
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 12 September 2023
Sec. Adolescent and Young Adult Psychiatry
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1183916
 Yalan Li1†
Yalan Li1† Xin Li2†
Xin Li2† Yunge Li1†
Yunge Li1† Yu Xiao1
Yu Xiao1 Chunya Li1
Chunya Li1 Jia Chen1
Jia Chen1 Yao Li1
Yao Li1 Lishi Luo1
Lishi Luo1 Ding Su1
Ding Su1 Juan Jia1
Juan Jia1 Haofei Cheng1
Haofei Cheng1 Tianjiao Liu2†
Tianjiao Liu2† Na Du1*
Na Du1*Introduction: Family environment is the primary environment for adolescent growth and development, which is believed to have an important impact on the occurrence of non-suicidal self-injury (NSSI) behavior in adolescents. This study aimed to explore the effects of family environment cognition and cognitive differences perceived by adolescents and their parents on the treatment effects of NSSI in adolescents and to provide more potential perspectives for NSSI treatment.
Methods: A one-year prospective longitudinal sub-cohort investigation was carried out among 199 adolescents engaged in NSSI and one of their important guardians from the Longitudinal Psychosomatic Disease Study (LoPDS). The NSSI behaviors of adolescents were evaluated at 3 months, 6 months and 1 year after enrollment. The family environment scale (FES) and NSSI Behavior Questionnaire were used as assessment tools for family environment and adolescents NSSI behaviors. Multiple linear regression was used to investigate the role of family environment perception difference in the treatment effect of adolescent NSSI.
Results: After one year of follow-up, the perceived self-injury impulse score in recent 2 weeks, self-injury impulse frequency in recent 2 weeks, total number of self-injury in recent 2 weeks decreased significantly. The higher the adolescent family cohesion (Beta: 1.130, 95% CI: 0.886,1.373; p=0.032), parental family expressiveness (Beta: 0.818, 95% CI: 0.375,1.260; p=0.037) and parental family active-recreational orientation score (Beta: 0.609, 95% CI: 0.236,0.981; p=0.048), the better the treatment effect. However, higher adolescent family conflict (Beta: -0.838, 95% CI: -1.377,-0.298; p=0.024) were associated with lower treatment outcomes. The greater the cognitive difference between parents and adolescents in family cohesion (Beta: -1.307, 95% CI: -2.074,-0.539; p=0.014) and family conflict(Beta: -0.665, 95% CI: -0.919,-0.410; p=0.037), the worse the therapeutic effect of NSSI might be.
Discussion: There were certain differences in the cognition of family relationships between parents and adolescents, and subjective family relationship cognition and cognitive differences had a significant effect on the treatment effect of NSSI in adolescents. Helping them identify the cause of cognitive differences and conducting systematic family therapy from the points of difference may be another perspective to improve the treatment effect of NSSI in adolescents.
Non-suicidal self-injury (NSSI) is characterised by intentional, direct, and repeated injury or destruction of one’s own body tissues without suicidal intention, and its incidence rate in adolescence is reported to be between 7.3 and 17.2% (1–3). The incidence rate of NSSI is higher among adolescents with psychological disorders than among adolescents without psychological disorders. Data from a mental health center in China showed that from 2016 to 2021, the proportion of mental disorders combined with NSSI increased from 29.2 to 95.9% (4).
The prevalence of NSSI peaks in mid-adolescence (approximately age 15–16 years) and decreases in late adolescence (approximately age 18 years) (5, 6). Although the prevalence of NSSI is significantly reduced in late adolescence, adolescents with repetitive NSSI appear to have other dysfunctional behaviors even after the treatment of NSSI. A recent study has suggested that adolescents who stop repeating NSSI are likely to exhibit high levels of substance abuse (7). In addition, NSSI is a significant risk factor for suicide attempts and suicides (8, 9). There is an approximately 30-fold higher suicide risk in patients with NSSI compared with the general population (10, 11).
Previously, NSSI was considered a symptom of borderline personality disorder (12). However, recently, most studies tend to consider NSSI an independent mental disorder (13, 14). Current studies have demonstrated that NSSI behaviors are mainly affected by individual psychological, environmental, and neurobiological factors. NSSI behavior is not the result of a single factor but the result of a combination of neurobiological factors related to genetics and acquired factors, such as personality, family, and adverse life events (15–18). This behavior may occur in isolation or in association with several specific psychiatric syndromes. Therefore, there are no unified international treatment guidelines for NSSI. For patients with other mental diseases, a targeted medication for complications is required. However, there are no specific drugs available for the treatment of NSSI. Moreover, different patients have significantly different treatment effects. Improving the therapeutic effect in patients with NSSI is an urgent problem that needs to be solved.
Environmental factors, especially the family environment, are the primary factors for adolescent growth and development, which have an important effect on adolescent mental health and are closely related to adolescent self-awareness, behaviors, and psychological symptoms (19–21). Previous studies have mainly focused on the effects of objective family environment on NSSI in adolescents. However, family relationships are interpersonal relationships between family members. In addition to the objective family environment, family members’ subjective cognition of the family environment is also important (22, 23). Moreover, our previous study found significant differences between parents and adolescents in their cognition of the familyenvironment.
Thus, we conducted a 1 year prospective cohort study on patients with NSSI. This study collected the family environment cognition data of adolescents and their parents and the treatment effects of NSSI. This study aimed to explore the effects of family environment cognition and cognitive differences perceived by adolescents and their parents on the treatment effects of NSSI in adolescents and to provide more potential perspectives for NSSI treatment.
