- 1Department of Epidemiology and Public Health, University of Ottawa, Ottawa, ON, Canada
- 2Counselling Psychology, Faculty of Education, University of Ottawa, Ottawa, ON, Canada
- 3Department of Psychiatry Research, Zucker Hillside Hospital, Northwell Health, Glen Oaks, NY, United States
- 4Donald and Barbara Zucker School of Medicine at Hofstra/Northwell Health, Hempstead, NY, United States
- 5Department of Psychology, University of Ottawa, Ottawa, ON, Canada
There is a notable disparity between the observed prevalence of schizophrenia-spectrum disorders in racialized persons in the United States and Canada and White individuals in these same countries, with Black people being diagnosed at higher rates than other groups. The consequences thereof bring a progression of lifelong punitive societal implications, including reduced opportunities, substandard care, increased contact with the legal system, and criminalization. Other psychological conditions do not show such a wide racial gap as a schizophrenia-spectrum disorder diagnosis. New data show that the differences are not likely to be genetic, but rather societal in origin. Using real-life examples, we discuss how overdiagnoses are largely rooted in the racial biases of clinicians and compounded by higher rates of traumatizing stressors among Black people due to racism. The forgotten history of psychosis in psychology is highlighted to help explain disparities in light of the relevant historical context. We demonstrate how misunderstanding race confounds attempts to diagnose and treat schizophrenia-spectrum disorders in Black individuals. A lack of culturally informed clinicians exacerbates problems, and implicit biases prevent Black patients from receiving proper treatment from mainly White mental healthcare professionals, which can be observed as a lack of empathy. Finally, we consider the role of law enforcement as stereotypes combined with psychotic symptoms may put these patients in danger of police violence and premature mortality. Improving treatment outcomes requires an understanding of the role of psychology in perpetuating racism in healthcare and pathological stereotypes. Increased awareness and training can improve the plight of Black people with severe mental health disorders. Essential steps necessary at multiple levels to address these issues are discussed.
1. Introduction
In the words of Martin Luther King Jr., “Of all the forms of inequality, injustice in health is the most shocking and the most inhuman…” (1).
2. Psychotic disorders in the United States and Canada
Psychosis is understood broadly to refer to mental states that involve a disconnect from reality. Positive symptoms include hallucinations (perceiving things that are not present, which can be auditory, tactile, visual, olfactory, or taste), delusions (false beliefs that are not easily changed), and disorganized thinking, speech, or behavior (2). Negative symptoms include difficulties with emotional and facial expressions, speech, thinking, task commencement, motivation, and social withdrawal. Other symptoms include cognitive deficits. Psychosis can be a symptom of many different mental and physical disorders such as schizophrenia as well as bipolar disorder and major depressive disorder (MDD), so there is no one simple course, presentation, or cause. Rather, research indicates that a psychotic episode can be brought on by a combination of factors. Biological factors, including genetic factors from genome-wide studies, emphasize the connections between common mental disorders and genes that regulate specific neuronal functions (3, 4). While genetic factors may increase the risk of experiencing psychosis, it is environmental stressors [such as traumatic life events, autoimmune insult, or substance use; (3, 4)] that often act as the trigger and barriers to care such as lack of knowledge about the symptoms, lack of possibilities for treatment (i.e., no local specialists), and lack of access (i.e., no insurance) which can exacerbate the condition.
Therefore, it is imperative that disorders that include psychosis are correctly diagnosed with adequate consideration of environmental factors, to receive appropriate care and early intervention, which can improve prognosis. In this paper, the term “psychotic disorders” will refer broadly to all schizophrenia-spectrum disorders and other conditions that may include psychotic episodes (e.g., bipolar disorder and severe MDD), whereas the term “schizophrenia-spectrum disorders” refers to all disorders in this category, as per the DSM-5. In the interest of space, we will not be focusing on MDD or bipolar disorder, although these disorders may include psychosis, and as such, many of the same issues still apply.
The literature suggests that schizophrenia-spectrum disorders affect up to 4% of the population (5), and for the subset of those affected by schizophrenia, the global prevalence is 1 in 300 people (0.32%) or 24 million people, as shown in Table 1 (6). In the United States, schizophrenia similarly affects 0.25–0.65% of the population [~2.6 million adults aged 18 years and older; (6, 7)], and 40% of individuals with schizophrenia go untreated in any given year. However, counting those with schizophrenia in the United States is complicated, and there is an undercount because so many are incarcerated, homeless, suffer an early death, or are otherwise excluded from official treatment channels. Therefore, a more accurate count based on the 2020 census reaches 1.62%, or 3.8 million adults, which is significantly higher than previous prevalence estimates (7).
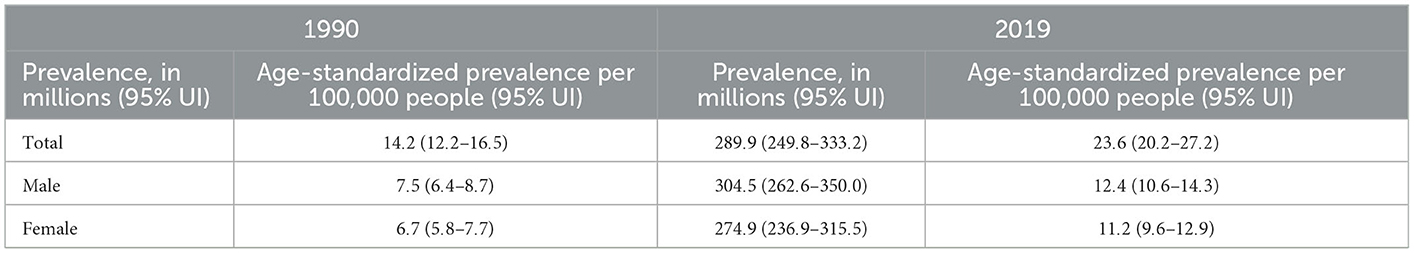
Table 1. Global prevalence and age-standardized prevalence for schizophrenia in 1990 and 2019 (6).
The development of schizophrenia-spectrum disorders has been found to vary by gender, with men experiencing the onset of symptoms earlier (late teens to early twenties) and women experiencing them later (early twenties to early thirties). Individuals with a family history of mental illness are at a higher risk of developing schizophrenia-spectrum disorders (8). The early adulthood or late adolescence onset of schizophrenia is particularly tragic as it negatively affects the trajectory of young people as they are poised to embark on an independent life. Globally, schizophrenia is among the top ten causes of disability-adjusted life-years. The annual costs in Canada of schizophrenia are estimated to reach up to Canadian $10 billion (5), while in the United States, the staggering direct and indirect costs of schizophrenia reached $281.6 billion in 2020. A large proportion of the direct costs are derived from healthcare, homelessness, incarceration, and necessary housing of these patients. The total lifetime economic cost of each individual diagnosed with schizophrenia at the age of twenty-five years comes to approximately $92,000 annually (9). These numbers testify to the urgent need for better care in this area.
3. Race and psychology (psychosis in the Black community)
In the United States and Canada, Black persons include those who are racialized as African American, Black American, Caribbean Black, and Black African, and may originate from any country. Persons racialized as Black typically have darker skin shades but may have any color of skin. Black is a racial grouping defined by the federal government (US Census Bureau, Statistics Canada) and is not the same as an ethnic group, nor synonymous with biological relatedness. For this study, Black refers to people racialized as Black by American and Canadian society who have some African ancestry.
In any conversation about racial disparities, it is common to wonder if observed differences are a reflection of socioeconomic differences (class and income). Although people of different classes may be treated differently in the healthcare system, the issue we are highlighting in this paper is specifically about Black people. Contrary to popular stereotypes, most Black people in the United States and Canada are middle class, not poor [81% of Black Americans are not in poverty; Figure 1; (10)]. Certainly, Black people are overrepresented among the poor, but this is due to racism, which takes us back to the issue of race, rather than socioeconomic status.
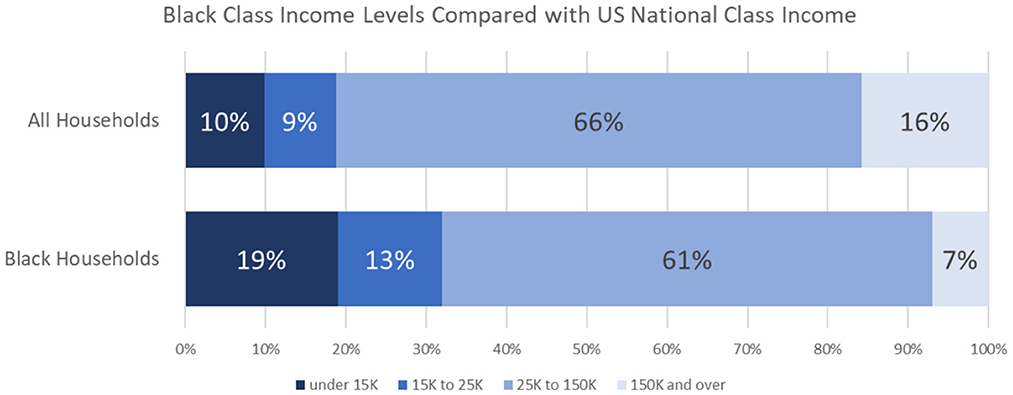
Figure 1. Socioeconomic class of Black households in the United States as compared with national class divisions.
Similarly, there are pathological stereotypes of Black people surrounding increased substance use, dysfunctional parenting, and poor social skills—which some might assume are factors in the development and maintenance of schizophrenia-spectrum disorders in this population. Addressing these false beliefs are beyond the scope of this paper; however, interested readers are directed to Williams et al. (11) and Jahn et al. (12) studies.
3.1. Epidemiology of race and psychosis
A national epidemiological study by Cohen and Marino (13) found that Black Americans had higher lifetime rates of disorders that included psychotic symptoms (15.3%) compared with Latino (13.6%), White (9.7%), and Asian Americans (9.6%). Furthermore, the lifetime probability of these disorders was associated with the Black and Hispanic race, the current level of disability, and a lifetime diagnosis of substance use disorder or posttraumatic stress disorder (PTSD). African American/Black communities are diagnosed with schizophrenia-spectrum disorders at a rate that is three to four times higher than White communities (14). Studies have shown that Black Americans are 2.4 times more likely to be diagnosed with schizophrenia (13) and are more likely to be diagnosed with schizophrenia-paranoid subtype or schizophrenia-undifferentiated subtype (14, 15). As will be further discussed, some of these disparities are due to clinician error, including overdiagnosis and misdiagnosis.
Finally, for Black people experiencing early symptoms of psychotic disorders, contact with law enforcement often represents the entry point into the medical system and is occurring even in the premorbid and prodromal stages (16). This means that these individuals have a high risk of becoming a target of law enforcement, due to negative stereotypes about Black people, which brings a host of negative life consequences (11, 17). Having been diagnosed with both a serious mental illness and a history of incarceration makes gainful employment nearly impossible. Furthermore, under United States laws, having a criminal record excludes both the patient and their family (if they live together) from assistance for public housing. Taken together, these inhumane and punitive barriers are a recipe for homelessness and marginalization and virtually ensure that first-episode patients will be unable to establish independent lives (16, 17).
