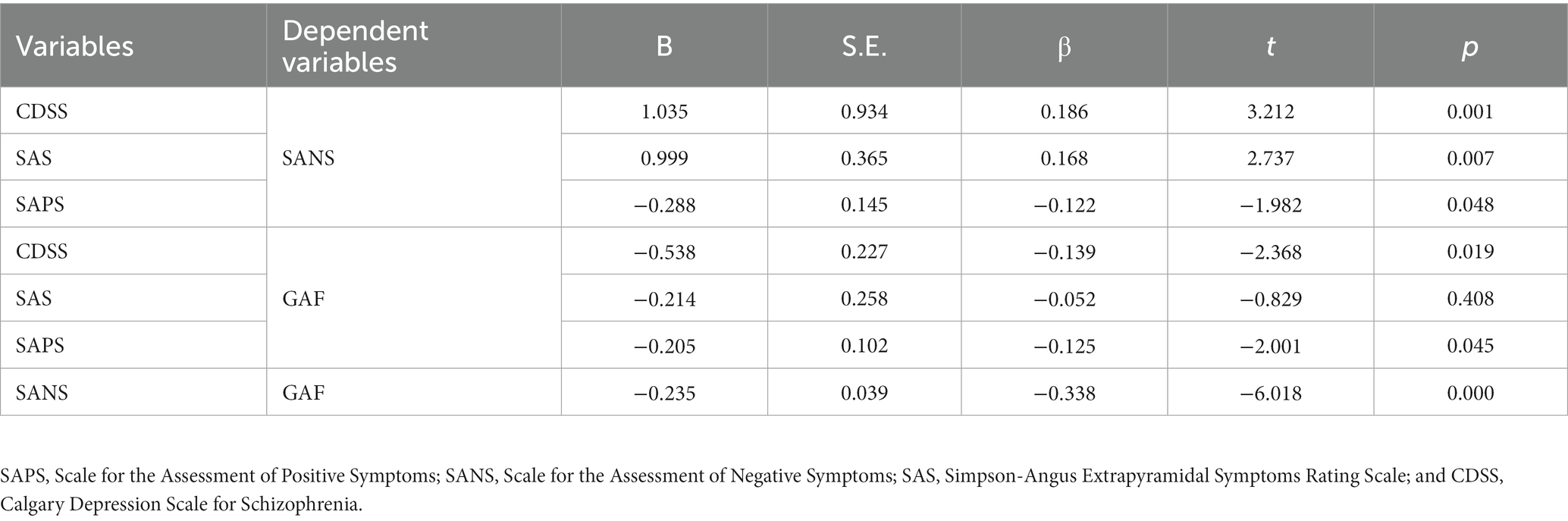
Table 2. Multiple linear regression analysis of secondary factors of negative symptoms and social function (N = 283).
We conducted an extensive investigation into the association between negative symptoms and social functioning. We examined the relationship between the four subscales of SANS and GAF score and found the score in Table 3 (avolition-apathy) predict GAF score (p < 0.001; see Table 3).
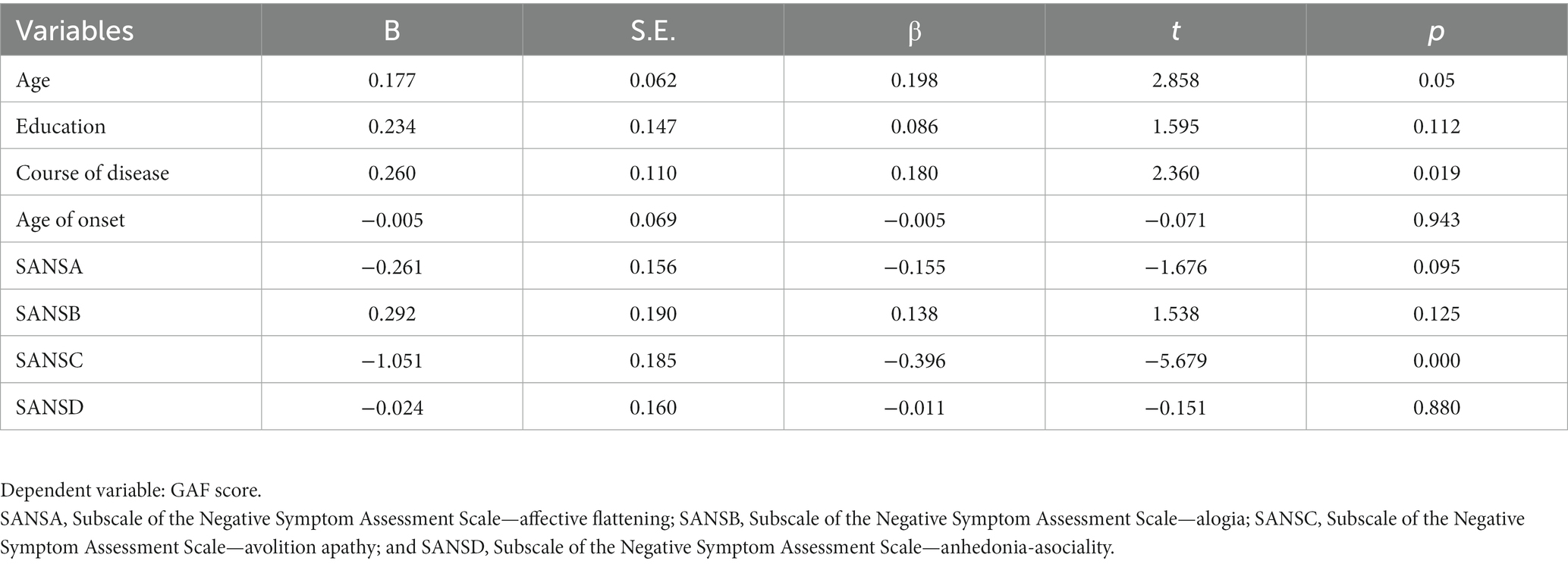
Table 3. The impact of the four subscales of SANS on social functioning by multiple linear regression analysis (N = 283).
In the final stage of data analyses, we investigated the mediating role of negative symptoms in the relationship between various secondary factors and social functioning. Results revealed that negative symptoms fully mediated the relationship between depressive symptoms (β = −0.287, p < 0.001) and social functioning, and partially mediated the relationship between positive symptoms (β = 0.115, p < 0.001) and social functioning (see Figure 1).
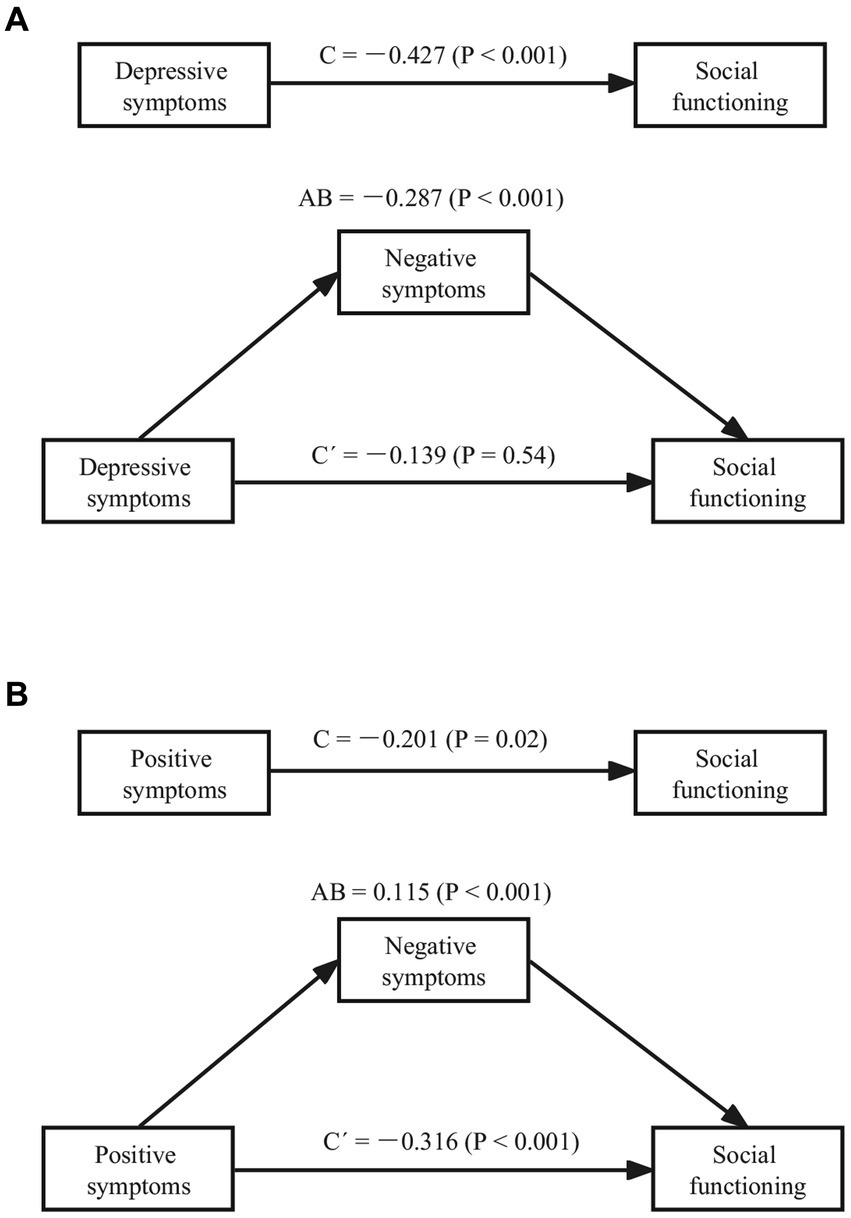
Figure 1. Mediating effect of negative symptoms on depressive symptoms, positive symptoms and social functioning (N = 283). (A) Mediating effect of negative symptoms on depressive symptoms and social functioning; (B) Mediating effect of negative symptoms on positive symptoms and social functioning (C, total effect; AB, indirect effect; C’, direct effect).
This study aimed to examine the presence of negative symptoms in patients with chronic schizophrenia and to identify factors associated with secondary negative symptoms. Our findings revealed that negative symptoms were significantly associated with positive symptoms and depressive symptoms.
