
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 13 March 2023
Sec. Anxiety and Stress Disorders
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1138361
This article is part of the Research Topic Assessing and Evaluating the Psychosocial Impact of the Covid-19 Pandemic on Anxiety and Stress: Perspectives from East Asia View all 14 articles
Background: Frontline healthcare workers (FHWs) experienced psychological stress and heavy workload during COVID-19 pandemic. This study examined the psychological symptoms and occupational burnout of FHWs in a fever clinic during different periods of the pandemic.
Methods: A cross-sectional survey of FHWs in the fever clinic of a tertiary hospital was carried out during both the outbreak period and regular period of COVID-19. Psychological measurement instruments including Generalized Anxiety Disorder 7-item, the 9-Question Patient Health Questionnaire, the Maslach Burnout Inventory-Human Service Survey, and the General Self-Efficacy Scale were used to evaluate anxiety, depression, burnout, and self-efficacy, respectively. The correlation between clinical variables was explored.
Results: A total of 162 participants were involved in this study, including 118 FHWs during the outbreak period (Group 1) and 44 FHWs during the regular period (Group 2). Anxiety symptoms were more prevalent in Group 2 (x2 = 27.477) while depressive symptoms were significantly more prevalent in Group 1 (x2 = 69.538). Burnout rate was higher in Group 2 (x2 = 29.526). Self-efficacy was higher in Group 1 (t = 3.194). Burnout was positively correlated with anxiety symptoms (r2 = 0.424) and negatively correlated with self-efficacy (r2 = −0.312).
Conclusion: Anxiety, depressive symptoms and burnout were prevalent in FHWs during different periods of the COVID-19 pandemic. There is a tendency to be less depressed, but more anxious and burned out over time, although the severity of the pandemic is decreasing. Self-efficacy may be an important factor in protecting FHWs from occupational burnout. Support and intervention plans for FHWs should be made at the institutional level.
Since December 2019, the COVID-19 pandemic has spread rapidly in China and around the world, becoming a public health emergency of global concern (1). Especially in the early days, the COVID-19 pandemic has put enormous pressure on governments and people around the world. The general public has had to cope with acute stress due to the uncertain source of disease, rapid transmission, and complexity of treatment (2). To date, the COVID-19 pandemic remains a major global public health issue and continues to pose a threat to all of humanity (3). Despite the increasing rate of vaccination against the virus, problems such as virus mutation, virus transmission and increased infection capacity remain prominent.
Every individual affected by the epidemic is facing great mental stress. WHO has identified addressing mental health needs as an essential part of the response to the COVID-19 pandemic (4), such as addressing public emotional reactions and stress among health workers. Medical staff were confronted with a variety of psychological stresses, including the risk of infection, high-intensity work stress, frustration at the lack of effective treatment, and loneliness in isolation (5). In the early days of the COVID-19 pandemic in China, a study of healthcare workers (HWs) in Wuhan (6) found that 50.4% of HWs exposed to the pandemic had clinically significant depressive symptoms. In another study of HWs in Beijing (7), 12.2% were depressed. Other studies around the world have found that during the first wave of the pandemic, HWs were under great mental stress and their mental health was significantly affected. In a study in Ethiopia (8), 58, 16.3, and 30.7% of HWs experienced moderate or severe stress, depression, and anxiety symptoms during the pandemic, and HWs’ poor coping was related to these psychological impairments, suggesting the need for psychological intervention for HWs. A study in Switzerland (9) found that 70% of HWs reported significant emotional stress and increased anxiety during the first wave of the pandemic, with a lack of protective equipment being an important source of stress. In the severely affected areas, the number of patients increased rapidly, far exceeding normal workload, and there was usually a serious shortage of personnel and supplies. The imbalance between resources and needs was first felt by frontline healthcare workers (FHWs). As the group most exposed to the disease, FHWs had a higher prevalence of anxiety, depression, and stress-related symptoms than the general public (10). Previous reviews of the psychological status of medical personnel in infectious disease outbreaks also found consistent evidence that gender, nurse occupation, and frontline working status are clear risk factors for psychological stress (11, 12), suggesting that psychological support for medical personnel needs to pay more attention to the female frontline nurse population.
