- 1Max Planck Institute of Psychiatry, Munich, Germany
- 2Department of Psychiatry and Psychotherapy, LMU University Hospital Munich, Munich, Germany
- 3Department of Psychology, LMU Munich, Munich, Germany
Background: Treatment guidelines for psychosis recommend offering psychotherapy already in the acute illness phase. However, there is a lack of available interventions adapted to the specific needs and key change mechanisms of inpatients experiencing severe symptoms and crisis. In this article we outline the scientific development process of a needs-oriented and mechanism-based group intervention for acute psychiatric inpatients with psychosis (MEBASp).
Methods: To guide our intervention design, we used Intervention Mapping (IM), a six-step framework for developing evidence-based health interventions that consisted of an extensive literature review, an in-depth problem definition and needs analysis, the modeling of change mechanisms and outcomes and the production of an intervention prototype.
Results: Our low-threshold modularized group intervention consists of nine stand-alone sessions (two per week) within three modules and targets different aspects of metacognitive and social change mechanisms. Module I and II aim to reduce acute symptoms by fostering cognitive insight, Module III focuses on reducing distress via cognitive defusion. Therapy contents are adapted from existing metacognitive treatments such as the Metacognitive Training and presented in a destigmatizing, simply understandable and experience-oriented way.
Conclusion: MEBASp is currently evaluated in a single-arm feasibility trial. Using a systematic and rigorous development methodology and providing a detailed description of the development steps demonstrated to be invaluable in improving the intervention’s scientific foundation, validity, and replicability for similar research.
1. Introduction
Psychological therapies have demonstrated to be effective for patients experiencing psychotic symptoms (1, 2) and are recommended by treatment guidelines already in the acute illness and treatment phase (3, 4). However, recent systematic reviews and meta-analyses investigating treatment effects for acute psychiatric inpatients with psychosis revealed an outcome superiority of third-wave therapies (5–7) over guideline-recommended second-wave cognitive behavioral therapy for psychosis (CBTp) (3, 4). In contrast to disorder-specific CBTp protocols that aim to alter the occurrence and form of psychotic symptoms such as delusional thoughts and hallucinations (8), third-wave therapies often focus on the behavioral function of internal experiences rather than their content per se (9). Instead of examining and disputing the content of voices and thus giving them increased attention and importance for example, third-wave therapies train patients to mindfully experience auditory hallucinations in order to reduce their negative impact on behavior (10). They also emphasize the therapeutic importance of targeting evidence-based change mechanisms, which are the underlying (psychological) processes responsible for positive treatment outcomes, instead of solely focusing on changing symptoms (11). Third-wave interventions e.g., aim at changing impaired reasoning processes behind delusional thoughts and not necessarily the content of the specific delusion (9). Change mechanisms thereby draw on impaired processes believed to contribute to the maintenance and onset of various mental health problems and thus often operate as transdiagnostic change factors (11). Cognitive distortions associated with depressive disorders for instance can also be improved through interventions targeting general reasoning abilities (12). Understanding what leads to change and tailoring therapy to directly address those change mechanisms hence seems to be important to generally optimize therapeutic strategies and thus to improve overall treatment outcomes for patients (9, 13).
Given the urgent need for effective inpatient care (14, 15), prioritizing change mechanisms in therapy therefore might hold a great potential to positively impact disease progression and prognosis of patients with acute psychosis (16). Major third-wave therapies that explicitly focus on potential change mechanisms in psychosis are the Acceptance and Commitment (ACT) and the Metacognitive Training (MCT) (9). ACT for instance fosters acceptance and cognitive distancing from delusions and hallucinations (17) and has shown to reduce general psychopathology and rehospitalization rates in acute inpatients with psychosis (18–20). MCT on the other hand aims to promote patients’ cognitive flexibility by raising metacognitive awareness and knowledge for cognitive biases (21) and showed significant effects on reducing positive symptoms (8, 22, 23). Although the mechanism-based principles of these approaches seem promising in the treatment of acute inpatients with psychosis, existing evidence has to be treated with caution (5). Until now, evidence is based on a small number of randomized controlled trials (RCTs) with relatively heterogeneous study conditions and methodological shortcomings (5–7). On top of that, ACT and MCT were developed for outpatient settings where patients’ symptom severity and hence key change mechanisms and needs can be assumed to differ from those of patients experiencing acute crises (24). Change mechanisms in acute inpatient environments for example mainly comprise of mechanisms associated with distress and risk reduction (16), while outpatient therapy focuses on processes like value commitment that support long term recovery goals (1). In addition, acute psychiatric settings by themselves represent challenging environments to deliver psychotherapy, counting involuntary admissions, brief inpatient stays and staff shortage as major obstacles (25). Researchers therefore argue that further intervention development is needed that (a) identifies and adapts to specific inpatient change mechanisms and (b) reflects the complex requirements of acute psychiatric ward (25–28).
However, the actual development process of interventions in psychotherapy is often kept short and under-reported (29). Neglecting the actual development phase can be problematic, as a poor problem definition, insufficient attention to existing evidence and context needs, a missing model underlying the intervention, and an unsound selection of hypothesized change mechanisms can lead to inefficient treatments (30–32). An “intervention black box” then makes it difficult to understand why specific therapy components didn’t work in a clinical trial (31). Furthermore, a published, in-depth description of the development process is necessary for other researchers to replicate findings and for clinicians to understand how to implement the intervention (33).
In order to overcome these shortcomings, Bleijenberg et al. (31) suggest using structured methodological frameworks such as the Intervention Mapping (IM) that fulfills the Medical Research Council’s (MRC) quality criteria on intervention development (31, 32). Although the use and reporting of IM approaches is prevalent in health and prevention research (34–39), there are only a limited number of comparable academic articles published in the field of (clinical) psychology (40, 41). The current article’s objectives are therefore twofold: We aim to describe the development and theoretical underpinnings of a mechanism-based and needs-oriented intervention for inpatients with psychosis (MEBASp) treated in an acute psychiatric setting. By using Intervention Mapping in doing so, we also hope to provide an example and highlight the benefits of how existing rigorous development frameworks can be used to enhance the design and reporting standards for psychological therapies in psychiatric research.
2. Materials and methods
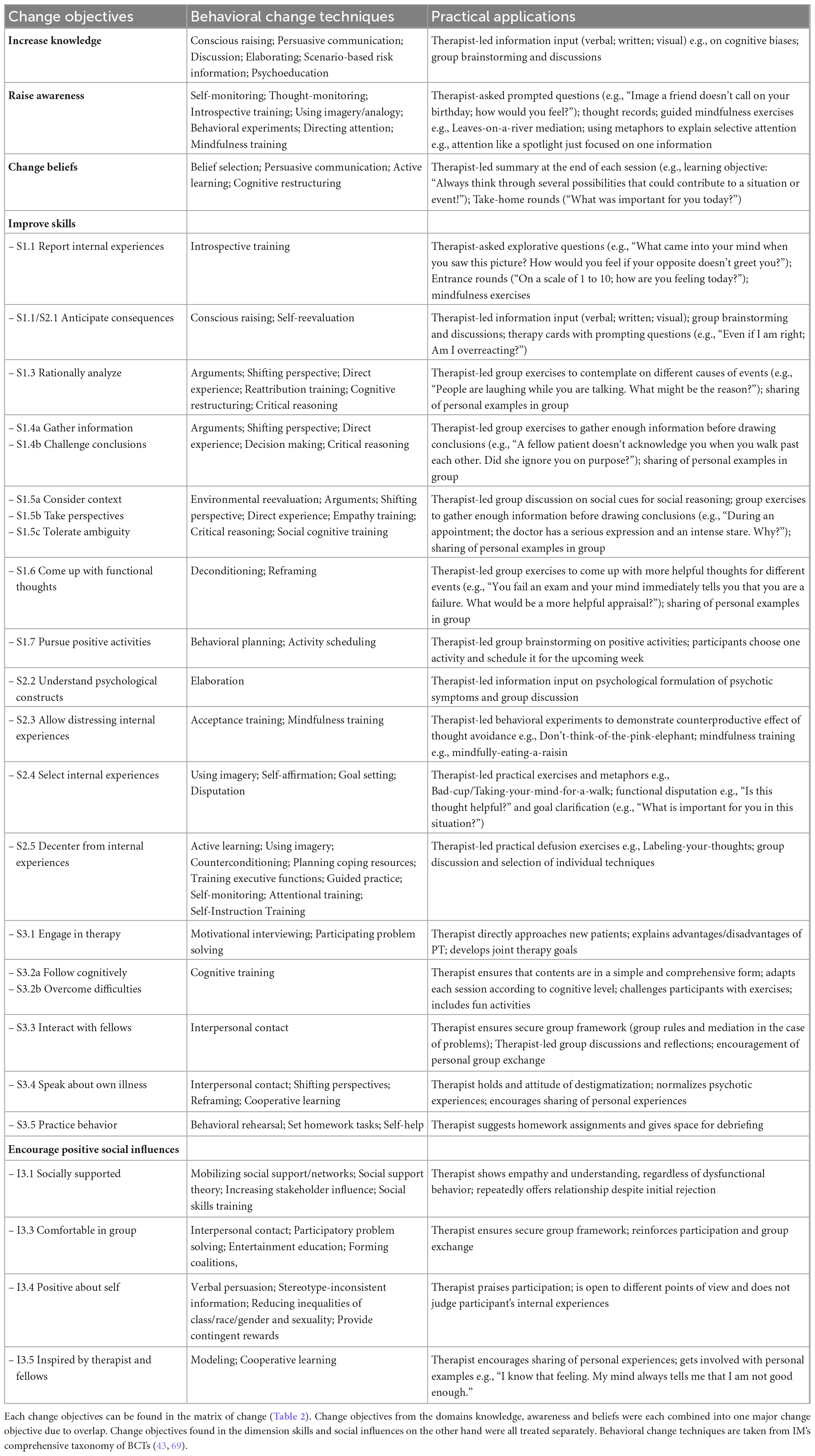
We chose IM as our conceptual development framework due to its systematic and detailed protocol allowing an effective selection of treatment mechanisms and procedures in six consecutive steps (42). In the practical application of those steps, we were guided by the approach of van Agteren et al. (40), who adapted the IM method for mental health research. Next to following IM principles, we made sure to adhere to relevant reporting guidelines (e.g., Template for Intervention Description and Replication) when describing and explaining our development milestones (33). Figure 1 provides an overview of the development steps undertaken to design our intervention that are described in detail in the sections below.
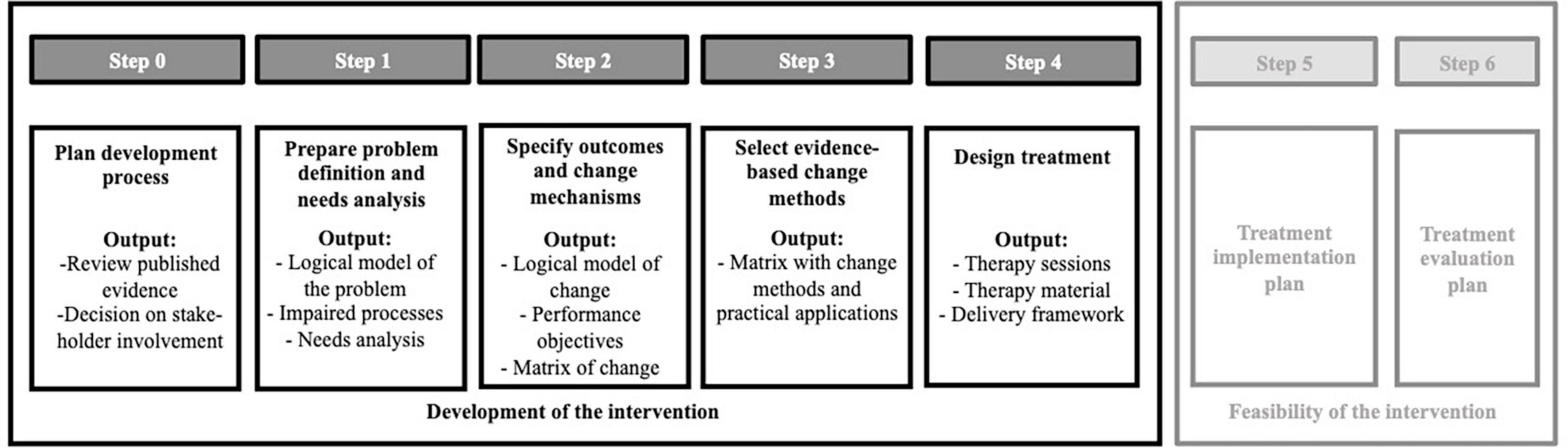
Figure 1. Illustration of the IM intervention development process and selected steps undertaken in the MEBASp project.
2.1. Step 0: planning process and decision on stakeholder involvement
Next to theory and evidence-based development principles, the IM approach emphasizes participatory research activities e.g., involving the target population in all planning phases trough qualitative research (43). Collaborative care planning approaches, such as codesign and coproduction, have thereby become increasingly important in mental health intervention design and delivery, and have been shown to improve service quality (44–47). Nevertheless, the implementation of codesign in psychiatric research settings can be challenging due to the significant time and cost involved (48), as well as the ethical challenges that arise when conducting qualitative research with severely burdened and highly vulnerable patient groups (49, 50). To address this challenge, Locock et al. developed an accelerated codesign approach that drew on pre-existing qualitative patient data and that proved to be acceptable to patients and staff (48). Building on this approach, we first of all reviewed pre-existing qualitative research involving acute inpatients with psychosis (for an overview see Supplementary Table 1). Published studies were primarily conducted in a psychiatric context in the UK, which was found to be very similar to the German system (51), thus making available data transferable to our current research context. By deciding to draw on secondary data for our project instead of conducting primary research, we aimed to take advantage of synergistic effects by implementing patients perspective from prior research, while also considering the constraints of time and resources discussed above. However, we included various codesign activities in our subsequent feasibility study such as feedback rounds and questionnaires, and interviews with both participants and staff (see future directions) to ensure that the intervention prototype will be refined according to the needs and preferences of our target population (52).