3.2. Racism and psychosis
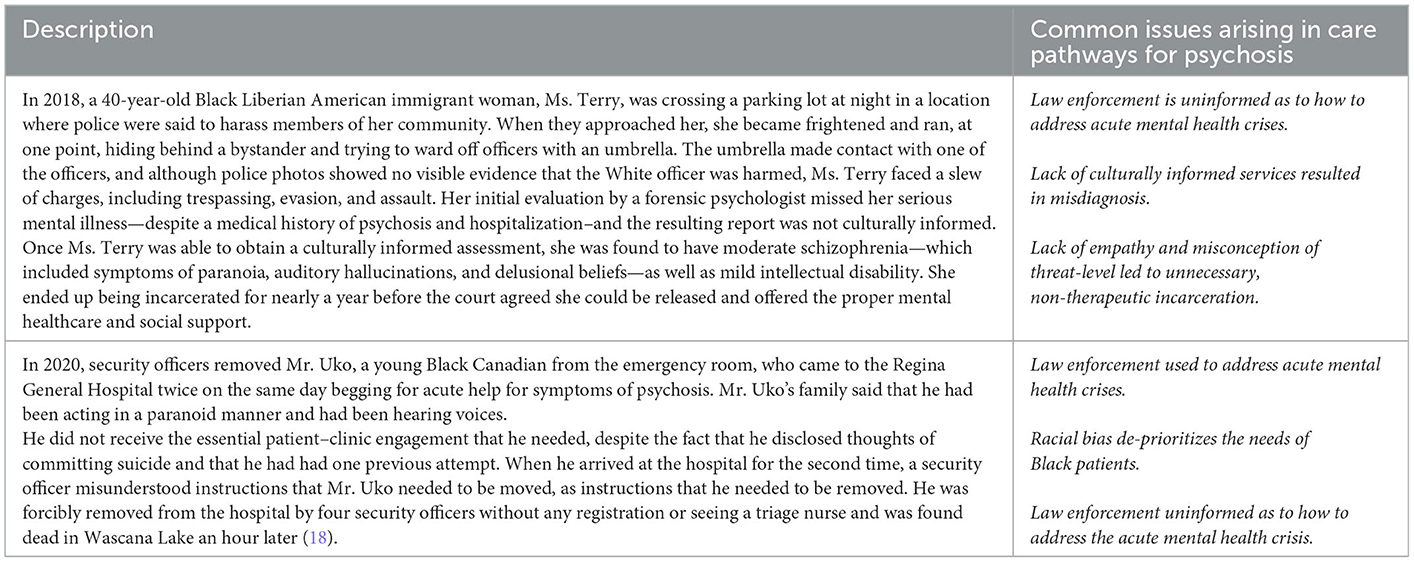
Black individuals suffering from psychotic disorders may be unable to access treatment or outright punished for becoming ill (Table 2). A case example, with which the authors were involved, is that of Grace Terry (pseudonym), a Black woman with schizophrenia who was incarcerated in the United States for allegedly evading arrest when frightened by police officers. In another example in Canada, Samuel Uko's family described that his race impacted how he was treated during his mental health crisis, leading to a fatal outcome. The CEO of the Saskatchewan Health Authority offered a formal apology, admitting that the staff spent too much time focusing on his identity rather than his care (18).
The situation today is that many Black people die because they do not have access to mental health services, but also because even when they have access they experience additional barriers once they are in the mental health services system (16). As a result of tragedies like this, there has been a public outcry from Black people across North America, noting a scarcity of providers representative of their communities and a lack of cultural competence in care [e.g., (19–21)].
3.3. Purpose of this paper
Racial disparities persist in mental health due to issues that include access to treatment and quality of care. Despite calls for cultural sensitivity and updates of diagnostic manuals, significant issues persist in diagnosis and treatment, especially in the case of psychotic disorders (14, 16, 22). Black individuals may have increased vulnerability to these disorders due to experiencing unique environmental stressors, such as alienation, discrimination, and racism, which contribute to etiology. Due to the double stigma of racism and having a serious mental illness, they are more likely to be marginalized and victimized by law enforcement.
The purpose of this study is to provide an overview of the experiences of Black people living in the United States and Canada with early schizophrenia-spectrum disorders and to discuss racially informed solutions for equitable mental healthcare. This study first describes racial differences in the diagnosis of schizophrenia-spectrum disorders; second, explains barriers to the treatment for Black communities; third, explains the role of bias and clinician empathy in misdiagnosis; fourth, describes the dangers of law enforcement involvement in mental health emergencies; and finally discusses solutions to address these disparities.
4. Medical racism and psychosis
4.1. Defining racism
To understand the connections among race, racism, racial discrimination, and psychosis, it is necessary to understand the terminology being used. Race is not a biological construct, but rather a sociopolitical construct that has no relevant genetic basis. The term racism refers to a system of beliefs (racial prejudices), practices (racial discrimination), and policies based on race that advantages individuals with historic power in most of the Western nations, including White people in the United States and Canada. In these societies, race categorizes people based on similar physical and social features, operating as a social caste system (23–26). Racial discrimination may be overt or covert. It ranges from microaggressions (everyday slights, either intentional or unintentional, that are based on race) to deprivation of societal goods or even acts of violence. Racial discrimination can be perpetrated by anyone, regardless of race or conscious intention (24, 26).
4.2. Implicit biases and empathy
It is important to understand that race, culture, ethnicity, and religion influence people's mental health and the need to be a part of an honest and healthy dialogue between a healthcare professional and their client or patient (26). However, conversations about race, racism, and racial disparities are difficult for many [e.g., (27, 28)]. In the case of psychotic disorders, the experience of a Black client can, for reasons explored in this study, differ drastically from those of White clients. If asked, Black clients may have harrowing tales about their experiences being stigmatized, harassed, or surveyed based on their race and mental illness. Hearing about the moral failing of an in-group member can cause discomfort if that individual identifies highly with their in-group members (29, 30). Therefore, for White individuals (most therapists in the United States and Canada), listening to stories about racism from BIPOC clients can lead to discomfort if those White persons identify highly with this group.
Such feelings of discomfort surrounding these topics may also be attributed to socialization in environments that do not have conversations about race. Thus, mental health professionals must resolve any anxieties they may have surrounding discussions about race, racism, and racial disparities because, unchecked biases can harm clients of color (31, 32).
4.3. Differential empathy for people of color influences diagnosis and treatment
Race has been shown to influence the level of empathy that individuals have toward each other. Several studies have demonstrated that those with similar skin color (Black or White) have greater empathetic resonance (33–35). Brain imaging furthermore reveals that White individuals perceive the pain of Black people as less painful than that of White people (33, 36). The evidence is compelling as it demonstrates that simply watching an individual being exposed to pain results in a measurable and quantifiable sensorimotor resonance, which is dependent on the racial similarity between the observer and the victim (37, 38).
These studies are important because reduced empathy on the part of White clinicians toward their Black patients may partially explain how mood symptoms in Black patients are often misinterpreted, or why psychotic disorders are overdiagnosed (39, 40). For example, instead of viewing a Black patient as “sad,” they are characterized as “mad.” Instead of being comforted because they are “afraid,” they are labeled as “paranoid.” These studies provide a mechanism for how what may traditionally be considered a reliable assessment of psychosis and schizophrenia across racial groups may in fact be biased.
4.4. History of medical racism and psychosis
These biases are not new but rather are rooted in our medical history. Racist discourse on mental health among medical professionals has occurred throughout the history of the United States. An early example of this can be found in the racist writings of a prominently published clinician, Dr. Samuel Cartwright, who taught at the University of Louisiana. In the article, Diseases and Peculiarities of the Negro Race, he identified/created two psychotic mental health conditions that he claimed to be unique to Black people. These conditions were “Drapetomania”—a disease that caused slaves to run away—and “Dyseathesia Aethiopica”—a disease that caused “rascality” in Black people both enslaved and free (41). He notes (p. 331–33), “They wander about at night, and keep in a half nodding sleep during the day. They slight their work, cut up corn, cane, cotton, or tobacco when hoeing it, as if for pure mischief. They raise disturbances with their overseers and fellow servants without cause or motive, and seem to be insensible to pain when subjected to punishment.” By pathologizing what were normal acts of survival and resistance by enslaved persons, he weaponized medicine in the service of upholding White supremacy.
Medical racism continues into the current time in its discriminatory treatment of Black people. For example, the practice of “race norming” for determining American football players' eligibility for settlement funds after traumatic brain injuries refers to the practice of generating different scales and thresholds for the assessment of cognitive functioning for White players than for Black ones. The norms used in the testing of decrement in cognitive function assumed that Black players have a lower cognitive function at baseline, and so must demonstrate a higher decline in cognitive function compared with non-Black players to qualify for financial settlements. This practice only ended in 2021 after public outcry (42). The NFL had defended this practice in the past, asserting its standards “relied on widely accepted and long-established cognitive tests and scoring methodologies.” As illustrated, race and racism contribute to the misdiagnosis of psychosis in African Americans with serious negative consequences for mental healthcare.
Notably, the care, treatment, diagnosis, and social understanding of psychosis in people racialized as Black in North America has a history of being fraught with issues that can confound the interpretation of patient data. This is because it is linked with the White supremacist roots in the very development of psychology as a scientific discipline and difficulty in identifying current racial myths, which may be anchored in the published literature as “scientific facts” (32, 43).
Before the 1960s, persons with schizophrenia were neither feared as criminals nor stigmatized as abnormal; in popular media, schizophrenia was more often associated with White women who developed psychosis due to the stresses associated with being a mother and homemaker (44), although this may not have been the conceptualization among those in the mental health community at the time. Even so, in 1968, a fundamental shift occurred subsequently transforming the meaning of psychosis in the minds of both healthcare professionals and the public. In that year, New York psychiatrists Walter Bromberg and Franck Simon coined the term “protest psychosis” to advance the idea that “Black power” sentiments drove “Negro men to insanity”, at which point schizophrenia became a condition used to pathologize Black people (44, 45). This weaponization of medicine was not a new phenomenon, rather only a continuation of the same war aimed at subjugating people by race. Not coincidentally did the emergence of codifying mental health as a tool to denigrate Black people occur just as the American Civil Rights movement was transforming society, inciting feelings of threat in many beneficiaries of the Jim Crow system (44). The purpose of redefining schizophrenia as a disorder to be feared was to support and preserve racial segregation and use the threat of mental illness to control agitators and punish social gains (44, 46). The race-based pathologization of psychosis that started in the 60s was exacerbated by legislative changes in the United States (de-institutionalization) between 1963 and 1965 that emptied psychiatric hospitals in the hope that discharged patients would be cared for in the community (47). But new medications were not simple cures for complex mental disorders and local communities were unprepared for the shift. Many former long-term patients whose families could not care for them were later found either on the street or in jails.
These events left their stain on the conceptualization of psychosis, which to this day continues to influence the understanding and perception of schizophrenia-spectrum disorders. Notably, from 1950 to 1996, the proportion of people who conceptualized those with schizophrenia-spectrum disorders as being violent increased by nearly 250% (48). The unexpected increase in perceptions of violence was confined to those who think of mental illness in terms of psychosis, and not for other conditions such as MDD, showing that this critical misperception about those with schizophrenia-spectrum disorders has become a socially learned bias.
The prism through which psychologists make diagnoses, which is initially based on the observation of behavior, is already tainted by socially learned biases (32). For example, a White psychologist interprets a remark about “people out to get me” as paranoid delusions while a Black psychologist may understand this as perfectly reasonable given that the patient has been stopped by police seven times in one month. Therefore, it is to be expected that racial disparities have been reported in the rates of diagnosis of these disorders (14). Upwards of 76% and an estimated 80% of licensed psychologists in the United States and Canada, respectively, are White (49, 50). Without lived experience to help understand the current social context, clinicians may have difficulty equitably diagnosing patients from cultures where they have little formal training. These unaddressed implicit biases around mental illness and psychosis with regard to other cultures also make it difficult to make comparisons across races.
It is through this lens that the recent increase in the diagnosis of schizophrenia-spectrum disorders in people of color should be considered (14). It has now been noted in several publications that providers interpret behavioral characteristics used in the diagnosis through their own racial or cultural biases, leading to misdiagnosis in Black individuals [e.g., (51, 52)]. Although studies from the United States show that the overall mental health of Black Americans was better or equivalent to that of Whites, with notably lower rates of alcohol and substance use than White groups, Black Americans in general have been diagnosed with higher rates of schizophrenia-spectrum disorders (12, 53, 54) for reasons that we now know may be difficult to disentangle from the initial weaponization of this diagnosis in the late sixties. The differences described are not genetic because, as previously stated, race is not a genetic construct (14).
A more nuanced reading of the literature, including new publications on genetics and socialization, points more to structural and identity-based exclusion as a primary cause that is affecting the variation in rates of schizophrenia-spectrum disorders among races (55). Therefore, it is with a critical eye, taking into account the history and politicization of schizophrenia-spectrum disorders and a lack of cultural competency of the primarily White clinician healthcare community who have been making these assessments, that one must view the literature.