The present study was embedded in the Longitudinal Psychosomatic Disease Study (LoPDS), an ongoing psychosomatic disease cohort study in adolescents conducted in Chengdu that aims to determine the relative contributions of biological factors and the environment to the development and prognosis of psychosomatic diseases (Chinese Clinical Trial Registry ChiCTR2200059437). This study was approved by the Ethics Committee of the Fourth People’s Hospital of Chengdu (No. 201830). This prospective sub-cohort study was conducted at the Fourth People’s Hospital of Chengdu and recruited all adolescents who engaged in NSSI behaviors between January 2019 and December 2020. Written informed consent was obtained from all participants and their parents or guardians. Patients with generalised developmental disorders, intellectual disability, schizophrenia pedigree, drug abuse, or other severe somatic diseases were excluded to reduce confusion.
Patients aged <12 or > 18 years were not included in this study. Those who were unable to participate in follow-ups and were unable to conduct the standardised questionnaire assessment were considered to have dropped out. Simultaneously, we invited one of the adolescents’ parents/guardians to complete the questionnaires at baseline. All adolescents needed to complete the subsequent three follow-ups at 3 months, 6 months, and 1 year thereafter. At each follow-up visit, patients were interviewed in the outpatient clinic or by telephone to determine their current condition. A total of 350 adolescents with NSSI behaviors as part of the LoPDS study were initially recruited for this subgroup study. After excluding parent–adolescent pairs who did not meet the inclusion criteria or did not complete a standardised questionnaire assessment, suicide, or were unable to participate in follow-up, the final analysis included 199 parent–adolescent pairs with NSSI, which can meet the quantity for statistical analysis.
Standardised questionnaires (Supplementary File 1) were used to collect the sociodemographic data of participants (including sex, age, educational background, parents’ marital status, parents’ educational background, parents’ age, and family life structure).
The Family Environment Scale-Chinese Version (FES-CV) (Supplementary File 2) was used to collect the perception of the participants’ family relationships at baseline. It can reflect nine aspects of family relationship, including family cohesion, expressiveness, conflict, independence, achievement orientation, intellectual–cultural orientation, active–recreational orientation, moral–religious emphasis, organization, and control (24, 25). The FES-CV was revised and rewritten by Fei Lipeng et al. in 1991 based on the Family Environment Scale (FES) prepared by Moss, an American psychologist, which has acceptable internal consistency and retest reliability in the Chinese population (26). Cognitive differences in family relationships between adolescents and their parents were defined as the differences between the scores of each item of the parents’ FES-CV and the scores of adolescents’ FES-CV.
The NSSI behavior questionnaire (Supplementary File 3) was used to evaluate the NSSI behaviors of participants at the time of enrolment, after 3 months treatment, 6 months treatment, and 1 year treatment. This questionnaire contains three parts: the first part is the participant’s self-assessment of the impulse to self-harm in the past 2 weeks, selected according to “0–10 points”, with the degree assessed from nothing to strong. The second part assesses the total number of self-injuries in the last 2 weeks, including self-injury behaviors without evident tissue injury and self-injury behaviors with significant tissue damage. The third part assesses whether the participant has had the urge to self-harm and the frequency of self-injury impulse in the past 2 weeks and uses a 7-level score to classify and select according to the frequency of self-injury impulse: grade 1 is once every 2 weeks; grade 2, once a week; grade 3, twice a week; grade 4, more than thrice a week; grade 5, more than five times a week; grade 6, an average of one time per day; and grade 7, an average of more than two times a day. Within a year, there were a total of 4 follow-up visits: at the time of enrolment, after 3 months treatment, 6 months treatment, and 1 year treatment.
According to the 5th Edition of the Diagnostic and Statistical Manual of Mental Disorders (27, 28), NSSI was diagnosed based on the description that the individual has, on 5 or more days, engaged in intentional self-inflicted damage to the surface of his or her body in the last year, of a sort likely to induce bleeding, bruising, or pain (e.g., cutting, burning, stabbing, hitting, and excessive rubbing), for purposes not socially sanctioned (e.g., body piercing and tattooing), but performed with the expectation that the injury will lead to only minor or moderate physical harm.
Recently, there are no unified international treatment guidelines for NSSI. At our hospital, the commonly used therapeutic methods in clinical practice are mainly divided into psychological, drug, and physical therapies (29–31). In our cohort, all patients were treated using a combination of medical, physical, and psychological approaches after enrolment by psychiatrists or medical technicians who have received professional training. All participants were administered Food and Drug Administration-approved antidepressants (sertraline/fluoxetine) for the treatment of anxiety and depression and mood stabilisers (lithium carbonate or valproate) to stabilise their mood. Group psychotherapy and repeated transcranial magnetic stimulation therapy were administered 5 times a week after enrolment during the first month of treatment and after 1 month, with medication maintenance therapy.
All statistical analyses were performed using the Statistical Package for the Social Sciences version 25.0 (IBM Corp., Armonk, NY, United States). The chi-squared or Fisher’s exact test was used to assess categorical data, which were reported as counts and percentages. The means and standard deviations of continuous variables were calculated using Student’s t-test, least significant difference Student’s t-test, one-way analysis of variance, or non-parametric test. Multiple linear regression analysis was performed to explore the association between the treatment effects of NSSI and parental/adolescent family environment cognition or the difference between them. Covariates were selected according to the significantly different variables in the univariate analysis and factors reported in previous studies that would affect the dependent variable. All tests were two-tailed, and statistical significance was set at p < 0.05.
