- 1Department of Psychiatry and Psychotherapy, Medical Faculty, Leipzig University, Leipzig, Germany
- 2Department of Psychiatry and Psychotherapy, University Leipzig Medical Center, Leipzig University, Leipzig, Germany
- 3Centre for Research, Further Education and Consulting, University of Applied Sciences for Social Work, Education and Nursing Dresden, Dresden, Germany
Background: The literature indicates a negative impact on the mental health of university students during the COVID-19 pandemic. It remains unclear if this negative impact persists even after lockdown measures are lifted. The current study therefore investigates the mental health status of students by drawing on two previous studies the present study seeks to investigate differences in the mental health status across three time points.
Methods: A cross-sectional, anonymous online survey among students of six universities was conducted between April and May 2022 (N = 5,510). Symptoms of depression, anxiety, hazardous alcohol use and eating disorders as well as social and emotional variables were assessed utilizing standardized instruments. Risk- and protective factors for severity of depressive and anxiety symptoms were investigated using multiple regression models. Differences in e.g., symptoms of depression across three time points were assessed with one-way analysis of variance.
Results: More than one third of students exhibited clinically relevant symptoms of depression (35.5%), hazardous alcohol use (33.0–35.5% depending on gender) or anxiety disorder (31.1%). Taken together, almost two out of three (61.4%) students reported clinically relevant symptoms in at least one of the aforementioned symptom patterns, while almost one fifth of students reported suicidal ideation or thoughts of self-harm (19.6%). Higher perceived stress and loneliness significantly predicted higher levels of depressive symptoms, while resilience and social support were identified as protective factors. Compared to 2020 and 2021, levels of depressive symptoms were significantly reduced in 2022, levels of hazardous alcohol consumption showed a small but significant increase from 2021 to 2022. Worryingly, prevalence of suicidal ideation was the highest yet, being significantly higher than in 2020 (14.5%) and 2021 (16.5%).
Conclusion: These results confirm previous results that the pandemic had and still has a negative impact on the mental health of university students. The present study broadens this view by the fact that some areas seem to recover quicker, while others seem to increase worryingly. Especially the persistent rise in suicidal ideation from 2020 to 2021 and to 2022, a constant reduction in reported social support and associated perceived loneliness is concerning. The claim for low-threshold and accessible mental health support for university students remains the same as in the beginning of the pandemic.
1. Introduction
Even before the onset of the COVID-19 pandemic, young adults and especially university students were considered to be a vulnerable group for mental disorders, with reports of one in five students suffering from mental health issues (1, 2). Similarly, hazardous alcohol use is known to be prevalent among students in Germany and associated with various negative somatic and mental health outcomes (3, 4). As the peak of onset of most mental disorders is located in teenage years and young adulthood, stressors associated with university life may additionally increase the vulnerability of university students to develop mental health issues. Further, these stressors may lead to a worsening of any existing symptoms with an onset before matriculation, as treatment rates for mental health issues were reported to be low among university students even before the pandemic hit (2, 5).
Beginning at the end of the year 2019, the COVID-19 pandemic made its way across the globe (6). Almost everywhere, people were impacted by the pandemic and the associated government mandated non-pharmaceutical interventions (NPIs), to stop the spreading of the virus. Universities across the globe also had to accommodate these NPIs. As such, much of the academic, occupational, social, and cultural life of students was disrupted. NPIs like government-mandated social distancing and lockdown measures undeniably saved lives and mitigated transmission rates of COVID-19 in the populace (7, 8). However, a number of studies investigating the impact on university students support the assumption that the disruptions of the day-to-day lives caused by the COVID-19 pandemic and the NPIs to control the pandemic may have had a negative impact on various aspects of their mental health (9–13).
Thus, a recent study conducted about a month after England's first national lockdown ended in 2020 found that more than half of students at a university in Northern England reported clinically relevant levels of symptoms of depression and anxiety (12). Another study, conducted by our research group, compared the outcomes of two surveys conducted at Leipzig University, Germany, in the summer of 2020, when the strict social distancing and quarantine measures were eased up (14, 15) and in the spring of 2021, when a federally mandated lockdown was in effect in Germany. The authors found an increase from 2020 to 2021 in the severity of depressive symptoms, suicidal ideation, as well as in alcohol and drug consumption among students (9, 16). Another survey, conducted in the United States, comparing frequencies of mental disorders before and during the pandemic, found evidence for higher frequencies of depression, alcohol use disorder, and bulimia as well as binge eating disorder (10). A systematic review encompassing 16 studies investigating the impact of the pandemic on the mental health of university students identified a relationship between university students' mental health and the onset of the pandemic (11). According to the authors, all studies incorporated in their review indicated that university students reported more feelings of anxiety, depression, fatigue, and distress than before the pandemic. Furthermore, meta-analyses investigating the prevalence of depression and anxiety among university students during the COVID-19 pandemic suggests that up to one third of university students were suffering from symptoms of depression and/or anxiety at some point during the pandemic (13, 17).
Clearly, the majority of the evidence suggests that the pandemic and (while the protective effects of NPIs need to be acknowledged) the associated NPIs designed to curb the spread of COVID-19 have had a negative effect on university students' mental health worldwide. In addition to the severe impact of mental health issues on one's current life, symptoms often recur in the biography of persons who experienced some sort of mental strain earlier in life (18). This adds up to several factors making the treatment of mental health issues a major cost and resource factor within the healthcare system: In Germany, the costs of treatment for depression in 2020 amounted to 9,453 mil. €, while mental disorders caused an outage of work-production depleting 0.4% of the gross domestic income (19, 20).
With the pandemic still ongoing, as of the beginning of April 2022, federally mandated NPIs were lifted in Germany. While there were, and as of the time of writing this article, still are, some NPIs to protect vulnerable groups that may also affect university students (e.g., mask mandates in university buildings and public transportation), there are no strict lockdown measures in effect and much of the academic, occupational, social, and cultural life has since resumed. In general, still little is known if the negative impact of the pandemic on the mental health of university students persists. However, some preliminary evidence suggests that with the ongoing of the pandemic and after strict lockdown measures were lifted, mental health of most students improved (21, 22). To explain the effects of the pandemic and NPIs regarding mental health, the literature suggests resilience, self-efficacy and social-support (23–28) as protective factors. Furthermore, stress and loneliness were indicated to act as risk factors for developing or intensifying symptoms of mental disorders (9, 29–32). Worryingly, recent research conducted by our research group with students from Leipzig University indicated a significant decrease in resilience, social-support, and self-efficacy as well as an increase in perceived stress and loneliness, although effect sizes were small (9, 16).
Additionally, some recent studies suggest a complex relationship between vaccination attitudes and fear of COVID-19 as those who are not willing to get vaccinated reported being less fearful of COVID-19 while receiving a vaccination also seems to reduce fear of COVID-19 (33–36). At the same time, a number of studies suggest that fear of COVID-19 shows associations with outcomes relevant to mental health such as depressive symptoms, anxiety or stress (37, 38).
In the light of past reports of an increase in the occurrence and severity of depressive symptoms, symptoms of generalized anxiety disorder and mixed results concerning hazardous alcohol use as well as general eating disorder psychopathology, the present study aims to (a) gauge the prevalence of those variables in a current post-lockdown convenience sample of German university students.
Further, drawing on the data and results from two congruent cross-sectional surveys (9, 16) conducted in 2020 and 2021, the current paper (b) examines the development of symptoms of depression, suicidal ideation and hazardous alcohol use across three points in time (i.e., 2020, 2021, and 2022). We hypothesized that the elevated levels of depressive symptoms, suicidal ideation and hazardous alcohol and substance use previously identified by Dogan-Sander et al. (9) would significantly decline to levels comparable to those found in the 2020 survey conducted by Kohls et al. (16). Drawing on the additional data sets collected the 2020 and 2021 surveys, (c) differences between the three samples in social and emotional outcomes that are known to act as protective and risk factors were investigated. Specifically it was hypothesized that reduced levels of resilience, social-support and self-efficacy as well as the elevated levels of loneliness and stress would recover to levels similar those found by Kohls (16). Finally, utilizing the current 2022 sample, the present study aims to (d) identify risk- and protective factors for symptoms of depression, symptoms of anxiety, hazardous alcohol use and eating disorder symptomatology.
2. Materials and methods
2.1. Participants and procedure
The current sample was recruited between April 11th, and May 27th, 2022, at six universities in Saxony, Germany. Participants were recruited using the official university email and social media channels of the universities: students received an email from the administrative office containing a link to the online survey, hosted via unipark, an online research platform (www.unipark.de). Two email reminders were sent out approximately 1 week and 4 weeks, respectively, after the initial email invitation. Additionally, an informational video on how to participate in the survey was provided to participating universities. The video was published by three of the participating universities in their social media channels, while the remaining three participating universities did not have their own social media profiles and thus, did not publish the video online. The video itself did not contain a participation link. Rather, the video called attention to the recruitment e-mail, which contained detailed information as well as a link to the survey and was sent to (and only accessible via) the students' institutional email addresses.
Criteria for inclusion in the study were current enrollment at one of the universities and being 18 years or older. There were no exclusion criteria. The ethics committee of the Medical Faculty of Leipzig University granted approval for the current study on November 11th, 2021 (file reference: 509/21-ek). All materials used in the study, as well as the declaration of informed consent, were checked and approved by the data protection officer of the Medical Faculty of Leipzig University. Informed consent was provided by all participants before participation in the study via an opt-in function at the beginning of the anonymous online survey.