Professional burnout was first described in 1975 by Freudenberger (13) on staff in a free medical clinic. Characteristics of occupational burnout in the context of physical and behavioral symptoms include increased anger, frustration, excessive rigidity and inflexibility in practice, and the appearance of depression characteristics. Those who are prone to burnout are often dedicated and committed to their profession. Burnout is not an acute condition but rather a chronic culmination of the effects of unsolvable, long-term work stress, professional responsibilities and the work environment. The three dimensions of burnout syndrome are emotional exhaustion, depersonalization or cynicism, and a decreased sense of personal accomplishment (13–15). Research indicates that burnout in healthcare professionals can lead to negative attitudes toward day-to-day work and a reduced focus on patients, which hinders medical safety and quality, and has serious consequences for the worker’s personal life (16–18). Professional burnout of FHWs during the COVID-19 pandemic has been reported in some studies. A study reported high rates of insomnia, burnout, and functional impairment among healthcare providers in Jordan during the first year of the COVID-19 pandemic (19). A study during the pandemic in Japan (20) found that more than 40% of nurses and more than 30% of radiological technicians and pharmacists met the criteria for occupational burnout. A study in Belgium (21) found that nearly half of HWs working on the front lines in the first wave of COVID-19 had significant occupational exhaustion, 28.8% had moderate or higher depression, 41.8% had moderate anxiety or higher, and 25.1% had moderate or higher stress, with increased workload and perceived support associated with these adverse outcomes. Researchers from Korea found that burnout had a direct effect on depression, anxiety, and physical and mental health in HWs (22). Combined, these factors can also pose a significant risk to the quality of patient management.
By 2023, many countries, including China, have adopted regular control measures to reduce the impact of the pandemic on the general public. However, FHWs were inevitably constantly faced with COVID-19. Recently, with more relaxed control measures adopted in China, the number of COVID-19 cases is expected to increase, possibly leading to more work-related stress in FHWs. To date, there have been few studies examining the current psychosomatic health status of FHWs during the regular period of the pandemic. In this study, we examine the psychological symptoms and occupational burnout of FHWs in a fever clinic during both the outbreak period and the regular period, in order to provide more evidence and help improve the psychosomatic intervention of FHWs during the pandemic.
This study was designed as a single-center cross-sectional study. All FHWs working in the fever clinic of a tertiary hospital in Beijing during the designated time period were considered eligible for this study, which included the COVID-19 outbreak period (January 2020 to April 2020, group 1) and the regular period (October 2021 to November 2021). Two researchers (JJ and HJ) contacted FHWs by telephone and invited them to participate. Of the 170 FHWs invited, 162 agreed to join the study. The enrollment of participants is shown in Figure 1. Participants were divided into two groups based on when they worked in the fever clinic, and there was no overlap in participants. The survey was conducted by telephone during the COVID-19 outbreak (Group 1) or via an online questionnaire during the regular period (Group 2). Demographic and psychological data were collected.
The study was reviewed and approved by the ethics committee of Peking Union Medical College Hospital (approval number S-K1045), which is located in Beijing, China. Oral informed consent was obtained from each participant.
Chinese validated versions of the following questionnaires were used to evaluate participants’ psychological symptoms: Generalized Anxiety Disorder 7-item (GAD-7) (23), Patient Health Questionnaire 9-item (PHQ-9) (24), Maslach Burnout Inventory-Human Service Survey (MBI-HSS) (25, 26), and General Self-Efficacy Scale (GSES) (27, 28).
GAD-7 consists of seven questions that assess the frequency of anxiety symptoms. Each question is scored from 0 (not at all) to 3 (almost every day), giving a total score of 0 to 21. Anxiety symptoms are defined as a GAD-7 score ≥ 5. A total score of 5–9, 10–14, and ≥ 15 are considered mild, moderate, and severe anxiety symptoms, respectively.
PHQ-9 consists of nine questions assessing the frequency of depressive symptoms. Each question is scored from 0 (not at all) to 3 (almost every day), summing up to a total score of 0 to 27. Depressive symptoms are defined as a PHQ-9 score ≥ 5. A total score of 5–9, 10–14, and ≥ 15 are considered mild, moderate, and severe depressive symptoms, respectively.
MBI-HSS is a 22-item instrument covering three aspects of burnout, emotional exhaustion (EE), depersonalization (DP), and personal accomplishment (PA). Each item has a 7-point Likert scale from “never” or 0 to “daily” or 6. We defined a 27 or higher EE score, a 10 or higher DP score, or a 33 or lower PA score as burnout for participants.
GSES is a 10-item self-rating scale that assesses the strength of an individual’s belief in his or her own ability to respond to novel or difficult situations and to cope with any associated obstacles or setbacks. For each item, there are four response choices from ‘not at all true’, which scores 1, to ‘exact true’, which scores 4. The scores for each of the 10 items are summed up to give a total score. The higher the score, the greater the individual’s generalized sense of self-efficacy.
All statistical analyses were performed using IBM SPSS Statistics 21.0.0.0. (IBM Corp., Armonk, NY, United States). Quantitative variables are described as mean ± standard deviation or median (interquartile range [IQR]) based on the normality of the variable. Categorical variables were described as frequencies (percentages). The Student’s t-test was used to compare the two groups for continuous variables. The Chi-square test was used to compare the distributions of categorical variables among the groups. The correlation between clinical variables was tested using Spearman’s correlation test. A value of p < 0.05 was considered statistically significant. This study was designed to search for clinical associations; therefore, only exploratory analyses are presented.