4.5. Why Black people are overdiagnosed with schizophrenia-spectrum disorders
Olbert et al. (15) conducted a meta-analysis to determine the disparities in the diagnosis of schizophrenia between Black and White people in the United States using the DSM-III or later. Furthermore, they investigated whether the use of structured-interview assessments could reduce these disparities. They found that Black individuals were ~2.4 times more likely to receive a diagnosis of schizophrenia than White people and that the use of structured-interview assessments did not have a significant effect in reducing these racial diagnostic disparities (but a power analysis showed that there may be a small effect). The fourteen studies that were coded as having used structured interviews, conducted a clinical diagnosis using “structured- or semistructured-interview methods or validated symptom checklists” [(3), p. 106]. However, it is unknown if these interviews were culturally informed or whether they were conducted by culturally competent clinicians, and if they had been, whether this would have reduced racial diagnostic disparities. In this regard, as noted by Olbert et al. (15), simply addressing clinician bias and modifying structured-interview instruments will not be sufficient to overcome these racial diagnostic disparities. Other factors such as social, cultural, structural, and institutional disparities that impact Black people would also need to be addressed, as has been stated earlier in this paper.
Black people may be misdiagnosed with schizophrenia-spectrum disorders for several reasons. One proposed reason is a healthy suspicion (56), also known as responsive paranoia (57) or cultural mistrust (58). Healthy suspiciousness refers to “normative reactions” such as guardedness and mistrust that occur in response to discrimination (59). A study by Combs et al. (60) found that Black individuals endorse higher levels of subclinical paranoia when compared with White control groups. It was also found that perceived racism predicts cultural mistrust and non-clinical paranoia in Black people, and some paranoia may also be viewed as a healthy and adaptive strategy for Black people (59). Healthy suspiciousness may be misunderstood by mental health clinicians and considered to be delusional (61).
A second proposed reason relates to the consequences of stereotypes and implicit bias. Implicit bias refers to unconscious thoughts and feelings, which, due to lack of consciousness, are often not acknowledged or controlled by the person holding them. While overt acts of discrimination may have lessened in the United States, more subtle forms of discrimination, such as implicit bias on an individual and institutional level continue and may impact mental health clinicians' behaviors and choice of treatment (62). For example, these biases may lead to misperceiving Black individuals as “scary, violent, unreliable, less educated, and noncommunicative” [(63), p. 1123], thus interfering with a proper assessment. The study by Plaisime et al. (63) explored how the biases of White and Black healthcare providers in the United States may impact their diagnosis and treatment of Black male patients. Participants indicated that their perceptions were influenced by the largely negative portrayals of Black people in the media. White healthcare providers expressed fear and discomfort regarding working with Black male patients, and that they had very little contact with Black and other people of color often until graduate school. In addition, Black male patients were not offered certain treatments due to assumptions about low economic status and noncompliance. Black patients may also not be prescribed medications because of assumptions about drug use and addiction that are racially driven (64, 65). Furthermore, patients of color may have longer wait times for assessment and treatment (62, 64, 65), be approached condescendingly without consultation and collaboration, not receive a thorough assessment, and be denied interpreters if needed, as well as treatment options and access to family visits (62).
Research by Strakowski et al. (66, 67) has shown there to be a clinician overemphasis on the relevance of psychotic symptoms and an underemphasis on mood-related symptoms in the diagnosis of schizophrenia-spectrum disorders in African Americans. This pattern was also found in a more recent study conducted by Gara et al. (39), which showed that, when compared with Non-Latino Whites, African Americans who screened positive for major depression (moderately severe to severe depression) were significantly more likely to receive a misdiagnosis of schizophrenia. Gara et al. (68) found no significant difference between blind ratings for the severity of depressive and manic symptoms between African American and White individuals; however, African American patients were assigned higher ratings of psychosis. This suggests that in Black patients, clinicians tend to overemphasize psychotic symptoms, and diagnoses may be “skewed” toward schizophrenia-spectrum disorders, even though they exhibit similar levels of depressive and manic symptoms as White individuals (68). Misdiagnosing patients through the influence of bias and stereotypes can harm patients psychologically or socially (14), as per Figure 2.
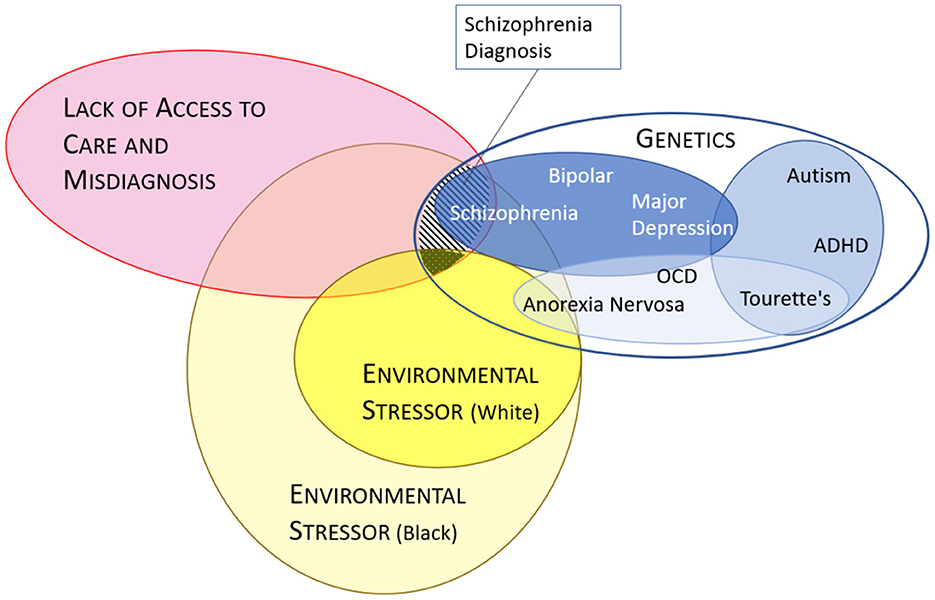
Figure 2. Potential factors leading to higher observed diagnoses of schizophrenia. Model of how factors leading to a diagnosis of schizophrenia can differ between Black and White individuals taking into account differences in environment, access to care, misdiagnoses and genetics (15). Stripped area represents diagnoses of schizophrenia in Black populations which has been observed to be greater than in White populations (dotted area). The blue ovals (genetics) are based on a risk model from the Cross-Disorder Group of the Psychiatric Genomics Consortium (3). Misdiagnosis and lack of care (red oval) appears to affect racialized individuals (i.e., Black) more often than White individuals (intersecting orange areas).
Finally, the failure to consider the role of spirituality and religious beliefs may lead to an inaccurate diagnosis of schizophrenia-spectrum disorders [e.g., (50)]. Results from the study by Peltier et al. (69) showed that for African Americans, the probability of a schizophrenia-spectrum disorder diagnosis decreased when unusual experiences were viewed by the clinician as spiritual or paranormal. A religious person who says that they have “heard the voice of God” should not automatically be assumed to have had a psychotic experience. Clinicians cannot assume that all visual and auditory hallucinations indicate the presence of a schizophrenia-spectrum disorder (69), as a culturally informed assessment must include the consideration of diverse spiritual beliefs and practices (69, 70), particularly in relation to hallucinations and religious-themed delusions.
It is important to note that schizophrenia is a diagnosis of exclusion, meaning that clinicians are expected to rule out other causes for symptoms and other diagnoses before assigning a diagnosis of schizophrenia (39, 68). This does not appear to sufficiently occur for Black communities due to assessment bias in the diagnostic process, as well as failure to account for the social and environmental risk factors and cultural factors that contribute to the development of symptoms (16). According to Gara et al. (68), understanding the impact of racial bias in clinical assessment is crucial and can reduce racial disparities in healthcare.
4.6. Genetics, race, and schizophrenia
The conflation of race, ethnicity, and genes has led to confusion around the understanding of findings that have been interpreted to mean that certain races are biologically inclined to have an increased incidence of schizophrenia. New data however shed light on the relationship of schizophrenia with specific genes (3, 4, 71). These data indicate that schizophrenia exists in a genetic category that places it in the same group as bipolar disorder (Figure 2). This categorization underscores that the diagnosis of schizophrenia, like most mental health disorders, does not rely on objective findings such as blood tests or brain scans and is based on observations from patients, family members, and the diagnosing physician. Lack of appreciation of the linkages among mood and psychotic disorders has resulted in schizophrenia being treated as if it were (i.e., by DSM-5) more disconnected from other psychological disorders than is warranted by the genetic data, which affects treatments and clinical care as well as the cultural and social meaning of having a diagnosis of schizophrenia or psychosis (72).
Two recent publications have been able to locate ultra-rare variations in several genes that increase a person's risk of developing schizophrenia. The basis for one of these studies was a whole-exome sequencing of about 24,000 persons from diverse global populations diagnosed with schizophrenia and 97,000 without schizophrenia (4). The nature of the discovered genes confirms that schizophrenia is a disorder of neuronal communication. The genomic regions that were identified are in ion channels, transporters, and genes regulating expression, primarily only active in neurons of the brain. These genes have their effects on mechanisms such as synaptic structure and some of the identified variants code for genetic mutations that result in a truncated version of the affected protein. If any given individual has a 1% chance of being diagnosed with schizophrenia over a lifetime, having one of the identified mutations can increase the risk by four to 50 times depending on the genetic mutation (4, 73).
Although fewer than one in 10,000 individuals carry any of these ultra-rare higher-risk mutations, simply having a variation in one of the ten most identified genes could boost the risk of contracting schizophrenia, and having combinations of these variants may further stack the odds toward the development of schizophrenia (4, 73).
Genes in the glutamate neurotransmitter pathway including GRIN2A, SP4, and GRIA3 are among the high-risk genes, which confirms the suspicions of researchers. It has long been observed that pharmaceuticals that antagonize receptors in the glutamate pathway including ketamine and PCP are capable in certain doses of triggering symptoms that look like schizophrenia (4, 73).
These breakthroughs in understanding the genetic risk factors for schizophrenia help clarify origins and point away from a risk model based on simplistic racial differences in diagnoses. None of the identified genes are thought to have a direct association with skin shade, a key basis for racial classification. There is no reason to assume a biological or genetic cause for the observed higher prevalence of schizophrenia-spectrum disorders in specific minoritized groups (74), rather strong evidence exists from other studies against a race-based genetic explanation of risk.
These studies examined the same ethnic groups that had vastly different incidences of schizophrenia-spectrum disorders depending on their geographic location. In one study of ethnically Norwegian migrants in the United States state of Minnesota, higher rates of schizophrenia were found in the migrant than in the original population in Norway. Similarly, ethnically similar groups originating from Trinidad, Suriname, and Jamaica had much higher rates of diagnosed psychotic disorders in Western Europe than in their home countries (74). Further empirical research shows, also, that adjusting for environmental risk factors such as social disadvantage and linguistic distance—markers associated with increased odds of psychotic disorders—led to equal risks between ethnic minority groups and White majorities in several EU countries (55). Taken together, these studies do not support the theory that some races or ethnic groups have an increased gene-based propensity to develop schizophrenia-spectrum disorders (55, 74).
Although there are now genes associated with the risk of developing schizophrenia, these do not directly correspond to higher risk by race, as race is a sociopolitical and not a genetic classification. Notably, since belonging to a certain race corresponds to an environmental risk of poor mental health (i.e., social disadvantage), or a tendency to be medically misdiagnosed, an association between race and schizophrenia-spectrum disorders may be expected to be observed (Figure 2).
4.7. Black people may have increased vulnerability due to more PTSD
In addition to overdiagnosis, Black people may have an increased vulnerability to schizophrenia-spectrum disorders due to the higher prevalence of posttraumatic stress disorder (PTSD) and trauma (75, 76), which is a well-established risk factor in the etiology of psychosis (77). The story of Josh Marks (Table 3) is illustrative of many of the issues facing Black people who struggle with severe mental illness.
A meta-analysis by Bailey et al. (79) showed that trauma experienced in childhood may increase the likelihood of hallucinations and delusions. In addition, social marginalization is a known risk factor for developing schizophrenia and psychosis (80), as are environmental factors such as neighborhood conditions—the neighborhood index of multiple deprivation (IMD) significantly predicted psychosis and depression, especially psychotic symptoms with paranoia (81). Black individuals are at high risk for traumatization, including racial trauma, due to discrimination and racism at individual, societal, and structural levels (26). An umbrella review by Varchmin et al. (82) found that one of the most significant social risk factors for psychosis was a vulnerability to racist discrimination, particularly for migrants in low ethnic density areas, minoritized individuals, and Black individuals.