Depressive symptoms are highly prevalent in patients with schizophrenia, occurring in approximately 25% of cases (31), and can manifest at any stage of the disease (11). Moreover, more than 60% of patients with schizophrenia experience depressive symptoms (32), whereas secondary comorbidities of depression are common in chronic schizophrenia (33). Our study confirmed previous findings, which suggest a significant positive correlation between depressive symptoms and negative symptoms in patients with chronic schizophrenia (34). For example, the degree and duration of depressive symptoms in psychiatric patients were correlated with negative symptoms (35).
Furthermore, an overlap between depressive symptoms and negative symptoms in patients with schizophrenia has been noted (11). Anhedonia and avolition are common symptoms of both schizophrenia and depression (36). The key feature of this overlap is anhedonia, which is a core symptom of depression and an important feature of schizophrenia (37, 38). Depressive symptoms are one of the most common factors associated with secondary negative symptoms of schizophrenia (15). Depression can lead to secondary negative symptoms, such as lack of energy, amotivation, and decreased interest (11). Our study also showed that both depressive symptoms and negative symptoms were significantly negatively correlated with GAF scores. A previous study has found that the more prominent the negative and depressive symptoms of schizophrenic patients were, the more severe their impairment of social function (39). In our study, we conducted a mediating analysis and found that negative symptoms completely mediated the relationship between depressive symptoms and social functioning. That is, depressive symptoms had no significant direct