2.2. Step 1: logical model of the problem and needs analysis
The first step of IM involved an exact description of our development context including our target population and setting. We moreover conducted an extensive literature study to create a logical model (theory) of our problem (see Figure 2) from which we derived the theoretical underpinnings, the requirements for and the scope of the intervention (43). To structure the literature research behind the problem determination and resulting needs analysis, IM suggests using the PRECEDE-framework (an acronym for Predisposing, Reinforcing and Enabling Constructs in Educational Diagnosis and Evaluation), which is an established research method to assess health issues on the basis of four predefined assessment phases (53). Going through the different phases, research teams ask themselves the following questions: What is the problem and who has it (epidemiological assessment)? How does it affect patients (social assessment)? What may be its causes (ecological assessment)? How do policies contribute to the problem (policy assessment)? (54). Following the framework’s phases, we covered information on (1) mental health problems of acute inpatients with psychotic symptoms, (2) their effects on quality of life (QoL), (3) potentially associated pathogenetic psychological and environmental processes causing the problem and 4) characteristics (policies) of acute psychiatric wards. Our sources of information included systematic reviews and meta-analyses (5–7, 55), qualitative interview studies (16, 25, 28, 56, 57), core competency frameworks and existing mechanism-based therapies for working with acute inpatients with psychosis (8, 18, 20, 22, 23, 26, 58, 59).
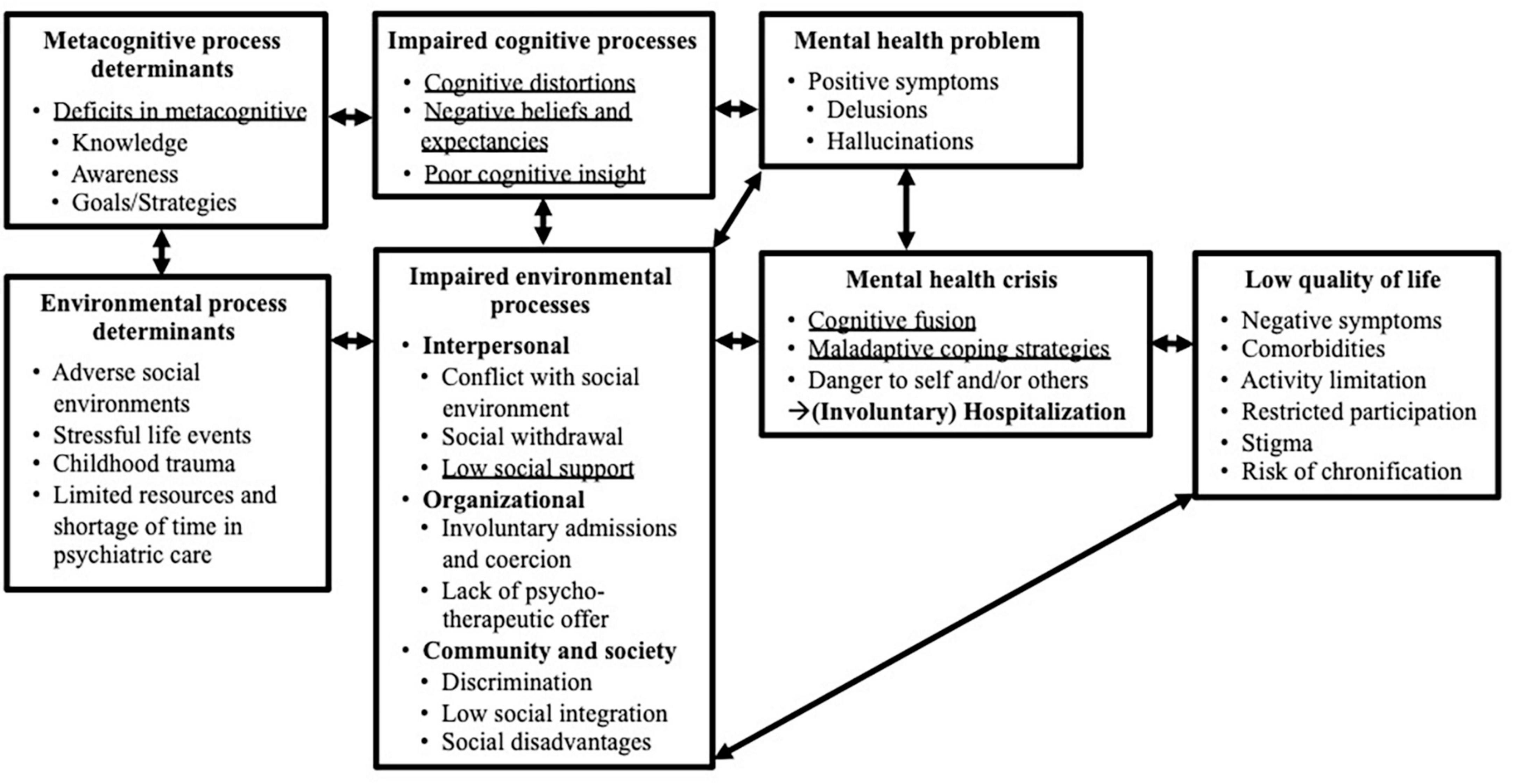
Figure 2. Logical model of the problem of severe psychotic symptoms, danger to self and others, (involuntary) hospitalization and a resulting low quality of life (Step 1). The model has a focus on psychological and social factors in the development of psychosis and does not consider biological factors e.g., genetics. It moreover does not map the moderating or mediating relationships between variables, but rather aims to visualize the variability of factors and impaired processes that contribute to these main health problems (40). Impaired processes that were identified as target areas for the logical model of change are underlined.
Impaired psychological processes e.g., cognitive distortions found to be relevant in psychosis (60) were grouped into different overarching process domains such as cognition (see Supplementary Table 2). A psychological process thereby refers to an aspect of human cognition, affect, behavior or physical sensation that may be involved in the predisposing, etiology or maintenance of a disorder (61). As impaired processes are believed to causally interrelate with several mental disorders (62), we made sure to include transdiagnostic findings in our overview. To organize the overview, we utilized the available subdivisions found in the transdiagnostic process collection by Harvey et al. (61) which summarizes research results on cross-diagnostic altered processes in five different domains. Using existing process-oriented etiological models for psychosis (63–67), we then identified the most important environmental and psychological processes for our problem model. Existing intervention concepts focusing on identified processes as mechanisms of change were then extensively studied to estimate common practices, their effectiveness and potential barriers (31) (see Supplementary Table 3).
2.3. Step 2: intervention outcomes, change mechanisms and logical model of change
In a second step, we used our logical problem model and needs analysis (Step 1) to define desired cognitive, behavioral and environmental intervention outcomes necessary to prevent or reduce our health problems (e.g., patient critically reflects on internal experiences) and thus positively influence quality of life effects. Following the IM framework, we then addressed the question of why patients would make these changes by selecting impaired processes from our problem theory (e.g., poor cognitive insight) and rewriting them into hypothesized change mechanisms (e.g., higher cognitive insight) (43). Overarching change domains were chosen from the Theoretical Domains Framework (TDF) (68), an integrative framework that provides intervention developers with a possible selection of 14 change domains e.g., behavioral regulation and 84 change mechanisms e.g., self-monitoring from evidence-based behavior change theories. We summarized our overall findings in a graphical logical model (theory) of change (43) (see Figure 3).
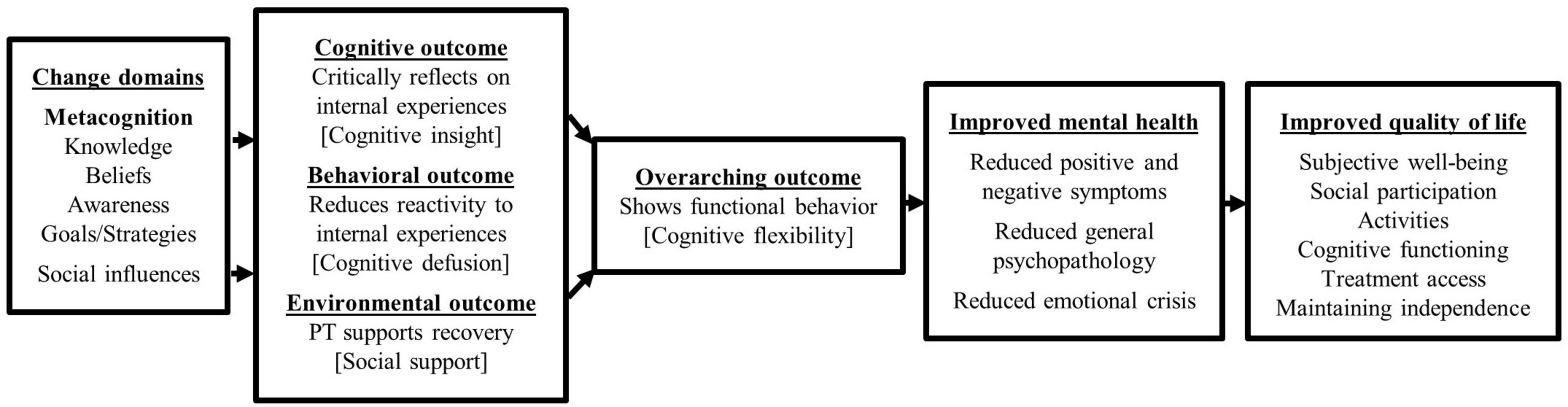
Figure 3. Logical model of change showing what change is needed to manage the main health problems of severe psychotic symptoms and danger to self and others (Step 2). It points out the change domains and belonging change mechanisms expected to influence the cognitive, behavioral and environmental outcomes that are in turn believed to improve mental health and quality of life. Hypothesized underlying target change mechanisms are put into square brackets.
Our intervention outcomes were further divided into so-called performance objectives (e.g., Patient understands the cognitive model of CBT) (see Table 1). These objectives describe specific behaviors that need to be pursued in order to reach the desired treatment outcome (43). By linking performance objectives with selected change mechanisms from above, we were able to phrase specific change objectives. Simply put, change objectives concretely verbalize what occurs through a change mechanism (e.g., The patient demonstrates increased knowledge about the impact of internal experiences on behavior) (40). As a result, all change objectives were organized in a matrix of change (43) (see Table 2).
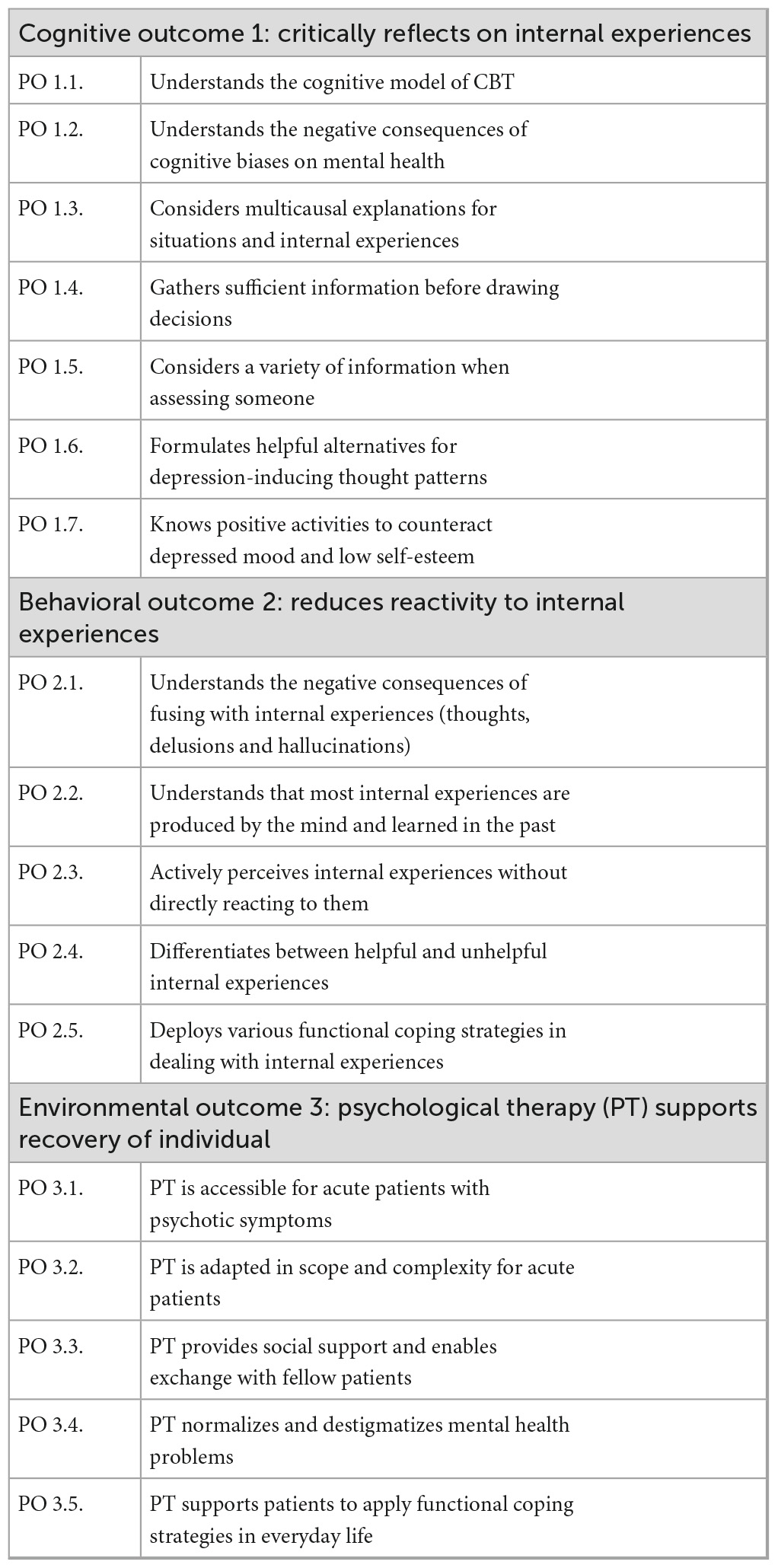
Table 1. Expected cognitive, behavioral and environmental outcomes and performance objectives (PO) for MEBASp (Step 2).