Overall, a total of N = 5,510 students completed the online survey. Of these, n = 28 (0.5%) participants were excluded in the final analysis because they indicated in a control question that they had not completed the survey conscientiously. Furthermore, n = 3 (0.1%) participants were excluded because they were underage and thus, not meeting inclusion criteria, while another n = 7 (0.1%) participants were excluded after manually checking the data for implausible cases (n = 4 [0.1%] participants indicated studying their current study program for more than 24 semesters and n = 3 [0.1%] indicated being aged 80 years or older). All in all, n = 5,474 participants were included in the final analysis.
Beside the current sample, the present study takes advantage of two further cross-sectional samples collected by our research group, each including data on surveys with content similar to the present survey: First, during July and August 2020, a survey with N = 3,382 students enrolled at Leipzig University, Germany, was conducted to investigate the impact of the pandemic on the mental health status of students at Leipzig University (16). Second, between March and April 2021, another survey with a total of N = 5,642 participating students enrolled at Leipzig University, Germany, was conducted to investigate differences in the mental health status of students between 2020 and 2021 (9).
2.2. Measures
The current study used a modified version of the online survey utilized in the 2020 and 2021 studies (9, 16). In contrast to the 2020 and 2021 version, items pertaining to aspects of the ongoing pandemic were removed, while other instruments regarding aspects of digitalization (not part of the analysis in the current paper) were added. Furthermore, in the previous surveys the Short Evaluation of Eating Disorders (39) was used for assessment of eating disorder symptoms, in the current survey another instrument was used (see below). The survey was offered in Germany and in English, depending on respondents preferred language.
2.2.1. Sociodemographic information
The survey contained items assessing sociodemographic and socioeconomic information (age, gender, family status, migration status, education, student status [currently enrolled, currently not re-registered or on leave of absence], sources of income, and monthly net income, presence of [chronic] somatic conditions), current vaccination status, and general attitude toward vaccinations (on a 5-point rating scale, ranging from 1 = “opposing” to 5 = “approving”). Parental educational attainment was categorized into four categories (low, middle, elevated, and high attainment) according to the highest educational and professional qualifications of parents (40). Parental educational attainment was considered to be high if both parents were holders of a university degree and considered elevated if only one parent was a holder of a university degree. If both parents completed an apprenticeship, skilled worker's qualification, master craftsman's examination, technical school, or technician's qualification, parental educational attainment was considered to be medium. If only one parent or none of the parents completed such a qualification, parental educational attainment was considered to be low. Migration status was assessed by asking the participants to indicate if they had a migratory background. Response options were to answer the question in the negative, to indicate that they themselves are immigrants, or to indicate that their parents are immigrants.
2.2.2. Mental health measures
Patient-health-questionnaire-9 (PHQ-9). The PHQ-9 (41) utilizes a 4-point rating scale, ranging from 0 = “not at all” to 3 = “nearly every day” to assess the occurrence of depressive symptoms over a 2 week period. More severe depressive symptoms are indicated by a higher total sum score (range: 0-27). Scores of 10 or more are indicative of clinically relevant symptoms (41, 42). Furthermore, suicidal ideation was assessed utilizing item 9 of the PHQ-9, which asks if respondents had any “thoughts that [they] would be better off dead, or of hurting [themselves]” during the past 2 weeks. For the English and for the German instrument, Cronbach's α was .85 and .91, respectively.
Alcohol use disorder identification test (AUDIT-C). The AUDIT-C (43, 44) consists of three items, scored on a 5-point rating scale, evaluating the frequency of alcohol use (0 = “never” to 4 = “4 times a week or more”), the typical quantity being consumed (0 = “1 or 2” to 4 = “10 or more”) as well as the frequency of binge drinking (i. e., consuming more than six alcoholic beverages on a single day; 0 = “never” to 4 = “once per week”). To identify alcohol misuse, a total sum score is computed, with a score of 4 or more indicating alcohol misuse in women, and a score of 5 or more indicating alcohol misuse in men (45). For the English and for the German instrument, Cronbach's α was .76 and .76, respectively.
To evaluate the frequency of drug or substance consumption, a single item adapted based on the structure of AUDIT-C items (“How often do you use drugs/substances?”), rated on a 5-point rating scale (0 = “never” to 4 = “4 times a week or more”) was used.
Eating disorder examination-questionnaire 8 (EDE-Q8). Derived from the long form of the EDE-Q, the EDE-Q8 (46) is a self-report measure to measure general eating disorder pathology. Utilizing eight items, the EDE-Q8 explores different facets of eating disorder psychopathology (e. g., preoccupation with food, discomfort seeing one's own body). The items are rated on a 6-point rating scale, but with differing answer cues depending on the content of the specific item. A scale mean score was computed, with higher scores indicating more severe symptomatology (46). For the English and for the German instrument, Cronbach's α was .92 and .92, respectively.
General anxiety disorder scale (GAD-7). The GAD-7 (47) consists of seven items assessing the frequency of occurring symptoms indicative of general anxiety disorder (GAD) during the previous 2 weeks. The items are rated on a 4-point rating scale (0 = “not at all” to 4 = “nearly every day”) and item scores are added up to compute a total score. According to the authors, a total score of 10 or higher identifies a probable case of GAD (47, 48). For the English and for the German instrument, Cronbach's α was .91 and .87, respectively.
In addition, one single choice item directly assessed if participating students had been diagnosed with a mental disorder in the past (answer options: “yes”, “no”). If participants indicated that they had been diagnosed with a disorder, they were asked to indicate which disorder had been diagnosed (answer options: “depression”, “bipolar disorder”, “anxiety disorder”, “obsessive-compulsive disorder”, “personality disorder”, “eating disorder”, “ADHD/ADD”, and “I don't know”) and for how long they were suffering from each diagnosed disorder (in years). A free text field was also provided if the diagnosed disorder was not listed. Finally, participants were asked if they were currently receiving professional treatment for any mental disorders and if yes, they could indicate if they received medication, psychotherapeutic treatment, both, or neither.
2.2.3. Measures of personal, social, and emotional variables
Data on a selection of personal (resilience, self-efficacy), social (social support), and emotional (perceived stress, loneliness) variables of interest were also collected in the online survey.
Brief Resilience Scale (BRS). While there is no scientific consensus on the definition of the construct of resilience (49, 50), according to the authors of the BRS (51), the ability to “bounce back” and recover from stress represents the original definition of resilience most closely. As such, the instrument is used to assess the ability of individuals to recover from stress using six items, rated on a 5-point Likert scale (1 = “strongly disagree” to 5 = “strongly agree”). A scale mean score is computed, with higher mean scores indicating a more pronounced ability to recover from stress quickly (51, 52). For the English and for the German instrument, Cronbach's α was .77 and .82, respectively.
General self-efficacy scale (GSE). The instrument consist of 10 items rated on a 4-point Likert scale (1 = “not at all true” to 4 = “exactly true”) evaluating general self-efficacy expectations (53). The total sum score reaches from 10 to 40, with higher scores indicating a higher subjective conviction that the individual is able to deal with demanding situations on their own accord (53). For the English and for the German instrument, Cronbach's α was .86 and .87, respectively.
ENRICHD social support inventory (ESSI). To measure the perceived emotional social support, the ESSI consists of five items, scored on a 5-point rating scale (1 = “none of the time” to 5 = “all of the time”) (54, 55). The total score has a range from 5 to 25. Greater levels of perceived social support are indicated by a higher total sum score (54, 55). For the English and for the German instrument, Cronbach's α was .93 and .88, respectively.
Perceived stress scale (PSS-4). A four item instrument assessing perceived stress during the previous month on a 5-point rating scale, ranging from 0 = “never” to 4 = “very often” (56). Item scores are summed up into a total sum score, ranging from 0 to 16. Higher levels of perceived stress are indicated by higher sum scores (54). For the English and for the German instrument, Cronbach's α was .80 and .79, respectively.
UCLA 3-item loneliness scale. The three items of the UCLA 3 are rated on a 3-point verbal rating scale (1 = “hardly ever” to 3 = “often”) and summed up into a total sum score, ranging from 3 to 9 (57). The higher the total sum score, the lonelier an individual is considered to be. According to the authors, individuals with a total score of 6 or higher may be considered lonely (57). For the English and for the German instrument, Cronbach's α was .86 and .80, respectively.
2.3. Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics version 27.0. A two-tailed α = 0.05 significance level was used for statistical testing. First, descriptive statistics for sociodemographic and socioeconomic variables as well as outcomes regarding mental health, personal, social, and emotional variables were computed. For a better overview of the age distribution in the present sample, age groups were calculated (Table 1). Second, differences between the three separate samples of the surveys conducted in 2020, 2021, and 2022 were investigated. Using χ2-tests, differences in categorical outcome variables (i. e. occurrence of mental disorders, suicidal ideation) sociodemographic and socioeconomic variables were analyzed. Where needed, effects found using χ2-tests were further decomposed by utilizing the z-test provided by SPSS to compare column proportions. Differences in metric variables (depressive symptoms, harmful alcohol consumption, perceived stress, resilience, social support, self-efficacy, loneliness) were assessed using one-way analysis of variance (ANOVA), followed by Tukey post-hoc tests to decompose significant effects. While sample sizes differed between the three surveys, the variance ratio for all variables of interest remained below 1.5 in all comparisons between groups. As such we remained confident in relying on ANOVA to compute group comparisons (58). Taking multiple testing into account, Bonferroni correction was used where needed. was interpreted as small when =0.001, as medium when =0.06 and as large when =0.14 (59). A comparison of GAD-7 and EDE-Q8 mean scores of the current and previous surveys was not possible, as those instruments were only utilized in the 2022 survey. As the surveys in 2020 and 2021 were exclusively conducted with students studying at Leipzig University, all comparisons were repeated including only students from Leipzig University to check for differences in the results.
