- 1School of Nursing, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
- 2School of Medical Laboratory, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
- 3Department of Midwifery, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
- 4Department of Emergency and Critical Care Medicine, School of Medicine, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
- 5Department of Obstetrics and Gynecology, School of Medicine, College of Medicine and Health Sciences, Hawassa University, Hawassa, Ethiopia
Background: COVID-19 has been causing significant mental health problems and other health-related issues. Despite the fact that COVID-19 has a significant impact on chronic disease patients, there is scant research on insomnia, common mental health disorders (CMD), and their associated factors among chronic disease patients.
Objective: The purpose of this study was to assess the prevalence of insomnia and common mental disorders (CMD) and their associated factors among patients with pre-existing chronic NCDs in Sidama, southern Ethiopia.
Methods: A multicenter cross-sectional study was undertaken between June 1 and September 1, 2021. The study included 633 participants. CMD and insomnia were assessed using a 20-item Self-Reported Questionnaire (SRQ-20) and a 7—item Insomnia Severity Index (ISI) scale, respectively. To describe the various variables, descriptive statistics were used. We performed multivariable logistic regression analysis to identify independent factors associated with CMD and insomnia. A value of p < 0.05 was considered statistically significant at a 95% confidence interval.
Results: The prevalence of insomnia and CMD was found to be 39.3% and 46.8%, respectively. Being merchant (AOR = 0.33; 95% CI = 0.13, 0.82), having a diagnosis of diabetes mellitus (AOR = 1.89; 95% CI = 1.04, 3.46), comorbid diagnosis (AOR = 3.96; 95% CI = 2.27, 6.89), low social support (poor (AOR = 3.37; 95% CI = 1.51, 7.57) and moderate (AOR = 3.13; 95% CI = 1.46, 6.69)), symptoms of insomnia (AOR = 12.08; 95% CI = 7.41, 19.72) and poor quality of life (QOL) (AOR = 1.67; 95% CI = 1.04, 2.72) were independent predictors of CMD. We also found out that, having cardiovascular disorders (CVDs) (AOR = 2.48; 95% CI = 1.18, 5.19), CMD (AOR = 12.09; 95% CI = 7.46, 19.61), and poor QOL (AOR = 2.04; 95% CI = 1.27, 3.26) were significantly associated with insomnia symptoms.
Conclusion: Our study suggests that substantially high prevalence of CMD and insomnia. Significant association between CMD and occupation, diagnosis, comorbidity, social support, insomnia, and QOL were found. We also revealed that having CVDs, CMD, and poor QOL were significantly associated with insomnia symptoms. Therefore, dealing with the mental health problems of patients with chronic NCDs is an essential component of public health intervention during the COVID-19 pandemic.
Introduction
Noncommunicable diseases (NCDs) are a group of chronic diseases that significantly increase morbidity and mortality in the community, including cardiovascular disease, stroke, cancer, diabetes, and mental health issues. NCDs have been exerting a significant global burden and considered as primary public health agenda for decades (1). NCDs account for three out of every 4 years lived with disability (YLD), whereas mental disorders contribute for nearly one-fourth of all YLD (2, 3). Mental illness and NCDs are commonly related by underlying individual, community, and social characteristics, and they commonly have a bidirectional relationship (4). Chronic NCDs, for instance, can lead to depression and anxiety, while mental disorders may result in decreased treatment seeking, poor adherence to treatment, and worse the outcome of NCD (5). Studies have discovered an association between chronic pain, long-term neurological conditions, or kidney illness, and depression, anxiety, and sleep problems (6–8).
COVID-19 also known as severe acute respiratory syndrome coronavirus-2 (SARS-CoV2), first appeared in the year 2020, causing a global health crisis and the collapse of several healthcare systems (9, 10). The ongoing COVID-19 outbreak overwhelmed the healthcare system, resulting in remarkable impact in the clinical management of patients with pre-existing chronic illness (11). Patients with pre-existing medical disorders such as diabetes mellitus (DM), hypertension, and cancers are considered to be among the most sensitive to COVID-19 infection, with higher severity and death (12). Patients with hypertension (6%), diabetes (7.3%) and cardiovascular disease (10.5%) had a higher case-fatality rate than the general population (2.3%) (13).
The COVID-19 pandemic is claimed to be the cause of a significant increase in the global prevalence of mental disorders such as sleep problems, anxiety and depression. In addition, WHO expressed concern regarding the influence of COVID-19 on an individual’s mental health and psychosocial implications (14). Evidences showed that individuals’ mental health were worsened during and after the COVID-19 pandemic, compared to before the pandemic (15, 16). Another study found that COVID-19 lockdown was linked to poor quality of sleep, sleep deprivation, and depressed symptoms (17). Moreover, a systematic review found that the COVID-19-affected population in many nations experienced somewhat high rates of insomnia, anxiety, depression, posttraumatic stress disorder, and psychological distress symptoms (18).
People may exhibit signs of depression, anxiety, and stress such loneliness, denial, insomnia, despair, boredom, and irritability, and they even face a greater chance of committing suicide (19). Isolation and loneliness, a lack of treatment options, and limited access to medical care, as well as widespread media coverage of COVID-19 infection’s high infectivity, mortality, and diseases predisposing to an adverse course, all contribute to a significant psychological burden that leads to distress and sleep disturbances (20, 21).
Insomnia is described as subjective complaints about difficulty of falling asleep, nocturnal awakenings, early morning awakening, or non-refreshing sleep (22). Insomnia is one of the most common sleep related disorder, affecting 5–19% of people globally (23, 24). According to Budhiraja and colleagues, one-fourth (27.3%) of people with chronic obstructive lung disease had sleep problems (25). One of the most prevalent issues during the pandemic is sleep disturbance. According to a recent systematic review and meta-analysis (SRMA) study, patients with COVID-19 (57%) had the highest pooled prevalence of insomnia, followed by healthcare professionals (31%), and the general population (18%) (26). The pooled prevalence of insomnia in the Chinese population was 39.1%, according to a recent systematic review (27). A similar review indicated that the prevalence of insomnia in Africa during the pandemic were found to be 28.1%, with higher prevalence in North Africa than Sub-Saharan Africa (31% Vs 24%) (28).
A study was conducted during the initial period of COVID-19 outbreak in China, and it indicated that 8.1% had moderate to severe level of stress, 16.5% had moderate to severe symptoms of depression, and 28.8% had moderate to severe symptoms of anxiety (29). A national survey found that distress was highly prevalent in the general population, with rates of 35, 60, and 45% in China, Iran, and the United States, respectively (30).
Furthermore, sleep disturbances were associated with higher levels of mental distress (26). Sleep is essential for both mental and physical well-being, and it can even enhance immunity and resistance to infections, not to mention the different metabolic, autonomic, and inflammatory systems that are impacted by sleep deprivation (31, 32). Insomnia is becoming more often considered as a distinct and comorbid disorder that requires sleep-focused therapy, despite the fact that sleep disturbance can be an indication of psychological problems (33). In addition to resulting in distress, insomnia initiates and/or worsens other mental health problems, contributes to stress and disability when associated with mental disorders, and frequently remains after other symptoms of mental disorders have subsided. This could be because lack of sleep sensitizes the stress system even more, resulting in more stressful impressions of life events as well as diminished resilience and stress recovery (34–39).
It has been established that the COVID-19 pandemic significantly affects the development of the illness and survival of NCD patients. As a result, worries regarding the mental health of NCD patients have increased. Comorbid anxiety and depression make it difficult for patients to take their medications, which decreases therapeutic safety and efficacy and raises the risk of disability and death. Comorbid mental problems, however, are frequently ignored and sometimes not adequately treated (40). Despite the fact that COVID-19 has a significant impact on chronic disease patients, there is scant research on insomnia, CMD, and their associated factors among chronic disease patients. We hypothesized that COVID-19 has increased the risk of developing insomnia and mental disorders in patients with pre-existing chronic medical illnesses. As a result, the purpose of this study was to examine the prevalence of insomnia and CMD of patients with pre-existing common chronic medical conditions throughout the COVID-19 pandemic times, as well as the factors that contributed to them. The research will provide evidence to policymakers, program planners, and health care practitioners to help them make better decisions, as well as be valuable for evidence-based interventions in treatment of common mental health concerns during a future pandemic.
Materials and methods
Study design, area and period
We conducted a cross-sectional study at four hospitals in Sidama National Regional State, southern Ethiopia, between June 1 and September 1, 2021 [Hawassa university comprehensive specialized hospital (HUCSH), Adare general hospital (AGH), Yirgalem general hospital (YGH), and Leku Primary hospital (LPH)]. The Hawassa University comprehensive specialized hospital, with about 500 beds in southern Ethiopia, serves a population of over 18 million in the Sidama region and surrounding regions of southern Ethiopia, Oromia and Somalia. It is the only specialized hospital in the region. It was provided inpatient services for COVID-19 patients and isolation center in the region and surroundings. Yirgalem General Hospital is found in Yirgalem town and it is one of the General Hospitals in Sidama region serving about 4 million people in the region and nearby. Adare general hospital is located in Hawassa city and serves for communities from Hawassa and nearby cities. Leku primary hospital is one of the primary hospitals found in Sidama region located around 25 kilo meter away from Hawassa city.
