- Department of Nursing, Shengjing Hospital of China Medical University, Shenyang, China
Background: Stigma is an important psychological concept that is being studied in many diseases. However, there have been few studies on stigma in renal dialysis patients in China. This study aimed to investigate the level of stigma and its potential influencing factors among Chinese renal dialysis patients.
Methods: A cross-sectional study was conducted among renal dialysis patients in two Chinese dialysis centers between April 2022 and July 2022. Two hundred four renal kidney patients were interviewed with a questionnaire on demographic variables using the Social Impact Scale (SIS), Resilience Scale-14 (RS-14), Herth Hope Index(HHI), Multidimensional Scale of Perceived Social Support (MSPSS), Revised Life Orientation Test(LOT-R), Perceived Stress Scale (PSS-4) and Fear of Progression (FoP). T-test/univariate one-way ANOVA, Pearson’s R, and hierarchical linear regression analysis were used to investigate the factors that influence stigma.
Results: Renal dialysis patients in China experienced a moderate level of stigma (52.36 ± 8.16). Stigma was negatively correlated with resilience, hope, and perceived social support, whereas it was positively associated with perceived stress and fear of progression. However, it showed no significant relationship between optimism and stigma. Hierarchical linear regression analysis showed that hope (β = -0.318, P < 0.001), social support (β = -0.193, P < 0.01), perceived stress (β = 0.197, P < 0.01), and fear of progression (β = 199, P < 0.01) were found to be associated with stigma among the renal dialysis patients. All four variables in the model could explain 34.6% of the variance in stigma among renal dialysis patients in China.
Conclusion: According to this study, renal dialysis patients in China face a moderate level of stigma. Stigma was found to be negatively related to hope and social support but positively associated with perceived stress and fear of progression. Future research on the stigma of renal dialysis patients should include hope-based interventions, proper and specific social support strategies, stress management interventions, and more disease-related information.
1. Introduction
End-stage kidney disease, which is the fifth stage of chronic kidney disease, is the most severe stage of chronic kidney failure caused by various factors (1). The patient’s renal function is completely or nearly completely lost, which seriously threatens the patient’s life (2). It was reported that the number of patients requiring renal replacement therapy ranged from 4.902 to 9.701 million worldwide and that this figure would more than double by 2030 (3). Similar conditions can be found in America (4), Europe (5), China (6), and other countries.
Renal dialysis is the most commonly used treatment for patients with end-stage kidney disease, with more than 90% receiving it. The therapy provides those patients with a potentially longer life span. However, the adverse effects of therapy include low quality of life (7), fatigue (8), sleep disorders (9), anorexia, nausea/vomiting, pruritus, sleepiness, difficulty concentrating, pain (10), which cannot be ignored. In addition to the physical effects, the psychological effects should be considered. It is reported that when patients decide on renal dialysis, they tend to avoid the therapy due to thinking that dialysis is the most stressful part of the disease (11). In addition to distress (12), loss (13), well-being (14), negative coping (15), anxiety (16), depression (17), and so on cannot be ignored as patients on dialysis. Many studies have found that renal dialysis patients’ experience feeling of passivity and restriction (18). They can hardly do their original jobs anymore (19), and their lives must be entirely re-planned to adapt to dialysis. Dialysis patients have low self-esteem, believe they are a burden on their family members and do not contribute to the family. They expose themselves to uncertain future and are hesitant to interact with others (20). These changes are visible and life-long and may result in the absence of individuals from full social acceptance, and patients themselves may have thoughts of escaping society, which corresponds to the concept of stigma.
Stigma describes a deeply discreditable attribute or characteristic, conveying a spoiled social identity and a sense of disgrace in a particular social context, disqualifying the individual from social recognition (21). Stigma is a psychological stress response. Patient’s self-assessment plays a crucial role in the production and formation of stigma (22, 23). Stigma increases the psychological burden of patients, causing them to be labeled, stereotyped, isolated, lose their status, and even face discrimination (24). It will affect the patient’s quality of life and follow-up treatment and even lead to adverse consequences such as social escape and suicide (25). Studies have also shown that stigma reduces self-esteem, self-efficacy, and belief in own abilities (26). Stigma has widely been used in patient populations such as cancer (27), chronic diseases (28), psychiatric disorders (29), addiction diseases (30), obesity (31), and geriatric diseases (32), and so on to provide many new perspectives and findings.
Stigma is an important concept in psychology and has been a research topic for many diseases. Surprisingly, little information is currently available about stigma in renal dialysis patients. Considering such immense pressure and its effect on renal dialysis patients and its importance, stigma should be approached from different perspectives. Therefore, the present study aimed to fill this knowledge gap. Studies examining the stigma associated with other diseases have revealed that, in addition to demographic and clinical characteristics, resilience (33), optimism (34), social support (35, 36), hope (37), perceived stress (38) were all related factors to stigma. Furthermore, renal dialysis was a life-long treatment with multiple complications. Many patients in the chronic kidney disease stage reported their fear of disease progression (39). Excessive fear of disease progression may cause patients to label the disease even more and devalue themselves. Thus, we would explore the relationship of the aforementioned factors in renal dialysis patients from the Chinese population. The hypothesis proposes that stigma is positively associated with stress and fear of progression and negatively associated with resilience, hope, social support, and optimism among renal dialysis patients. Accordingly, we will test this hypothesis in the current study. This study aimed to investigate the level of stigma and its potential influencing factors among Chinese renal dialysis patients. We hope that the findings of our study, particularly the identification of stigmatizing factors, will be useful and shed new light on the management of renal dialysis patients.
2. Materials and methods
2.1. Study settings
This is a cross-sectional designed study that was carried out at two renal dialysis centers in China. Data was collected between April 2022 and July 2022. The Ethics Committee of China Medical University approved this study (2022PS153K).