To evaluate predictors of mental health outcomes in the current sample collected in 2022, multiple regression analyses were performed for PHQ-9 scores, AUDIT-C scores, EDE-8 scores and GAD-7 scores as dependent variables. Continuous predictors included in the models were age, resilience, self-efficacy, perceived social support, loneliness and stress, as well as general vaccination attitude. Categorical predictors included in the models were gender, being a parent, residential status, marital status, migrant background, income, parental education, presence of (chronic) somatic conditions and mental disorders, as well as vaccination status. For vaccination status, being vaccinated was chosen as reference category, as it was suspected that most participants were already vaccinated. Categorical predictors were dummy coded as needed. All VIF were < 10, as such confirming the assumption that independent variables did not exhibit multicollinearity in the current analysis.
3. Results
3.1. Sociodemographic characteristics
Sociodemographic characteristics and descriptive results of the PHQ-9, PSS-4, ESSI, UCLA, and GSE sum scores of the present sample are shown in Table 1. In the present sample, the mean age was 23.71 years (SD = 4.81), with participants ranging from 18 to 56 years old. Regarding gender, n = 3,775 (69.0%) of the participants indicated being female, n = 1,599 (29.2%) being male, and n = 100 (1.8%) being diverse. In addition, n = 933 (17.0%) of participants indicated suffering from a (chronic) somatic condition. In the present sample, participants were generally in favor of vaccinations, with a mean score of 4.63 (SD = 0.78) regarding their general attitude toward vaccinations and a total of n = 5,102 (93.2%) of participants reporting that they were fully vaccinated against COVID-19. Furthermore, n = 59 (1.1%) participants stated that they were not fully vaccinated but wanted to do so and n = 313 (5.7%) indicated that they were not vaccinated and had no intention of doing so. Compared with the 2020 and 2021 samples, while no differences were found in gender χ2 (2, 14498) = 5.98, p = < 0.001, there was a significant difference in age, F(2, 14494) = 13.41, p < 0.001, between the samples. A Tukey post-hoc test indicated, that compared to 2020 (age M = 23.98, SD = 4.64) participants in 2021 (age M = 23.47, SD = 4.46), mean difference (MD) = 0.52, 95%-CI (0.28, 0.76), p < 0.001, and 2022, MD = 0.28, 95%-CI (0.04, 0.51), p = 0.018, were significantly younger, while participants in 2021 were significantly younger when compared to participants in 2022, MD = −0.24, 95%-CI (−0.45, 0.04), p = 0.016.
3.2. Mental health outcomes and comparisons to previous survey results from 2020 and 2021
All in all, 22.6% (n = 1,239) of participants disclosed that they had previously been diagnosed with a mental disorder and less than half of those (47.7%; n = 591) reported receiving any form of treatment (i. e., psychotherapy and/or medication) at the time of the survey. The three most frequent self-reported mental disorder diagnoses among the sample were depression (11.2%; n = 612), anxiety disorder (8.0%; n = 437), and eating disorders (3.9%; n = 215). In the current survey of 2022, nearly two-thirds (61.4%, n = 3363) of participants met the cut-off for clinically significant symptom severity on at least one of the instruments (PHQ-9, AUDIT-C, GAD-7) that specify such cut-offs.
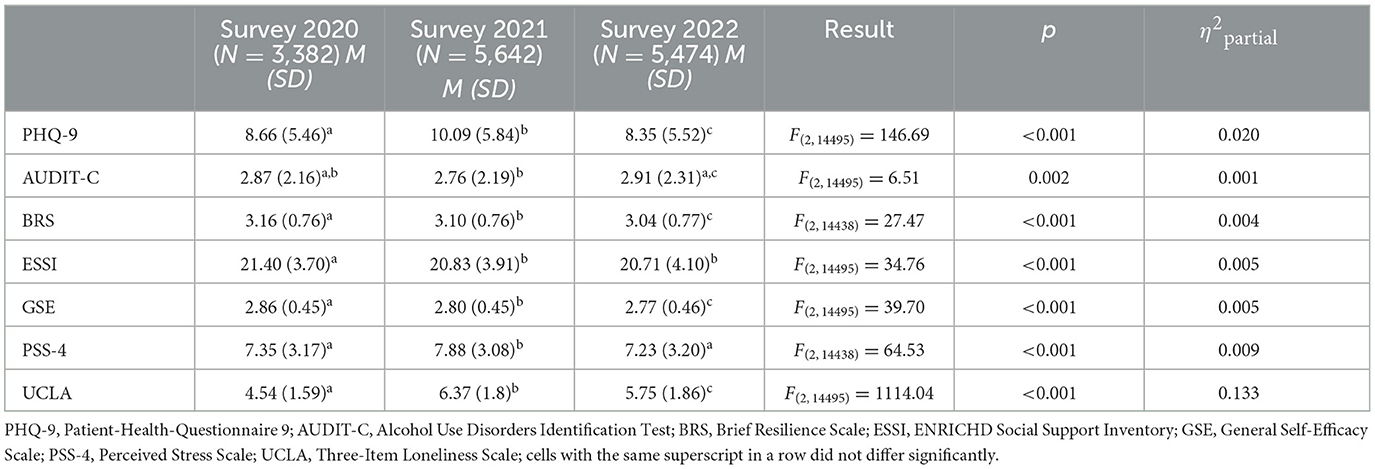
Regarding depressive symptoms, the mean sum score of the PHQ-9 was 8.34 (SD = 5.51), with n = 1,936 (35.5%) participants exhibiting a score of 10 or higher, indicating clinically relevant symptom severity. When compared to previous survey data from 2020 and 2021, significant differences in the mean PHQ-9 scores were found (Table 2). Results of the post-hoc analysis show that participants reported significantly less severe levels of depressive symptoms in 2020 than in 2021, MD = −1.43, 95%-CI (−1.72, −1.14), p < 0.001, and significantly more than in 2022, MD = 0.31, 95%-CI (0.03,0.60), p < 0.029. In 2021, participants reported significantly more severe levels of depressive symptoms than in 2022, MD = 1.74, 95%-CI (1.49, 1.99), p < 0.001. When repeating this comparison analyzing only participants studying at Leipzig University, results differed. While the overall difference remained significant, F(2, 11983) = 103.27, p < 0.001, = 0.017, a post-hoc analysis did not find a significant difference in mean scores between the surveys conducted in 2020 and 2022, MD = 0.12, 95%-CI (−0.12, 0.46), p = 0.666, while significant differences emerged when comparing 2020 and 2021, MD = 1.43, 95%-CI (−1.72, 1.14), p < 0.001, as well as 2021 and 2022, MD = 1.55, 95%-CI (1.25, 1.85), p < 0.001.
Significant differences in the occurrence of mental disorders, = 21.07, p < 0.001 were found between the three surveys. The proportion of participants stating that they had been diagnosed with a mental disorder in the past was significantly higher, p < 0.05, in 2022 (n = 1239, 41.5%) than in 2021 (n = 1105, 37.0%) and in 2020 (n = 644, 21.6%). Furthermore, n = 1,075 (19.6%) of the current sample indicated suicidal ideation or thoughts of self-harm in the 2 weeks preceding the survey, a significantly higher proportion than in both other samples (2020: n = 490, 14.5%; 2021: n = 936, 16.6%), = 38.11, p < 0.001. Repeating these analyses only using participants from Leipzig University, results remained the same.
The GAD-7 mean sum score was 7.76 (SD = 4.79), with n = 1,704 (31.1%) participants reaching the cut-off for clinically relevant symptom severity. Additionally, the mean sum score of the EDE-Q8 was 1.62 (SD = 1.49) (46).
Concerning alcohol consumption, n = 1,244 (33.0%) of female participants and n = 568 (35.5%) of male participants reached scores above the cut-off for alcohol misuse. In the diverse subgroup, n = 39 (39.0%) scored above the cut-off for women. This proportion declined to n = 32 (32.0%) when using the cut-off for males. While statistical significant differences in AUDIT-C scores between the surveys were found (Table 2), post-hoc analyses only identified a significant difference between the years 2021 and 2022, MD = −0.15, 95%-CI (−0.25, −0.05), p = 0.001, such that participants in 2021 reported significantly less alcohol use than in 2022. When repeating this comparison analyzing only participants studying at Leipzig University, results remained the same.
Finally, with reference to drug and substance consumption, n = 4,720 (86.2%) of participants in the 2022 survey reported having never consumed any drugs or substances, with a score of M = 1.24 (SD = 0.71) regarding the frequency of drug consumption. In comparison to the data of the previous surveys, significant differences in the frequency of drug consumption were found, F(2, 14440) = 22.73, p < 0.001, = 0.003, with post-hoc analysis indicating that in the 2022 survey, participants reported significantly less frequent drug consumption than participants in the 2020, MD = −0.06, 95%-CI (−0.10, −0.02), p = 0.002, and 2021, MD = −0.10, 95%-CI (−0.14, −0.06), p < 0.001, surveys. When repeating this comparison analyzing only participants studying at Leipzig University, the effect remained significant, F(2, 11928) = 10.73, p < 0.001, η2partial =0.002, but there was no significant difference between 2022 and 2020, MD = −0.04, 95%-CI (−0.09,0.01), p = 0.170, yet the difference between 2022 and 2021 remained significant, MD = −0.08, 95%-CI (−0.13, −0.04), p < 0.001.
