
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 15 June 2023
Sec. Personality Disorders
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1152352
Background: Severe posttraumatic stress disorder (PTSD) may lead to non-suicidal self-injury (NSSI), and borderline personality disorder (BPD) tendencies may play a role in this process. Secondary vocational students experience more social, familial and other pressures and are more vulnerable to psychological problems. Thus, we explored the effect of BPD tendencies and subjective well-being (SWB) on NSSI in secondary vocational students with PTSD.
Methods: A total of 2,160 Chinese secondary vocational students in Wuhan participated in our cross-sectional investigation. The Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), criteria for PTSD, NSSI Questionnaire, Personality Diagnostic Questionnaire-4+, subjective well-being scale, and family adaptation, partnership, growth, affection, and resolve (APGAR) Index were used. We conducted a binary logistic regression model and linear regression analysis.
Results: Sex (odds ratio [OR] = 0.354, 95% confidence interval [CI] = 0.171–0.733), BPD tendencies (OR = 1.192, 95% CI = 1.066–1.333) and SWB (OR = 0.652, 95% CI = 0.516–0.824) were independent factors that predicted NSSI in secondary vocational students with PTSD. Spearman’s correlation analysis showed that BPD tendencies were positively correlated with NSSI frequency (r = 0.282, P < 0.01). SWB was negatively correlated with NSSI frequency (r = −0.301, P < 0.01). The linear regression showed that BPD tendencies (β = 0.137, P < 0.05 and β = −0.230, P < 0.001) were significantly correlated with NSSI frequency. Spearman’s correlation analysis showed that family functioning was positively correlated with SWB (r = 0.486, P < 0.01) and negatively correlated with BPD tendencies (r = −0.296, P < 0.01).
Conclusion: In adolescents, PTSD in response to stressful events could lead to NSSI, and BPD tendencies promote the intensity of NSSI, while SWB diminishes its intensity. Improvement in family functioning may actively guide the development of mental health and improve SWB; such steps may constitute interventions to prevent or treat NSSI.
Non-suicidal self-injury (NSSI), defined as intentional and self-inflicted damage to body tissues without suicidal intent, is a perplexing but common phenomenon. NSSI involves cutting, burning, biting, or scratching the skin (1). The main purpose of NSSI is to reduce negative emotions (2). The lifetime prevalence of NSSI in children and adolescents is 29.26% (3). Furthermore, in early adolescence, the prevalence of NSSI is higher in girls than in boys (4). NSSI is a significant factor threatening adolescent mental health (5). In the long run, NSSI may increase the risk of suicide (6). Thus, it is important to identify factors influencing the occurrence of NSSI to establish effective interventions for individuals with NSSI.
Compared with adulthood, adolescence is a sensitive and psychologically vulnerable period. Adolescents are more likely to be affected by traumatic events and persistent injuries experienced in the school, societal, and familial environments and are prone to high-risk behaviors (7). Some studies have shown that patients with posttraumatic stress disorder (PTSD) are at risk of developing NSSI (8). PTSD occurs after a sudden, threatening, or catastrophic life event that leads to long-term persistence of a psychiatric symptoms (9). Typical symptoms of PTSD include intrusive thoughts, avoidance of specific contexts, negative changes in cognition and mood, and increased alertness. PTSD is prone to comorbid with many mental problems, such as sleep disorders, depressive disorders, and anxiety disorders (10). Timely interventions for patients with PTSD can reduce distress, which can help to reduce the occurrence of NSSI (11).
Adolescents need interpersonal support and exposure to positive coping styles; however, adolescents with borderline personality disorder (BPD) typically express themselves in extreme ways, such as with self-harm, when faced with interpersonal problems (12). BPD is a personality disorder characterized by difficulties in interpersonal relationships, emotional instability, and impulsive behavior (13). Moreover, BPD is often present in adolescents with a history of NSSI (14). Approximately 60–75% of BPD patients have exhibited at least one self-injury behavior in their lifetime (15). Impaired emotion regulation and increased impulsivity in BPD patients are strongly associated with NSSI (2). Some studies have explored the relationship between personality subtypes and self-injury behavior in adolescents with self-injury (16). And recent studies have noted that family conflict, lack of involvement, lack of regard and other familial environment aspects promote the development of BPD in adolescents (17). Additionally, parental neglect or invalidation of children’s emotional expression may create an unsupportive familial environment that promotes the development of BPD symptoms (18).
In addition, recent studies have shown that high levels of subjective well-being (SWB), a protective factor against NSSI, can change adolescents’ strategies of coping with negative emotions, which may reduce the occurrence of NSSI (19). In particular, SWB is negatively correlated with negative emotions, and adolescents with higher SWB have fewer psychological problems (20). SWB involves positive emotion and is an overall assessment of one’s perceived quality of life. However, in the past 10 years, there has been a downward trend in SWB among adolescents (21). Therefore, improving SWB in adolescents is important for reducing the occurrence of NSSI. Family functioning, which includes cohesion, communication, family satisfaction and low family conflict, is positively correlated with the SWB of children and adolescents. Higher cohesion and good communication lead to increased happiness (22).
Accumulating evidence suggests that PTSD, SWB, and BPD tendencies are associated with NSSI. Despite these findings, to our knowledge, no studies have explored the relationships among these four variables. The relationships of NSSI with SWB and BPD tendencies in Chinese secondary vocational students has never been explored. Chinese secondary vocational students constitute a special group with a large population. Most enter secondary vocational schools because of poor academic performance (23). Thus, they are regarded by society and even their parents as “undereducated” or “failed” students; therefore, they exhibit self-depreciation and low self-esteem and are more likely to have psychological problems (24). The purpose of this study is threefold: (1) to determine the association between PTSD and NSSI in secondary vocational students and (2) to determine the associations of SWB and BPD tendencies with NSSI. We hypothesized that SWB is a protective factor against NSSI and that BPD tendencies are risk factors for NSSI. Finally, we also aimed (3) to explore the relationships of family functioning with BPD tendencies and SWB to determine potential interventions for NSSI.