2.2. Subjects
Patients receiving renal dialysis therapy who understood and completed the questionnaire were invited to participate in the study under their consent, while patients in severe conditions were excluded. The study size was arrived at following the below formula: . The parameters in the study were set as follows: α = 0.05, Zα = 1.96, σ = 10.58 (which was arrived via pre-test), δ = 1.5; therefore, n = 1.962*10.582/1.52 = 191.1. The sample size was increased by 10%∼20%, considering invalid questionnaires, resulting in a final sample size of 211∼230.
2.3. Data collection
The entire research process was anonymous, and the patients were voluntary. The researchers of the study uniformly trained the five investigators. After the patients agreed to participate, the paper questionnaires were filled out in a separate and undisturbed space in the hospital to prevent patients from influencing each other while filling out questionnaires. The investigator is responsible for interpreting the questionnaire items without any incentive. Another trained investigator performed quality control on site. Epidata software (version 3.1) was used for data entry and review.
2.4. Tools
Questionnaires including demographic and clinical characteristics were self-developed in the study. The demographic section included age, gender, education level, job status, religious belief, income, family structure, and medical payments. Also, the clinical variables section included the approach and the course of dialysis of the patient (how long the dialysis lasted).
2.4.1. Stigma
The stigma of the respondents was measured using the Social Impact Scale (SIS) (40). SIS consists of 24 items divided into four categories: social rejection, financial insecurity, internalized shame, and social isolation. Each scale item has a four-point scale, with a total score ranging from 24 to 96. Cronbach’s α of stigma was 0.871 in this study.
2.4.2. Resilience
Resilience was assessed using the Resilience Scale-14 (RS-14) (41). The RS-14 consists of 14 items on a 7-point scale, with an overall score ranging from 14 and 98. In the current study, Cronbach’s α of resilience was 0.863.
2.4.3. Hope
The level of hope was assessed by the Herth Hope Index (HHI) (42). The HHI consists of 12 items, and each item is scored on a 4-point scale. The total HHI score ranges from 12 to 48, and a higher total score reflects a higher level of hope. In the present study, Cronbach’s α of hope was 0.866.
2.4.4. Social support
The Chinese version of the Multidimensional Scale of Perceived Social Support (MSPSS) was used to assess perceived social support (43). The MSPSS comprises ten items scored on a 7-point scale; the total score ranges from 12 to 84, with a higher score indicating more social support. Cronbach’s α of social support was 0.935 in the present research.
2.4.5. Optimism
The 10-item Revised Life Orientation Test (LOT-R) was used to assess optimism (44). The LOT-R uses a 5-point rating system. A higher score indicates a higher level of optimism. Cronbach’s α of optimism was 0.621 in this research.
2.4.6. Perceived stress
The 4-item Perceived Stress Scale (PSS-4) was used to assess perceived stress (45). PSS-4 is scored using a 5-point scale, with a total score ranging from 0 to 16. Higher scores indicate a higher level of perceived stress. Cronbach’s α of perceived stress was 0.764 in this study.
2.4.7. Fear of progression
The Fear of Progression Questionnaire-Short Form (Fo P-Q-SF) was used to assess the Fear of Progression (FoP) (46). The Fo P-Q-SF is a 12-item scale with a 5-point rating and a total score ranging from 12 to 60. A higher score indicates a greater fear of disease progression. Cronbach’s α for fear of progression was 0.895 in the present study.
2.5. Statistical analyses
Data analysis was performed using the statistical software package for social sciences (SPSS 20.0). The significance for all statistical tests was 0.05 (2-tailed). Each continuous variable is first tested for normality and homogeneity of variance. Independent-samples t-tests and one-way ANOVA were used to describe the distribution of stigma for categorical demographic and clinical variables in renal dialysis patients. Pearson’s R-test was used to assess the correlations between resilience, hope, social support, optimism, stress, fear of progress, and stigma. Hierarchical linear regression analysis was used to assess the research hypotheses. To avoid overfitting the regression model, the one-way ANOVA/t-test variable with P < 0.2 was entered as the control variable in the first step of the hierarchical regression analysis (47). Then, the independent variables (resilience, hope, perceived social support, perceived stress, fear of progress) also entered the second step of the hierarchical regression. Diagnostic tests for multicollinearity were performed using tolerance and variance inflation factor (VIF). The data provided by the regression model include standardized regression coefficient (β), R2, adjusted R2 (Adj. R2), R2-change, and F value.
3. Results
3.1. Descriptive statistics
A total of 230 questionnaires were distributed in this study. Twenty patients refused to participate in the survey, and six invalid questionnaires. There were 204 valid questionnaires with an effective response rate of 88.7%.
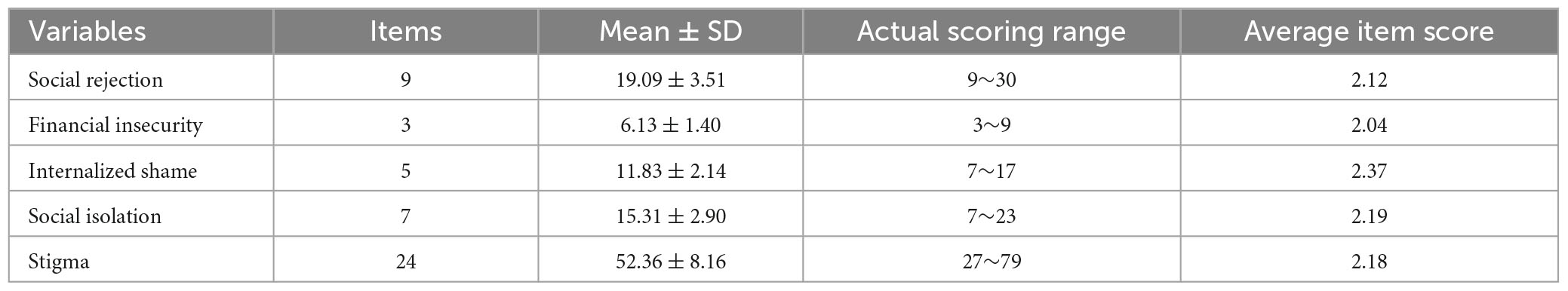
Out of the 204 respondents, 126 (61.8%) were male, and 78 (38.2%) were females. Nearly half of them (46.1%) were above 60 years old. All the patients had medical insurance. Only 12 (5.8%) patients had a regular employee. In terms of clinical variables, most respondents (96.1%) used an autogenous arteriovenous fistula to access dialysis. More than half of the respondents had dialysis for less than five years. Table 1 presents the details.