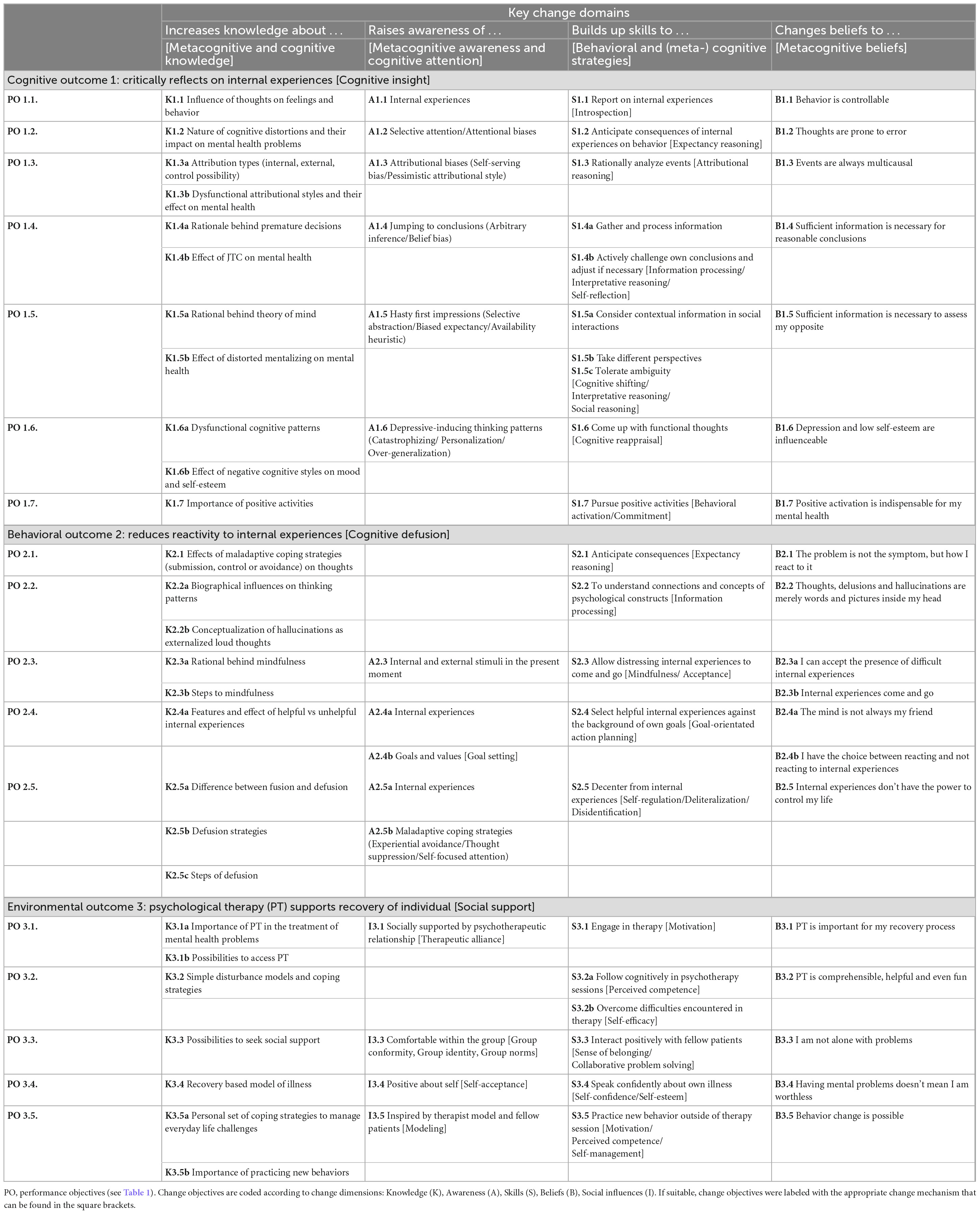
Table 2. Matrix of change for cognitive, behavioral and environmental outcomes showing the change objectives for each performance objective and change domain (Step 2).
2.4. Step 3: evidence-based change methods
In Step 3 of IM, we used our matrix of change to link our change objectives to so called change methods. Change methods describe theory-based behavior change techniques (BCTs) (69) that are believed to influence change objectives (e.g., knowledge increase may be achieved through the change method psychoeducation) (69). Instead of asking Why does change occur? we were now concerned with the question How does change occur? (43). We selected our evidence-based change methods from various literature resources (70, 71) including IM’s comprehensive taxonomy of BCTs (43, 69) and translated them into practical applications. A practical application refers to a therapeutic strategy derived from the change technique that can be implemented in a real-world setting (40). For example, to achieve our change objective of increasing knowledge about the impact of internal experiences on behavior, the intervention utilizes psychoeducation as a change technique. This is practically done by providing an everyday example (such as “Imagine your best friend doesn’t call on your birthday”) (72) (p. 104) to the patients and asking them how they might feel, think, and react (73). Practical applications were informed by existing mechanism-based intervention practices for (acute) settings as identified in Step 1 (8, 18, 20, 22, 23, 59). The final output for Step 3 comprised of a matrix of change methods containing all procedures planned to be incorporated into our intervention (43) (see Table 3).
2.5. Step 4: intervention outline
In line with our intervention draft of Step 3, we designed treatment modules, the associated sessions (see Table 4), produced therapy materials and decided on our delivery format outlining therapy frequency and duration of sessions. Next to creating completely new materials, we made sure to thoroughly examine existing therapy manuals for usable parts. If some materials of an intervention were suitable, we made adjustments before integrating them into our intervention. During the development process, project team members and independent clinical fellows constantly reviewed materials and session outlines. We also made sure to carry out some informal test-runs with patients whose verbal feedback was used to revise session contents for the final intervention that is currently tested in a feasibility study.
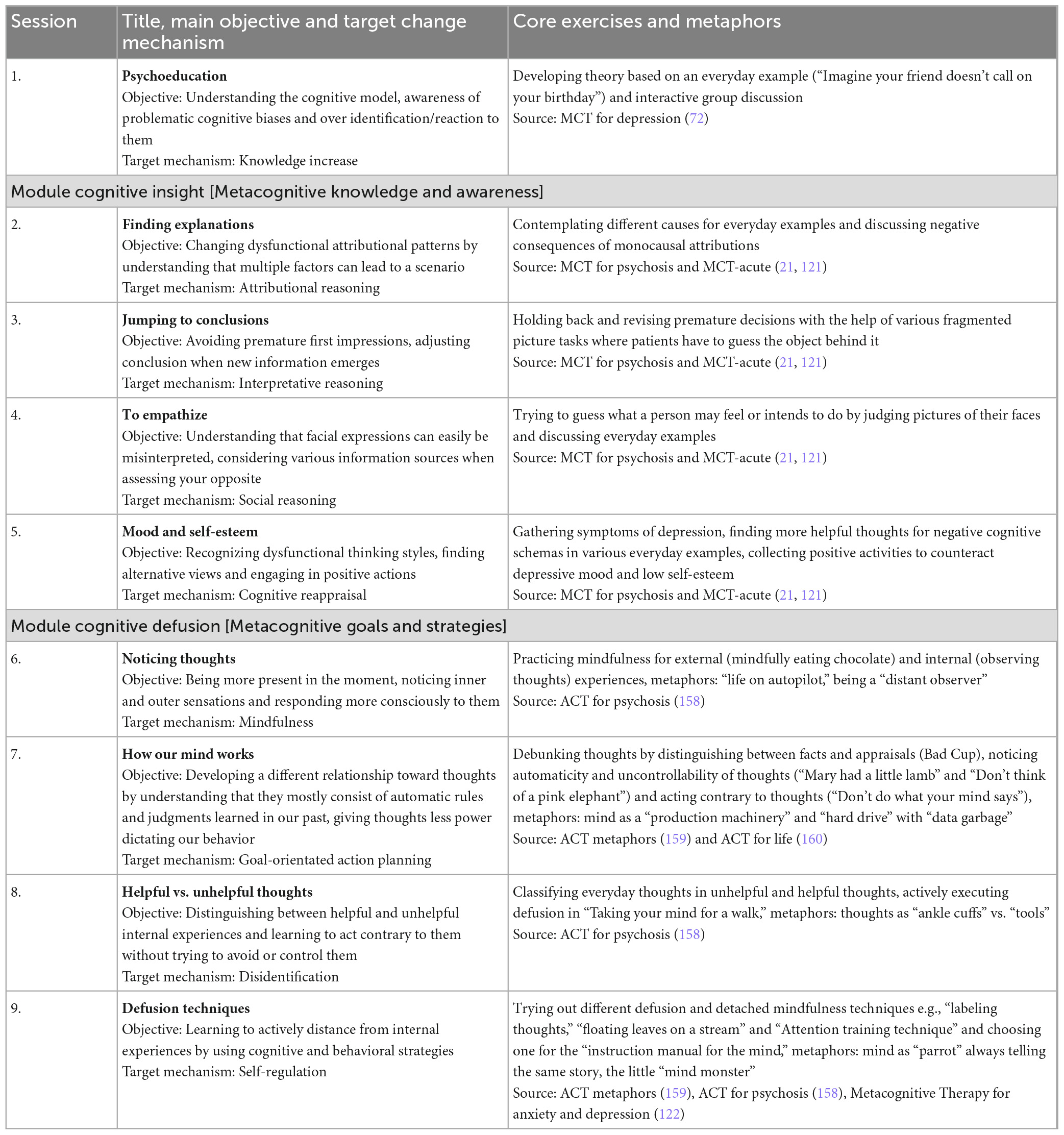
Table 4. Table giving an overview of the objective and core exercises for each session of MEBASp (Step 4).
2.6. Step 5 and 6: implementation and evaluation plan
After completing step 1–4, IM includes two additional steps consisting of setting up an implementation and evaluation plan (43). However, we decided to follow van Agteren and colleague’s decision to exclude these steps in our current research (40) as this allowed us to provide a more detailed insight into our intervention development process. Nevertheless, the evaluation of the intervention is covered by the above mentioned feasibility study (clinicalTrials.gov identifier: NCT04874974) (74). We will give a brief overview of our ongoing pilot study in the future directions part of the discussion section.
3. Results
3.1. Step 1: logical model of the problem and needs analysis
To facilitate a deeper understanding of our initial project phase and literature research, we present the results of Step 1 in a narrative format that begins with a brief description of our development context and population and progresses to the problem definition and the derivation of needs.
3.1.1. Development context and target population
MEBASp is part of a research initiative at the Max Planck Institute of Psychiatry in Munich, Germany, which aims to implement a clinic-wide mechanism-based treatment concept containing different group modules each focusing on a specific change mechanisms like emotion regulation or behavioral activation. By identifying individually relevant psychological processes and personal preferences of each patient on admission, the clinical team ensures a targeted treatment selection by combining indicated therapy modules (9, 75–77). In this context, our IM approach focused on the development of an intervention targeting change mechanisms found to be relevant in acute inpatients with positive and/or negative psychotic symptoms (according to ICD-10 criteria) treated in an (locked) acute psychiatric ward (78) (for a detailed research background on the concept see Supplementary Methods and Supplementary Figure 1). Based on the assumption of psychosis as an independent clinical trait (79), our target inpatient group covered the entire psychosis-spectrum as well as psychotic depression and psychotic bipolar disorder.
3.1.2. Defining the problem of acute inpatients with psychotic symptoms
In the course of our epidemiological assessment, we specified two main mental health problems for acute inpatients with psychosis (16, 25): (1) severe positive symptoms such as hallucinations and delusions and (2) resulting dangerous behaviors toward themselves and others making immediate (compulsory) hospitalization necessary. Our social assessment in turn revealed a tremendous negative impact of the severity of positive symptoms and crisis-associated hospitalization on patients’ QoL (27, 80–82). Both are believed to contribute to the secondary activation of negative symptoms such as poor rapport (83) and comorbid disorders like mood and anxiety disorders (84) resulting in an increased chronification risk (85). Relevant contributing psychological processes in the development of negative symptoms thereby seem to be a demoralization due to patients’ low expectancies for pleasure or success (64, 86), internalized stigma (87), a lack of participation and activities (88), and maladaptive coping responses such as social anhedonia and substance abuse to deal with aversive internal and external experiences (89).
