- 1Social and Health Psychology Laboratory, Department of Psychology, The University of Hong Kong, Hong Kong, Hong Kong SAR, China
- 2Department of Education, Johns Hopkins University, Baltimore, MD, United States
Introduction: In the first wave of the COVID-19 pandemic, the unknown etiology and treatment of the highly transmissible coronavirus posed considerable threats to public mental health. Many people around the globe turned to religion as an attempt to mitigate their heightened psychological distress, but mixed findings have been obtained regarding the association between the use of religious coping and two psychological symptoms—anxiety and depressive symptoms—widely reported in the initial wave.
Objective: The present meta-analysis was conducted to resolve the empirical inconsistency by synthesizing this body of studies and identifying both individual and national-level factors that accounted for the inconsistent findings.
Methods: Following PRISMA guidelines, the literature search and data screening procedures yielded 42 eligible studies, with 25,438 participants (58% females, average age = 36.50 years) from 24 countries spanning seven world regions.
Results: Overall, the results showed that only negative religious coping was positively associated with psychological symptoms (r = 0.2886, p < 0.0001). Although the associations of both general and positive religious coping with psychological symptoms were non-significant (rs = 0.0425 and −0.0240, ps > 0.39), the moderation analysis revealed significant positive associations between positive religious coping and psychological symptoms in two demographic groups who experienced greater pandemic distress than their counterparts: younger participants and female participants.
Discussion: This meta-analysis provides a nuanced understanding of the complex nature of religious coping in the initial wave of the COVID-19 pandemic when the levels of public anxiety and stress were heightened. The exclusive use of religious coping may not be associated with low levels of psychological symptoms, implying the importance of supplementing the deployment of this strategy with an array of other strategies. Therapists of mental health interventions should show their clients how to make good use of positive religious coping together with other strategies, and how to avoid the use of negative religious coping, to handle their psychological problems.
Systematic review registration: https://osf.io/shb32/
1. Introduction
Since late 2019, the COVID-19 outbreak has swept swiftly across the globe, affecting more than 650 million people in 228 countries and territories worldwide as of December 2022 (1). As COVID-19 was caused by an atypical, novel type of coronavirus when it first emerged (2, 3), levels of public anxiety and stress were heightened in the initial wave of the pandemic from December 2019 to July 2020 (4–9). Many individuals from affected regions perceived a low sense of control or hope (10, 11) when unprecedented mandatory disease mitigation measures were implemented during this period (12–15).
During the outbreak of COVID-19, many individuals have resorted to religion for stress relief. Religion constitutes an important part of human civilization and exerts a huge impact on people’s behavior (16), and religious coping has been commonly adopted for handling stressful life circumstances, especially those whose outcomes are perceived to be largely beyond one’s control (17–20). Religious coping is defined as to the use of religious beliefs or behavior to prevent or alleviate the unpleasant emotions elicited by stressful life circumstances (21). Religious coping is proposed to serve five major functions, namely searching for meaning, achieving a sense of mastery and control, seeking comfort or spirituality, increasing intimacy with others, and transforming life (22).
When the World Health Organization declared COVID-19 a pandemic in March 2020, the search volume of the keyword “prayer” on Google search engine increased by 30% relative to all other Google searches, soaring to a record-high level (23). Some scholars have maintained that the use of religious coping to deal with pandemic stress should have mental health benefits, primarily because religion could serve as an alternative source of emotional support during these difficult times, when support from social network members was largely inaccessible because of physical distancing measures (24, 25). In line with these notions, some studies conducted during the initial wave of COVID-19 have shown that more frequent use of religious coping was associated with lower levels of perceived stress, better mental health, and lower sense of helplessness, and that less frequent use of religious coping was associated with higher levels of psychological symptoms such as anxiety and depression (26–29).
Despite such psychological benefits, there were also studies that yielded null or even contrary findings regarding the association between the use of religious coping and certain mental health criteria. Specifically, some studies have revealed that the frequency of using religious coping was unrelated to stress, anxiety, and depressive symptoms (30–32), whereas others have revealed that these coping–symptom associations were positive (33–35). For example, in a study conducted among individuals diagnosed with COVID-19, the use of religious coping was positively associated with death anxiety (36). Furthermore, Cowden et al. (37) found that greater use of religious coping was positively associated with perceived suffering and resource losses across physical, psychological, and interpersonal domains.
To resolve this body of inconsistent empirical evidence regarding the association between the use of religious coping and psychological symptoms during the first wave of the COVID-19 pandemic, a meta-analysis was conducted to systematically evaluate the findings derived from prior studies and to provide a quantitative estimate of the overall effect size of the religious coping–symptom association (38, 39). In addition, a moderator analysis was performed to explain possible between-study variations in the effect size estimates.
A review of the literature revealed that three clusters of moderators could account for the between-study differences. First, the dimension of religious coping has been proposed to moderate the magnitude of the coping–symptom association. Earlier research (40, 41) conceptualized religious coping as a non-specific unidimensional construct labeled “general religious coping” (GRC) (40, 42). Subsequent works have found that GRC could have both desirable and undesirable effects on mental health and thus have argued for the need to distinguish positive religious coping (PRC) from negative religious coping (NRC) (16, 43).
Typical examples of PRC are seeking psychological comfort from God or a transcendent force and seeing God as a partner who guides one along the journey of life (16, 43). From psychodynamic and developmental perspectives (44), religion has beneficial effects on mental health through emphasizing the inner and long-lasting meaning of life, cultivating a sense of God’s blessings, and providing personal and community resources to cope with stressors that are largely beyond one’s control. Studies have supported this notion by revealing the mental health benefits of PRC, such as the amelioration of depressive symptoms and the improvement of health-related quality of life (19, 20).
Typical examples of NRC are perceived conflicts and struggles with God or spirituality, difficulty seeing the meaning of life, doubts about support from God, and anger toward God (16, 43, 45). In this perspective, NRC does not only fail to relieve stress but can even elicit greater unpleasant emotions such as agitation and fury. This dimension of religious coping has been found to be positively associated with anxiety and depressive symptoms, as well as with poor health-related quality of life across various life domains (20, 46).
Second, the magnitude of the religious coping–symptom association may vary according to age and sex. Our notion stems from studies that have revealed that individuals of different sexes and ages tended to react to stress and to use religious coping in diverse ways. With regard to age differences, older people were found to be more religious (47, 48). Moreover, older patients with chronic hepatitis C tended to rely more on religion and to search for meaning as coping mechanisms to deal with stress more than their younger counterparts (49).
With regard to sex differences, studies have shown that the spouses of male patients with lung cancer tended to use religious coping to handle stress more than those of female patients (50). Similar sex differences in the use of religious coping were also obtained in research conducted during the COVID-19 pandemic (51). These findings may be explained by research showing that women are characterized by a higher level of religiosity than men (48, 52). In addition, female adolescents tended to use PRC more to cope with pandemic stress, whereas their male counterparts tended to use NRC more. Such sex differences may be explained by men’s greater tendency to see God as controlling (53, 54).
Third, the strength of the religious coping–symptom association was proposed to vary by two religion-related characteristics at the national level: dominant religion and religiosity. COVID-19 has affected many countries with various dominant religions, and thus, the religious beliefs and practices of residents of these countries should differ considerably. According to an extensive global analysis of religion (55), Christianity is the most widely practiced religion worldwide, and it is the dominant religion in many Western countries in North and South America, Western Europe, and Oceania (56). Islam and Hinduism are the second and third most widely practiced religions, respectively, and are the dominant religions in many non-Western countries in the Middle East and Asia (57, 58). In addition to the dominant religion, there are also vast between-country variations in the extent of national religiosity, which reflects the overall level of religiosity of the residents of a country (59). National religiosity comprises the key components of religious affiliation, attendance of religious activities, and religious beliefs (60, 61).
In multinational comparisons, the potential confounding effects of certain national characteristics should be controlled to ensure robust hypothesis testing. Socioeconomic development is a crucial confounding factor. This notion stems from a previous multinational comparison that identified differences in national subjective well-being among countries with distinct levels of socioeconomic development (62). Residents of developed (vs. developing) countries are generally less susceptible to psychological problems because of the availability of better social welfare and healthcare services.
A multinational comparison may also be confounded by the between-country differences in the number of confirmed COVID-19 infections and mortality cases (1) as well as the strictness of the COVID-19 containment measures imposed (63). During the first wave of the pandemic, some governments (e.g., Italy) issued stay-at-home orders with exceptions for “essential” trips such as clinic visits, while others (e.g., France) required their residents not to leave home with minimal exceptions (e.g., once per week or one household member at a time). However, some governments (e.g., Japan) only advised their residents not to leave home and did not issue any mandates.
In summary, the present meta-analysis aimed to quantitatively synthesize the literature investigating religious coping and mental health issues amid the first wave of the COVID-19 pandemic, and to account for potential between-study variations in the associations between religious coping and psychological symptoms by three clusters of moderators (i.e., dimension of religious coping, demographics, and religion-related characteristics).
2. Methods
The present meta-analysis was conducted to address the research questions regarding the hypothesized variations in the magnitude of the three dimensions of religious coping (i.e., GRC, PRC, and NRC) and two major indicators of psychological symptoms (i.e., depressive and anxiety symptoms) experienced during the initial wave of the COVID-19 pandemic. The meta-analysis was performed and reported in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2020 guidelines (64). As all the data were extracted from previous primary studies, no institutional ethical approval was required. The study design, eligibility criteria, coding process, and data-analytic procedures of the meta-analysis were preregistered via the Open Science Framework1.