A total of 162 participants completed the questionnaire, including 60 (37.0%) doctors, 92 (56.8%) nurses and 10 (6.2%) laboratory or radiology technicians (Table 1). The majority (71.0%) were female. Participants had an average age of 31.1 ± 6.5 years. Group 1 (G1) consisted of 118 FHWs who worked in the fever clinic during the outbreak period, while Group 2 (G2) contained 44 FHWs during the regular period. There were no significant differences in age, sex, and occupation (physician, nurse, or technician) between G1 and G2.
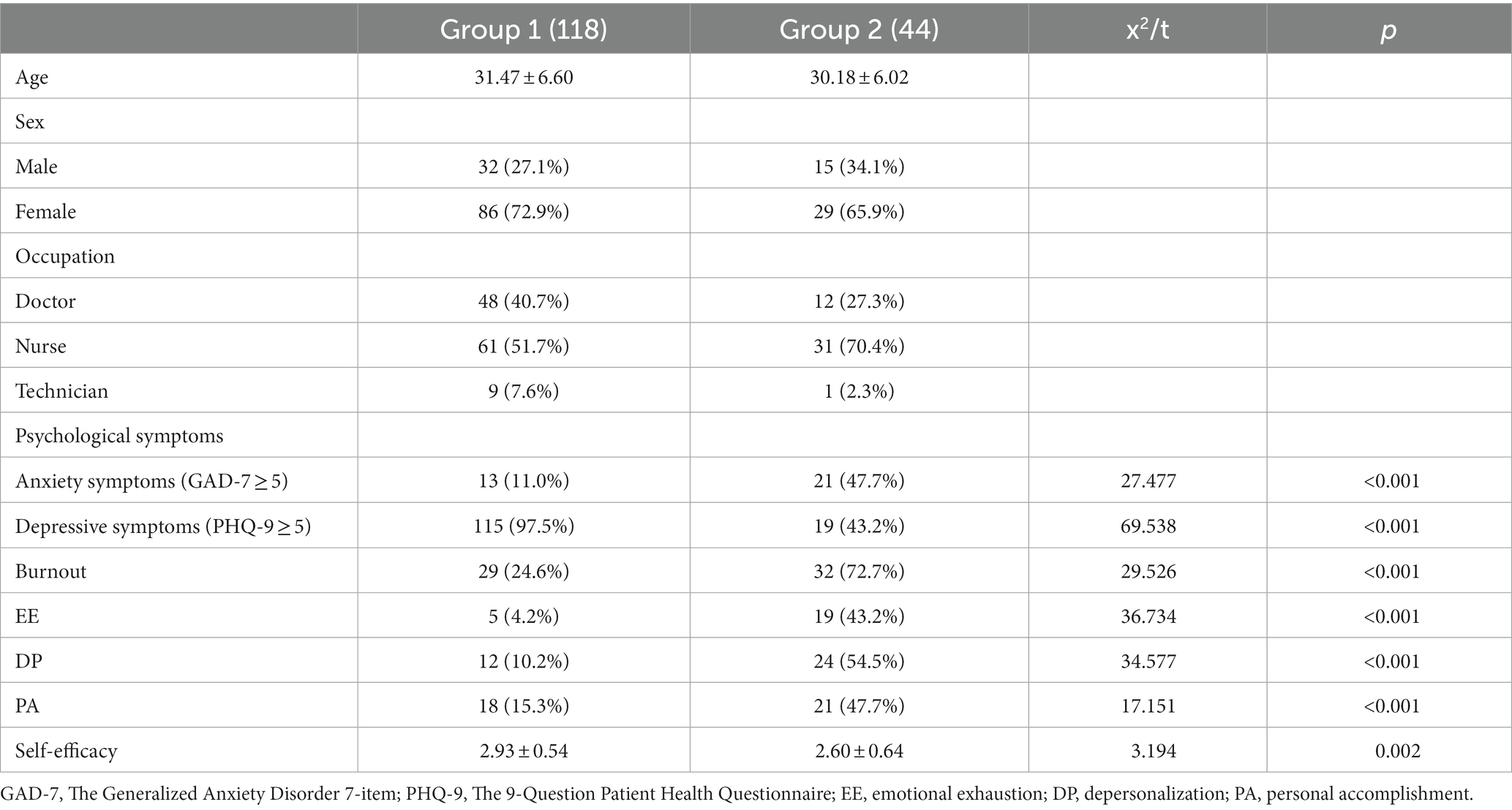
Table 1. Demographic information, psychological symptoms, burnout, and self-efficacy scores of participants.