Furthermore, our ecological assessment (see Supplementary Table 2) identified metacognitive deficits (90) to be the main determinant for pathogenetic cognitive processes associated with positive symptoms (first health problem). We also found associations of metacognitive deficits with negative symptoms and impaired processes discussed above (91). While metacognition is being broadly defined as “knowledge about knowledge” (92), it can be further distinguished into a knowledge (knowledge and beliefs about cognition), an awareness (conscious experience of and reflection about cognitive processes), a goal (setting goals on a meta-level), and a strategy part (conscious application of functional strategies for goal achievement) (93). Patients with psychotic symptoms thereby seem to show deficits in all four components (94). Deficits in metacognitive knowledge and awareness moreover are believed to lead to cognitive distortions (e.g., jumping to conclusions, attributional biases, theory of mind deficits) (60), dysfunctional beliefs and expectancies (associated with a low self-esteem and negative symptoms) (10, 95) and a lack of cognitive insight into those cognitive biases (96). For instance, a lack of knowledge about common human cognitive biases, poor awareness of one’s own thoughts, and the inability to recognize distortions in conclusions could lead to misinterpreting a crackling sound on a phone line as proof of being watched (21). Delusional thoughts and hallucinations alone however, do not automatically result in distress and dysfunctional behavior making compulsory hospitalization necessary (second health problem). It seems to be the appraisal and behavioral reactivity toward the thought and voice contents that increases the probability of danger to self and others (97). Psychological processes linked with this problem are cognitive fusion with internal experiences and maladaptive coping strategies such as experiential avoidance, thought suppression and worry (66, 98–100). Explained in highly simplified terms, cognitive fusion describes a cognitive process in which a person is fully entangled with the verbal content of internal experiences, beliefs it to be true and reacts to the content (101). Consistent with metacognitive process models, cognitive fusion can be associated with a deficit in metacognitive goal setting and strategies leading to the increased reactivity to dysfunctional thought content (102). The idea of being surveilled may e.g., take on great importance due to dysfunctional metacognitive beliefs, such as that one’s thoughts are true and need to be acted on. Without being aware of own goals and values, one may turn to dysfunctional coping strategies like aggression, social withdrawal or excessive worrying, which in turn can escalate into mental crisis followed by a decrease in functioning (103). In summary, there is convincing evidence for the contribution of metacognitive deficits to both severe psychotic symptoms and subsequent crisis development (104).
Lastly, our policy assessment identified bio-social vulnerabilities and structural (health) system barriers that lead to environmental risk factors such as social conflicts (interpersonal), a general shortfall of psychosocial treatments (organizational), stigma and societal disadvantages (society) that all seem to additionally contribute to our overall problem (105–107). For a visualization of our problem theory see Figure 2.
3.1.3. Determining the needs for development and implementation
Having a better understanding of our problem and the underlying impaired processes, we were now able to draw general implications for the implementation of the intervention itself.
Considering the severity of mental health problems and low QoL, we first of all determined a great need to generally expand and improve the psychotherapeutic offer for acute inpatients with psychosis. Although guidelines recommend psychological care already in the acute illness phase (3, 4), implementation rates on acute ward are still extremely low (28, 108, 109) resulting in a dissatisfaction among patients who criticize the predominant pharmacological and risk-focused treatment (27, 110). The demand for psychosocial treatments that do not involve medication but aim to assist with recovery, on the other hand, is high (25).
The second need we derived was the necessity to adapt existing mechanism-based interventions to the specific characteristics of acute ward and inpatients with psychotic symptoms (25). Available concepts are often lengthy and quite complex in content and it has to be doubted if they can actually work efficiently in acute settings (6, 16, 28). Main limitations consist of short hospital stays (111) and patients’ general difficulties to engage with traditional psychotherapy concepts due to treatment resistance (112, 113), high distrust levels toward the entire environment (114), emotional distress (115), severe cognitive deficits (116), and dual diagnoses (117). Despite the demanding patient clientele, therapists in acute settings are moreover challenged to provide psychological therapies with minimal resources (16). Staff shortage, economic pressure and administrative duties leave little room to offer individual therapy to each patient making group-based formats a cost-effective alternative to reach a large number of patients (118). Moreover, group interventions offer valuable opportunities for interpersonal skill development and peer support (26). Due to high patient turnovers, group therapies should be delivered in standalone formats with patients being able to already benefit when attending only one session or one module (118). Despite the economic and social benefits of group concepts, it is advisable to offer at least a minimum number of individual sessions to provide additional space for addressing personal needs and topics (119).
Thirdly, we formulated the need to consider both staff and patients’ needs when planning the content of the intervention. While care taker priorities often focus on symptom and risk management, patients themselves name social circumstances and intra- and interpersonal symptom distress (e.g., unwanted internal states, sleep difficulties, lost sense of identity, social isolation, and stigma) as their main concerns (16, 25, 28, 120).
In summary, our findings suggest that an effective and feasible intervention for acute psychiatric inpatients should focus on key mechanisms associated with changes in symptom severity and patients’ symptom distress. A group concept is favored over individual sessions due to economic and social reasons, although additional individual sessions should be offered based on individual needs or demand. Therapy sessions should be simple, brief, flexible, low key, and able to be delivered stand-alone.
3.1.4. Examining existing practice
Beside Metacognitive Training (MCT), we identified two more mechanism-based therapies for psychosis focusing explicitly on impaired metacognitive processes linked to our first health problem (positive symptoms) (36): Metacognitive insight and reflection therapy (MERIT) and Metacognitive interpersonal therapy for psychosis (MIT-P). However, sufficient evidence was only available for Metacognitive Training (37–40) that furthermore recently provided an open-source transdiagnostic group format suitable for acute inpatients and acute settings (121). The concept of MCT by Moritz and Woodward was originally inspired by research on cognitive biases in psychosis (65) and aims to convey metacognitive knowledge and raise metacognitive awareness for dysfunctional thought patterns (60, 122). Compared to Metacognitive Therapy by Wells and Matthews, MCT not only focuses on general thinking mechanisms from a metacognitive perspective, but also on specific thoughts from a cognitive one by directly addressing thought contents (60). MCT’s goals are implemented in a group therapy format that works with non-confrontational, educative and delusional-neutral material (21). Although MCT was originally developed for psychosis, it has been adapted for use in treating other disorders such as depression and personality disorders and can be applied in a transdiagnostic manner (60).
Our target processes cognitive fusion and maladaptive coping strategies related to our second health problem (dangerous behaviors and hospitalization) on the other hand are the main subject in the Acceptance and Commitment Therapy by Hayes (101) and the Metacognitive Therapy by Wells and Matthews (122). In contrast to traditional CBT principles of disputation and restructuring, ACT focuses on transdiagnostic change mechanisms such as acceptance and cognitive defusion to modify patients’ relationship toward internal experiences changing their function on behavior (19). Defusion thereby refers to a decentering-related mechanism that operates through metacognitive goal clarification (e.g., asking yourself if this thought is helpful for your broader goals and values) and the use of mindfulness-based distancing strategies (123). Similar to defusion techniques, Well’s Metacognitive Therapy aims to reduce toxic thinking styles such as worry and threat monitoring believed to maintain paranoid thoughts and hallucinations by changing dysfunctional metacognitive beliefs and practicing metacognitive strategies like detached mindfulness (124). Both ACT and Metacognitive Therapy share their transdiagnostic orientation and focus on metacognitive strategies and have demonstrated effectiveness in working with psychosis in smaller studies (18, 19, 59, 103, 124, 125). However, most studies were either conceptualized for individual therapy and/or outpatients (5–7) with most available concepts still rather unsuitable and demanding for group inpatient settings. For an overview and further description of differences between treatments and key change mechanisms see Supplementary Table 3.
3.2. Step 2: intervention outcomes, change mechanisms, and logical model of change
Looking at each target area of our problem model, we formulated desired intervention outcomes and constructed a logical model of change (see Figure 3) linking outcomes and hypothesized mechanisms of change. As we were challenged to address the very diverse needs of our target population in one intervention, we made sure to come up with treatment goals applicable to a wide range of mental health problems. Following the ACT nomenclature, we therefore no longer speak of specific symptoms such as delusional thoughts or hallucinations, but group them together under the term distressing internal experiences (97).
Our overarching treatment goal was to encourage functional behavior and coping via improving cognitive flexibility. Cognitive flexibility thereby can be understood as the capacity to switch between cognitive processes in order to generate effective behavioral regulation and is determined by general metacognitive abilities (126). To achieve this objective, we aimed to raise patients’ cognitive insight on cognitive distortions and hence the patients’ capability to reflect on internal experiences on a meta-level (127, 128). Cognitive insight is linked to functional metacognitive knowledge and awareness and has been identified as a potential promising candidate mechanism for a decline of positive symptoms in psychosis and favorable treatment outcome in other disorders (127).
Furthermore, we aimed to reduce patients’ reactivity to aversive internal experiences via promoting cognitive defusion, which is determined by functional metacognitive goals and strategies. Cognitive defusion has been found to generally improve functioning, reduce dysfunctional attitudes, anxiety, negative affect (102) and also post-traumatic-like symptoms (129) and sleep difficulties (130). It has also been found to mediate symptom distress in psychosis via reduced believability of thought and voice content (131), and changes in metacognitive beliefs and coping skills (18).
Lastly, our intervention was supposed to support patients’ recovery by providing positive social support and with this foster peer group relationships, and a strong therapeutic alliance found to be essential ingredients for treatment success (132, 133). Overall, we hoped that our identified transdiagnostic change mechanisms and outcomes would support patients in a wide range of needs and topics, thus improving their mental health and QoL in the long term and prevent or at least mitigate further relapses.
We then divided all intervention outcomes into performance objectives (PO) (see Table 1), which we subsequently linked to our overarching change dimension via change objectives in our change matrix (see Table 2).
3.3. Step 3: evidence-based change methods
All change objectives were assigned to change techniques and practical applications in our matrix of change methods (see Table 3). The main change methods in our intervention blueprint consisted of therapeutic techniques fostering knowledge increase, introspection, perspective-taking and cognitive/behavioral regulation (69). As we faced the challenge to translate a complex set of change objectives and methods into very simple and comprehensible end applications for a group format, we made sure to come up with lots of interactive information sharing and fun exercises inspired by techniques used in existing mechanism-based interventions such as MCT, ACT and Metacognitive Therapy (see Step 1). For the change objective “Patient is able to allow distressing internal experiences” we for example planned to integrate a mindfulness training by performing simple guided exercises such as the “Leaves-on-a-river” from the ACT for psychosis manual (134).
3.4. Step 4: intervention outline
3.4.1. Transdiagnostic conceptualization
Although our intervention development aims to target mainly change mechanisms behind psychotic symptoms and crisis development trough symptom distress, the identified underlying impaired processes are interrelated with several other disorders (see Supplementary Table 2). Metacognitive deficits (135), cognitive distortions (61), a lack of cognitive insight (136), and cognitive fusion (137) for example play an important explanatory role among others in anxiety, mood, personality disorders, and substance abuse (138). Cognitive insight, cognitive defusion, social support, cognitive flexibility, and in turn improved metacognitive skills are considered to function as transdiagnostic mechanisms of change in therapy (123, 139–141). Hence, our transdiagnostic concept allows us to address not only the different needs of our patients with psychotic and comorbid diagnosis, but also patients with diagnoses other than psychosis. Given the heterogeneous patient composition of acute ward, a transdiagnostic mindset and approach might be an especially valuable treatment component (24).
3.4.2. Modules and sessions
Our final intervention comprised a 5-week group therapy program consisting of three short treatment modules and a total of nine sessions.
Module I (Psychoeducation) gives a brief introduction into the rational of the therapy and the targeted change mechanisms. The terms cognitive distortions and cognitive fusion and their role in the development of general psychological problems are explained in a simple language and with the help of examples and small exercises. The importance of cognitive insight and cognitive defusion for mental health is made clear.
Module II (Cognitive Insight) consists of four sessions and aims to raise cognitive insight by explaining and illustrating different cognitive biases and demonstrating their negative consequences on mental health. The treatment module includes materials and interventions adapted from the MCT for psychosis, MCT for depression and MCT for acute psychiatric settings (MCT-acute) and focuses on the change domains metacognitive knowledge and awareness.
Module III (Cognitive Defusion) with another four sessions aims to change the function internal experiences have on the patient’s behavior by strengthening adaptive coping strategies. Exercises are assembled from various ACT and Metacognitive therapy manuals and cover the change domains metacognitive goals and strategies. An overview of the intervention’s contents and sources for used materials can be found in Table 4.
All sessions follow the same general procedure: entrance round with mood poll, brief introduction to the program and group rules, experience-based exercises and group discussions, linking therapy content to mental health problems, transferring knowledge into every-day life, take-home message and closing round.
3.4.3. Delivery format and framework
We propose group therapy takes place twice a week with each session lasting between 40 and 60 minutes depending on the group’s cognitive capacity. To ensure a maximum of flexibility for patients with brief treatment duration and attendance preferences, all modules are independent from each other and each session can be delivered stand-alone. Information is presented on simple PowerPoint slides with plain language, short inputs and illustrating imagery makes participation possible even for patients with pronounced cognitive impairments. Simple metaphors, concrete and personally relevant experience-based exercises and “touchable” therapy material (e.g., bringing dark sunglasses to demonstrate the information filter of our mind) make contents additionally easy to understand and create a relaxed atmosphere (97). All patients receive a patient workbook with short session summaries, exercises and optional homework assignments. Two therapy-cards in pocket size summarize the most important points of each module. See Figure 4 for therapy content examples. Due to high levels of distress and occasionally hostile and suspicious behaviors, group sizes are kept small with a maximum of seven participants. Group sessions can be carried out by a clinical psychologist, psychiatrist, trained nurse or an occupational therapist, as little prior knowledge is required because of its simple conceptualization and available therapy manual. Next to group therapy, we advise all patients receive psychosocial treatment-as-usual (see Supplementary Methods) and additional individual psychotherapy sessions.