effect on social functioning, but mainly influenced it through secondary negative symptoms. Therefore, in the rehabilitation of social functioning in chronic schizophrenia, it is important to pay attention to patients with depressive symptoms, and to intervene possible secondary negative symptoms associated with these depressive symptoms.
Another important factor contributing to negative symptoms being the positive symptoms. Our study found a significant negative correlation between positive and negative symptoms in patients with chronic schizophrenia. However, previous studies have suggested a positive correlation, with improvement of positive symptoms leading to remission of negative symptoms (40). For instance, delusions of victimhood or hallucinations can cause social withdrawal, hindering the patient’s ability to engage in communication or enjoy group activities (34). By treating positive symptoms, such as hallucinations and delusions, negative symptoms secondary to positive symptoms may be alleviated (40). Concerning the discrepancy between our findings and the previous ones, we suspect the characteristics of participants might played a role. All participants in our study were long-term hospitalized patients with chronic schizophrenia, whose negative symptoms were more prominent and positive symptoms relatively mild. When a patient’s condition fluctuates, psychiatrists may increase the dose of antipsychotics, potentially worsening negative symptoms (41). At the same time, decreased positive symptoms may lead to alleviated secondary negative symptoms, which can be relieved by antipsychotics. These results suggest a complex relationship between positive symptoms and secondary negative symptoms that may require further investigation.
