
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry, 25 May 2023
Sec. Addictive Disorders
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1134683
This article is part of the Research TopicAlcohol and Drug Use in Low- and Middle-Income CountriesView all 7 articles
Introduction: Opioid agonist treatments (OATs) with methadone and buprenorphine are known to be effective treatments for people with opioid use disorder (OUD). However, concomitant use of other substances such as alcohol can negatively affect OAT outcomes. This study aimed to determine the prevalence of alcohol use among clients of OAT centers in the Golestan province in the northern part of Iran.
Materials and methods: This is a secondary analysis of a sample of 706 clients who were receiving OATs from certified OAT centers in Golestan province in 2015. They had been on OATs for at least 1 month and were randomly selected for the study. Data were collected via interviews with selected OAT clients. The main indicators studied in the present study were lifetime history of alcohol consumption, alcohol consumption during last month, lifetime history of excessive alcohol use on one occasion, and years of regular alcohol consumption.
Results: The prevalence of lifetime history of alcohol consumption was estimated at 39.2%. Prevalence of alcohol consumption during last month and lifetime history of excessive alcohol use on one occasion was 6.9 and 18.8%, respectively.
Conclusion: Despite a total ban on alcohol consumption in Iran, a sub-sample of participants admitted past-month alcohol use concurrent with their OATs. The estimated past-month prevalence of alcohol use was lower than the reported prevalence in countries where the production, distribution, and consumption of alcohol are legal.
Opioid agonist treatments (OATs) with long-acting opioid medications including methadone and buprenorphine are safe and effective treatments for people with moderate to severe opioid use disorder (OUD) (1). The ultimate advantage of using OATs could be reducing death, particularly from overdoes, and criminal activities (2–4). It is estimated that one-third of those on OATs have concurrent alcohol use disorder (AUD) or harmful drinking (5, 6). This is based on studies conducted in different parts of the world and in different treatment settings (7–9). Although, alcohol use does not appear to change with OAT, concomitant alcohol use with opioid agonist medications is often problematic and can lead to a range of adverse consequences including hepatotoxicity, cirrhosis, intoxication, and overdose (10–14). In addition, unhealthy alcohol consumption has been identified as a risk factor for non-adherence to OAT, problems in social life, criminal activities, and illicit drug use (5, 6, 15–17). Moreover, drinking alcohol may exacerbate mental health problems of those receiving OAT (18, 19).
Alcohol use disorder and its physical and psychological effects should be considered when providing OAT services to people with OUD (20). International studies have shown that screening and brief motivational intervention, could effectively reduce hazardous or harmful drinking and improve treatment outcomes among OAT clients (21). Therefore, professional staff working in OAT centers can play a crucial role in early detection and management of problematic alcohol use in this population (22).
International studies have shown the prevalence of alcohol use up to 30% among people receiving OATs, but this data is mainly from countries where drinking alcohol is legal and culturally acceptable (5). However, the prevalence could be quite different in Muslim-majority countries such as Iran, Afghanistan, Pakistan, and Saudi Arabia, where there is complete ban on the production, sale, and consumption of alcohol (23). Results from a recent study in Iran show the overall pooled prevalence of lifetime alcohol consumption among the general population in 31% (24).
To answer this question, we analyzed data from previous research on the simultaneous use of amphetamines and opioids among clients of OAT centers to estimate the prevalence of alcohol consumption among these clients (15). Therefore, this is a secondary analysis on a random sample of 706 clients attending in OAT centers in Golestan province.
The initial study was a cross-sectional study on a random sample of 706 clients referred to outpatient OAT centers in Golestan province, in the northern part of Iran. The detailed methods of the study were reported elsewhere (15).
In brief, the participants were selected by two-stage cluster sampling with two strata based on the location of the centers (Gorgan and the other cities of Golestan province). In the first stage, 25 centers were randomly selected from all 150 centers in Golestan province. Then, in the second stage, 30 clients of the selected centers were recruited through convenience sampling. Inclusion criteria were at least 18 years old at the time of the interview, receiving OAT with methadone, buprenorphine, or opium tincture for at least 1 month prior to the interview, and providing informed consent to participate in the study.