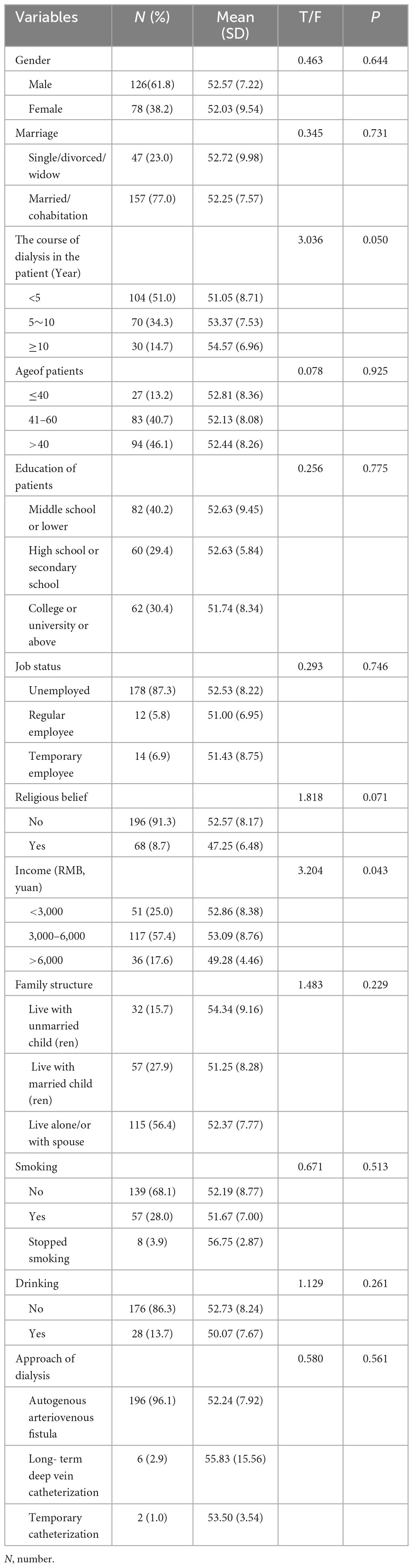
Table 1. Demographic and clinical characteristics and the level of stigma among renal dialysis patients (n = 204).
3.2. Stigma level
Table 2 depicts the level of stigma and its dimensions among renal dialysis patients.
3.3. Correlation among continuous variables
Table 3 depicts the correlation analysis results of resilience, hope, perceived social support, optimism, perceived stress, fear of progression, and stigma among renal dialysis patients. Stigma was negatively correlated with resilience (r = -0.386, P < 0.001), hope (r = -0.448, P < 0.001), perceived social support (r = -0.393, P < 0.001), and positively associated with and perceived stress (r = 0.255, P < 0.001), fear of progression (r = 0.314, P < 0.001). Besides, it showed no significant relationship between optimism and stigma (P > 0.05).
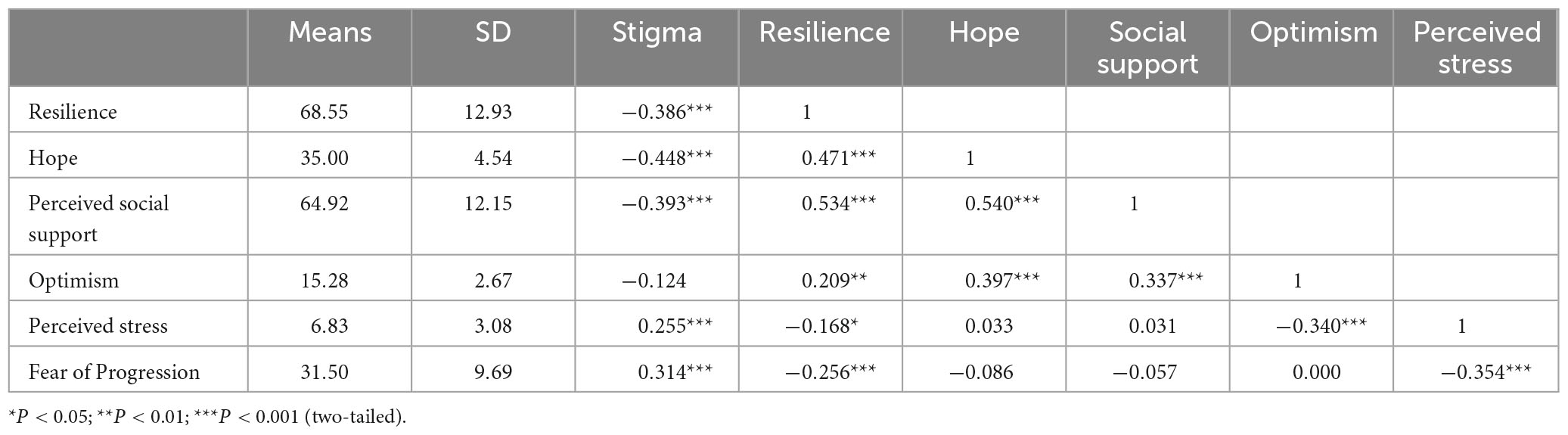
Table 3. Descriptive statistics and correlations in continuous variables among renal dialysis patients (N = 204).
