
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychiatry , 18 July 2023
Sec. Psychological Therapy and Psychosomatics
Volume 14 - 2023 | https://doi.org/10.3389/fpsyt.2023.1098122
This article is part of the Research Topic Assessments and Measures in Psychotherapy Research: Going Beyond Self-Report Data View all 12 articles
 Andrea Andorfer1,2
Andrea Andorfer1,2 Sabina Kraler3
Sabina Kraler3 Paul Kaufmann4
Paul Kaufmann4 Ewald Pollheimer4
Ewald Pollheimer4 Christoph Spah4
Christoph Spah4 Jürgen Fuchshuber2,5
Jürgen Fuchshuber2,5 Christian Rominger3
Christian Rominger3 Claudia Traunmüller3
Claudia Traunmüller3 Andreas Schwerdtfeger3
Andreas Schwerdtfeger3 Human-Friedrich Unterrainer1,2,3,6,7*
Human-Friedrich Unterrainer1,2,3,6,7*Objectives: Mindfulness-based interventions (including self-compassion interventions) are effective in improving stress management at psychological and physical levels. Mindful Self-Compassion (MSC) is a newly developed program particularly aimed at increasing self-compassion. The main objective of this study was to determine whether the psychophysiological stress response during a social-evaluative speaking task differs in inpatients participating in the MSC or the Progressive Muscle Relaxation (PMR) program at the end of their 6-week psychiatric rehabilitation stay (i.e., post-test only design).
Method: Data from 50 inpatients (25 MSC, 25 PMR, 35 female) aged 19 to 76 years (M = 47.22, SD = 12.44) were analyzed in terms of psychophysiological stress response. For this purpose, heart rate variability, heart rate, and blood pressure were assessed together with several psychometric variables: positive and negative affect (PANAS), subjective stress perception (Visual Analog Scale), self-compassion (Self-Compassion Scale), cognitive reappraisal and suppression (Emotion Regulation Questionnaire), psychological distress (Brief Symptom Inventory-18), and appraisal and rumination (selected items).
Results: After correction for alpha inflation no differences in the psychophysiological stress response and psychometric parameters between the MSC and PMR group were found.
Discussion: In general, our results indicate that MSC is not superior to PMR training. However, more research with clinical randomized controlled trials investigating larger samples are needed to further affirm these initial findings.
Stress plays an important role in psychiatric diseases and can be responsible for the frequency and actual course of mental illness (1, 2). According to Selye (3) stress is related to a physical reaction in the body. It helps us to survive by converting the unbalanced state in our body to homeostasis (4). Immediate adaptations include a rise in Heart Rate (HR), Blood Pressure (BP), and glucose consumption, concurrent lack of appetite, activation of the immune system and mobilization for energy regulated by the Autonomic Nervous System (ANS) comprising the Sympathetic Nervous System (SNS) and the Parasympathetic Nervous System (PNS) (5–7). Parasympathetic activity is associated with vagal tone which can be measured by the changes in duration of heartbeats (8). These rapid beat-to-beat changes are predominantly due to the PNS, which is reflected in Heart Rate Variability (HRV) and can be used to assess ANS function (9, 10). Accordingly, the brain and heart are bidirectionally connected, as the brain influences the heart and vice versa (10, 11).
Elevated HRV, which refers to greater variability and higher vagal tone, signifies greater stress adaptability (12). Additionally, it has been associated with more positive emotions, more enjoyment of social interaction, less negative emotions during stressful tasks and higher social connectedness (13–15). In contrast, lowered HRV has been suggested to be a marker for all types of diseases and can predict mortality (16, 17). In correspondence to this, various mental diseases such as panic disorder, posttraumatic stress disorder and depression are linked with an imbalance in the ANS, as evidenced by attenuated HRV compared to healthy controls (18–20). The Neurovisceral Integration Model, introduced by Thayer and Lane (21), offers a possible explanation regarding the relationship between psychopathology, stress, and HRV. It postulates that stress could impact brain function, thus hampering adaptive and flexible behavior as indicated by low HRV (10, 22, 23). Therefore, developing effective treatment programs to counter stress associated with psychopathology is of special interest in scientific research (24).
Treatment methods of high relevance and increased recognition in recent years are MBI (25, 26). These techniques are about accepting the reality we live in, letting go off thoughts and living in the here and now, which could facilitate psychological well-being (27). Evidence showed efficacy of MBI in reducing stress, anxiety, and depression in clinical populations (28–30) as well as in healthy subjects (31–33). Furthermore, they appeared to be linked with a substantial increase in self-compassion, quality of life, coping with problems, happiness, resilience and overall psychological well-being (34–37).
A specific MBI essential in the present study is the MSC program founded by Neff and Germer (38). Self-compassion has gained increased attention since its introduction in 2003 (39) and can be described as “the ability to be kind and understanding toward ourselves when we suffer, fail, or feel inadequate” (40, p. 861). The program contains the three important aspects: self-kindness versus self-judgment, mindfulness versus over-identification, and common humanity versus isolation (40). MSC comprises an 8-week program, with one session each week (2.5 h) and a half-day silent meditation retreat (38). It consists of guided sessions including various topics regarding self-compassion (i.e., practicing loving-kindness) and additional homework which enables to practice self-compassion in a formal (sitting meditation) as well as an informal (during everyday life) way (38, 40). Neff and Germer (38) demonstrated that the MSC program improved self-compassion, mindfulness, sympathy for others, life happiness, as well as well-being, and lowers stress, anxiety, and depression.
Self-compassion has shown to be repeatedly associated with well-being and coping with unpleasant or stressful life events (41–46). People high in self-compassion showed decreased worry, rumination, subjective stress, and positive emotion regulation (47–49). In sum, self-compassion is a well-established program to reduce psychological stress and help to better cope with stressful situations (50–52). However, to the authors’ knowledge, there are few findings on self-compassion and physiological stress reactivity. In general, research demonstrated that mindfulness could buffer physiological stress responses (53, 54). Correspondingly, literature showed an increase in HRV and decrease in BP during mindfulness training (55–57). Additionally, self-compassion and mindfulness training could lead to better stress coping and buffer physiological stress (58–61). However, findings are heterogenous (62–64).
In the psychiatric rehabilitation clinic Sonnenpark Neusiedlersee in Rust, Austria, the MSC program was modified to fit the typical 6-week length of stay at the clinic to see if this form of MSC shows positive results. While some of the meditations and exercises, such as the inquiry, are identical to the 8-week MSC course, other parts are modified to suit the patients need in the rehabilitation clinic. Gaiswinkler et al. (51) demonstrated higher self-compassion and happiness after 6-week MSC program in comparison to the active control intervention of Progressive Muscle Relaxation (PMR) in this rehabilitation clinic. Moreover, they observed psychiatric and quality of life parameters improving in both groups to the same extent (51). PMR is a very well-established and empirically strong validated relaxation technique (65). Individual muscle groups are tensed and loosened immediately after to increase inner relaxation (66). More specifically it can be useful to decrease stress (67). Since it does not include the mindful/ self-compassion aspect it previously has been chosen as an adequate option for an active control group (68, 69).
The primary aim of this study was to investigate if rehabilitation in-patients who received MSC training show less pronounced stress reactions compared to patients who received PMR training regarding psychophysiological stress reactivity using a social-evaluative stress paradigm. HRV, HR, BP, Positive and Negative Affect (PA/NA), and Subjective Stress Perception (SSP) were compared between groups. So far, the MSC program has only been explored on a psychometric level (51). Therefore, this study served to explore the MSC program on a biometric level in a clinical setting. We expected lower physiological responses to the stressor in the MSC group (i.e., lower HRV decrease, HR increase, and blood pressure increase, from baseline to stress). For secondary outcome, we intended to investigate whether Self-Compassion, Emotion Regulation (Cognitive Reappraisal and Suppression), and Appraisal are higher in the MSC compared to the PMR group. Furthermore, we expected that Rumination and Psychological Distress should be higher in the PMR group.