Our study results indicate a correlation between extrapyramidal symptoms and negative symptoms. However, these extrapyramidal symptoms do not seem to influence social functioning through negative symptoms. Currently, the relationship between extrapyramidal symptoms and negative symptoms remains unclear. In the two-factor model of negative symptoms, the deficit in the expressive dimension could be affected by extrapyramidal symptoms (2). Therefore, it is plausible that extrapyramidal symptoms could exacerbate the deficit in the expressive dimension of negative symptoms. However, these relationships need further exploration, it is indeed very challenging to differentiate between the Expressive Deficit domain of negative symptoms, which includes blunted affect and alogia (7). Another critical point is the use of antipsychotic medications. The dosage of antipsychotic medications may be a significant factor (7). Future research could focus on exploring the relationship between the dosage of antipsychotic medications, extrapyramidal symptoms, and the deficit in the expressive dimension of negative symptoms.
Additionally, our study found a strong association between apathy, one of the subscales of SANS (24), and social functioning. Apathy is a prevalent negative symptom (42) that significantly affects the social functioning of patients with chronic schizophrenia (43). Our results hinted that reducing apathy should be a priority in the rehabilitation of patients with schizophrenia. Moreover, we proposed that factors leading to secondary negative symptoms might indirectly affect social functioning through negative symptoms. However, our findings indicated that positive symptoms had a direct negative effect on social functioning, consistent with a previous study (44), which reported a significant negative association between positive symptom clusters and social functioning. However, we also found that positive symptoms can positively moderate social functioning by moderating negative symptoms. The relationship between positive symptoms, negative symptoms, and social functioning is complex, and it is affected by drug treatment, side effects, and other factors.
Our study has several clinical implications. First, patients with chronic schizophrenia require special attention and treatment of negative symptoms during social functioning recovery. Among factors contributing to negative symptoms, depressive symptoms and positive symptoms should be the focus of intervention. The intervention of extrapyramidal symptoms should also be considered comprehensively. The treatment process would benefit from controlling depressive symptoms and positive symptoms while minimizing adverse drug reactions, which may aggravate negative symptoms.
Certain limitations in our study merit attention. First, our assessment of negative symptoms solely relied on the SANS and PANSS scales. Future research might benefit from incorporating more recent second-generation negative symptom scales, such as the Brief Negative Symptom Scale (BNSS) and Clinical Assessment Interview for Negative Symptoms (CAINS). These updated scales resonate more with current conceptualizations of negative symptoms and enable a clear distinction between primary and secondary negative symptoms. Secondly, our study lacked data pertaining to the temporal relationship between the onset of negative symptoms and the commencement and augmentation of antipsychotic treatment. As such, we were unable to verify whether all extrapyramidal symptoms we noted were indeed secondary to antipsychotic treatment. Thirdly, considering that not all aspects of function might be impacted by negative symptoms, future research could potentially adopt rating scales that offer a clear separation of functional aspects. This could provide a more nuanced assessment of patients’ social functioning. Fourthly, the relatively small sample size in our study may limit the extrapolation of our findings. To validate our results, larger-scale studies are recommended. Finally, to further unravel the temporal dynamics of negative symptoms and their contributory factors, it would be beneficial for future research to include longitudinal data.