The research subjects were students from grade one to grade three in a secondary vocational school in Wuhan. Participants ranged in age from 15 to 18 years. To ensure the rigor and accuracy of this study, we consulted with experts in the relevant disciplines before developing and finalizing the questionnaire. A pilot survey was conducted to further refine the questionnaire. In the formal investigation, students were asked to independently complete the questionnaire onsite; the questionnaire took approximately 30 min to complete.
Investigation period: April–May 2022.
After obtaining informed consent, a total of 2,500 questionnaires were distributed to all students at the school (i.e., whole-group sampling); of these, 2,160 questionnaires were returned, for an effective rate of 86.4%. Among the participants, 992 were grade one students, 902 were grade two students and 266 were grade three students, accounting for 45.9, 41.8, and 9.5% of the sample, respectively. This study was approved by the Ethics Committee of the Affiliated Wuhan Mental Health Center, Tongji Medical College of Huazhong University of Science and Technology.
Vocational school students completed a questionnaire designed by the researchers. The questionnaire collected sociodemographic information, such as sex, grade, and family socioeconomic status.
The PC-PTSD was modified according to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), and included five topics corresponding to the five factors of re-experiencing, avoidance, hyperarousal, numbness, and negative changes in mood and cognition. Each item is scored as yes (1) or no (0); the score on all items is summed to determine the total score. A score of 3 is the threshold for the diagnosis of clinical PTSD (25). Cronbach’s α of the scale was 0.83, indicating high reliability (26).
Non-suicidal self-injury was assessed in this study using one question. The question was “In the past 12 months, have you hurt yourself intentionally without attempting to commit suicide? For example, did you hurt yourself for other reasons, such as to release stress, feel better, elicit sympathy, or make something else happen?” The score of each question is 1 point for “yes” and 0 points for “no.” Participants were also asked to answer the following questions: “In the past 12 months, how many times have you hurt yourself?”, “Please indicate the main ways that you hurt yourself: (A) cutting, (B) hitting, (C) scalding/burning, or (D) other (please fill in)” and “How and where did you hurt yourself?” We provided specific questionnaires in Supplementary material.
In 2000, Yang Yunping and other experts to developed the Chinese version of the PDQ-4+, which is widely used in domestic research and clinical practice. This questionnaire includes 107 items to assess the pathological severity of 12 types of personality disorders (27). We selected the 11 items relevant to BPD. There are 2 sets of items, 100(6) and 101(19), and the items outside the brackets are scored. The 11th item contains 6 questions and is scored as 1 if ≥2 questions are answered with “yes” or 0 if <2 questions are answered with “yes.” Scores range from 0 to 9, with a threshold score of 5 (28). The scale has good reliability and validity in the general Chinese population, and the Cronbach’s α coefficient is 0.73–0.77 (29).
The scale was developed by Andrews FM and Whitney SB in 1976 (30). Seven facial expressions (very happy, happy, relatively happy, average, relatively unhappy, miserable, and very miserable) are used to measure the respondent’s happiness and correspond to the letters A–G. Participants are asked to select the facial expression consistent with their overall perceived quality of life.
The family APGAR index (APGAR) was developed by Smilkstein (31). The questionnaire includes five components: adaptation, partnership, growth, affection, and resolve. There are three possible answers for each item (2 = almost always, 1 = sometimes, or 0 = hardly ever) (32). Higher scores indicate higher satisfaction with family function. Total scores of 0–3 suggest severe family dysfunction, 4–6 suggest moderate family dysfunction, and 7–10 suggest good family functioning. The Chinese version used in this study showed great reliability and validity. The Cronbach’s α values reported by studies range from 0.80 to 0.85 (33).
The data were analyzed using SPSS 26.0. First, we screened participants for PTSD and NSSI. Descriptive analyses of NSSI in patients with PTSD were performed, and count data are described with proportions or rates. The χ2 test or precise probability method were used for group comparisons. Measurement data conforming to a normal distribution are expressed as the mean ± standard deviation (x ± s), and an independent-sample t-test was used to compare the two groups. Measures that did not conform to a normal distribution are expressed as the mean and interquartile range (IQR), i.e., M (P25, P75), and the Wilcoxon rank sum test was used for comparisons between groups. The Wilcoxon rank sum test was also used to compare the demographic characteristics of the subjects. Then, Spearman correlation analyses were performed to explore the relationships of SWB and BPD tendencies with NSSI and the frequency of NSSI. Spearman correlation analysis was also used to explore the relationships of family function and BPD tendencies with SWB. P < 0.05 was considered statistically significant.
Among the 2,160 students in this study, 566 had experienced major life events or traumatic events in the past year. Among them, 241 people had PTSD, and the prevalence rate was 11% (241/2,160). The prevalence rate of PTSD in males (10.8%, 100/929) was lower than that in females (11.5%, 141/1,230). There were 122 grade one students (50.6%), 94 grade two students (39.0%), and 25 grade three students (10.4%). There were no significant differences in sex or grade between students with and without PTSD (P > 0.05). There was a statistically significant difference in the occurrence of NSSI among secondary vocational students (χ2 = 15.953, P < 0.05), as shown in Table 1.

Table 1. Posttraumatic stress disorder (PTSD) and sociodemographic factors of secondary vocational students in a secondary vocational school in Wuhan.
There were 55 PTSD students with NSSI, and the prevalence rate of NSSI was 22.8% (55/241). Among students with PTSD, the prevalence rate of NSSI in boys (5.8%, 14/241) was lower than that in girls (17.0%, 41/241). Among PTSD students with NSSI, the most frequent family function rating was severe (65.45%). Differences in sex and family functioning between PTSD students with and without NSSI were statistically significant (P < 0.05). The prevalence rate of NSSI among PTSD students did not significantly vary according to grade, family socioeconomic status, or the presence of one or multiple traumatic events (all P > 0.05), as shown in Table 2. There were 154 non-PTSD students with NSSI, with a total prevalence rate of 8.0% (154/1919). There were significant differences in sex, age, family socioeconomic status, and the number of traumatic events between NSSI students with and without PTSD (P < 0.05). NSSI was detected in a total of 209 (9.68%) students. The most common method of self-injury was cutting (55.5%), and the most common self-injury site was the limbs (78.0%). Among the 55 PTSD students with NSSI, the most common mode of NSSI was cutting (63.6%), and the most common self-injury site was the limbs (81.8%).