2.1. Eligibility criteria
To screen potentially relevant eligible articles, eligibility criteria were developed a priori. Specifically, inclusion criteria were primary studies that included measures of both religious coping and any of the aforementioned target symptoms. Studies were excluded if at least one of the following criteria were met: (a) no empirical data (e.g., reviews and qualitative studies); (b) no relevant measures of religious coping or target symptoms; (c) data were collected before the COVID-19 pandemic; (d) duplicate samples; or (e) inadequate information for effect size estimation.
2.2. Information sources
Computerized literature searches were first conducted to systematically locate primary studies. These general and discipline-specific databases spanned the social science (e.g., Applied Social Sciences Index and Abstracts and PsycInfo®), health and medical science (e.g., Health and Safety Science Abstracts and MEDLINE®), and multi-disciplinary (e.g., Scopus and Web of Science) research fields. Moreover, gray literature (e.g., Google Scholar and OpenGrey) and dissertation databases (e.g., Open Access Theses and Dissertations and Networked Digital Library of Theses and Dissertations) were searched for additional primary studies, especially unpublished ones. Finally, scholars were contacted to request unpublished or unavailable works. Requests were made to 24 investigators, of whom 13 provided articles, data, or statistics.
2.3. Search strategy
When conducting the various literature searches, the following thesaurus text words and MeSH (Medical Subject Headings) were combined using the Boolean operators “AND” and “OR”: (“religious coping” OR “religion coping”) AND (“COVID” OR “coronavirus”) AND (“anxiety*” OR “depressi*” OR “mental health” OR “distress” OR “disorder”). These combined terms were searched in the title, abstract, and subject of potentially relevant works.
To obtain as many potentially relevant articles as possible, we did not impose any restrictions regarding the articles’ publication status, publication date, language, study design, or sample characteristics (i.e., country of origin, age group, race, and ethnicity).
2.4. Selection and data collection processes
As the search results were derived from multiple sources, duplicate records were identified and removed using the EndNote software (version 20.4.1). Then, two independent reviewers conducted preliminary relevance screening and perused the full-text articles for further screening and coding.
After the pool of eligible studies was finalized, the data extraction task was carried out by the same two reviewers according to a coding manual with full descriptions of the pre-established inclusion and exclusion criteria. The triangulation method was used to enhance inter-reviewer reliability (65). Specifically, the two reviewers were calibrated using a random sample of 10% of the eligible studies. Upon completion of the calibration process, each reviewer coded the remaining studies on their own. Any discrepancies between the reviewers were resolved with the assistance of the first author in post-hoc meetings.
Inter-reviewer reliability was evaluated using the concordance statistic of Krippendorff alpha (66). The results showed adequate inter-reviewer reliability for the final coding (Krippendorff alphas ≥ 0.69 for all the coded items).
2.5. Data items
Pearson r was chosen as the target effect size for the present meta-analysis because of its high interpretability (67), and the effect size indicated the magnitude of the association between a dimension of religious coping and psychological symptoms. If Pearson r was not reported in any eligible studies, relevant statistics (e.g., t-values and odds ratios) were transformed into Pearson r using the esc package written in the R programing language (68).
The following data items were also recorded for each of the eligible studies: author(s), year of publication, publication status (1 = published, 0 = unpublished), country in which the study was conducted, dominant religion of the country, gender composition (% of females), age composition (mean or median age), measure of religious coping, dimension of religious coping, measure of symptom, type of symptom, and language of the article. Any missing information, clarifications, or verifications were requested from the authors of individual primary studies through email.
The religion-related data were extracted from the GALLUP and NationMaster databases (69, 70). The numbers of confirmed COVID-19 cases and deaths reported during the study period were extracted from the Our World in Data database (71). The national data regarding the strictness of containment measures imposed during the study period were obtained from the database of the Oxford COVID-19 Government Response Tracker (63).
2.6. Statistical analysis
Many studies have examined and reported more than one effect size, and it is noteworthy that the problem of dependence could bias the standard errors and statistical inferences of a meta-analysis. This potential methodological problem was addressed using a three-level meta-analysis (72), taking into account the hierarchically nested structure of the present data.
A χ2-based homogeneity test was performed to assess heterogeneity across the eligible studies. The presence of between-study heterogeneity was indicated by a significant Cochran’s Q statistic (i.e., p < 0.05). The level of heterogeneity was indicated by the inconsistency index I2. In line with a widely adopted standard (73), heterogeneity was interpreted as (a) no to low for an I2 value that was less than 25%, (b) moderate for an I2 value that fell within the 25–75% range, and (c) high for an I2 value that was greater than 75% (73). A random-effects model should be used if the results indicate a significant moderate to high level of heterogeneity, and a fixed-effects model should be used otherwise.
Mixed-effects meta-regression analysis was used to test the moderation effects that might explain the between-study heterogeneity. The meta-regression was undertaken in a multivariate manner, with relevant predictors and control variables entered simultaneously (72). To unpack the significant moderation effects, simple slope analysis was conducted to estimate the effect sizes of the subgroups that were high (+1.5 SD) and low (−1.5 SD) in a particular dimension.
Outlier analysis was performed on the individual effect size estimates to detect possible outliers (74). If outliers were identified, the outlier removal method was used (75). The results yielded by this method were compared with those derived from the full dataset. If there were discrepancies, both sets of results were reported. If both sets of data yielded a highly similar pattern of findings, only the full findings were reported.
For the major analyses, both the three-level meta-analysis and meta-regression analysis were conducted using RStudio for Windows (version 2022.02.0+443; RStudio Team, Boston, MA) with the R package metafor (76). Krippendorff alpha was derived from the SPSS macro KALPHA (66) conducted in IBM® SPSS® (version 26.0; IBM Corp, Armonk, NY).
2.7. Study risk of bias and certainty assessments
The meta-analysis pooled the effect size estimates from an array of individual studies, and inevitably, the methodological quality varied vastly across the studies. The risk of study bias was evaluated using study quality assessment (77). The following indicators were coded and evaluated based on previous meta-analytic reviews (e.g., (78, 79)): statistical power (1 = Cronbach alpha ≥ 0.70, 0 = Cronbach alpha < 0.70), sampling method (1 = probabilistic sampling, 0 = non-probabilistic sampling), study design (1 = longitudinal, 0 = cross-sectional), measurement reliability (proportion of measures with adequate internal consistencies), and measurement validity (proportion of validated measures).
It is also important to detect the potential confounding effects of various biases and to verify the robustness of the study conclusions. To detect the possible risk of single-study bias, one-study-removed sensitivity analysis was conducted for all six effect size estimates. This sensitivity analysis examined whether the overall meta-analytic findings would be altered by the omission of any single eligible study. The robustness of the findings would be demonstrated if an overall effect size estimate remained stable across the various stages of study removal. However, significant changes in any of the effect size estimates indicated the presence of single-study bias.
Publication bias was estimated using various common statistical techniques. Specifically, potential publication bias was first visualized by a funnel plot, and then Egger’s linear regression test was conducted to identify funnel plot asymmetry (80). A significant test result revealed that the funnel plot was asymmetrical, suggesting the presence of publication bias. Finally, trim-and-fill techniques were used to adjust for missing studies, and the effect size estimates yielded after this adjustment were compared with those yielded by the original dataset (81). Publication bias was revealed if substantial differences were detected between these two effect size estimates. The sensitivity analysis and all the methods for publication bias assessment were performed using Comprehensive Meta Analysis version 2.2.020 (Biostat, Englewood, NJ).
Finally, p-curve analysis was used to assess the robustness of the present meta-analytic findings by estimating the true effect size (82). This analysis yielded curves that showed the distribution of p-values reported in the eligible studies, and the evidential value of the present pool of eligible studies was demonstrated by significant right-skewed p-curves.