A questionnaire designed by researchers was used to collect the data (15). Face-to-face interviews were conducted to collect information on drug and alcohol use history (i.e., lifetime history of alcohol consumption, alcohol consumption during the last month, lifetime history of excessive alcohol use on one occasion, and years of regular alcohol consumption). Excessive alcohol consumption was defined as consumption of 6 standard drinks of alcohol or more containing 10 grams or 12.7 ml of pure alcohol on one occasion. Years of regular alcohol consumption was defined as number of years in which the participants were drinking three or more times in a week. Age, gender, employment status, monthly income, level of education, type of OAT medication (methadone, buprenorphine, or opium tincture), duration of OAT, and history of imprisonment were among the variables collected in the initial study. These variables were used as possible factors related to alcohol consumption. To confirm the participants’ response to the recent drug use, urine samples were collected from the participants to identify their status regarding recent consumption of morphine, tramadol, amphetamine, methamphetamine, cannabis (THC), and benzodiazepines. Information about alcohol consumption was based on self-report.
The analyses of this study were performed by survey data analysis commands using STATA software (version 10). Descriptive statistics were calculated for demographic characteristics, type of OAT, and imprisonment history of the study participants. Results for the prevalence of alcohol consumption were presented by point estimate and 95% confidence interval. To examine possible correlated factors, a multiple logistic regression model was used and the adjusted odds ratio and 95% confidence interval of the estimates were calculated. Sex, age, education, type of OAT, treatment duration, and history of imprisonment were included in the model using the forward method. All data analysis were two-tailed, and the results with a p-value of < 0.05 was considered to be statistically significant.
Participation in the study was completely voluntary and the participants provided written informed consent to participate in this study. The study protocol and questionnaire were approved by the ethics committee of the Golestan University of Medical Sciences GOUMS (code: IR.GOUMS.REC.1394.112).
A sample of 706 OAT clients was include in the study. Table 1 shows demographic characteristics, socioeconomic status, type and duration of OAT, and history of imprisonment of the study participants. The majority of participants were male (93.6%) and most of them were on methadone maintenance treatment (89.2%). The prevalence of lifetime alcohol consumption was 39.2% (95% CI, 29.5–48.9). Alcohol consumption during last month and lifetime history of excessive alcohol use on one occasion were 6.9% (95% CI, 3.8–10.0) and 18.8% (95% CI, 12.2–25.4), respectively. Average number of days of alcohol consumption in people who had consumed alcohol in the past month was 1 day (0.94: 95% CI, 0.44–1.4). Only 8 of the 45 female participants (18%) reported lifetime drinking. None of them had consumed alcohol in the 30 days prior to the interview. The mean age of alcohol consumption initiation was 20.8 years (95% CI, 19.7–21.9) and the average years of regular alcohol consumption was 5 years among those who admitted lifetime alcohol use (95% CI, 4–6).