This study indicates that factors depressive symptoms and positive symptoms may play significant roles in the evolution of secondary negative symptoms in schizophrenia. Our findings propose that negative symptoms act as pivotal mediators in the correlation between “secondary factors” (including the depressive symptoms and positive symptoms) and social functioning. Therefore, in managing chronic schizophrenia, the targeted treatment of depressive symptoms, as well as the positive symptoms could represent a crucial strategy for enhancing social functioning by addressing secondary negative symptoms.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
The study protocol was approved by the Ethics Committee of one Mental Health Center in Beijing (protocol number: 109). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
The concept for this article was proposed by YL, and NH, WL, HD, JS, HY, JC, WH, HW, XZ, PZ, SH, YC, and TF collaborated to develop the protocol, establish the search strategy, and define the inclusion and exclusion criteria. Data collection was conducted by NH, WL, HD, JS, HY, JC, WH, HW, PZ, SH, XZ, and YC, while YL performed the statistical analyses, interpreted the data, and created the figures and tables. NH and TF drafted the initial version of the report with critical feedback from YL and YC. NH, WL, HD, JS, HY, JC, WH, HW, XZ, PZ, SH, YC, TF, and YL participated in the interpretation of the findings, and revision of the report, and gave their final approval of the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China under Grant Nos. 81901345, 82001445, and 82171538, the Natural Science Foundation of Beijing Municipality under Grant Nos. 7212035, and the Beijing Municipal Administration of Hospitals’ Youth Program under Grant No. QML20232006, QML20232003, and QML20211203.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Foussias, G, and Remington, G. Negative symptoms in schizophrenia: avolition and Occam’s razor. Schizophr Bull. (2010) 36:359–69. doi: 10.1093/schbul/sbn094
2. Mosolov, SN, and Yaltonskaya, PA. Primary and secondary negative symptoms in schizophrenia. Front Psychol. (2021) 12:766692. doi: 10.3389/fpsyt.2021.766692
3. Galderisi, S, Rossi, A, Rocca, P, Bertolino, A, Mucci, A, Bucci, P, et al. The influence of illness-related variables, personal resources and context-related factors on real-life functioning of people with schizophrenia. World Psychiatry. (2014) 13:275–87. doi: 10.1002/wps.20167
4. Harvey, PD, and Strassnig, M. Predicting the severity of everyday functional disability in people with schizophrenia: cognitive deficits, functional capacity, symptoms, and health status. World Psychiatry. (2012) 11:73–9. doi: 10.1016/j.wpsyc.2012.05.004
5. Ventura, J, Subotnik, KL, Gitlin, MJ, Gretchen-Doorly, D, Ered, A, Villa, KF, et al. Negative symptoms and functioning during the first year after a recent onset of schizophrenia and 8 years later. Schizophr Res. (2015) 161:407–13. doi: 10.1016/j.schres.2014.10.043
6. Galderisi, S, Mucci, A, Buchanan, RW, and Arango, C. Negative symptoms of schizophrenia: new developments and unanswered research questions. Lancet Psychiatry. (2018) 5:664–77. doi: 10.1016/S2215-0366(18)30050-6
7. Galderisi, S, Mucci, A, Dollfus, S, Nordentoft, M, Falkai, P, Kaiser, S, et al. EPA guidance on assessment of negative symptoms in schizophrenia. Eur Psychiatry. (2021) 64:e23. doi: 10.1192/j.eurpsy.2021.11
8. Giordano, GM, Caporusso, E, Pezzella, P, and Galderisi, S. Updated perspectives on the clinical significance of negative symptoms in patients with schizophrenia. Expert Rev Neurother. (2022) 22:541–55. doi: 10.1080/14737175.2022.2092402
9. Kirkpatrick, B, Fenton, WS, Carpenter, WT Jr, and Marder, SR. The NIMH-MATRICS consensus statement on negative symptoms. Schizophr Bull. (2006) 32:214–9. doi: 10.1093/schbul/sbj053
10. Moller, HJ. Clinical evaluation of negative symptoms in schizophrenia. Eur Psychiatry. (2007) 22:380–6. doi: 10.1016/j.eurpsy.2007.03.010
11. Kirschner, M, Aleman, A, and Kaiser, S. Secondary negative symptoms—a review of mechanisms, assessment and treatment. Schizophr Res. (2017) 186:29–38. doi: 10.1016/j.schres.2016.05.003