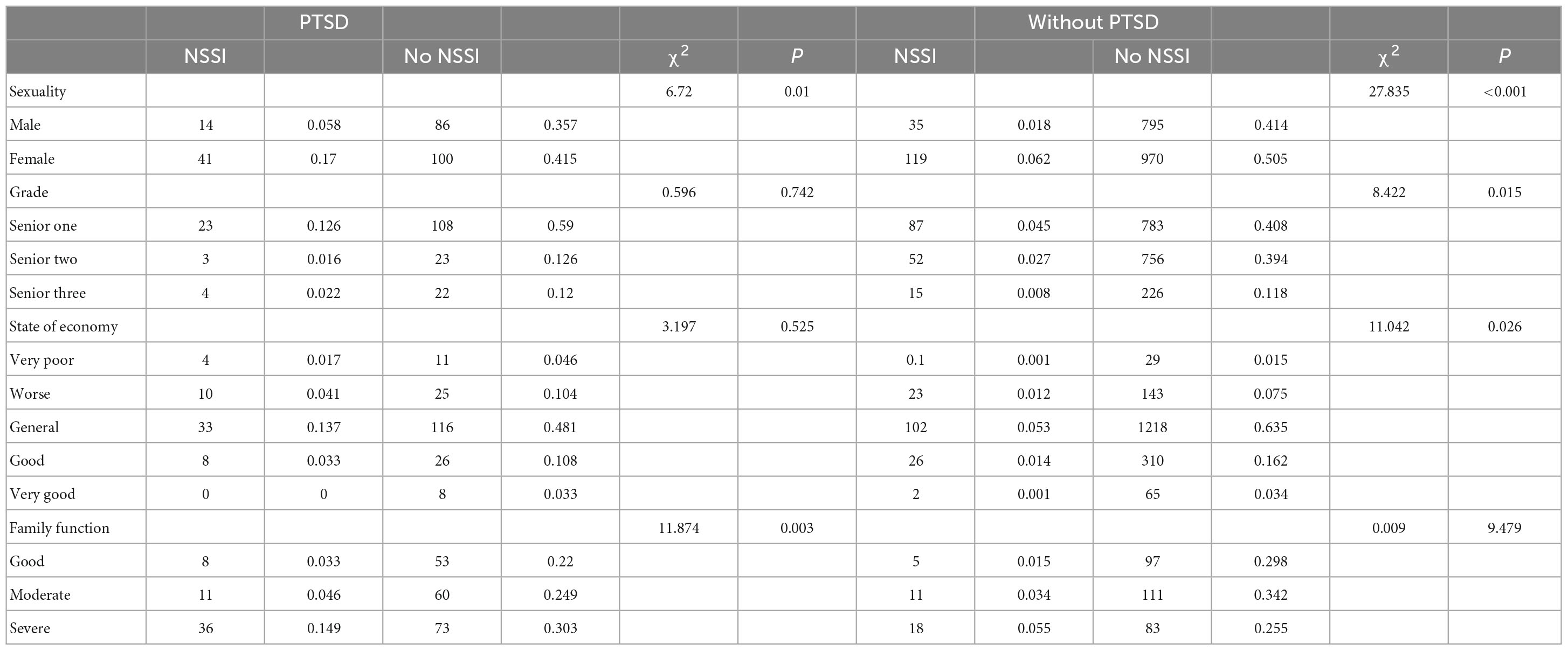
Table 2. Non-suicidal self-injury (NSSI) and sociodemographic factors of secondary vocational students with and without PTSD in a secondary vocational school in Wuhan.
Our data analysis shows that SWB is mainly concentrated in “average, relatively unhappy,” regardless of whether NSSI behavior occurs. Among NSSI students with PTSD, 23 (41.8%) of them had a average level of SWB. And 11 (20.0%) of them had a relatively unhappy level of SWB. Among non-NSSI students with PTSD, 57 (30.6%) of them had a average level of SWB. And 47 (25.3%) of them had a relatively unhappy level of SWB. Among the NSSI students, 44 (80%) of them had BPD tendencies. And among the non-NSSI students, 99 (53.2%) of them had BPD tendencies. A binary logistic regression was run with NSSI as the dependent variable, sex as a covariate, and BPD tendencies and SWB as independent variables. Variables identified as significant in the univariate regression were incorporated into the multivariate regression. BPD tendencies (odds ratio [OR] = 1.192, P < 0.01) were an independent risk factor for NSSI, and SWB (OR = 0.652, P < 0.01) was an independent protective factor against NSSI, as shown in Table 3.
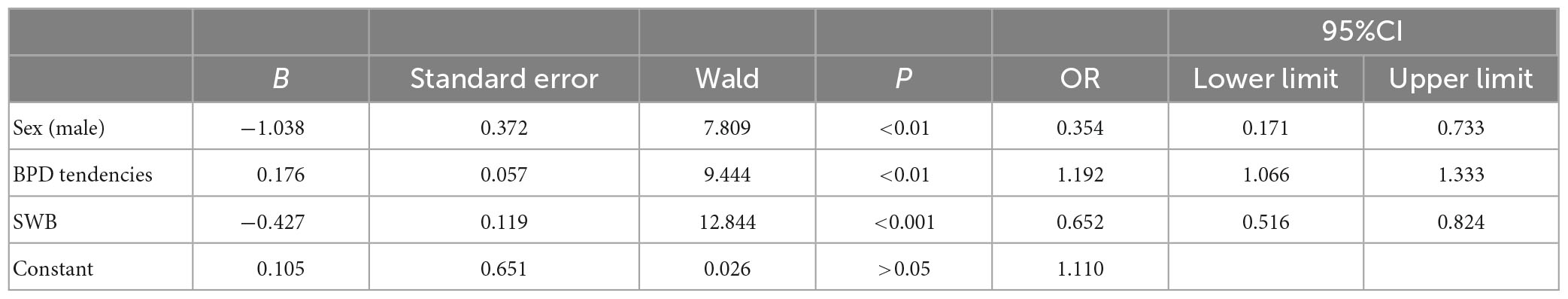
Table 3. Results of binary regression analysis of the relationships of NSSI with BPD tendencies or SWB.