Study participants
In this study we have included patients with chronic NCDs such as diabetes, hypertension, chronic cardiovascular diseases, respiratory diseases such as asthma, and others who had regular follow-up visit at the selected hospitals. Individuals with pre-existing chronic medical illnesses receiving follow-up care in the outpatient departments (OPDs) of the four hospitals were contacted and requested to take part in the study if they met the following criteria: (I) patients above the age of 18 with confirmed chronic NCDs; (II) patients with stable clinical condition and able to understand the objective of the survey; and (III) patients with no known serious mental or neurocognitive problems. Patients with pre-existing chronic NCDs who were admitted to the emergency or inpatient units for any reason were not included in the study. The required sample size was estimated using single population proportion formula: (Zα/2)2 × p × (1 − p)/d2, where n is the sample size, z is the standard normal score set at 1.96, d is the desired degree of accuracy and p is the estimated proportion of the target population. By taking p = 50% (because there were no similar study in the area and to get adequate or maximum sample size), Zα/2 = 1.96 and d = 5%, the computed sample size was 384; and by taking 10% non-response rate, the total sample size computed was 422. Using design effect 1.5, our final sample size was estimated to be 633 (we used level of hospitals as a cluster, i.e., primary, general and specialized hospital). Sample size was proportionally allocated to each hospital based on the patient flow of the hospitals.
Data collection methods
A standardized structured interviewer administered questionnaire was used to collect data. The questionnaire included items or scales that assess patients’ socio-demographic characteristics, clinical characteristics, social support, common mental disorders (CMD), insomnia, and quality of life (QOL). The questionnaire was written in English before being translated into Amharic, the local language. The questionnaire was translated from English into Amharic by native speakers of the language who are fluent in English, then back-translated into English by other translators to guarantee consistency. Finally, the Amharic version of the questionnaire was used to collect data.
Data were collected by nurses who had received 2 days of training on data collection processes and assessment tools. A pretest was performed on 5% of the sample to discover potential difficulties with the data collection procedures, as well as to assess the consistency of the questionnaires and the competency of the data collectors. The investigators reviewed each questionnaire for completeness on a regular basis during data collection.
Data collection tools
Social support
Social support of patients with pre-existing chronic NCDs was measured using the three-item Oslo social support scale (OSSS). The scale has a score of minimum 3 and maximum 14. It has three categories. A score of 3–8, 9–11, and 12–14 indicates poor, moderate, and strong social support, respectively (41).
Common mental disorder
The World Health Organization developed the SRQ-20, a 20-item screening tool for common mental disorders (42). There are only binary (yes/no) questions, where “1” denotes the presence of a symptom and “0” denotes its absence. The SRQ-20 item questions categorize depression, anxiety, and psychosomatic issues as CMD (43). The SRQ-20’s validity, reliability, and cut-off differ according to the population (culture, language, setting, and gender) in various circumstances (43–46). The SRQ-20 exhibited good internal reliability (= 0.78) and an ideal cut-off score of 5/6, with a sensitivity of 78.6% and a specificity of 81.5% (47). The SRQ-20 measure demonstrated good internal consistency (Cronbach’s α = 0.89) in our study.
Insomnia
The nature, intensity, and effects of insomnia are evaluated using the ISI, a seven-item self-assessment questionnaire (48). The following elements are taken into account: the severity of difficulty of falling asleep, staying asleep, and waking up early in the morning; sleep dissatisfaction; how sleep issues affect daytime functioning; how others perceive the difficulty of sleep; and the distress caused by recent difficulty of sleep. Each item is rated on a 5-point Likert scale (0 = no problem; 4 = very severe difficulty, for example), with the total score ranging from 0 to 28. The overall score is divided into four categories: no insomnia (0–7), sub-threshold insomnia (8–14), moderate insomnia (15–21), and severe insomnia (22–28). A higher score illustrates severe insomnia (48–50). In the present study, the ISI measure showed very high internal consistency (Cronbach’s alpha = 0.96).
Quality of life
To analyze the impact of the COVID-19 pandemic on QOL, we used an adapted version of 12 items (51), from the WHOQOL-BREF scale (52, 53). The 12-item WHOQOL-BREF scale that was modified had a minimum score of 12 and a maximum score of 60. Due to the detrimental impacts of the COVID-19 pandemic, low scores indicate a lower QOL. In a prior study, the modified WHOQOL-BRIEF (12-items) showed acceptable internal consistency (Cronbach’s alpha = 0.81) (51). The 12-item WHOQOL-BRIEF that was used in our study had good internal consistency (Cronbach’s alpha = 0.82).
Data analysis
For analysis, the data collected were entered into Epi-data version 3.1 and exported to SPSS version 24 for Windows. Various variables were described using descriptive statistics such as frequency, percentage, mean, standard deviation, and median. Binary and multivariable logistic regression were used to identify independent factors of insomnia and CMD. The Hosmer-Lemeshow test was used to assess model fitness. At 95% confidence interval (CI), p-values of <0.05 were considered as statistically significant.
Results
Socio-demographic characteristics of study participants
A total of 633 patients with pre-existing chronic NCDs were involved in this study. Majority were male 357(56.4%), 410(64.8%) participants were married, 352(55.6%) were Protestant by religion and about one-fourth 175(27.6%) were illiterate. Of the total participants, about one-fifth 144(22.7%) were farmer by occupation and majority 353(55.8%) were urban residents. The mean age of the respondents was 46.49 ± 17.71 as described in Table 1.
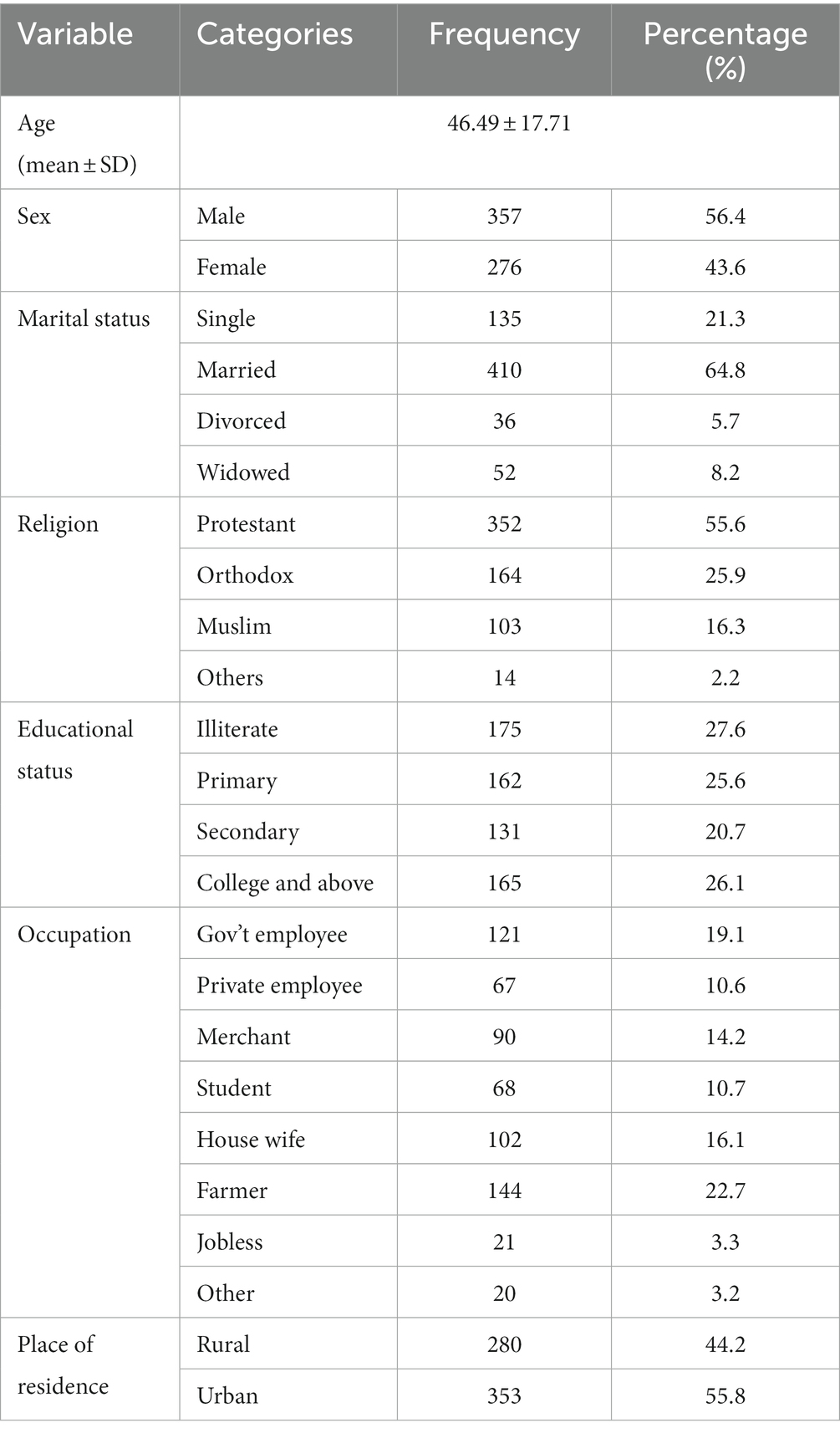
Table 1. Socio-demographic characteristics of study participants at Sidama National Regional State, southern Ethiopia, 2021 (n = 633).