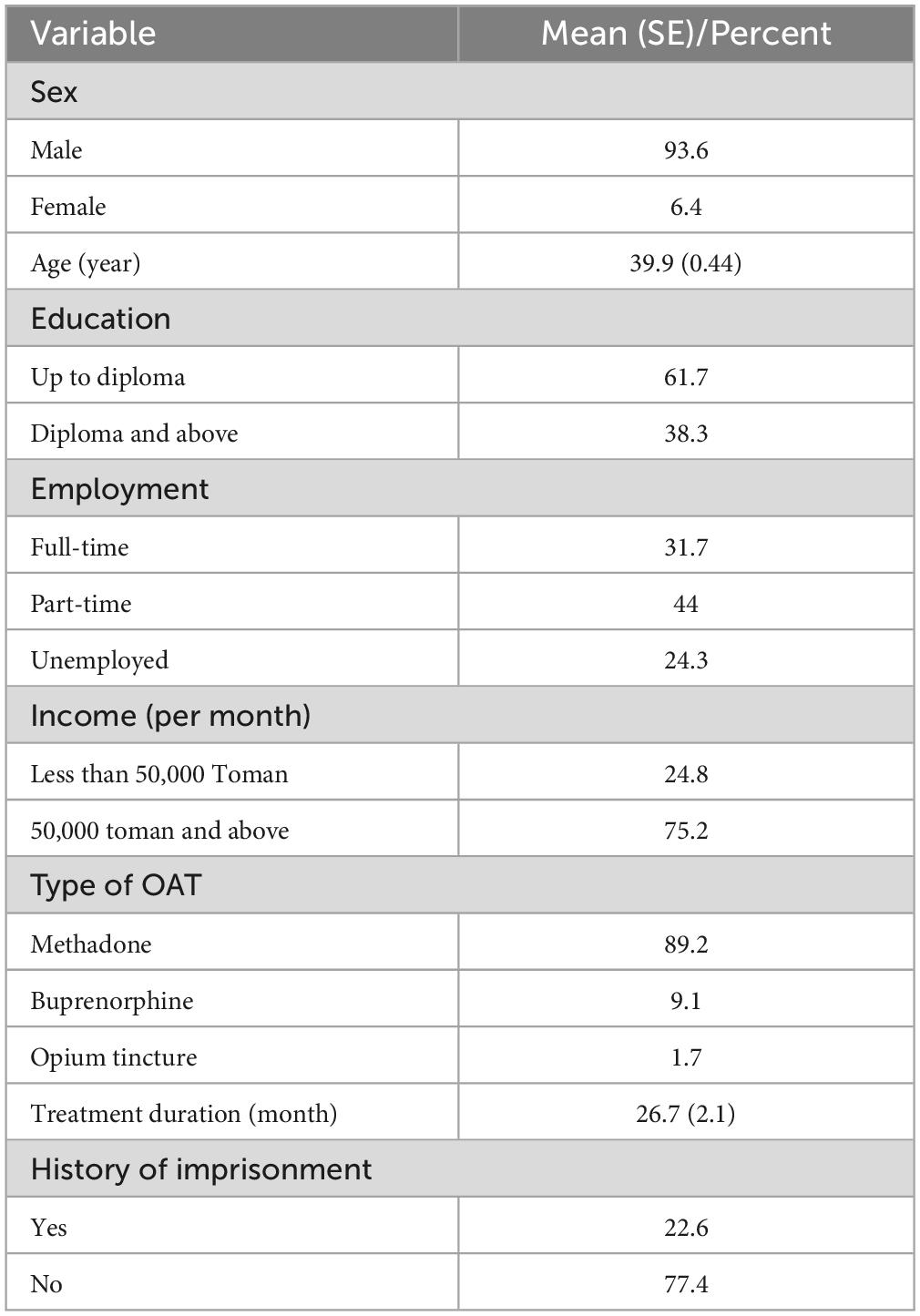
Table 1. Demographic characteristics, type of OAT (opioid agonist treatment), and imprisonment history of the study participants (706 people; 661 men and 45 women).
Prevalence of lifetime history of alcohol consumption for participants receiving methadone, buprenorphine, and opium tincture treatments were 41.9% (95% CI, 33.1–50.8), 17.2% (95% CI, 3.3–31.1), and 40% (95% CI, 18.5–61.4), respectively. It seems that there is no difference between methadone and buprenorphine groups in terms of lifetime history of alcohol consumption, alcohol consumption during last month, and lifetime history of excessive alcohol use in one occasion (Table 2).