The selection process of the study population is shown in Figure 1. A total of 350 adolescents with NSSI behaviors as part of the LoPDS study were initially recruited for this subgroup study. After excluding parent–adolescent pairs who did not meet the inclusion criteria or did not complete a standardised questionnaire assessment, suicide, or were unable to participate in follow-up, the final analysis included 199 parent–adolescent pairs with NSSI. The descriptive data of the study participants are shown in Table 1. The average age at baseline was 15.44 ± 1.90 years, 87.9% of the participants were female, and 58.3% lived in the city. Moreover, 94.5 of the participants were still at school, and 30.1% of their parents had been divorced or remarried. Approximately half of the adolescents were left-behind children, and 10.9% had a family history of psychosis. The main diagnoses of the participants were as follows: depressive episode (43.5%), anxiety disorder (16.9%), post-traumatic stress disorder (9.0%), bipolar disorder (8.0%), personality disorder (7.0%), and obsessive-compulsive disorder (14.6%).
During treatment, the patients in the cohort were continuously followed up at baseline, after 3 months treatment, 6 months treatment, and 1 year treatment. The perceived self-injury impulse score in the last 2 weeks, self-injury impulse frequency in the last 2 weeks, and total number of self-injuries in the last 2 weeks were used to assess the therapeutic effect, which all dropped significantly (p < 0.001) (Table 2).
Further comparing the subjective perception differences in family relationships between parents and adolescents, the results showed that adolescents with NSSI rated positive family relationships (family cohesion, expressiveness, independence, active–recreational orientation, moral–religious emphasis, and organization) lower than their parents, but they had a higher perception of family conflict than their parents (p < 0.05). There was no significant difference in parent–adolescent’s cognition of family achievement orientation and intellectual–cultural orientation (Table 3).
Although patients with NSSI have evident therapeutic effects in general, there are significant differences among individuals. Therefore, the 2 weeks total number of self-injury differences between the 1 year treatment and baseline was used as the evaluation standard of the treatment effect to further analyse the influence of family environment factors on the treatment effect of patients with NSSI. After adjusting for age, sex, family history of psychosis, left-behind children, and partial content of FES, the results revealed correlations between the treatment effect of NSSI and adolescent family cohesion, adolescent family conflict, parental family expressiveness, and parental family active–recreational orientation. The higher the adolescent family cohesion (beta, 1.130; 95% confidence interval [CI], 0.886–1.373; p = 0.032), parental family expressiveness (beta, 0.818; 95% CI, 0.375–1.260; p = 0.037), and parental family active–recreational orientation score (beta, 0.609; 95% CI, 0.236–0.981; p = 0.048), the better the treatment effect. However, higher adolescent family conflict (beta, −0.838; 95% CI, −1.377 to −0.298; p = 0.024) was associated with lower treatment outcomes (Table 4).
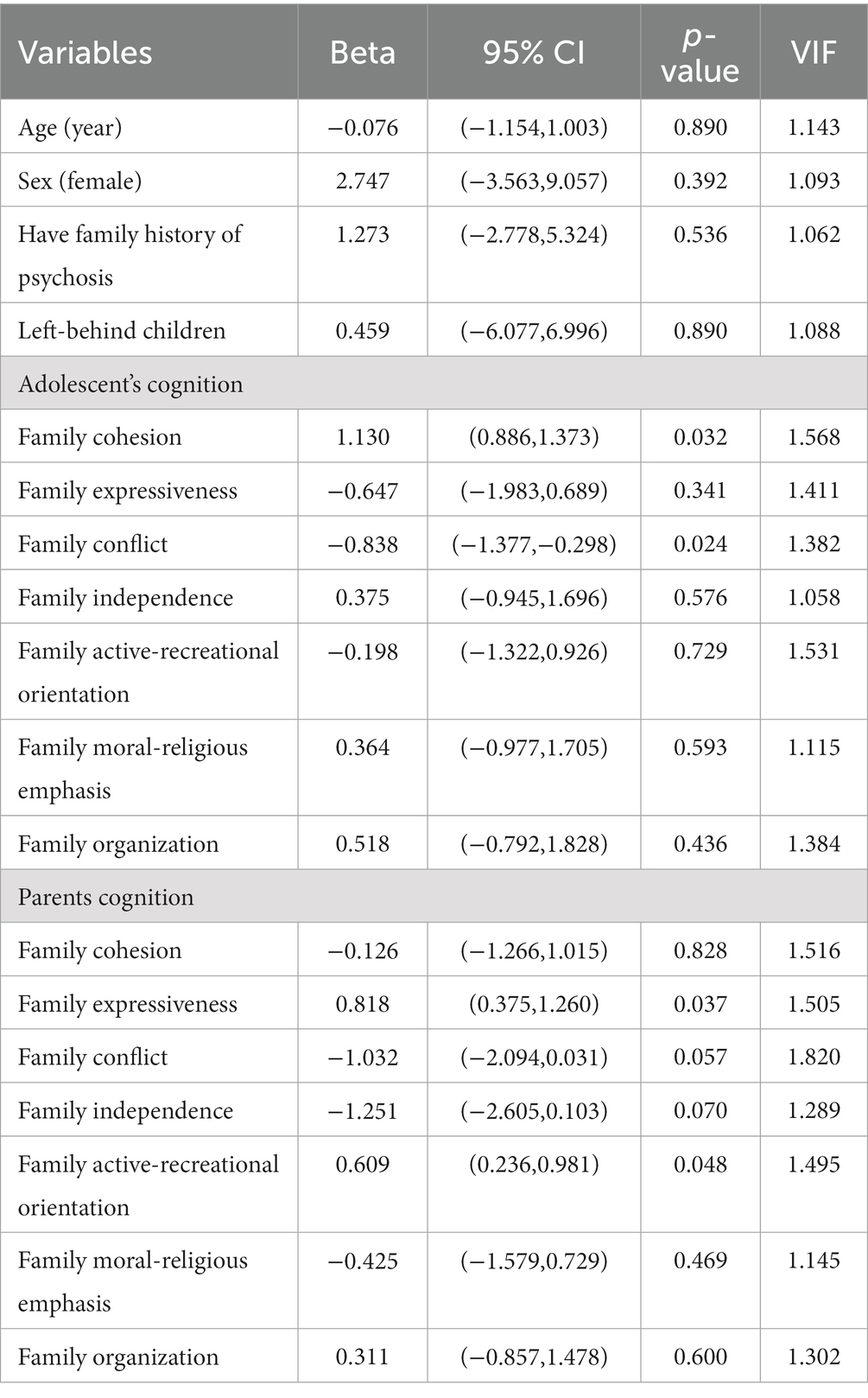
Table 4. Association between the parental and adolescent family cognition and treatment effect of NSSI.