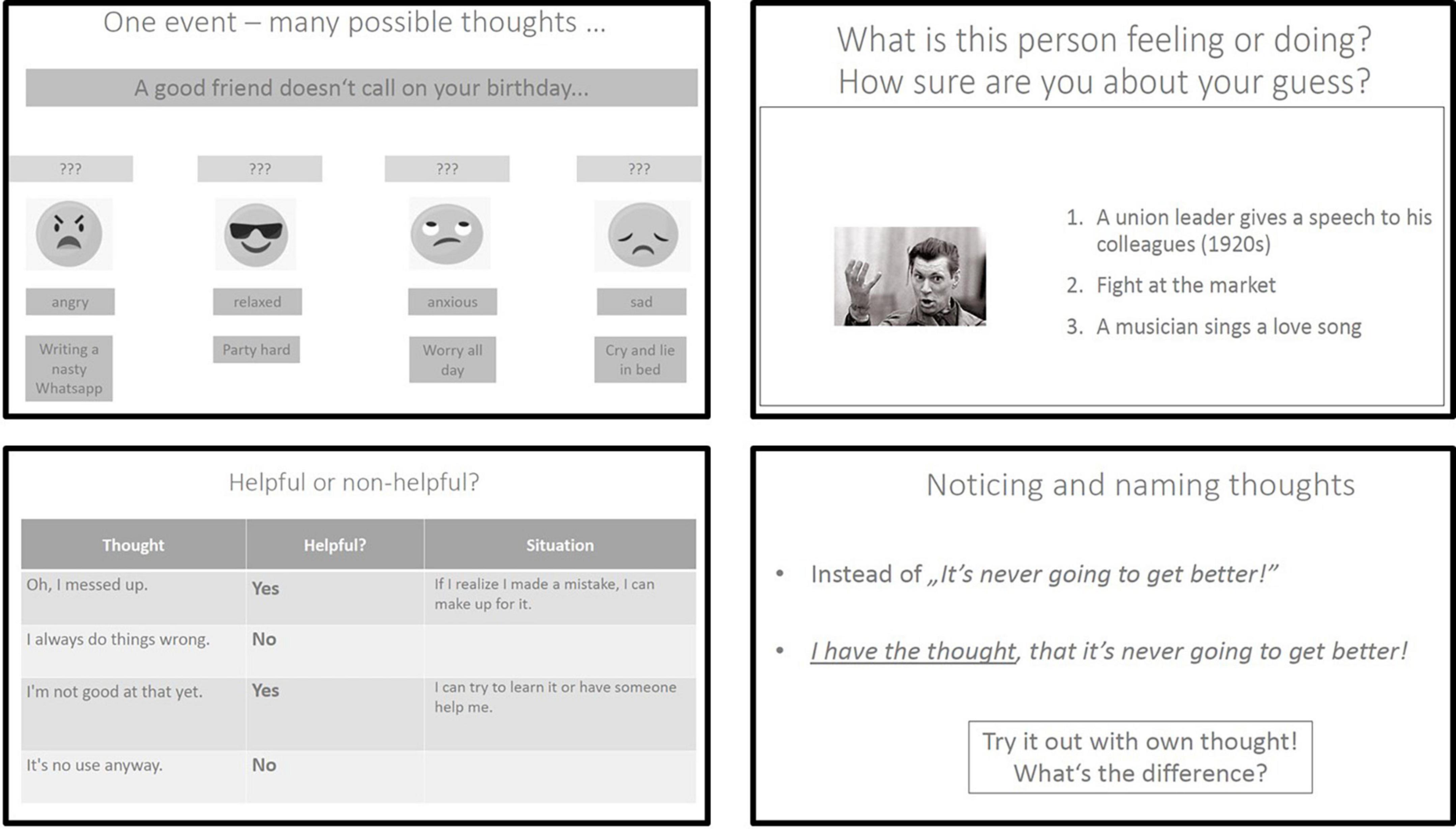
Figure 4. Example slides from each module. Top left: Slide from the module “Psychoeducation”. Patients learn to understand that different thoughts can lead to different feelings and behaviors (slight adapted from the MCT manual for depression) (72) (p. 105). Top right: Slide from the module “Cognitive Insight” and session “To empathize”. Patients learn to understand that facial expressions can easily be misinterpreted (slide used from the MCT-acute concept, open source on the MCT website, https://clinical-neuropsychology.de/metacognitive_training/). Bottom left: Slide from the module “Cognitive Defusion” and session “Helpful vs. unhelpful thoughts”. Patients learn to distinguish between helpful and unhelpful internal experiences. Bottom right: Slide from the module “Cognitive Defusion” and session “Defusion techniques”. Patients learn to notice and name thoughts in order to create distance to them instead of getting entangled in thought contents and automatic reactions.
3.4.4. Therapeutic attitude
The therapists general therapeutic attitude should be empowering trying to support patients to pursue their valued goals despite symptoms of serious mental illness (28, 97). They should moreover try to create an open, acceptance-based and destigmatizing atmosphere (142). The therapists’ process-oriented stance, which sees psychotic symptoms as extreme manifestations of normal human cognitive distortions and dysfunctional strategies, can thereby foster rapid alliance building (21). Self-disclosure by therapists is strongly recommended at this point, as it allows them to convey to patients that they too are often “victims” of their own cognitive biases (97). Thereby, they work in accordance to key features of third-wave therapies that place therapists on an equal level to patients in the sense of “you cannot teach what you cannot do” (9) (p. 369). A focus on mechanisms of change rather than symptom disputation moreover reveals room for change and returns a sense of control to patients (10).
Group attendance is voluntary, however, participants should be personally approached before each session to encourage participation (28). During sessions, patients have the possibility to leave the group if they feel uncomfortable as well as the option to return. Contents of psychotic thoughts and experiences can be talked about openly without being judged as wrong, right or even pathological (142). Therapy sessions should not be rushed and therapists should give enough time for discussion and exchange between the participants. They can promote involvement by directly approaching patients with simple questions and thus encouraging socially anxious participants. Following the transdiagnostic concept of the intervention, disease-related language is rarely used (143).
4. Discussion
The current research aimed to develop a novel mechanism-based therapy for acute inpatients with psychotic symptoms using Intervention Mapping as a structured development framework to improve the intervention’s scientific foundation, reporting standards and potential reproducibility. To our knowledge, this is the first research for this specific setting and patient group, which has attempted to do so.
MEBASp is a low-threshold transdiagnostic and modularized group therapy that focuses on symptom and distress reduction and responds to a central priority of health care services to develop, test and offer effective and needs-oriented care for acute inpatients with psychosis (5–7). We believe that our underlying intervention model and format will be able to meet the complex needs of those patients and the settings they are treated in due to several reasons.
Firstly, our intervention directly targets hypothesized change mechanisms instead of specific symptom content and hence follows a current promising paradigm shift in intervention science toward process-based treatments (13, 75, 144). We believe that our mechanism focus will not only allow us to optimize patients’ treatment outcomes (13), but will be especially helpful when working with acute (involuntary) inpatients. As suggested by Moritz and Woodward (21), MEBASp operates through a non-confrontational and symptom-neutral “backdoor” approach (p. 623) that could be beneficial to address a transdiagnostic spectrum of patients and diverse needs, foster rapid alliance building, motivate resistant patients, lower drop-out rates, and enhance recovery rather than illness elimination (6, 16, 19, 145). By combining evidence-based mechanisms and procedures from various theories and therapy schools into one approach, we moreover refocus on key questions of why and how interventions work best for patients instead of if they align or differ from specific therapy approaches (75).
Our intervention’s overarching emphasis on transdiagnostic metacognitive change mechanisms (cognitive insight and cognitive defusion) furthermore fits in a new generation of treatments promoting recovery from serious mental illnesses including psychosis (104, 138). The concept of metacognition thereby is believed to serve as a valid candidate for filling the gap between simplistic biological treatment models and psychosocial ones (104). A main benefit of metacognitive treatment models is the promotion of overall wellbeing beyond the positive symptom reduction achieved through psychopharmaceuticals, an aspect considered to be essential when working in psychiatric inpatient care (27). However, authors criticize that existing treatments only cover certain aspects of the larger construct of metacognition (see Supplementary Table 3) (93) and call for intervention development that incorporate all four metacognitive domains into hybrid approaches (104). Due to our modularized treatment concept, MEBASp is actually able to enclose the whole spectrum of metacognitive mechanisms into one intervention. Patients therefore not only benefit from a broad range of hypothesized positive treatment effects when attending all three modules, but already profit when attending only one or two (76).
Despite an underlying change theory seeming complex at first sight, we moreover believe that we managed to adapt the intervention for the inpatient context. MEBASp is brief, flexible, experience oriented, low-key and easy to learn for therapists and thus takes into account key treatment elements proposed by competence frameworks in working with acute patients (26, 58). The modularized approach moreover allows to combine and integrate different independent treatment modules and therewith ensures high flexibility and goodness-of-fit to patient needs and preferences (146). All procedures taken from in- and outpatient concepts are simplified and adapted for a crisis-focused setting addressing both priorities of symptom (cognitive insight) and distress reduction (cognitive defusion) (25). On top of that, the group-based design permits high therapy frequency and dose, is cost-effective, resource saving and offers opportunities for peer social support and interpersonal skill development (147).
4.1. Advantages to the IM approach
Although the research base on process-oriented care is growing, authors do not yet provide a standardized method on how to construct evidence-based problem models, choose adequate sets of change mechanisms, procedures and change measures (13, 148). In this context, IM offers different structured elements to overcome those challenges. The PRECEDE-model allowed us the synthetization of multi-level data and an in-depth understanding of our situation necessary for identifying evidence-based change mechanisms (31). Building matrices of change and change procedures represented a valuable method to ensure our change mechanisms were precisely defined (148) and got effectively linked to therapeutic applications (75). In doing so, we could refer back to IM-associated extensive frameworks such as the Theoretical Domains Framework (68) and the taxonomy of behavior change methods (69) that clearly close the gap of comparable compositions in the literature (144). Thereby, IM per se works according to principles of mechanism-based therapies by being “theory agnostic,” flexibly combining evidence-based concepts from across paradigms and thus creating synergistic effects between different approaches (149). Lastly, the detailed mapping of all change mechanisms and procedures in an intervention blueprint reflects the underlying complexity of our intervention and allows the derivation of matching outcome measures to monitor change in future studies (as described in the future direction sections) (148).
4.2. Limitations
There are several limitations to the current research. First, the mechanism and procedure selection were based on considerations and decisions made by our development team in each step of the IM framework. A different working group could have created a different needs analysis and chosen a different treatment focus, change methods and practical applications (see for example the CRISIS-, the WIT- or the OASIS-study) (150–152). Nevertheless, thanks to our detailed documentation of each decision step, potential differences become transparent and are made objectifiable.
Second, we encountered an excessive concept overlap in the literature (148). Cognitive defusion for example shares significant variance with constructs such as deliteralization, decentering, distancing and detached mindfulness (102). Moreover, the concept of metacognition is also somewhat “blurry” making it difficult to separate accurately what is a metacognitive and what a purely cognitive change mechanism (153). A central source integrating processes, mechanisms and procedures and using a common language and conceptualization would have made our selection much easier and the final intervention potentially more comparable with other mechanism-based treatments.
Thirdly, the complex set of mechanisms underlying the intervention could be seen as a challenge. From a clinical perspective, an intervention focusing on trying to change such a variety of mechanisms might be an overload for acute inpatients. Along with this, our mechanism-based group will naturally not provide the appropriate content and format for all patients due to varying needs and preferences. In addition to alternative therapy options (see Supplementary Figure 1), further research should investigate which patients can particularly benefit to make appropriate therapy offers.
Fourthly, due to time and resource constraints and in consideration of protecting the wellbeing our vulnerable target population, we did not conduct codesign activities during the first development stage. This decision may have limited the intervention prototype’s suitability and acceptability for patients. Although we relied on pre-existing qualitative data and plan to integrate codesign activities in the second stage of the development process (feasibility study), future research should explore appropriate and sensitive ways to involve patients already in the first development stage.
Finally, although we found the detailed approach of IM helpful in creating our intervention and followed most of its steps, the overall development process was time consuming and took up a lot of resources. If teams thus require rapid intervention development, a more pragmatic approach such as the 6SQuID (“Six steps in quality intervention development”) (154) might be favored over IM.
4.3. Implications and future directions
Our mechanistic treatment design enables us to conduct necessary research to determine whether our proposed mechanisms are capable of producing therapeutic change (13). A single-arm feasibility study investigating the impact of MEBASp is currently in progress (clinicalTrials.gov identifier: NCT04874974) (74). The study includes a mixed methods evaluation to assess the feasibility and test key change mechanisms of our logical model of change. Next to primary outcome measures such as trial entry rate, patient engagement and satisfaction, the study includes metacognitive measures e.g., the Beck Cognitive Insight Scale (155) and the Cognitive Fusion Questionnaire (156). Intensive involvement of participants trough codedesign activities such as feedback questionnaires, feedback rounds and interviews moreover ensures the revision of the intervention prototype will be in accordance to patients’ needs and preferences (157). If feasible and acceptable, future research will further investigate on the effects of change mechanisms by involving a control condition and performing mediation analyses in a larger scale study. Our ultimate goal is to individualize treatment allocation by matching patients to the treatment module most likely to produce change and fit with personal preferences (see Supplementary Figure 1). The allocation process could in the long term involve e.g., moderation studies, complex network approaches and ecological momentary assessments (75).
4.4. Conclusion
Our research demonstrates the importance of a) developing needs-oriented and mechanism-based interventions for acute inpatients with psychotic symptoms and b) using a structured development methodology to ensure their scientific foundation and replicability. Our rigorous and evidence-based intervention design focuses on addressing metacognitive change mechanisms associated with both acute symptoms and crisis development and adapts to key components required to deliver psychotherapy in psychiatric inpatient settings. It therefore has the potential to positively impact a neglected patient group. However, a pilot study is required to assess the intervention for safety, feasibility and preliminary effectiveness.