Anxiety symptoms were more prevalent in G2 (11.0% vs. 47.7%, x2 = 27.477, p < 0.001) while depressive symptoms were significantly more prevalent in G1 (97.5% vs. 43.2%, x2 = 69.538, p < 0.001). In G1, the mean score of GAD-7 was 0 (IQR 0–2). Nine (7.6%) participants had mild anxiety symptoms (GAD-7 score 5–9) and four (3.4%) had moderate symptoms (GAD-7 score 10–14). G2 had a mean score of 4.5 (IQR 2–9) in GAD-7. There were 16 (36.4%) participants in G2 with mild anxiety symptoms and 5 (11.4%) participants with moderate anxiety symptoms. None of the participants in either group had severe anxiety symptoms (GAD-7 score > 15). With depressive symptoms, G1 and G2 had mean PHQ-9 scores of 9 (IQR 7–10) and 4 (IQR 1–7). In G1, the number of participants with mild (PHQ-9 score 5–9), moderate (PHQ-9 score 10–14), and severe (PHQ-9 score ≥ 15) depressive symptoms were 84 (71.2%), 25 (21.2%), and 6 (5.1%) respectively. In G2, 15 (34.1%) participants had mild depressive symptoms, 2 (4.5%) had moderate symptoms, and another 2 (4.5%) had severe symptoms.
Occupational burnout rate was significantly higher in G2 than in G1 (24.6% vs. 72.7%, x2 = 29.526, p < 0.001). The three factors of burnout, emotional exhaustion (4.2% vs. 43.2%), depersonalization (10.2% vs. 54.5%), and personal accomplishment (15.3% vs. 47.7%) all reflected a similar trend. Self-efficacy was significantly lower in G2 than in G1 (2.93 ± 0.54 vs. 2.60 ± 0.64, t = 3.194).
Depressive symptoms were positively correlated with age (r2 = 0.178, p = 0.025) and anxiety symptoms (r2 = 0.164, p = 0.039). Anxiety symptoms were positively associated with burnout (r2 = 0.424, p < 0.001) and all three aspects of burnout (Figure 2), depressive symptoms (r2 = 0.164, p = 0.039), and negatively associated with self-efficacy (r2 = −0.254, p = 0.001). Burnout and self-efficacy were negatively correlated (r2 = −0.312, p < 0.001, Figure 3), while both were not correlated with age, sex, or occupation. There was no significant correlation between depressive symptoms and burnout (r2 = −0.101, p = 0.211).
As a global public health crisis, COVID-19 has particularly affected healthcare workers (29). In the early days of the pandemic, many researchers in China focused on the psychological stress of medical personnel and identified several possible contributing factors. Some suggested that during the outbreak, shortages of personal protective equipment (PPE), long working hours, and overwork were common factors affecting the stress levels of healthcare workers (3). In our colleagues’ previous qualitative study (30), FHWs commonly reported nervousness and worrying symptoms, as well as insomnia and physical discomfort. Similar findings were found in several studies (31–34). In a systematic review and meta-analysis of the psychological impact of COVID-19 on Chinese healthcare workers in early 2020 (12), pooled prevalence rates of anxiety, depression, and sleep disturbances were 17% (13–21%), 15% (13–16%), and 15% (7–23%), respectively. Tong et al. (35) reported the prevalence of anxiety and depression in FHWs during the outbreak period and regular period was 1.6 and 13.1% and 6.1 and 8.1%, respectively. In our study, the trend of “less depressed, more anxious” from outbreak to regular period was similar to Tong et al.’s findings, although the prevalence rates of both symptoms were higher in our study. The difference may result from different clinical settings and questionnaires used to evaluate anxiety and depressive symptoms.
Occupational burnout among medical personnel is often higher than in the general population (36). Since the start of the COVID-19 pandemic, studies of burnout among front-line and non-front-line HWs have shown a high burnout rate (20, 37–41), and these HWs often have more emotional distress. Factors related to HWs’ burnout include female sex, less work experience, nurse occupation, and work location (37–41). Using the Effort-Reward Imbalance theory to explore the relationships between burnout and emotional distress, Zhang et al. (42) found that effort and over-commitment were positively associated with depression and anxiety, reward was negatively associated with depression and anxiety, and buffered the harmful effect of effort/over-commitment on depression and anxiety. In our study, FHWs during the outbreak period had lower burnout rates and higher self-efficacy than their colleagues during the regular period. Considering the correlation between burnout and self-efficacy, it is possible that self-efficacy protects FHWs from occupational burnout.
To the general public, COVID-19 has become a constant stressor in the background. One segment of the population that is severely affected by this pandemic is the FHWs. Morioka et al. (43) proposed that some HWs continue to suffer from prolonged psychological distress during the regular period of the COVID-19 pandemic, which may lead to emotional symptoms and somatic discomfort. Risk factors for this include nurse occupation, underlying physical condition, and being prejudiced against due to involvement in COVID-19 healthcare. According to a review of retrospective studies on SARS and MERS (44), an event that occurs over a limited period—however severe—is less traumatic than chronic and prolonged stress over time with no end in sight. Professional identity as a caregiver also makes HWs vulnerable to stress. Yang et al. (45) reported 2,878 out of 15,531 (18.5%) FHWs experienced workplace violence during the outbreak period.