3. Results
3.1. Study selection
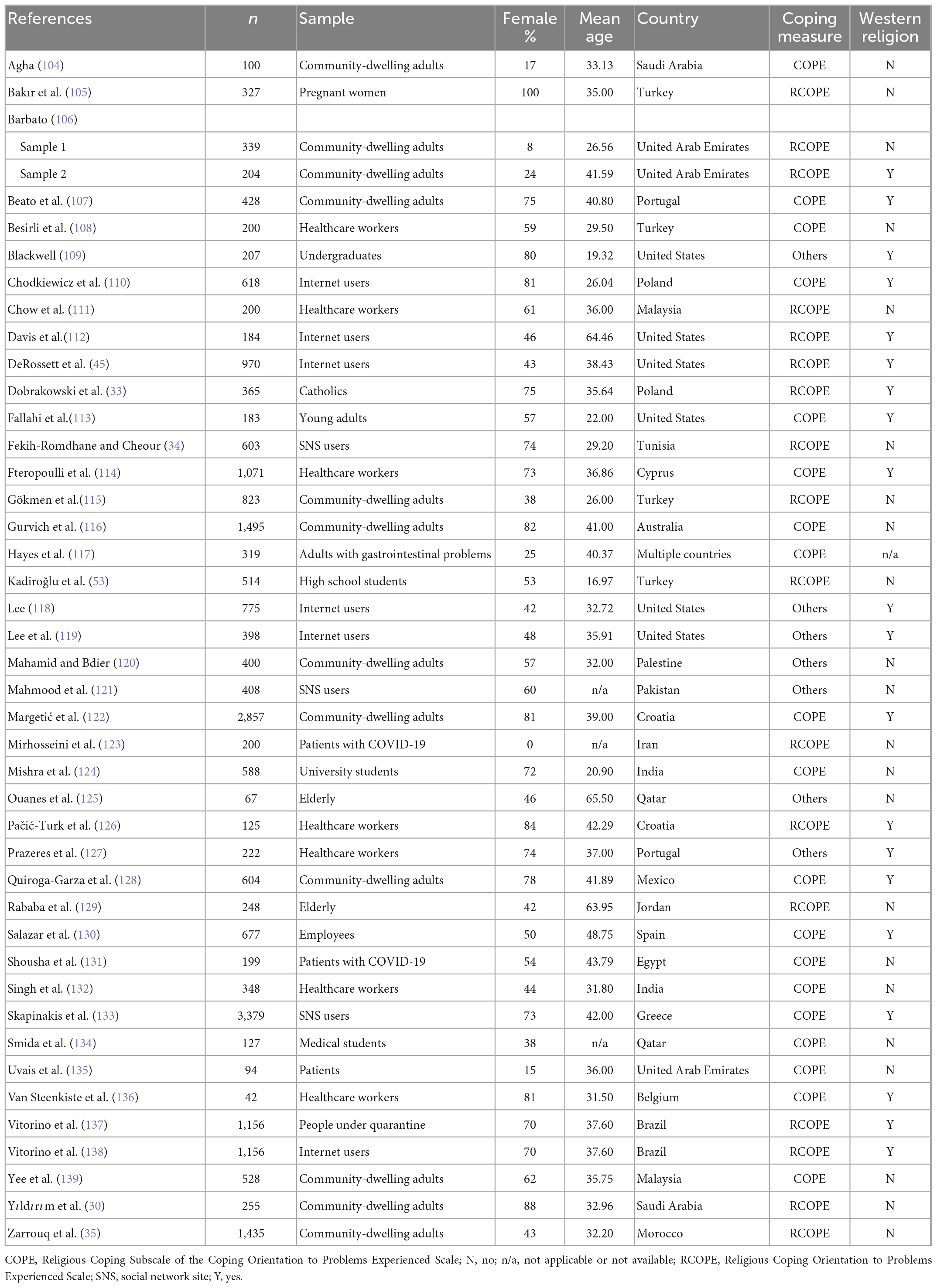
The literature search and coding stages involved in this meta-analytic review are summarized in a PRISMA flow chart (see Figure 1). After we applied the predefined eligibility criteria, the final dataset consisted of 42 primary studies. Table 1 summarizes the study characteristics of these studies included in the meta-analysis.
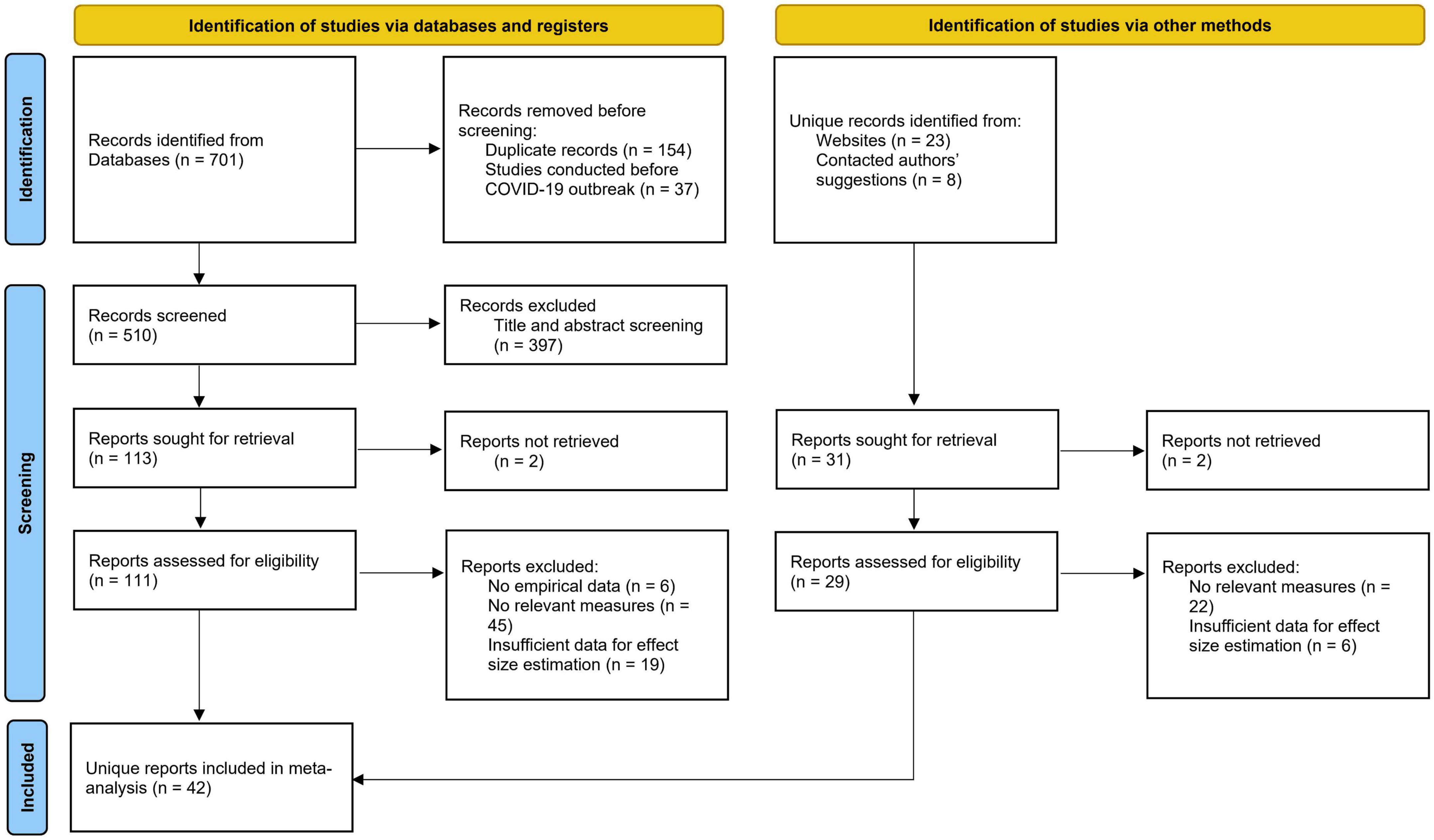
Figure 1. Flow diagram of search and selection strategies for reports in the present meta-analysis (64).
3.2. Study characteristics
Of the 42 primary studies, the majority (96%) were journal articles, 2% were research reports, and 2% were unpublished theses or dissertations. The pool of eligible studies comprised 43 independent samples with a total of 25,438 participants (mean = 592; SD = 674.57). In the samples, 58% were females, and the mean age was 36.50 years (SD = 10.67). The samples were drawn from 24 countries spanning seven world regions: 33% from Europe (e.g., Croatia and Spain), 26% from the Middle East (e.g., Palestine and the United Arab Emirates), 15% from North America (e.g., Mexico and the United States), 12% from Asia (e.g., India and Malaysia), 7% from South America (Brazil), 5% from Africa (Egypt and Morocco), and 2% from Oceania (Australia).
Western religion (Protestant Christianity, Roman Catholicism, Orthodoxy) was dominant in 47% of the countries, and non-Western religion (Islam and Hinduism) was dominant in 51% of the countries. The remaining 2% were studies that included more than two countries, and thus, the national religion-related data could not be coded. The average national religiosity score of the entire pool of eligible studies was 78.55 (SD = 16.17), and ranged from 32 (Australia) to 97 (Egypt).
3.3. Main-effect analysis of religious coping–symptom associations
Table 2 summarizes the results of the main-effect analysis of all the associations between the three dimensions of religious coping (i.e., GRC, PRC, and NRC) and psychological symptoms. As shown in the left panel of the table, there were significant positive associations between NRC and psychological symptoms (ps < 0.0004). In contrast, all the other religious coping–symptom associations were non-significant.