The cumulative effects of racism can exacerbate any genetic predispositions and contribute to PTSD and racial trauma that can go untreated due to institutional racism and lack of access to appropriate care (26, 83). Structural racism, experienced “disproportionately” by Black people, confers social disadvantage through neighborhood factors, discrimination, and collective stress and trauma, which may place them at risk for developing schizophrenia-spectrum disorders (16, 80). Adequate mental healthcare needs to also address these social and environmental factors that include everyday racism, structural racism, and their impact on informing symptoms.
Misdiagnosing patients with schizophrenia-spectrum disorders has many serious implications. If misdiagnosed, patients do not get the correct treatment for their symptoms and conditions. For example, patients with bipolar disorders who are misdiagnosed as having schizophrenia may not be prescribed mood stabilizers (e.g., lithium) to address symptoms of mania. Depressed patients who receive antipsychotic medications due to misdiagnosis must endure serious side effects such as weight gain, metabolic syndrome, diabetes, and movement disorders, which can cause unnecessary physical harm and health consequences (39). Misdiagnosis also contributes to potential lifelong stigma and hopelessness (8), lower expectations for prognosis, and restricted options for treatment (39, 68).
5. Black experiences in medical contexts
5.1. Access to care in the first episode
Overall, people of color experience discrimination in access to and the quality of healthcare at both individual and structural levels (26). The United States cohort study of 3,017 privately insured patients (age 10–21 years) found that White patients were more likely than Black and Hispanic patients to be given behavioral health diagnoses and treatment before the identification of first-episode psychosis. Controlling for socioeconomic variables did not change these observed racial/ethnic disparities. Specific to first-episode psychosis, newly diagnosed youth of color do not see a mental healthcare professional unless they are admitted to the emergency room (84).
There is evidence that people of color are receiving less mental healthcare in the year leading up to their diagnosis of first-episode psychosis (84). Usually, there are subtle attenuated prodromal symptoms (85) that occur before a first-episode psychosis, which are critical for detecting individuals at clinically high-risk for psychosis (84, 86). Timely or early intervention at this stage can reduce the duration of untreated psychopathology, prevent the worsening of symptoms, and improve clinical prognosis (84, 87, 88). Historically, efforts to recruit clinical high-risk individuals for research studies have resulted in the majority of White samples (89), while first-episode psychosis research studies report an overrepresentation of Black patients. These data suggest that Black patients are more likely to access care once the overt symptoms of psychosis have emerged, and efforts are needed to improve their access to clinical high-risk programs. According to Heun-Johnson et al. (84), unequal access to healthcare in the prodromal period may worsen long-term treatment outcomes after diagnosis. These studies demonstrate that it is essential to address racial/ethnic disparities in accessing healthcare so that people of color can receive early intervention, which is critical for a good prognosis (16).
5.2. Overmedicated due to exaggerated fears of dangerousness
When in treatment, Black patients are more likely to be overmedicated due to being stereotyped as “dangerous” by clinicians (16, 90). Segal et al. (90) found that patients' medication status was impacted by their race. Specifically, African American patients were more likely to be prescribed psychiatric medications and administered more high-potency antipsychotic medications at higher doses. They were also given significantly less time for evaluations by clinicians. Furthermore, Black Americans are also often prescribed older medications or first-generation antipsychotic medications, which can have severe side effects such as tardive dyskinesia and extrapyramidal side effects (91, 92). Herbeck et al. (91) found that in comparison to White Americans, African Americans were significantly less likely to be given second-generation antipsychotics, which are generally considered to be a better treatment for schizophrenia-spectrum disorders. In particular, young, male African Americans, or those with schizophrenia, were less likely to be given second-generation antipsychotics. This is of concern because younger patients may benefit from second-generation antipsychotics because of their decreased side effects (91). In addition, Herbeck et al. (91) found that individuals without health insurance were less likely to be given second-generation antipsychotic medications, noting that 10% of African Americans did not have health insurance in comparison to the 3% of White Americans. Similarly, Cook et al. (92) found that Black individuals in high-poverty communities were more than two times as likely to be treated using high-potency first-generation antipsychotics. These racial disparities in treatment continue even though second-generation antipsychotics have been prescribed for over 30 years (92).
Overmedication and the side effects associated with first-generation antipsychotics can negatively impact health and may contribute to decreased compliance with medication (91). This may then result in coercive techniques by healthcare providers to gain compliance. For example, Knight et al. (93) found that Black Canadians of Caribbean or African descent were more likely to receive coercive referral and treatment (through police, ambulance, and court) compared with White Canadians, and were at greater risk for legal coercion and detention for treatment. These disproportionate rates of coercive referrals of Black individuals make a strong case for researching how “authority figures” determine dangerousness in the case of Black patients, especially those with first-episode psychosis (93).
Such discriminatory practices are indicative of racial bias and institutional racism and are highly problematic because coercive treatments often foster cultural mistrust and create a poor patient–clinician relationship. Coercive approaches can also be very harmful, as techniques such as involuntary hospitalization and mandated medication may induce trauma in the patient and their families, leading to greater distrust and avoidance of mental healthcare in the future (94, 95). It is abundantly clear that how Black patients are assessed for treatments needs to be changed. Along these lines, Segal et al. (90) showed that when clinicians in emergency services make efforts to engage patients in treatment, overmedication decreases, underscoring the critical need for engaging Black patients in the evaluation and treatment process.
5.3. Pathways to care vary by ethnoracial group
“Pathways to care” refers to the sequence of interactions, both positive and negative, with individuals, organizations, or events, when an individual or their family attempts to seek help (96, 97). Ideally, each person will have a clear pathway for receiving appropriate care; however, this concept is also used to assess delays in help-seeking and treatment to better understand ways of providing early intervention (98). People of different races and socioeconomic statuses have different pathways that provide them with access to care (96, 99). “Aversive pathways” to specialized care for first-episode psychosis are associated with delays in treatment resulting in longer periods of untreated psychosis, poor engagement with treatment, and poorer outcomes. However, there is little research conducted on the “unique pathways” to care for Black individuals seeking care for schizophrenia-spectrum disorders (16, 96).
A qualitative study of coordinated specialty care for schizophrenia-spectrum disorders among Black Americans with first-episode psychosis found that before the onset of psychosis, participants reported exposure to childhood trauma, diminished social functioning, and greater contact with law enforcement that families described as “overly aggressive” (96). In addition, many prodromal experiences persisted following the onset of psychosis and were associated with delays in treatment and difficulties with navigating services, leading to increased delays in receiving coordinated specialized care. These barriers, which were specifically associated with longer durations of untreated psychosis for African Americans, had been previously described in a qualitative study by Bergner et al. (100). First, they found that healthcare professionals tended to misattribute symptoms of psychosis as depression, stress, or drug use. Second, they initiated treatment based on the presence of positive symptoms of psychosis, waiting for an increase in the severity of symptoms. Third, they required symptoms to reach a certain threshold, using issues of patient autonomy as an excuse. And finally, they allowed systemic factors such as lack of social support, lack of affordable services, and difficulties with scheduling appointments to interfere with the delivery of adequate care (100). In other words, healthcare professionals were providing racially biased and substandard care targeted specifically at Black individuals.
For Black communities, there is an extreme and damning gap between those who require mental health services and those who actually receive timely expertise and compassionate services. According to Tambling et al. (101), a full 70% of those who require treatment fail to access appropriate services (101, 102). The picture in Canada is similarly bleak, with a national survey finding that 42.2% of those seeking care for schizophrenia had difficulty accessing services “often” or “just about every time” (103).
6. Role of law enforcement
6.1. Disturbing statistics
Disparities in pathways to care may arise when law enforcement is involved. Young Black people with psychotic symptoms may be stereotyped as dangerous, and police may be called to deal with patients, putting them at increased risk of harm. However, people experiencing a mental health crisis are more likely to be victimized than cause harm to others (104).
Individuals with untreated severe mental illness are involved in at least one in four and as many as half of all fatal police shootings (105). Saleh et al. (106) included demographics and the presence of mental illness in their investigation of independent databases of killings of civilians by police in the United States. They found that in 2015, 23% of people killed by police showed symptoms of a mental illness. Such tragedies have resulted in a call for action from Black communities and from organizations such as The Centre for Addiction and Mental Health (107), which holds the position that racism and anti-Black racism exacerbate the interactions of individuals experiencing mental illness with law enforcement that compounds their mental health crisis.
Implicit bias and racism on the part of the police are a cause for violence against Black individuals in need of mental healthcare (108, 109). In the United States, the twenty first century Cures Act, passed by Congress and signed by President Obama in December 2016, included a mandate for the United States Attorney General to collect and report data on the role of serious mental illness in fatal law enforcement encounters. The Bureau of Justice Statistics overhauled its system for collecting law enforcement homicide data and at that point resumed reporting arrest-related death statistics. Using the new methodology approximately doubled the number of arrest-related deaths that were verified and reported by the Department of Justice. However, the role of mental illness in them has not yet been reported (105).
6.2. Disturbing examples
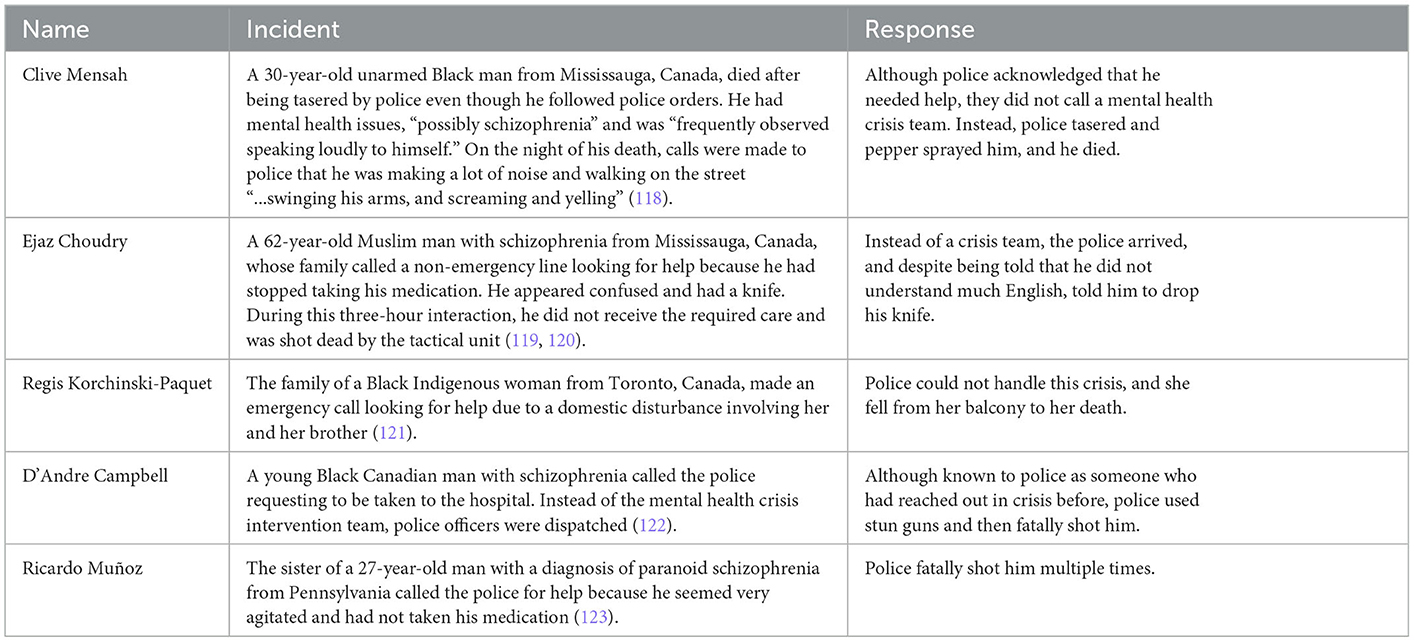
There are many problems with including police in situations involving a mental health crisis, as illustrated in Table 4. In all of these cases, police used disproportionate force resulting in tragic deaths, which is already a problem facing Black people (110). These shootings are driven by racism and fear, which has now become a part of the public discourse (20, 111, 112). Simply being Black and being associated with a mentally ill person is perceived as a danger, as evidenced by the case of an unarmed Black therapist shot while laying down with his hands in the air trying to prevent his autistic White patient with a toy firetruck from being shot by police (113). In addition, in many cases, Black people coping with schizophrenia-spectrum disorders are not killed or taken to a hospital but are simply criminally charged and jailed, as we saw in the case of Grace Terry, where today the United States prison system is the largest provider of mental health services in the world (114). Black Americans are incarcerated in state prisons at nearly five times the rate of White Americans and makeup 38% of the total prison population (115, 116), while one study in Ontario also found disproportionately higher incarceration of Black individuals [Black men are five times more likely to be imprisoned than White men; (117)]. Notably, one study found that in a sample of 109 urban, low-income, predominantly African American patients hospitalized for first-episode psychosis, an outsized 57.8% had been previously incarcerated, and for predominantly non-violent crimes (17).