Occupational burnout among HWs is an important issue because it impairs medical quality and safety. Our study revealed the correlation between burnout and anxiety, the latter commonly present under chronic stress, which was found to be correlated with burnout as well (39). Depression and burnout have been considered as synonymous in some literature (46, 47), while others argue that they are categorically distinct (48, 49). We did not find significant correlations between depressive symptoms and burnout in the participants. A recent meta-analysis (48) reported only moderate correlations between scores on burnout and depression measures. One possible explanation for the lack of correlation may be that the tool used to measure burnout in many studies, including this study, is MBI-HSS, which does not include any depressive symptoms (25, 26). Burnout and chronic stress are intertwined and form a vicious circle. Given the increasingly relaxed pandemic control measures and the increasing number of infected patients, FHWs are expected to embrace a wider range and greater intensity of stress. In future studies, follow-up studies on the psychosomatic status and occupational burnout trajectories of FHWs should be continued.
Quoting Dow et al. (50), a crisis – including the COVID-19 pandemic – should never be wasted. Our findings, like others, may provide evidence for tailoring support and intervention plans for FHWs. At the institutional level, there is a need to strengthen the protection and support of FHWs during the pandemic, but proactive prevention against possible psychological distress and occupational burnout should be equally or even more important. The role and function of each individual and the boundaries between roles should be clearly defined (17), and the rotation work pattern should be mandatory to ensure sufficient “off time,” “worry-free time” or “self-care time” for each individual (51). In the routine training of HWs, attention should be paid to reserving personnel in case of special periods such as COVID-19 to be mobilized at any time. At the same time, if there is a shortage of PPEs, priority should be given to ensuring supply at the frontline (9). Psychologically, FHWs should be provided with the necessary psychological support at the individual level, such as counseling and support groups (8, 9, 21). In daily work, enhancing the psychological resilience of HWs also helps to cope with professional burnout (51). Our colleagues have previously reported that in some FHWs, experience at the frontline has led to a more positive assessment of one’s self, and the belief that occupation and life are purposeful and meaningful (30). This may be a sign of good psychological resilience, which affects one’s perception of setbacks (52). It is also important to fully recognize and reward FHWs for their dedication. At the level of government management, short-term responses to the pandemic crisis need to address gaps in the distribution of medical resources in different regions and appropriately increase support for areas lacking medical resources. Since the outbreak of COVID-19, the Chinese Health Commission has organized the transfer of HWs from areas with more medical resources to less developed areas (53). It is important to note that while this measure directly relieved local HW pressures, transferred FHWs faced more complex stressors, such as adaptation needs (54). Long-term measures should focus on further strengthening medical education and enhancing the flexibility and adaptability of HWs.
Our research has some limitations. First, the study was designed to be single-centered, which may limit its generalizability. Second, although we were able to include participants from different periods of the COVID-19 pandemic, we did not follow the same group to see the trend in their emotional distress over time. However, this limitation was compensated for by the fact that the two groups matched in demographic characteristics. Third, we were unable to obtain more sociodemographic information from participants, which may be confounding factors for emotional distress and occupational burnout. Finally, similar to most COVID-19 studies, our study used self-report questionnaires about psychological symptoms rather than diagnostic interviews for mental disorders, which may be affected by recall bias. In future studies, it is recommended to assess factors and coping mechanisms for burnout and psychological symptoms among HWs. It is also important to compare research findings from different cultures and socioeconomic backgrounds.
In conclusion, anxiety, depressive symptoms and burnout are prevalent in FHWs during both the outbreak period and the regular period of COVID-19. There is a tendency to be less depressed, but more anxious and burned out over time, although the severity of the pandemic is decreasing. Self-efficacy may be an important factor in protecting FHWs from occupational burnout. During the regular period of COVID-19, more attention and active interventions are still needed for the mental health and occupational burnout of healthcare workers.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Ethics Committee of Peking Union Medical College Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
WG, JC, XH, and JW conceived and designed the study. WG, JJ, JH, and YD collected the data. WG performed the statistical analyses. WG and JC wrote the first draft of the manuscript draft. All authors had access to the data, played a role in writing the manuscript, and commented on the posterior versions and approved the final manuscript.
This study was supported by the Capital Funds for Health Improvement and Research (project number: CFH 2022–2-4012) and the STI2030-Major Projects (project number: 2021ZD0202001).
The authors would like to thank our colleagues at the fever clinic for their diligent work and participation in this study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1.Wang, C, Horby, PW, Hayden, FG, and Gao, GF. A novel coronavirus outbreak of global health concern. Lancet. (2020) 395:470–3. doi: 10.1016/S0140-6736(20)30185-9
2.Davidson, JR, and McFarlane, AC. The extent and impact of mental health problems after disaster. J Clin Psychiatry. (2006) 67:9–14.