Considering the significant differences between parents and adolescents in their subjective perceptions of family relationships, multiple linear regression analysis was performed to analyse the effects of parent–adolescent cognitive differences in family relations (parent score − teenager score) on the therapeutic effects of NSSI. After adjusting for age, sex, family history of psychosis, and left-behind children, parent–adolescent perceptions of family cohesion and family conflict were significantly related to the treatment effect. Differences between parents and adolescents in family cohesion (beta, −1.307; 95% CI, −2.074 to −0.539; p = 0.014) and family conflict (beta, −0.665; 95% CI, −0.919 to −0.410; p = 0.037) would reduce the treatment effect. The greater the cognitive difference between parents and adolescents in family cohesion and conflict, the worse the therapeutic effect of NSSI (Table 5).

Table 5. Association between the family cognitive differences of parents and adolescents and treatment effect of NSSI.
Binary logistic regression was used to explore the association between the occurrence of suicide and family environmental factors. After adjusting for the family structure and contents of the FES, the results revealed correlations between the occurrence of suicide and age, sex, family history of psychosis, left-behind children, adolescent family conflict, adolescent family independence, and parental family expressiveness. Female sex (odds ratio [OR], 6.921; 95% CI, 2.826–16.945; p < 0.001), family history of psychosis (OR, 4.023; 95% CI, 1.791–12.589; p = 0.080), and left-behind children (OR, 3.831; 95% CI, 3.013–9.410; p = 0.010) increased the risk of suicide by 6.9, 4.0, and 3.8, respectively. Moreover, the risk of suicide was reduced by 27.9% when age increased by 1 year (OR, 0.721; 95% CI, 0.558–0.931; p = 0.012). Regarding the association between the occurrence of suicide and parental and adolescent family cognition, the risk of suicide reduced by 26.0 and 37.3% when adolescent family independence and parental family expressiveness increased by 1 score, respectively. However, the risk of suicide increased by 39.6% when adolescent family conflict increased by 1 score (Supplementary Table S1).
In this 1 year prospective preliminary study, we investigated parent–adolescent family relationship cognition data and analysed the influence of cognition and cognitive differences on the treatment effect of NSSI. This study found that adolescents’ perceptions of family cohesion, adolescent family conflict, parental family expressiveness, and parental family active–recreational orientation affected the efficacy of NSSI treatment in adolescents. Differences in adolescent and parental cognition of family cohesion and family conflict were also strongly associated with NSSI outcomes.
In our cohort, the proportion of girls in the test was significantly higher than that of boys. A previous study has demonstrated that the rate of self-mutilation in women is higher than that in men. This may be because adolescent girls are more precocious than boys, and their sex and self-awareness gradually increases. Although the level of intelligence is significantly improved due to changes in hormone levels, the psychological state and emotional regulation ability of some girls will become unstable (32–34). Nearly half of them are left-behind children. An unstable family relationship may lead to more social adjustment problems among adolescents (35, 36). Parents go out to work, resulting in adolescents getting less parental care, easily having a sense of alienation from their parents and forming a negative perception of the unfavourable situation, and then inducing negative emotions and NSSI behaviors. The lack of parental care has a significant positive predictive effect on the behaviors of adolescents with NSSI (37). A complete family structure is conducive to the play of good family functions and is the foundation for the healthy physical and mental development of adolescents.
Consistent with previous studies, this study found that adolescents with NSSI consistently rated the positives in family relationships lower than their parents (38, 39). In other words, adolescents tend to view family relationships as negative. Adolescents reported higher levels of family conflict than parents, whereas their intimacy and emotional expressions were lower than those of their parents (40, 41). They are more likely to be dissatisfied with their families than their parents are. During adolescence, important changes occur in family relations, and there is a sharp increase in intergenerational conflicts or differences between parents and children. The increase in intergenerational conflict affects differences in parents’ and adolescents’ perceptions of family relationships and the quality of parenting. Differences in the perception of family relationships between adolescents and parents may reflect poor family adjustment during adolescent growth. Adolescents tend to strive for greater autonomy and try to renegotiate their family relationships (42). Cognitive changes enable adolescents to question others’ views (43). If parents are unable to perceive and support such development or if adolescents are unable to adapt to such development, they may develop cognitive and emotional dysfunctions, and further maladaptive behaviors, such as NSSI, will occur.
Notably, this study suggests that the higher the scores of adolescents’ perception of family cohesion, the more NSSI behavior decreases after 1 year; the higher the adolescent family conflict, the worse the effect of NSSI treatment. Family cohesion reflects the emotional connection between personal perception and family and is an indicator of family intimacy and a positive family atmosphere (29, 30). Individuals who grow up in unhealthy family relationships cannot reasonably regulate their emotions or take extreme measures (such as NSSI) when facing negative emotions. Individuals with high family cohesion are conducive to the formation of positive, optimistic, and other good psychological traits in the process of growth and are more able to reasonably deal with negative events (44, 45).