Clinical characteristics of study participants
About half 336(53.1%) of the participants were diagnosed with diabetes mellitus followed by hypertension 111(17.5%) and nearly one-third 200(31.6%) participants had comorbid diagnosis. Majority 364(57.5%) of the participants were ill for ≤5 years, 61(9.6%) and 49(7.7%) participants were using alcohol and khat in the past three months, respectively. Among the total participants, more than one-third 224(35.4%) and about half 332(52.4%) had poor and moderate social support, respectively. Moreover, 293(46.3%) of participants were poor QOL (Table 2).
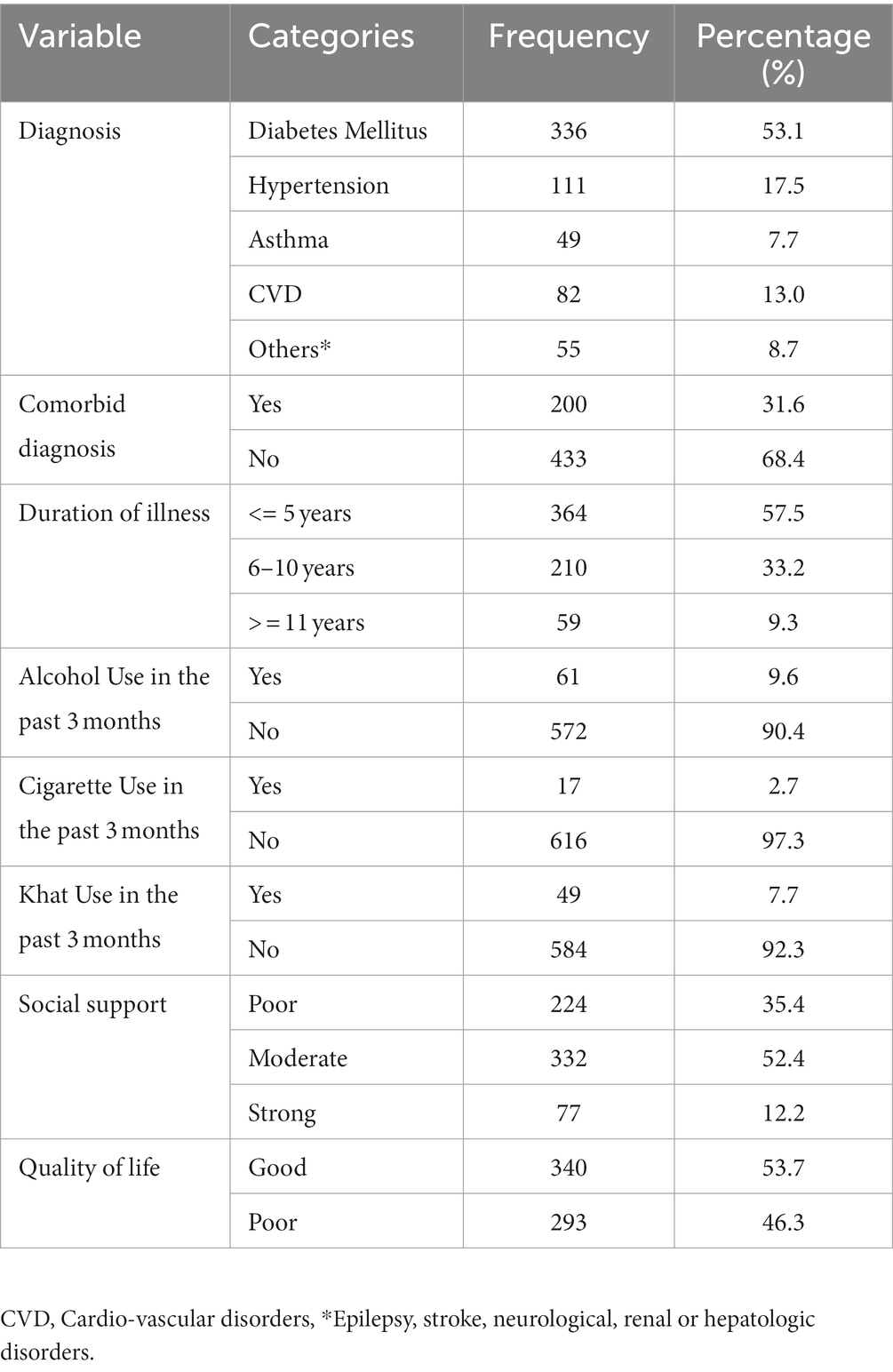
Table 2. Clinical characteristics of study participants at Sidama National Regional State, southern Ethiopia, 2021 (n = 633).
Prevalence of insomnia and CMD
The prevalence of insomnia and CMD were found to be 39.3% (95% CI = 35.3–43.3%) and 46.8% (95% CI = 42.8–50.6%), respectively as shown in Figure 1.
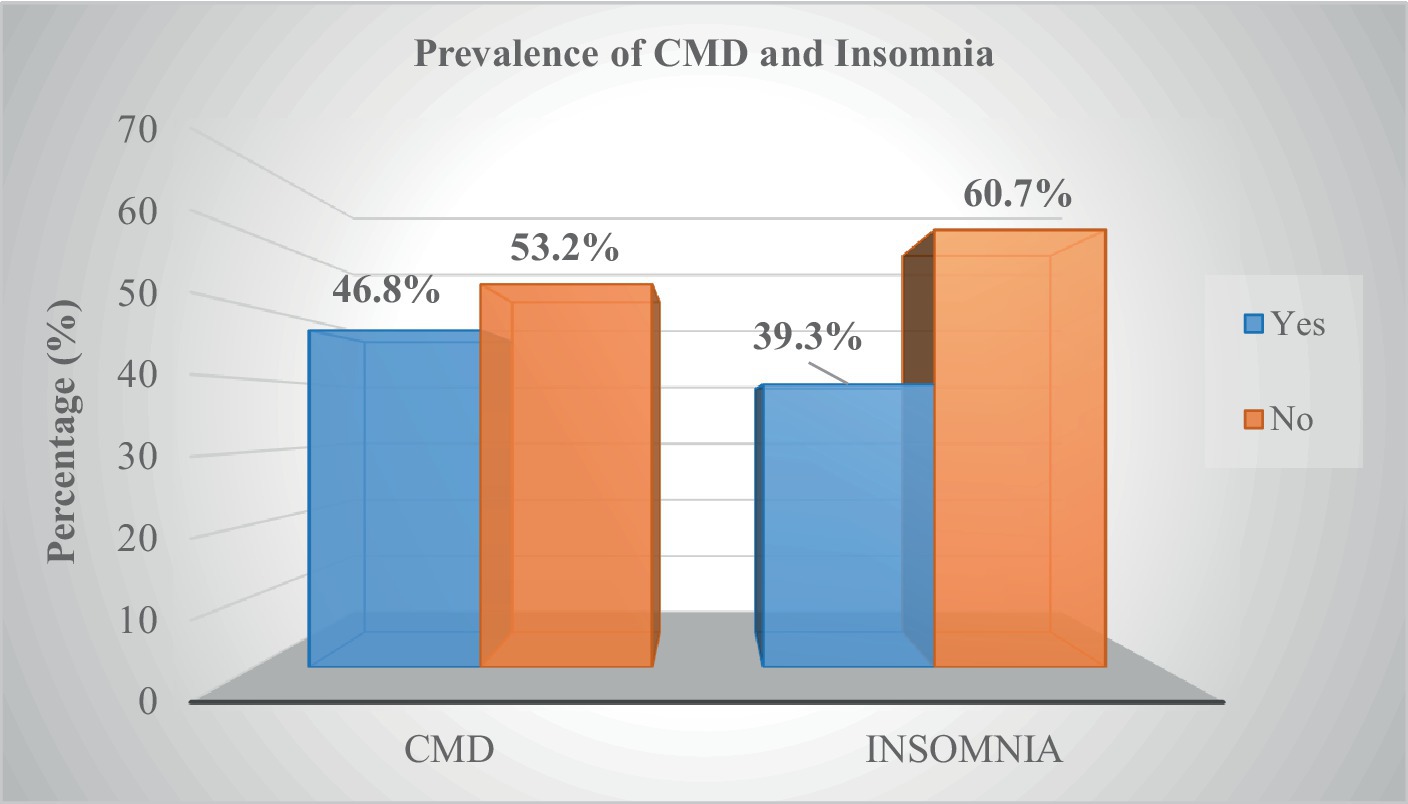
Figure 1. Prevalence of insomnia and CMD study participants at Sidama National Regional State, southern Ethiopia, 2021 (n = 633).
Independent predictors of CMD and insomnia
In a multivariable logistic regression model, occupation, diagnosis, comorbid diagnosis, social support, insomnia, and quality of life were all significantly associated with CMD. When compared to government employees, being a merchant is 66% (AOR = 0.33; 95% CI = 0.13, 0.82) less likely to develop CMD. Regression analyses revealed that having a diagnosis of diabetes mellitus (AOR = 1.89; 95% CI = 1.04, 3.46) and a comorbid diagnosis (AOR = 3.96; 95% CI = 2.27, 6.89) increased the likelihood of reporting CMD significantly more than having a diagnosis of hypertension and their counterparts. Poor social support (AOR = 3.37; 95% CI = 1.51, 7.57) and moderate social support (AOR = 3.13; 95% CI = 1.46, 6.69) were both associated with an increased risk of developing CMD. Individuals with symptoms of insomnia (AOR = 12.08; 95% CI = 7.41, 19.72) and poor QoL (AOR = 1.67; 95% CI = 1.04, 2.72) were more likely to report CMD as shown in Table 3. We also found out that, having CVDs (AOR = 2.48; 95% CI = 1.18, 5.19), CMD (AOR = 12.09; 95% CI = 7.46, 19.61), and poor QOL (AOR = 2.04; 95% CI = 1.27, 3.26) increased the odds of having insomnia (Table 4).