3.World Health Organization. (2020). Overview of public health and social measures in the context of COVID-19 (interim guidance). Available at: https://www.who.int/publications/i/item/overview-of-public-health-and-social-measures-in-the-context-of-covid-19
4.Adhanom, GT. Addressing mental health needs: an integral part of COVID-19 response. World Psychiatry. (2020) 19:129–30. doi: 10.1002/wps.20768
5.Halms, T, Strasser, M, Kunz, M, and Hasan, A. How to reduce mental health burden in health care workers during COVID-19?-a scoping review of guideline recommendations. Front Psych. (2022) 12:770193. doi: 10.3389/fpsyt.2021.770193
6.Lai, J, Ma, S, Wang, Y, Cai, Z, Hu, J, Wei, N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
7.Zhang, WR, Wang, K, Yin, L, Zhao, WF, Xue, Q, Peng, M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. (2020) 89:242–50. doi: 10.1159/000507639
8.Jemal, K, Deriba, BS, and Geleta, TA. Psychological distress, early behavioral response, and perception toward the COVID-19 pandemic among health care workers in North Shoa Zone. Oromiya Region Front Psychiatry. (2021) 12:628898. doi: 10.3389/fpsyt.2021.628898
9.Riguzzi, M, and Gashi, S. Lessons from the first wave of COVID-19: work-related consequences, clinical knowledge, emotional distress, and safety-conscious behavior in healthcare workers in Switzerland. Front Psychol. (2021) 12:628033. doi: 10.3389/fpsyg.2021.628033
10.Hu, N, Deng, H, Yang, H, Wang, C, Cui, Y, Chen, J, et al. The pooled prevalence of the mental problems of Chinese medical staff during the COVID-19 outbreak: a meta-analysis. J Affect Disord. (2022) 303:323–30. doi: 10.1016/j.jad.2022.02.045
11.Sirois, FM, and Owens, J. Factors associated with psychological distress in health-care workers during an infectious disease outbreak: a rapid systematic review of the evidence. Front Psych. (2021) 11:589545. doi: 10.3389/fpsyt.2020.589545
12.Xiong, N, Fritzsche, K, Pan, Y, Löhlein, J, and Leonhart, R. The psychological impact of COVID-19 on Chinese healthcare workers: a systematic review and meta-analysis. Soc Psychiatry Psychiatr Epidemiol. (2022) 57:1515–29. doi: 10.1007/s00127-022-02264-4
13.Freudenberger, HJ. Staff Burn-Out. J Soc Issues. (1974) 30:159–65. doi: 10.1111/j.1540-4560.1974.tb00706.x
14.Dyrbye, LN, Varkey, P, Boone, SL, Satele, DV, Sloan, JA, and Shanafelt, TD. Physician satisfaction and burnout at different career stages. Mayo Clin Proc. (2013) 88:1358–67. doi: 10.1016/j.mayocp.2013.07.016
15.Bridgeman, PJ, Bridgeman, MB, and Barone, J. Burnout syndrome among healthcare professionals. Am J Health Syst Pharm. (2018) 75:147–52. doi: 10.2146/ajhp170460
16.Humphries, N, Morgan, K, Conry, MC, McGowan, Y, Montgomery, A, and McGee, H. Quality of care and health professional burnout: narrative literature review. Int J Health Care Qual Assur. (2014) 27:293–307. doi: 10.1108/IJHCQA-08-2012-0087
17.Maresca, G, Corallo, F, Catanese, G, Formica, C, and Lo Buono, V. Coping strategies of healthcare professionals with burnout syndrome: a systematic review. Medicina. (2022) 58:327. doi: 10.3390/medicina58020327
18.Aust, F, Beneke, T, Peifer, C, and Wekenborg, M. The relationship between flow experience and burnout symptoms: a systematic review. Int J Environ Res Public Health. (2022) 19:3865. doi: 10.3390/ijerph19073865
19.Yassin, A, Al-Mistarehi, AH, Soudah, O, Karasneh, R, Al-Azzam, S, Qarqash, AA, et al. Trends of prevalence estimates and risk factors of depressive symptoms among healthcare workers over one year of the COVID-19 pandemic. Clin Pract Epidemiol Ment Heal. (2022) 18:e174501792206160. doi: 10.2174/17450179-v18-e2206160
20.Matsuo, T, Kobayashi, D, Taki, F, Sakamoto, F, Uehara, Y, Mori, N, et al. Prevalence of health care worker burnout during the coronavirus disease 2019 (COVID-19) pandemic in Japan. JAMA Netw Open. (2020) 3:e2017271. doi: 10.1001/jamanetworkopen.2020.17271
21.Tiete, J, Guatteri, M, Lachaux, A, Matossian, A, Hougardy, JM, Loas, G, et al. Mental health outcomes in healthcare workers in COVID-19 and non-COVID-19 care units: a cross-sectional survey in Belgium. Front Psychol. (2021) 11:612241. doi: 10.3389/fpsyg.2020.612241