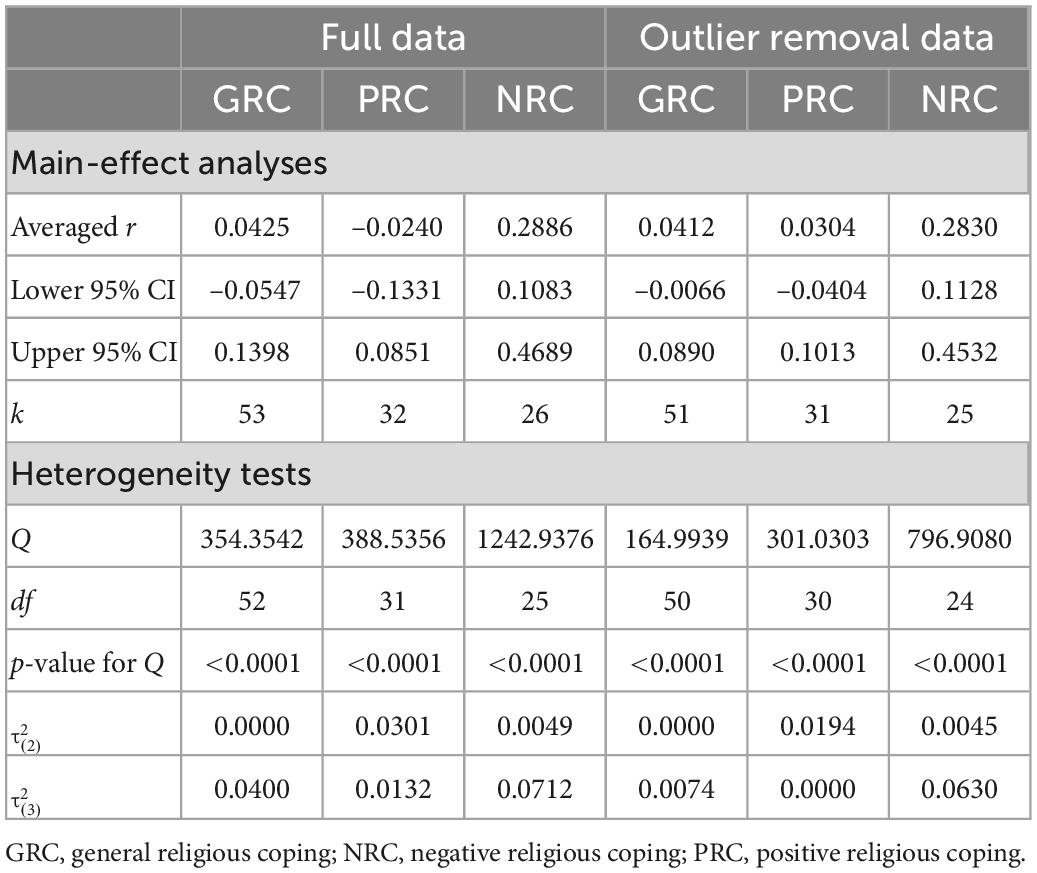
Table 2. Main-effect analyses and homogeneity tests for the associations between three dimensions of religious coping and psychological symptoms (r).
The outlier analysis revealed four outliers. Two were identified in the studies that examined GRC, one in the studies that examined PRC, and one in the studies that examined NRC. Using the outlier removal method, the pattern of results was highly similar to that yielded from the full dataset, and the conclusions drawn from both sets of findings were the same (see the right panel of Table 2). Hence, the meta-analysis and moderation analysis were performed using the full dataset.
All the Cochran’s Q statistics indicated the presence of heterogeneity (ps < 0.0001), and all the I2 statistics indicated moderate levels of heterogeneity. These results demonstrated that the random-effects model should be used and that moderation analysis should be conducted to identify the sources of heterogeneity.
3.4. Moderation analysis
The results of the moderation analysis are summarized in Table 3. As shown in this table, there were some significant moderation effects for PRC and NRC, but all the moderation effects for GRC were non-significant. Two sample characteristics—age and sex composition—moderated the associations between PRC and psychological symptoms. Specifically, post-hoc simple slope analysis indicated that the hypothesized negative PRC–symptom association was marginally significant in samples with a greater proportion of older participants (r = –0.2015, SE = 0.1172, p = 0.0854), but this association was positive in samples with a larger proportion of younger participants (r = 0.4078, SE = 0.0743, p < 0.0001). Moreover, there was a significant positive PRC–symptom association in samples including more female participants (r = 0.2618, SE = 0.0800, p = 0.0011), whereas this association was non-significant in samples including fewer female participants (r = –0.0556, SE = 0.0888, p = 0.5315).
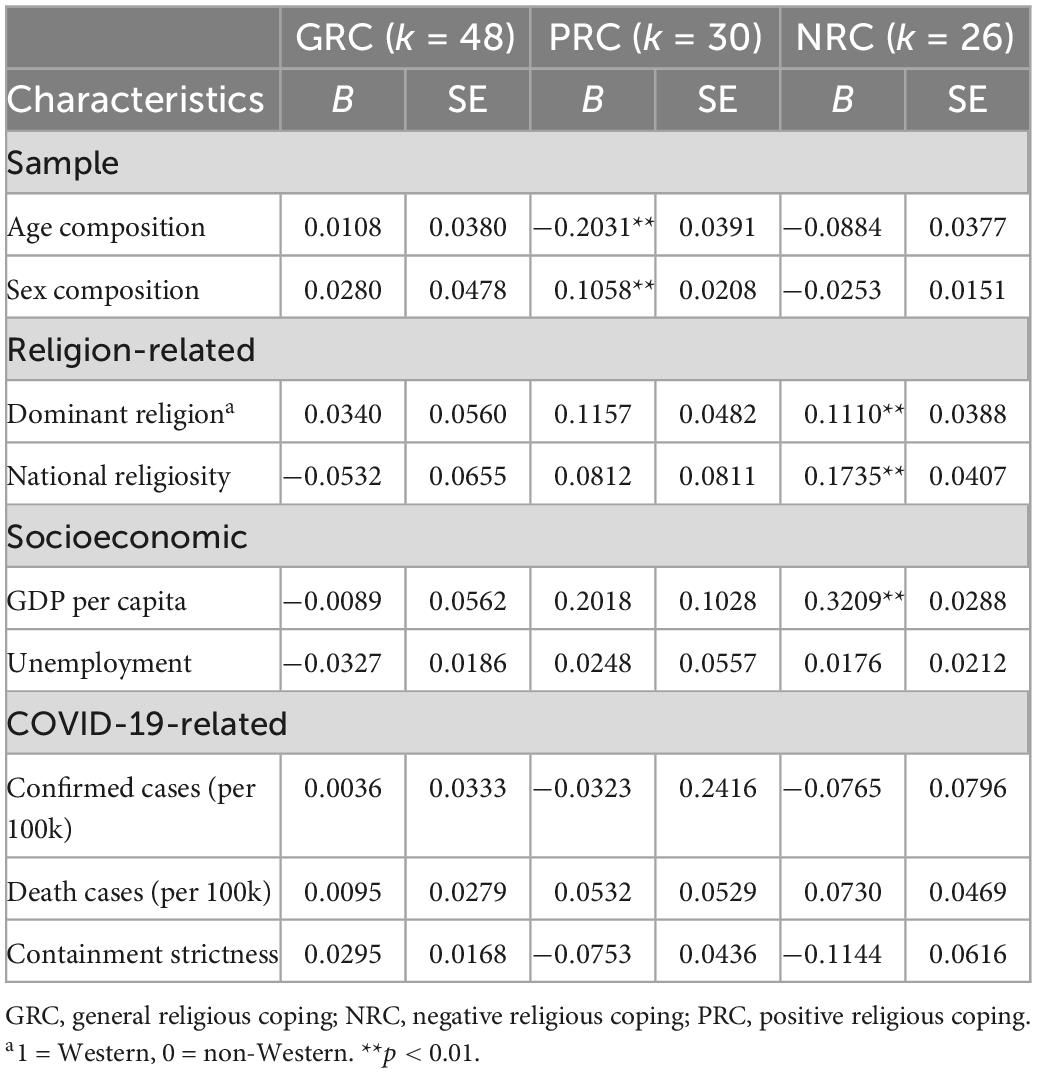
Table 3. Moderator analyses for the associations between three dimensions of religious coping and psychological symptoms.
Two national religion-related characteristics—dominant religion (Western vs. non-Western) and religiosity—were found to moderate the associations between NRC and psychological symptoms. The positive NRC–symptom associations were significant in countries with a non-Western dominant religion (r = 0.1668, SE = 0.0490, p = 0.0007) as well as in countries with a Western dominant religion (r = 0.4249, SE = 0.1857, p = 0.0221), but the magnitude of these significant positive associations differed. In addition, the hypothesized positive NRC–symptom association was significant in countries with higher religiosity (r = 0.6639, SE = 0.0679, p < 0.0001) but only marginally significant in those with lower religiosity (r = 0.1434, SE = 0.0749, p = 0.0556).
3.5. Risk of bias in studies
The results indicated that the majority of the eligible studies (91%) had adequate statistical power. Approximately two-thirds of the studies included measures that displayed adequate internal consistency (67%) and included validated measures (65%). However, only 7% of the studies used a random sampling method, and only 2% adopted a longitudinal or prospective design.
The results of the moderation analysis revealed that study design had significant moderating effects on the association between GRC and psychological symptoms (B = –0.1625, SE = 0.0289, p < 0.0001). Although the GRC–symptom association was non-significant in the majority of studies adopting a cross-sectional design (r = 0.0569, SE = 0.0537, p = 0.2892), it is noteworthy that the negative GRC–symptom association was marginally significant in the small subset of studies adopting a longitudinal or prospective design (r = –0.1265, SE = 0.0654, p = 0.0530).
Significant moderation effects of scale reliability were also found on the association between PRC and psychological symptoms (B = 0.1330, SE = 0.0502, p = 0.0081). The hypothesized positive PRC–symptom association was obtained in studies adopting less reliable measures (r = –0.2540, SE = 0.0992, p = 0.0104), but this association was non-significant in studies adopting more reliable measures (r = 0.1449, SE = 0.0866, p = 0.0942).
The one-study-removed sensitivity analysis revealed considerable stability for each of the six effect size estimates, indicating low risk of single-study bias. Regarding publication bias, the results revealed that the Egger’s tests failed to indicate publication bias (all ps > 0.05). Similarly, the trim-and-fill techniques did not alter the pooled effect size estimates. Finally, the p-curves of all three religious coping–symptom associations were significant and right-skewed, demonstrating considerable evidence value and the absence of the p-hacking problem. The statistical power of the three religious coping–symptom associations were also high, ranging from 0.96 to 0.99. Taken together, these analyses provided empirical evidence for the robustness of the meta-analytic findings.