3.3. Social and emotional outcomes and comparisons to previous survey results from 2020 and 2021
The results of the comparison of social and emotional outcomes between the three surveys are displayed in Table 2. Results imply that the scores of resilience (BRS), social support (ESSI), general self-efficacy (GSE), perceived stress (PSS-4) as well as loneliness (UCLA) differed significantly between the three surveys. Participants in 2020 indicated to be significantly more resilient than in 2021 MD = 0.06, 95%-CI (0.02, 0.10), p < 0.001, or 2022, MD = 0.12, 95%-CI (0.08, 0.16), p < 0.001, while participants in 2021 reported being significantly more resilient than in 2022, MD = 0.06, 95%-CI (0.03, 0.10), p < 0.001. Repeating these analyses only using participants from Leipzig University, results did not differ.
Regarding self-efficacy, participants in 2020 reported significantly more self-efficacy than in 2021 MD = 0.05, 95%-CI (0.03, 0.08), p < 0.001, or 2022, MD = 0.08, 95%-CI (0.06, 0.11), p < 0.001, while participants in 2021 reported significantly more self-efficacy than in 2022, MD = 0.03, 95%-CI (0.01, 0.05), p < 0.001. A repetition of the analyses only utilizing participants from Leipzig University did not lead to different results.
Investigating social support (ESSI), Tukey's post-hoc test indicated significant differences (both p < 0.001) between the ESSI scores of the years 2020 and 2021, MD = 0.57, 95%-CI (0.37, 0.77), as well as 2020 and 2022 (MD = 0.69, 95%-CI (0.49, 0.90), while the difference between 2021 and 2022, MD = 0.12, 95%-CI (−0.05, 0.30) did not reach statistical significance (p = 0.123). As before, results remained the same when repeating the analysis only utilizing participants from Leipzig University.
In terms of perceived stress, participants in 2020 indicated to be significantly less stressed than in 2021 MD = −0.53, 95%-CI (−0.70, −0.37), p < 0.001, while no significant difference emerged when compared to 2022, MD = 0.11, 95%-CI (−0.05, 0.28), p = 0.286. Participants in 2021 reported being significantly more stressed than in 2022, MD = 0.65, 95%-CI (0.50, 0.79), p < 0.001. Again, the pattern of effects remained the same, when repeating the analysis only utilizing participants from Leipzig University.
On the subject of perceived loneliness, participants in 2020 reported to be significantly less lonely than in 2021 MD = −1.82, 95%-CI (−1.92, −1.73), p < 0.001, or 2022, MD = −0.12, 95%-CI (−1.30, 1.11), p < 0.001, while participants in 2021 reported being significantly more lonely than in 2022, MD = 0.62, 95%-CI (0.54, 0.70), p < 0.001. A repetition of the analysis only utilizing participants from Leipzig University showed the same pattern of significant differences.
3.4. Predictors of mental health outcomes
Results of the regression analysis investigating predictors of depressive symptoms are displayed in Table 3. Results indicate that the regression model explained 56% of the variance, R2 = 0.56, F(25, 5399) = 277.63, p < 0.001. Being gender diverse (p < 0.001), having parents with a migrant background (p = 0.012) suffering from (chronic) somatic disorders (p < 0.001), suffering from mental disorders (p < 0.001) and higher levels of perceived loneliness and stress (both p < 0.001) were predictors of higher levels of depressive symptoms. Being older age, (p = 0.001), having parents with an elevated educational background (p = 0.036) and higher levels of resilience, self-efficacy and social support (all p < 0.001) were identified as protective factors.
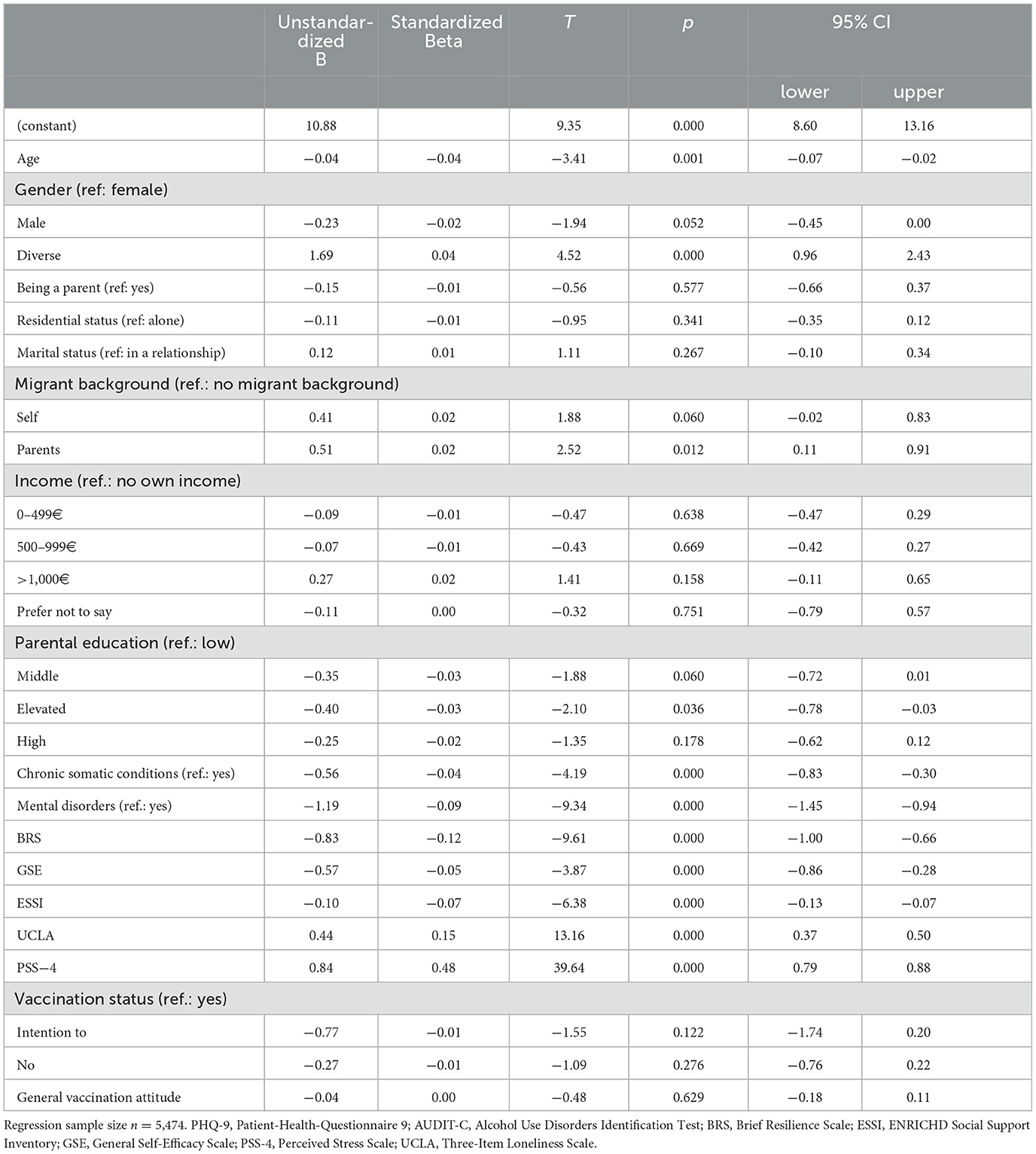
Table 3. Linear regression analysis for predictors of depressive symptomatology measured by PHQ-9 (Patient Health Questionnaire-9).
Concerning general anxiety disorder symptomatology, results are displayed in Table 4. 53% of the variance in the outcome variable, R2 = 0.53, F(25, 5399) = 245.02, p < 0.001, could be explained by the regression model. Higher levels of general anxiety disorder symptomatology were predicted by having an income of >1,000€ (when compared to not having an own income; p = 0.010), suffering from a (chronic) somatic condition (p < 0.001), suffering from a mental disorder (p < 0.001) and higher levels of loneliness and perceived stress (both p < 0.001). Being of older age (p = 0.012), being male (when compared to being female; p = 0.003), being single (p = 0.002), higher levels of resilience (p < 0.001) as well as reporting to not be vaccinated predicted lower levels of general anxiety disorder symptomatology.