6.3 Weaponization of medicines by law enforcement
Substances that are intended to be therapeutic can be used to control or harm people of color, and this is also referred to as “weaponized medicine” (124). The first account in the literature of this was in 1928, in the Journal of the American Medical Association, which reported that in Hawaii, an ethnically Japanese handyman and chauffeur had been arrested as the chief suspect in the kidnapping and murder of a young White boy. A police surgeon injected him with a substantial dose of hyoscyamine to extract a confession, which he later recanted, and another person was later found to be the perpetrator. This approach was later used on hundreds of convicts.
Recently, two tragic incidents in 2020 involving law enforcement raised concerns over the use of anesthetic ketamine—a powerful sedative normally used in hospitals—as a law enforcement tool to subdue suspects in the field (124, 125). Over a four-day period in Aurora, Colorado, 23-year-old Elijah McClain and 25-year-old Elijah McKnight were both given doses of ketamine in separate police incidents. McClain went into cardiac arrest and died several days later. McKnight was hospitalized on life support but survived. Video footage of both incidents shows that neither McClain nor McKnight was resisting arrest when the ketamine was administered.
These incidents demonstrate that the lawlessness of law enforcement in punitive interactions with Black persons is ongoing. Not only are Black people targeted simply because of their race, but psychosis-inducing substances are also being used to create the veneer of an excuse, which may be justified through myths around the danger of Black psychosis (44). In these cases, the police used the label “excited delirium” to justify the subjugation of suspects with ketamine. However, the diagnosis of excited delirium is not recognized by major medical organizations such as the American Medical Association (126). Furthermore, police officers are not trained to diagnose any sort of delirium, rather this role belongs to medical personnel (127). It may be more accurate to describe the incident involving McClain as an extra-judicial murder using psychosis-inducing drugs, as the circumstances were suspicious. It is now known that McClain only weighed 143 pounds at the time of his arrest yet was given a ketamine dose while handcuffed, he was given a dose for a 200-pound man (128). In 2022, two years after his death, two paramedics and three police officers were indicted by a Colorado grand jury on charges of manslaughter and criminally negligent homicide (129). Despite these issues, the diagnosis of “excited delirium” continues to be used throughout the United States to justify the use of ketamine and to explain deaths in police custody, especially the deaths of young Black men (130).
7. Addressing the issues
Given the unique issues faced by Black people with early symptoms of schizophrenia-spectrum disorders, solutions must be tailored to address their needs, which are complicated by systemic racism in healthcare and law enforcement. Critical issues to address include (1) improving diagnostic accuracy which includes educating psychologists about the unique cultural history and stigmas around psychosis as well as its genetic origins, (2) public education in communities of color to increase mental health literacy, (3) improving interventions surrounding law enforcement for mental health crises, and (4) anti-racism training for mental health clinicians. Examples of how to accomplish this are shown in Table 5.
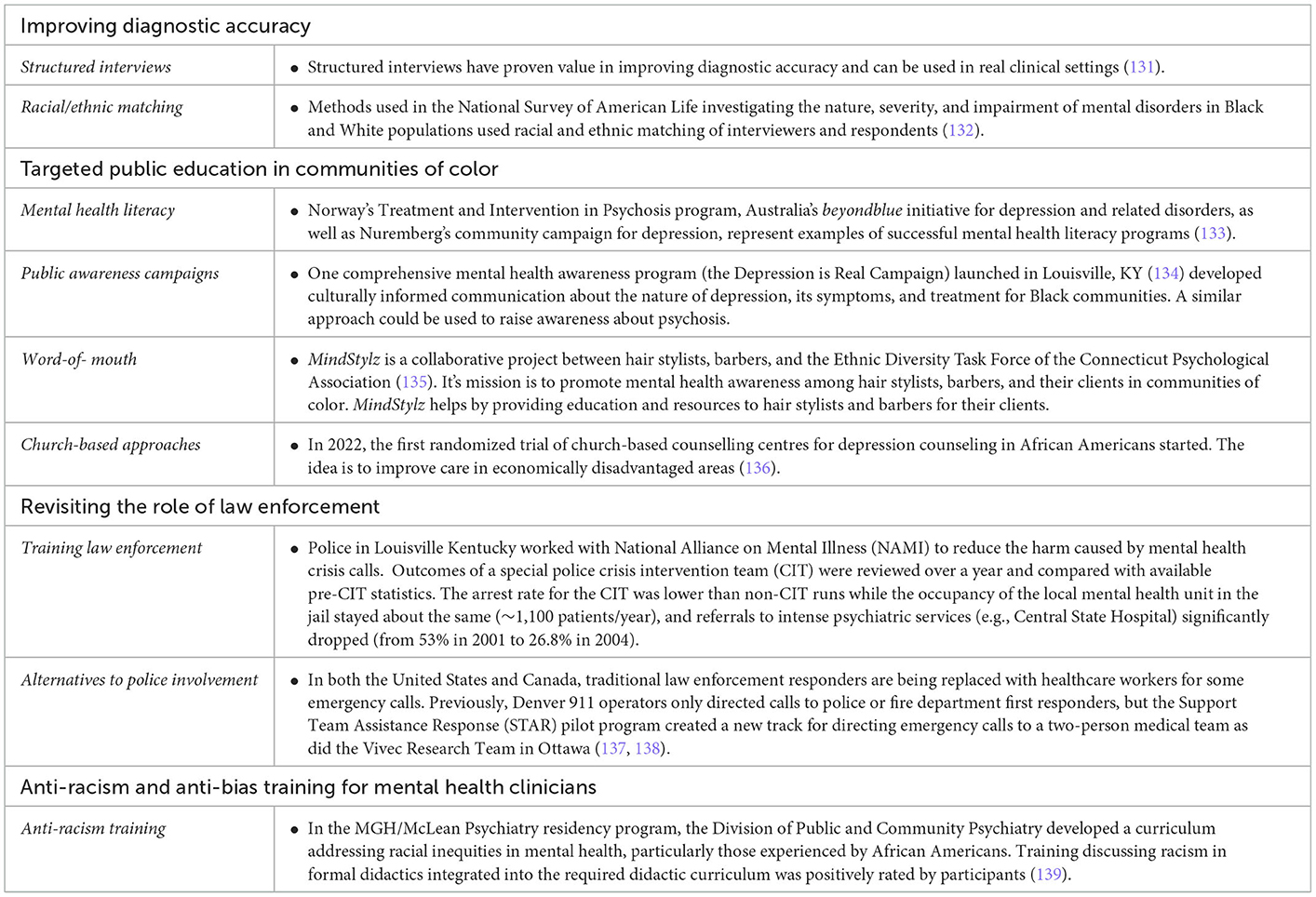
Table 5. Examples of how to reduce racial disparities in mental healthcare pathways for Black individuals.
7.1. Improving diagnostic accuracy
A more deliberate diagnostic process through greater use of the structured clinical interview for schizophrenia-spectrum disorders could reduce reliance on stereotypes and help minimize misdiagnoses [e.g., (3)]. Furthermore, when possible, the benefits of racial and ethnic matching should be considered, as many clinicians do not have the proper training to work effectively across race, ethnicity, and culture (32). For example, a Black person may be cautious or seem reluctant to share details with clinicians from other racial groups due to realistic mistrust that can then be misinterpreted as pathological paranoia.
7.2. Public education
Increasing mental health literacy at the community and population level can improve the early detection of and intervention for psychological disorders (140). Public awareness educational campaigns aimed at the general public can be beneficial in increasing awareness of the nature of schizophrenia and its treatment, although these campaigns should be a continuing process, as single campaigns usually do not have much effect (141). Specific messages disconnecting schizophrenia from violent behavior should be crafted as there appears to be a widely held misconception that they are linked (48). Key components of public education can include an emphasis on increasing positive word-of-mouth from trusted leaders in communities of color where long-term relationships are critical. Church-based interventions are effective strategies for reaching Black communities as these resources are connected to a trusted source (142).
7.3. Improving interventions surrounding law enforcement
As previously noted, people with severe mental disorders are much more likely to be killed by police, and the risks multiply when the victim is Black. Therefore, there is a need to address this problem at the level of law enforcement (108, 143, 144). Training for law enforcement on how to recognize and manage mental health crises is essential, but there is also a need for the formal separation of mental health interventions from policing. Police are not mental health providers, and armed persons in uniform should not be the first point of contact for people experiencing psychotic symptoms, especially Black people who are often already highly fearful of police (145, 146). Alternate first responders should be enlisted for crisis intervention and wellness checks as per examples in Table 5 (138, 147).
7.4. Anti-racism training
Organizations serving racialized groups can frame their actions and practices in anti-racist and anti-oppressive philosophies to be more responsive to the populations they serve (20). This can result in better care for racialized groups while addressing the issue of racism and oppression in mental health and medical services (148–150).
8. Conclusion
Black people in the early phases of a schizophrenia-spectrum disorder face barriers to proper diagnosis, impediments to proper care, greater mistrust of mental healthcare systems, and violence from law enforcement. Psychologists and psychiatrists are often the gatekeepers to proper care for these individuals. The clinical treatment of mental disorders is dependent on cultural norms, and the empathetic, culturally informed diagnosis of mental health professionals. Timely awareness of the significance of culture can make a difference in the pathways to care for Black individuals suffering from psychosis and correct any mistaken interpretations of psychopathology (2, 14). Failure to act in accordance with this can result in misdiagnosis and poor outcomes for those served.
While the research, training, and application of culturally responsive assessment and diagnosis have increased over the last several decades, there is a continued need for a focus on training culturally responsive clinicians. The skills of a culturally responsive clinician are similar to those of an effective clinician more broadly, developing cultural humility (to avoid mistaking difference for inferiority), compassion (for self and others), and critical thinking skills (the process of continually questioning one's assumptions and biases). Clinicians who attend to these principles achieve the overarching goal of every clinician: client wellbeing (32, 151). With this in mind, multifaceted approaches are needed to holistically address these problems that include interventions in the community as well.
Author contributions
SF and MW: conceptualization—ideas formulation or evolution of overarching research goals and aims, methodology, development or design of methodology, creation of models, project administration—management, coordination responsibility for the research activity planning, and execution, supervision—oversight, leadership responsibility for the research activity planning and execution, and including mentorship external to the core team. SF, AKR, TM, and MW: investigation—conducting a research and investigation process, specifically performing the experiments, or data/evidence collection, writing—original draft, preparation, creation and/or presentation of the published work, specifically writing the initial draft (including substantive translation), and writing—review and editing. SF: visualization—preparation, creation and/or presentation of the published work, and specifically visualization/data presentation. All authors contributed to the article and approved the submitted version.
Funding
This research was undertaken, in part, thanks to funding from the Canada Research Chairs Program, Canadian Institutes of Health Research (CIHR) grant number 950-232127 (PI: MW).
Conflict of interest
SF has an affiliation with the German GmbH Bioville. This company has no influence and is no involved in any enterprises that would affect this manuscript.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. King ML,. King berates medical care given negroes. Oshkosh Daily Northwestern. (1996). Available online at: https://pnhp.org/news/dr-martin-luther-king-on-health-care-injustice/ (accessed March 26, 1996).