Data availability statement
The original contributions presented in this study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
EG, SL, PF, FP, SE, and JK-B: research objectives, project methodology, needs-analysis, guidance of process and clinical input, review intervention prototype, and manuscript write-up. EG: theoretical framework for intervention, material development and beta testing with patients. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by the Max Planck Institute of Psychiatry and the Alfred Golombek Foundation.
Acknowledgments
We thank the team and the patients of the acute closed ward of the Max Planck Institute of Psychiatry that gave their informal and very valuable feedback on the intervention’s prototype. We also thank Prof. Steffen Moritz (University Clinic Hamburg), who provides Metacognitive Training therapy material free of charge and open source, and thereby makes a major contribution to the advancement of research in the field of psychosis and other disorders.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1160075/full#supplementary-material
References
1. Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull. (2007) 34:523–37. doi: 10.1093/schbul/sbm114
2. van der Gaag M, Valmaggia L, Smit F. The effects of individually tailored formulation-based cognitive behavioural therapy in auditory hallucinations and delusions: a meta-analysis. Schizophr Research. (2014) 156:30–7. doi: 10.1016/j.schres.2014.03.016
4. NICE. Psychosis and Schizophrenia in Adults: Prevention and Management. 2 Redman Place: National Institute of Clinical Excellence (2014).
5. Barnicot K, Michael C, Trione E, Lang S, Saunders T, Sharp M, et al. Psychological interventions for acute psychiatric inpatients with schizophrenia-spectrum disorders: a systematic review and meta-analysis. Clin Psychol Rev. (2020) 82:101929. doi: 10.1016/j.cpr.2020.101929
6. Wood L, Williams C, Billings J, Johnson S. A systematic review and meta-analysis of cognitive behavioural informed psychological interventions for psychiatric inpatients with psychosis. Schizophr Res. (2020) 222:133–44. doi: 10.1016/j.schres.2020.03.041
7. Jacobsen P, Hodkinson K, Peters E, Chadwick P. A systematic scoping review of psychological therapies for psychosis within acute psychiatric in-patient settings. Br J Psychiatry. (2018) 213:490–7. doi: 10.1192/bjp.2018.106
8. Aghotor J, Pfueller U, Moritz S, Weisbrod M, Roesch-Ely D. Metacognitive training for patients with schizophrenia (MCT): feasibility and preliminary evidence for its efficacy. J Behav Ther Exp Psychiatry. (2010) 41:207–11. doi: 10.1016/j.jbtep.2010.01.004
9. Hayes S, Hofmann S. The third wave of cognitive behavioral therapy and the rise of process-based care. World Psychiatry. (2017) 16:245–6. doi: 10.1002/wps.20442
10. Pankey, J, Hayes S. Acceptance and commitment therapy for psychosis. Int. J. Psychol. Psychol. Ther. (2003) 3:311–28.
11. Schaeuffele C, Schulz A, Knaevelsrud C, Renneberg B, Boettcher J. CBT at the crossroads: the rise of transdiagnostic treatments. J Cogn Ther. (2021) 14:86–113. doi: 10.1007/s41811-020-00095-2
12. Roiser J, Elliott R, Sahakian B. Cognitive mechanisms of treatment in depression. Neuropsychopharmacol. (2012) 37:117–36. doi: 10.1038/npp.2011.183
13. Kazdin A. Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol. (2007) 3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432
14. Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry. (2005) 62:975. doi: 10.1001/archpsyc.62.9.975
15. Drake R, Husain N, Marshall M, Lewis S, Tomenson B, Chaudhry I, et al. Effect of delaying treatment of first-episode psychosis on symptoms and social outcomes: a longitudinal analysis and modelling study. Lancet Psychiatry. (2020) 7:602–10. doi: 10.1016/S2215-0366(20)30147-4
16. Wood L, Williams C, Billings J, Johnson S. Psychologists’, perspectives on the implementation of psychological therapy for psychosis in the acute psychiatric inpatient setting. Qual Health Res. (2019) 29:2048–56. doi: 10.1177/1049732319843499
17. Morris E, Johns L, Oliver J. Acceptance and Commitment Therapy and Mindfulness for Psychosis. Oxford: John Wiley & Sons (2013). doi: 10.1002/9781118499184
18. Bach P, Gaudiano B, Hayes S, Herbert J. Acceptance and commitment therapy for psychosis: intent to treat, hospitalization outcome and mediation by believability. Psychosis. (2013) 5:166–74. doi: 10.1080/17522439.2012.671349
19. Gaudiano B, Herbert J. Acute treatment of inpatients with psychotic symptoms using acceptance and commitment therapy: pilot results. Behav Res Ther. (2006) 44:415–37. doi: 10.1016/j.brat.2005.02.007
20. Tyrberg M, Carlbring P, Lundgren T. Brief acceptance and commitment therapy for psychotic inpatients: a randomized controlled feasibility trial in Sweden. Nordic Psychology. (2017) 69:110–25. doi: 10.1080/19012276.2016.1198271
21. Moritz S, Woodward T. Metacognitive training in schizophrenia: from basic research to knowledge translation and intervention. Curr Opin Psychiatry. (2007) 20:619–25. doi: 10.1097/YCO.0b013e3282f0b8ed
22. Kumar D, Menon M, Moritz S, Woodward T. Using the back door: metacognitive training for psychosis. Psychosis. (2015) 7:166–78. doi: 10.1080/17522439.2014.913073
23. Moritz S, Veckenstedt R, Bohn F, Hottenrott B, Scheu F, Randjbar S, et al. Complementary group Metacognitive Training (MCT) reduces delusional ideation in schizophrenia. Schizophr Res. (2013) 151:61–9. doi: 10.1016/j.schres.2013.10.007
24. Bowers L, Chaplin R, Quirk A, Lelliott P. A conceptual model of the aims and functions of acute inpatient psychiatry. J Ment Health. (2009) 18:316–25. doi: 10.1080/09638230802053359
25. Wood L, Williams C, Billings J, Johnson S. The therapeutic needs of psychiatric in-patients with psychosis: a qualitative exploration of patient and staff perspectives. BJPsych Open. (2019) 5:e45. doi: 10.1192/bjo.2019.33
26. Wood L, Williams C. Acute Mental Health Inpatient Competence Framework: Adults and Older Adults. London: University College London (2022).
27. Wood L, Alsawy S. Patient experiences of psychiatric inpatient care: a systematic review of qualitative evidence. J. Psych. Intensive Care (2016) 12:35–43. doi: 10.20299/jpi.2016.001
28. Wood L, Jacobsen P, Ovin F, Morrison A. Key components for the delivery of cognitive behavioral therapies for psychosis in acute psychiatric inpatient settings: a delphi study of therapists’, views. Schizophr Bull Open. (2022) 3:sgac005. doi: 10.1093/schizbullopen/sgac005
29. Duncan E, O’Cathain A, Rousseau N, Croot L, Sworn K, Turner K, et al. Guidance for reporting intervention development studies in health research (GUIDED): an evidence-based consensus study. BMJ Open. (2020) 10:e033516. doi: 10.1136/bmjopen-2019-033516
30. Ioannidis J. Why most clinical research is not useful. PLoS Med. (2016) 13:e1002049. doi: 10.1371/journal.pmed.1002049
31. Bleijenberg N, de Man-van Ginkel J, Trappenburg J, Ettema R, Sino C, Heim N, et al. Increasing value and reducing waste by optimizing the development of complex interventions: enriching the development phase of the Medical Research Council (MRC) Framework. Int J Nurs Stud. (2018) 79:86–93. doi: 10.1016/j.ijnurstu.2017.12.001
32. Skivington K, Matthews L, Simpson S, Craig P, Baird J, Blazeby J, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. (2021) 374:n2061. doi: 10.1136/bmj.n2061
33. Hoffmann T, Glasziou P, Boutron I, Milne R, Perera R, Moher D, et al. Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. BMJ. (2014) 348:g1687. doi: 10.1136/bmj.g1687
34. Hurley D, Murphy L, Hayes D, Hall A, Toomey E, McDonough S, et al. Using intervention mapping to develop a theory-driven, group-based complex intervention to support self-management of osteoarthritis and low back pain (SOLAS). Implementation Sci. (2015) 11:56. doi: 10.1186/s13012-016-0418-2
35. van Mol M, Nijkamp M, Markham C, Ista E. Using an intervention mapping approach to develop a discharge protocol for intensive care patients. BMC Health Serv Res. (2017) 17:837. doi: 10.1186/s12913-017-2782-2
36. O’Donnell R, Dobson R, De Bruin M, Turner S, Booth L, Semple S. Development of a smoke-free homes intervention for parents: an intervention mapping approach. HPB. (2019) 3:67. doi: 10.5334/hpb.20
37. Ravicz M, Muhongayire B, Kamagaju S, Klabbers R, Faustin Z, Kambugu A, et al. Using Intervention Mapping methodology to design an HIV linkage intervention in a refugee settlement in rural Uganda. AIDS Care. (2022) 34:446–58. doi: 10.1080/09540121.2021.1900532
38. Orgeta V, Palpatzis E, See Y, Tuijt R, Verdaguer E, Leung P. Development of a psychological intervention to promote meaningful activity in people living with mild dementia: an intervention mapping approach. Gerontologist. (2022) 62:629–41. doi: 10.1093/geront/gnab047
39. Brendryen H, Johansen A, Nesvåg S, Kok G, Duckert F. Constructing a theory- and evidence-based treatment rationale for complex ehealth interventions: development of an online alcohol intervention using an intervention mapping approach. JMIR Res Protoc. (2013) 2:e6. doi: 10.2196/resprot.2371
40. van Agteren J, Iasiello M, Ali K, Fassnacht D, Furber G, Woodyatt L, et al. Using the intervention mapping approach to develop a mental health intervention: a case study on improving the reporting standards for developing psychological interventions. Front Psychol. (2021) 12:648678. doi: 10.3389/fpsyg.2021.648678
41. Machado D, Murta S, da Costa I. Applying intervention mapping approach to a program for early intervention in first-episode mental crisis of a psychotic type. Psicol Refl Crít. (2020) 33:3. doi: 10.1186/s41155-020-00141-0
42. Fernandez M, Ruiter R, Markham C, Kok G. Intervention mapping: theory- and evidence-based health promotion program planning: perspective and examples. Front Public Health. (2019) 7:209. doi: 10.3389/fpubh.2019.00209
43. Bartholomew Eldredge L. Planning Health Promotion Programs: An Intervention Mapping Approach. 4th ed. San Francisco, CA: Jossey-Bass & Pfeiffer Imprints, Wiley (2016). 1.
44. Palmer V, Chondros P, Furler J, Herrman H, Pierce D, Godbee K, et al. The CORE study—An adapted mental health experience codesign intervention to improve psychosocial recovery for people with severe mental illness: a stepped wedge cluster randomized-controlled trial. Health Expect. (2021) 24:1948–61. doi: 10.1111/hex.13334
45. Mooney R, Newbigging K, McCabe R, McCrone P, Halvorsrud K, Raghavan R, et al. Experience-based investigation and codesign of approaches to prevent and reduce Mental Health Act use (CO-PACT): a protocol. BMJ Open. (2022) 12:e060086. doi: 10.1136/bmjopen-2021-060086
46. Schouten S, Kip H, Dekkers T, Deenik J, Beerlage-de Jong N, Ludden G, et al. Best-practices for co-design processes involving people with severe mental illness for eMental health interventions: a qualitative multi-method approach. Design Health. (2022) 6:316–44. doi: 10.1080/24735132.2022.2145814
47. Illarregi E, Alexiou K, DiMalta G, Zamenopoulos T. Is designing therapeutic? A case study exploring the experience of co-design and psychosis. Psychosis. (2022) 7:1–15. doi: 10.1080/17522439.2022.2052450
48. Locock L, Robert G, Boaz A, Vougioukalou S, Shuldham C, Fielden J, et al. Testing accelerated experience-based co-design: a qualitative study of using a national archive of patient experience narrative interviews to promote rapid patient-centred service improvement. Health Serv Deliv Res. (2014) 2:1–122. doi: 10.3310/hsdr02040
49. Davies B. Coercion or collaboration? Nurses doing research with people who have severe mental health problems. J. Psychiatr. Ment. Health Nurs. (2005) 12:106–11. doi: 10.1111/j.1365-2850.2004.00808.x
50. Owen S. The practical, methodological and ethical dilemmas of conducting focus groups with vulnerable clients. J Adv Nurs. (2001) 36:652–8. doi: 10.1046/j.1365-2648.2001.02030.x
51. Nicaise P, Giacco D, Soltmann B, Pfennig A, Miglietta E, Lasalvia A, et al. Healthcare system performance in continuity of care for patients with severe mental illness: a comparison of five European countries. Health Policy. (2020) 124:25–36. doi: 10.1016/j.healthpol.2019.11.004
52. O’Cathain A, Croot L, Sworn K, Duncan E, Rousseau N, Turner K, et al. Taxonomy of approaches to developing interventions to improve health: a systematic methods overview. Pilot Feasibility Stud. (2019) 5:41. doi: 10.1186/s40814-019-0425-6
53. Green L, Kreuter M, Green L. Health Program Planning: An Educational and Ecological Approach. 4th ed. New York, NY: McGraw-Hill (2005). 1.
54. Glanz K, Rimer B, Viswanath K. Health Behavior and Health Education: Theory, Research, and Practice. 4th Edn. San Francisco, CA: Jossey-Bass (2008). 552.