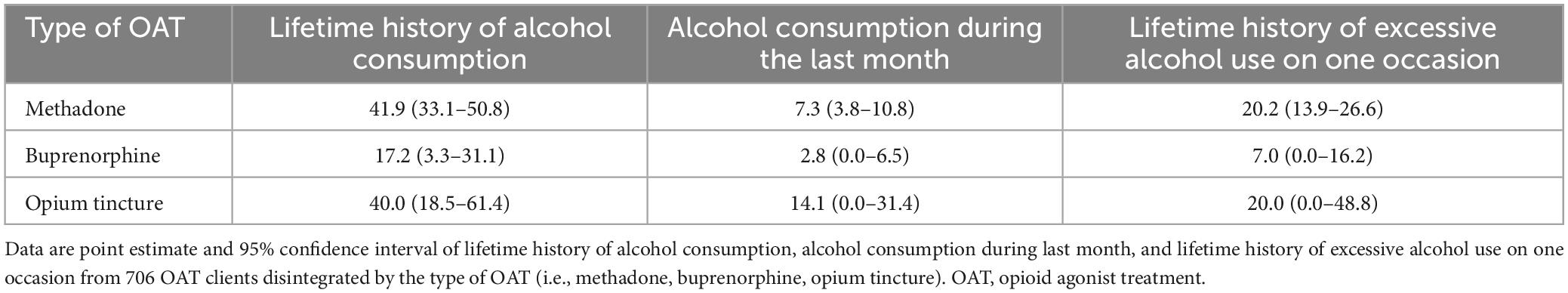
Table 2. Prevalence of alcohol consumption history (lifetime history of alcohol consumption, alcohol consumption during the last month, lifetime history of excessive alcohol use on one occasion) based on the type of OAT (i.e., methadone, buprenorphine, opium tincture).
Table 3 shows the prevalence of alcohol consumption by demographic characteristics, socioeconomic status, type and duration of treatment, and imprisonment history. Those who reported alcohol consumption (lifetime, past month, and lifetime excessive alcohol consumption) were younger and had a higher level of education. Duration of regular alcohol consumption in people with higher levels of education (high school diploma and above) was significantly longer than people with lower level of education. It was 6.3 years (95% CI, 4.4–8.1) for people with a higher level of education and 3.8 years (95% CI, 3.2–4.5) for a lower level of education. People with lifetime history of alcohol consumption were more likely to report lifetime incarceration. People who were on methadone maintenance treatment or had a history of incarceration were more likely to report lifetime history of alcohol consumption. Those who reported lifetime history of excessive alcohol consumption on one occasion were more likely to have a history of incarceration. In the multivariate logistic model only history of imprisonment was significantly associated with lifetime history of alcohol consumption (OR = 3.2 with 95% confidence interval; 2.1–4.9), alcohol consumption during last month (OR = 2.3 with 95% confidence interval; 1.4–3.7), and lifetime history of excessive alcohol use on one occasion (OR = 3.9 with 95% confidence interval; 2.3–6.7).

Table 3. Prevalence of alcohol consumption (lifetime, during the last month) and lifetime history of excessive alcohol consumption by demographic characteristics, socioeconomic status, type and duration of OAT, and prison history.
Table 4 presents prevalence of lifetime history of alcohol consumption, alcohol consumption during last month, and lifetime history of excessive alcohol use on one occasion based on participants’ rapid urine test results for morphine, amphetamines, cannabis, benzodiazepines, and tramadol. The prevalence of alcohol consumption was the same among those with positive rapid urine tests of morphine, cannabis, or tramadol. Participants who tested positive for amphetamines included 7.6% of the sample (with 95% confidence interval; 1.4–13) and reported higher lifetime history of alcohol consumption and lifetime history of excessive alcohol use on one occasion as compared to participants who tested negative for amphetamines. Although the difference between these two groups regarding lifetime history of excessive alcohol use on one occasion was statistically significant, the 95% confidence intervals had some overlap (Table 3). In addition, this group had a significantly longer duration of regular alcohol consumption than those who tested negative for amphetamines: 7.3 years (with 95% confidence interval; 9.1–5.6) compared to 4.7 years (with 95% confidence interval; 5.6–3.8). Participants whose urine test was positive for benzodiazepines expressed more alcohol consumption during last month than those whose urine test was negative for benzodiazepines (p = 0.038).