Parental positive cognition of family expressiveness and family active–recreational orientation helps adolescents reduce the occurrence of NSSI behaviors, which may be due to parental emotional expression and communication activities for their children, affecting their future behavioral cognition, emotional expression, and emotion regulation (19, 46). In addition, adolescents are in a critical period of independent needs and independent consciousness development, and parents will try to control their children through strong control of the changes in parent–child relationship during this period, reduce family entertainment activities, and try to increase their connection with children. Adolescents experience a sense of contradiction in the intense conflict between autonomous development and parental control, and to get rid of their parents’ shackles and realise the desire for independent exploration, they will see parental control as a risk factor that threatens their independence and even normal intimate relationships as a threat. To further confirm the independence of the self, it will prove itself by considering NSSI behaviors (21, 47). Thus, parents can improve their parent–child relationship through positive emotional expression, which is conducive to enhancing emotional communication with children, thus improving the closeness between parents and children, forming a virtuous circle of parent–child relationships, and helping to cultivate children’s good behaviors. Simultaneously, parents reduce the control over adolescents, provide children more power to make independent choices, allow adolescents to express different views, and accept children’s negative emotions, which may be helpful in preventing and reducing the occurrence of NSSI behaviors.
Cognitive differences between parents and children regarding family relationships were mainly concentrated in the evaluation of family cohesion and conflict, which significantly affected the treatment effect of adolescent NSSI behaviors (48–50). When a child has already committed self-harm, if there is a lack of emotional resonance between parents and children and there is no sense of family intimacy or family conflict, parents cannot truly understand and accept the child’s emotional changes and self-harming behaviors, increasing family conflict. An increase in family conflict may, in turn, lead to the frequent occurrence of NSSI and poor treatment effects. According to the strain theory, when an individual encounters a certain crisis situation, is at a certain pressure for a long time, and does not have sufficient ability to cope, he/she will experience coping with torque, and the extreme torque consequence is self-harm or even suicide (51–53). When parents and children have the same feelings about the family relationship, both parties believe that family cohesion is higher and family conflict is less, reflecting a warm and safe positive parent–child relationship, which is a protective factor for bad behaviors. If both parties feel a low degree of family cohesion and family conflicts, adequate family support and social support need to be provided during the treatment process, and psychological intervention can be actively provided, which can effectively improve the occurrence of NSSI behaviors in adolescents (36, 54, 55).
The strengths of our study are the specialised study population and large sample size. The study participants were screened using the inclusion and exclusion criteria. Patients with generalised developmental disorders, mental disorders, schizophrenia pedigree, or other psychotic disorders were excluded to reduce confusion. Additionally, the effect of NSSI treatment in adolescents was tracked throughout the 1 year follow-up, resulting in a comprehensive study design. As there are several scales that need to be filled out accurately by the participants and their parents, collecting and obtaining study data is time-consuming. As a result, recruiting and follow-up such a large sample of patients with NSSI at a single hospital for 1 year is challenging. Our hospital is one of the largest and most professional psychiatric hospitals in Southwest China. As a result, we were able to examine such important diseases in a large patient cohort.
This preliminary study has significantly contributed to our understanding of the potential effects of parent–adolescent family relationship cognition and cognitive differences on the treatment effect of NSSI. However, this study has some limitations. First, all data were obtained using self-completed questionnaires, with some degree of reporting bias. Second, parent–adolescent family cognitive data were only collected at baseline, failing to assess changes in their cognition of family relationships during treatment. It was best to evaluate their family relationship cognitive data after 1 year follow-up to explore the effects of improved NSSI in adolescents on family relationship cognition. Third, owing to the wide gap between rich and poor among regions in China, NSSI-related variables, such as economic conditions or regions, were limited. To further understand the potential effects of parent–adolescent family relationship cognition and cognitive differences on NSSI in China, a large-scale study involving more regions and populations conducted in multiple centres is required.
There were certain differences in the cognition of family relationships between parents and adolescents, and subjective family relationship cognition and cognitive differences had a significant effect on the treatment effect of NSSI in adolescents. Helping them identify the cause of cognitive differences and conducting systematic family therapy from the points of difference may be another perspective to improve the treatment effect of NSSI in adolescents.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was approved by the Ethics Committee of the Fourth People’s Hospital of Chengdu (No. 96 201830). Written informed consent was obtained from all participants and their parents or guardians.
YalL and XL designed the research protocol, analysed the data, and drafted the manuscript. ND conducted the study and provided the funding resources. YuL, YX, CL, JC, YaoL, LL, DS, JJ, HC, and TL critically revised the manuscript. All authors contributed to the article and approved the submitted version.
Financial support of this work was provided by Sichuan Medical Association (Q20017), Chengdu Municipal Health Commission (2021103 and 2022441), and Sichuan Provincial Department of Science and Technology (2023YFS0219 and 2023YFS0228). The funding agencies did not have any role in the design of the study, collection, analysis, and interpretation of data, and in writing the manuscript.