3.4. Hierarchical linear regression analysis
The influencing factors of stigma in renal dialysis patients were investigated using hierarchical linear regression analysis. Multiple regression analysis included variables significantly related to stigma in univariate analysis and variables related to the psychological status of renal dialysis patients. This study included demographic variables (the course of dialysis in the patient, religious belief, and income), resilience, hope, perceived social support, perceived stress, and fear of progression in the regression analysis. Hope (β = -0.318, P < 0.001), social support (β = -0.193, P < 0.01), perceived stress (β = 0.197, P < 0.01), fear of progression (β = 199, P < 0.01) were associated with stigma in renal dialysis patients, with all four variables in the model explaining 34.6% of the variance in stigma in renal dialysis patients. There is no collinearity between the variables (Tolerance > 0.5, VIF < 2). Table 4 lists the details.
4. Discussion
4.1. Stigma levels among renal dialysis patients
There have been a few studies on stigma in dialysis patients. We found that the level of stigma in the study was higher (48) than in previous studies of renal dialysis patients in limited studies. We speculate that this is due to age differences in the target population. Furthermore, we found that the level of stigma among renal dialysis patients was lower than that of some cancer patients (49–51), which could be attributed to the age and job status of patients in the study. In this study, nearly half of the patients (46.1%) were above 60 years old, and only 12 (5.8%) were regular employees. The conditions mentioned above may weaken the social stigma of renal dialysis patients. However, it does not mean that stigma on renal dialysis patients is insignificant. A recent study in Japan quantitatively elucidated dialysis-related stigma in patients on dialysis (52). Renal dialysis patients are subjected to long-term continuous treatment that may last until the end of their lives, disrupting their routines, social interactions, quality of life, mental health, and family life (7) as stigma is impossible to avoid. Some researchers reported that patients with dialysis (53) and chronic kidney disease (54–56) had an unspoken stigma, reminding us that we should pay more attention to stigma among patients with this disease. In terms of dimensions, we found that internalized shame scored highest. Previous studies showed that stigma could be most harmful when internalized (57), which could devalue themselves (58). Besides, the most stigma dialysis patients experienced were internalized shame and social isolation, which were consistent with patients with COPD (59) and diabetes (60). This implies that it is critical to change patients’ inner beliefs, values, idea and give them support in order to reduce the stigma associated with renal dialysis patients.
4.2. Factors associated with stigma among renal dialysis patients
In the present study, hope, social support, perceived stress, and fear of progression were potentially related to stigma among renal dialysis patients.
According to the results of hierarchical linear regression analysis, hope may have the strongest effect on stigma among renal dialysis patients, similar to previous studies on patients with other diseases (37, 61). It has been reported that hope is related to almost all health outcomes (62) for two reasons. Rather, hope is a vital positive psychological variable. Hope is a dynamic life force to expect a good future when facing uncertainty (63). Patients with a high level of hope have a promising attitude to the disease, which is beneficial to avoid devaluing themselves. Conversely, hope has been reported to have a positive effect on resilience (64), quality of life (65), stress (66, 67), anxiety (66), and depression (66) which may reduce the level of stigma indirectly. Furthermore, interventions based on Snyder’s hope theory have been reported effective in reducing the stigma level (68, 69). Therefore, we can take interventions based on hope of reducing the level of stigma in patients.
In the study, perceived social support was another variable that had a positive effect on decreasing the level of stigma among renal dialysis patients; a similar condition has also been found in previous related studies (70, 71). Social support is a vital strength for the patients. It is important to have a high level of social support due to the long-term, uninterrupted nature of the disease. And previous studies have also shown that social support had an important effect in deciding whether patients with end-stage kidney disease should receive dialysis (72). In the literature, social support is divided into instrumental support and emotional support (73). The supports mentioned above were both critical to the patients. However, some studies suggest that dialysis patients’ personal views about their illness can provide insight into whether patients could benefit from support (18, 74). It reminds us that we should pay attention to the thinking, and value of patients. It is in line with some research about social support, which has shown that social support works through hope and resilience (75). Given the preceding discussion, we should focus on using personalized combined with group intervention for dialysis patients in future work to improve the level of social support of patients. The content of the intervention is comprehensive, and the content of the intervention is what the patients need.
It was not surprising that perceived stress was an essential factor in the stigma among renal dialysis patients confirmed in previous studies on other diseases (76, 77). The levels of perceived stress are not the real level of stress but rather the stress that the patient perceives as an event. For the same event, different people may have different stress. The right amount of pressure is beneficial. However, if the patient’s stress perception level is excessive, it means that the disease has a significant impact on them. They usually look at the disease negatively and even look at themselves negatively. The patients may not believe in their future and themselves. The feelings mentioned above may make them more shamed. In this case, the stigma is more likely to arise. Not to mention that the severe disease was taboo and easily associated with uniformed and misinformed social impressions (78). Therefore, managing stress and maintaining it is a crucial issue. A study about stress management training has shown that stigma was reduced after the training (79), suggesting that stress management interventions can be implemented in dialysis patients.
Finally, fear of progression was identified as a significant potential influencing factor of stigma in dialysis patients. The fear of progression has been reported in patients with chronic kidney disease (39) without data on renal dialysis patients. Fear of progression (FoP) is a feeling of worry and fear caused by disease and its treatment that is different from traditional psychological dysfunction (80). The fear of progression in disease has been proved to related to quality of life (81), social function (82), happiness (83), well-being (84), and so on. Patients who are afraid of disease progression are unable to recognize and accept it. Even minor changes in illness can cause emotional panic. The abovementioned factors are detrimental to patients and would cause them to undervalue themselves. For renal dialysis patients, the possibility of disease cure is low. And, to some extent, the development of the disease in a negative direction is known. A high level of fear during the disease development process will make the patient more reluctant to reveal to others and make the patient look down on himself. It will also harm the patient’s treatment and quality of life. In the previous studies, group-based intervention (82) and illness perception (85) have been reported to be effective. Thus, actions and interventions aimed at increasing renal dialysis patients’ knowledge of disease-related information aided in the formation of a good group intervention.
However, in the study, some results were inconsistent with our hypotheses, such as optimism and resilience showed no significant relationship. Therefore, the exact mechanism of action of these two variables still needs further research.