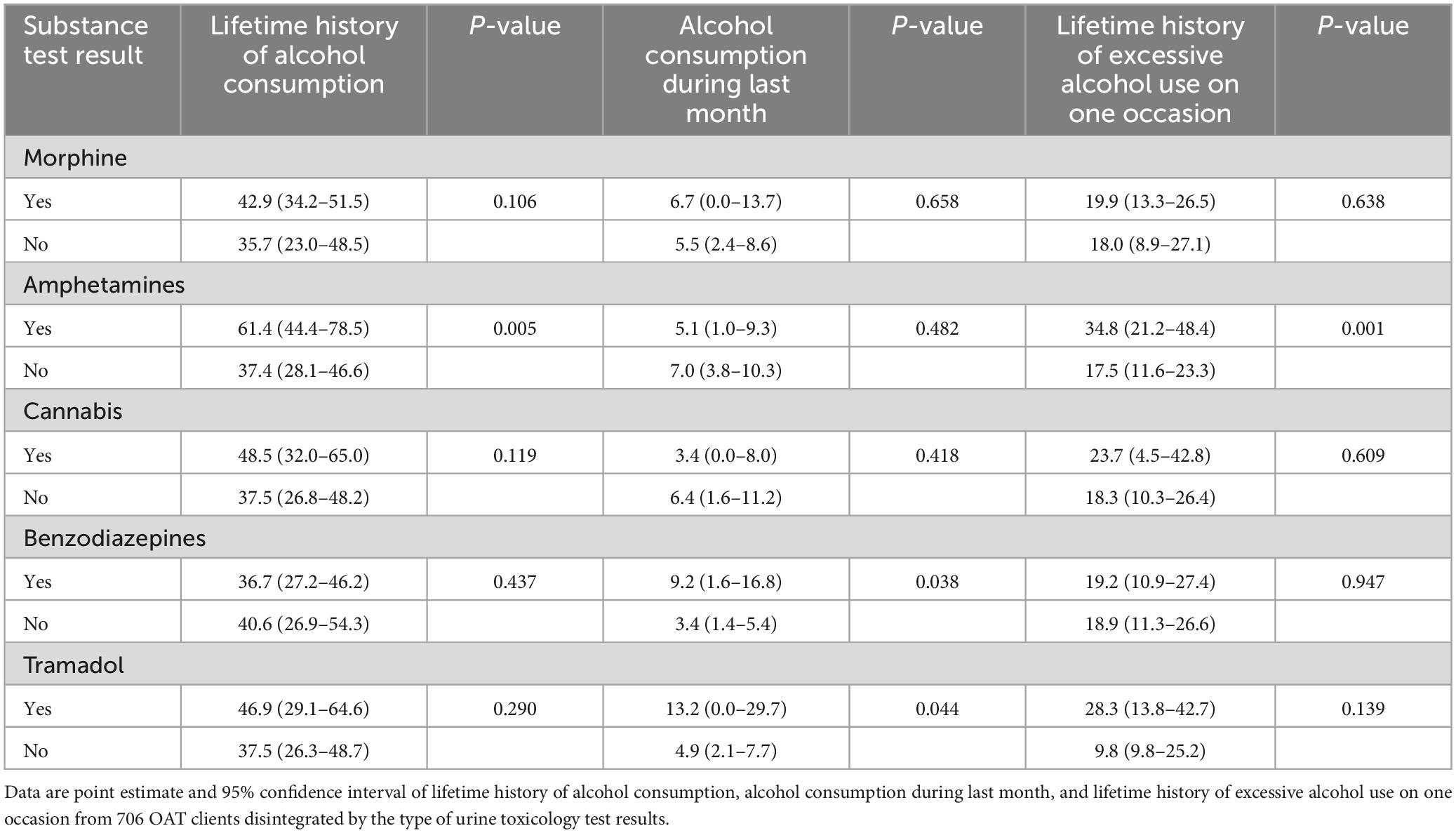
Table 4. Prevalence of alcohol consumption (lifetime, last month) and lifetime excessive alcohol consumption based on participants’ urine test results for morphine, amphetamines, THC, benzodiazepines, and tramadol.