4. Discussion
The present meta-analysis investigated the use of religious coping and its association with psychological symptoms experienced amid the initial wave of the COVID-19 pandemic, a period during which a series of unprecedented physical distancing measures were in place and public stress levels were heightened. The magnitude of the religious coping–symptom association was found to vary according to the dimension of religious coping. Overall, the hypothesized negative association between NRC and psychological symptoms was identified, but the associations with psychological symptoms were non-significant for both GRC and PRC.
Although the overall PRC–symptom association was found to be non-significant, the strength of this association was moderated by the age and sex composition of the samples. A significant positive PRC–symptom association was obtained in eligible studies including a higher proportion of younger participants and those including more female participants. It is noteworthy that younger individuals and women have been identified as two psychologically vulnerable groups amid the initial wave of the COVID-19 pandemic, with both women (vs. men) and the younger (vs. older) generation generally reporting higher levels of anxiety and depression (35, 51, 83–86). Both of these psychologically vulnerable groups may have a greater need to cope with their heightened distress, but the sole use of religious coping may not adequately mitigate their heightened levels of psychological symptoms. These findings did not reveal the hypothesized mental health benefits of PRC in mitigating psychological symptoms, but more frequent use of this type of religious coping was associated with higher levels of psychological symptoms during the first wave of the COVID-19 pandemic, especially for psychologically vulnerable people.
Previous research has unveiled two major cognitive mechanisms—cognitive reappraisal and perceived coping efficacy—that accounted for the mental health benefits of PRC (87, 88). These findings imply that the use of PRC as the sole strategy to mitigate stress-related distress may not be sufficient. In light of the previous findings, the use of PRC should be accompanied by the deployment of other adaptive cognitive and behavioral strategies, namely positive reframing, emotion regulation, and seeking social support (87). The hypothesized mental health benefits of PRC was not found in the first wave of the COVID-19 pandemic, a particular context when the etiology, treatment, and preventive measures were still unknown (89–92). In this period of high stress and uncertainty, many residents of COVID-19-affected regions reported a strong sense of helplessness and lack of control (93, 94). In addition, social isolation tends to decrease opportunities for these residents to receive support from social network members living apart (95). Such unusual circumstances and heightened stress levels may weaken the effectiveness of PRC in handling pandemic stress, which is largely beyond people’s control (93).
The present meta-analysis revealed robust findings regarding the hypothesized positive association between NRC and psychological symptoms. In the literature, three psychological mechanisms have been identified to account for this positive association: life stress, cognitive processes, and delay in seeking professional treatment (21). Public anxiety and stress reached unusually high levels during the initial wave of the COVID-19 pandemic. The use of problem-focused coping, such as doing regular exercise and practicing hand hygiene, has been found to be effective in reducing pandemic stress (96). Excessive attention to religious activities may enhance people’s tendency to neglect the deployment of these effective strategies; in particular, the use of NRC may lead vulnerable people to pay excessive attention to real or imagined “sin” (21). More importantly, excessive dependence on religious rituals and activities may delay professional treatment for mental health problems, which may lead to an aggravation of psychological symptoms (21). Hence, a “balanced” use of PRC together with other complementary adaptive coping strategies (e.g., cognitive reframing and emotion regulation) should be more effective in bolstering mental wellness during the COVID-19 pandemic (97).
Apart from demographic differences, national differences in the strength of the NRC–symptom association were also found in both the dominant religion (Western vs. non-Western) and religiosity, especially the latter. The positive NRC–symptom association was weaker in countries characterized by a Western religion and lower in religiosity. This intricate finding may reflect the recent observations in the decline in the level of religiosity in Western countries such as the United States (98). However, a stronger positive NRC–symptom association was found in countries with greater religiosity. This is probably because excessive attention to religious activities may increase one’s tendency to ignore work and family, which may in turn elicit additional sources of life stress such as job stress and family conflict (99). Also, excessive dependence on religious rituals and activities may delay the seeking of professional assistance for treating psychological problems, thus leading to more serious psychiatric disorders over time (21).
The present findings may have practical implications for mental health professionals. As religious coping is a preferred strategy for many people, facilitators of mental health treatment programs should make good use of PRC and also work to reduce the use of NRC when treating their clients who have experienced mental health issues during the COVID-19 pandemic (28, 97). As reviewed above, the use of religious coping may not be adequate for attaining this treatment goal, but clients need to acquire a variety of effective coping skills to broaden their coping repertoire (100, 101). For instance, facilitators may mitigate clients’ sense of helplessness by showing them how to distinguish between aspects of the pandemic that are under their control (e.g., perceived responsibility for one’s own health and adherence to health advice on COVID-19 prevention) and those that are beyond their control (e.g., implementation of mandatory disease mitigation measures and undesirable behaviors by others such as stockpiling). PRC should be used together with a number of complementary strategies to mitigate psychological symptoms and enhance mental wellness amid the COVID-19 pandemic (102).
In addition to practical implications, our meta-analytic findings also have implications for researchers. The null findings for the GRC–symptom association suggest that conceptualizing and assessing religious coping as a unidimensional construct should be avoided. Rather, the findings provide further evidence that PRC and NRC are conceptually distinct and thus should be assessed by separate scales, each with a unique set of coping behaviors. In addition, it is important to note that the mental health benefits of GRC were found in a small subset of studies that contained more than a single time point. In this small but significant body of longitudinal or prospective studies, GRC was found to reduce psychological symptoms over time during the COVID-19 pandemic. The overall null findings for the GRC–symptom association may have been yielded by the cross-sectional studies that currently dominate the literature on coping with COVID-19. More longitudinal or prospective studies should be conducted to capture the trajectory of the use of religious coping and an array of other coping strategies to deal with stress as the pandemic unfolds.
Finally, our study quality assessment revealed some methodological limitations in the studies included in the present meta-analysis. Very few (7%) of the studies relied on probabilistic sampling for participant recruitment, and even fewer (2%) investigated the use of religious coping over more than one time point; thus, possible changes in strategy deployment and mental health levels over time remain largely unknown. As public anxiety tends to fluctuate across various waves of a disease outbreak (103), more follow-up studies using probabilistic sampling methods should be conducted to address these methodological issues, thus advancing our understanding of when and how the use of religious coping can exert desirable and undesirable effects on the general public’s mental health.
Data availability statement
The original contributions presented in this study are included in this article, further inquiries can be directed to the corresponding author.
Author contributions
CC contributed to the study design, investigation, supervision and coordination of data coding and all other research tasks, statistical analysis, data interpretation, and wrote the first draft of the manuscript. WY contributed to the investigation, literature search, data interpretation, and wrote portions of the manuscript. Both authors contributed to the article and approved the submitted version.
Funding
This study was funded by the Hong Kong Research Grants Council’s General Research Fund (17601420) and the University of Hong Kong’s Seed Fund for Basic Research (202011159134).
Acknowledgments
We would like to thank Ellick Wong for statistical advice and comments on earlier drafts. We would also like to thank Boris Chung, Yan Guo, Janice Leung, and Terrence Sun for research and clerical assistance.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Johns Hopkins Coronavirus Resource Center. Coronavirus COVID-19 Global Cases: Johns Hopkins University and Medicine. (2022). Available online at: https://coronavirus.jhu.edu/map.html (accessed December 28, 2022).
2. Arabi Y, Murthy S, Webb S. COVID-19: a novel coronavirus and a novel challenge for critical care. Intensive Care Med. (2020) 46:833–6.
3. Borges do Nascimento I, Cacic N, Abdulazeem H, von Groote T, Jayarajah U, Weerasekara I, et al. Novel coronavirus infection (COVID-19) in humans: a scoping review and meta-analysis. J Clin Med. (2020) 9:941.
4. Cheng C, Wang H, Chau C. Mental health issues and health disparities amid COVID-19 outbreak in China: comparison of residents inside and outside the epicenter. Psychiatry Res. (2021) 303:114070. doi: 10.1016/j.psychres.2021.114070
5. Killgore W, Cloonan S, Taylor E, Dailey N. Mental health during the first weeks of the COVID-19 pandemic in the United States. Front Psychiatry. (2021) 12:535. doi: 10.3389/fpsyt.2021.561898
6. Pancani L, Marinucci M, Aureli N, Riva P. Forced social isolation and mental health: a study on 1,006 Italians under COVID-19 lockdown. Front Psychol. (2021) 12:1540. doi: 10.3389/fpsyg.2021.663799
7. Folayan M, Ibigbami O, El Tantawi M, Brown B, Aly N, Ezechi O, et al. Factors associated with financial security, food security and quality of daily lives of residents in Nigeria during the first wave of the COVID-19 pandemic. Int J Environ Res Public Health. (2021) 18:7925. doi: 10.3390/ijerph18157925
8. Cheng C, Wang H, Chan L. Multiple forms of mass anxiety in coronavirus disease-2019 pandemic. J Affect Disord. (2021) 291:338–43.
9. Lentoor A, Maepa M. Psychosocial aspects during the first wave of COVID-19 infection in South Africa. Front Psychiatry. (2021) 12:663758. doi: 10.3389/fpsyt.2021.663758
10. Roberts M, Knestrick J, Resick L. The lived experience of COVID-19. J Nurse Pract. (2021) 17:828–32.
11. Twenge J, Joiner T. Mental distress among U.S. adults during the COVID-19 pandemic. J Clin Psychol. (2020) 76:2170–82.