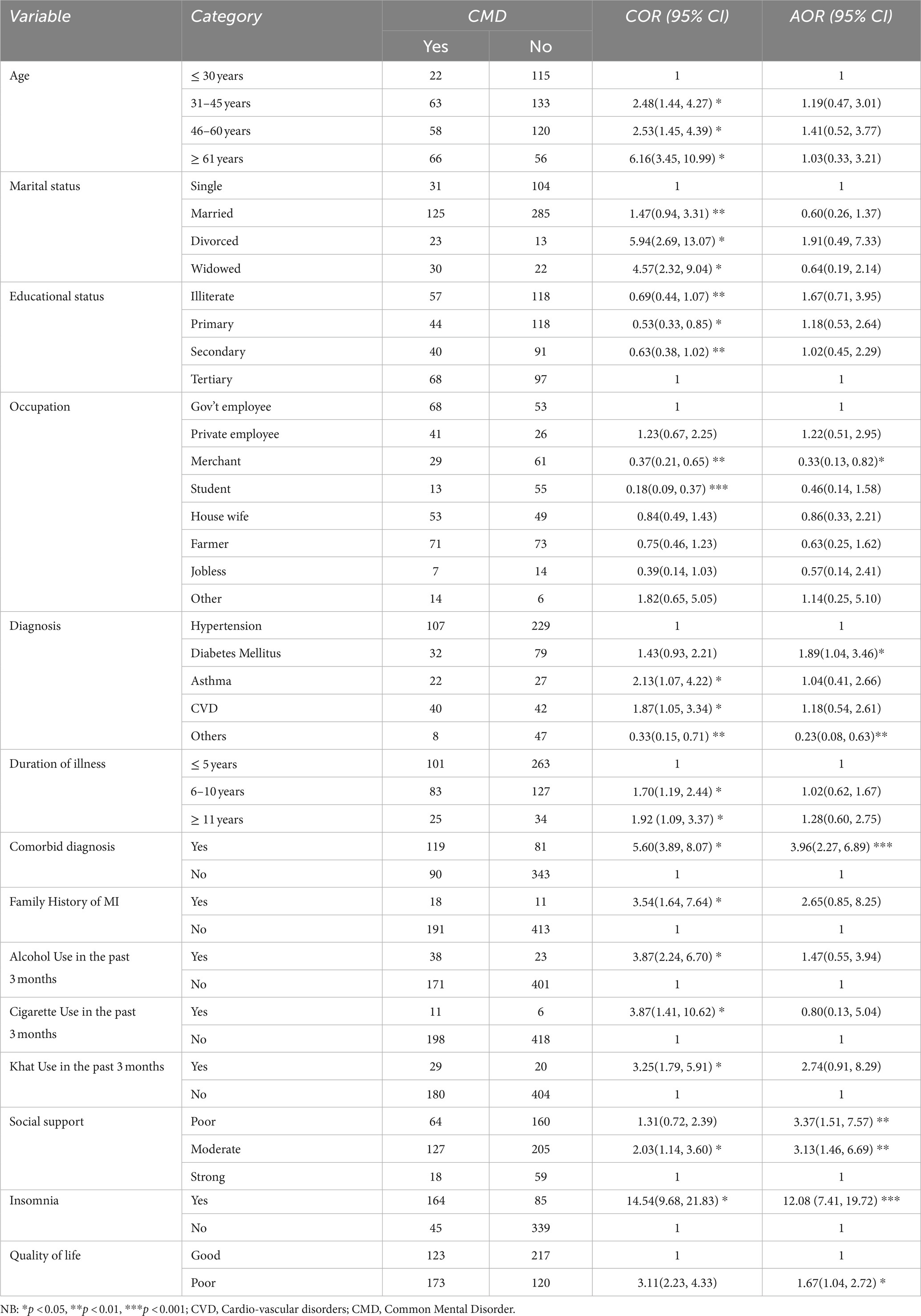
Table 3. Factors associated with CMD among patients with chronic NCDs during COVID-19 pandemic in selected hospitals of Sidama national regional state, 2021 (n = 633).
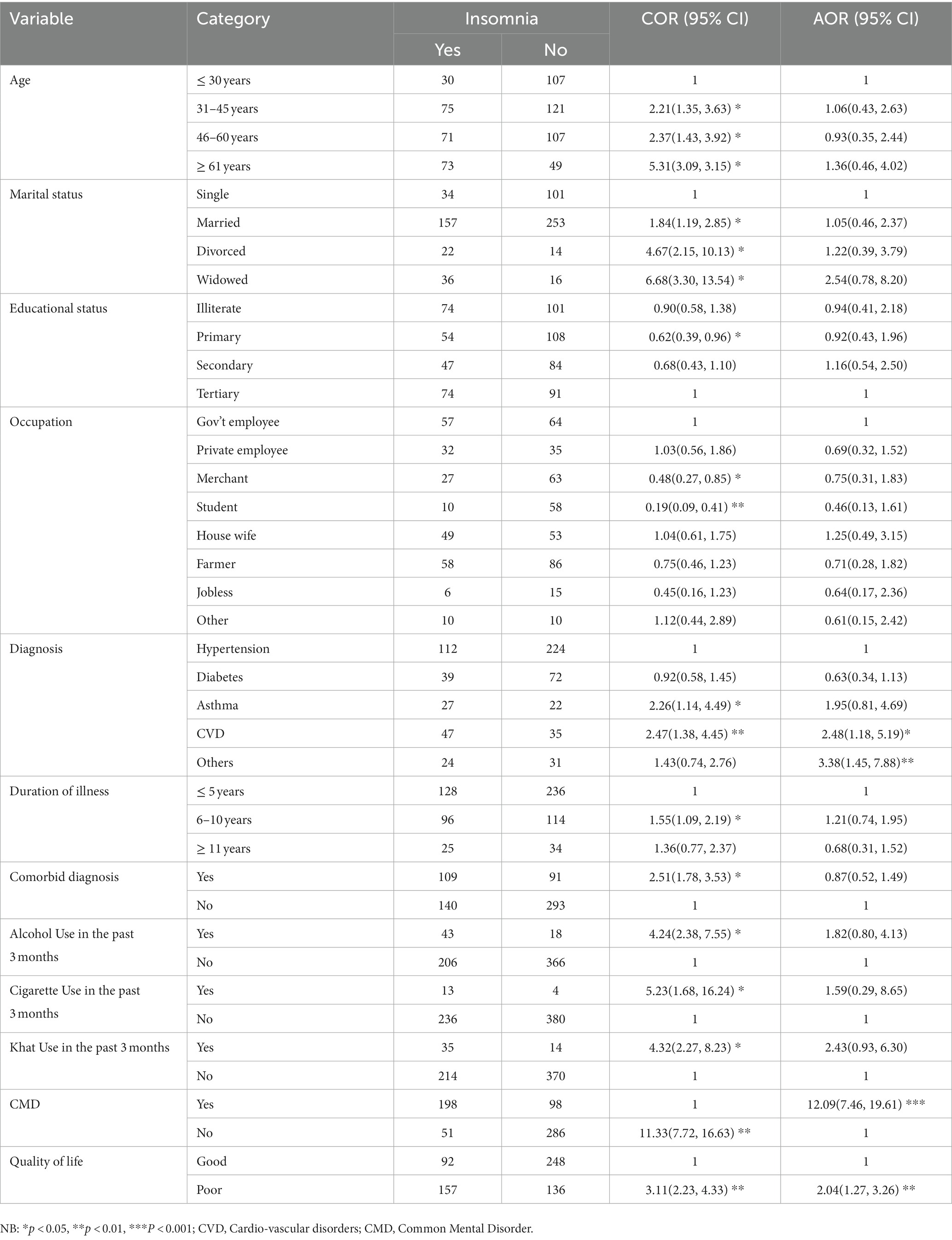
Table 4. Factors associated with Insomnia among patients with chronic NCDs during COVID-19 pandemic in selected hospitals of Sidama national regional state, 2021 (n = 633).
Discussion
The COVID-19 pandemic appears to be having a severe impact on the mental health of individuals with pre-existing medical conditions. In this study, we examined the prevalence and predictors of COVID-19 pandemic related common mental disorders (CMD) and insomnia in patients with chronic medical conditions in south Ethiopia. CMD and insomnia levels were surprisingly high, according to our research. Being a merchant, having diabetes mellitus, having a longer illness duration, having comorbid diagnoses, having low social support, having comorbid insomnia, and having a poor quality of life (QoL) were significant predictors of CMD. Additionally, a significant association between a high risk of insomnia and a diagnosis of cardio-vascular disorders, concurrent CMD, and poor QoL was found. The prevalence of insomnia and CMD indicates a need for mental health and psychosocial support (MHPSS) during the COVID-19 pandemic.