Non-suicidal self-injury frequency did not exhibit a normal distribution and is described by the median (IQR). Among the 55 (22.8%) secondary vocational students with PTSD and NSSI, the median NSSI frequency in the past 12 months was 2 (1, 4). Spearman correlation analysis was used to analyze the relationships between PTSD (M = 4.062, SD = 0.817) and BPD tendencies (M = 4.160, SD = 3.38) and between SWB (M = 4.523, SD = 1.565) and the frequency of NSSI (M = 0.544, SD = 1.143). Sex was correlated with the frequency of NSSI (r = 0.180, P < 0.01). BPD tendencies were positively correlated with the frequency of NSSI (r = 0.282, P < 0.01), and SWB was negatively correlated with the frequency of NSSI (r = −0.301, P < 0.01). See Table 4.
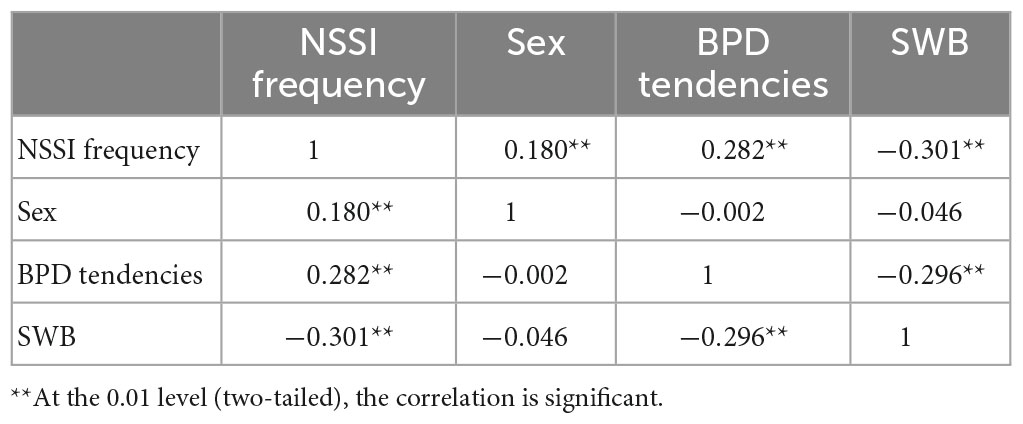
Table 4. Results of Spearman correlation analyses of the relationships of NSSI frequency with SWB or BPD tendencies among students with PTSD (r) (n = 241).
A stepwise regression was used to select the best model according to the fit indexes and number of variables; NSSI frequency was included as the dependent variable, BPD tendencies and SWB were included as independent variables, and sex was included as the control variable. The final model exhibited good fit (F = 10.740, P < 0.01, adjusted R2 = 0.109, dependent variable standard error of prediction = 1.07961). BPD tendencies (β = 0.137, P < 0.05) and SWB (β = −0.230, P < 0.001) were independent influencing factors of NSSI frequency, as shown in Table 5.
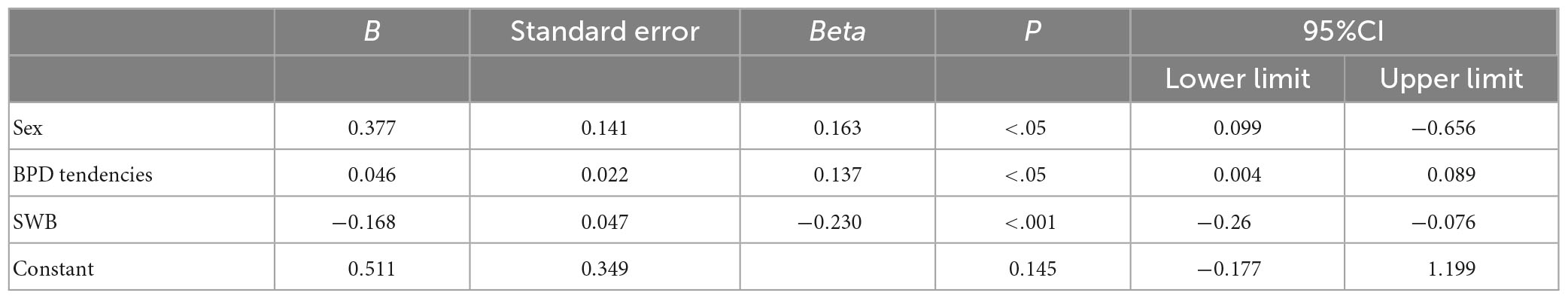
Table 5. Results of linear regression analysis of the relationships of NSSI with BPD tendencies or SWB.
Among secondary vocational students with PTSD, 109 (45.2%) reported severe family dysfunction, 71 (29.5%) reported moderate family dysfunction, and 61 (25.3%) reported good family functioning. Among secondary vocational students without PTSD, 101 (31.1%), 122 (37.5%), and 102 (31.4%) students reported severe family dysfunction, moderate family dysfunction, and good family functioning, respectively. Spearman correlation analyses were used to analyze the associations of family functioning (M = 4.403, SD = 9.337) with BPD tendencies (M = 4.160, SD = 3.38) and SWB (M = 4.523, SD = 1.565) in secondary vocational students with PTSD. Family functioning was positively correlated with SWB (r = 0.486, P < 0.01) and negatively correlated with BPD tendencies (r = −0.314, P < 0.01). Sex was not significantly correlated with SWB or BPD tendencies (r = −0.046 or r = −0.119, respectively; P > 0.05) (Table 6).
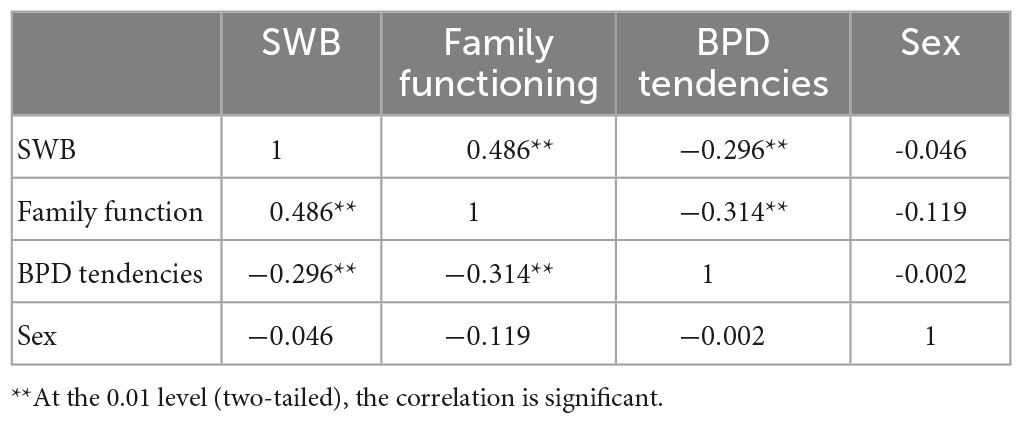
Table 6. Spearman correlation analysis among SWB, family functioning and BPD tendencies of students with PTSD (r) (n = 241).