12. Benke C, Autenrieth L, Asselmann E, Pané-Farré C. Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. (2020) 293:113462. doi: 10.1016/j.psychres.2020.113462
13. Cheng C, Lau Y. Social media addiction during COVID-19-mandated physical distancing: relatedness needs as motives. Int J Environ Res Public Health. (2022) 19:4621. doi: 10.3390/ijerph19084621
14. Ebrahimi OV, Hoffart A, Johnson SU. Viral mitigation and the COVID-19 pandemic: factors associated with adherence to social distancing protocols and hygienic behaviour. Psychol Health. (2021). doi: 10.1080/08870446.2021.1960987
15. Wang H, Cheng C. Role of COVID-19 anxiety and community risk factors on physical distancing practice. Behav Sci. (2022) 12:110. doi: 10.3390/bs12040110
16. Pargament K, Brant C. Religion and coping. In: H Koenig editor. Handbook of Religion and Mental Health. San Diego, CA: Academic Press (1998). p. 111–28.
17. Nairn R, Merluzzi T. The role of religious coping in adjustment to cancer. Psychooncology. (2003) 12:428–41.
18. Maciejewski P, Phelps A, Kacel E, Balboni T, Balboni M, Wright A, et al. Religious coping and behavioral disengagement: opposing influences on advance care planning and receipt of intensive care near death. Psychooncology. (2012) 21:714. doi: 10.1002/pon.1967
19. Ramirez S, Macêdo D, Sales P, Figueiredo S, Daher E, Araújo S, et al. The relationship between religious coping, psychological distress and quality of life in hemodialysis patients. J Psychosom Res. (2012) 72:129–35. doi: 10.1016/j.jpsychores.2011.11.012
20. Areba E, Duckett L, Robertson C, Savik K. Religious coping, symptoms of depression and anxiety, and well-being among somali college students. J Relig Health. (2018) 57:94–109. doi: 10.1007/s10943-017-0359-3
22. Pargament K, Koenig H, Perez L. The many methods of religious coping: development and initial validation of the RCOPE. J Clin Psychol. (2000) 56:519–43. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1
23. Bentzen J. In crisis, we pray: religiosity and the COVID-19 pandemic. J Econ Behav Organ. (2021) 192:541–83. doi: 10.1016/j.jebo.2021.10.014
24. Counted V, Pargament K, Bechara A, Joynt S, Cowden R. Hope and well-being in vulnerable contexts during the covid-19 pandemic: does religious coping matter? J Posit Psychol. (2020) 17:70–81. doi: 10.1080/17439760.2020.1832247
25. Pirutinsky S, Cherniak A, Rosmarin D. Covid-19, mental health, and religious coping among American Orthodox Jews. J Relig Health. (2020) 59:2288–2301. doi: 10.1007/s10943-020-01070-z
26. Bulisig J, Aruta J. Measurement and predictors of mental well-being in community samples in the Philippines during the COVID-19 crisis: does religious coping matter? Ment Health Relig Cult. (2022). doi: 10.1080/13674676.2022.2031939
27. Lucchetti G, Góes L, Amaral S, Ganadjian G, Andrade I, Almeida P, et al. Spirituality, religiosity and the mental health consequences of social isolation during Covid-19 pandemic. Int J Soc Psychiatry. (2020) 67:672–9. doi: 10.1177/0020764020970996
28. Che Rahimi A, Bakar R, Mohd Yasin M. Psychological well-being of Malaysian university students during COVID-19 pandemic: do religiosity and religious coping matter? Healthcare. (2021) 9:1535. doi: 10.3390/healthcare9111535
29. Yıldırım M, Kızılgeçit M, Seçer I, Karabulut F, Angın Y, Dağcı A, et al. Meaning in life, religious coping, and loneliness during the coronavirus health crisis in Turkey. J Relig Health. (2021) 60:2371–85.
30. Yıldırım M, Arslan G, Alkahtani A. Do fear of COVID-19 and religious coping predict depression, anxiety, and stress among the Arab population during health crisis? Death Stud. (2021) 46:2070–6. doi: 10.1080/07481187.2021.1882617
31. del Castillo F, del Castillo C, Corpuz J. Dungaw: re-imagined religious expression in response to the COVID-19 pandemic. J Relig Health. (2021) 60:2285–305. doi: 10.1007/s10943-021-01266-x
32. Dutra C, Rocha H. Religious support as a contribution to face the effects of social isolation in mental health during the pandemic of COVID-19. J Relig Health. (2021) 60:99–111. doi: 10.1007/s10943-020-01140-2
33. Dobrakowski P, Skalski S, Surzykiewicz J, Muszyńska J, Konaszewski K. Religious coping and life satisfaction during the COVID-19 pandemic among polish Catholics. The mediating effect of coronavirus anxiety. J Clin Med. (2021) 10:4865. doi: 10.3390/jcm10214865
34. Fekih-Romdhane F, Cheour M. Psychological distress among a Tunisian community sample during the COVID-19 pandemic: correlations with religious coping. J Relig Health. (2021) 60:1446–61. doi: 10.1007/s10943-021-01230-9
35. Zarrouq B, Abbas N, Hilaly J, Asri A, Abbouyi S, Omari M, et al. An investigation of the association between religious coping, fatigue, anxiety and depressive symptoms during the COVID-19 pandemic in Morocco: a web-based cross-sectional survey. BMC Psychiatry. (2021) 21:264. doi: 10.1186/s12888-021-03271-6
36. Özer Z, Aksoy M, Turan G. The relationship between death anxiety and religious coping styles in patients diagnosed with COVID-19: a sample in the east of Turkey. J Death Dying. (2021). doi: 10.1177/00302228211065256
37. Cowden R, Rueger S, Davis E, Counted V, Kent B, Chen Y, et al. Resource loss, positive religious coping, and suffering during the COVID-19 pandemic: a prospective cohort study of US adults with chronic illness. Ment Health Relig Cult. (2022) 25:288–304.
38. Borenstein M, Hedges L, Higgins J, Rothstein H. Introduction to Meta-Analysis. Hoboken, NJ: John Wiley and Sons (2009).
39. Cooper H, Hedges L, Valentine J. The Handbook of Research Synthesis and Meta-Analysis. 3rd ed. New York, NY: Russell Sage Foundation (2019).
40. Carver C, Scheier M, Weintraub J. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. (1989) 56:267–83.
42. Folkman S, Lazarus R. Manual of the Ways of Coping Questionnaire. Palo Alto, CA: Mind Garden (1988).
43. Hebert R, Zdaniuk B, Schulz R, Scheier M. Positive and negative religious coping and well-being in women with breast cancer. J Palliat Med. (2009) 12:537–45.
44. Tobin S. Personhood in Advanced Old Age: Implications for Practice. New York, NY: Springer (1991).
45. DeRossett T, LaVoie D, Brooks D. Religious coping amidst a pandemic: impact on covid-19-related anxiety. J Relig Health. (2021) 60:3161–76. doi: 10.1007/s10943-021-01385-5
46. Kızılgeçit M, Yıldırım M. Fear of COVID-19, death depression and death anxiety: religious coping as a mediator. Arch Psychol Relig. (2022). doi: 10.1177/00846724221133455
47. Amadi K, Uwakwe R, Ndukuba A, Odinka P, Igwe M, Obayi N, et al. Relationship between religiosity, religious coping and socio-demographic variables among out-patients with depression or diabetes mellitus in Enugu, Nigeria. Afr Health Sci. (2016) 16:497–506.
48. Moreira-Almeida A, Pinsky I, Zaleski M, Laranjeira R. Envolvimento religioso e fatores sociodemográficos: resultados de um levantamento nacional no Brasil. Arch Psychiatry Psychother. (2010) 37:12–5.
49. Kraus M, Schäfer A, Csef H, Scheurlen M, Faller H. Emotional state, coping styles, and somatic variables in patients with chronic hepatitis C. Psychosomatics. (2000) 41:377–84. doi: 10.1176/appi.psy.41.5.377
50. Abernethy A, Chang H, Seidlitz L, Evinger J, Duberstein P. Religious coping and depression among spouses of people with lung cancer. Psychosomatics. (2002) 43:456–63. doi: 10.1176/appi.psy.43.6.456
51. Masha’al D, Shahrour G, Aldalaykeh M. Anxiety and coping strategies among nursing students returning to university during the COVID-19 pandemic. Heliyon. (2022) 8:e08734.
52. Hvidtjørn D, Hjelmborg J, Skytthe A, Christensen K, Hvidt N. Religiousness and religious coping in a secular society: the gender perspective. J Relig Health. (2014) 53:1329–41. doi: 10.1007/s10943-013-9724-z
53. Kadiroğlu T, Güdücü Tüfekci F, Kara A. Determining the religious coping styles of adolescents in Turkey during COVID-19. J Relig Health. (2021) 60:3406–17. doi: 10.1007/s10943-021-01410-7
54. Krejci M. Gender comparison of god schemas: a multidimensional scaling analysis. Int J Psychol Relig. (1998) 8:57–66.
55. Pew Research Center. The Changing Global Religious Landscape. Washington, DC: Pew Research Center (2017).
56. Australian Bureau of Statistics. Reflecting a Nation: Stories from the 2011 Census, 2012–2013 2012. (2022). Available online at: https://www.abs.gov.au/ausstats/abs@.nsf/lookup/2071.0main+features902012-2013 (accessed June 21, 2012).
58. Neo J. Religious minorities in Asia: between the scylla of minority protection and charybdis of religious freedom rights? Religions. (2021) 12:881.
59. Guo J, Hu X, Marsh H, Pekrun R. Relations of epistemic beliefs with motivation, achievement, and aspirations in science: generalizability across 72 societies. J Educ Psychol. (2022) 114:734–51.