12. Barlati, S, Nibbio, G, Calzavara-Pinton, I, Invernizzi, E, Cadei, L, Lisoni, J, et al. Primary and secondary negative symptoms severity and the use of psychiatric care resources in schizophrenia spectrum disorders: a 3-year follow-up longitudinal retrospective study. Schizophr Res. (2022) 250:31–8. doi: 10.1016/j.schres.2022.10.002
13. Kirkpatrick, B. Developing concepts in negative symptoms: primary vs secondary and apathy vs expression. J Clin Psychiatry. (2014) 75:3–7. doi: 10.4088/JCP.13049su1c.01
14. Buchanan, RW. Persistent negative symptoms in schizophrenia: an overview. Schizophr Bull. (2007) 33:1013–22. doi: 10.1093/schbul/sbl057
15. Correll, CU, and Schooler, NR. Negative symptoms in schizophrenia: a review and clinical guide for recognition, assessment, and treatment. Neuropsychiatr Dis Treat. (2020) 16:519–34. doi: 10.2147/NDT.S225643
16. Hiser, J, and Koenigs, M. The multifaceted role of the ventromedial prefrontal cortex in emotion, decision making, social cognition, and psychopathology. Biol Psychiatry. (2018) 83:638–47. doi: 10.1016/j.biopsych.2017.10.030
17. Long, M, Stansfeld, JL, Davies, N, Crellin, NE, and Moncrieff, J. A systematic review of social functioning outcome measures in schizophrenia with a focus on suitability for intervention research. Schizophr Res. (2022) 241:275–91. doi: 10.1016/j.schres.2022.02.011
18. Popolo, R, Smith, E, Lysaker, PH, Lestingi, K, Cavallo, F, Melchiorre, L, et al. Metacognitive profiles in schizophrenia and bipolar disorder: comparisons with healthy controls and correlations with negative symptoms. Psychiatry Res. (2017) 257:45–50. doi: 10.1016/j.psychres.2017.07.022
19. van Rooijen, G, Vermeulen, JM, Ruhe, HG, and de Haan, L. Treating depressive episodes or symptoms in patients with schizophrenia. CNS Spectr. (2019) 24:239–48. doi: 10.1017/S1092852917000554
20. Nadesalingam, N, Chapellier, V, Lefebvre, S, Pavlidou, A, Stegmayer, K, Alexaki, D, et al. Motor abnormalities are associated with poor social and functional outcomes in schizophrenia. Compr Psychiatry. (2022) 115:152307. doi: 10.1016/j.comppsych.2022.152307
21. Tandon, R, Lenderking, WR, Weiss, C, Shalhoub, H, Barbosa, CD, Chen, J, et al. The impact on functioning of second-generation antipsychotic medication side effects for patients with schizophrenia: a worldwide, cross-sectional, web-based survey. Ann General Psychiatry. (2020) 19:42. doi: 10.1186/s12991-020-00292-5
22. Kay, SR, Fiszbein, A, and Opler, LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. (1987) 13:261–76. doi: 10.1093/schbul/13.2.261
23. Wu, BJ, Lan, TH, Hu, TM, Lee, SM, and Liou, JY. Validation of a five-factor model of a Chinese mandarin version of the positive and negative syndrome scale (CMV-PANSS) in a sample of 813 schizophrenia patients. Schizophr Res. (2015) 169:489–90. doi: 10.1016/j.schres.2015.09.011
24. Andreasen, N. Scale for the Assessment of Negative Symptoms (SANS). Iowa City: University of Iowa (1984).
25. Phillips, MR, Xiong, W, Wang, RW, Gao, YH, Wang, XQ, and Zhang, NP. Reliability and validity of the Chinese versions of the scales for assessment of positive and negative symptoms. Acta Psychiatr Scand. (1991) 84:364–70. doi: 10.1111/j.1600-0447.1991.tb03161.x
26. Simpson, GM, and Angus, JW. A rating scale for extrapyramidal side effects. Acta Psychiatr Scand Suppl. (1970) 212:11–9. doi: 10.1111/j.1600-0447.1970.tb02066.x
27. Addington, D, Addington, J, and Maticka-Tyndale, E. Specificity of the Calgary depression scale for schizophrenics. Schizophr Res. (1994) 11:239–44. doi: 10.1016/0920-9964(94)90017-5
28. Startup, M, Jackson, MC, and Bendix, S. The concurrent validity of the global assessment of functioning (GAF). Br J Clin Psychol. (2002) 41:417–22. doi: 10.1348/014466502760387533
29. Jones, SH, Thornicroft, G, Coffey, M, and Dunn, G. A brief mental health outcome scale-reliability and validity of the global assessment of functioning (GAF). Br J Psychiatry. (1995) 166:654–9. doi: 10.1192/bjp.166.5.654