According to Chinese educational policies, vocational education has long been stigmatized in the field of secondary education. Most people believe that vocational education is poor quality and that secondary vocational students exhibit poor educational performance and thus must enter vocational schools. Secondary vocational students experience unfair treatment and reduced social and educational resources and may be denigrated by their families and society; thus, these individuals are at higher risk of psychological problems such as depression and anxiety (24). Secondary vocational school students have low self-esteem and negative self-perceptions (34). Unfortunately, parents are often the origin of these stereotypes, and family support and family education level are very important influences. Greater attention to the psychological state of higher vocational students is needed in China, but there are few studies on this population.
A meta-analysis of the incidence of NSSI in adolescents worldwide from 1989 to 2018 indicated a lifetime prevalence of 22.1% and a 12-month prevalence of 19.8% (35). An analysis by Sarah et al. (36) reported that the incidence rates of NSSI were 17.2% in adolescents, 13.4% in young adults and 5.5% in adults. In this survey, the prevalence rate of NSSI among students in a secondary vocational school in Wuhan in the past year was 14.0%, which differs from the above results. This difference may be due to the different NSSI measurement methods used. Use of a single yes or no question may not provide results as accurate as the use of a checklist, as individuals may not immediately recall the event for yes or no answers (37). The prevalence rate of NSSI among students with PTSD in our study was 22.9%, which was higher than that among students without PTSD. This finding is similar to that of previous studies in which PTSD was a risk factor for NSSI (38). People with PTSD have persistent negative perceptions of themselves, others, and the world and a persistent negative emotional state, which promotes the occurrence of NSSI.
In this study, the prevalence of NSSI was lower in males than in females regardless of PTSD status. This result is consistent with the findings of Bresin et al. (39) that females were significantly more likely than males to develop NSSI, possibly because of differences in sex hormones. Estrogen levels around the time of menarche increase rapidly and fluctuate dramatically in the body, and physiological systems may not be able to adapt to these changes (40). It has also been suggested that the sex difference in NSSI stem from greater susceptibility of female adolescents to negative emotions. Emotion regulation strategies differ between males and females. Females tend to use avoidance strategies (41). Previous studies have shown that adolescent NSSI peaks at the age of 15.9–17.4 years and that the incidence of NSSI decreases with age (42). This may be due to environmental changes (from middle school to secondary vocational school), maladjustment, or academic pressure. Among the students in the present study, the prevalence rate of NSSI among PTSD students was not related to grade, whereas the prevalence rate of NSSI among students without PTSD was related to grade and was highest among senior students. The effect of PTSD on NSSI may mask the effect of grade on NSSI. However, because our survey was conducted at only one school, the results may have limited generalizability. Studies have shown a higher incidence of NSSI among adolescents with low family socioeconomic status, but some studies have reported a non-significant association of these variables (43). In the present study, the incidence of NSSI among PTSD students was not related to family socioeconomic status. However, the incidence of NSSI among students without PTSD was related to family socioeconomic status, with the highest prevalence rate of NSSI among economically average students. The difference in results from those of previous studies may be due to the socioeconomic conditions in different regions, with the largest proportion of people in China having average socioeconomic status, which led to bias in the results. We demonstrated that family functioning differs between adolescents with and without NSSI. A study showed that poor family communication and lack of support may promote the development of NSSI, which in turn affects the relationship between children and parents and damages family function, forming a vicious circle (44, 45). The specific role of the familial environment in the occurrence of NSSI needs further study.
Patients with BPD are characterized by emotional instability, unstable interpersonal relationships, impulsiveness, and irritability. Patients with BPD have cognitive impairments and tend to focus on negative information (46). Adolescents with BPD have difficulties identifying and expressing emotions when dealing with interpersonal problems and often resort to extreme forms of self-harm to regulate negative emotions (12). Indeed, NSSI is one of the core symptoms of BPD, and NSSI and BPD may represent a developmental continuum (47). One study reported that compared with non-BPD individuals with NSSI, BPD individuals with NSSI are more prone to severe depression and suicidal behavior (48). Some studies have noted that people with BPD have a higher risk of NSSI than the general population (49, 50), and there is an interaction between BPD and NSSI (51). Our analysis showed that BPD tendencies are significantly positively correlated with NSSI in PTSD students, which further confirms that BPD tendencies can increase the risk of NSSI. Possible mechanisms by which BPD tendencies influence NSSI risk should be explored in future studies. Some studies have demonstrated that the probability of PTSD among patients with BPD is 30–50% and that BPD patients with PTSD are more likely to develop NSSI (52). Another study demonstrated that BPD patients use extreme methods, such as NSSI and substance use, to relieve PTSD symptoms (53). BPD tendencies and PTSD are associated with more pronounced mood dysregulation and higher risk of NSSI (54). We found that BPD tendencies were significantly associated with NSSI occurrence and positively associated with NSSI frequency in students with PTSD. BPD tendencies may lead to an increase in NSSI frequency in individuals with PTSD. Thus, symptoms of PTSD and BPD need to be addressed to reduce the risk of NSSI.
The results of this study are consistent with those of previous studies showing that SWB is a protective factor against NSSI; thus, poor SWB increases the risk of NSSI. Improving SWB may reduce the occurrence of NSSI in adolescents. Additionally, we found that family functioning significantly influenced SWB among secondary vocational students, and better family functioning led to higher SWB. Secondary vocational student with PTSD reported the largest proportion of severe family dysfunction and the smallest proportion of good family functioning. The familial environment is important for the development of emotional relationships, and a stable parent-child relationship leads to solid emotional support. Family relationships have an important influence on adolescents’ SWB, and good communication and warm relationships with family members lead to a higher level of life satisfaction (55). SWB may reflect adolescents’ social adjustment and close relationships between parents and children (56). Effective communication among family members may improve family functioning and, consequently, adolescents’ life satisfaction.