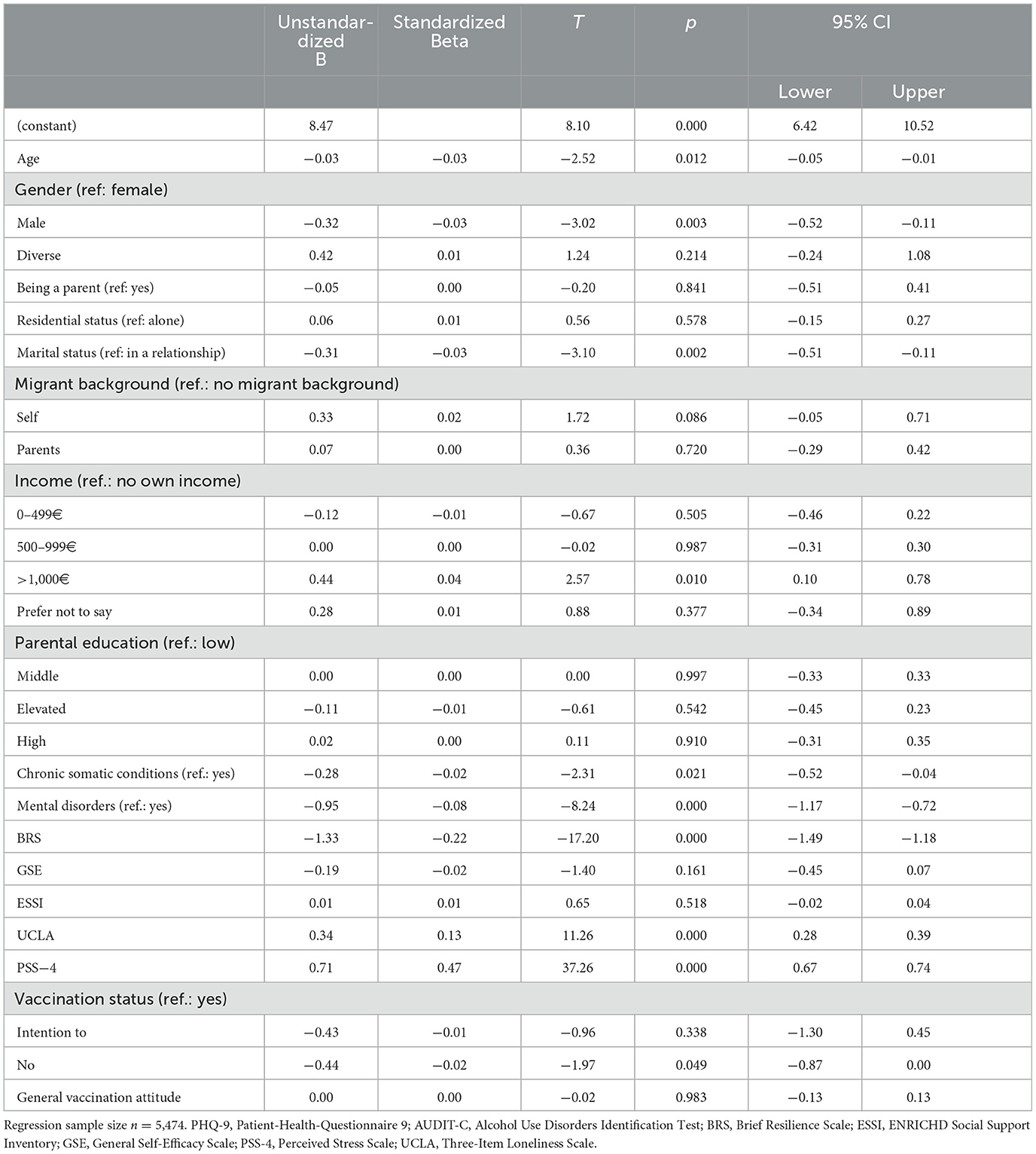
Table 4. Linear regression analysis for predictors of generalized anxiety disorder symptoms by GAD-7 (General Anxiety Disorder scale 7).
Finally, regarding harmful alcohol use, only 7% of the variance, R2 = 0.07, F(25, 5399) = 16.50, p < 0.001, in the outcome variable could be explained by the regression model. Furthermore, as only 15% of the variance, R2 = 0.15, F(25, 5399) = 39.45, p < 0.001, could be explained by the regression model predicting eating disorder symptomatology, we elected to omit further interpretation of these models.
4. Discussion
The present study examined the occurrence and severity of depressive symptoms, symptoms of generalized anxiety disorder, hazardous alcohol use as well as general eating disorder psychopathology among university students. Further, risk and protective factors relevant for students' mental health in a current post-lockdown sample of German university students were explored. Ultimately, the development of symptoms of mental health disorders in university students had been analyzed, drawing on three separate samples collected across three time points (2020, 2021, 2022).
The results from the present study confirm the picture from the international literature that the pandemic has overall a negative impact on the mental health of university students- and that this picture overall seems to persist, with a trend to decrease in some areas. Nevertheless, the hypothesized decline of elevated levels of depressive symptoms and hazardous alcohol use previously identified by Dogan-Sander et al. (9) could be confirmed by the present study.
4.1. Mental health outcomes and comparisons to previous survey results from 2020 and 2021
Taken together, almost one in three (61.4%) students reached the cut-off for clinically relevant symptom severity on at least one of the instruments (PHQ-9, AUDIT-C, or GAD-7) that specified such cut-off values. While the EDE-Q8 does not specify cut-off values, the sample mean roughly corresponds to the 78th percentile in a sample of the general population, which may indicate an elevated level of eating disorder symptoms in the present sample (46). It is important to highlight that those instruments are self-report-based screening instruments to determine specific symptom loads (i.e., depressive symptoms, general anxiety symptoms, and alcohol misuse or dependency symptoms) and are not a clinical diagnosis or an indication for further treatment by themselves. Nevertheless, this result is a clear indication of a worrying level of psychological distress and clinically relevant symptom load among students in the present sample. More specifically, a substantial number of students still exhibited clinically relevant symptoms of depression in 2022 (n = 1,936; 35.5%). The levels of depressive symptoms were significantly reduced in 2022, when compared to the 2021 sample. Although it has to be kept in mind that the current study draws on three separate cross-sectional samples, it can be summarized, that the overall trend seems to be slightly positive, rather than sustained negative regarding depressive symptoms in university students in Germany over time. Nevertheless, more than one third of students report clinically relevant depressive symptoms, which is still a very worrying result. This result is also in line with several other studies among university students in other countries (60–63).
Further, nearly one fourth (n = 1,239; 22.6%) of participants reported that they had been diagnosed with a mental disorder and less than half of those (47.7%; n = 591) reported not to receive any form of treatment. This result has remained unchanged over time and may indicate persistent barriers to seeking help or to accessing mental health care in university students (9). However, it is also possible that participants had received a diagnosis in their lifetime but were no longer in need of professional treatment at the time when the survey was conducted. That being said, past studies in the U.S. indicate low treatment rates as well as significant barriers to accessing mental health care among university students (2, 5, 64). As such, further research seems warranted to evaluate treatment needs in German university students.
Although the effect size was small, hazardous alcohol consumption significantly increased, when comparing the 2021 and 2022 samples, while no difference emerged when comparing the 2020 and 2022 samples. Because even minor differences can produce statistically significant results in large samples, caution is advised when interpreting such effects. As such, it is unclear whether the found reported effect can be interpreted as a meaningful change in consumption behavior. So far, very heterogeneous results had been reported in the international literature regarding alcohol consumption among students during the COVID-19 pandemic ranging from a clear increase, decrease or unchanged status (65–70). This picture seems to continue in 2022, supported by the present results and it might need further studies to be able to draw a more comprehensive picture and understand all related factors.
Worryingly, the prevalence of suicidal ideation was the highest in the 2022 survey, with 19.6% of all participants indicating suicidal ideation or thoughts of self-harm in the 2 weeks preceding the survey, which was significantly higher than in the 2020 (14.5%) sample and the 2021 (16.5%) sample. This worrying increase of an already high level of suicidal ideation among students measured by the PHQ-9 cannot be sufficiently explained by the analyzed data of this survey, but the magnitude is comparable with other recent results from other countries (71). It may be explained by the fact that, during the pandemic outbreak, death became a more salient topic in everyday life, communication, and in all media contents. Additionally, a large proportion of the population experienced the loss of family members or beloved ones among the over 150,000 deaths due to COVID-19 in Germany (72). Nevertheless, recent studies indicate that an increased salience of death due to the COVID-19 pandemic would also be associated with an increase in the level of depressive symptoms, which was not the case in the present study (73–75). Additionally, Russia's invasion of Ukraine, which started in February 2022, the recent energy crisis, economic changes, rising inflation rates, climate change and related worry in youths and adolescents (76–78) could, to some extent, contribute to an explanation of this specific increase in only suicidal ideation, but further research is needed.
It might also be important to take aspects of loneliness and social isolation into account to potentially explain the recent results regarding suicidal ideation in university students. Feeling alone and a lack of social contacts can cause several uncomfortable feelings and tension- and could additionally be understood as a lack of distraction from suicidal thoughts (if already present) and yield in higher rumination behavior. Following this, coronavirus-related NPIs could be understood as making vulnerable people even more vulnerable to suicidal thoughts and reduce the desire to live (79). Still, it remains unclear, if suicidal ideation (in the current situation after 2 years of pandemic and several lockdowns) comports with higher depressive symptoms, or not. Some studies report it does (triggered by various risk factors such as stress, fears of contracting the infection from others, financial instability) (80–84), some does, it might occur (and change) independently (85)—as in the present study.
4.2. Social and emotional outcomes and comparisons to previous survey results from 2020 and 2021
Results of the present analysis implied that scores for resilience, social support, general self-efficacy, perceived stress, and loneliness differed significantly between the three surveys.
The scores for social support, self-efficacy, and resilience all showed a continuous decrease, when comparing the 2020, 2021, and 2022 in chronological order. The reported levels of social support and loneliness by the university students did not (fully) recover in the 2022 sample, when compared to the 2020 sample, which might be explained by a sustainable loss of relationships due to extended lock-down periods and phases of social isolation, which is also in line with the results of a recent longitudinal study across several countries (86).
There were significant differences between the reported scores for resilience, self-efficacy and perceived stress across the three samples in university students. However, the directions of these changes were not consistent, and interpretability remains limited because the present study is not longitudinal and resilience and self-efficacy are generally considered rather stable traits. There is consensus that resilience and self-efficacy are important protective factors and associated with positive mental health (26–28), but it remains unclear if and where changes might occur due to the pandemic.
4.3. Predictors of mental health outcomes
In the present analysis, while controlling for a past diagnosis of mental disorders, higher perceived stress and loneliness significantly predicted higher levels of depressive symptoms, while resilience and social support were identified as protective factors- which is in line with previous results from the other time points (9, 16). However, results concerning the role of age and gender seem inconsistent in the literature: gender was either found to be a significant predictor limited to symptoms of anxiety (in U.S. students) (87) and panic but not for depression (in German students) (88). Being female was identified as a risk factor (30, 89–92) and being male as a protective factor (93) in some German studies. Older age was identified as a risk factor for depressive symptoms by Karing (31) whereas being younger was also found to be a risk factor for heightened distress (94) while another study reported no significant effects on depression, depressive symptoms, or anxiety related to the age of students in German students (32). Also, in line with other recent literature (35), not having received a vaccination and not intending to do so was a significant predictor for lower levels of anxiety, though only marginally so.