55. Paterson C, Karatzias T, Dickson A, Harper S, Dougall N, Hutton P. Psychological therapy for inpatients receiving acute mental health care: a systematic review and meta-analysis of controlled trials. Br J Clin Psychol. (2018) 57:453–72. doi: 10.1111/bjc.12182
56. Wood L, Birtel M, Alsawy S, Pyle M, Morrison A. Public perceptions of stigma towards people with schizophrenia, depression, and anxiety. Psychiatry Res. (2014) 220:604–8. doi: 10.1016/j.psychres.2014.07.012
57. Wood L, Williams C, Billings J, Johnson S. The role of psychology in a multidisciplinary psychiatric inpatient setting: perspective from the multidisciplinary team. Psychol Psychother Theory Res Pract. (2019) 92:554–64. doi: 10.1111/papt.12199
58. Roth A, Pilling S. A Competence Framework for Psychological Interventions With People With Psychosis and Bipolar Disorder. London: University College London (2012).
59. Bach P, Hayes S. The use of acceptance and commitment therapy to prevent the rehospitalization of psychotic patients: a randomized controlled trial. J Consul Clin Psychol. (2002) 70:1129–39. doi: 10.1037/0022-006X.70.5.1129
60. Moritz S, Klein J, Lysaker P, Mehl S. Metacognitive and cognitive-behavioral interventions for psychosis: new developments. Dialog Clin Neurosci. (2019) 21:309–17. doi: 10.31887/DCNS.2019.21.3/smoritz
61. Harvey A, Watkins E, Mansell W, Shafran R. Cognitive Behavioural Processes across Psychological Disorders (DRAFT): A Transdiagnostic Approach to Research and Treatment. Oxford: University Press (2004). doi: 10.1093/med:psych/9780198528883.001.0001
62. Krueger R, Eaton N. Transdiagnostic factors of mental disorders. World Psychiatry. (2015) 14:27–9. doi: 10.1002/wps.20175
63. Mawson A, Cohen K, Berry K. Reviewing evidence for the cognitive model of auditory hallucinations: the relationship between cognitive voice appraisals and distress during psychosis. Clin Psychol Rev. (2010) 30:248–58. doi: 10.1016/j.cpr.2009.11.006
64. Ebrahimi A, Poursharifi H, Dolatshahi B, Rezaee O, Hassanabadi H, Naeem F. The cognitive model of negative symptoms in schizophrenia: a hierarchical component model with PLS-SEM. Front Psychiatry. (2021) 12:707291. doi: 10.3389/fpsyt.2021.707291
65. Garety P, Freeman D. Cognitive approaches to delusions: a critical review of theories and evidence. Br J Clin Psychol. (1999) 38:113–54. doi: 10.1348/014466599162700
66. Freeman D. Persecutory delusions: a cognitive perspective on understanding and treatment. Lancet Psychiatry. (2016) 3:685–92. doi: 10.1016/S2215-0366(16)00066-3
67. Garety P, Kuipers E, Fowler D, Freeman D, Bebbington P. A cognitive model of the positive symptoms of psychosis. Psychol Med. (2001) 31:189–95. doi: 10.1017/S0033291701003312
68. Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implementation Sci. (2012) 7:37. doi: 10.1186/1748-5908-7-37
69. Kok G, Gottlieb N, Peters G, Mullen P, Parcel G, Ruiter R, et al. A taxonomy of behaviour change methods: an Intervention Mapping approach. Health Psychol Rev. (2016) 10:297–312. doi: 10.1080/17437199.2015.1077155
70. Hayes S, Hofmann S. Process-based C: The Science and Core Clinical Competencies of Cognitive Behavioral Therapy. Oakland, CA: New Harbinger Publications, Inc (2018). 452.
71. Frank R, Davidson J. The Transdiagnostic Road Map to Case Formulation and Treatment Planning Practical Guidance for Clinical Decision Making. Oakland, CA: New Harbinger Publications, Inc (2014).
72. Jelinek L, Hauschildt M, Moritz S. Metakognitives Training bei Depression (D-MKT): mit E-Book inside und Trainingsmaterial. 1. Aufl. Weinheim: Beltz (2015). 186.
73. Jelinek, L, Faissner M, Moritz S, Kriston L. Long-term efficacy of Metacognitive Training for Depression (D- MCT): a randomized controlled trial. Br J Clin Psychol. (2018) 58:245–59. doi: 10.1111/bjc.12213
74. Gussmann E. Feasibility of a Novel Process-Based Treatment for Patients With Psychosis. Bethesda, MD: ClinicalTrials.gov (2021).
75. Hofmann S, Hayes S. The future of intervention science: process-based therapy. Clin Psychol Sci. (2019) 7:37–50. doi: 10.1177/2167702618772296
76. Philippot P, Bouvard M, Baeyens C, Dethier V. Case conceptualization from a process-based and modular perspective: rationale and application to mood and anxiety disorders. Clin Psychol Psychother. (2019) 26:175–90. doi: 10.1002/cpp.2340
77. Pavlacic J, Young J. Process-based cognitive behavioral therapy: a framework for conceptualization and treatment. Clin Case Stud. (2020) 19:456–72. doi: 10.1177/1534650120951858
78. World Health Organization. The I-10 Classification of Mental and Behavioural Disorders: Diagnostic Criteria for Research. Geneva: World Health Organization (1993). 248.
79. Dubovsky S, Ghosh B, Serotte J, Cranwell V. Psychotic depression: diagnosis, differential diagnosis, and treatment. Psychother Psychosom. (2021) 90:160–77. doi: 10.1159/000511348
80. Penttilä M, Jääskeläinen E, Hirvonen N, Isohanni M, Miettunen J. Duration of untreated psychosis as predictor of long-term outcome in schizophrenia: systematic review and meta-analysis. Br J Psychiatry. (2014) 205:88–94. doi: 10.1192/bjp.bp.113.127753
81. Murru A, Carpiniello B. Duration of untreated illness as a key to early intervention in schizophrenia: a review. Neurosci Lett. (2018) 669:59–67. doi: 10.1016/j.neulet.2016.10.003
82. Petkari E, Pietschnig J. Associations of quality of life with service satisfaction in psychotic patients: a meta-analysis. PLoS One. (2015) 10:e0135267. doi: 10.1371/journal.pone.0135267
83. Karow A, Moritz S, Lambert M, Schoder S, Krausz M. PANSS syndromes and quality of life in schizophrenia. Psychopathology. (2005) 38:320–6. doi: 10.1159/000088921
84. Pascal de Raykeer R, Hoertel N, Blanco C, Lavaud P, Kaladjian A, Blumenstock Y, et al. Effects of depression and cognitive impairment on quality of life in older adults with schizophrenia spectrum disorder: results from a multicenter study. J. Affect. Disord. (2019) 256:164–75.
85. Dong M, Lu L, Zhang L, Zhang Y, Ng C, Ungvari G, et al. Quality of life in schizophrenia: a meta-analysis of comparative studies. Psychiatr Q. (2019) 90:519–32. doi: 10.1007/s11126-019-09633-4
86. Rector, N, Beck A, Stolar N. The negative symptoms of schizophrenia: a cognitive perspective. Can J Psychiatry. (2005) 50:247–57. doi: 10.1177/070674370505000503
87. Kim E, Jang M. The Mediating effects of self-esteem and resilience on the relationship between internalized stigma and quality of life in people with schizophrenia. Asian Nurs Res. (2019) 13:257–63. doi: 10.1016/j.anr.2019.09.004
88. Leendertse P, Myin-Germeys I, Lataster T, Simons C, Oorschot M, Lardinois M, et al. Subjective quality of life in psychosis: evidence for an association with real world functioning? Psychiatry Res. (2018) 261:116–23. doi: 10.1016/j.psychres.2017.11.074
89. White R, McCleery M, Gumley A, Mulholland C. Hopelessness in schizophrenia: the impact of symptoms and beliefs about illness. J Nervous Ment Dis. (2007) 195:968–75. doi: 10.1097/NMD.0b013e31815c1a1d
90. Lysaker P, Olesek K, Warman D, Martin J, Salzman A, Nicolò G, et al. Metacognition in schizophrenia: correlates and stability of deficits in theory of mind and self-reflectivity. Psychiatry Res. (2011) 190:18–22. doi: 10.1016/j.psychres.2010.07.016
91. Lysaker P, Kukla M, Dubreucq J, Gumley A, McLeod H, Vohs J, et al. Metacognitive deficits predict future levels of negative symptoms in schizophrenia controlling for neurocognition, affect recognition, and self-expectation of goal attainment. Schizophr Res. (2015) 168:267–72. doi: 10.1016/j.schres.2015.06.015
92. Tulving E, Madigan S. Memory and verbal learning. Annu Rev Psychol. (1970) 21:437–84. doi: 10.1146/annurev.ps.21.020170.002253
93. Moritz S, Lysaker P. Metacognition – What did James H. Flavell really say and the implications for the conceptualization and design of metacognitive interventions. Schizophr Res. (2018) 201:20–6. doi: 10.1016/j.schres.2018.06.001
94. Arnon-Ribenfeld N, Hasson-Ohayon I, Lavidor M, Atzil-Slonim D, Lysaker P. The association between metacognitive abilities and outcome measures among people with schizophrenia: a meta-analysis. Eur Psychiatr. (2017) 46:33–41. doi: 10.1016/j.eurpsy.2017.08.002
95. Moritz S, Veckenstedt R, Randjbar S, Vitzthum F, Karow A, Lincoln T. Course and determinants of self-esteem in people diagnosed with schizophrenia during psychiatric treatment. Psychosis. (2010) 2:144–53. doi: 10.1080/17522430903191791
96. David A, Bedford N, Wiffen B, Gilleen J. Failures of metacognition and lack of insight in neuropsychiatric disorders. Phil Trans R Soc B. (2012) 367:1379–90. doi: 10.1098/rstb.2012.0002
97. Bach, Patricia. Acceptance and commitment therapy for psychosis: applying acceptance and mindfulness in the context of an inpatient hospitalization. In: Gaudiano BA, editor, Incorporating Acceptance and Mindfulness into the Treatment of Psychosis: Current Trends and Future Directions. New York, NY: Oxford Academic (2016). Available online at: https://doi.org/10.1093/med:psych/9780199997213.003.0004 (accessed May 12, 2023).
98. Moritz S, Lüdtke T, Westermann S, Hermeneit J, Watroba J, Lincoln T. Dysfunctional coping with stress in psychosis. An investigation with the Maladaptive and Adaptive Coping Styles (MAX) questionnaire. Schizophr Res. (2016) 175:129–35. doi: 10.1016/j.schres.2016.04.025
99. Udachina A, Varese F, Myin-Germeys I, Bentall R. The role of experiential avoidance in paranoid delusions: an experience sampling study. Br J Clin Psychol. (2014) 53:422–32. doi: 10.1111/bjc.12054
100. de Leede-Smith S, Barkus E. A comprehensive review of auditory verbal hallucinations: lifetime prevalence, correlates and mechanisms in healthy and clinical individuals. Front Hum Neurosci. (2013) 7:367. doi: 10.3389/fnhum.2013.00367
101. Hayes S, Strosahl K, Wilson K. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change. 2 Edn. New York, NY: Guilford Press (2012). 402.
102. Bernstein A, Hadash Y, Lichtash Y, Tanay G, Shepherd K, Fresco D. Decentering and related constructs: a critical review and metacognitive processes model. Perspect Psychol Sci. (2015) 10:599–617. doi: 10.1177/1745691615594577
103. Morrison A, Pyle M, Chapman N, French P, Parker S, Wells A. Metacognitive therapy in people with a schizophrenia spectrum diagnosis and medication resistant symptoms: a feasibility study. J Behav Ther Exp Psychiatry. (2014) 45:280–4. doi: 10.1016/j.jbtep.2013.11.003
104. Lysaker P, Gagen E, Moritz S, Schweitzer R. Metacognitive approaches to the treatment of psychosis: a comparison of four approaches. PRBM. (2018) 11:341–51. doi: 10.2147/PRBM.S146446
105. Norman R, Malla A, Manchanda R, Harricharan R, Takhar J, Northcott S. Social support and three-year symptom and admission outcomes for first episode psychosis. Schizophr Res. (2005) 80:227–34. doi: 10.1016/j.schres.2005.05.006
106. Read J, Os J, Morrison A, Ross C. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr Scand. (2005) 112:330–50. doi: 10.1111/j.1600-0447.2005.00634.x
107. Leonhardt B, Huling K, Hamm J, Roe D, Hasson-Ohayon I, McLeod H, et al. Recovery and serious mental illness: a review of current clinical and research paradigms and future directions. Expert Rev Neurotherap. (2017) 17:1117–30. doi: 10.1080/14737175.2017.1378099
108. Haddock G, Eisner E, Boone C, Davies G, Coogan C, Barrowclough C. An investigation of the implementation of NICE-recommended CBT interventions for people with schizophrenia. J Ment Health. (2014) 23:162–5. doi: 10.3109/09638237.2013.869571
109. Bundespsychotherapeutenkammer. BPtK-Studie zur Stationären Versorgung Psychisch kranker Menschen Ergebnisse einer Befragung der in Krankenhäusern Angestellten Psychotherapeuten. Berlin: IGES (2014).
110. Slemon A, Jenkins E, Bungay V. Safety in psychiatric inpatient care: the impact of risk management culture on mental health nursing practice. Nurs Inq. (2017) 24:e12199. doi: 10.1111/nin.12199
111. Samele C, Frew S, Urquia N. Mental health Systems in the European Union Member States, Status of Mental Health in Populations and Benefits to be Expected from Investments into Mental Health. Brussels: European Commision (2013).