The presented study is part of a broader study (n = 170) which has not yet been published. Within that study, patients were randomly assigned into two groups (MSC, PMR) prior to their start of the rehabilitation stay. For the present study, the randomized allocation was adopted. Participants were adults attending a 6-week psychiatric rehabilitation stay at Sonnenpark Neusiedlersee clinic, located in Burgenland, Austria. All exclusion criteria of the rehabilitation clinic applied to the current study, such as acute suicidal and psychotic episodes or acute addiction disorders, determined by the treating psychiatrist at the clinic. Besides, people with severe cardiovascular diseases were not included. In this investigation, 59 participants were recruited of which nine were excluded (4 = drop out, 3 = no speech, 1 = cardiac arrythmia, 1 = previous stroke). All participants signed a consent form and the investigator ensured that participation was voluntary and withdrawal from consent throughout possible. After the examination, they got a coffee voucher from the in-house café. A sample of 50 individuals (35 female) aged from 19 to 76 (M = 47.22, SD = 12.44) was examined (25 MSC, 25 PMR). The study was ethically approved by the ethics committee of the University of Graz (GZ. 39/84/63 ex 2020/21).
A mobile electrocardiogram [ECG; VarioPort (70)] provided by the University of Graz with sampling rate of 256 Hz was used to measure HRV and HR non-invasively (Becker Meditec, Karlsruhe, Germany). Three electrodes were placed on the right collar bone, below the left ribcage and on the lower abdomen [modified Einthoven Lead II; (71, 72)]. As indices of HRV established time-domain (Root Mean Square of Successive Differences (RMSSD); Standard Deviation of NN Intervals (SDNN)) and frequency-domain measures (High-Frequency HRV (HF-HRV [0.15–0.4 Hz]); Low-Frequency HRV (LF-HRV [0.04–0.15 Hz])) were assessed (73, 74). RMSSD is mostly used in HRV research and indicates mainly vagal, parasympathetic activity as well as HF (10, 75). SDNN and LF represent the cumulative variance of sympathetic and parasympathetic function (74, 76). Respiration rate, assessed via a respiration belt, was added as a control variable (73). An automated BP device (Bosch + Sohn, Boso Medicus (77),) was used to assess Systolic (SYS) and Diastolic (DIA) BP, and was applied on the right upper arm.
Before the arrival in the rehabilitation clinic an independent work counsellor assigned patients randomly to the MSC and PMR group with permuted block for gender, age, and psychiatric diagnosis, which allowed maintaining a balance between treatment groups (78). Both interventions took place once a week for 75 min over 6 weeks and were guided by an experienced MSC or PMR trainer. On the basis of this initial assignment, the patients also participated in the present experimental study (see Figure 1).
The stress intervention was based on common social-evaluative stress protocols that have proven to be valid in inducing stress comparable to a negative stress situation, such as the Trier Social Stress Test (TSST) or public speaking tasks (79–85). Participants were prompted to give a 5-min speech introducing themselves for a job offer of their choice. They were filmed and told that the speech was going to be evaluated by experts. Beforehand, they could prepare some ideas by means of questions. After 3 min the judge stopped the speech. If the participants finished their speech before the expiration of time, the investigator asked standardized questions to not stop the flow of speech.
For primary outcome: The Positive and Negative Affect Schedule [PANAS; (86)] measures PA and NA with 10 adjectives each on a 5-point Likert scale (1 = not at all to 5 = extremely). Participants rated how much the adjectives described their emotional state at that moment. Internal consistency (Cronbach’s α) was high (PA: baseline = 0.86, speech prep. = 0.92, recovery = 0.93; NA: baseline = 0.87, speech prep. = 0.86, recovery = 0.87).
Participants’ SSP was assessed on a visual analogue scale (0–100) where 100 (extremely stressed) was the highest degree to which they perceived the situation as stressful (81, 87).
Appraisal items were administered with a 6-point Likert scale (1 = not at all to 6 = extremely). A Demand Resource Evaluation Score (DRES) was formed by subtracting means of evaluated demands (task demand/threat) from means of resources (coping, performance, perceived control, experience) (85, 88, 89). A positive score stands for an Appraisal more of a challenge state and a negative score for threat state (88). Internal consistency was acceptable (threat = 0.78, resources = 0.83).
Rumination was assessed with seven items based on the Rumination Thought Style Scale (RTS), the Rumination-Suppression Scale (RS-8), and the Thoughts Questionnaire [TQ; (90–92)]. Participants rated on a 6-point Likert scale (1 = strongly disagree to 6 = strongly agree). Cronbach’s α was 0.83.
Secondary outcomes included the Self-Compassion Scale [SCS-D; (93, 94)] which assesses Self-Compassion via 26 items on a 5-point Likert scale (1 = almost never to 5 = almost always). Cronbach’s α was observed to be 0.89.
The Emotion Regulation Questionnaire [ERQ; (95)] tests Reappraisal and Suppression as emotion regulation strategies using 10 items on a 7-point Likert scale (1 = strongly disagree to 7 = strongly agree; Cronbach’s αreappraisal = 0.84; Cronbach’s αsuppression = 0.77).
The Brief-Symptom Inventory [BSI-18; (96)] measures the Global Severity Index (GSI) of psychological distress via 18 items on a 5-point Likert scale (0 = not at all to 4 = extremely). Cronbach’s α was 0.88.
Participants were tested in the last week of their stay at the clinic (post-test only experimental design; see Figure 1). They were requested not to consume caffeine, alcohol, nicotine, and sugary drinks, as well as to refrain from physical exertion 2 h before the testing (73, 97, 98). Initially, participants’ height, hip, and waist circumference were measured, and anamnestic data collected. During the recording, participants sat quietly in an upright position and were asked not to move (98). HRV and HR were measured continuously. BP was measured 6 times (baseline & recovery: min 2:30, 4:00; speech prep.: min 0:30, 2:00). For the 5-min baseline recording, landscape pictures were presented on a screen. After the 3-min speech preparation, the actual 3-min speech took place. The recovery phase followed, identical to baseline. After baseline, speech preparation, and recovery PANAS and SSP were presented. Appraisal was collected after speech preparation and recovery and Rumination after recovery. Finally, participants were debriefed. It was made clear that the video recordings were not evaluated at all and were deleted immediately, but only served to reinforce stress (99). One female judge (S.K.) was present during all stress induction, wearing a white coat. There was always the same judge (S.K.). One camera was mounted right beside the computer screen. SCS-D, ERQ, and BSI-18 were presented on the last day of the 6-week stay. The time of day when the stress induction took place could not be controlled, otherwise it would not have been possible to give all patients an appointment for testing.
HRV analyzes were conducted with the software packages AcqKnowledge 4.3 (100) and Kubios HRV Premium 3.3.1 (101). R-R time series (interbeat intervals) were interpolated with 4 Hz (101). Fast Fourier Transformation (FFT) was applied to quantify HF-HRV [0.15–0.4 Hz] and LF-HRV [0.04–0.15 Hz] with 180 s window and no overlap (73, 102). The smoothness priors algorithm was used for detrending (101). To control for artifacts, HRV data were visually inspected by the examiner and corrected with the automatic correction algorithm in Kubios software if necessary (101). For further analyzes, only data containing less than 5% of artifacts were considered. An exception was made for one subject due to the small violation of the limit during recovery (artifacts = 5.16%). One person had to be excluded due to excessive artifacts (baseline = 23.63%, speech prep. = 20.09%, recovery = 25.85%). In addition, one participant could not be included in HRV, and HR analyzes due to flawed recordings. RMSSD, HF, SDNN, LF, and HR means of the last 3 min of the 5 min recordings (baseline, recovery) as well as means of the 3 min recording (speech prep.) were analyzed which seemed a sufficient length for ultra-short term HRV measures (74). Due to the sensitivity to movement in HRV recordings, an a priori decision was made to incorporate speech preparation as a stress phase (73). Research shows, stress anticipation can also trigger adequate stress responses (103). Prior to analyses, RMSSD and SDNN data were subjected to a natural log transformation to account for skewness (73, 104).
Statistical analyzes were done with SPSS, version 27 by IBM. Group comparisons regarding anamnestic variables were conducted by means of chi-square and unpaired t-tests. For primary outcome, separate two-way mixed ANOVAs with the between-subject factor group (MSC, PMR) and the within-subject factor time (baseline, speech prep., recovery) regarding psychophysiological measures (HRV, HR, BP, PA, NA, SSP) were performed. For post-hoc analyzes, Bonferroni pairwise comparisons were implemented. Secondary outcome analyzes included unpaired t-tests with the independent variable group (MSC, PMR) regarding Self-Compassion, Emotion Regulation, Psychological Distress, Appraisal, and Rumination. The statistical significance was set to p < 0.05 (two-sided). Alpha-error-accumulation was controlled via Bonferroni correction.