CMDs such as anxiety and depression were found to be more common in pre-existing physical conditions with a higher risk of COVID-19 infection in previous studies (54, 55). Our finding suggests that nearly half (46.8%) of the participants experience CMD. Comparable findings were reported from previous studies in India (52.9%), Saudi Arabia (45.6%), and China (45%) (56–58). This shows that COVID-19 had a serious impact on the mental health of people with pre-existing NCDs. Mental health of the population was significantly impacted by the public health measures implemented to stop the spread of COVID-19 and the fear of getting the infection (59). The association between chronic medical problems and mental disorders is generally speculated to be bidirectional. People suffering from a significant mental illness are more likely to develop a variety of chronic physical illnesses. People with chronic medical illnesses, on the other hand, more likely to experience psychological problems than the general population (60). For instance, compliance with chronic medication use and regular use of the healthcare system may be challenging during infectious disease outbreaks, adding to psychological distress.
However, lower prevalence were reported in Ethiopia (22.8%) (61), and India (33.2%) (62). A similar study conducted in Bangladesh found a low prevalence of anxiety (35.2%) and depression (38.9%) (60). On the other hand, higher prevalence were also reported in studies conducted in Harar (62%) (60), and Mettu Karl Referral Hospital 55.7% (depression) and 61.8% (anxiety) (59). Moreover, other pre-COVID-19 researches indicated higher estimates of mental health problems in different parts of the world such as 63.3% in Ethiopia (63), 60.2% in Pakistan (64), 64.4% in Nigeria (65), and (58.7%) in Delhi, India (66). These disparities could be due to changes in sample size, inclusion criteria, screening instrument, setting, study period, and study population. Consequently, physical illnesses were associated with a higher likelihood of mental health problems, which could be explained by underlying physical disorders and a lack of medical help during an epidemic (67, 68). The findings suggested that different strategies should be designed to address mental health issues during epidemics.
This result of this study revealed that the prevalence of insomnia among chronic medical conditions was found to be 39.3%. Previous investigations and systematic review reports in different situations and populations provided almost approximate results in line with our findings (69–72). Similar results were recently observed in a variety of populations, including outpatients (39.5%), healthcare professionals (44.6%), and general population (39.8%) (73) and patients with chronic medical illness (32.6%) (74), during the COVID-19 pandemic. However, lower prevalence were also reported by Nochaiwong et al., (28%) and Liu et al., (30%) among general population and Mulyadi et al., (33%) among college students (75–77). On the other hand, higher prevalence were reported in COVID-19 patients (57%), cancer outpatients (48.6%), and depression outpatients (80.9%), individuals living with disabilities (71%) during the COVID-19 era (78–81). Therefore, variations in people’s underlying medical conditions may account for variations in the prevalence rates of insomnia.
Being a governmental employee increases the likelihood to have CMD as compared to merchants. This finding is consistent with a recent study (82). The civil servants who participated in COVID-19 control were reported to have various types of psychological disorders (83). It has been noted that lack of public support, long working hours, a high degree of work related stress, work instability, and an unfavorable physical environment are risk factors for the development of symptoms of mental disorders in government employees (84–86). Furthermore, many government employees encounter emotional distress due to psychological disorders like depression and anxiety during and even after pandemics (87).
Similarly, those with inadequate (poor and moderate) social support were more likely to have CMD than those with strong social support, which is consistent with previous studies (59, 88, 89). Individuals with higher levels of social support may be more likely to believe they will obtain the necessary assistance when confronted with the stressful event of a pandemic outbreak. This idea would improve their views about dealing with adversity and difficulty in the fight against COVID19, resulting in greater levels of resilience (88). This could be associated with the fact that those who did not have social support throughout the pandemic are more vulnerable to mental illness since their social health is disrupted (61). Furthermore, a lack of social support has a detrimental effect on self-care, adherence, and the ability to react to or deal with stressful events, and it may lead to the development of depression (90). Also, perceived social support may help individuals resist and successfully cope the risk factors associated with their mental health (91). As a result, our findings highlight the importance of strong social support during pandemics, as it may have a positive impact on mental health.
This study indicated that patients diagnosed with diabetes were more prone to develop CMD as compared to hypertension. Mental health problems such as depression is more likely to occur in people with diabetes (92–94). Several studies have recently revealed that patients with diabetes mellitus had significant psychological problems during the COVID-19 pandemic (95–98). This has been linked to hypothalamic–pituitary–adrenal (HPA) dysfunction in both diabetes and depression (99). The immune system, glucose metabolism, and sleep—indicators of impaired health in both diseases—are regulated by this route, which is crucial under stress (100). Moreover, we found out that patients diagnosed with cardiovascular disorders such as heart failure were more likely to develop insomnia as compared to patients with hypertension. Previous studies suggested that patients with CVD are more prone to sleep disturbances (101, 102). Insomnia is linked to fatigue, depressed symptoms, daytime sleepiness, and decreases in self-reported and objective functional status, all of which are major issues for CVD patients (103). This could be explained by the hypothalamic–pituitary axis (HPA) dysregulation, inappropriate modulation of the autonomic nervous system, elevated sympathetic nervous system activity, and systemic inflammation that are all factors in the etiology of cardiovascular disease (102). In addition, several pandemic-specific factors, such as fear of acquiring the virus and being unable to visit loved ones, suggest that insomnia may increase during this time (104).
In this study, participants with CMD were more likely to be at risk to develop insomnia and vice versa. In general, there is evidence that mental health problems are associated to sleep disturbances and that insomnia is related to the psychological stress. That is, a bidirectional relationship between insomnia and psychological problems were clearly demonstrated (105). Furthermore, people who have a chronic medical condition may experience severe physical discomfort, which can lead to anxiety and depression and disturbed sleep (106). The conclusion could be attributed to COVID-19’s direct psychosocial effects on those with chronic medical conditions, fear of contracting COVID-19, and the virus’s deadly effect on chronic medical patients.
Our study also showed that participants who had poor QoL were more likely to develop CMD and insomnia. Similarly, recent studies have discovered that poor QoL is associated with insomnia and poor sleep quality (107, 108) and lower QoL scores were indicated by individuals who felt more stress, depression, and anxiety (51). Previous research has shown that there is an inverse relationship between QOL and mental health disorders such as depression and anxiety (109) and sleep disturbances (110). As a result, it is not surprising that poor QOL in individuals with chronic medical illnesses has an impact on mental health and sleep, as shown in this study.
There were certain limitations in this study. First, due to the study’s cross-sectional methodology, it was unable to demonstrate causal links between the variables investigated. Second, because all of the data was self-reported and the participants’ responses were not independently validated, social desirability bias and recall bias could have occurred. Third, because the study’s participants were all people with chronic illnesses, the findings cannot be generalized to the general public.
Conclusion
This study highlights the prevalence of CMD and Insomnia among patients with chronic NCDs were found to be considerably high. Occupation, diagnosis, comorbid diagnosis, social support, insomnia, and quality of life were all significantly associated with CMD. We also found out that, having CVDs, CMD, and poor QOL significantly increases the likelihood of having insomnia symptoms. As a result, addressing mental health issues among patients with chronic CMD is an essential component of public health interventions during the COVID-19 pandemic.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Hawassa University, College of Medicine and Health Sciences, Institutional Review Board (IRB) with reference number IRB/076/13. The participants provided their written informed consent to participate in this study.