30. Lange, T, Hansen, KW, Sorensen, R, and Galatius, S. Applied mediation analyses: a review and tutorial. Epidemiol Health. (2017) 39:e2017035. doi: 10.4178/epih.e2017035
31. Buckley, PF, Miller, BJ, Lehrer, DS, and Castle, DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. (2009) 35:383–402. doi: 10.1093/schbul/sbn135
32. Gozdzik-Zelazny, A, Borecki, L, and Pokorski, M. Depressive symptoms in schizophrenic patients. Eur J Med Res. (2011) 16:549–52. doi: 10.1186/2047-783X-16-12-549
33. Treen, D, Savulich, G, Mezquida, G, Garcia-Portilla, MP, Toll, A, Garcia-Rizo, C, et al. Influence of secondary sources in the brief negative symptom scale. Schizophr Res. (2019) 204:452–4. doi: 10.1016/j.schres.2018.10.004
34. Farreny, A, Savill, M, and Priebe, S. Correspondence between negative symptoms and potential sources of secondary negative symptoms over time. Eur Arch Psychiatry Clin Neurosci. (2018) 268:603–9. doi: 10.1007/s00406-017-0813-y
35. Klaassen, RM, Heins, M, Luteijn, LB, van der Gaag, M, van Beveren, NJ, and Genetic, R. Outcome of psychosis i: depressive symptoms are associated with (sub)clinical psychotic symptoms in patients with non-affective psychotic disorder, siblings and healthy controls. Psychol Med. (2013) 43:747–56. doi: 10.1017/S0033291712001572
36. Krynicki, CR, Upthegrove, R, Deakin, JFW, and Barnes, TRE. The relationship between negative symptoms and depression in schizophrenia: a systematic review. Acta Psychiatr Scand. (2018) 137:380–90. doi: 10.1111/acps.12873
37. Demyttenaere, K, Anthonis, E, Acsai, K, and Correll, CU. Depressive symptoms and PANSS symptom dimensions in patients with predominant negative symptom schizophrenia: a network analysis. Front Psychol. (2022) 13:795866. doi: 10.3389/fpsyt.2022.795866
38. Watson, D, and Naragon-Gainey, K. On the specificity of positive emotional dysfunction in psychopathology: evidence from the mood and anxiety disorders and schizophrenia/schizotypy. Clin Psychol Rev. (2010) 30:839–48. doi: 10.1016/j.cpr.2009.11.002
39. Gao, T, Huang, Z, Huang, B, Zhou, T, Shi, C, Yu, X, et al. Negative symptom dimensions and social functioning in Chinese patients with schizophrenia. Front Psychol. (2022) 13:1033166. doi: 10.3389/fpsyt.2022.1033166
40. Chen, L, Johnston, JA, Kinon, BJ, Stauffer, V, Succop, P, Marques, TR, et al. The longitudinal interplay between negative and positive symptom trajectories in patients under antipsychotic treatment: a post hoc analysis of data from a randomized, 1-year pragmatic trial. BMC Psychiatry. (2013) 13:320. doi: 10.1186/1471-244X-13-320
41. Veerman, SRT, Schulte, PFJ, and de Haan, L. Treatment for negative symptoms in schizophrenia: a comprehensive review. Drugs. (2017) 77:1423–59. doi: 10.1007/s40265-017-0789-y
42. Faerden, A, Finset, A, Friis, S, Agartz, I, Barrett, EA, Nesvag, R, et al. Apathy in first episode psychosis patients: one year follow up. Schizophr Res. (2010) 116:20–6. doi: 10.1016/j.schres.2009.10.014
43. Evensen, J, Rossberg, JI, Barder, H, Haahr, U, Hegelstad, W, Joa, I, et al. Apathy in first episode psychosis patients: a ten year longitudinal follow-up study. Schizophr Res. (2012) 136:19–24. doi: 10.1016/j.schres.2011.12.019
Keywords: secondary negative symptoms, chronic schizophrenia, depression, positive symptoms, social functioning
Citation: Hu N, Li W, Deng H, Song J, Yang H, Chai J, Huang W, Wang H, Zhou X, Zhang P, He S, Cui Y, Fan T and Li Y (2023) The mediating role of negative symptoms in “secondary factors” determining social functioning in chronic schizophrenia. Front. Psychiatry. 14:1196760. doi: 10.3389/fpsyt.2023.1196760
Received: 30 March 2023; Accepted: 31 July 2023;
Published: 15 August 2023.
Edited by:
Gabriele Nibbio, University of Brescia, ItalyReviewed by:
Irene Calzavara-Pinton, University of Brescia, ItalyCopyright © 2023 Hu, Li, Deng, Song, Yang, Chai, Huang, Wang, Zhou, Zhang, He, Cui, Fan and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ying Li, bGl5aW5nQGJjaC5jb20uY24=; Yonghua Cui, Y3VpeW9uZ2h1YUBiY2guY29tLmNu; Tengteng Fan, ZmFudGVuZ3RlbmdAYmptdS5lZHUuY24=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.