Factors with more consistent results across the literature on German students were loneliness and stress as risk factors (29–32) and social support as an overall protective factor (32, 90, 91). Bearing in mind that the considered studies were conducted through different phases of the pandemic while using a heterogenous set of measurements and reporting on various samples of university students, it is crucial to aim for clarification through further research.
4.4. Strengths and limitations
This study has several strengths and limitations. First, a major limitation is the cross-sectional design across all three time points. Because of the anonymity of the surveys, it was not possible to identify participants who participated in which (or all of the) surveys. Nevertheless, these nearly identical surveys across three time points over 3 years of pandemic in Germany provide very important insights into mental health outcomes and changes in mental health and related variables in university students. All surveys were conducted in a large German university, including various faculties and students in different stages of their studies and high response rates. However, the generalizability might be limited due to the reliance on a convenience sample, a possible self-selection bias of students with a mental disorder and the fact that only self-report measures had been applied. Furthermore, the sample does not represent the general student population, as certain groups, women, master program students and students without a migratory background were overrepresented. Additionally, due to the observational character of the study, causal inferences cannot be made.
5. Conclusion
In general, the results of the present study confirm previous results and results from the international literature that the pandemic had and still has a negative impact on the mental health of university students. The present study broadens this view by the fact that some areas seem to recover quicker, while others seem to increase worryingly. Especially the persistent rise in suicidal ideation from 2020 to 2021 and to 2022, a constant reduction in reported social support and associated perceived loneliness is concerning. The claim for low-threshold and accessible mental health support for university students remains the same as in 2021 (9) and should get more impetus by the present results, regardless of some positive results. Still, online interventions seem to be feasible, evidence-based, easy to implement and promising to fulfill this need of young students. In addition, barriers to accessing the mental health care system should be reduced, not exclusively but especially for young individuals, to prevent the chronification of mental health issues.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Medical Faculty, University Leipzig, Germany. The patients/participants provided their written informed consent to participate in this study.
Author contributions
LG, EK, SB, and CR-K designed the study. LG performed the statistical analysis. LG and EK drafted the article. LG, EK, SB, TB, JS, and CR-K discussed the results and contributed to the final manuscript. All authors have approved the final manuscript.
Funding
This work was funded by the Saxon Ministry for Science, Culture and Tourism (Sächsisches Staatsministerium für Wissenschaft, Kultur und Tourismus; SMWK) with tax funds on the basis of the budget approved by the Saxon State Parliament (grant No: 100586917). This manuscript was funded by the Open Access Publishing Fund of Leipzig University supported by the German Research Foundation within the program Open Access Publication Funding.
Acknowledgments
The authors would like to thank all the students for the participation in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Solmi M, Radua J, Olivola M, Croce E, Soardo L, Salazar de Pablo G, et al. Age at onset of mental disorders worldwide: large-scale meta-analysis of 192 epidemiological studies. Mol Psychiatry. (2022) 27:281–95. doi: 10.1038/s41380-021-01161-7
2. Auerbach RP, Alonso J, Axinn WG, Cuijpers P, Ebert DD, Green JG, et al. Mental disorders among college students in the world health organization world mental health surveys. Psychol Med. (2016) 46:2955–70. doi: 10.1017/S0033291716001665
3. Schaller K, Kahnert S, Garcia-Verdugo R, Treede I, Graen L, Ouédraogo N. Alkoholatlas Deutschland 2022. Lengerich: Pabst Science Publishers (2022), p. 166.
4. Schaller K, Kahnert S, Mons U. Alkoholatlas Deutschland. Lengerich, Westf: Pabst Science Publishers (2017), p. 152.
5. Bruffaerts R, Mortier P, Auerbach RP, Alonso J, La Hermosillo De Torre AE, Cuijpers P, et al. Lifetime and 12-month treatment for mental disorders and suicidal thoughts and behaviors among first year college students. Int J Methods Psychiatr Res. (2019) 28:e1764. doi: 10.1002/mpr.1764
6. WHO. Timeline: WHO's COVID-19 response. (2022). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline#event-0 (accessed Aug 24, 2022).
7. Ge Y, Zhang W-B, Wu X, Ruktanonchai CW, Liu H, Wang J, et al. Untangling the changing impact of non-pharmaceutical interventions and vaccination on European COVID-19 trajectories. Nat Commun. (2022) 13:3106. doi: 10.1038/s41467-022-30897-1
8. Le Huy D, Nguyen NT, Phuc PT, Huang C-C. The effects of non-pharmaceutical interventions on COVID-19 epidemic growth rate during pre- and post-vaccination period in Asian Countries. Int J Environ Res Public Health. (2022) 19:1139. doi: 10.3390/ijerph19031139
9. Dogan-Sander E, Kohls E, Baldofski S, Rummel-Kluge C. More Depressive symptoms, alcohol and drug consumption: increase in mental health symptoms among University students after one year of the COVID-19 pandemic. Front Psychiatry. (2021) 12:790974. doi: 10.3389/fpsyt.2021.790974
10. Kim H, Rackoff GN, Fitzsimmons-Craft EE, Shin KE, Zainal NH, Schwob JT, et al. College mental health before and during the COVID-19 pandemic: results from a nationwide survey. Cognit Ther Res. (2022) 46:1–10. doi: 10.1007/s10608-021-10241-5
11. Elharake JA, Akbar F, Malik AA, Gilliam W, Omer SB. Mental health impact of COVID-19 among children and college students: a systematic review. Child Psychiatry Hum Dev. (2022). doi: 10.1007/s10578-021-01297-1
12. Chen T, Lucock M. The mental health of university students during the COVID-19 pandemic: an online survey in the UK. PLoS ONE. (2022) 17:e0262562. doi: 10.1371/journal.pone.0262562
13. Li Y, Wang A, Wu Y, Han N, Huang H. Impact of the COVID-19 Pandemic on the mental health of college students: a systematic review and meta-analysis. Front Psychol. (2021) 12:669119. doi: 10.3389/fpsyg.2021.669119
14. Tagesschau D. Einigung auf umfassendes Kontaktverbot: Maßnahmen gegen Coronavirus. (2020). Available online at: https://www.tagesschau.de/inland/kontaktverbot-coronavirus-101.html (accessed Aug 30, 2022).
15. Presse-und Informationsamt der Bundesregierung. Telefonkonferenz der Bundeskanzlerin mit den Regierungschefinnen und Regierungschefs der Länder am 30. April 2020. (2020), p. 8.
16. Kohls E, Baldofski S, Moeller R, Klemm S-L, Rummel-Kluge C. Mental health, social and emotional well-being, and perceived burdens of university students during COVID-19 pandemic lockdown in Germany. Front Psychiatry. (2021) 12:643957. doi: 10.3389/fpsyt.2021.643957
17. Fang Y, Ji B, Liu Y, Zhang J, Liu Q, Ge Y, et al. The prevalence of psychological stress in student populations during the COVID-19 epidemic: a systematic review and meta-analysis. Sci Rep. (2022) 12:12118. doi: 10.1038/s41598-022-16328-7
18. Murphy L, Markey K. O' Donnell C, Moloney M, Doody O. The impact of the COVID-19 pandemic and its related restrictions on people with pre-existent mental health conditions: A scoping review. Arch Psychiatr Nurs. (2021) 35:375–94. doi: 10.1016/j.apnu.2021.05.002
19. Statistisches Bundesamt. Krankheitskosten: Deutschland, Jahre, Krankheitsdiagnosen (ICD-10), Geschlecht, Altersgruppen. (2022). Available online at: https://www-genesis.destatis.de/genesis/online?sequenz=tabelleErgebnis&selectionname=23631-0003&sachmerkmal=ICD10Y&sachschluessel=ICD10-F32-F34&transponieren=true#abreadcrumb (accessed Mar 11, 2023).
20. Bundesanstalt für Arbeitsschutz und Arbeitsmedizin. Volkswirtschaftliche Kosten durch Arbeitsunfähigkeit. Available online at: https://www.baua.de/DE/Themen/Arbeitswelt-und-Arbeitsschutz-im-Wandel/Arbeitsweltberichterstattung/Kosten-der-AU/Kosten-der-Arbeitsunfaehigkeit_node.html (accessed Mar 11, 2023).