This study aimed to determine the prevalence of alcohol consumption among clients of OAT centers using data from previous study. Estimates were based on data collected from a random sample of 706 clients referred to outpatient centers for OAT in Golestan province.
The prevalence of self-reported past month alcohol consumption in our study (6.9% with 95% confidence interval: 3.8–10.0) was lower than OAT clients in countries where alcohol is legally produced and consumed (5, 22, 25, 26).
Among those who admitted to the past month alcohol drinking, the average number of alcohol-drinking day was 1 day in a range from 0.44 to 1.4 days which show a low frequency of alcohol use during the last month. It is even less than the frequency of alcohol consumption in the EU general population (27).
One possible explanation for the low prevalence of alcohol use in our sample might be due to the self-reported nature of our data. Self-report as the method of data collection could result in underreporting due to social desirability bias (28). This possibility can be further strengthened, especially by considering the illegality of alcohol production and consumption in Iran, as well as heavy penalties for producers and consumers of alcohol (29). Although it should be noted that, according to Iran’s national protocols for OAT concurrent alcohol drinking is not associated with any negative effect on continuation of OAT services, rather treatment providers are recommended to provide more intensive services for such clients if their level of drinking would be at problematic levels (30). It should be noted that the reported indicators in our study do not provide needed data to estimate the prevalence of problematic alcohol use or alcohol use disorder. Further studies to measure the prevalence of alcohol use disorders using standard screening questionnaires or interviews are warranted.
Like studies on the general population, we found that OAT clients with a history of alcohol consumption were younger and had higher levels of education (31–33). The next point is the relationship between alcohol consumption and prison history, which may indicate an association between alcohol use and criminal activities in this sample (33). Further studies to explore the nature of this association are warranted. Moreover, alcohol consumption during the last month was higher among people who had a positive rapid urine test for benzodiazepines. It might be due to the concomitant use of these substances or adding benzodiazepines to alcoholic beverages by sellers in the illicit alcohol market as a cheap strategy to increase their intoxicating effects (34).
We found low alcohol consumption among clients of OAT centers in Golestan province, which is far lower than the figures provided by countries without legal restrictions on alcohol consumption. This finding does not necessarily indicate a low level of alcohol consumption in the general population but may suggest that people who use alcohol are probably a different class of people who use other substances in Iran. According to the latest finding in Iran, the overall pooled prevalence of alcohol consumption during the last 12-month, among the general population is 12% (24).
The relationship between alcohol consumption and some individual and social factors such as use of amphetamines and a history of imprisonment should lead treatment professionals to further examine and screen these people for alcohol consumption at treatment admission. It is also necessary for physicians to consider concomitant use of benzodiazepines and alcohol at the beginning of therapy because this can have a great impact on determining the dose required for the induction phase of OAT. According to the findings of this study and the previous study by the same group (15), it is recommended that these clients must first be screened for the possibility of using several substances before starting to treatment. It is also recommended to have such evaluation during the treatment process.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study involving humans was approved by the Ethic Committee of Golestan University of Medical Sciences GOUMS (code: IR.GOUMS.REC.1394.112). The participants provided their written informed consent to participate in this study.
Both authors made contribution to the concept and design of the article, analysis, and interpretation of data, drafted and revised the manuscript critically, reviewed the results, and approved the final version of the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. WHO. Guidelines for the Psychosocially Assisted Pharmacological Treatment of Opioid Dependence. Geneva: WHO (2007).