Author contributions
MA, BD, AG, SH, and ET participated in the conception and designed the study and involved in the data collection. MA, BD, and SD do the analysis of the study. MA and SD prepares the manuscript for publication. BD, AG, SH, SD, and ET critically reviewed the manuscript. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to thank Hawassa University for providing fund to conduct this study. Our heartfelt gratitude also goes to the data collectors and participants for their valuable contributions to the study process.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. GBD 2019 diseases and injuries collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990– 2019: a systematic analysis for the global burden of disease study 2019. Lancet. (2020) 396:1204. doi: 10.1016/S0140-6736(20)30925-9
2. Whiteford, HA, Ferrari, AJ, Degenhardt, L, Feigin, V, and Vos, T. The global burden of mental, neurological and substance use disorders: an analysis from the global burden of disease study 2010. PLoS One. (2015) 10:e0116820. doi: 10.1371/journal.pone.0116820
3. Roth, GA, Abate, D, Abate, KH, Abay, SM, Abbafati, C, Abbasi, N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392:1736–88. doi: 10.1016/S0140-6736(18)32203-7
4. Stein, DJ, Benjet, C, Gureje, O, Lund, C, Scott, KM, Poznyak, V, et al. Integrating mental health with other non-communicable diseases. BMJ. (2019) 364:l295. doi: 10.1136/bmj.l295
5. Aebischer Perone, S, Martinez, E, du Mortier, S, Rossi, R, Pahud, M, Urbaniak, V, et al. Non-communicable diseases in humanitarian settings: ten essential questions. Confl Heal. (2017) 11:17. doi: 10.1186/s13031-017-0119-8
6. Theofilou, P. Quality of life and mental health in hemodialysis and peritoneal dialysis patients: the role of health beliefs. Int Urol Nephrol. (2011) 44:245–53. doi: 10.1007/s11255-011-9975-0
7. Gerontoukou, EI, Michaelidoy, S, Rekleiti, M, Saridi, M, and Souliotis, K. Investigation of anxiety and depression in patients with chronic diseases. Heal. Psychol Res. (2015) 3:2123. doi: 10.4081/hpr.2015.2123
8. Wankowicz, P, Szylinska, A, and Rotter, I. Evaluation of mental health factors among people with systemic lupus erythematosus during the SARS-CoV-2 pandemic. J Clin Med. (2020) 9:9092872. doi: 10.3390/jcm9092872
9. Shamasunder, S, Holmes, SM, Goronga, T, Carrasco, H, Katz, E, Frankfurter, R, et al. COVID-19 reveals weak health systems by design: why we must re-make global health in this historic moment. Glob Public Heal. (2020) 15:1083–9. doi: 10.1080/17441692.2020.1760915
10. Maani, N, and Abdalla, SMGS. Avoiding a legacy of unequal non-communicable disease burden after the COVID-19 pandemic. Lancet Diabetes Endocrinol. (2021) 9:133–5. doi: 10.1016/S2213-8587(21)00026-7
11. Favalli, EG, Monti, S, Ingegnoli, F, Balduzzi, S, and Caporali, RMC. Incidence of COVID-19 in patients with rheumatic diseases treated with targeted immunosuppressive drugs: what can we learn from observational data? Arthritis Rheumatol. (2020) 72:1600–6. doi: 10.1002/art.41388
12. Bai, Y, Yao, L, Wei, T, Tian, F, Jin, DY, Chen, L, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. (2020) 323:1406–7. doi: 10.1001/jama.2020.2565
13. Wu, ZMJ. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese center for disease control and prevention. JAMA. (2020) 323:1239–42. doi: 10.1001/jama.2020.2648
14. World Health Organization (WHO). Mental health and psychosocial considerations post Covid-19 outbreak [internet]. World Health Organization. (2021) 1–6. Available at: https://apps.who.int/iris/bitstream/handle/10665/331490/WHO-2019-nCoV-MentalHealth-2020.1-eng.pdf
15. Breslau, J, Finucane, ML, Locker, AR, Baird, MD, Roth, EA, and Collins, RL. A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Prev Med (Baltim) [Internet]. 2021; (2020) 143:106362. doi: 10.1016/j.ypmed.2020.106362
16. Benke, C, Autenrieth, LK, Asselmann, E, and Pané-Farré, CA. Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res [Internet]. (2020) 293:113462. doi: 10.1016/j.psychres.2020.113462
17. Gupta, R, Grover, S, Basu, A, Krishnan, V, Tripathi, A, Subramanyam, A, et al. Changes in sleep pattern and sleep quality during COVID-19 lockdown. Indian J Psychiatry. (2020) 62:370–8. doi: 10.4103/psychiatry.IndianJPsychiatry_523_20
18. Xiong, J, Lipsitz, O, Nasri, F, Lui, LMW, Gill, H, Phan, L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. (2020) 277:55–64. doi: 10.1016/j.jad.2020.08.001
19. Brooks, SK, Webster, RK, Smith, LE, Woodland, L, Wessely, S, Greenberg, N, et al. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet (London, England). (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
20. Bohlken, J, Schömig, F, Lemke, MR, Pumberger, M, and Riedel-Heller, SG. COVID-19 pandemic: stress experience of healthcare workers—A short current review. Psychiatry Pr. (2020) 47:190–7. doi: 10.1055/a-1159-5551
21. Zhang, C, Yang, L, Liu, S, Ma, S, Wang, Y, Cai, Z, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front. Psychiatry. (2020) 11:306. doi: 10.3389/fpsyt.2020.00306
23. Pallesen, S, Sivertsen, B, and Nordhus, IHBB. A 10-year trend of insomnia prevalence in the adult Norwegian population. Sleep Med. (2014) 15:173–9. doi: 10.1016/j.sleep.2013.10.009
24. Ohayon, MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. (2002) 6:97–111. doi: 10.1053/smrv.2002.0186
25. Budhiraja, R., Parthasarathy, S., Budhiraja, P., Habib, M. P., Wendel, C., and Quan, SF. Insomnia in patients with COPD. Sleep (2012);35:369–375, doi: 10.5665/sleep.1698
26. Tsang, HWH, Grif, MD, Alimoradi, Z, Brostr, A, Haghayegh, S, Ohayon, MM, et al. Sleep problems during COVID-19 pandemic and it’s association to psychological distress: A systematic review and meta-analysis. EClinicalMed. (2021) 36:100916. doi: 10.1016/j.eclinm.2021.100916
27. Li, Y, Chen, B, Hong, Z, Sun, Q, and Dai, Y. Insomnia symptoms during the early and late stages of the COVID-19 pandemic in China: a systematic review and meta-analysis. Sleep Med. (2021) 91:262–72. doi: 10.1016/j.sleep.2021.09.014
28. Chen, J, Farah, N, Dong, RK, Chen, RZ, Xu, W, Yin, J, et al. Mental health during the COVID-19 crisis in Africa: A systematic review and Meta-analysis. Int J Environ Res Public Heal. (2021) 18:1–19. doi: 10.3390/ijerph182010604
29. Wang, C, Pan, R, Wan, X, Tan, Y, Xu, L, Ho, CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Heal. (2020) 17:1–25. doi: 10.3390/ijerph17051729
30. United Nations Policy Brief: COVID-19 and the need for action on mental health. UN Secretary-General, UN Sustainable Development Group. (2020). Available at: https://reliefweb.int/report/world/policy-brief-covid-19-and-need-action-mental-health-13-may-2020?gclid=CjwKCAjwo9unBhBTEiwAipC11wYCarVA3YvW6pdbQE5jnPmus8BLxRCgpfnLuZOdbyny6dc78pMi5xoCw2sQAvD_BwE.
31. Fernandez-Mendoza, JVA. Insomnia and its impact on physical and mental health. Curr Psychiatry Rep. (2013) 15:418. doi: 10.1007/s11920-013-0418-8
32. Kumar, A, and Goel, HNS. Short sleep duration and the risk of hypertension: snoozing away high blood pressure? J Hum Hypertens. (2019) 33:174–6. doi: 10.1038/s41371-019-0177-z
33. Vargas, IPM. Insomnia and depression: clinical associations and possible mechanistic links. Curr Opin Psychol. (2020) 34:95–9. doi: 10.1016/j.copsyc.2019.11.004
34. Palagini, L, Moretto, U, Novi, M, Masci, I, Caruso, D, Drake, CL, et al. Lack of resilience is related to StressRelated sleep reactivity, hyperarousal, and emotion dysregulation in insomnia disorder. J Clin Sleep Med. (2018) 14:759–66. doi: 10.5664/jcsm.7100
35. Morin, CM, and Rodrigue, SIH. Role of stress, arousal, and coping skills in primary insomnia. Psychosom Med. (2003) 65:259–67. doi: 10.1097/01.PSY.0000030391.09558.A3
36. Kalmbach, DA, Pillai, V, Arnedt, JT, and Anderson, JRDC. Sleep system sensitization: evidence for changing roles of etiological factors in insomnia. Sleep Med. (2016) 21:63–9. doi: 10.1016/j.sleep.2016.02.005
37. Gehrman, P, Seelig, AD, Jacobson, IG, Boyko, EJ, Hooper, TI, Gackstetter, GD, et al. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment. Sleep. (2013) 36:1009–18. doi: 10.5665/sleep.2798
38. Carney, CE, Segal, ZV, and Edinger, JDKA. A comparison of rates of residual insomnia symptoms following pharmacotherapy or cognitive-behavioral therapy for major depressive disorder. J Clin Psychiatry. (2007) 68:254–60. doi: 10.4088/JCP.v68n0211
39. Hertenstein, E, Feige, B, Gmeiner, T, Kienzler, C, Spiegelhalder, K, Johann, A, et al. Insomnia as a predictor of mental disorders: A systematic review and meta-analysis. Sleep Med Rev. (2019) 43:96–105. doi: 10.1016/j.smrv.2018.10.006
40. DeJean, D, Giacomini, M, Vanstone, M, and Brundisini, F. Patient experiences of depression and anxiety with chronic disease: a systematic review and qualitative meta-synthesis. Ont Health Technol Assess Ser [Internet]. (2013) 13:1–33. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3817854/.
41. Bøen, H, Dalgard, OS, and Bjertness, E. The importance of social support in the associations between psychological distress and somatic health problems and socio-economic factors among older adults living at home: a cross sectional study. BMC Geriatr. (2012) 12:1–12. doi: 10.1186/1471-2318-12-27
42. Sartorius, NJA. Psychiatric assessment instruments developed by the World Health Organization. Soc Psychiatry Psychiatr Epidemiol. (1996) 31:55–69. doi: 10.1007/BF00801901
43. Beusenbrg, MOJ. A user’s guide to the self-reporting questionnaire (SRQ). Geneva: World Health Organization, Division of Mental Health. World Heal Organ (1994).
44. Khan, AMFM. Maternal common mental disorders and associated factors: a cross-sectional study in an urban slum area of Dhaka, Bangladesh. Int J Ment Heal Syst. (2017) 11:11. doi: 10.1186/s13033-017-0129-3
45. Cherian, VI, Peltzer, K, and Cherian, L. The factor structure of the self-reporting questionnaire (SRQ-20) in South Africa. East Afr Med J. (1998) 75:654–6.