5. Strength and limitations
This study aimed to identify potential factors related to stigma in renal dialysis patients. In this regard, our research provided some new information. The results showed that stigma in kidney dialysis patients were associated with hope, social support, perceived stress, and fear of progression. It emphasizes the significance of changing patients’ inner beliefs, values and ideas. Future work to reduce stigma among renal dialysis patients should include hope-based intervention, proper and specific strategies to improve social support, stress management interventions, and more disease-related information. This result indicated that stigma should be a major focus when dealing with renal dialysis patients.
Causation could not be established in this study due to the cross-sectional design. Future studies should assess whether the intervention can reduce stigma levels in renal dialysis patients. Furthermore, we focused only on the associations between stigma and resilience, hope, perceived social support, optimism, perceived stress, and fear of progress, whereas other factors that might affect stigma have been disregarded. Moreover, larger samples are required to improve representativeness. And the number of questions may limit the quality of the responses. The last but not the least, stigma is multifaceted in nature, dialysis patients experience stigma for multiple reasons, thus additional qualitative studies could be explored in the future research. Despite some limitations, our study provides important new information on stigma in renal dialysis patients with useful clinical implications.
6. Conclusion
According to this study, renal dialysis patients in China face a moderate level of stigma. Stigma was found to be negatively related to hope and social support but positively associated with perceived stress and fear of progression. Future research on the stigma of renal dialysis patients should include hope-based interventions, proper and specific social support strategies, stress management interventions, and more disease-related information.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Committee of China Medical University (2022PS153K). The patients/participants provided their written informed consent to participate in this study.
Author contributions
BL and PX were responsible for conception and design of the study. BL, DL, and YZ performed data extraction. BL did the data analysis and wrote the manuscript. PX contributed to the revision of the manuscript. All authors have reviewed the manuscript and given final approval of the version to be published.
Acknowledgments
We would like to thank all our patients who were willing to take part in the study. We would also like to thank all the reviewers who participated in the review, as well as MJEditor (www.mjeditor.com) for providing English editing services during the preparation of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. (2002) 39(Suppl 2. 1):S1–266.
2. Charles C, Ferris AH. Chronic kidney disease. Primary Care. (2020) 47:585–95. doi: 10.1016/j.pop.2020.08.001
3. Liyanage T, Ninomiya T, Jha V, Neal B, Patrice HM, Okpechi I, et al. Worldwide access to treatment for end-stage kidney disease: a systematic review. Lancet. (2015) 385:1975–82. doi: 10.1016/s0140-6736(14)61601-9
4. Johansen KL, Chertow GM, Gilbertson DT, Herzog CA, Ishani A, Israni AK, et al. US renal data system 2021 annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. (2022) 79:A8–12. doi: 10.1053/j.ajkd.2022.02.001
5. Kramer A, Boenink R, Stel VS, Santiuste de Pablos C, Tomović F, Golan E, et al. The ERA-EDTA registry annual report 2018: a summary. Clin Kidney J. (2021) 14:107–23. doi: 10.1093/ckj/sfaa271
6. Yuan Y, Yang Y, Zhang X, Ying C, Lu Y, Gan H. Research progress of self-management of arteriovenous fistula in maintenance hemodialysis patients. Nurs Pract Res. (2022) 19:2273–7.
7. Brown EA, Zhao J, McCullough K, Fuller DS, Figueiredo AE, Bieber B, et al. Burden of kidney disease, health-related quality of life, and employment among patients receiving peritoneal dialysis and in-center hemodialysis: findings from the DOPPS program. Am J Kidney Dis. (2021) 78:489–500.e1. doi: 10.1053/j.ajkd.2021.02.327
8. Joshwa B, Peters RM, Malek MH, Yarandi HN, Campbell ML. Multiple dimensions and correlates of fatigue in individuals on hemodialysis. Nephrol Nurs J. (2020) 47:215–51.
9. Carneiro ER, Azoubel LA, Dias RC, Dias CJ, Sá ES, Brito DA, et al. Correlation of sleep quality and cardiac autonomic modulation in hemodialysis patients. Sleep Sci. (2022) 15:59–64. doi: 10.5935/1984-0063.20200126
10. Rhee EP, Guallar E, Hwang S, Kim N, Tonelli M, Moe SM, et al. Prevalence and persistence of uremic symptoms in incident dialysis patients. Kidney360. (2020) 1:86–92. doi: 10.34067/kid.0000072019
11. Montalescot L, Dorard G, Speyer E, Legrand K, Ayav C, Combe C, et al. Patient perspectives on chronic kidney disease and decision-making about treatment. Discourse of participants in the French CKD-REIN cohort study. J Nephrol. (2022) 35:1387–97. doi: 10.1007/s40620-022-01345-6
12. Lai AY, Loh AP, Mooppil N, Krishnan DS, Griva K. Starting on haemodialysis: a qualitative study to explore the experience and needs of incident patients. Psychol Health Med. (2012) 17:674–84. doi: 10.1080/13548506.2012.658819
13. Monaro S, Stewart G, Gullick J. A ‘lost life’: coming to terms with haemodialysis. J Clin Nurs. (2014) 23:3262–73. doi: 10.1111/jocn.12577
14. Clarke AL, Yates T, Smith AC, Chilcot J. Patient’s perceptions of chronic kidney disease and their association with psychosocial and clinical outcomes: a narrative review. Clin Kidney J. (2016) 9:494–502. doi: 10.1093/ckj/sfw014
15. Subramanian L, Quinn M, Zhao J, Lachance L, Zee J, Tentori F. Coping with kidney disease - qualitative findings from the Empowering Patients on Choices for Renal Replacement Therapy (EPOCH-RRT) study. BMC Nephrol. (2017) 18:119. doi: 10.1186/s12882-017-0542-5
16. Yoong RK, Mooppil N, Khoo EY, Newman SP, Lee VY, Kang AW, et al. Prevalence and determinants of anxiety and depression in end stage renal disease (ESRD). A comparison between ESRD patients with and without coexisting diabetes mellitus. J Psychosom Res. (2017) 94:68–72. doi: 10.1016/j.jpsychores.2017.01.009
17. Farrokhi F, Abedi N, Beyene J, Kurdyak P, Jassal SV. Association between depression and mortality in patients receiving long-term dialysis: a systematic review and meta-analysis. Am J Kidney Dis. (2014) 63:623–35. doi: 10.1053/j.ajkd.2013.08.024
18. Montalescot L, Rascle N, Combe C, Untas A. Patients’ experience one year after dialysis initiation: a lexicometric analysis. Health Psychol Behav Med. (2021) 9:380–97. doi: 10.1080/21642850.2021.1918552
19. Kim MH, Kim YC, Lee JP, Kim H, Kim DK, Ryu DR, et al. Three-year income trends in Korean adults commencing haemodialysis: a prospective cohort. Nephrology. (2018) 23:625–32. doi: 10.1111/nep.13065
20. Reid C, Seymour J, Jones C. A thematic synthesis of the experiences of adults living with hemodialysis. Clin J Am Soc Nephrol. (2016) 11:1206–18. doi: 10.2215/cjn.10561015