The authors would like to thank all the participants and researchers who contributed to this cohort study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1183916/full#supplementary-material
1. Dunlop, BJ, Hartley, S, Oladokun, O, and Taylor, PJ. Bisexuality and non-suicidal self-injury (NSSI): a narrative synthesis of associated variables and a meta-analysis of risk. J Affect Disord. (2020) 276:1159–72. doi: 10.1016/j.jad.2020.07.103
2. Kim, H, Ryu, JM, and Kim, HW. Characteristics and trends of suicide attempt or non-suicidal self-injury in children and adolescents visiting emergency department. J Korean Med Sci. (2020) 35:e276. doi: 10.3346/jkms.2020.35.e276
3. Ye, Z, Xiong, F, and Li, W. A meta-analysis of co-occurrence of non-suicidal self-injury and suicide attempt: implications for clinical intervention and future diagnosis. Front Psych. (2022) 13:976217. doi: 10.3389/fpsyt.2022.976217
4. Du, N, Ouyang, Y, Xiao, Y, and Li, Y. Psychosocial factors associated with increased adolescent non-suicidal self-injury during the COVID-19 pandemic. Front Psych. (2021) 12:743526. doi: 10.3389/fpsyt.2021.743526
5. Buelens, T, Luyckx, K, Verschueren, M, Schoevaerts, K, Dierckx, E, Depestele, L, et al. Temperament and character traits of female eating disorder patients with(out) non-suicidal self-injury. J Clin Med. (2020) 9:1207. doi: 10.3390/jcm9041207
6. Wilkinson, PO, Qiu, T, Jesmont, C, Neufeld, SAS, Kaur, SP, Jones, PB, et al. Age and gender effects on non-suicidal self-injury, and their interplay with psychological distress. J Affect Disord. (2022) 306:240–5. doi: 10.1016/j.jad.2022.03.021
7. Nakar, O, Brunner, R, Schilling, O, Chanen, A, Fischer, G, Parzer, P, et al. Developmental trajectories of self-injurious behavior, suicidal behavior and substance misuse and their association with adolescent borderline personality pathology. J Affect Disord. (2016) 197:231–8. doi: 10.1016/j.jad.2016.03.029
8. Andover, MS, Morris, BW, Wren, A, and Bruzzese, ME. The co-occurrence of non-suicidal self-injury and attempted suicide among adolescents: distinguishing risk factors and psychosocial correlates. Child Adolesc Psychiatry Ment Health. (2012) 6:11. doi: 10.1186/1753-2000-6-11
9. Hawton, K, Bergen, H, Cooper, J, Turnbull, P, Waters, K, Ness, J, et al. Suicide following self-harm: findings from the multicentre study of self-harm in England, 2000–2012. J Affect Disord. (2015) 175:147–51. doi: 10.1016/j.jad.2014.12.062
10. Overs, BJ, Roberts, G, Ridgway, K, Toma, C, Hadzi-Pavlovic, D, Wilcox, HC, et al. Effects of polygenic risk for suicide attempt and risky behavior on brain structure in young people with familial risk of bipolar disorder. Am J Med Genet B Neuropsychiatr Genet. (2021) 186:485–507. doi: 10.1002/ajmg.b.32879
11. Zalsman, G, Levy, Y, Sommerfeld, E, Segal, A, Assa, D, Ben-Dayan, L, et al. Suicide-related calls to a national crisis chat hotline service during the COVID-19 pandemic and lockdown. J Psychiatr Res. (2021) 139:193–6. doi: 10.1016/j.jpsychires.2021.05.060
12. Spitzen, TL, Tull, MT, Baer, MM, Dixon-Gordon, KL, Chapman, AL, and Gratz, KL. Predicting engagement in nonsuicidal self-injury (NSSI) over the course of 12 months: the roles of borderline personality disorder pathology and emotional consequences of NSSI. J Affect Disord. (2020) 277:631–9. doi: 10.1016/j.jad.2020.08.049
13. Naifeh, JA, Nock, MK, Dempsey, CL, Georg, MW, Bartolanzo, D, Ng, THH, et al. Self-injurious thoughts and behaviors that differentiate soldiers who attempt suicide from those with recent suicide ideation. Depress Anxiety. (2020) 37:738–46. doi: 10.1002/da.23016
14. Zhou, R, Zhang, JJ, Liu, YD, Chen, HB, Wang, SB, Jia, FJ, et al. Internet addiction in adolescent psychiatric patient population: a hospital-based study from China. Clin Child Psychol Psychiatry, 13591045221115289. (2022) 28:199–211. doi: 10.1177/13591045221115289
15. Cai, S, Guo, Z, Wang, X, Huang, K, Yuan, K, and Huang, L. Cortical thickness differences are associated with cellular component morphogenesis of astrocytes and excitatory neurons in nonsuicidal self-injuring youth. Cereb Cortex. (2022) 33:811–22. doi: 10.1093/cercor/bhac103
16. Ho, TC, Walker, JC, Teresi, GI, Kulla, A, Kirshenbaum, JS, Gifuni, AJ, et al. Default mode and salience network alterations in suicidal and non-suicidal self-injurious thoughts and behaviors in adolescents with depression. Transl Psychiatry. (2021) 11:38. doi: 10.1038/s41398-020-01103-x
17. Mürner-Lavanchy, I, Koenig, J, Reichl, C, Brunner, R, and Kaess, M. Altered resting-state networks in adolescent non-suicidal self-injury-a graph theory analysis. Soc Cogn Affect Neurosci. (2022) 17:819–27. doi: 10.1093/scan/nsac007
18. Pollak, OH, Kwon, SJ, Jorgensen, NA, Lindquist, KA, Telzer, EH, and Prinstein, MJ. Neural reactivity to social punishment predicts future engagement in nonsuicidal self-injury among peer-rejected adolescents. Biol Psychiatry. (2022) 94:40–9. doi: 10.1016/j.biopsych.2022.09.030