60. Mathur A. Measurement and meaning of religiosity: a cross-cultural comparison of religiosity and charitable giving. J Target Meas Anal Mark. (2012) 20:84–95.
61. Mathur A, Barak B, Zhang Y, Lee K, Yoo B, Ha J. Social religiosity: concept and measurement across divergent cultures. Asia Pacific J Mark Logist. (2022) 27:717–34.
62. Cheng C, Cheung M, Montasem A, 44 members of the International Network of Well-Being Studies. Explaining differences in subjective well-being across 33 nations using multilevel models: universal personality, cultural relativity, and national income. J Pers. (2016) 84:46–58. doi: 10.1111/jopy.12136
63. Thomas H, Webster S, Petherick A, Phillips T, Kira B. Oxford COVID-19 Government Response Tracker. Oxford: Blavatnik School of Government (2020).
64. Page M, McKenzie J, Bossuyt P, Boutron I, Hoffmann T, Mulrow C, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 372:n71.
66. Hayes A, Krippendorff K. Answering the call for a standard reliability measure for coding data. Commun Methods Meas. (2007) 1:77–89.
67. Rosenthal R. Parametric measures of effect size. In: H Cooper, L Hedges editors. The Handbook of Research Synthesis. New York, NY: Russell Sage Foundation (1994). p. 231–44.
68. Lüdecke D. esc: Effect Size Computation for Meta Analysis (Version 0.5.1). (2022). Available online at: https://CRAN.R-project.org/package=esc (accessed December 04, 2019).
69. Gallup. GALLUP Worldview. (2022). Available online at: https://www.gallup.com/analytics/213617/gallup-analytics.aspx (accessed January 17, 2022).
70. NationMaster. Religion. (2022). Available online at: https://www.nationmaster.com/country-info/stats/Religion/Religions/All (accessed January 17, 2022).
71. OurWorldInData.org. Coronavirus Pandemic (COVID-19) – Statistics and Research. (2022). Available online at: https://ourworldindata.org/coronavirus (accessed August 18, 2022).
73. Higgins J, Thompson S. Quantifying heterogeneity in a meta-analysis. Stat Med. (2002) 21:1539–58.
75. Viechtbauer W, Cheung M. Outlier and influence diagnostics for meta-analysis. Res Synth Methods. (2010) 1:112–25.
76. Viechtbauer W. Conducting meta-analyses in R with the metafor package. J Stat Softw. (2010) 36:1–48.
78. Cheng C, Cheung M, Lo B. Relationship of health locus of control with specific health behaviours and global health appraisal: a meta-analysis and effects of moderators. Health Psychol Rev. (2016) 10:460–77. doi: 10.1080/17437199.2016.1219672
79. Cheng C, Wang H, Sigerson L, Chau C. Do socially rich get richer? A nuanced perspective on social network site use and online social capital accrual. Psychol Bull. (2019) 145:734–64. doi: 10.1037/bul0000198
80. Egger M, Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. (1997) 315:629–34.
81. Duval S. The trim and fill method. In: H Rothstein, A Sutton, M Borenstein editors. Publication Bias in Meta-Analysis. Chichester: John Wiley and Sons (2005). p. 127–44.
82. Simonsohn U, Nelson L, Simmons J. P-curve: a key to the file drawer. J Exp Psychol Gen. (2014) 143:534–47. doi: 10.1037/a0033242
83. Thomas J, Barbato M, Verlinden M, Gaspar C, Moussa M, Ghorayeb J, et al. Psychosocial correlates of depression and anxiety in the United Arab Emirates during the COVID-19 pandemic. Front Psychiatry. (2020) 11:564172. doi: 10.3389/fpsyt.2020.564172
84. Coiro M, Watson K, Ciriegio A, Jones M, Wolfson A, Reisman J, et al. Coping with COVID-19 stress: associations with depression and anxiety in a diverse sample of U.S. adults. Curr Psychol. (2022). doi: 10.1007/s12144-021-02444-6
85. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho C, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
86. Janati Idrissi A, Lamkaddem A, Benouajjit A, Ben El Bouaazzaoui M, El Houari F, Alami M, et al. Sleep quality and mental health in the context of COVID-19 pandemic and lockdown in Morocco. Sleep Med. (2020) 74:248–53. doi: 10.1016/j.sleep.2020.07.045
87. Das S, Punnoose V, Doval N, Nair V. Spirituality, religiousness and coping in patients with schizophrenia: a cross sectional study in a tertiary care hospital. Psychiatry Res. (2018) 265:238–43. doi: 10.1016/j.psychres.2018.04.030
88. Dolcos F, Hohl K, Hu Y, Dolcos S. Religiosity and resilience: cognitive reappraisal and coping self-efficacy mediate the link between religious coping and well-being. J Relig Health. (2021) 60:2892–905. doi: 10.1007/s10943-020-01160-y
89. Zhang Y, Holmes EC. A genomic perspective on the origin and emergence of SARS-CoV-2. Cell. (2020) 181:223–7.
90. Zeidler A, Karpinski T. SARS-CoV, MERS-CoV, SARS-CoV-2 comparison of three emerging Coronaviruses. Jundishapur J Microbiol. (2020) 13:e103744.
91. Prompetchara E, Ketloy C, Palaga T. Immune responses in COVID-19 and potential vaccines: lessons learned from SARS and MERS epidemic. Asian Pac J Allergy Immunol. (2020) 38:1–9. doi: 10.12932/AP-200220-0772
92. Jean S, Lee P, Hsueh P. Treatment options for COVID-19: the reality and challenges. J Microbiol Immunol Infect. (2020) 53:436–43.
93. Brailovskaia J, Margraf J. The relationship between burden caused by coronavirus (Covid-19), addictive social media use, sense of control and anxiety. Comput Hum Behav. (2021) 119:106720. doi: 10.1016/j.chb.2021.106720
94. van Mulukom V, Muzzulini B, Rutjens B, van Lissa C, Farias M. The psychological impact of threat and lockdowns during the COVID-19 pandemic: exacerbating factors and mitigating actions. Transl Behav Med. (2021) 11:1318–29. doi: 10.1093/tbm/ibab072
95. Wu B. Social isolation and loneliness among older adults in the context of COVID-19: a global challenge. Health Res Policy Syst. (2020) 5:27.
96. Ying W, Cheng C. Public emotional and coping responses to the COVID-19 infodemic: a review and recommendations. Front Psychiatry. (2021) 2319:755938. doi: 10.3389/fpsyt.2021.755938
97. Cheng C, Wang H, Ebrahimi O. Adjustment to a “new normal:” coping flexibility and mental health issues during the COVID-19 pandemic. Front Psychiatry. (2021) 12:626197. doi: 10.3389/fpsyt.2021.626197
98. Ruck D, Bentley R, Lawson D. Religious change preceded economic change in the 20th century. Sci Adv. (2018) 4:eaar8680.
99. Cheng C, Wang F, Golden D. Unpacking cultural differences in interpersonal flexibility: role of culture-related personality and situational factors. J Cross Cult Psychol. (2011) 42:425–44.
100. Cheng C, Lau H, Chan M. Coping flexibility and psychological adjustment to stressful life changes: a meta-analytic review. Psychol Bull. (2014) 140:1582–607. doi: 10.1037/a0037913
101. Cheng C, Chau C. Gamification-based intervention for enhancing team effectiveness and coping flexibility: randomized controlled trial. Front Psychiatry. (2022) 13:941252. doi: 10.3389/fpsyt.2022.941252
102. Cabatbat K, Camarines T. Self-actualization through religious coping is needed in the time of COVID-19 pandemic. J Public Health. (2022) 44:e335. doi: 10.1093/pubmed/fdab243
103. Cheng C, Cheung M. Psychological responses to outbreak of severe acute respiratory syndrome: a prospective, multiple time-point study. J Pers. (2005) 73:261–85. doi: 10.1111/j.1467-6494.2004.00310.x
104. Agha S. Mental well-being and association of the four factors coping structure model: a perspective of people living in lockdown during COVID-19. Ethics Med Public Health. (2021) 16:100605. doi: 10.1016/j.jemep.2020.100605
105. Bakır N, Irmak Vural P, Demir C. Relationship of depression, anxiety and stress levels with religious coping strategies among Turkish pregnant women during the covid-19 pandemic. J Relig Health. (2021) 60:3379–93. doi: 10.1007/s10943-021-01391-7
106. Barbato M. Positive religious coping and mental health among christians and muslims in response to the covid-19 pandemic. Religions. (2020) 11:498. doi: 10.3390/rel11100498
107. Beato A, da Costa L, Nogueira R. “everything is Gonna be alright with me”: the role of self-compassion, affect, and coping in negative emotional symptoms during coronavirus quarantine. Int J Environ Res Public Health. (2021) 18:2017. doi: 10.3390/ijerph18042017
108. Besirli A, Erden S, Atilgan M, Varlihan A, Habaci M, Yeniceri T, et al. The relationship between anxiety and depression levels with perceived stress and coping strategies in health care workers during the COVID-19 pandemic. Sisli Etfal Hastan Tip Bul. (2021) 55:1–11. doi: 10.14744/SEMB.2020.57259
109. Blackwell R. Coping and Covid-19 Ph.D. thesis. Ann Arbor, MI: Southeastern Louisiana University (2021).
110. Chodkiewicz J, Miniszewska J, Krajewska E, Biliński P. Mental health during the second wave of the COVID-19 pandemic—polish studies. Int J Environ Res Public Health. (2021) 18:3423. doi: 10.3390/ijerph18073423
111. Chow S, Francis B, Ng Y, Naim N, Beh H, Ariffin M, et al. Religious coping, depression and anxiety among healthcare workers during the COVID-19 pandemic: a malaysian perspective. Healthcare (Basel). (2021) 9:79. doi: 10.3390/healthcare9010079
112. Davis E, McElroy-Heltzel S, Lemke A, Cowden R, VanderWeele T, Worthington E Jr, et al. Psychological and spiritual outcomes during the COVID-19 pandemic: a prospective longitudinal study of adults with chronic disease. Health Psychol. (2021) 40:347. doi: 10.1037/hea0001079
113. Fallahi C, Blau J, Mitchell M, Rodrigues H, Daigle C, Heinze A, et al. Understanding the pandemic experience for people with a preexisting mental health disorder. Traumatology. (2021) 27:471–8. doi: 10.1037/trm0000344
114. Fteropoulli T, Kalavana T, Yiallourou A, Karaiskakis M, Koliou Mazeri M, Vryonides S, et al. Beyond the physical risk: psychosocial impact and coping in healthcare professionals during the covid-19 pandemic. J Clin Nurs. (2022). doi: 10.1111/jocn.15938 [Epub ahead of print].