21. Goffman E. Stigma: notes on the management of spoiled identity. Englewood Cliffs, NJ: Prentice-Hall (1963).
22. Kurzban R, Leary M. Evolutionary origins of stigmatization: the functions of social exclusion. Psychol Bull. (2001) 127:187–208. doi: 10.1037/0033-2909.127.2.187
23. Hatzenbuehler ML, Phelan JC, Link BG. Stigma as a fundamental cause of population health inequalities. Am J Public Health. (2013) 103:813–21. doi: 10.2105/ajph.2012.301069
24. Stergiou-Kita M, Pritlove C, Kirsh B. The “Big C”-stigma, cancer, and workplace discrimination. J Cancer Survivorship. (2016) 10:1035–50. doi: 10.1007/s11764-016-0547-2
25. Chu Q, Wong CCY, Chen L, Shin L, Chen LJ, Lu Q. Self-stigma and quality of life among Chinese American breast cancer survivors: a serial multiple mediation model. Psychooncology. (2021) 30:392–9. doi: 10.1002/pon.5590
26. Avdibegović E, Hasanović M. The stigma of mental illness and recovery. Psychiatr Danub. (2017) 29:900–5.
27. Shim S, Kang D, Bae KR, Lee WY, Nam SJ, Sohn TS, et al. Association between cancer stigma and job loss among cancer survivors. Psychooncology. (2021) 30:1347–55. doi: 10.1002/pon.5690
28. O’Donnell AT, Habenicht AE. Stigma is associated with illness self-concept in individuals with concealable chronic illnesses. Br J Health Psychol. (2022) 27:136–58. doi: 10.1111/bjhp.12534
29. Bravo-Mehmedbašić A, Kučukalić S. Stigma of psychiatric diseases and psychiatry. Psychiatr Danub. (2017) 29:877–9.
30. Matthews S, Dwyer R, Snoek A. Stigma and self-stigma in addiction. J Bioethic Inq. (2017) 14:275–86. doi: 10.1007/s11673-017-9784-y
31. Hill B, Bergmeier H, Incollingo Rodriguez AC, Savaglio M, Skouteris H, Barlow FK, et al. Weight stigma and obesity-related policies: a systematic review of the state of the literature. Obesity Rev. (2021) 22:e13333. doi: 10.1111/obr.13333
32. Rewerska-Juśko M, Rejdak K. Social stigma of people with dementia. J Alzheimers Dis. (2020) 78:1339–43. doi: 10.3233/jad-201004
33. Post F, Buchta M, Kemmler G, Pardeller S, Frajo-Apor B, Hofer A. Resilience predicts self-stigma and stigma resistance in stabilized patients with bipolar I disorder. Front. Psychiatry. (2021) 12:678807. doi: 10.3389/fpsyt.2021.678807
34. Ammirati RJ, Lamis DA, Campos PE, Farber EW. Optimism, well-being, and perceived stigma in individuals living with HIV. AIDS Care. (2015) 27:926–33. doi: 10.1080/09540121.2015.1018863
35. Chen X, Xu J, Chen Y, Wu R, Ji H, Pan Y, et al. The relationship among social support, experienced stigma, psychological distress, and quality of life among tuberculosis patients in China. Sci Rep. (2021) 11:24236. doi: 10.1038/s41598-021-03811-w
36. Arshi M, Yavari M, Fekr Azad H, Safi M, Moghanibashi-Mansourieh A, Moshayyedi MH. Investigation of relationship between family social support and the level of stigma perceived by PLWHA in Iran. Soc Work Public Health. (2020) 35:90–9. doi: 10.1080/19371918.2020.1742840
37. Baksi A, Arda Sürücü H, Genç H. Hope, sociodemographic and clinical characteristics as predictors of stigma-related negative discrimination experiences of patients with primary malignant brain tumor. J Neurosci Nurs. (2021) 53:81–6. doi: 10.1097/jnn.0000000000000579
38. Öztürk R, Bloom TL, Li Y, Bullock LFC. Stress, stigma, violence experiences and social support of US infertile women. J Reprod Infant Psychol. (2021) 39:205–17. doi: 10.1080/02646838.2020.1754373
39. Novak M, Mucsi I, Mendelssohn DC. Screening for depression: only one piece of the puzzle. Nephrol Dialysis Transpl. (2013) 28:1336–40. doi: 10.1093/ndt/gfs581
40. Fife BL, Wright ER. The dimensionality of stigma: a comparison of its impact on the self of persons with HIV/AIDS and cancer. J Health Soc Behav. (2000) 41:50–67.