Participants were on average overweight [BMI: M = 28.01, SD = 5.93; (105)]. All individuals had a psychiatric diagnosis and 33 (66%) of them at least one comorbid psychiatric diagnosis as reported by the International Classification of Diseases [ICD-10; (106), Chapter F), presented in Table 1. Primarily, people with affective disorders (F30-F39) participated in the study [44 (88%) people; (106)], followed by neurotic, stress-related, and somatoform disorders [F40-F49; (106)]. Thirty-eight (76%) participants took psychotropic drugs, all of them antidepressants, followed by additional neuroleptics intake (14 (36.8%) people). Of note, 24 (48%) participants reported doing sports on a regular basis. Sixteen (32%) people smoked regularly, and four (8%) participants drank alcohol habitually.
Group comparisons regarding anamnestic data (health-related variables, psychiatric diagnoses, medication) did not reveal significant differences (see Table 1).
Forty-eight participants were included in the HRV and HR-analyzes, 47 for Respiration and 44 for the BP analyzes. If there were no more than 10% missing data in a questionnaire, the mean of the remaining items was inserted for the missing item (107). This procedure was applied for three participants for PA, two for NA and three for SCS-D. For SSP, Appraisal, and Rumination 49 people were enclosed. Data of 44 participants were included in the analyses of SCS-D and BSI-18. For ERQ Reappraisal, 42 people and for ERQ Suppression, 43 people were included (see Tables 1, 2).
Published resting short-term HRV norms of approximately 5 min length collected in 21,438 non-clinical individuals in sitting or lupine position (74) were compared to the 3 min baseline measurement in this clinical sample for exploratory reasons. The present sample showed significantly lower RMSSD, HF-HRV, and SDNN during baseline measurement as compared to the non-clinical norms. For LF-HRV, no significant difference was found (see Table 3). According to Shaffer and Ginsberg (74) participants should breathe at 11–20 breaths per minute (BPM) that short-term HRV values are adequate. Respiration rate for baseline measurement was on average 15 BPM (M = 15.30, SD = 4.46), for speech preparation 17 BPM (M = 17.21, SD = 3.12), and for recovery 15 BPM (M = 15.41, SD = 4.86). Mixed ANOVA with Respiration rate showed no significant main difference between MSC and PMR group (see Table 2). Therefore, no further analyzes including Respiration deemed necessary.
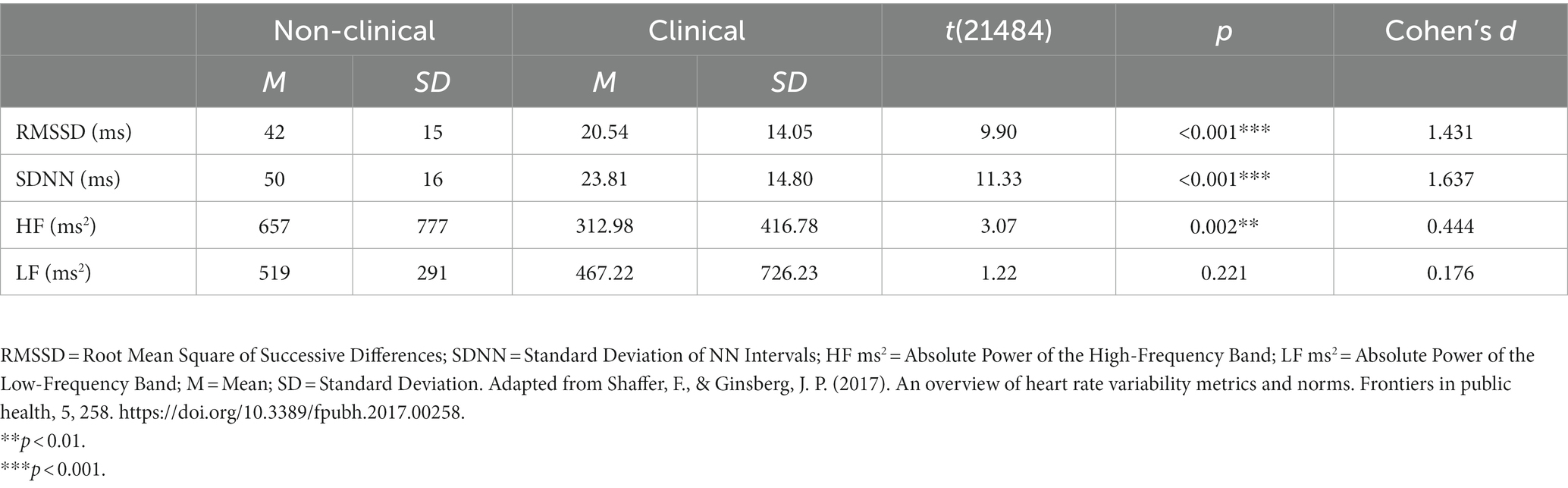
Table 3. Non-clinical short-term HRV norms (n = 21,438) in comparison to clinical sample (n = 48) (108).
For all Mixed ANOVA calculations, prerequisites have been checked. When the assumption of sphericity was not fulfilled, the Greenhouse–Geisser correction was applied (see Table 2a) (109). Normal distribution was assessed by Shapiro–Wilk test (p > 0.05), and if violated, ANOVAs were still calculated due to the central limit theorem (110). Box’s Test showed homogeneity of covariances for all calculations [p > 0.05; (111)]. Except for SSP in recovery phase, homogeneity of variances was given by Levene’s test (p > 0.05). Post-hoc comparisons were still interpreted for SSP (112).
For HRV, HR, and BP, calculations revealed significant main effects of time for SDNN (p = 0.42; ns after Bonferroni correction), LF (p = 0.019; ns after Bonferroni correction), HR, SYS BP, and DIA BP (all p < 0.001), respectively. There were no significant main effects group or interaction effects regarding HRV, HR and BP (see Table 2).
For SDNN, pairwise comparison showed no significant results between baseline and speech preparation (p = 0.106), and speech preparation and recovery (p = 0.130), respectively. LF-HRV was significantly lower during baseline (M = 5.13, SD = 1.55) than during speech preparation (M = 5.52, SD = 1.52, p = 0.023). No significant changes were found towards recovery (p = 0.151). For HR, pairwise comparisons indicated a significant increase from baseline (M = 76.26, SD = 12.59) to speech preparation (M = 80.06, SD = 11.92, p < 0.001) and decrease from speech preparation to recovery (M = 76.52, SD = 12.22, p < 0.001). Pairwise comparison for SYS BP revealed a significant rise from baseline (M = 117.00, SD = 14.07) to speech preparation (M = 124.83, SD = 14.13, p < 0.001). No significant decrease towards recovery was found (p = 0.059). DIA BP revealed a significant increase from baseline (M = 89.15, SD = 9.65) to speech preparation (M = 93.02, SD = 9.61, p < 0.001) and a decline from speech preparation to recovery (M = 89.93, SD = 10.31, p < 0.001).
As detailed in Table 2 the results of the stress intervention indicated expected reactions with significant main effects time on PA, NA and SSP. PA showed a significant rise from baseline (M = 2.55, SD = 0.68) to speech preparation (M = 2.86, SD = 0.87, p < 0.001) and significant decline to recovery phase (M = 2.52, SD = 0.88, p = 0.003).
For NA, there was no significant increase to speech preparation (M = 1.72, SD = 0.65, p = 0.085), but a significant decrease to recovery (M = 1.41, SD = 0.55, p < 0.001). SSP was significantly higher at speech preparation (M = 44.98, SD = 27.99) than at baseline (M = 24.04, SD = 22.29, p < 0.001) and lower at recovery (M = 26.71, SD = 24.55, p < 0.001) than at speech preparation. No significant main effects group nor interaction effects were found (see Table 2).
For unpaired t-tests, normal distribution was given, as assessed by Shapiro–Wilk test (p > 0.05) except for PMR group regarding Psychological Distress and Rumination (110). Homoscedasticity was evident in all calculations (Levene’s test: p > 0.05). For Self-Compassion, Suppression, Psychological Distress, Appraisal, and Rumination, no group differences were detected. The MSC group showed significantly higher values in Reappraisal than the PMR group (see Table 1), indicating a medium effect size (Cohen’s d = 0.64; ns after Bonferroni correction). However, this result was non-significant after Bonferroni correction.