Adolescence is the period with the highest risk of PTSD and NSSI. Prevention measures focusing on adolescents after middle school graduation are important, especially those involving proper parental guidance. Based on the findings of this study, we need to pay attention to PTSD symptoms, BPD tendencies and SWB to reduce the occurrence of NSSI among adolescents. Parents’ cognitive model and emotion regulation impact children’s PTSD; additionally, parental guidance can reduce the severity of PTSD in adolescents (57). Middle school is a critical period for personality development, and good parenting at this time strengthens the parent-child bond and makes it easier for children to cultivate positive and stable mental health (58). In the field of parenting styles, parental behavior may reduce the vulnerability of children to psychological problems. Our research confirms that better family functioning reduces the risk of BPD tendencies. Based on the findings of this study, addressing PTSD symptoms, BPD tendencies, and SWB is necessary to reduce the occurrence of NSSI.
There are also some limitations in this study. First, this study is cross-sectional in design and cannot determine causal relationships among variables. Future longitudinal studies may explore whether there are differences in personality traits and SWB among adolescents with PTSD. Second, all data were self-report data (i.e., obtained by questionnaires rather than clinical interviews) and are susceptible to answer bias. Third, the focus on secondary vocational students limit the generalization of the results to other PTSD patients. Finally, when determining the factors related to NSSI among students with PTSD, we did not adjust for variables other than sex.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
WD, SY, and YX designed the study and developed the idea in consultation with LL, YZ, and MC. WD, SY, and ZL responsible for the review of the literature. YX, LL, and YZ extracted the data. WD performed the statistical analyses. WD, SY, and YX drafted the manuscript. LL, YZ, and MC revised the manuscript. All authors read and agreed to the published version of the manuscript.
We are grateful to all of the participants for their contribution.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1152352/full#supplementary-material
1. Westlund Schreiner M, Klimes-Dougan B, Mueller BA, Eberly LE, Reigstad KM, Carstedt PA, et al. Multi-modal neuroimaging of adolescents with non-suicidal self-injury: amygdala functional connectivity. J Affect Disord. (2017) 221:47–55. doi: 10.1016/j.jad.2017.06.004
2. Wilkinson P. Non-suicidal self-injury. Eur Child Adolesc Psychiatry. (2013) 22(Suppl. 1):S75–9. doi: 10.1007/s00787-012-0365-7
3. Liang K, Zhao L, Lei Y, Zou K, Ji S, Wang R, et al. Nonsuicidal self-injury behaviour in a city of China and its association with family environment, media use and psychopathology. Compr Psychiatry. (2022) 115:152311. doi: 10.1016/j.comppsych.2022.152311
4. Hawton K, Saunders KE, O’Connor RC. Self-harm and suicide in adolescents. Lancet. (2012) 379:2373–82. doi: 10.1016/s0140-6736(12)60322-5
5. Xiao Q, Song X, Huang L, Hou D, Huang X. Global prevalence and characteristics of non-suicidal self-injury between 2010 and 2021 among a non-clinical sample of adolescents: a meta-analysis. Front Psychiatry. (2022) 13:912441. doi: 10.3389/fpsyt.2022.912441
6. Liu H, Wang W, Yang J, Guo F, Yin Z. The effects of alexithymia, experiential avoidance, and childhood sexual abuse on non-suicidal self-injury and suicidal ideation among Chinese college students with a history of childhood sexual abuse. J Affect Disord. (2021) 282:272–9. doi: 10.1016/j.jad.2020.12.181
7. Nooner KB, Linares LO, Batinjane J, Kramer RA, Silva R, Cloitre M. Factors related to posttraumatic stress disorder in adolescence. Trauma Violence Abuse. (2012) 13:153–66. doi: 10.1177/1524838012447698
8. Brown LA, Contractor A, Benhamou K. Posttraumatic stress disorder clusters and suicidal ideation. Psychiatry Res. (2018) 270:238–45. doi: 10.1016/j.psychres.2018.09.030
9. Gratz KL, Tull MT. Exploring the relationship between posttraumatic stress disorder and deliberate self-harm: the moderating roles of borderline and avoidant personality disorders. Psychiatry Res. (2012) 199:19–23. doi: 10.1016/j.psychres.2012.03.025
10. Maercker A, Cloitre M, Bachem R, Schlumpf YR, Khoury B, Hitchcock C, et al. Complex post-traumatic stress disorder. Lancet. (2022) 400:60–72. doi: 10.1016/s0140-6736(22)00821-2
11. Baralla F, Ventura M, Negay N, Di Napoli A, Petrelli A, Mirisola C, et al. Clinical correlates of deliberate self-harm among migrant trauma-affected subgroups. Front Psychiatry. (2021) 12:529361. doi: 10.3389/fpsyt.2021.529361
12. Guénolé F, Spiers S, Gicquel L, Delvenne V, Robin M, Corcos M, et al. Interpersonal relatedness and non-suicidal self-injurious behaviors in female adolescents with borderline personality disorder. Front Psychiatry. (2021) 12:731629. doi: 10.3389/fpsyt.2021.731629
13. Ditrich I, Philipsen A, Matthies S. Borderline personality disorder (Bpd) and attention deficit hyperactivity disorder (Adhd) revisited - a review-update on common grounds and subtle distinctions. Borderline Personal Disord Emot Dysregul. (2021) 8:22. doi: 10.1186/s40479-021-00162-w
14. Koposov R, Stickley A, Ruchkin V. Non-Suicidal self-injury among incarcerated adolescents: prevalence, personality, and psychiatric comorbidity. Front Psychiatry. (2021) 12:652004. doi: 10.3389/fpsyt.2021.652004