41. Wagnild GM, Young HM. Development and psychometric evaluation of the resilience scale. J Nurs Meas. (1993) 1:165–78.
42. Herth K. Development and refinement of an instrument to measure hope. Schol Inq Nurs Pract. (1991) 5:39–51.
43. Dahlem NW, Zimet GD, Walker RR. The multidimensional scale of perceived social support: a confirmation study. J Clin Psychol. (1991) 47:756–61.
44. Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the Life Orientation Test. J. Person Soc Psychol. (1994) 67:1063–78. doi: 10.1037//0022-3514.67.6.1063
45. Herrero J, Meneses J. Short web-based versions of the perceived stress (PSS) and Center for Epidemiological Studies-Depression (CESD) scales: a comparison to pencil and paper responses among Internet users. Comput Hum Behav. (2006) 22:830–46. doi: 10.1016/j.chb.2004.03.007
46. Mehnert A, Herschbach P, Berg P, Henrich G, Koch U. Fear of progression in breast cancer patients–validation of the short form of the Fear of Progression Questionnaire (FoP-Q-SF). Z Psychosom Med Psychother. (2006) 52:274–88. doi: 10.13109/zptm.2006.52.3.274
47. Babyak MA. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med. (2004) 66:411–21. doi: 10.1097/01.psy.0000127692.23278.a9
48. Hamilton AJ, Caskey FJ, Casula A, Inward CD, Ben-Shlomo Y. Associations with wellbeing and medication adherence in young adults receiving kidney replacement therapy. Clin J Am Soc Nephrol. (2018) 13:1669–79. doi: 10.2215/cjn.02450218
49. Liu XH, Zhong JD, Zhang JE, Cheng Y, Bu XQ. Stigma and its correlates in people living with lung cancer: a cross-sectional study from China. Psychooncology. (2020) 29:287–93. doi: 10.1002/pon.5245
50. Jin R, Xie T, Zhang L, Gong N, Zhang J. Stigma and its influencing factors among breast cancer survivors in China: a cross-sectional study. Eur J Oncol Nurs. (2021) 52:101972. doi: 10.1016/j.ejon.2021.101972
51. Tan C, Zhong C, Mei R, Yang R, Wang D, Deng X, et al. Stigma and related influencing factors in postoperative oral cancer patients in China: a cross-sectional study. Support Care Cancer. (2022) 30:5449–58. doi: 10.1007/s00520-022-06962-2
52. Sugisawa H, Shimizu Y, Kumagai T, Shishido K, Koda Y, Shinoda T. Influence of dialysis-related stigma on health-related indicators in Japanese patients undergoing hemodialysis. Ther Apheresis Dialysis. (2023): doi: 10.1111/1744-9987.13992 [Epub ahead of print].
53. James LJ, Wong G, Craig JC, Ju A, Williams N, Lim WH, et al. Beliefs and attitudes to bowel cancer screening in patients with CKD: a semistructured interview study. Clin J Am Soc Nephrol. (2017) 12:568–76. doi: 10.2215/cjn.10090916
54. Abreu IS, Nascimento LC, de Lima RA, dos Santos CB. Children and adolescents with chronic kidney disease in haemodialysis: perception of professionals. Rev Brasil Enfermagem. (2015) 68:1020–6. doi: 10.1590/0034-7167.2015680604i
55. Walker RC, Walker S, Morton RL, Tong A, Howard K, Palmer SC. Mâori patients’ experiences and perspectives of chronic kidney disease: a New Zealand qualitative interview study. BMJ Open. (2017) 7:e013829. doi: 10.1136/bmjopen-2016-013829
56. Gutman T, Kelly A, Scholes-Robertson N. Patient and caregiver experiences and attitudes about their involvement in research in Chronic Kidney Disease. Clin J Am Soc Nephrol. (2022) 17:215–27. doi: 10.2215/cjn.05960521
57. Ritsher J, Phelan J. Internalized stigma predicts erosion of morale among psychiatric outpatients. Psychiatry Res. (2004) 129:257–65. doi: 10.1016/j.psychres.2004.08.003
58. Chang C, Yen C, Jang F, Su J, Lin C. Comparing affiliate stigma between family caregivers of people with different severe mental illness in Taiwan. J Nerv Ment Dis. (2017) 205:542–9. doi: 10.1097/nmd.0000000000000671
59. Jerpseth H, Knutsen I, Jensen K, Halvorsen K. Mirror of shame: patients experiences of late-stage COPD. A qualitative study. J Clin Nurs. (2021) 30:2854–62. doi: 10.1111/jocn.15792
60. Korsah K, Agyeman-Yeboah J. Narratives of type 2 diabetes mellitus patients regarding the influence of social issues on diabetes self-management: implications for patient care. Nurs Open. (2023) 10:5741–8. doi: 10.1002/nop2.1825
61. Gomes D, Zanetti A, Miasso A, Castro F, Vedana K. Internalized stigma in people with mood disorders: predictors and associated factors. J Nerv Ment Dis. (2021) 209:54–8. doi: 10.1097/nmd.0000000000001257
62. Yuan L, Gao Y, Pan B, Wang J, Wang Y, Gong C, et al. Resilience and related factors: a comparison of fathers and mothers of patients with cleft lip and/or palate in China. Front Psychiatry. (2021) 12:791555. doi: 10.3389/fpsyt.2021.791555
63. Dufault K, Martocchio B. Symposium on compassionate care and the dying experience. Hope: its spheres and dimensions. Nurs Clin North Am. (1985) 20:379–91.