The main purpose of this study was to determine whether the psychophysiological stress response differed in inpatients attending the MSC or PMR program at the end of their 6-week psychiatric rehabilitation stay in the Sonnenpark Neusiedlersee clinic. Overall, no difference was found. Participants were comparable on several anamnestic variables such as diagnoses or medication intake, Self-Compassion, Suppression, and Psychological Distress, as well as in HRV, HR, BP, PA, NA, SSP, Respiration rate, Appraisal, and Rumination in the course of the stress induction. While participants in the MSC group exhibited increased Cognitive Reappraisal as an emotion regulation strategy, as compared to the PMR group, this difference did not remain significant after controlling for multiple testing.
On a psychophysiological level, substantial stress-related changes were observed in both groups, thus demonstrating effectiveness of the stress task. In particular, alterations in SDNN, LF-HRV, HR, BP, PA, NA, and SSP throughout the three measurement points (baseline, speech prep., recovery) of the stress task could be observed. However, no significant changes were detected for RMSSD and HF-HRV.
This study is, to the authors’ knowledge, the first to compare MSC training with an active PMR control group regarding psychophysiological stress reactivity. Initial indications for group differences were provided by the study of Gaiswinkler et al. (51), where MSC training was associated with higher self-compassion and happiness than PMR training after a 6-week intervention in the Sonnenpark Neusiedlersee clinic. In this study, a tendency for higher Self-Compassion in the MSC group (p = 0.095) was found, as well as a superior Cognitive Reappraisal (p = 0.045), which confirms recent findings on how self-compassion increases the ability of cognitive reappraisal as self-compassion helps us to look at ourselves and situations we are in with more kindness (47, 113, 114). Higher reappraisal could also help to better deal with stressful situations as they are perceived as evolving (115, 116). Besides, the MSC and the PMR training seem to produce quite similar results like several other studies comparing mindfulness and PMR (66, 68, 117, 118). Although - resonating with previous research - our findings hint towards effects of MBIs on psychological stress response regarding SSP (119), Emotion Suppression (120), Psychological Distress (117), Appraisal (85, 121), and Rumination (49, 122), this study did not employ a placebo group which significantly restricts the generalizability of our findings.
In psychophysiological research, heterogeneous findings exist where differences between mindfulness and relaxation interventions were found (53, 119, 123). Especially for brief self-compassion and meditation interventions on physiological stress reactivity, adaptive psychophysiological reactions could not be confirmed (32, 124). These results may be due to short-term interventions that have predominantly been conducted in healthy or subclinical populations (53, 119). In contrast, in this study, a 6-week-long intervention was performed in a clinical population. Generally speaking, there are studies showing mindfulness and self-compassion training increasing HRV and buffering psychophysiological stress response (33, 55, 57, 58, 125, 126). Similar to self-compassion programs, PMR may buffer psychophysiological stress reactivity (67, 127). These studies suggest that both programs might be equivalent. To further test this hypothesis future studies should apply equivalence testing on the effects of both relaxation techniques.
A moderate stress response was evident in individual psychophysiological parameter. The stress response of HR, BP, NA, and SSP was observed congruent with literature since both groups showed a rise from baseline to speech preparation and a decline towards recovery (82, 119, 125, 128, 129). Additionally, a significant increase to speech preparation was observed in PA, which seems surprising at first glance (130, 131). Nevertheless, no parasympathetic change regarding RMSSD and HF-HRV was observed, possibly indicating no adaptive stress behavior (20, 132). This is rather uncommon in stress experiments, but could be due to the clinical population and their low flexibility of the ANS (18, 19, 133, 134).
While we did not find significant differences between MSC and PMR, future investigations might examine characteristics of specific groups for whom MSC works particularly well or people who do not benefit from it. E.g. previous research identified neuroticism and conscientiousness as possible moderators of mindfulness based interventions (135). Regarding the moderate stress response, the stress induction might be applicable for future stress experiments. Especially in clinical populations, it may be advantageous not to obtain a strong but moderate stress response due to vulnerability.
The first point to be mentioned is the sample size in this study. This only allows for large effects to be revealed by statistical evaluation (136, 137). To detect medium and small effects, a larger sample size is certainly required. Additionally, a within subject design study would be desirable (73). Quintana and Heathers (131) recommend collecting multiple data from one individual at several times in psychophysiological studies. Due to the selected stressor, we were not able to apply the speaking task twice, otherwise a learning effect and therefore an inadequate stress response might have been detected (73). For future studies, however, we should consider presenting a different stress task at the beginning of the 6-week stay as well as at the end to reveal the changes within a person pre- and post-treatment (73). Recently, Asbrand et al. (138) showed that the standardized TSST could be used in repeated measures, which might constitute an additional approach for future replication studies.
Besides, a non-clinical control group additionally to the active PMR control group would be essential to compare clinical and non-clinical subjects (139). In this study, an attempt was made to compare HRV norm values in non-clinical studies with the present sample, which indicated lower HRV values in comparison to norms. However, to our knowledge, no norm values exist for stress reactivity (74). Still, studies show blunted HRV reactivity in a stress experiment in patients with mental illness as compared to healthy individuals, which is in line with the Neurovisceral Integration Model and makes comparative values preferable in future studies (18, 19, 21, 79, 140). Considering that affective disorders are most frequent in the rehabilitation clinic, this is of particular interest since Jandackova et al. (141) consider HRV as an influencing factor on the onset of depression.
In the present study, the two instructors, teaching MSC and PMR, were not supervised. Thus, it would be interesting to address the training of the instructors as well as their mindset. Showing compassion for others requires us to be aware of our own pain and may help clinicians be more effective in therapy (142).
In sum, this study was the first one to compare MSC and PMR program with respect to psychophysiological stress reactivity with clinical context. The results of this experiment showed no significant difference in the psychophysiological stress responses of inpatients at the end of their psychiatric rehabilitation stay, thus suggesting no difference in the response profile of both the MSC and PMR program.
Yet, larger studies will be needed to further explore differences and similarities of both interventions in more detail.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by Ethics Committee of the University of Graz. The patients/participants provided their written informed consent to participate in this study.
SK, AA, PK, EP, AS, and H-FU conceptualized the study. SK, CS, and AA collected the data. SK and CT analyzed the data. SK interpreted the data. SK, JF, AA, AS, and H-FU drafted the manuscript. AS, CT, CR, JF, AA, and H-FU critically reviewed it. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Esch, T, Stefano, GB, Fricchione, GL, and Benson, H. The role of stress in neurodegenerative diseases and mental disorders. Neuroendocrinol Lett. (2002) 23:199–208.
2. Zaman, R, Hankir, A, and Jemni, M. Lifestyle factors and mental health. Psychiatr Danub. (2019) 31:217–20.
3. Selye, H. Thymus and adrenals in response of the organism to injuries and intoxication. Br J Exp Pathol. (1936) 17:234–48.