19. Deng, Y, Li, M, Wang, H, Li, J, He, X, and Yu, C. Parent-adolescent conflict, depressive symptoms, and non-suicidal self-injury among Chinese adolescents: the moderating effect of the COMT gene rs4680 polymorphism. Int J Environ Res Public Health. (2022) 19:10567. doi: 10.3390/ijerph191710567
20. Lan, Z, Pau, K, Mohd Yusof, H, and Huang, X. Hierarchical topological model of the factors influencing adolescents’ non-suicidal self-injury behavior based on the DEMATEL-TAISM method. Sci Rep. (2022) 12:17238. doi: 10.1038/s41598-022-21377-z
21. Xu, H, Jiang, Z, Li, S, Zhang, X, Xu, S, Wan, Y, et al. Differences in influencing factors between non-suicidal self-injury and suicide attempts in Chinese adolescents: the role of gender. Front Psych. (2022) 13:870864. doi: 10.3389/fpsyt.2022.870864
22. Schiffler, T, Seiler-Ramadas, R, Štefanac, S, Haider, S, Mües, HM, and Grabovac, I. Implementation of a mobile DBT app and its impact on suicidality in transitional age youth with borderline personality disorder: a qualitative study. Int J Environ Res Public Health. (2022) 19:701. doi: 10.3390/ijerph19020701
23. Westers, NJ, Needham, HE, and Walsh, JB. Effectiveness of a curriculum for pediatric residents to address adolescent nonsuicidal self-injury. Acad Psychiatry. (2022) 47:18–24. doi: 10.1007/s40596-022-01684-3
24. Gorenstein, G, Gorenstein, C, de Oliveira, MC, Asbahr, FR, and Shavitt, RG. Child-focused treatment of pediatric OCD affects parental behavior and family environment. Psychiatry Res. (2015) 229:161–6. doi: 10.1016/j.psychres.2015.07.050
25. Yu, Y, Yang, X, Yang, Y, Chen, L, Qiu, X, Qiao, Z, et al. The role of family environment in depressive symptoms among university students: a large sample survey in China. PLoS One. (2015) 10:e0143612. doi: 10.1371/journal.pone.0143612
26. Phillips, MR, West, CL, Shen, Q, and Zheng, Y. Comparison of schizophrenic patients’ families and normal families in China, using Chinese versions of FACES-II and the family environment scales. Fam Process. (1998) 37:95–106. doi: 10.1111/j.1545-5300.1998.00095.x
27. Wilkinson, P, and Goodyer, I. Non-suicidal self-injury. Eur Child Adolesc Psychiatry. (2011) 20:103–8. doi: 10.1007/s00787-010-0156-y
28. Zulauf Logoz, M . The revision and 5th edition of the diagnostic and statistical manual of mental disorders (DSM-5): consequences for the diagnostic work with children and adolescents. Prax Kinderpsychol Kinderpsychiatr. (2014) 63:562–76. doi: 10.13109/prkk.2014.63.7.562
29. Rizvi, SL, and Fitzpatrick, S. Changes in suicide and non-suicidal self-injury ideation and the moderating role of specific emotions over the course of dialectical behavior therapy. Suicide Life Threat Behav. (2021) 51:429–45. doi: 10.1111/sltb.12691
30. Rootes-Murdy, K, Carlucci, M, Tibbs, M, Wachtel, LE, Sherman, MF, Zandi, PP, et al. Non-suicidal self-injury and electroconvulsive therapy: outcomes in adolescent and young adult populations. J Affect Disord. (2019) 250:94–8. doi: 10.1016/j.jad.2019.02.057
31. Walton, CJ, Bendit, N, Baker, AL, Carter, GL, and Lewin, TJ. A randomised trial of dialectical behavior therapy and the conversational model for the treatment of borderline personality disorder with recent suicidal and/or non-suicidal self-injury: an effectiveness study in an Australian public mental health service. Aust N Z J Psychiatry. (2020) 54:1020–34. doi: 10.1177/0004867420931164
32. Greene, D, Hasking, P, and Boyes, M. The associations between alexithymia, non-suicidal self-injury, and risky drinking: the moderating roles of experiential avoidance and biological sex. Stress Health. (2019) 35:457–67. doi: 10.1002/smi.2879
33. Kądziela-Olech, H, Zak, G, Kalinowska, B, Wągrocka, A, Perestret, G, and Bielawski, M. The prevalence of non-suicidal self-injury (NSSI) among high school students in relation to age and sex. Psychiatr Pol. (2015) 49:765–78. doi: 10.12740/psychiatriapolska.pl/online-first/3
34. Wang, S, Xu, H, Zhang, S, Wan, Y, and Tao, F. Mediating effects of self-esteem in the relationship between childhood maltreatment and non-suicidal self-injury among adolescents: the roles of sex and only-child status. Soc Sci Med. (2020) 249:112847. doi: 10.1016/j.socscimed.2020.112847
35. Wang, Q, and Liu, X. Child abuse and non-suicidal self-injury among Chinese migrant adolescents: the moderating roles of beliefs about adversity and family socioeconomic status. J Interpers Violence, 8862605221104537. (2022) 38:3165–90. doi: 10.1177/08862605221104537
36. Wang, Y, Luo, B, Hong, B, Yang, M, Zhao, L, and Jia, P. The relationship between family functioning and non-suicidal self-injury in adolescents: a structural equation modeling analysis. J Affect Disord. (2022) 309:193–200. doi: 10.1016/j.jad.2022.04.124
37. You, J, and Leung, F. The role of depressive symptoms, family invalidation and behavioral impulsivity in the occurrence and repetition of non-suicidal self-injury in Chinese adolescents: a 2-year follow-up study. J Adolesc. (2012) 35:389–95. doi: 10.1016/j.adolescence.2011.07.020