22.Lee, YJ, Yun, J, and Kim, T. Stress- and work-related burnout in frontline health-care professionals during the COVID-19 pandemic. Disaster Med Public Health Prep. (2021) 17:e38. doi: 10.1017/dmp.2021.279
23.He, XY, Li, CB, Qian, J, Cui, HS, and Wu, WY. Reliability and validity of a generalized anxiety disorder scale in general hospital outpatients (in Chinese). Shanghai Arch Psychiatry. (2010) 22:200–3. doi: 10.3969/j.issn.1002-0829.2010.04.002
24.Zhang, YL, Liang, W, Chen, ZM, Zhang, HM, Zhang, JH, Weng, XQ, et al. Validity and reliability of patient health questionnaire-9 and patient health questionnaire-2 to screen for depression among college students in China. Asia Pac Psychiatry. (2013) 5:268–75. doi: 10.1111/appy.12103
25.Doulougeri, K, Georganta, K, and Montgomery, A. "Diagnosing" burnout among healthcare professionals: Can we find consensus? Cogent Med. (2016) 3:1. doi: 10.1080/2331205X.2016.1237605
26.Lee, HF, Chien, TW, and Yen, M. Examining factor structure of Maslach burnout inventory among nurses in Taiwan. J Nurs Manag. (2013) 21:648–56. doi: 10.1111/j.1365-2834.2012.01427.x
27.Luszczynska, A, Scholz, U, and Schwarzer, R. The general self-efficacy scale: multicultural validation studies. J Psychol. (2005) 139:439–57. doi: 10.3200/JRLP.139.5.439-457
28.Wang, C, Hu, Z, and Liu, Y. Evidences for reliability and validity of the Chinese version of general self-efficacy scale (in Chinese). Chinese J. Appl. Psychol. (2001) 7:37–40. doi: 10.3969/j.issn.1006-6020.2001.01.007
29.Suresh, R, Alam, A, and Karkossa, Z. Using peer support to strengthen mental health during the COVID-19 pandemic: a review. Front. Psychiatry. (2021) 12:714181. doi: 10.3389/fpsyt.2021.714181
30.Duan, YP, Cao, JY, Wei, J, Jiang, J, Zhao, XH, Geng, WQ, et al. Basic needs of the first batch of medical staff in the fever Clinic of Peking Union Medical College Hospital during coronavirus disease 2019 outbreak: a qualitative study (in Chinese). Med J Pek Union Med Coll Hosp. (2021) 12:54–8. doi: 10.3969/j.issn.1674-9081.2021.01.001
31.Xie, J, Liu, Q, Jiang, X, Manandhar, U, Zhu, Z, Li, Y, et al. Psychological health issues of medical staff during the COVID-19 outbreak. Front Psychiatry. (2021) 12:611223. doi: 10.3389/fpsyt.2021.611223
32.Xie, C, Zhang, J, Ping, J, Li, X, Lv, Y, and Liao, L. Prevalence and influencing factors of psychological distress among nurses in Sichuan, China during the COVID-19 outbreak: A cross-sectional study. Front Psychiatry. (2022) 13:854264. doi: 10.3389/fpsyt.2022.854264
33.Huang, D, Shu, W, Li, M, Ma, J, Li, Z, Gong, J, et al. Social media survey and web posting assessment of the COVID-19 response in China: health worker attitudes toward preparedness and personal protective equipment shortages. Open Forum Infect Dis. (2020) 7:ofaa400. doi: 10.1093/ofid/ofaa400
34.Yusefi, AR, Faryabi, R, Bordbar, S, Daneshi, S, and Nikmanesh, P. Job burnout status and its relationship with resilience level of healthcare workers during COVID-19 pandemic: A case of southern Iran. Iran J Health Sci. (2021) 9:1–11. doi: 10.18502/jhs.v9i3.7305
35.Tong, Y, Zhang, Q, Wang, X, du, Y, Chang, D, Cui, Y, et al. Dynamic changes in mental health status related to the COVID-19 pandemic among health care workers and inpatients in China. Front Psychiatry. (2022) 13:956068. doi: 10.3389/fpsyt.2022.956068
36.Matsuo, T, Yoshioka, T, Okubo, R, Nagasaki, K, and Tabuchi, T. Burnout and its associated factors among healthcare workers and the general working population in Japan during the COVID-19 pandemic: a nationwide cross-sectional internet-based study. BMJ Open. (2022) 12:e64716:e064716. doi: 10.1136/bmjopen-2022-064716
37.Peng, SY, Deng, XF, Yang, H, Lu, L, and Zhang, JH. Study on occupational burnout status and its influencing factors in front-line medical staff of anti-COVID-19 in Wuhan (in Chinese). J Psychiatry. (2020) 33:169–72. doi: 10.3969/j.issn.2095-9346.2020.03.003
38.Pan, S, Qian, W, Yang, Y, Zhang, MX, Hu, XM, Chen, HX, et al. Evaluation of burnout among stay-behind healthcare workers during the current Omicron wave of COVID-19 in Taizhou, China. Front Psychiatry. (2022) 13:1022881. doi: 10.3389/fpsyt.2022.1022881