112. Carballedo A, Doyle M. Criteria for compulsory admission in some European countries. Int Psychiatry. (2011) 8:68–71. doi: 10.1192/S1749367600002617
113. Priebe S, Badesconyi A, Fioritti A, Hansson L, Kilian R, Torres-Gonzales F, et al. Reinstitutionalisation in mental health care: comparison of data on service provision from six European countries. BMJ. (2005) 330:123–6. doi: 10.1136/bmj.38296.611215.AE
114. Sharp M, Gulati A, Barker C, Barnicot K. Developing an emotional coping skills workbook for inpatient psychiatric settings: a focus group investigation. BMC Psychiatry. (2018) 18:208. doi: 10.1186/s12888-018-1790-z
115. Moos R. Iatrogenic effects of psychosocial interventions: treatment, life context, and personal risk factors. Substance Use Misuse. (2012) 47:1592–8. doi: 10.3109/10826084.2012.705710
116. Holloway F, Kalidindi S, Killaspy H, Roberts G. Enabling Recovery. (2015). Available online at: https://login.proxy.bib.uottawa.ca/login?url=https://www.cambridge.org/core/product/identifier/9781108673723/type/BOOK (accessed June 8, 2022).
117. Baigent M. Managing patients with dual diagnosis in psychiatric practice. Curr Opin Psychiatry. (2012) 25:201–5. doi: 10.1097/YCO.0b013e3283523d3d
118. Isham L, Grafahrend H, Nickless A, Pugh K, Pleasants S, Smedley N, et al. Group-based worry intervention for persecutory delusions: an initial feasibility study. Behav Cogn Psychother. (2018) 46:619–25. doi: 10.1017/S1352465818000383
119. Small C, Pistrang N, Huddy V, Williams C. Individual psychological therapy in an acute inpatient setting: service user and psychologist perspectives. Psychol Psychother Theory Res Pract. (2018) 91:417–33. doi: 10.1111/papt.12169
120. Griffiths R, Mansell W, Edge D, Tai S. Sources of distress in first-episode psychosis: a systematic review and qualitative metasynthesis. Qual Health Res. (2019) 29:107–23. doi: 10.1177/1049732318790544
121. Fischer R, Scheunemann J, Bohlender A, Duletzki P, Nagel M, Moritz S. ‘You are trying to teach us to think more slowly!’: adapting Metacognitive Training for the acute care setting—A case report. Clin Psychol Psychoth. (2022) 29:1877–85. doi: 10.1002/cpp.2755
122. Wells A. Metacognitive therapy for anxiety and depression. New York, NY: Guilford (2011). 316 p.
123. Assaz D, Roche B, Kanter J, Oshiro C. Cognitive defusion in acceptance and commitment therapy: what are the basic processes of change? Psychol Rec. (2018) 68:405–18. doi: 10.1007/s40732-017-0254-z
124. Hutton P, Morrison A, Wardle M, Wells A. Metacognitive therapy in treatment-resistant psychosis: a multiple-baseline study. Behav Cogn Psychother. (2014) 42:166–85. doi: 10.1017/S1352465812001026
125. Gaudiano B, Ellenberg S, Ostrove B, Johnson J, Mueser K, Furman M, et al. Feasibility and preliminary effects of implementing acceptance and commitment therapy for inpatients with psychotic-spectrum disorders in a clinical psychiatric intensive care setting. J Cogn Psychother. (2020) 34:80–96. doi: 10.1891/0889-8391.34.1.80
126. Uddin L. Cognitive and behavioural flexibility: neural mechanisms and clinical considerations. Nat Rev Neurosci. (2021) 22:167–79. doi: 10.1038/s41583-021-00428-w
127. Van Camp L, Sabbe B, Oldenburg J. Cognitive insight: a systematic review. Clin Psychol Rev. (2017) 55:12–24. doi: 10.1016/j.cpr.2017.04.011
128. Cooke M, Peters E, Greenwood K, Fisher P, Kumari V, Kuipers E. Insight in psychosis: influence of cognitive ability and self-esteem. Br J Psychiatry. (2007) 191:234–7. doi: 10.1192/bjp.bp.106.024653
129. Ito D, Watanabe A, Osawa K. Mindful attention awareness and cognitive defusion are indirectly associated with less PTSD-like symptoms via reduced maladaptive posttraumatic cognitions and avoidance coping. Curr Psychol. (2023) 42:1182–92. doi: 10.1007/s12144-021-01521-0
130. Salari N, Khazaie H, Hosseinian-Far A, Khaledi-Paveh B, Ghasemi H, Mohammadi M, et al. The effect of acceptance and commitment therapy on insomnia and sleep quality: a systematic review. BMC Neurol. (2020) 20:300. doi: 10.1186/s12883-020-01883-1
131. Gaudiano B, Herbert J, Hayes S. Is it the symptom or the relation to it? Investigating potential mediators of change in acceptance and commitment therapy for psychosis. Behav Ther. (2010) 41:543–54. doi: 10.1016/j.beth.2010.03.001
132. Krijnen L, Lemmers-Jansen I, Fett A, Krabbendam L. Benefits of social contact in individuals with psychotic symptoms: do closeness of the contact and empathic skills make the difference? Front Psychol. (2021) 12:769091. doi: 10.3389/fpsyg.2021.769091
133. Shattock L, Berry K, Degnan A, Edge D. Therapeutic alliance in psychological therapy for people with schizophrenia and related psychoses: a systematic review. Clin Psychol Psychother. (2018) 25:e60–85. doi: 10.1002/cpp.2135
134. O’Donoghue E, Morris E, Oliver J, Johns L. ACT for Psychosis Recovery: A practical Manual for Group-Based Interventions Using Acceptance & Commitment Therapy. Oakland, CA: New Harbinger Publications (2018).
135. Harvey AG. A cognitive model of insomnia. Behav Res Ther. (2002) 40:869–93. doi: 10.1016/S0005-7967(01)00061-4
136. Colis M, Steer R, Beck A. Cognitive insight in inpatients with psychotic, bipolar, and major depressive disorders. J Psychopathol Behav Assess. (2006) 28:242–9. doi: 10.1007/s10862-005-9012-7
137. Bardeen J, Fergus T. The interactive effect of cognitive fusion and experiential avoidance on anxiety, depression, stress and posttraumatic stress symptoms. J Contextual Behav Sci. (2016) 5:1–6. doi: 10.1016/j.jcbs.2016.02.002
138. Lysaker P, Hamm J, Hasson-Ohayon I, Pattison M, Leonhardt B. Promoting recovery from severe mental illness: implications from research on metacognition and metacognitive reflection and insight therapy. WJP. (2018) 8:1–11. doi: 10.5498/wjp.v8.i1.1
139. Dennis J, Vander Wal J. The cognitive flexibility inventory: instrument development and estimates of reliability and validity. Cogn Ther Res. (2010) 34:241–53. doi: 10.1007/s10608-009-9276-4
140. Barker C, Pistrang N. Psychotherapy and social support. Clin Psychol. Rev. (2002) 22:361–79. doi: 10.1016/S0272-7358(01)00101-5
141. Castonguay L, Hill C. Transformation in Psychotherapy: Corrective Experiences Across Cognitive Behavioral, Humanistic, and Psychodynamic Approaches. Washington, DC: American Psychological Association (2012). doi: 10.1037/13747-000
142. Moritz S, Vitzthum F, Randjbar S, Veckenstedt R, Woodward T. Detecting and defusing cognitive traps: metacognitive intervention in schizophrenia. Curr Opin Psychiatry. (2010) 23:561–9. doi: 10.1097/YCO.0b013e32833d16a8
143. Nolen-Hoeksema S, Watkins ERA. Heuristic for developing transdiagnostic models of psychopathology: explaining multifinality and divergent trajectories. Perspect Psychol Sci. (2011) 6:589–609. doi: 10.1177/1745691611419672
144. Hayes S, Hofmann S. “Third-wave” cognitive and behavioral therapies and the emergence of a process-based approach to intervention in psychiatry. World Psychiatry. (2021) 20:363–75. doi: 10.1002/wps.20884
145. Evlat G, Wood L, Glover N. A systematic review of the implementation of psychological therapies in acute mental health inpatient settings. Clin Psychol Psychoth. (2021) 28:1574–86. doi: 10.1002/cpp.2600
146. Elsaesser M, Herpertz S, Piosczyk H, Jenkner C, Hautzinger M, Schramm E. Modular-based psychotherapy (MoBa) versus cognitive–behavioural therapy (CBT) for patients with depression, comorbidities and a history of childhood maltreatment: study protocol for a randomised controlled feasibility trial. BMJ Open. (2022) 12:e057672. doi: 10.1136/bmjopen-2021-057672
147. Newton E, Larkin M, Melhuish R, Wykes T. More than just a place to talk: young people’s experiences of group psychological therapy as an early intervention for auditory hallucinations. Psychol Psychother. (2007) 80:127–49. doi: 10.1348/147608306X110148
148. Ong C, Levin M, Twohig M. Beyond acceptance and commitment therapy: process-based therapy. Psychol. Rec. (2020) 70:637–48. doi: 10.1007/s40732-020-00397-z
149. Bartholomew Eldredge L, Markham C, Ruiter R, Fernández M, Kok G, Parcel G. Planning Health Promotion Programs: An Intervention Mapping Approach. 4th ed. San Francisco, CA: Jossey-Bass, a Wiley Brand (2016). 678.
150. Wood L, Williams C, Pinfold V, Nolan F, Morrison A, Morant N, et al. Crisis-focused Cognitive Behavioural Therapy for Psychosis (CBTp) vs Treatment as Usual in Acute Mental Health Inpatient Settings (The CRISIS Study): Protocol For a Feasibility Randomised Controlled Trial. (2021). Available online at: https://www.researchsquare.com/article/rs-270658/v1 (accessed July 15, 2022). doi: 10.21203/rs.3.rs-270658/v1
151. Freeman D, Dunn G, Startup H, Pugh K, Cordwell J, Mander H, et al. Effects of cognitive behaviour therapy for worry on persecutory delusions in patients with psychosis (WIT): a parallel, single-blind, randomised controlled trial with a mediation analysis. Lancet Psychiatry. (2015) 2:305–13. doi: 10.1016/S2215-0366(15)00039-5
152. Freeman D, Sheaves B, Goodwin G, Yu L, Nickless A, Harrison P, et al. The effects of improving sleep on mental health (OASIS): a randomised controlled trial with mediation analysis. Lancet Psychiatry. (2017) 4:749–58. doi: 10.1016/S2215-0366(17)30328-0
153. Andreou C, Balzan R, Jelinek L, Moritz S. Letter to the editor: metacognitive training and metacognitive therapy. A reply to Lora Capobianco and Adrian Wells. J Behav Ther Exp Psychiatry. (2018) 59:162–3. doi: 10.1016/j.jbtep.2018.01.006
154. Wight D, Wimbush E, Jepson R, Doi L. Six steps in quality intervention development (6SQuID). J Epidemiol Community Health. (2016) 70:520–5. doi: 10.1136/jech-2015-205952
155. Beck A. A new instrument for measuring insight: the Beck Cognitive Insight Scale. Schizophr Res. (2004) 68:319–29. doi: 10.1016/S0920-9964(03)00189-0
156. Gillanders D, Bolderston H, Bond F, Dempster M, Flaxman P, Campbell L, et al. The development and initial validation of the cognitive fusion questionnaire. Behav Ther. (2014) 45:83–101. doi: 10.1016/j.beth.2013.09.001
157. Levati S, Campbell P, Frost R, Dougall N, Wells M, Donaldson C, et al. Optimisation of complex health interventions prior to a randomised controlled trial: a scoping review of strategies used. Pilot Feasibility Stud. (2016) 2:17. doi: 10.1186/s40814-016-0058-y
158. Pearson, A, Tingey R. ACT for psychosis: A treatment protocol for group therapy. Jenison, MI: Contextual Behavioral Science (2011).
159. Stoddard J, Afari N. The Big Book of ACT Metaphors: a Practitioner’s Guide to Experiential Exercises and Metaphors in Acceptance and Commitment Therapy. Oakland, CA: New Harbinger Publications (2014). 228.
160. Johns L, Oliver J, Khondoker M, Byrne M, Jolley S, Wykes T, et al. The feasibility and acceptability of a brief Acceptance and Commitment Therapy (ACT) group intervention for people with psychosis: the ‘ACT for life’ study. J Behav Ther Exp Psychiatry. (2016) 50:257–63. doi: 10.1016/j.jbtep.2015.10.001
Keywords: intervention mapping, intervention development, mechanism-based, acute inpatients, psychosis, metacognition, group therapy
Citation: Gussmann E, Lucae S, Falkai P, Padberg F, Egli S and Kopf-Beck J (2023) Developing a mechanism-based therapy for acute psychiatric inpatients with psychotic symptoms: an Intervention Mapping approach. Front. Psychiatry 14:1160075. doi: 10.3389/fpsyt.2023.1160075
Received: 06 February 2023; Accepted: 05 May 2023;
Published: 01 June 2023.
Edited by:
Padmavati Ramachandran, Schizophrenia Research Foundation, IndiaReviewed by:
Warren Mansell, The University of Manchester, United KingdomRamesh Kumar, Schizophrenia Research Foundation, India
M. Suresh Kumar, Schizophrenia Research Foundation, India
Copyright © 2023 Gussmann, Lucae, Falkai, Padberg, Egli and Kopf-Beck. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eva Gussmann, ZXZhX2d1c3NtYW5uQHBzeWNoLm1wZy5kZQ==
 Eva Gussmann
Eva Gussmann Susanne Lucae1,2
Susanne Lucae1,2 Peter Falkai
Peter Falkai Frank Padberg
Frank Padberg Johannes Kopf-Beck
Johannes Kopf-Beck