4. Rohleder, N. Stress and inflammation – the need to address the gap in the transition between acute and chronic stress effects. Psychoneuroendocrinology. (2019) 105:164–71. doi: 10.1016/j.psyneuen.2019.02.021
5. Gibbons, CH. Basics of autonomic nervous system function. Handb Clin Neurol. (2019) 160:407–18. doi: 10.1016/B978-0-444-64032-1.00027-8
6. Porges, SW, Doussard-Roosevelt, JA, and Maiti, AK. Vagal tone and the physiological regulation of emotion. Monogr Soc Res Child Dev. (1994) 59:167–86. doi: 10.1111/j.1540-5834.1994.tb01283.x
7. Sapolsky, RM, Romero, LM, and Munck, AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr Rev. (2000) 21:55–89. doi: 10.1210/edrv.21.1.0389
8. Grossman, P, Wilhelm, FH, and Spoerle, M. Respiratory sinus arrhythmia, cardiac vagal control, and daily activity. Am J Phys Heart Circ Phys. (2004b) 287:H728–34. doi: 10.1152/ajpheart.00825.2003
9. Shi, B, Zhang, Y, Yuan, C, Wang, S, and Li, P. Entropy analysis of short-term heartbeat interval time series during regular walking. Entropy. (2017) 19:568. doi: 10.3390/e19100568
10. Thayer, JF, Åhs, F, Fredrikson, M, Sollers, JJ, and Wager, TD. A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health. Neurosci Biobehav Rev. (2012) 36:747–56. doi: 10.1016/j.neubiorev.2011.11.009
11. Schwerdtfeger, AR, Schwarz, G, Pfurtscheller, K, Thayer, JF, Jarczok, MN, and Pfurtscheller, G. Heart rate variability (HRV): from brain death to resonance breathing at 6 breaths per minute. Clin Neurophysiol. (2020) 131:676–93. doi: 10.1016/j.clinph.2019.11.013
12. Porges, SW. The polyvagal perspective. Biol Psychol. (2007) 74:116–43. doi: 10.1016/j.biopsycho.2006.06.009
13. Diamond, LM, and Hicks, AM. Attachment style, current relationship security, and negative emotions: the mediating role of physiological regulation. J Soc Pers Relat. (2005) 22:499–518. doi: 10.1177/0265407505054520
14. Heiss, S, Vaschillo, B, Vaschillo, EG, Timko, CA, and Hormes, JM. Heart rate variability as a biobehavioral marker of diverse psychopathologies: a review and argument for an “ideal range.”. Neurosci Biobehav Rev. (2021) 121:144–55. doi: 10.1016/j.neubiorev.2020.12.004
15. Kok, BE, Coffey, KA, Cohn, MA, Catalino, LI, Vacharkulksemsuk, T, Algoe, SB, et al. How positive emotions build physical health: perceived positive social connections account for the upward spiral between positive emotions and vagal tone. Psychol Sci. (2013) 24:1123–32. doi: 10.1177/0956797612470827
16. Cattaneo, LA, Franquillo, AC, Grecucci, A, Beccia, L, Caretti, V, and Dadomo, H. Is low heart rate variability associated with emotional dysregulation, psychopathological dimensions, and prefrontal dysfunctions? An integrative view. J Person Med. (2021) 11:872. doi: 10.3390/jpm11090872
17. Thayer, JF, and Lane, RD. The role of vagal function in the risk for cardiovascular disease and mortality. Biol Psychol. (2007) 74:224–42. doi: 10.1016/j.biopsycho.2005.11.013
18. Schiweck, C, Piette, D, Berckmans, D, Claes, S, and Vrieze, E. Heart rate and high frequency heart rate variability during stress as biomarker for clinical depression. A systematic review. Psychol Med. (2019) 49:200–11. doi: 10.1017/S0033291718001988
19. Schneider, M, and Schwerdtfeger, A. Autonomic dysfunction in posttraumatic stress disorder indexed by heart rate variability: a meta-analysis. Psychol Med. (2020) 50:1937–48. doi: 10.1017/S003329172000207X
20. Schwerdtfeger, A, and Rosenkaimer, A-K. Depressive symptoms and attenuated physiological reactivity to laboratory stressors. Biol Psychol. (2011) 87:430–8. doi: 10.1016/j.biopsycho.2011.05.009
21. Thayer, JF, and Lane, RD. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord. (2000) 61:201–16. doi: 10.1016/S0165-0327(00)00338-4
22. Smith, R, Thayer, JF, Khalsa, SS, and Lane, RD. The hierarchical basis of neurovisceral integration. Neurosci Biobehav Rev. (2017) 75:274–96. doi: 10.1016/j.neubiorev.2017.02.003
23. Thayer, JF, and Friedman, BF. A neurovisceral integration model of health disparities in aging In: NB Anderson, RA Bulatao, and B Cohen, editors. Critical perspectives on racial and ethnic differences in health in late life. Washington (DC): National Academies Press (2004).
24. Lederbogen, F, and Ströhle, A. Stress, psychische Erkrankungen und koronare Herzkrankheit. Nervenarzt. (2012) 83:1448–57. doi: 10.1007/s00115-012-3666-7
25. Rosenkranz, MA, Dunne, JD, and Davidson, RJ. The next generation of mindfulness-based intervention research: what have we learned and where are we headed? Curr Opin Psychol. (2019) 28:179–83. doi: 10.1016/j.copsyc.2018.12.022
26. De, VM, Solhaug, I, Rosenvinge, JH, Tyssen, R, Hanley, A, and Garland, E. Six-year positive effects of a mindfulness-based intervention on mindfulness, coping and well-being in medical and psychology students; results from a randomized controlled trial. PLoS One. (2018) 13:e0196053. doi: 10.1371/journal.pone.0196053
27. Kabat-Zinn, J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract. (2003) 10:144–56. doi: 10.1093/clipsy.bpg016
28. Chiesa, A, and Serretti, A. Mindfulness based cognitive therapy for psychiatric disorders: a systematic review and meta-analysis. Psychiatry Res. (2011) 187:441–53. doi: 10.1016/j.psychres.2010.08.011
29. Oberoi, S, Yang, J, Woodgate, RL, Niraula, S, Banerji, S, Israels, SJ, et al. Association of mindfulness-based interventions with anxiety severity in adults with cancer: a systematic review and meta-analysis. JAMA Netw Open. (2020) 3:e2012598. doi: 10.1001/jamanetworkopen.2020.12598
30. Zhang, D, Lee, EKP, Mak, ECW, Ho, CY, and Wong, SYS. Mindfulness-based interventions: an overall review. Br Med Bull. (2021) 138:41–57. doi: 10.1093/bmb/ldab005
31. Chiesa, A, and Serretti, A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. J Altern Complement Med. (2009) 15:593–600. doi: 10.1089/acm.2008.0495
32. Dawson, AF, Brown, WW, Anderson, J, Datta, B, Donald, JN, Hong, K, et al. Mindfulness-based interventions for university students: a systematic review and meta-analysis of randomised controlled trials. Appl Psychol Health Well Being. (2020) 12:384–410. doi: 10.1111/aphw.12188
33. Zhang, Y, Xue, J, and Huang, Y. A meta-analysis: internet mindfulness-based interventions for stress management in the general population. Medicine (Baltimore). (2020) 99:e20493. doi: 10.1097/MD.0000000000020493
34. Gaiswinkler, L, and Unterrainer, HF. The relationship between yoga involvement, mindfulness and psychological well-being. Complement Ther Med. (2016) 26:123–7. doi: 10.1016/j.ctim.2016.03.011
35. Grossman, P, Niemann, L, Schmidt, S, and Walach, H. Mindfulness-based stress reduction and health benefits: a meta-analysis. J Psychosom Res. (2004a) 57:35–43. doi: 10.1016/S0022-3999(03)00573-7
36. Proeve, M, Anton, R, and Kenny, M. Effects of mindfulness-based cognitive therapy on shame, self-compassion and psychological distress in anxious and depressed patients: a pilot study. Psychol Psychother Theory Res Pract. (2018) 91:434–49. doi: 10.1111/papt.12170
37. Wasson, RS, Barratt, C, and O’Brien, WH. Effects of mindfulness-based interventions on self-compassion in health care professionals: a meta-analysis. Mindfulness. (2020) 11:1914–34. doi: 10.1007/s12671-020-01342-5
38. Neff, KD, and Germer, CK. A pilot study and randomized controlled trial of the Mindful Self-Compassion program. J Clin Psychol. (2013) 69:28–44. doi: 10.1002/jclp.21923
39. Neff, KD. Self-compassion: an alternative conceptualization of a healthy attitude toward oneself. Self Identity. (2003) 2:85–101. doi: 10.1080/15298860309032
40. Germer, CK, and Neff, KD. Self-compassion in clinical practice. J Clin Psychol. (2013) 69:856–67. doi: 10.1002/jclp.22021
41. Barnard, LK, and Curry, JF. Self-compassion: conceptualizations, correlates, & interventions. Rev Gen Psychol. (2011) 15:289–303. doi: 10.1037/a0025754