21. Charles NE, Strong SJ, Burns LC, Bullerjahn MR, Serafine KM. Increased mood disorder symptoms, perceived stress, and alcohol use among college students during the COVID-19 pandemic. Psychiatry Res. (2021) 296:113706. doi: 10.1016/j.psychres.2021.113706
22. Meda N, Pardini S, Slongo I, Bodini L, Zordan MA, Rigobello P, et al. Students' mental health problems before, during, and after COVID-19 lockdown in Italy. J Psychiatr Res. (2021) 134:69–77. doi: 10.1016/j.jpsychires.2020.12.045
23. Chan AC, Piehler TF, Ho GW. Resilience and mental health during the COVID-19 pandemic: findings from Minnesota and Hong Kong. J Affect Disord. (2021) 295:771–80. doi: 10.1016/j.jad.2021.08.144
24. Hu T, Zhang D, Wang J, A. meta-analysis of the trait resilience and mental health. Pers Individ Dif. (2015) 76:18–27. doi: 10.1016/j.paid.2014.11.039
25. Riehm KE, Brenneke SG, Adams LB, Gilan D, Lieb K, Kunzler AM, et al. Association between psychological resilience and changes in mental distress during the COVID-19 pandemic. J Affect Disord. (2021) 282:381–5. doi: 10.1016/j.jad.2020.12.071
26. Kowalski E, Graf J, Schneider A, Zipfel S, Stengel A. Resilienz und Selbstwirksamkeitserwartung hängen mit der Wahrnehmung der COVID-19-Symptomatik, der psychischen Gesundheit und dem Umgang mit einer akuten COVID-19-Infektion zusammen. Psychother Psychosom Med Psychol. (2022). doi: 10.1055/a-1876-2777
27. Peñacoba C, Catala P, Velasco L, Carmona-Monge FJ, Garcia-Hedrera FJ, Gil-Almagro F. Stress and quality of life of intensive care nurses during the COVID-19 pandemic: self-efficacy and resilience as resources. Nurs Crit Care. (2021) 26:493–500. doi: 10.1111/nicc.12690
28. Hong J, Mreydem HW, Abou Ali BT, Saleh NO, Hammoudi SF, Lee J, et al. Mediation effect of self-efficacy and resilience on the psychological well-being of lebanese people during the crises of the COVID-19 pandemic and the Beirut explosion. Front Psychiatry. (2021) 12:733578. doi: 10.3389/fpsyt.2021.733578
29. Weber M, Schulze L, Bolzenkötter T, Niemeyer H, Renneberg B. Mental health and loneliness in university students during the COVID-19 pandemic in Germany: a longitudinal study. Front Psychiatry. (2022) 13:1–11. doi: 10.3389/fpsyt.2022.848645
30. Supke M, Hahlweg K, Kelani K, Muschalla B, Schulz W. Mental health, partnerships, and sexual behavior of German university students after the third wave of the COVID-19 pandemic. J Am College Health. (2022) 1–10. doi: 10.1080/07448481.2022.2119398
31. Karing C. Prevalence and predictors of anxiety, depression and stress among university students during the period of the first lockdown in Germany. J Affect Disorders Rep. (2021) 5:100174. doi: 10.1016/j.jadr.2021.100174
32. Matos Fialho PM, Spatafora F, Kühne L, Busse H, Helmer SM, Zeeb H, et al. Perceptions of study conditions and depressive symptoms during the COVID-19 pandemic among university students in Germany: results of the international COVID-19 student wellbeing study. Front Public Health. (2021) 9:674665. doi: 10.3389/fpubh.2021.674665
33. Seddig D, Maskileyson D, Davidov E, Ajzen I, Schmidt P. Correlates of COVID-19 vaccination intentions: attitudes, institutional trust, fear, conspiracy beliefs, and vaccine skepticism. Soc Sci Med. (2022) 302:114981. doi: 10.1016/j.socscimed.2022.114981
34. Seddig D, Maskileyson D, Davidov E. Vaccination against COVID-19 reduces virus-related fears: findings from a German longitudinal study. Front Public Health. (2022) 10:878787. doi: 10.3389/fpubh.2022.878787
35. Mertens G, Lodder P, Smeets T, Duijndam S. Fear of COVID-19 predicts vaccination willingness 14 months later. J Anxiety Disord. (2022) 88:102574. doi: 10.1016/j.janxdis.2022.102574
36. Willis DE, Andersen JA, Bryant-Moore K, Selig JP, Long CR, Felix HC, et al. COVID-19 vaccine hesitancy: race/ethnicity, trust, and fear. Clin Transl Sci. (2021) 14:2200–7. doi: 10.1111/cts.13077
37. Alimoradi Z, Ohayon MM, Griffiths MD, Lin C-Y, Pakpour AH. Fear of COVID-19 and its association with mental health-related factors: systematic review and meta-analysis. BJPsych Open. (2022) 8:e73. doi: 10.1192/bjo.2022.26
38. Simşir Z, Koç H, Seki T, Griffiths MD. The relationship between fear of COVID-19 and mental health problems: a meta-analysis. Death Stud. (2022) 46:515–23. doi: 10.1080/07481187.2021.1889097
39. Bauer S, Winn S, Schmidt U, Kordy H. Construction, scoring and validation of the short evaluation of eating disorders (SEED). Eur Eat Disorders Rev. (2005) 13:191–200. doi: 10.1002/erv.637
40. Middendorff E, Apolinarski B, Becker K, Bornkessel P, Brandt T, Heißenberg S, et al. Die wirtschaftliche und soziale Lage der Studierenden in Deutschland 2016: 21. Sozialerhebung des Deutschen Studentenwerks durchgeführt vom Deutschen Zentrum für Hochschul- und Wissenschaftsforschung. Berlin (2017), p. 196.
41. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Int Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
42. Gräfe K, Zipfel S, Herzog W, Löwe B. Screening psychischer Störungen mit dem “Gesundheitsfragebogen für Patienten (PHQ-D). Diagnostica. (2004) 50:171–81. doi: 10.1026/0012-1924.50.4.171
43. Allen JP, Litten RZ, Fertig JB, Babor T. A review of research on the alcohol use disorders identification test (AUDIT). Alcoholism Clin Exp Res. (1997) 21:613–9. doi: 10.1111/j.1530-0277.1997.tb03811.x
44. Higgins-Biddle JC, Babor TF. A review of the alcohol use disorders identification test (AUDIT), AUDIT-C, and USAUDIT for screening in the United States: past issues and future directions. Am J Drug Alcohol Abuse. (2018) 44:578–86. doi: 10.1080/00952990.2018.1456545
45. Ganz T, Braun M, Laging M, Heidenreich T. Erfassung des riskanten Alkoholkonsums bei Studierenden deutscher Hochschulen. Zeitschrift für Klinische Psychologie und Psychotherapie. (2017) 46:187–97. doi: 10.1026/1616-3443/a000432
46. Kliem S, Mößle T, Zenger M, Strauß B, Brähler E, Hilbert A. The eating disorder examination-questionnaire 8: a brief measure of eating disorder psychopathology (EDE-Q8). Int J Eat Disord. (2016) 49:613–6. doi: 10.1002/eat.22487
47. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
48. Löwe B, Decker O, Müller S, Brähler E, Schellberg D, Herzog W, et al. Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Med Care. (2008) 46:266–74. doi: 10.1097/MLR.0b013e318160d093
49. Sisto A, Vicinanza F, Campanozzi LL, Ricci G, Tartaglini D, Tambone V. Towards a transversal definition of psychological resilience: a literature review. Medicina. (2019) 55:745. doi: 10.3390/medicina55110745
50. Fletcher D, Sarkar M. Psychological resilience. Eur Psychol. (2013) 18:12–23. doi: 10.1027/1016-9040/a000124
51. Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. (2008) 15:194–200. doi: 10.1080/10705500802222972
52. Chmitorz A, Wenzel M, Stieglitz R-D, Kunzler A, Bagusat C, Helmreich I, et al. Population-based validation of a German version of the brief resilience scale. PLoS ONE. (2018) 13:e0192761. doi: 10.1371/journal.pone.0192761
53. Jerusalem M, Schwarzer R. Dokumentation der psychometrischen Verfahren im Rahmen der Wissenschaftlichen Begleitung des Modellversuchs Selbstwirksame Schulen: Skalen zur erfassung von Lehrer-und schülermerkmalen. Berlin: Freie Universität berlin (1999), p. 133.