2. Mattick R, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochr Database Syst Rev. (2009) 2009:Cd002209.
3. Santo T Jr., Clark B, Hickman M, Grebely J, Campbell G, Sordo L, et al. Association of opioid agonist treatment with all-cause mortality and specific causes of death among people with opioid dependence: a systematic review and meta-analysis. JAMA Psychiatry. (2021) 78:979–93. doi: 10.1001/jamapsychiatry.2021.0976
4. Larney S, Hall W. A major expansion of opioid agonist treatment is needed to reduce overdose deaths in the USA. Lancet Public Health. (2019) 4:e77–8. doi: 10.1016/S2468-2667(19)30001-5
5. Soyka M. Alcohol use disorders in opioid maintenance therapy: prevalence, clinical correlates and treatment. Eur Addict Res. (2015) 21:78–87.
6. Nolan S, Klimas J, Wood E. Alcohol use in opioid agonist treatment. Addict Sci Clin Pract. (2016) 11:17.
7. Rittmannsberger H, Silberbauer C, Lehner R, Ruschak M. Alcohol consumption during methadone maintenance treatment. Eur Addict Res. (2000) 6:2–7.
8. Ryder NC, Barry J, Bury G, Keenan E, Smyth B. Prevalence of problem alcohol use among patients attending primary care for methadone treatment. BMC Fam Pract. (2009) 10:42. doi: 10.1186/1471-2296-10-42
9. Islam M, Day C, Conigrave K, Topp L. Self-perceived problem with alcohol use among opioid substitution treatment clients. Addict Behav. (2013) 38:2018–21. doi: 10.1016/j.addbeh.2012.12.001
10. Srivastava A, Kahan M, Ross S. The effect of methadone maintenance treatment on alcohol consumption: a systematic review. J Subst Abuse Treat. (2008) 34:215–23.
11. Best D, Gossop M, Lehmann P, Harris J, Strang J. The relationship between overdose and alcohol consumption among methadone maintenance patients. J Substance Use. (1999) 4:41–4. doi: 10.1016/j.comppsych.2015.07.004
12. McCance-Katz E, Sullivan L, Nallani S. Drug interactions of clinical importance among the opioids, methadone and buprenorphine, and other frequently prescribed medications: a review. Am J Addict. (2010) 19:4–16. doi: 10.1111/j.1521-0391.2009.00005.x
13. Ostapowicz G, Watson K, Locarnini S, Desmond P. Role of alcohol in the progression of liver disease caused by hepatitis C virus infection. Hepatology. (1998) 27:1730–5.
14. Rodger A, Roberts S, Lanigan A, Bowden S, Brown T, Crofts N. Assessment of long-term outcomes of community-acquired hepatitis C infection in a cohort with sera stored from 1971 to 1975. Hepatology. (2000) 32:582–7. doi: 10.1053/jhep.2000.9714
15. Danesh A, Noroozi A. Concurrent amphetamine and methamphetamine use among clients of opioid maintenance treatment programs in Golestan, Iran. Iran J Psychiatry Behav Sci. (2019) 13:e74234.
16. Ferri M, Finlayson A, Wang L, Martin P. Predictive factors for relapse in patients on buprenorphine maintenance. Am J Addict. (2014) 23:62–7.
17. Liu D, Gu J, Xu H, Hao C, Jiao M, Zhang X, et al. Club drugs and alcohol abuse predicted dropout and poor adherence among methadone maintenance treatment patients in Guangzhou. China. AIDS Care. (2017) 29:458–63. doi: 10.1080/09540121.2016.1259452
18. Gamble D, Josefson C, Hennessey M, Davis A, Waters R, Jones B, et al. Social interaction with an alcohol-intoxicated or cocaine-injected peer selectively alters social behaviors and drinking in adolescent male and female rats. Alcohol Clin Exp Res. (2019) 43:2525–35.
19. Moussas G, Fanouraki I, Pachi A, Asomatou A, Drylli O, Paschalakis G, et al. Comorbid psychopathology and alcohol use patterns among methadone maintenance treatment patients. J Addict. (2015) 2015:197652.