42. Deniz, ME. Self-compassion, intolerance of uncertainty, fear of COVID-19, and well-being: a serial mediation investigation. Personal Individ Differ. (2021) 177:110824. doi: 10.1016/j.paid.2021.110824
43. Ewert, C, Vater, A, and Schröder-Abé, M. Self-compassion and coping: a meta-analysis. Mindfulness. (2021) 12:1063–77. doi: 10.1007/s12671-020-01563-8
44. Ferrari, M, Hunt, C, Harrysunker, A, Abbott, MJ, Beath, AP, and Einstein, DA. Self-compassion interventions and psychosocial outcomes: a meta-analysis of RCTs. Mindfulness. (2019) 10:1455–73. doi: 10.1007/s12671-019-01134-6
45. Leary, MR, Tate, EB, Adams, CE, Batts Allen, A, and Hancock, J. Self-compassion and reactions to unpleasant self-relevant events: the implications of treating oneself kindly. J Pers Soc Psychol. (2007) 92:887–904. doi: 10.1037/0022-3514.92.5.887
46. Neff, KD, Hsieh, Y-P, and Dejitterat, K. Self-compassion, achievement goals, and coping with academic failure. Self Identity. (2005) 4:263–87. doi: 10.1080/13576500444000317
47. Diedrich, A, Hofmann, SG, Cuijpers, P, and Berking, M. Self-compassion enhances the efficacy of explicit cognitive reappraisal as an emotion regulation strategy in individuals with major depressive disorder. Behav Res Ther. (2016) 82:1–10. doi: 10.1016/j.brat.2016.04.003
48. Förster, K, and Kanske, P. Exploiting the plasticity of compassion to improve psychotherapy. Curr Opin Behav Sci. (2021) 39:64–71. doi: 10.1016/j.cobeha.2021.01.010
49. Frostadottir, AD, and Dorjee, D. Effects of mindfulness based cognitive therapy (MBCT) and compassion focused therapy (CFT) on symptom change, mindfulness, self-compassion, and rumination in clients with depression, anxiety, and stress. Front Psychol. (2019) 10:1099. doi: 10.3389/fpsyg.2019.01099
50. Aranda Auserón, G, Elcuaz Viscarret, MR, Fuertes Goñi, C, Güeto Rubio, V, Pascual Pascual, P, de Murieta, S, et al. Evaluation of the effectiveness of a mindfulness and self-compassion program to reduce stress and prevent burnout in primary care health professionals. Aten Primaria. (2018) 50:141–50. doi: 10.1016/j.aprim.2017.03.009
51. Gaiswinkler, L, Kaufmann, P, Pollheimer, E, Ackermann, A, Holasek, S, Kapfhammer, H-P, et al. Mindfulness and self-compassion in clinical psychiatric rehabilitation: a clinical trial. Mindfulness. (2020) 11:374–83. doi: 10.1007/s12671-019-01171-1
52. Neff, KD, and Pommier, E. The relationship between self-compassion and other-focused concern among college undergraduates, community adults, and practicing meditators. Self Identity. (2013) 12:160–76. doi: 10.1080/15298868.2011.649546
53. Pascoe, MC, Thompson, DR, Jenkins, ZM, and Ski, CF. Mindfulness mediates the physiological markers of stress: systematic review and meta-analysis. J Psychiatr Res. (2017) 95:156–78. doi: 10.1016/j.jpsychires.2017.08.004
54. Tung, Y-H, and Hsieh, J-C. The impacts of mindfulness on heart rate variability: a brief review. IJPMBS. (2019) 8:132–7. doi: 10.18178/ijpmbs.8.4.132-137
55. Azam, MA, Katz, J, Fashler, SR, Changoor, T, Azargive, S, and Ritvo, P. Heart rate variability is enhanced in controls but not maladaptive perfectionists during brief mindfulness meditation following stress-induction: a stratified-randomized trial. Int J Psychophysiol. (2015) 98:27–34. doi: 10.1016/j.ijpsycho.2015.06.005
56. Ng, CG, Lai, KT, Tan, SB, Sulaiman, AH, and Zainal, NZ. The effect of 5 minutes of mindful breathing to the perception of distress and physiological responses in palliative care cancer patients: a randomized controlled study. J Palliat Med. (2016) 19:917–24. doi: 10.1089/jpm.2016.0046
57. Noh, S, and Cho, H. Psychological and physiological effects of the mindful lovingkindness compassion program on highly self-critical university students in South Korea. Front Psychol. (2020) 11:585743. doi: 10.3389/fpsyg.2020.585743
58. Arch, JJ, Brown, KW, Dean, DJ, Landy, LN, Brown, KD, and Laudenslager, ML. Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology. (2014) 42:49–58. doi: 10.1016/j.psyneuen.2013.12.018
59. Lindsay, EK, Young, S, Smyth, JM, Brown, KW, and Creswell, JD. Acceptance lowers stress reactivity: dismantling mindfulness training in a randomized controlled trial. Psychoneuroendocrinology. (2018) 87:63–73. doi: 10.1016/j.psyneuen.2017.09.015
60. Nyklíček, I, Mommersteeg, P, van Beugen, S, Ramakers, C, and Van Boxtel, G. Mindfulness-based stress reduction and physiological activity during acute stress: a randomized controlled trial. Health Psychol. (2013) 32:1110–3. doi: 10.1037/a0032200
61. Steffen, P, and Larson, M. A brief mindfulness exercise reduces cardiovascular reactivity during a laboratory stressor paradigm. Mindfulness. (2014) 6:803–11. doi: 10.1007/s12671-014-0320-4
62. Ceccarelli, LA, Giuliano, RJ, Glazebrook, CM, and Strachan, SM. Self-compassion and psycho-physiological recovery from recalled sport failure. Front Psychol. (2019) 10:1564. doi: 10.3389/fpsyg.2019.01564
63. Engert, V, Kok, BE, Papassotiriou, I, Chrousos, GP, and Singer, T. Specific reduction in cortisol stress reactivity after social but not attention-based mental training. Sci Adv. (2017) 3:e1700495. doi: 10.1126/sciadv.1700495
64. Heckenberg, RA, Eddy, P, Kent, S, and Wright, BJ. Do workplace-based mindfulness meditation programs improve physiological indices of stress? A systematic review and meta-analysis. J Psychosom Res. (2018) 114:62–71. doi: 10.1016/j.jpsychores.2018.09.010
66. Gao, L, Curtiss, J, Liu, X, and Hofmann, SG. Differential treatment mechanisms in mindfulness meditation and progressive muscle relaxation. Mindfulness. (2018) 9:1268–79. doi: 10.1007/s12671-017-0869-9
67. Toussaint, L, Nguyen, QA, Roettger, C, Dixon, K, Offenbächer, M, Kohls, N, et al. Effectiveness of progressive muscle relaxation, deep breathing, and guided imagery in promoting psychological and physiological states of relaxation. Evid Based Complement Alternat Med. (2021) 2021:e5924040. doi: 10.1155/2021/5924040
68. Mander, J, Blanck, P, Neubauer, AB, Kröger, P, Flückiger, C, Lutz, W, et al. Mindfulness and progressive muscle relaxation as standardized session-introduction in individual therapy: a randomized controlled trial. J Clin Psychol. (2019) 75:21–45. doi: 10.1002/jclp.22695
69. Morledge, TJ, Allexandre, D, Fox, E, Fu, AZ, Higashi, MK, Kruzikas, DT, et al. Feasibility of an online mindfulness program for stress management – a randomized, controlled trial. Ann Behav Med. (2013) 46:137–48. doi: 10.1007/s12160-013-9490-x
70. Becker Meditec (n.d.). VarioPort. Available at: https://bisigma.de/pdf/varioport-b_english.pdf [Accessed September 1, 2022].
71. Trappe, H-J. Das Elektrokardiogramm 100 Jahre nach Einthoven: Tipps und Tricks zur richtigen Diagnose. Notfall Rettungsmed. (2009) 12:635–48. doi: 10.1007/s10049-009-1247-5
72. Xhyheri, B, Manfrini, O, Mazzolini, M, Pizzi, C, and Bugiardini, R. Heart rate variability today. Prog Cardiovasc Dis. (2012) 55:321–31. doi: 10.1016/j.pcad.2012.09.001
73. Laborde, S, Mosley, E, and Thayer, JF. Heart rate variability and cardiac vagal tone in psychophysiological research – recommendations for experiment planning, data analysis, and data reporting. Front Psychol. (2017) 8:213. doi: 10.3389/fpsyg.2017.00213
74. Shaffer, F, and Ginsberg, JP. An overview of heart rate variability metrics and norms. Front Public Health. (2017) 5:258. doi: 10.3389/fpubh.2017.00258
75. Grossman, P, and Taylor, EW. Toward understanding respiratory sinus arrhythmia: relations to cardiac vagal tone, evolution and biobehavioral functions. Biol Psychol. (2007) 74:263–85. doi: 10.1016/j.biopsycho.2005.11.014
76. Shaffer, F, McCraty, R, and Zerr, CL. A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability. Front Psychol. (2014) 5:1040. doi: 10.3389/fpsyg.2014.01040
77. Sohn, Bosch (2000). Boso Medicus family. Available at: https://www.boso.de/produkte-fuer-heimanwender/blutdruckmessung/boso-medicus-family [Accessed September 1, 2022].