115. Gökmen A, Toprak Y, Said S. A coping model for the fear of COVID-19 in the context of coping and psychological resilience. FSM Ýlmî Araştırmalar İnsan ve Toplum Bilimleri Dergisi. (2022):513–66.
116. Gurvich C, Thomas N, Hx T, Abdul-Rahman H, Sood L, Fabiatos K, et al. Coping styles and mental health in response to societal changes during the COVID-19 pandemic. Int J Soc Psychiatry. (2021) 67:540–9. doi: 10.1177/0020764020961790
117. Hayes B, Apputhurai P, Mikocka-Walus A, Barreiro-de Acosta M, Bernstein C, Burgell R, et al. Extending the common sense model to explore the impact of the fear of covid-19 on quality of life in an international inflammatory bowel disease cohort. J Clin Psychol Med Settings. (2022). doi: 10.1007/s10880-021-09823-y
118. Lee S. Coronavirus anxiety scale: a brief mental health screener for COVID-19 related anxiety. Death Stud. (2020) 44:393–401. doi: 10.1080/07481187.2020.1748481
119. Lee S, Mathis A, Jobe M, Pappalardo E. Clinically significant fear and anxiety of COVID-19: a psychometric examination of the coronavirus anxiety scale. Psychiatry Res. (2020) 290:7. doi: 10.1016/j.psychres.2020.113112
120. Mahamid F, Bdier D. The association between positive religious coping, perceived stress, and depressive symptoms during the spread of coronavirus (covid-19) among a sample of adults in Palestine: across sectional study. J Relig Health. (2021) 60:34–49. doi: 10.1007/s10943-020-01121-5
121. Mahmood Q, Jafree S, Sohail M, Akram MB. A cross-sectional survey of Pakistani Muslims coping with health anxiety through religiosity during the covid-19 pandemic. J Relig Health. (2021) 60:1462–74. doi: 10.1007/s10943-021-01218-5
122. Margetić B, Peraica T, Stojanović K, Ivanec D. Predictors of emotional distress during the COVID-19 pandemic; a croatian study. Pers Individ Differ. (2021) 175:1. doi: 10.1016/j.paid.2021.110691
123. Mirhosseini S, Nouhi S, Janbozorgi M, Mohajer H, Naseryfadafan M. The role of spiritual health and religious coping in predicting death anxiety among patients with coronavirus. Stud Islam Psychol. (2020) 14:29–42. doi: 10.30471/psy.2020.6545.1701
124. Mishra J, Samanta P, Panigrahi A, Dash K, Behera M, Das R. Mental health status, coping strategies during covid-19 pandemic among undergraduate students of healthcare profession. Int J Environ Res Public Health. (2022). doi: 10.1007/s11469-021-00611-1 [Epub ahead of print].
125. Ouanes S, Kumar R, Doleh E, Smida M, Al-Kaabi A, Al-Shahrani A, et al. Mental health, resilience, and religiosity in the elderly under COVID-19 quarantine in Qatar. Arch Gerontol Geriatr. (2021) 96:104457. doi: 10.1016/j.archger.2021.104457
126. Pačić-Turk L, Ćepulić D, Haramina A, Bošnjaković J. Povezanost različitih psiholoških čimbenika s izraženosti stresa, anksioznosti i depresivnosti u zdravstvenih djelatnika tijekom pandemije bolesti COVID-19 u republici hrvatskoj. Suvremena Psihologija. (2020) 23:35–53.
127. Prazeres F, Passos L, Simões J, Simões P, Martins C, Teixeira A. COVID-19-related fear and anxiety: spiritual-religious coping in healthcare workers in portugal. Int J Environ Res Public Health. (2020) 18:220. doi: 10.3390/ijerph18010220
128. Quiroga-Garza A, Cepeda-Lopez A, Villarreal Zambrano S, Villalobos-Daniel V, Carreno D, Eisenbeck N. How having a clear why can help us cope with almost anything: meaningful well-being and the COVID-19 pandemic in México. Front Psychol. (2021) 12:648069. doi: 10.3389/fpsyg.2021.648069
129. Rababa M, Hayajneh A, Bani-Iss W. Association of death anxiety with spiritual well-being and religious coping in older adults during the covid-19 pandemic. J Relig Health. (2022). doi: 10.1007/s10943-020-01129-x
130. Salazar A, Palomo-Osuna J, de Sola H, Moral-Munoz J, Dueñas M, Failde I. Psychological impact of the lockdown due to the COVID-19 pandemic in university workers: factors related to stress, anxiety, and depression. Int J Environ Res Public Health. (2021) 18:4367. doi: 10.3390/ijerph18084367
131. Shousha H, Madbouly N, Afify S, Asem N, Fouad E, Maher R, et al. Anxiety, depression and coping strategies among chronic medical patients with coronavirus disease-2019: a multicenter follow-up cohort study. J Ment Health. (2022):1–9. doi: 10.1080/09638237.2021.1979491
132. Singh J, Sood M, Chadda R, Singh V, Kattula D. Mental health issues and coping among health care workers during COVID19 pandemic: Indian perspective. Asian J Psychiatr. (2021) 61:102685. doi: 10.1016/j.ajp.2021.102685
133. Skapinakis P, Bellos S, Oikonomou A, Dimitriadis G, Gkikas P, Perdikari E, et al. Depression and its relationship with coping strategies and illness perceptions during the COVID-19 lockdown in Greece: a cross-sectional survey of the population. Depress Res Treat. (2020) 2020:11. doi: 10.1155/2020/3158954
134. Smida M, Khoodoruth MAS, Al-Nuaimi SK, Al-Salihy Z, Ghaffar A, Khoodoruth WNC, et al. Coping strategies, optimism, and resilience factors associated with mental health outcomes among medical residents exposed to coronavirus disease 2019 in Qatar. Brain Behav. (2021) 11:e2320. doi: 10.1002/brb3.2320
135. Uvais N, Nalakath M, Shihabudheen P, Hafi N, Salman C. Depression, anxiety, and coping during the covid-19 pandemic among Indian expats in the Middle East: a survey study. Prim Care Companion CNS Disord. (2021) 23:20m02761. doi: 10.4088/PCC.20m02761
136. Van Steenkiste E, Schoofs J, Gilis S, Messiaen P. Mental health impact of COVID-19 in frontline healthcare workers in a Belgian Tertiary care hospital: a prospective longitudinal study. Acta Clin Belg. (2022):1–8. doi: 10.1080/17843286.2021.1903660
137. Vitorino L, Júnior G, Gonzaga G, Dias I, Ribeiro I, Pereira J, et al. Impact of Social Isolation Strategies Due to COVID-19 on Mental Health and Quality of Life in Brazil. (2022). Available online at: https://ssrn.com/abstract=3666238.
138. Vitorino L, Yoshinari Júnior G, Gonzaga G, Dias I, Pereira J, Ribeiro I, et al. Factors associated with mental health and quality of life during the COVID-19 pandemic in Brazil. BJPsych Open. (2021) 7:1. doi: 10.1192/bjo.2021.62
139. Yee A, Hodori N, Tung Y, Ooi P, Latif S, Isa H, et al. Depression level and coping responses toward the movement control order and its impact on quality of life in the Malaysian community during the COVID-19 pandemic: a web-based cross-sectional study. Ann Gen Psychiatry. (2021) 20:31. doi: 10.1186/s12991-021-00352-4
Keywords: coping, stress, anxiety, mental health, public health, epidemic, depression, coronavirus (COVID-19)
Citation: Cheng C and Ying W (2023) A meta-analytic review of the associations between dimensions of religious coping and psychological symptoms during the first wave of the COVID-19 pandemic. Front. Psychiatry 14:1097598. doi: 10.3389/fpsyt.2023.1097598
Received: 14 November 2022; Accepted: 04 January 2023;
Published: 19 January 2023.
Edited by:
Murat Yildirim, Ağrı İbrahim Çeçen University, TürkiyeReviewed by:
Roberto Ariel Abeldaño Zuñiga, University of the South Sierra, MexicoPriya Alat, Indian Institute of Management Shillong, India
Copyright © 2023 Cheng and Ying. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cecilia Cheng,  Y2VjaS1jaGVuZ0Boa3UuaGs=
Y2VjaS1jaGVuZ0Boa3UuaGs=
 Cecilia Cheng
Cecilia Cheng Weijun Ying
Weijun Ying