46. Giang, KB, Allebeck, P, Kullgren, G, and van Tuan, N. The Vietnamese version of the self-reporting questionnaire 20 (SRQ 20) in detecting mental disorders in rural Vietnam: a validation study. Int J Soc Psychiatry. (2006) 52:175–84. doi: 10.1177/0020764006061251
47. Netsereab, TB, Kifle, MM, Tesfagiorgis, RB, Habteab, SG, Weldeabzgi, YK, and Tesfamariam, OZ. Validation of the WHO self –reporting questionnaire – 20 (SRQ – 20) item in primary health care settings in Eritrea. Int J Ment Health Syst. (2018) 12:1–9. doi: 10.1186/s13033-018-0242-y
48. Bastien, CH, and Vallières, AMC. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. (2001) 2:297–307. doi: 10.1016/S1389-9457(00)00065-4
49. Yu, DS. Insomnia severity index: psychometric properties with Chinese community-dwelling older people. J Adv Nurs. (2010) 66:2350–9. doi: 10.1111/j.1365-2648.2010.05394.x
50. Morin, CM, Belleville, G, Bélanger, L, and Ivers, H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. (2011) 34:601–8. doi: 10.1093/sleep/34.5.601
51. Algahtani, FD, Hassan, S, and Alsaif, B. Assessment of the quality of life during COVID-19 pandemic: A cross-sectional survey from the Kingdom of Saudi Arabia. Int J Environ Res Public Heal. (2021) 18:847. doi: 10.3390/ijerph18030847
52. Ohaeri, JU, and Awadalla, AW. The reliability and validity of the short version of the WHO quality of life instrument in an Arab general population. Ann Saudi Med. (2009) 29:98–104. doi: 10.4103/0256-4947.51790
53. World Health Organization (WHO). WHOQOL-BREF; introduction, administration, scoring and generic version of the assessment. Geneva: World Health Organization. (1996). 1–18 p.
54. Wang, Y, Kala, MP, and Id, THJ. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLoS One [Internet]. (2020) 15:1–27. Available from:. doi: 10.1371/journal.pone.0244630
55. Yu, JY, Kim, JS, Hong, CM, Lee, KY, Cho, NJ, Park, S, et al. Psychological distress of patients with endstage kidney disease undergoing dialysis during the 2019 coronavirus disease pandemic: A cross-sectional study in a university hospital. PLoS One [Internet]. (2021) 16:1–14. Available from:. doi: 10.1371/journal.pone.0260929
56. Arora, U, Chaudhary, C, Babu, GK, Kona, JSSP, and Babji, K. Effect of anxiety, stress, and depression on hypertension and diabetes during COVID – 19 lockdown period in Faridabad: A cross – sectional study. MRIMS J Heal Sci. (2021) 9:122–31. doi: 10.4103/mjhs.mjhs_18_21
57. Mukrim, ME, Alshammari, NM, Alshammari, WM, Alshammari, MS, Alshammari, YN, Alshammari, AS, et al. Prevalence of depression, anxiety, and stress among diabetes mellitus patients in Arar. Northern Saudi Arabia IJMDC. (2019) 3:229–33. doi: 10.24911/IJMDC.51-1542576396
58. Deng, J, Zhou, F, Wenteng Hou, ZS, Wong, CY, Chang, O, Huang, E, et al. The prevalence of depression, anxiety, and sleep disturbances in COVID-19 patients: a meta-analysis. Ann N Y Acad Sci. (2021) 1486:90–111. doi: 10.1111/nyas.14506
59. Hajure, M, Tariku, M, Mohammedhussein, M, and Dule, A. Depression, anxiety and associated factors among chronic medical patients amid covid-19 pandemic in Mettu Karl referral hospital, Mettu, Ethiopia, 2020. Neuropsychiatr Dis Treat. (2020) 16:2511–8. doi: 10.2147/NDT.S281995
60. Tareke, M, Bayeh, AB, Birhanu, M, and Belete, A. Psychological distress among people living with chronic medical illness and the general population, Northwest Ethiopia: A comparative cross-sectional study. PLoS One [Internet]. (2022) 17:e0278235. Available from:. doi: 10.1371/journal.pone.0278235
61. Gedamu, S, Dires, A, and Goshiye, D. Psychological impact of COVID-19 pandemic on chronic disease patients in Dessie town government and private hospitals, Northeast Ethiopia. Diabetes Metab Syndr Clin Res Rev. (2020) 15:129–35. doi: 10.1016/j.dsx.2020.12.019
62. Wang, C, Pan, R, Wan, X, Tan, Y, Xu, L, Ho, CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Heal. (2019) 17:1–25. doi: 10.3390/ijerph17051729
63. Ayana, T, and Roba, KMM. Psychological distress and associated factors among adult tuberculosis patients attending public health institutions in Dire Dawa and Harar cities Eastern Ethiopia. BMC Public Health. (2019) 19:1392. doi: 10.1186/s12889-019-7684-2
64. Vaswani, M, and Haider, AZ-NR-R. Frequency of depression and anxiety among adult epileptic patients. Baqai J Heal Sci. (2018) 21:8–17. Available at: https://applications.emro.who.int/imemrf/Baqai_J_Health_Sci/Baqai_J_Health_Sci_2018_21_2_8_17.pdf.
65. Nkporbu, AKSP. Psychiatric comorbidity in essential hypertension. Updat Essent Hypertens. (2016):71–99. doi: 10.5772/64104
66. Bhatia, MMS. Prevalence of depression in people living with HIV/AIDS undergoing ART and factors associated with it. J Clin diagnostic Res. (2014) 8:4927. doi: 10.7860/JCDR/2014/7725.4927
67. Wang, Y, Duan, Z, Ma, Z, Mao, Y, Li, X, Wilson, A, et al. Epidemiology of mental health problems among patients with cancer during COVID-19 pandemic. Transl. Psychiatry. (2020) 10:263. doi: 10.1038/s41398-020-00950-y
68. Naser, MA. One aspect of coronavirus disease (COVID-19) outbreak in Iran: high anxiety among MS patients. Mult Scler Relat Disord. (2020) 41:102138. doi: 10.1016/j.msard.2020.102138
69. Zhang, SX, Batra, K, Xu, W, Liu, T, Dong, RK, Yin, A, et al. Mental disorder symptoms during the COVID-19 pandemic in Latin America - a systematic review and meta-analysis. Epidemiol Psychiatr Sci. (2022) 31:e23. doi: 10.1017/S2045796021000767
70. Varghese, A, George, G, Kondaguli, SV, Naser, AY, Khakha, DCA, and Chatterji, R. Decline in the mental health of nurses across the globe during COVID-19: A systematic review and meta-analysis. J Glob Heal. (2021) 11:05009. doi: 10.7189/jogh.11.05009
71. Al Maqbali, M, Al Sinani, M, and Al-Lenjawi, B. Prevalence of stress, depression, anxiety and sleep disturbance among nurses during the COVID-19 pandemic: A systematic review and metaanalysis. J Psychosom Res. (2021) 141:110343. doi: 10.1016/j.jpsychores.2020.110343
72. Pappa, S, Ntella, V, Giannakas, T, Giannakoulis, VG, Papoutsi, EA, and Katsaounou, P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav Immun. (2020) 88:901–7. doi: 10.1016/j.bbi.2020.05.026
73. Lin, YH, Chen, JS, Huang, PC, Lu, MY, Strong, C, Lin, CY, et al. Factors associated with insomnia and suicidal thoughts among outpatients, healthcare workers, and the general population in Taiwan during COVID-19 pandemic: a cross-sectional study. BMC Public Health [Internet]. (2022) 22:2135–11. Available from:. doi: 10.1186/s12889-022-14557-z
74. Dule, A, Abdu, Z, Hajure, M, Mohammedhussein, M, and Tariku, M. Insomnia among patients with chronic medical illness during COVID-19 pandemic: association with sociodemographic variables and social support. Sci J Public Heal. (2021) 9:204. doi: 10.11648/j.sjph.20210906.14
75. Mulyadi, M, Tonapa, SI, Luneto, S, Lin, WT, and Lee, BO. Prevalence of mental health problems and sleep disturbances in nursing students during the COVID-19 pandemic: A systematic review and meta-analysis. Nurs Educ Pr. (2021) 57:103228. doi: 10.1016/j.nepr.2021.103228
76. Liu, X, Zhu, M, Zhang, R, Zhang, J, Zhang, C, Liu, P, et al. Public mental health problems during COVID-19 pandemic: A large-scale meta-analysis of the evidence. Transl Psychiatry. (2021) 11:384. doi: 10.1038/s41398-021-01501-9
77. Nochaiwong, S, Ruengorn, C, Thavorn, K, Hutton, B, Awiphan, RP, C,, et al. Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: A systematic review and meta-analysis. Sci Rep. (2021) 11:10173. doi: 10.1038/s41598-021-89700-8
78. Necho, M, Birkie, M, Gelaye, H, Beyene, A, Belete, A, and Tsehay, M. Depression, anxiety symptoms, insomnia, and coping during the COVID-19 pandemic period among individuals living with disabilities in Ethiopia, 2020. PLoS One [Internet]. (2020) 15:1–18. Available from:. doi: 10.1371/journal.pone.0244530
79. Akturk Esen, S, Acikgoz, Y, Yildirim, M, Ucar, G, Ergun, Y, Dirikoc, M, et al. Anxiety, insomnia and pandemic awareness of cancer patients receiving chemotherapy during the covid-19 pandemic period. Int J Hematol Oncol. (2021) 31:161–9. doi: 10.4999/uhod.214677