78. Broglio, K. Randomization in clinical trials: permuted blocks and stratification. JAMA. (2018) 319:2223–4. doi: 10.1001/jama.2018.6360
79. Kircanski, K, Waugh, CE, Camacho, MC, and Gotlib, IH. Aberrant parasympathetic stress responsivity in pure and co-occurring major depressive disorder and generalized anxiety disorder. J Psychopathol Behav Assess. (2016) 38:5–19. doi: 10.1007/s10862-015-9493-y
80. Kirschbaum, C, Pirke, K-M, and Hellhammer, DH. The ‘Trier social stress test’ – a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. (1993) 28:76–81. doi: 10.1159/000119004
81. Kudielka, BM, Buske-Kirschbaum, A, Hellhammer, DH, and Kirschbaum, C. Differential heart rate reactivity and recovery after psychosocial stress (TSST) in healthy children, younger adults, and elderly adults: the impact of age and gender. Int J Behav Med. (2004) 11:116–21. doi: 10.1207/s15327558ijbm1102_8
82. Petrowski, K, Wichmann, S, Siepmann, T, Wintermann, G-B, Bornstein, SR, and Siepmann, M. Effects of mental stress induction on heart rate variability in patients with panic disorder. Appl Psychophysiol Biofeedback. (2017) 42:85–94. doi: 10.1007/s10484-016-9346-9
83. Shahrestani, S, Stewart, EM, Quintana, DS, Hickie, IB, and Guastella, AJ. Heart rate variability during adolescent and adult social interactions: a meta-analysis. Biol Psychol. (2015) 105:43–50. doi: 10.1016/j.biopsycho.2014.12.012
84. Skoluda, N, Strahler, J, Schlotz, W, Niederberger, L, Marques, S, Fischer, S, et al. Intra-individual psychological and physiological responses to acute laboratory stressors of different intensity. Psychoneuroendocrinology. (2015) 51:227–36. doi: 10.1016/j.psyneuen.2014.10.002
85. Trotman, GP, Williams, SE, Quinton, ML, and Veldhuijzen van Zanten, JJCS. Challenge and threat states: examining cardiovascular, cognitive and affective responses to two distinct laboratory stress tasks. Int J Psychophysiol. (2018) 126:42–51. doi: 10.1016/j.ijpsycho.2018.02.004
86. Breyer, B, and Bluemke, M. Deutsche version der positive and negative affect schedule PANAS (GESIS panel). ZIS. (2016) 1–20. doi: 10.6102/ZIS242
87. Chen, IY, Jarrin, DC, Ivers, H, and Morin, CM. Investigating psychological and physiological responses to the Trier social stress test in young adults with insomnia. Sleep Med. (2017) 40:11–22. doi: 10.1016/j.sleep.2017.09.011
88. O’Brien, J, Fryer, S, Parker, J, and Moore, L. The effect of ego depletion on challenge and threat evaluations during a potentially stressful public speaking task. Anxiety Stress Coping. (2020) 34:266–78. doi: 10.1080/10615806.2020.1839732
89. Tomaka, J, Blascovich, J, Kelsey, RM, and Leitten, CL. Subjective, physiological, and behavioral effects of threat and challenge appraisal. J Pers Soc Psychol. (1993) 65:248–60. doi: 10.1037/0022-3514.65.2.248
90. Brinker, JK, and Dozois, DJA. Ruminative thought style and depressed mood. J Clin Psychol. (2009) 65:1–19. doi: 10.1002/jclp.20542
91. Edwards, SL, Rapee, RM, and Franklin, J. Postevent rumination and recall bias for a social performance event in high and low socially anxious individuals. Cogn Ther Res. (2003) 27:603–17. doi: 10.1023/A:1026395526858
92. Pjanic, I, Bachmann, M, Znoj, H, and Messerli-Bürgy, N. Entwicklung eines Screening-Instruments zu Rumination und Suppression RS-8. Psychother Psychosom Med Psychol. (2013) 63:456–62. doi: 10.1055/s-0032-1333302
93. Hupfeld, J, and Ruffieux, N. Validierung einer deutschen Version der Self-Compassion Scale (SCS-D). Z Klin Psychol Psychother. (2011) 40:115–23. doi: 10.1026/1616-3443/a000088
94. Neff, KD. The development and validation of a scale to measure self-compassion. Self Identity. (2003) 2:223–50. doi: 10.1080/15298860309027
95. Abler, B, and Kessler, H. Emotion Regulation Questionnaire – Eine deutschsprachige Fassung des ERQ von Gross und John. Diagnostica. (2009) 55:144–52. doi: 10.1026/0012-1924.55.3.144
96. Spitzer, C, Hammer, S, Löwe, B, Grabe, HJ, Barnow, S, Rose, M, et al. Die Kurzform des Brief Symptom Inventory (BSI -18): erste Befunde zu den psychometrischen Kennwerten der deutschen Version. Fortschr Neurol Psychiatr. (2011) 79:517–23. doi: 10.1055/s-0031-1281602
97. Kingsley, JD, and Figueroa, A. Acute and training effects of resistance exercise on heart rate variability. Clin Physiol Funct Imaging. (2016) 36:179–87. doi: 10.1111/cpf.12223
98. Quintana, DS, Alvares, GA, and Heathers, JAJ. Guidelines for reporting articles on psychiatry and heart rate variability (GRAPH): recommendations to advance research communication. Transl Psychiatry. (2016) 6:e803–3. doi: 10.1038/tp.2016.73
99. Labuschagne, I, Grace, C, Rendell, P, Terrett, G, and Heinrichs, M. An introductory guide to conducting the Trier social stress test. Neurosci Biobehav Rev. (2019) 107:686–95. doi: 10.1016/j.neubiorev.2019.09.032
100. Biopac-Systems (2013). AcqKnowledge. Available at: https://acqknowledge.software.informer.com/4.3/ [Accessed September 1, 2022].
101. Kubios (2019). Kubios HRV Premium. Available at: https://www.kubios.com/kubios-hrv-version-3-3-1-released/ [Accessed September 1, 2022].
102. Camm, AJ, Malik, M, Bigger, JT, Breithardt, G, Cerutti, S, Cohen, RJ, et al. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Task force of the European Society of Cardiology and the north American Society of Pacing and Electrophysiology. Circulation. (1996) 93:1043–65. doi: 10.1161/01.CIR.93.5.1043
103. Pulopulos, MM, Vanderhasselt, M-A, and De Raedt, R. Association between changes in heart rate variability during the anticipation of a stressful situation and the stress-induced cortisol response. Psychoneuroendocrinology. (2018) 94:63–71. doi: 10.1016/j.psyneuen.2018.05.004
104. Stanley, J, Peake, JM, and Buchheit, M. Consecutive days of cold water immersion: effects on cycling performance and heart rate variability. Eur J Appl Physiol. (2013) 113:371–84. doi: 10.1007/s00421-012-2445-2
105. World Health Organization (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight [Accessed July 28, 2022].
106. World Health Organization (1992). The ICD-10 classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. World Health Organization 362 p. Available at: https://apps.who.int/iris/handle/10665/37958 [Accessed July 27, 2022].
107. Donders, ART, van der Heijden, GJMG, Stijnen, T, and Moons, KGM. Review: a gentle introduction to imputation of missing values. J Clin Epidemiol. (2006) 59:1087–91. doi: 10.1016/j.jclinepi.2006.01.014
108. Nunan, D, Sandercock, GRH, and Brodie, DA. A quantitative systematic review of normal values for short-term heart rate variability in healthy adults. Pacing Clin Electrophysiol. (2010) 33:1407–17. doi: 10.1111/j.1540-8159.2010.02841.x
109. Greenhouse, SW, and Geisser, S. On methods in the analysis of profile data. Psychometrika. (1959) 24:95–112. doi: 10.1007/BF02289823
110. Shapiro, SS, and Wilk, MB. An analysis of variance test for normality (complete samples). Biometrika. (1965) 52:591–611. doi: 10.2307/2333709
111. Box, GEP. A general distribution theory for a class of likelihood criteria. Biometrika. (1949) 36:317–46. doi: 10.2307/2332671