15. Rogers ML, Joiner TE Jr. Borderline personality disorder diagnostic criteria as risk factors for suicidal behavior through the lens of the interpersonal theory of suicide. Arch Suicide Res. (2016) 20:591–604. doi: 10.1080/13811118.2016.1158681
16. Floyd PN, Charles NE, Sigurdson L, Barry CT. Optimal Pai-a cutoffs to determine risk for non-suicidal self-injury (Nssi) and suicide-related behavior (Srb) among at-risk adolescents. Arch Suicide Res. (2022) 26:208–25. doi: 10.1080/13811118.2020.1784334
17. Fatimah H, Wiernik BM, Gorey C, McGue M, Iacono WG, Bornovalova MA. Familial factors and the risk of borderline personality pathology: genetic and environmental transmission. Psychol Med. (2020) 50:1327–37. doi: 10.1017/s0033291719001260
18. Lee SSM, Keng SL, Yeo GC, Hong RY. Parental invalidation and its associations with borderline personality disorder symptoms: a multivariate meta-analysis. Personal Disord. (2022) 13:572–82. doi: 10.1037/per0000523
19. Muehlenkamp JJ, Xhunga N, Brausch AM. Self-injury age of onset: a risk factor for Nssi severity and suicidal behavior. Arch Suicide Res. (2019) 23:551–63. doi: 10.1080/13811118.2018.1486252
20. Yuan W, Xu T, Liu M, Hu B. Vocational identity status in Chinese emerging adults with and without hearing impairment: latent profiles and relationships with self-esteem and subjective well-being. Int J Environ Res Public Health. (2022) 19:14473. doi: 10.3390/ijerph192114473
21. Katsantonis I, McLellan R, Marquez J. Development of subjective well-being and its relationship with self-esteem in early adolescence. Br J Dev Psychol. (2022) 41:157–71. doi: 10.1111/bjdp.12436
22. Izzo F, Baiocco R, Pistella J. Children’s and adolescents’ happiness and family functioning: a systematic literature review. Int J Environ Res Public Health. (2022) 19:16593. doi: 10.3390/ijerph192416593
23. Liu J, Teng Z, Chen Z, Wei Z, Zou T, Qin Y, et al. Exploring the associations between behavioral health risk factors, abnormal eating attitudes and socio-demographic factors among Chinese youth: survey of 7,984 vocational high school students in Hunan in 2020. Front Psychiatry. (2022) 13:1000821. doi: 10.3389/fpsyt.2022.1000821
24. Wang X, Leng J, Cong X, Fan Z. Development of junior high school students to secondary vocational students stigma scale. Psychol Res Behav Manag. (2022) 15:2957–70. doi: 10.2147/prbm.S381069
25. Li J, Zhang W, Chen W, Yuan H, Zhang S, Tian M, et al. Applications of the Chinese version of the primary care Ptsd screen for dsm-5 (Pc-Ptsd-5) for children. J Affect Disord. (2019) 254:109–14. doi: 10.1016/j.jad.2019.05.021
26. Cheng P, Jasinski N, Zheng W, Yadava A, Wang L, Li L, et al. Psychometric properties of the primary care Ptsd screen for Dsm-5: findings from family members of Chinese healthcare workers during the outbreak of COVID-19. Front Psychiatry. (2021) 12:695678. doi: 10.3389/fpsyt.2021.695678
27. Calvo N, Gutiérrez F, Casas M. Diagnostic agreement between the personality diagnostic questionnaire-4+ (Pdq-4+) and its clinical significance scale. Psicothema. (2013) 25:427–32. doi: 10.7334/psicothema2013.59
28. Yang J, Bagby RM, Costa PT Jr., Ryder AG, Herbst JH. Assessing the Dsm-Iv structure of personality disorder with a sample of Chinese psychiatric patients. J Pers Disord. (2002) 16:317–31. doi: 10.1521/pedi.16.4.317.24127
29. Yang H, Lei X, Zhong M, Zhou Q, Ling Y, Jungkunz M, et al. Psychometric properties of the Chinese version of the brief borderline symptom list in undergraduate students and clinical patients. Front Psychol. (2018) 9:605. doi: 10.3389/fpsyg.2018.00605
30. Frank M, Andrews SBW. Social indicators of well-being: American’s perception of life quality. New York, NY: Plenum (1976). doi: 10.1007/978-1-4684-2253-5
31. Shao R, He P, Ling B, Tan L, Xu L, Hou Y, et al. Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and coping styles among Chinese medical students. BMC Psychol. (2020) 8:38. doi: 10.1186/s40359-020-00402-8
32. Ribé JM, Salamero M, Pérez-Testor C, Mercadal J, Aguilera C, Cleris M. Quality of life in family caregivers of schizophrenia patients in Spain: caregiver characteristics, caregiving burden, family functioning, and social and professional support. Int J Psychiatry Clin Pract. (2018) 22:25–33. doi: 10.1080/13651501.2017.1360500
33. Wang B, He P, Dong B. Association between family functioning and cognitive impairment among chinese nonagenarians/centenarians. Geriatr Gerontol Int. (2015) 15:1135–42. doi: 10.1111/ggi.12410
34. Zheng Y, Fang Y, Jin Y, Zuo X, Lian Q, Lou C, et al. Parenting practice profiling and its associated factors among secondary vocational school students in China. Int J Environ Res Public Health. (2022) 19:7497. doi: 10.3390/ijerph19127497
35. Lim KS, Wong CH, McIntyre RS, Wang J, Zhang Z, Tran BX, et al. Global lifetime and 12-month prevalence of suicidal behavior, deliberate self-harm and non-suicidal self-injury in children and adolescents between 1989 and 2018: a meta-analysis. Int J Environ Res Public Health. (2019) 16:4581. doi: 10.3390/ijerph16224581
36. Sarah V, Swannell P, Graham E, Martin MD, Franzcp DPM, Andrew Page P, et al. Prevalence of nonsuicidal self-injury in nonclinical samples: systematic review, meta-analysis and meta-regression. Suicide Life-Threat Behav. (2014) 44:273–303.