38. Martin-Storey, A, Dirks, M, Holfeld, B, Dryburgh, NSJ, and Craig, W. Family relationship quality during the COVID-19 pandemic: the value of adolescent perceptions of change. J Adolesc. (2021) 93:190–201. doi: 10.1016/j.adolescence.2021.11.005
39. Wong, RS, Tung, KTS, Wong, WHS, Ho, FKW, Tso, WWY, Yip, PSF, et al. Associations of family meals with adolescent perception of family relationship and compliance with parental guidance in Hong Kong: results of a representative cross-sectional survey. Int J Environ Res Public Health. (2021) 18:5402. doi: 10.3390/ijerph18105402
40. Haines, J, Rifas-Shiman, SL, Horton, NJ, Kleinman, K, Bauer, KW, Davison, KK, et al. Family functioning and quality of parent-adolescent relationship: cross-sectional associations with adolescent weight-related behaviors and weight status. Int J Behav Nutr Phys Act. (2016) 13:68. doi: 10.1186/s12966-016-0393-7
41. Kelada, L, Hasking, P, and Melvin, G. The relationship between nonsuicidal self-injury and family functioning: adolescent and parent perspectives. J Marital Fam Ther. (2016) 42:536–49. doi: 10.1111/jmft.12150
42. Smetana, JG, Campione-Barr, N, and Metzger, A. Adolescent development in interpersonal and societal contexts. Annu Rev Psychol. (2006) 57:255–84. doi: 10.1146/annurev.psych.57.102904.190124
43. Anastasiadou, D, Sepulveda, AR, Parks, M, Cuellar-Flores, I, and Graell, M. The relationship between dysfunctional family patterns and symptom severity among adolescent patients with eating disorders: a gender-specific approach. Women Health. (2016) 56:695–712. doi: 10.1080/03630242.2015.1118728
44. Baker, AC, Wallander, JL, Elliott, MN, and Schuster, MA. Non-suicidal self-injury among adolescents: a structural model with socioecological connectedness, bullying victimization, and depression. Child Psychiatry Hum Dev. (2022) 54:1190–208. doi: 10.1007/s10578-022-01319-6
45. Drubina, B, Kökönyei, G, and Reinhardt, M. Associations between non-suicidal self-injury and negative romantic relationship life events in male justice-involved adolescents. BMC Psychiatry. (2021) 21:401. doi: 10.1186/s12888-021-03408-7
46. Yu, L, Zhao, J, Zhao, T, Xiao, Y, Ou, Q, He, J, et al. Multicenter analysis on the non-suicidal self-injury behaviors and related influencing factors-a case study of left-behind children in northeastern Sichuan. J Affect Disord. (2023) 320:161–8. doi: 10.1016/j.jad.2022.09.081
47. Xiao, Q, Song, X, Huang, L, Hou, D, and Huang, X. Global prevalence and characteristics of non-suicidal self-injury between 2010 and 2021 among a non-clinical sample of adolescents: a meta-analysis. Front Psych. (2022) 13:912441. doi: 10.3389/fpsyt.2022.912441
48. Liu, CR, Wan, LP, Liu, BP, Jia, CX, and Liu, X. Depressive symptoms mediate the association between maternal authoritarian parenting and non-suicidal self-injury among Chinese adolescents. J Affect Disord. (2022) 305:213–9. doi: 10.1016/j.jad.2022.03.008
49. Meng, L, Qu, D, Bu, H, Huo, L, Qi, L, Yang, J, et al. The psychosocial correlates of non-suicidal self-injury within a sample of adolescents with mood disorder. Front Public Health. (2022) 10:768400. doi: 10.3389/fpubh.2022.768400
50. Miscioscia, M, Angelico, C, Raffagnato, A, and Gatta, M. Psychopathological and interactive-relational characteristics in non-suicidal self-injury adolescent outpatients. J Clin Med. (2022) 11:1218. doi: 10.3390/jcm11051218
51. Lew, B, Chistopolskaya, K, Liu, Y, Talib, MA, Mitina, O, and Zhang, J. Testing the strain theory of suicide – the moderating role of social support. Crisis. (2020) 41:82–8. doi: 10.1027/0227-5910/a000604
52. Zhang, J, and Lester, D. Psychological tensions found in suicide notes: a test for the strain theory of suicide. Arch Suicide Res. (2008) 12:67–73. doi: 10.1080/13811110701800962
53. Zhang, J, Liu, Y, and Sun, L. Life satisfaction and degree of suicide intent: a test of the strain theory of suicide. Compr Psychiatry. (2017) 74:1–8. doi: 10.1016/j.comppsych.2016.12.002
54. Qian, H, Shu, C, Feng, L, Xiang, J, Guo, Y, and Wang, G. Childhood maltreatment, stressful life events, cognitive emotion regulation strategies, and non-suicidal self-injury in adolescents and young adults with first-episode depressive disorder: direct and indirect pathways. Front Psych. (2022) 13:838693. doi: 10.3389/fpsyt.2022.838693
Keywords: non-suicidal self-injury, adolescent, family environment, prospective study, treatment
Citation: Li Y, Li X, Li Y, Xiao Y, Li C, Chen J, Li Y, Luo L, Su D, Jia J, Cheng H, Liu T and Du N (2023) The effects of family environment cognition and its difference perceived by adolescents and their parents on the treatment effect of non-suicidal self-injury behaviors in adolescents: a 1-year prospective cohort study. Front. Psychiatry. 14:1183916. doi: 10.3389/fpsyt.2023.1183916
Received: 10 March 2023; Accepted: 29 August 2023;
Published: 12 September 2023.
Edited by:
Hanliang Fu, Xi'an University of Architecture and Technology, ChinaCopyright © 2023 Li, Li, Li, Xiao, Li, Chen, Li, Luo, Su, Jia, Cheng, Liu and Du. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Na Du, MTM5MjA3ODUwNTdAMTYzLmNvbQ==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.