2. APA. Bipolar and Related Disorders. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: APA (2013).
3. CGPGC. Genomic relationships, novel loci, and pleiotropic mechanisms across eight psychiatric disorders. Cell. (2019). 179:1469–82. doi: 10.1016/j.cell.2019.11.020
4. Singh T, Poterba T, Curtis D, Akil H, Al Eissa M, Barchas JD, et al. Rare coding variants in ten genes confer substantial risk for schizophrenia. Nature. (2022) 604:509–16. doi: 10.1038/s41586-022-04556-w
5. Lecomte T, Addington J, Bowie C, Lepage M, Potvin S, Shah J, et al. The Canadian network for research in schizophrenia and psychoses: a nationally focused approach to psychosis and schizophrenia research. Can J Psychiatr. (2022) 67:172–5. doi: 10.1177/07067437211009122
6. GBD 2019 Mental Disorders Collaborators. Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet Psychiatr. (2022) 9:137–150. doi: 10.1016/S2215-0366(21)00395-3
7. Mojtabai R. Estimating the prevalence of schizophrenia in the United States using the multiplier method. Schizophr Res. (2021) 230:48–9. doi: 10.1016/j.schres.2021.02.010
8. Herbst D,. Schizophrenia in Black people: Racial disparities explained. PsyCom. (2021). Available online at: https://www.psycom.net/schizophrenia-racial-disparities-black-people#improvingschizophreniatreatmentsinblackpeople (accessed October 14, 2021).
9. Murphy T, Krasa H, Lavigne G, Frangiosa T, Palsgrove A, Stalters L, et al. Societal costs of schizophrenia and related disorders, Alexandria, VA: Schizophrenia and Psychosis Action Alliance (2021).
10. Semega J, Kollar, M,. Income in the United States: 2021. United States Census Bureau, Report Number P60-276, Table A2. (2022). Available online at: https://www.census.gov/library/publications/2022/demo/p60-276.html (accessed September 13, 2022).
11. Williams MT, Gooden AM, Davis D. African Americans, European Americans, and pathological stereotypes: An African-centered perspective. In GR Hayes, MH. Bryant, editors, Psychology of Culture. Hauppauge, NY: Nova Science Publishers (2012) pp. 25–46.
12. Jahn ZW, Lopez J, de la Salle S, Faber S, Williams MT. (2021). Racial/ethnic differences in prevalence of hallucinogen use by age cohort: findings from the 2018 national survey on drug use and health. J Psych Stu. (2021) 5:69–82. doi: 10.1556/2054.2021.00166
13. Cohen CI, Marino L. Racial and ethnic differences in the prevalence of psychotic symptoms in the general population. Psychiatric Services. (2013) 64:1103–9. doi: 10.1176/appi.ps.201200348
14. Schwartz RC, Blankenship DM. Racial disparities in psychotic disorder diagnosis: a review of empirical literature. World J Psychiatr. (2014) 4:133–40. doi: 10.5498/wjp.v4.i4.133
15. Olbert CM, Nagendra A, Buck B. Meta-analysis of Black vs. White racial disparity in schizophrenia diagnosis in the United States: do structured assessments attenuate racial disparities? J Abnorm Psychol. (2018) 127:104–15. doi: 10.1037/abn0000309
16. OluwoyeO, Davis B, Kuhney FS, Anglin DM. Systematic review of pathways to care in the U.S. for Black individuals with early psychosis. Nat Partner J Schizophrenia. (2021) 7:1–10. doi: 10.1038/s41537-021-00185-w
17. Ramsay CE, Goulding SM, Broussard B, Cristofaro SL, Abedi GR, Compton MT, et al. Prevalence and psychosocial correlates of prior incarcerations in an urban, predominantly African-American sample of hospitalized patients with first-episode psychosis. J Am Acad Psychiatry Law. (2011) 39:57–64.
18. Issa O, Quon, A,. Samwel Uko's Family Continues Search for Justice From the System That Failed Their Son. CBC News. (2022). Available online at: https://www.cbc.ca/news/canada/saskatchewan/samwel-uko-parents-speak-out-1, 6472561 (accessed May 31, 2022).
19. Cénat JM. How to provide anti-racist mental health care. Lancet Psychiatry. (2020) 7:929–31. doi: 10.1016/S2215-0366(20)30309-6
20. Haeny AH, Holmes SC, Williams MT. Applying anti-racism to clinical care and research. JAMA Psychiatry. (2021) 78:1187–8. doi: 10.1001/jamapsychiatry.2021.2329
21. Soloducha A,. Petition calls on Sask. government to hire Black mental health therapists. CBC News. (2020). Available online at: https://www.cbc.ca/news/canada/saskatchewan/petition-for-black-mental-health-therapists-sask-1 (accessed July 2, 2020).
22. Jarvis GE. The social causes of psychosis in North American psychiatry: a review of a disappearing literature. Can J Psychiatry. (2007) 52:287–94. doi: 10.1177/070674370705200503
23. Bryant BE, Jordan A, Clark US. Race as a social construct in psychiatry research and practice. JAMA Psychiatry. (2022) 79:93–4. doi: 10.1001/jamapsychiatry.2021.2877
24. Haeny AM, Holmes SC, Williams MT. The need for shared nomenclature on racism and related terminology in psychology. Pers Psychol Sci. (2021) 16:886–92. doi: 10.1177/17456916211000760
25. Smedley A, Smedley BD. Race as biology is fiction, racism as a social problem is real: anthropological and historical perspectives on the social construction of race. Am Psychol. (2005) 60:16–26. doi: 10.1037/0003-066X.60.1.16
26. Williams MT, Khanna Roy A, MacIntyre MP, Faber S. The traumatizing impact of racism in Canadians of colour. Current Trauma Reports. (2022) 8:17–34. doi: 10.1007/s40719-022-00225-5
27. DiAngelo R. White Fragility: Why It's So Hard for White People to Talk About Racism. Boston, MA: Beacon Press. (2018).
28. Sue DW, Rivera DP, Capodilupo CM, Lin AI, Torino GC. Racial dialogues and White trainee fears: Implications for education and training. Cult Div Ethnic Minority Psychol. (2010) 16:206–14. doi: 10.1037/a0016112
29. Castano E, Paladino MP, Coull A, Yzerbyt VY. Protecting the ingroup stereotype: Ingroup identification and the management of deviant ingroup members. Br J Soc Psychol. (2002) 41:365–85. doi: 10.1348/014466602760344269
30. Scheepers D, Ellemers N. Status stress: Explaining defensiveness to the resolution of social inequality in members of dominant groups. In:J Jetten, K Peters, Editors, The social psychology of Inequality. Springer, Cham (2019) 267–87.
31. Williams MT. Managing Microaggressions: Addressing Everyday Racism in Therapeutic Spaces. Oxford: Oxford University Press. (2020).
32. Williams MT, Faber SC, Duniya C. Being an anti-racist clinician. Cognit Behav Ther. (2022) 15:1–22. doi: 10.1017/S1754470X22000162
33. Harjunen VJ, Sjö P, Ahmed I, Saarinen A, Farmer H, Salminen M, et al. Increasing self-other similarity modulates ethnic bias in sensorimotor resonance to others' pain. Soc Cognit Aff Neurosci. (2021) 17:673–82. doi: 10.1093/scan/nsab113
34. Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between Blacks and Whites. Proc Natl Acad Sci U S A. (2016) 113:4296–301. doi: 10.1073/pnas.1516047113
35. Mathur VA, Richeson JA, Paice JA, Muzyka M, Chiao JY. Racial bias in pain perception and response: experimental examination of automatic and deliberate processes. J Pain. (2014) 15:476–84. doi: 10.1016/j.jpain.2014.01.488
36. Berlingeri M, Gallucci M, Danelli L, Forgiarini M, Sberna M, Paulesu E, et al. Guess who's coming to dinner: brain signatures of racially biased and politically correct behaviors. Neuroscience. (2016) 332:231–41. doi: 10.1016/j.neuroscience.2016.06.048
37. Zhou Y, Han S. Neural dynamics of pain expression processing: Alpha-band synchronization to same-race pain but desynchronization to other-race pain. Neuroimage. (2021) 224:1–12. doi: 10.1016/j.neuroimage.2020.117400
38. Balliet D, Wu J, De Dreu CKW. Ingroup favoritism in cooperation: a meta-analysis. Psychol Bullet. (2014) 140:1556–81. doi: 10.1037/a0037737
39. Gara MA, Minsky S, Silverstein SM, Miskimen T, Strakowski SM. A naturalistic study of racial disparities in diagnoses at an outpatient behavioral health clinic. Psychiatric Serv. (2019) 70:130–4. doi: 10.1176/appi.ps.201800223
40. Kuno E, Rothbard AB. Racial disparities in antipsychotic prescription patterns for patients with schizophrenia. Am J Psychiatry. (2002) 159:567–72. doi: 10.1176/appi.ajp.159.4.567
41. Cartwright S. Diseases and peculiarities of the Negro race. De Bow's Review Southern and Western States. New York, NY: AMS Press, Inc. (1851).
42. Canada T, Carter, CR,. The NFL's Racist ‘Race Norming' is an Afterlife of Slavery. Scientific American. (2021). Available online at: https://www.scientificamerican.com/article/the-nfls-racist-race-norming-is-an-afterlife-of-slavery/ (accessed July 8, 2021).
43. Dupree CH, Kraus MW. Psychological science is not race neutral. Pers Psychol Sci. (2022) 17:270–5. doi: 10.1177/1745691620979820
44. Metzl JM. The Protest Psychosis : How Schizophrenia Became a Black Disease. Boston, MA: Beacon Press. (2009).
45. Hazin R. [Review of the book The protest psychosis: How schizophrenia became a Black disease, by J. M Metzl] J Nat Med Assoc. (2011) 103:375. doi: 10.1016/S0027-9684(15)30321-7
46. Metzl JM, MacLeish KT. Mental illness, mass shootings, and the politics of American firearms. Am J Pub Health. (2015) 105:240–9. doi: 10.2105/AJPH.2014.302242
47. Chow WS, Priebe S. Understanding psychiatric institutionalization: a conceptual review. BMC Psychiatry. (2013) 13:1–14. doi: 10.1186/1471-244X-13-169
48. Phelan JC, Link BG, Stueve A, Pescosolido BA. Public conceptions of mental illness in 1950 and 1996: what is mental illness and is it to be feared? J Health Soc Behav. (2000) 41:188–207. doi: 10.2307/2676305
49. Lin L, Stamm K, Christidis P. How Diverse is the Psychology Workforce? Worcester, MA: American Psychological Association (2018).
50. Faber S, Williams MT, Metzger IW, MacIntyre MM, Strauss D, Duniya CG, et al. Lions at the gate: How weaponization of policy prevents people of colour from becoming professional psychologists in Canada. Canadian Psychol. (In Press). doi: 10.1037/cap0000352
51. Chapman LK, DeLapp R, Williams MT. Impact of race, ethnicity, and culture on the expression and assessment of psychopathology. In DC Beidel, BC Frueh, M Hersen, editors, Adult Psychopathology and Diagnosis. John Wiley and Sons, Inc, 131–56 (2018).
52. Ninan PT, Shelton S. Managing psychotic symptoms when the diagnosis is unclear. Hospital Commun. Psychiatry. (1993) 44:107–8. doi: 10.1176/ps.44.2.107
53. Louie P, Wheaton B. Prevalence and patterning of mental disorders through adolescence in 3 cohorts of Black and White Americans. Am J Epidemiol. (2018) 187:2332–8. doi: 10.1093/aje/kwy144
54. Thomas Tobin CS, Erving CL, Hargrove TW, Satcher LA. Is the Black-White mental health paradox consistent across age, gender, and psychiatric disorders? Aging Mental Health. (2022) 26:196–204. doi: 10.1080/13607863.2020.1855627
55. Jongsma HE, Gayer-Anderson C, Tarricone I, Velthorst E, van der Ven E, Quattrone D, et al. Social disadvantage, linguistic distance, ethnic minority status and first-episode psychosis: Results from the EU-GEI case–control study. Psychol Med. (2021) 51:1536–48. doi: 10.1017/S003329172000029X
56. Fernando S. Cultural Diversity, Mental Health and Psychiatry : The Struggle Against Racism. New York, NY: Brunner-Routledge. (2003).
57. Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Pub Health. (2003) 93:200–8. doi: 10.2105/AJPH.93.2.200
58. Whaley AL. Cultural mistrust and mental health services for African Americans: a review and meta-analysis. Couns Psychol. (2001) 29:513–31. doi: 10.1177/0011000001294003
59. Rouhakhtar PR, Roemer C, Reeves G, Schiffman J. The associations between attenuated psychosis symptoms and functioning in Black and White youth at clinical high-risk for psychosis. Schizophr Res. (In press) 1–8. doi: 10.1016/j.schres.2021.11.032
60. Combs DR, Penn DL, Fenigstein A. Ethnic differences in subclinical paranoia: an expansion of norms of the Paranoia Scale. Cult Div Ethnic Minority Psychol. (2002) 8:248–56. doi: 10.1037/1099-9809.8.3.248
61. Mosley DV, Owen KH, Rostosky SS, Reese RJ. Contextualizing behaviors associated with paranoia: perspectives of Black men. Psychol Men Masculinity. (2017) 18:165–75. doi: 10.1037/men0000052
62. Hall WJ, Chapman MV, Lee KM, Merino YM, Thomas TW, Payne BK, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Pub Health. (2015) 105:60–76. doi: 10.2105/AJPH.2015.302903
63. Plaisime MV, Malebranche DJ, Davis AL, Taylor JA. Healthcare providers' formative experiences with race and Black male patients in urban hospital environments. J Racial Ethnic Health Disp. (2017) 4:1120–7. doi: 10.1007/s40615-016-0317-x
64. Cuevas AG, O'Brien K, Saha S. African American experiences in healthcare: “I always feel like I'm getting skipped over”. Health Psychology. (2016) 35:987–95. doi: 10.1037/hea0000368
65. Cuevas AG, O'Brien K, Saha S. What is the key to culturally competent care: Reducing bias or cultural tailoring? Psychol Health. (2017) 32:493–507. doi: 10.1080/08870446.2017.1284221
66. Strakowski SM, Hawkins JM, Keck PE Jr, McElroy SL, West SA, Bourne ML, et al. The effects of race and information variance on disagreement between psychiatric emergency service and research diagnoses in first-episode psychosis. J Clin Psychiatry. (1997) 58:457–63. doi: 10.4088/JCP.v58n1010a
67. Strakowski SM, Keck PE, Arnold LM, Collins J, Wilson RM, Fleck DE, et al. Ethnicity and diagnosis in patients with affective disorders. J Clin Psychiatry. (2003) 64:747–54. doi: 10.4088/JCP.v64n0702
68. Gara MA, Vega WA, Arndt S, Escamilla M, Fleck DE, Lawson WB, et al. Influence of patient race and ethnicity on clinical assessment in patients with affective disorders. Arch Gen Psychiatr. (2012) 69:593–600. doi: 10.1001/archgenpsychiatry.2011.2040
69. Peltier MR, Cosgrove SJ, Ohayagha K, Crapanzano KA, Jones GN. Do they see dead people? Cultural factors and sensitivity in screening for schizophrenia spectrum disorders. Ethnicity Health. (2017) 22:119–29. doi: 10.1080/13557858.2016.1196650
70. Siddle R, Haddock G, Tarrier N, Faragher EB. Religious delusions in patients admitted to hospital with schizophrenia. Soc Psychiatry Psychiatr Epidemiol. (2002) 37:130–8. doi: 10.1007/s001270200005
71. Schizophrenia Working Group. Biological insights from 108 schizophrenia-associated genetic loci. Nature. (2014) 511, 421–427. doi: 10.1038/nature13595
72. Marshall M. The hidden links between mental disorders. Nature. (2020) 581:19–21. doi: 10.1038/d41586-020-00922-8
73. Trubetskoy V, Pardiñas AF, Qi T, Panagiotaropoulou G, Awasthi S, Bigdeli TB, et al. Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature. (2022) 604:502–8. doi: 10.1038/s41586-022-04434-5
74. Jongsma HE, Karlsen S, Kirkbride JB, Jones PB. Understanding the excess psychosis risk in ethnic minorities: the impact of structure and identity. Soc Psychiatry Psychiatr Epidemiol. (2021) 56:1913–21. doi: 10.1007/s00127-021-02042-8
75. McLaughlin KA, Alvarez K, Fillbrunn M, Green JG, Jackson JS, Kessler RC, et al. Racial/ethnic variation in trauma-related psychopathology in the United States: a population-based study. Psychol Med. (2019) 49:2215–26. doi: 10.1017/S0033291718003082
76. Sibrava NJ, Bjornsson AS, Pérez Benítez ACI, Moitra E, Weisberg RB, Keller MB, et al. Posttraumatic stress disorder in African American and Latinx adults: Clinical course and the role of racial and ethnic discrimination. Am Psychol. (2019) 74:101–6. doi: 10.1037/amp0000339
77. Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A, et al. Childhood trauma and children's emerging psychotic symptoms: a genetically sensitive longitudinal cohort study. Am J Psychiatry. (2011) 168:65–72. doi: 10.1176/appi.ajp.2010.10040567
78. Smith B,. Why Chicago's MasterChef Star Killed Himself. Chicago Magazine. (2014). Available online at: https://www.chicagomag.com/Chicago-Magazine/July-2014/Josh-Marks/ (accessed June 23, 2014).
79. Bailey T, Alvarez-Jimenez M, Garcia-Sanchez AM, Hulbert C, Barlow E, Bendall S, et al. Childhood trauma is associated with severity of hallucinations and delusions in psychotic disorders: a systematic review and meta-analysis. Schizophr Bull. (2018) 44:1111–22. doi: 10.1093/schbul/sbx161
80. Anglin DM, Ereshefsky S, Klaunig MJ, Bridgwater MA, Niendam TA, Ellman LM, et al. From womb to neighborhood: a racial analysis of social determinants of psychosis in the United States. Am J Psychiatr. (2021) 178:599–610. doi: 10.1176/appi.ajp.2020.20071091
81. Wickham S, Taylor P, Shevlin M, Bentall RP. The impact of social deprivation on paranoia, hallucinations, mania and depression: the role of discrimination social support, stress and trust. PLoS ONE. (2014) 9:e105140. doi: 10.1371/journal.pone.0105140
82. Varchmin L, Montag C, Treusch Y, Kaminski J, Heinz A. Traumatic events, social adversity and discrimination as risk factors for psychosis - An umbrella review. Front Psychiatry. (2021) 12:1–15. doi: 10.3389/fpsyt.2021.665957
83. Williams MT, Metzger IW, Leins C, DeLapp C. Assessing racial trauma within a DSM−5 framework: The UConn racial/ethnic stress and trauma survey. Prac Innov. (2018) 3:242–60. doi: 10.1037/pri0000076
84. Heun-Johnson H, Menchine M, Axeen S, Lung K, Claudius I, Wright T, et al. Association between race/ethnicity and disparities in health care use before first-episode psychosis among privately insured young patients. JAMA Psychiatry. (2021) 78:311–9. doi: 10.1001/jamapsychiatry.2020.3995
85. McGlashan TH, Walsh BC, Woods SW, editors. Psychosis-risk syndromes and psychosis in the SIPS. In: The Psychosis-Risk Syndrome: Handbook for Diagnosis and Follow-Up. Oxford: Oxford University Press (2010), pp. 24–33.
86. Nørgaard HCB, Søndergaarde Pederson H, Fenger-Grøn M, Mors O, Nordencroft M, Vestergaarde T, et al. Increased use of primary care during 6 years of prodromal schizophrenia. Acta Psychiatr Scand. (2016) 134:225–33. doi: 10.1111/acps.12600
87. Kane JM, Robinson DG, Schooler NR, Mueser KT, Penn DL, Rosenheck RA, et al. Comprehensive versus usual community care for first-episode psychosis: 2-year outcomes from the NIMH RAISE early treatment program. Am J Psychiatry. (2016) 173:362–72. doi: 10.1176/appi.ajp.2015.15050632
88. Melle I, Larsen TK, Haahr U, Friis S, Johannesen JO, Opjordsmoen S, et al. Prevention of negative symptom psychopathologies in first-episode schizophrenia: two-year effects of reducing the duration of untreated psychosis. Arch Gen Psychiatry. (2008) 65:634–40. doi: 10.1001/archpsyc.65.6.634
89. Michaels TI, Carrion R, Addington J. Ethnoracial discrimination and the development of suspiciousness symptoms in individuals at clinical high-risk for psychosis. Schizophrenia Res. (2022).
90. Segal SP, Bola JR, Watson MA. Race, quality of care, and antipsychotic prescribing practices in psychiatric emergency services. Psychiatric Serv. (1996) 47:282–6. doi: 10.1176/ps.47.3.282
91. Herbeck DM, West JC, Ruditis I, Duffy FF, Fitek DJ, Bell CC, et al. Variations in use of second-generation antipsychotic medication by race among adult psychiatric patients. Psychiatric Serv. (2004) 55:677–84. doi: 10.1176/appi.ps.55.6.677
92. Cook TB, Reeves GM, Teufel J, Postolache TT. Persistence of racial disparities in prescription of first-generation antipsychotics in the USA. Pharmacoepidemiol Drug Saf. (2015) 24:1197–206. doi: 10.1002/pds.3819
93. Knight S, Jarvis GE, Ryder AG, Lashley M, Rousseau C. Ethnoracial differences in coercive referral and intervention among patients with first-episode psychosis. Psychiatric Services. (2022) 73:2–8. doi: 10.1176/appi.ps.202000715
94. Swartz MS, Swanson JW, Hannon MJ. Does fear of coercion keep people away from mental health treatment? Evidence from a survey of persons with schizophrenia and mental health professionals. Behav Sci Law. (2003) 21:459–72. doi: 10.1002/bsl.539
95. Paksarian D, Mojtabai R, Kotov R, Cullen B, Nugent KL, Bromet EJ, et al. Perceived trauma during hospitalization and treatment participation among individuals with psychotic disorders. Psychiatric Serv. (2014) 65:266–9. doi: 10.1176/appi.ps.201200556
96. Oluwoye O, Stokes B. The unique pathways to coordinate specialty care for Black families navigating early psychosis: a preliminary report. Schizophrenia Res. (2021) 4:1–6. doi: 10.1016/j.schres.2021.11.004
97. Rogler LH, Cortes DE. Help-seeking pathways: a unifying concept in mental health care. Am J Psychiatry. (1993) 150:554–61. doi: 10.1176/ajp.150.4.554
98. Allan SM, Hodgekins J, Beazley P, Oduola S. Pathways to care in at-risk mental states: a systematic review. Early Interv Psychiatry. (2021) 15:1092–103. doi: 10.1111/eip.13053
99. Rotenberg M, Tuck A, Ptashny R, McKenzie K. The role of ethnicity in pathways to emergency psychiatric services for clients with psychosis. BMC Psychiatry. (2017) 17:137–47. doi: 10.1186/s12888-017-1285-3
100. Bergner E, Leiner AS, Carter T, Franz L, Thompson NJ, Compton MT, et al. The period of untreated psychosis before treatment initiation: a qualitative study of family members' perspectives. Compr Psychiatry. (2008) 49:530–6. doi: 10.1016/j.comppsych.2008.02.010
101. Tambling RR, D'Aniello C, Russell BS. Mental health literacy: a critical target for narrowing racial disparities in behavioral health. Int J Ment Health Addict. (2021) 11:1–15. doi: 10.1007/s11469-021-00694-w
102. Thornicroft G. Most people with mental illness are not treated. Lancet. (2007) 370:807–8. doi: 10.1016/S0140-6736(07)61392-0
103. Williams MT. Race-Based Determinants of Mental Health and Racial Trauma. Clinical Health Psychology, Grand Rounds. Winnipeg, MB: University of Manitoba (2022).
104. De Vries D, van Busschbach B, van der Stouwe JT, Aleman ECD, van Dijk A, Lysaker JJM, et al. Prevalence rate and risk factors of victimization in adult patients with a psychotic disorder: a systematic review and meta-analysis. Schizophr Bull. (2019) 45:114–26. doi: 10.1093/schbul/sby020
105. Fuller DA, Lamb HR, Biasotti M, Snook J. Overlooked in the Undercounted: The Role of Mental Illness in Fatal Law Enforcement Encounters. Arlington, VA: Treatment Advocacy Center (2015).
106. Saleh AZ, Applebaum PS, Liu X, Stroup TS, Wall M. Deaths of people with mental illness during interactions with law enforcement. Int J Law Psychiatry. (2018) 58:110–6. doi: 10.1016/j.ijlp.2018.03.003
107. Centre for Addiction Mental Health. CAMH Statement on Police Interactions With People in Mental Health Crisis. CAMH News and Stories. (2020). Available online at: https://www.camh.ca/en/camh-news-and-stories/camh-statement-on-police-interactions-with-people-in-mental-health-crisis (accessed June 23, 2020).