37. Arnold S, Wiese A, Zaid S, Correll CU, Jaite C. Lifetime prevalence and clinical correlates of nonsuicidal self-injury in youth inpatients with eating disorders: a retrospective chart review. Child Adolesc Psychiatry Ment Health. (2022) 16:17. doi: 10.1186/s13034-022-00446-1
38. Ennis CR, Tock JL, Daurio AM, Raines AM, Taylor J. An initial investigation of the association between Dsm-5 posttraumatic stress disorder symptoms and nonsuicidal self-injury functions. Psychol Trauma. (2022) 14:1201–7. doi: 10.1037/tra0000549
39. Bresin K, Schoenleber M. Gender differences in the prevalence of nonsuicidal self-injury: a meta-analysis. Clin Psychol Rev. (2015) 38:55–64. doi: 10.1016/j.cpr.2015.02.009
40. Liu X, Liu ZZ, Fan F, Jia CX. Menarche and menstrual problems are associated with non-suicidal self-injury in adolescent girls. Arch Womens Ment Health. (2018) 21:649–56. doi: 10.1007/s00737-018-0861-y
41. Tang J, Ma Y, Lewis SP, Chen R, Clifford A, Ammerman BA, et al. Association of internet addiction with nonsuicidal self-injury among adolescents in China. JAMA Netw Open. (2020) 3:e206863. doi: 10.1001/jamanetworkopen.2020.6863
42. Moran P, Coffey C, Romaniuk H, Olsson C, Borschmann R, Carlin JB, et al. The natural history of self-harm from adolescence to young adulthood: a population-based cohort study. Lancet. (2012) 379:236–43. doi: 10.1016/s0140-6736(11)61141-0
43. Jeong JY, Kim DH. Gender differences in the prevalence of and factors related to non-suicidal self-injury among middle and high school students in South Korea. Int J Environ Res Public Health. (2021) 18:5965. doi: 10.3390/ijerph18115965
44. Wang Y, Luo B, Hong B, Yang M, Zhao L, Jia P. The relationship between family functioning and non-suicidal self-injury in adolescents: a structural equation modeling analysis. J Affect Disord. (2022) 309:193–200. doi: 10.1016/j.jad.2022.04.124
45. Miscioscia M, Angelico C, Raffagnato A, Gatta M. Psychopathological and interactive-relational characteristics in non-suicidal self-injury adolescent outpatients. J Clin Med. (2022) 11:1218. doi: 10.3390/jcm11051218
46. Kelly Grealy M, Godfrey E, Brady F, Whyte O’Sullivan E, Carroll GA, Burke T. Borderline personality disorder traits and mentalising ability: the self-other social cognition paradox. Front Psychiatry. (2022) 13:1023348. doi: 10.3389/fpsyt.2022.1023348
47. Brown RC, Plener PL, Groen G, Neff D, Bonenberger M, Abler B. Differential neural processing of social exclusion and inclusion in adolescents with non-suicidal self-injury and young adults with borderline personality disorder. Front Psychiatry. (2017) 8:267. doi: 10.3389/fpsyt.2017.00267
48. Tschan T, Peter-Ruf C, Schmid M, In-Albon T. Temperament and character traits in female adolescents with nonsuicidal self-injury disorder with and without comorbid borderline personality disorder. Child Adolesc Psychiatry Ment Health. (2017) 11:4. doi: 10.1186/s13034-016-0142-3
49. Vanek J, Prasko J, Ociskova M, Hodny F, Holubova M, Minarikova K, et al. Insomnia in patients with borderline personality disorder. Nat Sci Sleep. (2021) 13:239–50. doi: 10.2147/nss.S295030
50. Beeney JE, Forbes EE, Hipwell AE, Nance M, Mattia A, Lawless JM, et al. Determining the key childhood and adolescent risk factors for future bpd symptoms using regularized regression: comparison to depression and conduct disorder. J Child Psychol Psychiatry. (2021) 62:223–31. doi: 10.1111/jcpp.13269
51. Reichl C, Kaess M. Self-harm in the context of borderline personality disorder. Curr Opin Psychol. (2021) 37:139–44. doi: 10.1016/j.copsyc.2020.12.007
52. Sagioglou TGC. Predictors of nonsuicidal self-injury: the independent contribution of benign masochism and antisocial personality. Personal Individ Differ. (2021) 168:110380. doi: 10.1016/j.paid.2020.110380
53. Harned MS, Gallop RJ, Valenstein-Mah HR. What changes when? the course of improvement during a stage-based treatment for suicidal and self-injuring women with borderline personality disorder and Ptsd. Psychother Res. (2018) 28:761–75. doi: 10.1080/10503307.2016.1252865
54. Harned MS, Rizvi SL, Linehan MM. Impact of co-occurring posttraumatic stress disorder on suicidal women with borderline personality disorder. Am J Psychiatry. (2010) 167:1210–7. doi: 10.1176/appi.ajp.2010.09081213
55. Lampropoulou A. Personality, school, and family: what is their role in adolescents’ subjective well-being. J Adolesc. (2018) 67:12–21. doi: 10.1016/j.adolescence.2018.05.013
56. Zhou J, Hu F, Wu J, Zou ZY, Wang YX, Peng HC, et al. Subjective well-being and family functioning among adolescents left behind by migrating parents in Jiangxi province. China. Biomed Environ Sci. (2018) 31:382–8. doi: 10.3967/bes2018.049
57. Cisler JM, Herringa RJ. Posttraumatic stress disorder and the developing adolescent brain. Biol Psychiatry. (2021) 89:144–51. doi: 10.1016/j.biopsych.2020.06.001
Keywords: posttraumatic stress disorder, non-suicidal self-injury, personality characteristics, subjective happiness, adolescent, family function
Citation: Deng W, Yan S, Xu Y, Lu Z, Liu L, Zhou Y and Chen M (2023) Effects of BPD tendencies and subjective well-being on NSSI in adolescents with PTSD. Front. Psychiatry 14:1152352. doi: 10.3389/fpsyt.2023.1152352
Received: 27 January 2023; Accepted: 04 May 2023;
Published: 15 June 2023.
Edited by:
Jie Zhong, Peking University, ChinaReviewed by:
Jianing You, South China Normal University, ChinaCopyright © 2023 Deng, Yan, Xu, Lu, Liu, Zhou and Chen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lianzhong Liu, MTg0OTIzMDQ3QHFxLmNvbQ==; Yang Zhou, MzA3ODU4NzMyQHFxLmNvbQ==; Mo Chen, Y2hlbm1vMDY2QGh1c3QuZWR1LmNu
†These authors share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.