64. Wu X, Xu H, Zhang X, Han S, Ge L, Li X, et al. Self-efficacy, hope as mediators between positive coping and resilience among patients with gastric cancer before the first chemotherapy. Cancer Nurs. (2021) 44:79–85. doi: 10.1097/ncc.0000000000000753
65. Vrbova K, Prasko J, Ociskova M, Kamaradova D, Marackova M, Holubova M, et al. Quality of life, self-stigma, and hope in schizophrenia spectrum disorders: a cross-sectional study. Neuropsychiatr Dis Treat. (2017) 13:567–76. doi: 10.2147/ndt.s122483
66. Rahimipour M, Shahgholian N, Yazdani M. Effect of hope therapy on depression, anxiety, and stress among the patients undergoing hemodialysis. Iran J Nurs Midwif Res. (2015) 20:694–9. doi: 10.4103/1735-9066.170007
67. Wang D, Liu X, Xiao J, Chen J, Li X, Yu C, et al. Hope during the COVID-19 epidemic decreased anxiety and depression symptoms mediated by perceived stress: coping style differences among patients with COVID-19. Curr Med Sci. (2022) 42:885–94. doi: 10.1007/s11596-022-2624-2
68. Ge C, Zhang H, Zhu G, Cao A, Zhang J. Intervention study of Snyder’s hope theory on the stigma of stroke in young and middle-aged patients: a randomised trial. Ann Palliat Med. (2021) 10:5721–8. doi: 10.21037/apm-21-441
69. Öztürk Z, Şahi N. The effect of nursing interventions to instill hope on the internalized stigma, hope, and quality of life levels in patients with schizophrenia. Perspect Psychiatr Care. (2022) 58:364–73. doi: 10.1111/ppc.12800
70. Parcesepe A, Tymejczyk O, Remien R, Gadisa T, Kulkarni S, Hoffman S, et al. HIV-related stigma, social support, and psychological distress among individuals initiating ART in Ethiopia. AIDS Behav. (2018) 22:3815–25. doi: 10.1007/s10461-018-2059-8
71. Bergmann T, Sengupta S, Bhrushundi M, Kulkarni H, Sengupta P, Fergus I. HIV related stigma, perceived social support and risk of premature atherosclerosis in South Asians. Indian Heart J. (2018) 70:630–6. doi: 10.1016/j.ihj.2018.06.018
72. Hu C, Chang K, Hsish H, Chang H, Yu S. Social support as a mediator of the relationship between hope and decisional conflict in patients deciding whether to receive dialysis. J Healthcare Eng. (2021) 2021:5607219. doi: 10.1155/2021/5607219
73. Silva S, Braido N, Ottaviani A, Gesualdo G, Zazzetta M, Orlandi Fde S. Social support of adults and elderly with chronic kidney disease on dialysis. Rev Latino Am Enfermagem. (2016) 24:e2752. doi: 10.1590/1518-8345.0411.2752
74. Jansen DL, Rijken M, Kaptein AA, Boeschoten EW, Dekker F, Groenewegen P. The role of social support in dialysis patients’ feelings of autonomy and self-esteem: is support more beneficial for patients with specific illness perceptions? Fam Syst Health. (2014) 32:313–27. doi: 10.1037/fsh0000028
75. Zhao X, Sun M, Yang Y. Effects of social support, hope and resilience on depressive symptoms within 18 months after diagnosis of prostate cancer. Health Qual Life Outcomes. (2021) 19:15. doi: 10.1186/s12955-020-01660-1
76. Boyle M, Fearon A. Self-stigma and its associations with stress, physical health, and health care satisfaction in adults who stutter. J Fluency Disord. (2018) 56:112–21. doi: 10.1016/j.jfludis.2017.10.002
77. Kabiyea F, Manor-Binyamini I. The relationship between stress and stigma, somatization and parental self-efficacy among fathers of adolescents with developmental disabilities in the Bedouin community in Israel. Res Dev Disabil. (2019) 90:31–40. doi: 10.1016/j.ridd.2019.04.004
78. Liu H, Yang Q, Narsavage G, Yang C, Chen Y, Xu G, et al. Coping with stigma: the experiences of Chinese patients living with lung cancer. SpringerPlus. (2016) 5:1790. doi: 10.1186/s40064-016-3486-5
79. Shamsaei F, Tahour N, Sadeghian E. Effect of Stress Management Training on Stigma and Social Phobia in HIV-Positive Women. J Int Assoc Provid AIDS Care. (2020) 19:2325958220918953. doi: 10.1177/2325958220918953
80. Dankert A, Duran G, Engst-Hastreiter U, Keller M, Waadt S, Henrich G, et al. Fear of progression in patients with cancer, diabetes mellitus and chronic arthritis. Die Rehabil. (2003) 42\:155–63. doi: 10.1055/s-2003-40094
81. Gu Z, Qiu T, Yang S, Tian F, Wu HA. Study on the psychological factors affecting the quality of life among ovarian cancer patients in China. Cancer Manag Res. (2020) 12:905–12. doi: 10.2147/cmar.s239975
82. Herschbach P, Dinkel A. Fear of progression. Recent Results Cancer Res. (2014) 197:11–29. doi: 10.1007/978-3-642-40187-9_2
83. Dinkel A, Herschbach P. Fear of progression in cancer patients and survivors. Recent Results Cancer Res. (2018) 210:13–33. doi: 10.1007/978-3-319-64310-6_2
84. Meissner V, Olze L, Schiele S, Ankerst D, Jahnen M, Gschwend J, et al. Fear of cancer recurrence and disease progression in long-term prostate cancer survivors after radical prostatectomy: a longitudinal study. Cancer. (2021) 127:4287–95. doi: 10.1002/cncr.33836
Keywords: renal dialysis, stigma, fear of progression, hope, social support
Citation: Li B, Liu D, Zhang Y and Xue P (2023) Stigma and related factors among renal dialysis patients in China. Front. Psychiatry 14:1175179. doi: 10.3389/fpsyt.2023.1175179
Received: 27 February 2023; Accepted: 17 July 2023;
Published: 31 July 2023.
Edited by:
Abdrabo Moghazy Soliman, Qatar University, QatarReviewed by:
Insa Schmidt, Boston University, United StatesRudval Souz Da Silva, Bahia State University, Brazil
Copyright © 2023 Li, Liu, Zhang and Xue. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pengshi Xue, MzI0Nzc5NjAxMEBxcS5jb20=
 Bing Li
Bing Li Di Liu
Di Liu Yue Zhang
Yue Zhang Pengshi Xue
Pengshi Xue