112. Hsu, J. Multiple comparisons: Theory and methods. Boca Raton, Florida, USA: CRC Press (1996). 306 p.
113. Edwards, D, and Pinna, T. A systematic review of associations between interoception, vagal tone, and emotional regulation: potential applications for mental health, wellbeing, psychological flexibility, and chronic conditions. Front Psychol. (2020) 11:1792. doi: 10.3389/fpsyg.2020.01792
114. Keng, S-L, Smoski, MJ, and Robins, CJ. Effects of mindfulness on psychological health: a review of empirical studies. Clin Psychol Rev. (2011) 31:1041–56. doi: 10.1016/j.cpr.2011.04.006
115. Hanley, AW, and Garland, EL. Dispositional mindfulness co-varies with self-reported positive reappraisal. Personal Individ Differ. (2014) 66:146–52. doi: 10.1016/j.paid.2014.03.014
116. Jamieson, JP, Mendes, WB, and Nock, MK. Improving acute stress responses: the power of reappraisal. Curr Dir Psychol Sci. (2013) 22:51–6. doi: 10.1177/0963721412461500
117. Gok Metin, Z, Karadas, C, Izgu, N, Ozdemir, L, and Demirci, U. Effects of progressive muscle relaxation and mindfulness meditation on fatigue, coping styles, and quality of life in early breast cancer patients: an assessor blinded, three-arm, randomized controlled trial. Europ J Oncol Nurs. (2019) 42:116–25. doi: 10.1016/j.ejon.2019.09.003
118. Izgu, N, Gok Metin, Z, Karadas, C, Ozdemir, L, Metinarikan, N, and Corapcıoglu, D. Progressive muscle relaxation and mindfulness meditation on neuropathic pain, fatigue, and quality of life in patients with type 2 diabetes: a randomized clinical trial. J Nurs Scholarsh. (2020) 52:476–87. doi: 10.1111/jnu.12580
119. Morton, ML, Helminen, EC, and Felver, JC. A systematic review of mindfulness interventions on psychophysiological responses to acute stress. Mindfulness. (2020) 11:2039–54. doi: 10.1007/s12671-020-01386-7
120. Brockman, R, Ciarrochi, J, Parker, P, and Kashdan, T. Emotion regulation strategies in daily life: mindfulness, cognitive reappraisal and emotion suppression. Cogn Behav Ther. (2017) 46:91–113. doi: 10.1080/16506073.2016.1218926
121. Ma, J, Liu, C, Bao, H, and Gu, X. How to ward off the threat of workplace ostracism? The merit of self-compassion. Personal Individ Differ. (2022) 187:111396. doi: 10.1016/j.paid.2021.111396
122. Knowles, LM, Jovel, KS, Mayer, CM, Bottrill, KC, Kaszniak, AW, Sbarra, DA, et al. A controlled trial of two mind–body interventions for grief in widows and widowers. J Consult Clin Psychol. (2021) 89:640–54. doi: 10.1037/ccp0000653
123. Solarikova, P, and Bartolen, I. Higher HRV and lower anxiety in buddhist concentrative and zen-seated meditation in response to acute stress. Act Nerv Super Rediviva. (2020) 62:11.
124. Volkaert, B, Verbeken, S, Debeuf, T, Michels, N, and Braet, C. Training self-compassion: exploring the effects on adolescents’ physiological and self-reported stress responses. Mindfulness. (2022) 13:897–907. doi: 10.1007/s12671-022-01838-2
125. Luo, X, Qiao, L, and Che, X. Self-compassion modulates heart rate variability and negative affect to experimentally induced stress. Mindfulness. (2018) 9:1522–8. doi: 10.1007/s12671-018-0900-9
126. Zhu, B, Hedman, A, Feng, S, Li, H, and Osika, W. Designing, prototyping and evaluating digital mindfulness applications: a case study of mindful breathing for stress deduction. J Med Internet Res. (2017) 19:e197. doi: 10.2196/jmir.6955
127. Groß, D, and Kohlmann, C-W. Increasing heart rate variability through progressive muscle relaxation and breathing: a 77-day pilot study with daily ambulatory assessment. Int J Environ Res Public Health. (2021) 18:11357. doi: 10.3390/ijerph182111357
128. Krkovic, K, Clamor, A, and Lincoln, TM. Emotion regulation as a predictor of the endocrine, autonomic, affective, and symptomatic stress response and recovery. Psychoneuroendocrinology. (2018) 94:112–20. doi: 10.1016/j.psyneuen.2018.04.028
129. Seddon, JA, Rodriguez, VJ, Provencher, Y, Raftery-Helmer, J, Hersh, J, Labelle, PR, et al. Meta-analysis of the effectiveness of the Trier social stress test in eliciting physiological stress responses in children and adolescents. Psychoneuroendocrinology. (2020) 116:104582. doi: 10.1016/j.psyneuen.2020.104582
130. Allen, AP, Kennedy, PJ, Dockray, S, Cryan, JF, Dinan, TG, and Clarke, G. The Trier social stress test: principles and practice. Neurobiol Stress. (2017) 6:113–26. doi: 10.1016/j.ynstr.2016.11.001
131. Quintana, DS, and Heathers, JAJ. Considerations in the assessment of heart rate variability in biobehavioral research. Front Psychol. (2014) 5:805. doi: 10.3389/fpsyg.2014.00805
132. Hartmann, R, Schmidt, FM, Sander, C, and Hegerl, U. Heart rate variability as indicator of clinical state in depression. Front Psychol. (2019) 9:735. doi: 10.3389/fpsyt.2018.00735
133. Campbell, AA, Wisco, BE, Silvia, PJ, and Gay, NG. Resting respiratory sinus arrhythmia and posttraumatic stress disorder: a meta-analysis. Biol Psychol. (2019) 144:125–35. doi: 10.1016/j.biopsycho.2019.02.005
134. Castaldo, R, Melillo, P, Bracale, U, Caserta, M, Triassi, M, and Pecchia, L. Acute mental stress assessment via short term HRV analysis in healthy adults: a systematic review with meta-analysis. Biomed Signal Proces Cont. (2015) 18:370–7. doi: 10.1016/j.bspc.2015.02.012
135. de Vibe, M, Solhaug, I, Tyssen, R, Friborg, O, Rosenvinge, J, Sorlie, T, et al. Does personality moderate the effects of mindfulness training for medical and psychology students? Mindfulness. (2015) 6:281–9. doi: 10.1007/s12671-013-0258-y
136. Faul, F, Erdfelder, E, Lang, A-G, and Buchner, A. G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. (2007) 39:175–91. doi: 10.3758/BF03193146
137. Faul, F, Erdfelder, E, Buchner, A, and Lang, A-G. Statistical power analyses using G*power 3.1: tests for correlation and regression analyses. Behav Res Methods. (2009) 41:1149–60. doi: 10.3758/BRM.41.4.1149
138. Asbrand, J, Heinrichs, N, Nitschke, K, Wolf, OT, Schmidtendorf, S, and Tuschen-Caffier, B. Repeated stress leads to enhanced cortisol stress response in child social anxiety disorder but this effect can be prevented with CBT. Psychoneuroendocrinology. (2019) 109:104352. doi: 10.1016/j.psyneuen.2019.06.003
139. Brugnera, A, Zarbo, C, Tarvainen, MP, Carlucci, S, Tasca, GA, Adorni, R, et al. Higher levels of depressive symptoms are associated with increased resting-state heart rate variability and blunted reactivity to a laboratory stress task among healthy adults. Appl Psychophysiol Biofeedback. (2019) 44:221–34. doi: 10.1007/s10484-019-09437-z
140. Hu, MX, Lamers, F, de Geus, EJC, and Penninx, BWJH. Differential autonomic nervous system reactivity in depression and anxiety during stress depending on type of stressor. Psychosom Med. (2016) 78:562–72. doi: 10.1097/PSY.0000000000000313
141. Jandackova, VK, Britton, A, Malik, M, and Steptoe, A. Heart rate variability and depressive symptoms: a cross-lagged analysis over a 10-year period in the Whitehall II study. Psychol Med. (2016) 46:2121–31. doi: 10.1017/S003329171600060X
Keywords: heart rate variability, blood pressure, mindfulness, self-compassion, stress task, clinical trial
Citation: Andorfer A, Kraler S, Kaufmann P, Pollheimer E, Spah C, Fuchshuber J, Rominger C, Traunmüller C, Schwerdtfeger A and Unterrainer H-F (2023) Psychophysiological stress response after a 6-week Mindful Self-Compassion training in psychiatric rehabilitation inpatients: a randomized post-test only study. Front. Psychiatry. 14:1098122. doi: 10.3389/fpsyt.2023.1098122
Received: 14 November 2022; Accepted: 30 June 2023;
Published: 18 July 2023.
Edited by:
Brian Schwartz, University of Trier, GermanyReviewed by:
Jeffrey M. Greeson, Rowan University, United StatesCopyright © 2023 Andorfer, Kraler, Kaufmann, Pollheimer, Spah, Fuchshuber, Rominger, Traunmüller, Schwerdtfeger and Unterrainer. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Human-Friedrich Unterrainer, aHVtYW4udW50ZXJyYWluZXJAdW5pdmllLmFjLmF0
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.