39.Noh, E, Park, Y, Chai, YJ, Kim, HJ, and Kim, E. Frontline nurses’ burnout and its associated factors during the COVID-19 pandemic in South Korea. Appl Nurs Res. (2022) 67:151622. doi: 10.1016/j.apnr.2022.151622
40.Nishimura, Y, Miyoshi, T, Hagiya, H, Kosaki, Y, and Otsuka, F. Burnout of healthcare workers amid the COVID-19 pandemic: a Japanese cross-sectional survey. Int J Environ Res Public Health. (2021) 18:2434. doi: 10.3390/ijerph18052434
41.Yassin, A, Al-Mistarehi, A-H, El-Salem, K, Karasneh, RA, Al-Azzam, S, Qarqash, AA, et al. Prevalence estimates and risk factors of anxiety among healthcare Workers in Jordan over one year of the COVID-19 pandemic: a cross-sectional study. Int J Environ Res Public Health. (2022) 19:2615. doi: 10.3390/ijerph19052615
42.Zhang, J, Wang, Y, Xu, J, You, H, Li, Y, Liang, Y, et al. Prevalence of mental health problems and associated factors among front-line public health workers during the COVID-19 pandemic in China: an effort–reward imbalance model-informed study. BMC Psychol. (2021) 9:55. doi: 10.1186/s40359-021-00563-0
43.Morioka, S, Tan, BH, Kikuchi, H, Asai, Y, Suzuki, T, Ashida, S, et al. Factors associated with prolonged psychological distress among nurses and physicians engaged in COVID-19 patient care in Singapore and Japan. Front Psych. (2022) 13:781796. doi: 10.3389/fpsyt.2022.781796
44.Saladino, V, Auriemma, V, and Campinoti, V. Healthcare professionals, post-traumatic stress disorder, and COVID-19: a review of the literature. Front Psychiatry. (2022) 12:795221. doi: 10.3389/fpsyt.2021.795221
45.Yang, Y, Li, Y, An, Y, Zhao, YJ, Zhang, L, Cheung, T, et al. Workplace violence against Chinese frontline clinicians during the COVID-19 pandemic and its associations with demographic and clinical characteristics and quality of life: a structural equation modeling investigation. Front Psych. (2021) 12:649989. doi: 10.3389/fpsyt.2021.649989
46.Bianchi, R, Boffy, C, Hingray, C, Truchot, D, and Laurent, E. Comparative symptomatology of burnout and depression. J Health Psychol. (2013) 18:782–7. doi: 10.1177/1359105313481079
47.Ahola, K, Hakanen, J, Perhoniemi, R, and Mutanen, P. Relationship between burnout and depressive symptoms: a study using the person-centred approach. Burn Res. (2014) 1:29–37. doi: 10.1016/j.burn.2014.03.003
48.Koutsimani, P, Montgomery, A, and Georganta, K. The relationship between burnout, depression, and anxiety: a systematic review and meta-analysis. Front Psychol. (2019) 10:284. doi: 10.3389/fpsyg.2019.00284
49.Parker, G, and Tavella, G. Distinguishing burnout from clinical depression: A theoretical differentiation template. J Affect Disord. (2021) 281:168–73. doi: 10.1016/j.jad.2020.12.022
50.Dow, AW, DiPiro, JT, Giddens, J, Buckley, P, and Santen, SA. Emerging from the COVID-19 crisis with a stronger health care workforce. Acad Med. (2020) 95:1823–6. doi: 10.1097/ACM.0000000000003656
51.Sullivan, EE, McKinstry, D, Adamson, J, Hunt, L, Phillips, RS, and Linzer, M. Burnout among Missouri primary care clinicians in 2021: roadmap for recovery? Mo Med. (2022) 119:397–400.
52.Fava, GA, and Guidi, J. The pursuit of euthymia. World Psychiatry. (2020) 19:40–50. doi: 10.1002/wps.20698
53.National Health Commission of the People’s Republic of China. (2020). Notice on strengthening medical treatment for severe cases of new coronavirus pneumonia. Available at: http://www.nhc.gov.cn/xcs/zhengcwj/202001/9fbefc9a5fe747e98ea5baeedfb68158.shtml (published Jan 23, 2020, accessed Jan 20, 2023).
Keywords: COVID-19, burnout, healthcare workers, China, anxiety, depression
Citation: Geng W, Cao J, Hong X, Jiang J, Hu J, Duan Y and Wei J (2023) Emotional distress and burnout at a fever clinic in China: Comparison between different periods of COVID-19. Front. Psychiatry. 14:1138361. doi: 10.3389/fpsyt.2023.1138361
Received: 05 January 2023; Accepted: 20 February 2023;
Published: 13 March 2023.
Edited by:
Baojuan Ye, Jiangxi Normal University, ChinaReviewed by:
Rikinkumar S. Patel, Duke University Medical Center, United StatesCopyright © 2023 Geng, Cao, Hong, Jiang, Hu, Duan and Wei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinya Cao, Y2FvamlueWFAcHVtY2guY24=; Jing Wei, d2VpamluZ0BwdW1jaC5jbg==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.