20. Zhong B, Xu Y, Xie W, Lu J, Yu W, Yan J. Alcohol drinking in chinese methadone-maintained clients: a self-medication for depression and anxiety? J Addict Med. (2019) 13:314–21. doi: 10.1097/ADM.0000000000000500
21. Varshney M, Ambekar A, Lal R, Yadav D, Rao R, Mishra A. Brief interventions for harmful alcohol use in opioid-dependent patients on maintenance treatment with buprenorphine: a prospective study from India. Addict Disord Their Treat. (2016) 15:129–35.
22. MacManus E, Fitzpatrick C. Alcohol dependence and mood state in a population receiving methadone maintenance treatment. Irish J Psychol Med. (2007) 24:19–22. doi: 10.1017/S0790966700010107
23. Wikipedia. List of Countries With Alcohol Prohibition (2020). Available online at: https://en.wikipedia.org/wiki/List_of_countries_with_alcohol_prohibition (accessed May 10, 2022).
24. Chegeni M, Kamel Khodabandeh A, Karamouzian M, Shokoohi M, Abedi L, Khalili M, et al. Alcohol consumption in Iran: a systematic review and meta-analysis of the literature. Drug Alcohol Rev. (2020) 39:525–38.
25. Hartzler B, Donovan D, Huang Z. Comparison of opiate-primary treatment seekers with and without alcohol use disorder. J Subst Abuse Treat. (2010) 39:114–23. doi: 10.1016/j.jsat.2010.05.008
26. Hillebrand J, Marsden J, Finch E, Strang J. Excessive alcohol consumption and drinking expectations among clients in methadone maintenance. J Subst Abuse Treat. (2001) 21:155–60. doi: 10.1016/s0740-5472(01)00198-2
28. Althubaiti A. Information bias in health research: definition, pitfalls, and adjustment methods. J Multidiscip Healthc. (2016) 9:211–7. doi: 10.2147/JMDH.S104807
29. Tran B, Nguyen H, Le Q, Mai H, Ngo C, Hoang C, et al. Alcohol and tobacco use among methadone maintenance patients in Vietnamese rural mountainside areas. Addict Behav Rep. (2018) 7:19–25. doi: 10.1016/j.abrep.2017.11.005
30. Morki A, Noroozi A. Iran national protocol on treatment of opioid dependence with methadone. Deputy for Treat Iran Ministry Health Med Educat [In Persian] (2014). 151–156. Available online at: https://enincas.tums.ac.ir/uploads/128/1393-protocol-methadone.pdf (accessed May 10 2022).
31. Du Z. Investigation on alcohol use among the patients with methadone maintenance treatment in Shanghai. J Shanghai Jiaotong Univ (Med Sci). (2019) 12:193–7.
32. Al-Ansari B, Noroozi A, Thow A, Day C, Mirzaie M, Conigrave K. Alcohol treatment systems in Muslim majority countries: case study of alcohol treatment policy in Iran. Int J Drug Policy. (2020) 80:102753. doi: 10.1016/j.drugpo.2020.102753
33. Nikfarjam A, Hajimaghsoudi S, Rastegari A, Haghdoost A, Nasehi A, Memaryan N, et al. The frequency of alcohol use in Iranian Urban population: the results of a national network scale up survey. Int J Health Policy Manag. (2017) 6:97–102. doi: 10.15171/ijhpm.2016.103
Keywords: alcohol, opioid agonist treatment (OAT), opioid use disorder (OUD), methadone, buprenorphine
Citation: Noroozi A and Danesh A (2023) Prevalence of alcohol consumption among clients of opioid agonist treatment (OAT) centers in Golestan province, Iran. Front. Psychiatry 14:1134683. doi: 10.3389/fpsyt.2023.1134683
Received: 30 December 2022; Accepted: 04 May 2023;
Published: 25 May 2023.
Edited by:
Anthony DeFulio, Western Michigan University, United StatesReviewed by:
Brian J. Piper, Geisinger Commonwealth School of Medicine, United StatesCopyright © 2023 Noroozi and Danesh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ahmad Danesh, YWRkYW5lc2hAeWFob28uY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.