54. Mitchell P, Powell L, Blumenthal J, Norten J, Ironson G, Pitula CR, et al. A short social support measure for patients recovering from myocardial infarction: the Enrichd social support inventory. J Cardiopulm Rehabil Prev. (2003) 23:398–403. doi: 10.1097/00008483-200311000-00001
55. Kendel F, Spaderna H, Sieverding M, Dunkel A, Lehmkuhl E, Hetzer R, et al. Eine deutsche Adaptation des ENRICHD social support Inventory (ESSI). Diagnostica. (2011) 57:99–106. doi: 10.1026/0012-1924/a000030
56. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. (1983) 24:385. doi: 10.2307/2136404
57. Steptoe A, Shankar A, Demakakos P, Wardle J. Social isolation, loneliness, and all-cause mortality in older men and women. Proc Natl Acad Sci USA. (2013) 110:5797–801. doi: 10.1073/pnas.1219686110
58. Blanca MJ, Alarcón R, Arnau J, Bono R. Bendayan R. Effect of variance ratio on ANOVA robustness: Might 15 be the limit? Behav Res Methods. (2018) 50:937–62. doi: 10.3758/s13428-017-0918-2
59. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Milton Park: Routledge. (2013). doi: 10.4324/9780203771587
60. Chowdhury U, Suvro MA, Farhan SM, Uddin MJ. Depression and stress regarding future career among university students during COVID-19 pandemic. PLoS ONE. (2022) 17:e0266686. doi: 10.1371/journal.pone.0266686
61. Fruehwirth JC, Biswas S, Perreira KM. The Covid-19 pandemic and mental health of first-year college students: examining the effect of Covid-19 stressors using longitudinal data. PLoS ONE. (2021) 16:e0247999. doi: 10.1371/journal.pone.0247999
62. Gao D, Xiang Q, Lu G, Tong J, Jiang W, Yu X, et al. Evaluation and analysis of anxiety and depression symptoms for college students during COVID-19 pandemic. BMC Psychol. (2022) 10:227. doi: 10.1186/s40359-022-00934-1
63. Kavvadas D, Kavvada A, Karachrysafi S, Papaliagkas V, Cheristanidis S, Chatzidimitriou M, et al. Stress, anxiety and depression prevalence among greek university students during COVID-19 pandemic: a two-year survey. J Clin Med. (2022) 11:4263. doi: 10.3390/jcm11154263
64. Ebert DD, Mortier P, Kaehlke F, Bruffaerts R, Baumeister H, Auerbach RP, et al. Barriers of mental health treatment utilization among first-year college students: First cross-national results from the WHO World Mental Health International College Student Initiative. Int J Methods Psychiatr Res. (2019) 28:e1782. doi: 10.1002/mpr.1782
65. Fernandez MD, Vieira IS, Silva NR, Cardoso Td, Bielavski CH, Rakovski C, et al. Anxiety symptoms and alcohol abuse during the COVID-19 pandemic: a cross-sectional study with Brazilian dental undergraduate students. J Dent Educ. (2021) 85:1739–48. doi: 10.1002/jdd.12742
66. Lechner WV, Laurene KR, Patel S, Anderson M, Grega C, Kenne DR. Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. Addict Behav. (2020) 110:106527. doi: 10.1016/j.addbeh.2020.106527
67. Graupensperger S, Jaffe AE, Fleming CN, Kilmer JR, Lee CM, Larimer ME. Changes in college student alcohol use during the COVID-19 pandemic: are perceived drinking norms still relevant? Emerg Adulthood. (2021) 9:531–40. doi: 10.1177/2167696820986742
68. Yehudai M, Bender S, Gritsenko V, Konstantinov V, Reznik A, Isralowitz R. COVID-19 fear, mental health, and substance misuse conditions among university social work students in Israel and Russia. Int J Ment Health Addict. (2022) 20:316–23. doi: 10.1007/s11469-020-00360-7
69. Zysset A, Volken T, Amendola S, Wyl A. von, Dratva J. Change in alcohol consumption and binge drinking in university students during the early COVID-19 pandemic. Front Public Health. (2022) 10:854350. doi: 10.3389/fpubh.2022.854350
70. Bountress KE, Cusack SE, Conley AH, Aggen SH, The SF Vassileva J. The COVID-19 pandemic impacts psychiatric outcomes and alcohol use among college students. Eur J Psychotraumatol. (2022) 13:2022279. doi: 10.1080/20008198.2021.2022279
71. Batterham PJ, Calear AL, Shou Y, Farrer LM, Gulliver A, McCallum SM, et al. Effects of the COVID-19 pandemic on suicidal ideation in a representative Australian population sample-Longitudinal cohort study. J Affect Disord. (2022) 300:385–91. doi: 10.1016/j.jad.2022.01.022
72. Robert Koch Institut. COVID-19: Fallzahlen in Deutschland und weltweit. Available online at: https://www.rki.de/DE/Content/InfAZ/N/Neuartiges_Coronavirus/Fallzahlen.html (accessed Oct 27, 2022).
73. Sapara A, Shalaby R, Osiogo F, Hrabok M, Gusnowski A, Vuong W, et al. COVID-19 pandemic: demographic and clinical correlates of passive death wish and thoughts of self-harm among Canadians. J Ment Health. (2021) 30:170–8. doi: 10.1080/09638237.2021.1875417
74. Evers NF, Greenfield PM, Evers GW. COVID-19 shifts mortality salience, activities, and values in the United States: Big data analysis of online adaptation. Hum Behav Emerg Technol. (2021) 3:107–26. doi: 10.1002/hbe2.251
75. Fairlamb S. The relationship between COVID-19-induced death thoughts and depression during a national lockdown. J Health Psychol. (2021) 27: 2770-2776. doi: 10.1177/13591053211067102
76. Sanson A, Dubicka B. Editorial: the climate and ecological mental health emergency - evidence and action. Child Adolesc Ment Health. (2022) 27:1–3. doi: 10.1111/camh.12540
77. Oswald TK, Langmaid GR. Considering ecological determinants of youth mental health in the era of COVID-19 and the Anthropocene: a call to action from young public health professionals. Health Promot J Austr. (2022) 33:324–8. doi: 10.1002/hpja.560
78. Leonhardt M, Granrud MD, Bonsaksen T, Lien L. Associations between mental health, lifestyle factors and worries about climate change in Norwegian adolescents. Int J Environ Res Public Health. (2022) 19:12826. doi: 10.3390/ijerph191912826
79. van der Burgt MC, Mérelle S, Beekman AT, Gilissen R. The impact of COVID-19 on the suicide prevention helpline in the Netherlands. Crisis. (2022). doi: 10.1027/0227-5910/a000863
80. Ganesan B, Al-Jumaily A, Fong KN, Prasad P, Meena SK, Tong RK-Y. Impact of coronavirus disease 2019 (COVID-19) outbreak quarantine, isolation, and lockdown policies on mental health and suicide. Front Psychiatry. (2021) 12:565190. doi: 10.3389/fpsyt.2021.565190
81. Reger MA, Stanley IH, Joiner TE. Suicide mortality and coronavirus disease 2019-a perfect storm? JAMA Psychiatry. (2020) 77:1093–4. doi: 10.1001/jamapsychiatry.2020.1060
82. Gunnell D, Appleby L, Arensman E, Hawton K, John A, Kapur N, et al. Suicide risk and prevention during the COVID-19 pandemic. The Lancet Psychiatry. (2020) 7:468–71. doi: 10.1016/S2215-0366(20)30171-1
83. Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. Lancet. (2009) 374:315–23. doi: 10.1016/S0140-6736(09)61124-7
84. Bersia M, Koumantakis E, Berchialla P, Charrier L, Ricotti A, Dalmasso P, et al. Suicide spectrum among young people in early phases of the COVID-19 pandemic: a systematic review and meta-analysis. SSRN J. (2022). doi: 10.2139/ssrn.4143702
85. Batterham PJ, van Spijker BA, Mackinnon AJ, Calear AL, Wong Q, Christensen H. Consistency of trajectories of suicidal ideation and depression symptoms: evidence from a randomized controlled trial. Depress Anxiety. (2019) 36:321–9. doi: 10.1002/da.22863
86. van Breen JA, Kutlaca M, Koç Y, Jeronimus BF, Reitsema AM, Jovanović V, et al. Lockdown lives: a longitudinal study of inter-relationships among feelings of loneliness, social contacts, and solidarity during the COVID-19 lockdown in early 2020. Pers Soc Psychol Bull. (2022) 48:1315–30. doi: 10.31234/osf.io/hx5kt
87. Fu SQ, Greco LM, Lennard AC, Dimotakis N. Anxiety responses to the unfolding COVID-19 crisis: patterns of change in the experience of prolonged exposure to stressors. J Appl Psychol. (2021) 106:48–61. doi: 10.1037/apl0000855
88. Holm-Hadulla RM, Klimov M, Juche T, Möltner A, Herpertz SC. Wellbeing and mental health of students during the COVID-19 pandemic. Psychopathology. (2021) 54:291–7. doi: 10.1159/000519366
89. Elmer T, Mepham K, Stadtfeld C. Students under lockdown: comparisons of students' social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE. (2020) 15:e0236337. doi: 10.1371/journal.pone.0236337
90. Voltmer E, Köslich-Strumann S, Walther A, Kasem M, Obst K, Kötter T. The impact of the COVID-19 pandemic on stress, mental health and coping behavior in German University students—a longitudinal study before and after the onset of the pandemic. BMC Public Health. (2021) 21:1–15. doi: 10.1186/s12889-021-11295-6
91. Werner AM, Tibubos AN, Mülder LM, Reichel JL, Schäfer M, Heller S, et al. The impact of lockdown stress and loneliness during the COVID-19 pandemic on mental health among university students in Germany. Sci Rep. (2021) 11:1–11. doi: 10.1038/s41598-021-02024-5
92. Cordes A, Herrmann-Lingen C, Büchner B, Hessel A. Repräsentative normierung des ENRICHD-social-support-instrument (ESSI)—deutsche version. Klinische Diagnostik und Evaluat. (2009) 2:16–32.
93. Gewalt SC, Berger S, Krisam R, Breuer M. Effects of the COVID-19 pandemic on university students' physical health, mental health and learning, a cross-sectional study including 917 students from eight universities in Germany. PLoS ONE. (2022) 17:e0273928. doi: 10.1371/journal.pone.0273928
Keywords: COVID-19, university students, mental health, depressive symptoms, alcohol consumption, symptoms of anxiety
Citation: Kohls E, Guenthner L, Baldofski S, Brock T, Schuhr J and Rummel-Kluge C (2023) Two years COVID-19 pandemic: Development of university students' mental health 2020–2022. Front. Psychiatry 14:1122256. doi: 10.3389/fpsyt.2023.1122256
Received: 12 December 2022; Accepted: 21 March 2023;
Published: 06 April 2023.
Edited by:
S. M. Yasir Arafat, Enam Medical College, BangladeshReviewed by:
Abid Hasan Khan, Bangabandhu Sheik Mujib Medical University (BSMMU), BangladeshStefanie Maria Helmer, University of Bremen, Germany
Copyright © 2023 Kohls, Guenthner, Baldofski, Brock, Schuhr and Rummel-Kluge. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christine Rummel-Kluge, Q2hyaXN0aW5lLlJ1bW1lbC1LbHVnZUBtZWRpemluLnVuaS1sZWlwemlnLmRl
†These authors share first authorship
 Elisabeth Kohls
Elisabeth Kohls Lukas Guenthner
Lukas Guenthner Sabrina Baldofski
Sabrina Baldofski Tanja Brock3
Tanja Brock3 Jan Schuhr
Jan Schuhr Christine Rummel-Kluge
Christine Rummel-Kluge