80. Zulkifli, NA, Guan, NC, and Zainal, NZLT. Psychosocial factors associated with depression and anxiety during covid-19 pandemic among outpa-tients with depression. Anadolu Psikiyatr Dergisi. (2021) 22:185–93. doi: 10.5152/alphapsychiatry.2021.21107
81. Alimoradi, Z, Broström, A, Tsang, HW, Griffiths, MD, Haghayegh, S, Ohayon, MM, et al. Sleep problems during COVID-19 pandemic and its’ association to psychological distress: a systematic review and meta-analysis. EClini-calMedicine. (2021) 36:100916. doi: 10.1016/j.eclinm.2021.100916
82. Alkhathami, AD, Alamin, MA, Alqahtani, AM, Alsaeed, WY, Alkhathami, MA, and Al-dhafeeri, AH. Depression and anxiety among hypertensive and diabetic primary health care patients. Saudi Med J. (2017) 38:621–8. doi: 10.15537/smj.2017.6.17941
83. Hu, Q, Hu, X, Zheng, B, and Li, L. Mental health outcomes among civil servants aiding in coronavirus disease 2019 control. Front Public Heal. (2021) 9:1–10. doi: 10.3389/fpubh.2021.601791
84. Guan, S, Xiaerfuding, X, Ning, L, Lian, Y, Jiang, Y, Liu, J, et al. Effect of job strain on job burnout, mental fatigue and chronic diseases among civil servants in the Xinjiang Uygur autonomous region of China. Int J Env Res Public Heal. (2017) 14:4080872. doi: 10.3390/ijerph14080872
85. Virtanen, M, Ferrie, JE, Singh-Manoux, A, Shipley, MJ, Stansfeld, SA, Marmot, MG, et al. Long working hours and symptoms of anxiety and depression: a 5-year follow-up of the Whitehall II study. Psychol Med. (2011) 41:2485–94. doi: 10.1017/S0033291711000171
86. Aronsson, G, Theorell, T, Grape, T, Hammarström, A, Hogstedt, C, Marteinsdottir, I, et al. A systematic review including meta-analysis of work environment and burnout symptoms. BMC Public Health. (2017) 17:264. doi: 10.1186/s12889-017-4153-7
87. Lee, SM, Kang, WS, Cho, AR, and Kim, TPJ. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. (2018) 87:123–7. doi: 10.1016/j.comppsych.2018.10.003
88. Id, TH, Zhang, T, Cai, W, Song, X, Chen, A, Deng, G, et al. Social support and mental health among health care workers during coronavirus disease 2019 outbreak: A moderated mediation model. PLoS One [Internet]. (2020) 15:e0233831. doi: 10.1371/journal.pone.0233831
89. Mehari, EA, Kidane, RB, Areki, MF, Seid, AM, and Gelaye, AT. The magnitude and associated factors of anxiety and depression among non-communicable chronic disease patients during COVID-19 pandemic in a resource-limited setting, 101274. Clin Epidemiol Glob Heal [Internet]. (2023) 21. doi: 10.1016/j.cegh.2023.101274
90. Ilori, HTAO. Cross-sectional study of impact of social support on depression among type 2 diabetics in a secondary health care facility in Southwest Nigeria. JAMMR. (2019) 29:1–8. doi: 10.9734/jammr/2019/v29i230060
91. Xu, Q, and Li, SYL. Perceived social support and mental health for college students in mainland China: the mediating effects of self-concept. Psychol Heal Med. (2019) 24:595–604. doi: 10.1080/13548506.2018.1549744
92. Wang, F, Wang, S, Zong, QQ, Zhang, Q, Ng, CH, Ungvari, GS, et al. Prevalence of comorbid major depressive disorder in type 2 diabetes: a meta-analysis of comparative and epidemiological studies. Diabet Med. (2019) 36:961–9. doi: 10.1111/dme.14042
93. Messina, R, Iommi, M, Rucci, P, Reno, C, Fantini, MP, Lunghi, C, et al. Is it time to consider depression as a major complication of type 2 diabetes? Evidence from a large population-based cohort study. Acta Diabetol [Internet]. (2022) 59:95–104. Available from:. doi: 10.1007/s00592-021-01791-x
94. Khaledi, M, Haghighatdoost, F, and Feizi, AAA. The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol. (2019) 56:631–50. doi: 10.1007/s00592-019-01295-9
95. Sankar, P, Ahmed, WN, Mariam Koshy, V, and Jacob, RSS. Efects of COVID-19 lockdown on type 2 diabetes, lifestyle and psychosocial health: a hospital-based cross-sectional survey from South India. Diabetes Metab Syndr. (2020) 14:1815–9. doi: 10.1016/j.dsx.2020.09.005
96. Alessi, J, De, OGB, Franco, DW, Brino, B, Becker, AS, Knijnik, CP, et al. Mental health in the era of COVID - 19: prevalence of psychiatric disorders in a cohort of patients with type 1 and type 2 diabetes during the social distancing. Diabetol Metab Syndr [Internet]. (2020) 12:76–10. Available from:. doi: 10.1186/s13098-020-00584-6
97. Al-Sofani, ME, Albunyan, S, Alguwaihes, AM, Kalyani, RR, and Golden, SHAA. Determinants of mental health outcomes among people with and without diabetes during the COVID-19 outbreak in the Arab gulf region. J Diabetes. (2021) 13:339–52. doi: 10.1111/1753-0407.13149
98. Moradian, S, Teufel, M, Jahre, L, Musche, V, Fink, M, Dinse, H, et al. Mental health burden of patients with diabetes before and after the initial outbreak of COVID-19: predictors of mental health impairment. BMC Public Health. (2021) 21:2068. doi: 10.1186/s12889-021-12101-z
99. Hoogendoorn, CJ, Roy, JF, and Gonzalez, JS. Shared dysregulation of homeostatic brain-body pathways in depression and type 2 diabetes. Curr Diab Rep. (2017) 17:90. doi: 10.1007/s11892-017-0923-y
100. Berger, I, Werdermann, M, Bornstein, SR, and Steenblock, C. The adrenal gland in stress – adaptation on a cellular level. J Steroid Biochem Mol Biol [Internet]. (2019) 190:198–206. Available from:. doi: 10.1016/j.jsbmb.2019.04.006
101. Príncipe-Rodríguez, K, Strohl, KP, Hadziefendic, S, and Piña, IL. Sleep symptoms and clinical markers of illness in patients with heart failure. Sleep Breath. (2005) 9:127–33. doi: 10.1007/s11325-005-0023-0
102. Seko, Y, Yamamoto, E, Kato, T, Morimoto, T, Yaku, H, Inuzuka, Y, et al. Insomnia in patients with acute heart failure: from the KCHF registry. ESC Hear Fail. (2022) 9:2988–96. doi: 10.1002/ehf2.14025
103. Redeker, NS, Jeon, S, Muench, U, Campbell, D, and Walsleben, JRD. Insomnia symptoms and daytime function in stable heart failure. Sleep. (2010) 33:1210–6. doi: 10.1093/sleep/33.9.1210
104. Cox, RCOB. Sleep in a pandemic: implications of COVID-19 for sleep through the lens of the 3P model of insomnia. Am Psychol. (2021) 76:1159–71. doi: 10.1037/amp0000850
105. Garbarino, S, and Magnavita, N. Sleep problems are a strong predictor of stress-related metabolic changes in police officers. A prospective study PLoS One. (2019) 14:e0224259. doi: 10.1371/journal.pone.0224259
106. Hsiao, F, Chang, K, Kuo, W, Huang, C, Liu, Y, Lai, Y, et al. A longitudinal study of cortisol responses, sleep problems, and psychological well-being as the predictors of changes in depressive symptoms among breast cancer survivors. Psychoneuroendocrinology. (2013) 38:356–66. doi: 10.1016/j.psyneuen.2012.06.010
107. Greenberg, N, Docherty, M, and Gnanapragasam, SWS. Managing mental health challenges faced by healthcare workers during COVID-19 pandemic. BMJ. (2020) 368:1211. doi: 10.1136/bmj.m1211
108. Sayed, E, El, SS, Gomaa, S, Shokry, D, Kabil, A, and Eissa, A. Sleep in post - COVID - 19 recovery period and its impact on different domains of quality of life. Egypt J Neurol Psychiatry Neurosurg. (2021) 57:1–10. doi: 10.1186/s41983-021-00429-7
109. Farris, M, Leong, I, Abdullah, B, Yusof, HA, Shariff, NM, Hami, R, et al. Depression and anxiety in the Malaysian urban population and their association with demographic characteristics, quality of life, and the emergence of the COVID-19 pandemic. Curr Psychol. (2021) 40:6259–70. doi: 10.1007/s12144-021-01492-2
Keywords: common mental disorder, insomnia, COVID-19, NCDs, Ethiopia
Citation: Ayalew M, Deribe B, Hussen S, Defar S, Tesfaye E and Gedefaw A (2023) Insomnia and common mental disorder among patients with pre-existing chronic non-communicable diseases in southern Ethiopia: a survey during COVID-19 pandemic. Front. Psychiatry. 14:1142926. doi: 10.3389/fpsyt.2023.1142926
Edited by:
Runtang Meng, Hangzhou Normal University, ChinaReviewed by:
Rahim Badrfam, Alborz University of Medical Sciences, IranGiulia Avvenuti, IMT School for Advanced Studies Lucca, Italy
Copyright © 2023 Ayalew, Deribe, Hussen, Defar, Tesfaye and Gedefaw. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mohammed Ayalew, bWFtZWF5YWxlQGdtYWlsLmNvbQ==
 Mohammed Ayalew
Mohammed Ayalew Bedilu Deribe
Bedilu Deribe Siraj Hussen
Siraj Hussen Semira Defar3
Semira Defar3 Emnet Tesfaye
Emnet Tesfaye Abel Gedefaw
Abel Gedefaw