108. Mulay AL, Vayshenker B, West ML, Kelly E. Crisis intervention training and implicit stigma toward mental illness: reducing bias among criminal justice personnel. Int J Forensic Ment Health. (2016) 15:369–81. doi: 10.1080/14999013.2016.1208308
109. Spencer KB, Charbonneau AK, Glaser J. Implicit bias and policing. Soc Personal Psychol Compass. (2016) 10:50–63. doi: 10.1111/spc3.12210
110. Ross CT, Winterhalder B, McElreath R. Racial disparities in police use of deadly force against unarmed individuals persist after appropriately benchmarking shooting data on violent crime rates. Soc Psychol Personal Sci. (2021) 12:323–32. doi: 10.1177/1948550620916071
111. Brown SM,. Anxiety racism result in more Blacks killed by police. The Washington Informer. (2022). Available online at: https://www.washingtoninformer.com/anxiety-and-racism-result-in-more-blacks-killed-by-police/ (accessed April 26, 2022).
112. Williams M, Osman M, Gran-Ruaz S, Strauss D, Zare M. Performative shooting exercises do not predict real-world racial bias in police officers. Can J Behav Sci. (2022) 1–11. doi: 10.1037/cbs0000332
113. Alvarado F, Miller, ME, Berman, M,. North Miami Police Shoot Black Man Who Said his Hands Were Raised While he Tried to Help Autistic Group-Home Resident. The Washington Post. (2016). Available online at: https://www.washingtonpost.com/news/morning-mix/wp/2016/07/21/fla-police-shoot-black-man-with-his-hands-up-as-he-tries-to-help-autistic-patient/ (accessed July 21, 2016).
114. Al-Rousan T, Rubenstein L, Sieleni B, Deol H, Wallace RB. Inside the nation's largest mental health institution: a prevalence study in a state prison system. BMC Public Health. (2017). 17:1–9. doi: 10.1186/s12889-017-4257-0
115. Federal Bureau of Prisons. Inmate Race. Statistics. (2022). Available online at: https://www.bop.gov/about/statistics/statistics_inmate_race.jsp (accessed July 30, 2022).
116. Gramlich J,. The Gap Between the Number of Blacks Whites in Prison is Shrinking. Pew Research Center. (2019). Available online at: https://www.pewresearch.org/fact-tank/2019/04/30/shrinking-gap-between-number-of-blacks-and-whites-in-prison/ (accesssed April 30, 2019).
117. Owusu-Bempah A, Jung M, Sbaï F, Wilton AS, Kouyoumdjian F. Race and incarceration: the representation and characteristics of Black people in provincial correctional facilities in Ontario, Canada. Race Justice. (2021) 8:1–13. doi: 10.1177/21533687211006461
118. Nasser S. No Criminal Charges for Officers in Death of Black Man With Mental Illness Tasered in Own Backyard. CBC News. (2021). Available online at: https://www.cbc.ca/news/canada/toronto/clive-mensah-black-man-taser-peel-police-1 (accessed March 29, 2021).
119. Nasser S,. No Charges in Death of Ejaz Choudry, 62-Year-Old Shot Killed by Police While in Crisis. CBC News. (2021). Available online at: https://www.cbc.ca/news/canada/toronto/ejaz-choudry-no-charges-siu-peel-police-1 (accessed April 6, 2021).
120. Ramkaran R,. Police are Deadly to People in Crisis: No Justice as the Officer Who Killed Ejaz Ahmed Choudry Escapes Charges. An Injustice! (2021). Available online at: https://aninjusticemag.com/police-are-deadly-to-people-in-crisis-fbd36a3c45a1 (accessed April 7, 2021).
121. Westoll N,. Justice for Regis Korchinski-Paquet March held in Toronto as Anniversary of Death Approaches. Global News. (2021). Available online at: https://globalnews.ca/news/7887172/regis-korchinski-paquet-memorial-march-toronto-police/ (accessed May 24, 2021).
122. Kelley M, Syed R. Family of Young Black Man Killed in Brampton, Ont., Says He Was Shot by Police After Calling 911 Himself. CBC News. (2020). Available online at: https://www.cbc.ca/news/canada/toronto/fifth-estate-d-andre-campbell-police-shooting-family-1 (accessed June 8, 2020).
123. Sholtis B,. Family mourns man with mental illness killed by police calls for change. Kaiser Health News. (2020). Available online at: https://khn.org/news/police-killing-mental-illness-emergency-crisis-care-pennsylvania/ (accessed November 19, 2020).
124. Calkins L. Detained and drugged: a brief overview of the use of pharmaceuticals for the interrogation of suspects, prisoners, patients, and POWs in the US. Bioethics. (2010) 24:27–34. doi: 10.1111/j.1467-8519.2009.01774.x
125. Ortiz E,. Elijah McClain Was Injected With Ketamine While Handcuffed. Some Medical Experts Worry About its Use During Police Calls. US News. (2020). Available online at: https://www.nbcnews.com/news/us-news/elijah-mcclain-was-injected-ketamine-while-handcuffed-some-medical-experts-n1232697 (accessed July 3, 2020).
126. Mutchler C,. New AMA policy opposes “excited delirium” diagnosis. American Medical Association. (2021). Available online at: https://www.ama-assn.org/press-center/press-releases/new-ama-policy-opposes-excited-delirium-diagnosis (accessed June 14, 2021).
127. Grant JR, Southall PE, Mealey J, Scott SR, Fowler D. Excited delirium deaths in custody past and present. Am J Forensic Med Pathol. (2009) 30:1–5. doi: 10.1097/PAF.0b013e31818738a0
128. Young R, McMahon, S,. Some States Allow Authorities to Use Ketamine to Subdue Suspects in the Field. But is it Safe? WBUR. (2020). Available online at: https://www.wbur.org/hereandnow/2020/09/08/ketamine-police-safety-elijah-mcclain (accessed September 8, 2020).
129. Tompkins L,. Here's What You Need to Know About Elijah McClain's Death. The New York Times. (2022). Available online at: https://www.nytimes.com/article/who-was-elijah-mcclain.html (accessed January 18, 2022).
130. Appelbaum PS. Excited delirium, ketamine, and deaths in police custody. Psychiatric Serv. (2022) 73:827–9. doi: 10.1176/appi.ps.20220204
131. Aboraya A. Use of structured interviews by psychiatrists in real clinical settings: Results of an open-question survey. Psychiatry. (2009) 6:24–8.
132. Jackson JS, Neighbors HW, Nesse RM, Trierweiler SJ, Torres M. Methodological innovations in the National Survey of American life. Int J Methods Psychiatr Res. (2004) 13:289–98. doi: 10.1002/mpr.182
133. Jorm AF. Mental health literacy: empowering the community to take action for better mental health. Am Psychol. (2012) 67:231–43. doi: 10.1037/a0025957
134. Muvuka B, Combs R, Ali N, Scott H, Williams M. Depression is real: Developing a health communication campaign in an urban African American community. Res Educ Action. (2020) 14:161–72. doi: 10.1353/cpr.2020.0029
135. CPA. MindStylz. Connecticut Psychological Association. (2021). Available online at: https://connpsych.org/mindstylz/ (accessed October 24, 2021).
136. Hankerson SH, Shelton R, Weissman M, Wells KB, Teresi J, Mallaiah J, et al. Study protocol for comparing Screening, Brief Intervention, and Referral to Treatment (SBIRT) to referral as usual for depression in African American churches. Trials. (2022) 23:1–20. doi: 10.1186/s13063-021-05767-8
137. Hillel I, Ottenhof, N, Ahmad, S,. Alternatives for a safer Ottawa: Non-police mental health crisis response executive summary, Ottawa, ON: Vivic Research. (2021). Available online at: https://vivicresearch.ca/work/non-police-mental-health-crisis-response-for-the-city-of-ottawa (accessed December 20, 2022).
138. Support Team Assistance Response,. STAR program evaluation, Denver, CO: Support Team Assistance Response. (2021). Available online at: https://wp-denverite.s3.amazonaws.com/wp-content/uploads/sites/4/2021/02/STAR_Pilot_6_Month_Evaluation_FINAL-REPORT.pdf (accessed January 8, 2021).
139. Medlock M, Weissman A, Wong S, Carlo A, Zeng M, Borba C, et al. Racism as a unique social determinant of mental health: development of a didactic curriculum for psychiatry residents. MedEdPORTAL13. (2017) 1–9. doi: 10.15766/mep_2374-8265.10618
140. Miles R, Rabin L, Krishnan A, Grandoit E, Kloskowski K. Mental health literacy in a diverse sample of undergraduate students: demographic, psychological, and academic correlates. BMC Public Health. (2020) 20:1–13. doi: 10.1186/s12889-020-09696-0
141. Fleischhacker W, Arango C, Arteel P, Barnes TRE, Carpenter W, Duckworth K, et al. Schizophrenia—Time to commit to policy change. Schizophrenia Bulletin. (2014) 40:165–94. doi: 10.1093/schbul/sbu006
142. Hankerson SH, Weissman MM. Church-based health programs for mental disorders among African Americans: a review. Psychiatric Serv. (2012) 63:243–9. doi: 10.1176/appi.ps.201100216
143. El-Mallakh RS, Spratt D, Butler C, Strauss G. Evaluation of consequences of implementation of police crisis intervention team in Louisville. J Kentucky Med Assoc. (2008) 106:435–7.
144. Teller JL, Munetz MR, Gil KM, Ritter C. Crisis intervention team training for police officers responding to mental disturbance calls. Psychiatric Serv. (2006) 57:232–7. doi: 10.1176/appi.ps.57.2.232
145. Pickett JT, Graham A, Cullen FT. The American racial divide in fear of the police. Criminology. (2022) 60:291–320. doi: 10.1111/1745-9125.12298
146. Smith Lee JR, Robinson MA. “That's my number one fear in life. It's the police”: Examining young Black men's exposures to trauma and loss resulting from police violence and police killings. J Black Psychol. (2019) 45:143–84. doi: 10.1177/0095798419865152
147. Anene E, Nallajerla M, Bath EPJ, Castillo EG. Revisiting research safety protocols: the urgency for alternatives to law enforcement in crisis intervention. Psychiatric Servi. (2022) 25:1–4. doi: 10.1176/appi.ps.20220084
148. Corneau S, Stergiopoulos V. More than being against it: anti-racism and anti-oppression in mental health services. Transcult Psychiatry. (2012) 49:261–82. doi: 10.1177/1363461512441594
149. Williams MT, Faber S, Nepton A, Ching THW. Racial justice allyship requires civil courage: A behavioral prescription for moral growth and change. Am Psychol. (2023) 78:1–19. doi: 10.1037/amp0000940
150. Faber SC, Osman M, Williams MT. Access to mental health care in Canada. Int J Ment Health. (2022).
151. Graham-LoPresti J, Williams MT, Rosen DC. Culturally responsive assessment and diagnosis for clients of color. In MT Williams, DC Rosen, JW Kanter, editors Eliminating Race-Based Mental Health Disparities: Promoting Equity and Culturally Responsive Care Across Settings. New York, NY: New Harbinger Books, p. 169–85 (2019).
Keywords: psychosis, Black communities, discrimination, racism, misdiagnosis, weaponization of medicine, schizophrenia
Citation: Faber SC, Khanna Roy A, Michaels TI and Williams MT (2023) The weaponization of medicine: Early psychosis in the Black community and the need for racially informed mental healthcare. Front. Psychiatry 14:1098292. doi: 10.3389/fpsyt.2023.1098292
Received: 14 November 2022; Accepted: 11 January 2023;
Published: 09 February 2023.
Edited by:
April Joy Damian, Weitzman Institute, United StatesReviewed by:
Mary V. Seeman, University of Toronto, CanadaJude Bergkamp, Antioch University Seattle, United States
Copyright © 2023 Faber, Khanna Roy, Michaels and Williams. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sonya C. Faber,  ZGZhYmVyQHVvdHRhd2EuY2E=; Monnica T. Williams,
ZGZhYmVyQHVvdHRhd2EuY2E=; Monnica T. Williams,  bW9ubmljYS53aWxsaWFtc0B1b3R0YXdhLmNh
bW9ubmljYS53aWxsaWFtc0B1b3R0YXdhLmNh
 Sonya C. Faber
Sonya C. Faber Anjalika Khanna Roy
Anjalika Khanna Roy Timothy I. Michaels
Timothy I. Michaels Monnica T. Williams
Monnica T. Williams